Abstract
Objective
To estimate the prevalence of individual chronic conditions and multimorbidity among adults admitted to hospital in countries in sub–Saharan Africa.
Methods
We systematically searched MEDLINE®, Embase®, Global Index Medicus, Global Health and SciELO for publications reporting on patient cohorts recruited between 1 January 2010 and 12 May 2023. We included articles reporting prevalence of pre-specified chronic diseases within unselected acute care services (emergency departments or medical inpatient settings). No language restrictions were applied. We generated prevalence estimates using random-effects meta-analysis alongside 95% confidence intervals, 95% prediction intervals and I2 statistics for heterogeneity. To explore associations with age, sex, country-level income status, geographical region and risk of bias, we conducted pre-specified meta-regression, sub-group and sensitivity analyses.
Findings
Of 6976 identified studies, 61 met the inclusion criteria, comprising data from 20 countries and 376 676 people. None directly reported multimorbidity, but instead reported prevalence for individual conditions. Among medical admissions, the highest prevalence was human immunodeficiency virus infection (36.4%; 95% CI: 31.3–41.8); hypertension (24.4%; 95% CI: 16.7–34.2); diabetes (11.9%; 95% CI: 9.9–14.3); heart failure (8.2%; 95% CI: 5.6–11.9); chronic kidney disease (7.7%; 95% CI: 3.9–14.7); and stroke (6.8%; 95% CI: 4.7–9.6).
Conclusion
Among patients seeking hospital care in sub-Saharan Africa, multimorbidity remains poorly described despite high burdens of individual chronic diseases. Prospective public health studies of multimorbidity burden are needed to generate integrated and context-specific health system interventions that act to maximize patient survival and well-being.
Résumé
Objectif
Mesurer le taux de prévalence des maladies chroniques individuelles et de la multimorbidité chez les adultes hospitalisés en Afrique subsaharienne.
Méthodes
Nous avons analysé systématiquement MEDLINE®, Embase®, l'Index Medicus mondial, Global Health et SciELO à la recherche de publications mentionnant des cohortes de patients recrutés entre le 1er janvier 2010 et le 12 mai 2023. Nous avons retenu les articles traitant de la prévalence de certaines maladies chroniques prédéfinies au sein des services de soins intensifs, sans sélection préalable (aux urgences ou en milieu hospitalier). Aucune restriction de langue n'a été appliquée. Nous avons ensuite estimé le taux de prévalence au moyen d'une méta-analyse à effets aléatoires, tout en appliquant des intervalles de confiance de 95%, des intervalles de prévision de 95% et une statistique I2 pour l'hétérogénéité. Enfin, en vue d'examiner les liens avec l'âge, le sexe, le statut de revenu du pays, la situation géographique et le risque de biais, nous avons mené des analyses prédéfinies de méta-régression, de sous-groupe et de sensibilité.
Résultats
Sur les 6976 études identifiées, 61 correspondaient aux critères d'inclusion et contenaient des informations relatives à 20 pays et 376 676 personnes. Bien qu'aucune n'évoquait directement une multimorbidité, la prévalence des cas individuels était indiquée. Parmi les admissions à l'hôpital, le plus haut taux de prévalence concernait: les infections au virus de l'immunodéficience humaine (36,4%; IC de 95%: 31,3–41,8), l'hypertension (24,4%; IC de 95%: 16,7–34.2), le diabète (11,9%; IC de 95%: 9,9–14,3), l'insuffisance cardiaque (8,2%; IC de 95%: 5,6–11,9), les maladies rénales chroniques (7,7%; IC de 95%: 3,9–14,7) et les accidents vasculaires cérébraux (6,8%; IC de 95%: 4,7–9,6).
Conclusion
La multimorbidité des patients se rendant à l'hôpital en Afrique subsaharienne demeure peu documentée, en dépit de la lourde charge que font peser les maladies chroniques individuelles. Des études prospectives de santé publique sont nécessaires à ce sujet pour déclencher des interventions du système de santé adaptées au contexte et améliorer ainsi les chances de survie et le bien-être des patients.
Resumen
Objetivo
Estimar la prevalencia de enfermedades crónicas individuales y la multimorbilidad en adultos ingresados en hospitales en países del África Subsahariana.
Métodos
Buscamos publicaciones de manera sistemática en MEDLINE®, Embase®, Global Index Medicus, Global Health y SciELO que registraran grupos de pacientes reclutados entre el 1 de enero de 2010 y el 12 de mayo de 2023. Incluimos artículos que informaban sobre la prevalencia de enfermedades crónicas predefinidas en el marco de los servicios de cuidados intensivos no seleccionados (salas de urgencias o centros médicos hospitalarios). No se aplicaron restricciones lingüísticas. Generamos estimaciones sobre la prevalencia utilizando un metaanálisis de efectos aleatorios, junto con intervalos de confianza del 95%, intervalos de predicción del 95% y estadística I2 de heterogeneidad. Para analizar la relación con la edad, el sexo, el nivel de ingresos del país, la zona geográfica y el riesgo de sesgo, llevamos a cabo una metarregresión predefinida y un análisis de subgrupos y sensibilidad.
Resultados
De los 6976 estudios seleccionados, 61 cumplían los criterios de inclusión, y englobaban datos de 20 países y 376 676 personas. Ninguno registraba multimorbilidad de manera directa, sino prevalencia de enfermedades individuales. Entre los ingresos médicos, la prevalencia más alta correspondió a: la infección del virus de la inmunodeficiencia humana (36,4%; IC del 95%: 31,3–41,8), hipertensión (24,4%; IC del 95%: 16,7–34,2), diabetes (11,9%; IC del 95%: 9,9–14,3), insuficiencia cardíaca (8,2%; IC del 95%: 5,6–11,9), enfermedad crónica renal (7,7%; IC del 95%: 3,9–14,7) e ictus (6,8%; IC del 95%: 4,7–9,6).
Conclusión
Entre los pacientes que buscan atención hospitalaria en el África Subsahariana, la multimorbilidad sigue estando escasamente descrita, a pesar de las elevadas tasas de enfermedades crónicas individuales. Los estudios prospectivos de salud pública que versan sobre tasas de multimorbilidad son necesarios para generar intervenciones integradas y adaptadas a las circunstancias por parte del sistema sanitario, para poder aumentar así la supervivencia y el bienestar de los pacientes.
ملخص
الغرض
تقدير انتشار الحالات الفردية المزمنة وتعدد الأمراض بين البالغين الذين يدخلون المستشفيات في جنوب الصحراء الكبرى بأفريقيا.
الطريقة
قمنا بالبحث المنهجي في MEDLINE®، وEmbase®، وGlobal Index Medicus، وGlobal Health، وSciELO عن المنشورات التي تقدم تقارير عن مجموعات المرضى المعينين بين 1 يناير/كانون ثاني 2010، و12 مايو/أيار 2023. لقد قمنا بتضمين المقالات التي تشير إلى انتشار الأمراض المزمنة المحددة مسبقًا ضمن خدمات الرعاية الدقيقة غير المختارة (أقسام الطوارئ أو الأوضاع الطبية لمرضى العيادات الداخلية). لم يتم تطبيق أية قيود لغوية. لقد أنشأنا تقديرات الانتشار باستخدام التحليل التلوي للتأثيرات العشوائية جنبًا إلى جنب مع فواصل ثقة مقدارها %95، وفواصل للتنبؤ مقدارها %95، وإحصاءات I 2 عدم التجانس. لاستكشاف الارتباطات بالعمر، والجنس، وحالة الدخل على مستوى الدولة، والمنطقة الجغرافية، وخطر التحيز، قمنا بإجراء تحليلات التحوف التلوي، والمجموعة الفرعية، والحساسية، المحددة مسبقًا.
النتائج
من بين 6976 دراسة تم تحديدها، استوفت 61 دراسة منها معايير الاشتمال، وتضمنت بيانات من 20 دولة، و376676 شخصًا. لم يُبلغ أي منها بشكل مباشر عن تعدد الأمراض، ولكنها أبلغت بدلاً من ذلك عن انتشار الحالات الفردية. من بين الحالات الطبية للالتحاق بالمستشفى، كان أعلى معدل انتشار هو: الإصابة بفيروس اضطراب نقص المناعة البشرية (%36.4؛ بفاصل ثقة مقداره %95: 31.3 إلى 41.8)، وارتفاع ضغط الدم (%24.4؛ بفاصل ثقة مقداره %95: 16.7 إلى34.2)، ومرض السكري (%11.9؛ بفاصل ثقة مقداره %95: 9.9 إلى 14.3)، وقصور القلب (%8.2؛ بفاصل ثقة مقداره %95: 5.6 إلى 11.9)، ومرض الكلى المزمن (%7.7؛ بفاصل ثقة مقداره %95: 3.9 إلى 14.7)، والسكتة الدماغية (%6.8؛ بفاصل ثقة مقداره %95: 4.7 إلى 9.6).
الاستنتاج
يظل تعدد الأمراض فقير الوصف على الرغم من الأعباء الكبيرة للأمراض المزمنة الفردية، بين المرضى الذين يسعون للحصول على الرعاية في المستشفيات في جنوب الصحراء الكبرى بأفريقيا. هناك حاجة لدراسات الصحة العامة المستقبلية لعبء تعدد الأمراض، وذلك لتجهيز تدخلات نظام صحي متكامل ومحددة السياق، تعمل على زيادة فرص حياة المريض وعافيته.
摘要
目的
旨在评估撒哈拉以南非洲地区住院的成年患者中个体慢性病和共病的患病率。
方法
我们系统地检索了 MEDLINE®、Embase®、全球医学索引、全球健康 和 SciELO 中的数据,以获取关于在 2010 年 1 月 1 日至 2023 年 5 月 12 日期间报告招募患者群的论文。我们纳入了在未经选择的急症护理服务(急诊科或医疗住院场所)中报告预先指定的慢性疾病患病率的文章。没有语言限制。我们使用随机效应 meta 分析以及 95% 置信区间、95% 预测区间和 I2异质性统计量生成患病率估计值。为了探索与年龄、性别、国家收入状况、地理区域和偏倚风险的相关性,我们进行了预先指定的 meta 回归、亚组和敏感性分析。
结果
在 6,976 项识别出的研究中,有 61 项符合纳入标准,包括来自 20 个国家和 376,676 名患者的数据。没有研究直接报告共病,都是报告个体疾病的患病情况。在住院患者中,患病率最高的是:人类免疫缺陷病毒感染(36.4%;95% CI:31.3-41.8),高血压(24.4%;95% CI:16.7–34.2),糖尿病(11.9%;95% CI:9.9-14.3),心力衰竭(8.2%;95% CI:5.6-11.9),慢性肾脏病(7.7%;95% CI:3.9-14.7)以及中风(6.8%;95% CI:4.7-9.6)。
结论
在撒哈拉以南非洲地区寻求医院治疗的患者中,尽管个体慢性疾病治疗负担沉重,但对共病的报告仍然很少。需要对共病治疗负担进行前瞻性公共卫生研究,以制定综合和针对具体情况的卫生系统干预措施,最大限度地提高患者的生存率和福祉。
Резюме
Цель
Оценить распространенность отдельных хронических заболеваний и мультиморбидности среди взрослого населения, поступившего в стационар в странах Африки к югу от Сахары.
Методы
Проведен систематический поиск в MEDLINE®, Embase®, Global Index Medicus, Global Health и SciELO публикаций, содержащих сведения о когортах пациентов, набранных в период с 1 января 2010 г. по 12 мая 2023 г. Включены статьи, в которых сообщалось о распространенности определенных хронических заболеваний в невыборочных службах неотложной помощи (отделениях скорой помощи или медицинских стационарах). Языковые ограничения отсутствовали. Были получены оценки распространенности с помощью метаанализа со случайными эффектами, а также 95%-е доверительные интервалы, 95%-е интервалы предсказания и статистика I2 для оценки гетерогенности. Для изучения ассоциаций с возрастом, полом, уровнем дохода в стране, географическим регионом и риском систематической ошибки авторы провели заранее оговоренные анализы метарегрессии, подгрупп и чувствительности.
Результаты
Из 6976 выявленных исследований 61 отвечало критериям включения и содержало данные из 20 стран и 376 676 человек. Ни в одном из них не было прямого указания на мультиморбидность, а вместо этого приводились данные о распространенности отдельных заболеваний. Среди госпитализаций наибольшую распространенность имели вирусная инфекция иммунодефицита человека (36,4%; 95%-й ДИ: 31,3–41,8), гипертония (24,4%; 95%-й ДИ:16,7–34,2), диабет (11,9%; 95%-й ДИ: 9,9–14,3), сердечная недостаточность (8,2%; 95%-й ДИ: 5,6–11,9), хроническая болезнь почек (7,7%; 95%-й ДИ: 3,9–14,7) и инсульт (6,8%; 95%-й ДИ: 4,7–9,6).
Вывод
Среди пациентов, обращающихся за стационарной медицинской помощью в странах Африки к югу от Сахары, мультиморбидность остается малоописанной, несмотря на высокое бремя отдельных хронических заболеваний. Проспективные исследования общественного здравоохранения по изучению мультиморбидности необходимы для разработки комплексных и учитывающих конкретные условия вмешательств в систему здравоохранения, направленных на максимальное увеличение выживаемости и благополучия пациентов.
Introduction
As life expectancy increases in sub-Saharan Africa, so too does the number of people who live with chronic conditions. Multimorbidity is defined as living with two or more chronic health conditions, inclusive of interactions between chronic communicable diseases and noncommunicable diseases.1–3 Inequalities in access to health care for chronic conditions affect early detection and control, and therefore on healthy life expectancy. Where primary care provision is limited, the index presentation of chronic disease is commonly through hospital acute care services.4,5 Acute medical services in these contexts traditionally have a single disease focus and may overlook multimorbidity in vulnerable patients.
In sub-Saharan Africa, the burden from chronic diseases is projected to increase: an estimated 125 million adults will have hypertension by 2025;6 and 26.9 million adults will have diabetes by 2030.7 Although dramatic reductions in the incidence and mortality of human immunodeficiency virus (HIV) have been observed in sub-Saharan Africa over the past 30 years, with increasing life expectancy, the high prevalence of HIV infection is presenting new challenges and demands within existing health-care systems.8 As such, integration of multimorbidity care into hospitals in sub-Saharan Africa will be of increasing importance over coming years. Cohort studies of adults in community settings have reported prevalence of multimorbidity of 69% (absolute numbers not available) in South Africa and 65% (252/389) in Burkina Faso.2,9 However, data on the prevalence of individual chronic diseases and multimorbidity in sub-Saharan African hospital settings are limited.10
To estimate prevalence of chronic disease within unselected cohorts of adult patients admitted to medical wards and emergency departments within sub-Saharan Africa, we conducted a systematic review of observational epidemiological studies. We focused on hospital rather than community presentations as populations in sub-Saharan Africa commonly have limited access to primary care. As such, hospital presentation represents an important node of intervention to control chronic disease and prevent development of secondary complications. Development of prevalence estimates within the region are important for policy-makers to prioritize and optimize service design and care delivery in sub-Saharan Africa.9,11
Methods
We conducted and reported this PROSPERO-registered systematic review (ID: CRD42021262708) in line with the PRISMA 2020 statement.12
Eligibility criteria
We employed the condition, context and population strategy (Box 1) to define our study population, in line with guidance for systematic reviews of observational epidemiological studies reporting prevalence data.13 Inclusion criteria were studies on adults in sub-Saharan Africa who had an acute hospital admission to emergency department or medical ward (representative of an unselected inpatient population in either emergency departments or medical wards). Data on outcome conditions are available (Box 2).
Box 1. Conditions, context, population criteria and search strategy used for the systematic review on patients with chronic conditions in sub-Saharan Africa.
Criteria
Conditions: Chronic diseases or risk factors that are likely to contribute to multimorbidity.
Context: Acute admission to adult medical wards or emergency departments in hospitals in sub-Saharan Africa.
Population: Adults of both sexes that meet the ‘context’ criteria (above).
Search strategy
(Hypertension OR diabetes OR obesity OR alcohol use OR tobacco OR kidney dysfunction OR hypercholesterolaemia OR HIV/AIDS OR HIV treatment failure OR HIV treatment non-compliance OR stroke OR ischaemic heart disease OR chronic liver disease OR heart failure OR chronic kidney disease OR chronic obstructive pulmonary disease OR multimorbidity) AND sub-Saharan Africa AND acute hospital care AND adults
Box 2. Outcome conditions used for the systematic review on patients with chronic conditions in sub-Saharan Africa.
We identified chronic conditions contributing to potential multimorbidity in adults in sub-Saharan Africa from the Global Burden of Disease 2019 databases for risks (risk factor conditions) and causes (diseases).14 The top 15 common causes resulting in death were included. In addition, HIV treatment failure and non-compliance were included a priori as significant drivers of HIV morbidity and mortality.15
Primary outcomes
Prevalence of the pre-selected primary preventive conditions and secondary (end-organ) conditions
Primary preventive conditions:
HIV, hypertension, diabetes, obesity, alcohol use, smoking and dyslipidaemia
Secondary (end-organ) conditions:
Stroke, ischaemic heart disease (including acute coronary syndrome), heart failure, chronic liver disease, chronic kidney disease and chronic obstructive pulmonary disease (COPD)
Secondary outcomes:
(i) prevalence of multimorbidity in acutely unwell adult patients presenting to hospitals in sub-Saharan Africa; (ii) prevalence of decompensated chronic disease-associated admission; and (iii) prevalence of HIV treatment failure, HIV treatment non-compliance, undiagnosed HIV and HIV status awareness.
HIV: human immunodeficiency virus.
Exclusion criteria were paediatric populations; community or out-patient settings (not acute care); denominator not available for population of interest (e.g. selected disease-specific cohorts or patients recruited solely from renal or cardiology wards); mental health conditions; trauma or surgical conditions; maternal, obstetric or gynaecological conditions; behavioural risk factors (excluding alcohol and tobacco); conference abstracts.
We excluded paediatric populations as patterns and clustering of multimorbidity in children younger than five years has been reviewed elsewhere, and found to be different than adult populations.16 Similarly, multimorbidity in maternal care in sub-Saharan Africa has recently been examined, suggesting a specific analysis for non-pregnant adults would complement these efforts.17 We restricted studies to those published and conducted since 1 January 2010 to avoid the use of data before the accelerated roll-out of antiretroviral treatment (ART) in sub-Saharan Africa which has driven changes in disease patterns.18 The 2010 cut-off is aligned with reporting frames of the Joint United Nations Programme on HIV/AIDS (UNAIDS) and Global Burden of Disease (GBD) studies.8,18,19 We did not apply language restrictions to inclusion criteria.
Databases and search terms
We systematically searched MEDLINE®, Embase®, Global Index Medicus, Global Health and SciELO databases on 12 May 2023 for articles published since 1 January 2010. EndNote X9.3.3 software (Thomson Reuters, Eagan, United States of America) was used to export references, and to identify and remove duplicates. Box 1 shows key search terms; the full search strategy is available in the online data repository.20
Selection process and data collection
Two authors independently assessed article titles, abstracts and full manuscripts to select studies meeting the eligibility criteria. Subsequently they piloted and refined the data collection tool20 using the first five eligible studies. These two authors then independently and manually extracted data from each manuscript, and assessed for bias using the modified Newcastle-Ottawa Scale for non-randomized studies21 (online repository).20 We categorized scores of ≤ 3 as very high risk of bias; 3–6 as high risk of bias; and scores of 7–9 as high quality.22 Discrepancies in selection and bias decisions were resolved through discussion and arbitration by a third reviewer.
Analysis
We captured extracted data using Microsoft Excel (Microsoft Corporation, Redmond, USA) and analysed using Stata 15 (StataCorp LLC, College Station, USA). We assessed publication bias by visual inspection of funnel plots of prevalence data when > 10 prevalence estimates were included,23 and Egger’s test.24 To visualize and assess individual disease prevalence alongside both 95% confidence and prediction levels, we generated forest plots with meta-analyses.25 We chose random effects modelling a priori due to the expected high level of heterogeneity,26 and we calculated pooled confidence with heterogeneity by the Hartung-Knapp-Sidik-Jonkman method.27,28 Data were logit transformed except when close to the extreme boundaries, where Freeman-Tukey double-arcsine transformation29 was employed (the full STATA statistical analysis code is available in the online repository).20
Heterogeneity was assessed by I2 statistic and by 95% prediction intervals (95% PI) which estimate the range of values in which future similar studies would be expected to fall.30 Random effects models were used to calculate 95% PIs when ≥ 5 study estimates were included in the meta-analysis, due to the high degree of imprecision with very low numbers of estimates.31,32
We performed meta-regression analysis where > 10 prevalence estimates were present per condition.33 We included a priori within univariable meta-regression analyses: age (median or mean); sex; date of study. In view of continued expansion in ART availability across sub-Saharan Africa,34 we also examined the temporal changes in the prevalence of conditions through meta regression. We also used meta regression to assess the association between study-level HIV prevalence and country-level adult HIV prevalence (as given by GBD 2019 database for adults ≥ 20 years).14
We pre-planned to report all prevalence estimates stratified by hospital population (medical vs emergency department); country-level income status defined by the World Bank 2022 Fiscal Year;35 geographical regions defined by the African Union (Central, Eastern, Southern, and Western Africa);36 and Newcastle-Ottawa-Scale. We also planned in advance to report prevalence estimates among the high- and mid-quality graded studies through sensitivity analyses once studies with a very high risk of bias were removed.
Results
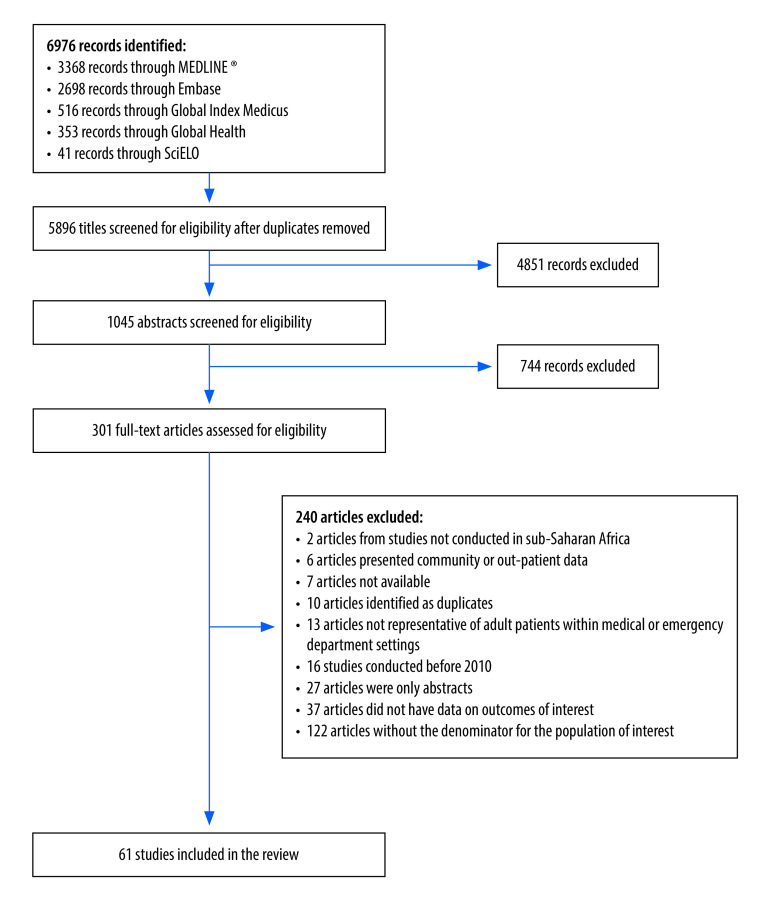
We identified 6976 manuscripts, of which 61 studies met the inclusion criteria (Fig. 1). These articles included 17 prospective cohort studies;37–53 11 retrospective cohorts;54–64 and 33 cross-sectional studies.65–97 The pooled sample size was 376 676 participants, including 97 737 participants admitted to the emergency department, and 278 939 admitted to medical wards. We did not identify any studies that intentionally investigated prevalence of multimorbidity as a primary objective. We have therefore structured the results section to explore the prevalence of the most commonly identified individual chronic diseases, followed by a section exploring available data on multimorbidity from secondary analyses of included studies.
Fig. 1.
Flowchart showing the selection of studies included in the systematic review on patients with chronic conditions in sub-Saharan Africa
Characteristics of studies that met the inclusion criteria are described in Table 1 (available at: https://www.who.int/publications/journals/bulletin/). Data derived from 20 of the 48 countries in sub-Saharan Africa, predominantly from South Africa (10/61; 16.4%), United Republic of Tanzania (7/61; 11.5%) and Ethiopia (7/61; 11.5%). Forty-two studies (68.9%) examined unselected patients on medical wards and 19 (31.2%) studies examined unselected patients from the emergency department. Studies were assessed as high quality in 27 (44.3%) cases, with high risk of bias in 26 (42.6%), and very high risk of bias in eight (13.1%; online repository).20
Table 1. Included studies in the systematic review on patients with chronic conditions, sub-Saharan Africa .
| Study | Country | Data collection year | Site | Study design | Outcome and outcome assessment | Sample size | Age of patients, years | No. of female patients (%) |
|---|---|---|---|---|---|---|---|---|
| Sheikh Hassan et al., 202393 | Somalia | 2021–2022 | Emergency department | Cross sectional | Stroke. Neurologist confirmed diagnosis based on clinical symptoms, signs, CT, MRI, EEG and laboratory results |
8500 | NR | NR |
| Sendekie et al., 202353 | Ethiopia | 2022 | Medical ward | Prospective cohort | Stroke, heart failure, diabetes mellitus, chronic kidney disease and chronic liver disease. All diagnoses ascertained from patient notes |
237 | Mean: 53 (SD: 18) | 114 (48.1) |
| Ronny et al., 202252 | Uganda | 2020 | Medical ward | Prospective cohort | Hypertension, HIV, diabetes mellitus, smoking and renal impairment. Renal impairment: diagnosed using urinalysis and/or estimated glomerular filtration rate. Other diagnoses ascertained from medical history. |
357 | Median: 47 (IQR: 32–63) | 168 (47.1) |
| Musung et al., 202291 | Democratic Republic of the Congo | 2018–2020 | Medical ward | Cross sectional | Stroke. Clinical presentation of stroke confirmed by CT scan |
9919 | NR | NR |
| Kemal et al., 202294 | Ethiopia | 2022 | Medical ward | Cross sectional | Stroke, diabetic emergencies and HIV status not known (at discharge). All diagnoses ascertained from medical notes |
423 | Median: 45 | 217 (51.3) |
| Kazibwe et al., 202264 | Uganda | 2011–2019 | Medical ward | Retrospective cohort study | HIV, diabetes mellitus and hypertension. Clinical diagnoses extracted from notes, based on history, examination and laboratory findings |
108 357 | Mean: 43 (SD: 19) | 55 620 (51.3) |
| Ibrahim et al., 202254 | Nigeria | 2015–2019 | Emergency department | Retrospective cohort | Stroke. Clinical presentation of stroke, confirmed by CT scan |
5944 | NR | NR |
| Roberts et al., 202165 | South Africa | 2018 | Emergency department | Cross sectional | HIV, HIV new diagnosis and HIV status not known (at discharge). Point-of-care HIV test |
790 | NR | 431 (54.6) |
| Iradukunda et al., 202166 | Burundi | 2019 | Medical ward | Cross sectional | Hypertension, diabetes mellitus, alcohol use and smoking. Hypertension: SBP > 140 mmHg and/or DBP > 90 mmHg after three readings |
353 | NR | 147 (41.6) |
| Ephraim et al., 202167 | Ghana | 2017–2018 | Medical ward | Cross sectional | Hypertension, alcohol use, smoking and renal impairment. Hypertension: duplicate blood pressure readings after 5 minutes rest. Renal impairment: creatinine at admission and 48 hours. Kidney disease criteriaa |
76 | Mean: 47 (SD: 18) | 45 (59.2) |
| Pintye et al., 202168 | Botswana | 2018–2019 | Emergency department | Cross sectional | HIV new diagnosis. HIV: HIV testing conducted per national guidelines |
9695 | Median: 30 (IQR 23–41) | 4953 (51.1) |
| Mouton et al., 202169 | South Africa | 2014–2015 | Medical ward b | Cross sectional | Hypertension, HIV, diabetes mellitus, heart failure, chronic kidney disease and chronic obstructive pulmonary disease. All diagnoses ascertained from medical notes |
1010 | Median: 44 (IQR: 31–61) | 580 (57.4) |
| Moretti et al., 202155 | Rwanda | 2013–2016 | Medical ward b | Retrospective cohort | Hypertension, HIV, stroke, chronic liver disease, heart failure, chronic kidney disease and renal impairment. All diagnoses ascertained from medical notes and vital signs |
1704 | Median: 41 (IQR: 29–59) | 795 (57.4) |
| Mkoko et al., 202170 | South Africa | 2016 | Medical ward | Cross sectional | Hypertension, Hypertension emergency, HIV, stroke, acute coronary syndrome and diabetes mellitus. Diagnoses based on medical records, available imaging and laboratory results. Diagnosis made by qualified physicians |
4884 | NR | 2727 (55.8) |
| Laher et al., 202137 | South Africa | 2017–2018 | Emergency department | Prospective cohort | HIV, HIV new diagnosis and ART compliance. Questionnaire on HIV treatment adherence, rapid HIV diagnostic test and ELISA |
11 383 | Median: 36 (IQR: 31–44) | 653 (54.2) |
| Fiseha et al., 202171 | Ethiopia | 2020 | Medical ward | Cross sectional | Hypertension, HIV, diabetes mellitus, chronic kidney disease and smoking. Chronic kidney disease: single creatinine measurement defined as estimated glomerular filtration rate < 60.c Patients with acute kidney injury excluded |
369 | Mean: 49 (SD: 18) | 192 (52.0) |
| Burke et al., 202156 | Malawi | 2012–2019 | Medical ward | Retrospective cohort | HIV. Electronic medical record database capture |
32 814 | NR | 16 618 (50.6) |
| Agazhe et al., 202157 | Ethiopia | 2017–2019 | Medical ward | Retrospective cohort | Stroke. Stroke: 62 patients diagnosed with imaging (53 with CT and 9 with MRI) and 33 diagnosed clinically without imaging |
3016 | NR | NR |
| Rao et al., 202072 | South Africa | 2017 | Emergency department | Cross sectional | HIV: HIV new diagnosis and HIV status not known (at admission and discharge). Two HIV rapid tests |
1880 | Median: 33 (IQR: 24–59) | 825 (47.4) |
| Nkoke et al.,202073 | Cameroon | 2018–2019 | Medical ward | Cross sectional | Hypertension emergency. Average of two blood pressure measurements. Hypertensive crisis: SBP/DBP ≥ 180/110 |
1536 | NR | NR |
| Mulugeta et al., 202074 | Ethiopia | 2017–2019 | Medical ward | Cross sectional | Stroke. Clinical diagnosis with imaging (CT or MRI) |
2100 | NR | NR |
| Hertz et al., 202038 | United Republic of Tanzania | 2019–2019 | Emergency department | Prospective cohort | Acute coronary syndrome. Patients with chest pain or shortness of breath had ECG and single troponin |
6083 | NR | NR |
| Gilbert et al., 202039 | Zimbabwe | 2018–2019 | Medical ward | Prospective cohort | Hypertension, HIV, diabetes mellitus, heart failure, chronic kidney disease and renal impairment. Chronic kidney disease, hypertension, diabetes and HIV diagnoses from past medical history |
253 | Mean: 48 | 137 (54.2) |
| Du Plooy et al., 202040 | South Africa | 2013–2014 | Medical ward | Prospective cohort | HIV. HIV: medical records and laboratory CD4 T-lymphocytes count |
808 | Median: 51 (IQR: 36– 65) | 534 (52.0) |
| Woyessa et al., 201975 | Ethiopia | 2017 | Emergency department | Cross sectional | Hypertension emergency, stroke, diabetes mellitus, diabetic emergency, heart failure and chronic obstructive pulmonary disease. No information provided for assessment |
889 | Mean: 35 (SD: 15) | 386 (43.4) |
| Sheikh et al.,201976 | Botswana | 2016 | Medical ward | Cross sectional | Renal impairment Review of medical charts and serum creatinine results. Renal impairment: estimated glomerular filtration rate < 60c |
804 | NR | NR |
| Shitandi et al., 201941 | Kenya | 2015–2016 | Medical ward | Prospective cohort | Stroke. Stroke: based on WHO definition with aid of CT and/or MRI imaging |
3200 | NR | NR |
| Nkoke et al., 201977 | Cameroon | 2016–2017 | Medical ward | Cross sectional | Hypertension emergency, stroke, acute coronary syndrome and heart failure. All diagnoses ascertained from medical notes |
3140 | NR | NR |
| Nakalema et al., 201978 | Uganda | 2015–2016 | Medical ward b | Cross sectional | Hypertension emergency. Average of two blood pressure recordings. Hypertensive crises: SBP/DBP ≥ 180/110 |
4000 | NR | NR |
| Mwenda et al., 201979 | Kenya | 2018 | Medical ward | Cross sectional | Hypertension, alcohol use, smoking, HIV, diabetes mellitus and chronic kidney disease. Renal impairment: estimated glomerular filtration rate < 60c chronic kidney disease: estimated glomerular filtration rate < 60, with markers of chronic renal damage (laboratory, ultrasound or history of chronic kidney disease > 3 months) |
306 | Median: 40 | 144 (47.1) |
| Mocumbi et al., 201980 | Mozambique | 2016–2017 | Emergency department | Cross sectional | Hypertension emergency, HIV, diabetes mellitus and smoking All diagnoses. ascertained from medical notes |
4100 | Mean: 37 (SD: 15) | 2049 (50.0) |
| Mandi et al., 201942 | Burkina Faso | 2016 | Medical ward b | Prospective cohort | Hypertension emergency. Average of two blood pressure recordings. Hypertensive crisis: SBP/DBP ≥ 180/120 mmHg |
1254 | NR | NR |
| Lakoh et al., 201943 | Sierra Leone | 2017 | Medical ward | Prospective cohort | HIV and HIV new diagnosis. Rapid test for HIV |
402 | NR | NR |
| Kalyesubula et al., 201981 | Uganda | 2011–2014 | Medical ward | Cross sectional | Hypertension emergency, HIV, stroke, diabetic emergency, heart failure, alcohol use and renal impairment. Electronic database capture of physician documented diagnoses. Diagnoses base on blood tests, ultrasound, X-ray, ECG, and echocardiography |
50 624 | Median: 38 | 26 175 (51.7) |
| Hertz et al., 201958 | United Republic of Tanzania | 2017–2018 | Emergency department | Retrospective cohort | Hypertension, hypertension emergency, diabetes mellitus and diabetic emergency. Physician documented diagnoses, or any of: hypertension: SBP/DBP ≥ 140/90 mmHg, uncontrolled hypertension: SBP/DBP ≥ 160/100 mmHg, diabetes: random glucose ≥ 200 mg/dL, uncontrolled diabetes mellitus: diabetic ketoacidosis or hyperosmolar hyperglycaemic state or hyperglycaemia > 250 mg/dL |
3961 | Median: 50 (IQR: 32–67) | 2194 (55.4) |
| Hertz et al., 201959 | United Republic of Tanzania | 2017–2018 | Medical ward b | Retrospective cohort | Stroke, acute coronary syndrome, heart failure and renal impairment. Physician documented diagnoses, supported by laboratory serum analysis (including troponin), imaging (CT and X-ray), ECG, echocardiography |
2418 | Median: 52 | 1328 (54.9) |
| Hansoti et al., 201982 | South Africa | 2016–2016 | Emergency department | Cross sectional | HIV and HIV treatment failure. HIV: laboratory serum analysis for HIV and viral load. HIV treatment failure > 1 000 copies/mL3 |
2100 | NR | NR |
| Hansoti et al., 201944 | South Africa | 2017–2018 | Emergency department | Prospective cohort | HIV, HIV treatment failure, HIV new diagnosis and HIV status not known (at discharge). HIV: laboratory serum analysis for HIV and viral load. HIV treatment failure > 1 000 copies/mL3 |
3537 | NR | 1123 (38.7) |
| Haachambwa et al., 201945 | Zambia | 2017–2018 | Medical ward b | Prospective cohort | HIV, HIV treatment failure, HIV new diagnosis and HIV status not known (at discharge). HIV history or dried spot HIV viral load testing. HIV treatment failure > 1 000 copies/mL3 |
1283 | Median: 38 (IQR: 30–48) | 657 (51.2) |
| Mchomvu et al., 201983 | United Republic of Tanzania | 2016–2017 | Emergency department | Cross sectional | Hypertension emergency, diabetic emergency, heart failure and renal impairment. Clinician diagnoses. supported by ECG, imaging, blood, urine dip, and echocardiography |
23 156 | NR | NR |
| Barak et al., 201984 | Botswana | 2015–2017 | Medical ward | Cross sectional | Hypertension, HIV treatment failure, HIV, HIV new diagnosis, HIV status not known (admission and discharge), stroke, diabetes mellitus and heart failure. HIV: history or CD4 T-lymphocytes count or HIV viral load testing. HIV treatment failure: > 400 copies/mL3. Other diagnoses ascertained from clinical notes |
2316 | Median: 51 (IQR: 34–71) | 1237 (53.4) |
| Shao et al., 201846 | United Republic of Tanzania | 2015 | Emergency department | Prospective cohort | Hypertension emergency. All adult patients screened with blood pressure measurement. Hypertensive crises: SBP/DBP ≥ 180/110 mmHg |
8002 | NR | NR |
| Matoga et al., 201847 | Malawi | 2011–2012 | Medical ward | Prospective cohort | HIV, HIV new diagnosis and HIV status not known (at discharge), heart failure. HIV status: history or HIV testing. Other diagnoses ascertained from clinical notes |
2911 | Mean: 39 (SD: 17) | 1457 (50.1) |
| Perry et al., 201748 | Botswana | 2011–2012 | Medical ward | Prospective cohort | Hypertension emergency, HIV, HIV new diagnosis, HIV status not known (admission and discharge), stroke, diabetic emergency and heart failure. HIV tests. Other diagnoses ascertained from medical records, supported by laboratory and microbiological tests |
972 | Mean: 48 (SD: 20) | 427 (43.9) |
| Kingery et al., 201749 | United Republic of Tanzania | 2014 | Medical ward | Prospective cohort | HIV, diabetes mellitus, hypertension, hypertension emergency, renal impairment, heart failure, obesity, alcohol use and smoking. Heart failure: Framingham criteria with echocardiography. All patients offered HIV tests, urine dip, serum creatinine. Smoking, alcohol use, hypertension, diabetes from medical history |
588 | NR | 330 (52.0) |
| Evans et al., 201785 | Malawi | 2015 | Medical ward | Cross sectional | Hypertension, renal impairment, chronic kidney disease, HIV, stroke, chronic liver disease, diabetes mellitus and heart failure. Chronic kidney disease: estimated glomerular filtration rate < 60 for > 3 months. Creatinine and urine measured every 48 hours. Other diagnoses ascertained from medical history |
892 | Median: 37 (IQR: 30–52) | 392 (43.9) |
| Allain et al., 201786 | Malawi | 2013–2014 | Medical ward | Cross sectional | Hypertension emergency, HIV, stroke, chronic liver disease, diabetes mellitus emergency, heart failure, alcohol use and renal impairment. All diagnoses ascertained from medical notes |
10 191 | NR | 5071 (49.8) |
| Peck et al., 201650 | United Republic of Tanzania | 2013 | Medical ward | Prospective cohort | HIV, new HIV, diabetes mellitus, hypertension, alcohol use, chronic kidney disease, renal impairment and smoking. HIV tests. Other diagnoses ascertained from medical notes |
637 | Mean: 47 (SD: 18) | 307 (48.2) |
| Long et al., 201660 | South Africa | 2010 | Medical ward | Retrospective cohort | Hypertension emergency, HIV, HIV status not known (admission), acute coronary syndrome, diabetic emergency and renal impairment. All diagnoses ascertained from electronic medical notes |
1041 | Median: 42 (IQR: 32–56) | 555 (53.3) |
| Stone et al., 201561 | Kenya | 2012 | Medical ward | Retrospective cohort | HIV. Diagnoses ascertained from medical notes |
956 | Mean: 42 (SD: 19) | 449 (47.0) |
| Noor et al., 201595 | Sudan | 2013–2014 | Medical ward | Cross sectional | Stroke and diabetic emergency. All diagnoses ascertained from medical notes |
2614 | Mean: 52 (SD: 19) | 1298 (49.7) |
| Meintjes et al., 201551 | South Africa | 2012–2013 | Medical ward | Prospective cohort | HIV treatment failure, HIV, HIV new diagnosis and HIV status not known (at discharge). HIV status: patients not known to be positive for HIV were offered test with two rapid tests. HIV treatment failure: viral load > 400 copies/mL3 |
1018 | NR | NR |
| Gizaw et al., 201562 | Ethiopia | 2010–2013 | Medical wards | Retrospective cohort | Diabetes mellitus. Diagnoses ascertained from medical notes |
8048 | NR | NR |
| Biney et al., 201596 | Ghana | 2013 | Emergency department | Cross-sectional | HIV and HIV status not known (at discharge). Two HIV rapid diagnostic tests |
667 | Median: 42 (IQR: 30–59) | 299 (44.8) |
| Ogunmola & Oladosu, 201498 | Nigeria | 2010–2012 | Emergency department | Retrospective cohort | HIV, stroke, hypertension emergency, renal impairment, chronic kidney disease, chronic liver disease, acute coronary syndrome, diabetic emergency, heart failure and chronic obstructive pulmonary disease. All diagnoses extracted from medical notes. Echocardiography performed on 59.5% in 2011, not available in 2010. Stroke: CT available for 3.9% |
2922 | Mean: 52 (SD: 20) | 1243 (42.5) |
| Kakoma et al., 201492 | Democratic Republic of the Congo | 2011–2012 | Medical wards | Cross-sectional | Diabetes mellitus and diabetic emergency. Diabetes mellitus: medical history. Diabetic ketoacidosis: glucose > 11 mmol/L in addition to ketonuria and glycosuria (no plasma pH available) |
1020 | NR | NR |
| SanJoaquin et al., 201387 | Malawi | 2010–2011 | Medical wards | Cross sectional | Hypertension, HIV, HIV status not known (discharge), renal impairment, stroke, chronic liver disease and diabetic emergency. Electronic data capture of primary diagnosis |
7103 | Mean: 37 | (50%) |
| Eyo et al., 201388 | Nigeria | 2010 | Emergency department | Cross sectional | Stroke Diagnoses ascertained from medical notes |
1104 | Median: 50 | NR |
| Kendig et al., 201389 | Malawi | 2012–2013 | Medical wards | Cross sectional | HIV, new HIV diagnosis and HIV status not known (at discharge). HIV status reviewed on all patients with HIV testing offered if HIV status unknown or last test > 3 months |
2985 | NR | 1325 (44.4) |
| Anyanwu et al., 201397 | Nigeria | 2011–2012 | Emergency department | Cross sectional | Diabetic emergency. Diagnoses ascertained from medical notes |
1703 | Mean: 48 (SD: 14) | 744 (43.7) |
| Wachira et al., 201290 | Kenya | 2010 | Emergency department | Cross sectional | Hypertension emergency. Diagnoses ascertained from medical notes |
1321 | NR | NR |
ART: antiretroviral therapy; CT: computed tomography; DBP: diastolic blood pressure; EEG: electroencephalogram; ELISA: enzyme linked immunosorbent assay; HIV: human immunodeficiency virus; IQR: interquartile range; mmHg: millimetres of mercury; MRI: magnetic resonance imaging; NR: not reported or not representative of unselected hospital population; SBP: systolic blood pressure; SD standard deviation.
a The Modification of Diet in Renal Disease equation, as modified by the criteria set by the Kidney Disease Improving Global Outcomes, is used to calculate the estimated glomerular filtration rate.
b Studies recruited participants with acute medical illnesses in emergency departments and triaged for medical care. We have therefore categorised these studies as prevalence estimates among patients from medical wards.
c The estimated glomerular filtration rate is calculated using the Chronic Kidney Disease Epidemiology Collaboration equation.
Note: The average age and the percentage of females reflect values from the unselected hospital population (either emergency department or medical wards). Where studies have not reported figures representative of the unselected population, we have marked this as NR (not reported or not representative of the unselected emergency department or medical ward population.
Prevalence of primary conditions
HIV
HIV prevalence was reported in 32 studies (Table 2). The pooled prevalence of HIV in medical wards was 36.4% (95% CI: 31.3–41.8; 25 studies)39,40,43,45,47–49,51,52,55,56,60,61,64,69–71,79,81,84–87,89 higher than the prevalence in emergency departments (21.9%; 95% CI: 14.5–31.7; seven studies).37,44,65,72,80,82,96 HIV infection was reported using laboratory or point-of-care diagnostics in 18 studies,37,40,43–45,47–51,56,65,68,72,82,84,89,96 and by medical records or clinical history in the remaining studies (Table 1).
Table 2. Prevalence data of chronic health conditions and risk factors in patients admitted to medical wards or emergency departments, sub-Saharan Africa.
| Condition, by patient population | No. of patients (no. of studies) | Prevalence, % (range) | 95% CI | 95% PI | Between group heterogeneity, P |
|---|---|---|---|---|---|
| Patients in medical wards | |||||
| Primary preventive conditions | |||||
| HIV | 231 032 (25) | 36.4 (11.4–67.0) | 31.3–41.8 | 14.6–65.8 | 0.01 |
| Treatment failure | 1 037 (3) | 31.2 (24.5–45.2) | 19.2–46.5 | – | 0.56 |
| Unknown status on admission | 4 329 (3) | 37.4 (35.2–41.3) | 34.1–40.8 | – | < 0.0001 |
| New diagnosis | 12 524 (8) | 8.8 (4.3–17.2) | 4.3–17.2 | 0.6–62.6 | 0.20 |
| Unknown status at discharge | 19 011 (8) | 16.8 (0.5–53.2) | 12.3–22.7 | 5.0–43.7 | 0.05 |
| Hypertension | 122 108 (14) | 24.4 (4.1–71.1) | 16.7–34.2 | 4.1–71.1 | 0.20 |
| Hypertensive emergency | 85 333 (11) | 5.2 (1.4–14.2) | 2.9–8.9 | 0.5–36.1 | 0.89 |
| Diabetes | 129 627 (15) | 11.9 (3.8–25.2) | 9.9–14.3 | 5.4–24.3 | 0.41 |
| Diabetic emergency | 73 988 (8) | 4.8 (1.1–17.9) | 2.7–8.4 | 0.6–31.8 | 0.54 |
| Secondary end-organ conditions | |||||
| Heart failure | 76 509 (13) | 8.2 (2.3–34.2) | 5.6–11.9 | 1.6–33.1 | 0.34 |
| Stroke | 105 506 (17) | 6.8 (1.6–32.9) | 4.7–9.6 | 1.3–29.5 | 0.56 |
| Acute coronary syndrome | 11 483 (4) | 1.0 (0.1–12.2) | 0.2–6.0 | – | 0.75 |
| Chronic kidney disease | 5 408 (8) | 7.7 (0.7–38.6) | 3.9–14.7 | 0.6–54.3 | 0.05 |
| Chronic liver disease | 20 550 (6) | 2.8 (1.3–5.0) | 1.8–4.3 | 0.6–12.3 | 0.73 |
| Chronic obstructive pulmonary disease | 1 010 (1) | 2.0 (2.0–2.0) | 1.2–3.0 | – | 0.20 |
| Risk factors | |||||
| Alcohol use | 1 960 (5) | 21.8 (7.8–51.0) | 8.0–47.1 | 0.3–96.5 | – |
| Smoking | 2 686 (7) | 9.6 (4.0–31.4) | 5.0–17.7 | 0.8–57.3 | 0.14 |
| Obesity | 588 (1) | 10.4 (0.10) | 8.0–13.1 | – | – |
| Dyslipidaemia | 0 (0) | – | – | – | – |
| Patients in emergency departments | |||||
| Primary preventive conditions | |||||
| HIV | 23 050 (7) | 21.9 (6.8–30.2) | 14.5–31.7 | 4.2–64.4 | 0.01 |
| Treatment failure | 463 (2) | 25.4 (19.4–32.8) | 14.6–40.6 | – | 0.56 |
| Unknown status on admission | 1 880 (1) | 75.3 (75.3–75.3) | 73.3–77.2 | – | < 0.0001 |
| New diagnosis | 27 285 (5) | 5.0 (3.0–8.1) | 3.0–8.1 | 0.6–29.7 | 0.20 |
| Unknown status at discharge | 7 332 (4) | 27.6 (18.0–40.7) | 18.5–39.0 | – | 0.05 |
| Hypertension | 8 061 (2) | 31.5 (28.9–34.3) | 26.4–37.1 | – | 0.20 |
| Hypertensive emergency | 40 251 (6) | 5.5 (2.5–14.5) | 3.1–9.5 | 0.6–35.0 | 0.89 |
| Diabetes | 8 950 (3) | 9.3 (5.5–13.1) | 5.1–16.2 | – | 0.41 |
| Diabetic emergency | 32 631 (5) | 3.4 (0.6–6.7) | 1.3–8.7 | 0.1–64.5 | 0.54 |
| Secondary end-organ conditions | |||||
| Heart failure | 26 967 (3) | 4.0 (1.7–11.3) | 0.9–16.1 | – | 0.34 |
| Stroke | 19 359 (5) | 5.4 (2.2–13.5) | 2.8–10.2 | 0.4–45.4 | 0.56 |
| Acute coronary syndrome | 9 005 (2) | 0.5 (0.1–2.5) | 0.0–11.2 | – | 0.75 |
| Chronic kidney disease | 2 922 (1) | 3.7 (3.7–3.7) | 3.1–4.5 | – | 0.05 |
| Chronic liver disease | 2 922 (1) | 3.1 (3.1–3.1) | 2.5–3.8 | – | 0.73 |
| Chronic obstructive pulmonary disease | 3 811 (2) | 1.0 (0.6–1.5) | 0.4–2.6 | – | 0.20 |
| Risk factors | |||||
| Alcohol use | 0 (0) | – | – | – | – |
| Smoking | 4 100 (1) | 14.8 (14.8–14.8) | 13.7–15.9 | – | 0.14 |
| Obesity | 0 (0) | – | – | – | – |
| Dyslipidaemia | 0 (0) | – | – | – | – |
Note: We calculated between group heterogeneity using a random effects meta-analysis model, which compares prevalence in medical wards to prevalence in emergency departments. Some conditions have no 95% PI because prediction intervals were calculated when ≥ 5 prevalence estimates were included in the meta-analysis.
Due to limited emergency department data (< 10 studies), only data from medical wards were included in the meta-regression and sub-group analyses. HIV infection prevalence among medical in-patients correlated with national HIV prevalence (odds ratio, OR: 1.33; 95% CI: 1.09–1.63; online repository).20 Higher HIV prevalence was noted in southern Africa (46.0%; 95% CI: 40.5–51.7), as compared to eastern Africa (22.5%; 95% CI: 19.8–25.4). There was no association between HIV prevalence and year of study (OR: 0.93; 95% CI: 0.84–1.04); or country-level income status, sex or average age (online repository).20 Prevalence of HIV was also unaffected by the removal of studies with a very high risk of bias (36.9%; 95% CI: 31.6–42.6).
Previously undiagnosed HIV was reported in 13 studies, with a pooled prevalence of 8.8% (95% CI: 4.3–17.2; eight studies)43,45,47,48,50,51,84,89 among medical patients, and 5.0% (95% CI:3.0–8.1; five studies)37,44,65,68,72 among emergency department patients (Fig. 2). Among patients established on antiretroviral therapy, the pooled prevalence of treatment failure was 31.2% (95% CI: 19.2–46.5; three studies)45,51,84 among medical patients and 25.4% (95% CI: 14.6–40.6; two studies)44,82 among emergency department patients.
Fig. 2.
Prevalence of primary preventive chronic conditions in patients admitted to medical wards or emergency departments, sub-Saharan Africa
CI: confidence interval; PI: prediction interval.
Note: Values are also presented in Table 2. Some conditions have no 95% PI because prediction intervals were calculated when ≥ 5 prevalence estimates were included in the meta-analysis
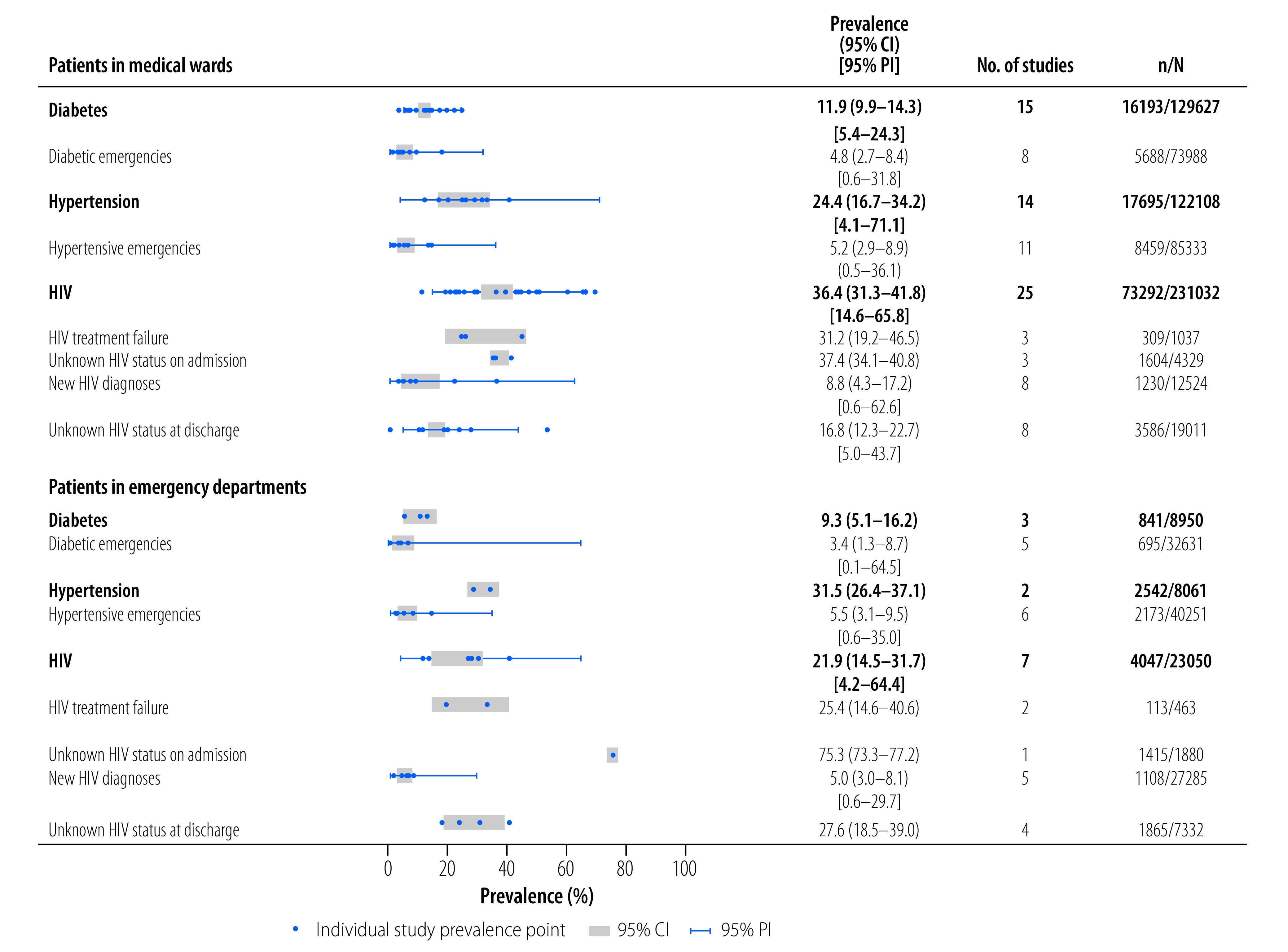
Hypertension
We estimated the prevalence of hypertension from 16 studies. Pooled prevalence was 24.4% (95% CI: 16.7–34.2; 14 studies)39,49,50,52,55,64,66,67,69–71,79,84,85 in medical wards, and 31.5% (95% CI: 26.4–37.1; two studies)58,80 in emergency departments. A high degree of heterogeneity in prevalence estimates was observed in the medical setting (95% PI: 4.1–71.1; I2: 99.7%). Hypertension diagnoses were classified according to in-patient assessment of blood pressure in two studies (≥ 140/90 mmHg), and from medical records alone in 14 studies (Table 1).
Hypertension prevalence correlated positively with country-level economic status (OR: 1.50; 95% CI: 1.12–2.00; online repository).20 We did not find evidence that hypertension prevalence varied by age, sex, study region, study year or study quality (online repository).20
Acute hypertensive presentations to hospital were reported in 17 studies, with a pooled prevalence of 5.2% (95% CI: 2.9–8.9; 11 studies)42,48,49,60,70,73,77,78,81,86,87 among medical settings and 5.5% (95% CI: 3.1–9.5; six studies)46,58,75,83,90,98 in emergency departments.
Diabetes
The pooled prevalence of diabetes in medical settings was 11.9% (95% CI: 9.9–14.3; 15 studies; Table 2).39,49,50,52,53,62,64,66,69–71,79,84,85,92 In emergency departments, we found an overlapping prevalence estimate of 9.3% (95% CI: 5.1–16.2; three studies).58,75,80 A high degree of heterogeneity of estimates in both settings is noted (medical wards 95% PI: 5.4–24.3; I2: 97.6% and emergency departments I2: 98.5%; < 5 studies). The heterogeneity within the medical wards could not be explained by differences in age, sex, study quality or study region (online repository).20 Diabetes was classified using random glucose measurement (≥ 200 mg/dL) in one study,58 and ascertained from medical notes in all other studies (Table 1). Diabetic emergencies were observed in 4.8% (95% CI: 2.7–8.4; eight studies)48,60,81,86,87,92,94,95 of medical patients and 3.4% (95% CI: 1.3–8.7; five studies)58,75,83,97,98 of emergency department patients (Fig. 2).
Prevalence of secondary conditions
Heart failure presentations affected 8.2% (95% CI: 5.6–11.9; 13 studies)39,47–49,53,55,59,69,73,81,84–86 of medical patients, and 4.0% (95% CI: 0.9–16.1; three studies)75,83,98 of emergency department patients (Fig. 3). Only 31.2% of studies reporting on heart failure described the use of echocardiography.49,59,63,81,83 None of the studies reported prevalence of ischaemic heart disease. However, acute coronary syndrome was found in 1.0% (95% CI: 0.2–6.0; four studies)59,60,70,73 of medical patients, and 0.5% (95% CI: 0.0–11.2; two studies)38,98 of emergency department patients. Two studies used electrocardiogram and troponin criteria in making the diagnosis.38,59
Fig. 3.
Prevalence of secondary end-organ conditions in patients admitted to medical wards or emergency departments, sub-Saharan Africa
CI: confidence interval; PI: prediction interval.
Note: Values are also presented in Table 2. Some conditions have no 95% PI because prediction intervals were calculated when ≥ 5 prevalence estimates were included in the meta-analysis
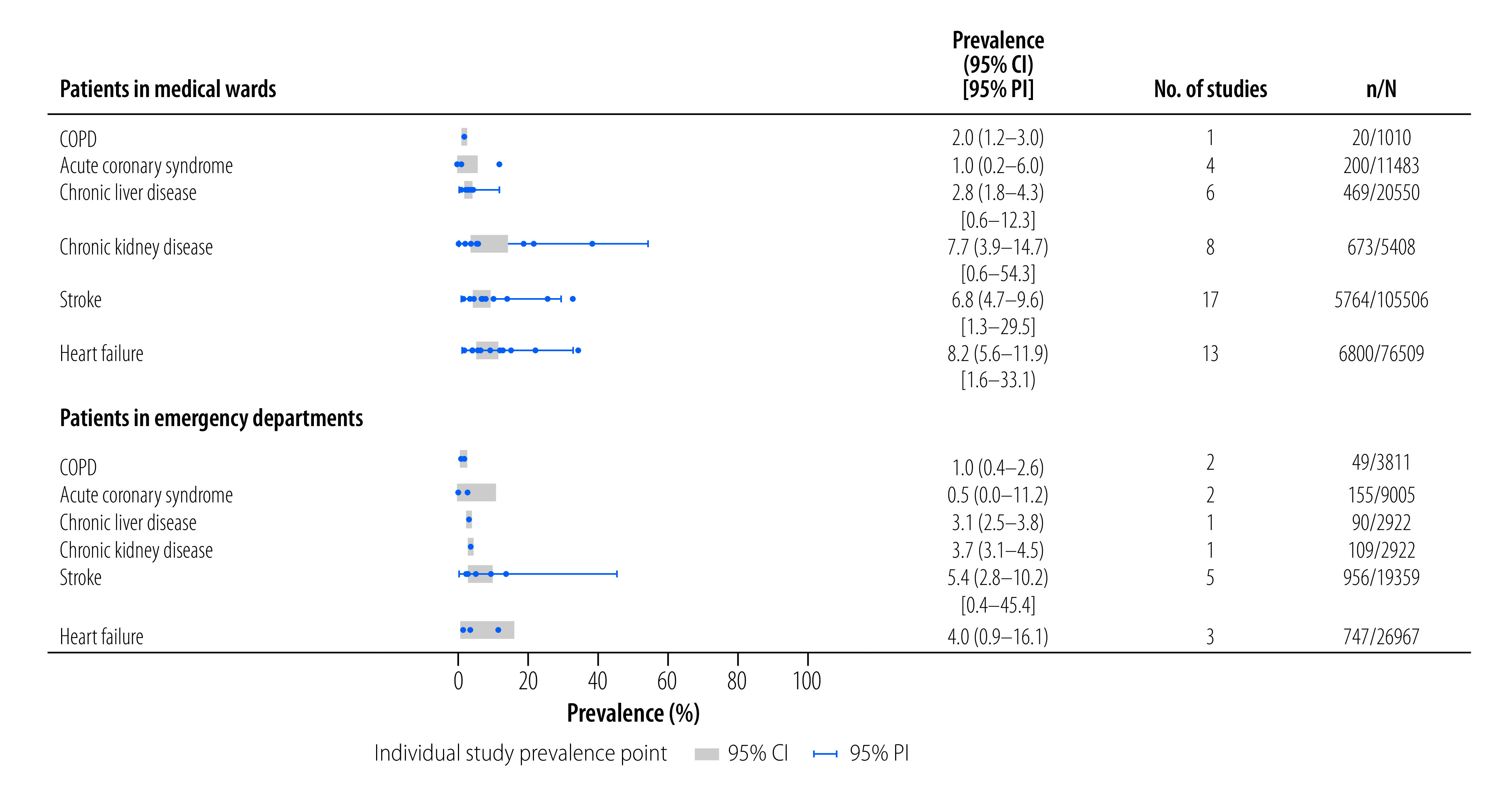
Acute exacerbation of chronic obstructive pulmonary disease was observed in 2.0% (95% CI: 1.2–3.0; one study)69 of medical patients, and 1.0% (95% CI: 0.4–2.6; two studies)75,98 of emergency department patients. No studies described the use of spirometry to classify diagnoses.
The prevalence of stroke admissions was 6.8% (95% CI: 4.7–9.6; 17 studies)41,48,53,55,57,59,70,73,74,81,84–87,91,94,95in medical settings, and 5.4% (95% CI: 2.8–10.2; five studies)54,75,88,93,98 in emergency departments. Of these 22 studies, eight used radiological imaging to confirm the diagnosis.41,54,57,59,74,91,93,98
Nine studies reported prevalence of background chronic kidney disease in isolation. Pooled prevalence was 7.7% (95% CI: 3.9–14.7; eight studies)39,50,53,55,69,71,79,85 in medical patients, and 3.7% (95% CI: 3.1–4.5; one study)98 in the sole emergency department study. However, only two studies confirmed chronicity using serum and/or sonographic markers of kidney disease.79,85
Multimorbidity
None of the selected studies investigated multimorbidity prevalence per se. Fourteen studies reported comorbid chronic diseases alongside a primary condition (online repository).20 Hypertension and diabetes co-prevalence was reported in three studies: 3790/108 357 (3.5%);64 33/353 (9.3%);66 and 273/3961 (6.9%).58 HIV and hypertension co-prevalence was reported in three studies: 665/108 357 (0.6%);64 6/972 (0.6%);48 and 140/2316 (6.0%).84 HIV and diabetes co-prevalence was also reported in three studies: 666/108 358 (0.6%);64 78/2316 (3.4%);84 and 78/972 (8.0%).48
Reporting bias
We found evidence of publication bias from small studies reporting prevalence of hypertension (Egger’s P -value: 0.04), but no evidence of publication bias for other conditions (online repository).20 To reduce very high risk of bias, we conducted sensitivity analyses, and eight studies with very high risk of bias were subsequently excluded from the meta-analyses, with no observed changes in synthesized prevalence estimates (online repository).20
Discussion
Here we present synthesized prevalence data for multiple individual chronic diseases among hospitalized adults in sub-Saharan Africa. We found no studies that directly measured the prevalence of multimorbidity, although secondary analyses within these studies suggest this to be a major problem. HIV, hypertension and diabetes were all common, mirrored by high proportions of patients presenting with decompensated disease. These presentations included hypertensive or diabetic emergencies; undiagnosed or undertreated HIV; and end-organ secondary complications such as heart failure, chronic kidney disease and stroke. Improvements in early recognition and management of chronic diseases are likely to result in improved healthy life expectancy for the most vulnerable patients.
Our estimated HIV prevalence in sub-Saharan African hospitals is about eightfold higher than reported estimates at the community level in sub-Saharan Africa (36.4% versus 4.7%).14 Reassuringly, more than 90% of HIV-infected patients included in this review knew their diagnosis; however, treatment failure in about one third of patients indicates that viral control should be a keystone issue for future public health campaigns. Absence of temporal changes in our review may reflect regional and sub-national variability in the HIV epidemic and ART scale-up.8,34 This result contrasts data from Malawi which shows falling HIV admissions from 2012 to 2019.56
For hypertension, prevalence in sub-Saharan communities is estimated at 30.8%,99 which is similar to hospital prevalence found in our study (24.4%). We found that admission with severe uncontrolled hypertension was higher than in high-income countries (5.2% versus 1.9%).100 With diabetes, the estimated hospital prevalence was 11.9% which is higher than community levels in sub-Saharan Africa (4.2%).14 Diabetic emergencies represented 40% of patients admitted with diabetes. In contrast, findings from the National Diabetes Inpatient Audit England 2019 found that diabetic emergencies were approximately one in 20 in diabetic inpatients.101 In sub-Saharan hospitals, the high burden of decompensated illness presentations indicate missed opportunities to better diagnose and control disease.
A similar pattern was seen in disease burden from end-organ complications, dominated by heart failure and stroke (8.2% and 6.8%, respectively), which are higher than estimates from outside sub-Saharan Africa (1–2%102,103 and 3.7–4.4%).104,105 This reinforces observations that in sub-Saharan Africa: (i) hypertension is the leading cause of heart failure and stroke; and (ii) 88% of the global hypertension mortality is found in low- and middle-income countries.106 Estimates from the Global Burden of Disease 2017 suggest that ischaemic heart disease is the most common cause of cardiovascular-related death in sub-Saharan Africa (5% of all deaths).107 Although we did not find data on the prevalence of ischaemic heart disease, our result on prevalence of acute coronary syndromes (1%) suggests low rates of ischaemic heart disease in sub-Saharan hospitals, in line with previous hospital-based observations.108–111
The strengths of our study include studies reporting data from unselected medical and emergency department populations, designed to reduce selection bias. There were no language restrictions in our search strategy, and we were able to include data from 20 sub-Saharan African countries, representative of nearly 400 000 patient admissions. We explored heterogeneity by calculating 95% prediction intervals to provide clinically relevant information on the degree of heterogeneiety.30 In addition, we restricted our pooled synthesis and used robust methods to explore potential explanations, including predetermined sensitivity, subgroup, and meta-regression analysis.
The heterogeneity observed in our analysis is a common limitation of systematic reviews of disease prevalence.7,112 The reasons for this include differences in population demographics; criteria and tools used to ascertain outcomes; and study quality. Given differences between countries in terms of access to health care, socioeconomic status, geography and ethnicity, heterogeneity both between and within countries in sub-Saharan Africa is expected. For example, HIV prevalence is likely to be higher in hospitalized patients compared to the general population for a given country, with multiple factors (e.g. success in meeting the UNAIDS 90–90–90 objectives)113 influencing this relationship.
Another limitation was the non-uniform application of diagnostic criteria, and likely inconsistent access to laboratory assays, equipment and technical expertise. Quality issues relating to outcome ascertainment were identified in over half of all included studies. For instance, troponin, electrocardiogram and angiography were underutilized in the diagnosis of acute coronary syndrome, and spirometry for chronic obstructive pulmonary disease. This underutilization may have led to underreporting of these conditions. Although 13.1% of studies were at very high risk of bias, sensitivity analyses demonstrated consistent disease prevalence estimates.
A key finding from this systematic review is the lack of primary outcome data on multimorbidity in sub-Saharan hospitals. Synthesized community-level data from predominantly high-income settings have estimated multimorbidity prevalence is 33.1%,114 with disease combinations reflecting the most prevalent individual long-term conditions within the population.115 Prospective cohort studies, designed explicitly to examine multimorbidity prevalence using standardized diagnostic tools and criteria, could support the development of health services more responsive to patient need.
We found high prevalence of single chronic diseases in hospital settings. From the limited data on multimorbidity identified within the secondary analyses of included studies, it is probable that there is a high burden of missed multimorbidity in sub-Saharan Africa. When examining the secondary outcome data from the studies included in this analysis, it was revealed that there may be a significant burden of multimorbidity in this particular context. For instance, one study primarily focused on investigating the prevalence of hypertension among medical in-patients, but it also discovered that out of the 59 patients with hypertension, 33 of them were also diagnosed with diabetes.66 We also found high prevalence of acute decompensated presentations. We observed increased chronic disease prevalence within hospitals compared to community settings. Hospitalized patients in sub-Saharan Africa are therefore likely to have increased preventable disability and early mortality compared to high-income settings.
Our review suggests important clinical and policy implications. Similarly, the need for context-appropriate diagnostics was underscored by a 2023 World Health Assembly resolution.116 Inconsistent use of diagnostic tools and criteria has also been described within the Lancet commission on diagnostics, showing limited or no access for 47% of the global population.117 Implementation of standardized chronic disease programmes which focus on community care (e.g. the WHO package of noncommunicable disease interventions)118 could be strengthened by explicit linkages to secondary clinical pathways.
Successful implementation of such linkages will require broad health systems approaches including: health-care worker training; development of financial models that promote reliable access to diagnostics and essential medicines; integration with existing health information systems;119 robust governance structures; and strengthened local leadership.116 The need to shift away from disease- to patient- centred approaches is a consistent theme highlighted in recent Lancet commissions.120,121 Improved health literacy is likely to empower patients and their caregivers in managing their health and chronic conditions, and navigating care pathways. Policies which link primary and secondary care for chronic disease management could facilitate more accessible and cost-effective models of care delivery, from both provider and patient perspectives.
Acknowledgements
SS is also affiliated with Malawi-Liverpool-Wellcome Trust Clinical Research Programme, Blantyre, Malawi. SS and SG are also affiliated with Queen Elizabeth Central Hospital, Blantyre, Malawi. PD is also affiliated with Northern Care Alliance NHS Foundation Trust, Salford Care Organisation, Salford, England. BM is also affiliated with Critical Care, Liverpool University Hospitals NHS Foundation Trust, Liverpool, England.
Funding:
SS was funded by a Wellcome Trust Clinical PhD Fellowship (203919/Z/16/Z); JR by a Wellcome Trust Career Development Award (211098Z); and PD by the Manchester National Institute for Health and Care Research (NIHR) Biomedical Research Centre and a NIHR Senior Investigator award (203745). BM was supported by a NIHR Research and Innovation for Global Health Transformation award (NIHR201708) using British aid from the United Kingdom of Great Britain and Northern Ireland Government to support global health research. In addition, this publication is associated with the Research, Evidence and Development Initiative (project number 300342-104).
Competing interests:
None declared.
References
- 1.Chang AY, Gómez-Olivé FX, Payne C, Rohr JK, Manne-Goehler J, Wade AN, et al. Chronic multimorbidity among older adults in rural South Africa. BMJ Glob Health. 2019. Aug 5;4(4):e001386. 10.1136/bmjgh-2018-001386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Price AJ, Crampin AC, Amberbir A, Kayuni-Chihana N, Musicha C, Tafatatha T, et al. Prevalence of obesity, hypertension, and diabetes, and cascade of care in sub-Saharan Africa: a cross-sectional, population-based study in rural and urban Malawi. Lancet Diabetes Endocrinol. 2018. Mar;6(3):208–22. 10.1016/S2213-8587(17)30432-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mathabire Rücker SC, Tayea A, Bitilinyu-Bangoh J, Bermúdez-Aza EH, Salumu L, Quiles IA, et al. High rates of hypertension, diabetes, elevated low-density lipoprotein cholesterol, and cardiovascular disease risk factors in HIV-infected patients in Malawi. AIDS. 2018. Jan 14;32(2):253–60. 10.1097/QAD.0000000000001700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Xu X, Mishra GD, Jones M. Evidence on multimorbidity from definition to intervention: an overview of systematic reviews. Ageing Res Rev. 2017. Aug;37:53–68. 10.1016/j.arr.2017.05.003 [DOI] [PubMed] [Google Scholar]
- 5.Rodrigues LP, de Oliveira Rezende AT, Delpino FM, Mendonça CR, Noll M, Nunes BP, et al. Association between multimorbidity and hospitalization in older adults: systematic review and meta-analysis. Age Ageing. 2022. Jul 1;51(7):afac155. 10.1093/ageing/afac155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Twagirumukiza M, De Bacquer D, Kips JG, de Backer G, Stichele RV, Van Bortel LM. Current and projected prevalence of arterial hypertension in sub-Saharan Africa by sex, age and habitat: an estimate from population studies. J Hypertens. 2011. Jul;29(7):1243–52. 10.1097/HJH.0b013e328346995d [DOI] [PubMed] [Google Scholar]
- 7.Mbanya JC, Motala AA, Sobngwi E, Assah FK, Enoru ST. Diabetes in sub-Saharan Africa. Lancet. 2010. Jun 26;375(9733):2254–66. 10.1016/S0140-6736(10)60550-8 [DOI] [PubMed] [Google Scholar]
- 8.Jahagirdar D, Walters MK, Novotney A, Brewer ED, Frank TD, Carter A, et al. Global, regional, and national sex-specific burden and control of the HIV epidemic, 1990-2019, for 204 countries and territories: the Global Burden of Diseases Study 2019. Lancet HIV. 2021. Oct;8(10):e633–51. 10.1016/S2352-3018(21)00152-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hien H, Berthé A, Drabo MK, Meda N, Konaté B, Tou F, et al. Prevalence and patterns of multimorbidity among the elderly in Burkina Faso: cross-sectional study. Trop Med Int Health. 2014. Nov;19(11):1328–33. 10.1111/tmi.12377 [DOI] [PubMed] [Google Scholar]
- 10. Multimorbidity: a priority for global health research. London: Academy of Medical Sciences; 2018. [Google Scholar]
- 11.Multimorbidity: technical series on safer primary care. Geneva: World Health Organization; 2016. [Google Scholar]
- 12.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021. Mar 29;372(71):n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munn Z, Moola S, Lisy K, Riitano D, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid-Based Healthc. 2015. Sep;13(3):147–53. 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 14.Institute for Health Metrics and Evaluation. GBD results [internet]. Seattle: University of Washington; 2019. Available from: http://ghdx.healthdata.org/gbd-results-tool [cited 2021 Jun 30].
- 15.Gupta-Wright A, Fielding K, van Oosterhout JJ, Alufandika M, Grint DJ, Chimbayo E, et al. Virological failure, HIV-1 drug resistance, and early mortality in adults admitted to hospital in Malawi: an observational cohort study. Lancet HIV. 2020. Sep;7(9):e620–8. 10.1016/S2352-3018(20)30172-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Obasohan PE, Walters SJ, Jacques R, Khatab K. Risk factors associated with multimorbidity among children aged under five years in sub-Saharan African countries: a scoping review. Int J Environ Res Public Health. 2023. Jan 12;20(2):1377. 10.3390/ijerph20021377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCauley M, Zafar S, van den Broek N. Maternal multimorbidity during pregnancy and after childbirth in women in low- and middle-income countries: a systematic literature review. BMC Pregnancy Childbirth. 2020. Oct 20;20(1):637. 10.1186/s12884-020-03303-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miles to go: Global AIDS update 2018. Geneva: UNAIDS; 2018. [Google Scholar]
- 19.Ghys PD, Williams BG, Over M, Hallett TB, Godfrey-Faussett P. Epidemiological metrics and benchmarks for a transition in the HIV epidemic. PLoS Med. 2018. Oct 25;15(10):e1002678. 10.1371/journal.pmed.1002678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Spencer S, Rylance J, Quint JK, Gordon SB, Dark P, Morton B. Prevalence of multimorbidity among hospitalised adults in sub-Saharan Africa: a systematic review [online repository]. Boston: Dataverse, The President & Fellows of Harvard College; 2023. 10.7910/DVN/EEQLNG 10.7910/DVN/EEQLNG [DOI]
- 21.Lo CK-L, Mertz D, Loeb M. Newcastle-Ottawa Scale: comparing reviewers’ to authors’ assessments. BMC Med Res Methodol. 2014. Apr 1;14(1):45. 10.1186/1471-2288-14-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wells GSB, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute; 2009. [Google Scholar]
- 23.Sterne JA, Sutton AJ, Ioannidis JP, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011. Jul 22;343 jul22 1:d4002. 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 24.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997. Sep 13;315(7109):629–34. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Chapter 40: When Does it Make Sense to Perform a Meta-Analysis? Introduction to meta-analysis. Chichester: John Wiley & Sons; 2009. 10.1002/9780470743386.ch40 [DOI] [Google Scholar]
- 26.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010. Apr;1(2):97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 27.Nyaga VN, Arbyn M, Aerts M. Metaprop: a Stata command to perform meta-analysis of binomial data. Arch Public Health. 2014. Nov 10;72(1):39. 10.1186/2049-3258-72-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Veroniki AA, Jackson D, Bender R, Kuss O, Langan D, Higgins JPT, et al. Methods to calculate uncertainty in the estimated overall effect size from a random-effects meta-analysis. Res Synth Methods. 2019. Mar;10(1):23–43. 10.1002/jrsm.1319 [DOI] [PubMed] [Google Scholar]
- 29.Lin L, Xu C. Arcsine-based transformations for meta-analysis of proportions: Pros, cons, and alternatives. Health Sci Rep. 2020. Jul 27;3(3):e178. 10.1002/hsr2.178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.IntHout J, Ioannidis JP, Rovers MM, Goeman JJ. Plea for routinely presenting prediction intervals in meta-analysis. BMJ Open. 2016. Jul 12;6(7):e010247. 10.1136/bmjopen-2015-010247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riley RD, Higgins JP, Deeks JJ. Interpretation of random effects meta-analyses. BMJ. 2011. Feb 10;342 feb10 2:d549. 10.1136/bmj.d549 [DOI] [PubMed] [Google Scholar]
- 32.Spineli LMP, Pandis N. Prediction interval in random-effects meta-analysis. Am J Orthod Dentofacial Orthop. 2020. Apr;157(4):586–8. 10.1016/j.ajodo.2019.12.011 [DOI] [PubMed] [Google Scholar]
- 33.Deeks JJHJ, Altman DG. Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions. version 6.3 (updated February 2022). Chichester: Cochrane; 2022. [Google Scholar]
- 34.Access to Antiretroviral Therapy in Africa: Status Report on Progress towards the 2015 Targets. Geneva: UNAIDS; 2013. [Google Scholar]
- 35.World Bank Country and Lending Groups [internet]. Washington, DC: World Bank; 2022. Available from: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [cited 2022 Nov 9].
- 36.Member States [internet]. Addis Ababa: The African Union Commission; 2022. Available from: https://au.int/en/member_states/countryprofiles2 [cited 2022 Aug 20].
- 37.Laher AE, Venter WDF, Richards GA, Paruk F. Profile of presentation of HIV-positive patients to an emergency department in Johannesburg, South Africa. South Afr J HIV Med. 2021. Jan 29;22(1):1177. 10.4102/sajhivmed.v22i1.1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hertz JT, Sakita FM, Kweka GL, Limkakeng AT, Galson SW, Ye JJ, et al. Acute myocardial infarction under-diagnosis and mortality in a Tanzanian emergency department: A prospective observational study. Am Heart J. 2020. Aug;226:214–21. 10.1016/j.ahj.2020.05.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gilbert A, Robertson L, Heron JE, Chadban S, Ndhlovu C, Dahwa RF, et al. Risk factors for development of acute kidney injury in hospitalised adults in Zimbabwe. PLoS One. 2020. Oct 26;15(10):e0241229. 10.1371/journal.pone.0241229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Du Plooy N, Day C, Manning K, Abdullah F, James K, Grace L, et al. Prevalence and outcome of delirium among acute general medical inpatients in Cape Town, South Africa. S Afr Med J. 2020. May 29;110(6):519–24. [DOI] [PubMed] [Google Scholar]
- 41.Shitandi OB, Ogeng’o JA, Misiani MK, Kariuki BN. Pattern of stroke in a rural Kenyan hospital. Malawi Med J. 2019. Mar;31(1):50–5. 10.4314/mmj.v31i1.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mandi DG, Yaméogo RA, Sebgo C, Bamouni J, Naibé DT, Kologo KJ, et al. Hypertensive crises in sub-Saharan Africa: Clinical profile and short-term outcome in the medical emergencies department of a national referral hospital in Burkina Faso. Ann Cardiol Angeiol (Paris). 2019. Oct;68(4):269–74. 10.1016/j.ancard.2019.07.007 [DOI] [PubMed] [Google Scholar]
- 43.Lakoh S, Jiba DF, Kanu JE, Poveda E, Salgado-Barreira A, Sahr F, et al. Causes of hospitalization and predictors of HIV-associated mortality at the main referral hospital in Sierra Leone: a prospective study. BMC Public Health. 2019. Oct 21;19(1):1320. 10.1186/s12889-019-7614-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hansoti B, Mwinnyaa G, Hahn E, Rao A, Black J, Chen V, et al. Targeting the HIV Epidemic in South Africa: The Need for Testing and Linkage to Care in Emergency Departments. EClinicalMedicine. 2019. Aug 19;15:14–22. 10.1016/j.eclinm.2019.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Haachambwa L, Kandiwo N, Zulu PM, Rutagwera D, Geng E, Holmes CB, et al. Care Continuum and Postdischarge Outcomes Among HIV-Infected Adults Admitted to the Hospital in Zambia. Open Forum Infect Dis. 2019. Jul 16;6(10):ofz336. 10.1093/ofid/ofz336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shao PJ, Sawe HR, Murray BL, Mfinanga JA, Mwafongo V, Runyon MS. Profile of patients with hypertensive urgency and emergency presenting to an urban emergency department of a tertiary referral hospital in Tanzania. BMC Cardiovasc Disord. 2018. Aug 2;18(1):158. 10.1186/s12872-018-0895-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Matoga MM, Rosenberg NE, Stanley CC, LaCourse S, Munthali CK, Nsona DP, et al. Inpatient mortality rates during an era of increased access to HIV testing and ART: A prospective observational study in Lilongwe, Malawi. PLoS One. 2018. Feb 7;13(2):e0191944. 10.1371/journal.pone.0191944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Perry ME, Kalenga K, Watkins LF, Mukaya JE, Powis KM, Bennett K, et al. HIV-related mortality at a district hospital in Botswana. Int J STD AIDS. 2017. Mar;28(3):277–83. 10.1177/0956462416646492 [DOI] [PubMed] [Google Scholar]
- 49.Kingery JR, Yango M, Wajanga B, Kalokola F, Brejt J, Kataraihya J, et al. Heart failure, post-hospital mortality and renal function in Tanzania: A prospective cohort study. Int J Cardiol. 2017. Sep 15;243:311–7. 10.1016/j.ijcard.2017.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Peck RN, Wang RJ, Mtui G, Smart L, Yango M, Elchaki R, et al. Linkage to Primary Care and Survival After Hospital Discharge for HIV-Infected Adults in Tanzania: A Prospective Cohort Study. J Acquir Immune Defic Syndr. 2016. Dec 15;73(5):522–30. 10.1097/QAI.000000000001107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Meintjes G, Kerkhoff AD, Burton R, Schutz C, Boulle A, Van Wyk G, et al. HIV-Related Medical Admissions to a South African District Hospital Remain Frequent Despite Effective Antiretroviral Therapy Scale-Up. Medicine (Baltimore). 2015. Dec;94(50):e2269. 10.1097/MD.0000000000002269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ronny SF, Joaniter NI, Robert K, Bonnie W, Bruce K, James K, et al. Comparison of the prevalence of kidney disease by proteinuria and decreased estimated glomerular filtration rate determined using three creatinine-based equations among patients admitted on medical wards of Masaka Regional Referral Hospital in Uganda: a prospective study. BMC Nephrol. 2022. Jul 7;23(1):242. 10.1186/s12882-022-02865-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sendekie AK, Netere AK, Tesfaye S, Dagnew EM, Belachew EA. Incidence and patterns of adverse drug reactions among adult patients hospitalized in the University of Gondar comprehensive specialized hospital: A prospective observational follow-up study. PLoS One. 2023. Feb 24;18(2):e0282096. 10.1371/journal.pone.0282096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ibrahim AO, Shabi OM, Agbesanwa TA, Olowoyo P. Five-year analysis of clinical presentations and predictors of stroke mortality in rural Southwestern Nigeria: A retrospective observational study. Afr J Emerg Med. 2022. Mar;12(1):12–8. 10.1016/j.afjem.2021.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Moretti K, Uwamahoro DL, Naganathan S, Uwamahoro C, Karim N, Nkeshimana M, et al. Emergency medicine matters: epidemiology of medical pathology and changes in patient outcomes after implementation of a post-graduate training program at a Tertiary Teaching Hospital in Kigali, Rwanda. Int J Emerg Med. 2021. Jan 21;14(1):9. 10.1186/s12245-021-00331-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Burke RM, Henrion MYR, Mallewa J, Masamba L, Kalua T, Khundi M, et al. Incidence of HIV-positive admission and inpatient mortality in Malawi (2012-2019). AIDS. 2021. Nov 1;35(13):2191–9. 10.1097/QAD.0000000000003006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Agazhe M, Eshetu D, Arsicha A, Hamato A, Petros A, Dabaro D, et al. Incidence and pattern of stroke among patients admitted to medical ward at Yirgalem General Hospital, Sidama Regional State, Southern-Ethiopia. SAGE Open Med. 2021. Mar 15;9. 10.1177/20503121211001154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hertz JT, Sakita FM, Manavalan P, Madut DB, Thielman NM, Mmbaga BT, et al. The Burden of Hypertension and Diabetes in an Emergency Department in Northern Tanzania. Ethn Dis. 2019. Oct 17;29(4):559–66. 10.18865/ed.29.4.559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hertz JT, Sakita FM, Limkakeng AT, Mmbaga BT, Appiah LT, Bartlett JA, et al. The burden of acute coronary syndrome, heart failure, and stroke among emergency department admissions in Tanzania: A retrospective observational study. Afr J Emerg Med. 2019. Dec;9(4):180–4. 10.1016/j.afjem.2019.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Long LC, Fox MP, Sauls C, Evans D, Sanne I, Rosen SB. The High Cost of HIV-Positive Inpatient Care at an Urban Hospital in Johannesburg, South Africa. PLoS One. 2016. Feb 17;11(2):e0148546. 10.1371/journal.pone.0148546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stone GS, Aruasa W, Tarus T, Shikanga M, Biwott B, Ngetich T, et al. The relationship of weekend admission and mortality on the public medical wards at a Kenyan referral hospital. Int Health. 2015. Nov;7(6):433–7. 10.1093/inthealth/ihu100 [DOI] [PubMed] [Google Scholar]
- 62.Gizaw M, Harries AD, Ade S, Tayler-Smith K, Ali E, Firdu N, et al. Diabetes mellitus in Addis Ababa, Ethiopia: admissions, complications and outcomes in a large referral hospital. Public Health Action. 2015. Mar 21;5(1):74–8. 10.5588/pha.14.0107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ogunmola OJ, Olamoyegun MA. Patterns and outcomes of medical admissions in the accident and emergency department of a tertiary health center in a rural community of Ekiti, Nigeria. J Emerg Trauma Shock. 2014. Oct;7(4):261–7. 10.4103/0974-2700.142744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kazibwe A, Bisaso KR, Kyazze AP, Ninsiima S, Ssekamatte P, Bongomin F, et al. HIV, tuberculosis, diabetes mellitus and hypertension admissions and premature mortality among adults in Uganda from 2011 to 2019: is the tide turning? Trop Med Health. 2022. Aug 10;50(1):54. 10.1186/s41182-022-00447-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Roberts JS, Hahn EA, Black J, Maharaj R, Farley JE, Redd AD, et al. Determining the prevalence of tuberculosis in emergency departments in the Eastern Cape region of South Africa and the utility of the World Health Organization tuberculosis screening tool. S Afr Med J. 2021. Sep 2;111(9):872–8. [PubMed] [Google Scholar]
- 66.Iradukunda A, Odjidja EN, Ndayishima SK, Ngendakumana E, Ndayishimiye GP, Sinarinzi D, et al. Prevalence and predictive risk factors of hypertension in patients hospitalized in Kamenge Military hospital and Kamenge University teaching hospital in 2019: A fixed effect modelling study in Burundi. PLoS One. 2021. Dec 13;16(12):e0260225. 10.1371/journal.pone.0260225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ephraim RKD, Awuku YA, Tetteh-Ameh I, Baffe C, Aglagoh G, Ogunajo VA, et al. Acute kidney injury among medical and surgical in-patients in the Cape Coast Teaching Hospital, Cape Coast, Ghana: a prospective cross-sectional study. Afr Health Sci. 2021. Jun;21(2):795–805. 10.4314/ahs.v21i2.40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Pintye J, Ortblad KF, Mawandia S, Bakae O, Tau L, Grande M, et al. Frequent Detection of Undiagnosed HIV Within Emergency Departments in Botswana. Sex Transm Dis. 2021. Jul 1;48(7):e97–100. [DOI] [PubMed] [Google Scholar]
- 69.Mouton JP, Jobanputra N, Njuguna C, Gunter H, Stewart A, Mehta U, et al. Adult medical emergency unit presentations due to adverse drug reactions in a setting of high HIV prevalence. Afr J Emerg Med. 2021. Mar;11(1):46–52. 10.1016/j.afjem.2020.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mkoko P, Naidoo S, Niazi M, Tahira A, Godlwana X, Ndesi N, et al. The spectrum, prevalence and in-hospital outcomes of cardiovascular diseases in a South African district hospital: a retrospective study. Cardiovasc J S Afr. 2021. Sep-Oct 23;32(5):237–42. 10.5830/CVJA-2021-016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fiseha T, Ahmed E, Chalie S, Gebreweld A. Prevalence and associated factors of impaired renal function and albuminuria among adult patients admitted to a hospital in Northeast Ethiopia. PLoS One. 2021. Feb 4;16(2):e0246509. 10.1371/journal.pone.0246509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Rao A, Kennedy C, Mda P, Quinn TC, Stead D, Hansoti B. Patient acceptance of HIV testing services in rural emergency departments in South Africa. South Afr J HIV Med. 2020. Jul 22;21(1):1105. 10.4102/sajhivmed.v21i1.1105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Nkoke C, Noubiap JJ, Dzudie A, M Jingi A, Njume D, Teuwafeu D, et al. Epidemiology of hypertensive crisis in the Buea Regional Hospital, Cameroon. J Clin Hypertens (Greenwich). 2020. Nov;22(11):2105–10. 10.1111/jch.14035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Mulugeta H, Yehuala A, Haile D, Mekonnen N, Dessie G, Kassa GM, et al. Magnitude, risk factors and outcomes of stroke at Debre Markos Referral Hospital, northwest Ethiopia: a retrospective observational study. Egypt J Neurol Psychiatr Neurosurg. 2020;56(1):41–49. 10.1186/s41983-020-00173-4 [DOI] [Google Scholar]
- 75.Woyessa AH, Dibaba BY, Hirko GF, Palanichamy T. Spectrum, Pattern, and Clinical Outcomes of Adult Emergency Department Admissions in Selected Hospitals of Western Ethiopia: A Hospital-Based Prospective Study. Emerg Med Int. 2019. Aug 6;2019:1–10. 10.1155/2019/8374017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Sheikh AM, Rwegerera GM, Godman B, Habte D. Adjustments of medication dosages in patients with renal impairment in Botswana; findings and implications to improve patient care. Hosp Pract. 2019. Dec;47(5):231–40. 10.1080/21548331.2019.1685800 [DOI] [PubMed] [Google Scholar]
- 77.Nkoke C, Jingi AM, Makoge C, Teuwafeu D, Nkouonlack C, Dzudie A. Epidemiology of cardiovascular diseases related admissions in a referral hospital in the South West region of Cameroon: A cross-sectional study in sub-Saharan Africa. PLoS One. 2019. Dec 19;14(12):e0226644. 10.1371/journal.pone.0226644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nakalema I, Kaddumukasa M, Nakibuuka J, Okello E, Sajatovic M, Katabira E. Prevalence, patterns and factors associated with hypertensive crises in Mulago hospital emergency department; a cross-sectional study. Afr Health Sci. 2019. Mar;19(1):1757–67. 10.4314/ahs.v19i1.52 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mwenda V, Githuku J, Gathecha G, Wambugu BM, Roka ZG, Ong’or WO. Prevalence and factors associated with chronic kidney disease among medical inpatients at the Kenyatta National Hospital, Kenya, 2018: a cross-sectional study. Pan Afr Med J. 2019. Aug 23;33:321. 10.11604/pamj.2019.33.321.18114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Mocumbi AO, Cebola B, Muloliwa A, Sebastião F, Sitefane SJ, Manafe N, et al. Differential patterns of disease and injury in Mozambique: New perspectives from a pragmatic, multicenter, surveillance study of 7809 emergency presentations. PLoS One. 2019. Jul 10;14(7):e0219273. 10.1371/journal.pone.0219273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kalyesubula R, Mutyaba I, Rabin T, Andia-Biraro I, Alupo P, Kimuli I, et al. Trends of admissions and case fatality rates among medical in-patients at a tertiary hospital in Uganda; A four-year retrospective study. PLoS One. 2019. May 14;14(5):e0216060. 10.1371/journal.pone.0216060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hansoti B, Stead D, Eisenberg A, Mvandaba N, Mwinnyaa G, Patel EU, et al. A window into the HIV Epidemic from a South African emergency department. AIDS Res Hum Retroviruses. 2019. Feb;35(2):139–44. 10.1089/aid.2018.0127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Mchomvu E, Mbunda G, Simon N, Kitila F, Temba Y, Msumba I, et al. Diagnoses made in an emergency department in rural sub-Saharan Africa. Swiss Med Wkly. 2019. Feb 4;149(5-6):w20018. 10.4414/smw.2019.20018 [DOI] [PubMed] [Google Scholar]
- 84.Barak T, Neo DT, Tapela N, Mophuthegi P, Zash R, Kalenga K, et al. HIV-associated morbidity and mortality in a setting of high ART coverage: prospective surveillance results from a district hospital in Botswana. J Int AIDS Soc. 2019. Dec;22(12):e25428. 10.1002/jia2.25428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Evans RD, Hemmilä U, Craik A, Mtekateka M, Hamilton F, Kawale Z, et al. Incidence, aetiology and outcome of community-acquired acute kidney injury in medical admissions in Malawi. BMC Nephrol. 2017. Jan 14;18(1):21. 10.1186/s12882-017-0446-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Allain TJ, Aston S, Mapurisa G, Ganiza TN, Banda NP, Sakala S, et al. Age-Related Patterns of Disease and Mortality in Hospitalised Adults in Malawi. PLoS One. 2017. Jan 18;12(1):e0168368. 10.1371/journal.pone.0168368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.SanJoaquin MA, Allain TJ, Molyneux ME, et al. Surveillance Programme of IN-patients and Epidemiology (SPINE): implementation of an electronic data collection tool within a large hospital in Malawi. PLoS Medicine. 2013; 10(3):e1001400. 10.1371/journal.pmed.1001400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Eyo E, Philip-Ephraim E, Eyong KI, Oparah SK, Williams U, Udonwa N, et al. Profile of neurologic emergencies at the accident & emergency department of a tertiary hospital in south Nigeria. J Neurol Sci. 2013;30(1):72–80. [Google Scholar]
- 89.Kendig CE, McCulloch DJ, Rosenberg NE, Samuel JC, Mabedi C, Shores CG, et al. Prevalence of HIV and disease outcomes on the medical and surgical wards at Kamuzu Central Hospital, Lilongwe, Malawi. Trop Med Health. 2013. Dec;41(4):163–70. 10.2149/tmh.2013-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wachira BW, Wallis LA, Geduld H. An analysis of the clinical practice of emergency medicine in public emergency departments in Kenya. Emerg Med J. 2012. Jun;29(6):473–6. 10.1136/emj.2011.113753 [DOI] [PubMed] [Google Scholar]
- 91.Musung JM, Kakoma PK, Bugeme M, Banze JPM, Mukeng CK, Muyumba ON, et al. Risk Factors for Haemorrhagic Stroke among Adults in the Democratic Republic of the Congo: A Hospital-Based Study in a Limited Resource Setting. Stroke Res Treat. 2022. Nov 7;2022:1–7. 10.1155/2022/7840921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kakoma PK, Kadiebwe DM, Kayembe AM, Makonga PK, Bugeme M, Mukuku O. [Diabetic ketoacidosis in adults in Sendwe Hospital Lubumbashi: about 51 cases]. Pan Afr Med J. 2014. May 1;17:324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sheikh Hassan M, Osman Sidow N, Gökgül A, Ali Adam B, Farah Osman M, Hassan Mohamed H, et al. Pattern of neurological disorders among patients evaluated in the emergency department; cross-sectional study. Arch Acad Emerg Med. 2023. Jan 21;11(1):e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kemal LK, Shewaga TG, Sema FD. Drug-related hospital admissions and associated factors among adults admitted to Felege Hiwot comprehensive and specialized hospital, north west Ethiopia. J Environ Public Health. 2022. Mar 29;2022(6767488):6767488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Noor SK, Elmadhoun WM, Bushara SO, Ahmed MH. The changing pattern of hospital admission to medical wards: burden of non-communicable diseases at a hospital in a developing country. Sultan Qaboos Univ Med J. 2015. Nov 15(4):466–71. 10.18295/squmj.2015.15.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Biney EA, Oduro GD, Yar DD, Oppong CK, Nyame K, Forson PK, et al. HIV/AIDS prevalence at the accident & emergency centre of a tertiary and referral health institution in Ghana. Ghana Med J. 2015;49(4):220–6. 10.4314/gmj.v49i4.1 [DOI] [Google Scholar]
- 97.Anyanwu AC, Odeniyi IA, Fasanmade OA, Adewunmi AJ, Adegoke O, Mojeed AC, et al. Endocrine-related diseases in the emergency unit of a Tertiary Health Care Center in Lagos: A study of the admission and mortality patterns. Niger Med J. 2013. Jul;54(4):254–7. 10.4103/0300-1652.119651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Ogunmola OJ, Oladosu OY. Pattern and outcome of admissions in the medical wards of a tertiary health center in a rural community of Ekiti State, Nigeria. Ann Afr Med. 2014. Oct-Dec;13(4):195–203. 10.4103/1596-3519.142291 [DOI] [PubMed] [Google Scholar]
- 99.Adeloye D, Basquill C. Estimating the prevalence and awareness rates of hypertension in Africa: a systematic analysis. PLoS One. 2014. Aug 4;9(8):e104300. 10.1371/journal.pone.0104300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Duckitt R, Palsson R, Bosanska L, Dagna L, Durusu TM, Vardi M; CDIME group. Common diagnoses in internal medicine in Europe 2009: a pan-European, multi-centre survey. Eur J Intern Med. 2010. Oct;21(5):449–52. 10.1016/j.ejim.2010.06.012 [DOI] [PubMed] [Google Scholar]
- 101.National Diabetes Inpatient Audit England. 2019. Leeds: NHS Digital: 2019. Available from: https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-inpatient-audit/2019 [cited 2022 Dec 1].
- 102.Nieminen MS, Brutsaert D, Dickstein K, Drexler H, Follath F, Harjola VP, et al. ; EuroHeart Survey Investigators; Heart Failure Association, European Society of Cardiology. EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006. Nov;27(22):2725–36. 10.1093/eurheartj/ehl193 [DOI] [PubMed] [Google Scholar]
- 103.Savarese G, Becher PM, Lund LH, Seferovic P, Rosano GMC, Coats A. Global burden of heart failure: A comprehensive and updated review of epidemiology. Cardiovasc Res. 2023. Jan 18;118(17):3272–87. [DOI] [PubMed] [Google Scholar]
- 104.Kellett J, Deane B. The diagnoses and co-morbidity encountered in the hospital practice of acute internal medicine. Eur J Intern Med. 2007. Oct;18(6):467–73. 10.1016/j.ejim.2007.02.019 [DOI] [PubMed] [Google Scholar]
- 105.Verma AA, Guo Y, Kwan JL, Lapointe-Shaw L, Rawal S, Tang T, et al. Prevalence and Costs of Discharge Diagnoses in Inpatient General Internal Medicine: a Multi-center Cross-sectional Study. J Gen Intern Med. 2018. Nov;33(11):1899–904. 10.1007/s11606-018-4591-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Zhou B, Perel P, Mensah GA, Ezzati M. Global epidemiology, health burden and effective interventions for elevated blood pressure and hypertension. Nat Rev Cardiol. 2021. Nov;18(11):785–802. 10.1038/s41569-021-00559-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. ; GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018. Nov 10;392(10159):1736–88. 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Yuyun MF, Sliwa K, Kengne AP, Mocumbi AO, Bukhman G. Cardiovascular Diseases in Sub-Saharan Africa Compared to High-Income Countries: An Epidemiological Perspective. Glob Heart. 2020. Feb 12;15(1):15. 10.5334/gh.403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Damasceno A, Mayosi BM, Sani M, Ogah OS, Mondo C, Ojji D, et al. The causes, treatment, and outcome of acute heart failure in 1006 Africans from 9 countries. Arch Intern Med. 2012. Oct 8;172(18):1386–94. 10.1001/archinternmed.2012.3310 [DOI] [PubMed] [Google Scholar]
- 110.Sliwa K, Wilkinson D, Hansen C, Ntyintyane L, Tibazarwa K, Becker A, et al. Spectrum of heart disease and risk factors in a black urban population in South Africa (the Heart of Soweto Study): a cohort study. Lancet. 2008. Mar 15;371(9616):915–22. 10.1016/S0140-6736(08)60417-1 [DOI] [PubMed] [Google Scholar]
- 111.Agbor VN, Essouma M, Ntusi NAB, Nyaga UF, Bigna JJ, Noubiap JJ. Heart failure in sub-Saharan Africa: A contemporaneous systematic review and meta-analysis. Int J Cardiol. 2018. Apr 15;257:207–15. 10.1016/j.ijcard.2017.12.048 [DOI] [PubMed] [Google Scholar]
- 112.Amberbir A, Lin SH, Berman J, Muula A, Jacoby D, Wroe E, et al. Systematic Review of Hypertension and Diabetes Burden, Risk Factors, and Interventions for Prevention and Control in Malawi: The NCD BRITE Consortium. Glob Heart. 2019. Jun;14(2):109–18. 10.1016/j.gheart.2019.05.001 [DOI] [PubMed] [Google Scholar]
- 113.Fast-track: ending the AIDS epidemic by 2030. Geneva: UNAIDS; 2015. Available from: https://www.unaids.org/sites/default/files/media_asset/JC2686_WAD2014report_en.pdf [cited 2023 May 30].
- 114.Nguyen H, Manolova G, Daskalopoulou C, Vitoratou S, Prince M, Prina AM. Prevalence of multimorbidity in community settings: A systematic review and meta-analysis of observational studies. J Comorb 2019. Aug 22;9: 2235042X19870934. 10.1177/2235042X19870934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Violan C, Foguet-Boreu Q, Flores-Mateo G, Salisbury C, Blom J, Freitag M, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One. 2014. Jul 21;9(7):e102149. 10.1371/journal.pone.0102149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Resolution WHA76. 5. Strengthening diagnostics capacity. Seventy-sixth World Health Assembly, Geneva, 21–30 May 2023. Geneva: World Health Organization; 2023. Available from: https://apps.who.int/gb/ebwha/pdf_files/WHA76/A76_R5-en.pdf [cited 2023 Jun 27].
- 117.Fleming KA, Horton S, Wilson ML, Atun R, DeStigter K, Flanigan J, et al. The Lancet Commission on diagnostics: transforming access to diagnostics. Lancet. 2021. Nov 27;398(10315):1997–2050. 10.1016/S0140-6736(21)00673-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. WHO package of essential noncommunicable (PEN) disease interventions for primary health care. Geneva: World Health Organization; 2020. [Google Scholar]
- 119.Dehnavieh R, Haghdoost A, Khosravi A, Hoseinabadi F, Rahimi H, Poursheikhali A, et al. The District Health Information System (DHIS2): A literature review and meta-synthesis of its strengths and operational challenges based on the experiences of 11 countries. HIM J. 2019. May;48(2):62–75. 10.1177/1833358318777713 [DOI] [PubMed] [Google Scholar]
- 120.Agyepong IA, Sewankambo N, Binagwaho A, Coll-Seck AM, Corrah T, Ezeh A, et al. The path to longer and healthier lives for all Africans by 2030: the Lancet Commission on the future of health in sub-Saharan Africa. Lancet. 2017. Dec 23;390(10114):2803–59. 10.1016/S0140-6736(17)31509-X [DOI] [PubMed] [Google Scholar]
- 121.Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health. 2018. Nov;6(11):e1196–252. 10.1016/S2214-109X(18)30386-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Spencer S, Rylance J, Quint JK, Gordon SB, Dark P, Morton B. Prevalence of multimorbidity among hospitalised adults in sub-Saharan Africa: a systematic review [online repository]. Boston: Dataverse, The President & Fellows of Harvard College; 2023. 10.7910/DVN/EEQLNG 10.7910/DVN/EEQLNG [DOI]