Abstract
Identifying genes whose expression is associated with schizophrenia (SCZ) risk by transcriptome-wide association studies (TWAS) facilitates downstream experimental studies. Here, we integrated multiple published datasets of TWAS, gene coexpression, and differential gene expression analysis to prioritize SCZ candidate genes for functional study. Convergent evidence prioritized Propionyl-CoA Carboxylase Subunit Beta (PCCB), a nuclear-encoded mitochondrial gene, as an SCZ risk gene. However, the PCCB’s contribution to SCZ risk has not been investigated before. Using dual luciferase reporter assay, we identified that SCZ-associated SNPs rs6791142 and rs35874192, two eQTL SNPs for PCCB, showed differential allelic effects on transcriptional activities. PCCB knockdown in human forebrain organoids (hFOs) followed by RNA sequencing analysis revealed dysregulation of genes enriched with multiple neuronal functions including gamma-aminobutyric acid (GABA)-ergic synapse. The metabolomic and mitochondrial function analyses confirmed the decreased GABA levels resulted from inhibited tricarboxylic acid cycle in PCCB knockdown hFOs. Multielectrode array recording analysis showed that PCCB knockdown in hFOs resulted into SCZ-related phenotypes including hyper-neuroactivities and decreased synchronization of neural network. In summary, this study utilized hFOs-based multi-omics analyses and revealed that PCCB downregulation may contribute to SCZ risk through regulating GABAergic pathways, highlighting the mitochondrial function in SCZ.
Subject terms: Stem cells in the nervous system, Molecular neuroscience, Schizophrenia
Identifying schizophrenia risk genes is essential for illuminating the disease etiology. Here, authors prioritized Propionyl-CoA Carboxylase Subunit Beta (PCCB) as a schizophrenia-associated gene, and linked PCCB to GABAergic pathways using human forebrain organoids-based transcriptomic and metabolomic analysis.
Introduction
Schizophrenia (SCZ) is a complex polygenic psychiatric disorder with risk contributed by environmental and genetic factors1. Genetic studies such as genome-wide association studies (GWAS) have identified hundreds of common single nucleotide polymorphisms (SNPs) associated with SCZ2,3. Most of the SCZ-associated SNPs are noncoding variants located in regulatory DNA elements4–6, suggesting that gene expression mediates the connection between genetic variants and SCZ phenotypes7. Identifying genes whose expression is associated with SCZ phenotypes facilitates discovering SCZ risk genes for downstream functional studies.
By integrating SCZ GWAS and brain expression quantitative trait loci (eQTL) data, several approaches, which are collectively described as transcriptome-wide association studies (TWAS) have been used to identify SCZ risk genes. These TWAS approaches, including FUSION8–10, PrediXcan11, summary-data-based Mendelian randomization (SMR)2,10,12,13, and joint-tissue imputation approach with Mendelian randomization (MR-JTI)14, aimed to identify the association between predicted gene expression and SCZ risk. Though MR-JTI could improve gene expression prediction performance in TWAS and provide a causal inference framework15, experimental validation is still needed.
Here we integrated results from MR-JTI14 and other published SCZ TWAS datasets2,8–13 to prioritize promising SCZ risk genes for functional study. Through this integrative analysis, we identified Propionyl-CoA Carboxylase Subunit Beta (PCCB), a protein-coding gene that plays important roles in mitochondrial metabolism16,17, as an SCZ risk gene with the most supporting evidence in our analysis. However, the PCCB’s contribution to SCZ risk has not been investigated before. Using human forebrain organoids (hFOs), three-dimensional cell cultures that recapitulate key aspects of the human brain18, we found that PCCB knockdown in hFOs resulted into SCZ pathology-related cellular phenotypes. We also identified that SCZ-associated common SNPs rs6791142 and rs35874192 may regulate PCCB expression, supporting that PCCB expression may mediate the genetic effects on SCZ risk.
Results
PCCB is prioritized as a promising SCZ risk gene
To obtain reliable SCZ risk genes for downstream functional study, we integrated multiple published TWAS datasets (Supplementary Data 1) to prioritize genes with sufficient supporting evidence. We also checked whether the prioritized genes are located in SCZ risk-associated gene coexpression module or dysregulated in postmortem SCZ brains. These analyses prioritized PCCB, GATAD2A, and GNL3 as the top three SCZ risk genes (Table 1). Notably, PCCB was also identified as an SCZ risk gene in the gene-based MAGMA analysis19. Moreover, PCCB was located in the gene coexpression module (M2) downregulated in SCZ based on the PsychENCODE data10. PCCB was also found to be nominally downregulated in postmortem SCZ brains (P = 0.01, FDR = 0.14) by checking the SZDB database20, which integrated transcriptome data from the CommonMind consortium21. These lines of evidence suggested that PCCB expression mediated the genetic effects on SCZ risk. Therefore, we focused on studying how PCCB contributes to SCZ risk in this study.
Table 1.
Prioritized top three SCZ risk genes
| Gene | MR-JTI | TWAS | SMR | Differential expression | Coexpression module | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| FUSION | PrediXcan | FUSION | FUSION | |||||||
| Wu et al.14 | Hall et al.9 | Huckins et al.11 | Gusev et al.8 | Gandal et al.10 | Yang et al.13 | Gandal et al.10 | Li et al.12 | Goncalves et al.19 | Gandal et al.10 | |
| PCCB | PBonferroni = 3.17E-11 | PTWAS = 5.39E-12 | P = 2.05E-08 | PTWAS = 3.07E-10 | PBonferroni = 2.42E-05 | – | PSMR = 3.74E-10 | PSMR = 4.17E-15 | ↓ P = 0.01 | ↓ FDR = 6.71E-03 |
| GATAD2A | PBonferroni = 1.87E-08 | PTWAS = 8.67E-11 | P = 2.18E-10 | PTWAS = 8.83E-07 | PBonferroni = 6.98E-09 | PSMR-multi < 1.00E-05 | PSMR = 2.21E-10 | – | – | ↑ FDR = 5.03E-03 |
| GNL3 | PBonferroni = 1.58E-18 | – | P = 1.39E-11 | PTWAS = 6.00E-07 | PBonferroni = 8.24E-03 | PSMR-multi < 1.00E-05 | PSMR = 4.71E-09 | PSMR = 4.53E-13 | – | – |
↓, Downregulation in SCZ; ↑, Upregulation in SCZ. P values are adjusted by the Benjamini-Hochberg or Bonferronid methods.
PCCB eQTL SNPs rs6791142 and rs35874192 affect transcriptional activities
Since PCCB expression is genetically associated with SCZ, we investigated the functional impacts of SCZ-associated SNPs on PCCB expression. Based on the TWAS results used in this study, we retrieved the top SNPs (rs7432375, rs7427564, rs527888, rs66691851) and their linkage disequilibrium (LD) SNPs that were associated with PCCB expression. To narrow down to the putatively causal variants, we focused on those eQTL SNPs (eSNPs) that are likely to affect PCCB expression in the brain. Since opening chromatin facilitates gene expression activation, we used brain ATAC-seq data from the PsychENCODE consortium22 to identify PCCB eSNPs located in active transcription regions. By integrating PsychENCODE ATAC-seq data and SNP annotation information from the Roadmap Epigenetics Consortium23, we prioritized six eSNPs (rs6791142, rs35874192, rs900818, rs7616204, rs570621, and rs7349597) (Table 2) that were located in genomic regions strongly suggested as enhancers or promoters in the human brain tissues or neural cell cultures.
Table 2.
Prioritized six eQTL SNPs for PCCB
| Source | References | Best GWAS SNP | LD eSNP | LD (r2) | Ref/Alt | Chromatin states (Core 15-state model) | PsychENCODE ATAC-seq Peak |
|---|---|---|---|---|---|---|---|
| MR-JTI | Wu et al., Mol. Neurobiol.14 | – | – | – | – | – | – |
| TWAS | Hall et al., Hum. Mol. Genet.9 | rs7432375 | rs6791142 | 0.81 | T/C | 7_Enh | YES |
| rs35874192 | 0.62 | G/C | 1_TssA | YES | |||
| rs900818 | 0.63 | C/T | 1_TssA, 2_TssAFlnk | YES | |||
| Huckins et al., Nat. Genet.11 | – | – | – | – | – | – | |
| Gusev et al., Nat. Genet.8 | rs7432375 | rs7616204 | 0.64 | C/T | 7_Enh | YES | |
| Gandal et al., Science10 | rs7427564 | rs6791142 | 0.73 | T/C | 7_Enh | YES | |
| SMR | Gandal et al., Science10 | rs527888 | rs570621 | 0.95 | A/G | 7_Enh | YES |
| rs7349597 | 0.69 | C/T | 1_TssA, 2_TssAFlnk, 7_Enh | YES | |||
| Li et al., Nat. Genet.12 | rs66691851 | rs7349597 | 0.6 | C/T | 1_TssA, 2_TssAFlnk, 7_Enh | YES | |
| rs570621 | 0.81 | A/G | 7_Enh | YES | |||
| rs6791142 | 0.6 | T/C | 7_Enh | YES |
1_TssA, Active transcription start site (TSS); 2_TssAFlnk, Flanking active TSS; 7_Enh, Enhancer; Ref/Alt, Reference /Alternative allele.
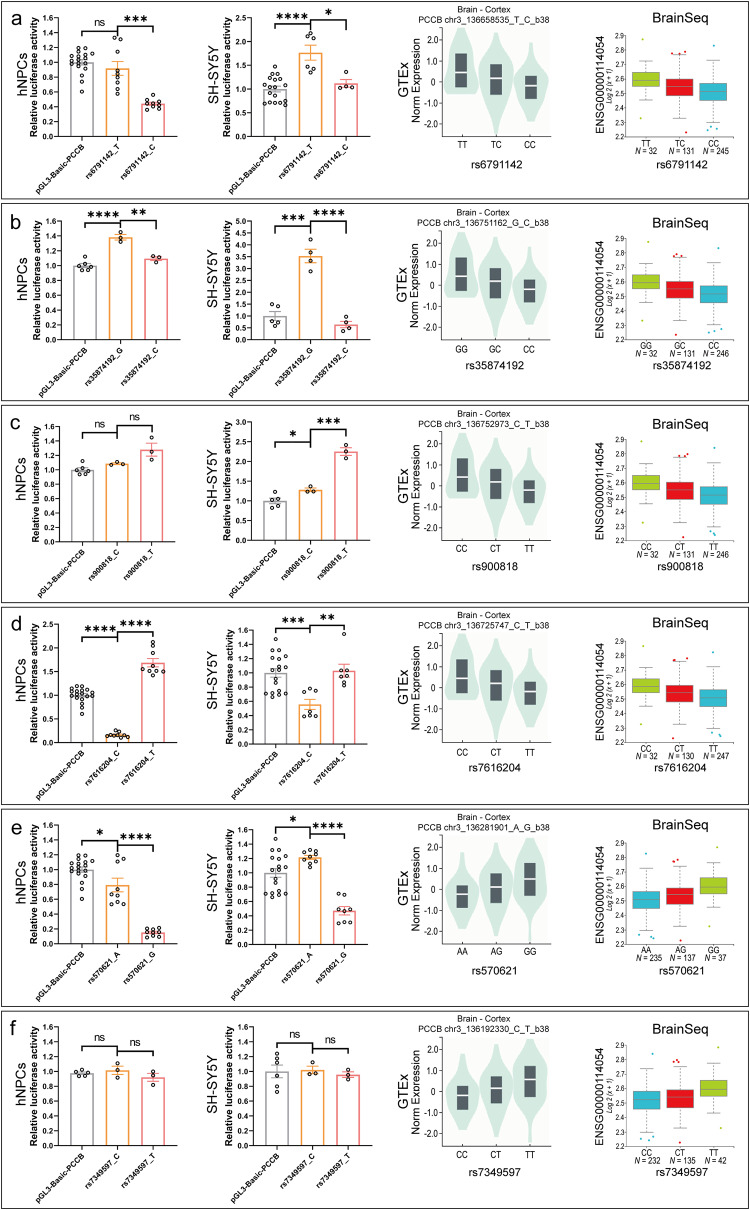
We then performed dual luciferase reporter assay (DLRA) in both human neural progenitor cells (hNPCs) and SH-SY5Y cell lines to validate the regulatory effects of the six eSNP-containing DNA elements. For each eSNP, 50 base pairs (bp) eSNP-containing DNA fragment was synthesized and cloned into the upstream of the PCCB promoter in the PGL3-basic luciferase reporter vector (Supplementary Fig. S1). In DLRA, the eSNPs rs6791142 (T/C) and rs35874192 (G/C) showed allelic effects on transcriptional activities in both hNPCs and SH-SY5Y cell lines, with SCZ-associated allele C corresponding to a lower gene expression (Fig. 1a, b). Notably, the directions of allelic effects of rs6791142 and rs35874192 were consistent with eQTL patterns detected in brain tissues from the GTEx24 and BrainSeq consortium25 (Fig. 1a, b). While the eSNPs rs900818, rs7616204, rs570621, and rs7349597 had no differential allelic effects on transcriptional activities or showed inconsistent directions of allelic effects with the eQTL patterns (Fig. 1c–f).
Fig. 1. DLRA results in hNPCs and SH-SY5Y cell lines.
a–f DLRA results for PCCB eSNPs rs6791142 (a), rs35874192 (b), rs900818 (c), rs7616204 (d), rs570621 (e), and rs7349597 (f) in hNPCs and SH-SY5Y cell lines. The PRL-TK Renilla vector was used as internal control. At least three biological replicates were used in per group. Data are shown as Mean ± SEM. Unpaired two tailed t-test was used for comparison between two groups. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001. eQTL plots in this figure were downloaded from the GTEx portal (https://www.gtexportal.org/home/) and BrainSeq phaseI eQTL data (http://eqtl.brainseq.org/phase1/eqtl/). Source data underlying a-f are provided as a Source Data file.
PCCB knockdown in hFOs affects expression of genes enriched in GABAergic synapse
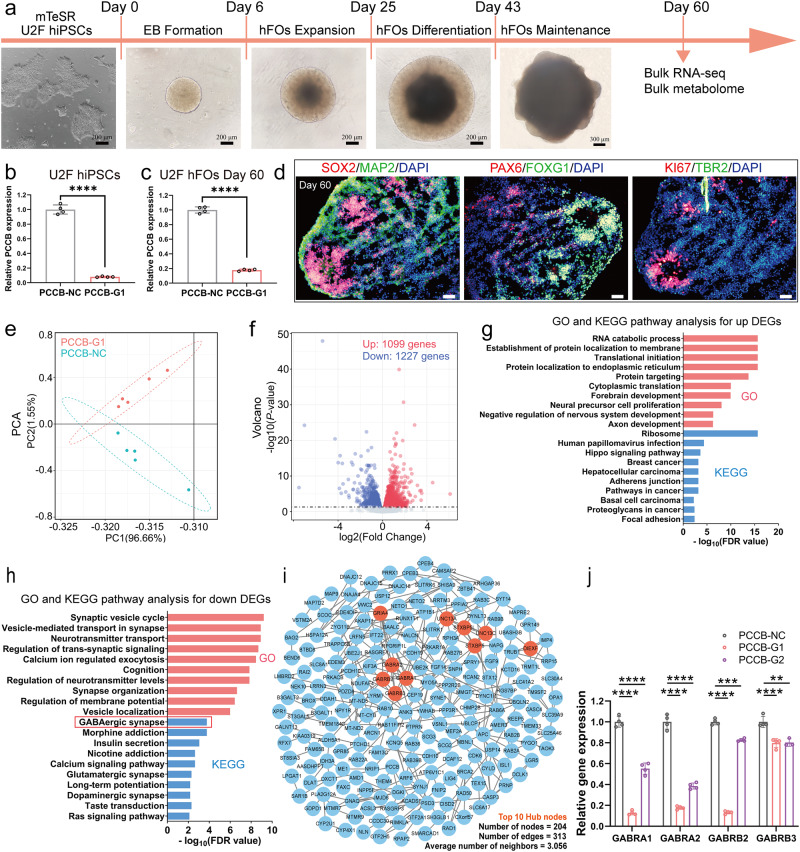
According to the TWAS and DLRA results, lower PCCB expression is associated with increased SCZ risk. We established PCCB knockdown and control human induced pluripotent stem cells (hiPSCs, U2F) using CRISPR interference (CRISPRi). In CRISPRi, one guide RNA (gRNA) sequence targeting PCCB (PCCB-G1) and one nontargeting control gRNA were designed. The established PCCB knockdown and control U2F hiPSCs were then used to generate hFOs (Fig. 2a–d) to investigate the functional impacts of PCCB knockdown. On day 60 of organoid culture, PCCB knockdown and control hFOs were used for RNA-sequencing (RNA-seq). Differential gene expression analysis identified 2326 differentially expressed genes (DEGs) [false discovery rate (FDR) < 0.05] between the PCCB knockdown and control hFOs (Supplementary Data 2). Among the 2326 DEGs, 1099 genes were upregulated and 1227 genes were downregulated in PCCB knockdown hFOs (Fig. 2e, f).
Fig. 2. Functional effects of PCCB knockdown in U2F hFOs.
a Workflow of hFOs culture in this study. Scale bar, 200 μm and 300 μm. b, c RT-qPCR analysis for PCCB expression in hiPSCs (b) and hFOs (c), n = four technical replicates per group. d Immunostaining characterization for representative control hFOs. N ≥ three biologically independent samples in each group. Cortical plate marker, MAP2; intermediate zone marker, TBR2; ventricular zone markers, SOX2 and ki67; forebrain-specific markers, FOXG1 and PAX6. Scale bar, 50 μm. e PCA plot for the PCCB knockdown and control hFOs. f Volcano plot of DEGs between the PCCB knockdown and control hFOs. Upregulated genes are shown with red dots and downregulated genes are shown with blue dots. g, h GO and KEGG analysis for the PCCB knockdown-induced upregulated (g) and downregulated DEGs (h), respectively. GO terms are shown with red bars, and KEGG pathways are shown with blue bars. i PPI network analysis for 350 downregulated DEGs shared in both PCCB-G1 and PCCB-G2 hFOs. The top 10 hub nodes are shown with orange nodes. j RT-qPCR analysis for GABRA1, GABRA2, GABRB2, and GABRB3 (The hub nodes in the PPI network), n = four technical replicates per group. Data are shown as Mean ± SD. The unpaired two-tailed t-test was used to assess difference between the PCCB-NC and PCCB-G1 or PCCB-G2 group. **P < 0.01, ***P < 0.001, ****P < 0.0001. Source data underlying b, c, and j are provided as a Source Data file.
We next used WebGestalt 201926 to annotate biological functions of the PCCB knockdown-induced DEGs. For the upregulated DEGs, Gene Ontology (GO) analysis revealed their significant enrichment in biological functions including RNA catabolic process (FDR < 2.20E-16), forebrain development (FDR = 1.11E-10), and neural precursor cell proliferation (FDR = 8.96E-09). The Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis implicated the upregulated DEGs in pathways including the ribosome (FDR < 2.20E-16) and hippo signaling (FDR = 2.43E-04) pathway (Fig. 2g and Supplementary Data 2). For the downregulated DEGs, GO analysis showed that they were enriched with neuronal functions, including synaptic vesicle cycle (FDR = 6.28E-10), neurotransmitter transport (FDR = 1.23E-09), and synapse organization (FDR = 2.27E-07). The KEGG pathway analysis implicated the downregulated DEGs in the gamma-aminobutyric acid (GABA)-ergic synapse (FDR = 1.73E-04), morphine addiction (FDR = 1.73E-04), and nicotine addiction (FDR = 2.31E-03) pathways (Fig. 2h and Supplementary Data 2). These results highlighted that reduced expression of PCCB may downregulate genes related to neuronal functions, including the GABAergic synapse.
To confirm the RNA-seq results and to minimize potential off-target effects in CRISPRi, we generated PCCB knockdown U2F hFOs using a second gRNA (PCCB-G2) and performed RNA-seq (Supplementary Fig. S2). We found that 1079 of 2326 DEGs in PCCB-G1 hFOs overlapped with those identified in PCCB-G2 hFOs. The 1079 overlapped DEGs were also enriched with neuronal functions such as synapse organization (FDR = 5.66E-04), forebrain development (FDR = 1.13E-02), and axon development (FDR = 1.51E-02) (Supplementary Fig. S2 and Supplementary Data 2). Of the 1079 overlapped DEGs, 350 genes were downregulated in both PCCB-G1 and PCCB-G2 hFOs. Using the shared 350 downregulated DEGs, we constructed a protein-protein interaction (PPI) network and found that GABA receptor genes including GABRA1, GABRA2, GABRB2, and GABRB3 were hub nodes in the PPI network (Fig. 2i). Real-time quantitative PCR (RT-qPCR) further confirmed the decreased expression of these GABA receptor genes in PCCB knockdown U2F hFOs (Fig. 2j). These results further highlighted that PCCB knockdown may affect the GABAergic pathways.
PCCB knockdown-induced DEGs in hFOs are enriched with SCZ-related genes
To explore PCCB’s connection to SCZ, we evaluated the enrichment of 1079 PCCB knockdown-induced DEGs in hFOs with SCZ-related gene sets. The first SCZ gene set was 4096 differentially expressed protein-coding genes between postmortem brains of 559 SCZ patients and 936 controls from the PsychENCODE consortium10. The second SCZ gene set was 2809 DEGs between cerebral organoids (6 months) derived from eight SCZ patients and eight controls from the Kathuria et al. study27 (Supplementary Data 2). We found that the 1079 PCCB knockdown-induced DEGs were significantly overlapped with genes dysregulated in PsychENCODE SCZ brains (Overlapped genes = 282, P = 5.84E-04) and SCZ patient-derived cerebral organoids (Overlapped genes = 255, P = 1.92E-14) (Supplementary Fig. S3a). We also found that the 1079 PCCB knockdown-induced DEGs were significantly (Padjust = 7.09E-03) overlapped with genes reported in SCZ GWAS from the FUMA analysis28 (Supplementary Fig. S3b). Interestingly, the overlapped SCZ-related genes included sveral GABAergic synapse-related genes such as GABRA1, GABRA2, GABRB2, and GABRB3 (Supplementary Data 2). These results suggested that PCCB may function through affecting the expression of SCZ-related genes, including the GABAergic synapse-related genes.
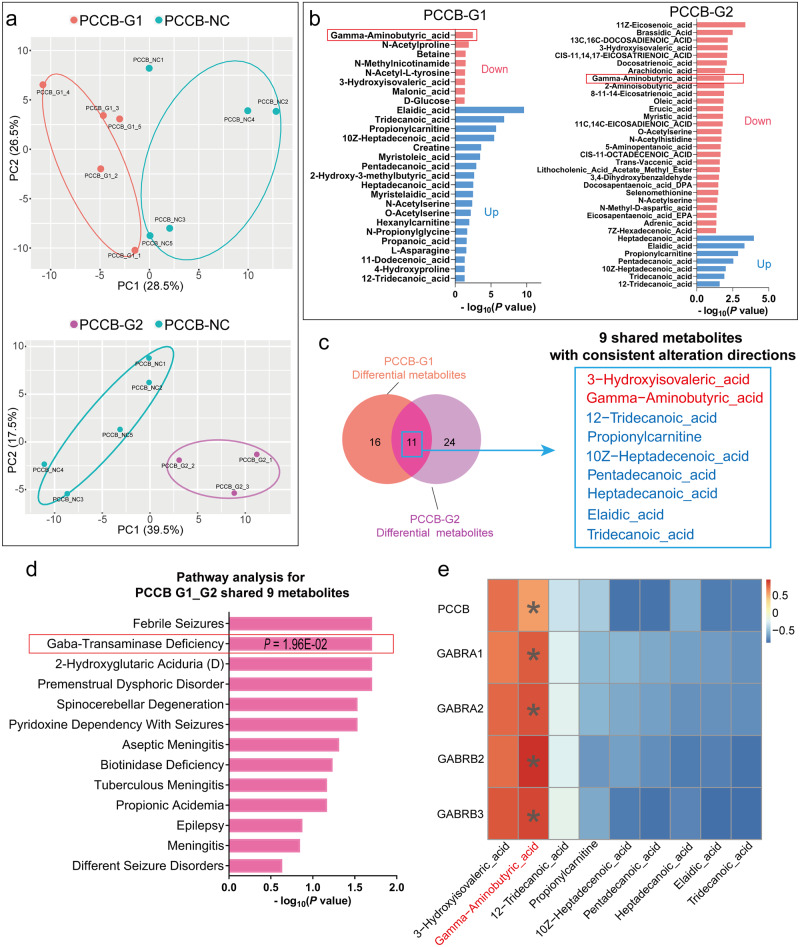
Metabolomic analysis confirms the decreased GABA levels in PCCB knockdown hFOs
RNA-seq analysis revealed the effects of PCCB knockdown on GABAergic synapse, we further used metabolomic analysis to examine whether PCCB knockdown decreased GABA levels in hFOs. Of the 178 detected metabolites in U2F hFOs (day 60), 27 and 35 metabolites were differentially expressed in PCCB-G1 and PCCB-G2 hFOs (Fig. 3a–c and Supplementary Data 3), respectively. A total of 11 differential metabolites were shared in both groups with 9 metabolites showing consistent alteration directions (Fig. 3c). The 9 shared differential metabolites were enriched in pathways including febrile seizures (P = 1.96E-02), GABA-transaminase deficiency (P = 1.96E-02), and spinocerebellar degeneration (P = 2.93E-02) (Fig. 3d). Notably, GABA levels were decreased in both PCCB-G1 (decreased by 59%, P = 3.42E-03) and PCCB-G2 hFOs (decreased by 22%, P = 1.31E-02) when compared with control hFOs (Supplementary Data 3). The Pearson correlation analysis between the 9 shared differential metabolites and PCCB knockdown-induced DEGs further confirmed a positive correlation (r = 0.51, P = 0.03) between PCCB expression and GABA. Notably, GABA showed strong positive correlations (r > 0.73, P < 5.50E-04) with GABA receptor genes GABRA1, GABRA2, GABRB2 and GABRB3, respectively (Fig. 3e and Supplementary Data 3).
Fig. 3. Metabolomic analysis after PCCB knockdown in U2F hFOs.
a PCA plot for the metabolomic analysis in U2F hFOs. N ≥ three biologically independent samples in each group. b Metabolomic analysis identified 27 and 35 differentially expressed metabolites in PCCB-G1 and PCCB-G2 hFOs, respectively. GABA (indicated by red box) was downregulated in both groups. c Overlap for differential metabolites identified in PCCB-G1 and PCCB-G2 hFOs. d Functional annotation for 9 shared differential metabolites with consistent alteration directions in PCCB-G1 and PCCB-G2 hFOs. P values were calculated by the hypergeometric test. e Pearson correlation analysis between PCCB knockdown-induced DEGs and differential metabolites. The unpaired two-tailed t-test was used to calculated the P value. *P < 0.05. Their correlation coefficients are indicated by the color bar.
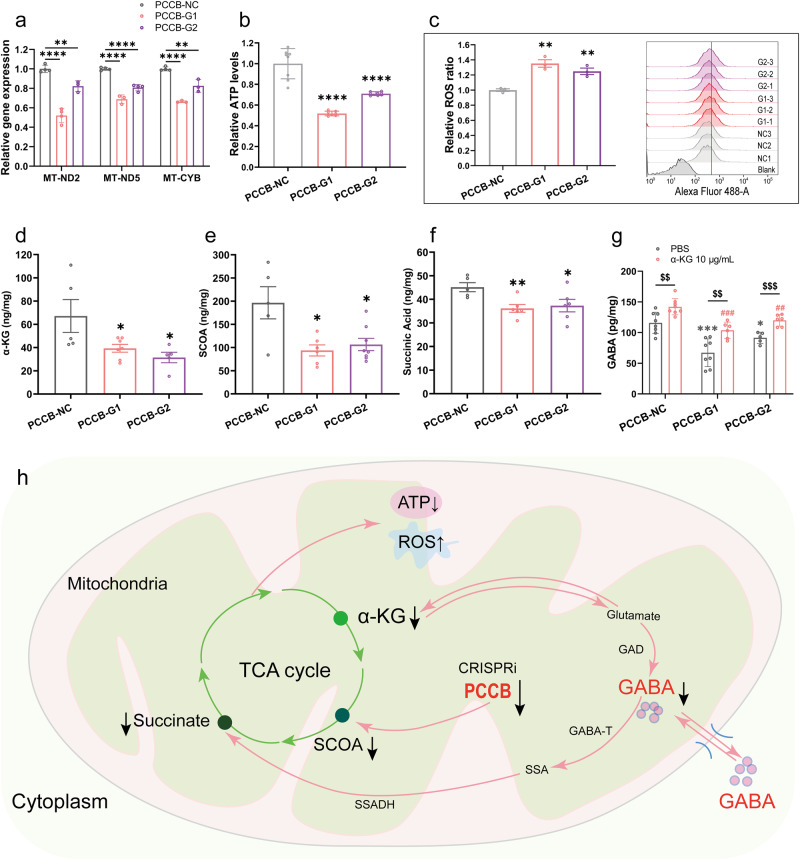
PCCB knockdown in hFOs leads to mitochondrial dysfunction and reduction of GABA levels
PCCB encodes the β subunit of the propionyl-CoA carboxylase, a mitochondrial enzyme involved in the catabolism of propionyl-CoA29. PCCB mutation has been reported to impair mitochondrial energy metabolism by disrupting the tricarboxylic acid (TCA) cycle16. We would expect mitochondrial dysfunction caused by PCCB knockdown. Indeed, we found several mitochondrial genes that function in cellular oxidative phosphorylation, including MT-ND2, MT-ND5, and MT-CYB, were downregulated in both PCCB-G1 and PCCB-G2 U2F hFOs (Supplementary Data 2), which was further validated by the RT-qPCR analysis (Fig. 4a). Adenosine triphosphate (ATP) and reactive oxygen species (ROS) detection assays showed that PCCB knockdown reduced ATP generation and increased ROS levels in U2F hFOs (Fig. 4b, c), indicating the mitochondrial dysfunction caused by PCCB knockdown.
Fig. 4. PCCB knockdown leads to mitochondrial dysfunction and decreased GABA levels in U2F hFOs.
a RT-qPCR analysis revealed downregulated expression of mitochondrial genes in PCCB knockdown hFOs. b, c Decreased ATP (b) and increased ROS contents (c) were observed in PCCB knockdown hFOs. d, e, f ELISA analysis validated the reduction of α-KG (d), SOCA (e), and succinic acid (f) in PCCB knockdown hFOs. g Adding α-KG (10 μg/mL) into the culture medium of PCCB knockdown hFOs restored the GABA levels. h Potential pathways involved in the regulation of PCCB knockdown on GABA synthesis. GAD, glutamate decarboxylase; GABA-T, GABA transaminase; SSA, Succinic semialdehyde; SSADH, succinic semialdehyde dehydrogenase; ↓, downregulation; ↑, upregulation. N ≥ three biologically independent samples in each group. Data are shown as Mean ± SEM. The unpaired two-tailed t-test was used to assess difference between the PCCB-NC and PCCB-G1 or PCCB-G2 group. *P < 0.05, **P < 0.01, ***P < 0.001, ****P < 0.0001, ##P < 0.01, ###P < 0.001, $$P < 0.01, $$$P < 0.001. Source data underlying a-g are provided as a Source Data file.
Since GABA metabolism involves a route from α-ketoglutarate (α-KG) generated by the TCA cycle to succinate via glutamate, GABA, and succinic semialdehyde30,31, we examined whether PCCB knockdown decreased GABA levels by inhibiting the TCA cycle. We performed enzyme linked immunosorbent assay (ELISA) and confirmed that PCCB knockdown decreased α-KG, succinyl-CoA (SCOA), and succinic acid (Fig. 4d–f), three key metabolites that connect the GABA shunt and TCA cycle30,31. Considering that α-KG is an upstream metabolite that could be converted to GABA, we added α-KG (10 μg/mL) into culture media of U2F hFOs and found a restored GABA levels in PCCB knockdown hFOs (Fig. 4g).
To confirm the functional impacts of PCCB knockdown observed in U2F hFOs, we generated hFOs using another hiPSC line (U1M) (Supplementary Fig. S4a, b). The RT-qPCR and mitochondrial functional analyses showed that PCCB knockdown in U1M hFOs also resulted into decreased expression of mitochondrial genes (MT-ND2, MT-ND5 and MT-CYB), reduced ATP generation and increased ROS levels (Supplementary Fig. S4c-e). The ELISA showed that PCCB knockdown decreased α-KG, SCOA, succinic acid, and GABA levels in U1M hFOs (Supplementary Fig. S4f-i). Adding α-KG (10 μg/mL) into culture media of U1M hFOs restored the GABA levels (Supplementary Fig. S4i) as detected in U2F hFOs. These results indicated that PCCB knockdown decreased GABA levels by inhibiting the TCA cycle and led to mitochondrial dysfunction (Fig. 4h).
PCCB knockdown in hFOs leads to abnormal electrophysiological activities
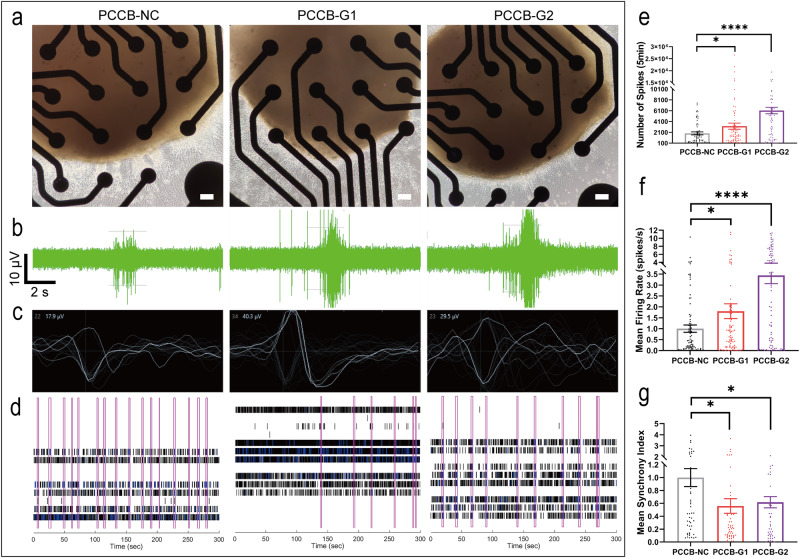
Since GABA, the major inhibitory neurotransmitter in the brain32, was decreased in PCCB knockdown hFOs, we used multielectrode array (MEA) recording assay to test whether PCCB knockdown affected neuroactivities. The PCCB knockdown and control U2F hFOs at day 160 were seeded on Matrigel-coated 24-well MEA plate (Fig. 5a). After 7 days of culture, electroactivities of hFOs were recorded (Fig. 5b–d). We found that PCCB knockdown in hFOs led to increased number of spikes (Fig. 5e) and mean neuron firing rate (Fig. 5f), suggesting a hyper neuroactivity after PCCB knockdown in U2F hFOs. However, PCCB knockdown decreased the synchronization of the neural network (Fig. 5g). These MEA results were further replicated in U1M hFOs (Supplementary Fig. S5). Since hyper neuroactivity and decreased synchronization of neural network in SCZ brains have been reported by the electroencephalography and magnetoencephalography33, these results supported that PCCB knockdown led to abnormal electrophysiological activities that link to SCZ phenotypes.
Fig. 5. MEA assay after PCCB knockdown in U2F hFOs.
a Bright field of hFOs cultured in 24-well MEA plate. Scale bar, 100 μm. b Representative burst traces for individual electrode recorded from hFOs. c Schematic diagram of a single unit event. d Raster plot of neural network activity. Each pink box represents a synchronized burst. e–g PCCB knockdown increased the number of spikes (e) and mean neuron firing rate (f) but reduced the synchronized burst index in hFOs (g). N ≥ 13 biologically independent samples in each group. Data are shown as Mean ± SEM. The unpaired two-tailed t-test was used to assess difference between the PCCB-NC and PCCB-G1 or PCCB-G2 group. *P < 0.05, ****P < 0.0001. Source data underlying e-g are provided as a Source Data file.
Discussion
SCZ is a polygenic psychiatric disorder with risk contributed by multiple genes. Identifying genes whose expression is associated with SCZ risk by TWAS is a powerful approach to prioritize SCZ risk genes. By integrating multiple published datasets from TWAS, gene coexpression, and differential gene expression analysis, we prioritized PCCB as a reliable SCZ risk gene. PCCB is a gene encoding β subunit of propionyl-coA carboxylase enzyme29, defect of which has been reported as a cause of propionic acidemia34. Though several case reports have shown neuropathological symptoms including autistic features35 in propionic acidemia36,37, how PCCB deficiency led to neuropathology is largely unknown. Moreover, what roles PCCB plays in the etiology of SCZ has not been investigated.
To investigate PCCB’s contribution to SCZ risk, we performed RNA-seq analysis and identified that PCCB knockdown in U2F hFOs downregulated expression of genes related to multiple neuronal functions including the GABAergic synapse pathway. Several GABA receptor genes including GABRA1, GABRA2, GABRB2, and GABRB3 were highlighted as hub genes in the PCCB’s regulatory network (Fig. 2i). To confirm these results, we generated PCCB knockdown hFOs using two other hiPSC lines (U1M and ACS-1011) (Supplementary Fig. S6a, b). The RT-qPCR analysis confirmed that PCCB knockdown also led to decreased expression of GABRA1, GABRA2, GABRB2, and GABRB3 in both U1M and ACS-1011 hFOs (Supplementary Fig. S6c, d).
The downregulated GABAergic synapse pathway caused by PCCB knockdown attracted our attention, since GABAergic dysfunction plays important roles in SCZ etiology38,39. To validate the GABA findings in this study, we used immunostaining assay and confirmed the existence of cells expressing the GABAergic markers GAD1 (GAD67) and DLX2 in hFOs (Supplementary Fig. S7). We further performed metabolomic analysis and confirmed the decreased GABA levels in PCCB knockdown hFOs. The following electrophysiological analysis showed that PCCB knockdown in both U1M and U2F led to hyper neuroactivity and decreased synchronization of neural network activities, cellular phenotypes reported to be associated with SCZ risk33,40. Through the hFOs-based multiomics analyses, we revealed the functional impacts of PCCB knockdown and highlighted that PCCB dysregulation may contribute to SCZ etiology through regulating the GABAergic pathways.
Since the GABA shunt connected the GABA metabolism pathway and TCA cycle30,31, we expected that PCCB regulates GABAergic pathways by affecting the TCA cycle. As expected, PCCB knockdown led to reduced production of α-KG, SCOA, and succinic acid in the TCA cycle. Since α-KG produced from the TCA cycle could be converted into SCOA or serve as a source for GABA synthesis41, the decrease of α-KG may be responsible for the reduced production of GABA. On the other hand, PCCB knockdown leads to the reduction of SCOA and succinic acid, which may exacerbate the entry of GABA into the TCA cycle through GABA shunt pathway and further reduce GABA content in the cytoplasm41. Overall, PCCB knockdown decreased GABA levels by reducing the content of α-KG, SCOA and succinic acid in the TCA cycle (Fig. 4h). Our study highlighted that mitochondrial dysfunction caused by PCCB knockdown not only impaired cellular energy production, but also resulted into GABAergic dysfunction. Since mitochondrial dysfunction is associated with GABAergic dysfunction42 and the etiology of SCZ43,44, our study connected the “mitochondrial hypothesis” and “GABA hypothesis” of SCZ.
In addition to mitochondrial dysfunction, one of the major effects of PCCB defect is the cellular accumulation of propanoic acid, propionyl carnitine, and other metabolites16. Indeed, we did observe a dramatic increase of propanoic acid or propionyl carnitine in PCCB knockdown hFOs (Supplementary Data 3). Interestingly, hFOs exposed to propanoic acid at 3.2 μM, an average serum concentration in SCZ patients45, led to decreased expression of GABA receptor genes (GABRA1, GABRA2, GABRB2, and GABRB3) (Supplementary Fig. S8), which is consistent with those observed in PCCB knockdown hFOs. These results suggested that the accumulation of propanoic acid may mediate the effects of PCCB knockdown, and partially explain how propionic acidemia could lead to neuropathological symptoms. These results also suggested the potential effects of short-chain fatty acids on SCZ risk, since short-chain fatty acids including propanoic acid, acetic acid, and butyric acid were found to be upregulated in the serum of SCZ patients46.
This study reveals the connection between PCCB and SCZ risk, some limitations also exist. First, PCCB knockdown affects multiple types of synapses, including GABAergic, glutamatergic, dopaminergic, and cholinergic synape, as revealed by bulk RNA-seq analysis. The cell-type specific effects of PCCB knockdown is unclear. Further investigations such as RNA-seq and other omics analysis at single-cell level are needed. Second, hFOs (day 60) are immature in this study since the average proportion of GAD67+ or DLX2+ GABAergic neurons only account for about 5% of the total cells in hFOs (Supplementary Fig. S7). A long-term organoid culture could allow hFOs develop further to generate abundant GABAergic neurons to validate the GABA findings. Last, we showed that SCZ-associated SNPs rs6791142 and rs35874192, two eQTL SNPs for PCCB, affected transcriptional activities. But whether these two eSNPs could affect PCCB expression in vivo remains unclear. In the future, using CRISPR-Cas9 gene editing to confirm the regulatory effects of eSNPs rs6791142 and rs35874192 on PCCB expression is needed.
In summary, this study used hFOs-based multiomics analyses and revealed connection between PCCB and SCZ, highlighting that PCCB may contribute to SCZ etiology through regulating the GABAergic pathways and mitochondrial function.
Methods
Prioritization of SCZ risk genes and SNPs
We collected the published data from TWAS8–11, MR-JTI15, and SMR2,10,12,13 analyses to prioritize SCZ risk genes with sufficient supporting evidence. We also checked whether the prioritized genes are located in SCZ risk-associated gene coexpression modules or differentially expressed in postmortem brains of SCZ patients.
To prioritize SCZ risk SNPs, we first collected the top SNPs from the TWAS data. We then retrieved SNPs in LD (r2 ≥ 0.6, European population genome) with the top SNPs. We prioritized candidate causal SNPs that likely affected gene expression in the brain using the following criteria: 1) candidate SNPs are eSNPs for the SCZ risk genes in the brain based on the BrainSeq25, GTEx24, or PsychENCODE eQTL data47; 2) SNPs are located within chromatin open regions based on ATAC-seq data from the PsychENCODE consortium; 3) SNPs are located in genomic regions predicted as enhancers or promoters in human brain tissues or neural cell cultures based on the Roadmap Epigenomics data23.
Cell culture
Three hiPSC lines (U1M, U2F, and ACS-1011) used in this study were derived from healthy individuals. The U1M and U2F hiPSCs were obtained from the Cellapy Technology (Beijing, China), and the ACS-1011 cell line was obtained from the American type culture collection. Pluripotency and karyotype of hiPSCs were confirmed by immunofluorescence and karyotype analysis as shown in our previous studies48,49. The hiPSCs were cultured in Matrigel (Corning, 354277)-coated plate and supplemented with the mTeSR Plus medium (STEMCELL Technologies, 05825) and 1% penicillin/streptomycin (Gibco, 10378016).
hNPCs were induced from U2F hiPSCs using the STEMdiff™ Neural Induction Medium (STEMCELL Technologies, 05835) as described in our previous study48. In brief, hiPSCs were dissociated into single cells using Accutase solution (Sigma-Aldrich, A6964) on day 0. Cells were then cultured in Matrigel-coated12-well plate and fed with 600 μL Neural Induction Medium supplemented with 1x penicillin/streptomycin and 10 μM Y27632 (Selleck, SCM075). On day 3, each well was fed with 600 μL fresh Neural Induction Medium without Y27632. From day 18, the hNPCs were cultured and maintained in the STEMdiff™ Neural Progenitor Medium (STEMCELL Technologies, 05833). The culture medium was completely replaced with fresh medium every two days.
The SH-SY5Y neuroblastoma cells were cultured in high-glucose DMEM (Gibco, C11995500BT) supplemented with 10% fetal bovine serum (Gibco, A3161001C) and 1% penicillin/streptomycin.
DLRA
About 50 bp DNA sequence (Supplementary Data 4) flanking the PCCB eSNP was synthesized and cloned into the pGL3-basic vector using the restriction enzymes KpnI and XhoI (New England BioLabs). The PCCB promoter sequence (~600 bp) was amplified from the genomic DNA using the PCR primers (F, 5′-CCGCTCGAGTTTGAATCCTGGCCAACCAC-3′; R, 5′-CCC AAGCTTTGCTAAAGCGTGGGTACGG-3′) and Phanta®Max Super-fidelity DNA Polymerase (Vazyme, P505-d1). The amplified PCCB promoter was then cloned into downstream of the eSNP-containing DNA fragment using the restriction enzymes XhoI and Hind III (New England BioLabs). DLRA was performed in both hNPCs and SH-SY5Y cells. For DLRA, 1 × 105 cells per well were plated into 24-well plate. After 24 hours of culture, 500 ng recombinant pGL3-basic luciferase reporter vector and 20 ng PRL-TK Renilla internal control vector for each well were co-transfected into cells using Lipofectamine™ 3000 (Invitrogen, L3000015). 36 h post transfection, the Firefly and Renilla luciferase activities were measured on the LumiPro luminescence detector (Lu-2021-C001) using the DLRA kit (Vazyme, DL101-01). Experiments were conducted in at least three biological replicates.
Establishment of PCCB knockdown and control hiPSCs
We used CRISPRi to establish PCCB knockdown and control hiPSCs. Two gRNA sequences targeting PCCB (PCCB-G1, 5′-GCATTACGGGTGGCGGCGGT-3′; PCCB-G2, 5′-GCGTACTCAGGTGCGCCGGT-3′) were designed using the online tool CRISPR-ERA (http://crispr-era.stanford.edu/). The PCCB-targeting gRNA or control gRNA sequence (5′-GCGCCAAACGTGCCCTGACGG-3′)50 were synthesized and cloned into the lentiviral vector pLV-hU6-sgRNA-hUbC-dCas9-KRAB-T2a-Puro. The constructed vectors were then used for lentiviral package (ObiO Technoliges, China). For viral infection in hiPSCs, when cell confluence reached 40–50% in 12-well plate, cells were cultured in 0.6 mL medium and incubated with the lentiviruses for 24 h. The culture medium was fully replaced in the next day. 48 h post viral infection, cells were treated with 0.5–1 µg/mL puromycin for 3–7 days to kill cells that were not infected by the lentiviruses. PCCB knockdown efficiency was confirmed by RT-qPCR analysis.
RT-qPCR analysis
Total RNA was used to generate complementary DNA using HiScript III RT SuperMix for qPCR (+gDNA wiper) (Vazyme, R323-01). RT-qPCR assay was performed using ChamQ SYBR qPCR Master Mix (Vazyme, Q711-02) on the Real-Time PCR System (Roche, LightCycler 480 II). GAPDH was used as the internal reference gene. At least three technical replicates were used in the RT-qPCR analysis. RT-qPCR primers are provided in Supplementary Data 4.
Generation of hFOs
The established PCCB knockdown and control hiPSCs were used to generate hFOs using the STEMdiff Dorsal Forebrain Organoid Differentiation Kit (STEMCELL Technologies, 08620) based on the manufacturer’s instructions with some modifications. Briefly, hiPSCs were dissociated into single cells using Accutase solution (Sigma-Aldrich, A6964) on day 0. 1 × 104 cells per well were then plated into 96-well round-bottom ultra-low attachment plate (Corning, 7007) and fed with 50 μL Forebrain Organoid Formation Medium supplemented with 1x penicillin/streptomycin and 10 μM Y27632 (Selleck, SCM075). On day 3, each well was gently added with 50 μL fresh Forebrain Organoid Formation Medium without Y27632. On day 6, the medium was replaced with the Forebrain Organoid Expansion Medium. On day 25, the Forebrain Organoid Expansion Medium was replaced with the Forebrain Organoid Differentiation Medium. From day 43, organoids were cultured in the Forebrain Organoid Maintenance Medium. hFOs were characterized using immunostaining analysis.
Immunostaining analysis
hFOs were sectioned at a thickness of 16 μm. hFOs sections were treated with 1% Triton X-100 for 30 mins. After washing with PBS three times, hFOs sections were blocked with 5% bovine serum albumin (Solarbio, A8020) for 1 h at 37 °C. The hFOs sections were then incubated with primary antibodies overnight at 4 °C. After washing with PBS three times, hFOs sections were incubated with secondary antibodies for 1 h and DAPI (10 μg/ml Invitrogen, D1306) for 5 mins at room temperature. Primary antibodies used in this study were mouse anti-Ki67 (1:1,000, Cell Signaling Technologies, 9449), rabbit anti-FOXG1 (1:100, Abcam, ab18259), rabbit anti-TBR2 (1:800, Cell Signaling Technologies, 81493), mouse anti-SOX2 (1:200, Invitrogen, MA1-014), rabbit anti-PAX6 (1:100, Proteintech, 12323-1-AP), rabbit anti-MAP2 (1:200, Proteintech, 17490-1-AP), mouse anti-GAD67 (1:200, Abcam, ab26116) and mouse anti-DlX2 (1:200, Santa cruz, sc-393879). The secondary antibodies were Alexa Fluor 594-conjugated goat anti-mouse IgG (1:300, Abcam, ab150116), Alexa Fluor 594-conjugated goat anti-rabbit IgG (1:200, Invitrogen, A-11012), Alexa Fluor 488-conjugated goat anti-rabbit (1:200, Invitrogen, A-11008), goat anti-mouse Cy3 (1:200, BOSTER, BA1031) and goat anti-mouse CoraLite488 (1:200, Proteintech, SA00013-1). All antibodies used in this study were also shown in Supplementary Data 4.
Bulk organoid RNA-seq and data analysis
Two hFOs from PCCB knockdown or control group were randomly selected and pooled together as one mixed sample. Five mixed samples in each group were used for total RNA extraction using the miRNeasy Mini Kit (Qiagen, 217004). RNA quality was evaluated on the Agilent 2100 Bioanalyzer system. RNA samples with RNA integrity numbers over 7 were used for RNA-seq (150 bp, paired-end) on the Illumina NovaSeq 6000 system.
Raw RNA-seq data were filtered to get clean reads using FastQC (v0.20.0). The clean reads were aligned to the human genome hg38 using STAR (v2.7.9a). Gene expression quantification was conducted using RSEM (v1.3.0) based on Gencode v40 comprehensive gene annotation. The filterByExpr function in the edgeR package (v3.36.0) was used to filter out low-expression genes. The sva function in the SVA package (v3.42.0) was used to estimate batch effect and other artifacts. Differential gene expression analysis between the PCCB knockdown and control group was performed using the DEseq2 package (v1.34.0). P values were adjusted using the Benjamini–Hochberg method. To annotate the functions of DEGs, we used the online tool WebGestalt2019 (http://www.webgestalt.org/) to perform GO and KEGG pathway enrichment analysis.
PPI analysis
The STRING database (v11.5) (http://www.string-db.org/) was used to construct a high-confidence (interaction score > 0.7) PPI network for the PCCB knockdown-induced DEGs. Active interaction sources included text-mining, experiments, databases, coexpression, neighborhood, gene fusion, and co-occurrence. The PPI network was visualized using Cytoscape (v 3.9.1). CytoHubba51, a Cytoscape plugin, was used to explore hub nodes in the PPI network.
Metabolomic analysis of bulk hFOs
For metabolomic analysis, three hFOs (day 60) in PCCB knockdown or control group were randomly selected and pooled together as one mixed sample. At least three mixed samples in each group were then used for HM400 metabolomic analysis (Beijing Genomics Institute, China). Briefly, hFOs or quality control samples were lysed in 140 μL 50% water/methanol solution. The lysate was centrifuged (18,000 g, 4 °C, 20 min) to get the supernatant. The supernatant was used for derivatization reaction and then centrifuged at 4000 g, 4 °C, 10 min. The supernatant was further used for high performance liquid chromatography tandem mass spectrometer (LC-MS/MS) analysis on the SCIEX QTRAP 6500 + LC-MS/MS system. Parameters of liquid chromatographic column were BEH C18 (2.1 mm×10 cm, 1.7 μm, Waters). The parameter of mass spectrometry was ESI + /ESI-. Content of metabolites (μmol/g) was quantified using the HMQuant software based on the formula (C*0.14/m), where C represents the calculated concentration (μmol/L) and m represents the sample weight (mg). Two-tailed t-test was used to identify differential metabolites between PCCB knockdown and control hFOs. Functional annotation for the differentially expressed metabolites was performed using the online tool MetaboAnalyst 5.0 (https://www.metaboanalyst.ca/).
ATP assay
The ATP Assay Kit (Beyotime, S0026) was used to examine the effects of PCCB knockdown on ATP production in hFOs. At day 60, PCCB knockdown or control hFOs were washed twice with PBS and lysed with 200 µL lysis buffer per well. The lysate was centrifuged at 12,000 g for 5 min at 4 °C. The supernatant was used to measure ATP content on the LumiPro luminescence detector (Lu-2021-C001). Experiments were conducted in at least three biological replicates.
ROS assay
The ROS Assay Kit (Beyotime, S0033S) was used to measure ROS levels in PCCB knockdown and control hFOs. Briefly, hFOs (day 60, three hFOs were randomly pooled together as one mixed sample) were dissociated into single cells using Accutase. After centrifuging at 1500 rpm for 5 min, cells were resuspended with prewarmed serum-free DMEM-F12 medium. The collected cells were incubated with 10 µM DCFH-DA fluorescent probes in serum-free DMEM-F12 for 20-30 min at 37 °C, 5% CO2. 1 × 104 cells were analyzed on the flow cytometry (BD FACSAria II). Experiments were conducted in at least four biological replicates.
ELISA assay
The ELISA kits (CAMILO, Nanjing, China) were used to measure SOCA (Cat No. 2H-KMLJh315292), succinic Acid (Cat No. 2H-KMLJh313077), α-KG (Cat No. 2H-KMLJh313735) and GABA (Cat No. 2H-KMLJh310295) levels in PCCB knockdown and control hFOs according to the manufacturer’s instructions. Briefly, protein was extracted from hFOs (day 60, two hFOs were randomly pooled together as one mixed sample) using RIPA buffer (Beyotime, P0013B) containing 1% protease inhibitor. The lysate was centrifuged at 12,000 g for 10 min at 4 °C. Protein concentration was determined using the BCA protein assay kit (Vazyme, E112-01). The supernatant was used to detect SCOA, succinic Acid, α-KG and GABA. We also used ELISA to determine the GABA levels in PCCB knockdown hFOs after incubating the hFOs with 10 μg/mL exogenous α-KG52 for 3 h at 37 °C, 5% CO2. Experiments were conducted in at least four biological replicates.
MEA assay
We used an MEA assay to evaluate the effects of PCCB knockdown on electrophysiological properties in hFOs. Briefly, hFOs were cultured in the Matrigel-coated 24-well MEA plate with one organoid seeded in each well. After 7 days of culture, electro activities were recorded using the Axion Biosystems for 7 days. Each recording duration was 5 min. The MEA data including the number of spikes, burst frequency, and network synchronization were analyzed using the software Axis Navigator 3.6.2.2.
Statistical analysis
Data were analyzed with GraphPad Prism 9.0.0 and shown as Mean ± SEM. A two-tailed t-test was used to assess the difference between two groups. The hypergeometric test was used to assess the enrichment of PCCB knockdown-induced DEGs with SCZ-related gene sets. P values in the differential gene expression analysis were adjusted for multiple testing using the Benjamini–Hochberg method. For all statistical analyses, a P value less than 0.05 is considered statistically significant.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Source data
Acknowledgements
This work was supported by grants from the National Natural Science Foundation of China (Nos. 82171504, 82022024, 31970572, and 81901359), the Natural Science Foundation of Hunan Province (No. 2022JJ20035), the Science and Technology Innovation Program of Hunan Province (2022RC1214), the Innovation-Driven Project of Central South University (No. 2020CX003), and the National Institute of Health (No. 1U01MH116489). ATAC-seq data were generated as part of the PsychENCODE Consortium (U01MH103392, U01MH103365, U01MH103346, U01MH103340, U01MH103339, R21MH109956, R21MH105881, R21MH105853, R21MH103877, R21MH102791, R01MH111721, R01MH110928, R01MH110927, R01MH110926, R01MH110921, R01MH110920, R01MH110905, R01MH109715, R01MH109677, R01MH105898, R01MH105898, R01MH094714, and P50MH106934).
Author contributions
Q.M., C.C., and C.L. supervised the overall study, as well as guided the procedures and analyses. Q.M. and W.Z. wrote the manuscript. W.Z. did the CRISPRi experiment and organoid culture, as well as the mitochondrial function assay, ELISA, and MEA assay. M.Z. and H.Y. performed the differential gene expression analysis. Z.X., and H.W. performed the metabolomic and RT-qPCR analysis. B.T., C.C., C.L., J.J., and J.W. revised the manuscript.
Peer review
Peer review information
Nature Communications thanks Matthew Girgenti and the other, anonymous, reviewers for their contribution to the peer review of this work. A peer review file is available.
Data availability
RNA-seq data generated in this study have been deposited in the Gene Expression Omnibus under accession code GSE226233. Because the raw data of the MEA and metabolomic data are huge and presented in highly diverse nature and formats, these raw data are available on request from the corresponding authors. All the other data associated with this study are shown in the manuscript, Supplementary Information, and Source Data file. Source data are provided with this paper. Public database: STRING (https://cn.string-db.org/), WebGestalt (https://www.webgestalt.org/option.php), MetaboAnalyst 5.0 (https://www.metaboanalyst.ca/). Source data are provided with this paper.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Chunyu Liu, Email: liuch@upstate.edu.
Chao Chen, Email: chenchao@sklmg.edu.cn.
Qingtuan Meng, Email: mengqingtuan@glmc.edu.cn.
Supplementary information
The online version contains supplementary material available at 10.1038/s41467-023-40861-2.
References
- 1.Hilker R, et al. Heritability of Schizophrenia and Schizophrenia Spectrum Based on the Nationwide Danish Twin Register. Biol. Psychiatry. 2018;83:492–498. doi: 10.1016/j.biopsych.2017.08.017. [DOI] [PubMed] [Google Scholar]
- 2.Trubetskoy V, et al. Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature. 2022;604:502–508. doi: 10.1038/s41586-022-04434-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schizophrenia Working Group of the Psychiatric Genomics C. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–427. doi: 10.1038/nature13595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maurano MT, et al. Systematic Localization of Common Disease-Associated Variation in Regulatory DNA. Science. 2012;337:1190. doi: 10.1126/science.1222794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Degner JF, et al. DNaseI sensitivity QTLs are a major determinant of human expression variation. Nature. 2012;482:390–394. doi: 10.1038/nature10808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huo Y, Li S, Liu J, Li X, Luo XJ. Functional genomics reveal gene regulatory mechanisms underlying schizophrenia risk. Nat. Commun. 2019;10:670. doi: 10.1038/s41467-019-08666-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boyle EA, Li YI, Pritchard JK. An Expanded View of Complex Traits: From Polygenic to Omnigenic. Cell. 2017;169:1177–1186. doi: 10.1016/j.cell.2017.05.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gusev A, et al. Transcriptome-wide association study of schizophrenia and chromatin activity yields mechanistic disease insights. Nat. Genet. 2018;50:538–548. doi: 10.1038/s41588-018-0092-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hall LS, et al. A transcriptome-wide association study implicates specific pre- and post-synaptic abnormalities in schizophrenia. Hum. Mol. Genet. 2020;29:159–167. doi: 10.1093/hmg/ddz253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gandal MJ, et al. Transcriptome-wide isoform-level dysregulation in ASD, schizophrenia, and bipolar disorder. Science. 2018;362:eaat8127. doi: 10.1126/science.aat8127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huckins LM, et al. Gene expression imputation across multiple brain regions provides insights into schizophrenia risk. Nat. Genet. 2019;51:659–674. doi: 10.1038/s41588-019-0364-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li Z, et al. Genome-wide association analysis identifies 30 new susceptibility loci for schizophrenia. Nat. Genet. 2017;49:1576–1583. doi: 10.1038/ng.3973. [DOI] [PubMed] [Google Scholar]
- 13.Yang Z, et al. The genome-wide risk alleles for psychiatric disorders at 3p21.1 show convergent effects on mRNA expression, cognitive function, and mushroom dendritic spine. Mol. Psychiatry. 2020;25:48–66. doi: 10.1038/s41380-019-0592-0. [DOI] [PubMed] [Google Scholar]
- 14.Wu Y, Yu XL, Xiao X, Li M, Li Y. Joint-Tissue Integrative Analysis Identified Hundreds of Schizophrenia Risk Genes. Mol. Neurobiol. 2022;59:107–116. doi: 10.1007/s12035-021-02572-x. [DOI] [PubMed] [Google Scholar]
- 15.Zhou D, et al. A unified framework for joint-tissue transcriptome-wide association and Mendelian randomization analysis. Nat. Genet. 2020;52:1239–1246. doi: 10.1038/s41588-020-0706-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chapman KA, et al. Propionyl-CoA carboxylase pcca-1 and pccb-1 gene deletions in Caenorhabditis elegans globally impair mitochondrial energy metabolism. J. Inherit. Metab. Dis. 2018;41:157–168. doi: 10.1007/s10545-017-0111-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stathopoulos S, et al. DNA Methylation Associated with Mitochondrial Dysfunction in a South African Autism Spectrum Disorder Cohort. Autism Res. 2020;13:1079–1093. doi: 10.1002/aur.2310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lancaster MA, et al. Cerebral organoids model human brain development and microcephaly. Nature. 2013;501:373–379. doi: 10.1038/nature12517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goncalves VF, et al. A Comprehensive Analysis of Nuclear-Encoded Mitochondrial Genes in Schizophrenia. Biol. Psychiatry. 2018;83:780–789. doi: 10.1016/j.biopsych.2018.02.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu Y, Yao YG, Luo XJ. SZDB: A Database for Schizophrenia Genetic Research. Schizophr. Bull. 2017;43:459–471. doi: 10.1093/schbul/sbw102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fromer M, et al. Gene expression elucidates functional impact of polygenic risk for schizophrenia. Nat. Neurosci. 2016;19:1442–1453. doi: 10.1038/nn.4399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Psych EC, et al. The PsychENCODE project. Nat. Neurosci. 2015;18:1707–1712. doi: 10.1038/nn.4156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kundaje A, et al. Integrative analysis of 111 reference human epigenomes. Nature. 2015;518:317–330. doi: 10.1038/nature14248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Consortium GT. The GTEx Consortium atlas of genetic regulatory effects across human tissues. Science. 2020;369:1318–1330. doi: 10.1126/science.aaz1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jaffe AE, et al. Developmental and genetic regulation of the human cortex transcriptome illuminate schizophrenia pathogenesis. Nat. Neurosci. 2018;21:1117–1125. doi: 10.1038/s41593-018-0197-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liao Y, Wang J, Jaehnig EJ, Shi Z, Zhang B. WebGestalt 2019: gene set analysis toolkit with revamped UIs and APIs. Nucleic Acids Res. 2019;47:W199–W205. doi: 10.1093/nar/gkz401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kathuria A, et al. Transcriptomic Landscape and Functional Characterization of Induced Pluripotent Stem Cell-Derived Cerebral Organoids in Schizophrenia. JAMA Psychiatry. 2020;77:745–754. doi: 10.1001/jamapsychiatry.2020.0196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Watanabe K, Taskesen E, van Bochoven A, Posthuma D. Functional mapping and annotation of genetic associations with FUMA. Nat. Commun. 2017;8:1826. doi: 10.1038/s41467-017-01261-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jiang H, Rao KS, Yee VC, Kraus JP. Characterization of four variant forms of human propionyl-CoA carboxylase expressed in Escherichia coli. J. Biol. Chem. 2005;280:27719–27727. doi: 10.1074/jbc.M413281200. [DOI] [PubMed] [Google Scholar]
- 30.Morland C, et al. Propionate enters GABAergic neurons, inhibits GABA transaminase, causes GABA accumulation and lethargy in a model of propionic acidemia. Biochem. J. 2018;475:749–758. doi: 10.1042/BCJ20170814. [DOI] [PubMed] [Google Scholar]
- 31.Kim K, Yoon H. Gamma-Aminobutyric Acid Signaling in Damage Response, Metabolism, and Disease. Int. J. Mol. Sci. 2023;24:4584. doi: 10.3390/ijms24054584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCormick DA. GABA as an inhibitory neurotransmitter in human cerebral cortex. J. Neurophysiol. 1989;62:1018–1027. doi: 10.1152/jn.1989.62.5.1018. [DOI] [PubMed] [Google Scholar]
- 33.Uhlhaas PJ, Singer W. Abnormal neural oscillations and synchrony in schizophrenia. Nat. Rev. Neurosci. 2010;11:100–113. doi: 10.1038/nrn2774. [DOI] [PubMed] [Google Scholar]
- 34.Ugarte M, et al. Overview of mutations in the PCCA and PCCB genes causing propionic acidemia. Hum. Mutat. 1999;14:275–282. doi: 10.1002/(SICI)1098-1004(199910)14:4<275::AID-HUMU1>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 35.Witters P, et al. Autism in patients with propionic acidemia. Mol. Genet. Metab. 2016;119:317–321. doi: 10.1016/j.ymgme.2016.10.009. [DOI] [PubMed] [Google Scholar]
- 36.Schreiber J, et al. Neurologic considerations in propionic acidemia. Mol. Genet. Metab. 2012;105:10–15. doi: 10.1016/j.ymgme.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 37.Cao LX, et al. Neuropathological report of propionic acidemia. Neuropathology. 2022;43:143–150. doi: 10.1111/neup.12861. [DOI] [PubMed] [Google Scholar]
- 38.Jahangir M, Zhou JS, Lang B, Wang XP. GABAergic System Dysfunction and Challenges in Schizophrenia Research. Front. Cell Dev. Biol. 2021;9:663854. doi: 10.3389/fcell.2021.663854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marques TR, et al. GABA-A receptor differences in schizophrenia: a positron emission tomography study using [(11)C]Ro154513. Mol. Psychiatry. 2021;26:2616–2625. doi: 10.1038/s41380-020-0711-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schmidt MJ, Mirnics K. Neurodevelopment, GABA system dysfunction, and schizophrenia. Neuropsychopharmacology. 2015;40:190–206. doi: 10.1038/npp.2014.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bown AW, Shelp BJ. Does the GABA Shunt Regulate Cytosolic GABA? Trend Plant. Sci. 2020;25:422–424. doi: 10.1016/j.tplants.2020.03.001. [DOI] [PubMed] [Google Scholar]
- 42.Kanellopoulos AK, et al. Aralar Sequesters GABA into Hyperactive Mitochondria, Causing Social Behavior Deficits. Cell. 2020;180:1178–1197 e1120. doi: 10.1016/j.cell.2020.02.044. [DOI] [PubMed] [Google Scholar]
- 43.Oraki Kohshour M, et al. Association between mitochondria-related genes and cognitive performance in the PsyCourse Study. J. Affect. Disord. 2023;325:1–6. doi: 10.1016/j.jad.2023.01.013. [DOI] [PubMed] [Google Scholar]
- 44.Li J, et al. Mitochondrial deficits in human iPSC-derived neurons from patients with 22q11.2 deletion syndrome and schizophrenia. Transl. Psychiatry. 2019;9:302. doi: 10.1038/s41398-019-0643-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li X, et al. The effect of serum lipids and short-chain fatty acids on cognitive functioning in drug-naive, first episode schizophrenia patients. Psychiatry Res. 2022;313:114582. doi: 10.1016/j.psychres.2022.114582. [DOI] [PubMed] [Google Scholar]
- 46.Zhu, F. et al. Role of short-chain fatty acids in the gut-brain axis in schizophrenia: contribution to immune activation and pathophysiology in humans and mice. bioRxiv, 2020.2004.2011.021915 (2020). https://www.biorxiv.org/content/10.1101/2020.04.11.021915v1.
- 47.Wang D, et al. Comprehensive functional genomic resource and integrative model for the human brain. Science. 2018;362:eaat8464. doi: 10.1126/science.aat8464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Meng Q, et al. Integrative analyses prioritize GNL3 as a risk gene for bipolar disorder. Mol. Psychiatry. 2020;25:2672–2684. doi: 10.1038/s41380-020-00866-5. [DOI] [PubMed] [Google Scholar]
- 49.Meng Q, et al. Human forebrain organoids reveal connections between valproic acid exposure and autism risk. Transl. Psychiatry. 2022;12:130. doi: 10.1038/s41398-022-01898-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gilbert LA, et al. Genome-Scale CRISPR-Mediated Control of Gene Repression and Activation. Cell. 2014;159:647–661. doi: 10.1016/j.cell.2014.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chin CH, et al. cytoHubba: identifying hub objects and sub-networks from complex interactome. BMC Syst. Biol. 2014;8:S11. doi: 10.1186/1752-0509-8-S4-S11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Glaros T, et al. Discovery of treatment for nerve agents targeting a new metabolic pathway. Arch. Toxicol. 2020;94:3249–3264. doi: 10.1007/s00204-020-02820-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
RNA-seq data generated in this study have been deposited in the Gene Expression Omnibus under accession code GSE226233. Because the raw data of the MEA and metabolomic data are huge and presented in highly diverse nature and formats, these raw data are available on request from the corresponding authors. All the other data associated with this study are shown in the manuscript, Supplementary Information, and Source Data file. Source data are provided with this paper. Public database: STRING (https://cn.string-db.org/), WebGestalt (https://www.webgestalt.org/option.php), MetaboAnalyst 5.0 (https://www.metaboanalyst.ca/). Source data are provided with this paper.