Abstract
Background
Worldwide, bystander CPR rates are low; one effective way to increase these rates is to train schoolchildren; however, the most effective way to train them is currently unknown.
Methods
This systematic review and meta-analysis of randomized controlled trials (RCTs) and observational studies, evaluated whether CPR training for schoolchildren, using innovative teaching modalities (nonpractical, self, or peer-training) versus standard instructor-led training, resulted in higher quality CPR, self-confidence and short-term (≤3 months post-training) or long-term (>3 months post-training) retention of CPR skills.
Results
From 9793 citations, 96 studies published between 1975 and 2022 (44 RCTs and 52 before/after studies) were included. There were 43,754 students, average age of 11.5 ± 0.9 (range 5.9–17.6) and 49.2% male. Only 13 RCTs compared practical vs. nonpractical training (n = 5), self- vs. instructor-led training (n = 7) or peer- vs. instructor-led training (n = 5). The observed statistically significant differences in mean depth and rate of compressions between children with hands-on practical training and those without were not clinically relevant. Regardless of training modality, compression depth was consistently suboptimal. No differences were observed in CPR skills immediately or ≤ 3 months post-training, between children who were self- or peer-trained vs. instructor-led. Due to lack of data, we were unable to evaluate the impact of these novel training modalities on student self-confidence.
Conclusion
Although innovative training modalities are equally effective to instructor-led training when teaching schoolchildren CPR, compression depth was frequently suboptimal. Recommendations on standardized training and evaluation methods are necessary to understand the best ways to train children.
Keywords: Cardiopulmonary resuscitation, Automated external defibrillators, Training, Education, Schoolchildren
Introduction
Two of the most important factors for improving survival from sudden cardiac arrest (SCA), are cardiopulmonary resuscitation (CPR) and early defibrillation using an automated external defibrillator (AED).1 SCA victims are almost twice as likely to survive, if they receive bystander CPR before Emergency Medical Services (EMS) arrival.2 Worldwide, bystander CPR rates range between 6% and 70%.3, 4 One effective way to increase rates of bystander CPR is to train schoolchildren. Countries like Denmark, who have mandated CPR training in schools for decades, have shown a doubling in the rate of bystander CPR after five years, and a threefold improvement in survival following SCA over ten years.5
Recent scientific position statements from the International Liaison Committee on Resuscitation (ILCOR) and the European Resuscitation Council (ERC) recommend mandating CPR training for all schoolchildren, starting as early as possible. 6, 7 Training children in CPR is effective at improving their skills and knowledge.8 Beyond learning practical skills, children can also act as multipliers and transmit information to other family members.9, 10, 11 Furthermore, learning CPR at a young age, may help children develop self-confidence in their ability to perform it.12 This can help to facilitate the development of practical skills, as they become more capable of performing physical maneuvers and make them more likely to help in emergency situations as adults.13, 14
As there are many barriers to implementing CPR training in schools,14 investigating whether innovative training modalities (i.e. nonpractical, self- or peer-based training), are as effective as traditional, instructor-led methods, could provide guidance as to whether these strategies can be used to increase implementation of CPR training in schools.12
Previous reviews have narratively described the best method(s) for training children how to perform CPR7, 8, 15, 16, 17 however, few have meta-analyzed this data, due to the diversity of the literature. The objective of this systematic review and meta-analysis was to examine if CPR training using innovative training modalities, resulted in higher quality CPR and/or retention of CPR skills compared to standard instructor-led training among schoolchildren.
Methods: We conducted this systematic review and meta-analysis in accordance with the Cochrane Handbook for Systematic Reviews of Interventions18 and followed the Preferred Reporting Items for Systematic review and Meta-Analysis (PRISMA) statement for meta-analysis in health care interventions (PRISMA Checklist, Supplemental Appendix Table S1).19 This review was registered on PROSPERO (International prospective register of systematic reviews) ID: CRD42019139005.
Eligibility criteria: We included all randomized controlled trials (RCTs) and observational studies, where schoolchildren (ages 4–18) were taught CPR. We included studies that trained both children and adults if we could separate their data. We excluded studies with children < age 4 and that had only adults (i.e. age > 18).
Search strategy and study selection: A search strategy was developed by an experienced information specialist (TK), in close collaboration with the lead author (KA). The following bibliographic databases were searched from inception to May 24, 2023: Medline (Ovid), the Cochrane Central Register of Controlled Trials (Ovid), CINAHL Plus with Full Text (EBSCO), Embase (Ovid), Web of Science, and ERIC (ProQuest). A combination of subject headings and text words were used for each of the main search concepts: CPR, education and schoolchildren, which were combined using Boolean operators. No year/language restrictions were placed on the searches. The initial Medline search strategy was peer reviewed by another information specialist using the PRESS checklist.20 An example search strategy is available in Supplemental Appendix 1. The final search results were exported into EndNote, and duplicates were removed by the information specialist. Ongoing trials were identified using the World Health Organization International Clinical Trials Registry Platform and ClinicalTrials.gov. Experts were contacted to inquire about additional studies and unpublished data.
Eight reviewers working in pairs independently examined the titles, abstracts, and full-text articles retrieved by the search, in Covidence (Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia). We included studies for full-text review based on agreement between two reviewers or when there was disagreement or uncertainty. Data from multiple reports of the same study were linked together and used to supplement information obtained from the primary report. We examined citations of included studies to identify additional studies not identified in the electronic search. A priori, we decided to include single arms of RCTs that did not directly compare our outcomes of interest in the observational analyses.
Data extraction: Eight reviewers working in pairs used standardized forms created in Covidence to independently perform data extraction, in duplicate, with discrepancies resolved through consensus. We abstracted data on both study characteristics and individual participants: study variables included author and year of publication, location, design, setting, number of participants, description of the intervention, reported outcomes, time points measured and length of training. Participant characteristics included average age, average height, average weight, proportion male sex and the proportion with any prior CPR training.
Endpoints and subgroup analyses
The primary analysis evaluated whether CPR training in schoolchildren (population) using practice (comparison) (defined as any training with a hands-on component) compared to CPR training using no practice (intervention), resulted in higher quality CPR (i.e. mean rate, mean depth), self-confidence and short (≤3 months post-training) or long term retention (>3 months post-training) of CPR skills (outcomes). Secondary analyses compared differing modalities of CPR training to evaluate their impact on CPR skills, self-confidence and retention. Specifically, we compared traditional instructor-led CPR training to self-training and peer-training formats. Instructor-led training was defined as, any training led by instructors and involving any format (i.e. didactic lecture, teaching by video, etc). Additionally, instructors could be of any background (i.e. certified instructors, teachers, healthcare professionals, etc). We used the ILCOR definition of self-training: “as any form of digital (e.g. video, phone application [app] based, internet based, game based, virtual reality, augmented reality) education or training for BLS that can be completed without an instructor”.17 We defined peer-training as any format of education or training for CPR that was led by peers, but may also have included a teacher facilitator.
Planned subgroup analyses included evaluating the effect of age, sex and teaching modality on CPR performance. Sensitivity analyses were planned to evaluate potential sources of bias resulting from variability in studies.
Risk of bias and quality assessment: Risk of bias for RCTs was assessed using the Cochrane Collaboration Risk of Bias 1.0 tool, as “low risk,” “high risk of bias,” or “unclear” for the following measures: adequacy of sequence generation, adequacy of allocation concealment, adequacy of blinding for participants, study personnel and outcome assessors, completeness of outcome data for each primary and secondary outcome, selective outcome reporting, and other potential sources of bias (i.e. funding).21 As all of the observational studies were interrupted time series, we used the Cochrane Effective Practice and Organization of Care (EPOC) tool22 to assess risk of bias for the following domains: intervention independent of other changes, shape of the intervention effect pre-specified, intervention unlikely to affect data collection, knowledge of the allocated interventions adequately prevented during the study, incomplete outcome data adequately, selective outcome reporting and other risks of bias. Risk of bias tables were completed independently by the 8 reviewers in pairs and compared for consensus.
Statistical analysis: We used inverse-variance random-effects models to compare CPR outcomes (mean depth, mean rate, % correct depth, % correct rate and % correct hand position) and self-confidence, incorporating for heterogeneity between studies. Data were pooled at consistent time points across studies immediately post-training, ≤3 months’ post-training (short term retention) and >3 months’ post-training (long term retention) to measure differences between training modalities (i.e. practical training vs. nonpractical training).
Weighted mean differences with confidence intervals were calculated for continuous outcomes and we calculated the odds ratio (OR) for binary data, using Review Manager (RevMan) Version 5.3.5 (The Nordic Cochrane Centre, The Cochrane Collaboration, Copenhagen, 2014) software. For data that were unavailable numerically, we used approximations based on graphic output. For studies reporting only medians and interquartile ranges, means and standard deviations were estimated.23 Point estimates with 95% confidence intervals are reported. We did not perform funnel plots due to the limited number of RCTs included in each analysis.
We evaluated studies for heterogeneity using the χ2 test for homogeneity with an alpha = 0.10 and the I2 statistic to quantify inconsistency.24 I2 values of 0%–40% were considered as not important, 30%–60% as moderate heterogeneity, and 75%–100% as considerable heterogeneity.24
For data from cohort studies and single arms of RCTs, we pooled proportions of CPR outcomes with binary data including, % correct depth, % correct rate and % correct hand position and % improved self-confidence. We pooled means of CPR outcomes with continuous data, including mean compression depth and mean compression rate. Similar to the analyses of RCTs, data were pooled at consistent time points across studies and between training modalities. Generated forest plots provide graphical representation of the results, without estimates, due to considerable heterogeneity, particularly with the proportional meta-analyses. We used the metaprop, metamean, and forest functions in R version 1.4.1106 (R Foundation for Statistical Computing, Vienna, Austria) to analyze the study data.
Results
Literature search and study selection
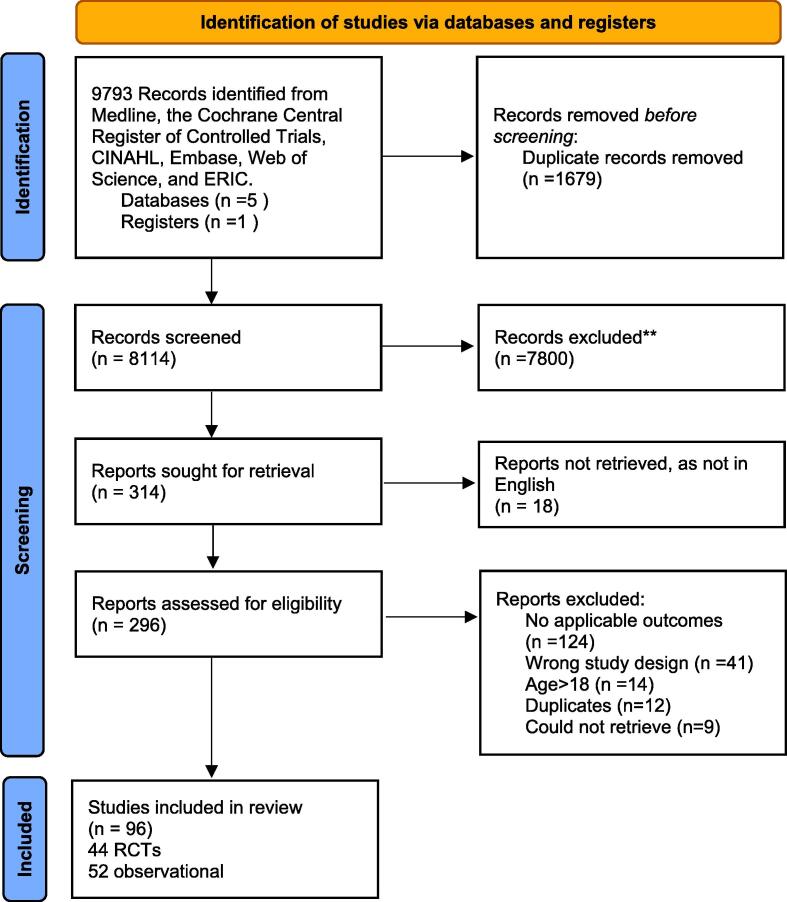
We identified 9793 records. After removing 1679 duplicates, 8114 records were screened by title and abstract, 296 full-text articles were assessed for eligibility and 96 studies were included (Fig. 1).
Fig. 1.
PRISMA Flow Diagram.
Study characteristics
A total of 43,754 students were included in the 96 studies (44 RCTs,25, 26, 27, 28, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67 30 uncontrolled before/after studies68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97 and 22 controlled before/after studies98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119, ranging from 30 to 6352 students per study. Studies spanned the globe, including Europe, North America, Asia, the Middle East and New Zealand and were published between 1975 and 2022. Supplemental Table S2 summarizes the included study characteristics.
Student characteristics
The average weighted age of the students was 11.5 ± 0.9 (range 5.9–17.6) with 49.2% male (Table 1). Only 4 studies included students with age < 10.69, 99, 102, 107 The average weighted height and weight of the students were 158.5 ± 8.1 cm and 46.3 ± 8.9 kg, respectively. Almost 30% of the students had prior CPR training before participation.
Table 1.
Student characteristics.
| Author, Year | Number of Children Analyzed | Mean Age of Children |
Mean Height of Children (cm) |
Mean Weight of Children (kg) |
Male Sex N (%) |
Number of Children with any Prior CPR Training N (%) |
|---|---|---|---|---|---|---|
| Abelairas-Gomez 2014 | 721 | 12.5 | 156.3 ± 7.9 | 51.5 ± 10.9 | 361 (50.1) | NR |
| Abelairas-Gomez 2021 | 472 | 10.0 ± 2.0 | NR | NR | NR | NR |
| Abelsson 2020 | 50 | 17.0 ± 1.0 | NR | NR | 20 (40.0) | NR |
| Akiteru 2022 | 88 | 9.1 ± 1.7 | 134.9 ± 12.2 | 34.8 ± 10.4 | 41 (46.6) | NR |
| Aloush 2018 | 121 | NR | NR | NR | 40 (33.3) | 18 (14.9) |
| Andresen 2012 | 195 | 13.8 | NR | NR | 100 (51.3) | 0 (0) |
| Barsom 2020 | 40 | 16.0 | NR | NR | 20 (50.0) | NR |
| Banfai 2018 | 118 | 5.9 ± 0.5 | 121.3 ± 1.0 | 21.1 ± 0.5 | 47 (39.8) | 0 (0) |
| Banfai 2017 | 582 | 10.2 ± 2.0 | 146.9 ± 13.1 | 38.7 ± 9.9 | 265 (45.5) | 75 (12.9) |
| Banfai 2019 | 524 | 9.7 ± 1.9 | NR | NR | 236 (45.0) | 524 (100) |
| Beard 2015 | 87 | 11.1 ± 2.6 | 151.0 ± 16.7 | 44.4 ± 12.2 | 45 (51.7) | 0 (0) |
| Beck 2015 | 937 | 13.9 ± 1.1 | 168.1 ± 9.6 | 55.4 ± 11.6 | 439 (46.9) | 111 (12.6) |
| Berthelot 2013 | 82 | 10.6 ± 0.5 | NR | NR | 47 (57.3) | 6 (7.4) |
| Beskind 2016 | 159 | 14.9 ± 0.9 | NR | NR | 146 (81.5) | 33 (18.4) |
| Bohn 2012 | 280 | NR | NR | NR | 223 (51.5) | 0 (0) |
| Borovnik Lesjak 2022 | 611 | 13 ± 1 | NR | NR | 53 (45.7) | NR |
| Brown 2018 | 795 | 15.0 | NR | 62.9 | 386 (48.5) | 795 (100.0) |
| Chamdawala 2021 | 220 | 16.0 ± 0.5 | 170.5 ± 9.5 | 63 ± 13.5 | 123 (55.9) | 47 (21.4) |
| Chang 2022 | 385 | 10.5 ± 0.5 | NR | NR | 180 (46.8) | 96 (25) |
| Chan 2017 | 112 | 10.3 | 142 | 37.4 | 81 (72.3) | NR |
| Cons-Ferreiro 2022 | 160 | 10.7 ± 0.6 | 150.6 ± 11.7 | 46.2 ± 12.2 | 170 (55.2) | 78 (23.5) |
| Contri 2016 | 36 | 17.3 ± 1.5 | NR | NR | 17 (47.2) | NR |
| Cuijpers 2016 | 144 | 14.4 ± 0.6 | NR | NR | 82 (56.9) | NR |
| Damvall 2022 | 982 | NR | NR | NR | NR | NR |
| Desailly 2017 | 97 | NR | NR | NR | NR | NR |
| Doucet 2019 | 165 | NR | NR | NR | 81 (43.8) | 113 (71.9) |
| Dumcke 2021 | 365 | 13.7 ± 0.8 | NR | NR | 193 (52.9) | 77 (21.1) |
| Fleischhackl 2009 | 162 | 13.8 ± 2.6 | 160.0 ± 16.3 | 61.8 ± 27.9 | NR | 0 (0) |
| Gabriel 2019 | 210 | 17.0 ± 1.5 | NR | NR | 126 (60.0) | 0 (0) |
| Greer 2010 | 122 | 13.5 | NR | NR | 47 (38.5) | NR |
| Han 2021 | 62 | 17.0 ± 0.6 | NR | NR | 13 (20.9) | 50 (80.6) |
| He 2018 | 360 | 11.6 ± 0.5 | 153.1 ± 6.7 | 44.6 ± 8.2 | 180 (50.0) | 0 (0) |
| Hill 2009 | 85 | 11.1 | 148.5 | 40.8 | 37 (43.5) | 85 (100.0) |
| Hori 2016 | 6352 | 14.3 ± 1.7 | NR | NR | 4966 (78.2) | 1423 (22.4) |
| Isbye 2007 | 72 | 13.0 | NR | NR | 45 (62.5) | 0 (0) |
| Iserbyt 2013 | 111 | 13.0 ± 0.8 | NR | NR | NR | 0 (0) |
| Iserbyt 2014 | 128 | 16.9 ± 0.7 | NR | NR | 25 (18.1) | NR |
| Iserbyt 2021 | 235 | 13.0 ± 1.0 | NR | NR | 72 (30.6) | 0 (0) |
| Jones 2007 | 157 | 11.6 ± 0.3 | 149.2 ± 8.5 | 43.2 ± 11.8 | 74 (47.1) | NR |
| Kalluri 2018 | 267 | NR | NR | NR | NR | 47(17.6) |
| Kaweenuttayanon 2017 | 275 | 15.4 ± 1.6 | 163.0 ± 8.0 | 58.0 ± 13.6 | 118 (42.9) | 16 (58.2) |
| Kelley 2006 | 33 | 13.6 | NR | NR | 17 (51.5) | 8 (24.2) |
| Kesici 2021 | 130 | 14.0 | NR | NR | NR | 23 (14.7) |
| Kherbeche 2017 | 52 | 13.2 | 160 | 54.7 | 28 (53.8) | 0 (0) |
| KimSe 2011 | 439 | NR | NR | NR | 271 (59.2) | NR |
| Kłosiewicz 2021 | 402 | 9.5 ± 2.5 | 142.0 ± 11.7 | 39.8 ± 16.4 | 202 (50.2) | 0 (0) |
| Lanzas 2022 | 318 | 16.4 ± 0.5 | NR | NR | 140 (44.0) | 246 (77.4) |
| Lester 1997 | 233 | 11.5 | NR | NR | 128 (54.9) | 81 (34.8) |
| Li 2018 | 489 | 12.6 ± 1.1 | NR | NR | 547 (50.1) | 170 (15.6) |
| Lorem 2008 | 102 | 11.9 ± 0.04 | NR | NR | 39 (38.2) | 63 (61.8) |
| Lorem 2010 | 145 | NR | NR | NR | NR | 51 (35.2) |
| Martinez-Isasi 2021 | 62 | 11.9 ± 0.5 | 149.6 ± 7.0 | 45.0 ± 10.9 | 27 (43.5) | NR |
| Martinez-Isasi 2022 | 567 | 10.0 ± 2.0 | NR | NR | 295 (52.0) | NR |
| Martins 2022 | 102 | 11.72 ± 0.75 | 151.62 ± 3.59 | 53.27 ± 4.67 | 48 (47.1) | NR |
| Mathew 2020 | 617 | 13.4 ± 0.3 | 150.8 ± 3.8 | 39.5 ± 2.8 | 351 (56.9) | 50 (8.1) |
| Meissner 2012 | 98 | 14.6 ± 1.4 | 170.8 ± 7.0 | 58.1 ± 0.1 | 57 (43.2) | 44 (33.3) |
| Metelmann 2021 | 200 | 14.6 | NR | NR | 95 (48.2) | 121 (60.5) |
| Mpotos 2017 | 265 | 15 ± 1.6 | 169.3 ± 2.0 | 56.1 ± 1.5 | 156 (58.4) | 11 (4.2) |
| Napp 2020 | 808 | 14.9 ± 0.9 | 167.3 ± 9.3 | 55.9 ± 10.5 | 375 (46.1) | 277 (36.5) |
| Naqvi 2011 | 30 | 13.4 ± 1.7 | 144.2 ± 8.1 | 50.0 ± 11.8 | 11 (36.6) | NR |
| Nord 2016 | 1061 | 13.0 | NR | NR | 579 (47.0) | 363 (29.5) |
| Nord 2017 #1 | 432 | 13.0 | NR | NR | 213 (49.3) | 124 (28.7) |
| Nord 2017 #2 | 587 | 13.0 | NR | NR | 283 (48.2) | 152 (25.9) |
| Oliveira 2022 | 104 | 13.9 | 156.2 ± 0.1 | 55.7 ± 13.8 | 38 (36.5) | 0 (0) |
| Onan 2019 | 77 | 17.5 | NR | NR | NR | NR |
| Otero-Agra 2019 #1 | 196 | 11.1 ± 1.5 | 148.9 ± 10.0 | 44.2 ± 10.5 | 71 (36) | 0 (0) |
| Otero-Agra 2019 #2 | 489 | 13.5 ± 1.2 | 163.0 ± 8.9 | 56.8 ± 12.4 | 246 (50.3) | 0 (0) |
| Oulego-Erroz 2011 | 59 | 13.5 | NR | NR | NR | 0 (0) |
| Paglino 2017 | 203 | NR | NR | NR | NR | NR |
| Paglino 2019 | 622 | 16.8 ± 1.4 | 169.9 ± 9.4 | 61.6 ± 11.9 | 277 (44.5) | NR |
| Ramesh 2022 | 414 | 14.2 ± 0.5 | 158.5 ± 8.5 | 48.9 ± 10.9 | 227 (54.8) | NR |
| Reder 2006 | 779 | NR | NR | NR | 424 (54.4) | 534 (68.6) |
| Sabihah 2020 | 36 | 16.0 | NR | NR | NR | 1 (2.8) |
| Santomauro 2018 | 320 | 16.4 ± 2.0 | 164.3 ± 8.1 | 65.2 ± 10.0 | 154 (48.1) | 8 (2.5) |
| Schmitz 2015 | 201 | 15.1 ± 1.6 | NR | NR | 94 (46.8) | 201 (100) |
| Schuffelen 2015 | 108 | 15.9 ± 0.8 | NR | NR | 55 (50.9) | NR |
| Semeraro 2017 | 50 | 16.0 ± 1.0 | NR | NR | 49 (75.0) | 0 (0) |
| So 2020 | 128 | 13.5 ± 0.5 | NR | NR | 35 (27.3) | 0 (0) |
| Suss-Havemann 2020 | 600 | 12.0 ± 1.0 | 160.5 ± 8.2 | 47.0 ± 8.7 | 286 (47.7) | 42 (7.0) |
| Suwanpairoj 2020 | 313 | 10.1 | NR | NR | NR | NR |
| Tanaka 2020 | 54 | 17.6 ± 0.6 | 167.2 ± 7.9 | 59.7 ± 9.1 | 40 (74.1) | 28 (51.9) |
| Uhm 2010 | 71 | 11.6 ± 0.6 | 151.6 ± 6.5 | 44.5 ± 9.3 | 45 (63.4) | NR |
| Uzendu 2021 | 77 | NR | NR | NR | NR | 38 (49.4) |
| Vanderschmidt 1975 | 400 | 15.0 | NR | NR | NR | NR |
| Vanderschmidt 1976 | 216 | 15.0 | NR | NR | NR | 216 (100.0) |
| VanRaemdonck 2014 | 165 | 15.5 | NR | NR | 165 (100.0) | 0 (0) |
| Vetter 2016 | 412 | 15.9 ± 1.3 | NR | NR | 150 (36.4) | NR |
| Wang 2021 | 198 | 11.8 ± 0.5 | 152.8 ± 7.3 | 41.9 ± 8.7 | 97 (49.0) | 64 (32.3) |
| Watanabe 2017 | 41 | NR | NR | NR | NR | 1 (2) |
| Weidenauer 2018 | 322 | 10.0 | 145.7 | 40.8 | 141 (43.8) | 147 (45.6) |
| Wingen 2018 | 424 | 15.0 ± 0.6 | NR | NR | 207 (48.8) | 177 (41.7) |
| Yeow 2021 | 118 | 16.0 | NR | NR | 68 (57.6) | 1 (0.8) |
| Yeung 2017 | 81 | 12.5 | NR | NR | 36 (44.4) | NR |
| Younas 2006 | 59 | 14.5 | NR | NR | NR | 34 (57.6) |
| Zalewski 2016 | 235 | NR | NR | NR | 87 (37.0) | NR |
| Zeleke 2019 | 160 | 12.0 | NR | NR | NR | 160 (100.0) |
Risk of bias
Most RCTs had low risk of bias for 6 of 7 categories (Supplemental Fig. S1A) with description of the allocation sequence being unclear in more than 60% of the included studies. With the uncontrolled/controlled before and after studies, the majority had low risk of bias in 6/7 categories, with the exception of other bias (Supplemental Fig. S1B).
Outcomes and sensitivity analyses
Of the 44 RCTs, only 13 directly compared practical vs. nonpractical training (n = 5)28, 51, 55, 62, 67, self-training vs. instructor-led training (n = 7)28, 32, 34, 51, 55, 61, 67 or peer-training vs. instructor-led training (n = 5)27, 56, 57, 59, 61. We treated the remaining RCTs (n = 31)29, 54, 56, 21, 22, 25, 26, 27, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 48, 49, 50, 59, 60, 61, 62 as one arm cohorts and combined them with the uncontrolled before/after studies (n = 30)68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92, 93, 94, 95, 96, 97 and controlled before/after studies (n = 22)98, 99, 100, 101, 102, 103, 104, 105, 106, 107, 108, 109, 110, 111, 112, 113, 114, 115, 116, 117, 118, 119 to perform the same comparisons (Supplemental Appendix 2). Most studies did not report their data according to age or sex, so we could not assess the effect of these variables on CPR metrics. Where applicable, we examined the effect of different training modalities on outcomes.
Primary analysis – Instructor-led practical versus NonPractical training RCTs
For the primary analysis, two RCTs28, 67 compared the mean depth and mean rate of compressions performed by children immediately post-training, who received hands-on practical training versus those without any practical training. There was no statistically significant difference in the mean compression depth immediately post-training (Fig. 2), however, there was high heterogeneity, likely due to the differing ages of the children included in both studies (15 vs. 12.5 years) and proportion male (81% vs. 44%). In contrast, there was a significant, non-clinical difference in the mean compression rate immediately post-training (MD = −9.30 [−12.31, −6.29], I2 = 0%, p < 0.00001, two trials, n = 164), favouring nonpractical training over practical training (Fig. 2). No studies reported self-confidence immediately post-training.
Fig. 2.
Randomized Controlled Trials - Mean depth and mean rate by Practical vs NonPractical training – post-training.
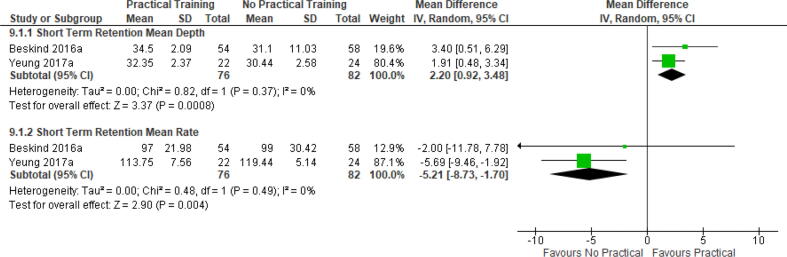
Short term retention (≤3 months) RCTs
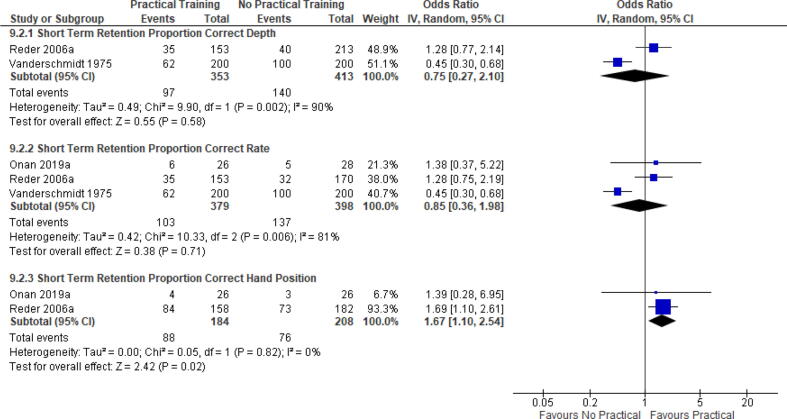
The same two RCTs28, 67 compared the mean depth and mean rate of compressions performed by children ≤ 3 months post-training, who received hands-on practical training versus those without any practical training. There was a statistically significant difference in the mean compression depth (MD = 2.20 [0.92, 3.48], I2 = 0%, p = 0.004, 2 trials, n = 158) favouring practical training (Fig. 3). Conversely, there was a significant, non-clinical difference in short-term mean compression rate (MD = −5.21 [−8.73, −1.70], I2 = 0%, p = 0.004, 2 trials, n = 158) favouring nonpractical training (Fig. 3). Three different RCTs evaluated the impact of practical versus nonpractical training on the proportion of children with correct depth, correct rate and correct hand position of compressions, ≤3 months post training.51, 55, 62 There was no observed difference in the percentage of students with correct depth or correct rate of compressions between students who completed practical vs. nonpractical training (Fig. 4), however, heterogeneity was also high. Neither age nor sex were reported consistently in these studies, so we could not determine if these had any effect. In contrast, there was a significant improvement in the percentage of students with correct hand position (OR = 1.67 [1.10, 2.54], I2 = 0%, p = 0.02, 2 trials, n = 392) favoring practical training vs. nonpractical training (Fig. 4).
Fig. 3.
Randomized Controlled Trials - Mean depth and mean rate by Practical vs NonPractical training – short term retention.
Fig. 4.
Randomized Controlled Trials - Proportion correct depth, rate, hand position Practical vs NonPractical training - short term Retention.
Only one RCT reported self-confidence51; in this study, students who received video-based instruction with hands-on practice and mobile-assisted feedback had the highest self-confidence scores one-week post training, in comparison to students who received only one or neither of these interventions.
There were an insufficient number of RCTs that reported long-term retention outcomes, preventing meta-analysis.
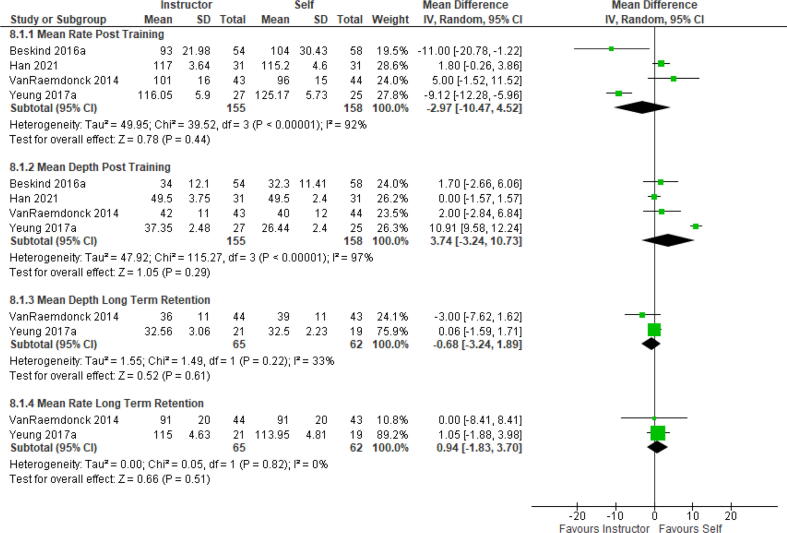
Secondary analyses – Self-training versus instructor-led training RCTs
Five RCTs31, 32, 34, 61, 67 compared CPR skills immediately post-training for children who were self-taught versus those who received traditional instructor-led training. Methods of self-learning included video instruction or using an online application with (n = 4)32, 34, 61, 67 or without hands-on practice (n = 2).28, 67 There were no observed differences in the mean depth, mean rate, percent correct depth, percent correct rate or percent correct hand position of compressions between children in either group post-training (Fig. 5, Fig. 6). Heterogeneity was high in both mean compression depth and rate post-training. Removing studies based on age or proportion male did not affect the I2 value for mean compression rate post-training; however, for mean compression depth post-training, removing the study67 with the youngest participants completely eliminated the heterogeneity. Subgrouping the type of training by hands-on training vs. without, seemed to eliminate the heterogeneity in mean compression rate post-training (Supplemental Appendix 1: Supplemental Fig. S2).
Fig. 5.
Randomized Controlled Trials - Mean depth, rate by self vs. instructor-led training – post-training and long term retention.
Fig. 6.
Randomized Controlled Trials - Proportion correct depth, rate, hand position by self vs. instructor-led training – post-training and short term retention.
Two RCTs51, 55 compared CPR skills ≤ 3 months post-training and two RCTs compared CPR skills > 3 months post-training61, 67, for children who were self-taught (video based training with hands-on practice (n = 2) and online app without hands on practice (n = 2)), versus those who received traditional instructor-led training. Similar findings were observed in both short term and long-term retention outcomes (Fig. 5, Fig. 6, with the exception of correct hand position. There was a significantly higher proportion of children with correct hand position in those who were instructor-led trained in comparison to children who were self-trained (OR 0.63 [0.40, 0.99], I2 = 3%, p = 0.05, 2 trials, n = 392), ≤ 3 months of initial training. Only one study reported self-confidence, preventing meta-analysis.
Peer-trained versus instructor-led trained – RCTs
Five RCTs compared CPR metrics immediately post-training in children who were trained by peers versus those who received traditional instructor-led training.27, 56, 57, 59, 61 In all 5 studies, students were taught by peers, which included hands-on practice. No differences were observed when comparing the proportion of children with percent correct depth, percent correct rate and percent correct hand position in compressions, immediately post-training in those who received peer-training versus those who received traditional instructor-led training (see Supplemental Appendix 1: Supplemental Fig. S3). No retention or self-confidence data were available for comparison from the RCTs.
Observational data
Due to the considerable heterogeneity of the cohort and single arm RCT data, we did not conduct formal meta-analyses of proportional or continuous CPR outcomes; however, we did generate forest plots to graphically summarize the data. (Supplemental Appendix 2).
Discussion
We performed a comprehensive systematic review and meta-analysis, evaluating the impact of innovative training modalities on the performance and retention of CPR skills in schoolchildren. We observed some statistically significant, but non-clinical differences in mean depth and mean rate of compressions, both immediately post-training and ≤3 months, between groups that were provided practical training and those without. No differences were observed when comparing CPR skills between children who were trained using traditional instructor-led methods versus those who were self or peer-trained. The exception to this was children who were trained by instructors had better short-term retention of correct hand position in comparison to those who did not receive any practical training or were peer or self-trained. Due to lack of data, we were unable to meta-analyze self-confidence measures.
ILCOR recently performed a systematic review of CPR and AED self-training using digital formats in both adults and children17, 120 and demonstrated comparable outcomes for most CPR skills immediately post-training and up to 1 year later.120 Similar results were observed when comparing instructor-led training with hands-on practice to digital training without hands-on practice. They recommended that either method could be used to teach adults and high school children (>10 years of age) CPR knowledge and skills, as long as they incorporated hands-on practice and manikins with feedback devices.17 Since children are known to act as multipliers, sending students home with digital self-training kits, could be an effective and cost-savings method to train both students and adults, especially in under-resourced areas.11
In contrast to another recent systematic review,15 we did not find a difference in CPR skills, between children who were self-taught using digital training methods compared to those who were instructor-led. Regardless of who trained them or training modality, children consistently did not compress deep enough, although compression rate remained on target. Lim et al. evaluated the effectiveness of technology-based CPR training on adolescents’ CPR skills and knowledge and found that overall, instructor-led training improved CPR skills in adolescents (ages 12–18), while the use of self-directed learning produced less optimal skills.15 Our results likely differ, because we included a broader age range and we defined “standard training” as instructor-led, in any format (i.e. in person, by video, etc), while their definition included only instructor-led training without a technology component. We also did not differentiate between self-training with or without hands-on practice, which may have led to the equivalency result.
Yet this raises an important point; current CPR training methods fail to teach children how to compress deeply enough. This is problematic, as optimal compression depth and rate are well correlated with survival from SCA.121, 122 The use of CPR feedback devices or manikins that are easier to compress, may help children to achieve guideline targets for compression depth. Very few of the studies that we reviewed, evaluated the effect of feedback devices on CPR performance. Chamdawala et al. compared the use of real-time visual feedback on high school students’ CPR performance and retention, to those taught without it.29 They found that post-training, students taught with real-time feedback had significantly higher compression scores, including depth, at both baseline and retention testing, compared to those without it. In both groups however, CPR depth remained well below recommended guidelines. More research is clearly needed to help determine how we can help children to achieve optimal CPR performance.
Additionally, the lack of standardization on how these training courses are taught and evaluated, poses a significant barrier to determining the most effective method to teach children. Due to the wide variation in teaching methods, type of instructor, ages of the children trained and forms of evaluation, most systematic reviews on this topic have been limited to narratively describing them, as authors were unable to meta-analyze the results.120, 123 This was clearly evident when we attempted to synthesize the results from the observational studies and one arm RCTs. Visual inspection of the forest plots showed that mean depth and mean rate of compressions were consistent across studies, yet those that reported the proportion with correct rate, depth or hand position during compressions were extremely variable, potentially due to observer bias. This highlights the pressing need for recommendations on how to objectively measure the impact of training schoolchildren how to perform CPR, which ideally should include knowledge, skills and some measurement of self-confidence or willingness to help.
A novel finding from our systematic review was that there were no differences in CPR skills between children who were trained by their peers versus those who were instructor-led. To the best of our knowledge, no other systematic review has evaluated this training modality in comparison to instructor-led courses. Numerous studies across health disciplines have found that peer trainers are equally effective as teachers, and can help boost students’ self-confidence.124, 125 In the context of first aid and CPR training, a 2010 study by Carruth et al. used a train-the-trainer model for high school students to teach their peers first aid and risk reduction in rural communities.126 Peer trainers reported improved self-confidence in teaching and that students were more comfortable asking questions, because they were peers and not “traditional” instructors. Using a peer trainer method may help facilitate implementation of CPR training programs in schools, as schoolteacher’s willingness to teach, is often tied to their own perceived CPR proficiency level.14 Additionally, it may be more cost effective and sustainable than hiring certified instructors, which are often cited as a major barrier for schools.127
Limitations
As other reviews have noted, there was a high degree of heterogeneity in the training programs and how outcomes were measured.8, 15, 120 We attempted to explore the causes of this heterogeneity in the RCTs, by examining the effect of age, sex and training modality on CPR performance, but we were limited by the small number of studies reporting them. Additionally, roughly half of the studies included in the final meta-analysis had high risk of bias due to incomplete outcome data. Furthermore, many of the studies we found were observational and spanned a period of almost 50 years. Guidelines on optimal CPR performance and approaches to CPR training have changed substantially since then, thus insight from those studies may not align with present day practice. Lastly, we only included studies written in English.
Conclusion
Our review observed that innovative approaches, such as peer and self-based CPR training are equally effective as instructor-led methods when teaching schoolchildren. While there were statistically significant differences noted in mean depth and rate of compressions between children provided opportunities to engage in practical training and those without, these differences were not clinically relevant. Due to extensive heterogeneity between observational studies, we were unable to meta-analyze the impact of these novel training methods on student self-confidence. Best practice guidance on standardized training and evaluation methods is necessary, in order to consistently and effectively train schoolchildren in CPR.
Funding
This research did not receive any grants from funding agencies in the government, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Katherine S. Allan: Conceptualization, Methodology, Data curation, Writing – original draft, Investigation, Supervision, Writing – review & editing. Bianca Mammarella: Data curation, Methodology, Writing – original draft, Writing – review & editing. Mika'il Visanji: Data curation, Methodology, Writing – original draft, Writing – review & editing. Erinda Moglica: Data curation, Methodology, Writing – original draft, Writing – review & editing. Negin Sadeghlo: Data curation, Methodology, Writing – original draft, Writing – review & editing. Emma O'Neil: Data curation, Methodology, Writing – review & editing. Tiffany T. Chan: Data curation, Methodology, Writing – original draft, Writing – review & editing. Teruko Kishibe: Data curation, Methodology, Writing – original draft, Writing – review & editing. Theresa Aves: Conceptualization, Methodology, Data curation, Writing – original draft, Investigation, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.resplu.2023.100439.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.Panchal A.R., Bartos J.A., Cabanas J.G., et al. Adult B and advanced life support writing G. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;2020(142):S366–S468. doi: 10.1161/CIR.0000000000000916. [DOI] [PubMed] [Google Scholar]
- 2.Song J., Guo W., Lu X., Kang X., Song Y., Gong D. The effect of bystander cardiopulmonary resuscitation on the survival of out-of-hospital cardiac arrests: a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med. 2018;26:86. doi: 10.1186/s13049-018-0552-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindner T.W., Soreide E., Nilsen O.B., Torunn M.W., Lossius H.M. Good outcome in every fourth resuscitation attempt is achievable–an Utstein template report from the Stavanger region. Resuscitation. 2011;82:1508–1513. doi: 10.1016/j.resuscitation.2011.06.016. [DOI] [PubMed] [Google Scholar]
- 4.Wnent J., Bohn A., Seewald S., et al. Bystander resuscitation: the impact of first aid on survival. Anasthesiol Intensivmed Notfallmed Schmerzther. 2013;48:562–565. doi: 10.1055/s-0033-1355238. [DOI] [PubMed] [Google Scholar]
- 5.Wissenberg M., Lippert F.K., Folke F., et al. Association of national initiatives to improve cardiac arrest management with rates of bystander intervention and patient survival after out-of-hospital cardiac arrest. JAMA. 2013;310:1377–1384. doi: 10.1001/jama.2013.278483. [DOI] [PubMed] [Google Scholar]
- 6.Bottiger B.W., Lockey A., Georgiou M., et al. KIDS SAVE LIVES: ERC Position statement on schoolteachers' education and qualification in resuscitation. Resuscitation. 2020;151:87–90. doi: 10.1016/j.resuscitation.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schroeder D.C., Semeraro F., Greif R., et al. Basic life support education for schoolchildren: A narrative review and scientific statement from the international liaison committee on resuscitation. Circulation. 2023;147:1854–1868. doi: 10.1161/CIR.0000000000001128. [DOI] [PubMed] [Google Scholar]
- 8.Plant N., Taylor K. How best to teach CPR to schoolchildren: a systematic review. Resuscitation. 2013;84:415–421. doi: 10.1016/j.resuscitation.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Bohn A., Lukas R.P., Breckwoldt J., Bottiger B.W., Van Aken H. 'Kids save lives': why schoolchildren should train in cardiopulmonary resuscitation. Curr Opin Crit Care. 2015;21:220–225. doi: 10.1097/MCC.0000000000000204. [DOI] [PubMed] [Google Scholar]
- 10.Bray J., Acworth J., Page G., et al. Aussie KIDS SAVE LIVES: A position statement from the Australian Resuscitation Council and supported by stakeholders. Emerg Med Australas. 2021;33:944–946. doi: 10.1111/1742-6723.13840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Del Rios M., Han J., Cano A., et al. Pay It Forward: High School Video-based Instruction Can Disseminate CPR Knowledge in Priority Neighborhoods. West J Emerg Med. 2018;19:423–429. doi: 10.5811/westjem.2017.10.35108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pivac S., Gradisek P., Skela-Savic B. The impact of cardiopulmonary resuscitation (CPR) training on schoolchildren and their CPR knowledge, attitudes toward CPR, and willingness to help others and to perform CPR: mixed methods research design. BMC Public Health. 2020;20:11. doi: 10.1186/s12889-020-09072-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ecker H., Schroeder D.C., Böttiger B.W. “Kids save lives” – School resuscitation programs worldwide and WHO initiative for this. Trends Anaesthesia Critical Care. 2015;5:163–166. [Google Scholar]
- 14.Wingen S., Jeck J., Schroeder D.C., Wingen-Heimann S.M., Drost R., Bottiger B.W. Facilitators and barriers for the implementation of resuscitation training programmes for schoolchildren: A systematic review. Eur J Anaesthesiol. 2022;39:711–719. doi: 10.1097/EJA.0000000000001643. [DOI] [PubMed] [Google Scholar]
- 15.Lim X.M.A., Liao W.A., Wang W., Seah B. The effectiveness of technology-based cardiopulmonary resuscitation training on the skills and knowledge of adolescents: systematic review and meta-analysis. J Med Internet Res. 2022;24 doi: 10.2196/36423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tse E., Plakitsi K., Voulgaris S., Alexiou G.A. The role of a first aid training program for young children: A systematic review. Children (Basel) 2023:10. doi: 10.3390/children10030431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wyckoff M.H., Singletary E.M., Soar J., et al. 2021 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; neonatal Life support; education, implementation, and teams; first aid task forces; and the COVID-19 working group. Resuscitation. 2021;169:229–311. doi: 10.1016/j.resuscitation.2021.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA. Cochrane handbook for systematic reviews of interventions. 2022.
- 19.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6 [PMC free article] [PubMed] [Google Scholar]
- 20.McGowan J., Sampson M., Salzwedel D.M., Cogo E., Foerster V., Lefebvre C. PRESS peer review of electronic search strategies: 2015 guideline statement. J Clin Epidemiol. 2016;75:40–46. doi: 10.1016/j.jclinepi.2016.01.021. [DOI] [PubMed] [Google Scholar]
- 21.Higgins J.P., Altman D.G., Gotzsche P.C., et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011;343 doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.(EPOC). CEPaOoC. EPOC Resources for review authors. 2017;2020.
- 23.Hozo S.P., Djulbegovic B., Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. doi: 10.1186/1471-2288-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins J.P., Thompson S.G. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 25.Abelairas-Gomez C., Martinez-Isasi S., Barcala-Furelos R., et al. Training frequency for educating schoolchildren in basic life support: very brief 4-month rolling-refreshers versus annual retraining-a 2-year prospective longitudinal trial. BMJ Open. 2021;11:e052478. doi: 10.1136/bmjopen-2021-052478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barsom E.Z., Duijm R.D., Dusseljee-Peute L.W.P., et al. Cardiopulmonary resuscitation training for high school students using an immersive 360-degree virtual reality environment. Br J Educ Technol. 2020;51:2050–2062. [Google Scholar]
- 27.Beck S., Issleib M., Daubmann A., Zollner C. Peer education for BLS-training in schools? Results of a randomized-controlled, noninferiority trial. Resuscitation. 2015;94:85–90. doi: 10.1016/j.resuscitation.2015.06.026. [DOI] [PubMed] [Google Scholar]
- 28.Beskind D.L., Stolz U., Thiede R., et al. Viewing a brief chest-compression-only CPR video improves bystander CPR performance and responsiveness in high school students: A cluster randomized trial. Resuscitation. 2016;104:28–33. doi: 10.1016/j.resuscitation.2016.03.022. [DOI] [PubMed] [Google Scholar]
- 29.Chamdawala H., Meltzer J.A., Shankar V., Elachi D., Jarzynka S.M., Nixon A.F. Cardiopulmonary resuscitation skill training and retention in teens (CPR START): A randomized control trial in high school students. Resusc Plus. 2021;5:8. doi: 10.1016/j.resplu.2021.100079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cuijpers P.J., Bookelman G., Kicken W., de Vries W., Gorgels A.P. Medical students and physical education students as CPR instructors: an appropriate solution to the CPR-instructor shortage in secondary schools? Neth Heart J. 2016;24:456–461. doi: 10.1007/s12471-016-0838-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Desailly V HDPPBPIPHJMCCAECTTMJRDRJ. The use of the serious game Stayingalive(R) at school improves basic life support performed by secondary pupils: a randomized controlled study. Annals Intensive Care. 2017;7:64.
- 32.Doucet L., Lammens R., Hendrickx S., Dewolf P. App-based learning as an alternative for instructors in teaching basic life support to school children: a randomized control trial. Acta Clin Belg. 2019;74:317–325. doi: 10.1080/17843286.2018.1500766. [DOI] [PubMed] [Google Scholar]
- 33.Greer N.M.C.M.D. Assessment of CPR performance by 13 to 14-year-old schoolchildren after a single 2 h training session. Heart. 2010;96:A28. [Google Scholar]
- 34.Han S., Park H.J., Nah S., et al. Instructor-led distance learning for training students in cardiopulmonary resuscitation: A randomized controlled study. PLoS One. 2021;16 doi: 10.1371/journal.pone.0251277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.He D.X., Huang K.S., Yang Y.I., Jiang W., Yang N.L., Yang H. What is the Optimal Age for Students to Receive Cardiopulmonary Resuscitation Training? Prehospital Disaster Med. 2018;33:394–398. doi: 10.1017/S1049023X1800047X. [DOI] [PubMed] [Google Scholar]
- 36.Hill K., Mohan C., Stevenson M., McCluskey D. Objective assessment of cardiopulmonary resuscitation skills of 10–11-year-old schoolchildren using two different external chest compression to ventilation ratios. Resuscitation. 2009;80:96–99. doi: 10.1016/j.resuscitation.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 37.Iserbyt P., Byra M. The design of instructional tools affects secondary school students' learning of cardiopulmonary resuscitation (CPR) in reciprocal peer learning: a randomized controlled trial. Resuscitation. 2013;84:1591–1595. doi: 10.1016/j.resuscitation.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 38.Iserbyt P., Charlier N., Mols L. Learning basic life support (BLS) with tablet PCs in reciprocal learning at school: are videos superior to pictures? A randomized controlled trial. Resuscitation. 2014;85:809–813. doi: 10.1016/j.resuscitation.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 39.Iserbyt P., Madou T. The effect of content knowledge and repeated teaching on teaching and learning basic life support: a cluster randomised controlled trial. Acta Cardiol. 2021:1–10. doi: 10.1080/00015385.2021.1969109. [DOI] [PubMed] [Google Scholar]
- 40.Kaweenuttayanon N., Phungoen P., Kotruchin P., Ianghong K., Chantawattanaruk S., Pongchaiyakul C. Defining the optimal age for basic life support and cardiac compression training in Thai Adolescents. J Med Assoc Thai. 2017;100:967–971. [Google Scholar]
- 41.Kesici S., Bayrakci Z., Birbilen A.Z., et al. Peer education model for basic life support training among high school children: A randomized trial. Prehosp Disaster Med. 2021;36:553–560. doi: 10.1017/S1049023X21000674. [DOI] [PubMed] [Google Scholar]
- 42.Kherbeche H., Exer N., Schuhwerk W., Ummenhofer W., Osterwalder J. Chest compression using the foot or hand method: a prospective, randomized, controlled manikin study with school children. Eur J Emerg Med. 2017;24:262–267. doi: 10.1097/MEJ.0000000000000335. [DOI] [PubMed] [Google Scholar]
- 43.Kim Se LSJNHLDHKCW. Is there any difference in cardiopulmonary resuscitation performance according to different instructional models of cardiopulmonary resuscitation education for junior and senior high school students? Hong Kong J Emergency Med. 2011;18:375.
- 44.Li H., Shen X., Xu X., et al. Bystander cardiopulmonary resuscitation training in primary and secondary school children in China and the impact of neighborhood socioeconomic status: A prospective controlled trial. Medicine (Baltimore) 2018;97 doi: 10.1097/MD.0000000000012673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lorem T., Steen P.A., Wik L. High school students as ambassadors of CPR–a model for reaching the most appropriate target population? Resuscitation. 2010;81:78–81. doi: 10.1016/j.resuscitation.2009.09.030. [DOI] [PubMed] [Google Scholar]
- 46.Martinez-Isasi S., Garcia-Suarez M., De La Pena Rodriguez M.A., et al. Basic life support training programme in schools by school nurses: How long and how often to train? Medicine. 2021;100 doi: 10.1097/MD.0000000000024819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Napp A., Kosan J., Hoffend C., et al. Implementation of basic life support training for school children: Online education for potential instructors? Results of a cluster randomised, controlled, non-inferiority trial. Resuscitation. 2020;152:141–148. doi: 10.1016/j.resuscitation.2020.04.041. [DOI] [PubMed] [Google Scholar]
- 48.Nord A., Hult H., Kreitz-Sandberg S., Herlitz J., Svensson L., Nilsson L. Effect of two additional interventions, test and reflection, added to standard cardiopulmonary resuscitation training on seventh grade students' practical skills and willingness to act: a cluster randomised trial. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-014230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nord A., Svensson L., Claesson A., et al. The effect of a national web course “Help-Brain-Heart” as a supplemental learning tool before CPR training: a cluster randomised trial. Scand J Trauma Resusc Emerg Med. 2017;25:93. doi: 10.1186/s13049-017-0439-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nord A., Svensson L., Hult H., Kreitz-Sandberg S., Nilsson L. Effect of mobile application-based versus DVD-based CPR training on students' practical CPR skills and willingness to act: a cluster randomised study. BMJ Open. 2016;6 doi: 10.1136/bmjopen-2015-010717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Onan A., Turan S., Elcin M., Erbil B., Bulut S.C. The effectiveness of traditional Basic Life Support training and alternative technology-enhanced methods in high schools. Hong Kong J Emergency Med. 2019;26:44–52. [Google Scholar]
- 52.Otero-Agra M., Barcala-Furelos R., Besada-Saavedra I., Peixoto-Pino L., Martinez-Isasi S., Rodriguez-Nunez A. Let the kids play: gamification as a CPR training methodology in secondary school students. A quasi-experimental manikin simulation study. Emerg Med J. 2019;36:653–659. doi: 10.1136/emermed-2018-208108. [DOI] [PubMed] [Google Scholar]
- 53.Otero-Agra M R-NAREA-GCB-SIA-OAPL-GSM-CJLB-F. What biomechanical factors are more important in compression depth for children lifesavers? A randomized crossover study. Am J Emergency Med. 2019;37:100. [DOI] [PubMed]
- 54.Oulego-Erroz I., Busto-Cuinas M., Garcia-Sanchez N., Rodriguez-Blanco S., Rodriguez-Nunez A. A popular song improves CPR compression rate and skill retention by schoolchildren: a manikin trial. Resuscitation. 2011;82:499–500. doi: 10.1016/j.resuscitation.2011.01.001. [DOI] [PubMed] [Google Scholar]
- 55.Reder S., Cummings P., Quan L. Comparison of three instructional methods for teaching cardiopulmonary resuscitation and use of an automatic external defibrillator to high school students. Resuscitation. 2006;69:443–453. doi: 10.1016/j.resuscitation.2005.08.020. [DOI] [PubMed] [Google Scholar]
- 56.Sabihah A., Shamsuriani M.J., Fadzlon M.Y., et al. Peer trainers compared with basic life support trainers in delivering effective cardiopulmonary resuscitation training to secondary school students. Med Health (Universiti Kebangsaan Malaysia) 2020;15:88–95. [Google Scholar]
- 57.Santomauro M., Iaccarino V., Riganti C., et al. Future perspective in BLSD Training: The importance of peer-to peer education in high school students. J Translat Sci. 2018;5:1–6. [Google Scholar]
- 58.Schmitz B., Schuffelen P., Kreijns K., Klemke R., Specht M. Putting yourself in someone else's shoes: The impact of a location-based, collaborative role-playing game on behaviour. Comput Educ. 2015;85:160–169. [Google Scholar]
- 59.Suss-Havemann C., Kosan J., Seibold T., et al. Implementation of Basic Life Support training in schools: a randomised controlled trial evaluating self-regulated learning as alternative training concept. BMC Public Health. 2020;20:9. doi: 10.1186/s12889-020-8161-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Tanaka S., Hara T., Tsukigase K., et al. A pilot study of Practice While Watch based 50 min school quality cardiopulmonary resuscitation classroom training: a cluster randomized control trial. Acute Med Surg. 2020;7:e455. doi: 10.1002/ams2.455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Van Raemdonck V., Monsieurs K.G., Aerenhouts D., De Martelaer K. Teaching basic life support: a prospective randomized study on low-cost training strategies in secondary schools. Eur J Emerg Med. 2014;21:284–290. doi: 10.1097/MEJ.0000000000000071. [DOI] [PubMed] [Google Scholar]
- 62.Vanderschmidt H., Burnap T.K., Thwaites J.K. Evaluation of a cardiopulmonary resuscitation course for secondary schools. Med Care. 1975;13:763–774. doi: 10.1097/00005650-197509000-00006. [DOI] [PubMed] [Google Scholar]
- 63.Vanderschmidt H., Burnap T.K., Thwaites J.K. Evaluation of a cardiopulmonary resuscitation course for secondary schools retention study. Med Care. 1976;14:181–184. doi: 10.1097/00005650-197602000-00008. [DOI] [PubMed] [Google Scholar]
- 64.Watanabe K., Lopez-Colon D., Shuster J.J., Philip J. Efficacy and retention of Basic Life Support education including Automated External Defibrillator usage during a physical education period. Prev Med Rep. 2017;5:263–267. doi: 10.1016/j.pmedr.2017.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Weidenauer D., Hamp T., Schriefl C., et al. The impact of cardiopulmonary resuscitation (CPR) manikin chest stiffness on motivation and CPR performance measures in children undergoing CPR training-A prospective, randomized, single-blind, controlled trial. PLoS One. 2018;13 doi: 10.1371/journal.pone.0202430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wingen S., Schroeder D.C., Ecker H., et al. Self-confidence and level of knowledge after cardiopulmonary resuscitation training in 14 to 18-year-old schoolchildren: A randomised-interventional controlled study in secondary schools in Germany. Eur J Anaesthesiol. 2018;35:519–526. doi: 10.1097/EJA.0000000000000766. [DOI] [PubMed] [Google Scholar]
- 67.Yeung J., Kovic I., Vidacic M., Skilton E., Higgins D., Melody T., Lockey A. The school Lifesavers study-A randomised controlled trial comparing the impact of Lifesaver only, face-to-face training only, and Lifesaver with face-to-face training on CPR knowledge, skills and attitudes in UK school children. Resuscitation. 2017;120:138–145. doi: 10.1016/j.resuscitation.2017.08.010. [DOI] [PubMed] [Google Scholar]
- 68.Abelairas-Gomez C., Rodriguez-Nunez A., Casillas-Cabana M., Romo-Perez V., Barcala-Furelos R. Schoolchildren as life savers: at what age do they become strong enough? Resuscitation. 2014;85:814–819. doi: 10.1016/j.resuscitation.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 69.Banfai B., Pandur A., Schiszler B., Pek E., Radnai B., Banfai-Csonka H., Betlehem J. Little lifesavers: Can we start first aid education in kindergarten? - A longitudinal cohort study. Health Educ J. 2018;77:1007–1017. [Google Scholar]
- 70.Banfai B., Pek E., Pandur A., Csonka H., Betlehem J. 'The year of first aid': effectiveness of a 3-day first aid programme for 7–14-year-old primary school children. Emerg Med J. 2017;34:526–532. doi: 10.1136/emermed-2016-206284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Berthelot S., Plourde M., Bertrand I., et al. Push hard, push fast: quasi-experimental study on the capacity of elementary schoolchildren to perform cardiopulmonary resuscitation. Scand J Trauma Resusc Emerg Med. 2013;21:41. doi: 10.1186/1757-7241-21-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Chan C.Y., Ko H.F., Chan O.Y., Tang T.H., Ching C.Y., Tsui S.Y. Could Hong Kong primary schoolchildren be taught to perform compression-only CPR: A pilot study. Hong Kong J Emerg Med. 2017;24:67–72. [Google Scholar]
- 73.Contri E., Baggiani M., Bonomo M.C., Tonani M., Fichtner F.E., Cornara S., Baldi E. Video-based compression-only CPR teaching: A feasible and effective way to spread CPR in secondary schools. Resuscitation. 2016;106:e60–e. [Google Scholar]
- 74.Fleischhackl R., Nuernberger A., Sterz F., et al. School children sufficiently apply life supporting first aid: a prospective investigation. Crit Care. 2009;13:R127. doi: 10.1186/cc7984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Hori S., Suzuki M., Yamazaki M., Aikawa N., Yamazaki H. Cardiopulmonary resuscitation training in schools: A comparison of trainee satisfaction among different age groups. Keio J Med. 2016;65:49–56. doi: 10.2302/kjm.2015-0009-OA. [DOI] [PubMed] [Google Scholar]
- 76.Isbye D.L., Meyhoff C.S., Lippert F.K., Rasmussen L.S. Skill retention in adults and in children 3 months after basic life support training using a simple personal resuscitation manikin. Resuscitation. 2007;74:296–302. doi: 10.1016/j.resuscitation.2006.12.012. [DOI] [PubMed] [Google Scholar]
- 77.Jones I., Whitfield R., Colquhoun M., Chamberlain D., Vetter N., Newcombe R. At what age can schoolchildren provide effective chest compressions? An observational study from the Heartstart UK schools training programme. BMJ. 2007;334:1201. doi: 10.1136/bmj.39167.459028.DE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kalluri N.S., Knopov A., Kue R. A service-learning initiative to teach hands-only CPR to high school students: PumpStart. J Educ. 2018;198:240–246. [Google Scholar]
- 79.Kelley J., Richman P.B., Ewy G.A., Clark L., Bulloch B., Bobrow B.J. Eighth grade students become proficient at CPR and use of an AED following a condensed training programme. Resuscitation. 2006;71:229–236. doi: 10.1016/j.resuscitation.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 80.Lester C., Donnelly P., Weston C. Is peer tutoring beneficial in the context of school resuscitation training? Health Educ Res. 1997;12:347–354. doi: 10.1093/her/12.3.347. [DOI] [PubMed] [Google Scholar]
- 81.Mathew R., Sahu A.K., Thakur N., Katyal A., Bhoi S., Aggarwal P. Hands-only cardiopulmonary resuscitation training for schoolchildren: A comparison study among different class groups. Turkish J Emerg Med. 2020;20:186–192. doi: 10.4103/2452-2473.297464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mpotos N., Iserbyt P. Children saving lives: Training towards CPR excellence levels in chest compression based on age and physical characteristics. Resuscitation. 2017;121:135–140. doi: 10.1016/j.resuscitation.2017.10.024. [DOI] [PubMed] [Google Scholar]
- 83.Paglino M, Contri E, Tonani M, Costantini G, Baggiani M, Bonomo MC, Baldi E. ScuolaSalvaVita.it (“SchoolSavesLifes.it”): How to teach effectively CPR in all the secondary schools of a whole province. Resuscitation. 2017;118:e25–e25.
- 84.Ramesh A.C., Hariprasad K.V., Abhishek K.B., Murthy M.R.K., Edison M., Hoek T.L.V. Teaching Hands-Only CPR (HOCPR) skills to 8th-grade students in urban Bengaluru: Development of a comprehensive Hands-Only CPR programme for high school students. Indian J Anaesthesia. 2022;66:140–145. doi: 10.4103/ija.ija_685_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Schuffelen P, Sijmons J, Ghossein A, Amin H, Weerts J, Gorgels A. Annual CPR-training can provide secondary school students with the essential skills – A three-year cohort study in The Netherlands monitoring the quality of their CPR-skills. Resuscitation. 2015;96:91–91.
- 86.So K.Y., Ko H.F., Tsui C.S.Y., Yeung C.Y., Chu Y.C., Lai V.K.W., Lee A. Brief compression-only cardiopulmonary resuscitation and automated external defibrillator course for secondary school students: a multischool feasibility study. BMJ Open. 2020;10 doi: 10.1136/bmjopen-2020-040469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Suwanpairoj C., Wongsombut T., Maisawat K., et al. Outcome of basic life support training among primary school students in Southeast Asia. Clin Expe Emerg Med. 2020;7:245–249. doi: 10.15441/ceem.19.095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Uhm T.H., Oh J.K., Park J.H., Yang S.J., Kim J.H. Correlation between physical features of elementary school children and chest compression depth. Hong Kong J Emerg Med. 2010;17:218–223. [Google Scholar]
- 89.Uzendu A., Pagliaro J., Betancourt J., Egun C., Drachman D., Bhatt A., Chan P. Make Basic Life Support Basic: A novel virtual Hands Only CPR training program in minority school age youth. Resuscitation. 2021;167:93–94. doi: 10.1016/j.resuscitation.2021.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wang M.-F., Wu Y.-K., Chien C.-Y., et al. Learning effectiveness assessment between primary school students and adults in basic life support education. Emerg Med Int. 2021;2021 doi: 10.1155/2021/5579402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Younas S., Raynes A., Morton S., Mackway-Jones K. An evaluation of the effectiveness of the Opportunities for Resuscitation and Citizen Safety (ORCS) defibrillator training programme designed for older school children. Resuscitation. 2006;71:222–228. doi: 10.1016/j.resuscitation.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 92.Zalewski T., Jedrzejek M., Kazimierczak A., Nikodemski T. Knowledge level in four years after completion of Cardiopulmonary Resuscitation Training Program among students attending Safety Education Classes in Polish State Schools. Resuscitation. 2016;106:e57–e. [Google Scholar]
- 93.Zeleke B.G., Biswas E.S., Biswas M. Teaching Cardiopulmonary Resuscitation to Young Children (<12 Years Old) Am J Cardiol. 2019;123:1626–1627. doi: 10.1016/j.amjcard.2019.02.011. [DOI] [PubMed] [Google Scholar]
- 94.Borovnik Lesjak V, Sorgo A, Strnad M. Retention of knowledge and skills after a basic life support course for schoolchildren: A prospective study. Inquiry : J Med Care Organ, Provision Financ. 2022;59:469580221098755. [DOI] [PMC free article] [PubMed]
- 95.Chang J, Biswas A, Iftikhar S, Gelman S and Biswas M. The impact of video-based instruction on CPR knowledge in elementary school students (10-11 years). Eur Heart J. 2022;43:688–688.
- 96.Damvall D.A., Birkenes T.S., Nilsen K., Haaland S.H., Myklebust H., Nordseth T. Can high school students teach their peers high quality cardiopulmonary resuscitation (CPR)? Resuscitation Plus. 2022;10 doi: 10.1016/j.resplu.2022.100250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Oliveira K.M.G., Carmona M.J.C., Mansur A.P., et al. CPR Quality Assessment in Schoolchildren Training. J Cardiovasc Develop Dis. 2022;9 doi: 10.3390/jcdd9110398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Abelsson A., Odestrand P., Nygardh A. To strengthen self-confidence as a step in improving prehospital youth laymen basic life support. BMC Emerg Med. 2020;20:8. doi: 10.1186/s12873-020-0304-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Akiteru T., Mari M., Sayori I., Kaori M., Yusuke R., Yuna I., Ariyuki H. Factors affecting the training of basic life support for school children. Int Med J. 2022;29:59–63. [Google Scholar]
- 100.Aloush S, Tubaishat A, M AL, Suliman M, Alrimawi I, Al Sabah A, Banikhaled Y. Effectiveness of Basic Life Support Training for Middle School Students. J Sch Nurs. 2018:1059840517753879. [DOI] [PubMed]
- 101.Andresen M., Castro R., Hasbun P., Rojas L., Sarfatis A., Riquelme A. Immediate cardiac arrest resuscitation skills are acquired in 8th grade students during normal class hours with a low-cost, short-term, self-instruction video. Resuscitation. 2012;83:e156–e157. doi: 10.1016/j.resuscitation.2012.03.035. [DOI] [PubMed] [Google Scholar]
- 102.Banfai B., Pandur A., Schiszler B., Pek E., Radnai B., Csonka H., Betlehem J. 'The (second) year of first aid': a 15-month follow-up after a 3-day first aid programme. Emerg Med J. 2019;36:666–669. doi: 10.1136/emermed-2018-208110. [DOI] [PubMed] [Google Scholar]
- 103.Bohn A., Van Aken H.K., Mollhoff T., et al. Teaching resuscitation in schools: annual tuition by trained teachers is effective starting at age 10. A four-year prospective cohort study. Resuscitation. 2012;83:619–625. doi: 10.1016/j.resuscitation.2012.01.020. [DOI] [PubMed] [Google Scholar]
- 104.Brown L.E., Carroll T., Lynes C., Tripathi A., Halperin H., Dillon W.C. CPR skill retention in 795 high school students following a 45-minute course with psychomotor practice. Am J Emerg Med. 2018;36:1110–1112. doi: 10.1016/j.ajem.2017.10.026. [DOI] [PubMed] [Google Scholar]
- 105.Dumcke R., Rahe-Meyer N., Wegner C. Does age still matter? An age-group comparison of self-efficacy, initial interest and performance when learning bystander resuscitation in secondary schools. Int J First Aid Educ. 2021;4:5–22. [Google Scholar]
- 106.Gabriel I.O., Aluko J.O. Theoretical knowledge and psychomotor skill acquisition of basic life support training programme among secondary school students. World J Emerg Med. 2019;10:81–87. doi: 10.5847/wjem.j.1920-8642.2019.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kłosiewicz T., Zalewski R., Szkudlarek W., Węglewska M., Purandare B., Puślecki M. Quality of chest compressions performed by school-age children – a quasi-experimental simulation-based study. Med Res J (2451–2591) 2021;6:295–300. [Google Scholar]
- 108.Lanzas D., Nunes P., Perelman J. Training program in resuscitation maneuvers delivered by teachers in a school setting: An economic argument. Rev Port Cardiol. 2022;41:135–144. doi: 10.1016/j.repc.2021.02.015. [DOI] [PubMed] [Google Scholar]
- 109.Lorem T., Palm A., Wik L. Impact of a self-instruction CPR kit on 7th graders' and adults' skills and CPR performance. Resuscitation. 2008;79:103–108. doi: 10.1016/j.resuscitation.2008.04.030. [DOI] [PubMed] [Google Scholar]
- 110.Martinez-Isasi S., Abelairas-Gomez C., Pichel-Lopez M., et al. Learning to resuscitate at school. Study in 8–12 year-old schoolchildren. Anales de pediatria. 2022;96:17–24. doi: 10.1016/j.anpede.2020.09.013. [DOI] [PubMed] [Google Scholar]
- 111.Meissner T.M., Kloppe C., Hanefeld C. Basic life support skills of high school students before and after cardiopulmonary resuscitation training: a longitudinal investigation. Scand J Trauma Resusc Emerg Med. 2012;20:31. doi: 10.1186/1757-7241-20-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Metelmann C., Metelmann B., Schuffert L., Hahnenkamp K., Vollmer M., Brinkrolf P. Smartphone apps to support laypersons in bystander CPR are of ambivalent benefit: a controlled trial using medical simulation. Scand J Trauma Resusc Emerg Med. 2021;29:76. doi: 10.1186/s13049-021-00893-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Naqvi S., Siddiqi R., Hussain S.A., Batool H., Arshad H. School children training for basic life support. J Coll Physicians Surg Pak. 2011;21:611–615. doi: 10.2011/JCPSP.611615. [DOI] [PubMed] [Google Scholar]
- 114.Paglino M., Contri E., Baggiani M., Tonani M., Costantini G., Bonomo M.C., Baldi E. A video-based training to effectively teach CPR with long-term retention: the ScuolaSalvaVita.it (“SchoolSavesLives.it”) project. Intern. 2019;14:275–279. doi: 10.1007/s11739-018-1946-3. [DOI] [PubMed] [Google Scholar]
- 115.Semeraro F., Frisoli A., Loconsole C., et al. Kids (learn how to) save lives in the school with the serious game Relive. Resuscitation. 2017;116:27–32. doi: 10.1016/j.resuscitation.2017.04.038. [DOI] [PubMed] [Google Scholar]
- 116.Vetter V.L., Haley D.M., Dugan N.P., Iyer V.R., Shults J. Innovative cardiopulmonary resuscitation and automated external defibrillator programs in schools: Results from the Student Program for Olympic Resuscitation Training in Schools (SPORTS) study. Resuscitation. 2016;104:46–52. doi: 10.1016/j.resuscitation.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 117.Yeow M.W.X., Ng J.Y.X., Nguyen V.H., et al. Knowledge and attitudes of Vietnamese high school students towards cardiopulmonary resuscitation: Results from a pilot student-led cross-country bystander training workshop. Proc Singapore Healthcare. 2021 [Google Scholar]
- 118.Cons-Ferreiro M., Mecias-Calvo M., Romo-Perez V., Navarro-Paton R. The effects of an intervention based on the flipped classroom on the learning of basic life support in schoolchildren aged 10-13 Years: A quasi-experimental study. Children (Basel, Switzerland) 2022;9 doi: 10.3390/children9091373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Martins I., Nakano G.S., Nakano M.S., et al. Kids save hearts project: hands-only cardiopulmonary resuscitation training for schoolchildren. Circulation. 2022;146:3. [Google Scholar]
- 120.Eastwood K HS, Nguyen A, Han C, Seneviratne J, Bray J. A systematic review of digital-based basic life support training: EIT 647 task force systematic review. 2021.
- 121.Stiell I.G., Brown S.P., Nichol G., et al. Idris AH and Resuscitation Outcomes Consortium I. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. 2014;130:1962–1970. doi: 10.1161/CIRCULATIONAHA.114.008671. [DOI] [PubMed] [Google Scholar]
- 122.Idris A.H., Guffey D., Pepe P.E., et al. Aufderheide TP and Resuscitation Outcomes Consortium I. Chest compression rates and survival following out-of-hospital cardiac arrest. Crit Care Med. 2015;43:840–848. doi: 10.1097/CCM.0000000000000824. [DOI] [PubMed] [Google Scholar]
- 123.Zenani N.E., Bello B., Molekodi M., Useh U. Effectiveness of school-based CPR training among adolescents to enhance knowledge and skills in CPR: A systematic review. Curationis. 2022;45:e1–e9. doi: 10.4102/curationis.v45i1.2325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Secomb J. A systematic review of peer teaching and learning in clinical education. J Clin Nurs. 2008;17:703–716. doi: 10.1111/j.1365-2702.2007.01954.x. [DOI] [PubMed] [Google Scholar]
- 125.Rees E.L., Quinn P.J., Davies B., Fotheringham V. How does peer teaching compare to faculty teaching? A systematic review and meta-analysis (.) Med Teach. 2016;38:829–837. doi: 10.3109/0142159X.2015.1112888. [DOI] [PubMed] [Google Scholar]
- 126.Carruth A.K., Pryor S., Cormier C., Bateman A., Matzke B., Gilmore K. Evaluation of a school-based train-the-trainer intervention program to teach first aid and risk reduction among high school students. J Sch Health. 2010;80:453–460. doi: 10.1111/j.1746-1561.2010.00527.x. [DOI] [PubMed] [Google Scholar]
- 127.Dumcke R, Wegner C, Böttiger B, Kucknat L, Rahe-Meyer N. The process of implementing cardiopulmonary resuscitation training in schools: A review of current research. 2020:141–166.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.