Supplemental Digital Content is Available in the Text.
Key Words: pelvic floor physical therapy, powerlifting, weightlifting, strongman
Abstract
Mahoney, K, Heidel, RE, and Olewinski, L. Prevalence and normalization of stress urinary incontinence in female strength athletes. J Strength Cond Res 37(9): 1877–1881, 2023—Strength training is increasing in popularity in women but is also a potential risk factor for stress urinary incontinence (SUI). There is potential for normalization of SUI in sports with high rates of SUI. Pelvic floor physical therapy is an effective treatment for SUI in both athletes and nonathletes, but female strength athletes may not be aware of this option. Our study sought to assess prevalence, normalization, rates of treatment, and preferred sources of information about SUI in female strength athletes. A novel cross-sectional survey was distributed online through social media groups dedicated to female strength athletes with 425 women responding within 4 days. Statistical significance of results was assumed at a 2-sided alpha value of 0.05. 43.5% of athletes experienced incontinence with daily tasks, 59.1% experienced incontinence with normal strength training, and 50.2% experienced incontinence during competition. Of the athletes who experienced incontinence, 61.4% did not have incontinence before starting their sport and only 9.4% had ever sought treatment. 67.9% of all athletes surveyed believed that urinary incontinence was a normal part of their sport. Our findings indicate that SUI is common in female strength athletes and may be a consequence of the sport itself. Normalization of SUI is common, and few athletes seek treatment.
Introduction
Stress urinary incontinence (SUI; involuntary leakage of urine from increased intra-abdominal pressure) affects 10–39% of women throughout their lifetime, with peaks in rates at ages 50–54 years and older than 75 (9). Low-intensity activity can be protective against SUI, but intense physical activity and high-impact physical activity increase rates of SUI in women (18). Although nonathletic control groups in various studies report SUI rates of 3.5–14.3% (6,7), a 2020 meta-analysis of urinary incontinence in nulliparous female athletes found SUI in 20.9% (19), similar to the rate of 19.6% found in a study of 372 Portuguese athletes (6). The overall prevalence increased to 25.6% for high-impact athletes, with the highest rates seen in volleyball (75%) and trampolining (80%); however, rates vary from study to study. In a review of 278 athletes, only 19.6% of 51 nulliparous volleyball players reported SUI (13). Strength training has been found to be a risk factor for stress urinary incontinence in studies evaluating women in CrossFit (73%) (10), powerlifting (43.9%) (26), and weightlifting (41.7%) (22).
Studies in sports with high rates of SUI found that SUI impairs confidence and performance (22,27), reduces quality of life (14), and leads to athletes leaving sport (18). Athletes also engage in behaviors to limit or hide SUI, including reduced fluid intake (5,14,26), which can be deleterious to performance and health. Surveys of women participating in athletics, basketball, indoor football, and weightlifting found that women often believed that SUI was a normal part of their sports (14), and many had never talked to anyone about SUI (22). Although pelvic floor physical therapy is the most effective treatment for SUI, athletes are often unaware of this as a treatment option (12,14). However, if the concept of pelvic floor training is introduced, athletes are interested in learning more and in incorporating this into their training (22).
The internal urethral sphincter, the elaborate external or urogenital urethral sphincter, and the pelvic floor muscles contribute to control of urinary continence in women (8,15). The pelvic floor muscles (levator ani muscles, Figure 1) are contracted at rest using type 1 fibers; type 2 fibers are activated to accommodate sudden increases in intra-abdominal pressure (8,15). Research on the effect of exercise in general on female pelvic floor function shows light to moderate physical activity can decrease in rates of SUI while more vigorous activity can increase the risk of SUI (7). The exact mechanism of this increased risk has yet to be defined. Long-term athletics can increase, decrease, or have no effect on pelvic floor muscle size and strength (3). Repetitive increases in intra-abdominal pressure can lead to stretch and fatigue of the perineal muscles over time, or strength training can result in increased strength in pelvic floor musculature that is still not enough to overcome the rapid increase in intra-abdominal pressure that occurs with certain movements (7). Timing of pelvic floor muscles in relation to response of other trunk muscles may play a role, with higher rates of SUI found in women with delayed activation of pelvic floor muscles relative to other trunk muscles (17). Although the etiology of the increased risk is still being explored, research has shown that both specific activity to strengthen pelvic floor muscles and increased awareness of the mechanics of abdominal and pelvic floor muscle activation reduce rates of SUI (19).
Figure 1.
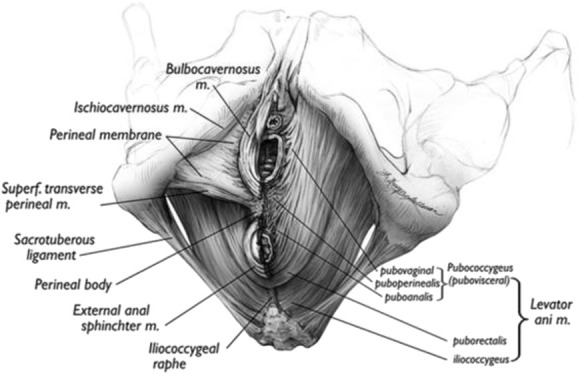
Inferior view of the pelvic floor. Superficial perineal muscles and perineal membrane have been removed on the left to show attachments of the levator ani (LA) muscles to distal vagina, anus, perineal body, and perineal membrane. Note the absence of direct attachments of LA to urethra. (Courtesy of Lianne Kruger Sullivan, Dallas, TX; originally published in Corton MM. Anatomy of pelvic floor dysfunction. Obstetrics Gynecol Clin. 2009; 36(3):401–419, reproduced here with permission from Elsevier).
Weightlifting, powerlifting, and strongman are competitive strength sports with lifts that lead to increased intra-abdominal pressure and the need to activate pelvic floor musculature to prevent SUI. Weightlifting has 2 barbel events: the snatch and the clean and jerk. Powerlifting has 3 events: the squat, the deadlift, and the bench press. Strongman competitions do not have set components but instead have varied events of lifting, carrying, and pushing heavy objects such as cars, stones, or logs with a goal of attaining a maximum weight or of attaining maximum repetitions of a set weight in a set time.
The number of women partaking in strength sports has been growing in recent years. The USA Weightlifting national championships had 99 female athletes in 2014 and 223 female athletes in 2019 (25). The purpose of this study was to add to the body of research on incontinence specific to female strength athletes by exploring prevalence of SUI, normalization of SUI, preferences on sources for information on SUI, and rates of seeking treatment for SUI in female strength athletes participating in weightlifting, powerlifting, and strongman. This information can be used to guide coaches and support personnel in counseling athletes about SUI and treatment to improve pelvic floor health, performance, and quality of life.
Methods
Experimental Approach to the Problem
We developed a novel 19 question survey to share on social media addressed to female athletes in powerlifting, weightlifting, and strongman. It was reviewed by 3 physicians who were also strength athletes and a statistician with expertise in surveys. The anonymous, voluntary survey received IRB approval from the University of Tennessee Graduate School of Medicine, Knoxville before distribution. Subjects were informed of the risks and benefits of participation before beginning the study and were aware that proceeding with the study indicated they were consenting to participate. Subjects were asked about their demographics, duration of participation in strength training, risk factors for SUI, experience with SUI in relation to training and competition, normalization of SUI, preferred sources of information about SUI, and if SUI was present, whether they had tried treatment (see Appendix A, Supplemental Digital Content, http://links.lww.com/JSCR/A386). Our hypothesis was that rates of SUI would be above average for active women and that women in strength sports would tend to see incontinence as a normal part of their sport.
Subjects
The requirements for the survey respondents were women >18 years who self-identified powerlifting, weightlifting, or strongman as their primary sport. To isolate strength athletes, CrossFit athletes were excluded unless they mainly participated in exclusive strength training sessions. Informed consent was obtained before starting the survey. Given the difficulty in estimating the true number of English-speaking female strength athletes worldwide, a power analysis was not performed before distribution of the survey. We hoped to capture as many athletes as possible.
Procedures
The cross-sectional, web-based survey was shared on Facebook in Powerlifting Women, Strong Friends, Women of Strongman, Starting Strongman, and between athletes on Instagram and within training groups. The survey was freely shared among these social media groups and within 4 days a total of 425 athletes had responded. Study data were collected and managed using REDCap electronic data capture tools hosted at the University of Tennessee Graduate School of Medicine, Knoxville, Tennessee.
Statistical Analyses
Frequency and percentage statistics were used to calculate measures of prevalence. Chi-square analysis was performed to compare independent groups on categorical outcomes. Unadjusted odds ratios (ORs) with 95% confidence intervals (95% CIs) were reported and interpreted. The statistics were performed using SPSS version 26 (IBM Corp., Armonk, NY), and statistical significance was assumed at a 2-sided alpha value of 0.05.
Results
Of the 425 athletes who responded to the survey (refer to Table 1 for demographics), 43.5% of athletes experienced SUI with daily tasks, 59.1% experienced SUI with normal strength training, and 50.2% experienced SUI during competition. 69.6% of athletes reported SUI in some aspect of their life at the time the survey was taken. Of the athletes who experienced SUI, 61.4% did not have it before starting their sport.
Table 1.
Demographics of respondents.
| Variable | Level | Frequency (%) or M ± SD |
| Primary sport | ||
| Powerlifting | 199 (47.3%) | |
| Weightlifting | 30 (7.1%) | |
| Strongman | 173 (41.1%) | |
| Other | 19 (4.5%) | |
| Missing | 4 (0.9%) | |
| Years involved in strength training | ||
| <1 y | 13 (3.1%) | |
| 1–3 y | 150 (35.3%) | |
| 3–5 y | 154 (36.2%) | |
| 5–10 y | 86 (20.2%) | |
| >10 y | 22 (5.2%) | |
| Age (y) | 18–69 | 36.02 ± 9.35 |
| Height (cm) | 142.24–193.04 | 65.19 ± 3.45 |
| Body mass (kg) | 45.4–136.1 | 178.10 ± 44.70 |
A total of 67.9% of all athletes surveyed stated that they think urinary incontinence is a normal part of their sport (Table 2). There was a statistically significant difference in normalization between athletes currently experiencing SUI in any part of their activities and athletes who did not currently have SUI (p < 0.001, OR 3.20, 95% CI 2.02–5.05), but there was not a statistically significant difference in normalization between athletes currently experiencing SUI who had it before or after becoming a strength athlete (p = 0.29, OR 0.75, 95% CI 0.44–1.28). Athletes who had SUI during training and competition were more likely to think it was normal than those who did not (training: p < 0.001, OR 2.95, 95% CI 1.94–4.49; competition: p < 0.001, OR 3.52, 95% CI 2.27–5.46), but normalization among athletes who had SUI during daily tasks was higher but not statistically significantly different than those who did not have SUI during daily tasks (p = 0.26, OR 1.27, 95% CI 0.84–1.92). Duration of participation in sport did not affect perception that SUI was a normal part of the strength training (p = 0.613).
Table 2.
Normalization of SUI compared with presence before or after initiation of sport and to when in sport SUI occurred.*
| Variable | Level | Believed SUI was normal (total) |
| SUI before sport | ||
| Yes | 82 (71.9%) | |
| No | 140 (77.3%) | |
| Not applicable | 66 (51.2%) | |
| SUI during daily tasks | ||
| Yes | 131 (70.8%) | |
| No | 157 (65.7%) | |
| SUI during training | ||
| Yes | 194 (77.6%) | |
| No | 94 (54.0%) | |
| SUI during competition | ||
| Yes | 172 (81.1%) | |
| No | 116 (55.0%) |
SUI = stress urinary incontinence.
Women who had a history of vaginal birth were more likely to experience SUI before sport (50.4 vs. 29.1%, p < 0.001, OR 2.48, 95% CI 1.53–4.00) and in daily tasks (60.4 vs. 35.2%, p < 0.001, OR 3.16, 95% CI 2.11–4.73), training (66.3 vs. 54.5%, p < 0.001, OR 1.64, 95% CI 1.10–2.45), and competition (58.3 vs. 45.1%, p < 0.008, OR 1.70, 95% CI 1.15–2.53). However, women who had given birth vaginally were less likely to normalize SUI (57.7 vs. 74.9%, p < 0.001, OR 54.2, 95% CI 30.5–69.8).
Only 17.2% of all athletes stated that they had talked to their doctor about urinary incontinence, and 9.4% had sought treatment. Of that percentage, the intervention could have been before or after starting weightlifting with some athletes having recovered from SUI because 129 athletes responded “not applicable” to having SUI in weightlifting or daily activities at the time the survey was taken and 80 athletes responded “not applicable” to ever having spoken to their doctor about SUI.
44.2% of respondents reported that they talked to someone other than their doctor about incontinence. 29.6% sought advice about incontinence from videos and articles on the internet, 22.5% talked to their friends at their gymnasium, and 13.2% talked to their coach. Only 8.5% of all athletes had tried pelvic floor physical therapy for SUI.
Discussion
Female strength athletes experience high rates of SUI, and there is a culture of normalization of SUI within the sport. This is consistent with reports of normalization in focus group subsets of previous studies in elite female athletes with SUI (14). Most of our athletes believed that SUI was a normal part of their sport. Although comparison of subgroups of our subjects based on presence of SUI in different situations showed some differences in normalization, over half the women in every subset agreed that SUI was a normal part of strength training. Women who had SUI were more likely to think it was normal than those who did not, and this trend was stronger for women who had SUI during sport than those who had during their daily activities. Duration of time spent in sport did not affect perception of normalization but having had a vaginal birth made women less likely to normalize SUI.
Less is known about rates of normalization of incontinence in nonathletic premenopausal women; however, 29.3% of postmenopausal women seeing a physician with any type of incontinence reported that they had believed incontinence was normal (1). A 2020 meta-ethnography examining women's attitudes toward incontinence found that women see incontinence as “part and parcel” of their lives, an issue that was more of a “personal matter” than a “serious” medical problem (the study was not designed to provide statistical measure of prevalence of normalization). Because of that perception, they were less likely to speak to their doctor about stress, urge, or overflow incontinence (24). The women who did seek treatment preferred working with a health care professional for feedback that they were doing exercises correctly and that they were making progress (24). Regular supervised visits at least once a week with daily home exercises also result in higher rates of treatment success and improvement in quality of life than a home program alone, regardless of whether performed one-on-one or in group settings (2,20).
Stress urinary incontinence was common in the women who participated in our study, but only 8.3% of all subjects had tried pelvic floor physical therapy. Multiple Cochrane reviews on treatment for SUI have shown that pelvic floor physical therapy is the most efficacious intervention for SUI, leading to reduction in symptoms and improvement in quality of life or a complete cure (9). A clear benefit of pelvic floor physical therapy for SUI has also been demonstrated in elite female athletes (23). Historically women were guided to Kegel exercises (voluntary contraction of the pelvic floor muscles with an inward lift) to increase tone of levator ani muscles, and therapy focusing on pelvic floor musculature is most supported in the literature (16). Practicing contraction of pelvic floor muscles slightly before or at the same time as sports-specific motions that increase intra-abdominal pressure is known as the Knack Principle. Physical therapy for SUI is evolving to address increased strength, endurance, and specific control of the abdominal wall muscles, diaphragm, lumbar musculature, and hip flexors, extensors, and rotators in addition to the pelvic floor muscles (16). Pelvic floor physical therapy techniques have resulted in measurable improvements in pelvic floor muscle size and tone (4), reduction in SUI in experimental settings (11), and self-reported reduction of SUI during activity (9). Improving SUI could improve athletes' confidence and success because 87.8% of the Norwegian powerlifters and weightlifters with SUI believed that incontinence impaired their performance (22).
In addition to affecting performance, SUI can impair quality of life (9) and lead to women leaving sports (21). Female strength athletes report interest in learning more about exercises for their pelvic floor muscles to prevent or treat SUI (22). Indeed, female athletes who knew more about pelvic floor anatomy or felt confident in their ability to perform a pelvic floor contraction have less risk of SUI in sports (5,26). Pelvic floor training is effective in primary prevention in non-athletes (2). With evidence that pelvic floor physical therapy can prevent and treat SUI, incorporating pelvic floor muscle exercises into training routines could reduce SUI associated with strength training.
Like women in previous studies (5,14), our athletes frequently did not talk about SUI, and those that did turned to the internet or their friends far more than coaches or health care professionals. This suggests a need for information about SUI not being a normal part of the sport, the relationship of SUI to pelvic floor anatomy, and treatment options for SUI being discussed by reputable sources on social media or web pages. This could be an avenue for pelvic floor physical therapists and other clinicians to spread awareness and to connect with athletes and coaches to refine the culture of the sport. The percent of athletes in our study affected by SUI in some aspect of their lives increased from 26.8 to 69.6% after starting strength training. If pelvic floor education was routinely incorporated into training for weightlifting, powerlifting, and strongman, it could bypass the need for women to overcome their perceptions of normalization and tendency to not discuss their SUI with their coaches.
Study weaknesses: This was the first use of this survey tool. Although it received statistical review, it was not reviewed by nonmedically trained athletes or independent expert in the survey design. We did not include free text responses, which would have allowed us to gain deeper insight into why women normalize SUI in powerlifting. Because the survey was voluntary, there is a possibility that women with SUI were more likely to respond, increasing the chance of self-selection bias.
Practical Applications
The results from this survey highlight high rates of SUI in female strength athletes and high rates of normalization of SUI. Our results suggest a need to share information about the treatment and prevention options for SUI on the internet and social media because that is where female strength athletes are more likely to turn for advice. In addition, increased awareness among strength and conditioning coaches and trainers about treatment and prevention of SUI could allow them to better discuss SUI with their athletes and reduce normalization of SUI. Awareness of treatment options will hopefully prompt athletes to connect with their health care provider for pelvic floor physical therapy resources and referrals.
Acknowledgments
The authors are grateful to the subjects in this study for their time and input. The authors have no financial relationships or funding sources to disclose. Author 1 developed the research concept and study design, performed the literature review, data collection, data analysis and interpretation, and writing of the manuscript. Author 2 participated in the study design, data analysis and interpretation, statistical analyses, and writing of the manuscript. Author 3 participated in developing the study design, and performed the literature review, data collection, data analysis and interpretation, and writing of the manuscript. Please direct any questions or correspondence to Luci Olewinski, lolewinski@utmck.edu. Research was conducted at the University of Tennessee Graduate School of Medicine, Knoxville, Tennessee.
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (http://journals.lww.com/nsca-jscr).
Contributor Information
Kaitlin Mahoney, Email: kaitlin.mahoney@ortho.virginia.com.
R. Eric Heidel, Email: rheidel@utmck.edu.
References
- 1.Biyik I, Kucuk B, Arpaci HF, Demirci H. Factors affecting doctor visits of postmenopausal women with urinary incontinence. Low Urin Tract Symptoms 11: 200–205, 2019. [DOI] [PubMed] [Google Scholar]
- 2.Bø K. Physiotherapy management of urinary incontinence in females. J Physiother 66: 147–154, 2020. [DOI] [PubMed] [Google Scholar]
- 3.Bø K, Nygaard IE. Is physical activity good or bad for the female pelvic floor? A narrative review. Sports Med 50: 471–484, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brækken IH, Majida M, Engh ME, Bø K. Morphological changes after pelvic floor muscle training measured by 3-dimensional ultrasonography: A randomized controlled trial. Obstet Gynecol 115: 317–324, 2010. [DOI] [PubMed] [Google Scholar]
- 5.Cardoso AMB, Lima CROdP, Ferreira CWS. Prevalence of urinary incontinence in high-impact sports athletes and their association with knowledge, attitude and practice about this dysfunction. Eur J Sport Sci 18: 1405–1412, 2018. [DOI] [PubMed] [Google Scholar]
- 6.Carvalhais A, Natal Jorge R, Bø K. Performing high-level sport is strongly associated with urinary incontinence in elite athletes: A comparative study of 372 elite female athletes and 372 controls. Br J Sports Med 52: 1586–1590, 2018. [DOI] [PubMed] [Google Scholar]
- 7.Chisholm L, Delpe S, Priest T, Reynolds WS. Physical activity and stress incontinence in women. Curr Bladder Dysfunct Rep 14: 174–179, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Corton MM. Anatomy of pelvic floor dysfunction. Obstet Gynecol Clin North Am 36: 401–419, 2009. [DOI] [PubMed] [Google Scholar]
- 9.Dumoulin C, Cacciari LP, Hay‐Smith EJC. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database Syst Rev 10: 93–107, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Elks W, Jaramillo-Huff A, Barnes KL, Petersen TR, Komesu YM. The Stress Urinary Incontinence in CrossFit (SUCCeSS) study. Female Pelvic Med Reconstr Surg 26: 101–106, 2020. [DOI] [PubMed] [Google Scholar]
- 11.Ferreira S, Ferreira M, Carvalhais A, et al. Reeducation of pelvic floor muscles in volleyball athletes. Rev Assoc Méd Bras 60: 428–433, 2014. [Google Scholar]
- 12.Gram MCD, Bø K. High level rhythmic gymnasts and urinary incontinence: Prevalence, risk factors, and influence on performance. Scand J Med Sci Sports 30: 159–165, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hagovska M, Švihra J, Buková A, Dračková D, Švihrová V. Prevalence and risk of sport types to stress urinary incontinence in sportswomen: A cross‐sectional study. Neurourol Urodyn 37: 1957–1964, 2018. [DOI] [PubMed] [Google Scholar]
- 14.Jácome C, Oliveira D, Marques A, Sá-Couto P. Prevalence and impact of urinary incontinence among female athletes. Int J Gynecol Obstet 114: 60–63, 2011. [DOI] [PubMed] [Google Scholar]
- 15.Jung J, Ahn HK, Huh Y. Clinical and functional anatomy of the urethral sphincter. Int Neurourol J 16: 102–106, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marques A, Stothers L, Macnab A. The status of pelvic floor muscle training for women. Can Urol Assoc J 4: 419–424, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Moser H, Leitner M, Baeyens JP, Radlinger L. Pelvic floor muscle activity during impact activities in continent and incontinent women: A systematic review. Int Urogynecol J 29: 179–196, 2018. [DOI] [PubMed] [Google Scholar]
- 18.Nygaard IE, Shaw JM, Bardsley T, Egger MJ. Lifetime physical activity and female stress urinary incontinence. Am J Obstet Gynecol 213: 601–640. e10, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pires T, Pires P, Moreira H, Viana R. Prevalence of urinary incontinence in high-impact sport athletes: A systematic review and meta-analysis. J Hum Kinet 73: 279–288, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Radzimińska A, Strączyńska A, Weber-Rajek M, et al. The impact of pelvic floor muscle training on the quality of life of women with urinary incontinence: A systematic literature review. Clin Interv Aging 13: 957–965, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Salvatore S, Serati M, Laterza R, et al. The impact of urinary stress incontinence in young and middle-age women practising recreational sports activity: An epidemiological study. Br J Sports Med 43: 1115–1118, 2009. [DOI] [PubMed] [Google Scholar]
- 22.Skaug KL, Engh ME, Frawley H, Bø K. Prevalence of pelvic floor dysfunction, bother and risk factors and knowledge of the pelvic floor muscles in Norwegian male and female powerlifters and Olympic weightlifters. J Strength Cond Res 36: 2800–2807, 2022. [DOI] [PubMed] [Google Scholar]
- 23.Sorrigueta-Hernández A, Padilla-Fernandez BY, Marquez-Sanchez M-T, et al. Benefits of physiotherapy on urinary incontinence in high-performance female athletes. Meta-analysis. J Clin Med 9: 3240, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Toye F, Barker KL. A meta-ethnography to understand the experience of living with urinary incontinence:‘is it just part and parcel of life? BMC Urol 20: 1–25, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.USA Weightlifting Results Archive. Available at: https://www.teamusa.org/usa-weightlifting/resources/results-archive.
- 26.Wikander L, Kirshbaum MN, Waheed N, Gahreman DE. Urinary incontinence in competitive women powerlifters: A cross-sectional survey. Sports Med Open 7: 89–11, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wikander L, Kirshbaum MN, Waheed N, Gahreman DE. Urinary incontinence in competitive women weightlifters. J Strength Cond Res 36: 3130–3135, 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]


