Abstract
Study Design
Retrospective Case Series.
Objective
This study aims to evaluate readmission rates, risk factors, and reason for unplanned 30-day readmissions after thoracolumbar spine trauma surgery.
Methods
A retrospective chart review was conducted for patients undergoing operative treatment for thoracic or lumbar trauma with open or minimally invasive surgical approach at a Level 1 urban trauma center. Patients were divided into two groups based on 30-day readmission status. Reason for readmission, reoperation rates, injury type, trauma severity, and incidence of polytrauma were compared between the two groups.
Results
A total of 312 patients, 69.9% male with an average age of 47 ± 19 years were included. The readmitted group included 16 patients (5.1%) of which 9 (56%) were readmitted for medical complications and 7 for surgical complications. Wound complications (31.3% of readmissions) were the most common cause of readmission, followed by non-wound related sepsis (18.9% of readmissions). A total of 6 patients (37.5%) required reoperation; 2 instrumentation failures underwent revision surgery, and 4 wound complications underwent irrigation and debridement. Patients with higher Injury Severity Scale (ISS) were more likely to be readmitted (27.8% vs 22.1%, P = .045). Concomitant lower limb surgery increased odds of readmission (OR, 4.40; 95% CI, 1.10–17.83; P = .037).
Conclusion
Spine trauma 30-day readmission rate was 5.1%, comparable to those reported in the elective spine surgery literature. Readmitted patients were more likely to sustain concomitant operative lower limb trauma. Wound complications were the most common cause of readmission, and almost half of the patients were readmitted due to surgery-related complications.
Keywords: thoracic trauma, thoracolumbar trauma, 30-day readmission, spinal fractures, spinal trauma
Introduction
Healthcare in the United States is shifting toward value-based models to reduce costs and improve overall care. All-cause 30-day readmissions represent a significant proportion of the Centers for Medicare & Medicaid Services (CMS) healthcare expenditures and have become a target for cost reduction. 1 Preventable readmissions cost Medicare up to approximately $12 billion a year.1,2 The Centers for Medicare & Medicaid Services Hospital Readmissions Reduction Program (CMS-HRRP) implemented repayment penalties for hospitals with high 30-day readmissions to contain these costs. 3 The CMS-HRRP does not include spine surgery; however, unplanned 30-day readmissions after elective spine surgery have been thoroughly studied.2,4-6 In elective spine surgery, total 30-day readmission rates range from 2.6 to 14.2%. Age, comorbidities, and public insurance status have emerged as readmission risk factors; however, these rates can vary widely.2,6-8 High-quality granular data are need to stratify readmissions attributable to physician-dependent practice patterns and physician-independent factors to guide policy change.9-11
Compared to the elective spine population, the trauma population encompasses more unpredictable clinical presentations and may require immediate intervention. 12 Due to the greater complexity and acuity in the trauma population, we seek to examine unplanned 30-day readmission rates after surgical thoracolumbar spine trauma. We hypothesize that patients with multiple comorbidities, higher Injury Severity Score (ISS), and American Society of Anesthesiologist (ASA) scores will be associated with an increased rate of unplanned 30-day readmission.
Methods
Study Population
A billings database was queried for operative thoracolumbar trauma cases from January 1, 2012 to December 31, 2017 at an urban Level 1 tertiary trauma center. Patients who underwent operative treatment for upper thoracic (T1-T5), lower thoracic (T6-T10), thoracolumbar (T11-L2), and lumbar (L3-L5) trauma either through traditional open or minimally invasive surgical approach were included in the study. Patients undergoing surgery for other indications including degenerative conditions, infection, and pathologic fractures were excluded. Patients with previous spine surgery, chronic fractures, and those who required operative treatment after more than 6 weeks of failed non-operative treatment were also excluded. Patients were divided into two groups based on the occurrence of an unplanned 30-day readmission. Institutional Review Board (IRB) approval was obtained by the University of Maryland IRB (Protocol: HP-00082698). This study was conducted in accordance with the 1964 Helsinki Declaration, its amendments, and other equivalent ethical standards.
Outcomes Measure
Readmission data were obtained using the clinical quality database MIDAS+ DataVision (Conduent Inc., Florham Park, New Jersey) utilized at our institution in combination with local trauma databases and data from 11 acute care hospitals across the state. Readmissions were classified as an inpatient admission at our healthcare institutions or affiliated hospitals within 30-days of discharge from the index admission. All-cause and all-payer readmission encounters were included with the exception of (1) elective or planned readmissions, (2) admissions for rehabilitation services, or (3) admissions for delivery of a newborn. Readmissions for rehabilitation, psychiatric, and non-acute care centers were excluded. For each readmission, the medical records were reviewed to determine the reason for readmission and if a revision procedure was performed. Readmissions were broadly classified into the following: medical or surgical complications. Medical complications included all non-operative management and non-spine related readmissions. Surgical complications included wound complications (dehiscence or infection) and instrumentation failure.
Data Collection
A retrospective chart review was performed by two researchers blinded to outcome results. Patient demographic information collected included the following: age, gender, BMI, and discharged facility. Insurance payor information, in-patient length of stay, and intensive care unit (ICU) length of stay were recorded from billing’s database. ASA score, Charlson Comorbidity Index (CCI), fracture level, and fracture morphology were also collected from medical record chart review. ISS scores, Glasgow coma scale (GSC), neurological status at admission, and polytraumatic status were obtained from institutional trauma database. Operations for non-spine related trauma (head, neck, abdominal, or extremity surgery) were obtained from the medical records and confirmed with an electronic billings database query. The same process was done for mechanical ventilator status during initial admission, although duration of ventilation could not be properly acquired through these methods. Medical and surgical complications during the index admission were recorded during initial data collection and were later confirmed by a third researcher via chart review and billing database queries. Index admission complications included the following: arrhythmia, bacteremia, deep venous thrombosis (DVT), fever, pulmonary embolism, pneumonia, septic shock, transfusion, urinary retention, urinary tract infection (UTI), wound infection, and wound dehiscence. Operative approach, surgical procedure, number of instrumentation levels, estimated blood loss (EBL), and surgery duration (from incision to closure) were obtained from intraoperative anesthesia record and surgeon’s operative note.
Statistical Analysis
Data were collected in Microsoft Excel (Microsoft Office Professional Plus, Microsoft Corporation, Redmond, WA). JMP® Pro (Version 13.0.0, SAS Institute Inc., Cary, NC) was used for statistical analysis. Significance threshold was set at P < .05. Continuous variables were tested for normality with the Shapiro–Wilk test. Unpaired t-tests were used for all normally distributed continuous variables, and Wilcoxon rank-sum test was used as the nonparametric variables. Nominal variables were compared using chi-square analysis or Fisher’s exact test. Logistic multivariate regression analysis was conducted including the variables identified in the univariate analysis.
Results
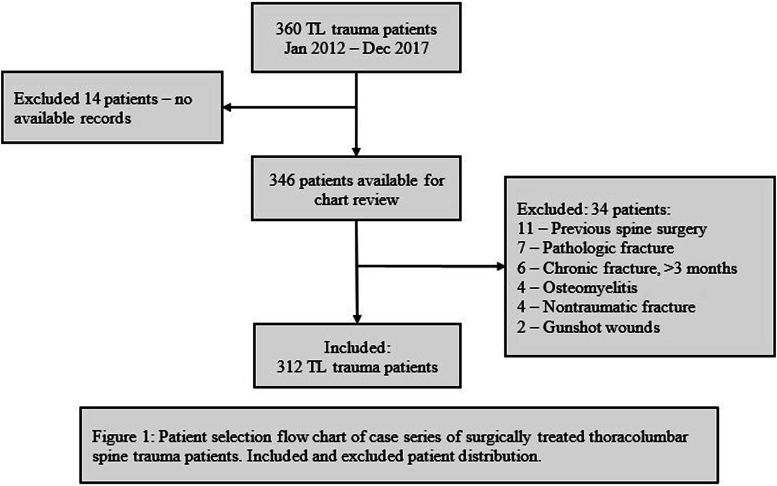
A total of 360 patients undergoing operative treatment for thoracolumbar spine trauma met the study inclusion criteria. Fourteen patients without available records and 34 patients who met exclusion criteria were excluded resulting in a study population of 312 patients (Figure 1). A total of 16 patients were readmitted, resulting in a 5.1% rate of unplanned 30-day readmission. The remaining 296 patients composed the non-readmitted group. The majority of patients in both groups were male (75.0% in the readmitted group vs 69.6% in the non-admitted group, P = .78). Patients in the readmitted group were older, 52.8 ± 24.7 years (vs 46.3 ± 19.1 years, P = .23). However, there were no statistically significant differences in age, sex, BMI, insurance status, and mechanisms of injury between the groups (Table 1).
Figure 1.
Patient selection flow chart of case series of surgically treated thoracolumbar spine trauma patients. Included and excluded patient distribution.
Table 1.
Demographic Characteristics Between Readmitted and Non-Readmitted Thoracolumbar Spine Trauma Patients.
| Readmitted | Non-readmitted | P-value | |
|---|---|---|---|
| Patients, n (%) | 16 (5.1) | 296 (94.9) | — |
| Age (years), mean ± SD | 52.8 ± 24.7 | 46.3 ± 19.1 | .23 |
| Sex (males) | 12 (75) | 206 (69.6) | .78 |
| BMI (kg/m2) | 28.6 ± 4.5 | 28.5 ± 7.9 | .38 |
| Insurance | |||
| Private insurance | 8 (50) | 119 (40.2) | .67 |
| Medicaid | 4 (25) | 73 (24.7) | |
| Medicare | 2 (12.5) | 61 (20.6) | |
| No insurance | — | 20 (6.8) | |
| Other | 2 (12.5) | 23 (7.8) | |
| Mechanism of injury | |||
| Motor vehicle crash | 9 (56.3) | 139 (50) | .26 |
| Fall | 5 (31.3) | 131 (44.3) | |
| Pedestrian struck | 2 (12.5) | 12 (4.1) | |
| Other | — | 14 (4.7) |
BMI, body mass index.
The readmitted group had a significantly higher ISS (27.8 ± 10.4 vs 22.1 ± 12.5, P = .045) and rates of concomitant non-spine operative trauma (62.5 vs32.8%, P = .027) compared to the non-readmitted group (Table 2). In the readmitted group, 37.5% required operation for concomitant lower limb trauma vs 7.8% in the non-readmitted group (P = .0016). Patients in the readmitted group had a 7.1 times greater odds of sustaining operative lower limb trauma compared to those in the non-readmitted group (OR: 7.1; 95% CI, 2.3–22.3, P = .0014). CCI, ASA score, GSC, neurological status at admission, and polytraumatic status were similar between the groups.
Table 2.
Patient Trauma Characteristics Between Readmitted and Non-Readmitted Thoracolumbar Spine Trauma Patients.
| Readmitted | Non-readmitted | P-value | |
|---|---|---|---|
| Patients, n (%) | 16 (5.1) | 296 (94.9) | — |
| ISS, mean ± SD | 27.8 ± 10.4 | 22.1 ± 12.5 | .045* |
| CCI | .44 ± .81 | .64 ± 1.2 | .87 |
| GSC ≥14 | 9 (69.2) | 209 (80.1) | .31 |
| ASA ≥3 | 11 (68.8) | 150 (55.8) | .44 |
| LOC | 2 (12.5) | 95 (32.1) | .16 |
| Pulmonary injury | 5 (31.3) | 110 (37.2) | .79 |
| Mechanical ventilation at arrival | 5 (31.3) | 47 (15.9) | .16 |
| Neurological status | |||
| Intact | 6 (40) | 141 (49.1) | .57 |
| Incomplete | 5 (33.3) | 88 (30.7) | |
| Complete | 4 (26.7) | 58 (20.1) | |
| Polytrauma | 14 (87.5) | 233 (78.8) | .54 |
| Abdominal | 5 (31.3) | 68 (23.7) | .55 |
| Chest | 7 (43.8) | 161 (56.1) | .44 |
| Extremity and pelvis | 8 (50) | 105 (36.6) | .30 |
| Face | 1 (6.3) | 30 (10.5) | 1 |
| Head | 4 (25) | 54 (18.8) | .52 |
| Neck | 3 (18.8) | 32 (11.1) | .41 |
| Non-spine surgery | 10 (62.5) | 97 (32.8) | .027* |
| Abdominal | 2 (12.5) | 29 (9.8) | .67 |
| Upper limb | 2 (12.5) | 21 (7.1) | .33 |
| Lower limb ‡ | 6 (37.5) | 23 (7.8) | .00216* |
| Head and neck | 3 (18.8) | 10 (3.4) | .023* |
Patients with lower limb surgery had a 7-fold increased risk of being readmitted (OR, 7.1; 95% CI, 2.3–22.3, P = 0.001 4).
*indicates a statistically significant value P < 0.05.
ISS, Injury Severity Score; CCI, Charlson Comorbidity Index; LOC, loss of consciousness; GSC, Glasgow coma scale; ASA, American Society of Anesthesiologist score.
The most common spinal fracture level was the thoracolumbar spine, and the most common fracture morphology was burst/compression fractures in both groups. There was no statistically significant difference in spinal level (P = .36), fracture morphology (P = .78), surgical technique (P = 1.0), surgical approach (P = .86), number of instrumented levels (P = .55), surgery duration (P = .81), EBL (P = .64), and intraoperative packed red blood cell (PRBC) transfusion (P = .72) between the groups (Table 3).
Table 3.
Fracture Characteristics and Operative Details Between Readmitted and Non-Readmitted Thoracolumbar Spine Trauma Patients.
| Readmitted | Non-readmitted | P-value | |
|---|---|---|---|
| Patients, n (%) | 16 (5.1) | 296 (94.9) | — |
| Spinal level | |||
| Upper thoracic (T1-T5) | 1 (6.3) | 52 (17.6) | .36 |
| Lower thoracic (T6-T10) | 5 (31.3) | 84 (28.4) | |
| TL (T11-L2) | 7 (43.8) | 136 (46) | |
| Lumbar (L3-L5) | 3 (18.8) | 24 (8.1) | |
| Fracture morphology | |||
| Burst/compression | 5 (31.3) | 132 (44.6) | .78 |
| Fracture dislocation | 3 (18.8) | 47 (15.9) | |
| Flexion-distraction | 4 (25) | 44 (14.9) | |
| Extension-distraction | 2 (12.5) | 28 (9.5) | |
| Combination | 2 (12.5) | 28 (9.5) | |
| Surgical technique | |||
| Open | 10 (62.5) | 191 (64.5) | 1 |
| Percutaneous | 6 (37.5) | 105 (35.5) | |
| Surgical approach | |||
| Posterior | 15 (93.8) | 275 (92.9) | .86 |
| Anterior | 1 (6.3) | 16 (5.4) | |
| Combined | — | 5 (1.7) | |
| Surgical details | |||
| Instrumented spinal segments, mean ± SD | 3.7 ± 1.6 | 3.8 ± 1.5 | .55 |
| Length of surgery (minutes) | 189 ± 125 | 188 ± 121 | .81 |
| EBL (mL) | 806 ± 1235 | 660 ± 764 | .64 |
| Intraoperative PRBC transfusion | 6 (37.5) | 106 (36.2) | 1 |
| Units of PRBC | 1.9 ± 3.4 | 1.1 ± 2.1 | .72 |
TL, thoracolumbar; EBL, estimated blood loss; PRBC, packed red blood cells.
Postoperative in-hospital variables and complication rates were similar between the groups (Table 4). The readmitted group had a shorter length of stay (12.9 ± 11.6 days vs 14.7 ± 16.1 days, P = .87), more patients discharged to a subacute rehabilitation facility (93.8 vs 67.9%, P = .33), and higher rates of in-hospital postoperative arrhythmia (18.8 vs 16.2%, P = .056). However, these differences did not reach statistical significance. There was no difference in complications during the index admission between patient groups.
Table 4.
Postoperative Course and Complications During Hospital Stay between Readmitted and Non-readmitted patients.
| Readmitted | Non-readmitted | P-value | |
|---|---|---|---|
| Patients, n (%) | 16 (5.1) | 296 (94.9) | — |
| LOS (days), mean ± SD | 12.9 ± 11.6 | 14.7 ± 16.1 | .87 |
| Discharge to rehab facility | 15 (93.8) | 203 (67.9) | .33 |
| Complications during hospital stay | |||
| Arrhythmia | 4 (25) | 26 (8.8) | .056 |
| Bacteremia | 3 (18.8) | 48 (16.2) | .73 |
| DVT | 2 (12.5) | 12 (4.1) | .16 |
| Fever | 2 (12.5) | 41 (13.9) | 1 |
| Pulmonary embolism | 0 | 36 (12.2) | .23 |
| Pneumonia | 0 | 24 (8.1) | .62 |
| Septic shock | 0 | 11 (3.7) | 1 |
| Transfusion | 3 (18.8) | 46 (15.5) | .72 |
| Urinary retention | 0 | 52 (17.6) | .08 |
| UTI | 3 (18.8) | 42 (14.2) | .71 |
| Wound infection | 0 | 16 (5.4) | 1 |
| Wound dehiscence | 0 | 3 (1) | 1 |
*indicates a statistically significant P-value <0.05.
EBL, estimated blood loss; UTI, urinary tract infection; DVT, deep venous thrombosis.
The average days to readmission were 12.8 ± 7.6 days after initial discharge. In the readmission group, 37.5% required reoperation. Of all readmissions, medical complications accounted for 56.3% and surgical complications accounted for 43.7%. Table 5 details both complication class and subtype resulting in readmissions; the most common reason was wound complications, responsible for 31.3% of readmissions. All 5 patients readmitted for wound complications were related to their spinal fusion incision. All of the 6 patients requiring reoperation were due to surgery-related complications. Four patients developed wound complications requiring irrigation and debridement of their spinal fusion incision. Two patients required revision surgery for instrumentation failure. One instrumentation failure of a sacroiliac screw resulted in pseudarthrosis, requiring extension of the proximal fusion and lumbopelvic fixation. The other, a proximal screw pull-out following short-segment fixation, resulted in dislocation and loss of reduction, requiring a revision T8-L2 fusion. An in-depth description of the 16 readmitted cases is included in Table 6.
Table 5.
Summary of Characteristics in Unplanned 30-Day Readmitted Thoracolumbar Spine Trauma Patients.
| Total patients | 312 |
| Readmitted Patients, n (%) | 16 (5.1) |
| Reoperations, n ( % total readmitted, % total patients ) | 6 (37.5, 1.9) |
| Days to readmission, mean ± std. dev | 12.8 ± 7.6 |
| Causes of readmission, n ( % total readmitted, % total patients ) | |
| Medical complications | 9 (56.3, 2.9) |
| Sepsis | 3 (18.9, .96) |
| Anemia | 2 (12.5, .64) |
| Stroke | 1 (6.3, .3) |
| Respiratory distress | 1 (6.3, .3) |
| Ileus | 1 (6.3, .3) |
| Lumbar muscle strain | 1 (6.3, .3) |
| Surgical complications | 7 (43.7, 2.2) |
| Wound complications | 5 (31.3, 1.6) |
| Wound infection | 3 (18.9, .96) |
| Wound dehiscence | 2 (12.5, .64) |
| Instrumentation failure | 2 (12.5, .64) |
Table 6.
Reasons for Readmission and Description of Initial Trauma and Polytraumatic Status for Patients with Unplanned 30-Day Readmission in Thoracolumbar Spine Trauma Patients.
| Age/Sex | LOS | Days to Re-admin | Classification of readmission–Reason for readmission/reoperation | Initial diagnosis/index spine procedure | Polytraumatic?/other surgery during index stay |
|---|---|---|---|---|---|
| 16 M | 7 | 10 | Medical–sepsis, UTI | T7-T8 burst + fracture dislocation/open T5–T10 PSF | Yes |
| 73 M | 20 | 8 | Medical–sepsis, gastrostomy | T7-T8 extension-distraction/MIS T6-T9 PSF | Yes |
| 83 M | 9 | 6 | Medical–sepsis, pneumonia | T11 flexion-distraction/open T9-L1 PSF | Yes/CRPP radius |
| 34 M | 13 | 3 | Medical–anemia, thigh wound hematoma | T6-T7 flexion-distraction/MIS T4-T8 PSF | Yes/ORIF femur |
| 64 F | 50 | 15 | Medical–anemia, retroperitoneal hematoma | T10-T11 fracture dislocation/open T9-T12 PSF | Yes/Ex-Lap, splenectomy, TAH-BSO, PEG, and trach |
| 23 M | 3 | 13 | Medical–lumbar strain | T11 fracture dislocation/open T9-T12 PSF | Yes |
| 62 M | 16 | 13 | Medical–hemorrhagic stroke | L4 burst/compression/MIS L3-L5 PSF | Yes/ORIF femur and tib/fib; craniectomy; PEG; and trach |
| 30 F | 21 | 24 | Medical–respiratory distress, tracheal stenosis secondary prolonged intubation | T5-T6 flexion-distraction/open T3-T11 PSF | Yes/ORIF femur |
| 17 F | 4 | 2 | Medical–ileus | T12 burst/compression/open T11-L1 ASF | Yes |
| 70 M | 6 | 14 | Surgical–instrumentation failure, SI screw pseudo/revision lumbopelvic fixation | L4 burst/compression/MIS L3-S1 PSF | Yes/ORIF pelvis |
| 34 M | 4 | 10 | Surgical–instrumentation failure, proximal screw pullout/revision T8-L2 | T12 burst + fracture dislocation/open T11-L1 PSF | No |
| 38 M | 20 | 10 | Wound–dehiscence/I + D | T3 flexion-distraction/open T1-T5 PSF | Yes/multiple ORIF, fasciotomy, ex-lap |
| 82 F | 12 | 7 | Wound–dehiscence/I + D | T12-L1 extension-distraction/open T10-L4 PSF | No |
| 61 M | 8 | 19 | Wound–infection/I + D | T8-T9 burst/compression/open T6-T10 PSF | Yes/ex-lap, splenectomy, ex-fix femur, ORIF humerus |
| 87 M | 9 | 22 | Wound–infection | L4-L5 burst/compression/MIS L4-S1 PSF | Yes |
| 70 M | 5 | 29 | Wound–infection | T12 fracture dislocation/MIS T10-L2 PSF | Yes/ORIF femur |
LOS, length of stay; UTI, urinary tract infection; I + D, irrigation and debridement; PSF, posterior spinal fusion; ASF, anterior spinal fusion; MIS, minimally invasive surgery; CRPP, close reduction and percutaneous pinning; ORIF, open reduction and internal fixation; ex-lap, exploratory laparotomy; TAH-BSO, total abdominal hysterectomy and bilateral salphingo-oophorectomy; tib/fib, tibia, and fibula; PEG, percutaneous endoscopic gastrostomy; trach, tracheostomy.
Multivariable regression was performed to control for variables identified as significant in the univariate analysis: ISS, non-spine surgery, head and neck surgery, and lower limb surgery (Table 7). Controlling for these variables concomitant lower limb trauma requiring operative treatment remained significant (P = .037). The odds ratio from the multivariate analysis for lower limb trauma was 4.40 (95% CI: 1.10–17.83). ISS, non-spine surgery, and head and neck surgery were not significant in this analysis.
Table 7.
Summary of Multivariable Regression Analysis.
| Odds ratio (95% CI) | P-value | |
|---|---|---|
| ISS | .97 † (.93–1.01) | .21 |
| Non-spine surgery | 1.50 (.38–6.02) | .57 |
| Lower limb surgery | 4.40 (1.10–17.83) | .037* |
| Head and neck surgery | 2.56 (.51–12.81) | .27 |
*indicates a statistically significant P-value <0.05.
†Unit ddds ratio was conducted for ISS, a continuous variable.
ISS, Injury Severity Score; CI, confidence interval.
Discussion
Unplanned readmissions are costly to the healthcare system.13,14 The implementation of financial penalties for high 30-day readmission rates seeks to contain all-cause 30-day readmissions and associated costs. Currently, CMS monitors readmission in a subset of common medical diagnosis and procedures, which does not include surgical spine trauma. 3 There is evidence that 30-day readmission rates can vary widely between patient populations, institution, and geographic location. 4 Additionally, 30-day readmission reduction programs that effectively reduced unplanned readmission also found increased 30-day mortality rates.15,16 Our study seeks to evaluate 30-day readmission rates, risk factors, and causes in the surgical spine trauma population.
In our study, 16 of 312 patients were readmitted resulting in a 5.1% 30-day readmission rate. This rate is comparable to those reported in the literature after elective spine surgery.2,4,6,7 In a systematic review of 13 studies and 488,049 patients evaluating 30-day readmissions in elective spine surgery, Bernatz, and Anderson 4 reported a pooled 30-day readmission rate of 5.5% (95% confidence interval, 4.2–7.4%). Despite a higher acuity in the spine trauma population, we found no increase in readmission rates compared with elective spine surgery rates reported in the literature. Readmission rates in our study were also similar to those in the orthopedic trauma population, with rates ranging from 4.8 to 6%.12,17-19
Trauma severity by ISS was significantly higher in the readmitted group compared to the non-readmitted group. ISS is a continuous metric used to predict outcomes based on the three most affected anatomic areas. 20 It is a measure of clinical severity. In the elective spine surgery, other surrogates for disease severity such as ASA score and CCI have been shown to be associated with 30-day readmission.2,4,6 However, no association with ASA and CCI was found in our study, most likely due to heterogeneity within the trauma population. Age is another factor associated with 30-day readmission in the elective spine surgery literature,2,6 but was not associated with 30-day readmission in our trauma population.
Medical complications accounted for the majority of unplanned readmissions. However, wound-related complications were the most common individual cause for readmission. This is consistent with causes of readmission reported in elective spine surgery. Pugely et al conducted a retrospective review of over 15,000 patients undergoing lumbar spine surgery. They found the most common cause of readmission was wound-related complications, accounting for 38.6% of readmissions. 6 A systematic review and meta-analysis of 30-day readmission after spine surgery by Bernatz and Anderson 4 also found wound-related complications were the most common reason for readmission, occurring in 39.3% of readmissions. In the current study, non-wound related sepsis was the second most common cause of readmission. Pugely et al 6 found similar results in elective lumbar spine surgery.
Unplanned 30-day readmission was associated with operative lower limb trauma. Readmitted patients were 4.40 times more likely to have required an operation for lower limb trauma than non-readmitted patients. Six of the 16 readmitted patients had concomitant LE surgery at presentation, and 3 out of the 6 patients requiring reoperation had lower limb trauma treated surgically during the initial admission. Additionally, patients in the readmitted group had significantly higher ISS and rates of head and neck surgery. Contrary to literature in elective spine surgery, length of stay, operative time, and in-hospital complications were not associated with unplanned 30-day readmission in our study population.2,6 Physician-dependent factors such as surgical technique, instrumented segments, surgical duration, EBL, and intraoperative transfusions were not different between groups. As 30-day readmission rate becomes a widely adopted performance metric, it is important to consider factors beyond providers control that may impact readmission. Performance metric benchmarks and financial penalties are only capable of containing healthcare costs when factors influencing the metric can be modified by the hospitals and physicians bearing the penalties.
The limitations in our study are predominantly due to the retrospective nature of the study design. Readmission data was collected from a database of multiple hospitals across the state to achieve the most complete patient follow-up possible. It is difficult to obtain complete patient follow-up in the trauma population at a tertiary referral center due to the substantial number of regional patients treated. The duration of ventilation and ICU stay could not be determined from the available medical records. These factors likely influence unplanned readmission and should be included in future studies. Despite limitations, this study is one of the first to evaluate readmissions in the spine trauma population. We found that injury severity and concomitant operative lower limb trauma were associated with unplanned readmission rates. Future studies are needed to determine the comprehensive impact of modifiable and non-modifiable factors on readmission rates in the thoracolumbar trauma population. Future cost analysis for readmissions is another topic of investigation needed in this population.
Conclusions
This study found a patients undergoing operative treatment for thoracolumbar spine trauma had unplanned 30-day readmission rates similar to those reported in elective spine surgery. The results of this study suggest operative concomitant trauma, particularly lower limb trauma, and higher trauma severity may be key considerations in 30-readmission rates. Wound-related complications were the most common reason for readmission, highlighting the importance of preventable measures targeted toward reducing wound-related complications. In the current healthcare environment with financial penalties for high readmission rates, it is paramount we understand the factors associated with unplanned 30-day readmission.
Footnotes
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: The authors disclose the following outside of the current work: payment for lectures from AOSpine NA and DePuy Synthes Spine; royalties from DePuy Synthes Spine; stock in the American Society for Investigative Pathology; consultant for Biomet; board member for the American Board of Orthopedic Surgery, the American Orthopedic Association, the Cervical Spine Research Society, and the Society for Minimally Invasive Spine Surgery; consultant for DePuy Synthes and K2M/Stryker; payment for lectures and travel accommodations from DePuy Synthes and K2M/Stryker; payment for patents and royalties from DePuy Synthes; stock in Innovative Surgical Designs and the American Society for Investigative Pathology; research support from AO Spine North America Spine Fellowship support and AOA Omega Grant; a board member of Maryland Development Corporation; royalties from Thieme, Quality Medical Publishers; editorial board of Journal of Spinal Disorders and Techniques, The Spine Journal, and Contemporary Spine Surgery. The authors have no further potential conflicts of interest to disclose.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: RB approval was obtained by the University of Maryland IRB (Protocol: HP-00082698) due to the retrospective nature of the study specific consent requirement was waived by the IRB. This study was conducted in accordance with the 1964 Helsinki Declaration, its amendments, and other equivalent ethical standards.
ORCID iDs
Jael E Camacho https://orcid.org/0000-0002-2153-455X.
Alexandra E. Thomson https://orcid.org/0000-0001-5378-4417.
Daniel E Gelb https://orcid.org/0000-0002-7263-6177.
Steven C Ludwig https://orcid.org/0000-0002-3962-5724.
References
- 1.Systems MHI . Potentially Preventable Readmissions Classification System: Methodology Overview, 5/08. https://multimedia.3m.com/mws/media/1042610O/resources-and-references-his-2015.pdf. [Google Scholar]
- 2.Wang MC, Shivakoti M, Sparapani RA, Guo C, Laud PW, Nattinger AB. Thirty-day readmissions after elective spine surgery for degenerative conditions among US medicare beneficiaries. Spine J. 2012;12(10):902-911. doi: 10.1016/j.spinee.2012.09.051. [DOI] [PubMed] [Google Scholar]
- 3.Services USCfMM . Hospital Readmissions Reduction Program (HRRP). Baltimore, MD: Centers for Medicare and Medicaid Services.
- 4.Bernatz JT, Anderson PA. Thirty-day readmission rates in spine surgery: systematic review and meta-analysis. Neurosurg Focus. 2015;39(4):E7. doi: 10.3171/2015.7.FOCUS1534. [DOI] [PubMed] [Google Scholar]
- 5.Hills J, Sivaganesan A, Khan I, et al. Causes and timing of unplanned 90-day readmissions following spine surgery. Spine. 2018;43(14):991-998. doi: 10.1097/BRS.0000000000002535. [DOI] [PubMed] [Google Scholar]
- 6.Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S. Causes and risk factors for 30-day unplanned readmissions after lumbar spine surgery. Spine. 2014;39(9):761-768. doi: 10.1097/BRS.0000000000000270. [DOI] [PubMed] [Google Scholar]
- 7.Akins PT, Harris J, Alvarez JL, et al. Risk factors associated with 30-day readmissions after instrumented spine surgery in 14,939 patients: 30-day readmissions after instrumented spine surgery. Spine. 2015;40(13):1022-1032. doi: 10.1097/BRS.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 8.Keeney JA, Adelani MA, Nunley RM, Clohisy JC, Barrack RL. Assessing readmission databases: how reliable is the information? J Arthroplasty. 2012;27(8 suppl l):72-76. doi: 10.1016/j.arth.2012.03.032. [DOI] [PubMed] [Google Scholar]
- 9.Singh S, Sparapani R, Wang MC. Variations in 30-day readmissions and length of stay among spine surgeons: a national study of elective spine surgery among US medicare beneficiaries. J Neurosurg Spine. 2018;29(3):286-291. doi: 10.3171/2018.1.SPINE171064. [DOI] [PubMed] [Google Scholar]
- 10.Amin BY, Tu TH, Schairer WW, et al. Pitfalls of calculating hospital readmission rates based on nonvalidated administrative data sets: : presented at the 2012 joint spine section meeting: clinical article. J Neurosurg Spine. 2013;18(2):134-138. doi: 10.3171/2012.10.SPINE12559. [DOI] [PubMed] [Google Scholar]
- 11.Ibrahim AM, Dimick JB, Sinha SS, Hollingsworth JM, Nuliyalu U, Ryan AM. Association of coded severity with readmission reduction after the hospital readmissions reduction program. JAMA Intern Med. 2018;178(2):290-292. doi: 10.1001/jamainternmed.2017.6148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Metcalfe D, Olufajo OA, Zogg CK, et al. Unplanned 30-day readmissions in orthopaedic trauma. Injury. 2016;47(8):1794-1797. doi: 10.1016/j.injury.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Chilingerian JA, Sherman HD. Managing physician efficiency and effectiveness in providing hospital services. Health Serv Manage Res. 1990;3(1):3-15. doi: 10.1177/095148489000300101. [DOI] [PubMed] [Google Scholar]
- 14.Emanuel EJ, Fuchs VR. The perfect storm of overutilization. JAMA. 2008;299(23):2789-2791. doi: 10.1001/jama.299.23.2789. [DOI] [PubMed] [Google Scholar]
- 15.Fonarow GC, Konstam MA, Yancy CW. J Am Coll Cardiol. 2017;70(15):1931-1934. doi:doi: 10.1016/j.jacc.2017.08.046. [DOI] [PubMed] [Google Scholar]
- 16.Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the hospital readmissions reduction program with mortality among medicare beneficiaries hospitalized for heart failure, acute myocardial infarction, and pneumonia. J Am Med Assoc. 2018;320(24):2542-2552. doi: 10.1001/jama.2018.19232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bernatz JT, Tueting JL, Anderson PA. Thirty-day readmission rates in orthopedics: a systematic review and meta-analysis. PloS One. 2015;10(4):e0123593. doi: 10.1371/journal.pone.0123593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hageman MG, Bossen JK, Smith RM, Ring D. Predictors of readmission in orthopaedic trauma surgery. J Orthop Trauma. 2014;28(10):e247-e249. doi: 10.1097/BOT.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 19.Moore L, Stelfox HT, Turgeon AF, et al. Rates, patterns, and determinants of unplanned readmission after traumatic injury: a multicenter cohort study. Ann Surg. 2014;259(2):374-380. doi: 10.1097/SLA.0b013e31828b0fae. [DOI] [PubMed] [Google Scholar]
- 20.Kuhls DA, Malone DL, McCarter RJ, Napolitano LM. Predictors of mortality in adult trauma patients: the physiologic trauma score is equivalent to the trauma and injury severity score. J Am Coll Surg. 2002;194(6):695-704. doi: 10.1016/s1072-7515(02)01211-5. [DOI] [PubMed] [Google Scholar]