Abstract
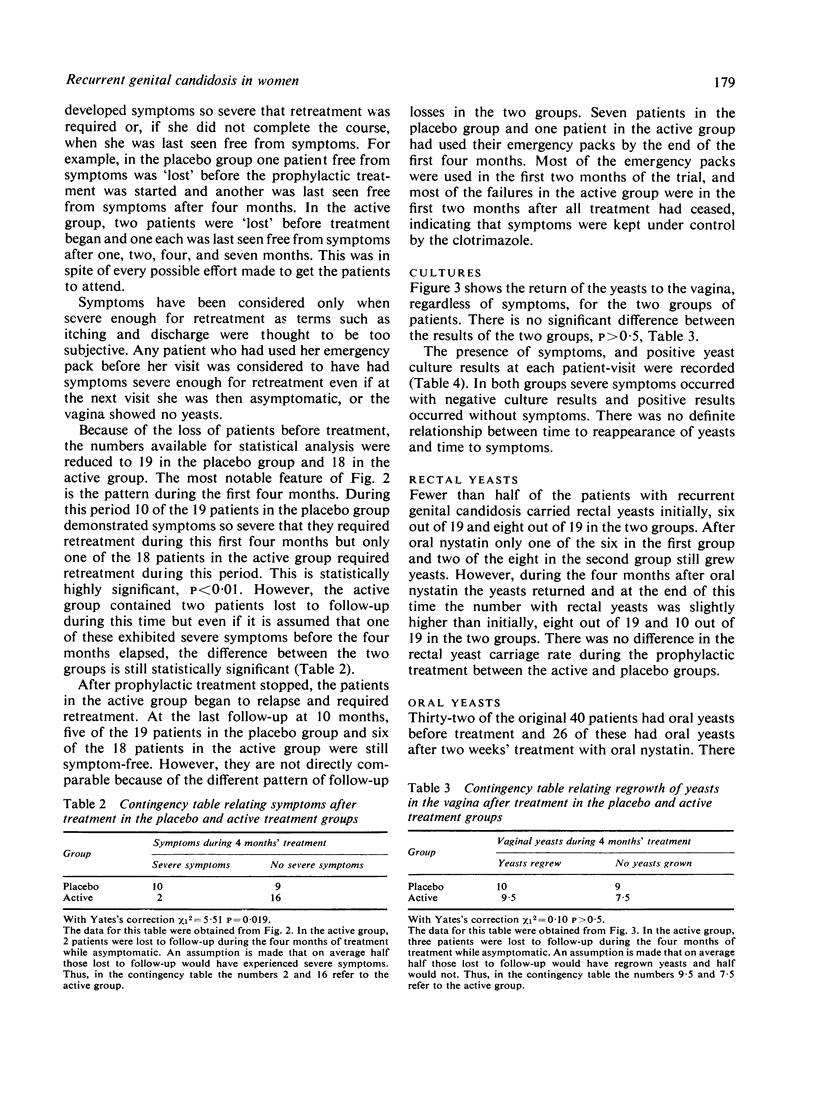
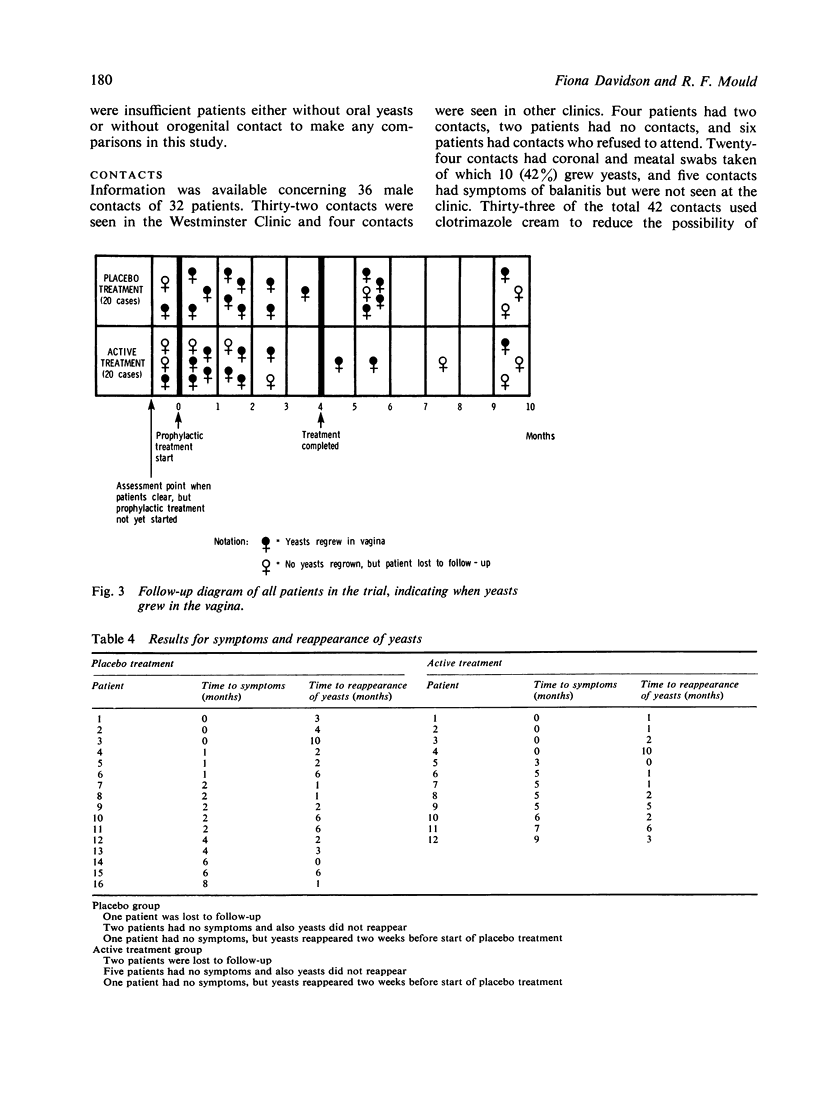
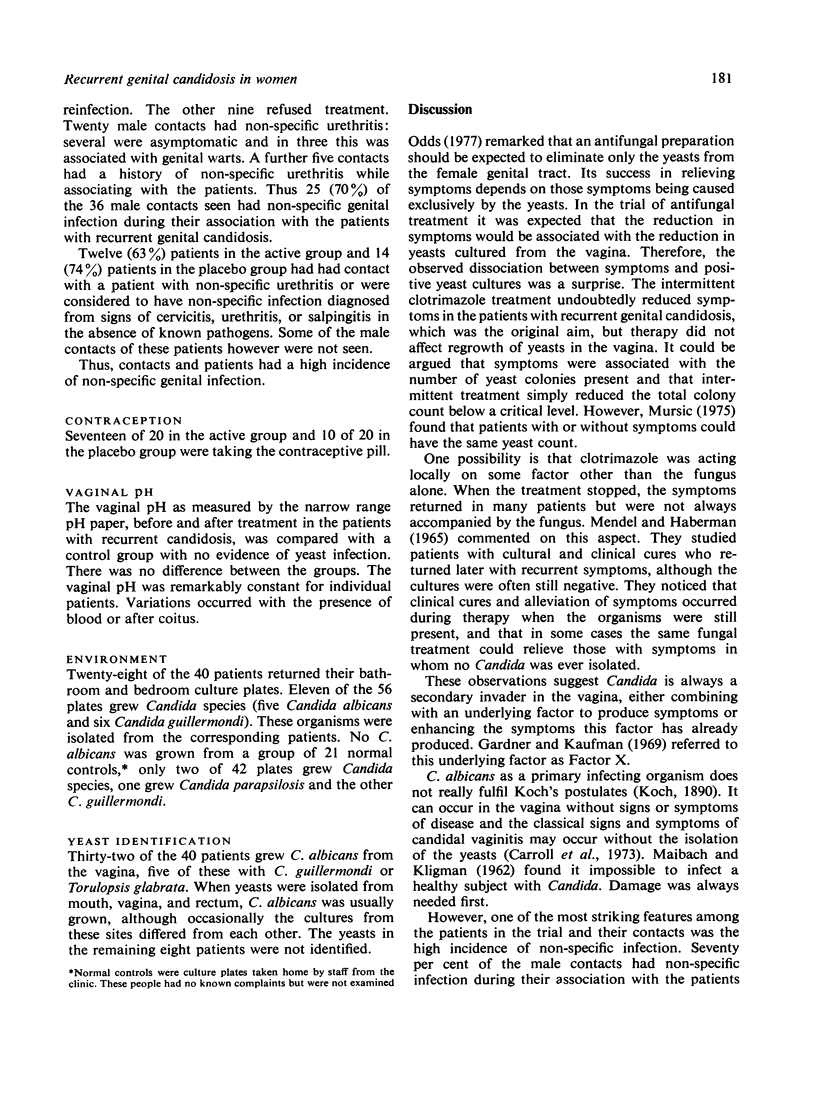
A study of clotrimazole for the treatment of recurrent genital candidosis unexpectedly showed that symptoms and infection can be dissociated. The aim of the study was to see if intermittent antifungal treatment would reduce symptoms in women constantly distressed by recurrent genital candidosis. Forty women seriously affected by the condition were initially given oral and local antifungal treatment. When the patients were symptom-free and the vagina was free of yeasts, they were entered into a double-blind clinical trial and were treated prophylactically for four months with either intermittent clotrimazole pessaries and cream or a placebo. The prophylactic treatment kept symptoms below a critical level but did not affect the return of the yeasts to the vagina. This dissociation between symptoms and vaginal yeasts was unexpected. Rectal yeast carriage was unaffected by prophylactic vaginal treatment. Male contacts and patients both showed a high incidence of non-specific genital infection. This association has seldom been reported. A few patients cultured yeasts from their homes but this environment was not considered a major source of reinfection. The vaginal pH did not appear to be altered by the presence of yeasts. The results of the study suggested that symptoms in women with recurrent genital candidosis were not caused by yeasts alone, and possibly the reason for recurrences might lie not in constant reinfection by yeasts, but in failure to recognise and remove a primary underlying factor, perhaps infection with other sexually transmitted agents. The question of a synergistic action between yeasts and other organisms is discussed.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bull M. J. Wearing tights. Br Med J. 1969 Jan 11;1(5636):120–120. doi: 10.1136/bmj.1.5636.120-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll C. J., Hurley R., Stanley V. C. Criteria for diagnosis of candida vulvovaginitis in pregnant women. J Obstet Gynaecol Br Commonw. 1973 Mar;80(3):258–263. doi: 10.1111/j.1471-0528.1973.tb02195.x. [DOI] [PubMed] [Google Scholar]
- Cohen L. Influence of pH on vaginal discharges. Br J Vener Dis. 1969 Sep;45(3):241–247. doi: 10.1136/sti.45.3.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson F. Yeasts and circumcision in the male. Br J Vener Dis. 1977 Apr;53(2):121–122. doi: 10.1136/sti.53.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desmond F. B., Eastcott D. F., Anyon C. P. A study of candida in one thousand and seven women. N Z Med J. 1971 Jan;73(464):9–13. [PubMed] [Google Scholar]
- Hilton A. L., Warnock D. W. Vaginal candidiasis and the role of the digestive tract as a source of infection. Br J Obstet Gynaecol. 1975 Nov;82(11):922–926. doi: 10.1111/j.1471-0528.1975.tb00599.x. [DOI] [PubMed] [Google Scholar]
- Hurley R., Leask B. G., Faktor J. A., De Fonseka C. I. Incidence and distribution of yeast species and of Trichomonas vaginalis in the vagina of pregnant women. J Obstet Gynaecol Br Commonw. 1973 Mar;80(3):252–257. doi: 10.1111/j.1471-0528.1973.tb02194.x. [DOI] [PubMed] [Google Scholar]
- Kirkpatrick C. H., Rich R. R., Bennett J. E. Chronic mucocutaneous candidiasis: model-building in cellular immunity. Ann Intern Med. 1971 Jun;74(6):955–978. doi: 10.7326/0003-4819-74-6-955. [DOI] [PubMed] [Google Scholar]
- LOH W. P., BAKER E. E. Fecal flora of man after oral administration of chlortetracycline or oxytetracycline. AMA Arch Intern Med. 1955 Jan;95(1):74–82. doi: 10.1001/archinte.1955.00250070090011. [DOI] [PubMed] [Google Scholar]
- MAIBACH H. I., KLIGMAN A. M. The biology of experimental human cutaneous moniliasis (Candida albicans). Arch Dermatol. 1962 Feb;85:233–257. doi: 10.1001/archderm.1962.01590020073009. [DOI] [PubMed] [Google Scholar]
- MAIBACH H. I., KLIGMAN A. M. The biology of experimental human cutaneous moniliasis (Candida albicans). Arch Dermatol. 1962 Feb;85:233–257. doi: 10.1001/archderm.1962.01590020073009. [DOI] [PubMed] [Google Scholar]
- MENDEL E. B., HABERMAN S. THE VAGINAL ECOLOGY AND ITS RELATIONSHIP TO SYMPTOMS IN VAGINITIS. South Med J. 1965 Mar;58:374–378. doi: 10.1097/00007611-196503000-00025. [DOI] [PubMed] [Google Scholar]
- Mursic V. P. Zur Diagnostik, Pathogenität und Therapie der Candidiasis. MMW Munch Med Wochenschr. 1975 May 23;117(21):893–896. [PubMed] [Google Scholar]
- Oates J. K., Selwyn S., Breach M. R. Polyester sponge swabs to facilitate examination for genital infection in women. Br J Vener Dis. 1971 Aug;47(4):289–292. doi: 10.1136/sti.47.4.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohatiner J. J. Relationship of Candida albicans in the genital and anorectal tracts. Br J Vener Dis. 1966 Sep;42(3):197–200. doi: 10.1136/sti.42.3.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Söltz-Szöts J., Thurner J. Sprosspilzinfektion des männlichen und weiblichen Genitale. Z Haut Geschlechtskr. 1969 Aug 15;44(16):545–548. [PubMed] [Google Scholar]
- Willmott F. E. Genital yeasts in female patients attending a VD clinic. Br J Vener Dis. 1975 Apr;51(2):119–122. doi: 10.1136/sti.51.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]