Abstract
Introduction
While large progress has been achieved in identifying and treating the most common pathogens involved in periprosthetic joint infections (PJI), there remains limited knowledge on atypical pathogens such as Corynebacterium. For that reason, we analyzed infection and diagnostical characteristics, as well as treatment outcome in Corynebacterium PJI.
Methods
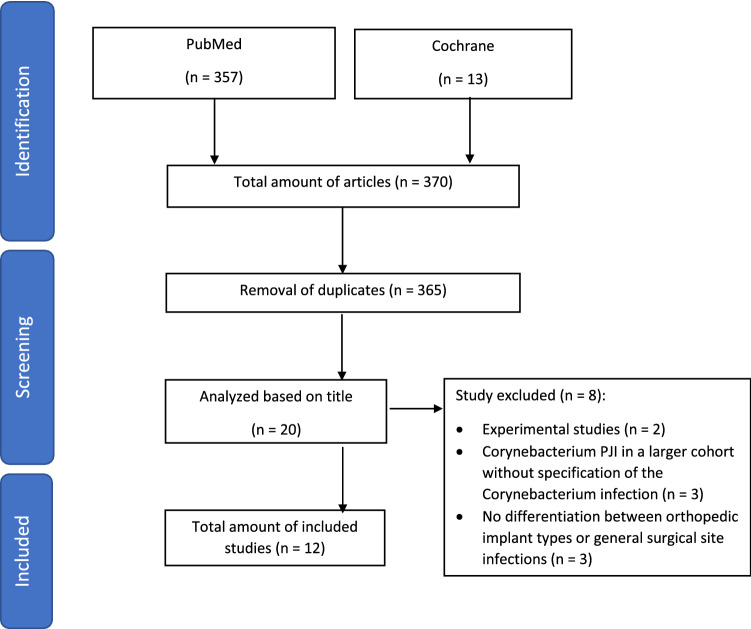
A systematic review was performed based on a structured PubMed and Cochrane Library analysis using the PRISMA algorithm. The search was performed by 2 independent reviewers, and articles from 1960 to 2022 considered eligible for inclusion. Out of 370 search results, 12 studies were included for study synthesis.
Results
In total, 52 cases of Corynebacterium PJI were identified (31 knees, 16 hips, 4 elbows, 1 shoulder). Mean age was 65 years, with 53% females, and a mean Charlson Comorbidity Index of 3.9. The most common species was Corynebacterium striatum in 37 cases (71%). Most patients were treated with two-stage exchange (40%), isolated irrigation and debridement (21%), and resection arthroplasty (19%). Mean duration of antibiotic treatment was 8.5 weeks. At a mean follow-up of 2.5 years, there were 18 reinfections (33%), and 39% were for Corynebacterium. Initial infection by Corynebacterium striatum species was predictive of reoperation (p = 0.035) and reinfection (p = 0.07).
Conclusion
Corynebacterium PJI affects multimorbid and elderly patients, with one in three developing a reinfection at short term. Importantly, the relative majority of reinfections was for persistent Corynebacterium PJI.
Keywords: Difficult to treat pathogens, Hip infection, Knee infection, Elbow infection, Shoulder infection, Gram-positive PJI, Atypical pathogens
Introduction
Periprosthetic joint infections (PJIs) remain a devastating complication following arthroplasty [1, 2]. Although large progress was made in identifying the most common pathogens involved, such as Staphylococcus aureus in acute infections, as well as coagulase-negative Staphylococci (CNS) in chronic infections, there is limited knowledge on characteristics of atypical pathogens such as Candida or gram-negative bacteria [3, 4].
Gram-positive bacilli are an atypical cause of PJI and often considered a contaminant in microbiology findings. The gram-positive bacillus Corynebacterium spp. is a facultatively anaerobically growing, gram-positive rod, and part of the standard flora of human skin and mucosa [3, 4]. Given its primary consideration as a contaminant in the context of PJI, as well as difficulties in cultivation, and oftentimes missing standardized diagnostical tools for assessment, there are limited reports on PJI caused by Corynebacterium [3–5].
As such, this systematic review aimed to summarize all cases of Corynebacterium PJI, diagnostical and clinical characteristics, as well as possible treatment strategies, and reported outcomes.
Material and methods
A systematic review was performed based on a structured PubMed and Cochrane Library analysis using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) criteria. Search terms were as followed: “Corynebacterium PJI OR Corynebacterium periprosthetic joint infection OR Corynebacterium joint infection OR Corynebacterium hip infection OR Corynebacterium knee infection OR Corynebacterium shoulder infection OR Corynebacterium elbow infection OR Corynebacterium finger infection OR Corynebacterium foot infection OR Corynebacterium septic arthritis OR Corynebacterium osteomyelitis “.
Final inclusion criteria were: (1) studies published from 1960 to September 2022, (2) PJI caused by Corynebacterium, and (3) clinical and diagnostical case description as well as an available follow-up. Exclusion criteria were: (1) non arthroplasty infections (soft tissue, osteosynthesis material, native joints, osteomyelitis), (2) animal and experimental studies without patients, (3) Corynebacterium PJI in the context of new diagnostical tests without detailed clinical follow-up and case description, and (4) Corynebacterium PJI as part of larger PJI cohorts or combined with other infection types without a detailed and separate description of the Corynebacterium PJI. Although cases of osteomyelitis and septic arthritis in native joints without a prosthesis in situ were excluded in the study, search criteria included these terms as older studies partially used a different terminology than PJI.
Search was divided into two phases (Fig. 1). Phase one included the identification of publications using the upper search terms. In phase two, screening of abstract was performed based on the eligibility criteria of this study. The search was performed by two independent reviewers (YS, DK). Outcome parameters included infection characteristics (affected joint, corynebacterium species, coexisting microbes), patient characteristics (age, sex, Body Mass Index (BMI), Charlson Comorbidity Index (CCI) [6], secondary diseases), arthroplasty details (year and indication for primary implantation), diagnostical work-up (CRP, ESR, preoperative joint aspiration, intraoperative tissue samples, symptoms, histopathology), surgical and antibiotic treatment, as well as outcome evaluation (follow-up, reinfection rates, revision rates, perioperative complications, mortality).
Fig. 1.
PRISMA Flowchart
Statistical analysis was performed using SPSS (SPSS Inc., Chicago, IL, USA), with T- and Mann–Whitney U tests for continuous variables, as well as Fisher exact test for categorical variables. A p-value < 0.05 was considered significant whereas a p-value < 0.1 was interpreted as a trend to significance.
Results
In total, 370 studies were identified using the aforementioned search terms. After exclusion of duplicates, 365 titles were screened for study inclusion, and 20 articles analyzed in detail. Of these 20 studies, 2 investigations were excluded as they were experimental studies without clinical details [7, 8], 3 studies as they reported of Corynebacterium PJI as part of a larger epidemiological cohort without specification of the Corynebacterium PJI itself [9–11], and another 3 as they were not differentiating between orthopedic implant types or referred to general surgical site infections without implants [12–14].
As such, a total of 12 studies with 52 cases of Corynebacterium PJI were included. Among these, there were 31 total knee arthroplasties (TKAs), 16 total hip arthroplasties (THAs), 4 elbow prosthesis and one shoulder prosthesis (Table 1) [15–26]. Cases were reported from North America, Europe and Asia between 1994 and 2022. The pathogen spectrum was as followed: Corynebacterium striatum (37 cases), Corynebacterium jeikeium (8 cases), Corynebacterium amycolatum (2 cases), Corynebacterium bovis (1 case) and unspecified species (4 cases). Mean age at time of Corynebacterium PJI was 64.7 years (± 12.1). Two studies did not clarify the patient’s sex. Among the remaining 10 studies, 19 were females, and 17 were males. Rheumatoid arthritis (29%) and diabetes mellitus type II (25%) were the most common secondary diseases. Mean Charlson Comorbidity Index (CCI) was 3.9 (range 0–11). A total of 6 cases had a prior PJI, none for Corynebacterium.
Table 1.
Included cases of Corynebacterium PJI
| Study | Weller et al. [15], 1994 Case 1 |
Case 2 | Yildiz S et al. [16], 1995 | Tleyjeh et al. [17], 2005 | Achermann et al. [18], 2009 | Wee et al. [19], 2013 | Streubel et al. [20], 2016 Case 1 |
Case 2 | Case 3 | Ferry et al. [21], 2017 | Fernández-Esgueva et al. [22], 2019 | Hernandez et al. [23], 2020 Case 1 |
x Case 2 |
x Case 3 |
Case 4 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country, Region | U.K., Oxford | U.K., Oxford | Turkey, Ankara | USA, Rochester | Switzerland, Zurich | Singapore, Singapore | USA, Omaha | USA, Omaha | USA, Omaha | France, Lyon | Spain, Zaragoza | USA, Durham | USA, Durham | USA, Durham | USA, Durham |
| PJI type | Hip | Hip | Knee | Hip | Shoulder | Elbow | Elbow | Elbow | Elbow | Knee | Knee | Hip | Hip | Hip | Knee |
| Age (years) | 52 | 44 | 67 | 78 | 62 | 67 | 39 | 61 | 54 | 54 | 85 | 69 | 77 | 72 | 63 |
| Sex | Female | Male | Female | Male | Female | Female | Female | Female | Male | NA | Female | Female | Female | Female | Male |
| BMI (kg/m2) | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | 30 | 37 | 36.13 | 40 |
| CCI | NA | NA | NA | NA | NA | NA | 1 | NA | 1 | 2 | 6 | 3 | 3 | 4 | 5 |
| Secondary diseases | NA | NA | NA | Multiple | NA | NA | Rheumatoid arthritis | NA | Post-traumatic arthritis | Hemophilia, hepatitis C | Hypertension, chronic atrial fibrillation, asthma, breast cancer | Rheumatoid arthritis | Atrial fibrillation, bilateral TKA | Rheumatoid arthritis | Diabetes, stroke, tobacco use |
| Primary implantation (PI) | 1986 | 1974 | 1988 | 2002 | 2007 | NA | NA | NA | NA | NA | 2000 | 2017 | 2011 | 2012 | 2015 |
| Indication for PI | NA | Osteoarthritis | Osteoarthritis | NA | Secondary arthrosis | NA | NA | NA | NA | NA | Osteoarthritis | NA | NA | NA | Osteoarthritis |
| Year of initial PJI | 1992 | 1992 | 1994 | 2002 | 2008 | NA | NA | NA | NA | 2015 | 2016 | 2017 | 2013 | 2015 | 2018 |
| Microbe identified in PJI prior to Corynebacterium PJI | NA | NA | NA | NA | NA | NA | NA | NA | NA | Klebsiella pneumoniae, Staphylococcus aureus | - | NA | NA | E. coli, VRE, Proteus vulgaris, Serratia marcescens | NA |
| Year of initial Corynebacterium PJI | 1992 | 1992 | 1994 | 2004 | 2008 | NA | NA | NA | NA | 2016 | 2016 | 2017 | 2019 | 2018 | 2018 |
| Corynebacterium species | C. jeikeium | C. jeikeium | C. jeikeium | C. jeikeium | C. bovis | C. spp. | C. spp. | C. spp | C. spp | C. striatum | C. striatum | C. striatum | C. striatum | C. striatum | C. striatum |
| Coexisting microbe/Polymicrobial | None | None | None | CNS | None | None | NA | NA | MSSA, MRSA, CNS | Enterobacter asburiae | None | None | Mycobacterium avius | None | None |
| Onset type | Chronic onset | Chronic onset | Chronic onset | Chronic onset | Chronic onset | NA | NA | NA | NA | Chronic onset | Chronic onset | Acute onset | Chronic onset | Chronic onset | Chronic onset |
| Initial diagnosis | Tissue samples | Tissue samples | Joint aspiration | Joint aspiration | Joint aspiration | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Joint aspiration | Tissue samples | Tissue samples | Tissue samples | Tissue samples |
| CRP | NA | NA | NA | High CRP | 0.7 mg/dl | NA | NA | NA | NA | NA | 10.93 mg/dl | 24 mg/dl | 12.71 mg/dl | 17.9 mg/dl | 1.91 mg/dl |
| ESR | NA | NA | NA | High ESR | 22 mm/hr | NA | NA | NA | NA | NA | NA | 100 mm/hr | 90 mm/hr | 108 mm/hr | 100 mm/hr |
| Leading symptoms | Pain, persistent discharging sinus tract | Sinus tract | Disabling pain | Local inflammation signs | Pain, stiffness | NA | NA | NA | NA | Bloody discharge | Local signs of inflammation, pain, limited flexion | Local inflammation signs | Local inflammation signs, draining sinus tract | Sinus tract | 15-degree flexion contracture |
| Intraoperative histopathology | Acute and chronic inflammatory changes | NA | NA | Krenn and Morawitz II | Krenn and Morawitz III | No acute inflammation | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Initial surgical treatment for Corynebacterium PJI | Two-stage exchange | Two-stage exchange | Two-stage exchange | I&D, revision of the acetabular component | Two-stage exchange | None (identified during revision) | Two times I&D | Two times I&D | Two times I&D |
None, instead antibiotic treatment (due to high risk of potential bleeding); After 3 months resection |
NA | DAIR | Two-stage exchange | I&D | Two-stage exchange |
| Prosthesis reimplantation/ prosthesis in situ | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No | Yes | No | Yes |
| Total treatment for Corynebacterium PJI |
Vancomycin 42 days |
Vancomycin 42 days |
Vancomycin 35 days + Tetracycline 56 days |
Vancomycin 42 days |
Imipenem, followed by oral Amoxicillin 84 days |
Cephalexin 14 days |
Amoxicillin Duration NA |
Vancomycin Duration NA |
Vancomycin Duration NA |
Vancomycin + Imipenem + Fosfomycin 84 days |
Vancomycin + Ceftazidime 5 days; later 9 days i.v. Linezolid |
Vancomycin 42 days |
Vancomycin + Ertapenem 56 days |
Tedizolid (Vancomycin resistant organism) 56 days |
Vancomycin 42 days |
| Outcome of initial treatment | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | Reinfection without pathogen detection I&D | Periprosthetic fracture treated with open reduction and internal fixation | No clinical signs of infection | New infection due to E. asburiae Resection arthroplasty | No clinical signs of infection | Reinfection due to C. striatum Resection arthroplasty | Dislocation (subsequent infection; couned as aseptic revision) | Reinfection due to C. striatum and E. faecium I&D | No clinical signs of infection |
| Follow-up | 12 months | 12 months | 7 months | 6 months | 2.5 months | 67 months | 72 months | 204 months | 24 months | 9 months | NA | 30 months | 9 months | 14 months | 13 months |
| Perioperative complications | NA | NA | None | None | Central bone necrosis of the humerus | NA | None | None | Complex regional pain syndrome | Hematoma with bloody discharge, hemorrhagic discharge | None | None | None | None | None |
| Death by PJI | No | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| Study | Case 5 | Case 6 | Streifel et al. [24], 2022 | Tabaja et al. [25], 2022 Case 1 |
Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | Case 8 | Case 9 | Case 10 | Case 11 | Case 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country, Region | USA, Durham | USA, Durham | USA, Portland | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester |
| PJI type | Knee | Knee | Knee | Knee | Knee | Knee | Knee | Hip | Knee | Knee | Knee | Knee | Knee | Knee | Hip |
| Age (years) | 70 | 66 | 65 | 79 | 91 | 60 | 82 | 40 | 59 | 75 | 58 | 65 | 50 | 59 | 63 |
| Sex | Female | Male | Male | Male | Male | Male | Female | Female | Male | Male | Female | Female | Male | Male | Female |
| BMI (kg/m2) | 28.8 | 24.13 | NA | 25.8 | 32.2 | 32.3 | 36 | 34.6 | 62 | 36.4 | 29.8 | 37 | 21.9 | 42.4 | 20 |
| CCI | 5 | 4 | NA | 3 | 6 | 3 | 11 | 0 | 2 | 3 | 3 | 9 | 2 | 4 | 3 |
| Secondary diseases | Rheumatoid arthritis, diabetes, hypoalbuminemia | Rheumatoid arthritis, olecranon septic bursitis | NA | Coronary artery disease, chronic left lower extremity ulcer | Chronic kidney disease | Diabetes | Chronic artery disease, diabetes, congestive heart failure, chronic kidney disease, peripheral artery disease, Hodgkin-lymphoma | Teratologic hip dislocation | Congestive heart failure | Chronic artery disease | Chronic kidney disease | Liver cirrhosis, diabetes, congestive heart failure, chronic right lower extremity ulcer, chronic kidney disease | Klipperl-trenaunay syndrome, asplenia | Coronary artery disease, congestive heart failure, chronic kidney disease, chronic left lower extremity ulcer | Rheumatoid arthritis, morbus Crohn, immunosuppressive medications |
| Primary implantation (PI) | 2018 | 2015 | 1980 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Indication for PI | Osteoarthritis | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Year of initial PJI | 2018 | NA | 2008 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Microbe identified in PJI prior to Corynebacterium PJI | - | Pseudomonas aeruginosa, Staphylococcus warneri, Staphylococcus epidermidis | Stpahylococcus hominis, Dermacoccus spp. | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | MSSA | NA |
| Year of initial Corynebacterium PJI | 2018 | 2018 | 2008 | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Corynebacterium species | C. striatum | C. striatum | C. striatum | C. striatum | C. striatum | C. striatum | C. striatum | C. amycolatum | C. jeikeium | C. striatum | C. striatum | C. striatum | C. jeikeium | C. striatum | C. striatum |
| Coexisting microbe/Polymicrobial | Peptoniphilus asaccharolyticus, Prevotella bivia | None | Staphylococcus haemolyticus, Staphylococcus epidermidis | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Onset type | Acute onset | Chronic onset | Chronic onset | Chronic onset | Chronic onset | Acute onset | Chronic onset | Acute onset | Chronic onset | Chronic onset | Chronic onset | Chronic onset | Chronic onset | Chronic onset | Chronic onset |
| Initial diagnosis | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples |
| CRP | 35 mg/dl | 43.9 mg/dl | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| ESR | 116 mm/hr | 65 mm/hr | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Leading symptoms | Wound dehiscence, purulent drainage, fever | Sinus tract, non-healing wound | Persistent drainage | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Intraoperative histopathology | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Initial surgical treatment for Corynebacterium PJI | DAIR | Resection arthroplasty | I&D | DAIR | DAIR | DAIR | DAIR | DAIR | DAIR | DAIR | Two-stage exchange | Two-stage exchange | Two-stage exchange | Two-stage exchange | Two-stage exchange |
| Prosthesis reimplantation/ prosthesis in situ | No | No | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Total treatment for Corynebacterium PJI |
Vancomycin + Piperacillin-Tazobactam 14 days |
Vancomycin 42 days |
Daptomycin 33 days, Linezolid 2 days |
Doxycycline 350 days |
Amoxicillin + Minocycline 14 days |
49 days Vancomycin + 91 days minocycline |
Vancomycin 49 days |
Daptomycin 28 days |
Daptomycin + Ertapenem 42 days |
Vancomycin 42 days |
Vancomycin 42 days |
NA |
Vancomycin 42 days |
Vancomycin 42 days |
Vancomycin + Ertapenem 98 days |
| Outcome of initial treatment | Reinfection due to C. striatum Resection arthroplasty | Above knee amputation without pathogen detection | Reinfection due to C. striatum DAIR | Reinfection due to C. striatum Two-stage exchange | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | Chronic sinus tract with culture negative DAIR | No clinical signs of infection | No clinical signs of infection | Reinfection with culture negative DAIR | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection |
| Follow-up in months | 11 months | 12 months | 12 months | 12 months | 7 months | 18 months | 4 months | 23 months | 6 months | 11 months | 79 months | 24 months | 75 months | 39 months | 15 months |
| Perioperative complications | Increased left lower extremity pain and darkening of her toes | None | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
| Death by PJI | Yes | No | No | No | No | No | No | No | No | No | No | No | No | No | No |
| Study | Case 13 | Case 14 | Case 15 | Case 16 | Case 17 | Case 18 | Case 19 | Panuu et al. [26], 2022 Case 1—3 |
Case 4 | Case 5 | Case 6—7 | Case 8—10 | Case 11—14 | Case 15 | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Country, Region | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Rochester | USA, Cleveland | USA, Cleveland | USA, Cleveland | USA, Cleveland | USA, Cleveland | USA, Cleveland | USA, Cleveland | ||||||||||||||
| PJI type | Knee | Hip | Knee | Hip | Knee | Hip | Knee | Hip | Hip | Hip | Knee | Knee | Knee | Knee | ||||||||||||||
| Age (years) | 55 | 69 | 68 | 57 | 85 | 69 | 65 | NA | ||||||||||||||||||||
| Sex | Female | Male | Female | Male | Male | Female | Male | NA | ||||||||||||||||||||
| BMI (kg/m2) | 25.5 | 32 | 33.5 | 31.3 | 27.9 | 26.1 | 42.8 | NA | ||||||||||||||||||||
| CCI | 2 | NA | 3 | 5 | 7 | 7 | 3 | NA | ||||||||||||||||||||
| Secondary diseases | Rheumatoid arthritis, marfan syndrome, immunosuppressive medications | NA | Rheumatoid arthritis, Sjogren syndrome | Diabetes, chronic kidney disease, COPD, ataxia | Coronary artery disease, diabetes, colon carcinoma | Peripheral artery disease, chronic kidney disease, localized bladder carcinoma | Diabetes, chronic inflammatory demyelinating polyneuropathy, immunosuppressive medications | NA | ||||||||||||||||||||
| Primary implantation (PI) | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Indication for PI | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Year of initial PJI | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Microbe identified in PJI prior to Corynebacterium PJI | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Year of initial Corynebacterium PJI | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Corynebacterium species | C. jeikeium | C. amycolatum | C. jeikeium | C. striatum | C. striatum | C. striatum | C. striatum | C. striatum | ||||||||||||||||||||
| Coexisting microbe/Polymicrobial | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Onset type | Chronic onset | Chronic onset | Chronic onset | Chronic onset | Chronic onset | Chronic onset | Chronic onset | NA | ||||||||||||||||||||
| Initial diagnosis | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | Tissue samples | NA | ||||||||||||||||||||
| CRP | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| ESR | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Leading symptoms | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Intraoperative histopathology | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Initial surgical treatment for Corynebacterium PJI | Two-stage exchange | Two-stage exchange | Two-stage exchange | Two-stage exchange | Resection arthroplasty with spacer insertion | Resection arthroplasty with residual cerclage wires | Resection arthroplasty with spacer insertion | Two-stage exchange | Resection with spacer insertion | Girdlestone | Resection with spacer insertion | Two-stage exchange | I&D | I&D | ||||||||||||||
| Prosthesis reimplantation/ prosthesis in situ | Yes | Yes | Yes | Yes | No | No | No | Yes | No | No | No | Yes | Yes | No | ||||||||||||||
| Total treatment for Corynebacterium PJI |
Vancomycin 42 days |
Vancomycin 42 days |
daptomycin + Ertapenem 42 days |
Vancomycin 42 days |
Vancomycin 56 days |
Meropenem 56 days |
Vancomycin 42 days |
Combination of Vancomycin, Cephalosporines, Penicillin, Beta-lactam, Doxycycline, Carbapenems, Fluocinolones 81.4 ± 97.8 days |
Combination of Vancomycin, Aminoglycosides, Carbapenems, Cephalosporine, Doxycycline 50 days |
Combination of Piperacillin-Tazobactam, Vancomycin. Cephalosporines 40 days |
Combination of Vancomycin, Cephalosporines, Carbapenems, Penicillin 26.5 ± 7.8 days |
Combination of Vancomycin, Cephalosporines, Daptomycin, Penicillin, Beta-lactam, Fluconazole (1 case) 71.3 ± 70.3 days |
Combination of Vancomycin, Cephalosporines, Penicillin + Beta-lactam, Daptomycin, Doxycycline, Fluorchinolones 27 ± 32.1 days |
Combination of Daptomycin, Doxycycline, Rifampin, Ciprofloxacin, Linezolid 172 days |
||||||||||||||
| Outcome of initial treatment | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection | No clinical signs of infection |
New infection due to: Case 1: VRE, E. faecium, C. albicans I&D Case 2: Proteus mirabilis DAIR Case 3: VRE Resection arthroplasty |
New infection due to MRSA I&D |
No clinical signs of infection |
Case 6: New infection due to VRE Above knee amputation Case 7: No clinical signs of infection |
Case 8: Infection with culture negative Revision arthroplasty Case 9–10: No clinical signs of infection |
Case 11: Reinfection due to C. striatum Above knee amputation Case 12–14: No clinical signs of infection |
Reinfection due to C. striatum and Enterobacter cloacae Resection arthroplasty | ||||||||||||||
| Follow-up in months | 6 months | 67 months | 15 months | 55 months | 29 months | 54 months | 31 months | 33.7 ± 24.2 months | 17.4 months | 42.5 months | 34.9 ± 14 months | 11.7 ± 1.9 months | 41.9 ± 22.8 months | 7 months | ||||||||||||||
| Perioperative complications | NA | NA | NA | NA | NA | NA | NA | NA | ||||||||||||||||||||
| Death by PJI | No | No | No | No | No | No | No | No | No | No | No | No | No | No | ||||||||||||||
The initial diagnosis of Corynebacterium PJI was confirmed via intraoperative tissue samples in 33, and preoperative joint aspiration in 4 cases. Panuu et al. [26] did not clarify the methods used for initial diagnosis (15 cases). A polymicrobial Corynebacterium PJI was identified in 6 cases, with co-existing pathogens including Mycobacterium avius, Peptoniphilus asaccharolyticus, Prevotella bivia, Enterobacter asburiae, Staphylococcus aureus as well as multiresistant Staphylococcus aureus (MRSA) and CNS. Among 33 cases with a description of symptom onset, 29 were of chronic entity (symptoms longer than 4 weeks), whereas 4 were acute infections (shorter than 4 weeks). Mean preoperative CRP was 18.4 mg/dl (± 15.3), mean ESR was 85.88 mm/hr (± 32.5).
Surgical treatment included debridement, antibiotics and implant retention with exchange of mobile components (DAIR) in 9 joints, permanent resection arthroplasty in 10 cases, isolated irrigation and debridement (I&D) in 11 cases, and two-stage exchange in 21 patients. One Corynebacterium PJI was identified incidentally in the course of an elbow revision due to loosening, but considered PJI by the authors, as two positive intraoperative samples of Corynebacterium spp. were found.
The mean duration of antibiotic treatment was 8.5 weeks (± 8.1 weeks). The most common antibiotic groups used were Vancomycin (75%), Cephalosporines (31%), Penicillin with beta-lactam antibiotics (31%), Carbapenems (27%), and Tetracyclines (25%).
Mean follow-up was 30.1 months (± 35 months). There were 20 reoperations, including one for periprosthetic fracture requiring open reduction and internal fixation, one for dislocation treated with open reduction and head exchange, and 18 for reinfections. Mortality was low, with one patient dying from sepsis at 11 months. A total of 4 nonoperative complications occurred, including knee hematoma, chronic pain syndrome, and darkening of the toes in 3 TKAs, as well as one central humerus necrosis in case of a shoulder PJI.
Treatment for the 18 reinfections included DAIR in 4 cases, resection arthroplasty with spacer insertion in 4 cases, irrigation and debridement in 4 cases, above knee amputation in 3 cases, spacer exchange in one case, unspecified revision arthroplasty with extensor mechanism reconstruction in one case, and two-stage exchange in another case. In total, there were 7 reinfections by Corynebacterium striatum, including 2 mixed infections with Enterococcus faecium and Enterobacter cloacae, 6 reinfections by a different pathogen (Enterobacter asburiae; Enterococcus faecium and Candida albicans; Proteus mirabilis; Vancomycin Resistant Enterococcus (VRE); VRE; MRSA), and 5 culture negative cases.
The most common Corynebacterium species, Corynebacterium striatum, demonstrated a significantly higher rate of reoperations when compared to other Corynebacterium species (p = 0.035), and trended towards increased rates of reinfection (p = 0.07). The remaining baseline and surgical characteristics including age, CRP, ESR, presence of coexisting pathogens, duration of antibiotic treatment, and follow-up did not show a statistically significant difference among species (Table 2).
Table 2.
Subanalysis depending on Corynebacterium species
| Parameters | C. striatum | Other C. spp. | P-value |
|---|---|---|---|
| Joints (n) | 37 | 11 | - |
| Age in years (mean) | 70 | 59 | 0.588 |
| CRP in mg/dl (mean) | 21 | 1 | 0.127 |
| ESR in mm/hr (mean) | 97 | 22 | 0.13 |
| Coexisting pathogen (n) | 4 | 1 | 0.99 |
| Duration of total antibiotic treatment in days (mean) | 65 | 49 | 0.662 |
| Perioperative complications (n) | 2 | 1 | 0.551 |
| Follow-up in months (mean) | 24 | 21 | 0.146 |
| Reoperation (n) | 17 | 1 | 0.035 |
| Reinfection (n) | 16 | 1 | 0.070 |
Cases without specification of C. spp. were excluded for subanalysis
Discussion
Nondiphtheria Corynebacteria are widely considered an opportunistic commensal of the human skin and mucosa with little to unknown potential to cause infections [3]. As such, little attention has been paid to this bacterium in the context of PJI with a limited number of reports to date. This systematic review analyzed all existing Corynebacterium PJIs to date while including a total of 52 infections at a mean follow-up of 2.5 years. Our results demonstrated Corynebacterium PJIs to primarily affect total knee arthroplasties (60%) in old and multimorbid patients, with one in three joints developing recurrent infection at short term.
Knowledge on epidemiological characteristics is essential, as certain pathogens are known to be attributable to certain risk groups [27, 28]. Our cohort demonstrated no tendency to a certain sex, although patients were multimorbid. In fact, more than 50% of patients showed secondary diseases, with rheumatoid arthritis and diabetes mellitus being most prevalent. Moreover, the mean age of our patients was high, falling in line with previous reports on gram-positive PJIs, and representing another risk factor for PJI [29, 30]. Importantly, the knee was the most common joint affected. We believe this to be attributable to gram-positive Corynebacterium being a part of the normal skin flora, whereas gram-negative pathogens were described to more frequently affect the hip, possibly due to its proximity to the gastrointestinal tract [31].
Diagnostical work-up of Corynebacterium PJI is challenging. This is due to the fact that Corynebacterium may not be part of the standard work-up, is universal part of the human microbiome, and the identification process itself is expensive [3, 4, 32]. Our results showed most cases to be identified out of intraoperative tissue samples. As previously acknowledged, the identification of Corynebacterium spp. as commensals of the human skin and mucosa must always be considered in the context of a possible contamination before drawing a final conclusion. Importantly, only six cases were of polymicrobial nature, and CRP and ESR were significantly increased, reducing the likelihood of possible contamination.
All but 4 infections showed a chronic symptom onset. Accordingly, the majority of cases were treated without implant retentions attempts, given a high likelihood of completed biofilm formation [33]. However, not all patients were treated according to current guidelines with a substantial number of patients undergoing DAIR and/or isolated irrigation in case of chronic infections. We believe this to be associated with a multimorbid and old patient cohort being at high risk of perioperative complications in case of complete prosthesis removal and later reimplantation. In fact, Ferry et al. attempted a pure antibiotic treatment attempt given a high risk of bleeding in their patient, before deciding upon resection arthroplasty 3 months later [21].
In addition to an adequate surgical strategy, the selection of a correct antimicrobial therapy plays an essential role [34]. In our cohort, the majority of cases were treated with Vancomycin and Cephalosporines. This is important, as Corynebacterium spp., especially the jeikeium species, has shown a resistance rate of up to 60% against various groups of antimicrobials, including Aminoglycosides, Penicillin, and Cephalosporines [12]. Although no detailed resistance pattern was reported in included studies, the use of the aferomentioned antibiotics might indicate a low rate of resistance against standard antibiotics in cases of Corynebacterium PJI.
With respect to the outcome, one in three joints developed reinfection at short term. We believe this devastating outcome to be caused by a number of factors, including a substantial number of secondary diseases, an old age, as well as a number of implant retention attempts in chronic infections [35, 36]. Importantly, Corynebacterium striatum had a significantly higher rate of reinfections as opposed to other species, resulting in a failure rate of nearly 50%. While this might lead to the assumption that striatum species are a risk factor for failure in Corynebacterium PJIs, we acknowledge mean age, CRP, and ESR to be higher in this group of patients, although the effect was statistically not significant.
This systematic review had several limitations that were primarily attributable to its included studies. Foremost, we included a small number of cases with inconsistent information, resulting in a highly heterogenous group of patients. Moreover, PJI among 4 different joint types was inconsistently defined between studies, and treatment occurred over nearly 3 decades with substantially different strategies used. Finally, our results represent short-term outcomes only.
In conclusion, Corynebacterium PJI is a rare, yet severe complication occurring in the elderly and multimorbid, while resulting in significant treatment failures. One in five patients will experience Corynebacterium persistence at short term. Further studies will be necessary to draw additional conclusions on the midterm outcomes, as well as the role of the different species involved.
Acknowledgements
None.
Author contributions
Conception and design: DK, YS. Administrative support: DK. Provision of study materials or patients: DK, YS. Collection and assembly of data: DK, YS, HB, DA, SA, PK, MG. Data analysis and interpretation: DK, YS, HB, DA, SA, PK, MG. Manuscript writing: DK, YS, HB, DA, SA, PK, MG. Final approval of manuscript: DK, YS, HB, DA, SA, PK, MG.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Data availability
Does not apply.
Declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
Does not apply.
Consent to participate
Does not apply.
Consent to publish
Does not apply.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tande AJ, Patel R. Prosthetic joint infection. Clin Microbiol Rev. 2014;27(2):302–345. doi: 10.1128/CMR.00111-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Izakovicova P, Borens O, Trampuz A. Periprosthetic joint infection: current concepts and outlook. EFORT open reviews. 2019;4(7):482–494. doi: 10.1302/2058-5241.4.180092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zasada, A. A., & Mosiej, E. (2018). Contemporary microbiology and identification of Corynebacteria spp. causing infections in human. Letters in applied microbiology, 66(6), 472–483. 10.1111/lam.12883 [DOI] [PubMed]
- 4.Cazanave C, Greenwood-Quaintance KE, Hanssen AD, Patel R. Corynebacterium prosthetic joint infection. J Clin Microbiol. 2012;50(5):1518–1523. doi: 10.1128/JCM.06439-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chauvelot P, Ferry T, Tafani V, Diot A, Tasse J, Conrad A, Chidiac C, Braun E, Lustig S, Laurent F, Valour F (2021) Bone and Joint Infection Involving Corynebacterium spp.: From Clinical Features to Pathophysiological Pathways. Frontiers in medicine, 7, 539501. 10.3389/fmed.2020.539501 [DOI] [PMC free article] [PubMed]
- 6.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8 [DOI] [PubMed]
- 7.Roux V, Drancourt M, Stein A, Riegel P, Raoult D, La Scola B. Corynebacterium species isolated from bone and joint infections identified by 16S rRNA gene sequence analysis. J Clin Microbiol. 2004;42(5):2231–2233. doi: 10.1128/JCM.42.5.2231-2233.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ueda N, Oe K, Nakamura T, Tsuta K, Iida H, Saito T. Sonication of extracted implants improves microbial detection in patients with orthopedic implant-associated infections. J Arthroplasty. 2019;34(6):1189–1196. doi: 10.1016/j.arth.2019.02.020. [DOI] [PubMed] [Google Scholar]
- 9.Flurin L, Greenwood-Quaintance KE, Patel R. Microbiology of polymicrobial prosthetic joint infection. Diagn Microbiol Infect Dis. 2019;94(3):255–259. doi: 10.1016/j.diagmicrobio.2019.01.006. [DOI] [PubMed] [Google Scholar]
- 10.Achermann Y, Vogt M, Leunig M, Wüst J, Trampuz A. Improved diagnosis of periprosthetic joint infection by multiplex PCR of sonication fluid from removed implants. J Clin Microbiol. 2010;48(4):1208–1214. doi: 10.1128/JCM.00006-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wouthuyzen-Bakker M, Benito N, Soriano A. The effect of preoperative antimicrobial prophylaxis on intraoperative culture results in patients with a suspected or confirmed prosthetic joint infection: a systematic review. J Clin Microbiol. 2017;55(9):2765–2774. doi: 10.1128/JCM.00640-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rizvi M, Khan F, Raza A, Shukla I, Sabir AB. Emergence of coryneforms in osteomyelitis and orthopaedic surgical site infections. Australas Med J. 2011;4(7):412–417. doi: 10.4066/AMJ.2011.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kalt F, Schulthess B, Sidler F, Herren S, Fucentese SF, Zingg PO, Berli M, Zinkernagel AS, Zbinden R, Achermann Y. Corynebacterium species rarely cause orthopedic infections. J Clin Microbiol. 2018;56(12):e01200–e1218. doi: 10.1128/JCM.01200-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arciola CR, An YH, Campoccia D, Donati ME, Montanaro L. Etiology of implant orthopedic infections: a survey on 1027 clinical isolates. Int J Artif Organs. 2005;28(11):1091–1100. doi: 10.1177/039139880502801106. [DOI] [PubMed] [Google Scholar]
- 15.Weller TM, Smith PM, Crook DW. Corynebacterium jeikeium osteomyelitis following total hip joint replacement. J Infect. 1994;29(1):113–114. doi: 10.1016/s0163-4453(94)95438-0. [DOI] [PubMed] [Google Scholar]
- 16.Yildiz S, Yildiz HY, Cetin I, Ucar DH. Total knee arthroplasty complicated by Corynebacterium jeikeium infection. Scand J Infect Dis. 1995;27(6):635–636. doi: 10.3109/00365549509047081. [DOI] [PubMed] [Google Scholar]
- 17.Tleyjeh IM, Qutub MO, Bakleh M, Sohail MR, Virk A. Corynebacterium jeikeium prosthetic joint infection: case report and literature review. Scand J Infect Dis. 2005;37(2):151–153. [PubMed] [Google Scholar]
- 18.Achermann Y, Trampuz A, Moro F, Wüst J, Vogt M. Corynebacterium bovis shoulder prosthetic joint infection: the first reported case. Diagn Microbiol Infect Dis. 2009;64(2):213–215. doi: 10.1016/j.diagmicrobio.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 19.Wee AT, Morrey BF, Sanchez-Sotelo J (2013) The fate of elbows with unexpected positive intraoperative cultures during revision elbow arthroplasty. J Bone Joint Surg Am volume, 95(2), 109–116. 10.2106/JBJS.K.00121 [DOI] [PubMed]
- 20.Streubel PN, Simone JP, Morrey BF, Sanchez-Sotelo J, Morrey ME (2016) Infection in total elbow arthroplasty with stable components: outcomes of a staged surgical protocol with retention of the components. Bone Joint J 98-B(7): 976–983. 10.1302/0301-620X.98B7.36397 [DOI] [PubMed]
- 21.Ferry T, Desmarchelier R, Magréault S, Valour F, Lyon BJI Study group (2017). Gentamicin-vancomycin-colistin local antibiotherapy in a cement spacer in a 54-year-old haemophilic patient with relapsing plurimicrobial severe prosthetic joint infection. BMJ Case Rep 2017: bcr2017221743. 10.1136/bcr-2017-221743 [DOI] [PMC free article] [PubMed]
- 22.Fernández-Esgueva M, Pérez-Jimeno N, Roda-Rojo V, Ferrer-Cerón I (2019) Corynebacterium striatum prosthetic joint infection. Infección de prótesis de rodilla por Corynebacterium striatum. Enfermedades infecciosas y microbiologia clinica (English ed.), 37(7), 480–481. 10.1016/j.eimc.2018.05.007 [DOI] [PubMed]
- 23.Hernandez NM, Buchanan MW, Cullen MM, Crook BS, Bolognesi MP, Seidelman J, Jiranek WA. Corynebacterium total hip and knee arthroplasy prosthetic joint infections. Arthroplasty today. 2020;6(2):163–168. doi: 10.1016/j.artd.2020.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Streifel AC, Varley CD, Ham Y, Sikka MK, Lewis JS., 2nd The challenge of antibiotic selection in prosthetic joint infections due to Corynebacterium striatum: a case report. BMC Infect Dis. 2022;22(1):290. doi: 10.1186/s12879-022-07270-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tabaja H, Tai D, Beam E, Abdel MP, Tande AJ (2022) Clinical Profile of Monomicrobial Corynebacterium Hip and Knee Periprosthetic Joint Infections. Open forum infectious diseases, 9(7), ofac193. 10.1093/ofid/ofac193 [DOI] [PMC free article] [PubMed]
- 26.Pannu TS, Villa JM, Ozery M, Piuzzi NS, Higuera CA, Riesgo AM. The fate of periprosthetic joint infection with corynebacterium striatum: a rare but catastrophic causative organism. J Arthroplasty. 2022;37(1):142–149. doi: 10.1016/j.arth.2021.09.023. [DOI] [PubMed] [Google Scholar]
- 27.Riaz T, Tande AJ, Steed LL, Demos HA, Salgado CD, Osmon DR, Marculescu CE. Risk factors for fungal prosthetic joint infection. J Bone Joint Infect. 2020;5(2):76–81. doi: 10.7150/jbji.40402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Li H, Fu J, Niu E, Chai W, Xu C, Hao LB, Chen J. The risk factors of polymicrobial periprosthetic joint infection: a single-center retrospective cohort study. BMC Musculoskelet Disord. 2021;22(1):780. doi: 10.1186/s12891-021-04664-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eka A, Chen AF. Patient-related medical risk factors for periprosthetic joint infection of the hip and knee. Ann Trans Med. 2015;3(16):233. doi: 10.3978/j.issn.2305-5839.2015.09.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hsieh PH, Lee MS, Hsu KY, Chang YH, Shih HN, Ueng SW. Gram-negative prosthetic joint infections: risk factors and outcome of treatment. Clin Infect Dis . 2009;49(7):1036–1043. doi: 10.1086/605593. [DOI] [PubMed] [Google Scholar]
- 31.Aboltins CA, Dowsey MM, Buising KL, Peel TN, Daffy JR, Choong PF, Stanley PA. Gram-negative prosthetic joint infection treated with debridement, prosthesis retention and antibiotic regimens including a fluoroquinolone. Clin Microbiol Infect. 2011;17(6):862–867. doi: 10.1111/j.1469-0691.2010.03361.x. [DOI] [PubMed] [Google Scholar]
- 32.Noussair L, Salomon E, El Sayed F, Duran C, Bouchand F, Roux AL, Gaillard JL, Bauer T, Rottman M, Dinh A. Monomicrobial bone and joint infection due to Corynebacterium striatum: literature review and amoxicillin-rifampin combination as treatment perspective. Euro J Clin Microbiol Infect Dis. 2019;38(7):1269–1278. doi: 10.1007/s10096-019-03542-x. [DOI] [PubMed] [Google Scholar]
- 33.Li C, Renz N, Trampuz A. Management of periprosthetic joint infection. Hip & pelvis. 2018;30(3):138–146. doi: 10.5371/hp.2018.30.3.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Le Vavasseur B, Zeller V. Antibiotic therapy for prosthetic joint infections: an overview. Antibiotics (Basel, Switzerland) 2022;11(4):486. doi: 10.3390/antibiotics11040486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chen W, Klemt C, Smith EJ, Tirumala V, Xiong L, Kwon YM. Outcomes and risk factors associated with failures of debridement, antibiotics, and implant retention in patients with acute hematogenous periprosthetic joint infection. J Am Acad Orthop Surg. 2021;29(23):1024–1030. doi: 10.5435/JAAOS-D-20-00939. [DOI] [PubMed] [Google Scholar]
- 36.Lenguerrand E, Whitehouse MR, Beswick AD, Kunutsor SK, Burston B, Porter M, Blom AW. Risk factors associated with revision for prosthetic joint infection after hip replacement: a prospective observational cohort study. Lancet Infect Dis. 2018;18(9):1004–1014. doi: 10.1016/S1473-3099(18)30345-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Does not apply.