Abstract
Evidence shows a growing trend of the HIV epidemic in the Middle East and North Africa (MENA). We aimed to project the incidence, mortality, and disability-adjusted life years (DALY) in the region from 1990 to 2019 and assess its trend by 2025, and 2030. We extracted the HIV incidence, mortality, and DALY data from the Global Burden of Disease (GBD) and UNAIDS databases. The joinpoint regression model was used to examine changes in HIV trends. The trend changes were estimated by average annual percent change (AAPC). In most countries, an increasing trend was observed in HIV incidence, mortality, and DALY. Specifically, the highest growth in the annual incidence rate was related to Egypt (AAPC = 14.4, GBD) and Iran (AAPC = 9.6, UNAIDS). Notably, Qatar (AAPC = − 5.6, GBD), Bahrain (AAPC = − 3.3, GBD), and Somalia (AAPC = − 4.2, UNAIDS) demonstrated a significant reduction in incidence. Regarding mortality rates, Djibouti (AAPC = 24.2, GBD) and Iran (AAPC = 16.2, UNAIDS) exhibited a significant increasing pattern. Furthermore, the estimated increase in incidence by 2030 was most marked in Djibouti (985%) and Iran (174%). Iran (422%) and Egypt (339%) showed a prominent rise in mortality rates. GBD data showed 16 countries had an increasing pattern in DALY in both genders. According to age and period effects, there was a significant upward trend in incidence, mortality rates, and DALY. Findings highlighted the urgent need for improved prevention and treatment services, including expanding access to HIV testing, promoting safe practices, increasing antiretroviral therapy coverage, and supporting targeted interventions for high-risk populations.
Subject terms: Infectious diseases, HIV infections, Statistics
Introduction
Worldwide, HIV continues to be a significant public health concern and has destructive health outcomes1. Reports globally show that in 2020, 37.7 million people were living with HIV, 1.5 million people became newly infected with HIV, and 680,000 people died due to AIDS-related consequences2. With the promising effectiveness of antiretroviral therapy (ART) to treat the infection and prevent transmission and worldwide efforts to implement treatment and prevention programs, UNAIDS declared the intention to end AIDS as a public health threat by 2030. In this regard, UNAIDS developed strategies for enhancing HIV response among societies to achieve 90% coverage for HIV testing, treatment, and sustained viral suppression by 2020 and 95% coverage by 20303. However, the burden of the epidemic continues to vary substantially between countries and regions, and there remains limited information about trends and projections of the incidence and mortality of HIV in some regions.
There are some barriers to the control of HIV in the Middle East and North Africa (MENA) including stigma and discrimination around key populations, internal wars, terrorism, and political problems4. These barriers lead to the region being one of the only world regions with rapidly rising HIV cases, making it a substantial area of concern within the global HIV landscape5. For example, this region, with 43% antiretroviral therapy coverage, has the lowest antiretroviral therapy coverage across all world regions6. Moreover, the HIV epidemic in some countries of the region among HIV key populations, including female sex workers (FSWs), People who inject drugs (PWID), and men who have sex with men (MSM) is concentrated5. While HIV epidemics have emerged over the past 20 years among these key populations in the region, evidence suggests that HIV incidence appears to have increased in the region since 20107. For example, a recent modelling study estimated that the number of new HIV infections in 2020 in the MENA was 3471 in FSWs, 6416 in their clients, and 4717 in the client spouses7. Another study estimated the HIV incidence rate in 2017 among PWID overall ranges widely from 0.7% per person-year in Tunisia and 7.8% per person-year in Pakistan to as high as 24.8% per person-year in Libya8. Among MSM, HIV prevalence was found to vary from 3.6% in Lebanon to 9.3% in Sudan, and the highest measured prevalence was 13.0% in Tunisia9. Despite the rapidly rising HIV epidemic and the fact that the HIV response in the MENA remains below global targets for prevention, testing, and treatment, the status of HIV incidence and mortality and their trends remains unknown. Notably, no model assessed the distribution trends of incidence, mortality, and disability-adjusted life years (DALY) of HIV in the region.
Utilizing joinpoint regression analysis can provide crucial insights into the dynamic changes over time, identify significant shifts in trends, and shed light on the evolving HIV epidemic in the MENA region. The joinpoint model does not have requirements for the distribution of data and can describe the long-term trend in a linear model. The basic idea is to divide a long-term linear trend into several segments, each of which is described by a continuous linear pattern10. However, to the best of our knowledge, no previous studies have comprehensively evaluated and quantified the trend of HIV incidence, mortality rates, and DALY within the MENA region. To address this evidence gap and consider the escalating HIV epidemic in the MENA region, this study aimed to analyze the trend changes and region distribution changes of HIV incidence and mortality between 1990 and 2019 using a joinpoint regression analysis. Additionally, the study sought to estimate the changes in incidence, mortality, and DALY by 2025 and 2030 in the MENA region. The findings of this study can inform strategies for enhancing access to HIV prevention and treatment services in the MENA. Moreover, the findings can provide a scientific basis for the governments to improve HIV prevention and control measures in the region.
Methods
Study design and data collection
In this ecological study, two sources of data from 21 countries, including Algeria, Bahrain, Djibouti, Egypt, Iran, Iraq, Jordan, Kuwait, Lebanon, Libya, Morocco, Oman, Palestine, Qatar, Saudi Arabia, Somalia, Sudan, Syria, Tunisia, United Arab Emirates (UAE), and Yemen were used. The first source of data was age-standardized incidence, mortality rates (ASRs), and disability-Adjusted Life Years (DALY) of HIV in 21 countries from the Global Burden of Disease (GBD) site, owned by the Institute for Health Metrics and Evaluation (IHME), University of Washington11. The second source of data was the data reported in 14 countries by UNAIDS, which was extracted from the official UNAIDS website12.
GBD provides comprehensive data on various health indicators, including incidence, prevalence, death (Years of life lost: YLLs), Years Lived with Disability (YLDs), and DALY for each disease and injury in each year, location, age group, and sex estimates and reports for 204 countries from 1990 to 2019. UNAIDS maintains a nationwide database of AIDS information reports, including estimates of HIV prevalence, incidence, mortality, and DALY associated with AIDS. The majority of these estimates are generated using Spectrum software13.
Informed consent was not applicable. Ethical approval was obtained from the Ethics Committee of Kerman University of Medical Sciences (Ethics Code: IR.KMU.REC.1401.263) and all methods were performed under the relevant guidelines and regulations.
Statistical analysis
Joinpoint regression was used to analyse the time trend and identify significant changes in the incidence, mortality rate, and DALY of HIV from 1990 to 201914. The joinpoint regression model is a method of segmenting the nonlinear regression model into separate linear fragments in which the fragments are separated by joinpoints. We performed a logarithmic transformation of the ASRs and computed the standard errors adopting binomial approximation. Annual Percent Change (APC) indicate the amount of increase or decrease in the percentage of change per year, which shows a decreasing trend if negative, an increasing trend if positive, and the Average Annual Percent Change (AAPC) is the average all these changes, which are calculated to describe linear trends based on each period.
To determine the number and locations of breakpoints and estimate the regression parameters of the components, Joinpoint regression software version 4.9.0.1 was used, which is specifically designed to perform connection point regression analysis. This software uses 4499 repetitions of the permutation test to estimate the failure points by default, in which the number of failure points was considered to be a maximum of four. The significance level of the tests was considered less than or equal to 0.05.
Prediction model
We estimated the percent change in incidence, mortality, and DALY by 2025 and 2030 when compared to the final segment (trend 5), and compute the standard errors of the projection, using the betas displayed on the APC in the final segment15,16.
Age–period–cohort analysis
We described the magnitude of the rates as a function of age (a), period (p), and birth cohort (c) using a log-linear model, with Poisson distribution and with the log of the person-years at risk defined as an offset of the method. Age-period-cohort model analyses were conducted using APC fit with the APC package in R, version 3.6.017.
Sensitivity analysis
The sensitivity analysis was performed in four steps. First, starting with the selection data as below:
Data from 1993 to 2013 were used to predict HIV incidence in 2014.
Data from 1994 to 2014 were used to predict HIV incidence in 2015.
Data from 1995 to 2015 were used to predict HIV incidence in 2016.
Data from 1996 to 2016 were used to predict HIV incidence in 2017.
Data from 1997 to 2017 were used to predict HIV incidence in 2018.
Second, we fitted the Joinpoint Regression model for each of the datasets.
Third, we estimated the prediction in incidence, mortality, and DALY using the betas displayed on the APC in the final segment.
To measure the accuracy of the prediction counts, the prediction error is estimated for each year by computing the predicted minus the observed value. We then find the ratio of the prediction error to the observed count, adding 0.5 to the denominator to avoid numerical error when the observed count is zero. The ratio is the percentage error of the prediction, compared to the observed count:
Fourth, the average absolute relative deviation (AARD) was computed as the average of the error ratios over all the cases considered in the data. More specifically, assume is the predicted mortality for specific scenario s, s = 1,…, S, and that is the true observed count.
Smaller values in AARD indicate closer estimates to the true values15,16.
The results of the prediction model of the incidence rate of Algeria country between 1993 and 2019 were shown in Supplementary Tables S1 and S2.
Ethics approval
Ethical approval was obtained (IR.KMU.REC.1401.263) from the Ethics Committee of Kerman University of Medical Sciences.
Results
Age-standardized incidence rate trend
According to the GBD database, out of the 21 countries analyzed, 14 countries had an increase in incidence, two countries showed a declining trend, and five countries reported stable trends from 1990 to 2019. According to the GBD database, Iran had the highest annual growth rate in HIV incidence (AAPC = 9.6, 95% CI 8.8, 10.5; P<0.001), and Morocco had the lowest annual growth rate (AAPC = 1.4, 95% CI 0.6, 2.2; P < 0.001). Qatar (AAPC = − 5.6, 95% CI − 6.1, − 5.0; P < 0.001) and Bahrain (AAPC = − 3.3, 95% CI − 4.3, − 2.3; P < 0.001) had the age-standardized incidence rate between 1990 and 2019 (Table 1 and Fig. 1). Furthermore, the results of modelling with UNAIDS data showed that the incidence of HIV has decreased annually in Somalia (AAPC = − 4.2, 95% CI − 4.9, − 3.5; P < 0.001), Djibouti (AAPC = − 2.0, 95% CI − 3.9, − 0.0; P = 0.049), and Morocco (AAPC = − 0.7, 95% CI − 1.0, − 0.3; P < 0.001). The highest annual growth rate was related to Egypt (AAPC = 14.4, 95% CI = 14.1, 14.8; P < 0.001), and the lowest annual growth rate was related to Lebanon (AAPC = 1.9, 95% CI 1.6, 2.1; P < 0.001) (Table 1).
Table 1.
Joinpoint regression analysis of age-standardized incidence rates, and incidence rates from HIV in MENA countries, 1990–2019.
| Country | Trend 1 | Trend 2 | Trend 3 | Trend 4 | Trend 5 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | |
| Age-standardized incidence rates (GBD database) | ||||||||||
| Algeria | 1990–2000 | 10.1* (9.7, 10.5) | 2001–2006 | 5.3* (4, 6.6) | 2007–2012 | 1.9* (0.7, 3.2) | 2013–2015 | −10.4* (−15.2, −5.3) | 2016–2019 | −0.6 (−3.2, 2.2) |
| Bahrain | 1990–1992 | −1.6 (−5.8, 2.8) | 1993–2001 | −6.2* (−7, −5.3) | 2002–2004 | −9.2* (−16.8, −1) | 2005–2019 | −0.5* (−0.9, −0.1) | – | – |
| Djibouti | 1990–1991 | 132.1* (120.2, 144.6) | 1992–1994 | 63.5* (55.2, 72.4) | 1995–1997 | 7.6* (2.1, 13.4) | 1998–2002 | −14* (−15.4, −12.5) | 2003–2019 | −5.7* (−5.9, −5.6) |
| Egypt | 1990–1999 | −3.5* (−3.8, −3.3) | 2000–2009 | 4.8* (4.5, 5.1) | 2010–2014 | 9 * (7.9, 10.2) | 2015–2019 | 4.1* (3.1, 5.2) | – | – |
| Iran | 1990–1992 | 0.9 (−3.3, 5.3) | 1993–1998 | 25.7* (23.3, 28.1) | 1999–2006 | 2.9* (1.8, 4.1) | 2007–2014 | 12.5* (11.3, 13.8) | 2015–2019 | 2.2 (−0.5, 5) |
| Iraq | 1990–1993 | 7.3* (5.9, 8.8) | 1994–1998 | 16* (14.4, 17.5) | 1999–2008 | 1.8* (1.4, 2.2) | 2009–2014 | 4.6* (3.6, 5.6) | 2015–2019 | 0.6 (−0.8, 1.9) |
| Jordan | 1990–1999 | 9.6* (9.1, 10.1) | 2000–2009 | 1.9* (1.4, 2.4) | 2010–2012 | −10.2* (−15, −5.2) | 2013–2019 | 1.9* (1, 2.9) | – | – |
| Kuwait | 1990–1992 | −8.7 (−17.8, 1.4) | 1993–2000 | 3.3* (0.5, 6.3) | 2001–2006 | −8.9* (−13.1, −4.5) | 2007–2019 | 1 (− 0.2, 2.3) | – | – |
| Lebanon | 1990–1999 | −4* (−4.6, −3.5) | 2000–2002 | 1.1 (−6.2, 9.1) | 2003–2008 | −4.5* (−6.1, −2.9) | 2009–2019 | 4.3* (3.7, 4.9) | – | – |
| Libya | 1990–1992 | 6.1* (3.3, 9) | 1993–1999 | 12.5* (11.4, 13.5) | 2000–2008 | −1.1* (−1.7, −0.6) | 2009–2014 | 6.4* (5.1, 7.6) | 2015–2019 | 2.2* (0.5, 3.9) |
| Morocco | 1990–1999 | 10.8* (10.3, 11.3) | 2000–2003 | 0 (−3, 3.2) | 2004–2009 | −5.5* (−6.8, −4.2) | 2010–2012 | −9.1* (−14.6, −3.3) | 2013–2019 | 0 (−1.1, 1) |
| Oman | 1990–1999 | 21* (18.5, 23.5) | 2000–2008 | −7.2* (−9.8, −4.5) | 2009–2019 | 3.4* (1.3, 5.5) | – | – | – | – |
| Palestine | 1990–1999 | 7.7* (7.4, 8.1) | 2000–2002 | 2.3 (−1.6, 6.5) | 2003–2009 | −1.4* (−2.1, −0.8) | 2010–2019 | 2.1* (1.8, 2.5) | – | – |
| Qatar | 1990–1995 | −7.1* (−7.8, −6.3) | 1996–1998 | 1.9 (−2.7, 6.7) | 1999–2002 | −20.2* (−22, −18.3) | 2002–2006 | −8.8* (−10.9, −6.7) | 2007–2019 | 0 (−0.3, 0.2) |
| Saudi Arabia | 1990–1993 | 5.8* (4, 7.6) | 1994–1998 | 11.3* (9.4, 13.2) | 1999–2007 | −3.8* (−4.4, −3.2) | 2008–2013 | 2.2* (1, 3.4) | 2014–2019 | −1.5* (−2.6, −0.3) |
| Somalia | 1990–1991 | 69.9* (65.4, 74.5) | 1992–1994 | 32.6* (29.1, 36.2) | 1995–1997 | −1.6 (−4.2, 1.1) | 1998–2003 | −13.1* (−13.6, −12.6) | 2004–2019 | −6.8* (−6.9, −6.7) |
| Sudan | 1990–1991 | 21.2* (19.1, 23.2) | 1992–1994 | 11.5* (9.6, 13.4) | 1995–1997 | 2.6* (0.9, 4.4) | 1998–2006 | −1.1* (−1.3, −0.9) | 2007–2019 | 2.4* (2.3, 2.5) |
| Syria | 1990–2004 | −0.2 (−1.6, 1.3) | 1995–2007 | 19.6 (−15.2, 68.7) | 2008–2019 | −2.9* (−5.2, −0.7) | – | – | – | – |
| Tunisia | 1990–2001 | 11.9* (11.7, 12.1) | 2002–2005 | 5.5* (3.7, 7.3) | 2006–2011 | 0.8* (0, 1.6) | 2012–2014 | 5* (1.5, 8.7) | 2015–2019 | 0.4 (−0.7, 1.5) |
| UAE | 1990–2004 | 9.3* (4.3, 14.6) | 2005–2011 | 30.7* (8.1, 57.9) | 2012–2019 | −21.1* (−32, −8.3) | – | – | – | – |
| Yemen | 1990–1993 | −0.7 (−1.7, 0.3) | 1994–1999 | 3.5* (2.8, 4.3) | 2000–2010 | 0.4* (0.2, 0.7) | 2011–2015 | 8.1* (7, 9.2) | 2016–2019 | 0.6 (−0.9, 2.3) |
| Total | 1990–1993 | 55* (49.9, 60.3) | 1994–1996 | 18.6* (6.7, 31.7) | 1997–2003 | −10.6* (−12.1, −9) | 2004–2019 | −3.5* (−3.9, −3.1) | – | – |
| Incidence rates (UNAIDS database) | ||||||||||
| Djibouti | 1990–1991 | 78.3* (57.3, 102.1) | 1992–1994 | 55.4* (37.1, 76.2) | 1995–1997 | 16.1* (2.4, 31.6) | 1998–2003 | −23.3* (−25.4, −21.1) | 2004–2019 | −11.9* (−12.4, −11.5) |
| Egypt | 1990–1993 | 20.3* (19.3, 21.4) | 1994–2003 | 15.5* (15.2, 15.8) | 2004–2012 | 14.1* (13.7, 14.4) | 2013–2016 | 11.3* (9.8, 12.9) | 2017–2019 | 5.5* (2.6, 8.5) |
| Iran | 1990–1992 | 25.4* (17.9, 33.4) | 1993–1995 | 59.8* (41.2, 80.8) | 1996–2003 | 28.9* (26.8, 31.1) | 2004–2012 | −16* (−17.2, −14.9) | 2013–2019 | −6.1* (−8, −4.1) |
| Jordan | 1990–1993 | 6.8* (6.1, 7.5) | 1994–2001 | 3.9* (3.6, 4.2) | 2002–2011 | 2.9* (2.7, 3.1) | 2012–2019 | 2.2* (2, 2.5) | – | – |
| Lebanon | 1990–1991 | 4.3* (2.3, 6.3) | 1992–1997 | 2.3* (1.9, 2.8) | 1998–2012 | 3* (3, 3.1) | 2013–2016 | −1.3* (−2.3, −0.4) | 2017–2019 | −4.4* (−6.2, −2.5) |
| Libya | 1990–1998 | 29.7* (29.1, 30.2) | 1999–2003 | 21* (19.2, 22.9) | 2004–2006 | 1.9 (−2.9, 6.8) | 2007–2011 | −21* (−22.2, −19.8) | 2012–2019 | 4.4* (3.8, 5.1) |
| Morocco | 1990–1992 | 12.5* (10.4, 14.6) | 1993–2001 | 4.5* (4, 4.9) | 2002–2007 | −1.1* (−1.9, −0.3) | 2008–2012 | −5.8* (−6.9, −4.7) | 2013–2019 | −9.1* (−9.7, −8.5) |
| Qatar | 1990–1994 | −39* (−40.9, −37.1) | 1995–2000 | 60.1* (55.1, 65.3) | 2001–2003 | 17* (1.5, 34.9) | 2004–2012 | −7.2* (−8.6, −5.8) | 2013–2019 | 17.3* (14.5, 20.1) |
| Saudi Arabia | 1990–1993 | 16.8* (13.9, 19.7) | 1994–1996 | 3.9 (−4, 12.4) | 1997–2003 | 9* (7.5, 10.4) | 2004–2006 | −7.6 (−14.6, 0) | 2007–2019 | 8.2* (7.7, 8.7) |
| Somalia | 1990–1994 | 19.9* (17.8, 22) | 1995–1999 | 6.7* (4.1, 9.3) | 2000–2004 | −5.3* (−7.6, −2.9) | 2005–2014 | −18.3* (−18.8, −17.7) | 2015–2019 | −4.5* (−6.8, −2.1) |
| Sudan | 1990–1994 | 46.6* (42.3, 51.1) | 1995–2000 | −0.5 (−3.4, 2.6) | 2001–2003 | −10.8 (−22.1, 2) | 2004–2019 | −2.5* (−3, −1.9) | – | – |
| Syria | 1990–1999 | 9.3* (8.9, 9.7) | 2000–2012 | 7.9* (7.6, 8.2) | 2013–2015 | 1.6 (−3, 6.5) | 2016–2019 | −14 * (−16, −11.9) | – | – |
| Tunisia | 1990–2001 | 15.1* (14.8, 15.4) | 2002–2004 | 6.1* (1.9, 10.5) | 2005–2007 | −12.2* (−15.7, −8.6) | 2008–2011 | 6.7* (4.5, 8.8) | 2012–2019 | 3.4* (2.9, 4) |
| Yemen | 1990–1993 | 4.6* (4.4, 4.7) | 1994–2006 | 3.8* (3.8, 3.8) | 2007–2010 | 3.4* (3.2, 3.7) | 2011–2014 | 3* (2.8, 3.2) | 2015–2019 | 2.3* (2.1, 2.4) |
APC annual percentage change, UAE United Arab Emirates.
*P <0.05 versus 0 (output from joinpoint regression analysis).
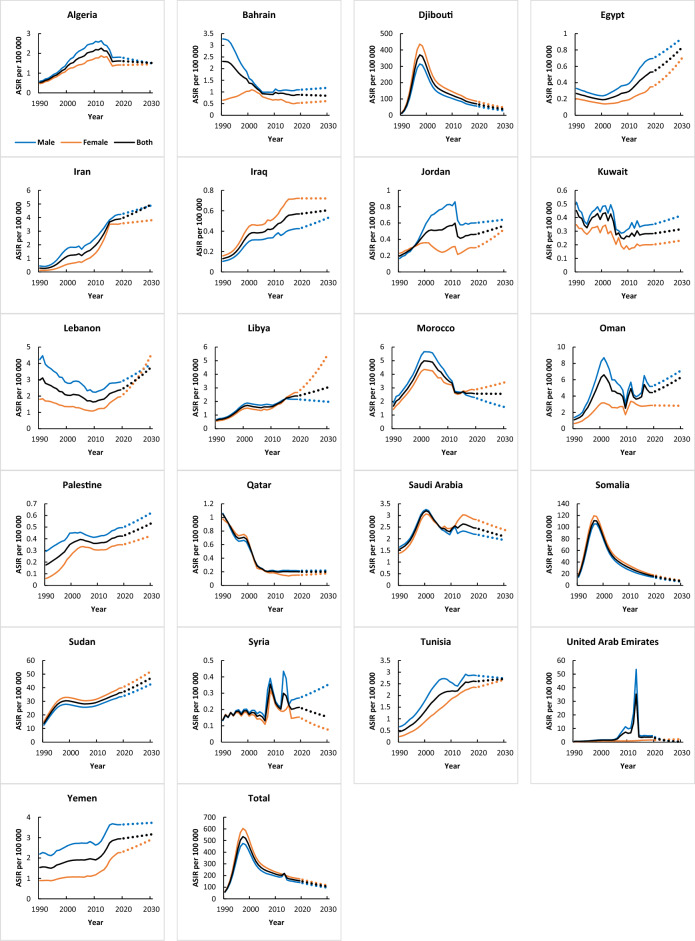
Figure 1.
Trends in age-standardized incidence rates (1990–2019) and prediction (2020–2030) per 100,000 from HIV in MENA countries (GBD).
Figure 1 presents the trends of the age-standardized incidence rates (ASIR) for HIV in MENA countries from 1990 to 2019. The ASIR of men was higher than women, except in Djibouti, Iraq, Somalia, and Sudan (Fig. 1). Table S3 presents the AAPC of HIV incidence in the region from 1990 to 2019. Among women (GBD data), seventeen countries had increases in ASIR and 4 countries showed declining trends. The highest AAPC was related to Iran (AAPC = 9.6, 95% CI 8.8, 10.5; P < 0.05) (12.3, and 8.3 in women and men, respectively). In the UNIAIDS dataset, the majority of incidence rises occurred in Egypt and Iran (P<0.05) (Table S3).
ASIR increased in almost all age groups in the region, especially those aged 44–64 years (AAPC = 3.8, 95% CI 1.4, 6.2; P < 0.05) and 25–34 years (AAPC = 3.3, 95% CI 2.6, 3.9; P < 0.05) (Table S4).
Age-standardized mortality rate trend
According to the GBD database, a total of 16 out of 21 countries reported increasing trends in the age-standardized mortality rate of HIV. Among them, Djibouti (AAPC = 24.2, 95% CI 23.0, 25.3; P < 0.001) and Somalia (AAPC = 15.1, 95% CI 14.1, 16.1 P < 0.001) showed the most marked increase in mortality rates. Qatar (AAPC = − 3.8, 95% CI − 4.3, − 3.3; P < 0.001), Kuwait (AAPC = − 3, 95% CI − 4.7, − 1.4; P < 0.001), Egypt (AAPC = − 2.7, 95% CI − 4.0, − 1.3; P < 0.001), Bahrain (AAPC = − 2.5, 95% CI − 3.6, − 1.5; P < 0.001) and Lebanon (AAPC = − 1.3, 95% CI − 1.8, − 0.8; P < 0.001) were the countries where a decrease in mortality rates was observed (Table 2 and Fig. 2). Modeling results with UNAIDS data indicate that the only country that showed decreasing mortality trends including Qatar (AAPC = − 3.8, 95% CI − 4.7, − 2.9; P < 0.001), and 13 countries showed an increasing trend in the mortality rate of HIV. The highest annual growth rate related to Iran (AAPC = 16.2, 95% CI 15.7, 16.7; P < 0.001) and the lowest annual growth rate related to Jordan (AAPC = 2.9, 95% CI 1.2, 4.7; P = 0.001) (Table 2).
Table 2.
Joinpoint regression analysis of age-standardized mortality rates, and mortality rates from HIV in MENA countries, 1990–2019.
| Country | Trend 1 | Trend 2 | Trend 3 | Trend 4 | Trend 5 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | |
| Age-standardized mortality rates (GBD database) | ||||||||||
| Algeria | 1990–1996 | 10.1* (9.7, 10.4) | 1997–1999 | 3.8* (1.3, 6.3) | 2000–2007 | 9.5* (9.1, 9.9) | 2008–2013 | −0.1 (−0.7, 0.4) | 2014–2019 | −8* (−8.4, −7.5) |
| Bahrain | 1990–1998 | 8.2* (7.3, 9.1) | 1999–2002 | −10.3* (−14.4, −6.1) | 2003–2007 | −1.2 (−4.1, 1.7) | 2008–2016 | −6.6* (−7.6, −5.7) | 2017–2019 | −15.7* (−23.2, −7.5) |
| Djibouti | 1990–1991 | 243.9* (215.9, 274.3) | 1992–1995 | 99.8* (91.5, 108.5) | 1996–2000 | 33.7* (30.2, 37.3) | 2001–2008 | 1.8* (0.6, 2.9) | 2009–2019 | −5.4* (−0.6, −4.8) |
| Egypt | 1990–1994 | 9.3* (6.5, 12.2) | 1995–2004 | −0.3 (−1.4, 0.7) | 2005–2007 | −11.6* (−21.3, −0.8) | 2008–2012 | 0.3 (−3.3, 4) | 2013–2019 | −13* (−14.7, −11.3) |
| Iran | 1990–1997 | 10.7* (10.2, 11.1) | 1998–2004 | 14.8* (14.1, 15.5) | 2005–2008 | 5.1* (3.1, 7.2) | 2009–2011 | 9.4* (5.3, 13.7) | 2012–2019 | 5.1* (4.6, 5.7) |
| Iraq | 1990–1995 | 12.5* (12.1, 13) | 1996–2002 | 10.4* (10, 10.9) | 2003–2005 | 5.3* (2.8, 7.8) | 2006–2019 | 1.7* (1.5, 1.8) | – | – |
| Jordan | 1990–1994 | 14.8* (13.5, 16.1) | 1995–2003 | 9.8* (9.2, 10.4) | 2004–2006 | −14.5* (−18.8, −10) | 2007–2012 | 10.8* (9.5, 10) | 2013–2019 | −3.3* (−4.1, −2.4) |
| Kuwait | – | – | – | – | – | – | – | – | – | – |
| Lebanon | 1990–1993 | 6.9* (4.7, 9.2) | 1994–1999 | 0.7 (−0.8, 2.3) | 2000–2005 | −5.8* (−7.3, −4.4) | 2006–2019 | −2.5* (−2.8, −2.1) | – | – |
| Libya | 1990–1991 | 14.1* (11.8, 16.4) | 1992–2003 | 10.2* (10.1, 10.4) | 2004–2011 | 3.3* (3.1, 3.6) | 2012–2015 | −1.3* (−2.3, −0.3) | 2016–2019 | 1.8* (0.8, 2.8) |
| Morocco | 1990–1993 | 19.2* (18.2, 20.3) | 1994–1998 | 13.8* (12.8, 14.9) | 1999–2002 | 10.5* (9, 12.1) | 2003–2011 | 1.2* (0.9, 1.5) | 2012–2019 | −9.6* (−9.9, −9.2) |
| Oman | 1990–1999 | 16.7* (16.3, 17) | 2000–2002 | −6.3* (−10.1, −2.3) | 2003–2008 | 20* (18.9, 21.1) | 2009–2019 | −3.1* (−3.4, −2.8) | – | – |
| Palestine | 1990–1992 | 17.5* (16.3, 18.6) | 1993–1996 | 12.5* (11.4,13.6) | 1997–2004 | 9.3* (9, 9.6) | 2005–2007 | 4.4* (2.3, 6.5) | 2008–2019 | 0.2* (0, 0.3) |
| Qatar | 1990–1994 | 9.9* (9, 10.9) | 1995–1998 | −1.8 (−3.7, 0.1) | 1999–2001 | −30.1* (−32.7, −27.4) | 2002–2008 | 1.8* (1.2, 2.5) | 2009–2019 | −5.6* (−5.9, −5.3) |
| Saudi Arabia | 1990–1992 | 11.6* (11.1, 12.1) | 1993–2002 | 8.8* (8.7, 8.9) | 2003–2005 | 4.1* (3.1, 5.1) | 2006–2011 | 0 (− 0.2, 0.2) | 2012–2019 | −1.6* (−1.7, −1.5) |
| Somalia | 1990–1991 | 153.6* (135.8, 172.6) | 1992–1995 | 55.7* (50.2, 61.5) | 1996–1999 | 26.8* (22.3, 31.4) | 2000–2005 | 4.5* (2.8, 6.2) | 2006–2019 | −5.8* (−6.1, −5.4) |
| Sudan | 1990–1991 | 49.9* (39.8, 60.8) | 1992–1995 | 27.1* (22.7, 31.6) | 1996–1999 | 14.5* (10.5, 18.6) | 2000–2004 | 6.8* (4.4, 9.2) | 2005–2019 | 0.4* (0, 0.7) |
| Syria | 1990–2001 | 6* (5.5, 6.5) | 2002–2009 | −3.1* (−4.1, −2.1) | 2010–2013 | 4.3* (0.2, 8.5) | 2014–2016 | −9.1* (−16.1, −1.6) | 2017–2019 | 4.3* (−3.7, 12.9) |
| Tunisia | 1990–1992 | 15.3* (13.7, 16.9) | 1993–2000 | 12.3* (11.9, 12.8) | 2001–2011 | 7.8* (7.6, 8.1) | 2012–2016 | 1.5* (0.6, 2.4) | 2017–2019 | −3.7* (−6.3, −1) |
| UAE | 1990–2000 | 11.5* (11, 12) | 2001–2008 | 8.6* (7.6, 9.6) | 2009–2013 | 24.1* (21.5, 26.7) | 2014–2016 | 17.3* (9.9, 25.3) | 2017–2019 | −7.3* (−13.2, −0.9) |
| Yemen | 1990–1994 | 8.3* (7.6, 9) | 1995–2006 | 2.7* (2.5, 2.9) | 2007–2010 | −3.5* (−4.9, −2.1) | 2011–2015 | −0.9* (−1.8, 0) | 2016–2019 | 2.2* (0.7, 3.7) |
| Total | 1990–1997 | 39.5* (38.7, 40.3) | 1998–2000 | 20.1* (14.1, 26.5) | 2001–2004 | 5.1* (2.4, 7.8) | 2005–2010 | −1.4* (−2.5, −0.2) | 2011–2019 | −4.7* (−5.3, −4.2) |
| Mortality rates (UNAIDS database) | ||||||||||
| Djibouti | 1990–1994 | 78.4* (74.3, 82.5) | 1995–1999 | 32.6* (28.3, 36.9) | 2000–2005 | 6.6* (4.2, 9.1) | 2006–2012 | −5* (−6.7, −3.4) | 2013–2019 | −14* (−15.5, −12.5) |
| Egypt | 1990–1994 | 35.5* (32.9, 38.1) | 1995–2003 | 21.1* (20, 22.2) | 2004–2006 | −1.2 (−9.4, 7.6) | 2007–2013 | 12.4* (10.8, 14.1) | 2014–2019 | 1.8 (−0.2, 3.7) |
| Iran | 1990–1994 | 19.2* (18.1, 20.3) | 1995–2004 | 33.4* (32.9, 33.9) | 2005–2008 | 18.9* (16.6, 21.3) | 2009–2013 | 5.1* (3.8, 6.4) | 2014–2019 | −6.8* (−7.6, −5.9) |
| Jordan | 1990–1998 | 7.6* (6.1, 9.2) | 1999–2001 | −16.2* (_28.3, −2.1) | 2002–2014 | 6.2* (5.2, 7.2) | 2015–2019 | −1.8 (−6.6, 3.1) | – | – |
| Lebanon | 1990–1992 | 25.2* (20.7, 29.9) | 1993–1996 | 14.3* (10.2, 18.5) | 1997–1999 | 6 (−1.5, 14.1) | 2000–2002 | −10.5* (−16.8, −3.7) | 2003–2019 | 0.8* (0.5, 1) |
| Libya | 1990–1998 | 31.6* (30.5, 32.8) | 1999–2001 | −0.4 (−9.4, 9.6) | 2002–2006 | 21.3* (17.7, 25) | 2007–2013 | 2.8* (1.1, 4.4) | 2014–2019 | −3.8* (−5.8, −1.8) |
| Morocco | 1990–1994 | 18.8* (16.2, 21.4) | 1995–2000 | 12.9* (10.5, 15.4) | 2001–2010 | 1* (0.1, 1.9) | 2011–2019 | −8.5* (−9.4, −7.5) | – | – |
| Qatar | 1990–1993 | 11.3* (8.7, 13.9) | 1994–2003 | −5.9* (−6.5, −5.3) | 2004–2013 | 9.6* (8.9, 10.3) | 2014–2016 | −39.6* (−43.9, −34.9) | 2017–2019 | −15.8* (−21.9, −9.3) |
| Saudi Arabia | 1990–1993 | 28.1* (23.8, 32.6) | 1994–1996 | −13.1* (−22, −3.1) | 1997–2004 | 11.1* (9.5, 12.7) | 2005–2013 | −1 (−2.1, 0.2) | 2014–2019 | 10.5* (7.8, 13.2) |
| Somalia | 1990–1994 | 29.2* (27.7, 30.6) | 1995–1999 | 18.3* (16.5, 20.2) | 2000–2005 | 8.1* (6.9, 9.3) | 2006–2012 | −5.1* (−5.9, −4.3) | 2013–2019 | −12.2* (−12.9, −11.4) |
| Sudan | 1990–1995 | 45.9* (42.4, 49.4) | 1996–1999 | 27.1* (18.3, 36.4) | 2000–2004 | 11.8* (6.9, 17) | 2005–2015 | −1.6* (−2.7, −0.6) | 2016–2019 | −9.2* (−15.4, −2.5) |
| Syria | 1990–2000 | 8.8* (7.7, 9.8) | 2001–2012 | 5.1* (4.1, 6.1) | 2013–2016 | 12.2* (4.4, 20.5) | 2017–2019 | − 7.7 (− 20, 6.6) | – | – |
| Tunisia | 1990–1999 | 17.6* (16.9, 18.3) | 2000–2002 | 3.1 (−4.4, 11.2) | 2003–2005 | 15.4* (7, 24.5) | 2006–2014 | 6.7* (5.8, 7.6) | 2015–2019 | −0.5 (−2.8, 1.9) |
| Yemen | 1990–1994 | 9.5* (7.9, 11) | 1995–2006 | 4.1* (3.6, 4.5) | 2007–2009 | −9.4* (−15, −3.4) | 2010–2019 | 2.5* (1.9, 3.1) | – | – |
APC annual percentage change, UAE United Arab Emirates.
*P <0.05 versus 0 (output from joinpoint regression analysis).
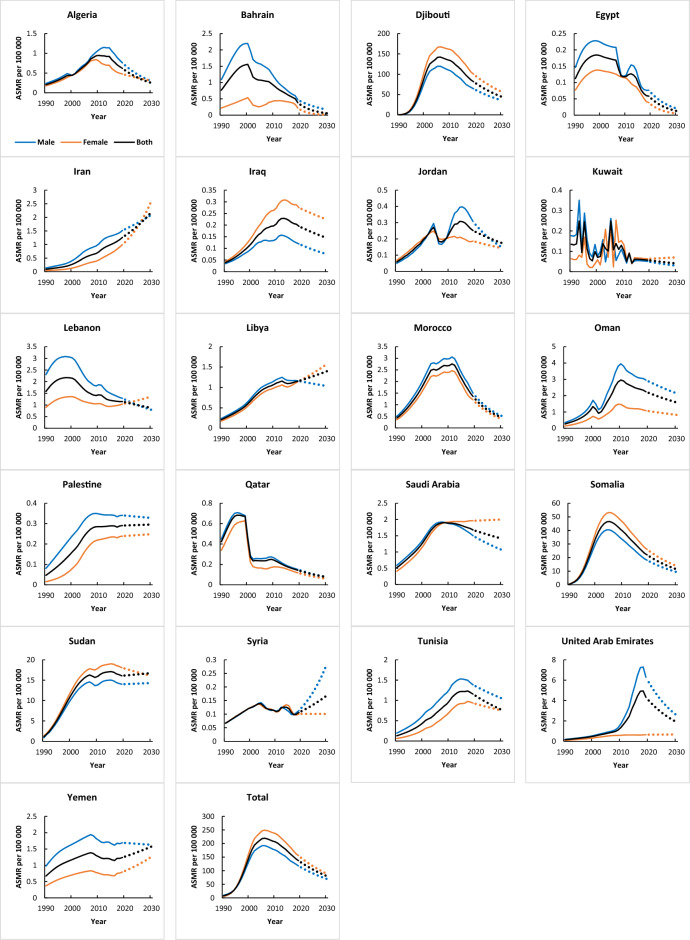
Figure 2.
Trends in age-standardized mortality rates (1990–2019) and prediction (2020–2030) per 100,000 from HIV in MENA countries (GBD).
A total of 17 and 18 out of 21 reported increasing mortality trends in men and women, respectively. Among them, Djibouti (AAPCmen = 23.3, 95% CI 21.5, 25, AAPC women = 24.6, 95%CI 23.4, 25.9; P < 0.05) showed the most marked increase in mortality rates. In UNIAIDS data, Iran had the greatest mortality increase (AAPC = 16.2, 95% CI 16, 16.4; P < 0.05) (Table S5). Table S6 presents the AAPC of mortality rates from HIV in MENA countries by age groups, 1990–2019.
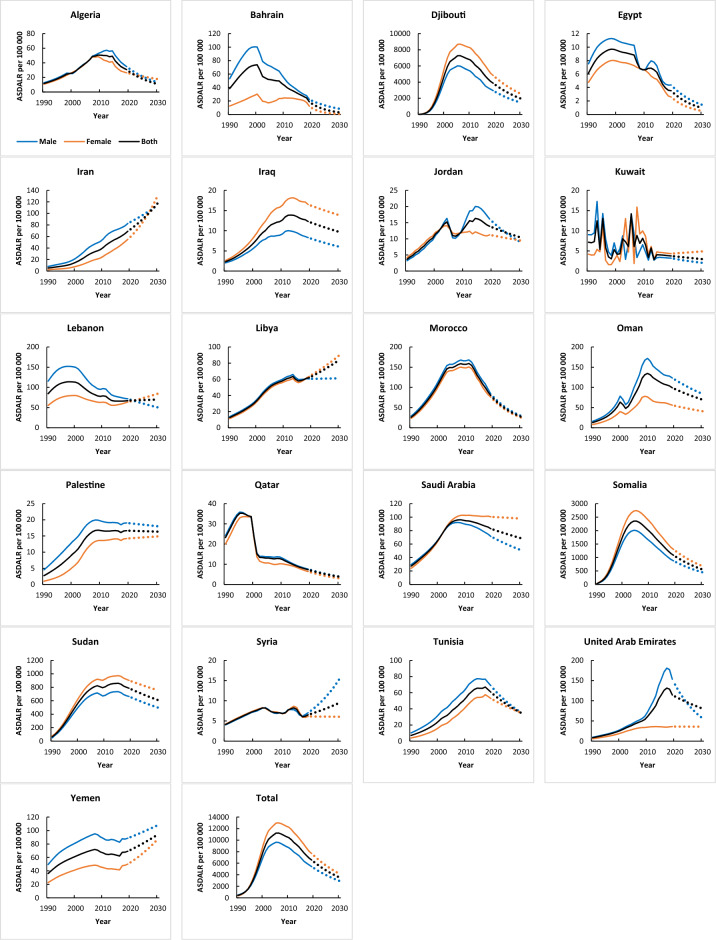
Disability-adjusted life years (DALY) trend
The DALY trends of each country were shown in Table 3 and Fig. 3, and the corresponding findings from the joinpoint regression analysis were presented in Tables S7 and S8. According to GBD datasets, 16 countries had an increasing pattern in DALY and five countries showed declining trends in both genders between 1990 and 2019 (Table S7).
Table 3.
Joinpoint regression analysis of disability-adjusted life years from HIV in MENA countries, 1990–2019.
| Country | Trend 1 | Trend 2 | Trend 3 | Trend 4 | Trend 5 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | Years | APC (95% CI) | |
| Age-standardized rates disability-adjusted life years (GBD database) | ||||||||||
| Algeria | 1990–1996 | 9.8* (9.2, 11) | 1997–1999 | 5.8* (4.8, 8) | 2000–2007 | 8.6 (−0.1, 10) | 2008–2013 | −1.3* (−2.8, −0.4) | 2014–2019 | −9.1* (−10.1, −8.1) |
| Bahrain | 1990–1997 | 8.6* (7.4, 9.7) | 1998–2003 | −6.6* (−9.3, −4.5) | 2004–2007 | −1.4 (−4.1, 1.4) | 2008–2016 | −6.4* (−7.4, −5.3) | 2017–2019 | −15.2* (−18.7, −10) |
| Djibouti | 1990–1991 | 211.3* (190.9, 235.5) | 1992–1995 | 93.1* (87.4, 99.1) | 1996–2000 | 31.3* (28.2, 34.3) | 2001–2008 | 1.3 (−0.2, 3.2) | 2009–2019 | −6.1* (−7.3, −5) |
| Egypt | 1990–1994 | 8.5* (6.4, 11.4) | 1995–2004 | −0.4 (−1.1, 0.6) | 2005–2007 | −9.4* (−11.4, −5.6) | 2008–2012 | −0.4 (−2.4, 4) | 2013–2019 | −11.3* (−12.8, −9.8) |
| Iran | 1990–1996 | 9.2* (8.7, 9.6) | 1997–2004 | 14.4* (14, 14.8) | 2005–2008 | 5.8* (4.7, 6.5) | 2009–2011 | 9.2* (7.8, 10) | 2012–2019 | 5* (4.5, 5.4) |
| Iraq | 1990–2001 | 11.7* (11.5, 11.9) | 2002–2005 | 6.6* (5.9, 7.8) | 2006–2012 | 3* (2.6, 3.4) | 20132019 | −2.1* (−2.5, −1.7) | – | – |
| Jordan | 1990–1996 | 13* (11.9, 14.6) | 1997–2003 | 8* (6.7, 9) | 2004–2006 | −12.1* (−13.8, −10.1) | 2007–2012 | 8* (6.6, 9.5) | 2013–2019 | −2.6* (−3.9, −1.2) |
| Kuwait | – | – | – | – | – | – | – | – | – | – |
| Lebanon | 1990–1993 | 6.6* (5.1, 9) | 1994–1999 | 0.7 (−0.6, 1.8) | 2000–2005 | −4.8* (−6.8, −4.1) | 2006–2014 | −2.8* (−3.4, −2.1) | 2015–2019 | 0.4 (−0.9, 3) |
| Libya | 1990–2002 | 10.2* (10, 10.4) | 2003–2005 | 5.7* (4.3, 8.3) | 2006–2012 | 2.2* (1.8, 2.6) | 2013–2015 | −3* (−3.8, −1.6) | 2016–2019 | 2.8* (1.7, 5) |
| Morocco | 1990–1993 | 18.7* (17.6, 20.1) | 1994–1998 | 13.6* (12.7, 14.8) | 1999–2002 | 10.7* (7.6, 11.4) | 2003–2011 | 0.8* (0.5, 1) | 2012–2019 | −9.3* (−9.6, −9) |
| Oman | 1990–1999 | 16.8* (14.2, 18.8) | 2000–2002 | −5.2 (−7.9, 18.9) | 2003–2005 | 22.1 (−5, 26.5) | 2006–2008 | 13.6 (−5.9, 18.2) | 2009–2019 | −3.1* (−6.6, −0.5) |
| Palestine | 1990–1992 | 16.5* (15.3, 18.1) | 1993–1996 | 12.6* (11.3, 13.6) | 1997–2004 | 10* (9.5, 10.3) | 2005–2007 | 4* (2.7, 5.4) | 2008–2019 | −0.2 (−0.4, 0) |
| Qatar | 1990–1994 | 8.9* (6.6, 12.7) | 1995–1998 | −2.9 (−5.5, 0) | 1999–2001 | −26.7* (−28.9, −21.8) | 2002–2008 | 0.2 (−1.2, 2.7) | 2009–2019 | −5.6* (−6.8, −4.8) |
| Saudi Arabia | 1990–1992 | 10.6* (10, 11.3) | 1993–2002 | 8.8* (8.7, 8.9) | 2003–2005 | 3.6* (3.3, 3.9) | 2006–2011 | −0.4* (−0.6, −0.1) | 2012–2019 | −1.7* (−1.9, −1.5) |
| Somalia | 1990–1991 | 132.2* (112.1, 149.2) | 1992–1995 | 53.2* (46.2, 61.7) | 1996–1999 | 24.6* (15.8, 32.8) | 2000–2005 | 3.7 (−0.1, 7.8) | 2006–2019 | −5.9* (−6.8, −5.1) |
| Sudan | 1990–1992 | 41.7* (39, 44.5) | 1993–1997 | 21* (19.5, 22.4) | 1998–2003 | 8.2* (7.1, 9.5) | 2004–2014 | 0.8* (0.4, 1.5) | 2015–2019 | −2.3* (−5.1, −0.7) |
| Syria | 1990–2001 | 5.6* (5.1, 6.1) | 2002–2009 | −2.7* (−3.9, −1.7) | 2010–2013 | 5.9* (3.9, 9.2) | 2014–2016 | −10.7* (−12.7, −8) | 2017–2019 | 3.5 (−0.8, 7.3) |
| Tunisia | 1990–1992 | 14.9* (13.6, 16.7) | 1993–2000 | 12.5* (11.9, 12.8) | 2001–2011 | 7.7* (7.5, 7.8) | 2012–2016 | 1.4* (1, 1.8) | 2017–2019 | −4.9* (−6.2, −2.9) |
| UAE | 1990–1992 | 13.7* (11.5, 16.9) | 1993–2002 | 10.9* (7.6, 11.3) | 2003–2008 | 7.1* (5.3, 9.1) | 2009–2015 | 13.5* (12.8, 14.5) | 2016–2019 | −3.1* (−4.6, −1.7) |
| Yemen | 1990–1994 | 7.7* (6.7, 8.9) | 1995–2005 | 2.8* (2.4, 3.1) | 2006–2014 | −1.6* (−2.2, −1.2) | 2015–2019 | 2.8* (1.5, 5) | – | – |
| Total | 1990–1996 | 40* (39.1, 41.2) | 1997–1999 | 25.4* (22.3, 29.2) | 2000–2003 | 7.6* (5.6, 9.4) | 2004–2010 | −1.4* (−2.2, −0.4) | 2011–2019 | −5.5* (−6.3, −4.9) |
APC annual percentage change, UAE United Arab Emirates.
*P < 0.05 versus 0 (output from joinpoint regression analysis).
Figure 3.
Trends in disability-adjusted life years (1990–2019) and prediction (2020–2030) per 100,000 from HIV in MENA countries (GBD).
Projection of incidence, mortality rates, and DALY
Tables 4, 5 and 6 summarize the projected age-standardized incidence, mortality rates, and DALY of HIV by 2025 and 2030 per 100,000 in the countries in the region. The estimated increase in the incidence by 2030 was most marked in Egypt (339%), based on UNAIDS estimates. However, the estimated higher age-standardized incidence rate by 2030 was found in Iran (174%), according to estimates from GBD. Countries with substantial growth rates of age-standardized incidence rates and incidence rates between 2019 and 2030 include Lebanon (59%) and Qatar (478%), respectively (Table 4 and Fig. 1).
Table 4.
Age-standardized incidence rates and prediction of age-standardized incidence rates from HIV in 2025 and 2030 per 100000 in MENA countries.
| Country | Age-standardized incidence rates (GBD database) | Incidence rates (UNAIDS database) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Available | Prediction | Growth rate (%) | Available | Prediction | Growth rate (%) | |||||||||||||||||
| 1990 | 2000 | 2010 | 2019 | 2025 | 2030 | 1990–2019 | 1990–2025 | 1990–2030 | 2019–2025 | 2019–2030 | 1990 | 2000 | 2010 | 2019 | 2025 | 2030 | 1990–2019 | 1990–2025 | 1990–2030 | 2019–2025 | 2019–2030 | |
| Algeria | 0.53 | 1.37 | 2.19 | 1.61 | 1.56 | 1.52 | 207 | 197 | 189 | −3 | −6 | – | – | – | – | – | – | – | – | – | – | – |
| Bahrain | 2.31 | 1.38 | 0.98 | 0.88 | 0.85 | 0.83 | −62 | −63 | −64 | −3 | −5 | – | – | – | – | – | – | – | – | – | – | – |
| Djibouti | 12.65 | 280.46 | 119.55 | 69.86 | 48.99 | 36.44 | 452 | 287 | 188 | −30 | −48 | 23.8 | 274.42 | 44.36 | 13.79 | 6.43 | 3.40 | −42 | −73 | −86 | −53 | −75 |
| Egypt | 0.27 | 0.19 | 0.29 | 0.53 | 0.68 | 0.83 | 99 | 154 | 211 | 28 | 56 | 0.06 | 0.31 | 1.2 | 3.04 | 4.18 | 5.47 | 4960 | 6873 | 9009 | 38 | 80 |
| Iran | 0.29 | 1.17 | 1.96 | 3.91 | 4.46 | 4.97 | 1264 | 1455 | 1635 | 14 | 27 | 0.33 | 7.61 | 6.73 | 2.9 | 1.99 | 1.45 | 788 | 510 | 346 | −31 | −50 |
| Iraq | 0.13 | 0.37 | 0.45 | 0.57 | 0.59 | 0.61 | 337 | 352 | 365 | 3 | 6 | – | – | – | – | – | – | – | – | – | – | – |
| Jordan | 0.2 | 0.48 | 0.57 | 0.46 | 0.52 | 0.57 | 136 | 165 | 192 | 12 | 24 | 0.29 | 0.47 | 0.65 | 0.8 | 0.92 | 1.02 | 175 | 214 | 250 | 14 | 28 |
| Kuwait | 0.45 | 0.43 | 0.26 | 0.28 | 0.30 | 0.32 | −37 | −34 | −30 | 6 | 12 | – | – | – | – | – | – | – | – | – | – | – |
| Lebanon | 2.98 | 2.05 | 1.66 | 2.38 | 3.06 | 3.78 | −20 | 3 | 27 | 29 | 59 | 1.66 | 2.21 | 2.98 | 2.83 | 2.16 | 1.73 | 70 | 30 | 4 | −24 | −39 |
| Libya | 0.62 | 1.67 | 1.63 | 2.4 | 2.74 | 3.05 | 286 | 339 | 389 | 14 | 27 | 0.4 | 5.1 | 5.55 | 4.97 | 6.44 | 7.99 | 1145 | 1514 | 1903 | 30 | 61 |
| Morocco | 1.66 | 4.8 | 3.48 | 2.58 | 2.57 | 2.56 | 55 | 54 | 54 | 0 | 0 | 2.69 | 5.26 | 4.74 | 2.17 | 1.23 | 0.76 | −19 | −54 | −72 | −44 | −65 |
| Oman | 1.09 | 6.29 | 3.93 | 4.42 | 5.39 | 6.37 | 306 | 395 | 484 | 22 | 44 | – | – | – | – | – | – | – | – | – | – | – |
| Palestine | 0.18 | 0.36 | 0.36 | 0.42 | 0.48 | 0.53 | 141 | 173 | 204 | 14 | 26 | – | – | – | – | – | – | – | – | – | – | – |
| Qatar | 1.05 | 0.59 | 0.2 | 0.2 | 0.20 | 0.20 | −81 | −81 | −81 | 0 | 0 | 1.91 | 1.72 | 2.38 | 5.61 | 14.60 | 32.41 | 194 | 666 | 1601 | 160 | 478 |
| Saudi Arabia | 1.55 | 3.2 | 2.45 | 2.46 | 2.25 | 2.09 | 58 | 45 | 35 | −8 | −15 | 0.63 | 1.69 | 2.35 | 4.62 | 7.43 | 11.04 | 637 | 1086 | 1661 | 61 | 139 |
| Somalia | 16.07 | 78.25 | 29.42 | 15.95 | 10.45 | 7.35 | −1 | −35 | −54 | −34 | −54 | 6.23 | 21.01 | 5.97 | 1.88 | 1.43 | 1.13 | −70 | −77 | −82 | −24 | −40 |
| Sudan | 13.84 | 30.01 | 29.55 | 36.46 | 42.02 | 47.31 | 163 | 204 | 242 | 15 | 30 | 2.83 | 17.7 | 10.75 | 9.1 | 7.82 | 6.90 | 222 | 176 | 144 | −14 | −24 |
| Syria | 0.13 | 0.17 | 0.24 | 0.21 | 0.18 | 0.15 | 58 | 32 | 14 | −16 | −28 | 0.07 | 0.17 | 0.37 | 0.32 | 0.13 | 0.06 | 345 | 81 | −15 | −59 | −81 |
| Tunisia | 0.45 | 1.38 | 2.2 | 2.6 | 2.66 | 2.72 | 476 | 490 | 502 | 2 | 4 | 0.45 | 1.89 | 2.32 | 3.28 | 4.01 | 4.74 | 627 | 789 | 951 | 22 | 45 |
| UAE | 0.51 | 1.45 | 6.47 | 3.76 | 0.91 | 0.28 | 634 | 77 | −46 | −76 | − 93 | – | – | – | – | – | – | – | – | – | – | – |
| Yemen | 1.54 | 1.84 | 1.91 | 2.94 | 3.06 | 3.16 | 91 | 99 | 105 | 4 | 7 | 1.28 | 1.92 | 2.75 | 3.5 | 4.01 | 4.48 | 173 | 213 | 250 | 14 | 28 |
| Total | 58.50 | 417.91 | 209.74 | 154.90 | 124.96 | 104.48 | 165 | 114 | 79 | −19 | −33 | – | – | – | – | – | – | – | – | – | – | – |
UAE United Arab Emirates.
Table 5.
Age-standardized mortality rates and prediction of age-standardized mortality rates from HIV in 2025 and 2030 per 100000 in MENA countries.
| Country | Age-standardized mortality rates (GBD database) | Mortality rates (UNAIDS database) | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Available | Prediction | Growth rate (%) | Available | Prediction | Growth rate (%) | |||||||||||||||||
| 1990 | 2000 | 2010 | 2019 | 2025 | 2030 | 1990–2019 | 1990–2025 | 1990–2030 | 2019–2025 | 2019–2030 | 1990 | 2000 | 2010 | 2019 | 2025 | 2030 | 1990–2019 | 1990–2025 | 1990–2030 | 2019–2025 | 2019–2030 | |
| Algeria | 0.21 | 0.44 | 0.95 | 0.62 | 0.38 | 0.25 | 201 | 83 | 21 | −39 | −60 | – | – | – | – | – | – | – | – | – | – | – |
| Bahrain | 0.77 | 1.56 | 0.9 | 0.38 | 0.14 | 0.06 | −50 | −82 | −92 | −64 | −85 | – | – | – | – | – | – | – | – | – | – | – |
| Djibouti | 0.17 | 94.32 | 133.57 | 81.48 | 58.40 | 44.24 | 48364 | 34633 | 26214 | −28 | −46 | 1.08 | 77.9 | 102.79 | 35.9 | 14.56 | 6.86 | 3229 | 1250 | 536 | −59 | −81 |
| Egypt | 0.11 | 0.18 | 0.12 | 0.06 | 0.03 | 0.01 | −48 | −78 | −89 | −57 | −78 | 0 | 0.06 | 0.17 | 0.27 | 0.30 | 0.33 | 6094 | 6778 | 7405 | 11 | 21 |
| Iran | 0.09 | 0.27 | 0.72 | 1.26 | 1.71 | 2.19 | 1302 | 1795 | 2335 | 35 | 74 | 0.06 | 0.59 | 5.25 | 4.43 | 2.91 | 2.05 | 7386 | 4821 | 3369 | −34 | −54 |
| Iraq | 0.04 | 0.12 | 0.2 | 0.23 | 0.17 | 0.14 | 400 | 325 | 271 | –15 | –26 | – | – | – | – | – | – | – | – | – | – | – |
| Jordan | 0.06 | 0.19 | 0.23 | 0.25 | 0.21 | 0.17 | 332 | 254 | 200 | –18 | –31 | 0.09 | 0.17 | 0.17 | 0.22 | 0.20 | 0.18 | 142 | 117 | 98 | –10 | –18 |
| Kuwait | 0.13 | 0.07 | 0.1 | 0.06 | 0.05 | 0.04 | –58 | –65 | –70 | –17 | –29 | – | – | – | – | – | – | – | – | – | – | – |
| Lebanon | 1.58 | 2.15 | 1.43 | 1.15 | 0.99 | 0.87 | –27 | –38 | –45 | –14 | –24 | 0.27 | 1.11 | 0.84 | 0.86 | 0.90 | 0.93 | 213 | 227 | 240 | 5 | 9 |
| Libya | 0.21 | 0.6 | 1.08 | 1.15 | 1.28 | 1.40 | 446 | 507 | 563 | 11 | 21 | 0.04 | 0.51 | 1.3 | 1.28 | 1.01 | 0.83 | 3184 | 2499 | 2039 | –21 | –35 |
| Morocco | 0.43 | 1.85 | 2.69 | 1.36 | 0.74 | 0.45 | 218 | 73 | 5 | –45 | –67 | 0.48 | 2.08 | 2.6 | 1.26 | 0.74 | 0.47 | 161 | 54 | –1 | –41 | –62 |
| Oman | 0.26 | 1.33 | 2.96 | 2.24 | 1.85 | 1.58 | 748 | 602 | 500 | –17 | –29 | – | – | – | – | – | – | – | – | – | – | – |
| Palestine | 0.05 | 0.16 | 0.29 | 0.29 | 0.29 | 0.30 | 522 | 528 | 533 | 1 | 2 | – | – | – | – | – | – | – | – | – | – | – |
| Qatar | 0.42 | 0.45 | 0.24 | 0.14 | 0.10 | 0.08 | –66 | –76 | –82 | –29 | –47 | 1.07 | 1.16 | 1.61 | 0.37 | 0.13 | 0.06 | –65 | –88 | –95 | –64 | –85 |
| Saudi Arabia | 0.52 | 1.3 | 1.89 | 1.68 | 1.53 | 1.41 | 224 | 195 | 172 | –9 | –16 | 0.07 | 0.18 | 0.26 | 0.42 | 0.77 | 1.27 | 524 | 1033 | 1763 | 82 | 199 |
| Somalia | 0.35 | 35.01 | 39.34 | 22.01 | 15.39 | 11.42 | 6270 | 4354 | 3205 | –30 | –48 | 0.72 | 5.9 | 8.18 | 3.12 | 1.43 | 0.75 | 335 | 99 | 4 | –54 | –76 |
| Sudan | 1.12 | 11.23 | 15.93 | 16.08 | 16.44 | 16.75 | 1330 | 1362 | 1389 | 2 | 4 | 0.19 | 4.68 | 7.04 | 5.48 | 3.07 | 1.89 | 2716 | 1475 | 871 | –44 | –66 |
| Syria | 0.07 | 0.12 | 0.11 | 0.11 | 0.14 | 0.17 | 59 | 105 | 152 | 29 | 58 | 0.02 | 0.05 | 0.09 | 0.13 | 0.08 | 0.06 | 523 | 287 | 160 | –38 | –58 |
| Tunisia | 0.13 | 0.45 | 0.99 | 1.16 | 0.92 | 0.77 | 796 | 615 | 493 | –20 | –34 | 0.08 | 0.42 | 0.9 | 1.26 | 1.22 | 1.19 | 1404 | 1361 | 1327 | –3 | –5 |
| UAE | 0.16 | 0.49 | 1.35 | 4.32 | 2.75 | 1.89 | 2597 | 1616 | 1077 | –36 | –56 | – | – | – | – | – | – | – | – | – | – | – |
| Yemen | 0.67 | 1.18 | 1.26 | 1.24 | 1.41 | 1.57 | 85 | 110 | 134 | 14 | 27 | 0.43 | 0.84 | 0.87 | 1.03 | 1.20 | 1.36 | 138 | 177 | 213 | 16 | 31 |
| Total | 7.54 | 153.47 | 206.35 | 137.22 | 102.51 | 80.40 | 1719 | 1259 | 966 | –25 | –41 | – | – | – | – | – | – | – | – | – | – | – |
UAE United Arab Emirates.
Table 6.
Disability-adjusted life years and prediction of disability-adjusted life years from HIV in 2025 and 2030 per 100000 in MENA countries.
| Country | Disability-adjusted life years (GBD database) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Available | Prediction | Growth rate (%) | |||||||||
| 1990 | 2000 | 2010 | 2019 | 2025 | 2030 | 1990–2019 | 1990–2025 | 1990–2030 | 2019–2025 | 2019–2030 | |
| Algeria | 11.67 | 26.08 | 50.43 | 30.64 | 17.30 | 10.74 | 162 | 48 | −8 | −44 | −65 |
| Bahrain | 38.39 | 73.76 | 43.02 | 18.73 | 6.96 | 3.05 | −51 | −82 | −92 | −63 | −84 |
| Djibouti | 13.07 | 5034.22 | 6749.16 | 3863.82 | 2656.56 | 1944.19 | 29472 | 20232 | 14780 | −31 | −50 |
| Egypt | 6.16 | 9.51 | 6.63 | 3.52 | 1.72 | 0.95 | −43 | −72 | −85 | −51 | −73 |
| Iran | 5.39 | 15.15 | 40.53 | 69.04 | 92.59 | 118.24 | 1182 | 1619 | 2096 | 34 | 71 |
| Iraq | 2.32 | 7.06 | 12.67 | 12.28 | 10.79 | 9.70 | 430 | 366 | 319 | −12 | −21 |
| Jordan | 3.66 | 11.52 | 13.26 | 13.88 | 11.85 | 10.39 | 279 | 223 | 184 | −15 | −25 |
| Kuwait | 7.15 | 4.16 | 6.52 | 3.76 | 3.30 | 2.97 | −47 | −54 | −59 | −12 | −21 |
| Lebanon | 84.37 | 112.86 | 79.02 | 67.22 | 68.72 | 69.99 | −20 | −19 | −17 | 2 | 4 |
| Libya | 12.66 | 34.04 | 59.44 | 62.09 | 73.27 | 84.12 | 391 | 479 | 565 | 18 | 35 |
| Morocco | 26.16 | 109.78 | 157.02 | 79.73 | 44.47 | 27.34 | 205 | 70 | 5 | −44 | −66 |
| Oman | 12.86 | 63.61 | 134.62 | 98.93 | 81.66 | 69.59 | 669 | 535 | 441 | −17 | −30 |
| Palestine | 2.73 | 9.37 | 16.68 | 16.67 | 16.49 | 16.35 | 511 | 505 | 499 | −1 | −2 |
| Qatar | 23.24 | 23.51 | 12.32 | 7.30 | 5.15 | 3.85 | −69 | −78 | −83 | −29 | −47 |
| Saudi Arabia | 27.43 | 67.03 | 94.63 | 82.84 | 74.78 | 68.68 | 202 | 173 | 150 | −10 | −17 |
| Somalia | 25.31 | 1839.48 | 1963.58 | 1087.26 | 754.22 | 556.08 | 4196 | 2880 | 2097 | −31 | −49 |
| Sudan | 64.08 | 580.63 | 806.73 | 786.51 | 684.77 | 610.11 | 1127 | 969 | 852 | −13 | −22 |
| Syria | 4.13 | 7.42 | 6.84 | 6.52 | 8.00 | 9.49 | 58 | 94 | 130 | 23 | 46 |
| Tunisia | 7.11 | 24.71 | 53.83 | 60.73 | 45.02 | 35.08 | 754 | 533 | 394 | −26 | −42 |
| UAE | 8.57 | 26.03 | 60.81 | 114.14 | 94.42 | 80.62 | 1232 | 1002 | 841 | −17 | −29 |
| Yemen | 36.13 | 61.71 | 66.80 | 69.27 | 81.94 | 94.26 | 92 | 127 | 161 | 18 | 36 |
| Total | 422.57 | 8141.65 | 10434.52 | 6554.88 | 4674.17 | 3526.31 | 1451 | 1006 | 734 | −29 | −46 |
UAE United Arab Emirates.
Most countries in the region showed increasing mortality rates, except Qatar (35%), Kuwait (28%), Egypt (26%), Bahrain (24%), and Lebanon (13%) which showed decreased rates. Djibouti (985%) and Egypt (339%) showed a prominent rise in mortality rates by 2030, according to estimates from GBD and UNAIDS, respectively. Table 5 shows the prediction and growth rate of age-standardized mortality rates and mortality rates between 1990 and 2030 (Table 5 and Fig. 2).
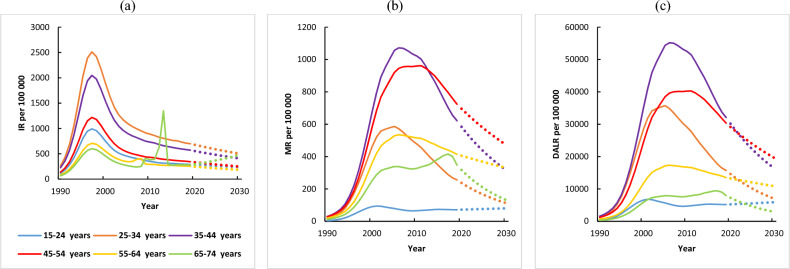
The estimated increase in DALY by 2030 was most marked in Djibouti, Sudan, Somalia, and Iran. Moreover, Iran (71%), Syria (46), Yemen (36), and Libya (35%) have the highest growth rate of DALY between 2019 and 2030 (Table 6 and Fig. 3). Additionally, the trends in incidence, mortality, and DALY (1990–2019) and their prediction (2019–2030) in the region are presented in Fig. 4a–c.
Figure 4.
Total trends in (a) incidence, (b) mortality, and (c) disability-adjusted life years (1990–2019) and prediction (2020–2030) per 100,000 from HIV in MENA countries (GBD).
APC model analysis results of HIV incidence, mortality rates, and DALY
Table 7 shows the estimated impact of age, period, and birth cohort of the whole population on the age-standardized incidence rate, mortality rates, and DALY of HIV in the region. The IE algorithm was used for quantitative analysis among different age groups and periods.
Table 7.
The age-period-cohort model analysis results of HIV incidence, mortality, and disability-adjusted life years in MENA countries (GBD).
| Index | Age | Period | Cohort | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Range | Coefficient | SE | P value | Range | Coefficient | SE | P value | Range | Coefficient | SE | P value | |
| Incidence | 15–24 years | – | – | – | 1990–94 | – | – | – | 1960–64 | 0.053 | 0.048 | <0.001 |
| 25–34 years | – | – | – | 1995–99 | – | – | – | 1965–69 | −0.028 | 0.030 | <0.001 | |
| 35–44 years | −1.113 | 0.015 | <0.001 | 2000–04 | −1.460 | 0.015 | <0.001 | 1970–74 | −0.019 | 0.023 | <0.001 | |
| 45–54 years | −0.266 | 0.015 | <0.001 | 2005–09 | 0.093 | 0.016 | <0.001 | 1975–79 | −0.199 | 0.017 | <0.001 | |
| 55–54 years | 0.110 | 0.019 | <0.001 | 2010–14 | 0.315 | 0.018 | <0.001 | 1980–84 | 0.064 | 0.016 | <0.001 | |
| 65–74 years | 0.496 | 0.023 | <0.001 | 2015–19 | −0.140 | 0.020 | <0.001 | 1985–89 | −0.027 | 0.018 | <0.001 | |
| – | – | – | – | – | – | – | – | 1990–94 | −0.009 | 0.021 | <0.001 | |
| – | – | – | – | – | – | – | – | 1995–99 | 0.018 | 0.026 | <0.001 | |
| – | – | – | – | – | – | – | – | 2000–04 | 0.052 | 0.039 | <0.001 | |
| Mortality | 15–24 years | – | – | – | 1990–94 | – | – | – | 1960–64 | −0.039 | 0.117 | <0.001 |
| 25–34 years | – | – | – | 1995–99 | – | – | – | 1965–69 | 0.020 | 0.054 | <0.001 | |
| 35–44 years | −1.102 | 0.033 | <0.001 | 2000–04 | −0.772 | 0.041 | <0.001 | 1970–74 | 0.050 | 0.034 | <0.001 | |
| 45–54 years | −0.627 | 0.019 | <0.001 | 2005–09 | −0.712 | 0.022 | <0.001 | 1975–79 | 0.031 | 0.025 | <0.001 | |
| 55–54 years | −0.460 | 0.019 | <0.001 | 2010–14 | −0.173 | 0.019 | <0.001 | 1980–84 | −0.076 | 0.020 | <0.001 | |
| 65–74 years | 0.253 | 0.024 | <0.001 | 2015–19 | −0.040 | 0.019 | <0.001 | 1985–89 | −0.088 | 0.020 | <0.001 | |
| – | – | – | – | – | – | – | – | 1990–94 | −0.155 | 0.024 | <0.001 | |
| – | – | – | – | – | – | – | – | 1995–99 | −0.057 | 0.036 | <0.001 | |
| – | – | – | – | – | – | – | – | 2000–04 | 0.075 | 0.039 | <0.001 | |
| Disability-adjusted life years | 15–24 years | – | – | – | 1990–94 | – | – | – | 1960–64 | −0.023 | 0.023 | <0.001 |
| 25–34 years | – | – | – | 1995–99 | – | – | – | 1965–69 | 0.022 | 0.010 | <0.001 | |
| 35–44 years | −1.108 | 0.004 | <0.001 | 2000–04 | −0.784 | 0.005 | <0.001 | 1970–74 | 0.051 | 0.006 | <0.001 | |
| 45–54 years | −0.662 | 0.002 | <0.001 | 2005–09 | −0.677 | 0.003 | <0.001 | 1975–79 | 0.028 | 0.004 | <0.001 | |
| 55–54 years | −0.505 | 0.003 | <0.001 | 2010–14 | −0.159 | 0.002 | <0.001 | 1980–84 | −0.071 | 0.003 | <0.001 | |
| 65–74 years | 0.179 | 0.004 | <0.001 | 2015–19 | −0.052 | 0.002 | <0.001 | 1985–89 | −0.114 | 0.002 | <0.001 | |
| – | – | – | – | – | – | – | – | 1990–94 | −0.146 | 0.003 | <0.001 | |
| – | – | – | – | – | – | – | – | 1995–99 | −0.040 | 0.004 | <0.001 | |
| – | – | – | – | – | – | – | – | 2000–04 | 0.495 | 0.009 | <0.001 | |
The age effect of HIV incidence, mortality rates, and DALY showed a net decrease of 0.83, 0.29, and 0.01 from the age of 35–74 years (the lowest value 35–44 years age group as a reference). According to period effects, there is a significant upward trend in the risk of incidence, mortality rates, and DALY from HIV among the total population. According to the analysis of cohort effects, the incidence, mortality rates, and DALY from HIV have no clear or consistent trend. The 1972–1975 period had the lowest cohort effect on incidence risk from HIV. Also, the 1990–1994 period had the lowest cohort effect on mortality and DALY risk from HIV in the region (Table 7).
Discussion
Our study showed that the incidence and mortality of HIV have increased in most countries in the MENA region from 1990 to 2019. Iran and Egypt showed the highest annual growth rates in incidence, while Qatar and Somalia experienced substantial reductions in incidence based on the modeling results using GBD and UNAIDS estimates, respectively. Djibouti and Iran had the highest mortality rates according to the modeling results using GBD and UNAIDS estimates, respectively, whereas Qatar had the lowest mortality rate according to both datasets. Moreover, incidence trends from 21 countries in a period of 30 years reported that a total of 14 and 11 countries experienced increases in the annual growth rate according to the GBD and UNAIDS estimates, respectively. Up to five out of 21 countries showed a reduction in mortality trends according to GBD information, with Qatar being the only country to demonstrate a significant decrease in mortality rate according to both estimates. Regarding the incidence rate, Iran, Egypt, Tunisia, Libya, and Djibouti exhibited the highest percentage of change from 1990 to 2019, while Lebanon, Morocco, Syria, and Somalia reported the lowest percentage of change in HIV incidence. A higher percentage of change in the HIV mortality rates is found in Sudan, UAE, Somalia, and Djibouti, while Syria, Lebanon, and Bahrain reported the lowest percentage of change in the mortality rate of HIV. We also found an increasing pattern of DALY in most countries in the region.
Our findings showed that most countries in the region encountered an increase in the incidence of HIV from 1990 to 2019 which is consistent with other studies9,18–21, while the global incidence of the disease was decreasing19,20,22. However, the incidence rate of HIV in MENA countries was lower than the global incidence rate22. A study, which followed the trend of HIV in the MENA region from 1999 to 2017, showed that the average global incidence rate of HIV declined dramatically from 36.52 to 25.05 per 100,000 population. The incidence rate of HIV in the countries of MENA was lower than the mean global incidence rates. In all other countries of the region except Sudan, the incidence, prevalence, mortality, and DALY rates were reported to be lower than the global average20. However, it is important to note that harm reduction and HIV prevention programs in most MENA countries have faced significant challenges due to security crises, as well as political, social, and financial obstacles23. For example, several countries in the region, such as Afghanistan, Iraq, Libya, Syria, and Yemen, have experienced an influx of refugees as a result of ongoing conflicts. The conflict in Syria, in particular, has placed a significant burden on neighboring countries like Lebanon, Jordan, and, to a lesser extent, Egypt. It is crucial to acknowledge that substance use, including injecting drug use, among refugee and immigrant populations is often neglected within the realm of public health, despite being recognized as an important risk environment for substance-related harm, including HIV transmission23,24. According to the World Health Organization (WHO), a total of 83 countries worldwide have repressive laws that create barriers to the HIV response. Additionally, 33 countries and territories still have the death penalty for drug offenses, with 16 of these countries located in the MENA region25. Furthermore, in the MENA region, the availability and validity of data on FSWs and MSMs are hindered by various barriers, including stigma and other factors20,26,27. Thus, making direct comparisons between countries in the region and those in Europe and North America becomes challenging due to these data limitations.
In this study, based on the GBD data, the incidence trend was increasing in 14 out of 21 countries, stable in five, and decreasing in only two countries. Also, according to UNAIDS data, there was an increase in 11 out of 14 countries and a decrease in 2 countries. These findings suggest that a significant proportion of countries in the region may lack effective programs to reduce HIV incidence or face challenges in implementing existing programs successfully. On the other hand, the increase in incidence can be attributed, at least in part, to improved diagnosis in these countries. In any case, these countries are likely experiencing a combination of different situations, and all aspects of each country need to be examined to obtain an accurate result. While the incidence trend decreased in Qatar and Bahrain during the whole period, it increased in Iran, Egypt, Iraq, Libya, Palestine, Tunisia, and Yemen. In the rest of the countries, the trend was unsteady. The significant decreasing trend we observed in Qatar was consistent with findings from a cohort study during a 17-year period, which demonstrated the lower incidence rate of HIV in comparison to the world average28. Shakiba, et al., reported Qatar as the country with the lowest HIV burden in 2017 in the region20. The declining trend of the HIV incidence rate in Qatar coincided with the implementation of diagnostic activity and the consumption of antiretroviral therapy29. This reduction trend may be explained by earlier diagnosis and implementation of the curative intervention. The HIV screening programs, prophylaxis, and early use of antiretroviral therapy may lead to a decrease in the rate of HIV-related morbidity and mortality28. The possible reasons for the reduction of morbidity and mortality of HIV in Qatar maybe the regular implementation of HIV early screening programs for immigrants, especially if they stay for more than one month, as well as premarital, pre-employment, and antenatal screening. Furthermore, HIV treatment is available for all patients29,30. In the MENA region, Egypt has the fastest-increasing newly discovered HIV cases (25-30% annually in the past 10 years)24. Whereas, based on modelling results from the WHO mortality database, 2001–2018, Egypt had the lowest age-standardized death rate (ASDR) for males (0.2/100,000) and modelling results showed a positive percent change in ASDR for females (114.38% between 2001 and 2015). In 2018, the disparity in ASDR rates in males, measured using rate ratios was the lowest rate observed in Egypt31.
In this study, utilizing GBD data, we observed that the trend of HIV-related mortality was increasing in 15 out of 21 countries, stable in two countries, and decreasing in four countries. Similarly, according to UNAIDS data, there was an increase in HIV-related mortality in 13 out of 14 countries and a decrease in one country. The total death trend in most MENA countries was increasing. But looking at the last years of the graphs, the death rate due to AIDS has decreased in most countries. This suggests that in recent years, these countries have made efforts to implement programs proposed by WHO and UNAIDS aimed at reducing HIV incidence and mortality, although the degree of success achieved thus far may be limited32,33. Only in Iran, Iraq, and Libya, the death trend has always been increasing, even in the last years of the study. Similar to the results presented here, Hasankhani, et al., in separate modelling revealed an ascending trend for the incidence and mortality of this disease in Iran over the past three decades34. According to the results of another study carried out in Iran, the raw number of mortality, incidence, and burden of HIV increased from 2008 to 2016 in Iran35. Studies about the trends of HIV incidence in Iran have shown that a change in the pattern of HIV transmission from injecting the drug to unsafe sexual contact has resulted in an increased number of HIV-positive cases among women36. Another explanation for the higher incidence could be attributed to the shortage of educational and preventive programs, lack of knowledge, social stigma, low access to counselling and diagnostic service, and prognostic diagnostic technique in the Iranian population34. The increase in HIV infection notifications is difficult to interpret because of changes in the availability of tests, and the willingness of both health professionals and individuals to be tested37.
This study predicted incidence and mortality results based on both GBD and UNAIDS databases. Based on GBD data, both incidence and mortality rates were decreasing in Qatar, Bahrain, Kuwait, and Lebanon. However, based on UNAIDS data, it was estimated that the incidence rate will decrease in Somalia, Djibouti, and Morocco, and the mortality rate will decrease only in Qatar. Based on both databases, it was estimated that the incidence and mortality rate will increase for most of the MENA countries, with the largest increase predicted for Iran. In 2019, Khalifa et al. conducted a study to predict the number of people living with HIV and the number of new HIV infections worldwide using UNAIDS data and Spectrum software. The findings indicated that the number of people living with HIV in the MENA region would increase until 2030 and gradually decrease thereafter, with a similar trend observed for the number of new HIV infections. However, the study did not report these indices by country, providing regional-level projections instead38.
In this study, different epidemiological patterns are observed in the five periods identified by the Joinpoint Regression analysis during the studied period. In most countries in the MENA region, the rising tendency in the incidence and mortality rate was the most pronounced in trends 1 and 2 (1990–2004). The drop in these rates can be explained by increased access to prevention, early diagnosis, and care services for HIV infection37. Significant progress in HIV response in the region has been witnessed in recent years. For instance, Algeria and Morocco have made remarkable progress in growing access to HIV care services. However, other countries, including Somalia and Sudan, have encountered considerable challenges1,39. A notable gap between available care services and required facilities existed in the region; the existing resources in 2020 were less than 20% of what is needed to boost HIV programs and achieve the 2025 targets1 Progress towards the 2030 targets will depend on cooperation between organizations, linking the HIV service to efforts to reach universal health coverage and improved access to reproductive health and social protection systems. These programs will be achieved with a stronger commitment from governments and more emphasis on the recognition of the social and economic impacts of HIV on the Sustainable Development Goals1.
Despite the expectation of similar results, some countries showed completely different trends in the data obtained from the two different datasets (GBD and UNAIDS). For example, the death rate in Egypt and Lebanon decreased based on GBD data but increased based on UNAIDS data. Similarly, the incidence rate for Qatar was decreasing based on GBD data, but increasing based on UNAIDS data. Except for some inconsistencies mentioned in the results obtained from the two different data, the incidence and mortality rates in the rest of the countries in the two data although not the same had almost similar results. One of the reasons for this discrepancy is that the GBD data calculated age-adjusted incidence and mortality rates, while the UNAIDS data calculated incidence and mortality rates. Another reason may be the different sources of data collection in some countries, which led to different results. In general, in countries where both incidence and mortality rates are decreasing, it can be concluded as a sign of correct policy making and planning and the accurate implementation of these programs. In countries where both the incidence and mortality rates are increasing, it is probably a sign of the lack of a correct program or proper implementation of existing programs. In these countries, it is difficult to conclude that the increase in incidence is due to the improvement in disease diagnosis. In countries where one of the incidence or mortality rates is increasing and the other is decreasing, it will be a very complicated task to interpret the results and more investigations will be needed.
Limitation
There are several limitations to the present analysis that need to be considered. First, we used two databases (GBD and UNIAIDS) to compute the AAPC. These databases can recognise only in-care patients diagnosed by physicians; therefore, there is a possibility of underestimating the results in modelling. Hence, our findings of modelling may underestimate the true incidence and mortality rate of HIV in the region. Although the GBD 2019 made various modifications to the source and evaluation of the HIV incidence to improve data accuracy, it was obvious that some deviations in the precision and completeness of the GBD data were unavoidable. To come up with this issue, we used two databases for modelling to cross-validate the results. Thus, both databases to estimate the trend of HIV infection in MENA countries have their particular advantage and restriction. The results of both of them showed a significant increase in incidence and mortality rates in most countries in the region, so there are not enough claims to identify a better database for our modelling. The outputs of the two sources supported each other in the majority of countries.
Second, it is essential to acknowledge the potential risk of the ecological fallacy, which arises from making individual-level inferences based on aggregate-level data. Despite the limitations, our study offers a comprehensive depiction of HIV status in MENA countries. This analysis provides an extensive overview of the trend of HIV infection and mortality in MENA countries.
Conclusion
Our study found increasing incidence and mortality rates, as well as DALYs, associated with HIV in several countries across the MENA region. Future studies are needed to explore the underlying mechanisms for these epidemiological trends with potential risk factors incorporated into further analysis. To effectively address this rising trend and control the epidemic, policymakers must prioritize preventive measures in each country, including educating the pathways of transmission, informing and using the early detection methods, and timely treatment. We suggest that governments should strengthen HIV prevention and treatment programs, especially in countries with high incidence and mortality of HIV. Special attention should be directed toward improving HIV testing scale-up approaches, designing targeted interventions, expanding harm reduction services, and enhancing HIV surveillance systems. There is still plenty of room for improvement to achieve public health goals, such as HIV elimination in the MENA. Some structural interventions like addressing stigma and discrimination, and implementing supportive laws for key populations and people living with HIV are necessary to manage the epidemic in this region.
Supplementary Information
Acknowledgements
The authors thank the HIV/STI Surveillance Research Center, and WHO Collaborating Center for HIV Surveillance, Institute for Futures Studies in Health, Kerman University of Medical Sciences.
Author contributions
Z.K., M.B.H. and M.K. have contributed to the acquisition, analysis, and interpretation of data and writing the manuscript. A.J.K., Y.J. and H.S. have contributed to the conception and design of the work and writing the manuscript. All authors have approved the final draft.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author upon reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
These authors contributed equally: Zahra Khorrami and Mohammadreza Balooch Hasankhani.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-023-40743-z.
Reference
- 1.Pandey A, Galvani AP. The global burden of HIV and prospects for control. Lancet HIV. 2019;6(12):e809–e811. doi: 10.1016/S2352-3018(19)30230-9. [DOI] [PubMed] [Google Scholar]
- 2.UNAIDS. Global HIV & AIDS statistics. 2020 [cited 2022 2/22]; https://www.unaids.org/en/resources/fact-sheet.
- 3.UNAIDS. Global AIDS Strategy 2021–2026. End inequalities. End AIDS. . 2021; https://www.unaids.org/sites/default/files/media_asset/global-AIDS-strategy-2021-2026_en.pdf.
- 4.Nasirian, M., M. Karamouzian, and A.-A. Haghdoost, Why is the number of HIV/AIDS-related publications low in the MENA region? Sexually transmitted infections, 2013. 89(Suppl 3): p. iii10-iii10. [DOI] [PMC free article] [PubMed]
- 5.Karamouzian M, Sharifi H. Simulating HIV dynamics in the Middle East and North Africa. Lancet HIV. 2022;9(7):e454–e455. doi: 10.1016/S2352-3018(22)00129-1. [DOI] [PubMed] [Google Scholar]
- 6.Global, A., Update. Confronting Inequalities-Lessons for pandemic responses from 40 years of AIDS. Geneva, Switzerland: UNAIDS Joint United Nations Programme on HIV/AIDS, 2021.
- 7.Chemaitelly H, et al. HIV incidence and impact of interventions among female sex workers and their clients in the Middle East and North Africa: A modelling study. Lancet HIV. 2022;9(7):e496–e505. doi: 10.1016/S2352-3018(22)00100-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mumtaz GR, et al. HIV incidence among people who inject drugs in the Middle East and North Africa: Mathematical modelling analysis. J. Int. AIDS Soc. 2018;21(3):e25102. doi: 10.1002/jia2.25102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gökengin D, et al. HIV/AIDS: Trends in the Middle East and North Africa region. Int. J. Infect. Dis. 2016;44:66–73. doi: 10.1016/j.ijid.2015.11.008. [DOI] [PubMed] [Google Scholar]
- 10.Zhou W, et al. Joinpoint regression analysis for the mortality trend of breast cancer in Chinese female from 1987 to 2014. J. Central South Univ. Med. Sci. 2018;43(2):210–215. doi: 10.11817/j.issn.1672-7347.2018.02.018. [DOI] [PubMed] [Google Scholar]
- 11.Global Burden of Disease (GBD). 2019. http://ghdx.healthdata.org/gbd-results-tool. Accessed 23 April 2022.
- 12.UNAIDS. AIDSinfo Online Database. In: UNAIDS, editor: UNAIDS; Accessed 23 April 2022.
- 13.Stover J, Brown T, Marston M. Updates to the Spectrum/Estimation and Projection Package (EPP) model to estimate HIV trends for adults and children. Sex. Transm. Infect. 2012;88(Suppl 2):i11–i16. doi: 10.1136/sextrans-2012-050640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 2000;19(3):335–351. doi: 10.1002/(SICI)1097-0258(20000215)19:3<335::AID-SIM336>3.0.CO;2-Z. [DOI] [PubMed] [Google Scholar]
- 15.Chen HS, et al. Predicting US-and state-level cancer counts for the current calendar year: Part I: Evaluation of temporal projection methods for mortality. Cancer. 2012;118(4):1091–1099. doi: 10.1002/cncr.27404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu L, et al. Predicting US-and state-level cancer counts for the current calendar year: Part II: Evaluation of spatiotemporal projection methods for incidence. Cancer. 2012;118(4):1100–1109. doi: 10.1002/cncr.27405. [DOI] [PubMed] [Google Scholar]
- 17.Nielsen B. apc: An R package for age-period-cohort analysis. R J. 2015;7(2):52. doi: 10.32614/RJ-2015-020. [DOI] [Google Scholar]
- 18.Karamouzian M, et al. Improving the quality and quantity of HIV data in the middle east and North Africa: Key challenges and ways forward. Int. J. Health Policy Manag. 2017;6(2):65–69. doi: 10.15171/ijhpm.2016.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.SeyedAlinaghi S, et al. HIV in Iran: Onset, responses, and future directions. AIDS. 2021;35(4):529–542. doi: 10.1097/QAD.0000000000002757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shakiba E, et al. Epidemiological features of HIV/AIDS in the Middle East and North Africa from 1990 to 2017. Int. J. STD AIDS. 2021;32(3):257–265. doi: 10.1177/0956462420960632. [DOI] [PubMed] [Google Scholar]
- 21.UNAIDS, Miles to Go, the Response to HIV in the Middle East and North Africa, in Global AIDS Updates. 2018.
- 22.UNAIDS, Miles to Go, Closing Gaps, Breaking Barriers, Righting Injustices, in Global AIDS Update. 2018.
- 23.Aaraj E, Chrouch MJA. Drug policy and harm reduction in the Middle East and North Africa: The role of civil society. Int. J. Drug Policy. 2016;31:168–71. doi: 10.1016/j.drugpo.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 24.Strathdee SA, et al. HIV and risk environment for injecting drug users: The past, present, and future. Lancet. 2010;376(9737):268–84. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gallahue, P. and R. Lines, The Extreme Fringe of Global Drug Policy. In the Death Penalty for Drug Offences. 2015.
- 26.Ballouz T, Gebara N, Rizk N. HIV-related stigma among health-care workers in the MENA region. Lancet HIV. 2020;7(5):e311–e313. doi: 10.1016/S2352-3018(19)30401-1. [DOI] [PubMed] [Google Scholar]
- 27.Delabre RM, et al. Fear of stigma from health professionals and family/neighbours and healthcare avoidance among PLHIV in Morocco: Results from the Stigma Index survey Morocco. BMC Public Health. 2022;22(1):1705. doi: 10.1186/s12889-022-14010-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ali M, et al. HIV and AIDS-defining opportunistic illnesses in the state of Qatar: A cohort population-based retrospective study covering 17 years (2000–2016) Ann. Med. Surg. 2022;78:103842. doi: 10.1016/j.amsu.2022.103842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ali M, Qasim M, AlSoub H. AIDS-defining opportunistic illnesses in Qatar, 2000–2016: A cohort study. J. Emerg. Med. Trauma Acute Care. 2021;2021:29. doi: 10.5339/jemtac.2021.qhc.29. [DOI] [Google Scholar]
- 30.Al Soub H, et al. Epidemiology and the changing face of HIV infection in Qatar. Infect. Dis. Clin. Pract. 2018;26(4):220–223. doi: 10.1097/IPC.0000000000000626. [DOI] [Google Scholar]
- 31.Jani C, et al. Trends of HIV mortality between 2001 and 2018: An observational analysis. Trop. Med. Infect. Dis. 2021;6(4):173. doi: 10.3390/tropicalmed6040173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.UNAIDS, Middle East and North Africa, Regional Report 2018-2019. 2020: Geneva, Switzerland.
- 33.UNAIDS, Middle East and North Africa, Regional Report 2020. 2021: Geneva, Switzerland.
- 34.Hasankhani, M.B., et al., Trend Analysis of HIV/AIDS Burden in Iran: Results from the Global Burden of Disease 2017 Study. Medical Journal of the Islamic Republic of Iran, 2021. 35. [DOI] [PMC free article] [PubMed]
- 35.Moradi G, et al. Incidence, mortality, and burden of HIV/AIDS and its geographical distribution in Iran during 2008–2016. Iran. J. Public Health. 2019;48(1):1–9. [Google Scholar]
- 36.Mirzaei M, et al. Survival rate and the determinants of progression from HIV to AIDS and from AIDS to the death in Iran: 1987 to 2016. Asian Pacific J. Trop. Med. 2019;12(2):72. doi: 10.4103/1995-7645.250840. [DOI] [Google Scholar]
- 37.Melo MC, Almeida VC, Donalísio MR. Trend incidence of HIV-AIDS according to different diagnostic criteria in Campinas-SP, Brazil from 1980 to 2016. Ciência Saúde Coletiva. 2021;26:297–307. doi: 10.1590/1413-81232020261.08652019. [DOI] [PubMed] [Google Scholar]
- 38.Khalifa A, et al. Demographic change and HIV epidemic projections to 2050 for adolescents and young people aged 15–24. Glob. Health Action. 2019;12(1):1662685. doi: 10.1080/16549716.2019.1662685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hermez J, et al. A review of HIV testing and counseling policies and practices in the Eastern Mediterranean Region. AIDS. 2010;24:S25–S32. doi: 10.1097/01.aids.0000386730.56683.e5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and analysed during the current study are available from the corresponding author upon reasonable request.