Abstract
The purpose of this study was to evaluate the functional and cosmetic outcomes of a new modified Fox pentagon technique performed using polytetrafluoroethylene in frontalis suspension surgery for blepharophimosis syndrome. This retrospective study enrolled 40 patients diagnosed with blepharophimosis syndrome from March 2016 to October 2018. All patients underwent frontalis suspension using a new modified Fox pentagon technique. The functional and cosmetic outcomes were evaluated. After the operation, the mean palpebral fissure height increased from 2.68 to 6.93 in right eyes and from 2.73 to 6.98 in left eyes. The mean MRD1 increased from 0.53 to 3.76 in right eyes and from 0.50 to 3.78 in left eyes. While preoperative to postoperative differences were statistically significant (p < 0.01), there were no significant differences between right and left eyes either before or after the surgery (p > 0.01). All patients achieved good cosmetic results with an average score of 0.6. We have experimentally created a modified Fox pentagon technique performed using a polytetrafluoroethylene sling in a frontalis suspension to treat BPES; this approach yielded favorable cosmetic and functional outcomes.
Keywords: Blepharophimosis syndrome, polytetrafluoroethylene sling, Fox pentagon technique, children, frontalis suspension
Introduction
Blepharophimosis-ptosis-epicanthus (BPES; OMIM#110100) is an autosomal dominant inherited disorder characterized by malformation of the eyelid, including ptosis, narrowed horizontal palpebral aperture, epicanthus inversus, and telecanthus. 1 It has a global prevalence of approximately 1 in 50,000. 2
Surgical treatments for BPES always be performed in stages due to the complexity of related eyelid deformities. The first stage includes epicanthus and telecanthus correction performed using techniques such as the V-Y procedure, Mustarde’s double Z-plasty, and so on.3–5 The second stage is ptosis correction. In some patients, lateral canthoplasty is also used to further extend the palpebral fissure length (PFL) and is performed simultaneously with medial canthoplasty or after ptosis correction. In BPES, frontalis suspension is often used to correct the ptosis because of poor levator palpebrae superioris muscle function. Frontalis suspension surgery may involve the use of several surgical techniques and sling materials, including fascia lata, collagen, polypropylene, silicone, silk, nylon monofilament, polyester, and polytetrafluoroethylene (PTFE).6,7 Polytetrafluoroethylene (Gore-Tex; Gore and Associates, Flagstaff, AZ, USA) is used for frontalis suspension and achieves good functional and cosmetic results because of its biocompatibility and resistance to infection.8,9 Several suture designs, including single loop, Crawford’s double triangle, and Fox’s pentagon or double pentagon configurations, are used for frontalis suspension surgery and achieve similar functional and cosmetic outcomes in blepharoptosis.10,11
However, in BPES, the contour is not as satisfactory due to the abnormal development of eyelid tissues, including the tarsus, orbicularis, and levator palpebrae superioris; in addition, the thickness and compliance of the lid are different from those found in normal eyelids and might lead to a less smooth curvature of the palpebral margin and unsatisfactory geometric tenting of the preseptal skin.
In this study, we introduced a modified Fox pentagon technique performed using a PTFE sling in a frontalis suspension of blepharophimosis syndrome and evaluated its functional and cosmetic outcomes.
Methods
We retrospectively reviewed the medical records of 40 consecutive patients who were diagnosed with BPES and underwent frontalis suspension from March 2016 to October 2018 in the Department of Ophthalmology, Beijing Children’s Hospital. The study was approved by the Beijing Children’s Hospital Ethics Committee and conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from all participants or their guardians.
BPES was diagnosed based on the presence of ptosis, a narrowed horizontal palpebral aperture, epicanthus inversus, and telecanthus, and all the patients had undergone Y-V medial canthoplasty performed by one of the authors (Q.W.) at least half a year before enrollment. Exclusion criteria included atypical BPES, congenital or acquired blepharoptosis, an absence of Bell’s phenomenon, and a history of other eyelid surgeries. All patients underwent ophthalmologic examinations that included visual acuity, ocular motility, a slit lamp examination, and a fundus examination. Eyelid measurements were performed preoperatively and postoperatively and included vertical interpalpebral fissure height (PFH), horizontal PFL, the inner intercanthal distance (IICD), and the distance between the corneal light reflex and upper lid margin centrally (MRD1). These measurements were taken preoperatively and 1 day, 1 week, and 1, 3, 6, and 12 months after the operation and every year thereafter.
All patients underwent cosmetic grading on a 0 to 2 scale, with 0 indicating excellent results, 1 indicating good, and 2 indicating poor. Excellent was defined as a less than 1-mm height difference between the bilateral eyelids as well as good crease and contour. Good was defined as a 1-mm difference in eyelid height and/or an asymmetric crease, and poor was defined as a poor eyelid crease and contour asymmetry. 12 Three masked observers evaluated and scored all the postoperative photographs separately. The average of the scores was used for analysis.
All surgeries were performed by the same ophthalmologist (Q.W.). Frontalis suspension was performed in all patients under general anesthesia. An eyelid plate was placed to avoid ocular trauma. The skin was incised 2–3 mm above the upper eyelid margin, and the pretarsal orbicularis oculi were excised to expose the tarsus. Then, three separate incisions were made down to the level of the periosteum; two of these were placed above the brow medially and laterally, and a mid-incision was placed centrally at 15 mm above the brow. First, two PTFE slings were fixed to the tarsus medially and laterally, the medial arm of the medial sling was passed through the medial and mid-incisions, and the lateral arm was passed directly through the mid-incision. Similarly, the lateral arm of the lateral sling was passed through the lateral and mid-incisions, and the medial arm was passed directly through the mid-incision. The slings were adjusted to maintain a satisfactory curvature and height of the upper eyelid. The four arms ended in the mid-incision and were tied together. The knot was buried under the frontalis. The incisions were sutured using 6-0 absorbable sutures, and a Frost suture was used to protect the cornea (Figure 1).
Figure 1.
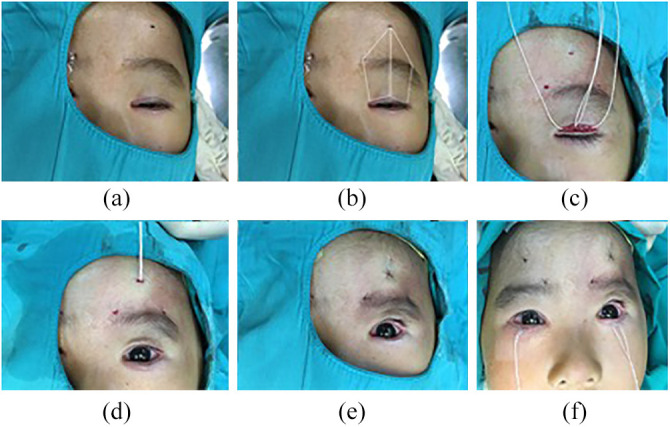
Steps of blepharoptosis correction: (a) skin marking, (b) diagrammatic representation of surgical techniques, (c) two PTFE slings were anchored to the tarsus medially and laterally, (d) the four arms of the PTFE slings were penetrated through the mid-incision, (e) the incisions were closed with 6-0 absorbable sutures, and (f) Frost sutures.
Statistical analyses were conducted using SPSS version 23.0 (IBM Corporation, Armonk, NY, USA). The paired t-test was used to compare the preoperative and postoperative PFH and MRD1 (the 6-month follow-up data were used for analysis). A p value less than 0.05 was considered statistically significant.
Results
A total of 40 patients who met the eligibility criteria were finally enrolled, including 23 males and 17 females. All patients were bilaterally involved, and a total of 80 eyes were included. The mean age of the participants was 3.25 (range: 2–7) years old. The postoperative follow-up duration was 21.6 (range: 6–36) months. The baseline characteristics were shown in Table 1.
Table 1.
Baseline characteristics of all patients.
| General characteristics | ||
|---|---|---|
| Sex (M: F), n | 23:17 | |
| Median age (range), years | 3.25 (2–7) | |
| Normal | Abnormal | |
| Ocular motility | 40 | 0 |
| Slit lamp examination | 40 | 0 |
| R | L | |
| Visual acuity (logMAR) | 0.23 ± 0.08 | 0.22 ± 0.13 |
| Spherical equivalents, D | 2.16 ± 2.37 | 1.99 ± 2.23 |
M: male, F: female, R: right, L: left, D: degree.
All patients achieved good cosmetic results without a chin-up head posture (Figure 2), and the average cosmetic outcome score was 0.6 ± 0.3. The mean PFH of the right eyes was 2.68 ± 0.62 mm preoperatively and 6.93 ± 0.87 mm postoperatively. The mean PFH of the left eyes was 2.73 ± 0.56 mm preoperatively and 6.98 ± 0.95 mm postoperatively. The mean MRD1 of the right eyes was 0.53 ± 0.80 mm preoperatively and 3.76 ± 0.55 mm postoperatively. The mean MRD1 of the left eyes was 0.50 ± 0.75 mm preoperatively and 3.78 ± 0.71 mm postoperatively. The differences in PFH and MRD1 between before and after surgery were statistically significant (p < 0.01). When right eyes and left eyes were compared, there was no significant difference either before or after the surgery (p > 0.01) (Table 2).
Figure 2.
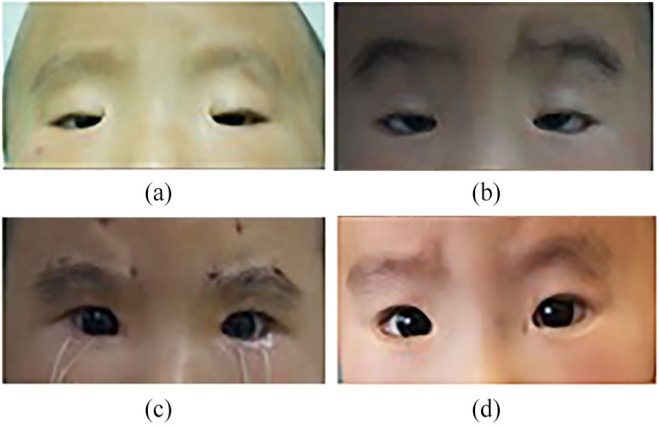
Comparison between before and after the surgeries: (a) before medial canthoplasty, (b) 6 months after medial canthoplasty, (c) 1 week after frontalis suspension, and (d) 6 months after frontalis suspension.
Table 2.
Preoperative and postoperative parameters for patients with BPES.
| Preoperative (mm) | Postoperative (mm) (6 months) | p | |
|---|---|---|---|
| PFH | |||
| Right | 2.68±0.62 | 6.93 ± 0.87 | 0.00 |
| Left | 2.73±0.56 | 6.98 ± 0.95 | 0.00 |
| MRD1 | |||
| Right | 0.53±0.80 | 3.76 ± 0.55 | 0.00 |
| Left | 0.50±0.75 | 3.78 ± 0.71 | 0.00 |
| BUT(s) | |||
| Right | 10.3±1.2 | 9.1 ± 1.3 | 0.63 |
| Left | 10.5±1.7 | 8.7 ± 1.6 | 0.71 |
| Corneal staining (N of positive) | |||
| Right | 0 | 8 | 0.00 |
| Left | 0 | 7 | 0.00 |
| Incomplete eyelid closure (N of positive) | |||
| Right | 0 | 40 | 0.00 |
| Left | 0 | 40 | 0.00 |
| Delayed upper eyelid (N of positive) | |||
| Right | 0 | 40 | 0.00 |
| Left | 0 | 40 | 0.00 |
BPES: blepharophimosis-ptosis-epicanthus; PFH: palpebral fissure height; BUT: break-up time.
Ptosis reoccurred in 1 of the 40 patients (2.5%) 1.5 years postoperatively, and 8 (20%) patients experienced conjunctival prolapse within 2 weeks postoperatively and recovered soon after using topical corticosteroid eye drops and undergoing binding up of the involved eyes. No infection, rejection of the PTFE sling, or exposure keratitis occurred in any patients.
Discussion
Blepharophimosis-ptosis-epicanthus inversus syndrome is a complex multiple eyelid malformation that is inherited in an autosomal-dominant pattern and often affects individuals with Asian ancestry. 13 Children born with BPES may experience psychological developmental problems due to the attitudes of the people around them, especially at kindergarten or school age. Visual development may also be affected by the occlusion of the eyelid. Affected children may adopt a chin-up posture to better expose their visual axis.14,15 Therefore, the goals of BPES surgery are symmetric and natural-appearing cosmetic results as well as improved visual and psychological development.
Some authors have recommended that one-stage surgical repair of BPES can achieve satisfactory results.16,17 Others have recommended that surgeries should be performed in stages due to the complexity of the eyelid malformation.4,18 One-stage technique is reported in some studies for the reduced chances of general anesthesia. However, the cosmetic outcomes are not satisfying due to the high skin tesion. To avoid the horizontal tension produced by performing medial canthoplasty against the vertical tension, we performed ptosis correction at 6 months after the medial canthoplasty. In BPES, frontalis suspension is often used to correct ptosis because of poor levator palpebrae superioris muscle function. Many biological or synthetic suspensory materials and frontalis flaps have been used for suspension. Autogenous fascia lata is still considered to be the most effective sling material because of its lower ptosis recurrence and lower complication rate, but it has certain limitations, including cicatricial contracture on the upper eyelid, scarring on the thigh, and the time-consuming general anesthesia required to harvest the graft.6,19 Many studies have shown that similar functional and cosmetic outcomes and ptosis recurrence were achieved using autogenous fascia and alloplastic materials.6,20
In this study, we chose PTFE as the sling material because of its good handling characteristics, lack of associated inflammatory response, and excellent biocompatibility.7,21 Some researchers reported that frontalis suspension for congenital blepharoptosis resulted in similar cosmetic and functional outcomes with autogenous fascia and other alloplastic materials. PTFE and autogenous fascia resulted in a lower recurrence rate, although that rate was not statistically significant.
Several suture designs, including a single loop, Crawford’s double triangle, and Fox’s pentagon or double pentagon configurations, have been used to perform frontalis suspension surgery and have yielded similar functional and cosmetic outcomes in congenital blepharoptosis.10,11 However, we found that this was not the case in BPES due to the presence of multiple malformations of the eyelid, the difference in thickness and compliance caused by congenital blepharoptosis, and because the margin and contour of the eyelid were not satisfactory after sling suspension. Thus, we created a modified Fox’s pentagon technique to add an upward force in the center of the pentagon baseline, thus effectively improving the shape of the upper eyelid contour, making it smoother and more natural. In this series, postoperative MRD1 values and PFH improved significantly, thus creating a very significant elevation of the upper eyelid and resolution of the ptosis in addition to obvious cosmetic improvement. Tenting of pretarsal and preseptal skin can influence cosmetic outcomes and are common in BPES; we found that sufficiently blunting the separation between the orbicularis muscle and orbital septum effectively improves this condition.
Complications of PTFE sling suspension include rejection, extrusion, granuloma, conjunctival prolapse, infection, and ptosis recurrence, all of which have been reported to be infrequent in the literature.6,21,22 In this study, we reported a recurrence rate of 2.5%, which was much lower than previously reported rates (4%–20%),6,20 potentially due to the fixation of PTFE on the tarsus. In this study, we used the open method, which allowed us to stabilize the PTFE position by directly securing the sling material to the tarsus and thereby reduce the recurrence rate. Notably, 20% (8/40) of the patients in this study experienced conjunctival prolapse and edema, mainly because of the shallow conjunctival sac observed in BPES patients. All patients resolved soon after administration of topical corticosteroid eye drops and binding up of the involved eyes. No rejection, extrusion, or granuloma was observed in this study, potentially due to the relatively deeper placement of the sling because the eyelids are thicker and more compact in BPES patients than in patients with congenital blepharoptosis. Furthermore, we immersed the sling in antibiotic solution before using it and reduced the amount of direct contact between the sling and the skin and eyelashes during the operation, and we found this approach to be useful in reducing the rate of infection.
There are several limitations to this study. First, the follow-up period was not long, and a longer follow-up period may possibly result in different findings regarding ptosis recurrence or postoperative complications. Second, we did not compare functional and cosmetic outcomes between our and other techniques, although our technique did yield satisfying results.
Conclusion
Experimentally, we created a modified Fox’s pentagon technique performed using a PTFE sling in frontalis suspension for BPES. This approach yielded favorable cosmetic and functional outcomes. Further observation is needed to obtain a more comprehensive evaluation of this technique.
Author biographies
Yuan Wang is an ophthalmologist in Beijing Children’s Hospital, Capital Medical University. Her work and research focus on pediatric ocular plastics and strabismus.
Qian Wu is an ophthalmologist in Beijing Children’s Hospital, Capital Medical University. Her work focus on pediatric ocular plastics and nasolacrimal diseases.
Li Li is an ophthalmologist in Beijing Children’s Hospital, Capital Medical University. Her research focus on ocular alignment and amblyopia.
Wen Liu is an ophthalmologist in Beijing Children’s Hospital, Capital Medical University. Her work focus on pediatric ocular plastics and amblyopia.
Cheng Li is an ophthalmologist in Beijing Children’s Hospital, Capital Medical University. Her work focus on pediatric ocular plastics and optometry.
Yunwei Fan is an ophthalmologist in Beijing Children’s Hospital, Capital Medical University. Her work focus on pediatric ocular plastics, nasolacrimal diseases and visual electrophysiology.
WenHong Cao is an ophthalmologist in Beijing Children’s Hospital, Capital Medical University. Her work focus on pediatric ocular plastics and Albers Schonberg disease.
Ningdong Li is an ophthalmologist in Beijing Children’s Hospital, Capital Medical University. His work and research bridges the field of genetic study of ophthalmology, ocular misalignment, congenital cranial disinnervation disorders.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Yuan Wang  https://orcid.org/0000-0001-9350-4061
https://orcid.org/0000-0001-9350-4061
References
- 1.Anttonen M, Pihlajoki M, Andersson N, et al. FOXL2, GATA4, and SMAD3 co-operatively modulate gene expression, cell viability and apoptosis in ovarian granulosa cell tumor cells. PLoS ONE 2014; 9(1): e85545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alexiadis M, Chu S, Leung D, et al. Transcriptomic analysis of stage 1 versus advanced adult granulosa cell tumors. Oncotarget 2016; 7(12): 14207–14219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beckingsale PS, Sullivan TJ, Wong VA, et al. Blepharophimosis: a recommendation for early surgery in patients with severe ptosis. Clin Exp Ophthalmol 2003; 31(2): 138–142. [DOI] [PubMed] [Google Scholar]
- 4.Li H, Li D, Jie Y, et al. Multistage correction of blepharophimosis: our rationale for 18 cases. Aesthetic Plast Surg 2009; 33(4): 576–581. [DOI] [PubMed] [Google Scholar]
- 5.Sa HS, Lee JH, Woo KI, et al. A new method of medial epicanthoplasty for patients with blepharophimosis-ptosis-epicanthus inversus syndrome. Ophthalmology 2012; 119(11): 2402–2407. [DOI] [PubMed] [Google Scholar]
- 6.Wasserman BN, Sprunger DT, Helveston EM. Comparison of materials used in frontalis suspension. Arch Ophthalmol 2001; 119(5): 687–691. [DOI] [PubMed] [Google Scholar]
- 7.Bajaj MS, Sastry SS, Ghose S, et al. Evaluation of polytetrafluoroethylene suture for frontalis suspension as compared to polybutylate-coated braided polyester. Clin Exp Ophthalmol 2004; 32(4): 415–419. [DOI] [PubMed] [Google Scholar]
- 8.Karesh JW. Polytetrafluoroethylene as a graft material in ophthalmic plastic and reconstructive surgery. An experimental and clinical study. Ophthalmic Plast Reconstr Surg 1987; 3(3): 179–185. [DOI] [PubMed] [Google Scholar]
- 9.Setzen G, Williams EF, 3rd. Tissue response to suture materials implanted subcutaneously in a rabbit model. Plast Reconstr Surg 1997; 100(7): 1788–1795. [DOI] [PubMed] [Google Scholar]
- 10.Fan J. Frontalis suspension technique with a temporalfasciae-complex sheet for repairing blepharoptosis. Aesthetic Plast Surg 2001; 25(3): 147–151. [DOI] [PubMed] [Google Scholar]
- 11.Crawford JS. Fascia lata: its nature and fate after implantation and its use in ophthalmic surgery. Trans Am Ophthalmol Soc 1968; 66: 673–745. [PMC free article] [PubMed] [Google Scholar]
- 12.Lee V, Konrad H, Bunce C, et al. Aetiology and surgical treatment of childhood blepharoptosis. Br J Ophthalmol 2002; 86(11): 1282–1286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nakajima T, Yoshimura Y, Onishi K, et al. One-stage repair of blepharophimosis. Plast Reconstr Surg 1991; 87(1): 24–31. [DOI] [PubMed] [Google Scholar]
- 14.Maras P, Brown R. Effects of different forms of school contact on children’s attitudes toward disabled and non-disabled peers. Br J Educ Psychol 2000; 70(Pt 3): 337–351. [DOI] [PubMed] [Google Scholar]
- 15.Westbom L. Well-being of children with chronic illness. A population-based study in a Swedish primary care district. Acta Paediatr 1992; 81(8): 625–629. [DOI] [PubMed] [Google Scholar]
- 16.Wu SY, Ma L, Tsai YJ, et al. One-stage correction for blepharophimosis syndrome. Eye 2008; 22(3): 380–388. [DOI] [PubMed] [Google Scholar]
- 17.Karacaoglan N, Sahin U, Ercan U, et al. One-stage repair of blepharophimosis: a new method. Plast Reconstr Surg 1994; 93(7): 1406–1409. [DOI] [PubMed] [Google Scholar]
- 18.Taylor A, Strike PW, Tyers AG. Blepharophimosis-ptosis-epicanthus inversus syndrome: objective analysis of surgical outcome in patients from a single unit. Clin Exp Ophthalmol 2007; 35(3): 262–269. [DOI] [PubMed] [Google Scholar]
- 19.Wilson ME, Johnson RW. Congenital ptosis. Long-term results of treatment using lyophilized fascia lata for frontalis suspensions. Ophthalmology 1991; 98(8): 1234–1237. [PubMed] [Google Scholar]
- 20.Wagner RS, Mauriello JA, Jr, Nelson LB, et al. Treatment of congenital ptosis with frontalis suspension: a comparison of suspensory materials. Ophthalmology 1984; 91(3): 245–248. [DOI] [PubMed] [Google Scholar]
- 21.Steinkogler FJ, Kuchar A, Huber E, et al. Gore-Tex soft-tissue patch frontalis suspension technique in congenital ptosis and in blepharophimosis-ptosis syndrome. Plast Reconstr Surg 1993; 92(6): 1057–1060. [DOI] [PubMed] [Google Scholar]
- 22.Mehta P, Patel P, Olver JM. Functional results and complications of Mersilene mesh use for frontalis suspension ptosis surgery. Br J Ophthalmol 2004; 88(3): 361–364. [DOI] [PMC free article] [PubMed] [Google Scholar]


