Abstract
This literature review focuses on the evidence implicating oxidative stress in the pathogenesis of manganese neurotoxicity. This review is not intended to be a systematic review of the relevant toxicologic literature. Instead, in keeping with the spirit of this special journal issue, this review highlights contributions made by Professor Michael Aschner’s laboratory in this field of study. Over the past two decades, his laboratory has made significant contributions to our scientific understanding of cellular responses that occur both in vitro and in vivo following manganese exposure. These studies have identified molecular targets of manganese toxicity and their respective roles in mitochondrial dysfunction, inflammation, and cytotoxicity. Other studies have focused on the critical role astrocytes play in manganese neurotoxicity. Recent studies from his laboratory have used C. elegans to discover new facets of manganese-induced neurotoxicity. Collectively, his body of work has dramatically advanced the field and presents broader implications beyond metal toxicology.
Keywords: manganese, neurotoxicity, oxidative stress, mechanisms, C. elegans
1. Introduction
Manganese is an essential nutrient that plays a critical role in protein, lipid, and carbohydrate metabolism in animals and humans. Manganese serves as an enzyme cofactor and is incorporated into several metalloenzymes, including manganese superoxide dismutase (MnSOD), arginase, glutamine synthetase, phosphoenolpyruvate decarboxylase, and pyruvate carboxylase [1,2]. Mammalian tissues normally contain 0.3–3.0 μg Mn/g wet tissue weight [3]. The body’s nutritional requirements for manganese are normally met through dietary intake via food and drinking water. The estimated safe and adequate daily dietary intakes (ESADDI) for manganese required to maintain body stores is 2 to 5 mg/day in adults and 1.5 to 2.0 mg/day for children 4 to 6 years of age [4]. To ensure adequate nutrition in neonates, manganese is often added to infant formula because there is a greater need for this element during growth and development [5].
Exposure to excessive amount of manganese can result in manganese neurotoxicity, producing adverse effects most notably in the human extrapyramidal system [6,7,8]. Neurotoxicity can occur following high-dose oral, inhalation, or parenteral exposure to manganese. The development of neurotoxicity following different routes of exposure indicates that the dose to target tissue is the critical determinant of manganese toxicity, regardless of route. This association between manganese and neurotoxicity was first noted by Couper in 1837 who reported abnormal neurologic effects in workers at an ore-grinding plant where “black oxide of manganese” was processed [9]. Most epidemiologic research on manganese conducted during the late 20th century focused on occupational inhalation exposure. Subsequent epidemiologic studies of welders, manganese miners, battery producers, and other manganese workers have clearly established a causal association between chronic high-dose-manganese exposure via inhalation and neurotoxicity [10]. Hallmarks of manganese neurotoxicity in adults include behavioral changes, cognitive deficits, progressive bradykinesia, dystonia, and other gait abnormalities [11,12,13]. There has been increasing concern regarding the role of environmental manganese exposure and children’s health [14]. Manganese has been identified as a risk factor for the development of aggressive behavior, attention deficit, cognitive decline resulting in lowered IQ, and learning deficits in infants and children [15,16,17,18].
Analysis of brain samples have shown that manganese accumulates within the human striatum, globus pallidus, and substantia nigra [3,19]. Manganese accumulation in these brain regions is associated with the presence of the divalent metal transporter 1 (DMT1) although additional transporters may play a role in brain uptake of manganese [20,21,22]. Brain imaging studies that rely on the paramagnetic properties of manganese that result in increased signal intensity seen with T1-weighted magnetic resonance imaging (MRI), allow for visual inspection of the brain for evidence of manganese accumulation at this site. Brain MRI studies of highly exposed people reveal signal intensity changes in the globus pallidus, striatum, and midbrain consistent with manganese accumulation at these sites [23,24]. Studies performed in nonhuman primates have shown that changes in the T1-weighted image correlate with manganese tissue concentration [25]. The primary neuropathologic target of manganese neurotoxicity is the globus pallidus (particularly the internal segment) with sparing of the substantia nigra pars compacta and an absence of Lewy bodies [26]. Studies of a manganese-exposed South African mine worker have revealed reduced astrocyte and neuron density in both the caudate and putamen [27]. Chronic manganese neurotoxicity in people is also associated with decreased γ-aminobutyric acid (GABA) neurons, reduced myelinated fibers, and moderate astrocytic proliferation in the medial segment of the globus pallidus [26].
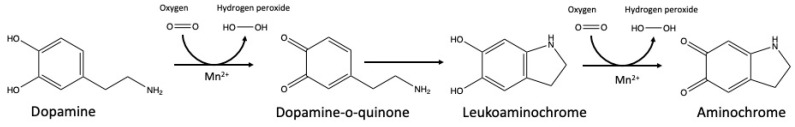
Several studies have examined neurochemical changes following high-dose-manganese exposure. Because manganese neurotoxicity results in dysregulation of motor control, many studies have focused on the striatal and pallidal dopaminergic system. Manganese reacts with dopamine and other biogenic amines resulting in oxidative damage to the neurotransmitters [28]. One pathway involves manganese catalyzed oxidation of the alpha hydroxyl group of dopamine forming a semi-quinone radical (Figure 1). The semi-quinone radical then reacts with oxygen to generate superoxide anion radical [O2•−] and a quinone. Oxygen can reoxidize the quinone to quinol to generate hydrogen peroxide [28]. Manganese-catalyzed dopamine auto-oxidation may also involve semiquinone and aminochrome intermediates, l-cysteine or copper, and NADH facilitation [29,30]. Excess manganese may also alter glutamate homeostasis in the basal ganglia [31]. Changes in glutamate homeostasis have been associated with excitotoxicity in the CNS [31].
Figure 1.
Manganese-catalyzed autoxidation of dopamine involves redox cycling of Mn2+ and Mn3+ in a series of reactions that generate hydrogen peroxide (H2O2), dopamine-o-quinone and aminochrome.
In vivo mammalian studies have shown that manganese exposure can result in altered levels of dopamine and its metabolites (e.g., 3,4-dihydroxyphenylacetic acid) and alter dopaminergic neurotransmission [32,33]. Alterations in manganese dopamine transmission can occur in the absence of detectable neuropathology. Although the initial focus on neurochemical effects is primarily centered on dopaminergic transmission, alterations in other neurotransmitter systems, including GABA and acetylcholine, also occur following manganese exposure [34,35]. Changes in striatal GABA, norepinephrine, and serotonin function are seen following manganese exposure in rodents [35].
Important species differences have been demonstrated with respect to manganese neurotoxicity [3]. Rodents generally fail to develop a behavioral syndrome or neuropathological lesion comparable to that seen in manganese-poisoned humans. Nevertheless, experimental studies have demonstrated that high-dose-intraperitoneal-manganese exposure impairs memory, learning ability and locomotor function in mice [36,37]. Manganese exposure also results in dopaminergic neuron loss in the striatum of MitoPark mice, a mitochondrially defective transgenic mouse model of Parkinson’s Disease [38]. Nonhuman primates best replicate the neurotoxic effects observed in humans. Manganese-exposed monkeys develop gait and other motor abnormalities that mimic those observed in affected humans [39,40,41]. Monkeys also develop reduced levels of striatal and pallidal dopamine and 3,4-dihydroxyphenylacetic acid, in conjunction with loss of dopaminergic neurons. These changes occur in the absence of loss of dopamine terminals in the caudate and putamen [39]. Monkeys also develop deficits in spatial and non-spatial working memory as well as effects on visuospatial-paired associate learning [42,43,44]. Histological assessment of the frontal cortex from manganese-exposed monkeys has also shown the presence of cells with apoptotic stigmata and astrocytosis in both the gray and white matter and α-synuclein aggregation in the frontal cortex gray and white matter [45].
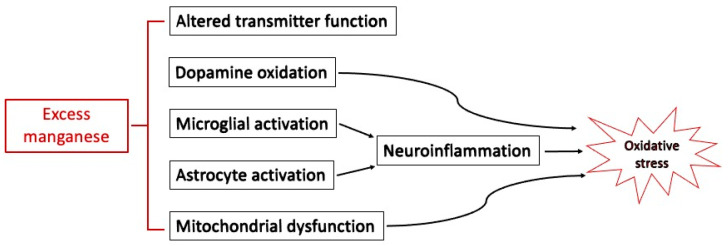
The mechanism of action of manganese neurotoxicity remains the subject of ongoing research [46]. Molecular mechanisms of manganese neurotoxicity involve multiple neuronal cell types and can include mitochondrial impairment, oxidative stress, inflammation, and excitotoxicity [46,47]. Manganese can trigger glial activation and neuroinflammation in both microglia and astrocytes [48]. Welders exposed to manganese have altered methylation patterns in the DNA that codes for inducible nitric oxide synthase [49]. This review largely focuses on the role of oxidative stress in manganese neurotoxicity (Figure 2) with special attention to the role of work from the Aschner laboratory.
Figure 2.
Mechanisms involved in manganese neurotoxicity.
2. Reactive Oxygen Species (ROS) and Neurotoxicity
Reactive oxygen species (ROS) are molecular oxygen products that play an important role in normal biology and disease [50]. Both non-radical (e.g., hydrogen peroxide, molecular oxygen) and free radical (e.g., superoxide anion radical [O2•−], hydroxyl radical [•OH], peroxyl radical [ROO•]) forms of ROS exist. Normal endogenous production of cellular ROS primarily occurs through mitochondrial oxidative phosphorylation at the electron transport chain when molecular oxygen is reduced [51]. During transport, some electrons react with molecular oxygen forming O2−• [52]. Elevated mitochondrial ROS production can cause mitochondrial dysfunction and contribute to neurologic disease [53,54].
Despite its role in disease, ROS are also required for numerous normal cellular processes including cell growth, differentiation, and death by acting as signaling molecules. ROS activates the nuclear factor erythroid 2 (NF-E2)-related factor 2/Kelch-like ECH-associated protein 1 (NRF2/KEAP1) pathway, which serves as a master regulator of ROS levels [55,56]. Other pathways regulated by ROS include nuclear factor-κB (NF-κB), phosphoinositide 3-kinase (PI3K)/AKT, and mitogen-activated protein kinase (MAPK) [57]. As a result, ROS activate diverse molecular targets, initiating pathways involved in growth promotion and survival (including autophagy) or apoptosis [58].
Redox homeostasis within cells is the result of cellular processes that balance ROS production and antioxidant capacity. Oxidative stress occurs when this balance is perturbed and ROS production overwhelms the cellular antioxidant defense, damaging nucleic acids, proteins, and lipids. The brain has several features that predispose it to oxidative stress, including disproportionately high-oxygen consumption, lack of stored ATP, high-lipid content, among others [28]. There is growing literature that oxidative stress plays a role in manganese neurotoxicity as well as other neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease (PD), Huntington’s disease (HD), and aging [59].
3. Oxidative Stress and Manganese: Physicochemical Properties
Manganese has eleven oxidation states ranging from Mn−3 to Mn+7, with Mn+7 having the strongest oxidation state of the group [60]. In the body, manganese exists in several valence states including divalent (Mn2+) and trivalent (Mn3+) forms. The reduced form of manganese (Mn+2) has a lower oxidative stress potential when compared with the trivalent (Mn+3) oxidized form of this metal [61,62,63]. The valence form of manganese can influence in vitro cytotoxicity with the trivalent form being more potent than the divalent form [63,64]. Intracellular formation of Mn3+, following oxidation of Mn2+, likely plays a minimal direct role in manganese neurotoxicity [65]. Manganese can secondarily alter the redox balance of iron, copper, and other transition metals [60,62,66]. Manganese promotes mitochondrial peroxide (H2O2) production even at physiologic concentrations [67]. Given the ability of manganese to participate in redox reactions, it is widely hypothesized that oxidative stress plays a role in manganese neurotoxicity [68].
In biological systems the redox active transition metals iron and copper, may participate in electron transfer reactions that produce hydroxyl free radical (·OH) via Fenton-type reactions resulting in oxygen radical damage [69,70]. Evolutionarily cells have developed protective antioxidant systems to scavenge these reactive oxygen products. The higher reduction potential of manganese when compared with iron limits its participation in Fenton-like redox chemistry [71].
4. Anti-Oxidants as Mediators of Manganese Neurotoxicity
Relative to the liver, the brain has lower levels of catalase activity, cytosolic GSH concentrations, and glutathione peroxidase 4 expression [28]. Reduced glutathione peroxidase 4 expression has been linked with ferroptosis, an intracellular iron-dependent form of cell death that has been proposed as a contributing mechanism in manganese neurotoxicity [72]. Another family of proteins with antioxidant properties are the peroxiredoxins. These peroxidases are involved in redox homeostasis, phospholipid turnover, glycolipid metabolism, and cellular signaling [73]. Peroxiredoxin 2 is present in the central nervous system and reduces ROS production by catalyzing hydrogen peroxide [74]. Metallothionein also plays a role as a free radical scavenger and is also involved in the metabolism of zinc and some other metals [75,76]
Manganese is incorporated into manganese superoxide dismutase (MnSOD) the principal antioxidant enzyme found in mammalian cells. This enzyme converts superoxide anion radicals to hydrogen peroxide and oxygen in mitochondria [77]. Thus, MnSOD plays a critical role in mitochondrial and cellular redox homeostasis and protects cells from oxidative stress. Genetic deletion of MnSOD is typically lethal in rodents, while a neuron specific deletion in spinal cord neurons results in extensive demyelination and axonal degeneration, elevated production of inflammatory cytokines, and microglia activation [78].
Additional discussion of the role of antioxidants in manganese neurotoxicity follows.
5. The Role of Mitochondrial Oxidative Stress in Manganese Neurotoxicity
The human brain’s reliance on ATP production leads to it consuming approximately 20% of the total basal oxygen budget [28]. Meeting neuronal ATP demands requires mitochondria, which in addition to ATP production are also involved in cell signaling, calcium homeostasis, and other cellular processes. Mitochondria are also the main intracellular storage site for manganese [79]. Manganese is mainly transported into the mitochondria via the mitochondrial Ca2+ uniporter system [80]. As mentioned earlier, mitochondrial manganese primarily exists as Mn2+ [79]. Although Mn+2 is less reactive when compared with Mn+3, increased mitochondrial manganese concentrations have numerous biological effects, including inhibition of oxidative phosphorylation [81,82], increased mitochondrial matrix calcium concentration [83], and inhibition of brain mitochondria respiratory complexes I–IV [84,85].
Altered mitochondrial activity in rat pheochromocytoma (PC12) cells treated with manganese is associated with altered mitochondrial activity [85]. Changes in mitochondrial function in the PC12 cells occurred along with reduced glutathione (GSH) concentrations and decreased catalase activity [85]. These effects can result in increased production of reactive oxygen (ROS) and reactive nitrogen species with subsequent oxidative stress. Pretreatment of cell cultures with antioxidants (e.g., ascorbic acid, GSH, N-acetyl cysteine) can mitigate some manganese-induced effects on mitochondrial function [86,87,88]. Manganese-induced impairment of mitochondrial membrane potential is partially rescued by pretreatment with inhibitors of p53 transcriptional activity and p53 mitochondrial translocation [89]. Rat striatal neurons develop dose-dependent decreases in mitochondrial membrane potential and complex II activity following in vitro exposure to manganese [90]. Striatal neurons exposed for two days to manganese at 5 μM developed DNA fragmentation and decreased expression of microtubule-associated protein MAP-2, suggesting that manganese may trigger apoptotic-like neuronal death secondary to mitochondrial dysfunction [90]. However, recent studies have shown that manganese-induced effects on mitochondrial function only occur at concentrations that initiate cell death, suggesting that mitochondrial dysfunction plays a limited role in cytotoxicity [91].
The weight of evidence suggests that mitochondrial dysfunction may be an initiating event for manganese neurotoxicity leading to overproduction of both ROS and reactive nitrogen species (RNS). Altered ROS and RNS production results in altered cell signaling, including activation of proinflammatory signaling and apoptotic cell death [92].
6. Caenorhabditis elegans as an Animal Model of Manganese Neurotoxicity
There is a growing interest in toxicology in the use of so-called New Alternative Models (NAMs) to reduce reliance on mammalian-based toxicity testing [93]. The Aschner laboratory has been at the forefront of using the nematode, C. elegans, to study the roles of oxidative stress, mitochondrial dysfunction, and dopaminergic neurodegeneration following manganese exposure [94,95]. The approximately 19,000 genes in the genome of this nematode have 60–80% homology with the mammalian genome [96] and C. elegans and mammals share many biological functions. The C. elegans nervous system is completely defined with 302 neurons and 56 glial cells or 381 neurons and 92 glial cells in either hermafrodite or males, respectively [97,98]. The C. elegans hermaphrodite possesses eight dopaminergic neurons, consisting of three pairs within the head and one pair in a posterior lateral position [99,100]. The dopaminergic system of C. elegans is more sensitive to the effects of manganese when compared with other neuron classes [101]. Exposure of early stage (L1) C. elegans larvae to manganese results in degeneration of these dopaminergic neurons in L1, L4 and young adults [102,103,104,105]. Exposure of C. elegans to manganese also results in behavioral changes. For example, manganese exposure alters olfactory learning and memory in L1 C. elegans [106].
Manganese toxicity in C. elegans can result in reduced GSH levels, generation of ROS, mitochondrial changes, and death [105,107,108]. Recent studies investigating this association have used nematodes with mutant forms of hpo-9 (e.g., tm3719), the worm homolog of BTBD9. These worms demonstrate hyperactive egg-laying behavior and have been proposed as a model organism for the study of restless leg syndrome in people [109]. When compared with wild type nematodes, tm3719 and hpo-9 knockout worms were more sensitive to manganese exposure with higher production of ROS and decreased numbers of intact mitochondria [110].
7. Astrocytes as Targets for Manganese Neurotoxicity
Interactions between neurons and astrocytes are critical for maintaining homeostasis of glutamate, glutamine, and GABA. Astrocytes contain glutamine synthetase, which catalyzes the conversion of L-glutamate, ATP, and ammonia into L-glutamine, ADP, and phosphate. Synthesized glutamine is subsequently released extracellularly and taken up by neurons and metabolized to glutamate by glutaminase. Synaptic glutamate released from neurons is removed by astrocytes through several cell membrane sodium-dependent transporters, including glutamate-aspartate transporter (GLAST) and glutamate transporter 1 (GLT1).
Manganese is preferentially localized in astrocytes in the brain at levels that are 50–200 times higher than those seen in neurons [111,112]. Manganese influences astrocyte morphology [113,114]. In vitro studies have shown that astrocyte uptake of Mn2+ depends on transferrin and DMT1 [115]. Expression and activity of glutamine synthetase in rat primary astrocytes is reduced following in vitro exposure to manganese [116]. In vitro studies using Chinese hamster ovary cells with increased expression of GLAST and GLT-1 have shown that manganese reduces glutamate transport into these cells [117]. Manganese deregulates expression of glutamine and glutamate transporters via protein kinase C pathway activation [118,119]. Downregulation of GLAST and GLT-1 transporter expression also occurs in rhesus monkeys following manganese inhalation [120]. Treatment of astrocytes with either estrogen or tamoxifen will reverse manganese-induced glutamate transporter impairment in astrocytes via increased transforming growth factor beta1 expression [121].
In vitro treatment of astrocytes with manganese results in shifts in the intracellular redox potential towards the oxidized state and results in induction of oxidative stress, mitochondrial dysfunction, and altered glutamine/glutamate cycling [122,123]. Exposure of astrocytes to manganese increases nitric oxide (NO) synthesis in these glial cells [124]. Astrocytes treated with manganese also demonstrate enhanced expression of inflammatory cytokines and chemokines that can be amplified by neighboring microglial cells [125,126]. Manganese activates astrocyte caspase-3 and phosphorylated extracellular signal-regulated kinase (p-ERK) via mitochondrial-dependent pathways [127]. Down regulation of the redox sensing protein 1 (DJ-1)/PARK7 increases the susceptibility of astrocytes to manganese-induced oxidative stress [128].
Impacts of manganese on other glial cells should not be ignored. For example, NF-κB signaling in microglia regulate the production and release of cytokines and chemokines that amplify the activation of astrocytes [125,126,129]. Thus, microglial play a role in mediating neuroinflammatory responses during manganese neurotoxicity. Microglial cells are also involved in ROS production and oxidative stress. In vitro exposure of rat microglia to manganese results in a time- and concentration-dependent release of hydrogen peroxide [130]. Manganese-induced release of hydrogen sulfide by microglia was reduced by mitogen-activated protein kinases inhibitors. Manganese treatment of microglia also activated ERK and p38-MAPK that preceded hydrogen peroxide production [130]. Studies with microglia-depleted dopaminergic neuron cultures show that depletion of microglia reduces manganese-induced neuron injury [131].
8. The Role of Oxidative Stress in Manganese Neurotoxicity: In Vivo Mammalian Studies
My laboratory enjoyed a multi-year collaboration with the Aschner laboratory that evaluated markers of oxidative stress in rodents following manganese inhalation [132]. Several exposure paradigms were used in these inhalation studies including 14-day, subchronic, and developmental studies [133,134,135,136]. During the subchronic study [135], young adult male and female CD rats and senescent male rats were exposed 6 h/day, 5 days/week for 90 days to air or manganese sulfate at 0.01, 0.1, or 0.5 mg Mn/m3 or manganese phosphate at 0.1 mg Mn/m3. Oxidative stress biomarkers that were evaluated by Aschner and colleagues included measurement of GSH and metallothionein concentrations, and glutamine synthetase protein levels, as well as metallothionein and glutamine synthetase mRNA levels in the cerebellum, olfactory bulb, striatum, hippocampus, and hypothalamus from control and manganese-exposed rats [137,138,139,140]. Depletion of oxidative scavengers such as glutathione and metallothionein occurred in some brain regions [138]. In juvenile and 16-month-old rats that inhaled either manganese sulfate or manganese phosphate, total GSH levels significantly decreased in the olfactory bulb of manganese-exposed young males and increased in the female olfactory bulb. Both aged and young female rats had significantly reduced GSH in the striatum following manganese inhalation. Senescent male rats exhibited decreased GSH levels in the cerebellum and hypothalamus following manganese inhalation [140]. Total GSH level was reduced in several brain regions of male rats exposed to manganese during early development. In female rats, GSH was unchanged, or upregulated in the olfactory bulb [68].
Other in vivo rodent studies also report manganese-induced oxidative stress in various regions of the rodent brain, particularly in the basal ganglia, such as globus pallidus, striatum, and substantia nigra [34,61,141,142,143,144]. Conflicting data from rodent studies have also been reported. For example, a study from our laboratory failed to demonstrate evidence of increased striatal ROS or whole-brain 8-hydroxy-2’ -deoxyguanosine (8-OHdG) levels despite increased brain and mitochondrial manganese concentrations, altered motor activity, and decreased body weight in rats following either adult or developmental exposure to oral manganese [145].
As noted earlier, unlike rodents, nonhuman primates largely replicate the neurotoxic effects observed in humans [7]. Chronic manganese exposure did not produce the loss of dopamine terminals in the caudate and putamen based on [11C]- methylphenidate PET imaging of exposed animals [146,147]. Histologic assessment of the frontal cortex from manganese-exposed monkeys has revealed the presence of cells with apoptotic stigmata and astrocytosis in both the gray and white matter and a-synuclein aggregation in the frontal cortex gray and white matter [45]
The role of oxidative stress in manganese neurotoxicity in nonhuman primates has also been examined and largely stems from studies performed in our laboratory to characterize manganese pharmacokinetics in young male rhesus monkeys following inhalation [148]. In this study, monkeys were exposed to either air or manganese sulfate at either 0.06, 0.3, or 1.5 mg Mn/m3 for 65 exposures. Additional monkeys were exposed to manganese sulfate at 1.5 mg Mn/m3 for 15 or 33 exposures and evaluated immediately thereafter or for 65 exposures followed by a 45- or 90-day delay before evaluation [148]. Brain imaging studies using T1-weighted magnetic resonance imaging revealed dose-dependent increases in MRI signal hyperintensities within the olfactory bulb and the globus pallidus [25]. As the exposure increased, manganese-induced hyperintensities involved multiple brain regions that were confirmed using chemical analysis of affected bran regions.
Biochemical endpoints indicative of oxidative stress and excitotoxicity were assessed in the cerebellum, frontal cortex, caudate, globus pallidus, olfactory cortex, and putamen of monkeys exposed to manganese [120,149]. Glutamine synthetase, GLT-1, GLAST and tyrosine protein levels, metallothionein, GLT-1, GLAST, tyrosine hydroxylase and GS mRNA levels, and total GSH levels were determined for all brain regions [120,149]. Manganese exposure differentially affected these biomarkers in each brain region. For example, GSH was increased in the frontal cortex and decreased in the caudate despite two- to threefold increases in manganese concentrations in these regions. Exposure to manganese sulfate persistently decreased metallothionein mRNA in the caudate when compared to air-exposed controls. In contrast, putamen metallothionein mRNA levels were unaffected by manganese exposure. The glutamate transporters GLT-1 and GLAST were relatively unaffected by short term manganese exposure, except in the globus pallidus where exposure for 33 days led to decreased protein levels, which persisted after 45 days of recovery for both proteins and 90 days of recovery in the case of GLAST. Exposure to 1.5 mg Mn/m3 caused a significant decrease in GSH levels in the caudate and increased GSH levels in the putamen of monkey exposed for 15 and 33 days, with both effects persisting at least 90 days post-exposure. Tyrosine hydroxylase protein levels were significantly lowered in the globus pallidus of the monkeys exposed for 33 days, but mRNA levels were significantly increased in this same region. All manganese-exposed monkeys had decreased pallidal glutamine synthetase protein, decreased caudate GLT-1 mRNA, decreased pallidal GLAST protein, and increased olfactory tyrosine hydroxylase mRNA levels.
Studies exploring the role of oxidative stress in human manganese neurotoxicity are extremely limited and primarily rely on in vitro exposure of human cells, as reviewed earlier. Additional studies using noninvasive methods to assess redox status in manganese-exposed humans are needed.
9. Conclusions
As this review demonstrates, molecular mechanisms are involved with manganese neurotoxicity. Although oxidative stress may play a critical role, it may not serve as the initiating event. Rather it is likely that the initiating event is an increase in intracellular levels of manganese because of manganese overexposure. Pharmacokinetic models predict that increases in globus pallidal manganese concentrations in humans above approximately 0.55 μg Mn/g trigger adverse neurologic effects [150]. Elevated brain manganese levels are partially sequestered in mitochondria, resulting in mitochondrial dysfunction and secondary oxidative stress. Elevated production of ROS can lead to further mitochondrial injury resulting in neurotoxicity. Thus, the respective roles of manganese overexposure, mitochondrial dysfunction, and oxidative stress are tightly interwoven.
This review has largely focused on only one aspect of research stemming from Professor Aschner’s laboratory. Work from Professor Aschner’s laboratory has provided a wealth of data demonstrating that oxidative stress and mitochondrial dysfunction are critical molecular mechanism involved in manganese neurotoxicity. His work has provided insights into how elevated intracellular manganese concentrations results in a cascade of events linking oxidative stress and mitochondrial dysfunction with abnormal cellular function. This research is not only relevant for manganese neurotoxicity but also promises to hold broader future impact in improving our understanding of mechanisms involved in other neurological disorders. Aschner’s work with C. elegans also helps pave the way for the use of this animal model in neurotoxicity research. This effort is well aligned with ongoing international efforts to decrease reliance on vertebrate animal models in neurotoxicology. Dr. Aschner’s work also helps to illustrate the power of collaborative science and serves as a model for other scientists.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
All data is contained herein.
Conflicts of Interest
The author declares no conflict of interest.
Funding Statement
Development of this review received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Balachandran R.C., Mukhopadhyay S., McBride D., Veevers J., Harrison F.E., Aschner M., Haynes E.N., Bowman A.B. Brain manganese and the balance between essential roles and neurotoxicity. J. Biol. Chem. 2020;295:6312–6329. doi: 10.1074/jbc.REV119.009453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horning K.J., Caito S.W., Tipps K.G., Bowman A.B., Aschner M. Manganese is essential for neuronal health. Annu. Rev. Nutr. 2015;35:71–108. doi: 10.1146/annurev-nutr-071714-034419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aschner M., Erikson K.M., Dorman D.C. Manganese dosimetry: Species differences and implications for neurotoxicity. Crit. Rev. Toxicol. 2005;35:1–32. doi: 10.1080/10408440590905920. [DOI] [PubMed] [Google Scholar]
- 4.Greger J.L. Dietary standards for manganese: Overlap between nutritional and toxicological studies. J. Nutr. 1998;128:368S–371S. doi: 10.1093/jn/128.2.368S. [DOI] [PubMed] [Google Scholar]
- 5.Aschner J.L., Aschner M. Nutritional aspects of manganese homeostasis. Mol. Aspects. Med. 2005;26:353–362. doi: 10.1016/j.mam.2005.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Andruska K.M., Racette A.B. Neuromythology of manganism. Curr. Epidemiol. Rep. 2015;2:143–148. doi: 10.1007/s40471-015-0040-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dorman D.C. Extrapyramidal system neurotoxicity: Animal models. Handb. Clin. Neurol. 2015;131:207–223. doi: 10.1016/B978-0-444-62627-1.00012-3. [DOI] [PubMed] [Google Scholar]
- 8.Kulshreshtha D., Ganguly J., Jog M. Manganese and movement disorders: A review. J. Mov. Disord. 2021;14:93–102. doi: 10.14802/jmd.20123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Couper J. On the effects of black oxide of manganese when inhaled into the lungs. Br. Ann. Med. Pharm. Vital Stat. Gen. Sci. 1837;1:41. [Google Scholar]
- 10.Lucchini R.G., Martin C.J., Doney B.C. From manganism to manganese-induced parkinsonism: A conceptual model based on the evolution of exposure. Neuromol. Med. 2009;11:311–321. doi: 10.1007/s12017-009-8108-8. [DOI] [PubMed] [Google Scholar]
- 11.Bowler R.M., Gysens S., Diamond E., Nakagawa S., Drezgic M., Roels H.A. Manganese exposure: Neuropsychological and neurological symptoms and effects in welders. Neurotoxicology. 2006;27:315–326. doi: 10.1016/j.neuro.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 12.Roels H.A., Bowler R.M., Kim Y., Claus Henn B., Mergler D., Hoet P., Gocheva V.V., Bellinger D.C., Wright R.O., Harris M.G., et al. Manganese exposure and cognitive deficits: A growing concern for manganese neurotoxicity. Neurotoxicology. 2012;33:872–880. doi: 10.1016/j.neuro.2012.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruiz-Azcona L., Fernández-Olmo I., Expósito A., Markiv B., Paz-Zulueta M., Parás-Bravo P., Sarabia-Cobo C., Santibáñez M. Impact of environmental airborne manganese exposure on cognitive and motor functions in adults: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health. 2021;18:4075. doi: 10.3390/ijerph18084075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zoni S., Lucchini R.G. Manganese exposure: Cognitive, motor and behavioral effects on children: A review of recent findings. Curr. Opin. Pediatr. 2013;25:255–260. doi: 10.1097/MOP.0b013e32835e906b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bjørklund G., Chartrand M.S., Aaseth J. Manganese exposure and neurotoxic effects in children. Environ. Res. 2017;155:380–384. doi: 10.1016/j.envres.2017.03.003. [DOI] [PubMed] [Google Scholar]
- 16.Carvalho C.F., Menezes-Filho J.A., de Matos V.P., Bessa J.R., Coelho-Santos J., Viana G.F., Argollo N., Abreu N. Elevated airborne manganese and low executive function in school-aged children in Brazil. Neurotoxicology. 2014;45:301–308. doi: 10.1016/j.neuro.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 17.Menezes-Filho J.A., de Carvalho-Vivas C.F., Viana G.F., Ferreira J.R., Nunes L.S., Mergler D., Abreu N. Elevated manganese exposure and school-aged children’s behavior: A gender-stratified analysis. Neurotoxicology. 2014;45:293–300. doi: 10.1016/j.neuro.2013.09.006. [DOI] [PubMed] [Google Scholar]
- 18.Rodrigues J.L.G., Araújo C.F.S., Dos Santos N.R., Bandeira M.J., Anjos A.L.S., Carvalho C.F., Lima C.S., Abreu J.N.S., Mergler D., Menezes-Filho J.A. Airborne manganese exposure and neurobehavior in school-aged children living near a ferro-manganese alloy plant. Environ. Res. 2018;167:66–77. doi: 10.1016/j.envres.2018.07.007. [DOI] [PubMed] [Google Scholar]
- 19.Nagatomo S., Umehara F., Hanada K., Nobuhara Y., Takenaga S., Arimura K., Osame M. Manganese intoxication during total parenteral nutrition: Report of two cases and review of the literature. J. Neurol. Sci. 1999;162:102–105. doi: 10.1016/S0022-510X(98)00289-5. [DOI] [PubMed] [Google Scholar]
- 20.Crossgrove J.S., Yokel R.A. Manganese distribution across the blood-brain barrier III. The divalent metal transporter-1 is not the major mechanism mediating brain manganese uptake. Neurotoxicology. 2004;25:451–460. doi: 10.1016/j.neuro.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 21.Fitsanakis V.A., Piccola G., Marreilha dos Santos A.P., Aschner J.L., Aschner M. Putative proteins involved in manganese transport across the blood-brain barrier. Hum. Exp. Toxicol. 2007;26:295–302. doi: 10.1177/0960327107070496. [DOI] [PubMed] [Google Scholar]
- 22.Nyarko-Danquah I., Pajarillo E., Digman A., Soliman K.F.A., Aschner M., Lee E. Manganese accumulation in the brain via various transporters and its neurotoxicity mechanisms. Molecules. 2020;25:5880. doi: 10.3390/molecules25245880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fitsanakis V.A., Zhang N., Avison M.J., Gore J.C., Aschner J.L., Aschner M. The use of magnetic resonance imaging (MRI) in the study of manganese neurotoxicity. Neurotoxicology. 2006;27:798–806. doi: 10.1016/j.neuro.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 24.Tuschl K., Mills P.B., Clayton P.T. Manganese and the brain. Int. Rev. Neurobiol. 2013;110:277–312. doi: 10.1016/B978-0-12-410502-7.00013-2. [DOI] [PubMed] [Google Scholar]
- 25.Dorman D.C., Struve M.F., Wong B.A., Dye J.A., Robertson I.D. Correlation of brain magnetic resonance imaging changes with pallidal manganese concentrations in rhesus monkeys following subchronic manganese inhalation. Toxicol. Sci. 2006;92:219–227. doi: 10.1093/toxsci/kfj209. [DOI] [PubMed] [Google Scholar]
- 26.Yamada M., Ohno S., Okayasu I., Okeda R., Hatakeyama S., Watanabe H., Ushio K., Tsukagoshi H. Chronic manganese poisoning: A neuropathological study with determination of manganese distribution in the brain. Acta Neuropathol. 1986;70:273–278. doi: 10.1007/BF00686083. [DOI] [PubMed] [Google Scholar]
- 27.Gonzalez-Cuyar L.F., Nelson G., Criswell S.R., Ho P., Lonzanida J.A., Checkoway H., Seixas N., Gelman B.B., Evanoff B.A., Murray J., et al. Quantitative neuropathology associated with chronic manganese exposure in South African mine workers. Neurotoxicology. 2014;45:260–266. doi: 10.1016/j.neuro.2013.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cobley J.N., Fiorello M.L., Bailey D.M. 13 reasons why the brain is susceptible to oxidative stress. Redox. Biol. 2018;15:490–503. doi: 10.1016/j.redox.2018.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Benedetto A., Au C., Aschner M. Manganese-induced dopaminergic neurodegeneration: Insights into mechanisms and genetics shared with Parkinson’s disease. Chem. Rev. 2009;109:4862–4884. doi: 10.1021/cr800536y. [DOI] [PubMed] [Google Scholar]
- 30.Martinez-Finley E.J., Gavin C.E., Aschner M., Gunter T.E. Manganese neurotoxicity and the role of reactive oxygen species. Free Radic. Biol. Med. 2013;62:65–75. doi: 10.1016/j.freeradbiomed.2013.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sidoryk-Wegrzynowicz M., Aschner M. Role of astrocytes in manganese mediated neurotoxicity. BMC Pharmacol. Toxicol. 2013;14:23. doi: 10.1186/2050-6511-14-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amos-Kroohs R.M., Davenport L.L., Gutierrez A., Hufgard J.R., Vorhees C.V., Williams M.T. Developmental manganese exposure in combination with developmental stress and iron deficiency: Effects on behavior and monoamines. Neurotoxicol. Teratol. 2016;56:55–67. doi: 10.1016/j.ntt.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Khalid M., Aoun R.A., Mathews T.A. Altered striatal dopamine release following a sub-acute exposure to manganese. J. Neurosci. Methods. 2011;202:182–191. doi: 10.1016/j.jneumeth.2011.06.019. [DOI] [PubMed] [Google Scholar]
- 34.Santos D., Milatovic D., Andrade V., Batoreu M.C., Aschner M., Marreilha dos Santos A.P. The inhibitory effect of manganese on acetylcholinesterase activity enhances oxidative stress and neuroinflammation in the rat brain. Toxicology. 2012;292:90–98. doi: 10.1016/j.tox.2011.11.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Soares A.T.G., Silva A.C., Tinkov A.A., Khan H., Santamaría A., Skalnaya M.G., Skalny A.V., Tsatsakis A., Bowman A.B., Aschner M., et al. The impact of manganese on neurotransmitter systems. J. Trace Elem. Med. Biol. 2020;61:126554. doi: 10.1016/j.jtemb.2020.126554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alsulimani H.H., Ye Q., Kim J. Effect of Hfe deficiency on memory capacity and motor coordination after manganese exposure by drinking water in mice. Toxicol. Res. 2015;31:347–354. doi: 10.5487/TR.2015.31.4.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Song Q., Deng Y., Yang X., Bai Y., Xu B., Liu W., Zheng W., Wang C., Zhang M., Xu Z. Manganese-disrupted interaction of dopamine D1 and NMDAR in the striatum to injury learning and memory ability of mice. Mol. Neurobiol. 2016;53:6745–6758. doi: 10.1007/s12035-015-9602-7. [DOI] [PubMed] [Google Scholar]
- 38.Langley M.R., Ghaisas S., Ay M., Luo J., Palanisamy B.N., Jin H., Anantharam V., Kanthasamy A., Kanthasamy A.G. Manganese exposure exacerbates progressive motor deficits and neurodegeneration in the MitoPark mouse model of Parkinson’s disease: Relevance to gene and environment interactions in metal neurotoxicity. Neurotoxicology. 2018;64:240–255. doi: 10.1016/j.neuro.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Guilarte T.R. Manganese neurotoxicity: New perspectives from behavioral, neuroimaging, and neuropathological studies in humans and non-human primates. Front. Aging Neurosci. 2013;5:23. doi: 10.3389/fnagi.2013.00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim C.Y., Sung J.H., Chung Y.H., Park J.D., Han J.H., Lee J.S., Heo J.D., Yu I.J. Home cage locomotor changes in non-human primates after prolonged welding-fume exposure. Inhal. Toxicol. 2013;25:794–801. doi: 10.3109/08958378.2013.849316. [DOI] [PubMed] [Google Scholar]
- 41.Olanow C.W., Good P.F., Shinotoh H., Hewitt K.A., Vingerhoets F., Snow B.J., Beal M.F., Calne D.B., Perl D.P. Manganese intoxication in the rhesus monkey: A clinical, imaging, pathologic, and biochemical study. Neurology. 1996;46:492–498. doi: 10.1212/WNL.46.2.492. [DOI] [PubMed] [Google Scholar]
- 42.Schneider J.S., Decamp E., Clark K., Bouquio C., Syversen T., Guilarte T.R. Effects of chronic manganese exposure on working memory in non-human primates. Brain Res. 2009;1258:86–95. doi: 10.1016/j.brainres.2008.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schneider J.S., Decamp E., Koser A.J., Fritz S., Gonczi H., Syversen T., Guilarte T.R. Effects of chronic manganese exposure on cognitive and motor functioning in non-human primates. Brain Res. 2006;1118:222–231. doi: 10.1016/j.brainres.2006.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schneider J.S., Williams C., Ault M., Guilarte T.R. Chronic manganese exposure impairs visuospatial associative learning in non-human primates. Toxicol. Lett. 2013;221:146–151. doi: 10.1016/j.toxlet.2013.06.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Verina T., Schneider J.S., Guilarte T.R. Manganese exposure induces α-synuclein aggregation in the frontal cortex of non-human primates. Toxicol. Lett. 2013;217:177–183. doi: 10.1016/j.toxlet.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pajarillo E., Nyarko-Danquah I., Adinew G., Rizor A., Aschner M., Lee E. Neurotoxicity mechanisms of manganese in the central nervous system. Adv. Neurotoxicol. 2021;5:215–238. doi: 10.1016/bs.ant.2020.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tinkov A.A., Paoliello M.M.B., Mazilina A.N., Salny A.V., Martins A.C., Voskresenskaya O.N., Aaseth J., Santamaria A., Notova S.V., Tsatsakis A., et al. Molecular targets of manganese-induced neurotoxicity: A five-year update. Int. J. Mol. Sci. 2021;22:4646. doi: 10.3390/ijms22094646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Martínez-Hernández M.I., Acosta-Saavedra L.C., Hernández-Kelly L.C., Loaeza-Loaeza J., Ortega A. Microglial activation in metal neurotoxicity: Impact in neurodegenerative diseases. Biomed. Res. Int. 2023;2023:7389508. doi: 10.1155/2023/7389508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Searles Nielsen S., Checkoway H., Criswell S.R., Farin F.M., Stapleton P.L., Sheppard L., Racette B.A. Inducible nitric oxide synthase gene methylation and parkinsonism in manganese-exposed welders. Park. Relat. Disord. 2015;21:355–360. doi: 10.1016/j.parkreldis.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu M., Sun X., Chen B., Dai R., Xi Z., Xu H. Insights into manganese superoxide dismutase and human diseases. Int. J. Mol. Sci. 2022;23:15893. doi: 10.3390/ijms232415893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Murphy M.P. How mitochondria produce reactive oxygen species. Biochem. J. 2009;417:1–13. doi: 10.1042/BJ20081386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nickel A., Kohlhaas M., Maack C. Mitochondrial reactive oxygen species production and elimination. J. Mol. Cell. Cardiol. 2014;73:26–33. doi: 10.1016/j.yjmcc.2014.03.011. [DOI] [PubMed] [Google Scholar]
- 53.Nissanka N., Moraes C.T. Mitochondrial DNA damage and reactive oxygen species in neurodegenerative disease. FEBS Lett. 2018;592:728–742. doi: 10.1002/1873-3468.12956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Islam M.T. Oxidative stress and mitochondrial dysfunction-linked neurodegenerative disorders. Neurol. Res. 2017;39:73–82. doi: 10.1080/01616412.2016.1251711. [DOI] [PubMed] [Google Scholar]
- 55.Kobayashi M., Yamamoto M. Nrf2-Keap1 regulation of cellular defense mechanisms against electrophiles and reactive oxygen species. Adv. Enzyme Regul. 2006;46:113–140. doi: 10.1016/j.advenzreg.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 56.Turpaev K.T. Keap1-Nrf2 signaling pathway: Mechanisms of regulation and role in protection of cells against toxicity caused by xenobiotics and electrophiles. Biochemistry. 2013;78:111–126. doi: 10.1134/S0006297913020016. [DOI] [PubMed] [Google Scholar]
- 57.Zhang J., Wang X., Vikash V., Ye Q., Wu D., Liu Y., Dong W. ROS and ROS-mediated cellular signaling. Oxid. Med. Cell. Longev. 2016;2016:4350965. doi: 10.1155/2016/4350965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Valko M., Leibfritz D., Moncol J., Cronin M.T., Mazur M., Telser J. Free radicals and antioxidants in normal physiological functions and human disease. Int. J. Biochem. Cell Biol. 2007;39:44–84. doi: 10.1016/j.biocel.2006.07.001. [DOI] [PubMed] [Google Scholar]
- 59.Bhat A.H., Dar K.B., Anees S., Zargar M.A., Masood A., Sofi M.A., Ganie S.A. Oxidative stress, mitochondrial dysfunction and neurodegenerative diseases; a mechanistic insight. Biomed. Pharmacother. 2015;74:101–110. doi: 10.1016/j.biopha.2015.07.025. [DOI] [PubMed] [Google Scholar]
- 60.Smith M.R., Fernandes J., Go Y.M., Jones D.P. Redox dynamics of manganese as a mitochondrial life-death switch. Biochem. Biophys. Res. Commun. 2017;482:388–398. doi: 10.1016/j.bbrc.2016.10.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ali S.F., Duhart H.M., Newport G.D., Lipe G.W., Slikker W., Jr. Manganese-induced reactive oxygen species: Comparison between Mn+2 and Mn+3. Neurodegeneration. 1995;4:329–334. doi: 10.1016/1055-8330(95)90023-3. [DOI] [PubMed] [Google Scholar]
- 62.HaMai D., Bondy S.C. Oxidative basis of manganese neurotoxicity. Ann. N. Y. Acad. Sci. 2004;1012:129–141. doi: 10.1196/annals.1306.010. [DOI] [PubMed] [Google Scholar]
- 63.Reaney S.H., Smith D.R. Manganese oxidation state mediates toxicity in PC12 cells. Toxicol. Appl. Pharmacol. 2005;205:271–281. doi: 10.1016/j.taap.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 64.Chen J.Y., Tsao G.C., Zhao Q., Zheng W. Differential cytotoxicity of Mn(II) and Mn(III): Special reference to mitochondrial [Fe-S] containing enzymes. Toxicol. Appl. Pharmacol. 2001;175:160–168. doi: 10.1006/taap.2001.9245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gunter T.E., Gavin C.E., Aschner M., Gunter K.K. Speciation of manganese in cells and mitochondria: A search for the proximal cause of manganese neurotoxicity. Neurotoxicology. 2006;27:765–776. doi: 10.1016/j.neuro.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 66.Chen P., Totten M., Zhang Z., Bucinca H., Erikson K., Santamaría A., Bowman A.B., Aschner M. Iron and manganese-related CNS toxicity: Mechanisms, diagnosis and treatment. Expert Rev. Neurother. 2019;19:243–260. doi: 10.1080/14737175.2019.1581608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fernandes J., Hao L., Bijli K.M., Chandler J.D., Orr M., Hu X., Jones D.P., Go Y.M. Manganese stimulates mitochondrial H2O2 production in SH-SY5Y human neuroblastoma cells over physiologic as well as toxicologic range. Toxicol. Sci. 2017;155:213–223. doi: 10.1093/toxsci/kfw196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Taylor M.D., Erikson K.M., Dobson A.W., Fitsanakis V.A., Dorman D.C., Aschner M. Effects of inhaled manganese on biomarkers of oxidative stress in the rat brain. Neurotoxicology. 2006;27:788–797. doi: 10.1016/j.neuro.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 69.Cheton P.L., Archibald F.S. Manganese complexes and the generation and scavenging of hydroxyl free radicals. Free Radic. Biol. Med. 1988;5:325–333. doi: 10.1016/0891-5849(88)90104-9. [DOI] [PubMed] [Google Scholar]
- 70.Jomova K., Makova M., Alomar S.Y., Alwasel S.H., Nepovimova E., Kuca K., Rhodes C.J., Valko M. Essential metals in health and disease. Chem. Biol. Interact. 2022;367:110173. doi: 10.1016/j.cbi.2022.110173. [DOI] [PubMed] [Google Scholar]
- 71.Aguirre J.D., Culotta V.C. Battles with iron: Manganese in oxidative stress protection. J. Biol. Chem. 2012;287:13541–13548. doi: 10.1074/jbc.R111.312181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aschner M., Skalny A.V., Martins A.C., Sinitskii A.I., Farina M., Lu R., Barbosa F., Jr., Gluhcheva Y.G., Santamaria A., Tinkov A.A. Ferroptosis as a mechanism of non-ferrous metal toxicity. Arch. Toxicol. 2022;96:2391–2417. doi: 10.1007/s00204-022-03317-y. [DOI] [PubMed] [Google Scholar]
- 73.Cao Z., Lindsay J.G. The Peroxiredoxin Family: An Unfolding Story. In: Harris J., Marles-Wright J., editors. Macromolecular Protein Complexes. Volume 83. Springer; Cham, Switzerland: 2017. Subcellular Biochemistry. [DOI] [PubMed] [Google Scholar]
- 74.Liu J., Su G., Gao J., Tian Y., Liu X., Zhang Z. Effects of peroxiredoxin 2 in neurological disorders: A review of its molecular mechanisms. Neurochem. Res. 2020;45:720–730. doi: 10.1007/s11064-020-02971-x. [DOI] [PubMed] [Google Scholar]
- 75.Sharma S., Ebadi M. Significance of metallothioneins in aging brain. Neurochem. Int. 2014;65:40–48. doi: 10.1016/j.neuint.2013.12.009. [DOI] [PubMed] [Google Scholar]
- 76.Santos C.R., Martinho A., Quintela T., Gonçalves I. Neuroprotective and neuroregenerative properties of metallothioneins. IUBMB Life. 2012;64:126–135. doi: 10.1002/iub.585. [DOI] [PubMed] [Google Scholar]
- 77.Wang Y., Branicky R., Noë A., Hekimi S. Superoxide dismutases: Dual roles in controlling ROS damage and regulating ROS signaling. J. Cell Biol. 2018;217:1915–1928. doi: 10.1083/jcb.201708007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Bhaskaran S., Kumar G., Thadathil N., Piekarz K.M., Mohammed S., Lopez S.D., Qaisar R., Walton D., Brown J.L., Murphy A., et al. Neuronal deletion of MnSOD in mice leads to demyelination, inflammation and progressive paralysis that mimics phenotypes associated with progressive multiple sclerosis. Redox Biol. 2023;59:102550. doi: 10.1016/j.redox.2022.102550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gunter T.E., Gavin C.E., Gunter K.K. The case for manganese interaction with mitochondria. Neurotoxicology. 2009;30:727–729. doi: 10.1016/j.neuro.2009.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Gunter T.E., Rosier R.N., Tucker D.A., Gunter K.K. Uptake of calcium and manganese by rat liver submitochondrial particles. Ann. N. Y. Acad. Sci. 1978;307:246–247. doi: 10.1111/j.1749-6632.1978.tb41954.x. [DOI] [PubMed] [Google Scholar]
- 81.Gavin C.E., Gunter K.K., Gunter T.E. Manganese and calcium efflux kinetics in brain mitochondria. Relevance to manganese toxicity. Biochem. J. 1990;266:329–334. doi: 10.1042/bj2660329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Galvani P., Fumagalli P., Santagostino A. Vulnerability of mitochondrial complex I in PC12 cells exposed to manganese. Eur. J. Pharmacol. 1995;293:377–383. doi: 10.1016/0926-6917(95)90058-6. [DOI] [PubMed] [Google Scholar]
- 83.Gunter T.E., Gerstner B., Lester T., Wojtovich A.P., Malecki J., Swarts S.G., Brookes P.S., Gavin C.E., Gunter K.K. An analysis of the effects of Mn2+ on oxidative phosphorylation in liver, brain, and heart mitochondria using state 3 oxidation rate assays. Toxicol. Appl. Pharmacol. 2010;249:65–75. doi: 10.1016/j.taap.2010.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhang S., Zhou Z., Fu J. Effect of manganese chloride exposure on liver and brain mitochondria function in rats. Environ. Res. 2003;93:149–157. doi: 10.1016/S0013-9351(03)00109-9. [DOI] [PubMed] [Google Scholar]
- 85.Seth K., Agrawal A.K., Date I., Seth P.K. The role of dopamine in manganese-induced oxidative injury in rat pheochromocytoma cells. Hum. Exp. Toxicol. 2002;21:165–170. doi: 10.1191/0960327102ht228oa. [DOI] [PubMed] [Google Scholar]
- 86.Maddirala Y., Tobwala S., Ercal N. N-acetylcysteineamide protects against manganese-induced toxicity in SHSY5Y cell line. Brain Res. 2015;1608:157–166. doi: 10.1016/j.brainres.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 87.Marreilha dos Santos A.P., Santos D., Au C., Milatovic D., Aschner M., Batoréu M.C. Antioxidants prevent the cytotoxicity of manganese in RBE4 cells. Brain Res. 2008;1236:200–205. doi: 10.1016/j.brainres.2008.07.125. [DOI] [PubMed] [Google Scholar]
- 88.Stredrick D.L., Stokes A.H., Worst T.J., Freeman W.M., Johnson E.A., Lash L.H., Aschner M., Vrana K.E. Manganese-induced cytotoxicity in dopamine-producing cells. Neurotoxicology. 2004;25:543–553. doi: 10.1016/j.neuro.2003.08.006. [DOI] [PubMed] [Google Scholar]
- 89.Wan C., Ma X., Shi S., Zhao J., Nie X., Han J., Xiao J., Wang X., Jiang S., Jiang J. Pivotal roles of p53 transcription-dependent and -independent pathways in manganese-induced mitochondrial dysfunction and neuronal apoptosis. Toxicol. Appl. Pharmacol. 2014;281:294–302. doi: 10.1016/j.taap.2014.10.013. [DOI] [PubMed] [Google Scholar]
- 90.Malecki E.A. Manganese toxicity is associated with mitochondrial dysfunction and DNA fragmentation in rat primary striatal neurons. Brain Res. Bull. 2001;55:225–228. doi: 10.1016/S0361-9230(01)00456-7. [DOI] [PubMed] [Google Scholar]
- 91.Warren E.B., Bryan M.R., Morcillo P., Hardeman K.N., Aschner M., Bowman A.B. Manganese-induced mitochondrial dysfunction Is not detectable at exposures below the acute cytotoxic threshold in neuronal cell types. Toxicol. Sci. 2020;176:446–459. doi: 10.1093/toxsci/kfaa079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Sarkar S., Rokad D., Malovic E., Luo J., Harischandra D.S., Jin H., Anantharam V., Huang X., Lewis M., Kanthasamy A., et al. Manganese activates NLRP3 inflammasome signaling and propagates exosomal release of ASC in microglial cells. Sci. Signal. 2019;12:eaat9900. doi: 10.1126/scisignal.aat9900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.National Academies of Sciences, Engineering, and Medicine . Building Confidence in New Evidence Streams for Human Health Risk Assessment: Lessons Learned from Laboratory Mammalian Toxicity Tests. The National Academies Press; Washington, DC, USA: 2023. [DOI] [PubMed] [Google Scholar]
- 94.Martins A.C., Gubert P., Li J., Ke T., Nicolai M.M., Moura A.V., Bornhorst J., Bowman A.B., Aschner M. Caenorhabditis elegans as a model to study manganese-induced neurotoxicity. Biomolecules. 2022;12:1396. doi: 10.3390/biom12101396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ruszkiewicz J.A., Pinkas A., Miah M.R., Weitz R.L., Lawes M.J.A., Akinyemi A.J., Ijomone O.M., Aschner M. C. elegans as a model in developmental neurotoxicology. Toxicol. Appl. Pharmacol. 2018;354:126–135. doi: 10.1016/j.taap.2018.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.C. elegans Sequencing Consortium Genome sequence of the nematode C. elegans: A platform for investigating biology. Science. 1998;282:2012–2018. doi: 10.1126/science.282.5396.2012. [DOI] [PubMed] [Google Scholar]
- 97.Melnikov K., Kucharíková S., Bárdyová Z., Botek N., Kaiglová A. Applications of a powerful model organism Caenorhabditis elegans to study the neurotoxicity induced by heavy metals and pesticides. Physiol. Res. 2023;72:149–166. doi: 10.33549/physiolres.934977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.White J.G., Southgate E., Thomson J.N., Brenner S. The structure of the nervous system of the nematode Caenorhabditis elegans. Philos. Trans. R. Soc. Lond. B Biol. Sci. 1986;314:1–340. doi: 10.1098/rstb.1986.0056. [DOI] [PubMed] [Google Scholar]
- 99.Nass R., Hall D.H., Miller D.M., 3rd, Blakely R.D. Neurotoxin-induced degeneration of dopamine neurons in Caenorhabditis elegans. Proc. Natl. Acad. Sci. USA. 2002;99:3264–3269. doi: 10.1073/pnas.042497999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sulston J., Dew M., Brenner S. Dopaminergic neurons in the nematode Caenorhabditis elegans. J. Comp. Neurol. 1975;163:215–226. doi: 10.1002/cne.901630207. [DOI] [PubMed] [Google Scholar]
- 101.Benedetto A., Au C., Avila D.S., Milatovic D., Aschner M. Extracellular dopamine potentiates Mn-induced oxidative stress, lifespan reduction, and dopaminergic neurodegeneration in a BLI-3-dependent manner in Caenorhabditis elegans. PLoS Genet. 2010;6:e1001084. doi: 10.1371/journal.pgen.1001084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Avila D.S., Benedetto A., Au C., Bornhorst J., Aschner M. Involvement of heat shock proteins on Mn-induced toxicity in Caenorhabditis elegans. BMC Pharmacol. Toxicol. 2016;17:1–9. doi: 10.1186/s40360-016-0097-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ijomone O.M., Miah M.R., Peres T.V., Nwoha P.U., Aschner M. Null allele mutants of trt-1, the catalytic subunit of telomerase in Caenorhabditis elegans, are less sensitive to Mn-induced toxicity and DAergic degeneration. Neurotoxicology. 2016;57:54–60. doi: 10.1016/j.neuro.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 104.Lawes M., Pinkas A., Frohlich B.A., Iroegbu J.D., Ijomone O.M., Aschner M. Metal-induced neurotoxicity in a RAGE-expressing C. elegans model. Neurotoxicology. 2020;80:71–75. doi: 10.1016/j.neuro.2020.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Settivari R., VanDuyn N., LeVora J., Nass R. The Nrf2/SKN-1-dependent glutathione S-transferase π homologue GST-1 inhibits dopamine neuron degeneration in a Caenorhabditis elegans model of manganism. Neurotoxicology. 2013;38:51–60. doi: 10.1016/j.neuro.2013.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Raj V., Nair A., Thekkuveettil A. Manganese exposure during early larval stages of C. elegans causes learning disability in the adult stage. Biochem. Biophys. Res. Commun. 2021;568:89–94. doi: 10.1016/j.bbrc.2021.06.073. [DOI] [PubMed] [Google Scholar]
- 107.Bornhorst J., Chakraborty S., Meyer S., Lohren H., Brinkhaus S.G., Knight A.L., Caldwell K.A., Caldwell G.A., Karst U., Schwerdtle T., et al. The effects of pdr1, djr1.1 and pink1 loss in manganese-induced toxicity and the role of α-synuclein in C. elegans. Metallomics. 2014;6:476–490. doi: 10.1039/C3MT00325F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Neumann C., Baesler J., Steffen G., Nicolai M.M., Zubel T., Aschner M., Bürkle A., Mangerich A., Schwerdtle T., Bornhorst J. The role of poly(ADP-ribose) polymerases in manganese exposed Caenorhabditis elegans. J. Trace Elem. Med. Biol. 2020;57:21–27. doi: 10.1016/j.jtemb.2019.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Lyu S., Doroodchi A., Xing H., Sheng Y., DeAndrade M.P., Yang Y., Johnson T.L., Clemens S., Yokoi F., Miller M.A., et al. BTBD9 and dopaminergic dysfunction in the pathogenesis of restless legs syndrome. Brain Struct. Funct. 2020;225:743–1760. doi: 10.1007/s00429-020-02090-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Chen P., Cheng H., Zheng F., Li S., Bornhorst J., Yang B., Lee K.H., Ke T., Li Y., Schwerdtle T., et al. BTBD9 attenuates manganese-induced oxidative stress and neurotoxicity by regulating insulin growth factor signaling pathway. Hum. Mol. Genet. 2022;31:2207–2222. doi: 10.1093/hmg/ddac025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Ke T., Sidoryk-Wegrzynowicz M., Pajarillo E., Rizor A., Soares F.A.A., Lee E., Aschner M. Role of astrocytes in manganese neurotoxicity revisited. Neurochem. Res. 2019;44:2449–2459. doi: 10.1007/s11064-019-02881-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Soto-Verdugo J., Ortega A. Critical involvement of glial cells in manganese neurotoxicity. Biomed. Res. Int. 2021;2021:1596185. doi: 10.1155/2021/1596185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Liao S.L., Chen C.J. Manganese stimulates stellation of cultured rat cortical astrocytes. Neuroreport. 2001;12:3877–3881. doi: 10.1097/00001756-200112210-00004. [DOI] [PubMed] [Google Scholar]
- 114.Rama Rao K.V., Reddy P.V., Hazell A.S., Norenberg M.D. Manganese induces cell swelling in cultured astrocytes. Neurotoxicology. 2007;28:807–812. doi: 10.1016/j.neuro.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 115.Erikson K.M., Aschner M. Increased manganese uptake by primary astrocyte cultures with altered iron status is mediated primarily by divalent metal transporter. Neurotoxicology. 2006;27:125–130. doi: 10.1016/j.neuro.2005.07.003. [DOI] [PubMed] [Google Scholar]
- 116.Deng Y., Xu Z., Xu B., Xu D., Tian Y., Feng W. The protective effects of riluzole on manganese-induced disruption of glutamate transporters and glutamine synthetase in the cultured astrocytes. Biol. Trace Elem. Res. 2012;148:242–249. doi: 10.1007/s12011-012-9365-1. [DOI] [PubMed] [Google Scholar]
- 117.Mutkus L., Aschner J.L., Fitsanakis V., Aschner M. The in vitro uptake of glutamate in GLAST and GLT-1 transfected mutant CHO-K1 cells is inhibited by manganese. Biol. Trace Elem. Res. 2005;107:221–230. doi: 10.1385/BTER:107:3:221. [DOI] [PubMed] [Google Scholar]
- 118.Sidoryk-Wegrzynowicz M., Lee E., Albrecht J., Aschner M. Manganese disrupts astrocyte glutamine transporter expression and function. J. Neurochem. 2009;110:822–830. doi: 10.1111/j.1471-4159.2009.06172.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Sidoryk-Wegrzynowicz M., Lee E., Mingwei N., Aschner M. Disruption of astrocytic glutamine turnover by manganese is mediated by the protein kinase C pathway. Glia. 2011;59:1732–1743. doi: 10.1002/glia.21219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Erikson K.M., Dorman D.C., Lash L.H., Aschner M. Duration of airborne-manganese exposure in rhesus monkeys is associated with brain regional changes in biomarkers of neurotoxicity. Neurotoxicology. 2008;29:377–385. doi: 10.1016/j.neuro.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 121.Lee E.S., Sidoryk M., Jiang H., Yin Z., Aschner M. Estrogen and tamoxifen reverse manganese-induced glutamate transporter impairment in astrocytes. J. Neurochem. 2009;110:530–544. doi: 10.1111/j.1471-4159.2009.06105.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Chen C.J., Liao S.L. Oxidative stress involves in astrocytic alterations induced by manganese. Exp. Neurol. 2002;175:216–225. doi: 10.1006/exnr.2002.7894. [DOI] [PubMed] [Google Scholar]
- 123.Milatovic D., Yin Z., Gupta R.C., Sidoryk M., Albrecht J., Aschner J.L., Aschner M. Manganese induces oxidative impairment in cultured rat astrocytes. Toxicol. Sci. 2007;98:198–205. doi: 10.1093/toxsci/kfm095. [DOI] [PubMed] [Google Scholar]
- 124.Spranger M., Schwab S., Desiderato S., Bonmann E., Krieger D., Fandrey J. Manganese augments nitric oxide synthesis in murine astrocytes: A new pathogenetic mechanism in manganism? Exp. Neurol. 1998;149:277–283. doi: 10.1006/exnr.1997.6666. [DOI] [PubMed] [Google Scholar]
- 125.Popichak K.A., Afzali M.F., Kirkley K.S., Tjalkens R.B. Glial-neuronal signaling mechanisms underlying the neuroinflammatory effects of manganese. J. Neuroinflamm. 2018;15:324. doi: 10.1186/s12974-018-1349-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Tjalkens R.B., Popichak K.A., Kirkley K.A. Inflammatory activation of microglia and astrocytes in manganese neurotoxicity. Adv. Neurobiol. 2017;18:159–181. doi: 10.1007/978-3-319-60189-2_8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yin Z., Aschner J.L., dos Santos A.P., Aschner M. Mitochondrial-dependent manganese neurotoxicity in rat primary astrocyte cultures. Brain Res. 2008;1203:1–11. doi: 10.1016/j.brainres.2008.01.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Lee E., Yin Z., Sidoryk-Węgrzynowicz M., Jiang H., Aschner M. 15-Deoxy-Δ12,14-prostaglandin J2 modulates manganese-induced activation of the NF-κB, Nrf2, and PI3K pathways in astrocytes. Free Radic. Biol. Med. 2012;52:1067–1074. doi: 10.1016/j.freeradbiomed.2011.12.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Kirkley K.S., Popichak K.A., Afzali M.F., Legare M.E., Tjalkens R.B. Microglia amplify inflammatory activation of astrocytes in manganese neurotoxicity. J. Neuroinflamm. 2017;14:99. doi: 10.1186/s12974-017-0871-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhang P., Hatter A., Liu B. Manganese chloride stimulates rat microglia to release hydrogen peroxide. Toxicol. Lett. 2007;173:88–100. doi: 10.1016/j.toxlet.2007.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Zhang P., Wong T.A., Lokuta K.M., Turner D.E., Vujisic K., Liu B. Microglia enhance manganese chloride-induced dopaminergic neurodegeneration: Role of free radical generation. Exp. Neurol. 2009;217:219–230. doi: 10.1016/j.expneurol.2009.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dorman D.C., Andersen M.E., Roper J.M., Taylor M.D. Update on a pharmacokinetic-centric alternative tier II program for MMT. Part I: Program implementation and lessons learned. J. Toxicol. 2012;2012:946742. doi: 10.1155/2012/946742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Dorman D.C., McElveen A.M., Marshall M.W., Parkinson C.U., James R.A., Struve M.F., Wong B.A. Tissue manganese concentrations in lactating rats and their offspring following combined in utero and lactation exposure to inhaled manganese sulfate. Toxicol. Sci. 2005;84:12–21. doi: 10.1093/toxsci/kfi060. [DOI] [PubMed] [Google Scholar]
- 134.Dorman D.C., McElveen A.M., Marshall M.W., Parkinson C.U., James R.A., Struve M.F., Wong B.A. Maternal-fetal distribution of manganese in the rat following inhalation exposure to manganese sulfate. Neurotoxicology. 2005;26:625–632. doi: 10.1016/j.neuro.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 135.Dorman D.C., McManus B.E., Marshall M.W., James R.A., Struve M.F. Old age and gender influence the pharmacokinetics of inhaled manganese sulfate and manganese phosphate in rats. Toxicol. Appl. Pharmacol. 2004;197:113–124. doi: 10.1016/j.taap.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 136.Dorman D.C., Struve M.F., James R.A., Marshall M.W., Parkinson C.U., Wong B.A. Influence of particle solubility on the delivery of inhaled manganese to the rat brain: Manganese sulfate and manganese tetroxide pharmacokinetics following repeated (14-day) exposure. Toxicol. Appl. Pharmacol. 2001;170:79–87. doi: 10.1006/taap.2000.9088. [DOI] [PubMed] [Google Scholar]
- 137.Dobson A.W., Weber S., Dorman D.C., Lash L.K., Erikson K.M., Aschner M. Oxidative stress is induced in the rat brain following repeated inhalation exposure to manganese sulfate. Biol. Trace Elem. Res. 2003;93:113–126. doi: 10.1385/BTER:93:1-3:113. [DOI] [PubMed] [Google Scholar]
- 138.Erikson K.M., Dorman D.C., Fitsanakis V., Lash L.H., Aschner M. Alterations of oxidative stress biomarkers due to in utero and neonatal exposures of airborne manganese. Biol. Trace Elem. Res. 2006;111:199–215. doi: 10.1385/BTER:111:1:199. [DOI] [PubMed] [Google Scholar]
- 139.Erikson K.M., Dorman D.C., Lash L.H., Aschner M. Persistent alterations in biomarkers of oxidative stress resulting from combined in utero and neonatal manganese inhalation. Biol. Trace Elem. Res. 2005;104:151–263. doi: 10.1385/BTER:104:2:151. [DOI] [PubMed] [Google Scholar]
- 140.Erikson K.M., Dorman D.C., Lash L.H., Dobson A.W., Aschner M. Airborne manganese exposure differentially affects end points of oxidative stress in an age- and sex-dependent manner. Biol. Trace Elem. Res. 2004;100:49–62. doi: 10.1385/BTER:100:1:049. [DOI] [PubMed] [Google Scholar]
- 141.Bahar E., Kim J.Y., Yoon H. Quercetin attenuates manganese-induced neuroinflammation by alleviating oxidative stress through regulation of apoptosis, iNOS/NF-κB and HO-1/Nrf2 pathways. Int. J. Mol. Sci. 2017;18:1989. doi: 10.3390/ijms18091989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Desole M.S., Esposito G., Migheli R., Fresu L., Sircana S., Miele M., De Natale G., Miele E. Allopurinol protects against manganese-induced oxidative stress in the striatum and in the brainstem of the rat. Neurosci. Lett. 1995;192:73–76. doi: 10.1016/0304-3940(95)11613-2. [DOI] [PubMed] [Google Scholar]
- 143.Szpetnar M., Luchowska-Kocot D., Boguszewska-Czubara A., Kurzepa J. The influence of manganese and glutamine intake on antioxidants and neurotransmitter amino acids levels in rats’ brain. Neurochem. Res. 2016;41:2129–2139. doi: 10.1007/s11064-016-1928-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Yang X., Yang H., Wu F., Qi Z., Li J., Xu B., Liu W., Xu Z., Deng Y. Mn Inhibits GSH synthesis via downregulation of neuronal EAAC1 and astrocytic xCT to cause oxidative damage in the striatum of mice. Oxid. Med. Cell Longev. 2018;2018:4235695. doi: 10.1155/2018/4235695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Brenneman K.A., Cattley R.C., Ali S.F., Dorman D.C. Manganese-induced developmental neurotoxicity in the CD rat: Is oxidative damage a mechanism of action? Neurotoxicology. 1999;20:477–487. [PubMed] [Google Scholar]
- 146.Guilarte T.R., Chen M.K., McGlothan J.L., Verina T., Wong D.F., Zhou Y., Alexander M., Rohde C.A., Syversen T., Decamp E., et al. Nigrostriatal dopamine system dysfunction and subtle motor deficits in manganese-exposed non-human primates. Exp. Neurol. 2006;202:381–390. doi: 10.1016/j.expneurol.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 147.Guilarte T.R., Burton N.C., McGlothan J.L., Verina T., Zhou Y., Alexander M., Pham L., Griswold M., Wong D.F., Syversen T., et al. Impairment of nigrostriatal dopamine neurotransmission by manganese is mediated by pre-synaptic mechanism(s): Implications to manganese-induced parkinsonism. J. Neurochem. 2008;107:1236–1247. doi: 10.1111/j.1471-4159.2008.05695.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Dorman D.C., Struve M.F., Marshall M.W., Parkinson C.U., James R.A., Wong B.A. Tissue manganese concentrations in young male rhesus monkeys following subchronic manganese sulfate inhalation. Toxicol. Sci. 2006;92:201–210. doi: 10.1093/toxsci/kfj206. [DOI] [PubMed] [Google Scholar]
- 149.Erikson K.M., Dorman D.C., Lash L.H., Aschner M. Manganese inhalation by rhesus monkeys is associated with brain regional changes in biomarkers of neurotoxicity. Toxicol. Sci. 2007;97:459–466. doi: 10.1093/toxsci/kfm044. [DOI] [PubMed] [Google Scholar]
- 150.Ramoju S.P., Mattison D.R., Milton B., McGough D., Shilnikova N., Clewell H.J., Yoon M., Taylor M.D., Krewski D., Andersen M.E. The application of PBPK models in estimating human brain tissue manganese concentrations. Neurotoxicology. 2017;58:226–237. doi: 10.1016/j.neuro.2016.12.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data is contained herein.