Abstract
Purpose
To evaluate the return to sport and daily activities in addition to clinical outcomes after modification of the Brostöm repair, specifically using suture augmentation for concomitant fixation of both the anterior talofibular ligament and calcaneofibular ligament.
Methods
Patients who had grade III ankle sprains and lateral ankle instability, all of whom failed supervised conservative management, were included. Patients underwent a modified Broström procedure consisting of suture augmentation for both the anterior talofibular ligament and calcaneofibular ligament. For clinical outcome evaluation, Foot and Ankle Ability Measure (FAAM) and Karlsson-Peterson Scoring System for Ankle Function questionnaires coupled with questions regarding time of return to sport and level of sports activity were used.
Results
Thirty-one patients were included. The differences in preoperative and postoperative FAAM scores for both the Activities of Daily Living subscale and Sports subscale were significant (P < .001). The FAAM Activities of Daily Living score improved from an average of 46.06 preoperatively to 77.49 postoperatively (P < .001, 99% confidence interval, 26.4–36.4). The FAAM Sports score improved from an average of 4 preoperatively to 19.31 postoperatively (P < .001, 99% confidence interval, 11.6–19.0). For the Karlsson-Peterson Scoring System for Ankle Function, the surveyed population reported a mean of 82.74 points out of 100 post-op (standard deviation 20.14). The mean time to return to sport activity was 5.72 months. Mean follow-up time was 24.12 months.
Conclusions
This variant Broström procedure with suture anchors and augmentation of both the anterior talofibular ligament and calcaneofibular ligament was effective in helping patients return to their preinjury functionality level in both daily life and sports activity.
Level of Clinical Evidence
Level IV, therapeutic case series.
Introduction
Ankle sprains are common injuries in the general population and in athletes.1 Ankle sprains commonly occur during sport activity but have been found to be the most common musculoskeletal injury regardless of type of sport or activity leading to injury.2,3,4,5 Most ankle sprains result from an inversion-supination mechanism and involve the ligaments of the lateral ankle, most notably the anterior talofibular ligament (ATFL) and calcaneofibular ligament (CFL).6 The ATFL, which is the primary structure injured in a lateral ankle sprain, prevents anterior talar displacement. The CFL is the second structure injured in a lateral ankle sprain and functions to prevent excessive inversion.7 Notably, it has been reported that two-thirds of all ankle sprains are isolated to the ATFL, but a combined injury to the ATFL and CFL occurs in 20% of ankle sprains.7,8 Lateral ankle sprains are graded on a scale of I to III, determined by anatomical disruption and laxity on physical exam.9 Grade I sprains involve stretching of the ATFL, grade II sprains involve partial rupture of the ATFL with mild instability, and grade III sprains involve complete rupture of the ATFL and CFL with marked instability.10 Most lateral ankle sprains can be treated conservatively with functional rehabilitation; however, ∼20% of patients with an acute complete tear of the lateral ankle ligament complex cannot regain stability without surgery.11 Gerber et al. reported that chronic ankle instability develops in 20-40% of ligamentous ankle injuries.12 This instability can result in functional inadequacy and require surgical correction.13 Additionally, meta-analysis has suggested that operative management of ruptured lateral ligaments leads to better outcomes than nonoperative management.14 Also, residual instability can result from lateral ankle sprains, and the presence of residual instability is a predictor of repeat injury.15 Therefore, surgery is a good option for patients with grade III sprains that have failed conservative treatment to reduce the risk of instability and recurrent sprains, as well as enabling prompt return to preinjury function and activity.
The gold standard surgical treatment for lateral ankle instability is the Broström procedure, which involves direct repair of the remnant ATFL with suture.16 Broström described this repair in 1966, and Gould et al. modified this procedure in 1980, introducing advancement of the inferior extensor retinaculum in addition to the repair.17 The Broström-Gould procedure was further modified by Hu et al., who used suture anchors to repair both the ATFL and CFL back to the fibula.18 The Broström repair is an excellent option for patients with preserved remnants of the ATFL and CFL but is contraindicated in patients with poor remnant ligament quality and general joint laxity.19 Other limitations to the Broström procedure exist. It has been questioned whether the Broström is an adequate procedure for patients with weakened native tissue from long-standing ankle instability and in patients with large body mass indices, or athletes, both of whom are likely to place extra stress on the ankle.20,21 Further, Waldrop et al. reported that direct suture repair of the ATFL and use of suture anchors in the fibula or talus had significantly inferior strength compared with an intact ATFL in a cadaveric model.22 To address these concerns, ligament augmentation using suture tape has been introduced.23 Suture augmentation is a ligament repair bridging concept using suture tape and bone anchors to reinforce ligament strength, acting as a secondary stabilizer after repair to prevent recurrence of injury.24 A modified Broström repair with suture augmentation has produced promising results.25 Biomechanical studies have reported a mechanical superiority of suture-tape augmentation of the ATFL.26,27,28 That being said, specific indications, functional outcomes, and return to sport with utilization of suture augmentation remain unclear. The purpose of this study was to evaluate the return to sport and daily activities in addition to clinical outcomes after modification of the Broström repair, specifically using one suture augmentation for concomitant fixation of both the ATFL and CFL. We hypothesize that patients will return to their preinjury level of activity after this procedure.
Materials and Methods
Patient Population
This retrospective study was approved by the Royal Oak Beaumont Institutional Review Board in compliance with all applicable federal regulations governing the protection of human subjects.
Patients undergoing ligament reconstruction for chronic lateral ankle instability using a variant of the Broström procedure with suture anchors and augmentation of both the ATFL and CFL between 2016 and 2018 were identified from surgical records. The inclusion criteria were grade III ankle sprains with lateral ankle instability and a normal hindfoot alignment, specifically no varus deformity. In addition, all patients failed at least a 6-month course of supervised conservative management. Any patient with concomitant ankle pathology or ankle malalignment identified on preoperative imaging was excluded. Preoperative MRIs and alignment view radiographs were performed for each patient to assess for additional pathology and malalignment. All surgeries were performed by one of two fellowship-trained orthopaedic surgeons (Z.V. and A.G.) specializing in the modified Broström technique. This modified technique involves suture anchors and suture-tape and augmentation with the utilization of a suture augmentation for both the ATFL and the CFL.
Surgical Technique
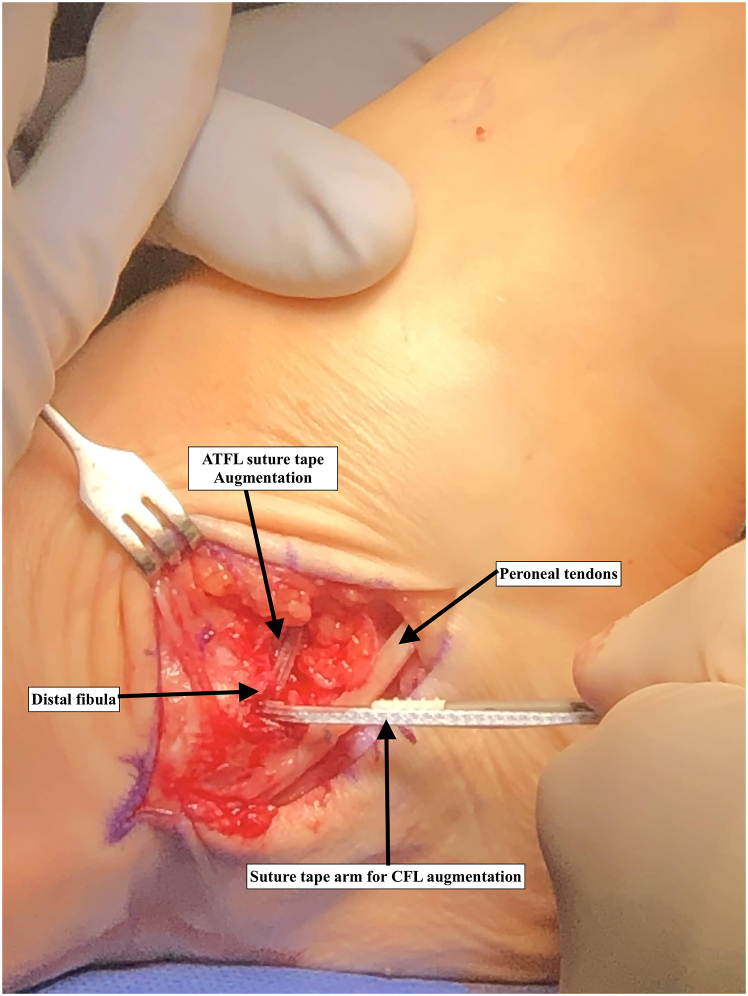
All patients were operated on in the supine position. After exsanguination, a thigh tourniquet was inflated. Standard anterolateral and anteromedial portals were used for ankle arthroscopy. Structures were palpated with a probe to assess for cartilage health. Attention was then turned to the repair of the ATFL and CFL. An incisional mark was made starting at the tip of the lateral fibula. A longitudinal incision was made at the tip of the lateral fibula with a 15-blade scalpel, penetrating skin and subcutaneous tissue. Blunt dissection was used down to the periosteum, and crossing vessels were subsequently cauterized with a Bovie. A small rent was then made to split the peroneal sheath. Peroneus longus and brevis tendons were identified and retracted away to prevent damage. A 15-blade scalpel was used to remove the capsule off the distal end of the tibia and fibula at the origin of the AFTL and CFL. Blunt dissection was performed deep in the capsule just anterior to the lateral articular surface of the talus, and a guidewire from the suture augmentation (Arthrex InternalBrace [Naples, FL]) was placed. Appropriate positioning of the guidewire was confirmed with C-arm fluoroscopy. A 4.75-mm SwiveLock loaded with FiberTape was then tapped into place with a mallet after appropriate drilling. A bump was then placed behind the leg, allowing the talus to fall posterior relative to the tibia. The anatomic origin of the ATFL was drilled and tapped, and 3.0-mm SutureTaks were subsequently placed on each side. The SutureTaks were then passed distally into the joint capsule recreating the ATFL and CFL. The SutureTak ends were tied to themselves, and a strand from each was secured into the lateral face of the fibula with a 2.5-mm PushLock. The FiberTape was then secured into the anatomic origin of the ATFL with suture anchors. A periosteal elevator was placed deep to the peroneal tendons, and C-arm fluoroscopy was used to identify the CFL insertion to guide accurate drilling. A 4.75-mm Arthrex SwiveLock was used to secure the FiberTape into the lateral aspect of the calcaneus (Fig 1). All steps described were performed with the ankle in neutral dorsiflexion and slight eversion. Range of motion and ligamentous laxity were assessed immediately after surgery, before skin closure.
Fig 1.
Operative image of the lateral ankle. Patient is in the supine position.
Postoperative Protocol
For weeks 0-2, patients were splinted and non-weight bearing. Weight-bearing was progressively increased in a walking boot from weeks 3 to 6 and ankle range of motion was initiated during this time. During weeks 7 to 8, patients were weight-bearing as tolerated in an ankle brace. Patients progressively returned to sport activity as tolerated 4-6 months postoperatively.
Data Collection
Clinical outcome surveys were conducted by a blinded member of the orthopedic staff after receiving a consent form. These surveys consisted of the Foot and Ankle Ability Measure (FAAM) and Karlsson-Peterson scoring criteria, as well as other general questions regarding qualitative and quantitative metrics relevant to the procedure. The other metrics collected included the type of injury sustained, time to return to sports and athletic activity, quality of said activity compared to presurgical baselines, and overall patient satisfaction. When considering return-to-sports activity, patients were asked to rate their current ability to engage in activity on a scale of 1-10. This metric was standardized, as follows. The 10 represented each patient’s ability to play before any injury was sustained, and therefore, their self-reported score would determine the level at which they were able to return as compared to their own baselines.
Statistical Analysis
Two-tailed t-tests were conducted on the preoperative and postoperative average scores obtained for each of the considered subscales: FAAM ADL and FAAM Sports. Karlsson-Peterson scoring criteria was only obtained postoperation; therefore, comparative statistics were not used. Summary and descriptive statistics were determined for time since surgery (postoperative time), patient age, and patient sex.
Results
Patient Population Characteristics
Thirty-one patients, 14 males and 17 females, met the inclusion criteria for this study. The patients had a mean age of 40.74 years (range: 20-69) and a mean follow-up of 24.06 months (range: 4-50). All but one of the patients claimed that they would have repeated the surgery again (96.77%). The one patient who would not have repeated the procedure claimed it was because their ankle had such little functionality to begin with that the marginal benefit experienced postoperation was outweighed by the burden of having to be operated on and recover once again. Overall, the mean rating the patients gave the surgery was 83.23 out of 100. A diagnostic arthroscopy was performed in all patients to assess for concomitant injuries, which were not present in any of the included patients.
FAAM and Karlsson-Peterson Questionnaire Results
The average score for the preoperative FAAM ADL subscale was 46.07 out of a possible 84. The average postoperative FAAM ADL subscale score was 77.49, a statistically significant improvement compared to preoperative scores (P < .001; 99% confidence interval 26.4–36.4) (Table 1). There was also a significant improvement in the postoperative FAAM Sports subscale compared to preoperation. The average postoperative FAAM Sports score was 19.31, compared to 4 preoperatively (P < .001, 99% confidence interval 11.6–19.0) (Table 1). The Karlsson-Peterson score postoperative average was 82.74 out of possible 100, indicative of excellent postoperative return of functionality (Table 1).
Table 1.
FAAM and Karlsson Scoring Criteria
| Preoperative Average | Standard Deviation | Postoperative Average | Standard Deviation | P Value | 99% Confidence Interval | |
|---|---|---|---|---|---|---|
| FAAM ADL | 46.07 | 8.36 | 77.49 | 10.61 | <0.001∗ | 26.43–36.41 |
| FAAM Sports | 4 | 3.34 | 19.31 | 8.11 | <0.001∗ | 11.62–19.00 |
| Karlsson-Peterson | 82.74 | 20.14 |
ADL, activities of daily living; FAAM, foot and ankle ability measure.
Statistically significant improvement in preoperative to postoperative scores.
Return to Sport
Of the 31 patients sampled, 14 of them claimed to be involved in recreational sport activity before they suffered an ankle injury, of which 12 were able to resume activity by the time the survey was administered. For these 14 patients, the average time to return to the activity was 5.71 months, and the average level at which they returned was determined to be 8.43 (Table 2). As aforementioned, the level of return is as compared to an individualized baseline. The standard deviations for the time to return and the level to return are listed in Table 2.
Table 2.
Patient Characteristics and Return to Sport Metrics
| Mean | Standard Deviation | |
|---|---|---|
| Age (years) | 40.74 | 13.31 |
| Mean Follow Up (months) | 24.06 | 10.96 |
| Number of Patients Engaged in Sports | 14 | |
| Time to Return of Sport (months) | 5.71 | 2.91 |
| Level of Return to Sport (1-10) | 8.43 | 1.29 |
| Overall Satisfaction with Surgery (Yes/No) (%) | 96.77 | |
| Surgery Rating (1-100) | 83.23 | 12.02 |
Discussion
Lateral ankle sprains are common orthopaedic injuries with an incidence of 2.5/1,000 person years.29 The first line management of these injuries is conservative physical therapy, but 20-40% of lateral ankle sprains result in recurrent instability.12 Surgery is indicated when patients continue to have symptoms of chronic lateral ankle instability after a 3 to 6-month course of physical rehabilitation and have lateral ankle instability on physical exam and imaging.30 The issue of recurrent instability has established a trend toward earlier surgical management after conservative measures have failed, particularly in high-level athletes and patients with mechanical ligamentous laxity.31 Tourne et al. details a review of surgical options, which are broadly categorized as repair or reconstruction of the lateral ankle ligaments.32 Reconstruction is used when the injured ligaments cannot be reinserted to their attachment sites, even with reinforcement. Options for graft include fibular periosteum, peroneus tertius, gracilis, plantar tendon, and allograft. The gold standard of lateral ankle ligamentous repair is the Broström-Gould procedure, which involves suturing of the torn ligaments to their attachment sites and reinforcement using the extensor retinaculum. The repair can also be achieved with synthetic reinforcement, such as the use of suture augmentation in our current study. The effectiveness of suture augmentation has been reported in some studies. Sarhan et al. found that polyester tape augmentation improved American Orthopaedic Foot and Ankle Society (AOFAS) and FAAM median scores in patients with lateral ankle instability.33 Xu et al. compared a modified Broström repair with and without augmentation using suture tape and found that patients with suture tape augmentation had significantly improved total outcome scores compared to the group without suture tape augmentation.25
Additionally, previous studies have evaluated the use of suture augmentation and its effect on return to sport, but only using suture augmentation for fixation of the ATFL. Yoo and Yang found that patients treated with suture augmentation were able to return to sport and activity quickly. They reported that the rate of returning to sports 12 weeks after surgery was significantly different between patients who did and did not receive suture augmentation. 81.8% of patients in the suture augmentation group returned to sport activity without limitations at 12 weeks versus 27% of patients without suture augmentation.34 Although this study reaffirms the effectiveness of using suture augmentation to correct lateral ankle instability and provides evidence that suture augmentation could potentially expedite return to sport, fixation of the CFL in addition to the ATFL was not investigated. To our knowledge, the use of suture augmentation for the fixation of both the ATFL and CFL and its effect on clinical outcome and return to sport has not been studied.
Whether to repair both the ATFL and CFL is debatable. A consensus statement published by Song et al. provided a recommendation that ATFL and CFL reconstruction be considered in patients with subtalar instability in addition to tears of both major lateral ligaments.30 This recommendation was supported by the findings of Maffuli et al., which compared singular ATFL and combined ATFL and CFL repair. Overall, they concluded that it is not necessary to repair the CFL in primary procedures based on their findings that clinical symptoms and talocrural joint motion measured on stress radiographs were similar when comparing singular ATFL and combined ATFL and CFL repair.35 However, 10 patients in the Maffuli study continued to have recurrent sprains and pain. These 10 patients also had subtalar joint instability, leading to the recommendation that CFL repair should be considered in patients with subtalar joint instability. That being said, Maffuli et al. did not assess athletes returning to sport when a CFL repair is included in surgery, as we did in our investigation. A cadaveric study comparing a two-ligament reconstruction group (ATFL and CFL) to a single ligament reconstruction group (ATFL only) found that the single ligament reconstruction can provide as much initial stability as a two-ligament reconstruction, as measured on stress radiograph with application of anterior drawer and varus stress forces.11 Despite there being no differences in anterior displacement, daily activity and return to sport outcomes could not be elucidated because of the design of this study. These clinical outcomes are important measures to evaluate when determining if fixation of both the ATFL and CFL is warranted. Further, a 2019 study found that ATFL and CFL ligament augmentation using suture tape for chronic ankle instability provided comparable intermediate-term clinical outcomes to the modified Broström repair.23 This study was limited due to the fact that it only included females under the age of 40 years with a body mass index under 28 and, therefore, the findings could not be generalized to patients that were male, had a high body mass index, or were high-demand athletes.
Return to sport is an important outcome measure when assessing management of lateral ankle sprains. Surgery is a good option for patients intending to return to their preinjury level of sport because it can maximize recovery and function.36 There is a lot of pressure in modern sports for a rapid return to activity, further emphasizing the importance of using return to sport as an outcome measure. However, there is a clear deficiency in the literature pertaining to a timeline of return to sport. Anatomical ligament reconstruction using a Broström-Gould procedure with suture anchors to treat lateral ankle instability has been found to be effective in restoring preinjury functional levels in high-demand athletes, as 94% of patients returned to their preinjury Tegner score of >6 by two years.37 Another study used the Broström repair without the Gould modification to assess return to sport in elite athletes with severe lateral ligament ruptures and reported that the procedure was safe and effective in providing a stable ankle and return to sport at ∼3 months in this population.10 The procedure in our current study differs in that we used reinforcement with suture augmentation providing fixation of the ATFL and CFL. We report the success of patients returning to preinjury functional levels with daily activities and recreational sport, but further studies would need to be done to determine if suture augmentation can be similarly effective in high-level athletes.
Limitations
This study is not without limitations. First, no control group was included to provide direct comparison of how outcomes of the described procedure might differ from a traditional reconstruction. A randomized controlled trial comparing our suture augmentation construct providing reinforcement of the ATFL and CFL to a well-established procedure using a different suture augmentation construct would strengthen the findings of this study. Additionally, of our cohort of 31 patients, only 14 participated in recreational sports. To more accurately assess return-to-sport activity after this procedure and to strengthen our findings, future studies should include a larger number of participants that participate in sports. Lastly, we did not account for the duration of symptoms preoperatively. Duration of symptoms preoperatively could affect functional preoperative scores, as well as postoperative outcomes. Either way, the overall change in any outcome that we measured could be affected by the duration of symptoms, and this information was not available for inclusion in our study.
Conclusion
This variant Broström procedure with suture anchors and augmentation of both the ATFL and CFL was effective in helping patients return to their preinjury functionality level in both daily life and sports activity.
Acknowledgments
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government. The views expressed in this article reflect the results of research conducted by the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Ferran N.A., Oliva F., Maffulli N. Ankle instability. Sports Med Arthrosc Rev. 2009;17:139–145. doi: 10.1097/JSA.0b013e3181a3d790. [DOI] [PubMed] [Google Scholar]
- 2.Fong D.T., Hong Y., Chan L.K., Yung P.S., Chan K.M. A systematic review on ankle injury and ankle sprain in sports. Sports Med. 2007;37:73–94. doi: 10.2165/00007256-200737010-00006. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan L.D., Jost P.W., Honkamp N., Norwig J., West R., Bradley J.P. Incidence and variance of foot and ankle injuries in elite college football players. Am J Orthop (Belle Mead NJ) 2011;40:40–44. [PubMed] [Google Scholar]
- 4.McKay G.D., Goldie P.A., Payne W.R., Oakes B.W. Ankle injuries in basketball: Injury rate and risk factors. Br J Sports Med. 2001;35:103–108. doi: 10.1136/bjsm.35.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sankey R.A., Brooks J.H., Kemp S.P., Haddad F.S. The epidemiology of ankle injuries in professional rugby union players. Am J Sports Med. 2008;36:2415–2424. doi: 10.1177/0363546508322889. [DOI] [PubMed] [Google Scholar]
- 6.Struijs P., Kerkhoffs G. Ankle sprain. Clin Evid. 2002;(8):1050–1059. [PubMed] [Google Scholar]
- 7.Boardman D.L., Liu S.H. Contribution of the anterolateral joint capsule to the mechanical stability of the ankle. Clin Orthop Relat Res. 1997;341:224–232. [PubMed] [Google Scholar]
- 8.Broström L. Fotleds- vrickning [Ankle sprains] Lakartidningen. 1967;64:1629–1644. [PubMed] [Google Scholar]
- 9.Kannus P., Renström P. Treatment for acute tears of the lateral ligaments of the ankle. Operation, cast, or early controlled mobilization. J Bone Joint Surg Am. 1991;73:305–312. [published correction appears in J Bone Joint Surg Am 2015;97:e76] [PubMed] [Google Scholar]
- 10.White W.J., McCollum G.A., Calder J.D. Return to sport following acute lateral ligament repair of the ankle in professional athletes. Knee Surg Sports Traumatol Arthrosc. 2016;24:1124–1129. doi: 10.1007/s00167-015-3815-1. [DOI] [PubMed] [Google Scholar]
- 11.Lee K.T., Lee J.I., Sung K.S., et al. Biomechanical evaluation against calcaneofibular ligament repair in the Brostrom procedure: A cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2008;16:781–786. doi: 10.1007/s00167-008-0557-3. [DOI] [PubMed] [Google Scholar]
- 12.Gerber J.P., Williams G.N., Scoville C.R., Arciero R.A., Taylor D.C. Persistent disability associated with ankle sprains: A prospective examination of an athletic population. Foot Ankle Int. 1998;19:653–660. doi: 10.1177/107110079801901002. [DOI] [PubMed] [Google Scholar]
- 13.Pijnenburg A.C., Bogaard K., Krips R., Marti R.K., Bossuyt P.M., van Dijk C.N. Operative and functional treatment of rupture of the lateral ligament of the ankle. A randomized, prospective trial. J Bone Joint Surg Br. 2003;85:525–530. doi: 10.1302/0301-620x.85b4.13928. [DOI] [PubMed] [Google Scholar]
- 14.Pijnenburg A.C., Van Dijk C.N., Bossuyt P.M., Marti R.K. Treatment of ruptures of the lateral ankle ligaments: A meta-analysis. J Bone Joint Surg Am. 2000;82:761–773. doi: 10.2106/00004623-200006000-00002. [DOI] [PubMed] [Google Scholar]
- 15.Verhagen E.A., Van der Beek A.J., Bouter L.M., Bahr R.M., Van Mechelen W. A one season prospective cohort study of volleyball injuries. Br J Sports Med. 2004;38:477–481. doi: 10.1136/bjsm.2003.005785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Broström L. Sprained ankles. VI. Surgical treatment of “chronic” ligament ruptures. Acta Chir Scand. 1966;132:551–565. [PubMed] [Google Scholar]
- 17.Gould N., Seligson D., Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980;1:84–89. doi: 10.1177/107110078000100206. [DOI] [PubMed] [Google Scholar]
- 18.Hu C.Y., Lee K.B., Song E.K., Kim M.S., Park K.S. Comparison of bone tunnel and suture anchor techniques in the modified Broström procedure for chronic lateral ankle instability. Am J Sports Med. 2013;41:1877–1884. doi: 10.1177/0363546513490647. [DOI] [PubMed] [Google Scholar]
- 19.Nishimura A., Nakazora S., Senga Y., et al. Arthroscopic internal brace augmentation with arthroscopic modified Broström operation for chronic ankle instability. Arthrosc Tech. 2021;10:e995–e1000. doi: 10.1016/j.eats.2020.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Girard P., Anderson R.B., Davis W.H., Isear J.A., Kiebzak G.M. Clinical evaluation of the modified Brostrom-Evans procedure to restore ankle stability. Foot Ankle Int. 1999;20:246–252. doi: 10.1177/107110079902000407. [DOI] [PubMed] [Google Scholar]
- 21.Schenck R.C., Jr., Coughlin M.J. Lateral ankle instability and revision surgery alternatives in the athlete. Foot Ankle Clin. 2009;14:205–214. doi: 10.1016/j.fcl.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 22.Waldrop N.E., 3rd, Wijdicks C.A., Jansson K.S., LaPrade R.F., Clanton T.O. Anatomic suture anchor versus the Broström technique for anterior talofibular ligament repair: A biomechanical comparison. Am J Sports Med. 2012;40:2590–2596. doi: 10.1177/0363546512458420. [DOI] [PubMed] [Google Scholar]
- 23.Cho B.K., Park J.K., Choi S.M., SooHoo N.F. A randomized comparison between lateral ligaments augmentation using suture-tape and modified Broström repair in young female patients with chronic ankle instability. Foot Ankle Surg. 2019;25:137–142. doi: 10.1016/j.fas.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 24.Lubowitz J.H., MacKay G., Gilmer B. Knee medial collateral ligament and posteromedial corner anatomic repair with internal bracing. Arthrosc Tech. 2014;3:e505–e508. doi: 10.1016/j.eats.2014.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Xu D.L., Gan K.F., Li H.J., et al. Modified Broström repair with and without augmentation using suture tape for chronic lateral ankle instability. Orthop Surg. 2019;11:671–678. doi: 10.1111/os.12516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schuh R., Benca E., Willegger M., et al. Comparison of Broström technique, suture anchor repair, and tape augmentation for reconstruction of the anterior talofibular ligament. Knee Surg Sports Traumatol Arthrosc. 2016;24:1101–1107. doi: 10.1007/s00167-015-3631-7. [DOI] [PubMed] [Google Scholar]
- 27.Viens N.A., Wijdicks C.A., Campbell K.J., Laprade R.F., Clanton T.O. Anterior talofibular ligament ruptures, Part 1: biomechanical comparison of augmented Broström repair techniques with the intact anterior talofibular ligament. Am J Sports Med. 2014;42:405–411. doi: 10.1177/0363546513510141. [DOI] [PubMed] [Google Scholar]
- 28.Willegger M., Benca E., Hirtler L., et al. Biomechanical stability of tape augmentation for anterior talofibular ligament (ATFL) repair compared to the native ATFL. Knee Surg Sports Traumatol Arthrosc. 2016;24:1015–1021. doi: 10.1007/s00167-016-4048-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Waterman B.R., Owens B.D., Davey S., Zacchilli M.A., Belmont P.J., Jr. The epidemiology of ankle sprains in the United States. J Bone Joint Surg Am. 2010;92:2279–2284. doi: 10.2106/JBJS.I.01537. [DOI] [PubMed] [Google Scholar]
- 30.Song Y., Li H., Sun C., et al. Clinical Guidelines for the Surgical Management of Chronic Lateral Ankle Instability: A consensus reached by systematic review of the available data. Orthop J Sports Med. 2019;7 doi: 10.1177/2325967119873852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Michels F., Pereira H., Calder J., et al. Searching for consensus in the approach to patients with chronic lateral ankle instability: Ask the expert. Knee Surg Sports Traumatol Arthrosc. 2018;26:2095–2102. doi: 10.1007/s00167-017-4556-0. [DOI] [PubMed] [Google Scholar]
- 32.Tourné Y., Mabit C. Lateral ligament reconstruction procedures for the ankle. Orthop Traumatol Surg Res. 2017;103:S171–S181. doi: 10.1016/j.otsr.2016.06.026. [DOI] [PubMed] [Google Scholar]
- 33.Sarhan I., Mubark I., Waly A. Chronic lateral ankle instability: Results of anatomic repair with polyester tape augmentation. Ortop Traumatol Rehabil. 2020;22:25–31. doi: 10.5604/01.3001.0013.9781. [DOI] [PubMed] [Google Scholar]
- 34.Yoo J.S., Yang E.A. Clinical results of an arthroscopic modified Brostrom operation with and without an internal brace. J Orthop Traumatol. 2016;17:353–360. doi: 10.1007/s10195-016-0406-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maffulli N., Del Buono A., Maffulli G.D., et al. Isolated anterior talofibular ligament Broström repair for chronic lateral ankle instability: 9-year follow-up. Am J Sports Med. 2013;41:858–864. doi: 10.1177/0363546512474967. [DOI] [PubMed] [Google Scholar]
- 36.Hunt K.J., Fuld R.D., III, Sutphin B.S., Pereira H., D’Hooghe P. Return to sport following lateral ankle ligament repair is under-reported: a systematic review. J ISAKOS. 2017;2:234–240. [Google Scholar]
- 37.Li X., Killie H., Guerrero P., Busconi B.D. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: functional outcomes after the modified Broström repair using suture anchors. Am J Sports Med. 2009;37:488–494. doi: 10.1177/0363546508327541. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.