Abstract
Background
During the pandemic, traditional family meetings were replaced by remote telecommunications. We assessed the families’ satisfaction with these communications using a survey-based questionnaire.
Methods
The study involved 20-minute telephonic surveys conducted with the family member who was updated during the hospitalization of the patient. A thematic-based questionnaire with responses on a scale of 5 ranging from very dissatisfied to very satisfied was used. The responses were dichotomized into bad and good reports for analysis.
Results
A total of 196 patients were eligible. Only 154 patients’ family representatives consented to the study. The frequency and content of the telephonic updates were satisfactory. The bad report was assigned to 5% of families only. Among features assessing empathy of communication providers, the satisfaction rate was much higher with 3% of families alone providing a bad report. The response was significantly biased against the final outcome of the patient with poor review often provided by relatives of patients who had succumbed to the illness. The dissatisfaction rate was much higher, above 12% for the trust of communication and ICU visitation. However, the final outcome of the patient did not affect the trust in the information conveyed by the physician.
Interpretation
This study highlights several drawbacks in the communication strategy during the second surge of coronavirus disease-2019 (COVID-19). The final outcome of the patient was the key decisive factor for the response to most of the questionnaire. Sustained faith in communication by the physician despite the final outcome of the patient, re-emphasizes the need for emotional connection and training for breaking bad news.
How to cite this article
Varghese MP, Selwyn T, Nair S, Samuel S, Chacko B, Pichamuthu K. Assessment of Family Satisfaction with Remote Communication for Critically Ill COVID-19 Patients: An Observational Cohort Study. Indian J Crit Care Med 2023;27(8):537–544.
Keywords: Communication, Coronavirus disease-2019, Empathy, Intensive care unit visitation, Trust, Satisfaction
Highlights
The survey not only looked at objective parameters such as the number of calls, and the number of audio, or visual aid used during the update but also at emotive responses like empathy and trust in the communicating physician. The results of the study lay a foundation for future preparedness for better communication during an emergency.
Introduction
Background
Being critically ill causes anxiety and stress to the patient, to the extent of precipitating postintensive care syndrome (PICS).1,2 While its impact on the patient is well understood, the effect on the patient's family may be overlooked.3 Several global studies have estimated the risk of family members developing postintensive care syndrome-family (PICS-F).4–6 The recognition of PICS-F has encouraged ICUs to practice family-centered care, inclusive of family members in patient care.7 This permits them to spend longer periods with the patient and interact with healthcare professionals along with reducing the incidence of posttraumatic stress disorder (PTSD) symptoms.8,9 Despite robust evidence favoring family-centered care with minimal risk of nosocomial infection, most ICUs have restricted visitation policy.7,10–14
Objective
In India, no standardized guidelines on family visitations have been laid down.15 With the outbreak of coronavirus disease-2019 (COVID-19), hospitals restricted family visits to the ICUs as well as family's presence in the hospital to curb virus outbreak. Due to the overwhelming nature of the pandemic, critical care providers along with physicians from other specialties were redeployed in critical care services. Our hospital, incorporated family-centered care elements throughout, until the number of COVID-19 cases became significantly high.16 After this, family updates were largely virtual. Direct visits were only permitted for very sick patients or when family requested for one. Family visits were limited to a maximum of two per day per patient. All visitors were required to wear personal protection equipment (PPE). The relatives were offered video communication twice a day using an internet video calling device to see and interact with the patient. However, only audio communication was possible for a few relatives who did not have access to video calling devices and for patients who were deeply sedated.
Our hospital did not have a dedicated professional or a team to perform this function.
Family satisfaction is a key indicator for quality of care.17 However, its importance during the pandemic has not been adequately studied.
In this study, we aim to measure the quality of telecommunication offered to family members of patients admitted to COVID-19 ICUs at our institute during the second surge of the COVID-19 virus outbreak. The objective of this study is to identify shortcomings and indicators for improved communication strategies.
Methods
Study Design and Setting
A prospective survey was performed by interviewing the family members of patients admitted to 8 COVID-19 ICUs (104 beds) for more than 24 hours from 1 May 2021 to 30 June 2021.
Participants, Variables, and Bias
For this study, contact details were obtained from the electronic medical records. The primary family member, who maintained contact with the ICU physician, was identified and selected for a one-time, structured, telephonic interview.
The data on the eventual outcome of the patient was available to the interviewing investigators to avoid surveying questions related to the functional status of patients after discharge from the hospital.
The interview was conducted by a neutral coinvestigator, who had no prior involvement with patient care or any previous family interaction. This helped avoid bias in the responses collected.
Data Sources/Measurement
Each interview lasted 20–30 minutes. The neutral coinvestigator read out the study information sheet and obtained verbal consent for the interviewee's participation and recorded the entire phone survey. The interviewer read out the survey questionnaire and simultaneously recorded the subject's responses into an electronic data entry sheet. The audio file, along with the digital data entry, was saved on a password-protected computer.
Study Size
A total of 196 subjects, who fulfilled the inclusion criteria, were selected for the survey. All these subjects had family members who had suffered from severe COVID-19 acute respiratory distress syndrome (ARDS) and had required more than 24 hours of stay in the ICU. Patients with missing family contact records and those who did not consent were excluded from the survey.
Statistical Analysis
Quantitative Variables
A survey questionnaire was developed by the investigators with input from a psychology professional (Table 1). The survey questionnaire consisted of thematic subgroups regarding family member's sociodemographic details and relationship to the patient, the patient's physical status after treatment, access to communication devices, the frequency of communication received, quality of information, empathy in communication, trust in communication, and direct ICU visitations. Each theme surveyed the overall quality of each subgroup, on a scale of 1 to 5, with “1” representing “very dissatisfied” and “5” “very satisfied”.
Table 1.
Survey questionnaire
| Access to the communication devices | ||||||
| A1 | What was the mode of communication available to you for communicating with the ICU? | Audio and video calls | Only audio calls | |||
| Frequency of the communication | ||||||
| B1 | How often did the ICU doctor conduct audio calls? | None | Once a day | Twice a day | Thrice a day | |
| B2 | How often did the ICU doctor conduct video calls? | None | Once a day | Twice a day | Thrice a day | |
| B3 | What is your overall satisfaction with the number of communications conducted? | Very dissatisfied | Dissatisfied | Fair | Satisfied | Very satisfied |
| Understanding the information | ||||||
| C1 | How would you rate the local language skill used by the doctor to communicate with you? | Very poor | Poor | Fair | Good | Very good |
| C2 | How would you rate the sufficiency of information given regarding the medical condition of the patient? | Very poor | Poor | Fair | Good | Very good |
| C3 | How would you rate the time given to you to ask questions and clear doubts? | Very poor | Poor | Fair | Good | Very good |
| C4 | Did you feel the need to ask more doubts when you were given bad news? | Never | Rarely | Sometimes | Often | Very often |
| C5 | Were you satisfied with shorter communication time if the patient was improving? | Never | Rarely | Sometimes | Often | Very often |
| C6 | Did you prefer having a family member or friend present during the doctor's communication? (Social support) | No | Maybe | Sometimes | Yes | Very often |
| C7 | Was the patient condition information given to you consistently? (Consistency of information) | Never | Rarely | Sometimes | Often | Very often |
| C8 | How would you rate your overall experience regarding the medical information the doctor had given? | Very dissatisfied | Dissatisfied | Fair | Satisfied | Very satisfied |
| Empathy in the communication | ||||||
| D1 | Did the communicating doctor always have a friendly(approachable) attitude? | Never | Rarely | Sometimes | Often | Very often |
| D2 | Did you find it easier to ask doubts and questions when the doctor has a friendly attitude? | Never | Rarely | Sometimes | Often | Very often |
| D3 | Did you experience any anger or rude behavior from the doctor? | Never | Rarely | Sometimes | Often | Very often |
| D4 | How would you rate your satisfaction with the empathy of the doctor? | Very dissatisfied | Dissatisfied | Fair | Satisfied | Very satisfied |
| Trust in the communication | ||||||
| E1 | Did you always feel that the doctor cared about the patient? | Never | Rarely | Sometimes | Often | Very often |
| E2 | Did you ever feel the doctor was withholding any information? | Never | Rarely | Sometimes | Often | Very often |
| E3 | Did you always feel the medical team was treating all patients and their family members equally? | Never | Rarely | Sometimes | Often | Very often |
| E4 | What is your overall satisfaction with the trust in your ICU doctor's communication? | Very dissatisfied | Dissatisfied | Fair | Satisfied | Very satisfied |
| Visitation and in-person communication | ||||||
| F1 | Are you aware of why direct COVID ICU visits were restricted? | Yes | No | Maybe | ||
| F2 | Did you fear contracting COVID-19 by visiting the ICU? | Yes | No | Maybe | ||
| F3 | Were you able to visit the patient in the ICU? | Never | Rarely | Sometimes | Often | Very often |
| F4 | Were you able to directly converse with the ICU doctor? | Never | Rarely | Sometimes | Often | Very often |
| F5 | Did direct ICU visits help you better understand the medical condition of the patient? | Yes | No | Maybe | ||
| F6 | Were you offered appropriate PPE for making safe ICU visits? | Yes | No | Maybe | ||
| F7 | What is your overall satisfaction with the ICU visitation? | Very dissatisfied | Dissatisfied | Fair | Satisfied | Very satisfied |
Analytic Approach
The sociodemographics of the family members and the eventual outcome of the patients were tabulated. The response to the satisfaction associated with each thematic question was analyzed with statistical package for the social sciences (SPSS), version 26, and represented in pictographic form (Highlighted in black font depicts bad response). The responses were cross-tabulated and analyzed with the use of Pearson's Fisher's Exact test. For the purpose of statistical analysis, responses—fair, satisfied, and very satisfied were grouped together, and dissatisfied and very dissatisfied into another group.
Results
The family members of 154 patients admitted to eight ICUs in our institution had consented to participate in the study. Of these, 86 (55.84%) were discharged from the ICU. The final outcome while in the ICU or after leaving the hospital is shown in Table 2.
Table 2.
Final outcome in ICU and after discharge from hospital
| The condition of the discharged patients after leaving the hospital | n | % |
|---|---|---|
| Returned to the original level and employment with no disability | 35 | 40.70 |
| A minor disability that does not interfere with daily functioning | 36 | 41.86 |
| A significant disability that interferes with daily functioning or work | 10 | 11.63 |
| Severe disability rendering the Patient totally dependent (requiring continued treatment at the same or different hospital) | 0 | 0 |
| Demise after discharge from hospital | 5 | 5.81 |
| Total | 86 | 100 |
| The outcome of the patients admitted to the ICU | n | % |
| Demise | 68 | 44.16 |
| Discharged from ICU | 86 | 55.84 |
| Total | 154 | 100 |
A total of 42 (21.32%) family members of the 196 study subjects declined to participate in the survey citing personal issues. Among the subjects that refused, 61.9% (26/42) were family members of patients that did not survive the illness. Telephone interviews were conducted with the remaining 154 family members who consented to the study.
Various reasons for not consenting predominantly involved, not wishing to recall past traumatic experiences 57.14% (24/42), lack of time 54.8% (23/42), unhappy with the quality of care 11.9% (5/42) and one declined on account of the rude behavior of the medical team.
The socioeconomic demographics of the respondents were recorded to evaluate if this affected the responder's judgment (Table 3).
Table 3.
Socioeconomic demographics of responders of the survey
| N | % | |
|---|---|---|
| Gender | ||
| Male | 57 | 37.01 |
| Female | 97 | 62.99 |
| Age (years) | ||
| 18–30 | 40 | 25.97 |
| 31–60 | 108 | 70.13 |
| >60 | 6 | 3.90 |
| Relation | ||
| Children | 39 | 25.32 |
| Sibling | 25 | 16.23 |
| Parent | 6 | 3.904 |
| Spouse | 66 | 2.86 |
| Distant relative | 18 | 11.69 |
| Education | ||
| Primary school | 8 | 5.19 |
| High school | 43 | 27.92 |
| Undergraduate | 76 | 49.35 |
| Postgraduate | 27 | 17.53 |
All family members of patients admitted to the ICUs were offered video interactions twice a day; however, 14.94% (23/154) did not have access to any video calling device.
Response to the Questionnaire
Frequency of Calls
When asked about the frequency of calls, only 7.74% of the family members expressed their dissatisfaction. Even though video calls were planned twice a day, only 20.78% received 2 or more video calls a day, while the majority (59.09%) received only one video call a day. There were 28 family members who claimed that they had not received any video calls. However, audio communication was regular, with 95.45% of caregivers receiving at least one audio call a day. Most of the respondents (90.91%) felt that the time given to ask questions and clarify their doubts was sufficient, but 9.9% felt it was insufficient. The final outcome of the patient and mode of communication, visual or audio affected the satisfaction of telecommunication (Table 4). Social factors such as level of education of the respondent did not affect the satisfaction rate.
Table 4.
Factors affecting overall satisfaction with telecommunication
| Fair/satisfied | Dissatisfied | p-value | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Final patient outcome | |||||
| Demise | 59 | 42.45 | 14 | 93.33 | |
| Discharged | 80 | 57.55 | 1 | 6.67 | 0.001 |
| Education | |||||
| College degree | 96 | 69.06 | 7 | 46.67 | |
| Without college degree | 43 | 30.94 | 8 | 53.33 | 0.080 |
| Mode of communication available | |||||
| Only audio | 18 | 12.95 | 5 | 33.33 | |
| Audio and video | 121 | 87.05 | 10 | 66.67 | 0.035 |
Quality of Information
When asked about the quality of information communicated to them, 9.09% of subjects described dissatisfaction while 24.03% described their experience as just fair. There were some respondents (8.44%) who highlighted the poor local language skills of the communicating physician. A majority of family members (59.74%) expressed the desire to ask more questions when they were given news of the worsening clinical status of their patients. The study showed that 67.53% of families were satisfied with shorter communication. Caregivers of deceased patients were likely to be dissatisfied (Table 4).
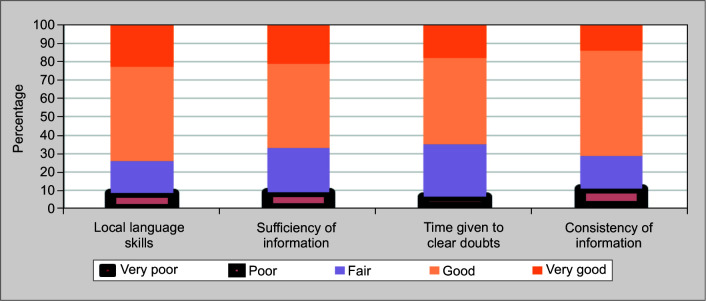
There were 3 (1.95%) respondents who experienced inconsistency in the information communicated regarding the clinical condition of their patient. Figure 1 depicts the satisfaction rate for the various elements of information provided.
Fig. 1.
Satisfaction rate for elements of information
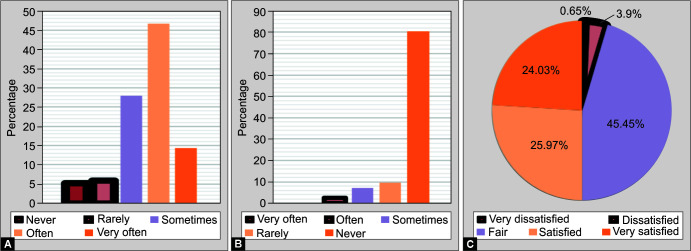
Figs 2A to C.
The various aspects of empathy in telecommunication surveyed. (A) The amenable and approachable character of the communicating physician; (B) Angry or rude behavior of the communicating physician; (C) Empathy in the communication
Empathy
Figure 3 represents the responses assessing empathetic approach of the caregiver during communication. Most caregivers (61.04%) described the conversation with the physician to be amenable and approachable. While 27.92% of the respondents felt the same only sometimes, and 5.84% felt it was a rare characteristic. There were 3 respondents (5.19%) who felt that the physician was neither friendly nor approachable. Further, 63.64% of subjects reported it was easier to ask questions and clarify doubts when the treating physician had a friendly attitude. There were 2.6% (4/154) and 9.74% (15/154) respondents respectively who “often” or “rarely” felt that the communicating doctor's conversation was rude. Six respondents (3.9%) described that they had felt an overall lack of empathy from the communicating physician.
Fig. 3.
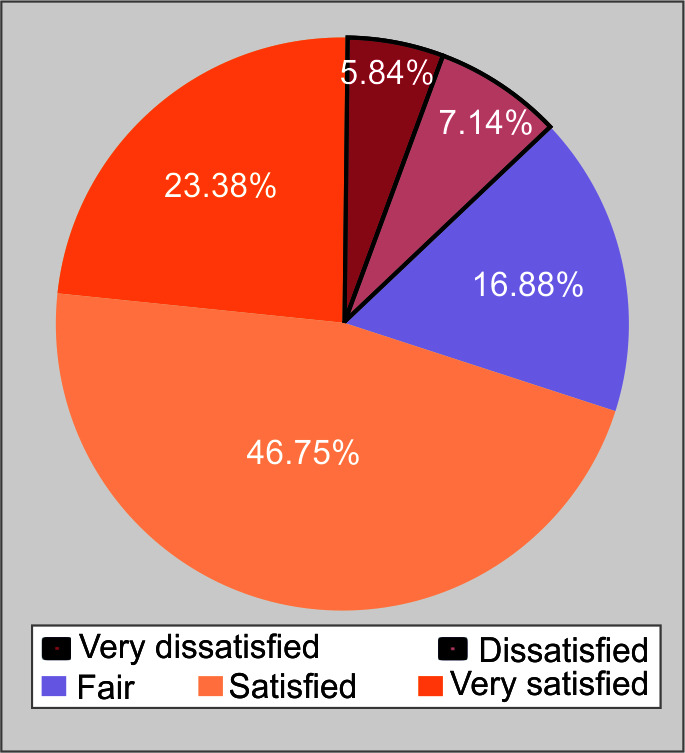
Trust in the communication
The patient's final outcome or respondent's educational level did not influence the evaluation.
Trust in Communication
There were four respondents who felt that the doctor did not care enough for their family members. Further, 8.44% (13/154) and 12.34% (19/154) of the respondents respectively felt that “often” or on “rare” occasions the communicating physicians were not honest with them or had withheld medical information from them. There were some respondents (7/154; 4.55%) who perceived an inequality in patient care. Figure 3 depicts the satisfaction rate on the trustworthiness of telecommunication. The final outcome of the patient did not affect the trust of the respondent in the communication given by the treating physician (Table 5).
Table 5.
Overall satisfaction with the trust in your doctor
| Fair/satisfied | Dissatisfied | p-value | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Final patient outcome | |||||
| Demise | 60 | 44.78 | 13 | 65.00 | |
| Discharged | 74 | 55.22 | 7 | 35.00 | 0.091 |
| Education | |||||
| College degree | 90 | 67.16 | 13 | 65.00 | |
| Without college degree | 44 | 32.84 | 7 | 35.00 | 0.848 |
| Mode of communication available | |||||
| Only audio | 18 | 14.94 | 5 | 25.00 | |
| Audio and video | 116 | 85.06 | 15 | 75.00 | 0.176 |
The various facts that emerged from the survey about ICU visitation policy (Fig. 4) included that only 4% were aware of the true reason for the restriction. A quarter of the respondents feared and 20.78% (32/154) had doubtful fears of contracting COVID-19 illness by visiting the ICUs. Less than a quarter 22.73% (35/154) visited the ICU on rare occasions, while almost one-third of family members (49/150) did not visit their patient in the ICU at all.
Fig. 4.
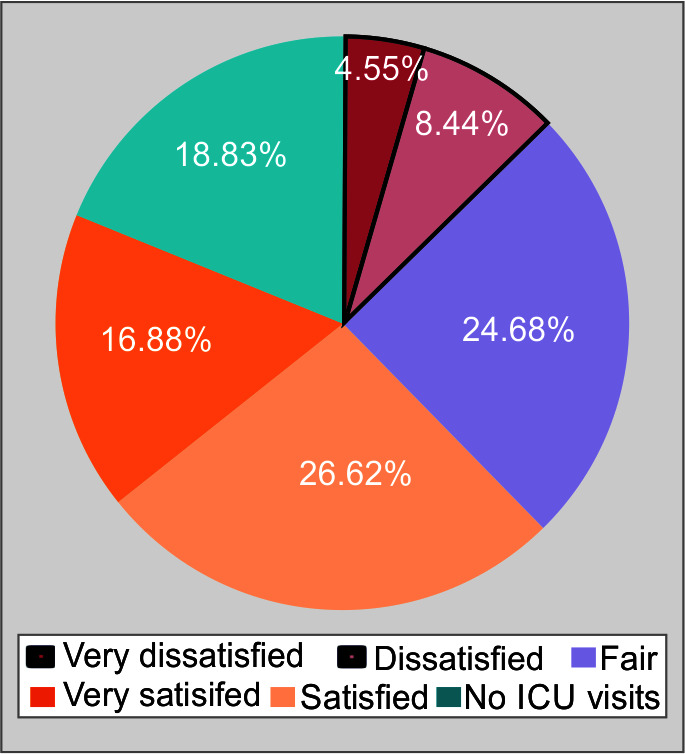
The ICU visitations
When able to visit the ICU, 82.29% (79/96) respondents were able to understand the condition better after discussing it with the treating physician. Only seven respondents were unable to meet a doctor at an ICU visit.
Very few (2.08%) caregivers complained about the personal protective gear provided for ICU visitation. Overall, limited ICU visitations proved to be the most dissatisfying experience for most of the respondents (12.99%).
The data collected on the frequency of ICU visits could not be cross-analyzed due to the inconsistency in the permitted visits. The direct ICU visits were permitted on a case-to-case basis influenced by the patient's prognosis.
The Eventual Outcome of the Patient
In the dichotomous evaluation of the results, there was an average of 5% bad report for most of the components of the survey except trust in communication and ICU visitation (>12%).
The eventual demise of the patient led to dissatisfied feedback in almost all thematic aspects of the interview. Approximately 86% (12/14) negative feedback on medical content of communication, 75% (5/7) for communicating physician's empathy, 65% (13/20) for the lack of trust, and 60% (12/20) for ICU visitations were all provided by family members of deceased patients. Hence, this was the single factor influencing the satisfaction of telecommunication during the pandemic.
Discussion
The traditional family updates in our institute include physician conveying the medically relevant information and additional communication regarding hospital proceedings being offered by social workers. We do not have any standardized communication protocol, and individual specialty ICUs have minor differences in their approach to communicating information to family members.
However, as with health facilities across the globe, COVID-19 mandates to limit ICU visits and direct communication disrupted our traditional practice.18 During the period of the surge in the virus outbreak, we limited communication to once-a-day phone calls to the family and twice-a-day virtual ICU visits as was the updated recommended practice.19 The study by Montauk and Kuhl identified that the limited ICU visitations during the pandemic were traumatic to the family members and was the greatest challenge experienced by them.20 However, the need for family members to have direct conversations with the medical team, to gauge the situation of their patient and receive honest information from the physicians has been highlighted by Mckiernan and McCarthy21 Visiting the ICU enables family members to demonstrate their support and bond for the patient, and allows the medical team to provide reassurance and validate their sincerity to establish trust.21 While virtual visits enabled update geographically distant relatives, making it an appealing option; it came with many flaws. The absence of support staff during counseling was found to be a big handicap.22
In our study 14.94% (23/154) of respondents did not own video devices. Thus, they were at a disadvantage, unable to see their loved ones during their time in the ICU. However, this did not interfere with the overall family satisfaction. We also found that the family's level of education did not affect their appreciation of the communication, which reflects the clinician's ability to convey medical information. In contrast, Fathallah et al., during a survey-based assessment of family satisfaction in ICU in non-pandemic times, found literacy level to be the most influential. They propose difficulty to accept stressful state among the illiterate to be the cause.23
Our results are in comparison to existing literature with an average of 5% dissatisfaction for aspects like quality of information, empathy of physician communicating information, and trust in the content of information.24 The exception was the ICU visiting policy which had a relatively higher 12% dissatisfaction. This could have been due to the inability to have virtual visits for many families and in-person visitations reserved for very sick patients. In contrast to our findings, Fathallah et al. did not find not allowing bed visits, a deterrent in family satisfaction.23
Among the subjects who had declined to participate in the survey, 11.9% (5/42) did so because they were unhappy with the quality of care, and one of the participants cited perceived rude behavior of the medical team. This data reinforces the need to focus on physician communication skills and ensure better family satisfaction through uniform communication guideline.
The ICU mortality at our center during the second surge of the pandemic was 50.25%, significantly higher than the 28.8% mortality reported during the second wave in some developed countries.25 The inadequacy of sufficient healthcare infrastructure made it difficult to meet the needs of a large number of critically ill patients. Only patients with severe illness were admitted into the ICUs, at which stage it was too late for many. The eventual demise of the patient had a strong association with poor approval of the number of phone calls and quality of information. It is reassuring to find that demise of the patient did not affect their trust in the clinicians and recognition of their empathy toward the family. In contrast, Reddy et al., with a lower participation response of 32.2% in comparison to our 78.57%, found patient's demise during hospitalization did not affect a family member's response to the survey.26
The shortage of medical professionals during the second surge of covid led to the redeployment of many non-intensivists without proper training for counseling. Hence, the treating physicians were tasked with the additional responsibility of incorporating both patient and family care duties. This may explain the major lacunae in meaningful communication which was the inability to provide time for respondent's questions and more descriptive answers on the medical status of the patient. Fritz et al. performed a similar study surveying patients’ surrogate decision makers and providers. They reported similar feelings regarding the adequacy of the information. Unlike our study, they had only once-a-day telecommunication for want of time away from patient care. Greater frequency of calls was found to be the most wanted by the caregivers. This study did not evaluate emotive responses as empathy and trust.27 A qualitative study by Hochendoner et al. collecting data from family members of COVID-19 ICU patients at ten U.S. hospitals described their three most valued communication principles to be direct contact, consistency, and compassion.28
Lopez et al. had an established family liaison team (FLT) comprising of external redeployed providers not involved in patient care. This team was to interact, counsel, and communicate medical information to the family members. As this team did not have clinical responsibilities, they were able to delegate sufficient time to family communication.24 The collaboration and integration of this external team did have efficiency issues; however, their importance was reflected in their ability to focus on communication, and to attend to family needs, especially for those nearing the end of life. This strategy of a dedicated communication team was associated with increased family satisfaction.24
The incorporation of communication bundles and protocols along with appropriate training of physicians to counsel and incorporate elements of family-centered care have been proposed by several studies and can ensure better family satisfaction.29
In our study, several family members of patients admitted to the ICU were not permitted to make any direct ICU visits. These patients had a good prognosis and were eventually discharged from the ICU. Relaxation of ICU visitation rules was made only for those patients who had a poor prognosis. The data collected at another center by Camões et al., although not statistically significant, showed higher satisfaction with information consistency among family members who were able to make direct ICU visits.30 Chanchalani et al., studied the visiting and communication policy in ICUs during the pandemic across South Asia and Middle East.31 In this survey health care practitioners (HCP), mostly ICU consultants found the altered communication process during COVID-19, a challenge and highly dissatisfying. The process of consent taking too was found by the families to be less clear than in- person's procedure and wanting in terms of medico–legal repercussions by the HCP. Our study differed to look into the family's viewpoint of communication satisfaction than the HCP and legal aspect.
Limitations
The rapid redeployment of providers from other specialties to meet the needs of the severe situation of the second surge made it challenging to ensure training in communication and counseling tasks. The lack of counseling guidelines and uniformity in the communication skills of the physicians may have influenced subject responses.
It is also possible that the eventual demise of the patient had a significant negative recall bias. This bias may have affected the reliability of the interview responses.
Conclusion
Our study revealed several shortcomings in our communication practices during the second surge of COVID-19 pandemic. The study subjects’ opinion was clearly swayed on the basis of the prognosis of the patient with greater compliance if the patient survived the illness. Despite the poor outcome of many patients, the faith and emotional connection with the treating team held well. This suggests the importance of providing communication that is not merely the transmission of medical information. Our experiences reflect the need to demonstrate a better emotional connection with the patient's family members. Hence, we recommend employing additional dedicated personnel with good communication skills and clinical awareness.
The implementation of a communication bundle or protocol could ensure better completeness of the information given to the family. Training redeployed physicians from other specialties in family communication and telemedicine may help them to deal with such circumstances in the future. Including nurses and social workers in the communication team could help improve and bolster the communication strategies.
We also recommend direct in-person daily communication with the use of appropriate infection control measures to improve family compliance. Silence in a phone conversation can mean many things; its interpretation is tough and is often misinterpreted as not being heard or lacking interest. A voiceless emotion needs to be seen and respected.
Authors’ Contributions
All the authors have contributed equally.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Marra A, Pandharipande PP, Girard TD, Patel MB, Hughes CG, Jackson JC, et al. Co-occurrence of post-intensive care syndrome problems among 406 survivors of critical illness. Crit Care Med. 2018;46(9):1393–1401. doi: 10.1097/CCM.0000000000003218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Elliott D, Davidson JE, Harvey MA, Bemis–Dougherty A, Hopkins RO, Iwashyna TJ, et al. Exploring the scope of post-intensive care syndrome therapy and care: Engagement of non-critical care providers and survivors in a second stakeholders meeting. Crit Care Med. 2014;42(12):2518–26. doi: 10.1097/CCM.0000000000000525. [DOI] [PubMed] [Google Scholar]
- 3.Davidson JE, Jones C, Bienvenu OJ. Family response to critical illness: Post-intensive care syndrome-family. Crit Care Med. 2012;40(2):618–424. doi: 10.1097/CCM.0b013e318236ebf9. [DOI] [PubMed] [Google Scholar]
- 4.Pandharipande PP, Girard TD, Ely EW. Long-term cognitive impairment after critical illness. N Engl J Med. 2014;370(2):185–186. doi: 10.1056/NEJMc1313886. [DOI] [PubMed] [Google Scholar]
- 5.Prendergast TJ. Resolving conflicts surrounding end-of-life care. New Horiz. 1997;5(1):62–71. 9017680 [PubMed] [Google Scholar]
- 6.Azoulay E, Pochard F, Kentish–Barnes N, Chevret S, Aboab J, Adrie C, et al. Risk of post-traumatic stress symptoms in family members of intensive care unit patients. Am J Respir Crit Care Med. 2005;171(9):987–994. doi: 10.1164/rccm.200409-1295OC. [DOI] [PubMed] [Google Scholar]
- 7.Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004–005. Crit Care Med. 2007;35(2):605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 8.Breitbart W, Gibson C, Tremblay A. The delirium experience: delirium recall and delirium-related distress in hospitalized patients with cancer, their spouses/caregivers, and their nurses. Psychosomatics. 2002;43(3):183–194. doi: 10.1176/appi.psy.43.3.183. [DOI] [PubMed] [Google Scholar]
- 9.Foa EB. Psychosocial therapy for posttraumatic stress disorder. J Clin Psychiatry. 2006;67(Suppl. 2):40–45. 16602814 [PubMed] [Google Scholar]
- 10.Riley BH, White J, Graham S, Alexandrov A. Traditional/restrictive vs patient-centered intensive care unit visitation: Perceptions of patients’ family members, physicians, and nurses. Am J Crit Care. 2014;23(4):316–324. doi: 10.4037/ajcc2014980. [DOI] [PubMed] [Google Scholar]
- 11.Liu V, Read JL, Scruth E, Cheng E. Visitation policies and practices in US ICUs. Crit Care. 2013;17(2):R71. doi: 10.1186/cc12677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berwick DM, Kotagal M. Restricted visiting hours in ICUs: time to change. JAMA. 2004;292(6):736–737. doi: 10.1001/jama.292.6.736. [DOI] [PubMed] [Google Scholar]
- 13.Livesay S, Gilliam A, Mokracek M, Sebastian S, Hickey JV. Nurses’ perceptions of open visiting hours in neuroscience intensive care unit. J Nurs Care Qual. 2005;20(2):182–189. doi: 10.1097/00001786-200504000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Nassar Junior AP, Besen BAMP, Robinson CC, Falavigna M, Teixeira C, Rosa RG. Flexible versus restrictive visiting policies in ICUs: A systematic review and meta-analysis. Crit Care Med. 2018;46(7):1175–1180. doi: 10.1097/CCM.0000000000003155. [DOI] [PubMed] [Google Scholar]
- 15.Datta R. ICU visitors: Is it time for a change in visitation policy? Med J Armed Forces India. 2007;63(3):308. doi: 10.1016/S0377-1237(07)80175-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sarkar A, Chakrabarti AK, Dutta S. COVID-19 infection in India: A comparative analysis of the second wave with the first wave. Pathogens. 2021;10(9):1222. doi: 10.3390/pathogens10091222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Vos M, Graafmans W, Keesman E, Westert G, van der Voort PH. Quality measurement at intensive care units: Which indicators should we use? J Crit Care. 2007;22(4):267–274. doi: 10.1016/j.jcrc.2007.01.002. [DOI] [PubMed] [Google Scholar]
- 18.Aziz S, Arabi YM, Alhazzani W, Evans L, Citerio G, Fischkoff K, et al. Managing ICU surge during the COVID-19 crisis: Rapid guidelines. Intensive Care Med. 2020;46(7):1303–1325. doi: 10.1007/s00134-020-06092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gaur S, Pandya N, Dumyati G, Nace DA, Pandya K, Jump RLP. A structured tool for communication and care planning in the era of the COVID-19 pandemic. J Am Med Dir Assoc. 2020;21(7):943–947. doi: 10.1016/j.jamda.2020.05.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Montauk TR, Kuhl EA. COVID-related family separation and trauma in the intensive care unit. Psychol Trauma. 2020;12(S1):S96–S97. doi: 10.1037/tra0000839. [DOI] [PubMed] [Google Scholar]
- 21.McKiernan M, McCarthy G. Family members’ lived experience in the intensive care unit: A phemenological study. Intensive Crit Care Nurs. 2010;26(5):254–261. doi: 10.1016/j.iccn.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 22.Xyrichis A, Pattison N, Ramsay P, Saha S, Cook A, Metaxa V, et al. Virtual visiting in intensive care during the COVID-19 pandemic: A qualitative descriptive study with ICU clinicians and non-ICU family team liaison members. BMJ Open. 2022;12(4):e055679. doi: 10.1136/bmjopen-2021-055679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fathallah I, Drira H, Habacha S, Kouraichi N. Can we satisfy family in intensive care unit? A Tunisian experience. Indian J Crit Care Med. 2022;26(2):185–191. doi: 10.5005/jp-journals-10071-24104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lopez–Soto C, Bates E, Anderson C, Saha S, Adams L, Aulakh A, et al. The role of a liaison team in ICU family communication during the COVID-19 pandemic. J Pain Symptom Manage. 2021;62(3):e112–e119. doi: 10.1016/j.jpainsymman.2021.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carbonell R, Urgelés S, Rodríguez A, Bodí M, Martín–Loeches I, Solé–Violán J, et al. Mortality comparison between the first and second/third waves among 3,795 critical COVID-19 patients with pneumonia admitted to the ICU: A multicentre retrospective cohort study. Lancet Reg Health Eur. 2021;11:100243. doi: 10.1016/j.lanepe.2021.100243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reddy MP, Kadam U, Lee JDY, Chua C, Wang W, McPhail T, et al. Family satisfaction with intensive care unit communication during the COVID-19 pandemic: A prospective multicentre Australian study. Family Satisfaction – COVID ICU. Intern Med J. 2023;53(4):481–491. doi: 10.1111/imj.15964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fritz C, Claude LA, Hamada S, Trosdorf M, de la Barre H, Yavchitz A, et al. Daily telephone call during the COVID-19 pandemic: Perceptions of families and providers. Am J Crit Care. 2022;31(1):77–81. doi: 10.4037/ajcc2022797. [DOI] [PubMed] [Google Scholar]
- 28.Hochendoner SJ, Amass TH, Curtis JR, Witt P, Weng X, Toyobo O, et al. Voices from the pandemic: A qualitative study of family experiences and suggestions regarding the care of critically ill patients. Ann Am Thorac Soc. 2022;19(4):614–624. doi: 10.1513/AnnalsATS.202105-629OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alhussaini A. Improve communicating uncertainty in intensive care unit with patient and family (ICU-PF). Cureus. 2021;13(12):e20837. doi: 10.7759/cureus.20837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Camões J, Lobato CT, Carvalho D, Gomes E, Araújo R. Family satisfaction in intensive care during the COVID-19 pandemic using the FS-ICU24 questionnaire. Acta Med Port. 2022;35(12):859–865. doi: 10.20344/amp.17128. [DOI] [PubMed] [Google Scholar]
- 31.Chanchalani G, Arora N, Nasa P, Sodhi K, Al Bahrani MJ, Al Tayar A, et al. Visiting and communication policy in intensive care units during COVID-19 pandemic: A cross-sectional survey from South Asia and the Middle East. Indian J Crit Care Med. 2022;26(3):268–275. doi: 10.5005/jp-journals-10071-24091. [DOI] [PMC free article] [PubMed] [Google Scholar]