Abstract
Background
Pre-eclampsia and eclampsia are the second-leading causes of maternal death. Health care providers have a critical role in preventing and managing these conditions. Lack of knowledge among healthcare providers on managing pre-eclampsia and eclampsia has been reported in other parts of Tanzania, but more information is needed in other parts of the country so as to design appropriate targeted interventions. Hence, this study assessed the knowledge and attitude of healthcare providers on the management of pre-eclampsia and eclampsia in the Mwanza region of Tanzania.
Method
A facility-based analytical cross-sectional study was conducted from April to May 2022 among 157 health care providers in the Mwanza region. A simple random sampling method was used to select districts and dispensaries, while a census method was used to recruit health care providers. A self-administered questionnaire was used for data collection. A descriptive statistics analysis was used to determine the distribution of background information of healthcare providers. Inferential statistics were used to determine the association between variables by using a chi-square test and logistic regression. A statistically significant variable in the final model was declared with a 95% confidence interval and a p-value of 0.05.
Results
The study results showed that only 40 (25%) of healthcare providers had adequate knowledge and 56.69% had positive attitude towards the management of pre-eclampsia and eclampsia. Knowledge was predicted by having more years of working experience (1–5 years) (AOR: 0.12, 95% CI 0.03–0.53, p-value 0.005) and working in a health center (AOR: 4.58, 95% CI 1.14–18.36, p-value 0.023). For attitude, no variable was significantly associated with it.
Conclusion
The study showed that the majority of the participants had inadequate knowledge of the management of pre-eclampsia or eclampsia, despite the positive attitude they possessed. This implies that HCP may be struggling to identify the signs and symptoms of the condition in pregnant women, and this could lead to delays in diagnosis despite believing that it is important to early diagnose the condition. To address this issue, it's crucial to invest in continuing medical education and training programs for healthcare providers to update their knowledge.
Keywords: pre-eclampsia and eclampsia, healthcare providers, knowledge, antenatal care, attitude, Tanzania, Mwanza
Introduction
Pre-eclampsia and eclampsia are hypertensive disorders of pregnancy that account for about 2% to 8% of pregnancy-related complications worldwide. It results in 9% to 26% of maternal deaths in low-income countries and 16% in high-income countries. According to the World Health Organization (WHO), the incidence of pre-eclampsia and eclampsia is seven times higher in developing countries (2.8% of live births) than in developed countries (0.4% of live births) (Olaoye et al., 2019)
Pre-eclampsia and eclampsia are among the top five leading causes of morbidity and mortality among women and babies in Sub-Saharan Africa (SSA). It is estimated that in Africa and Asia, nearly one-tenth of all maternal deaths are associated with hypertensive disorders of pregnancy. Tanzania is among the sub-Saharan African countries with a high maternal mortality rate (MMR) of 556 per 10,000 live births, contributing to the world's high MMR (National Bureau Statistics, 2016). The Tanzanian Demographic and Health Survey (TDHS) of the year 2015–2016 reported that 16% of MMR was due to pre-eclampsia and eclampsia. In the Mwanza region, eclampsia and severe pre-eclampsia accounted for about 26.2% of all deaths (Magoma et al., 2015).
Studies reported that the risk factors associated with pre-eclampsia are past history of pregnancy-induced hypertension, chronic kidney disease, type 1 and type 2 diabetes mellitus, low socioeconomic status, and a poor diet (low in vitamins C and E) (NICE, 2017; Soomro et al., 2019). The best time for identification and treatment of all these risk factors is during an antenatal care (ANC) visit, whereby a skilled healthcare provider (HCP) assesses pregnant women for risk and provides proper management of pregnancy related complications and prevention of concurrent disease (United Republic of Tanzania, 2018). Studies suggest that a large proportion of maternal deaths are due to poor quality preventive and promotional ANC services, missed or delayed diagnosis, and poor management of complications in pregnancy (Wolde et al., 2019).
Proper management requires the involvement of multi-professional expertise who have the up-to-date knowledge and attitude necessary to manage the woman with pre-eclampsia so as to reduce the effect of this disorder (Garti et al., 2021). Improper management, which was linked with inadequate knowledge of healthcare providers, has been reported in other parts of Tanzania (Joho et al., 2020). Moreover, there are limited studies targeting healthcare providers; most of the available studies have focused on the prevalence and contributing factors of pre-eclampsia and eclampsia. There is little understanding of HCP knowledge and attitude towards managing pre-eclampsia and eclampsia. Hence, the aim of this study was to assess the knowledge and attitude of HCP on managing pre-eclampsia and eclampsia during ANC in Mwanza Region, Tanzania.
Review of Literature
Knowledge and attitude of the HCP are among the important components of managing pre-eclampsia and eclampsia. Different studies have been conducted to assess the HCP knowledge and attitude towards managing pre-eclampsia and eclampsia. A study conducted in Kinshasa by Nkamba et al. (2020) about healthcare providers' knowledge as correlate of adequate diagnosis and management of pre-eclampsia revealed that 43.9% of the health care providers had adequate knowledge on management of pre-eclampsia and eclampsia. This varies with the descriptive cross-sectional study conducted in Nigeria by Olaoye et al. (2019) about knowledge, perception, and management of pre-eclampsia and eclampsia in a maternity hospital which reported the average knowledge of 64.2% and a positive attitude towards pre-eclampsia and eclampsia management.
Another study conducted in Bujumbura by (Ndirahisha et al., 2021) on the assessment of health personnel's knowledge, attitude, and practice regarding hypertension during pregnancy, which reported adequate knowledge of about 74% and positive attitude of about 96.9% of the HCP on management of pre-eclampsia and eclampsia. A study conducted in Moshi -Tanzania on evaluation of knowledge and management practices of hypertension in pregnancy among health care workers revealed that 18% of the HCP had adequate knowledge on how to manage hypertension during pregnancy according to the guidelines recommended by the WHO, and 50% had adequate knowledge according to the Tanzania guidelines (Liljevik & Lohre, 2012). Another study was conducted in Dodoma Tanzania on knowledge on prevention and management of pre-eclampsia and eclampsia among nurses in primary health care settings. Baseline Findings from an interventional study revealed that 51.2% of the HCP had adequate knowledge on management of pre-eclampsia and eclampsia (Joho et al., 2020). This is the same with the study conducted on management of pre-eclampsia and eclampsia in Dar es salaam-public health care facilities which reported 55% of the nurses as knowledgeable (Maembe & Pembe, 2015).
There is a limited number of published studies conducted on knowledge and attitude of pre-eclampsia management among healthcare providers. Moreover, most published studies were conducted in hospitals but few studies were conducted in health centers and dispensaries. Evidence suggests that knowledge is predicted by the availability of equipment while the low-level healthcare facilities mostly lack enough equipment. There is little understanding of HCP's knowledge and attitude towards managing pre-eclampsia and eclampsia during ANC in Mwanza Region, Tanzania, and this mark the aim of this study.
Methodology
Study Design and Study Population
This study was a hospital-based analytical cross-sectional design conducted from April to May 2022. Study participants were all licensed nurses, midwives, doctors, and clinical officers (who are medical doctor assistants with qualifications at diploma level) working in antenatal units and had an experience of 1 year and above. The study excluded the administrative HCP because they are not directly involved in providing antenatal care services. The study also excluded those who were on duty leave, as they were not available during the data collection.
Study Area and Settings
The study was conducted in the Mwanza region in the northern part of Tanzania. According to the 2012 national census, the region had a population of 2,772,509 and a pre-census projection of 3,771,067 (National Bureau of Statistics, 2016). It was the most densely populated region, with 293 people per square kilometer, of which 46.3 percent were women of reproductive age (15–49). The region has a total of seven districts, namely: Ilemela, Nyamagana, Kwimba, Magu, Misungwi, Sengerema, and Ukerewe. Generally, the region has a total of 369 health facilities that provide reproductive and child health services (Mwanza City Council, 2017). The region is reported to have a high maternal mortality rate of 305 per 100,000 live births (National Bureau Statistics, 2016); severe pre-eclampsia and eclampsia accounted for about 26.2% of all deaths (Magoma et al., 2015).
The study was conducted in three district hospitals, three health centers, and 18 dispensaries within the selected district councils. The dispensaries provide primary health care services, including all ANC services such as screening for pre-eclampsia. Health centers provide additional services such as delivery, laboratory, pharmacy, and minor operations. District hospitals provide second-line referral services, including basic surgery. All women with signs of severe pre-eclampsia seen in dispensaries are given pre-referral treatment and referred to the nearest health center or district hospital. On average, each ANC unit has 3–10 staff, which serves 5,679 people per month. The majority of the staff were nurses, followed by clinical officers and medical doctors.
Sample Size and Sampling Procedure
The minimum sample size (N) for this study was estimated by using the formula for finite population:
whereby n = sample size from infinite population formula, N = 4829 (Total number of HCP in Mwanza Region), n′ = required sample size, z = 1.96, e = 5% and p = 12% (knowledge of HCP on management of preeclampsia reported in Moshi (Liljevik & Lohre, 2012). Therefore, total number of 157 participants were recruited for this study.
Sampling Procedure

|
Data Collection Methods and Instruments
A self-administered questionnaire was used to collect information from HCP, while the observation method was used to assess the availability of medical supplies, equipment, and guidelines related to the management of pre-eclampsia and eclampsia. The knowledge questions were adapted from (Al-Rabeei, 2020), and the attitude questionnaire was adopted from (Olaoye et al., 2019). The questionnaires were modified for clarity. Before the actual data collection, a pilot study was conducted with 15 health care providers working in different regions to test the tools ability to obtain the needed information correctly All ambiguous questions were corrected. The reliability of the tool was tested with a crobanch coefficient of 0.7 for the knowledge tool and 0.72 for the attitude tool. The content's validity was assured through an extensive literature review.
Variable Measurement
Knowledge of pre-eclampsia and eclampsia was measured by eight items in a binary scale on whether HCP understood the immediate management of fits, its care, physical examination, recommended drugs, and prevention of drug toxicity. One point was awarded for the correct answer and a zero for the incorrect answer. The total score was 8, and those who scored more than 75% were considered to have adequate knowledge of the management of pre-eclampsia and eclampsia.
Attitude was measured by 12 Likert scale questions on the belief of HCP on the importance of each management of pre-eclampsia and eclampsia. Each response was scored using a five-point scale where 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, and 5 = strongly agree. The mean score was used to categorize those with positive and negative attitudes.
Data Analysis
The collected data were coded and entered into a Statistical Package for Social Science (SPSS) Version 25. Descriptive analysis was performed to describe the frequency distribution of background information of the respondents. Knowledge and attitude scores were computed to obtain total scores which later were categorized into adequate or inadequate knowledge and attitude as positive or negative attitude. A cross-tabulation was performed to assess the relationship between categorical variables using a Chi-square test. A logistic regression was used to determine significant association between variables. The level of significant was set at p-value of <0.05.
Results
Background Characteristics
The study comprises 157 participants with a response rate of 100%. Findings show that participants’ ages ranged from 20 to 59, with a mean age of 37.78 (SD 9.226). Most of the participants were female (77.1%). More than half of the participants 94 (59.9%) were working in dispensaries, and 54 (34.4%) were enrolled nurses. Less than half of 69 (43.9%) had a working experience of 11 years and above, 76 (48.4%) had attended on-the-job training related to the management of pre-eclampsia and eclampsia, and 42 (26.8%) of the training was conducted 6 months ago, but only 55 (35%) were satisfied with the training (Table 1).
Table 1.
Background Characteristics of Health Care Providers (N = 157).
| Variable | Frequency (n) | Percentage (%) |
|---|---|---|
| Age (Years) | ||
| 20–25 | 11 | 7.0 |
| 26–30 | 35 | 22.3 |
| 31and above | 111 | 70.7 |
| Gender | ||
| Female | 121 | 77.1 |
| Male | 36 | 22.9 |
| Cadre | ||
| Nurse midwife | 1 | 0.6 |
| Nurse officer | 18 | 11.5 |
| Assistant Nurse officer | 37 | 23.6 |
| Enrolled nurse | 54 | 34.4 |
| Clinical officer | 35 | 22.3 |
| Assistant medical officer | 2 | 1.2 |
| Medical doctor | 10 | 6.4 |
| Facility level | ||
| Dispensary | 94 | 59.9 |
| Health center | 30 | 19.1 |
| District hospital | 33 | 21.0 |
| Working experience (years) | ||
| 1–5 | 44 | 28.0 |
| 6–10 | 44 | 28.0 |
| 11 and above | 69 | 43.9 |
| Antenatal experience (years) | ||
| 1–5 | 84 | 53.5 |
| 6–10 | 49 | 31.2 |
| 11 and above | 24 | 15.3 |
| Worked in labor or Postnatal | ||
| Yes | 141 | 89.8 |
| No | 16 | 10.2 |
| Attended training on management of preeclampsia/eclampsia | ||
| Yes | 76 | 48.4 |
| No | 81 | 51.6 |
| Professional of the trainer | ||
| Medical doctor | 38 | 52.8 |
| Nurses | 26 | 36.1 |
| Team of doctors and nurses | 8 | 11.1 |
| Satisfaction of the training | ||
| Very satisfied | 55 | 75.0 |
| Somehow satisfied | 16 | 20.8 |
| Least satisfied | 1 | 1.4 |
| Not satisfied | 2 | 2.8 |
| Training period | ||
| Six months back | 14 | 19.4 |
| One year back | 12 | 16.7 |
| Two year back | 3 | 4.2 |
| More than 2 years back | 43 | 59.7 |
Proportion of HCP with Knowledge on Management of Pre-eclampsia and eclampsia
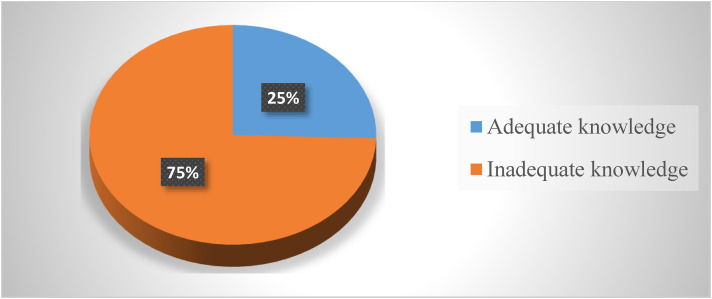
The result of this study showed that most of the participants 142 (90.4%) knew the recommended drug used to control convulsions, 133 (84.7%) knew the recommended intravenous fluid, and 106 (67.5%) knew the kind of physical examination needed after convulsions or fits. The frequency distribution of all items used to measure knowledge is found in Table 2. The knowledge score showed that the maximum score was 8 and the minimum score was 0. Only 40 (25%) were found to have adequate knowledge on the management of pre-eclampsia and eclampsia, and 117 (75%) had inadequate knowledge (Figure 1).
Table 2.
Frequency Distribution of Items Used to Measure Knowledge on Pre-eclampsia and Eclampsia (N = 157).
| Variable | Knowledge of Pre-eclampsia and Eclampsia | |
|---|---|---|
| Correct response n (%) |
Incorrect response n (%) |
|
| Immediate management during a fit (Shout for help, Ensure ABC) |
66 (42.0) | 91(58.0) |
| What care should be provided for a woman after a convulsion (Observe color and a need for oxygen) |
31(19.7) | 126(80.3) |
| What kind of physical examination is needed after convulsions/fits (Vital sign, fetal heart rate) |
106(67.5) | 51(32.5) |
| What is the recommended intravenous line for managing eclampsia? (Ringer lactate) | 133(84.7) | 24(15.3) |
| What is the recommended drug used to control convulsions in management of eclampsia? (MgSo4) | 142(90.4) | 15(9.6) |
| What is the prevention of toxicity of the drug selected in question 5. (Assess respiration, patellar and urine output) | 60(38.2) | 97(61.8) |
| What are the immediate measures in case the toxicity of the drug is selected in question 5? (Withhold drug and calcium gluconate) |
65(41.4) | 92(58.6) |
| Others management of eclampsia includes (Monitor urine output, do bedside clotting test) | 76(48.4) | 81(51.6) |
Figure 1.
Proportion of health care providers with knowledge of managing preeclampsia and eclampsia (N = 157).
Predictors of Knowledge on the Management of Pre-eclampsia and Eclampsia
A chi-square test was initially performed, and the results showed that knowledge was significantly associated with working facility level (p-value = 0.01), working experience (p-value = 0.012), and antenatal working experience (p-value = 0.001) (Table 3).
Table 3.
Relationship Between Knowledge and Background Characteristics (N = 157).
| Variable | Knowledge level | χ2 | p-value | |
|---|---|---|---|---|
| Adequate knowledge n (%) | Inadequate knowledge n (%) | |||
| Age groups | ||||
| 20–25 | 1(9.1) | 10(90.9) | 2.033 | 0.361 |
| 26–30 | 8(22.9) | 27(77.1) | ||
| 31and above | 31(27.9) | 80(72.1) | ||
| Gender | ||||
| Female | 34(28.1) | 87(71.9) | 1.910 | 0.167 |
| Male | 6(16.7) | 30(83.3) | ||
| Cadre | ||||
| Nurse midwife | 0(0.0) | 1(100) | 6.086 | 0.414 |
| Nurse officer | 8(44.4) | 10(55.6) | ||
| Assistant nurse officer | 7(18.9) | 30(81.1) | ||
| Enrolled nurse | 15(27.8) | 39(72.2) | ||
| Clinical officer | 7(20.0) | 28(80.0) | ||
| Assistant medical officer | 0(0.0) | 2(100) | ||
| Medical doctor | 3(30.0) | 7(70.0) | ||
| Working Facility level | ||||
| Dispensary | 32(34.0) | 62(66.0) | 9.270 | 0 . 010 |
| Health Center | 3(10.0) | 27(90.0) | ||
| District hospital | 5(15.2) | 28(84.8) | ||
| Working experience | ||||
| 1–5years | 4(9.1) | 40(90.9) | 8.849 | 0 . 012 |
| 6–10years | 13(29.5) | 31(70.5) | ||
| 11 and above | 23(33.3) | 46(66.7) | ||
| Antenatal experience (years) | ||||
| 1–5 | 12(14.3) | 72(85.7) | 14.472 | 0 . 001 |
| 6–10 | 16(32.7) | 33(67.3) | ||
| 11 and above | 12(50.0) | 12(50.0) | ||
| Worked in labor or postnatal | ||||
| Yes | 37(26.2) | 104(73.8) | 0.425 | 0.515 |
| No | 3(18.8) | 13(81.2) | ||
| Attended on job training | ||||
| Yes | 24(31.6) | 52(68.4) | 2.888 | 0.089 |
| No | 16(19.8) | 65(80.2) | ||
| Professional of the trainer | ||||
| Medical doctor | 6(15.8) | 32(84.2) | 8.136 | 0 . 017 |
| Nurses | 9(34.6) | 17(65.4) | ||
| Team of doctors and nurses | 5(62.5) | 3(37.5) | ||
| Satisfaction of the training | ||||
| Very satisfied | 13(24.1) | 41(75.9) | 4.855 | 0.183 |
| Somehow satisfied | 6(40.0) | 9(60.0) | ||
| Least satisfied | 1(100) | 0(0.0) | ||
| Not satisfied | 0(0.0) | 2(100) | ||
| Training conducted | ||||
| Six months back | 3(21.4) | 11(78.6) | 1.556 | 0.669 |
| One year back | 2(16.7) | 10(83.3) | ||
| Two years back | 1(33.3) | 2(66.7) | ||
| More than 2 years back | 14(32.6) | 29(67.4) | ||
| Availability of equipment and supplies | ||||
| Adequate equipment | 4(30.8) | 9(69.2) | 0.410 | |
| Inadequate equipment and supplies | 2(18.2) | 9(81.8) | ||
Multiple Logistic Regression Model
In multiple logistic regression model, results showed that, those health care providers who work in health centers were 4.5 times more likely to have adequate knowledge compared to those who were working in dispensary (AOR: 4.58, 95%CI 1.146–18.363, p-value 0.023). And HCP who have working experience of 1–5 years were less likely to have adequate knowledge by 88% compared to those who had working experience of 11 years and above (AOR: 0.129, 95%CI 0.031–0.531, p-value 0.005) (Table 4)
Table 4.
Predictors of HCP Knowledge on Managing Pre-eclampsia and Eclampsia (N = 157).
| Variable | 95% C.I. | p-value | AOR | 95% C.I | p-value | |||
|---|---|---|---|---|---|---|---|---|
| COR | Lower | Upper | Lower | Upper | ||||
| Gender | ||||||||
| Male | Ref. | |||||||
| Female | 0.512 | 0.196 | 1.339 | 0.172 | 0.772 | 0.227 | 2.621 | 0.678 |
| Working Facility level | ||||||||
| Dispensary | Ref. | |||||||
| Health Center | 0.516 | 0.337 | 0.791 | 0 . 002 | 4.586 | 1.146 | 18.363 | 0 . 023 |
| District hospital | 0.179 | 0.069 | 0.462 | <0.001 | 2.516 | 0.485 | 13.068 | 0.272 |
| Working experience | ||||||||
| 1–5 years | 0.200 | 0.064 | 0.627 | 0 . 006 | 0.129 | 0.031 | 0.531 | 0 . 005 |
| 6–10 years | 0.839 | 0.370 | 1.901 | 0.674 | 0.530 | 0.214 | 1.314 | 0.170 |
| 11 and above | Ref. | |||||||
| Antenatal experience | ||||||||
| 1–5 years | 0.167 | 0.061 | 0.456 | <0.001 | 0.346 | 0.090 | 1.324 | 0.121 |
| 6–10 years | 0.485 | 0.179 | 0.316 | 0.155 | 0.494 | 0.147 | 1.660 | 0.254 |
| 11 and above | Ref. | |||||||
| On job training | ||||||||
| Yes | 1.875 | 0.903 | 3.891 | 0.092 | 2.013 | 0.917 | 4.422 | 0.081 |
| No | Ref. | |||||||
Health Care Providers’ Response to the Question Related to Attitude
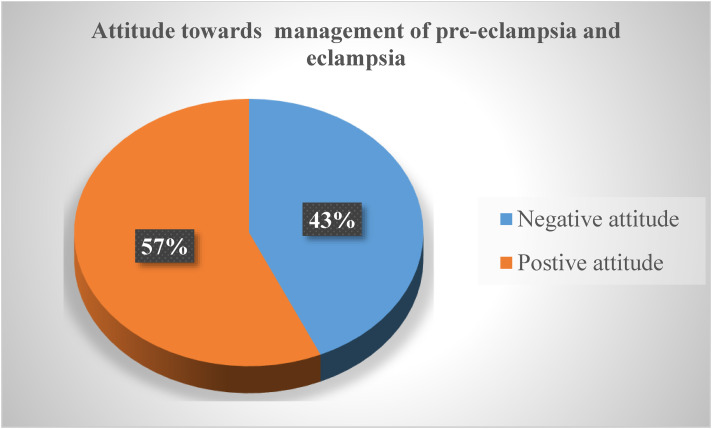
The result of this study showed that the majority of the participants 145(92.4%) strongly agreed that they think it is mandatory to check blood pressure for every pregnant mother in each antenatal visit, while 140 (89.2%), strongly agreed that it is important to initiate hypertensive treatment for pregnant mothers with blood pressure above 160/110 mmHg. However, only 16 (10.2%), strongly agreed that young women are susceptible to pre-eclampsia. The frequency distribution of all items used to measure attitude is found in Table 5. The knowledge score showed that the maximum score was 8 and the minimum score was 0. The attitude question score ranged from 26 to 60, with a total score of 60 and a mean score of 49.4. About 89 (57%) had a positive attitude toward the management of preeclampsia and eclampsia, and 68 (43%) had a negative attitude toward the management of preeclampsia (Figure 2).
Table 5.
The Attitude Analysis of Health Care Providers on Managing Pre-eclampsia and Eclampsia (N = 157).
| Variable | Strongly disagree n (%) | Disagree n (%) |
Neutral n (%) | Agree n (%) | Strongly agree n (%) |
|---|---|---|---|---|---|
| I believe checking of blood pressure for every pregnant mother in each ANC visit is mandatory | 3 (1.9) | 0 (0.0) | 2 (1.3%) | 7 (4.5) | 145 (92.3) |
| I think we should test proteinuria for all pregnant woman during ANC | 6 (3.8) | 9 (5.7) | 1 (0.6) | 28 (17.8) | 113 (72.0) |
| I believe proteinuria is always a sign of pre-eclampsia | 4 (2.5) | 2 (1.3) | 4 (2.5) | 29 (18.5) | 118 (75.2) |
| I believe it is important to initiate hypertensive treatment for pregnant mother with the blood pressure above 160/110mmHg | 2 (1.3) | 1(0.6) | 3 (1.9) | 11 (7.0) | 140 (89.2) |
| I believe an Up to date training will improve the knowledge and management practices of health care providers on pre-eclampsia | 2 (1.3) | 3 (1.9) | 3 (1.9) | 19 (12.1) | 130 (82.8) |
| I believe mean arterial BP is appropriate in diagnosing high BP | 2 (1.3) | 10 (6.4) | 18 (11.5) | 28 (17.8) | 99 (63.0) |
| I believe Methyldopa is the drug of choice on treating a hypertension during pregnancy | 1 (0.6) | 5 (3.2) | 4 (2.5) | 28 (17.8) | 119 (75.8) |
| I believe it is the duty all health care provider and pregnant women to prevent pre-eclampsia | 40 (25.5) | 27 (17.2) | 3 (1.9) | 19 (12.1) | 68 (43.3) |
| I believe eclampsia is always treated with magnesium sulphate | 6 (3.8) | 10 (6.3) | 7 (4.5) | 29 (18.5) | 105 (66.9) |
| I believe Preeclampsia can be prevented | 3 (1.9%) | 7 (4.5) | 0 (0.0) | 28 (17.8) | 119 (75.8) |
| I believe young women are susceptible to Pre-eclampsia | 72 (45.9) | 43 (27.4) | 10 (6.4) | 16 (10.2) | 16 (10.2) |
| I believe convulsion during pregnancy can be hereditary | 45 (28.6) | 64 (40.8) | 0 (0.0) | 22 (14.0) | 16 (16.6) |
Figure 2.
Proportion of health care provider with attitude on managing pre-eclampsia and eclampsia (N = 157).
Relationship Between Attitude and Background Characteristics
The chi-square test was conducted to assess the relationship between attitude of HCP and background information, the findings revealed that there is no statistical significant relationship between background variable and attitude of HCP.
Discussion
The main objective of this study was to assess whether the HCPs working in ANC have knowledge and positive attitudes toward managing pre-eclampsia and eclampsia. Knowledge and positive attitude of HCP are essential components for proper management of a client as they improve the quality of care, prevent complications and reduce mortality rate related to preeclampsia and eclampsia (Isangula et al., 2022) Developing a positive attitude that leads to proper practice also requires knowledge acquisition (Dvorak, 2017).
Despite positive attitude of HCP towards management of pre-eclampsia and eclampsia, a large proportion have a low understanding of the essential knowledge items assessed. The reason behind this low knowledge could possibly be due to a lack of on-the-job training, as it is indicated in this study that about half of the HCP had never attended any on-the-job training. On-the-job training acts as a reminder of information related to the management of preeclampsia and eclampsia. Literature also supports that on-the-job training improves knowledge of HCP (Bafaneli & Setibi, 2015; Gadalla & Mukhtad, 2021).
Our study finding are similar to what is reported in Pakistan (knowledge and routine management of pre-eclampsia), Egypt (Ahmed et al., 2017), Yemen (Al-Rabeei, 2020) and in Moshi, Tanzania, (Liljevik & Lohre, 2012) that HCPs lacked knowledge of the basic steps on managing pre-eclampsia and eclampsia. However, the current findings were inconsistent with what is reported (Nkamba et al., 2020; Olaoye et al., 2019) who reported HCP have an adequate knowledge on managing pre-eclampsia/eclampsia. The difference might be due to the nature of the study population, as the previous studies employed physicians and other professionals with higher education levels, while in the current study, the population consisted of nurses, medical doctors, nurse officers, midwives, and clinical officers. Also, the majority of the participants attended on-the-job training, while in the current situation, the majority were enrolled nurses, and a few attended on-the-job training.
On the part of predictors that contribute to the low knowledge of HCs, our findings reported that working experience of 1–5 years and working in a health center have higher odds of having low knowledge. This might be due to the fact that working experience is part of the learning process that someone undergoes with daily practice; in this way, it can be concluded that experience fosters knowledge, so those with short working periods could possibly have low knowledge. As supported in the literature, the first 5 years of clinical experience provide health care providers with abundant learning opportunities as they are exposed to a variety of successful and unsuccessful clinical experiences from which they gain new knowledge (Takase, 2013). Moreover, health care providers who were working in health centers had adequate knowledge compared to those who were working in dispensaries. The reason for this might be due to the available working system, as most of the dispensaries refer complicated cases to higher levels, and as a result, the HCPs working in health centers have more exposure to case management.
Similar findings have been reported in Yemen (Al-Rabeei, 2020), where they reported experience as the predictor of knowledge. On the other hand, the current findings are different from the findings of the study conducted in Dodoma, Tanzania, by (Joho et al., 2020), where they found that educational preparation is a key predictor of nurse's knowledge.
Conclusion
Based on the findings of this study, it is concluded that the majority of the HCPs had inadequate knowledge on the management of pre-eclampsia or eclampsia, despite the positive attitude they possess. The predictors of knowledge were working experience of more than 10 years and working in a higher health facility level. Thus, the study identifies the need to support junior health care providers who have fewer years of working experience in their practice and encourage regular shifts of HCPs from higher health facility level to lower healthcare facilities so that they can infuse knowledge into those working at lower levels.
Recommendations
Hospital administration should make sure that they have a planned program for providing on-the-job training about management of pre-eclampsia and eclampsia, and should encourage all HCP to attend the training. There is a need to ensure proper allocation of the staff with adequate qualifications in ANC units and provide additional training to enrolled nurses (assistant nurses) before task-shifting to them. The hospital administration should encourage a regular shift of HCP from higher to lower healthcare facilities so that they can infuse knowledge into those working at lower levels.
Strengths
This study made a comprehensive assessment of HCP working in all levels of health care facilities for the management of pre-eclampsia and eclampsia, thus giving a complete picture of the type of services provided for the management of pre-eclampsia and eclampsia at all healthcare facility levels. Moreover, the response rate for this study was 100%.
Limitations
The study was conducted in one region of Tanzania; therefore, these results cannot be generalized to all HCPs in Tanzania.
Implication of the Results to Practice
This study showed HCP have inadequate knowledge despite positive attitude towards management of pre-eclampsia and eclampsia. This implies that HCP may be struggling to identify the signs and symptoms of the condition in pregnant women, and this could lead to delays in diagnosis despite believing that it is important to early diagnose the condition. But the lack of knowledge could also impact the appropriate initiation of treatments, such as magnesium sulfate for seizure prevention, blood pressure control, and timely delivery of the baby, which are crucial to preventing complications. Moreover, they may fail to identify individuals at high risk and implement preventive measures early. To address this issue, it's crucial to invest in continuing medical education and training programs for healthcare providers to update their knowledge on pre-eclampsia management. This can help improve patient outcomes and minimize the associated risks of this condition.
Acknowledgments
We would like to acknowledge all health care facilities in which the study was conducted and all healthcare providers who participated in the study. We would also extend our appreciation to the administrative authority of Mwanza Region for allowing us to conduct research. Our appreciation also goes to staff from the University of Dodoma, particularly the College of Health Sciences for assisting in shaping the study.
Appendix 1: Questionnaire
Questionnaire Number
Date of Interview
Instructions:
For multiple choice questions Encircle the correct option
For short answers questions, Fill the answer on the dotted line provided
Part I: Background Characteristics
Name of health facility………………………………
- Facility level
- (a) Dispensary
- (b) Health center
- (c) District hospital
- (d) Regional hospital
- What is your cadre?
- Nurse midwife
- Nurse Officer
- Assistant nurse officer
- Enrolled nurse
- Clinical officer
- Assistant Medical Officer
- Medical Doctor
- Specialist (Obs/Gyn)
How old are you ………………….?
- Your gender
- (a) Female
- (b) Male
Years of working experience …………………..
How long have you been working in the antenatal unit………………………?
- Have you ever worked in labor or postnatal ward?
- (a) Yes
- (b) No
- Since you have worked in antenatal unit have you attended training on pre-eclampsia/eclampsia?
- (c) Yes
- (d) No
If yes who was the trainer (professional)……………………
- Where are you satisfied with the training?
- Very satisfied
- Somehow satisfied
- Least satisfied
- Not satisfied
- When was the training conducted?
- Six months’ back
- One-year back
- Two years’ back
- More than 2 years back…………………….
PART II
A. Knowledge of Health Care Provider on Managing pre-Eclampsia/Eclampsia
-
What are the immediate managements during fit?
…………………………………………………………………………………………
-
What care should be provided for a woman after convulsion?
…………………………………………………………………………………………
-
What kind of assessment which is needed after convulsions/fits?
…………………………………………………………………………………………
-
The recommended intravenous line for managing eclampsia is
…………………………………………………………………………………………
-
The recommended drug used to control convulsion in management of eclampsia
…………………………………………………………………………………………
-
What is the prevention of toxicity of drug selected in question 5?
…………………………………………………………………………………………
-
What are the immediate measures in case the toxicity of the drug selected in question 5 happens?
…………………………………………………………………………………………
-
Others management of eclampsia includes
…………………………………………………………………………………………
B. Attitude of Health Care Provider on Managing Pre-Eclampsia/Eclampsia
| Variable | Strongly Agree 5 |
Agree 4 |
Neutral 3 |
Disagree 2 |
Strongly disagree 1 |
|---|---|---|---|---|---|
| I believe checking of blood pressure for every pregnant mother in each ANC visit is mandatory | |||||
| I think we should test proteinuria for all pregnant woman during ANC | |||||
| I believe proteinuria is always a sign of pre-eclampsia | |||||
| I believe it is important to initiate hypertensive treatment for pregnant mother with the blood pressure above 160/110 mmHg | |||||
| I believe an Up to date training will improve the knowledge and management practices of health care providers on pre-eclampsia | |||||
| I believe mean arterial BP is appropriate in diagnosing high BP | |||||
| I believe Methyldopa is the drug of choice on treating a hypertension during pregnancy | |||||
| I believe it is the duty all health care provider and pregnant women to prevent pre-eclampsia | |||||
| I believe eclampsia is always treated with magnesium sulphate | |||||
| I believe pre-eclampsia can be prevented | |||||
| I believe young women are susceptible to pre-eclampsia | |||||
| I believe checking of blood pressure for every pregnant mother in each ANC visit is mandatory |
Footnotes
Author Contributions: AS conceived the concept study, SAS and AS designed the study design, AS did the data collection. SAS and AS did the data analysis and interpretation. AS wrote the manuscript text. All authors reviewed the manuscript and accept for submission.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article
ORCID iDs: Anna Sangito Pallangyo https://orcid.org/0000-0001-7779-0782
Saada Ali Seif https://orcid.org/0000-0001-6079-7646
References
- Ahmed S. S., Helmy H. K., Mohamed A. A. (2017). Impact of a tailored intensive educational program upon preeclampsia on nurses’ knowledge at Beni-Suef City, Egypt. International Journal of Nursing Science, 7(4), 79–83. 10.5923/J.NURSING.20170704.01 [DOI] [Google Scholar]
- Al-Rabeei N. (2020). Competences of midwives toward management of eclampsia at public hospitals in Sana’a City-Yemen. Al-Razi University Journal for Medical Sciences, 4(1), 28–36. 10.51610/RUJMS4.1.2020.79 [DOI] [Google Scholar]
- Bafaneli S., Setibi G. (2015). The impact of on-the-job training on employee performance: The case of Riley’s hotel. Journal of Business Theory and Practice, 3(2), 239. 10.22158/JBTP.V3N2P239 [DOI] [Google Scholar]
- Dvorak D. (2017). The 4 factors of learning—Knowledge, attitudes, skills, and habits (KASH). The# 1 Motivational Guide.
- Gadalla R. M., Mukhtad A. A. (2021). The effect of training programs on the performance of healthcare workers at Benghazi Medical Center (BMC). Libyan Journal of Dentistry , 5(2), 16–24. https://journals.uob.edu.ly/LJD/article/view/1745 [Google Scholar]
- Garti I., Gray M., Tan J. Y., Bromley A. (2021). Midwives’ knowledge of pre-eclampsia management: A scoping review. Women and Birth : Journal of the Australian College of Midwives, 34(1), 87–104. 10.1016/J.WOMBI.2020.08.010 [DOI] [PubMed] [Google Scholar]
- Isangula, K., Mbekenga, C., Mwansisya, T., Mwasha, L., Kisaka, L., Selestine, E., Siso, D., Rutachunzibwa, T., Mrema, S., & Pallangyo E. (2022). Healthcare providers’ experiences with a clinical mentorship intervention to improve reproductive, maternal and newborn care in Mwanza, Tanzania. Frontiers in Health Services, 2(5), 792909. 10.3389/frhs.2022.792909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joho A., Kibusi S., Ernest A. (2020). Knowledge on prevention and management of preeclampsia and eclampsia among nurses in primary health settings: Baseline findings from an interventional study in Dodoma Region, Tan…July. 10.24248/eahrj.v4i1.619 [DOI] [PMC free article] [PubMed]
- Liljevik S., Lohre E. S. V. B. (2012). Evaluation of knowledge and management practices of hypertension in pregnancy among health care workers in Moshi urban, Tanzania . 1–41.
- Maembe L. E., Pembe A. B. (2015). Managing pre-eclampsia and eclampsia in Dar es Salaam public health facilities: A focus on equipment, supplies, drugs and knowledge of healthcare workers. Tanzania Medical Journal, 27(1), 43–54. 10.4314/tmj.v27i1.192 [DOI] [Google Scholar]
- Magoma M., Massinde A., Majinge C., Rumanyika R., Kihunrwa A., Gomodoka B. (2015). Maternal death reviews at Bugando hospital north-western Tanzania: A 2008-2012 retrospective analysis. BMC Pregnancy and Childbirth, 15(1), 1–7. 10.1186/S12884-015-0781-Z/TABLES/2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ministry of Finance, National Bureau of Statistics and Mwanza City Council National Bureau of Statistics Mwanza City Council Dar es Salaam Mwanza Region. (2017).
- National Bureau Statistics. (2016). Tanzania demographic and health survey and malaria indicator survey 2015-2016 - final report [FR321] | enhanced reader. Report.
- Ndirahisha E., Nyandwi J., Manirakiza S., Barasukana P., Nahayo H., Baransaka E. (2021). Assessment of knowledges, attitudes, and practices of health personnel with regard to hypertension during pregnancy in Hospitals of Bujumbura. Indian Journal of Clinical Cardiology, 3(1), 12–15. 10.1177/26324636211003448 [DOI] [Google Scholar]
- NICE (2017). Overview | Hypertension in pregnancy: diagnosis and management | Guidance | NICE. (n.d.).
- Nkamba D. M., Vangu R., Elongi M., Magee L. A., Wembodinga G., Bernard P., Ditekemena J., Robert A. (2020). Health facility readiness and provider knowledge as correlates of adequate diagnosis and management of pre-eclampsia in Kinshasa, Democratic Republic of Congo. BMC Health Services Research, 20(1), 1–13. 10.1186/s12913-020-05795-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olaoye T., Oyerinde O. O., Elebuji O. J., Ologun O. (2019). Knowledge, perception and management of pre-eclampsia among health care providers in a maternity hospital. International Journal of MCH and AIDS (IJMA), 8(2), 80–88. 10.21106/ijma.275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soomro S., Kumar R., Lakhan H., Shaukat F. (2019). Risk factors for pre-eclampsia and eclampsia disorders in tertiary care center in Sukkur, Pakistan. Cureus, 11(11). 10.7759/CUREUS.6115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takase M. (2013). The relationship between the levels of nurses’ competence and the length of their clinical experience: A tentative model for nursing competence development. Journal of Clinical Nursing, 22(9–10), 1400–1410. 10.1111/J.1365-2702.2012.04239.X [DOI] [PubMed] [Google Scholar]
- United Republic of Tanzania. (2018). Antenatal care guidelines. MoHCDGEC. [Google Scholar]
- Wolde H. F., Tsegaye A. T., Sisay M. M. (2019). Late initiation of antenatal care and associated factors among pregnant women in Addis Zemen primary hospital, South Gondar, Ethiopia. Reproductive Health, 16(1), 1–8. 10.1186/S12978-019-0745-2/TABLES/4 [DOI] [PMC free article] [PubMed] [Google Scholar]