Abstract
Introduction:
Laparoscopic ventral hernia repair is undergoing a paradigm shift with the introduction of numerous new techniques to improve the outcomes. Enhanced-view totally extra-peritoneal (eTEP) is a novel approach for the repair of ventral herniae introduced by Belyansky et al. The key innovation lies in placing the mesh in a large retrorectus–pre-peritoneal space contrary to the widely practiced intra-peritoneal placement. This approach can be easily coupled with a component separation in the form of transversus abdominis release (TAR) for large herniae. We conducted a midterm analysis of ‘eTEP’ approach to ventral hernia at a high-volume tertiary care centre and present our results of over 3 years of employing this technique.
Methodology:
A retrospective study of 150 cases of ventral hernia repaired using eTEP approach from January 2018 to February 2021 at a tertiary care centre by a team of three surgeons. The procedures were performed by a single team of three members headed by the first author.
Results:
Out of total 150 cases, incisional hernia occurred in 73 cases (48.7%), primary hernia occurred in 48 cases (32%) and recurrent hernia in 29 cases (19.3%). Although the majority of incisional (87.7%) and recurrent (79.3%) ventral hernias occurred in female, the incidence of primary ventral hernia was equal at 24 cases in both genders. The majority of the cases (80.7%) underwent eTEP RS procedure, and the rest were W3 hernias, which were managed by including a component separation in the form of eTEP TAR. The operating time for eTEP TAR (222.24 min ± 32.56) compared to eTEP RS (124.33 ± 23.68) was significantly longer. The mean length of stay was significantly shorter for primary hernias (3.75 days ± 1.62) compared to recurrent (5.21 days ± 2.51) and incisional hernias (4.36 days ± 2.19) (F = 4.376) (P = 0.014). The peri-operative period was uneventful in majority of the cases. We experienced a seroma rate of 5.8% in our series. At follow-up of 1 year, 3.3% of patients complained of discomfort/bulge in the upper abdomen. There were no other surgical site occurrences (SSO) in the form infection, posterior rectus sheath disruption and skin necrosis. We observed no recurrences till date with a minimum follow-up of 1 year.
Conclusion:
eTEP approach to ventral hernia is a promising abdominal wall reconstruction technique. It is safe and offers good functional outcomes with restoration of abdominal wall dynamics. It is a reproducible and safe technique for tackling various types of ventral hernia. It is specifically useful in managing unusual lateral hernias, incisional and recurrent hernias with ease.
Keywords: Endoscopic hernia, enhanced-view totally extra-peritoneal, hernia, laparoscopic hernia, laparoscopic ventral hernia repair, transversus abdominis release
INTRODUCTION
Ventral hernia repair (VHR) has been evolving over the years. The science of restoration of a normal abdominal anatomy has grown from primary fascial or anatomical repairs across different layers of the abdominal wall to minimally invasive procedures in a natural anatomical plane, i.e., the retromuscular pre-peritoneal plane. The use of the retromucular preperitoneal plane for mesh placement in groin hernias was pioneered by Rives et al. who believed it to be the plane of choice for the placement of a broad mesh that worked on the principle of radially distributed intra-abdominal tension to the mesh for its fixation.[1] This technique was later applied to the large ventral hernias with successful outcomes.[2,3]
In 1993, Leblanc and Booth introduced the laparoscopic ventral hernia repair (LVHR) where an intra-peritoneal onlay mesh was placed as a barrier with successful outcomes in terms of recurrence rates and wound complications.[4] This approach was standardised by Heniford et al. and the superiority of laparoscopic repair over open was well established.[5] In spite of a readily adaptable technique and advances in biological composite mesh prosthesis, the short-comings of this intra-peritoneal placement of the mesh were seen over the years in the form of adhesive obstruction, enterocutanoeus fistula and mesh erosion due to the direct contact of the mesh with the abdominal viscera. Transabdominal pre-peritoneal (TAPP) technique was described by Prasad et al. to overcome these issues encountered with intra-peritoneal placement of mesh.[6] It requires the creation of thin peritoneal flaps for mesh placement in the pre-peritoneal space from the transabdominal route. The plane of placement might be ideal, but the technique is difficult to perform even in experienced hands and often progresses to salvage IPOM. Innovating from TEP for groin hernia, Jorge Dias popularized the ‘Enhanced’ or ‘Extended’ view (eTEP) which offered a more flexible port placement along with a wide space for better handling of the tissues.[7,8] It was only a matter of time until these principles were applied to ventral hernia by Igor Belyansky et al.[9] The eTEP approach can be readily combined with transversus abdominis release (TAR)[10] for large hernias. This provides an easily reproducible repair of complex ventral hernias even for beginners in the field of minimal access surgery.
The present study conducted retrospectively includes a total of 150 cases performed using the same principles of eTEP in our centre.
METHODOLOGY
Study design
This is a single centre retrospective study conducted at a tertiary care centre. One hundred and fifty cases of ventral hernia underwent eTEP repair during a period of 3 years between July 2018 and July 2021. The procedures were performed by a single team of 3 members headed by the first author.
All patients were assessed clinically and classified according to European Hernia Society (EHS) guidelines. Computed tomography evaluation was done only for complex hernias. After pre-operative surface marking under ultrasonography guidance, all patients were subjected to eTEP approach regardless of the complexity of hernia.
The exclusion criteria included a hernia defect size of >15 cm, loss of domain hernia, poor scar, ulceration over skin, previous mesh infection, sinus tract and previous retro-rectus mesh placement.
Relevant data from the medical records department were collected in specifically designed case sheets. Statistical analysis was done by using the descriptive and inferential statistics using the Chi-square test and software used in the analysis were SPSS 22.0 software (SPSS, Inc., Chicago, IL, USA) and GraphPad Prism version 5.0 (GraphPad Software, Inc., LaJolla, CA, USA) and P < 0.05 was considered level of significance.
Procedure
Our surgical technique follows the principles laid down by the landmark study of Igor Belyansky et al.[9,11] We have made some modifications to make it suitable for beginners in advanced endoscopic surgery so that it can be readily adopted by the masses.
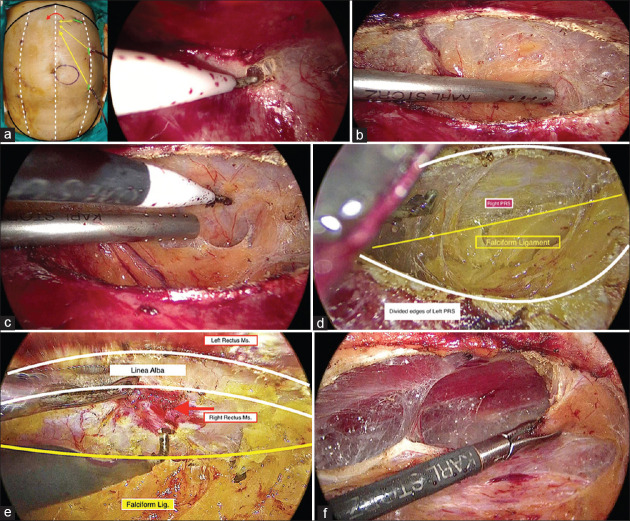
Patient positioning and surface marking
The patient is placed in a supine position with both arms by the side of the patient. The operating table is angulated to hyperextend the patient’s torso to increase the working space. After a thorough surgical scrub, the patient’s surface anatomy marking is used to highlight the important landmarks including the xiphisternum, linea Alba (LA), umbilicus, pubis, bilateral costal margins, bilateral linea semilunaris (LS), arcuate line (AL) and the hernia defect [Figures 1 and 2].
Figure 1.
Surface marking and patient positioning
Figure 2.
Operation theatre setup
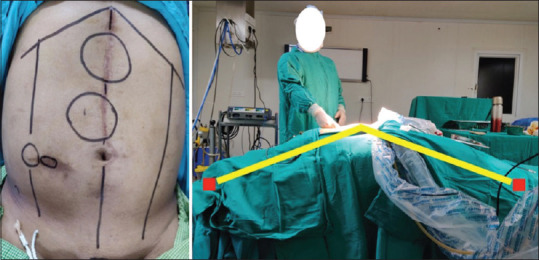
Enhanced-view totally extra-peritoneal (eTEP) access port
A left subcostal 10 mm incision is made for the camera port, deepened with blunt dissection using the index finger in a rotatory motion, until the anterior rectus sheath is reached.(It is incised sharply and blunt finger dissection continued deep to reach the rectus abdominis (RA) muscle. The posterior rectus sheath (PRS) can be palpated as a firm structure at the tip of the finger as the soft fibres of the RA muscle are split with dissection. A retro-rectus plane can be thus created gently using the index finger [Figure 3]. This allows for minimal dissection with a snugly fit trocar. A Hasson’s cannula can thus be avoided as a regular 10-mm port can be used without any CO2 leak. This method was standardised after a few cases of inadvertent ruptures of the PRS and peritoneum were seen with the balloon inflating method leading to an early creation of pneumo-peritoneum, limiting the working space. It was found to be safe even in patients with a thin PRS and peritoneum. Optical trocar entry has been practiced at various centres, but our experience with a blunt finger dissection is safe, cost-effective with a flexibility of using regular laparoscopic ports. Once the access port is secured in the retro-rectus plane, its position is confirmed with an endoscope and inflation with CO2 is started.
Figure 3.

eTEP access – Incision of anterior rectus sheath and finger dissection in left retro-rectus space
The avascular dissection continues inferiorly and it allows for two working ports (5 mm) to be inserted on the left side [Figure 4]. The position of the same may vary according the hernia defect. The left retro-rectus space and space of Retzius is completely defined till the pubic bone is visualised [Figure 5].
Figure 4.
Dissection of left retro-rectus space
Figure 5.
Complete left retro-rectus tunnel
Crossover
The next step of the dissection is the crossover [Figure 6a-f] from the left to right retro-rectus space. This can be done either from the epigastric region or from below the AL; bottom-top technique. During the epigastric crossover, it might become difficult to ascertain the point of right PRS division early in the learning curve. We follow a novel 3-needle technique to identify the same. The first needle is inserted in the midline and a 2nd needle is inserted in the same transverse plane on the left side at the level of PRS division. The distance between these two needles can be measured and a 3rd needle can be inserted on the right side at equal distance to ascertain the point of right PRS division.
Figure 6.
Top crossover. (a) Incision Left PRS, (b) Dissection plane superior to Falciform ligament, (c and d) Reaching the contralateral PRS, (e) Entering the contralateral Retro-rectus space, (f) Dissection of contralateral Retro-rectus space
Alternatively, a new access can be created in the contralateral retro-rectus space and crossover can be achieved under guidance.
We recommend crossover using the bottom-top technique, as the loose areolar tissue below the AL is easier to dissect.
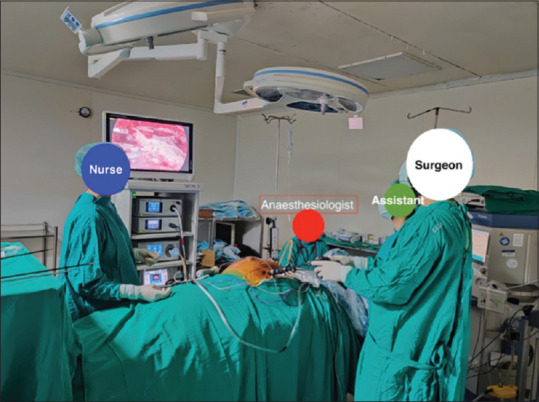
Dissection of plane and hernia sac
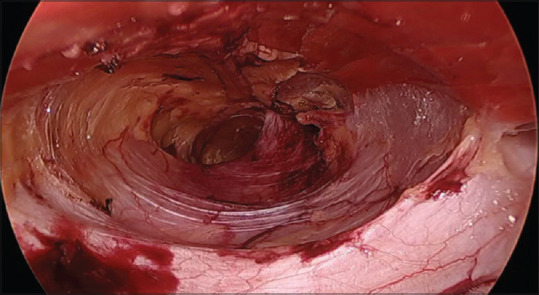
Once the right retro-rectus space is reached, the “lamppost sign”[11] guides the lateral limit of the dissection. Any dissection lateral to this can result in iatrogenic injury to the neurovascular bundles and LS. The dissection along the medial edges of both PRS eventually leads to the hernia defect. During this manoeuvre, an important sign is described as the “Volcano Sign,”[11] i.e., PRS of both sides along with falciform ligament and the LA above appear as an erupting volcano [Figure 7].
Figure 7.
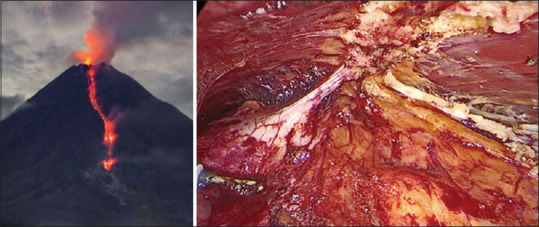
Volcano sign[11]
While tackling the hernia sac, care should be taken not to injure the bowel or other viscera. As the hernia is reduced completely, the peritoneal deficiency with the anterior abdominal defect becomes appreciable [Figure 8].
Figure 8.
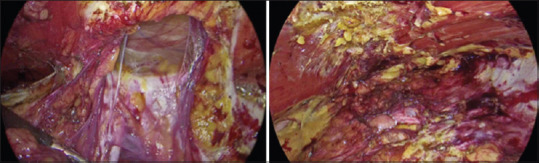
Anterior fascial defect and peritoneal defect
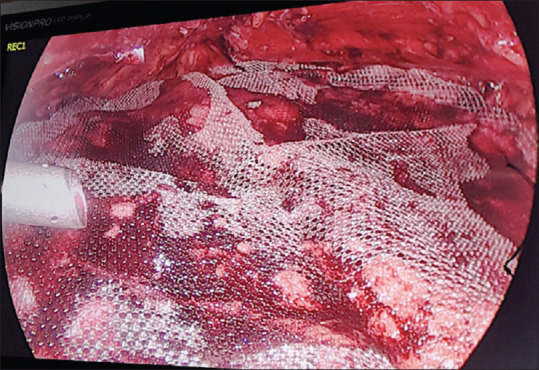
Peritoneal-posterior rectus sheath complex closure
We prefer closing posterior peritoneal layer before the anterior myo-fascial closure as it suggests an adequate tension-free repair without the need of a component separation. This peritoneal deficiency is closed primarily with a No. 1-0 monofilament absorbable barbed suture [Figure 9].
Figure 9.
Peritoneal defect closure
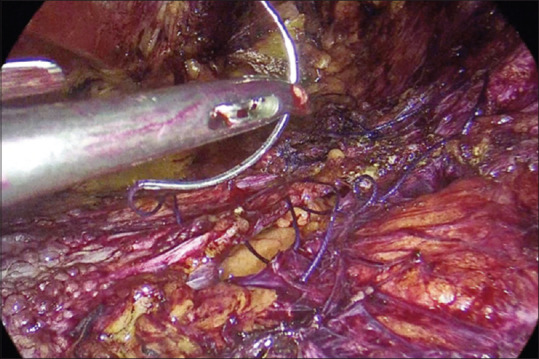
In cases of complex hernia, the size of the peritoneal defect can be measured to estimate the need of abdominal wall reconstruction (AWR). If the peritoneal-PRS layer closure is at the risk of being under tension, posterior component separation in the form of TAR can be done to accommodate for a tension-free repair. This manoeuvre also helps in the ease of the anterior defect closure. TAR was performed preferably using a hook unipolar device or harmonic scalpel [Figure 10].
Figure 10.
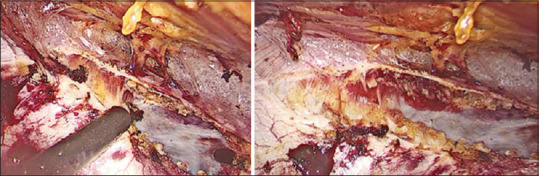
Transversus abdominis release
Anterior myo-fascial closure
Anterior myofascial closure can be done using a barbed 1-0 PDS or polypropylene suture to approximate the hernia defect. A divarication of recti (DR) should also be addressed at the same time [Figure 11].
Figure 11.
Anterior fascial closure with incorporation of pseudosac and plication of divarication of recti
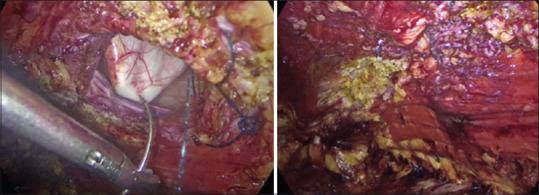
Mesh placement
Following this measurement for the size of mesh can be taken with the help of a Mersilk thread or a pliable ruler. Vertical and transverse distance can be measured and the mesh fashioned in a hexagonal shape to fit in the pre-peritoneal plane. We regularly use a lightweight macroporous polypropylene mesh, which provides adequate reinforcement along with ease of handling [Figure 12].
Figure 12.
Mesh placement - No fixation
Care is taken to ensure that the hernia defect is covered for at least 5 cm in all directions and all port sites are covered as well. Any type of fixation is unnecessary as the fundamentals of a Rives-Stoppa type repair allow for anatomical fixation of the mesh with the help of radially acting intra-abdominal forces. Subsequently, a negative suction drain is placed on the top of the mesh, which is kept in situ for 48–72 h to drain the seroma in the early post-operative period. The cavity can then be de-sufflated and insufflated to ensure correct positioning of the mesh. All ports are closed with nylon suture and an elastic adhesive dressing is placed over gauze compression and an abdominal binder is placed to support the repair.
RESULTS
The results are depicted in Table 1. The demographics of the study suggest that the mean age of patients presenting with a ventral hernia was 55.69 years (±7.90). The mean body mass index (BMI) for primary hernia was 26.53 (±3.46) and incisional hernia was 27.19 (±4.15), whereas the BMI was significantly higher in patients with recurrent hernia at 30.02 (±4.26) (F = 7.490) (P = 0.001).
Table 1.
Patient demographics and perioperative data
| Type | Incisional, n (%) | Primary, n (%) | Recurrent, n (%) | χ 2 | P | Total, n (%) |
|---|---|---|---|---|---|---|
| Gender | 73 (48.7) | 48 (32.0) | 29 (19.3) | 22.630 | 0.000 | 150 (100) |
| Female | 64 (87.7) | 24 (50) | 23 (79.3) | 111 (74) | ||
| Male | 9 (12.3) | 24 (50) | 6 (20.7) | 39 (26) | ||
| Age | 54.32±7.87 | 56.25±7.75 | 56.52±8.10 | 1.262 | 0.286 | |
| BMI (kg/m2) | 27.19±4.15 | 26.53±3.46 | 30.02±4.26 | 7.490 | 0.001 | |
| Defect width (cm) | 6.77±3.39 | 5.30±2.81 | 8.53±3.52 | 9.102 | 0.000 | |
| Defect area (cm2) | 20.96±13.97 | 15.09±11.57 | 26.94±14.28 | 7.369 | 0.001 | |
| LOS (days) | 4.36±2.19 | 3.75±1.62 | 5.21±2.51 | 4.376 | 0.014 | |
| ASA grade | ||||||
| 1 | 5 (6.8) | 2 (4.2) | 2 (6.9) | 9 (6) | ||
| 2 | 44 (60.3) | 27 (56.3) | 20 (69.0) | 91 (60.7) | ||
| 3 | 23 (31.5) | 19 (39.6) | 7 (24.1) | 49 (32.6) | ||
| 4 | 1 (1.4) | 0 | 0 | 1 (0.7) | ||
| Total | 73 (48.7) | 48 (32.0) | 29 (19.3) | 150 (100) | ||
| EHS classification | ||||||
| Midline, n=127; 84.7% | ||||||
| 1 | 2 (3.2) | 3 (6.8) | 0 | 5 (3.9) | ||
| 2 | 6 (9.6) | 15 (34.1) | 2 (9.5) | 23 (18.1) | ||
| 3 | 35 (56.5) | 21 (47.7) | 8 (38.1) | 64 (50.4) | ||
| 4 | 18 (29.1) | 5 (11.4) | 11 (52.4) | 34 (26.8) | ||
| 5 | 1 (1.6) | 0 | 0 | 1 (0.8) | ||
| Total | 62 (48.9) | 44 (34.6) | 21 (16.5) | 127 (100) | ||
| Lateral, n=23; 15.3% | ||||||
| 1 | 3 (27.2) | 0 | 3 (33.4) | 6 (26.1) | ||
| 2 | 2 (18.2) | 0 | 2 (22.2) | 4 (17.4) | ||
| 3 | 4 (36.4) | 3 (100.0) | 2 (22.2) | 9 (39.1) | ||
| 4 | 2 (18.2) | 0 | 2 (22.2) | 4 (17.4) | ||
| Total | 11 (47.8) | 3 (17.4) | 8 (34.8) | 23 (100) | ||
| Width | ||||||
| 1 | 15 (20.5) | 18 (37.5) | 1 (3.4) | 34 (22.7) | ||
| 2 | 44 (60.3) | 27 (56.3) | 16 (55.2) | 87 (58) | ||
| 3 | 14 (19.2) | 3 (6.3) | 12 (41.4) | 29 (19.3) | ||
| Total | 73 (48.7) | 48 (32.0) | 29 (19.3) | 150 (100) | ||
| Procedure | ||||||
| eTEP RS | 59 (80.8) | 45 (93.8) | 17 (58.6) | 121 (80.7) | ||
| eTEP TAR | 14 (19.2) | 3 (6.3) | 12 (41.4) | 29 (19.3) | ||
| Total | 73 (48.7) | 48 (32.0) | 29 (19.3) | 150 (100) | ||
| Operating time (min) | ||||||
| eTEP RS (n=121) | 124.33±23.68 | −18.499 | 0.000 | |||
| eTEP TAR (n=29) | 222.24±32.56 | |||||
BMI: Body mass index, LOS: Length of stay, ASA: American Society of Anaesthesiologists, EHS: European Hernia Society, eTEP: Enhanced-view totally extra-peritoneal, RS: Rives-Stoppa, TAR: Transversus abdominis release
For a detailed analysis, we divided the patients into three groups based on the type of hernia, namely incisional (I), primary (P) and recurrent (R). The majority of the patients with a ventral hernia were females (74%).
Out of total 150 cases, incisional hernia occurred in 73 cases (48.7%), primary hernia occurred in 48 cases (32%) and recurrent hernia in 29 cases (19.3%). Although the majority of incisional (87.7%) and recurrent (79.3%) ventral hernias occurred in female, the incidence of primary ventral hernia was equal at 24 cases in both genders.
According to ASA physical status grading, the majority of the patients were ASA Grade 2 (60.6%), followed by Grade 3 (32.6%) and Grade 1 (6%). One patient with obstructed primary umbilical hernia was classified as ASA Grade 4 due to a recent history of CAD-post-PTCA. The most common co-morbidity amongst the study group was hypertension (40.6%), followed closely by obesity (35.3%). Other significant co-morbidities amongst the group were DM-II (16.6%), COPD (9.3%) and CLD (2%). History of smoking was present in 16 cases (10.6%); all patients were motivated to cessation of the same for at least 4 weeks.
The hernias were further classified according to the EHS classification. The majority of the cases were midline (M) hernia (84.7%). We encountered 23 cases (15.3%) of lateral hernias in our study of 150 cases [Table 1].
The width of the hernia defect was significantly larger in recurrent hernia (8.53 cm ± 3.52) compared to primary (5.30 cm ± 2.81) and incisional hernias (6.77 cm ± 3.39) (F = 9.102) (P = 0.000). Similar results were seen in terms of hernia defect area as shown in the Table 1.
According to EHS classification, majority (58%) of hernias measured between 4-10 cm (W2). The majority of the cases (80.7%) underwent eTEP RS procedure, and the rest were W3 hernias, which were managed by including a component separation in the form of eTEP TAR. The operating time for eTEP TAR (222.24 min ± 32.56) compared to eTEP RS (124.33 ± 23.68) was significantly longer.
The mean length of stay (LOS) was significantly shorter for primary hernias (3.75 days ± 1.62) compared to recurrent (5.21 days ± 2.51) and incisional hernias (4.36 days ± 2.19) (F = 4.376) (P = 0.014).
We had one inadvertent enterotomy during an eTEP for a midline incisional hernia with a subacute intestinal obstruction involving ileum. As it was anticipated to be a difficult adhesiolysis endoscopically, an immediate laparotomy and repair of the enterotomy was done. We proceeded with an open RS for the same patient as the contamination was controlled. The patient as did well in the early post-operative period was discharged on day 5 in the healthy condition [Figure 13].
Figure 13.
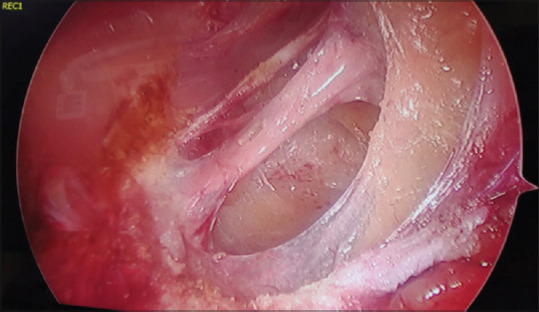
Inadvertent enterotomy in Ileum
The peri-operative period was uneventful in the rest of the cases. We experienced a seroma rate of 5.8% in our series. At the follow-up of 1 year, 3.3% of patients complained of discomfort/bulge in the upper abdomen. There were no other surgical site occurrences (SSO) in the form infection, PRS disruption and skin necrosis. We observed no recurrences till date with a minimum follow-up of 1 year.
DISCUSSION
In spite of developments of surgical specialities for each system, the art of hernia repair still remains in the domain of a general surgeon, majority of these being ventral hernia repairs (VHR). This might not be true in the near future with the advent of advanced endoscopic surgery and AWR techniques. This evolution in hernia surgery has led to produce an entity of ‘specialist’ hernia surgeon. A major factor for this endearing growth in the field has been the impact of hernia surgery specific organisations globally.
Ventral hernia repair is undoubtedly becoming the most exciting field of surgery with newer techniques being added to the arsenal of a hernia surgeon in recent times. Other than eTEP, techniques such as intra-peritoneal onlay (IPOM), endoscopic mini/less open sublay (EMILOS), subcutaneous onlay approach (SCOLA), laparoscopic TAPP, robotic TAPP and laparoscopic trans-abdominal retromuscular (TARM) have rendered the hernia surgeon spoilt for choice.[12] With these numerous approaches, the search for a one-fit-for-all standard technique is still afar as evidence is lacking. As all hernias are not the same in terms of patient and hernia characteristics, different scenarios mandate an approach, which is best suited for the said case. Another factor that has recently been debated is the ‘surgeon’ factor. Although this factor is hard to study and analyse, the level of training and expertise surely have a direct impact on the outcomes of the procedure.
Open approaches to ventral hernia are still gold standard for specific cases with loss of domain, poor skin condition, etc., but smaller hernias that are amenable to minimal access techniques should be approached in that fashion as there is evidence to suggest its superiority.[6] We believe that the inclination towards open techniques will remain unchanged in the mindset of the surgeon without adequate exposure and training in a high-volume minimal access centre.
The ideal plane of repair is still debated across the globe but there is strong evidence to suggest that sublay-retrorectus has better functional outcomes in the form of lower SSO, recurrence, chronic pain, avoiding complications of intra-peritoneal foreign body.[13,14]
A minimally invasive technique in the form of eTEP addresses this issue of the plane along with advantages of a large affordable mesh on a well vascularised flap with no fixation and an option to add a posterior component separation for large hernias seems to be a good option of majority of the cases.
Demographics of our study suggest that with a mean age of 55.69 years (±7.90), this technique is safe and feasible in elderly patients with minimal complications.
As suggested by ASMBS-AHS and IEHS guidelines, obesity is a risk factor for the development of primary as well as incisional hernia. It is also a risk factor for hernia recurrence and post-operative complications.[15,16] In our study, the mean BMI for primary hernia was 26.53 (±3.46) and incisional hernia was 27.19 (±4.15), whereas the BMI was significantly higher in patients with recurrent hernia at 30.02 (±4.26) (F = 7.490) (P = 0.001).
There is insufficient evidence to conclude the best management strategy for obese patients with abdominal wall hernia who are suitable candidates for bariatric surgery; the management maybe varied as per the scenario. However, laparoscopic repair is preferred over open repair in obese patients in terms of better efficacy, lesser complications and recurrence amongst control patients subjected to an open repair.[17-19]
Although ventral hernias occurred more commonly in females (74%), primary hernias were found in equal numbers with regard to gender. In our study, only 32% of cases out of 150 cases were primary hernias, majority of the cases being either incisional or recurrent hernias. In our practice, we have been managing smaller primary hernia without DR either by IPOM. Recent developments of techniques such as TARM by Masurkar[20] seem to be a promising alternative, but comparative evidence in the literature is limited to recommend it over eTEP or IPOM.
eTEP has been our preferred approach for all ventral hernias with DR. As described by Belyansky et al., concomitant plication of recti and hernia repair via an extra-peritoneal approach gives a more robust abdominal wall.[21] SCOLA described by Claus C et al. is another promising approach to small umbilical hernias with DR. It carries with it a higher seroma rate as compared to other techniques.[22] Our experience with the technique is limited, as we prefer to place the mesh in retromuscular plane. MILOS/eMILOS approach described by Schwarz et al. provides a sublay repair with good results. The technique is limited in the application to only primary umbilical and epigastric hernia.[23,24]
In our study, incisional and recurrent hernias were seen more commonly in females. These hernias can be challenging to manage with minimal access approach and were traditionally considered to be open cases only. Our experience in the study suggests that with 60% out 150 cases being incisional or recurrent, eTEP approach can be considered for these difficult hernias with good outcomes. A hybrid approach[25] can also be used in the setting where scar revision is required as it may decrease the operative time. In hybrid setting, the retro-muscular dissection is done endoscopically followed by mesh placement and anterior fascial closure by an open method.
In our experience, the most crucial application of eTEP is in the management of unusual hernias such as subcostal, iliac and lumbar hernias. We suggest that the EHS classification[26] should be used to classify ventral hernias as it standardises the nomenclature and can be used as an important parameter in research for ideal approach in various scenarios. Lateral (L) hernias can be difficult to manage, especially subcostal (L1) and Iliac (L3) as these are close to fixed bony structures and an adequate overlap of the mesh might be difficult to achieve. We encountered 23 out of 150 cases (15.3%) as lateral hernias. These were managed with ease using the eTEP approach. Most of these cases require a component separation in the form of TAR, which may be unilateral or bilateral. The extra-peritoneal space in the subcostal region can be utilised to reach the subdiaphragmatic space if required. The iliac and lumbar region can be approached similarly. This allows for adequate mesh coverage of these eccentrically placed hernias without the need of fixation which can be beneficial in terms of chronic pain post-operatively.
According to the width of the defect, most of the hernias in our study were W2 (58%) followed by W1 (22.7%). These were managed with eTEP RS. The remaining W3 hernias (19.3%) were managed with eTEP TAR. This indicates that even large hernias can be managed with minimal access approach in expert hands.
The operative time in our study was about 2 h for eTEP RS and 3 ½ h for eTEP TAR. A preliminary study by Penchev et al. suggests shorter operative time with IPOM.[12] The data in our study are inclusive of our learning curve period, subsequently with standardisation of steps and experience; our operative time has improved significantly.
Along with the benefits of avoiding an intra-peritoneal foreign body with fixation and its dreaded complications, it also incurs reduced cost to the patient in comparison to IPOM. Quantification of the same was not done in this study, but the average cost of the eTEP approach is significantly lower as the dual barrier mesh and tacking device used in IPOM are expensive.
In a recently published study on this approach by Khetan et al.,[27] rate of seroma and paralytic ileus was 20.7%. Our study showed a lower rate, likely due to the longer duration of post-operative drainage of the eTEP space.
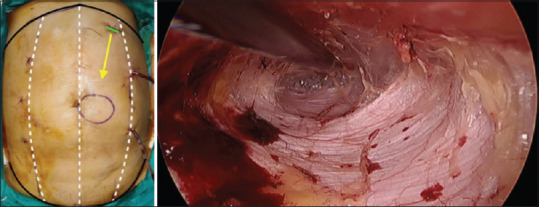
A significant post-operative issue that we noticed was an upper abdominal bulge/discomfort (3.3%). We understand that it is probably due to the upper crossover technique, leading to more than acceptable diastasis. Hence, we have modified our technique to do an infra- AL crossover for M3-5, so that upper abdominal area remains virgin. For M1-2, we still prefer the upper abdomen crossover [Figure 14]. In addition, a limited upper B/L TAR needs to be done for M1 subcostal to give a good subxiphoid space for mesh placement between the fibres of diaphragm and peritoneum. Similarly, M5 hernias may require a limited lower B/L TAR for adequate mesh coverage.
Figure 14.
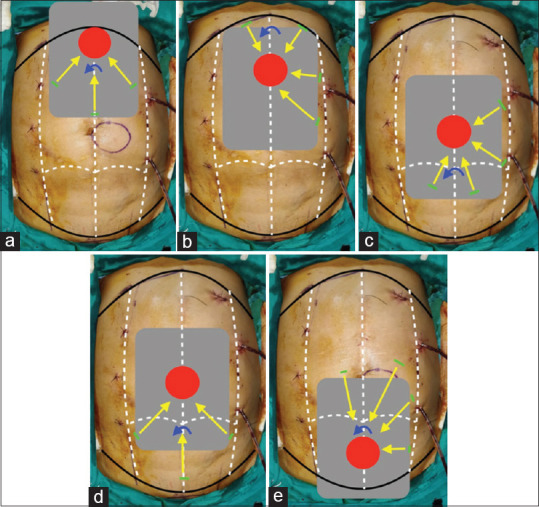
Port placement; top crossover (a) M1, (b) M2; bottom crossover (c) M3, (d) M3, (e) M4-5
The LOS in our study was between 3 and 5 days for all procedures. As most of our patients come from rural areas without adequate nursing care, we tend to keep the patient under observation longer in the post-operative period.
Although our early experience is favourable, more research is required to establish the benefits of eTEP in ventral hernia.
This approach is also amenable to be performed robotically as suggested by Liu,[28] Morrel et al.[29] and Bindal et al.[30] The robotic platform seems to be helpful in suturing of the layers and performing a TAR with ease. It is definitely a boon for the surgeon, but the cost of the robotic procedure for the patient seems to be unjustified at present. With more platforms coming into the practice, the future of robotics seems promising.
For a surgeon venturing into a new evolving domain like eTEP, we insist on training in a high volume centre, as the learning curve of a new technique can be decreased under supervision.
CONCLUSION
We believe that the ideal approach for ventral hernias cannot be pinpointed to one procedure. The approach should be idealised according to the setting, to include patient, hernia and surgeon characteristics into the picture. With the introduction of various minimal access techniques, the future of open repair for ventral hernias seems to be uncertain. The training for the same should be sought after before venturing into the field.
eTEP repair is a reproducible and safe technique for tackling various types of ventral hernia. Other than primary midline hernias, it is specifically useful in unusual lateral hernias. It is also useful in managing incisional and recurrent hernias with ease.
Despite the lack of evidence, this study adds to the growing body of knowledge in the field of innovative minimally invasive procedures for ventral hernia repair.
Informed patient consent
Taken.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rives J, Stoppa R, Fortesa L, Nicaise H. Dacron patches and their place in surgery of groin hernia. 65 cases collected from a complete series of 274 hernia operations. Ann Chir. 1968;22:159–71. [PubMed] [Google Scholar]
- 2.Stoppa RE. The treatment of complicated groin and incisional hernias. World J Surg. 1989;13:545–54. doi: 10.1007/BF01658869. [DOI] [PubMed] [Google Scholar]
- 3.Rives J, Pire JC, Flament JB, Palot JP, Body C. Treatment of large eventrations. New therapeutic indications apropos of 322 cases. Chirurgie. 1985;111:215–25. [PubMed] [Google Scholar]
- 4.LeBlanc KA, Booth WV. Laparoscopic repair of incisional abdominal hernias using expanded polytetrafluoroethylene: Preliminary findings. Surg Laparosc Endosc. 1993;3:39–41. [PubMed] [Google Scholar]
- 5.Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: Nine years'experience with 850 consecutive hernias. Ann Surg. 2003;238:391–9. doi: 10.1097/01.sla.0000086662.49499.ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prasad P, Tantia O, Patle NM, Khanna S, Sen B. Laparoscopic ventral hernia repair: A comparative study of transabdominal preperitoneal versus intraperitoneal onlay mesh repair. J Laparoendosc Adv Surg Tech A. 2011;21:477–83. doi: 10.1089/lap.2010.0572. [DOI] [PubMed] [Google Scholar]
- 7.Daes J. The enhanced view-totally extraperitoneal technique for repair of inguinal hernia. Surg Endosc. 2012;26:1187–9. doi: 10.1007/s00464-011-1993-6. [DOI] [PubMed] [Google Scholar]
- 8.Daes J. The extended-view totally extraperitoneal e-TEP technique for inguinal hernia repair. In: Novitsky YW, editor. Hernia Surgery, Current Principles. New York: Springer; 2016. pp. 467–72. [Google Scholar]
- 9.Belyansky I, Daes J, Radu VG, Balasubramanian R, Reza Zahiri H, Weltz AS, et al. A novel approach using the enhanced-view totally extraperitoneal (eTEP) technique for laparoscopic retromuscular hernia repair. Surg Endosc. 2018;32:1525–32. doi: 10.1007/s00464-017-5840-2. [DOI] [PubMed] [Google Scholar]
- 10.Novitsky YW, Elliott HL, Orenstein SB, Rosen MJ. Transversus abdominis muscle release: A novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg. 2012;204:709–16. doi: 10.1016/j.amjsurg.2012.02.008. [DOI] [PubMed] [Google Scholar]
- 11.Ramana B, Arora E, Belyansky I. Signs and landmarks in eTEP rives-stoppa repair of ventral hernias. Hernia. 2021;25:545–50. doi: 10.1007/s10029-020-02216-4. [DOI] [PubMed] [Google Scholar]
- 12.Penchev D, Kotashev G, Mutafchiyski V. Endoscopic enhanced-view totally extraperitoneal retromuscular approach for ventral hernia repair. Surg Endosc. 2019;33:3749–56. doi: 10.1007/s00464-019-06669-2. [DOI] [PubMed] [Google Scholar]
- 13.Vorst AL, Kaoutzanis C, Carbonell AM, Franz MG. Evolution and advances in laparoscopic ventral and incisional hernia repair. World J Gastrointest Surg. 2015;7:293–305. doi: 10.4240/wjgs.v7.i11.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alimi Y, Merle C, Sosin M, Mahan M, Bhanot P. Mesh and plane selection: A summary of options and outcomes. Plast Aesthet Res. 2020;7:5. [Google Scholar]
- 15.Menzo EL, Hinojosa M, Carbonell A, Krpata D, Carter J, Rogers AM. American society for metabolic and bariatric surgery and American Hernia Society consensus guideline on bariatric surgery and hernia surgery. Surg Obes Relat Dis. 2018;14:1221–32. doi: 10.1016/j.soard.2018.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Bittner R, Bingener-Casey J, Dietz U, Fabian M, Ferzli GS, Fortelny RH, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall Hernias International Endohernia Society (IEHS)-part 1. Surg Endosc. 2014;28:2–29. doi: 10.1007/s00464-013-3170-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sajid MS, Bokhari SA, Mallick AS, Cheek E, Baig MK. Laparoscopic versus open repair of incisional/ventral hernia: A meta-analysis. Am J Surg. 2009;197:64–72. doi: 10.1016/j.amjsurg.2007.12.051. [DOI] [PubMed] [Google Scholar]
- 18.Novitsky YW, Cobb WS, Kercher KW, Matthews BD, Sing RF, Heniford BT. Laparoscopic ventral hernia repair in obese patients: A new standard of care. Arch Surg. 2006;141:57–61. doi: 10.1001/archsurg.141.1.57. [DOI] [PubMed] [Google Scholar]
- 19.Maia R, Salgaonkar H, Lomanto D, Shabbir A. Ventral hernia and obesity: Is there a consensus? Ann Laparosc Endosc Surg. 2019;4:17. [Google Scholar]
- 20.Masurkar AA. Laparoscopic trans-abdominal retromuscular (TARM) repair for ventral hernia: A novel, low-cost technique for sublay and posterior component separation. World J Surg. 2020;44:1081–5. doi: 10.1007/s00268-019-05298-z. [DOI] [PubMed] [Google Scholar]
- 21.Belyansky I, Lu R, Addo A. Diastasis recti: Robotic extended-view totally extraperitoneal (eTEP) access hernia repair technique. In: LeBlanc K, editor. Robotic Assisted Hernia Repair. Cham: Springer; 2019. [Google Scholar]
- 22.Claus C, Cavazzola L, Malcher F. Subcutaneous onlay endoscopic approach (SCOLA) for midline ventral hernias associated with diastasis recti. Hernia. 2021;25:957–62. doi: 10.1007/s10029-021-02465-x. [DOI] [PubMed] [Google Scholar]
- 23.Schwarz J, Reinpold W, Bittner R. Endoscopic mini/less open sublay technique (EMILOS)-a new technique for ventral hernia repair. Langenbecks Arch Surg. 2017;402:173–80. doi: 10.1007/s00423-016-1522-0. [DOI] [PubMed] [Google Scholar]
- 24.Reinpold W, Schröder M, Berger C, Stoltenberg W, Köckerling F. MILOS and EMILOS repair of primary umbilical and epigastric hernias. Hernia. 2019;23:935–44. doi: 10.1007/s10029-019-02056-x. [DOI] [PubMed] [Google Scholar]
- 25.Addo A, Lu R, Broda A, George P, Zahiri HR, Belyansky I. Hybrid versus open retromuscular abdominal wall repair: Early outcomes. Surg Endosc. 2021;35:5593–8. doi: 10.1007/s00464-020-08060-y. [DOI] [PubMed] [Google Scholar]
- 26.Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, et al. Classification of primary and incisional abdominal wall hernias. Hernia. 2009;13:407–14. doi: 10.1007/s10029-009-0518-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Khetan M, Dey A, Bindal V, Suviraj J, Mittal T, Kalhan S, et al. e-TEP repair for midline primary and incisional hernia: Technical considerations and initial experience. Hernia. 2021;25:1635–46. doi: 10.1007/s10029-021-02397-6. [DOI] [PubMed] [Google Scholar]
- 28.Liu RC. Robotic etep retrorectus rives-stoppa repair for ventral hernia. J Med Insight 2021. 2021 doi.org/10.24296/jomi/315. [Google Scholar]
- 29.Morrell AL, Morrell AC, Cavazzola LT, Pereira GS, Mendes JM, Abdalla RZ, et al. Robotic assisted eTEP ventral hernia repair: Brazilian early experience. Hernia. 2021;25:765–74. doi: 10.1007/s10029-020-02233-3. [DOI] [PubMed] [Google Scholar]
- 30.Bindal V, Sethi D, Khetan M, Kalhan S, John S, Dadhich R, Ramana B. Robotic extended-view totally extraperitoneal transversus abdominis release (eTEP/TAR) without crossover for a large right boundary incisional hernia. CRSLS. :e2020.00025. doi: 10.4293/CRSLS.2020.00025. [Google Scholar]