Abstract
Tissue flossing (TF) is a novel device that has been shown to cause peripheral compression and concurrent change in joint range of motion, perception of mobility and muscular performance. However, the effect of tissue flossing on pain, perception of mobility and function at the elbow joint has not been thoroughly investigated. The purpose of this pilot study was to examine the acute effect of TF on pain and upper extremity functional performance in subjects with musculoskeletal-related complaints of pain surrounding the elbow joint. We utilized a randomized crossover design. Nine resistance trained participants (8 men/1 woman) mean age 35.6 ± 10.7 took part in this study. We measured the following outcome measures; Pain Visual Analog Scale, Short Form McGill Pain Questionnaire II, pain-pressure threshold and hand grip dynamometry (HHD) pre and post and a Likert scale for movement ability questionnaire, posttest only, following a TF and placebo condition for each participant. TF resulted in significant improvement in all test measures, except HHD, pre to post (p ≤ 0.05). All pre to post changes were associated with large effect sizes for TF compared to the placebo condition applied to the elbow improves pain quality and intensity, perception of mobility and pain-pressure threshold in resistance trained individuals with a history of musculoskeletal pain for greater than 1 month. The results of this pilot study suggest that TF may function as an adjunct to treatment in the management of musculoskeletal pathologies at the elbow joint.
Keywords: Flossband, tissue flossing, physical therapy, compression band, elbow pain
INTRODUCTION
Musculoskeletal pain at the elbow joint is a common ailment affecting a range of populations. Tendinopathy is one of the more common pathologies observed at the elbow (11, 12). Individuals affected by tendinopathy report local pain, edema, decreased strength, power and range of motion (ROM), as well as neuromuscular deficits (5, 8). Physical therapy (PT) is a non-surgical option for treatment employed during various stages of tendinopathy progression. Physical therapists may opt to provide manual therapy, compression modalities, amongst others, to manage symptoms and address the pathophysiological mechanisms of tendinopathy. Following treatment, patients have reported improved pain quality and intensity, mobility and functional performance (5, 21).
Tissue-flossing (TF) is the use of an elastic band to provide focal compression on soft tissue and joints, popularized by Starrett and Cordoza, the intervention requires active and/or passive ROM while the affected structure is under compression exerted by the band (40). Mounting anecdote and emerging research has led to strong consideration of this simple, cost-effective tool for clinical application (14, 15, 43). TF was utilized as an adjunct to treatment following a 6-week course of traditional PT which failed to produce clinical improvements in ankle pain and function (6). The subject in this case study significantly improved following the 6-weeks of TF treatment. Similarly, another case study reported on the clinical application of TF in a patient afflicted by Keinböck’s disease, an idiopathic avascular necrosis of the lunate bone (7). The subject presented with pain and concurrent loss of wrist and hand function. The subject reported improvements in both pain and function following 6-weeks of treatment.
Additional evidence supporting TF in the management of musculoskeletal pain was investigated in response to exercise-induced delayed-onset muscle soreness (EDOMS) (36). Frequently, EDOMS results in peak symptoms up to 72 hours post-exercise and is characterized by muscle pain, edema, decreased strength, power and ROM, with concurrent neuromuscular deficits. They reported significant improvement in the outcome measures throughout the follow-up period.
Along with clinical utility, TF has shown to enhance muscular performance in athletic populations (14, 15, 43). Driller et al. utilized a TF technique at the ankle and examined the acute effects on performance metrics including the weight-bearing lunge test (WBLT), dorsiflexion (DF) and plantar-flexion ROM and single-leg vertical jump test for both height and velocity (14). The results revealed significant improvements across all performance variables. Additionally, Driller et al. investigated the time-course of the TF effect; performance metrics included the WBLT, countermovement jump and 15m sprint test (15). Significant improvements were found in WBLT at all time-points, up to 45-minutes following application. The effect of an acute bout of TF versus static stretch and a control condition was also investigated (20). Outcomes were collected for several physiological measures including rate of force development (RFD) and DF ROM. Significance was achieved in DF ROM for TF vs. control and RFD for TF vs. static stretch.
Given the relative novelty of this modality and limited research regarding its application, the mechanism to change remains poorly understood. The current body of literature postulates the observed effect relative to local therapeutic compression, myofascial manipulation and/or reperfusion. Recent advances in the understanding of pain and its manifestations reveal a more complex relationship than previously concluded, relying on many domains including perception (29, 41). This has allowed an increased understanding of physical modalities and their role in the management of musculoskeletal pain (9, 38, 39). It has been reported that the mechanical force from manual therapy initiates a cascade of neurophysiological responses from the peripheral and central nervous system which are then responsible for the improved clinical outcomes (4). Kiefer et al. (22), to the authors’ knowledge, is the only investigation to link performance metrics and perception of mobility to a TF intervention. They reported a significant improvement in the perception of mobility of the glenohumeral joint in the TF group in comparison to a control group, However, the subjects utilized did not have any previous shoulder pain or limitations in ROM or function. It is well understood that perceptions of treatment and self-efficacy confer enhanced patient compliance and relative therapeutic outcomes (22, 34, 42). An investigation regarding the utility of TF on perception of mobility with subjects who have musculoskeletal deficits is warranted. There is also a gap in the knowledge investigating the effects of TF on subjects with elbow tendinopathy Thus, the purpose of the current investigation was to examine the acute effect of TF on pain and upper extremity functional performance in subjects with musculoskeletal-related complaints of pain surrounding the elbow joint.
METHODS
Participants
Nine resistance trained participants (8 men/1 woman) mean age 35.6 ± 10 volunteered to participate in this study. Participants were recruited through a privately-owned athletic performance facility (Gaglione Strength, Farmingdale, NY, United States) and college campus New York Institute of Technology (NYIT) Old Westbury, NY, United States. To be eligible for the study, participants had to be actively engaged in a consistent resistance training program, with at least 6 months of experience, in generally good health and have had pain in the elbow area for greater than 1 month with a pain visual analog score (VAS) of 3 or greater out of a 0–10 scale. Inclusion and exclusion criteria are presented in Table 1. The study was approved by NYIT Institutional Review Board (BHS # 1444) and the study was registered at www.ClinicalTrail.gov (NCT04899375) In addition, this manuscript adheres to the ethical policies of the Editorial board of the International Journal of Exercise Science and guidelines outlined by Navalta et. al. (30). The participants were informed of the methods, procedures, risks and were asked to sign the approved consent form prior to starting the study.
Table 1.
Inclusion/Exclusion Criteria
| Exclusion | Inclusion |
|---|---|
|
| |
| Evidence of acute injury (i.e. edema, erythema or petechiae) | Pain Visual Analog Scale (VAS) ≥ 3/10 |
| History of disease or condition to contraindicate peripheral compression | Tenderness to palpation (TTP) within 7cm above or below the olecranon process |
| History of elbow instability or recent surgical intervention | Painful passive range of motion in one or more the osteokinematic motions at the elbow complex |
| Recent corticosteroid or platelet rich plasma injection | |
The study utilized a randomized crossover design, in which participants performed a battery of tests pre and posttest outcome measures in the following order: Visual Analog Scale for pain (VAS), Short-form McGill Pain Questionnaire II (SF-MPQII), Likert Scale (LS) post-test only, Pain-pressure Threshold (PPT), and Handgrip Dynamometry (HGD). Both the experimental and placebo conditions consisted of an active ROM protocol immediately following the application of either a tissue floss band (TF) (MobilityWOD, Wilmington, DE) or generic, non-compressive bandage (NCB). Participants were blinded by a partition effectively blocking the view of the affected extremity throughout the intervention. Additionally, both bands were of similar color, length and width making them difficult to distinguish. Participants reported to the research site on two separate occasions. On the first visit, all were randomized, via computerized random list generator, in a crossover design to either TF or NCB. There was a minimum washout period of 1 week to reduce both order and carry-over effects. Prior to each trial, participants were instructed to refrain from the use of analgesic medication (i.e. non-steroidal anti-inflammatory drugs) for a minimum of 24 hours before reporting to the testing site.
A standardized wrapping technique was employed by applying the TF and NCB accordingly: distance measurements were taken extending a minimum of 7cm, and a maximum of 10cm, proximal and distal from the olecranon process. The FB, or NCB, was then applied (50% stretch for the FB and 0% stretch for NCB) beginning proximally and extending distally with approximately 50% overlap of the previous wrap. To complete the application, the remaining end was secured under the final wrap (Fig. 1).
Figure 1.
Floss band application
Protocol
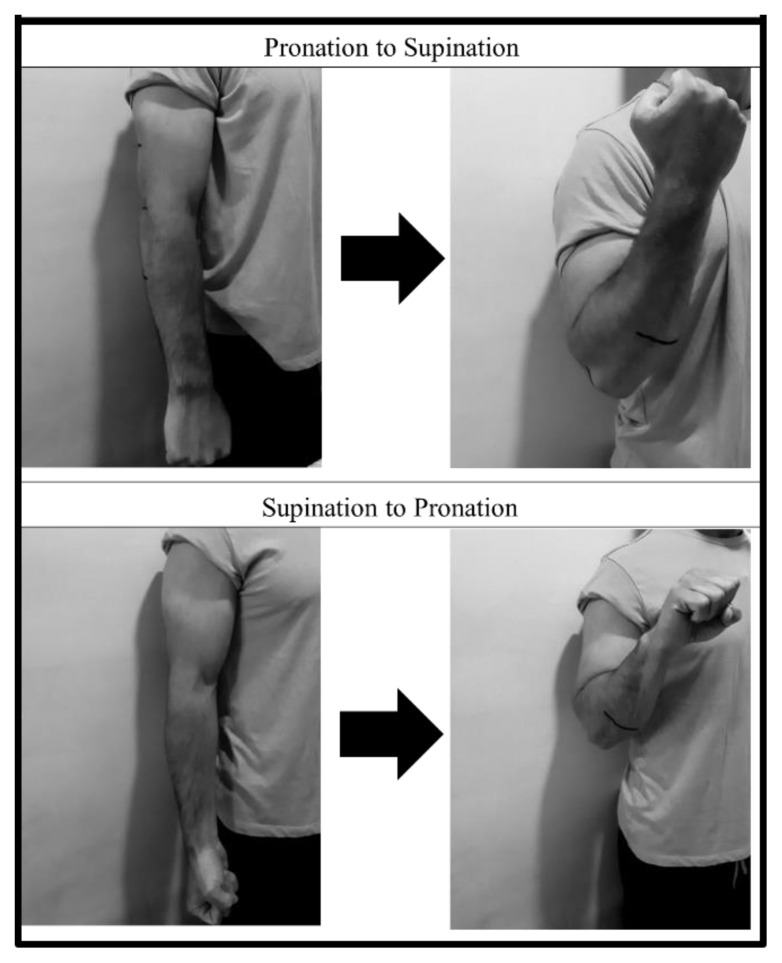
Immediately following the application of either condition, all participants completed a standardized AROM exercise protocol. The protocol was a total of 2 minutes, executed accordingly: 10 to 15 repetitions of elbow flexion and extension, beginning in extension and supination, ending in flexion and pronation (Fig. 2). Next, 10 to 15 repetitions beginning in extension and pronation, ending in flexion and supination (Fig. 2). Last, 10 to 15 repetitions of wrist flexion and extension in a neutral forearm position (Fig. 3).
Figure 2.
AROM Protocol: Elbow
Figure 3.
AROM Protocol: Wrist
Pain data were collected via paper form utilizing the VAS, prior to and immediately upon completion TF or NCB condition. Participants were provided a copy of the instrument and instructed to honestly assess their pain experience. VAS is a commonly employed self-completed scale for the assessment of pain in adults (17). The instrument is scored using a numerical scale from 0 to 10, whereas 0 indicates no pain and 10 indicates maximal pain.
Data relative to pain perception and affect were collected via paper form SF-MPQII. Prior to and immediately upon completion of either condition, participants were provided a copy of the instrument and instructed to honestly assess their pain experience. The SF-MPQII is a shorter version of the original McGill Pain Questionnaire. It is a multidimensional measure of pain. The SF-MPQII has been shown to be a valid and reliable tool to measure pain in adults (1, 17).
Perception of movement capacity was examined via LS, adapted from Kiefer et al. (22). The LS (Fig. 4) was employed during post-test data collection only and was administered in a pen and paper format. The typical LS is a 5- or 7-point ordinal scale used by respondents to rate the degree to which they agree or disagree with a statement (19).
Figure 4.
Likert Scale
PPT measurements were collected upon the completion of the preceding tests and were evaluated via algometry. Algometry is the assessment of load-dependent tenderness at a specific anatomical site. The Force Ten™ FDX Pressure Algometer (Wagner Instruments, Greenwich, CT) was used to quantify PPT and has been shown to be reliable and valid (23, 32). The procedure for algometric measurement was adapted from Park et al. (31) and was standardized according to the following: the algometer was applied to the subject-indicated, point-of-greatest-pain (Table 2.) Pressure was increased at a rate approximately 1 kg/cm2/s. The participant indicated increased pain by saying the word “ouch,” the test was then concluded, and the measurement recorded. The procedure was repeated for a total of 3 trials; average scores were calculated and recorded.
Table 2.
Point of Greatest Pain
| Point-Of-Greatest-Pain | Descriptor |
|---|---|
| Distal Biceps Brachii Tendon | 2cm proximal to the antecubital fossa |
| Common Extensor Tendon | 3cm distal to the lateral epicondyle |
| Common Flexor Tendon | 3cm distal to the medial epicondyle |
| Pronator Teres Muscle Belly | 5cm distal to the antecubital fossa |
| Distal Triceps Brachii Tendon | 3cm distal to the olecranon process |
HGD was evaluated by The Jamar hydraulic hand dynamometer (JLW Instruments, Chicago, IL), which has been shown to be reliable and valid when measuring strength in adults with injuries to the upper limb (16, 33). The HGD measurements were standardized according to the following: participants performed a measure of pain-free grip strength, followed by max grip strength regardless of pain in 90 degrees of elbow flexion, 0 degrees of shoulder extension, neutral wrist and hand position. Two trials were performed, separated by 60 seconds rest; average scores for both pain-free and maximal grip strength were calculated and recorded.
Statistical Analysis
All values are reported as mean ± standard deviation. Statistical analyses were performed using the Statistical Package for Social Science (V.25.0, SPSS Ins., Chicago, IL). A priori power analysis for a crossover design specified that a sample size of 9 subjects would provide sufficient power (80%) to observe differences assuming a moderate effect size. Differences between the pre and post test scores were utilized as change scores for the following dependent variables; VAS, SF-MPQ II, algometry, and handgrip strength scores for subsequent data analysis utilizing paired t–tests. The perception of movement ability as measured by the movement questionnaire was also analyzed utilizing a paired t–test. Data were considered significant at the p ≤ 0.05 level. In addition, for all t-tests, Cohen’s d effect sizes were calculated with small, medium, and large effects interpreted as greater than 0.2, 0.5, and 0.8, respectively (35).
RESULTS
The physiological characteristics of the nine participants (8 men and 1 woman) are presented in Table 3. Table 4 presents the results of the paired t-tests for the outcome measures. There were significant differences (p ≤ 0.05) between TF and the placebo on improving VAS, SF-MPQ II, and algometry with large effect sizes. Table 4 also contains the results of the Likert Scale movement ability questionnaire. There was significant improvement with the subjects’ perception of movement ability following TF (p = 0.04) with a large effect. There were no significant improvements in handgrip or pain free handgrip strength.
Table 3.
Physiological Characteristics (n = 9)
| Age (yrs) | 35.6 ± 10.7 |
| Height (cm) | 172.4 ± 6.89 |
| Weight (kg) | 94.9 ± 17.7 |
Table 4.
Results of Paired t-Tests for Outcome Measures
| Outcome measure | Mean Difference | P value | Effect Size |
|---|---|---|---|
| VAS | 1.11 ± 1.17 | 0.02* | 1.33 |
| SF-MPQ II | 17.67 ± 29.18 | 0.05* | 0.85 |
| Algometry (kg) | .45 ±.69 | 0.04* | 0.92 |
| Likert Scale | .98 ± 1.52 | 0.04* | 0.90 |
| Handgrip (kg) | 1.47 ± 5.84 | 0.47 | |
| Handgrip Pain Free (kg) | .42 ± 1.69 | 0.048 |
VAS- Visual Analog Scale for Pain 0–10, SF-MPQ II- Short Form McGill Pain Questionnaire
Denotes significance P ≤ 0.05
DISCUSSION
This is the first study to our knowledge, to examine the effects of TF on measures of pain and function in subjects with a history of musculoskeletal pain at the elbow joint. The results demonstrated significant improvement in pain quality and intensity, PPT and perceived capacity for movement. The SF-MPQII, VAS, PPT and LS were all associated with a large effect sizes, in favor of TF versus the placebo. Results for HGD were not significant. Our findings suggest TF may function as an effective means to alter pain and perception of mobility in a clinical setting.
The results of this pilot study are contrary to evidence presented by a similar investigation (43). Their study presented data on pain and function assessed via numeric rating scale, disabilities of the arm, shoulder and hand and ROM. Their results demonstrated improvement in all domains following an acute bout of TF; however, there was no significant difference between TF and a control condition. Additionally, they reported adverse effects including increased pain, skin changes and dyspnea in select subjects. It is important to note, the current investigation did not record any adverse events. Conversely, our results are in agreement with research performed on clinical populations (6, 7). They described positive effects following multiple treatments utilizing TF on functional capacity and markers of pain in their respective case studies. Our results are also in accord with Prill et al. (36) who demonstrated efficacy to reduce pain following a single application of TF in subjects affected by EDOMS. Our results are also in agreement with a study who investigated the perception of mobility in healthy subjects with normal shoulder ROM (22). The reported there was no effect on true glenohumeral joint ROM, however, noted significant effects in the subject’s perception of glenohumeral mobility, which was a similar result of this investigation.
Recently, there has been a shift in health care models to focus on patient-centered care (2, 10, 27, 28). Among the tenants of patient-centered care lies self-efficacy and patient beliefs and both have shown to be predictors of patient compliance and ultimately therapeutic outcome (13, 34, 37, 42). Due to the acute effects observed on clinical markers of pathology, it is possible that TF may serve as an adjunct in the management of musculoskeletal pathologies at the elbow (i.e. tendinopathy), through enhanced face validly of treatment and resultant patient compliance.
The physiological mechanisms by which pain and perception were altered remains to be fully understood. Previous research has presented several theories regarding myofascial manipulation, peripheral mechanoreceptor stimulation, vascular occlusion, reperfusion and local hormonal response (3, 14, 15, 36, 43). Pressure measurements between the floss band and subjects’ skin; pressures of 182 ± 38 mmHg have been measured (15). This pressure is significant enough to cause a high percentage of vascular and arterial occlusion (26). Being that the floss band, in this study, was applied in a similar manner, it is reasonable to suggest a comparable magnitude of pressure and resultant occlusion. Previous research has indicated that exercise under a state of partial vascular and arterial occlusion, known as blood flow restriction training, may produce favorable effects on pain and functional performance in clinical populations (18, 24, 25). Furthermore, it has been suggested compression garments, worn at the elbow joint, may serve to alter somatosensory feedback and nervous system excitability with concurrent improvements in proprioceptive precision and sensitivity (3).
Further research is recommended relative to the mechanisms discussed and their direct role in affecting change following a bout of TF. Additional investigations are also recommended regarding HGD as a measure of upper extremity function. A limitation in the current study is acknowledged relative to the HGD measures. Data were collected at only a single position, 90 degrees of elbow flexion and 0 degrees of shoulder extension. Future research should aim to collect data at a variety of shoulder and elbow positions to better capture changes in functional capacity. The authors also suggest including an outcome measure (i.e. DASH, Upper Extremity Functional Index) to more effectively quantify change. An additional limitation was noted for limited generalizability to other joints and soft tissues. Future investigations may consider the application at functionally similar joints (i.e. knee, wrist and ankle) due to ease and consistency of application.
Conclusion
The current pilot study is the first to describe the acute effects of TF in subjects with a history of elbow pain. The results of this pilot study may carry implications for the future management of patients affected by musculoskeletal related pain and concurrent loss of function at the elbow. As the medical field continues to evolve, incorporating patient centered care; increasing pressures are placed upon clinicians to provide effective means for improved patient compliance and related therapeutic outcomes. TF presents as a potential cost-effective and user-friendly modality with a capacity to yield immediate benefits for pain and perceived mobility, possibly boosting the face validity of treatment and resultant compliance.
REFERENCES
- 1.Adelmanesh F, Jalali A, Attarian H, Farahani B, Ketabchi SM, Arvantaj A, Raissi GR. Reliability, validity, and sensitivity measures of expanded and revised version of the short-form McGill pain questionnaire (SF-MPQII) in Iranian patients with neuropathic and non-neuropathic pain. Pain Med. 2012;13:1631–1638. doi: 10.1111/j.1526-4637.2012.01517.x. [DOI] [PubMed] [Google Scholar]
- 2.Barry MJ, Edgman-Levitan S. Shared decision making - the pinnacle of patient-centered care. New Engl J Med. 2012;366:780–1. doi: 10.1056/NEJMp1109283. [DOI] [PubMed] [Google Scholar]
- 3.Barss TS, Pearcey GEP, Munro B, Bishop JL, Zehr EP. Effects of a compression garment on sensory feedback transmission in the human upper limb. J Neurophysiol. 2018;120(1):186–195. doi: 10.1152/jn.00581.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14:531–538. doi: 10.1016/j.math.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bisset LM, Vicenzino B. Physiotherapy management of lateral epicondylalgia. J Physiother. 2015;61:174–181. doi: 10.1016/j.jphys.2015.07.015. [DOI] [PubMed] [Google Scholar]
- 6.Borda J, Selhorst M. The use of compression tack and flossing along with lacrosse ball massage to treat chronic Achilles tendinopathy in an adolescent athlete: a case report. J Man Manipulative Ther. 2016;25:57–61. doi: 10.1080/10669817.2016.1159403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cage SA, Warner BJ, Stevenson P, Arce-Esquivel AA. Flossing bands to treat Keinböck’s disease in a collegiate men’s basketball player: a case report. Int Phys Med Rehabil J. 2018;3(2):166–168. [Google Scholar]
- 8.Cain EL, Moroski NM. Elbow surgery in athletes. Sports Med Arthrosc Rev. 2018;26:181–184. doi: 10.1097/JSA.0000000000000227. [DOI] [PubMed] [Google Scholar]
- 9.Chris B, Skarabot J. Effects of self-myofascial release: a systematic review. J Bodyw Move Ther. 2015;19:747–758. doi: 10.1016/j.jbmt.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 10.Davis K, Schoenbaum SC, Audet AM. A 2020 vision of patient-centered primary care. J Gen Inter Med. 2005;20:953–957. doi: 10.1111/j.1525-1497.2005.0178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donaldson O, Vannet N, Gosens T, Kulkarni R. Tendinopathies around the elbow part 1: lateral elbow tendinopathy. Shoulder Elbow. 2013;5:239–250. doi: 10.1111/sae.12022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Donaldson O, Vannet N, Gosens T, Kulkarni R. Tendinopathies around the elbow part 2: medial elbow, distal biceps and triceps tendinopathies. Shoulder Elbow. 2014;6:47–56. doi: 10.1111/sae.12022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3:e001570. doi: 10.1136/bmjopen-2012-001570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Driller MW, Overmayer RG. The effects of tissue flossing on ankle range of motion and jump performance. Phy Ther Sport. 2017;25:20–24. doi: 10.1016/j.ptsp.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 15.Driller M, Mackay K, Mills B, Tavares F. Tissue flossing on ankle range of motion, jump and sprint performance: a follow-up study. Phy Ther Sport. 2017;28:29–33. doi: 10.1016/j.ptsp.2017.08.081. [DOI] [PubMed] [Google Scholar]
- 16.Hamilton GF, Mcdonald C, Chenier TC. Measurement of grip strength: validity and reliability of the sphygmomanometer and Jamar grip dynamometer. J Orthop Sports Phys Ther. 1992;16:215–219. doi: 10.2519/jospt.1992.16.5.215. [DOI] [PubMed] [Google Scholar]
- 17.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (VAS pain), numeric rating scale for pain (NRS pain), McGill pain questionnaire (MPQ), short form McGill pain questionnaire II (SF-MPQII), chronic pain grade scale (CPGS), short form 36 bodily pain scale (SF 36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP) Arthritis Care Res. 2011;63(Suppl 11):S240–252. doi: 10.1002/acr.20543. [DOI] [PubMed] [Google Scholar]
- 18.Hughes L, Patterson SD. Low intensity blood flow restriction exercise: rationale for a hypoalgesia effect. Med Hypotheses. 2019;132:109370. doi: 10.1016/j.mehy.2019.109370. [DOI] [PubMed] [Google Scholar]
- 19.Joshi A, Kale S, Chandel S, Pal DK. Likert scale: explored and explained. Br J Appl Sci Technol. 2015;7:396–403. [Google Scholar]
- 20.Kaneda H, Takahira N, Tsuda K. The effects of tissue flossing and static stretching on gastrocnemius exertion and flexibility. Iso Exerc Sci. 2020;25:205–213. [Google Scholar]
- 21.Khuman R, Trivedi P, Devi S, Sathyavani GN, Shah K. Myofascial release technique in chronic lateral epicondylitis: a randomized controlled study. Int J Health Sci Res. 2013;3:45–52. [Google Scholar]
- 22.Kiefer BN, Lemarr KE, Enriquez CC, Tivener KA, Daniel T. A pilot study: perceptual effects of the voodoo floss band on glenohumeral flexibility. Int J Athl Ther Train. 2017;22:29–33. [Google Scholar]
- 23.Kinser AM, Sands WA, Stone MH. Reliability and validity of a pressure algometer. J Strength Cond Res. 2009;23:312–314. doi: 10.1519/jsc.0b013e31818f051c. [DOI] [PubMed] [Google Scholar]
- 24.Korakakis V, Whiteley R, Epameinontidis K. blood flow restriction induces hypoalgesia in recreationally active adult male anterior knee pain patients allowing therapeutic exercise loading. Phys Ther Sport. 2018;32:235–243. doi: 10.1016/j.ptsp.2018.05.021. [DOI] [PubMed] [Google Scholar]
- 25.Ladlow P, Coppack RJ, Dharm-Datta S, Conway D, Sellon E, Patterson SD, Benett AN. Low-load resistance training with blood flow restriction improves clinical outcomes in musculoskeletal rehabilitation: a single-blind randomized controlled trial. Front Physiol. 2018;9:1269. doi: 10.3389/fphys.2018.01269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Loenneke JP, Fahs CA, Rossow LM, Thiebaud RS, Mattocks KT, Abe T, Bemben MG. Blood flow restriction pressure recommendations: a tale of two cuffs. Front Physiol. 2013;4:249. doi: 10.3389/fphys.2013.00249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mclean S, Burton M, Bradley L, Littlewood C. Interventions for enhancing adherence with physiotherapy: a systematic review. Man Ther. 2010;15:514–521. doi: 10.1016/j.math.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 28.Miller K. Patient centered care: A path to better health outcomes through engagement and activation. NeuroRehabilitation. 2016;39:465–470. doi: 10.3233/NRE-161378. [DOI] [PubMed] [Google Scholar]
- 29.Moseley GL. Reconceptualising pain according to modern neuroscience. Phys Ther Rev. 2007;12:169–178. [Google Scholar]
- 30.Navalta JW, Stone WJ, Lyons TS. Ethical issues relating to scientific discovery in exercise science. Int J Exerc Sci. 2019;12(1):1–8. doi: 10.70252/EYCD6235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Park G, Kim CW, Park SB, Kim MJ, Jang SH. Reliability and usefulness of the pressure pain threshold measurement in patients with myofascial pain. Ann Rehabil Med. 2011;35:412–417. doi: 10.5535/arm.2011.35.3.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pelfort X, Torres-Claramunt R, Sanchez-Soler JF, Hinarejos P, Leal-Blanquet J, Valverde D, Monllau JC. Pressure algometry is a useful tool to quantify pain in the medial part of the knee: an intra- and inter-reliability study in healthy subjects. Orthop Traumatol Surg Res. 2015;101:559–563. doi: 10.1016/j.otsr.2015.03.016. [DOI] [PubMed] [Google Scholar]
- 33.Peolsson A, Hedlund R, Oberg B. Intra- and inter-tester reliability and reference values for hand strength. J Rehabil Med. 2001;33:36–41. doi: 10.1080/165019701300006524. [DOI] [PubMed] [Google Scholar]
- 34.Picha KJ, Howell DM. A model to increase rehabilitation adherence to home exercise programmes in patients with varying levels of self efficacy. Musculoskeletal Care. 2018;16:233–237. doi: 10.1002/msc.1194. [DOI] [PubMed] [Google Scholar]
- 35.Portney LG. Foundations of clinical research: Applications to evidence based practice. 4th edition. F.A. Davis Company; 2020. [Google Scholar]
- 36.Prill R, Schulz R, Michel S. Tissue flossing: a new short-duration compression therapy for reducing exercise-induced delayed-onset muscle soreness. a randomized, controlled and double-blind pilot cross-over trial. J Sports Med Phys Fit. 2018;59:861–867. doi: 10.23736/S0022-4707.18.08701-7. [DOI] [PubMed] [Google Scholar]
- 37.Rathert C, Wyrwich MD, Boren SA. Patient-centered care and outcomes: a systematic review of the literature. Med Care Res Rev. 2012;70:351–379. doi: 10.1177/1077558712465774. [DOI] [PubMed] [Google Scholar]
- 38.Schleip R. Fascial plasticity – a new neurobiological explanation: Part 1. J Bodyw Move Ther. 2003;7:11–9. [Google Scholar]
- 39.Simmonds N, Miller P, Gemmell H. A theoretical framework for the role of fascia in manual therapy. J Bodyw Move Ther. 2012;16:83–93. doi: 10.1016/j.jbmt.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 40.Starrett K, Cordoza G. Becoming a supple leopard: the ultimate guide to resolving pain, preventing injury and optimizing athletic performance. 2nd edition. Victory Belt Publishing; 2015. [Google Scholar]
- 41.Thacker MA, Moseley GL. First-person neuroscience and the understanding of pain. Med J Aust. 2012;196:410–411. doi: 10.5694/mja12.10468. [DOI] [PubMed] [Google Scholar]
- 42.Vermeire E, Hearnshaw H, Van Royen P, Denekens J. Patient adherence to treatment three decades of research. A comprehensive review. J Clin PharmTher. 2001;26(5):331–342. doi: 10.1046/j.1365-2710.2001.00363.x. [DOI] [PubMed] [Google Scholar]
- 43.Wienke AK, Thiel C, Kopkow C. Effects of medical flossing in patients with shoulder diseases - randomised controlled pilot study. Physioscience. 2020;16:5–15. [Google Scholar]