This cohort study examines trends in inpatient and outpatient gender-affirming surgical procedures in the US and explores the temporal trends in the types of procedures across age groups.
Key Points
Question
What are the temporal trends in gender-affirming surgery (GAS) in the US?
Findings
In this cohort study of 48 019 patients, GAS increased significantly, nearly tripling from 2016 to 2019. Breast and chest surgery was the most common class of procedures performed overall; genital reconstructive procedures were more common among older individuals.
Meaning
These findings suggest that there will be a greater need for clinicians knowledgeable in the care of transgender individuals with the requisite expertise to perform gender-affirming procedures.
Abstract
Importance
While changes in federal and state laws mandating coverage of gender-affirming surgery (GAS) may have led to an increase in the number of annual cases, comprehensive data describing trends in both inpatient and outpatient procedures are limited.
Objective
To examine trends in inpatient and outpatient GAS procedures in the US and to explore the temporal trends in the types of GAS performed across age groups.
Design, Setting, and Participants
This cohort study includes data from 2016 to 2020 in the Nationwide Ambulatory Surgery Sample and the National Inpatient Sample. Patients with diagnosis codes for gender identity disorder, transsexualism, or a personal history of sex reassignment were identified, and the performance of GAS, including breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures, were identified.
Main Outcome Measures
Weighted estimates of the annual number of inpatient and outpatient procedures performed and the distribution of each class of procedure overall and by age were analyzed.
Results
A total of 48 019 patients who underwent GAS were identified, including 25 099 (52.3%) who were aged 19 to 30 years. The most common procedures were breast and chest procedures, which occurred in 27 187 patients (56.6%), followed by genital reconstruction (16 872 [35.1%]) and other facial and cosmetic procedures (6669 [13.9%]). The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020. Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged12 to 18 years. When stratified by the type of procedure performed, breast and chest procedures made up a greater percentage of the surgical interventions in younger patients, while genital surgical procedures were greater in older patients.
Conclusions and Relevance
Performance of GAS has increased substantially in the US. Breast and chest surgery was the most common group of procedures performed. The number of genital surgical procedures performed increased with increasing age.
Introduction
Gender dysphoria is characterized as an incongruence between an individual’s experienced or expressed gender and the gender that was assigned at birth.1 Transgender individuals may pursue multiple treatments, including behavioral therapy, hormonal therapy, and gender-affirming surgery (GAS).2 GAS encompasses a variety of procedures that align an individual patient’s gender identity with their physical appearance.2,3,4
While numerous surgical interventions can be considered GAS, the procedures have been broadly classified as breast and chest surgical procedures, facial and cosmetic interventions, and genital reconstructive surgery.2,4 Prior studies2,3,4,5,6,7 have shown that GAS is associated with improved quality of life, high rates of satisfaction, and a reduction in gender dysphoria. Furthermore, some studies have reported that GAS is associated with decreased depression and anxiety.8 Lastly, the procedures appear to be associated with acceptable morbidity and reasonable rates of perioperative complications.2,4
Given the benefits of GAS, the performance of GAS in the US has increased over time.9 The increase in GAS is likely due in part to federal and state laws requiring coverage of transition-related care, although actual insurance coverage of specific procedures is variable.10,11 While prior work has shown that the use of inpatient GAS has increased, national estimates of inpatient and outpatient GAS are lacking.9 This is important as many GAS procedures occur in ambulatory settings. We performed a population-based analysis to examine trends in GAS in the US and explored the temporal trends in the types of GAS performed across age groups.
Methods
Data Sources
To capture both inpatient and outpatient surgical procedures, we used data from the Nationwide Ambulatory Surgery Sample (NASS) and the National Inpatient Sample (NIS). NASS is an ambulatory surgery database and captures major ambulatory surgical procedures at nearly 2800 hospital-owned facilities from up to 35 states, approximating a 63% to 67% stratified sample of hospital-owned facilities. NIS comprehensively captures approximately 20% of inpatient hospital encounters from all community hospitals across 48 states participating in the Healthcare Cost and Utilization Project (HCUP), covering more than 97% of the US population. Both NIS and NASS contain weights that can be used to produce US population estimates.12,13 Informed consent was waived because data sources contain deidentified data, and the study was deemed exempt by the Columbia University institutional review board. This cohort study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Patients and Procedures
We selected patients of all ages with an International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) diagnosis codes for gender identity disorder or transsexualism (ICD-10 F64) or a personal history of sex reassignment (ICD-10 Z87.890) from 2016 to 2020 (eTable in Supplement 1). We first examined all hospital (NIS) and ambulatory surgical (NASS) encounters for patients with these codes and then analyzed encounters for GAS within this cohort. GAS was identified using ICD-10 procedure codes and Common Procedural Terminology codes and classified as breast and chest procedures, genital reconstructive procedures, and other facial and cosmetic surgical procedures.2,4 Breast and chest surgical procedures encompassed breast reconstruction, mammoplasty and mastopexy, or nipple reconstruction. Genital reconstructive procedures included any surgical intervention of the male or female genital tract. Other facial and cosmetic procedures included cosmetic facial procedures and other cosmetic procedures including hair removal or transplantation, liposuction, and collagen injections (eTable in Supplement 1). Patients might have undergone procedures from multiple different surgical groups. We measured the total number of procedures and the distribution of procedures within each procedural group.
Within the data sets, sex was based on patient self-report. The sex of patients in NIS who underwent inpatient surgery was classified as either male, female, missing, or inconsistent. The inconsistent classification denoted patients who underwent a procedure that was not consistent with the sex recorded on their medical record. Similar to prior analyses, patients in NIS with a sex variable not compatible with the procedure performed were classified as having undergone genital reconstructive surgery (GAS not otherwise specified).9
Covariates
Clinical variables in the analysis included patient clinical and demographic factors and hospital characteristics. Demographic characteristics included age at the time of surgery (12 to 18 years, 19 to 30 years, 31 to 40 years, 41 to 50 years, 51 to 60 years, 61 to 70 years, and older than 70 years), year of the procedure (2016-2020), and primary insurance coverage (private, Medicare, Medicaid, self-pay, and other). Race and ethnicity were only reported in NIS and were classified as White, Black, Hispanic and other. Race and ethnicity were considered in this study because prior studies have shown an association between race and GAS. The income status captured national quartiles of median household income based of a patient’s zip code and was recorded as less than 25% (low), 26% to 50% (medium-low), 51% to 75% (medium-high), and 76% or more (high). The Elixhauser Comorbidity Index was estimated for each patient based on the codes for common medical comorbidities and weighted for a final score.14 Patients were classified as 0, 1, 2, or 3 or more. We separately reported coding for HIV and AIDS; substance abuse, including alcohol and drug abuse; and recorded mental health diagnoses, including depression and psychoses. Hospital characteristics included a composite of teaching status and location (rural, urban teaching, and urban nonteaching) and hospital region (Northeast, Midwest, South, and West). Hospital bed sizes were classified as small, medium, and large. The cutoffs were less than 100 (small), 100 to 299 (medium), and 300 or more (large) short-term acute care beds of the facilities from NASS and were varied based on region, urban-rural designation, and teaching status of the hospital from NIS.8 Patients with missing data were classified as the unknown group and were included in the analysis.
Statistical Analysis
National estimates of the number of GAS procedures among all hospital encounters for patients with gender identity disorder were derived using discharge or encounter weight provided by the databases.15 The clinical and demographic characteristics of the patients undergoing GAS were reported descriptively. The number of encounters for gender identity disorder, the percentage of GAS procedures among those encounters, and the absolute number of each procedure performed over time were estimated. The difference by age group was examined and tested using Rao-Scott χ2 test. All hypothesis tests were 2-sided, and P < .05 was considered statistically significant. All analyses were conducted using SAS version 9.4 (SAS Institute Inc).
Results
A total of 48 019 patients who underwent GAS were identified (Table 1). Overall, 25 099 patients (52.3%) were aged 19 to 30 years, 10 476 (21.8%) were aged 31 to 40, and 3678 (7.7%) were aged 12 to 18 years. Private insurance coverage was most common in 29 064 patients (60.5%), while 12 127 (25.3%) were Medicaid recipients. Depression was reported in 7192 patients (15.0%). Most patients (42 467 [88.4%]) were treated at urban, teaching hospitals, and there was a disproportionate number of patients in the West (22 037 [45.9%]) and Northeast (12 396 [25.8%]). Within the cohort, 31 668 patients (65.9%) underwent 1 procedure while 13 415 (27.9%) underwent 2 procedures, and the remainder underwent multiple procedures concurrently (Table 1).
Table 1. Demographics of Transgender Patients Undergoing Gender-Affirming Surgery Overall and Stratified by Classes of Gender-Affirming Surgery.
| Characteristic | Overall | Breast/chest surgery | Genital surgery | Other cosmetic procedures | ||||
|---|---|---|---|---|---|---|---|---|
| No. (SE) | % (SE) | No. (SE) | % (SE) | No. (SE) | % (SE) | No. (SE) | % (SE) | |
| Age, y | ||||||||
| 12-18 | 3678 (272) | 7.7 (0.3) | 3215 (258) | 11.8 (0.5) | 405 (54) | 2.4 (0.3) | 350 (53) | 5.3 (0.7) |
| 19-30 | 25 099 (1442) | 52.3 (0.6) | 16 067 (1166) | 59.1 (0.6) | 7461 (437) | 44.2 (0.8) | 2946 (246) | 44.2 (1.2) |
| 31-40 | 10 476 (646) | 21.8 (0.4) | 4918 (384) | 18.1 (0.4) | 4423 (309) | 26.2 (0.6) | 1729 (165) | 25.9 (1.0) |
| 41-50 | 4359 (266) | 9.1 (0.3) | 1650 (132) | 6.1 (0.3) | 2168 (155) | 12.8 (0.5) | 784 (77) | 11.8 (0.6) |
| 51-60 | 2958 (193) | 6.2 (0.2) | 949 (78) | 3.5 (0.2) | 1546 (124) | 9.2 (0.5) | 610 (69) | 9.1 (0.7) |
| 61-70 | 1271 (92) | 2.6 (0.2) | 350 (33) | 1.3 (0.1) | 742 (68) | 4.4 (0.3) | 229 (31) | 3.4 (0.4) |
| >70 | 177 (26) | 0.4 (0.1) | 37 (8) | 0.1 (0) | 126 (23) | 0.7 (0.1) | 19 (6) | 0.3 (0.1) |
| Unknown | 3 (2) | 0 | 0 | 0 | 1 (1) | 0 | 2 (2) | 0 |
| Sex | ||||||||
| Male | 15 234 (965) | 31.7 (0.8) | 8707 (639) | 32.0 (0.7) | 5417 (460) | 32.1 (1.7) | 2144 (180) | 32.1 (1.3) |
| Female | 26 264 (1584) | 54.7 (1.0) | 17 852 (1294) | 65.7 (0.5) | 5455 (315) | 32.3 (1.6) | 4419 (386) | 66.3 (1.3) |
| Unknown | 6522 (612) | 13.6 (1.1) | 627 (137) | 2.3 (0.5) | 6000 (585) | 35.6 (2.2) | 106 (20) | 1.6 (0.3) |
| Race, inpatienta | ||||||||
| White | 6915 (642) | 65.1 (2.0) | 575 (77) | 58.4 (4.2) | 6050 (595) | 67.8 (2.0) | 635 (155) | 53.1 (6.2) |
| Black | 955 (123) | 9.0 (1.0) | 125 (28) | 12.7 (2.5) | 720 (105) | 8.1 (1.0) | 145 (36) | 12.1 (3.1) |
| Hispanic | 1050 (130) | 9.9 (0.9) | 130 (31) | 13.2 (2.6) | 820 (117) | 9.2 (0.9) | 140 (38) | 11.7 (3.0) |
| Other | 1380 (253) | 13.0 (1.9) | 95 (24) | 9.6 (2.1) | 1060 (188) | 11.9 (1.7) | 255 (82) | 21.3 (5.0) |
| Unknown | 325 (64) | 3.1 (0.6) | 60 (24) | 6.1 (2.2) | 275 (60) | 3.1 (0.6) | 20 (10) | 1.7 (0.8) |
| Insurance status | ||||||||
| Medicare | 2581 (157) | 5.4 (0.3) | 976 (78) | 3.6 (0.2) | 1369 (99) | 8.1 (0.5) | 308 (46) | 4.6 (0.6) |
| Medicaid | 12 127 (923) | 25.3 (1.1) | 7220 (647) | 26.6 (1.5) | 3749 (304) | 22.2 (1.1) | 1598 (194) | 24.0 (2.3) |
| Private | 29 064 (1698) | 60.5 (1.2) | 16 547 (1278) | 60.9 (1.6) | 10 589 (657) | 62.8 (1.1) | 3634 (352) | 54.5 (2.6) |
| Self-pay | 2814 (285) | 5.9 (0.5) | 1489 (177) | 5.5 (0.5) | 747 (125) | 4.4 (0.7) | 797 (143) | 11.9 (1.9) |
| Other | 1097 (204) | 2.3 (0.4) | 723 (181) | 2.7 (0.6) | 329 (67) | 2.0 (0.4) | 280 (110) | 4.2 (1.6) |
| Unknown | 337 (107) | 0.7 (0.2) | 232 (88) | 0.9 (0.3) | 89 (35) | 0.5 (0.2) | 53 (23) | 0.8 (0.3) |
| Income status | ||||||||
| Low | 9604 (519) | 20.0 (0.5) | 5547 (370) | 20.4 (0.7) | 3298 (208) | 19.5 (0.7) | 1248 (108) | 18.7 (1.1) |
| Medium low | 10 520 (635) | 21.9 (0.6) | 5796 (442) | 21.3 (0.8) | 4099 (266) | 24.3 (0.7) | 1236 (106) | 18.5 (0.9) |
| Medium high | 12 667 (795) | 26.4 (0.5) | 7282 (557) | 26.8 (0.6) | 4482 (317) | 26.6 (0.8) | 1657 (151) | 24.8 (1.1) |
| High | 14 325 (985) | 29.8 (1.0) | 8220 (748) | 30.2 (1.3) | 4636 (338) | 27.5 (1.0) | 2305 (241) | 34.6 (1.6) |
| Unknown | 904 (96) | 1.9 (0.2) | 342 (45) | 1.3 (0.1) | 357 (51) | 2.1 (0.3) | 224 (48) | 3.4 (0.6) |
| Hospital location or teaching status | ||||||||
| Rural | 480 (132) | 1.0 (0.3) | 334 (126) | 1.2 (0.5) | 148 (20) | 0.9 (0.1) | 1 (1) | 0 |
| Urban nonteaching | 5072 (585) | 10.6 (1.2) | 2302 (350) | 8.5 (1.3) | 2430 (399) | 14.4 (2.2) | 699 (124) | 10.5 (1.9) |
| Urban teaching | 42 467 (2630) | 88.4 (1.3) | 24 551 (1907) | 90.3 (1.4) | 14 293 (931) | 84.7 (2.2) | 5970 (528) | 89.5 (1.9) |
| Hospital bed size, inpatientb | ||||||||
| Small | 3620 (694) | 34.1 (4.8) | 255 (57) | 25.9 (5.1) | 3270 (611) | 36.6 (5.0) | 345 (125) | 28.9 (8.7) |
| Medium | 2015 (356) | 19.0 (3.1) | 145 (44) | 14.7 (4.2) | 1425 (285) | 16.0 (3.0) | 490 (165) | 41.0 (9.7) |
| Large | 4990 (535) | 47.0 (4.4) | 585 (93) | 59.4 (5.8) | 4230 (515) | 47.4 (4.7) | 360 (88) | 30.1 (7.3) |
| Hospital bed size, hospital ambulatory surgeryb | ||||||||
| Small | 1749 (331) | 4.7 (0.9) | 1176 (247) | 4.5 (1.0) | 373 (66) | 4.7 (0.9) | 259 (94) | 4.7 (1.7) |
| Medium | 12 041 (1540) | 32.2 (3.3) | 8592 (1293) | 32.8 (3.8) | 2139 (208) | 26.9 (2.6) | 2145 (369) | 39.2 (4.7) |
| Large | 23 604 (1980) | 63.1 (3.3) | 16 433 (1426) | 62.7 (3.8) | 5435 (508) | 68.4 (2.8) | 3069 (316) | 56.1 (4.7) |
| Hospital region | ||||||||
| Northeast | 12 396 (1189) | 25.8 (2.3) | 7054 (817) | 25.9 (2.8) | 4695 (548) | 27.8 (2.7) | 1208 (187) | 18.1 (2.7) |
| Midwest | 6881 (607) | 14.3 (1.3) | 4198 (464) | 15.4 (1.8) | 2514 (227) | 14.9 (1.4) | 826 (157) | 12.4 (2.3) |
| South | 6705 (688) | 14.0 (1.4) | 3572 (494) | 13.1 (1.8) | 2597 (274) | 15.4 (1.6) | 864 (132) | 13.0 (2.0) |
| West | 22 037 (2242) | 45.9 (2.9) | 12 362 (1627) | 45.5 (3.7) | 7065 (774) | 41.9 (3.1) | 3772 (466) | 56.6 (3.8) |
| HIV or AIDS | 421 (51) | 0.9 (0.1) | 204 (32) | 0.7 (0.1) | 125 (23) | 0.7 (0.1) | 110 (21) | 1.6 (0.3) |
| Substance abuse | 158 (27) | 0.3 (0.1) | 66 (15) | 0.2 (0.1) | 78 (19) | 0.5 (0.1) | 22 (8) | 0.3 (0.1) |
| Alcohol abuse | 158 (27) | 0.3 (0.1) | 66 (15) | 0.2 (0.1) | 78 (19) | 0.5 (0.1) | 22 (8) | 0.3 (0.1) |
| Drug abuse | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Mental health | 7351 (419) | 15.3 (0.7) | 4077 (315) | 15.0 (0.9) | 2693 (168) | 16.0 (0.8) | 1072 (118) | 16.1 (1.1) |
| Psychoses | 186 (23) | 0.4 ( 0) | 84 (11) | 0.3 ( 0) | 73 (15) | 0.4 (0.1) | 42 (12) | 0.6 (0.2) |
| Depression | 7192 (412) | 15.0 (0.7) | 4012 (311) | 14.8 (0.9) | 2631 (165) | 15.6 (0.8) | 1034 (116) | 15.5 (1.1) |
Race was only available in inpatient encounters (National Inpatient Sample).
Different cutoff was used to define bed size in inpatient encounters (National Inpatient Sample) and hospital ambulatory surgery encounters (Nationwide Ambulatory Surgery Sample).
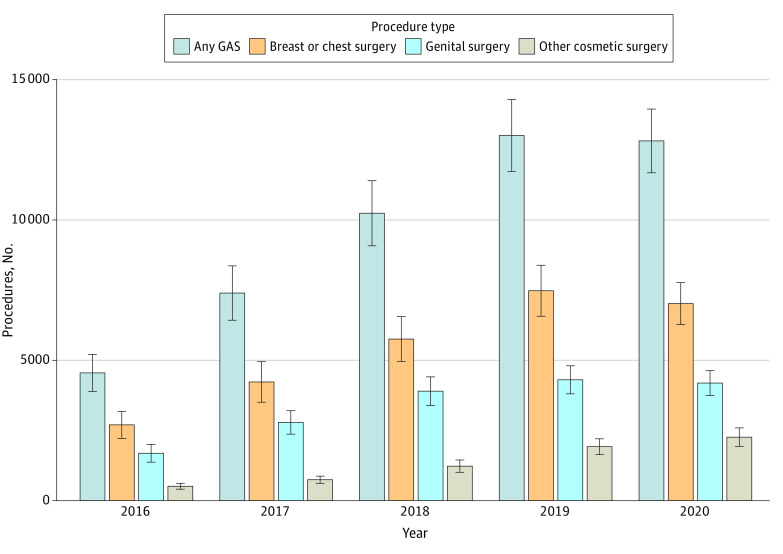
The overall number of health system encounters for gender identity disorder rose from 13 855 in 2016 to 38 470 in 2020. Among encounters with a billing code for gender identity disorder, there was a consistent rise in the percentage that were for GAS from 4552 (32.9%) in 2016 to 13 011 (37.1%) in 2019, followed by a decline to 12 818 (33.3%) in 2020 (Figure 1 and eFigure in Supplement 1). Among patients undergoing ambulatory surgical procedures, 37 394 (80.3%) of the surgical procedures included gender-affirming surgical procedures. For those with hospital admissions with gender identity disorder, 10 625 (11.8%) of admissions were for GAS.
Figure 1. Gender-Affirming Surgical Procedures Performed by Year Stratified by Type .
Error bars represent 95% CIs. GAS indicates gender-affirming surgery.
Breast and chest procedures were most common and were performed for 27 187 patients (56.6%). Genital reconstruction was performed for 16 872 patients (35.1%), and other facial and cosmetic procedures for 6669 patients (13.9%) (Table 2). The most common individual procedure was breast reconstruction in 21 244 (44.2%), while the most common genital reconstructive procedure was hysterectomy (4489 [9.3%]), followed by orchiectomy (3425 [7.1%]), and vaginoplasty (3381 [7.0%]). Among patients who underwent other facial and cosmetic procedures, liposuction (2945 [6.1%]) was most common, followed by rhinoplasty (2446 [5.1%]) and facial feminizing surgery and chin augmentation (1874 [3.9%]).
Table 2. Number of Gender-Affirming Procedures Overall.
| Surgical procedure | No. (SE) | % (SE) |
|---|---|---|
| Gender-affirming surgery | 48 019 (2697) | NA |
| Breast or chest surgery | 27 187 (1942) | 56.6 (1.7) |
| Breast reconstruction | 21 244 (1646) | 44.2 (1.7) |
| Mammaplasty | 4926 (375) | 10.3 (0.5) |
| Mastopexy or nipple reconstruction | 10 234 (1009) | 21.3 (1.3) |
| Genital surgery | 16 872 (1013) | 35.1 (1.6) |
| Orchitectomy | 3425 (288) | 7.1 (0.5) |
| Prostatectomy | 22 (9) | 0 |
| Penectomy | 671 (122) | 1.4 (0.3) |
| Vaginoplasty | 3381 (427) | 7.0 (0.9) |
| Clitoroplasty or labiaplasty | 424 (62) | 0.9 (0.1) |
| Hysterectomy | 4489 (229) | 9.3 (0.5) |
| Salpingo-oophorectomy | 666 (57) | 1.4 (0.1) |
| Vaginectomy | 272 (68) | 0.6 (0.1) |
| Vulvectomy | 39 (11) | 0.1 (0) |
| Metoidioplasty or phalloplasty | 1226 (265) | 2.6 (0.5) |
| Urethroplasty | 2233 (277) | 4.6 (0.6) |
| Scrotoplasty | 217 (39) | 0.5 (0.1) |
| Testicular prostheses | 400 (82) | 0.8 (0.2) |
| GAS NOS | 3760 (464) | 7.8 (1.0) |
| Other cosmetic procedures | 6669 (542) | 13.9 (0.9) |
| Rhinoplasty | 2446 (315) | 5.1 (0.6) |
| Rhytidectomy | 1721 (257) | 3.6 (0.5) |
| Blepharoplasty | 219 (36) | 0.5 (0.1) |
| Hair removal or hair transplantation | 10 (7) | 0 |
| Facial feminizing or chin augmentation | 1874 (257) | 3.9 (0.5) |
| Liposuction | 2945 (270) | 6.1 (0.5) |
| Collagen injections | 64 (21) | 0.1 (0) |
| Trachea shave or reduction thyroid chondroplasty | 632 (101) | 1.3 (0.2) |
| Other | 447 (82) | 0.9 (0.2) |
| No. of surgical groups | ||
| 1 | 45 333 (2573) | 94.4 (0.4) |
| 2 | 2664 (243) | 5.5 (0.4) |
| 3 | 22 (8) | 0 |
| No. of individual procedures | ||
| 1 | 31 668 (1739) | 65.9 (1.3) |
| 2 | 13 415 (1075) | 27.9 (1.2) |
| 3 | 2338 (219) | 4.9 (0.4) |
| 4 | 532 (72) | 1.1 (0.1) |
| 5 | 56 (20) | 0.1 (0) |
| 6 | 11 (7) | 0 |
| Mean (SE) | 1.42 (0.02) | NA |
Abbreviations: GAS, gender-affirming surgery; NA, not available; NOS, not otherwise specified.
The absolute number of GAS procedures rose from 4552 in 2016 to a peak of 13 011 in 2019 and then declined slightly to 12 818 in 2020 (Figure 1). Similar trends were noted for breast and chest surgical procedures as well as genital surgery, while the rate of other facial and cosmetic procedures increased consistently from 2016 to 2020. The distribution of the individual procedures performed in each class were largely similar across the years of analysis (Table 3).
Table 3. Number of GAS Procedures by Year.
| Characteristics | 2016 | 2017 | 2018 | 2019 | 2020 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. (SE) | % (SE) | No. (SE) | % (SE) | No. (SE) | % (SE) | No. (SE) | % (SE) | No. (SE) | % (SE) | |
| GAS | 4552 (658) | 9.5 (1.4) | 7397 (968) | 15.4 (1.6) | 10 242 (1162) | 21.3 (1.8) | 13 011 (1280) | 27.1 (2.4) | 12 818 (1136) | 26.7 (2.2) |
| Breast or chest surgery | 2700 (483) | 9.9 (1.8) | 4229 (723) | 15.6 (2.0) | 5757 (799) | 21.2 (2.1) | 7479 (907) | 27.5 (3.0) | 7022 (747) | 25.8 (2.7) |
| Breast reconstruction | 2027 (404) | 9.5 (1.9) | 3319 (618) | 15.6 (2.2) | 4582 (687) | 21.6 (2.3) | 6090 (781) | 28.7 (3.3) | 5226 (586) | 24.6 (2.7) |
| Mammaplasty | 577 (117) | 11.7 (2.3) | 788 (141) | 16.0 (2.2) | 1056 (160) | 21.4 (2.4) | 1272 (172) | 25.8 (3.1) | 1233 (143) | 25.0 (2.8) |
| Mastopexy or nipple reconstruction | 1014 (256) | 9.9 (2.5) | 1582 (399) | 15.5 (3.0) | 2120 (394) | 20.7 (2.8) | 2939 (519) | 28.7 (4.4) | 2580 (347) | 25.2 (3.5) |
| Genital surgery | 1689 (317) | 10.0 (1.8) | 2787 (418) | 16.5 (2.2) | 3901 (509) | 23.1 (2.5) | 4305 (500) | 25.5 (2.6) | 4190 (439) | 24.8 (2.4) |
| Orchitectomy | 394 (87) | 11.5 (2.4) | 514 (90) | 15.0 (2.2) | 732 (140) | 21.4 (3.2) | 830 (119) | 24.2 (3.2) | 955 (147) | 27.9 (3.7) |
| Prostatectomy | 5 (5) | 22.7 (19.3) | 0 | 0 | 5 (5) | 22.7 (19.3) | 4 (2) | 19.0 (11.8) | 8 (5) | 35.6 (19.9) |
| Penectomy | 75 (36) | 11.2 (5.1) | 66 (22) | 9.9 (3.4) | 86 (32) | 12.8 (4.7) | 162 (41) | 24.2 (6.2) | 281 (102) | 41.9 (9.8) |
| Vaginoplasty | 310 (114) | 9.2 (3.3) | 541 (212) | 16.0 (5.6) | 790 (248) | 23.4 (6.2) | 831 (194) | 24.6 (5.2) | 908 (188) | 26.9 (5.1) |
| Clitoroplasty or labiaplasty | 35 (13) | 8.2 (3.1) | 55 (20) | 13.0 (4.1) | 78 (27) | 18.5 (5.3) | 111 (27) | 26.0 (5.8) | 146 (37) | 34.4 (7.0) |
| Hysterectomy | 461 (52) | 10.3 (1.2) | 837 (85) | 18.6 (1.4) | 1059 (105) | 23.6 (1.7) | 971 (93) | 21.6 (1.9) | 1160 (106) | 25.8 (2.1) |
| Salpingo-oophorectomy | 99 (22) | 14.8 (3.0) | 146 (34) | 22.0 (4.3) | 133 (23) | 20.0 (3.2) | 139 (24) | 20.8 (3.3) | 149 (22) | 22.4 (3.2) |
| Vaginectomy | 69 (51) | 25.3 (14.5) | 39 (15) | 14.2 (5.8) | 54 (20) | 19.8 (7.5) | 27 (13) | 9.9 (4.8) | 84 (36) | 30.7 (11.2) |
| Vulvectomy | 3 (2) | 8.0 (5.7) | 3 (3) | 7.6 (7.3) | 4 (3) | 11.1 (8.4) | 10 (6) | 25.5 (13.4) | 19 (8) | 47.8 (14.5) |
| Metoidioplasty or phalloplasty | 224 (126) | 18.3 (9.1) | 261 (133) | 21.3 (9.4) | 236 (134) | 19.2 (9.5) | 284 (117) | 23.1 (8.6) | 222 (77) | 18.1 (6.4) |
| Urethroplasty | 119 (38) | 5.3 (1.7) | 346 (108) | 15.5 (4.5) | 567 (172) | 25.4 (6.3) | 624 (140) | 27.9 (5.5) | 577 (124) | 25.8 (5.0) |
| Scrotoplasty | 21 (11) | 9.8 (4.9) | 31 (13) | 14.2 (4.9) | 49 (18) | 22.6 (6.3) | 62 (17) | 28.7 (7.3) | 54 (16) | 24.8 (6.8) |
| Testicular prostheses | 48 (30) | 12.0 (7.0) | 54 (27) | 13.4 (5.6) | 79 (35) | 19.6 (7.0) | 108 (36) | 27.1 (8.3) | 112 (38) | 27.9 (8.6) |
| GAS NOS | 275 (148) | 7.3 (3.7) | 535 (180) | 14.2 (4.4) | 925 (228) | 24.6 (5.3) | 1155 (262) | 30.7 (5.8) | 870 (205) | 23.1 (4.9) |
| Other cosmetic procedures | 513 (105) | 7.7 (1.6) | 745 (129) | 11.2 (1.7) | 1228 (220) | 18.4 (2.8) | 1922 (280) | 28.8 (3.6) | 2262 (329) | 33.9 (3.9) |
| Rhinoplasty | 99 (30) | 4.0 (1.3) | 237 (69) | 9.7 (2.7) | 408 (120) | 16.7 (4.4) | 761 (161) | 31.1 (5.7) | 942 (220) | 38.5 (6.6) |
| Rhytidectomy | 72 (28) | 4.2 (1.7) | 204 (74) | 11.9 (4.0) | 295 (111) | 17.1 (5.7) | 521 (126) | 30.3 (6.5) | 629 (173) | 36.6 (7.6) |
| Blepharoplasty | 17 (7) | 7.6 (3.1) | 47 (15) | 21.3 (5.6) | 49 (22) | 22.5 (7.9) | 72 (16) | 33.1 (6.9) | 34 (10) | 15.5 (4.5) |
| Hair removal or hair transplantation | 5 (5) | 50.0 (35.4) | 0 | 0 | 5 (5) | 50.0 (35.4) | 0 | 0 | 0 | 0 |
| Facial feminizing or chin augmentation | 68 (25) | 3.7 (1.4) | 152 (52) | 8.1 (2.6) | 298 (104) | 15.9 (5.0) | 577 (123) | 30.8 (5.9) | 779 (186) | 41.5 (7.0) |
| Liposuction | 348 (85) | 11.8 (2.8) | 397 (78) | 13.5 (2.1) | 655 (139) | 22.2 (3.5) | 773 (120) | 26.2 (3.7) | 773 (104) | 26.2 (3.4) |
| Collagen injections | 4 (2) | 6.2 (3.9) | 17 (11) | 26.5 (10.6) | 21 (10) | 33.4 (8.2) | 10 (4) | 15.2 (7.2) | 12 (5) | 18.7 (8.3) |
| Trachea shave or reduction thyroid chondroplasty | 22 (9) | 3.5 (1.5) | 58 (19) | 9.2 (2.9) | 72 (23) | 11.4 (3.5) | 203 (54) | 32.1 (7.3) | 276 (74) | 43.7 (8.1) |
| Other | 4 (2) | 0.9 (0.5) | 14 (5) | 3.0 (1.2) | 29 (14) | 6.5 (3.2) | 24 (15) | 5.4 (3.4) | 376 (78) | 84.1 (5.2) |
Abbreviations: GAS, gender-affirming surgery; NOS, not otherwise specified.
When stratified by age, patients 19 to 30 years had the greatest number of procedures, 25 099 (Figure 2). There were 10 476 procedures performed in those aged 31 to 40 years and 4359 in those aged 41 to 50 years. Among patients younger than 19 years, 3678 GAS procedures were performed. GAS was less common in those cohorts older than 50 years. Overall, the greatest number of breast and chest surgical procedures, genital surgical procedures, and facial and other cosmetic surgical procedures were performed in patients aged 19 to 30 years.
Figure 2. Gender-Affirming Surgical Procedures Performed During the Study Stratified by Age.
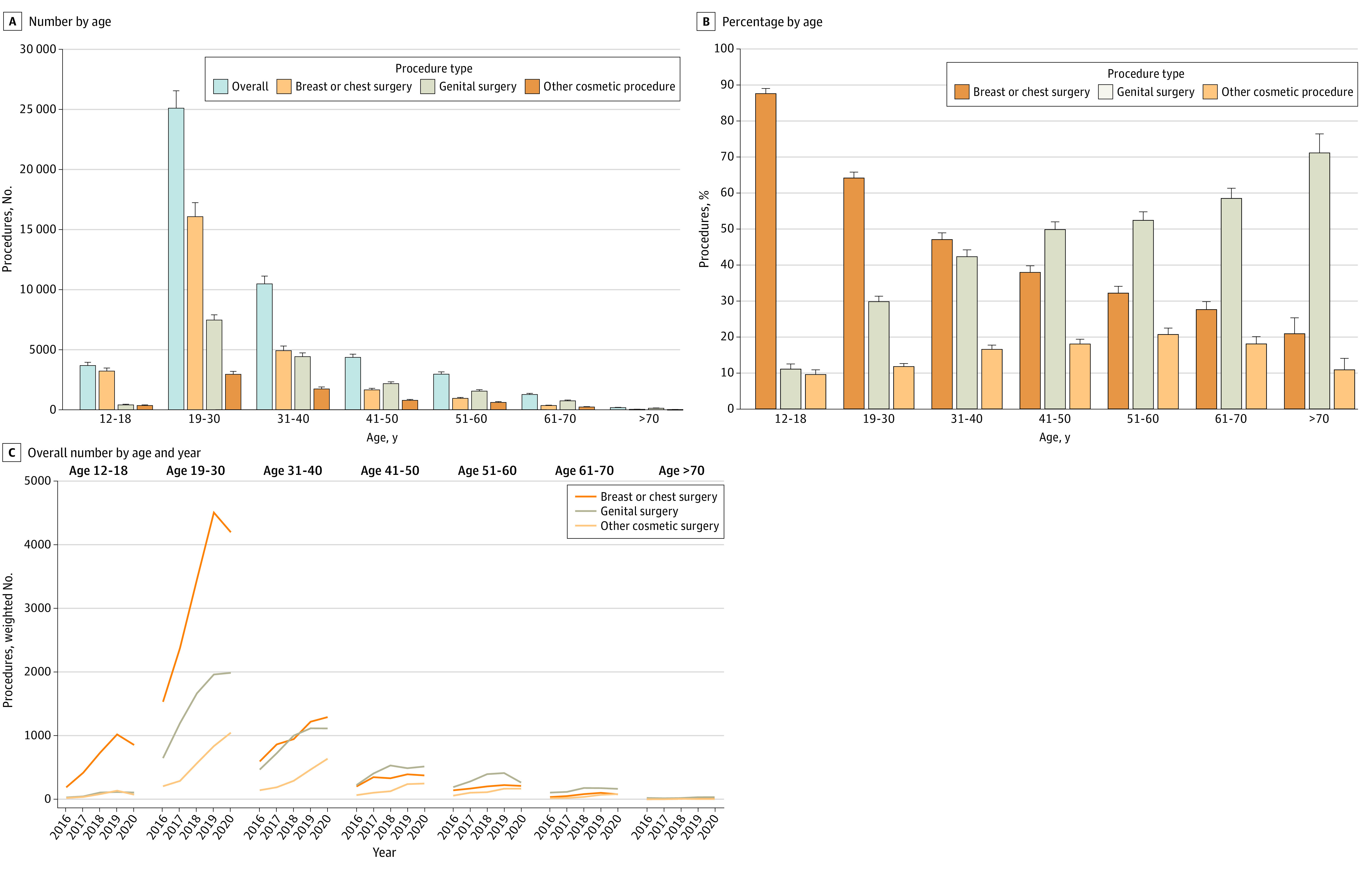
Percentages are based on the number of procedures divided by number of patients; thus, as some patients underwent multiple procedures the total may be greater than 100%. Error bars represent 95% CIs.
When stratified by the type of procedure performed, breast and chest procedures made up the greatest percentage of the surgical interventions in younger patients while genital surgical procedures were greater in older patients (Figure 2). Additionally, 3215 patients (87.4%) aged 12 to 18 years underwent GAS and had breast or chest procedures. This decreased to 16 067 patients (64.0%) in those aged 19 to 30 years, 4918 (46.9%) in those aged 31 to 40 years, and 1650 (37.9%) in patients aged 41 to 50 years (P < .001). In contrast, 405 patients (11.0%) aged 12 to 18 years underwent genital surgery. The percentage of patients who underwent genital surgery rose sequentially to 4423 (42.2%) in those aged 31 to 40 years, 1546 (52.3%) in those aged 51 to 60 years, and 742 (58.4%) in those aged 61 to 70 years (P < .001). The percentage of patients who underwent facial and other cosmetic surgical procedures rose with age from 9.5% in those aged 12 to 18 years to 20.6% in those aged 51 to 60 years, then gradually declined (P < .001). Figure 2 displays the absolute number of procedure classes performed by year stratified by age. The greatest magnitude of the decline in 2020 was in younger patients and for breast and chest procedures.
Discussion
These findings suggest that the number of GAS procedures performed in the US has increased dramatically, nearly tripling from 2016 to 2019. Breast and chest surgery is the most common class of procedure performed while patients are most likely to undergo surgery between the ages of 19 and 30 years. The number of genital surgical procedures performed increased with increasing age.
Consistent with prior studies, we identified a remarkable increase in the number of GAS procedures performed over time.9,16 A prior study examining national estimates of inpatient GAS procedures noted that the absolute number of procedures performed nearly doubled between 2000 to 2005 and from 2006 to 2011. In our analysis, the number of GAS procedures nearly tripled from 2016 to 2020.9,17 Not unexpectedly, a large number of the procedures we captured were performed in the ambulatory setting, highlighting the need to capture both inpatient and outpatient procedures when analyzing data on trends. Like many prior studies, we noted a decrease in the number of procedures performed in 2020, likely reflective of the COVID-19 pandemic.18 However, the decline in the number of procedures performed between 2019 and 2020 was relatively modest, particularly as these procedures are largely elective.
Analysis of procedure-specific trends by age revealed a number of important findings. First, GAS procedures were most common in patients aged 19 to 30 years. This is in line with prior work that demonstrated that most patients first experience gender dysphoria at a young age, with approximately three-quarters of patients reporting gender dysphoria by age 7 years. These patients subsequently lived for a mean of 23 years for transgender men and 27 years for transgender women before beginning gender transition treatments.19 Our findings were also notable that GAS procedures were relatively uncommon in patients aged 18 years or younger. In our cohort, fewer than 1200 patients in this age group underwent GAS, even in the highest volume years. GAS in adolescents has been the focus of intense debate and led to legislative initiatives to limit access to these procedures in adolescents in several states.20,21
Second, there was a marked difference in the distribution of procedures in the different age groups. Breast and chest procedures were more common in younger patients, while genital surgery was more frequent in older individuals. In our cohort of individuals aged 19 to 30 years, breast and chest procedures were twice as common as genital procedures. Genital surgery gradually increased with advancing age, and these procedures became the most common in patients older than 40 years. A prior study of patients with commercial insurance who underwent GAS noted that the mean age for mastectomy was 28 years, significantly lower than for hysterectomy at age 31 years, vaginoplasty at age 40 years, and orchiectomy at age 37 years.16 These trends likely reflect the increased complexity of genital surgery compared with breast and chest surgery as well as the definitive nature of removal of the reproductive organs.
Limitations
This study has limitations. First, there may be under-capture of both transgender individuals and GAS procedures. In both data sets analyzed, gender is based on self-report. NIS specifically makes notation of procedures that are considered inconsistent with a patient’s reported gender (eg, a male patient who underwent oophorectomy). Similar to prior work, we assumed that patients with a code for gender identity disorder or transsexualism along with a surgical procedure classified as inconsistent underwent GAS.9 Second, we captured procedures commonly reported as GAS procedures; however, it is possible that some of these procedures were performed for other underlying indications or diseases rather than solely for gender affirmation. Third, our trends showed a significant increase in procedures through 2019, with a decline in 2020. The decline in services in 2020 is likely related to COVID-19 service alterations. Additionally, while we comprehensively captured inpatient and ambulatory surgical procedures in large, nationwide data sets, undoubtedly, a small number of procedures were performed in other settings; thus, our estimates may underrepresent the actual number of procedures performed each year in the US.
Conclusions
These data have important implications in providing an understanding of the use of services that can help inform care for transgender populations. The rapid rise in the performance of GAS suggests that there will be a greater need for clinicians knowledgeable in the care of transgender individuals and with the requisite expertise to perform GAS procedures. However, numerous reports have described the political considerations and challenges in the delivery of transgender care.22 Despite many medical societies recognizing the necessity of gender-affirming care, several states have enacted legislation or policies that restrict gender-affirming care and services, particularly in adolescence.20,21 These regulations are barriers for patients who seek gender-affirming care and provide legal and ethical challenges for clinicians. As the use of GAS increases, delivering equitable gender-affirming care in this complex landscape will remain a public health challenge.
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement
References
- 1.American Psychiatric Association . What is gender dysphoria? Accessed July 6, 2023. https://www.psychiatry.org/patients-families/gender-dysphoria/what-is-gender-dysphoria
- 2.Oles N, Darrach H, Landford W, et al. Gender affirming surgery: a comprehensive, systematic review of all peer-reviewed literature and methods of assessing patient-centered outcomes (part 1: breast/chest, face, and voice). Ann Surg. 2022;275(1):e52-e66. doi: 10.1097/SLA.0000000000004728 [DOI] [PubMed] [Google Scholar]
- 3.Akhavan AA, Sandhu S, Ndem I, Ogunleye AA. A review of gender affirmation surgery: what we know, and what we need to know. Surgery. 2021;170(1):336-340. doi: 10.1016/j.surg.2021.02.013 [DOI] [PubMed] [Google Scholar]
- 4.Oles N, Darrach H, Landford W, et al. Gender affirming surgery: a comprehensive, systematic review of all peer-reviewed literature and methods of assessing patient-centered outcomes (part 2: genital reconstruction). Ann Surg. 2022;275(1):e67-e74. doi: 10.1097/SLA.0000000000004717 [DOI] [PubMed] [Google Scholar]
- 5.Papadopulos NA, Lellé JD, Zavlin D, et al. Quality of life and patient satisfaction following male-to-female sex reassignment surgery. J Sex Med. 2017;14(5):721-730. doi: 10.1016/j.jsxm.2017.01.022 [DOI] [PubMed] [Google Scholar]
- 6.El-Hadi H, Stone J, Temple-Oberle C, Harrop AR. Gender-affirming surgery for transgender individuals: perceived satisfaction and barriers to care. Plast Surg (Oakv). 2018;26(4):263-268. doi: 10.1177/2292550318767437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dy GW, Nolan IT, Hotaling J, Myers JB. Patient reported outcome measures and quality of life assessment in genital gender confirming surgery. Transl Androl Urol. 2019;8(3):228-240. doi: 10.21037/tau.2019.05.04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Papadopulos NA, Zavlin D, Lellé JD, et al. Male-to-female sex reassignment surgery using the combined technique leads to increased quality of life in a prospective study. Plast Reconstr Surg. 2017;140(2):286-294. doi: 10.1097/PRS.0000000000003529 [DOI] [PubMed] [Google Scholar]
- 9.Canner JK, Harfouch O, Kodadek LM, et al. Temporal trends in gender-affirming surgery among transgender patients in the United States. JAMA Surg. 2018;153(7):609-616. doi: 10.1001/jamasurg.2017.6231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ngaage LM, Knighton BJ, McGlone KL, et al. Health insurance coverage of gender-affirming top surgery in the United States. Plast Reconstr Surg. 2019;144(4):824-833. doi: 10.1097/PRS.0000000000006012 [DOI] [PubMed] [Google Scholar]
- 11.Padula WV, Baker K. Coverage for gender-affirming care: making health insurance work for transgender Americans. LGBT Health. 2017;4(4):244-247. doi: 10.1089/lgbt.2016.0099 [DOI] [PubMed] [Google Scholar]
- 12.NIS overview. Agency for Healthcare Research and Quality. Accessed March 3, 2023. https://hcup-us.ahrq.gov/nisoverview.jsp
- 13.NASS overview. Agency for Healthcare Research and Quality. Accessed March 3, 2023. https://hcup-us.ahrq.gov/nassoverview.jsp
- 14.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36(1):8-27. doi: 10.1097/00005650-199801000-00004 [DOI] [PubMed] [Google Scholar]
- 15.HCUP methods series calculating national inpatient sample (NIS) variances for data years 2012 and later. Agency for Healthcare Research and Quality. Accessed July 6, 2023. https://hcup-us.ahrq.gov/reports/methods/2015_09.jsp
- 16.Lane M, Ives GC, Sluiter EC, et al. Trends in gender-affirming surgery in insured patients in the United States. Plast Reconstr Surg Glob Open. 2018;6(4):e1738. doi: 10.1097/GOX.0000000000001738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Merrick E, Weissman JP, Ascha M, Jordan SW, Ellis M. National trends in gender-affirming surgical procedures: a google trends analysis. Cureus. 2022;14(6):e25906. doi: 10.7759/cureus.25906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emont J, Wen T, Friedman AM, Wright JD. Trends in hysterectomy rates associated with the coronavirus disease 2019 (COVID-19) pandemic. Obstet Gynecol. 2023;141(3):592-601. doi: 10.1097/AOG.0000000000005087 [DOI] [PubMed] [Google Scholar]
- 19.Zaliznyak M, Bresee C, Garcia MM. Age at first experience of gender dysphoria among transgender adults seeking gender-affirming surgery. JAMA Netw Open. 2020;3(3):e201236. doi: 10.1001/jamanetworkopen.2020.1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kraschel KL, Chen A, Turban JL, Cohen IG. Legislation restricting gender-affirming care for transgender youth: Politics eclipse healthcare. Cell Rep Med. 2022;3(8):100719. doi: 10.1016/j.xcrm.2022.100719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Youth access to gender affirming care: the federal and state policy landscape. Accessed July 6, 2023. https://www.kff.org/other/issue-brief/youth-access-to-gender-affirming-care-the-federal-and-state-policy-landscape/
- 22.US News and World Report. States that have restricted gender-affirming care for trans youth in 2023. Accessed June 26, 2023. https://www.usnews.com/news/best-states/articles/2023-03-30/what-is-gender-affirming-care-and-which-states-have-restricted-it-in-2023
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable. ICD-10 and CPT Codes of Gender-Affirming Surgery
eFigure. Percentage of Patients With Codes for Gender Identity Disorder Who Underwent GAS
Data Sharing Statement