Abstract
Purpose
The objectives of this study were to describe child characteristics associated with later autism spectrum disorder (ASD) identification and the health status and educational transition plans of adolescents with ASD.
Methods
Longitudinal population-based surveillance cohort from the Autism Developmental Disabilities Monitoring Network during 2002–2018 in 5 catchment areas in the United States. Participants included 3,148 children born in 2002 whose records were first reviewed for ASD surveillance in 2010.
Results
Of the 1,846 children identified in the community as an ASD case; 11.6% were first identified after age 8 years. Children were more likely to have ASD identified at older ages who were Hispanic; were born low birth weight; were verbal; had high intelligence quotient or adaptive scores; or had certain co-occurring neuropsychological conditions by age 8 years. By age 16 years, neuropsychological conditions were common with more than half of children with ASD having a diagnosis of attention-deficit/hyperactivity disorder or anxiety. Intellectual disability (ID) status was unchanged for the majority (>80%) of children from ages 8 to 16 years. A transition plan was completed for over 94% of children, but disparities were observed in planning by ID status.
Conclusion
A high percentage of adolescents with ASD have co-occurring neuropsychological conditions, markedly higher than at age 8. While most adolescents had transition planning, this occurred less often for those with ID. Ensuring access to services for all people with ASD during adolescence and transition to adulthood may help to promote overall health and quality of life.
Keywords: Autism spectrum disorder, public health surveillance, health care transition, adolescence, intellectual disability, educational transition planning
Improvements over time in community identification of autism spectrum disorder (ASD) during childhood have led to an increase in the ASD population that may seek services and supports.1–3 People continue to be newly identified with ASD into adolescence and adulthood although there are disparities associated with timing of identification.4,5 Despite impairments associated with ASD persisting through the life course, many adolescents and young adults experience a decrease in supports and services, sometimes called a “service cliff,” that starts during high school6 and continues when they age out of the school system or no longer can access pediatric health care providers.7,8 Data from the National Longitudinal Transition Survey-2 (NLTS2) among young adults in 2009 who received special education under an ASD eligibility found that 37% had never worked nor attended post-secondary education (e.g., college or vocational training) and few (19%) had lived independently.9 Even with this demonstrated need for planning, the NLTS2 found that only 58% of children with ASD had an educational transition plan by the federally required age.9,10 Moreover, recent data show children with ASD are more likely to have co-occurring mental health or other conditions than children without ASD.11, 12 Just 1 in 10 adolescents with ASD had completed health care transition planning recommended by the American Academy of Pediatrics for all children.13 Beginning planning for transition to adulthood early in health and education settings may help ensure adolescents are linked to the necessary supports and services they will need as adults.
Historically, proportionally few federally-funded ASD activities specifically focused on lifespan issues, including the transition of youth with ASD to adulthood.14,15 Increasing ASD transition-age research, services, and supports were identified as priority areas in the 2019 Autism Collaboration, Accountability, Research, Education and Support Act, including calls for surveillance of adolescents and adults with ASD.16,17 The existing data on the transition period among youth with ASD primarily rely on self-reported survey data limited to children with an autism special education eligibility, or longitudinal or clinical studies with small sample sizes; further, the seminal findings from the NLTS2 are based on children who were adolescents over 2 decades ago.13,18–22
This report marks an expansion of the Centers for Disease Control and Prevention’s ASD surveillance to capture the adolescence period to help communities identify health care needs and gaps in transition planning for youth with ASD.23 The aims of this report are to understand child characteristics associated with later ASD identification (after age 8 years) and to describe the health status and educational transition plans of adolescents with ASD.
Methods
Population and Data Collection
Children born in 2002 whose health and education records were reviewed for ASD surveillance in the 2010 Autism and Developmental Disabilities Monitoring (ADDM) Network surveillance year (SY2010) were followed-up during the 2018 ADDM Network surveillance year (SY2018) at age 16 years at five sites (Arkansas, Georgia, Maryland, Utah, and Wisconsin).23,24 Prior selection for review in SY2010 was based on the presence of ASD-specific information from special education exceptionalities or health provider billing codes.24 For SY2018, we reviewed education and health records from 2011–2018 for these children and linked these follow-up data to SY2010 data. See sample selection details in Figure 1. The surveillance activity was determined to be exempt by the CDC Institutional Review Board (Human Subjects Research 31806).
Figure 1.
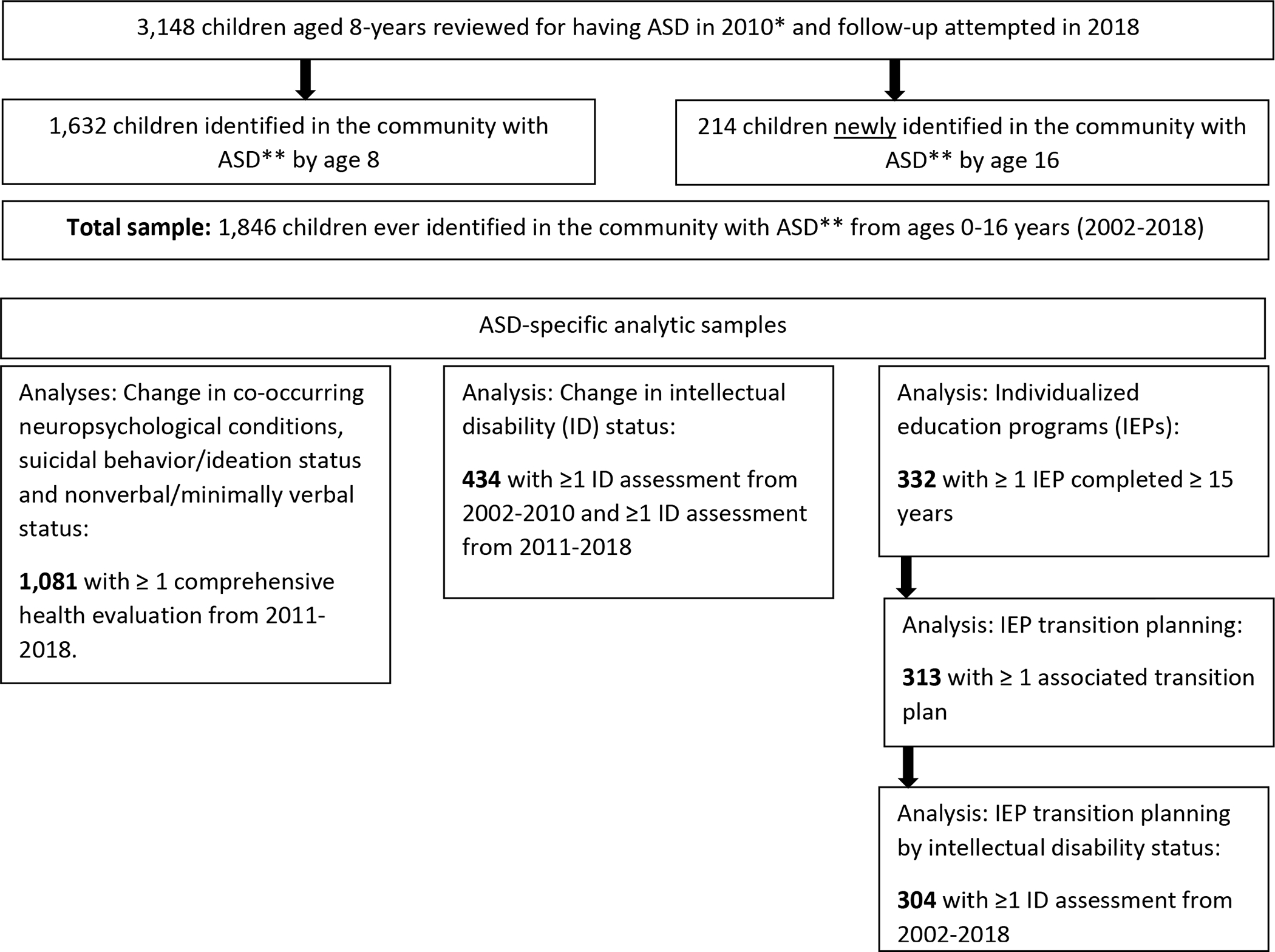
Study Population and Analytic Samples — Autism and Developmental Disabilities Monitoring Network, 5 sites, United States, 2018
Case Ascertainment
Children were determined to be ASD cases if they lived in the study area in 2010 and ever had a written statement from a qualified professional diagnosing ASD on a comprehensive evaluation (e.g., developmental assessment, neurological evaluation, psychological evaluation, individualized education program), a special education classification of autism in public school, or an ASD International Classification of Diseases (ICD) code obtained from administrative or billing information.23
Variable Definitions
Data collected in 2010.
Demographic data from 2002–2010 included sex, race/ethnicity, and birth characteristics (preterm, low birthweight, and maternal age at birth) for children with linked birth certificate data.
ADDM Network staff clinicians reviewed evaluations and documented whether children had ever been diagnosed with attention-deficit/hyperactivity disorder (ADHD), anxiety, depression, epilepsy, or obsessive-compulsive disorder or had documentation of self-injurious or aggressive behavior. Whether an ASD diagnosis or special education classification was ever ruled out in an evaluation was also documented. Scores from most recent intelligence quotient (IQ) and adaptive composite tests were used to classify children into cognitive (≤70, 71–85, >85) and adaptive functioning (≤70 and >70) categories. Children were considered nonverbal or minimally verbal if any of the following were identified in the records during clinician review: 1) most recent evaluation at ≥48 months of age describing a child as nonverbal; 2) language classified as primarily echolalia or jargon; or 3) being administered an Autism Diagnostic Observation Scale Module 1 (an assessment appropriate for nonverbal or minimally verbal children) at age ≥48 months.
Data collected in 2018.
As some children may have moved from the study area after 2010, limiting the amount of information available during 2011–2018, we documented the last known period a child resided in the study area as a proxy for available information using the most recent year of 1) known study area address (from service or other records), 2) a comprehensive evaluation, or 3) an Individualized Education Program (IEP). Children with none of these items were categorized as having an unknown residence location after 2010.
Similar to SY2010, historical and current diagnoses of selected co-occurring neuropsychological conditions, documented rule-outs of ASD, and most recent IQ composite tests were collected from records. Children were considered nonverbal/minimally verbal or having suicidal behavior/ideation if any evaluation included these descriptions.
The Individuals with Disabilities Education Act (Part B)25 requires a transition plan by age 16 years that includes an IEP. Select data from IEPs from ages 9–16 years were collected, including whether a child ever had a transition plan, an assessment of transition needs, a course of study to meet post-secondary goal(s), and post-secondary goals for education/training, career/employment, and independent living skills/daily living skills/community participation.
Analytic Methods
Children with ASD were categorized into younger (≤ 8 years) and older (9–16 years) age of identification based on their earliest ASD diagnosis, eligibility, or ICD code. Known child characteristics at age 8 years were compared for those identified ≤ 8 years versus 9–16 years using Pearson’s chi-square tests or Fisher’s exact tests when cell sizes were <5 for categorical variables and t-tests for continuous variables.
Among children with ≥ 1 comprehensive evaluation from a health source reviewed during 2011–2018, lifetime occurrence of co-occurring neuropsychological conditions or an ASD rule out by age 8 years and by age 16 years was estimated. Sex comparisons were made during both ASD identification time periods using two-sample tests of proportions.
Ninety-five percent confidence intervals (CIs) using the Wilson method were calculated around percentages for being non-verbal or exhibiting suicidal behavior/ideation by age 16 years. The estimate of children with intellectual disability (ID) (statement from a qualified professional that a child has an intellectual disability or an IQ ≤7026) by age 8 years and the change in status by age 16 years was calculated among those with an ID assessment before and after 8 years.
Among children who lived in the study area at age 16 years with ≥ 1 IEP between ages 15–16 years, the percentage who ever had a transition plan completed was estimated (transition plan data were unavailable in Wisconsin due to limitations in accessing educational records). Among the subset of children with ≥ 1 transition plan at age ≥ 15 years, the percentages who ever had selected components in their transition plan completed were estimated. For all IEP measures, 95% CIs using the Wilson method were calculated and differences by sex and ID status were assessed using two-sample tests of proportions. P values <0.05 were considered statistically significant. Stata SE/17.0 and R were used for data management and analyses.
Results
Of 3,148 8-year-old children whose records were reviewed in 2010 for ASD, by age 16 years, 1,846 were ever identified in the community as an ASD case (Table A1 and Table A2). While the vast majority were identified by age 8 years, 11.6% (214) were first identified during ages 9–16 years. Among ASD cases, 87.6% had a clinical diagnosis of ASD (Table A3).
Children who were non-Hispanic, born with appropriate birth weight, were nonverbal/minimally verbal, or who had lower IQ or adaptive scores were more likely to be identified ≤ 8 years compared to ages 9–16 years (Table 1). A diagnosis of anxiety, depression, or ADHD, or having ≥ 1 instance of ASD ruled out by age 8 years was associated with later age of identification.
Table 1.
Comparison of characteristics of children at age 8 years by period when ASD was first identified (n = 1846) — Autism and Developmental Disabilities Monitoring Network, 5 sites, United States, 2018
| First Identification Period |
|||||
|---|---|---|---|---|---|
| Overall | ≤ 8 years (n = 1632) |
9–16 years (n = 214) |
P Valuea | ||
| Missing (%) | No. (%b) | No. (%) | No. (%) | ||
|
| |||||
| Total | 1632 (88) | 214 (12) | |||
|
| |||||
| Demographic information | |||||
| Sex | 0 | 0.10 | |||
| Female | 339 (18) | 291 (18) | 48 (22) | ||
| Male | 1507 (82) | 1341 (82) | 166 (78) | ||
| Race (non-Hispanic) | 12 | 0.81 | |||
| White | 1245 (76) | 1105 (76) | 140 (79) | ||
| Black | 273 (17) | 247 (17) | 26 (15) | ||
| American Indian or Alaska Native |
6 (<1) | 5 (<1) | 1 (1) | ||
| Asian or Pacific Islander | 47 (3) | 43 (3) | 4 (2) | ||
| Other Race or Multiple Races |
58 (4) | 52 (4) | 6 (3) | ||
| Ethnicity | 2 | 0.003 | |||
| Non-Hispanic | 1629 (90) | 1452 (91) | 177 (84) | ||
| Hispanic | 179 (10) | 146 (9) | 33 (16) | ||
| Birth characteristics | |||||
| Preterm | 44 | 0.85 | |||
| No | 870 (84) | 772 (84) | 98 (83) | ||
| Yes | 170 (16) | 150 (16) | 20 (17) | ||
| Low Birthweight | 23 | 0.05 | |||
| No | 1258 (88) | 1109 (89) | 149 (84) | ||
| Yes | 168 (12) | 139 (11) | 29 (16) | ||
| Maternal Age at Birth, mean (SD), years | 23 | 28.4 (6.1) | 27.6 (6.0) | 0.13 | |
| Clinical/behavioral characteristics | |||||
| IQ Score | 24 | 0.002 | |||
| ≤70 | 424 (30) | 394 (32) | 30 (19) | ||
| 71–85 | 327 (23) | 287 (23) | 40 (25) | ||
| >85 | 652 (47) | 560 (45) | 92 (57) | ||
| Adaptive Score | 50 | 0.04 | |||
| ≤70 | 507 (55) | 471 (56) | 36 (44) | ||
| >70 | 412 (45) | 367 (44) | 45 (56) | ||
| Verbal Statusc | 0 | <0.001 | |||
| Verbal | 1547 (84) | 1350 (83) | 197 (92) | ||
| Nonverbal/Minimally Verbal |
299 (16) | 282 (17) | 17 (8) | ||
| Self-Injury | 0 | 0.40 | |||
| No | 1265 (69) | 1113 (68) | 152 (71) | ||
| Yes | 581 (32) | 519 (32) | 62 (29) | ||
| Aggression | 0 | 0.93 | |||
| No | 737 (40) | 651 (40) | 86 (40) | ||
| Yes | 1109 (60) | 981 (60) | 128 (60) | ||
| ADHD | 0 | 0.001 | |||
| No | 1335 (72) | 1200 (74) | 135 (63) | ||
| Yes | 511 (28) | 432 (26) | 79 (37) | ||
| Anxiety | 0 | 0.05 | |||
| No | 1545 (84) | 1376 (84) | 169 (79) | ||
| Yes | 301 (16) | 256 (16) | 45 (21) | ||
| Depression | 0 | <0.001 | |||
| No | 1814 (98) | 1610 (99) | 204 (95) | ||
| Yes | 32 (2) | 22 (1) | 10 (5) | ||
| Epilepsy | 0 | 0.46 | |||
| No | 1753 (95) | 1552 (95) | 201 (94) | ||
| Yes | 93 (5) | 80 (5) | 13 (6) | ||
| OCD | 0 | 0.30 | |||
| No | 1824 (99) | 1611 (99) | 213 (>99) | ||
| Yes | 22 (1) | 21 (1) | 1 (<1) | ||
| ASD Ruled Out | 0 | <0.001 | |||
| No | 1574 (85) | 1419 (87) | 155 (72) | ||
| Yes | 272 (15) | 213 (13) | 59 (28) | ||
Abbreviations: ASD, autism spectrum disorder; CI, confidence interval; SD, standard deviation; IQ, intelligence quotient; OCD, obsessive compulsive disorder; ADHD, attention-deficit/hyperactivity disorder.
Footnotes:
P values for categorical variables were Pearson’s chi-square or Fisher’s exact test when cell sizes were <5; for continuous variables were t-tests.
Due to rounding not all columns may sum to 100%
Classified as nonverbal in 2010 based on the presence of any of 3 criteria: (1) most recent autism evaluation noted as “nonverbal” at age >48 months, (2) most recent Autism Diagnostic Observation Scale administered at age >48 months was a module 1, or (3) language noted as primarily echolalia or jargon.
The percentage of children with ASD with a lifetime occurrence of specific co-occurring neuropsychological conditions statistically significantly increased from age 8 to 16 years (Figure 2, Table A4). By age 16, anxiety, depression, and epilepsy, were all more common in females compared to males. There was a larger increase in the percentage with anxiety from age 8 to 16 years for females compared to males. By age 16, the most common co-occurring neuropsychological conditions were ADHD and anxiety. Among all children with ASD, 14.7% had ASD ruled out before ASD was eventually identified with the majority of all ASD rule outs by age 8 years; there were no sex differences in lifetime occurrence of ASD ruled out by age 8 or age 16 years (data not shown).
Figure 2.
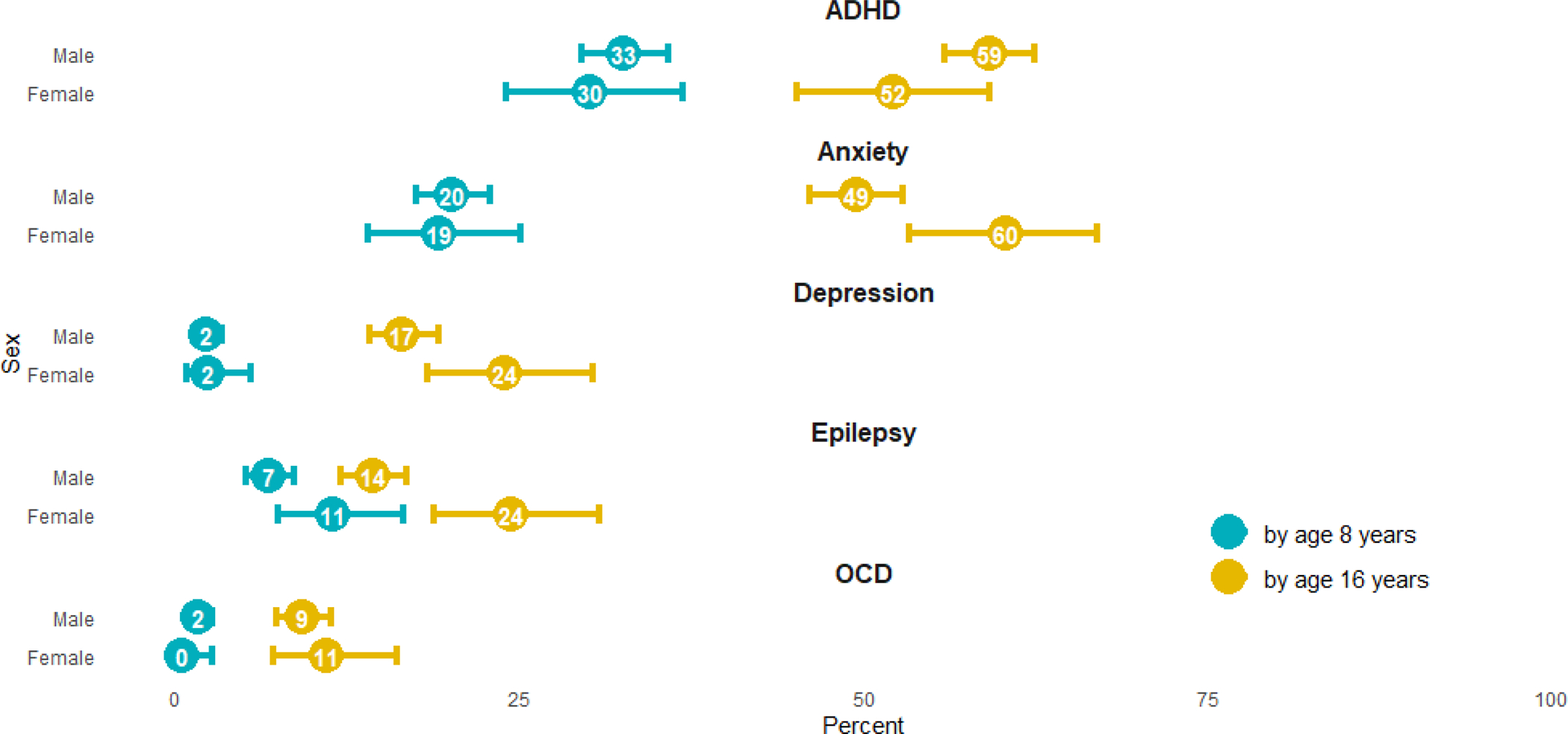
Differences in lifetime occurrence of specific co-occurring neuropsychological conditions, by age 8 years and age 16 years, and by sex (n=1081)a — Autism and Developmental Disabilities Monitoring Network, 5 sites, United States, 2018
Among children with an IQ score before and after age 8 years, 32.0% had ID by age 8 years compared to 36.6% by age 16 years (increase of 4.6%, 95% CI: 2.1–9.0) (Figure 3). The same ID status was maintained for 80.2% while 12.2% changed from no ID to having ID and 7.6% changed from ID to no ID.
Figure 3.
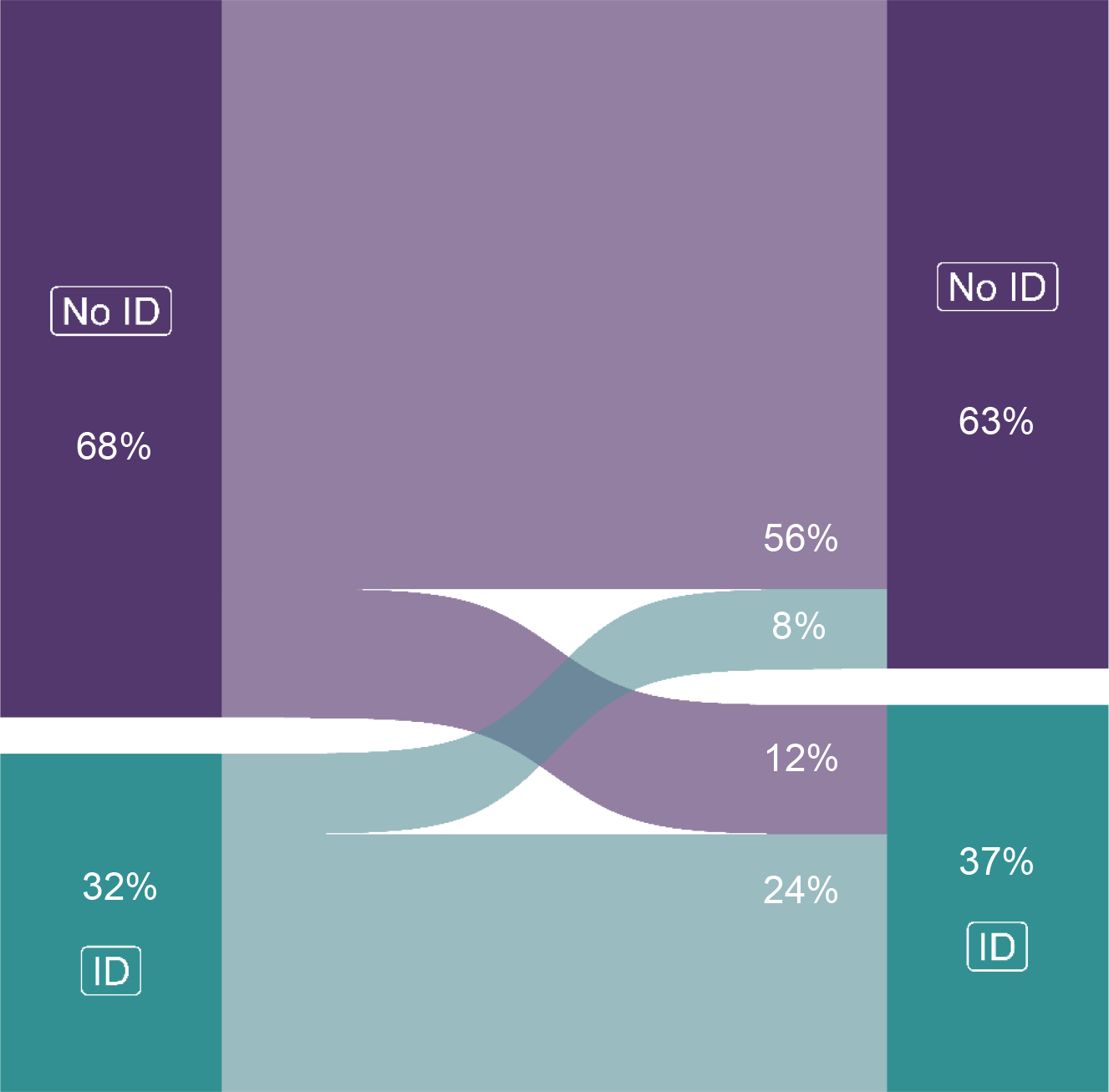
Change in the percentage of children with ASD with intellectual disabilitya from age 8 to 16 years (n=434)b — Autism and Developmental Disabilities Monitoring Network, 5 sites, United States, 2018
Among children with ASD by age 16 years, suicidal behavior/ideation was noted for 16.8% (95% CI: 14.7–19.2) and 14.8% (95% CI: 12.7–17.1) were nonverbal/minimally verbal (data not shown).
Of the 332 children who lived in the study area at age 16 years with ≥ 1 IEP at ages 15–16 years, 94.3% (95% CI: 91.2–96.3) had a least one transition plan associated with an IEP (data not shown). While no differences in presence of a transition plan were found by sex, those with ID were less likely to have a transition plan than those without ID (90.0%, 95% CI: 84.5–94.9 versus 96.5%, 95% CI: 93.0–98.3; p = 0.034).
Among children with a transition plan (n=313), over 95% had at least 1 assessment of their transition needs, course of study to meet their post-secondary goals, and education/training and career/employment post-secondary goals (Table A5). Only 65.5% (95% CI: 60.1–70.5) had at least 1 independent living skills/daily living skills/community participation goal. There were no sex differences in any of these transition planning components (data not shown). Those with ID were more likely to have an independent living skills/daily living skills/community participation goal compared to those without ID (80.9%, 95% CI: 72.6–87.2 versus 56.2%, 95% CI: 49.2–63.0; p <0.001) (Figure 4).
Figure 4.
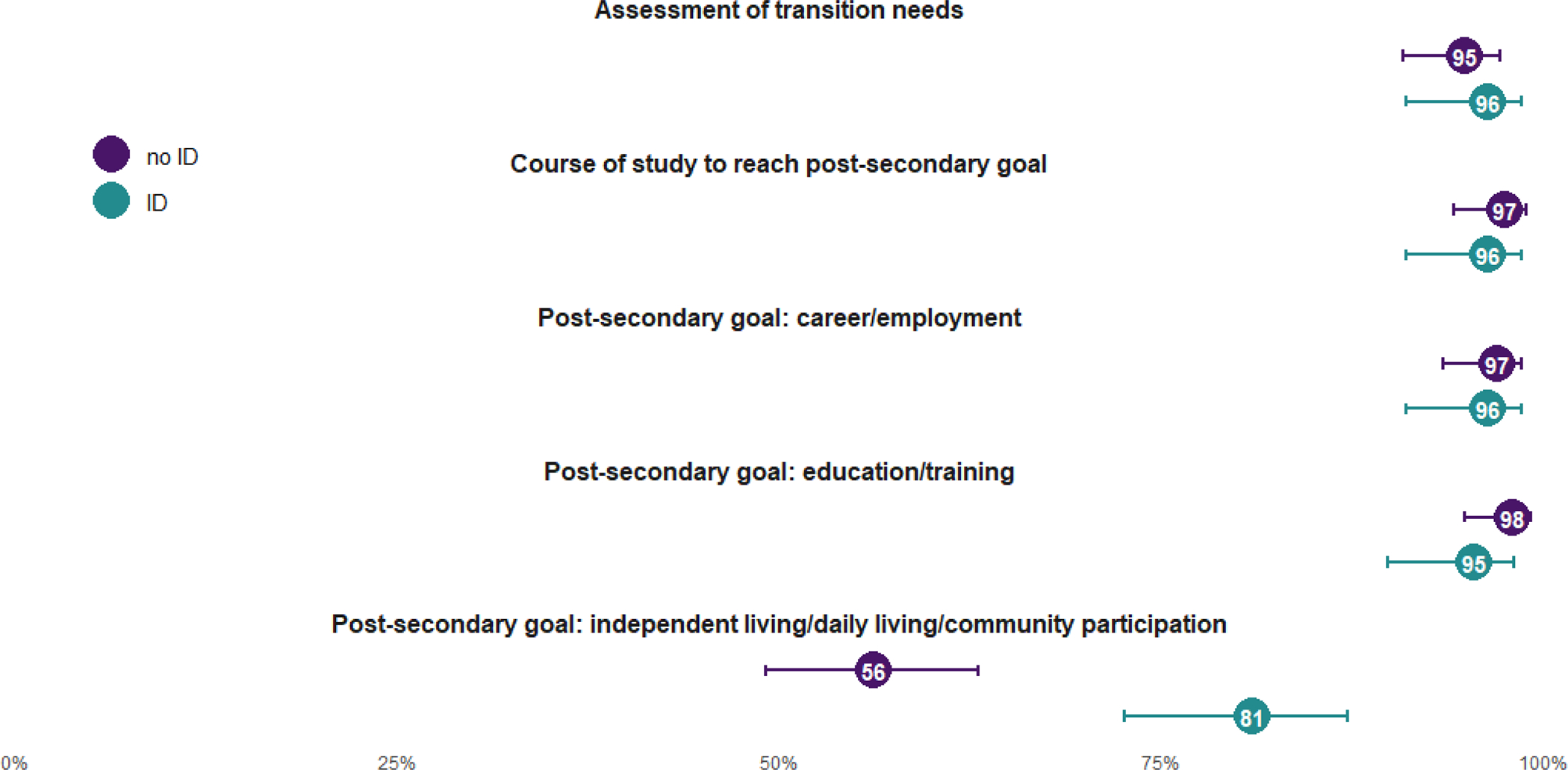
Ever documentation of educational transition planning components by intellectual disability statusa, by age 16 years (n = 304) — Autism and Developmental Disabilities Monitoring Network, 4 sites, United States, 2018
Discussion
Early identification of ASD can ensure that children receive evidence-based interventions to improve developmental outcomes.27 While the majority of children with ASD were identified by age 8 years, more than 1 in 10 were first identified between ages 9–16 years. The estimated percentage of children with ASD identified later is lower than reported by U.S. survey data4 (15–19%) or Canadian surveillance (28%); this lower percentage of later-identified ASD is likely due to the selective follow-up of children living in the surveillance area at age 8 years who had documented symptoms that could potentially indicate ASD.5 In the U.S. survey, children with mild ASD (as described by parents) were more likely to be identified later than children whose ASD was described as severe. Similarly, in the ADDM Network, children who were identified with ASD at older ages were more likely to be verbal and have higher IQ and adaptive functioning scores. Delayed ASD identification may be partly due to less impairment resulting in fewer needs for educational and health services supports. Diagnostic uncertainty may also contribute to later diagnoses. Children with ADHD, anxiety, depression, or at least one instance of ASD being ruled out, by age 8 years, were more likely to be identified at older ages than children without these histories. These neuropsychiatric conditions are common in children with ASD and several of their diagnostic criteria overlap with ASD;28 the presence of these co-occurring conditions may impede the ability to distinguish ASD symptoms as manifestations of ASD. Among all children identified with ASD by age 16 years, approximately 1 in 7 had ASD ruled out before ASD identification. Lastly, given the lower prevalence of ASD in Hispanic children in 2010 compared to non-Hispanic children,24 disparities in access to screening, diagnoses, or educational services may have contributed to Hispanic children being more likely to be identified after age 8 years.29
Neuropsychological conditions were common in children with ASD and substantially increased from age 8 to 16 years. Over half of children had a diagnosis of ADHD or anxiety by age 16 years. These estimates of co-occurring conditions were higher than those observed in a recent follow-up survey of adolescents with ASD11 or in representative national surveys of all children.30,31 Sex differences were more pronounced by age 16 years with females with ASD being more likely to have anxiety, depression, and epilepsy compared to males, similar to previous findings.32,33 Further, almost 17% of children with ASD had indications of suicidal behavior/ideation by age 16 years, likely putting them at risk for early mortality.34 The frequency of co-occurring neuropsychological conditions in this population of 16-year-old children with ASD is substantially higher than reported for the general population of children in this age range, and we observed increased prevalence during adolescence in this population. Therefore, screening for and management of these conditions can help clinicians support overall health care transition planning for youth with ASD;35 caring for the potentially complex needs of adults with ASD may require providers to receive additional training. Despite this need, recent evidence suggests there is a lack of health care transition guidance, especially for adolescents with ASD.11,13
Beyond neuropsychological conditions, many adolescents with ASD will likely need services and supports across their lifespans given that 15% were non-verbal and 37% had ID, among other impairments. While some children’s ID statuses changed, overall, ID status remained relatively stable through age 16 years with 80% of children maintaining their ID status during this period. This finding is in contrast to another study showing IQ gains during adolescence,36 but indicates that challenges associated with ID will likely remain in adulthood.
The vast majority (94%) of children with ASD who were served under a special education exceptionality had at least one transition plan associated with an IEP, which is substantially higher than a previous estimate of 58% from an older cohort.9 Those without a transition plan were more likely to have ID, which may be due to less urgency by educators to meet the deadline of 16 years for children who are more likely to stay in secondary education beyond age 18 years. Previous research found improved post-secondary outcomes for students who begin transition planning by age 14 years, giving two additional years for planning.10 While it was encouraging that most students with ASD received transition planning by age 16 years, additional attention may be needed to ensure students with co-occurring ID also complete transition plans by age 16. Schools may also consider starting the transition planning process earlier; over half of states require an IEP transition plan to be completed earlier than age 16 years.9
Among those who had at least one transition plan, there was high completion (>95%) across all the required transition components. However, the post-secondary goal of independent living skills/daily living skills/community participation, which was non-required, was completed for only 66% of children. Children with ID were more likely to have this goal completed compared to children without ID. While optional, this post-secondary goal is relevant for all children with ASD, and previous surveys show fewer than 1 in 5 children with ASD will live independently as young adults.9 Future analyses to evaluate the content and quality of post-secondary transition goals could better describe planned trajectories for children with ASD.
Limitations
Children who had not yet had contact with health or educational developmental specialists by age 8 years were not included and thus we may have missed children whose first suspicion of ASD occurred after 8 years of age, and our sample may not be representative of all children identified with ASD by age 16 years. Next, lack of data in SY2018 could be because the child no longer lived in the study area or no longer received services where records were reviewed or was able to function without the need for services and thus potentially biasing the population to those with higher needs among those with ASD; some data elements had higher levels of missingness due to variable completion in records. Thus, there may be selection bias in the sample where follow-up data were limited or unavailable through age 16 years. Next, the percentage of adolescents with ASD with co-occurring conditions may be underestimated if these conditions were only documented in a source not included in ADDM surveillance (e.g., primary care practices or billing data). Lastly, site populations may not be representative or generalizable to the state or the United States.
Future surveillance could expand to include the entire population of 16-year-old children in the community with ASD, which was not possible in our study that was only able to include 16-year-old children who had an indication of possible ASD by age 8; this expansion could increase generalizability and population size to better measure potential disparities in health and transition planning. Further, high school records could also be linked to post-secondary employment, education, and independent living outcomes to understand how plans made in high school for the future relate to what occurs after graduation.
In this first ADDM Network report on children aged 16 years with ASD, we identified factors associated with ASD identification after age 8 years that may be useful to providers when screening and diagnosing ASD to ensure that children are identified and receive services as early as possible. A substantial percentage of adolescents with ASD had co-occurring neuropsychiatric conditions, suicidal behavior/ideation, ID, or were non-verbal, indicating the need for screening, management, and transition planning for these conditions. While most children with ASD had at least one educational transition plan created by age 16 years, disparities existed by ID status in timeliness and completeness of transition planning. As impairments associated with ASD generally persist through adulthood, supports and services may be needed during the transition period and through adulthood to promote overall health and quality of life of people with ASD.
Supplementary Material
Implications and Contribution.
This CDC autism surveillance report is the first to include children through adolescence and provides details on the complex educational and health needs among adolescents with autism who likely would benefit from transition to adulthood planning and access to services and supports across their lifespans.
Acknowledgements:
Dr. Li-Ching Lee served as the site Principal Investigator for the Maryland Autism and Developmental Disabilities Monitoring (ADDM) Network site and passed away in 2021. We acknowledge and thank her for her significant contributions to the design and implementation of this project.
Funding/Support:
This surveillance activity was supported by funding from the CDC. CDC led the study design, data collection, data analysis, data interpretation, and writing of the report.
Abbreviations:
- ASD
autism spectrum disorder
- ADHD
attention-deficit/hyperactivity disorder
- NLTS2
National Longitudinal Transition Survey-2
- ADDM
Autism and Developmental Disabilities Monitoring
- SY
study year
- ICD
International Classification of Diseases
- IQ
intelligence quotient
- IEP
Individualized Education Program
- CI
confidence interval
- CDC
Centers for Disease Control and Prevention
Footnotes
Conflicts of Interest: All authors have no conflicts of interest to disclose.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.Dietz PM, Rose CE, McArthur D, Maenner M. National and state estimates of adults with autism spectrum disorder. J Autism Dev Disord. Dec 2020;50(12):4258–4266. doi: 10.1007/s10803-020-04494-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schendel DE, Thorsteinsson E. Cumulative incidence of autism into adulthood for birth cohorts in Denmark, 1980–2012. JAMA. 2018;320(17):1811–1813. doi: 10.1001/jama.2018.11328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Prevalence of autism spectrum disorders--autism and developmental disabilities monitoring network, six sites, United States, 2000. MMWR. Feb 9 2007;56(1):1–11. [PubMed] [Google Scholar]
- 4.Sheldrick RC, Maye MP, Carter AS. Age at first edentification of autism spectrum disorder: An analysis of two US surveys. J Am Acad Child Adolesc Psychiatry. Apr 2017;56(4):313–320. doi: 10.1016/j.jaac.2017.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Autism spectrum disorder among children and youth in Canada in 2018: A report of the national autism spectrum disorder surveillance system (Public Health Agency of Canada; ) (2018). [Google Scholar]
- 6.Laxman DJ, Taylor JL, DaWalt LS, Greenberg JS, Mailick MR. Loss in services precedes high school exit for teens with autism spectrum disorder: A longitudinal study. Autism Res. Jun 2019;12(6):911–921. doi: 10.1002/aur.2113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turcotte P, Mathew M, Shea LL, Brusilovskiy E, Nonnemacher SL. Service needs across the lifespan for individuals with autism. J Autism Dev Disord. Jul 2016;46(7):2480–9. doi: 10.1007/s10803-016-2787-4 [DOI] [PubMed] [Google Scholar]
- 8.Verlenden JV, Zablotsky B, Yeargin-Allsopp M, Peacock G. Healthcare access and utilization for young adults with disability: U.S., 2014–2018. J Adolesc Health. Oct 15 2021;doi: 10.1016/j.jadohealth.2021.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roux A, Shattuck PT, Rast JE, Rava J, Anderson K. National Autism Indicators Report: Transition into Young Adulthood. 2015. https://drexel.edu/~/media/Files/autismoutcomes/publications/National%20Autism%20Indicators%20Report%20-%20July%202015.ashx
- 10.Suk AL, Martin JE, McConnell AE, Biles TL. States decrease their required secondary transition planning age: Federal policy must change. J. Disabil. Policy Stud. 2020;31(2):112–118. doi: 10.1177/1044207320915157 [DOI] [Google Scholar]
- 11.Powell PS, Pazol K, Wiggins LD, et al. Health status and health care use among adolescents identified with and without autism in early childhood - four U.S. sites, 2018–2020. MMWR. Apr 30 2021;70(17):605–611. doi: 10.15585/mmwr.mm7017a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ames JL, Massolo ML, Davignon MN, Qian Y, Croen LA. Healthcare service utilization and cost among transition-age youth with autism spectrum disorder and other special healthcare needs. Autism. 2021/04/01 2020;25(3):705–718. doi: 10.1177/1362361320931268 [DOI] [PubMed] [Google Scholar]
- 13.Leeb RT, Danielson ML, Bitsko RH, et al. Support for transition from adolescent to adult health care among adolescents with and without mental, behavioral, and developmental disorders - United States, 2016–2017. MMWR. Aug 28 2020;69(34):1156–1160. doi: 10.15585/mmwr.mm6934a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Interagency Autism Coordinating Committee (IACC). 2017–2018 IACC Autism Spectrum Disorder Research Portfolio Analysis Report. 2021. https://iacc.hhs.gov/publications/portfolio-analysis/2018/
- 15.Report to Congress: Young Adults and Transitioning Youth with Autism Spectrum Disorder. 2017. https://www.hhs.gov/sites/default/files/2017AutismReport.pdf
- 16.113th Congress. Autism Collaboration, Accountability, Research, Education, and Support Act of 2014. In: 113th Congress, editor: U.S. Government Publishing Office; 2014. [Google Scholar]
- 17.116th Congress. Autism Collaboration, Accountability, Research, Education and Support (CARES) Act of 2019. In: 116th Congress, editor. Public Law No: 116–60: U.S. Government Publishing Office; 2019. [Google Scholar]
- 18.Shattuck PT, Wagner M, Narendorf S, Sterzing P, Hensley M. Post-high school service use among young adults with an autism spectrum disorder. Arch Pediatr Adolesc Med. Feb 2011;165(2):141–6. doi: 10.1001/archpediatrics.2010.279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shattuck PT, Narendorf SC, Cooper B, Sterzing PR, Wagner M, Taylor JL. Postsecondary education and employment among youth with an autism spectrum disorder. Pediatrics. Jun 2012;129(6):1042–9. doi: 10.1542/peds.2011-2864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Roux AM, Shattuck PT, Cooper BP, Anderson KA, Wagner M, Narendorf SC. Postsecondary employment experiences among young adults with an autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. Sep 2013;52(9):931–9. doi: 10.1016/j.jaac.2013.05.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Clarke EB, McCauley JB, Lord C. Post–high school daily living skills in autism spectrum disorder. J Am Acad Child Adolesc Psychiatry. 2021/08/01/ 2021;60(8):978–985. doi: 10.1016/j.jaac.2020.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Newman L, Wagner M, Knokey A-M, et al. The Post-High School Outcomes of Young Adults With Disabilities up to 8 Years After High School: A Report From the National Longitudinal Transition Study-2 (NLTS2). 2011. https://ies.ed.gov/ncser/pubs/20113005/pdf/20113005.pdf [Google Scholar]
- 23.Maenner MJ, Shaw KA, Bakian AV, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2018. MMWR. Dec 3 2021;70(11):1–16. doi: 10.15585/mmwr.ss7011a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention. Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR. Mar 28 2014;63(2):1–21. [PubMed] [Google Scholar]
- 25.U.S. Department of Education. Individuals with Disabilities Act. Section 1414(d). https://sites.ed.gov/idea/statute-chapter-33/subchapter-ii/1414/d [Google Scholar]
- 26.Patrick ME, Shaw KA, Dietz PM, et al. Prevalence of intellectual disability among eight-year-old children from selected communities in the United States, 2014. Disabil Health J. Apr 2021;14(2):101023. doi: 10.1016/j.dhjo.2020.101023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shaw KA, Maenner MJ, Bakian AV, et al. Early Identification of Autism Spectrum Disorder Among Children Aged 4 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2018. MMWR. Dec 3 2021;70(10):1–14. doi: 10.15585/mmwr.ss7010a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCauley JB, Elias R, Lord C. Trajectories of co-occurring psychopathology symptoms in autism from late childhood to adulthood. Dev Psychopathol. Oct 2020;32(4):1287–1302. doi: 10.1017/s0954579420000826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maenner MJ, Shaw KA, Baio J, et al. Prevalence of autism spectrum disorder among children aged 8 years - Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2016. MMWR. Mar 27 2020;69(4):1–12. doi: 10.15585/mmwr.ss6904a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ghandour RM, Sherman LJ, Vladutiu CJ, et al. Prevalence and treatment of depression, anxiety, and conduct problems in US children. J Pediatr. 2019/03/01/ 2019;206:256–267.e3. doi: 10.1016/j.jpeds.2018.09.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Danielson ML, Bitsko RH, Ghandour RM, Holbrook JR, Kogan MD, Blumberg SJ. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. J Clin Child Adolesc Psychol. 2018/03/04 2018;47(2):199–212. doi: 10.1080/15374416.2017.1417860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rødgaard E-M, Jensen K, Miskowiak KW, Mottron L. Autism comorbidities show elevated female-to-male odds ratios and are associated with the age of first autism diagnosis. Acta Psychiatrica Scandinavica n/a(n/a)doi: 10.1111/acps.13345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kirsch AC, Huebner ARS, Mehta SQ, et al. Association of comorbid mood and anxiety disorders with autism spectrum disorder. JAMA Pediatrics. 2019;doi: 10.1001/jamapediatrics.2019.4368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hosozawa M, Sacker A, Cable N. Timing of diagnosis, depression and self-harm in adolescents with autism spectrum disorder. Autism. Aug 8 2020:1362361320945540. doi: 10.1177/1362361320945540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hyman SL, Levy SE, Myers SM. Identification, evaluation, and management of children with autism spectrum disorder. Pediatrics. 2020;145(1):e20193447. doi: 10.1542/peds.2019-3447 [DOI] [PubMed] [Google Scholar]
- 36.Simonoff E, Kent R, Stringer D, et al. Trajectories in symptoms of autism and cognitive ability in autism from childhood to adult life: findings from a longitudinal epidemiological cohort. J Am Acad Child Adolesc Psychiatry. 2020/12/01/ 2020;59(12):1342–1352. doi: 10.1016/j.jaac.2019.11.020 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


