Abstract
Rationale
It is not certain the extent to which childhood smoking adds chronic obstructive pulmonary disease (COPD) risk independent of lifetime cigarette exposure.
Objectives
We examined the association between age started smoking cigarettes regularly, current smoking status, smoking history, and risk of COPD.
Methods
Cross-sectional survey of U.S. adults ⩾40 years old in the 2020 National Health Interview Survey. Respondents who were ever cigarette smokers were asked when they began smoking regularly. Multivariable analysis assessed self-report of COPD diagnosis as a function of age started smoking (<15 yr vs. ⩾15 yr) adjusting for current smoking, cigarette pack-years, and covariates.
Measurements and Main Results
Overall, 7.1% reported that they had COPD, 2.6% for never-smokers compared with 23.1% and 11.6% for smoking onset <15 and ⩾15 years, respectively. Persons who began smoking regularly at <15 years of age had higher pack-years of smoking (median, 29 vs. 15, respectively), and higher smoking intensity (median, 20 cigarettes/d for <15 yr vs. 10 cigarettes/d for ⩾15 yr for current smokers). In the multivariable analysis, the relative risk for COPD among childhood smokers was 1.41 (95% confidence interval, 1.22–1.63) compared with later-onset smokers. Substituting smoking duration for pack-years confounded the association between current smoking and COPD but did not change the childhood smoking estimate. In a stratified analysis, higher risk for childhood smoking was found at all current smoking intensity levels.
Conclusions
Among adults aged ⩾40 years, one-fifth of childhood smokers have COPD. Lifetime cigarette smoking explained some but not all of the higher risk. If replicated, this suggests a lung development window of enhanced vulnerability to cigarette smoking.
Keywords: COPD, cigarette, smoking, adolescence, lung development
At a Glance Commentary
Scientific Knowledge on the Subject
Lifetime cigarette smoking explains the majority of chronic obstructive pulmonary disease (COPD) prevalence in the United States. Early age of cigarette smoking is associated with higher smoking intensity and difficulty in quitting, but it is not certain whether it adds COPD risk independent of its relation to lifetime cigarette smoking.
What This Study Adds to the Field
In adults >40 years old, those with smoking onset at <15 years of age were less likely to be former smokers and had higher smoking intensity, higher mean pack-years, and higher risk of COPD independent of lifetime smoking. Results support a lung development window of enhanced vulnerability to cigarette smoking.
In most developed countries, the contribution of cigarette smoking in causing chronic obstructive pulmonary disease (COPD) far outweighs all other risk factors (1). Moreover, cigarette smoking interacts with other early childhood events, like acute respiratory illness, to further accentuate risk (2). Thus, although COPD is not a pediatric disease, its origins begin in childhood with the onset of cigarette smoking. Today, most smokers in the United States begin using cigarettes regularly during young adulthood. For example, in 2022, only 1% of middle school students (ages 10–14 yr) and 2% of high school students (ages 15–18 yr) reported smoking in the past 30 days (3). However, in 1974, when adults currently in their 50 s attended middle school, almost 25% of their peers smoked cigarettes (4).
Adolescence is a time of rapid lung growth, with most of peak predicted lung function developing between the ages of 10 and 20 years (1). Moreover, some 4–12% of adolescent smokers never reach their expected FEV1 for age and sex, which adds to their risk of COPD. Although it is known that prenatal exposure to cigarette smoke affects lung function in genetically susceptible children (5), and postnatal exposure to secondhand smoke is an established risk factor for childhood asthma (6), less is known about how early childhood smoking might independently affect risk for COPD. Recently, an analysis from a Swedish birth cohort revealed that both maternal smoking during pregnancy and adolescent smoking were associated with reduced FEV1/FVC ratios and increased peripheral airway resistance at age 16 years (7).
If early childhood smoking were shown to be a risk factor for COPD—above and beyond established smoking risk factors like duration of smoking, pack-years of smoking, and current smoking intensity—this could be taken as evidence of an adverse impact on lung development. In this study, we aimed to determine whether childhood-onset cigarette smoking is associated with prevalent self-reported COPD, independent of current smoking status, smoking intensity, cigarette pack-years, and sociodemographics in a nationally representative sample of U.S. adults aged ⩾40 years. Some of the results of these studies have been previously reported in the form of an abstract (8).
Methods
Study Participants
We analyzed data for 22,374 adults aged ⩾40 years from the 2020 National Health Interview Survey (NHIS). The presence of COPD was assessed through the question, “Have you ever been told by a doctor or other health professional that you had chronic obstructive pulmonary disease, COPD, emphysema, or chronic bronchitis?” The study qualified as exempt by guidelines of the Dartmouth Health Human Research Protection Program and the Westat Institutional Review Board.
Main Exposure Variable
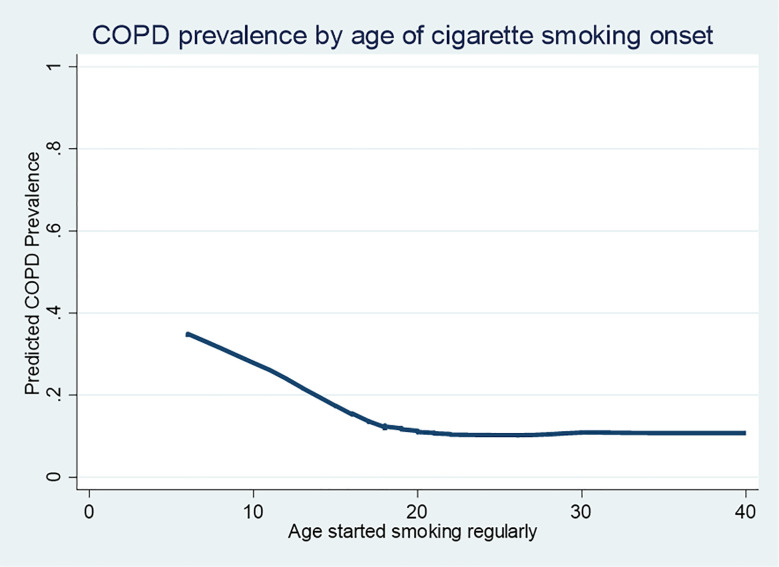
Lifetime smokers (of at least 100 cigarettes in their entire life) were asked, “How old were you when you FIRST started smoking regularly?” Among lifetime smokers in this sample, there was little evidence of a COPD association beyond smoking onset age 18 years (where COPD prevalence was about 12%); however, COPD prevalence increased linearly below this age and approached 30% at an age of onset of 10 years (Figure 1). Based on these data, we determined a cutoff of 15 years for defining childhood smoking (age of onset <15 or ⩾15 years).
Figure 1.
Lowess smoothed plot showing the relation between age started smoking regularly and COPD prevalence. COPD = chronic obstructive pulmonary disease.
Cigarette Smoking Covariates
Among lifetime smokers, current smoking was assessed by asking, “Do you NOW smoke cigarettes every day, some days, or not at all?”, recoded to never-smoker (<100 cigarettes lifetime), former smoker (>100 lifetime, not at all now), and current smoker (>100 lifetime, every day or some days). Former smokers were asked how many years since they quit smoking cigarettes and the usual amount smoked, which were used to determine their duration and pack-years of smoking. Smoking intensity (“On average how many cigarettes do you NOW smoke per day?”) was used to calculate pack-years before being coded into three categories: fewer than 10 (light), 11–19 (medium), and 20 or more (heavy) cigarettes per day.
For the primary analysis, age started smoking regularly was entered as a categorical variable, with ⩾15 as the reference category. A secondary analysis was conducted with a nine-category variable that stratified age started smoking regularly by cigarette smoking status (never, former, current) and smoking intensity for current smokers (light, medium, heavy).
Statistical Analysis
We examined the bivariable relation between childhood smoking and COPD as well as the covariates using weighted comparisons of means or proportions, as appropriate. We estimated the relative risk ratios (RRs) and 95% confidence intervals (CIs) for the association between childhood smoking and COPD, while adjusting for covariates (age, gender [male, female], race and ethnicity [non-Hispanic White, non-Hispanic Black, other], poverty [using the ratio of family income to the poverty threshold (0–1.99, 2–3.49, 3.5–4.99, and ⩾5); in 2020, a family of four with an income at the poverty line ($26,200) would have a poverty threshold score of 1.0], and geographic location/rurality) using multivariable weighted Poisson regression. We conducted two multivariable analyses: a primary one that entered current smoking status separately from childhood smoking and a secondary one that used the nine-category composite measure of smoking described previously.
Sensitivity Analyses
In a sensitivity analysis, we substituted smoking duration for cigarette pack-years. To explore the possibility that childhood smokers might systematically underreport cigarette pack-years compared with later-onset smokers, we examined how large that potential recall bias must be to nullify the age-of-onset finding, by rerunning the analysis while sequentially increasing cigarette pack-years by 5% increments for childhood smokers. Finally, we reran the primary analysis with a modified childhood smoking variable that tested whether individuals who began regular smoking in the 15- to 19-year-old range were also at higher risk for COPD than those who began at ⩾20 years. See the online supplement for additional methodological details.
Results
Sample Description
After applying weights, the 22,374 study participants (Table 1) were similar to the U.S. population, with women being slightly overrepresented, Black non-Hispanic individuals comprising 11% and White individuals 75%, and 25.9% having a family income below two times the poverty threshold. Never-smokers comprised 60% of the sample, former smokers 28%, and current smokers 13%. Mean pack-years was 8.7 for lifetime smokers, among whom 1,490 (16%) started smoking regularly before age 15 years. Mean pack-years was 12.4 for current smokers, among whom 79% smoked every day.
Table 1.
Description of the Sample, Overall and Childhood Smoking
| Variable | Overall (N = 22,374) | Cigarette Smoking Status |
||
|---|---|---|---|---|
| Never-Smokers (n = 13,024) | Age Started Smoking Regularly (yr) |
|||
| <15 (n = 1,490) | ⩾15 (n = 7,860) | |||
| Geographic location | ||||
| Large central metro | 28.9 | 31.8 | 20.6 | 25.5 |
| Large fringe metro | 24.9 | 25.5 | 24.2 | 24.1 |
| Medium and small metro | 30.4 | 29.1 | 33.5 | 31.9 |
| Nonmetropolitan | 15.8 | 13.6 | 21.8 | 18.6 |
| Region | ||||
| Northeast | 18.5 | 18.6 | 17.7 | 18.4 |
| Midwest | 20.8 | 19.2 | 22.1 | 23.3 |
| South | 37.8 | 37.1 | 39.0 | 38.9 |
| West | 22.9 | 25.1 | 21.1 | 19.5 |
| Age, yr | ||||
| 40–49 | 25.6 | 27.8 | 21.5 | 22.7 |
| 50–59 | 26.3 | 28.0 | 27.7 | 23.1 |
| 60–69 | 24.5 | 22.7 | 27.4 | 27.1 |
| 70–79 | 15.7 | 13.8 | 16.6 | 18.8 |
| ⩾80 | 7.9 | 7.8 | 6.9 | 8.3 |
| Gender | ||||
| Male | 47.2 | 42.7 | 59.5 | 52.6 |
| Female | 52.8 | 57.3 | 40.5 | 47.4 |
| Race | ||||
| White | 75.0 | 70.8 | 83.9 | 80.3 |
| Black | 11.0 | 12.5 | 5.1 | 9.7 |
| Other race and multiple | 14.0 | 16.7 | 11.0 | 10.0 |
| Family poverty ratio* | ||||
| 0.00–1.99 | 25.9 | 23.5 | 38.2 | 27.7 |
| 2.00–3.49 | 23.0 | 21.9 | 25.9 | 24.3 |
| 3.50–4.99 | 18.5 | 18.1 | 16.6 | 19.6 |
| ⩾5.00 | 32.5 | 36.4 | 19.3 | 28.4 |
Data are presented as weighted percentages.
Categorizes families with respect to household income and the U.S. poverty line, which was $26,200 in 2020. For example, a family of four with an income of $32,000 would be in the lowest category, which includes household incomes up to $42,399 for a family of four.
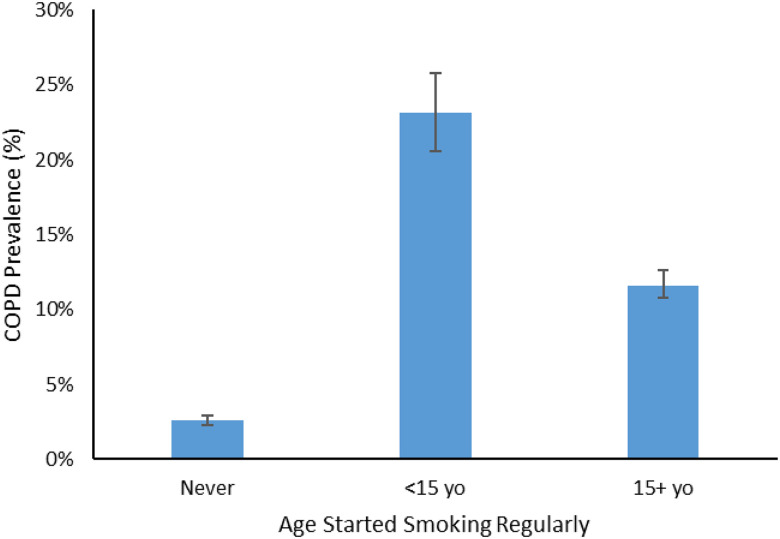
Bivariable Associations
A COPD diagnosis was reported by 7.1% overall and varied markedly by childhood smoking status, being 2.6% for never-smokers, 23.1% for childhood smokers, and 11.6% for those who started smoking regularly at ⩾15 years of age (Figure 2).
Figure 2.
Prevalence of COPD by childhood smoking. COPD = chronic obstructive pulmonary disease.
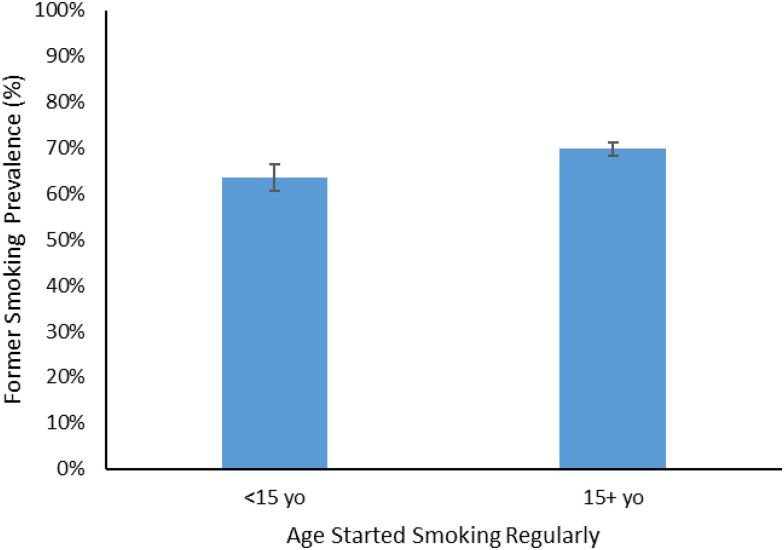
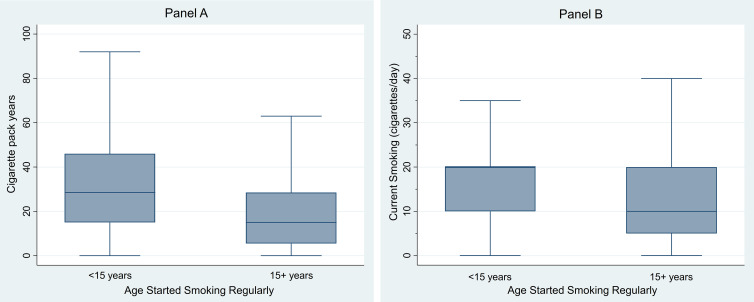
Childhood smoking was strongly associated with poverty (Table 1), with 38% of childhood smokers being in the poorest poverty category (0–1.99) compared with 28% for later-onset smokers. It was also associated with lower success at quitting smoking, with former smokers comprising 63.5% (95% CI, 60.5–66.5%) of childhood smokers and 69.8% (68.4–71.2%) for those who started smoking later (Figure 3; P < 0.001). As illustrated in Figure 4A, childhood smokers had much higher pack-years of smoking (mean, 34 [SD, 26] vs. 20 [19]); median pack-years for childhood smokers (28.5) was identical to the 75th percentile for those who initiated smoking later. Among current smokers, smoking intensity was much higher among childhood smokers (mean, 19 [SD, 14] vs. 14 [11]; Figure 4B), among whom 50% smoked 20 or more cigarettes per day compared with only 25% for those who initiated smoking later.
Figure 3.
Percentage of former smokers by childhood smoking. Percentages significantly different at P < 0.001.
Figure 4.
Box plots describing (A) cigarette smoking history and (B) current smoking by childhood smoking. Upper and lower bounds of the box are the interquartile range, and the line in the middle is the median. There is no median line in B for age started smoking <15 years, because the median = 75th percentile.
Multivariable Analyses
In the analysis that considered childhood smoking separately from other smoking variables (Tables 2 and 3), and compared with later-onset smokers, the adjusted RR for COPD in childhood smokers was 1.41 (95% CI, 1.22–1.63). Current smokers were also at higher risk than former + never-smokers, and the RR was 1.18 for each 10 additional pack-years (see Table E1 in the online supplement for the distribution for pack-years in this sample and Tables E2 and E3 for model output).
Table 2.
Multivariable Association between Chronic Obstructive Pulmonary Disease and Childhood Smoking by Current Smoking Status, Entering Age Started Smoking Regularly Separately from Smoking Status
| % with COPD | Relative Risk |
95% CI for Adjusted | P Value for Adjusted | ||
|---|---|---|---|---|---|
| Unadjusted | Adjusted* | ||||
| Age started smoking regularly, yr | |||||
| ⩾15 | 11.6 | Ref | Ref | Ref | Ref |
| <15 | 23.1 | 1.99 | 1.41 | 1.22–1.63 | <0.001 |
| Smoking status | |||||
| Never-smoker | 2.6 | 0.22 | 0.44 | 0.37–0.51 | <0.001 |
| Never + former smoker | 5.5 | Ref | Ref | Ref | Ref |
| Current smoker | 18.0 | 3.28 | 1.51 | 1.32–1.74 | <0.001 |
| Cigarette pack-years† | 1.37 | 1.18 | 1.16–1.21 | <0.001 | |
Definition of abbreviations: CI = confidence interval; COPD = chronic obstructive pulmonary disease; Ref = reference; RR = relative risk.
Adjusted also for age, gender, race, poverty, and urbanicity.
Represents the increased risk associated with each additional 10 pack-years.
Table 3.
Multivariable Association between Chronic Obstructive Pulmonary Disease and Childhood Smoking by Current Smoking Status, Combining Age Started Smoking Regularly with Smoking Status and Smoking Intensity
| Smoking Status/Intensity | Age Started Smoking Regularly (yr) | % with COPD | RR |
95% CI for Adjusted | P Value† | |
|---|---|---|---|---|---|---|
| Unadjusted | Adjusted* | |||||
| Never-smoker | — | 2.6 | Ref | Ref | Ref | Ref |
| Former smoker | <15 | 19.5 | 7.55 | 2.83 | 2.24–3.57 | 0.010 |
| ⩾15 | 10.0 | 3.88 | 2.22 | 1.90–2.60 | ||
| Current light smoker | <15 | 20.3 | 7.87 | 5.53 | 3.38–9.05 | 0.070 |
| ⩾15 | 9.7 | 3.75 | 2.83 | 1.64–4.88 | ||
| Current medium smoker | <15 | 30.6 | 11.86 | 6.00 | 4.40–8.17 | 0.030 |
| ⩾15 | 19.0 | 7.35 | 4.09 | 3.18–5.26 | ||
| Current heavy smoker | <15 | 35.1 | 13.61 | 4.03 | 2.95–5.50 | 0.004 |
| ⩾15 | 18.7 | 7.24 | 2.59 | 2.00–3.36 | ||
| Cigarette pack-years‡ | — | — | 1.37 | 1.20 | 1.18–1.23 | <0.001 |
Definition of abbreviations: CI = confidence interval; COPD = chronic obstructive pulmonary disease; Ref = reference; RR = relative risk.
Adjusted also for age, gender, race, poverty, and urbanicity.
P value compares the RR for COPD by age started smoking regularly within each smoking status/intensity category.
Represents the increased risk associated with each additional 10 pack-years.
When childhood smoking was considered in conjunction with current smoking status (Table 3), the RR for childhood smokers was higher within each stratum of current smoking, and these differences reached statistical significance, with one exception (see Table E3 for model output). For example, among those smoking 10–19 cigarettes per day, the RR of COPD for childhood smoking was 6.00, compared with 4.09 for those who began regularly smoking later (P = 0.03 for the difference between estimates).
Sensitivity Analyses
Substituting smoking duration for cigarette pack-years confounded the association with COPD for current smoking, which was no longer associated with COPD (RR, 0.92 [95% CI, 0.78–1.07]) but had little impact on the association for childhood smoking (RR, 1.41 [95% CI, 1.24–1.60]); smoking duration was also associated with COPD, with an RR of 1.39 (95% CI, 1.32–1.46) for each additional 10 years of smoking duration (see Table E1 for the distribution for smoking duration in this sample).
Adding to pack-years to simulate potential recall bias for childhood smokers’ recollection of their smoking history incrementally reduced the RR associated with childhood smoking. However, we had to add 35% to their pack-year total to nullify the statistical significance of the results reported in Table 2. We reran the primary analysis to explore if the window for increased risk extended beyond 15 years and to explore the dose–response relationship. We compared risk for those who started smoking regularly at ⩾20 years (reference) with those who began at 15–19 years (RR, 1.27 [95% CI, 1.05–1.53]) and <15 years (RR, 1.70 [95% CI, 1.37–2.11]), extending the range of the childhood smoking association with COPD to age 20 years. In addition, the RR for the 15- to 19-year group was significantly different from the <15-year group, suggesting a diminution in risk for those who began cigarette smoking during late adolescence.
Discussion
In this sample of older U.S. adults, one-fifth of childhood cigarette smokers reported COPD. As a risk factor for COPD, childhood smoking was independent of current smoking status and two measures of smoking history—pack-years and smoking duration. Compared with the strength of other smoking risk factors, the RR magnitude for childhood smoking was similar to current smoking (vs. former + never-smoking) and roughly equivalent to each additional 20 pack-years of cigarette smoking. Although those who began smoking before 15 years of age were at the greatest risk, those who began in the 15- to 19-year range were also at increased risk, although significantly lower than for the younger group. Thus, in this sample, the developmental window for increased risk due to childhood smoking ended at about age 20 years, which coincides with the time forced expiratory volume in 1 second (FEV1) reaches its peak during adolescence (1).
Age started smoking regularly was captured in some of the earliest studies of smoking and disease. However, most studies showing an association between childhood smoking and COPD prevalence or mortality did not adjust for other measures of lifetime smoking and current smoking (9–11), making it unclear whether the association is simply a proxy for smoking duration or pack-year exposure. In 2004, Patel and colleagues (12) reported a cross-sectional association between childhood smoking (onset <16 yr) and lifetime COPD that adjusted for cigarette pack-years, but the finding was only for women and did not adjust for current smoking status. In 2006, Geijer and colleagues (13) reported an association between childhood smoking (onset <15 yr) and COPD incidence independent of cigarette pack-years in a sample of adult cigarette smokers aged ⩾40 years but did not adjust for current smoking intensity. Ours is the first that we know of to adjust for both lifetime smoking risk factors.
The findings suggest chronic disease implications of the effects of active cigarette smoking on lung development during childhood. Cohort studies have examined lung function development in children in the 1980 s and 1990 s and its relation to cigarette smoking (14). Results were mixed about the effects of passive smoking. For example, the Tucson longitudinal study found no association between secondhand smoke exposure and lung function in children (15). However, active smoking had strong associations with lung function as assessed by spirometry (14), both in cross-sectional and longitudinal studies, showing reduced lung growth and a lower degree of maximally obtained FEV1 for active smokers. Although studies have demonstrated a dose–response relationship between active smoking and decreased lung function growth (16), less is known about how earlier-onset smoking affects lung development.
Childhood smoking was strongly associated with both the intensity of current smoking and pack-years of smoking. Longitudinal studies of smoking in children have found early-onset smoking associated with regular adult smoking (17). Previous studies of early-onset smoking in adults have found higher smoking intensity (18), higher levels of nicotine dependence (19, 20), and a higher risk of continued smoking (21, 22), together with a candidate gene associated with early-onset nicotine dependence (23). Lanza and Vasilenko examined nicotine dependence among smokers in a sample of lifetime smokers aged ⩽40 years and found, similar to our findings, no association with dependence for smokers whose age of onset was >18 years (prevalence of nicotine dependence, about 25%), but that prevalence increased linearly to a maximum at 10 years (45%) (24).
The study is subject to a number of limitations. The NHIS relies on participant self-report of physician diagnosis and not spirometry to define COPD, raising the potential for misclassification of self-report of physician-diagnosed COPD, a limitation of survey research in this area. COPD is often underdiagnosed (25), and self-reports of COPD underestimate the true prevalence of the disease when spirometry is performed (26). Age <15 years could be capturing unmeasured aspects of lifetime cigarette smoking not accounted for by current smoking and pack-years or duration of smoking. There could also be unmeasured third variables (e.g., fetal or secondhand smoke exposure) that explain the association we report for childhood cigarette smoking. Parental smoking not only increases exposure to smoke during childhood lung development but also increases the risk the child will take up smoking (27, 28). Unmeasured aspects of poverty, associated with both COPD and childhood smoking, could explain the results. Finally, the onset of “regular” smoking was left to the interpretation of the respondent, which could be taken as a limitation. However, a 2012 survey of U.S. adults 30–39 years old (National Survey of Drug Use and Health) found that among lifetime smokers, 23.3% recalled they started daily smoking by age 15 years (29), not dissimilar to our finding of 16%.
The present findings warrant replication; all cohort studies on the etiology of COPD should include the age of onset of regular cigarette smoking to test its association with COPD incidence. Future studies of cigarette smoking and adolescent lung development would benefit from capturing intermediate outcomes along the pathway from cigarette smoking initiation to development of COPD. Quantitative computed tomography scans can provide information about lung development, including measurements of dysanapsis, a mismatch of airway tree caliber to lung size that arises early in life and is associated with COPD (30). These outcomes were not available in NHIS but should be considered in focused cohorts that assess lifetime smoking and subsequent COPD risk.
This study also has several strengths. We found that the association between childhood cigarette smoking and COPD was independent of current smoking and cigarette smoking history. The association was robust across categories of current smoking status and alternative measurements of smoking history and not easily explained by downward bias in childhood smokers’ reports of smoking history. The findings add further support for the World Health Organization Framework Convention on Tobacco Control guidelines aimed at reducing childhood smoking, including smoke-free policies (article 9), plain packaging (article 11), public awareness campaigns aimed at teens (article 12), a ban on tobacco advertising (article 13), and a prohibition on the sale of tobacco to anyone >18 years of age (article 16) (31). Finally, the association was identified in a nationally representative sample of older U.S. adults. Although it would be worthwhile to replicate the findings in other studies of COPD, this study gives child health providers and public health officials reason to be very concerned about future chronic disease among patients who begin smoking during early adolescence, both because of the increased risk of nicotine addiction and perhaps because of its impact on lung development.
Footnotes
Supported by NIH grant R21HL161758.
Author Contributions: J.D.S. and L.M.P. conceptualized the study and oversaw the analysis and interpretation of the data and its contextualization with respect to the current literature. M.H., J.O., and Z.T. acquired the data and weights, conducted the data analysis, and offered critical feedback on data interpretation and on drafts of the manuscript. C.A.S. and A.W.S. provided feedback on analysis and interpretation of the data and on manuscript drafts. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Originally Published in Press as DOI: 10.1164/rccm.202303-0476OC on June 22, 2023
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Agustí A, Hogg JC. Update on the pathogenesis of chronic obstructive pulmonary disease. N Engl J Med . 2019;381:1248–1256. doi: 10.1056/NEJMra1900475. [DOI] [PubMed] [Google Scholar]
- 2. Allinson JP, Hardy R, Donaldson GC, Shaheen SO, Kuh D, Wedzicha JA. Combined impact of smoking and early-life exposures on adult lung function trajectories. Am J Respir Crit Care Med . 2017;196:1021–1030. doi: 10.1164/rccm.201703-0506OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Park-Lee E, Ren C, Cooper M, Cornelius M, Jamal A, Cullen KA. Tobacco product use among middle and high school students: United States, 2022. MMWR Morb Mortal Wkly Rep . 2022;71:1429–1435. doi: 10.15585/mmwr.mm7145a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nelson DE, Giovino GA, Shopland DR, Mowery PD, Mills SL, Eriksen MP. Trends in cigarette smoking among US adolescents, 1974 through 1991. Am J Public Health . 1995;85:34–40. doi: 10.2105/ajph.85.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gilliland FD, Li Y-F, Dubeau L, Berhane K, Avol E, McConnell R, et al. Effects of glutathione S-transferase M1, maternal smoking during pregnancy, and environmental tobacco smoke on asthma and wheezing in children. Am J Respir Crit Care Med . 2002;166:457–463. doi: 10.1164/rccm.2112064. [DOI] [PubMed] [Google Scholar]
- 6. He Z, Wu H, Zhang S, Lin Y, Li R, Xie L, et al. The association between secondhand smoke and childhood asthma: a systematic review and meta-analysis. Pediatr Pulmonol . 2020;55:2518–2531. doi: 10.1002/ppul.24961. [DOI] [PubMed] [Google Scholar]
- 7. Thacher JD, Schultz ES, Hallberg J, Hellberg U, Kull I, Thunqvist P, et al. Tobacco smoke exposure in early life and adolescence in relation to lung function. Eur Respir J . 2018;51:1702111. doi: 10.1183/13993003.02111-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sargent J, Halenar M, Tang Z, Stanton C, Steinberg A, Paulin LM. Age started smoking regularly and risk of COPD. Am J Respir Crit Care Med . 2023 doi: 10.1164/rccm.202303-0476OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chen Y, Breithaupt K, Muhajarine N. Occurrence of chronic obstructive pulmonary disease among Canadians and sex-related risk factors. J Clin Epidemiol . 2000;53:755–761. doi: 10.1016/s0895-4356(99)00211-5. [DOI] [PubMed] [Google Scholar]
- 10. Liaw K-M, Chen C-J. Mortality attributable to cigarette smoking in Taiwan: a 12-year follow-up study. Tob Control . 1998;7:141–148. doi: 10.1136/tc.7.2.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Liu B-Q, Peto R, Chen Z-M, Boreham J, Wu Y-P, Li J-Y, et al. Emerging tobacco hazards in China: 1. Retrospective proportional mortality study of one million deaths. BMJ . 1998;317:1411–1422. doi: 10.1136/bmj.317.7170.1411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Patel BD, Luben RN, Welch AA, Bingham SA, Khaw KT, Day NE, et al. Childhood smoking is an independent risk factor for obstructive airways disease in women. Thorax . 2004;59:682–686. doi: 10.1136/thx.2003.010215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Geijer RM, Sachs AP, Verheij TJ, Salomé PL, Lammers J-WJ, Hoes AW. Incidence and determinants of moderate COPD (GOLD II) in male smokers aged 40-65 years: 5-year follow up. Br J Gen Pract . 2006;56:656–661. [PMC free article] [PubMed] [Google Scholar]
- 14. Samet JM, Lange P. Longitudinal studies of active and passive smoking. Am J Respir Crit Care Med . 1996;154:S257–S265. doi: 10.1164/ajrccm/154.6_Pt_2.S257. [DOI] [PubMed] [Google Scholar]
- 15. Lebowitz MD, Holberg CJ. Effects of parental smoking and other risk factors on the development of pulmonary function in children and adolescents: analysis of two longitudinal population studies. Am J Epidemiol . 1988;128:589–597. doi: 10.1093/oxfordjournals.aje.a115006. [DOI] [PubMed] [Google Scholar]
- 16. Gold DR, Wang X, Wypij D, Speizer FE, Ware JH, Dockery DW. Effects of cigarette smoking on lung function in adolescent boys and girls. N Engl J Med . 1996;335:931–937. doi: 10.1056/NEJM199609263351304. [DOI] [PubMed] [Google Scholar]
- 17. Janson H. Longitudinal patterns of tobacco smoking from childhood to middle age. Addict Behav . 1999;24:239–249. doi: 10.1016/s0306-4603(98)00061-6. [DOI] [PubMed] [Google Scholar]
- 18. Klein H, Sterk CE, Elifson KW. Initial smoking experiences and current smoking behaviors and perceptions among current smokers. J Addict . 2013;2013:491797. doi: 10.1155/2013/491797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lando HA, Thai DT, Murray DM, Robinson LA, Jeffery RW, Sherwood NE, et al. Age of initiation, smoking patterns, and risk in a population of working adults. Prev Med . 1999;29:590–598. doi: 10.1006/pmed.1999.0590. [DOI] [PubMed] [Google Scholar]
- 20. Breslau N, Fenn N, Peterson EL. Early smoking initiation and nicotine dependence in a cohort of young adults. Drug Alcohol Depend . 1993;33:129–137. doi: 10.1016/0376-8716(93)90054-t. [DOI] [PubMed] [Google Scholar]
- 21. Khuder SA, Dayal HH, Mutgi AB. Age at smoking onset and its effect on smoking cessation. Addict Behav . 1999;24:673–677. doi: 10.1016/s0306-4603(98)00113-0. [DOI] [PubMed] [Google Scholar]
- 22. Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob Control . 1997;6:S57–S62. doi: 10.1136/tc.6.suppl_2.s57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Weiss RB, Baker TB, Cannon DS, von Niederhausern A, Dunn DM, Matsunami N, et al. A candidate gene approach identifies the CHRNA5-A3-B4 region as a risk factor for age-dependent nicotine addiction. PLoS Genet . 2008;4:e1000125. doi: 10.1371/journal.pgen.1000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lanza ST, Vasilenko SA. New methods shed light on age of onset as a risk factor for nicotine dependence. Addict Behav. 2015;50:161–164. doi: 10.1016/j.addbeh.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lamprecht B, Soriano JB, Studnicka M, Kaiser B, Vanfleteren LE, Gnatiuc L, et al. BOLD Collaborative Research Group, the EPI-SCAN Team, the PLATINO Team, and the PREPOCOL Study Group Determinants of underdiagnosis of COPD in national and international surveys. Chest . 2015;148:971–985. doi: 10.1378/chest.14-2535. [DOI] [PubMed] [Google Scholar]
- 26. Petty TL. Scope of the COPD problem in North America: early studies of prevalence and NHANES III data: basis for early identification and intervention. Chest . 2000;117:326S–331S. doi: 10.1378/chest.117.5_suppl_2.326s. [DOI] [PubMed] [Google Scholar]
- 27. Guerra S, Stern DA, Zhou M, Sherrill DL, Wright AL, Morgan WJ, et al. Combined effects of parental and active smoking on early lung function deficits: a prospective study from birth to age 26 years. Thorax . 2013;68:1021–1028. doi: 10.1136/thoraxjnl-2013-203538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Laverty AA, Filippidis FT, Taylor-Robinson D, Millett C, Bush A, Hopkinson NS. Smoking uptake in UK children: analysis of the UK Millennium Cohort Study. Thorax . 2019;74:607–610. doi: 10.1136/thoraxjnl-2018-212254. [DOI] [PubMed] [Google Scholar]
- 29.U.S. Department of Health and Human Services. 2014. https://www.cdc.gov/tobacco/sgr/50th-anniversary/index.htm [DOI] [PubMed]
- 30. Smith BM, Kirby M, Hoffman EA, Kronmal RA, Aaron SD, Allen NB, et al. MESA Lung, CanCOLD, and SPIROMICS Investigators Association of dysanapsis with chronic obstructive pulmonary disease among older adults. JAMA . 2020;323:2268–2280. doi: 10.1001/jama.2020.6918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. WHO framework convention on tobacco control. Geneva, Switzerland: World Health Organization; 2003. https://apps.who.int/iris/handle/10665/42811 [Google Scholar]