Abstract
The cystic dilatation of the common bile duct (CBD) is a rare pathology in an infant. It is the second-most common surgical cause of cholestatic jaundice in infants after biliary atresia. A 4-month-old female child was admitted to our department with complaints of abdominal distension. The physical examination revealed the presence of a huge palpable mass involving the right hypochondrium up to the right iliac fossa and umbilical region. Ultrasound abdomen revealed a large intra-abdominal cyst but unable to comment on the organ of origin of the cyst due to its huge size. Multidetector computed tomography of the abdomen was suggestive of possible origin of the cyst from CBD extending from porta hepatis to pelvis. At laparotomy, there was a huge choledochal cyst extending from porta hepatis to pelvis. The choledochal cyst was excised, followed by Roux-en-Y hepaticojejunostomy.
Keywords: Choledochal cyst, giant, infant, rare
INTRODUCTION
A choledochal cyst is defined as dilatation of the biliary tree without actual mechanical obstruction.[1] Females are most commonly affected than males with a ratio of 4:1.[2] Abdominal pain, jaundice and palpable mass are classic triads for choledochal cyst, but present in <20% of patients.[3] About 80% of patients will become symptomatic before 10 years of age.[4] Giant choledochal cysts generally present in the older age group. We are reporting a giant choledochal cyst in an infant without cholestatic features which was confirmed by radiological evaluation with multidetector computed tomography (MDCT) scan. It was managed by a classical approach, i.e., excision of cyst, followed by Roux-en-Y hepaticojejunostomy.
CASE REPORT
A 4-month-old female child presented to our outpatient department with complaints of abdominal distension for 1 month, excessive crying during defecation and non-bilious vomiting for 10 days. There was no history of jaundice and fever. Perinatal history was insignificant. The baby was immunised as per age. On general examination, the child was well preserved with a weight of 5.2 kg (birth weight – 2.5 kg), no pallor and icterus were noted. On per abdominal examination, the abdomen was grossly distended with a huge palpable mass of size approximately 15 cm × 12 cm involving the right hypochondrium up to the right iliac fossa and umbilical region. The lump was non-tender with smooth surface and cystic in nature. Finger cannot be insinuated under right costal margin and dullness over lump was continuous with liver dullness.
Laboratory values were: haemoglobin – 12.3 g/dl, total bilirubin – 0.69 mg/dl, glutamic-pyruvic transaminase – 233 IU/L, glutamic oxaloacetic transaminase – 233 IU/L and alkaline phosphatase – 568 IU/L. Ultrasound abdomen revealed a large intra-abdominal cyst but unable to comment on the organ of origin of the cyst due to its huge size. To characterise the lesion and organ of origin, MDCT whole abdomen was done. MDCT abdomen was suggestive of dilatation of intrahepatic biliary radicals with a large cyst measuring 16 cm × 12 cm × 8 cm, with possible origin from common bile duct extending from the porta hepatis to the pelvis [Figure 1a and b]. Due to the increasing symptomatology of the patient in the form of vomiting and progressive abdomen distension, an exploratory laparotomy was planned with a provisional diagnosis of choledochal cyst. On exploration, there was a huge choledochal cyst of size 16 cm × 12 cm extending from the porta hepatis to the pelvis [Figure 2a and b]. The cyst was decompressed before excision and approximately 1 l of bile was aspirated. The giant choledochal cyst was excised followed by Roux-en-Y hepaticojejunostomy. The baby was well in the initial post-operative period for 2 days. Thereafter, she developed features of sepsis which were managed by upgradation of intravenous antibiotics, inotropes and mechanical ventilation. There was no evidence of a bile leak. Despite all the conservative management, she could not be saved and died on the post-operative day 5.
Figure 1.
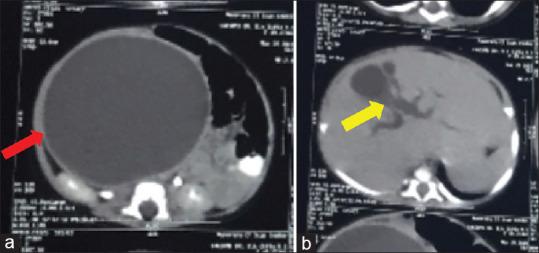
MDCT abdomen showing giant choledochal cyst of size 16 cm × 12 cm × 8 cm (red arrow) (a) and dilated IHBR (yellow arrow) (b). IHBR: Intrahepatic biliary radicals, MDCT: Multidetector computed tomography
Figure 2.
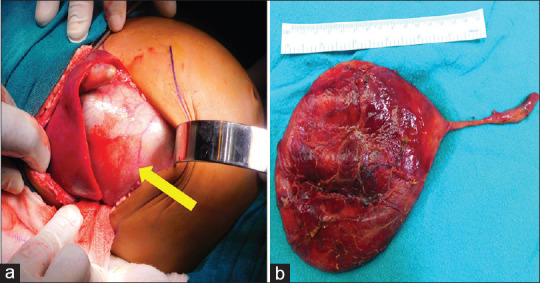
Intraoperative picture of the same patient showing giant choledochal cyst (yellow arrow) (a) and resected specimen (b)
DISCUSSION
Giant choledochal cyst in the infant is very rare and most of these present in the older age group of children.[5] Tang et al. reported a series of 62 children with choledochal cysts with the largest cyst dimension of 158 mm, but the age of the child was not mentioned.[6] Okoromah et al. reported a massive choledochal cyst presenting as an acute abdomen in a 5-month-old female infant.[7] Yurttutan et al. reported a case of a choledochal cyst in a 4-month-old female infant with a maximum cyst diameter of 160 mm.[8] In our index case, the child had neither jaundice nor any other features of cholestasis. This finding is consistent with the observation that a large choledochal cyst has low intracystic pressure and produces less cholestatic effects on the liver.[9] This is probably also the reason for grossly preserved liver functions in our case. The cystic dilatation of the biliary tract is a rare disease. Its symptoms are not specific and vary according to age. The diagnosis of such malformation is based on ultrasound, computed tomography scan and magnetic resonance cholangiopancreatography. Early diagnosis and surgical intervention are important to prevent the development of secondary biliary cirrhosis and malignant degeneration.
CONCLUSION
A giant choledochal cyst is a rare entity. The presentation is with abdominal distension with the absence of features of cholestasis possibly due to low intracystic pressure. Early diagnosis and surgical intervention are important to prevent the development of secondary biliary cirrhosis and malignant degeneration.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the guardian has given consent for the patient’s images and other clinical information to be reported in the journal. The guardian understands that the patient’s name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Soares KC, Arnaoutakis DJ, Kamel I, Rastegar N, Anders R, Maithel S, et al. Choledochal cyst:Presentation, clinical differentiation and management. J Am Coll Surg. 2014;104:816–9. doi: 10.1016/j.jamcollsurg.2014.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miyano T, Yamataka A, Li L. Congenital biliary dilatation. Semin Pediatr Surg. 2000;9:187–95. doi: 10.1053/spsu.2000.18843. [DOI] [PubMed] [Google Scholar]
- 3.Stringer MD, Dhawan A, Davenport M, Mieli-Vergani G, Mowat AP, Howard ER. Choledochal cysts:Lessons from a 20 year experience. Arch Dis Child. 1995;73:528–31. doi: 10.1136/adc.73.6.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hung MH, Lin LH, Chen DF, Huang CS. Choledochal cysts in infants and children:Experiences over a 20-year period at a single institution. Eur J Pediatr. 2011;170:1179–85. doi: 10.1007/s00431-011-1429-2. [DOI] [PubMed] [Google Scholar]
- 5.Anand U, Priyadarshi RN, Kumar B, Khandelwal C. Diagnosis and management of giant choledochal cysts:Complexities compared to smaller cysts. Indian J Gastroenterol. 2013;32:262–7. doi: 10.1007/s12664-013-0335-0. [DOI] [PubMed] [Google Scholar]
- 6.Tang ST, Yang Y, Wang Y, Mao YZ, Li SW, Tong QS, et al. Laparoscopic choledochal cyst excision, hepaticojejunostomy, and extracorporeal Roux-en-Y anastomosis:A technical skill and intermediate-term report in 62 cases. Surg Endosc. 2011;25:416–22. doi: 10.1007/s00464-010-1183-y. [DOI] [PubMed] [Google Scholar]
- 7.Okoromah CN, Odelola MA, Etukudo FS. Complicated massive choledochal cyst:A case report. Niger J Clin Pract. 2002;5:150–2. [Google Scholar]
- 8.Yurttutan N, Karakus SC, Koku N, Demirci M, Ucak R. A giant choledochal cyst in infancy:A case report. Korean J Pediatr. 2016;59:239–41. doi: 10.3345/kjp.2016.59.5.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sharma N, Bhatnagar V, Srinivas M, Agarwala S, Singh MK, Sharma R. Correlation of intracystic pressure with cyst volume, length of common channel, biochemical changes in bile and histopathological changes in liver in choledochal cyst. J Indian Assoc Pediatr Surg. 2014;19:10–6. doi: 10.4103/0971-9261.125946. [DOI] [PMC free article] [PubMed] [Google Scholar]


