Abstract
Background:
About a third of youth with suicidal ideation develop suicidal plans and about 60% of youth with suicidal plans make suicidal attempts. This study aimed to study different types of suicidal ideation and the risk factors in Kenyan youth.
Methods:
We studied a total of 9742 high school, college and university students using following self-administered instruments: - a researcher design socio-demographic questionnaire, Psychiatric Diagnostic Screening Questionnaire (PDSQ) to document psychiatric disorders and various types of suicidal ideas in previous two weeks, Washington Early Recognition Center Affectivity and Psychosis tool to assess stress, affectivity and psychosis, Wealth index questionnaire to document economic indicators based on household items for the families of the students. We used descriptive statistics, univariate analysis, bivariate logistic regression analysis and variables with a p-value of less than <.05 were entered into generalized linear models using logit links to identify independent predictors.
Results:
The overall prevalence of different types of suicidal ideation was (22.6%), major depression was found in 20.0%, affectivity, psychosis and stress was found in 10.4%, 8.7% and 26.0% respectively. Female gender, major depression, stress, affectivity and psychosis and being in high school were significant (p < 0.05) predictors of suicidal ideation.
Limitations:
This was a cross sectional study that focused only on suicidal ideas and associated economic factors and mental health disorders. It did not study suicidal behavior.
Conclusion:
Future studies are needed to study the progression from suicidal ideas to suicidal attempts and the factors associated with that progression.
Keywords: Different types of suicidal ideas, Risk factors, Students, Kenya
1. Introduction
Life prevalence of suicidal thoughts among young people has been reported to be 40.9% in the Philippines, 17% in Norway (Strandheim et al., 2014), 10.7% in Germany (Voss et al., 2019), 65% in Belgium 65% (Mortier et al., 2017), 12.6% in Portugal, 13.59% in Nepal (Pandey et al., 2019) and 17.9% in Turkey (Canbaz and Terzi, 2018). African studies have shown similar variations, including 34% in South West Ethiopia (Abdu et al., 2020) and 21.3% in Ghana (Quarshie et al., 2019). The 12-month prevalence rate of suicidal ideation was 19.9% in one study of Ethiopian youths (Dachew et al., 2018), while another Ethiopian study reported a 12-month prevalence of 22.5% and that 26.36% of those had thought about committing suicide in the last month and 24.03% had planned to commit suicide during their lifetime (Amare et al., 2018). In Tunisia, the prevalence rates were 26.9% for temporary suicidal ideation and 9.6% for serious suicidal ideation (Guedria-Tekari et al., 2019).
About 80% to more than 90% of youths with suicidal thoughts have major psychiatric disorder (Akca et al., 2018). Other associated psychiatric disorders include schizophrenia, with adolescents with an early onset of psychosis having the highest risk, (Crumlish et al., 2005; Dassori et al., 1990), anxiety and substance abuse. Factors associated with suicidal thoughts include financial stress, poor social support (Abdu et al., 2020; Dachew et al., 2018), losing parents (Eskin et al., 2016), bullying and physical fights (Canbaz and Terzi, 2018), pain, muscular tension, conduct problems and being overweight (Strandheim et al., 2014), disappointment with examination results, feeling hopeless or sad and being absent from school for more than three days (Amare et al., 2018).
Household items have also been used widely to determine household wealth (Harttgen and Vollmer, 2013), including in rural Africa (Morris et al., 2000). There is hardly any literature from Africa in general, and Kenya in particular, that demonstrate which specific household level economic indicators of poverty are related to suicidal ideas or to the matrix of suicidal thoughts of mental health issues and poverty.
We had three research aims: - (1) to study the different types of suicidal ideation among Kenyan high school, college and university students over the previous two weeks. (2) to determine the prevalence of different types of suicidal ideas; (3) to determine the predictors of suicidal ideation.
2. Methods
This study obtained Ethical approval from Maseno University Ethics Review Board in Kenya (IRB number MSU/DRPI/MUERC/00344/16). The methodology was designed so as to achieve our aims.
2.1. Recruitment and data collection
This was a cross-sectional study of adolescents and young adults aged 15–25 attending high schools, colleges and universities. In Kenya students normally attend colleges and universities from 19–23 year of age, but we added two years to take account of delayed entry. However, because there was a larger number of mature students than expected, the number who were over the age of 25 was only 3.4% and we decided to include all respondents in the analysis.
The participants were all Kenyans, who were recruited from Nairobi County and three counties in South Eastern Kenya: Machakos, Kitui and Makueni. We were already working with these four counties on other project and had gained acceptance from local people, so they seemed a natural choice for this project. The high school studies were all from these areas and the college and university students came from across Kenya as admission are handled centrally. The study comprised a convenience sample of following: - (1) one administrative location in which there are several high schools and because of school closure we only accommodated those students who could make it to the data collection points (2) all colleges located within the four counties and were in session at the time of the data collection and (3) one public university located in one of the four counties. It was conducted from July 2016 to October 2018. The subjects were recruited from the colleges and universities and the high school students were recruited from their local communities, because the schools were closed during the study period as the result of a lengthy teachers’ strike. The college and university students were approached in their classrooms after lectures, once the various institutions provided permission for their students to take part in the study. Permission to approach the high school students was obtained from local community administrators. The local administrators contacted the students and asked them to come along to local community centres at a specific time and date. Of all the 9,742 participants: − 6648 (68.6%) were university students and 1534(15.8%) were college students who were approached in their classrooms and agreed to take part in the study. Of the 1506(15.5%) high school students who presented themselves at the data collection points, agreed to participate. It is a Government requirement to seek permission for any activities taking place in the community so that logistical support can be provided, such as suitable meeting venues and security. The research assistants were informed of the schedules for the college and university students and the high school students were directed to specific public meeting areas, within walking distance, where they assessed them with the help of local community leaders. Participants were only included in the study if they were able to speak, read and write in English and had voluntarily agreed to participate in the study by signing the informed consent form. Consent was obtained from parents and guardians if the participants were under 18 years of age.
We worked with the colleges and universities to make sure there was mental health support available if the students needed help because of the issues raised by the survey. Trained staff from local health center facilities, who had received training on the World Health Organization (WHO) Mental Health Gap Action Programme Intervention Guide (World Health Organization, 2010) were available to support the high school students, if needed. This instrument was developed for use by non-mental health specialists to identify common mental health issues and suggest interventions that they could provide. We also informed the participants where they could seek help at institutional and community levels.
2.2. Instruments
We used several instruments. These instruments were selected so to capture the various types of suicidal ideas and the various socio-demographic, mental disorders, substance use and economic predictors.
Socio-demographic characteristics.
The questionnaire included questions about socio-demographic variables, including age, gender, whether they were attending high school, college or university, marital status and birth order.
Economic indicators.
The respondents provided details of their household, including what items were in their home and how they accessed water and toilet facilities and cooked. They were put into one of five wealth index categories, as a reflection of their economic status (Smits and Steendijk, 2015). The wealth index we used was based on the World Bank recommendation for low-income and middle-income countries and has been adopted by the Kenyan Government. It contains five levels, with one representing the lowest level of wealth and one indicating the highest level.
Psychiatric conditions.
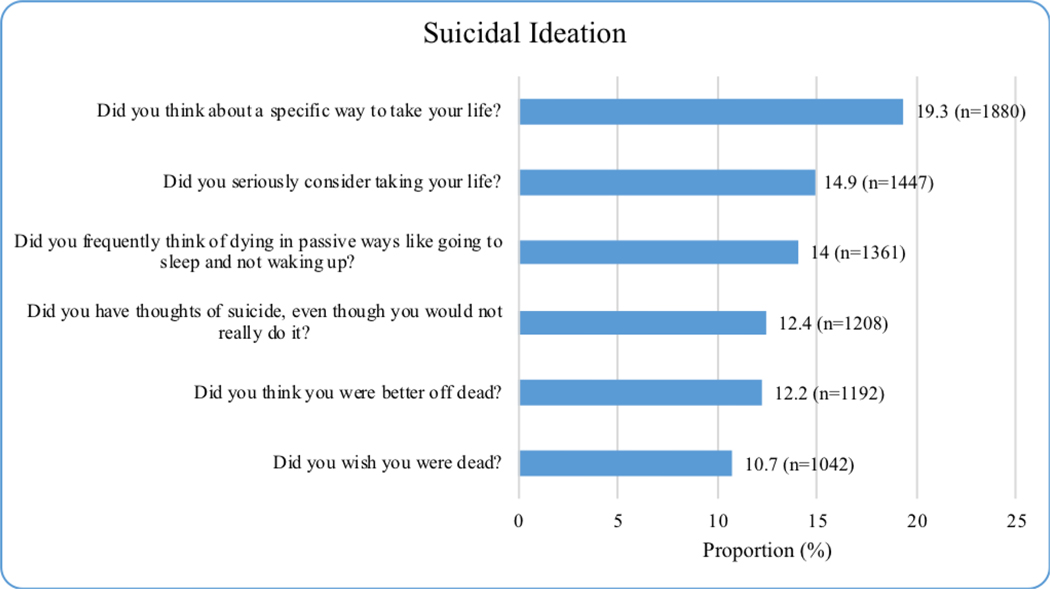
The Psychiatric Diagnostic Screening Questionnaire (PDSQ) was used to assess the respondents. It comprises 126 questions that assess the symptoms of 13 Axis I disorders in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (Del Barrio, 2016). These are: eating disorders (bulimia/binge-eating disorder), mood disorders (major depressive disorder), anxiety disorders (panic disorder, agoraphobia, post-traumatic stress disorder, obsessive-compulsive disorder, generalized anxiety disorder and social phobia), substance use disorders (alcohol abuse/dependence and drug abuse/dependence) and somatoform disorders (somatization disorder and hypochondriasis). It also contains a six-item psychosis screen. The disorders that were selected were the most prevalent in community-based epidemiological surveys (Kessler et al., 1994; Robins and Regier, 1991) and the most frequently reported in large clinical samples (Koenigsberg et al., 1985; Mezzich et al., 1989; Shear et al., 2000). In a validity study of 994 psychiatric outpatients (Zimmerman and Mattia, 2001), the 13 PDSQ subscales demonstrated good to excellent internal consistency. Cronbach’s alpha exceeded .80 for 12 of the 13 subscales and the mean of the alpha coefficients was .86. Test-retest reliability was examined in 185 subjects who completed the PDSQ twice in one week. The test-retest reliability coefficients exceeded .80 for nine subscales and the mean of the test-retest correlation coefficients was .83. The convergent and discriminant validity of the PDSQ subscales (Campbell and Fiske, 1959) were examined in 361 patients who completed a package of questionnaires at home less than a week after completing the PDSQ. The last six questions from the PDSQ major depressive episode domain are used to measure different types of suicidal ideation. These are related to people frequently thinking of dying in passive ways, like going to sleep and not waking up, wanting to be dead, thinking they would be better off dead, thinking about suicide, seriously considering taking their life and thinking about specific ways to take their life. The questions are coded as no (zero points) or yes (one point). The PDSQ does not differentiate which of these ideas are active or passive or which one of them is most likely to translate into actual suicidal attempt, with the possible exception of “Did you think about a specific way to take your life?” and “Do you seriously consider taking your life?” It is not worthy that these two possibly active suicidal ideas were the commonest.
Other Measures:
The Washington Early Recognition Center Affectivity and Psychosis (WERCAP) screen (Hsieh et al., 2016; Mamah et al., 2014) was used to quantitatively assesses psychosis-risk symptoms and bipolar-risk symptoms (affectivity) based on the frequency of symptoms and their effects on functioning (Mamah et al., 2014). It has high test-retest reliability and validity, with affectivity of sensitivity of .91, specificity of .71, psychosis sensitivity .88 and specificity of .82 (Mamah et al., 2014). We also used the WERC stress screen, a self-report questionnaire, to assess total stress burden and the severity of individual stressors (Hsieh et al., 2016; Mamah et al., 2014)
2.2.1. Data management and statistical analysis
The coded data were checked, cleaned and exported into SPSS, version 21 IBM Corp, NY, USA
2.3. Creation of suicidal index scores
Data reduction techniques were used to summarize the observed suicidal ideation variables, namely the last six questions of PDSQ on depression subscale, into a few dimensions by Rasch analysis through latent variable modeling using the eRm, ltm (Rizopoulos, 2006) and difR (Magis et al., 2010) R packages (R Foundation, Vienna, Austria). Component internal consistency and reliability were used to compute the suicidal ideation scores, by calculating Cronbach’s alpha and this was high (.776).
Before we performed the Rasch factor analysis, the correlation matrix was inspected to check for the strength of the correlation. Then the factorability was tested using exploratory factor analysis using the Kaiser-Meyer-Olkin measure of sampling adequacy and Bartlett’s test of sphericity. Exploratory factor analysis, with varimax rotation, was carried out to determine the dimensional structure suicidality using the following criteria: (a) eigenvalue >1(Kaiser, 1960), (b) variables should load >.50 on only one factor and less than 0.40 on other factors, (c) the interpretation of the factor structure should be meaningful and (d) the Scree plot should be accurate when the means of communalities are above .60 (Hakstian and Cattell, 1982). Computations were based on a covariance matrix, as all the variables received values from the same measurement scale (Hadzi-Pavlovic, 2010). Bartlett’s test of sphericity with p < .05 and a Kaiser-Meyer-Olkin measure of sampling adequacy of .6 were used when performing this factor analysis. A factor was considered as important if its eigenvalue exceeded 1.0 (Kaiser, 1960). Pairwise associations between the six items, corresponding to two-by-two contingency tables for all possible pairs, were computed. The Cronbach’s alpha of the six items was .776, with only one component loading. Factor scores were then generated because loadings were all similar. We used the computed factor scores as our suicidal ideation index because factor scores of exploratory factor analysis can be used as an index of all variables. The scores had bimodal negatively skewed distribution, suggesting there were two groups. Respondents scoring less than zero were classified as not having suicidal ideation while those with more than zero were classified as having suicidal ideation.
2.3.1. Statistical methods
The results of the exploratory and statistical data analysis are presented in the tables. We employed descriptive statistics to estimate the prevalence of suicidality as well as the participant’s characteristics. Mean prevalence rates were estimated. The outcome variable of suicidality scores were grouped into those with, and those without, suicidal ideation. Univariate associations between suicidal ideation and other variables were estimated using Chi-squared tests, after they were fitted to identify potential confounding factors. Variables with a p-value of less than <.05 were entered into generalized linear models using logit link to identify independent predictors of suicidality. Adjusted odds ratios (aOR) with 95% confidence intervals (CI) were calculated to assess the strength and significance of the association. All tests were two-sided and statistical significance was set at p < .05. We did not include depression in the analysis of psychiatric disorders, because of high collinearity between depression and suicidality.
2.3.2. Overlap between suicidal ideation, depression and the wealth index
We triangulated overlaps of the poorest and highest wealth indicator (quintiles 1 and 5) and the least and most potent suicidal ideations, which were (“Did you wish you were dead?” and “Did you think about a specific way to take your life?”) on Fig. 1. We then further triangulated this with depression, which was the mental disorder most significantly associated with suicidal ideation in the literature. Chi-square tests were used to test whether there were significant associations between the wealth index, suicidal ideation and depression.
Fig. 1.
Prevalence of different types of suicidal ideation during past two weeks.
3. Results
3.1. Socio-demographic, economic and mental health characteristics of the respondents
Table 1 summarizes the wealth index and mental health characteristics of the 9742 respondents (53.5% male). Their mean and median ages were age 21.4 and 21.3 (range 15–43) years. Most respondents were single (93.4%), at university (68.6%) and the first or second born in their families (56.9%). All the respondents completed the questions on household items. These contributed to the wealth index, which was evenly distributed among the lowest quintiles (quintiles one to three) with the lowest proportion in the fifth quintile (highest) (16.6%). There was a wide range of mental health problems and alcohol (22.6%) and substance dependence (17.1%) were among the least prevalent.
Table 1.
Socio-demographic economic and mental health characteristics of the respondents.
| Variable | Category | N = 9742 | % |
|---|---|---|---|
| Gender | Male | 5173 | 53.5 |
| Female | 4500 | 46.5 | |
| Missing | 69 | 0.7 | |
| Age | Mean and standard deviation, median; range | 21.4 ± 2.4; 21.3; 15–43 |
|
| Marital status | Married | 607 | 6.3 |
| Single | 9057 | 93.4 | |
| Other (Divorced, separated, widowed) | 38 | 0.4 | |
| Missing | 40 | 0.4 | |
| Religion | Protestant | 5512 | 57.1 |
| Catholic | 3359 | 34.8 | |
| Muslim | 410 | 4.2 | |
| Other | 368 | 3.8 | |
| Missing | 93 | 1.0 | |
| Birth order | 1–2 | 5539 | 56.9 |
| 3–5 | 3271 | 33.6 | |
| 6+ | 920 | 9.5 | |
| Missing | 12 | 0.1 | |
| Level of Education | High School | 1506 | 15.5 |
| College | 1534 | 15.8 | |
| University | 6648 | 68.6 | |
| Missing (Students who did not respond) | 54 | 0.6 | |
| Wealth Index | Quintile 1 (lowest) | 2044 | 21.0 |
| Quintile 2 | 1865 | 19.1 | |
| Quintile 3 | 2002 | 20.6 | |
| Quintile 4 | 2214 | 22.7 | |
| Quintile 5 (highest) | 1617 | 16.6 | |
| Condition screened positive for (PDSQ) | Obsessive compulsive disorder Social phobia |
6308 4885 |
64.8 50.1 |
| Psychosis | 4040 | 41.5 | |
| Agoraphobia | 3351 | 34.4 | |
| Post-traumatic stress disorder | 2652 | 27.2 | |
| Hypochondriasis | 2646 | 27.2 | |
| Somatization disorder | 2504 | 25.7 | |
| Alcohol abuse/dependence | 2198 | 22.6 | |
| Major depressive disorder | 2040 | 20.9 | |
| Panic disorder | 1894 | 19.4 | |
| Drug abuse/dependence | 1670 | 17.1 | |
| Generalized anxiety disorder | 1301 | 13.4 | |
| Bulimia/binge eating disorder | 316 | 3.2 | |
3.2. Prevalence of suicidal ideation (during the past two weeks)
Fig. 1 shows the prevalence of suicidal ideation. The most prevalent form was thinking about specific ways of taking their life (overall 19.3%, males 19.4%, females 19.1%) followed by seriously considering taking their life (overall 14.9%, males 14.8%, females 15.0%). The least prevalent was wishing to be dead (overall, 10.7%, males 9.1%, females12.5%). The overall prevalence of suicidal ideation was 23% (95% CI 21.8–23.5%) and it was higher for females (24.6%, 95% CI 23.4–25.9) than males (20.9%, 95% CI 19.7–22.1).
3.3. Factors associated with suicidal ideation
Table 2 summarizes the factors associated with suicidal ideation at the bivariate level. It was more common in females than males (24.6% vs 21.0%). Other factors associated with a higher prevalence of suicidal ideation (p < .05) were being younger than the median age of 21.3, and being single versus being married or divorced, separated or widowed, and being in university, rather than college or high school.
Table 2.
Socio-demographic and mental health factors associated with suicidality at the bivariate level.
| Parameter | Category | Suicidal ideation | chi-square | 1D.f | P-value | |
|---|---|---|---|---|---|---|
| No | Yes | |||||
| Gender | Male | 4089 (79.0%) | 1084 (21.0%) | 17.8 | 1 | <.001 |
| Female | 3395 (75.4%) | 1105 (24.6%) | ||||
| Age | 21.4 ± 2.4 | 21.3 ± 2.4 | 2.6* | 9740 | .011 | |
| Marital status | Married | 488 (80.4%) | 119 (19.6%) | 13.8 | 2 | .001 |
| Single | 7003(77.3%) | 2054(22.7%) | ||||
| Divorced/separated/widowed | 21 (55.3%) | 17 (44.7%) | ||||
| Religion | Protestant | 4302 (78.0%) | 1210 (22.0%) | 2.7 | 3 | 0.445 |
| Catholic | 2575 (76.7%) | 784 (23.3%) | ||||
| Muslim | 315 (76.8%) | 95 (23.2%) | ||||
| Other | 281 (76.4%) | 87 (23.6%) | ||||
| Birth order | 1–2 | 4251 (76.7%) | 1288 (23.3%) | 4.7 | 2 | .094 |
| 3–5 | 2573 (78.7%) | 698 (21.3%) | ||||
| 6+ | 704 (76.5%) | 216 (23.5%) | ||||
| Level of Education | High school | 1063 (70.6%) | 443 (29.4%) | 51.5 | 2 | <.001 |
| College | 1173 (76.5%) | 361 (23.5%) | ||||
| University | 5258 (79.1%) | 1390 (20.9%) | ||||
| Stress (WERCAP)† | 22.1 ± 24.6 | 39.2 ± 31.2 | − 23.7* | 3049.6 | <.001 | |
| Bipolar (WERCAP)† | 9.1 ± 7.8 | 14.9 ± 9.0 | − 27.2* | 3232.1 | <.001 | |
| Schizophrenia (WERCAP)† | 7.1 ± 8.7 | 14.4 ± 11.6 | − 27.5* | 2968 | <.001 | |
| Condition screened positive for (PDSQ) | Post-traumatic stress disorder | 1546 (58.3%) | 1106 (41.7%) | 757.65 | 1 | <.001 |
| Bulimia/binge eating disorder | 1546 (58.3%) | 1106 (41.7%) | 757.65 | 1 | <.001 | |
| Obsessive compulsive disorder | 120 (38%) | 196 (62%) | 289.54 | 1 | <.001 | |
| Panic disorder | 4495 (71.3%) | 1813 (28.7%) | 382.09 | 1 | <.001 | |
| Psychosis | 1039 (54.9%) | 855 (45.1%) | 680.55 | 1 | <.001 | |
| Agoraphobia | 2562 (63.4%) | 1478 (36.6%) | 767.97 | 1 | <.001 | |
| Social Phobia | 2159 (64.4%) | 1192 (35.6%) | 488.82 | 1 | <.001 | |
| Alcohol abuse/dependence | 3298 (67.5%) | 1587 (32.5%) | 544.31 | 1 | <.001 | |
| Drug Abuse/Dependence | 1288 (58.6%) | 910 (41.4%) | 571.55 | 1 | <.001 | |
| Generalized anxiety disorder | 948 (56.8%) | 722 (43.2%) | 488.92 | 1 | <.001 | |
| Somatization disorder | 704 (54.1%) | 597 (45.9%) | 464.11 | 1 | <.001 | |
| Hypochondriasis | 1544 (61.7%) | 960 (38.3%) | 475.31 | 1 | <.001 | |
D.f = degree of freedom
Independent t Test value;
High scores reflect higher risk.
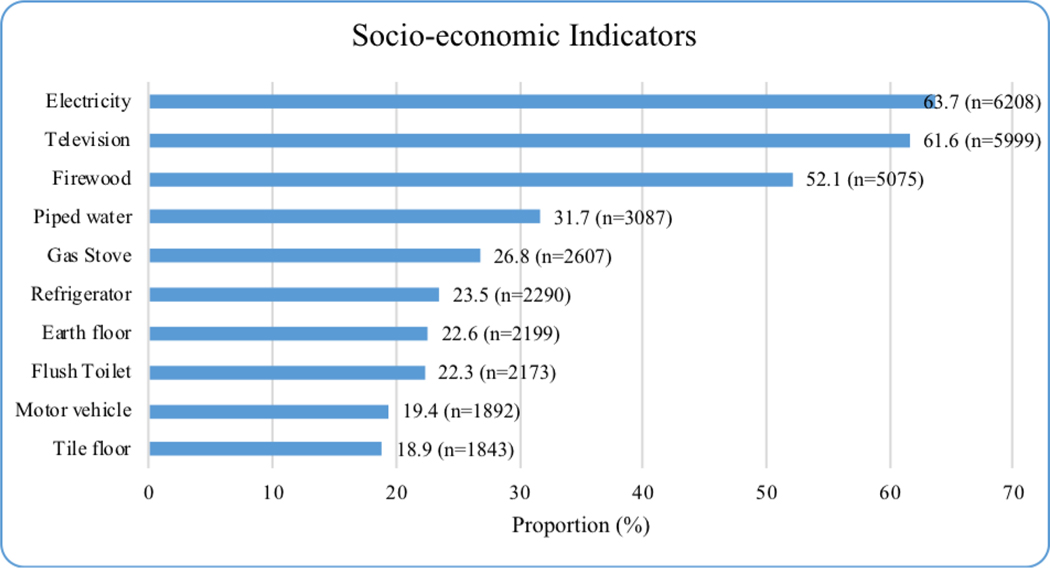
Fig. 2 summarizes the responses on household economic indicators. The two most basic indicators of poor household wealth, firewood as the source of energy and an earth floor, were reported by 52.1 and 22.6% of the respondents.
Fig. 2.
The prevalence of socio-economic indicators in the study participants.
Table 3 summarizes the associations between economic traits and suicidal ideation. Respondents in the poorest wealth quintile, had significantly higher levels of suicidal ideation (28.8%) than those in the highest (20.2%). Those in quintile three had significantly lower levels of suicidal ideation (18.2%) than those in quintile one (28.8%) and four (22.5%) (p < .001).
Table 3.
Economic indicators associated with suicidal ideation in the study participants.
| Characteristics* | Suicidal ideation | Chi-square | D. f | P-value | |
|---|---|---|---|---|---|
| No | Yes | ||||
| Household items | |||||
| Electricity | 4875 (78.5%) | 1333 (21.5%) | 13.0 | 1 | <.001 |
| Radio | 6268 (77.9%) | 1775 (22.1%) | 8.1 | 1 | .004 |
| Television | 4691 (78.2%) | 1308 (21.8%) | 6.0 | 1 | .014 |
| Refrigerator | 1804 (78.8%) | 486 (21.2%) | 3.4 | 1 | .067 |
| Cell phone | 5732 (77.9%) | 1629 (22.1%) | 4.2 | 1 | .041 |
| Bicycle | 3011 (78.3%) | 836 (21.7%) | 2.9 | 1 | .089 |
| Motorcycle | 1568 (79.1%) | 414 (20.9%) | 4.3 | 1 | .039 |
| Motor vehicle | 1468 (77.6%) | 424 (22.4%) | 0.1 | 1 | .805 |
| Homes source of water | |||||
| Piped water | 2452 (79.4%) | 635 (20.6%) | 15.2 | 4 | .004 |
| Public water | 1016 (76.3%) | 316 (23.7%) | |||
| Well water | 2048 (76.7%) | 622 (23.3%) | |||
| Surface water | 1857 (76.5%) | 570 (23.5%) | |||
| Other source | 117 (70.1%) | 50 (29.9%) | |||
| Home floor | |||||
| Earth floor | 1630 (74.1%) | 569 (25.9%) | 17.2 | 1 | <.001 |
| Cement floor | 4349 (78.6%) | 1183 (21.4%) | 11.2 | 1 | .001 |
| Tile floor | 1445 (78.4%) | 398 (21.6%) | 1.4 | 1 | .241 |
| Wood floor | 126 (69.6%) | 55 (30.4%) | 6.3 | 1 | .012 |
| Other floor material | 22 (73.3%) | 8 (26.7%) | 0.3 | 1 | .596 |
| Homes toilet | |||||
| No toilet | 87 (58.8%) | 61 (41.2%) | 37.4 | 3 | <.001 |
| Pit latrine | 5556 (77.4%) | 1622 (22.6%) | |||
| Flush toilet | 1718 (79.1%) | 455 (20.9%) | |||
| Other toilet facility | 165 (71.4%) | 66 (28.6%) | |||
| Household cooking method | |||||
| Firewood | 3891 (76.7%) | 1184 (23.3%) | 11.3 | 5 | .045 |
| Charcoal | 1049 (78.3%) | 290 (21.7%) | |||
| Kerosene stove | 255 (73.3%) | 93 (26.7%) | |||
| Gas stove | 2060 (79%) | 547 (21%) | |||
| Electric stove | 199 (77.7%) | 57 (22.3%) | |||
| Other | 80 (72.1%) | 31 (27.9%) | |||
| Wealth index | |||||
| Quintile one | 1455(71.2%) | 589 (28.8%) | 72.7 | 4 | <.001 |
| Quintile two | 1439 (77.2%) | 426 (22.8%) | |||
| Quintile three | 1638 (81.8%) | 364 (18.2%) | |||
| Quintile four | 1716 (77.5%) | 498 (22.5%) | |||
| Quintile five | 1290 (79.8%) | 327 (20.2%) | |||
This table uses row percentages. For example 78.5% of those who answered no to suicide ideation and 21.5% who said yes lived in a house with electricity; bold figures indicate significance; D.f represents degree of freedom.
3.4. Multivariate analysis of factors associated with suicidal ideation
Table 4 summarizes the results from the multivariate analysis of factors associated with suicidal ideation. The risk for suicidal ideation was higher for females than males (aOR 1.317, 95% CI (1.176–1.475) and being divorced/separated/widowed than married (aOR 2.736, 95% CI 1.255–5.964). Being in high school rather than university (aOR 1.340, 95% CI 1.150, 1.561) was significantly associated with suicidal ideation, even after controlling for age. All psychiatric conditions were significantly associated with suicidal ideation, except agoraphobia and OCD (p > .05).
Table 4.
Independent Predictors of suicidal ideation.
| Parameter | Category | A.O.R | 95% CI | Sig. | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Gender | Male | Ref. | |||
| Female | 1.317 | 1.176 | 1.475 | <.001 | |
| Age | 0.990 | 0.966 | 1.014 | 0.403 | |
| Marital status | Married | Ref. | |||
| Single | 1.229 | 0.967 | 1.561 | .092 | |
| Divorced/separated/widowed | 2.736 | 1.255 | 5.964 | .011 | |
| Level of Education | High School | 1.340 | 1.150 | 1.561 | <.001 |
| College | 1.018 | 0.876 | 1.182 | 0.817 | |
| University | Ref. | ||||
| Wealth Index | Quintile 1 | 1.396 | 1.172 | 1.662 | <.001 |
| Quintile 2 | 1.035 | 0.862 | 1.242 | 0.716 | |
| Quintile 3 | 0.828 | 0.688 | 0.997 | .047 | |
| Quintile 4 | 1.091 | 0.915 | 1.300 | 0.334 | |
| Quintile 5 | Ref. | ||||
| Stress (WERCAP)† | 1.005 | 1.003 | 1.008 | <.001 | |
| Bipolar (WERCAP)† | 1.028 | 1.019 | 1.036 | <.001 | |
| Schizophrenia (WERCAP)† | 1.016 | 1.009 | 1.023 | <.001 | |
| Post-traumatic stress disorder | 1.490 | 1.316 | 1.688 | <.001 | |
| Bulimia/binge eating disorder | 1.993 | 1.522 | 2.609 | <.001 | |
| Obsessive compulsive disorder | 1.133 | 0.980 | 1.309 | .091 | |
| Panic disorder | 1.275 | 1.111 | 1.464 | .001 | |
| Psychosis | 1.422 | 1.247 | 1.622 | <.001 | |
| Agoraphobia | 0.946 | 0.832 | 1.077 | 0.403 | |
| Social Phobia | 1.308 | 1.146 | 1.494 | <.001 | |
| Alcohol abuse/dependence | 1.534 | 1.324 | 1.778 | <.001 | |
| Drug Abuse/Dependence | 1.284 | 1.095 | 1.505 | .002 | |
| Generalized anxiety disorder | 1.286 | 1.107 | 1.496 | .001 | |
| Somatization disorder | 1.189 | 1.047 | 1.352 | .008 | |
| Hypochondriasis | 1.260 | 1.105 | 1.435 | .001 | |
Note:
High scores reflect higher risk.
The PDSQ score for major depression is not in the table because the scale we used to measure suicidality was obtained from the subset questions that measure depression (questions 16 to 21). This means that there was higher collinearity and variance inflation when it was included in the model.
Participants who screened positive for all the psychiatric conditions at different cut-off points had significantly higher proportions of suicidal ideation than those who screened negative (p < .001).
3.5. Overlaps between depression, poverty and suicidal thoughts
Of the 1042 (10.7%) who wished they were dead, 1.4% came from the highest wealth index quintile (five) and more than double that percentage (3.1%) came from the poorest quintile (one), which was a significance difference (p = .038). Of the 1880 (19.3%) who had thought about specific ways of taking their life, 3.0 and 5.3% were from quintiles five and one, respectively (p < .001). When the overlaps between the wealth index, specific ways to commit suicide and depression were computed, there was a higher proportion of participants in quintile one than five (2.8% vs. 1.5%), which was a significant difference (p = .039). No significant differences were observed between the wealth index and depression and wishing to be dead.
4. Discussion
Nearly a quarter (23%) of the participants in this study reported suicidal ideation in the last two weeks. It is not possible draw direct comparisons with suicidal ideation rates in other studies, due to different definitions and study periods. However, other studies have also reported different types of suicidal ideation and relatively high rates, without specifying the time limit. The exception is (Amare et al., 2018) who found that 26.36% of their Ethiopian sample had thought about committing suicide in the last one month, rather than the two weeks in our study. That figure was higher than average 23% reported by other studies. It was even higher than the 19.3% in our study, which asked if respondents had thought of a specific way to take their life. This was a significant finding, because it has been reported to be highly predictive of suicide attempts (Amare et al., 2018) and Kenya has very few resources to recognize and manage suicide attempts. We did not ask respondents about suicide attempts, because it was not included in instrument we used.
4.1. Suicidal ideation and socio-demographics
We found that suicidal ideation was associated with being in high school rather than university (p < .001), after controlling for level of education and age. These findings agreed with et al. (2019), who reported a similar association between age, sex, education and attitudes towards suicide. The differences related to education levels are understandable. Being in high school is an uncertain time for students, who are still undergoing biological, social and emotional development and academic challenges. Reaching college or university means that exams went well and being at university is seen as anindicator of success in life as most high school students do not make it this far. Other factors that differentiate high school from university students could include family background, resilience and cognitive and educational abilities, regardless of age. But equally important in the explanation of higher levels of depression in the high school students is the fact that these students had not been going to school because of nationwide closure of schools.
Males were more represented in the study than females and this could be explained in at least two ways. Boys enjoy more freedom and access to extra family activities and the high school boys were more likely to be allowed to go to the study data collection points schools were closed. Secondly, most of the colleges that participated in the studies were technical colleges, which attract more boys, apart from the few that provided nursing training. We found that 6.3% of the student were married, which reflects the fact older students were included. The breakdown by religion pattern reflected national Kenyan patterns (Kenya National Bureau of Statistics, 2019a). The 1–2 birth order in the majority of students was a reflection of the decreasing family size in Kenya, as shown in the 2019 National Census(Kenya National Bureau of Statistics, 2019b). Despite the over-representation of male gender in the sample, female gender was associated with suicidal ideation (p < .001), which is similar to the studies reviewed in the Introduction.
4.2. Suicidal ideation and mental disorders
To our knowledge, this was the first study report a wide range of different mental health issues, studied at the same time, and their association with suicidal ideas. High risk scores for stress, bipolar and schizophrenia and most of the PDSQ disorders, including alcohol and substance dependence, were significantly (p < .05) associated with suicidal ideation in this study. Similar results were reported by Bowen et al., who found that anxiety, depression/low mood and anger/irritability were important predictors of suicidal thoughts (Bowen et al., 2015). In our study, schizophrenia was significantly associated with suicidality (p < .001, aOR 1.02 95% CI 1.01–1.02, in agreement with previous findings (Kelleher and Cannon, 2011). Although the prevalence of the different types of mental health issues, alcoholic and substance dependence, were not the primary focus of our study, it was noteworthy that alcohol and drug dependence in this study were lower than in Western settings(Substance Abuse and Mental Health Services Administration, 2019; European Monitoring Centre for Drugs and Drug AddictionEMCDDA, 2017; Inter-American Drug Abuse Control Commission, 2015). We speculate that this may have been a reflection of stronger cultural restraint of these substances and parenting that goes beyond 18 years.
4.3. Suicidal ideation and wealth
When it came to economic measures, the wealth index quintiles were almost equally distributed, which suggests that the students in this study reflected the whole economic range in Kenyan society. The highest quintile was the least common, as expected, because wealthy families can send their children to private institutions. Nearly two-third of the respondents (63.7%) had electricity, which reflects the Kenyan Government policy that all rural electricity is very highly subsided, regardless of socio-economic status. This policy came after electricity was considered as an economic indicator. But since this happened to all Kenyans, electricity as an indicator balances out in all study participants. Other indicators that depend on electricity, such as refrigerators and TVs, can be viewed in the same way. More than half of the respondents (52%) used firewood as a source of energy and only 32% had piped water. These, plus earth floors at home, or even more basic than that, are the most clear indicators of poverty. Despite this, all the negative responses to most of the other economic indicators were associated with suicidal ideation.
Our study clearly demonstrated that poverty, mental health issues and severe suicidality were interlinked and this calls for both public health-oriented and individual suicide preventive measures(Wasserman, 2019).
4.4. Need for interventions
The findings of this study, particularly the fact that 19.3% of participants had thought of specific ways to commit suicide, calls for urgent and innovative interventions using existing resources. These include making communities and educational establishments more aware, integrated youth-centered approaches that identify those at highest risk and match them with much-needed help and training frontline workers to help the identified high risk youth to manage suicidal behavior. The WHO Mental Health Gap Action Programme Intervention Guide (World Health Organization, 2010) provides psychosocial and clinical interventions for suicidal behavior. We have demonstrated that frontline workers trained using this Guide can manage suicidal behavior and make referrals (Mutiso et al., 2019). These potential interventions support the recommendations by the WHO on suicide prevention (World Health Organization, 2014), particularly during and after the COVID-19 pandemic (Wasserman et al., 2020), as the pandemic is expected to lead to increased levels of suicidal behavior in all age groups (Ndetei et al., 2020).
4.5. Strengths and limitations of the present study
The study had a number of strengths and we believe it is unique with regard to studies in low-income and middle-income countries. It had the largest sample size of any single study using the same protocol. The study compared three kinds of educational establishments at the same time. Students from high schools, technical colleges and universities, ranging from 15–43 years of age, answered a wide range of questions on demographics, mental health and suicide. Another strength was that the colleges and university students came from diverse regions of Kenya, as admissions were handled centrally. In contrast, all the high school students came from the local communities. There was a nationwide closure of high schools at the time of the study and therefore if this closure had any effect on the results then it was the same across the country. This is not to say that if the study had been carried out when the schools had not been closed it could not have produced different results, as the mental health consequences could have been greater during closure. A third strength was the high response rates to the questions. These all exceeded 99%, with the exception of religion, which scored exactly 99%. High response rates are common in Kenyan community-based education survey (Ndetei et al., 2010, 2009). Students and parents place immense value on such surveys, as education is regarded as the best investment, with the highest potential to propel children into successful futures and help them and their families escape from poverty. Kenyan people feel that surveys help to improve education. However, we should point out that we approached colleges and university students at specific time points, but high school students had to come to the community centers. We do not know whether this affected our findings.
There were several limitations. We do not know what effect the high school closures, due to a long-running teachers strike, had on the students’ mental health. Another limitation was that student face different pressures at various ages, including examinations and uncertainties about the future, and these could also had have an impact on their mental health. Another limitation was that our findings cannot be compared to studies that used different methods to synthesize the data. However, our data provided preliminary findings on the basis that future comparisons can be made if comparable measures and analytical approaches are used. Further, our data calls for studies on which suicidal ideas could be regarded as “active” or “passive” in the sense they do or do not predict suicidal attempts.
4.6. Future research
There is need to go beyond cross-sectional studies and conduct prospective studies to determine progression from suicidal ideas to actual suicide attempts and completed suicides and to assess what kind of suicidal ideas most strongly predict these.
5. Conclusion
There was high prevalence of suicidal ideas in our study population, particularly specific thoughts about how to commit suicide. This calls for interventions. Suicidal ideation has been associated with a wide range of socio-demographic factors, mental health issues, alcohol and substance dependence and poverty. We have also seen overlaps between suicidal ideas, mental health issues and poverty and these highlight the need for integrated approaches. We recommend that the WHO evidence-based suicide prevention strategies should be adapted, particularly during and after the COVID-19 pandemic. Our findings supported our hypotheses and answered our research questions. However, there is still a need for prospective research to determine the factors that link suicidal ideas to suicide attempts.
Supplementary Material
Acknowledgments
Africa Mental Health Research and Training Foundation for financial and logistical support; Administrative Heads of the Colleges and the University for permission for their students to participate; the community leadership for facilitating participation of students in high schools; the research assistants. Lydia Onsinyo, Rita Alietsi and and Grace Mutevu of AMHRTF for editorial assistance.
Funding
Africa Mental Health Research and Training Foundation (AMHRTF) in-house support for this particular set of data collection and analysis. The Foundation did not influence researchers work independently.
Footnotes
Ethics approval
Ethical approval was granted by the Maseno University Ethics Review Board in Kenya (IRB number MSU/DRPI/MUERC/00344/16).
Availability of data and materials
On request
CRediT authorship contribution statement
David M. Ndetei: Conceptualization, Writing – original draft. Victoria N. Mutiso: Data curation, Writing – original draft. John R. Weisz:. Consolate A. Okoth:. Christine Musyimi: Formal analysis, Data curation. Esther N. Muia:. Tom L. Osborn:. Andre Sourander:. Danuta Wasserman:. Daniel Mamah:.
Declaration of Competing Interest
The author(s) declare no conflict of interest.
Supplementary materials
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jad.2022.01.055.
References
- Abdu Z, Hajure M, Desalegn D, 2020. Suicidal behavior and associated factors among students in mettu university, south west ethiopia, 2019: an institutional based cross-sectional study. Psychol. Res. Behav. Manag 13, 233–243. 10.2147/PRBM.S240827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akca SO, Yuncu O, Aydin Z, 2018. Mental status and suicide probability of young people: a cross-sectional study. Rev. Assoc. Med. Bras 64, 32–40. 10.1590/1806-9282.64.01.32. [DOI] [PubMed] [Google Scholar]
- Amare T, Meseret Woldeyhannes S, Haile K, Yeneabat T, 2018. Prevalence and associated factors of suicide ideation and attempt among adolescent high school students in Dangila Town, Northwest Ethiopia. Psychiatry J. 2018, 1–9. 10.1155/2018/7631453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen R, Balbuena L, Peters EM, Leuschen-Mewis C, Baetz M, 2015. The relationship between mood instability and suicidal thoughts. Arch. Suicide Res 19, 161–171. 10.1080/13811118.2015.1004474. [DOI] [PubMed] [Google Scholar]
- Campbell DT, Fiske DW, 1959. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychol. Bull 56, 81–105. 10.1037/h0046016. [DOI] [PubMed] [Google Scholar]
- Canbaz S, Terzi Ö, 2018. The prevalence of suicidal ideation in adolescents and associated risk factors: an example from Turkey. Adv. Ther 35, 839–846. 10.1007/s12325-018-0720-2. [DOI] [PubMed] [Google Scholar]
- Crumlish N, Whitty P, Kamali M, Clarke M, Browne S, McTigue O, Lane A, Kinsella A, Larkin C, O’Callaghan E, 2005. Early insight predicts depression and attempted suicide after 4 years in first-episode schizophrenia and schizophreniform disorder. Acta Psychiatr. Scand 112, 449–455. 10.1111/j.1600-0447.2005.00620.x. [DOI] [PubMed] [Google Scholar]
- Dachew BA, Bifftu BB, Tiruneh BT, Anlay DZ, Wassie MA, 2018. Suicidal thoughts among university students in Ethiopia. Ann. Gen. Psychiatry 17, 1. 10.1186/s12991-017-0172-0. [DOI] [Google Scholar]
- Dassori AM, Mezzich JE, Keshavan M, 1990. Suicidal indicators in schizophrenia. Acta Psychiatr. Scand 81, 409–413. 10.1111/j.1600-0447.1990.tb05472.x. [DOI] [PubMed] [Google Scholar]
- Del Barrio V, 2016. Diagnostic and statistical manual of mental disorders. The Curated Reference Collection in Neuroscience and Biobehavioral Psychology. American Psychiatric Association, Arlington VA, pp. 1–947. 10.1016/B978-0-12-809324-5.05530-9. [DOI] [Google Scholar]
- Eskin M, Sun JM, Abuidhail J, Yoshimasu K, Kujan O, Janghorbani M, Flood C, Carta MG, Tran US, Mechri A, Hamdan M, Poyrazli S, Aidoudi K, Bakhshi S, Harlak H, Moro MF, Nawafleh H, Phillips L, Shaheen A, Taifour S, Tsuno K, Voracek M, 2016. Suicidal behavior and psychological distress in university students: A 12-nation study. Arch. Suicide Res 20, 369–388. 10.1080/13811118.2015.1054055. [DOI] [PubMed] [Google Scholar]
- European Monitoring Centre for Drugs and Drug Addiction(EMCDDA), 2017. European Drug Report. European Drug Report 2017: Trends and Developments. European Union Publications Office, pp. 1–90. 10.1097/JSM.0b013e31802b4fda. . [DOI] [Google Scholar]
- Guedria-Tekari A, Missaoui S, Kalai W, Gaddour N, Gaha L, 2019. Suicidal ideation and suicide attempts among Tunisian adolescents: Prevalence and associated factors. Pan Afr. Med. J 34 10.11604/pamj.2019.34.105.19920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hadzi-Pavlovic D, 2010. Multivariate analysis of variance. Acta Neuropsychiatr. 10.1111/j.1601-5215.2010.00488.x. [DOI] [Google Scholar]
- Hakstian AR, Cattell RB, 1982. The behavior of number-of-factors rules with simulated data. Multivar. Behav. Res 17, 193–219. 10.1207/s15327906mbr1702_3. [DOI] [PubMed] [Google Scholar]
- Harttgen K, Vollmer S, 2013. Using an asset index to simulate household income. Econ. Lett 121, 257–262. 10.1016/j.econlet.2013.08.014. [DOI] [Google Scholar]
- Hsieh CJ, Godwin D, Mamah D, 2016. Utility of Washington early recognition center self-report screening questionnaires in the assessment of patients with schizophrenia and bipolar disorder. Front. Psychiatry 7, 149. 10.3389/fpsyt.2016.00149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inter-American Drug Abuse Control Commission, 2015. Report on Drug Use in the Americas 2015. Organization on American State, OEA/Ser.L/XIV.6.6. [Google Scholar]
- Kaiser HF, 1960. The application of electronic computers to factor analysis. Educ. Psychol. Meas 20, 141–151. 10.1177/001316446002000116. [DOI] [Google Scholar]
- Kelleher I, Cannon M, 2011. Psychotic-like experiences in the general population: characterizing a high-risk group for psychosis. Psychol. Med 10.1017/S0033291710001005. [DOI] [PubMed] [Google Scholar]
- Kenya National Bureau of Statistics, 2019a. 2019 Kenya Population and Housing Census; Volume IV: Distribution of Population by Socio-Economic Characteristics, 2019. KNBS. Journal of Visual Languages & Computing. Na. [Google Scholar]
- Kenya National Bureau of Statistics, 2019b. 2019 Kenya Population and Housing Census; Volume II: Distribution of Population by Administrative Units. KNBS. [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS, 1994. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the united states: results from the national comorbidity survey. Arch. Gen. Psychiatry 51, 8–19. 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Koenigsberg HW, Kaplan RD, Gilmore MM, Cooper AM, 1985. The relationship between syndrome and personality disorder in DSM-III: Experience with 2,462 patients. Am. J. Psychiatry 142, 207–212. 10.1176/ajp.142.2.207. [DOI] [PubMed] [Google Scholar]
- Magis D, Béland S, Tuerlinckx F, De Boeck P, 2010. A general framework and an R package for the detection of dichotomous differential item functioning. Behav. Res. Methods 42, 847–862. 10.3758/BRM.42.3.847. [DOI] [PubMed] [Google Scholar]
- Mamah D, Owoso A, Sheffield JM, Bayer C, 2014. The WERCAP screen and the WERC stress screen: psychometrics of self-rated instruments for assessing bipolar and psychotic disorder risk and perceived stress burden. Compr. Psychiatry 55, 1757–1771. 10.1016/j.comppsych.2014.07.004. [DOI] [PubMed] [Google Scholar]
- Mezzich JE, Fabrega H, Coffman GA, Haley R, 1989. DSM-III disorders in a large sample of psychiatric patients: frequency and specificity of diagnoses. Am. J. Psychiatry 146, 212–219. 10.1176/ajp.146.2.212. [DOI] [PubMed] [Google Scholar]
- Morris SS, Carletto C, Hoddinott J, Christiaensen LJM, 2000. Validity of rapid estimates of household wealth and income for health surveys in rural Africa. J. Epidemiol. Community Health 54, 381–387. 10.1136/jech.54.5.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortier P, Demyttenaere K, Auerbach RP, Cuijpers P, Green JG, Kiekens G, Kessler RC, Nock MK, Zaslavsky AM, Bruffaerts R, 2017. First onset of suicidal thoughts and behaviors in college. J. Affect. Disord 207, 291–299. 10.1016/j.jad.2016.09.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutiso VN, Pike KM, Musyimi CW, Gitonga I, Tele A, Rebello TJ, Thornicroft G, Ndetei DM, 2019. Feasibility and effectiveness of nurses and clinical officers in implementing the WHO mhGAP intervention guide: pilot study in Makueni county, Kenya. Gen. Hosp. Psychiatry 59, 20–29. 10.1016/j.genhosppsych.2019.04.005. [DOI] [PubMed] [Google Scholar]
- Ndetei D, Mutiso V, Musyimi C, Kameti F, 2020. Psychosocial response to COVID-19 in Africa, with special reference to Kenya. World Soc. Psychiatry 2, 97. 10.4103/wsp.wsp_47_20. [DOI] [Google Scholar]
- Ndetei DM, Khasakhala LI, Mutiso V, Ongecha-Owuor FA, Kokonya DA, 2010. Drug use in a rural secondary school in Kenya. Subst. Abus 31, 170–173. 10.1080/08897077.2010.495313. [DOI] [PubMed] [Google Scholar]
- Ndetei DM, Khasakhala LI, Mutiso V, Ongecha-Owuor FA, Kokonya DA, 2009. Patterns of drug abuse in public secondary schools in Kenya. Subst. Abus 30, 69–78. 10.1080/08897070802606436. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2019. Results from the 2018 National Survey on Drug Use and Health: Detailed tables., Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Rockville, MD. [Google Scholar]
- Pandey AR, Bista B, Ram Dhungana R, Aryal KK, Chalise B, Dhimal M, 2019. Factors associated with suicidal ideation and suicidal attempts among adolescent students in Nepal: findings from global school-based students health survey. PLoS One 14, e0210383. 10.1371/journal.pone.0210383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quarshie ENB, Cheataa-Plange HV, Annor F, Asare-Doku W, Lartey JKS, 2019. Prevalence of suicidal behavior among nursing and midwifery college students in Ghana. Nurs. Open 6, 897–906. 10.1002/nop2.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizopoulos D, 2006. Itm: An R package for latent variable modeling and item response theory analyzes. J. Stat. Softw 17, 1–25. 10.18637/jss.v017.i05. [DOI] [Google Scholar]
- Robins LN, Regier DA, 1991. Psychiatric Disorders in America, in: The Epidemiologic Catchment Area Study. The Free Press. [Google Scholar]
- Shear MK, Greeno C, Kang J, Ludewig D, Frank E, Swartz HA, Hanekamp M, 2000. Diagnosis of nonpsychotic patients in community clinics. Am. J. Psychiatry 157, 581–587. 10.1176/appi.ajp.157.4.581. [DOI] [PubMed] [Google Scholar]
- Smits J, Steendijk R, 2015. The international wealth index (IWI). Soc. Indic. Res 122, 65–85. 10.1007/s11205-014-0683-x. [DOI] [Google Scholar]
- Strandheim A, Bjerkeset O, Gunnell D, Bjørnelv S, Holmen TL, Bentzen N, 2014. Risk factors for suicidal thoughts in adolescence-a prospective cohort study: the young-HUNT study. BMJ Open 4. 10.1136/bmjopen-2014-005867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voss C, Ollmann TM, Miché M, Venz J, Hoyer J, Pieper L, Höfler M, Beesdo-Baum K, 2019. Prevalence, onset, and course of suicidal behavior among adolescents and young adults in germany. JAMA Netw. Open, e1914386. 10.1001/jamanetworkopen.2019.14386. American Medical Association. [DOI] [PMC free article] [PubMed]
- Wasserman D, 2019. Difficulties in preventing suicidal behaviors in spite of existing evidence-based preventive methods – an overview. Arch. Psychiatry Psychother 21, 7–12. 10.12740/APP/104408. [DOI] [Google Scholar]
- Wasserman D, Iosue M, Wuestefeld A, Carli V, 2020. Adaptation of evidence-based suicide prevention strategies during and after the COVID-19 pandemic. World Psychiatry 19, 294–306. 10.1002/wps.20801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, 2014. Preventing suicide: A global imperative Executive Summary. WHO Press, Geneva: [WWW Document]URL. http://www.who.int/mental_health/suicide-prevention/world_report_2014/en/. [Google Scholar]
- World Health Organization, 2010. mhGAP Intervention Guide - For Mental, Neurological and Substance Abuse Disorders in Non-Specialized Health Settings: Mental Health Gap Action Programme. World Health Organization. [PubMed] [Google Scholar]
- Zimmerman M, Mattia JI, 2001. The psychiatric diagnostic screening questionnaire: development, reliability and validity. Compr. Psychiatry 10.1053/comp.2001.23126. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.