Abstract
We used the BACTEC system to evaluate the effects of several decontamination methods and the addition of antibiotics on the viability of Mycobacterium ulcerans. The effects of polyoxyethylene stearate or egg yolk as supplements were also evaluated to determine their impact on the growth of M. ulcerans. Strains of different geographic origins were subjected to Petroff, reversed Petroff, oxalic acid, and mild HCl treatments. After treatment, the viability of each strain was assessed in the BACTEC system. All of the decontamination methods tested adversely affected bacterial viability. Treatment with mild HCl gave the best results, allowing better growth rates with some strains and causing a delay in growth with others, depending on the geographic origin of the strain. A mixture of polymyxin B, amphotericin B, nalidixic acid, trimethoprim, and azlocillin did not significantly inhibit growth. Supplementing BACTEC medium with egg yolk markedly improved the recovery of M. ulcerans following the use of each of the decontamination methods. Our findings demonstrate a detrimental impact on the viability of M. ulcerans by all of the decontamination methods currently in common use. This explains, at least in part, the difficulty often experienced in cultivating this organism from clinical specimens. Egg yolk should be added to enhance the rate of successful primary cultivation of M. ulcerans in the BACTEC system.
Mycobacterium ulcerans is the cause of Buruli ulcer, a necrotizing disease of the skin of humans, first described in Australia by MacCallum in 1948 (17).
After tuberculosis and leprosy, M. ulcerans infection is the third most common mycobacterial disease in immunocompetent humans (29). Recent reports have shown increased incidences of the disease in Australia, Benin, and Côte d’Ivoire (9, 13, 18).
The epidemiology of the disease is still not well understood. Buruli ulcer has been reported mostly in tropical countries in Africa, central and southeastern Asia, and, to a lesser extent, in the Americas. The infection is most common in riverine areas and swampy terrains or associated with lake (lacustrine) systems. Although there is evidence for a natural reservoir, M. ulcerans has never been isolated from the environment (12, 19, 22, 27, 28).
For a variety of reasons, the disease is often underdiagnosed and improperly treated. Because antibiotics that are active in vitro have little effect in vivo, the recommended treatment is usually surgical excision and skin grafting. Patients are frequently poorly managed and suffer permanent disabilities with devastating personal consequences (4, 20).
Isolation of M. ulcerans in culture from clinical samples is an important element in the laboratory diagnosis of Buruli ulcer. Successful cultivation of M. ulcerans depends on several parameters, including cultivation conditions, type of decontamination, and use of selective culture media.
M. ulcerans grows preferentially at 30 to 33°C on Löwenstein-Jensen (L-J) slants. Growth, however, is very slow, even under these generally accepted optimal conditions of cultivation (13). There is, thus, an urgent need for studies on alternative cultivation conditions that would improve the recovery of the bacterium in primary culture.
Use of selective media has not been adequately explored. Samples for primary isolation of M. ulcerans are usually inoculated onto standard L-J slants or other egg-based media after decontamination. Most decontamination methods are detrimental to the viability of mycobacteria (31).
Decontamination methods have usually been designed for treating either clinical or environmental samples. Methods used for the recovery of mycobacteria from environmental sources are more stringent, especially with regard to the duration of treatment and the reagents employed (16, 37, 39).
Although some of the methods now in use decontaminate the specimens acceptably, not all preserve the viability of mycobacteria. Differences in the susceptibility of different species of mycobacteria to the detrimental effects of decontamination are well known (29). Thus, there is a need to develop appropriate decontamination procedures that preserve the viability of each species of mycobacteria and effectively eliminate contaminating organisms.
Cultivation of mycobacteria, in particular, M. tuberculosis, has been improved recently by radiometric methods such as the BACTEC 460 system (35). This system has been used for primary isolation of other nontuberculous and difficult-to-grow mycobacteria such as M. genavense (2, 5). The BACTEC system has been successfully adapted for monitoring of the in vitro activity of drugs against noncultivable mycobacteria such as M. leprae (10). There are, however, no previous reports on the use of this system for the cultivation of M. ulcerans.
In the present study, we employed the BACTEC system to evaluate several decontamination methods and explored the use of antibiotics to improve the primary isolation of M. ulcerans. The effects of polyoxyethylene stearate (POES), a growth stimulant normally used in the BACTEC system, and the addition of egg yolk on the growth of M. ulcerans were also evaluated.
MATERIALS AND METHODS
Mycobacterial strains.
Six strains of M. ulcerans from different geographic origins were used throughout the study (32). Strains 9146, 5153, and 94-512 were from Africa; 94-1316 and 5142 (reference strain ATCC 19423) were both from Australia; and 5114 was from Mexico. Strains were maintained on L-J slants and subcultured before testing. For each experiment, a bacterial suspension containing 107 bacilli/ml was prepared by placing a loopful of the subcultured colonies in a vial containing sterile saline and a few glass beads and then agitating them in a Mickle apparatus for 2 min. Further dispersion of the bacilli was achieved by passing the suspension through a syringe fitted with a 25-gauge needle before inoculating the BACTEC vials. Colony count was verified by plating appropriate dilutions on Middlebrook 7H11 agar plates.
Decontamination procedures.
Several decontamination procedures were evaluated to assess their effect on the viability of M. ulcerans. The previously described bacterial suspension of each strain was subjected to one of four decontamination methods.
Method 1 was the Petroff method (26). The bacterial suspension (1 ml) was decontaminated with sodium hydroxide (NaOH) at a final concentration of 0.5 N for 20 min at room temperature with intermittent agitation and then neutralized with 1 N hydrochloric acid (HCl). This suspension was then centrifuged at 2,500 × g for 20 min to pellet the bacilli and then resuspended in sterile saline at a concentration of 107 bacilli/ml.
Method 2 was the reversed Petroff method (Fortep) (30). The bacterial suspension was treated with HCl at a final concentration of 0.5 N for 20 min at room temperature and then neutralized with 1 N NaOH. The suspension was then centrifuged at 2,500 × g for 20 min as before, and the bacilli were resuspended at 107/ml.
Method 3 was mild decontamination treatment (1). The bacterial suspension was treated with HCl at 0.03 N (final concentration) for 20 min and resuspended at 107 bacilli/ml.
Method 4 was oxalic acid treatment (14). The bacterial suspension was treated with a solution of 1.1 N oxalic acid (final concentration) for 20 min at room temperature, centrifuged at 2,500 × g for 20 min, and resuspended in sterile saline at a concentration of 107 bacilli/ml.
One untreated portion of the bacterial suspension served as the control. All of the test suspensions and controls were inoculated in 0.1-ml volumes in BACTEC 12B vials in triplicate and incubated at 33°C. Readings of the growth index (GI) were made twice a week.
Antimicrobial agent treatment.
To evaluate the effect of antibiotics on the viability of M. ulcerans, we employed a mixture of polymyxin B, amphotericin B, nalidixic acid, trimethoprim, and azlocillin (PANTA) which is routinely used in the BACTEC system for primary isolation of M. tuberculosis. Vials were inoculated in triplicate with 0.1 ml of the bacterial suspension (107 bacilli/ml) and incubated at 33°C. BACTEC vials without PANTA served as controls. The GI was read twice a week.
Effect of POES.
The effect of POES as a growth stimulant for M. ulcerans was tested by inoculating 0.1-ml volumes of a bacterial suspension in BACTEC 12B vials containing POES at a concentration of 100 μg/ml and incubated as described above. Inoculated BACTEC vials without POES served as controls.
Effect of supplementation with egg yolk.
To determine the effect of egg yolk on the growth of mycobacteria in the BACTEC system, 0.1 ml of a sterile emulsion of 50% egg yolk (Difco Laboratories, Detroit, Mich.) was added in triplicate to vials to give a final concentration of 1.25%. Vials were inoculated with 0.1 ml of a bacterial suspension as previously described. BACTEC 12B vials without egg yolk served as controls. The GI was read twice weekly.
Egg yolk supplementation was also tested in decontamination experiments to assess its effect on the recovery of mycobacteria in the BACTEC system after each decontamination procedure.
RESULTS
Effect of antimicrobial agents.
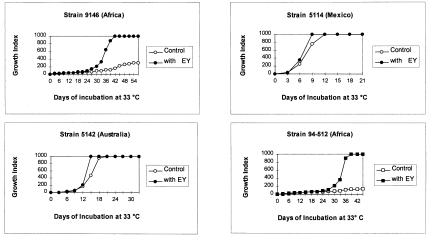
The effect of PANTA on the viability of M. ulcerans in the BACTEC system is shown in Fig. 1 for three strains of different geographic origins. Addition of PANTA caused a mild initial decrease in the growth of strain 5142 (Australian). This inhibition was evident only during the first 2 weeks of incubation; however, the maximum GI of 999 was attained at the same time as the control at day 18. For strain 5114 (Mexican), there was a delay in growth in the presence of PANTA, reaching the maximum GI of 999 at day 21. The control reached the maximum GI on day 10. PANTA had no significant effect on the growth of strain 5153 (African).
FIG. 1.
Effect of PANTA on the growth of M. ulcerans strains of different geographic origins in BACTEC 12B medium.
Effect of POES.
There was no stimulating effect of POES on three of the four strains tested (9146, 94-1316, and 5114); however, POES stimulated the growth of strain 94-512 (African) after 6 days of incubation. The maximum GI obtained was 417, compared to a GI of 239 for the control.
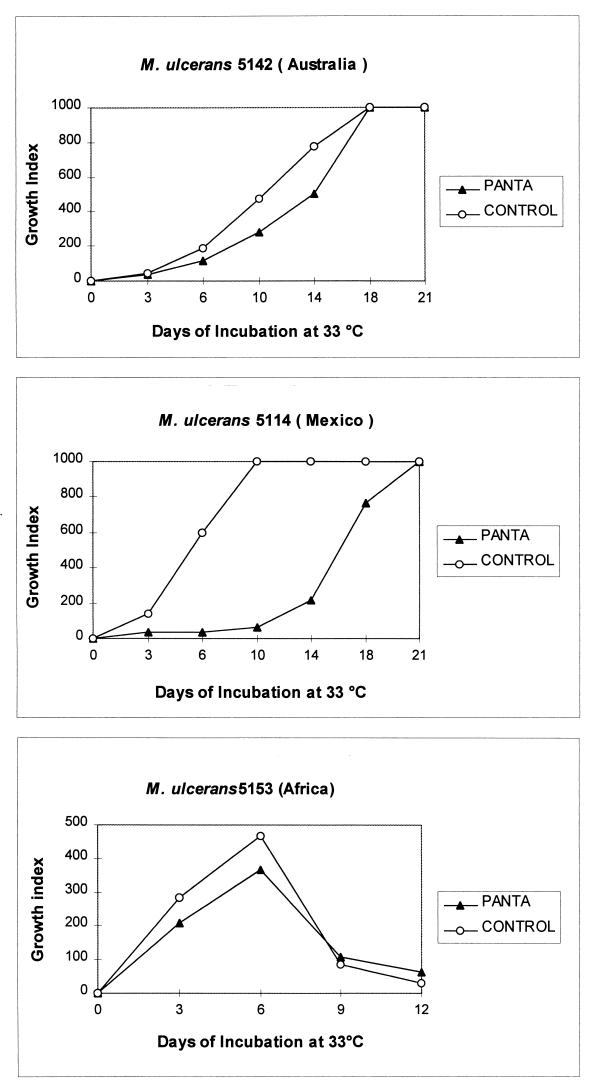
Effect of egg yolk supplementation.
The effect of egg yolk on four strains is shown in Fig. 2. Strain 9146 (African) was strongly stimulated by the addition of egg yolk, reaching a GI of 999 at 42 days of incubation. By comparison, the control GI at the same time was 152 and reached a maximum of only 319 at 54 days. Detection of growth, however, was achieved at the same time after 1 week of incubation. Comparable results were obtained with the other African strain (94-512). Strain 5114 (Mexican), was slightly stimulated by egg yolk, reaching a GI of 999 after 9 days, 3 days before the control. Strain 5142 (Australian) was also stimulated by egg yolk, reaching a GI of 999 after 15 days of incubation, while the control reached the maximum at day 21. Growth was detected at the same time as the control during the first week of incubation.
FIG. 2.
Effect of egg yolk (EY) on the growth of M. ulcerans strains from different geographic origins in BACTEC 12B medium.
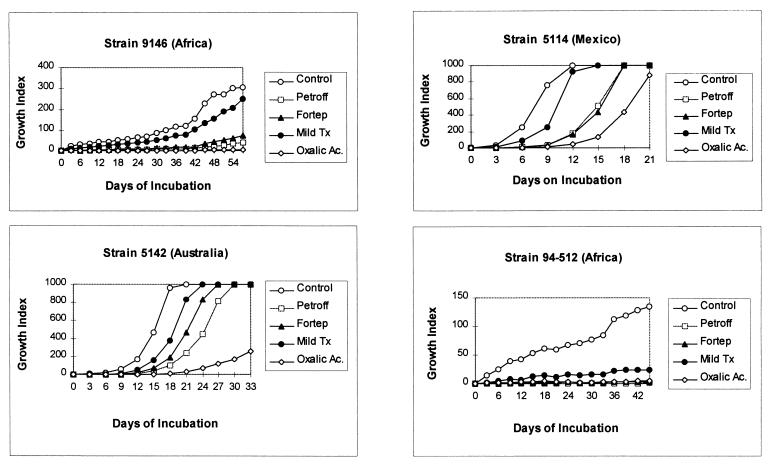
Effects of decontamination methods.
The effects of different decontamination procedures on four strains of M. ulcerans of different geographic origins are shown in Fig. 3. Decontamination by the Petroff, reversed Petroff (Fortep), and oxalic acid methods markedly inhibited the growth of African strain 9146 in the BACTEC system, resulting in maximum GIs of 39, 75, and 5, respectively, after 57 days of incubation. By contrast, the control reached a GI of 319 at day 54. Only decontamination with mild HCl gave a growth rate comparable to that of the control, giving a maximum GI of 231. Strain 94-512, also of African origin, showed less growth and was completely inhibited by all of the decontamination methods, remaining negative after the Petroff, reversed Petroff, and oxalic acid treatments. The control GI was 129. Comparable patterns of inhibition by the different decontamination methods were observed with the other two strains. Strain 5114 from Mexico grew better; however, decontamination by the Petroff, reversed Petroff, and oxalic acid methods caused marked delays of growth. Decontamination with mild HCl, however, led only to a minor delay in growth, reaching a maximum GI of 999 3 days later than the control. All of the decontamination procedures inhibited strain 5142 from Australia, but mild HCl treatment was the least inhibitory, and the strain reached a GI of 999 3 days after the control. Oxalic acid caused the greatest inhibition of this strain, with a maximum GI of 251 after 33 days of incubation. Additional experiments performed with the NaOH–N-acetyl-l-cysteine method of decontamination gave patterns of growth inhibition similar to those achieved with the Petroff, reversed Petroff, and oxalic acid methods of decontamination (data not shown).
FIG. 3.
Effect of decontamination methods on the growth of M. ulcerans strains from different geographic origins in BACTEC 12B medium.
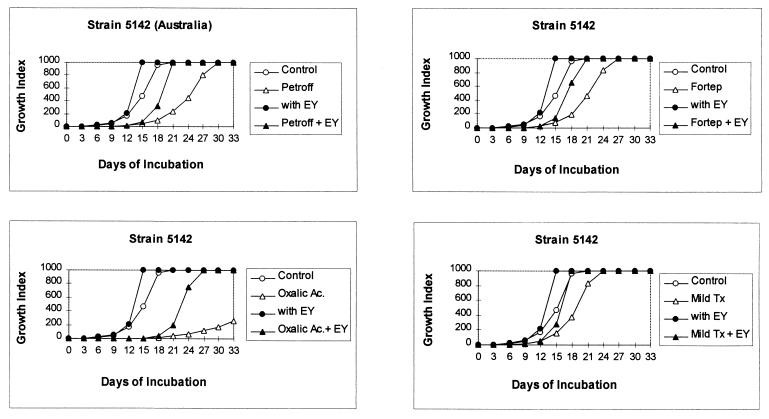
Effect of egg yolk on recovery of M. ulcerans after use of decontamination methods.
The effect of supplementation with egg yolk on the recovery of bacteria after the use of each decontamination method is shown in Fig. 4 for reference strain 5142 (ATCC 19423). As seen previously, decontamination with the Petroff method caused strong inhibition, reaching a maximum GI of 999 at day 30. This represents a delay of almost 10 days compared to the control. Supplementation of the BACTEC vials with egg yolk eliminated this delay. Both the test and control suspensions reached the maximum GI on day 21. Decontamination by the reversed Petroff method also inhibited growth, reaching a maximum GI of 999 at day 27, 1 week after the control. Addition of egg yolk eliminated this inhibition. Decontamination with oxalic acid strongly inhibited growth in the BACTEC system, reaching a maximum GI of 251 after only 33 days. Supplementation with egg yolk greatly improved growth, reaching a GI of 999 on day 27. Decontamination with mild HCl slightly decreased growth, but this inhibition was completely reversed by egg yolk supplementation.
FIG. 4.
Effect of egg yolk (EY) on the growth of M. ulcerans in BACTEC 12B medium after decontamination.
Egg yolk supplementation improved the recovery of bacteria of the other strains after decontamination (Table 1). With strain 9146, addition of egg yolk gave a GI of 999 after decontamination with the Petroff, reversed Petroff, and mild HCl methods. In contrast, vials without added egg yolk never reached high GIs; for example, addition of egg yolk following oxalic acid treatment increased the GI from 5 to 87 at day 57. With a strain of M. ulcerans which has a more rapid rate growth in the BACTEC system, for example, 5114 from Mexico, supplementation with egg yolk shortened the period required for the maximum GI of 999 in all instances. Strain 94-512, with a slower rate of growth in the BACTEC system, was stimulated by egg yolk; however, following decontamination, the maximum GI was never obtained.
TABLE 1.
Effect of egg yolk on the growth of M. ulcerans strains of different origins in BACTEC 12B medium after decontamination
| Decontamination method | Presence of egg yolka | Maximum GI obtained (incubation day)
|
||
|---|---|---|---|---|
| Strain 9146 (Africa) | Strain 5114 (Mexico) | Strain 94-512 (Africa) | ||
| None | − | 304 (57) | 999 (12) | 134 (45) |
| + | 999 (42) | 999 (9) | 999 (39) | |
| Petroff | − | 40 (57) | 999 (18) | 2 (45) |
| + | 999 (57) | 999 (15) | 27 (45) | |
| Reversed Petroff | − | 71 (57) | 999 (18) | 3 (45) |
| + | 895 (57) | 999 (12) | 111 (45) | |
| Mild HCl | − | 251 (57) | 999 (15) | 24 (15) |
| + | 999 (48) | 999 (9) | 389 (45) | |
| Oxalic acid | − | 5 (57) | 875 (21) | 4 (45) |
| + | 87 (57) | 999 (15) | 173 (45) | |
+, with egg yolk; −, without egg yolk.
DISCUSSION
M. ulcerans is a slow-growing organism and is highly susceptible to factors influencing its viability in vitro, making primary isolation of the organism a continuing problem in the study of Buruli ulcer. Few bacteriological studies have addressed the question of the primary isolation of this mycobacterium from both clinical and environmental sources (13).
An essential factor in the isolation of M. ulcerans in primary culture is the decontamination procedure employed for eliminating contaminating microorganisms in clinical and environmental samples. In this study, we evaluated several decontamination methods commonly used in attempts to isolate M. ulcerans from clinical and environmental specimens (30, 31) to establish their effect on the viability of M. ulcerans. The BACTEC system is especially appropriate for such studies.
The Petroff method is one of the most commonly employed procedures in the primary isolation of M. tuberculosis from sputum. We tested this method on four strains of M. ulcerans from different geographic origins and found that growth was suppressed 87 to 98.5%. The use of this decontamination procedure adversely affected the growth rate of the bacteria markedly in the BACTEC system. The reversed Petroff method led to similar results, suppressing the growth of strains 94-512 and 9146 of African origin 77 to 98% compared to the control. Strains 5114 of Mexican origin and 5142 of Australian origin, however, reached a GI of 999, but only after a 6-day delay compared with the control. The reversed method is commonly used for biopsy specimens (28) and exudates from Buruli ulcer patients (30).
Previous work has shown that mild HCl treatment permits good recovery of mycobacteria from clinical samples (1). With this method, recovery of M. ulcerans in the BACTEC system is improved; however, the growth of strains 94-512 and 9146 was suppressed 82 and 18%, respectively. There was no delay in the growth of strain 5114 and a delay of only 3 days in that of strain 5142.
Decontamination by oxalic acid is commonly used for isolation of nontuberculous mycobacteria (31). Yajko et al. (39) compared various decontamination methods for recovering M. avium from specifically seeded stools and found that oxalic acid gave the best results. In our study, oxalic acid reduced the growth rate of M. ulcerans markedly: in strain 9146 by 98% and in strain 94-512 by 97%. Strain 5114, with a normally good rate of growth, was adversely affected by treatment with oxalic acid. With the oxalic acid method, we omitted the usual addition of NaOH because preliminary experiments showed better recovery of M. ulcerans in the BACTEC system without neutralization. Yajko et al. reported similar results for M. avium (38). The harmful effect of oxalic acid decontamination is thus not related to neutralization, provided that the specimen is washed with distilled water before cultivation.
Isolation of mycobacteria from material heavily contaminated with other microorganisms (e.g., environmental specimens) requires drastic methods for decontamination. The procedures used in this study, with the exception of mild treatment with HCl, are adequate for the decontamination of a primary culture of mycobacteria from soil (31). Our data, however, demonstrate that these methods reduce the viability of M. ulcerans and may contribute to failures in the isolation of M. ulcerans from the environment.
Development of optimal selective media for the primary isolation of M. ulcerans has not been explored. By employing the BACTEC system, we evaluated the effect of the antimicrobial combination PANTA on the viability of M. ulcerans; PANTA inhibited only strain 5114 and not the other strains we studied. Observations by Conville et al. on the effect of PANTA on the growth of M. kansasii in the BACTEC system showed inhibition of the growth of two isolates, suggesting that nalidixic acid was inhibitory (3). Few studies have been done on the in vitro activity of antibiotics against M. ulcerans (8, 11, 25). We have not tested individual components of PANTA against M. ulcerans; however, a search for the ideal antimicrobial combination with the least harmful effects against the majority of M. ulcerans strains is a priority. Our findings suggest that PANTA as an adjunct for the primary isolation of M. ulcerans is currently the optimal choice.
The commercial preparation of PANTA (BACTEC) contains POES, which is claimed to stimulate the growth of many strains of M. tuberculosis (6). In the BACTEC system, Franzblau found that POES inhibited the metabolic activity of M. leprae (10) and Miller et al. reported the inhibition of some M. tuberculosis strains by POES in pyrazinamide susceptibility tests (21). We have observed that POES inhibited the growth of M. genavense (33). In our study, POES neither stimulated nor inhibited the growth of M. ulcerans.
In contrast to agar-based media, L-J medium compares favorably to BACTEC in terms of the rate of growth and the yield of colonies of M. ulcerans. Because egg yolk is a major difference between agar-based and L-J media, we evaluated the effect of egg yolk as a supplement in the BACTEC system on M. ulcerans growth. Egg yolk enhances the growth of M. tuberculosis in BACTEC 7H12 medium (15) and does not interfere with the radiometric detection of growth (37). Additionally, Cutler et al. (7) showed that supplementing 7H12 medium with 10% egg yolk increased the GIs of M. tuberculosis and increased the sensitivity of detection.
Addition of egg yolk to BACTEC medium improved the growth rates of all of the strains of M. ulcerans evaluated. This effect, however, was variable: African strains (9146 and 94-512) were strongly stimulated, while the other strains (5142 and 5114) were stimulated to a lesser degree. In all instances, however, first evidence of growth was noted at the same time with or without egg yolk. Kononov et al. first attributed this effect on the growth of M. tuberculosis to the utilization of nutrients in egg yolk which may compete with labeled palmitic acid, but additional observations suggested that this competition was insignificant (15). We believe the influence of different concentrations of egg yolk and known components thereof on the growth of M. ulcerans needs further study in the BACTEC system.
Use of egg yolk improved the recovery of all of the strains of M. ulcerans studied following the use of all of the decontamination methods examined (Fig. 4). This was most striking following oxalic acid treatment, a method that is quite harmful to the viability of M. ulcerans in the BACTEC system.
Morphologic observations suggest that a high proportion of the bacilli in clinical specimens from Buruli ulcer patients are degenerating (24), perhaps similar to M. leprae in most material from leprosy patients (34, 36). A comparable situation most likely prevails in attempts to isolate M. ulcerans from the environment. Such specimens are highly contaminated and require strong decontamination methods, perhaps partially explaining the complete failure thus far to cultivate M. ulcerans from nature. Our studies suggest that the use of egg yolk may aid the primary isolation of M. ulcerans in situations in which there is a paucity of viable organisms.
The various responses of different strains of M. ulcerans to the decontamination and culture methods we used are not unexpected because of the genetic and phenotypic variations described in strains from different geographic origins (32).
Our results led us to conclude that the decontamination methods most commonly employed for the primary isolation of M. ulcerans adversely affect the viability of the bacteria. This adverse effect was, to some extent, eliminated by supplementing the BACTEC medium with egg yolk. Thus, while egg yolk-based media may improve the efficiency of primary isolation, primary culture of M. ulcerans on L-J media is likely to remain difficult (30).
In summary, to improve the success of primary cultivation from contaminated samples, we recommend that future isolation strategies for M. ulcerans should consider the use of milder decontamination methods and the use of selective media. Further studies are needed to establish optimal cultivation conditions for M. ulcerans that are applicable particularly to paucibacillary clinical samples and, perhaps, environmental samples.
ACKNOWLEDGMENTS
This study was partly supported by the Fonds National de la Recherche Scientifique, Belgium (grant 15.192.95F), and by the Damien Foundation, Belgium. We thank Becton Dickinson for use of the BACTEC 460 TB instrument and for the culture media used in this study. J. C. Palomino was financially supported by the European Commission through contract CI1*-CT94-0556 and by the Damien Foundation, Belgium.
We thank Wayne Meyers for critically reviewing the manuscript.
REFERENCES
- 1.Bosquée L, Böttger E C, De Beenhouwer H, Fonteyne P A, Hirschel B, Larsson L, Meyers W M, Palomino J C, Realini L, Rigouts L, Silva M T, Teske A, Van der Auwera P, Portaels F. Cervical lymphadenitis caused by a fastidious Mycobacterium closely related to Mycobacterium genavense in an apparently immunocompetent woman. Diagnosis by culture-free microbiology. J Clin Microbiol. 1995;33:2670–2674. doi: 10.1128/jcm.33.10.2670-2674.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Böttger E C, Teske A, Kirschner P, Bost S, Chang H R, Beer V, Hirschel B. Disseminated Mycobacterium genavense infection in patients with AIDS. Lancet. 1992;340:76–80. doi: 10.1016/0140-6736(92)90397-l. [DOI] [PubMed] [Google Scholar]
- 3.Conville P S, Andrews J W, Witebsky F G. Effect of PANTA on growth of Mycobacterium kansasii in BACTEC 12B medium. J Clin Microbiol. 1995;33:2012–2015. doi: 10.1128/jcm.33.8.2012-2015.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cornet L, Richard-Kadio M, Nguessan H A, Yapo P, Hossoko H, Dick R, Casanelli J M. Le traitement des ulcères de Buruli par excision-greffe. Bull Soc Pathol Exot. 1992;85:355–358. [PubMed] [Google Scholar]
- 5.Coyle M B, Carlson L D C, Wallis C K, Leonard R B, Raisys V A, Kilbrun J O, Samadpour M, Böttger E C. Laboratory aspects of Mycobacterium genavense, a proposed species isolated from AIDS patients. J Clin Microbiol. 1992;30:3206–3212. doi: 10.1128/jcm.30.12.3206-3212.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cutler R R, Wilson P, Clarke W. The effect of polyoxyethylene stearate (POES) on the growth of mycobacteria in radiometric 7H12 Middlebrook TB medium. Tubercle. 1987;68:209–220. doi: 10.1016/0041-3879(87)90057-2. [DOI] [PubMed] [Google Scholar]
- 7.Cutler R R, Wilson P, Clarke F V. Evaluation of a modified BACTEC method to study the activity of disinfectants against Mycobacterium tuberculosis. Tubercle Lung Dis. 1995;76:254–260. doi: 10.1016/s0962-8479(05)80014-0. [DOI] [PubMed] [Google Scholar]
- 8.De Gentille P L, Mahaza C, Rolland F, Carbonnelle B, Verret J L, Chabasse D. L’ulcère cutané a Mycobacterium ulcerans. A propos d’une observation en provenance de Guyane française. Bull Soc Pathol Exot. 1992;85:212–214. [PubMed] [Google Scholar]
- 9.Flood P, Street A, O’Brien P, Hayman J. Mycobacterium ulcerans infection on Philip Island, Victoria. Med J Aust. 1994;160:160. [PubMed] [Google Scholar]
- 10.Franzblau S G. Drug susceptibility testing by Mycobacterium leprae in the BACTEC 460 system. Antimicrob Agents Chemother. 1989;33:2115–2117. doi: 10.1128/aac.33.12.2115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goutzamanis J J, Gilbert G L. Mycobacterium ulcerans infection in Australian children: report of eight cases and review. Clin Infect Dis. 1995;21:1186–1192. doi: 10.1093/clinids/21.5.1186. [DOI] [PubMed] [Google Scholar]
- 12.Hayman J. Postulated epidemiology of Mycobacterium ulcerans infection. Int J Epidemiol. 1991;20:1093–1098. doi: 10.1093/ije/20.4.1093. [DOI] [PubMed] [Google Scholar]
- 13.Josse R, Guedenon A, Darie H, Anagonou S, Portaels F, Meyers W M. Les infections cutanées àMycobacterium ulcerans: ulcères de Buruli. Med Trop. 1995;55:363–373. [PubMed] [Google Scholar]
- 14.Kent P T, Kubica G P. Public health mycobacteriology. A guide to the level III laboratory. Atlanta, Ga: Centers for Disease Control; 1985. [Google Scholar]
- 15.Kononov Y, Ta K D, Heifets L. Effect of egg yolk on growth of Mycobacterium tuberculosis in 7H12 liquid medium. J Clin Microbiol. 1988;26:1395–1397. doi: 10.1128/jcm.26.7.1395-1397.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Livanainen E. Isolation of mycobacteria from acidic forest soil samples: comparison of culture methods. J Appl Bacteriol. 1995;78:663–668. doi: 10.1111/j.1365-2672.1995.tb03113.x. [DOI] [PubMed] [Google Scholar]
- 17.MacCallum P, Tolhurst J C, Buckle G, Sissons H A. A new mycobacterial infection in man. I. Clinical aspects. J Pathol Bacteriol. 1948;60:93–101. [PubMed] [Google Scholar]
- 18.Marston B J, Diallo M O, Horsburgh C R, Diomande I, Saki M Z, Kanga J M, Patrice G, Lipman H B, Ostroff S M, Good R C. Emergence of Buruli ulcer disease in the Daloa region of Cote D’Ivoire. Am J Trop Med Hyg. 1995;52:219–224. doi: 10.4269/ajtmh.1995.52.219. [DOI] [PubMed] [Google Scholar]
- 19.Meyers W M. Mycobacterial infections of the skin. In: Doerr W, Seifert G, editors. Tropical pathology. Heidelberg, Germany: Springer-Verlag; 1995. pp. 291–377. [Google Scholar]
- 20.Meyers W M, Shelly W M, Connor D H. Heat treatment of Mycobacterium ulcerans infections without surgical excision. Am J Trop Med Hyg. 1974;23:924–929. doi: 10.4269/ajtmh.1974.23.924. [DOI] [PubMed] [Google Scholar]
- 21.Miller M A, Thiebert L, Desjardins F, Siddiqi S H, Dascal A. Growth inhibition of Mycobacterium tuberculosis by polyoxyethylene stearate present in the BACTEC pyrazinamide susceptibility test. J Clin Microbiol. 1996;34:84–86. doi: 10.1128/jcm.34.1.84-86.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mitchell J P, Jerret I V, Slee K J. Skin ulcers caused by Mycobacterium ulcerans in koalas near Bairnsdale, Australia. Pathology. 1994;16:256–260. doi: 10.3109/00313028409068533. [DOI] [PubMed] [Google Scholar]
- 23.Muelder K. Buruli ulcer in Benin. Trop Doct. 1988;18:53. [PubMed] [Google Scholar]
- 24.Pattyn S R, Boveroulle M T, Gatti F, Vandepitte J. Etude des souches de Mycobacterium ulcerans isolées au Congo (Léopoldville) Acad R Sci Outre-Mer. 1964;6:1576–1599. [Google Scholar]
- 25.Pattyn S R, Royackers J. Traitement de l’infection expérimentale de la souris par Mycobacterium ulcerans et Mycobacterium balnei. Ann Soc Bel Med Trop. 1965;45:31–38. [PubMed] [Google Scholar]
- 26.Petroff S A. A new and rapid method for the isolation and cultivation of tubercle bacilli directly from the sputum and feces. J Exp Med. 1915;21:38–42. doi: 10.1084/jem.21.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Portaels F. Etude d’Actinomycétales de l’homme et de son environment en Afrique Central. Ph.D. thesis. Brussels, Belgium: Université Libre de Bruxelles; 1978. [Google Scholar]
- 28.Portaels F. Epidémiologie des ulcères àMycobacterium ulcerans. Ann Soc Belg Med Trop. 1989;69:91–103. [PubMed] [Google Scholar]
- 29.Portaels F. Epidemiology of mycobacterial diseases. Clin Dermatol. 1995;13:207–222. doi: 10.1016/0738-081x(95)00004-y. [DOI] [PubMed] [Google Scholar]
- 30.Portaels F, Aguiar J, Fissette K, Fonteyne P A, De Beenhouwer H, de Rijk P, Guedenon A, Lemans R, Steunou C, Zinsou C, Dumonceau J M, Meyers W M. Direct detection and identification of Mycobacterium ulcerans in clinical specimens by PCR and oligonucleotide-specific capture plate hybridization. J Clin Microbiol. 1997;35:1097–1100. doi: 10.1128/jcm.35.5.1097-1100.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Portaels F, De Muynck A, Sylla M P. Selective isolation of mycobacteria from soil: a statistical analysis approach. J Gen Microbiol. 1988;134:849–855. doi: 10.1099/00221287-134-3-849. [DOI] [PubMed] [Google Scholar]
- 32.Portaels F, Fonteyne P A, De Beenhouwer H, de Rijk P, Guedenon A, Hayman J, Meyers W M. Variability in the 3′ end of the 16S rRNA sequence of the species Mycobacterium ulcerans is related to geographic origins of the isolates. J Clin Microbiol. 1996;34:962–965. doi: 10.1128/jcm.34.4.962-965.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Realini, L., et al. Unpublished data.
- 34.Rees R J, Valentine R C, Wong P C. Application of quantitative electron microscopy to the study of Mycobacterium lepraemurium and Mycobacterium leprae. J Gen Microbiol. 1960;22:443–457. doi: 10.1099/00221287-22-2-443. [DOI] [PubMed] [Google Scholar]
- 35.Roberts G D, Goodman N L, Heifets L, Larsh H W, Lindner T H, McClatchy J K, McGinnis M R, Siddiqi S H, Wright P. Evaluation of the BACTEC radiometric method for recovery of mycobacteria and drug susceptibility testing of Mycobacterium tuberculosis from acid-fast smear-positive specimens. J Clin Microbiol. 1983;18:689–696. doi: 10.1128/jcm.18.3.689-696.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Valentine R C. Quantitative electron microscopy of leprosy bacilli. Br Med Bull. 1962;18:242–244. doi: 10.1093/oxfordjournals.bmb.a069987. [DOI] [PubMed] [Google Scholar]
- 37.Whittier S, Hopfer R L, Knowles M R, Gilligan P H. Improved recovery of mycobacteria from respiratory secretions of patients with cystic fibrosis. J Clin Microbiol. 1993;31:861–864. doi: 10.1128/jcm.31.4.861-864.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Woodley C L, Smithwick R W. Radiometric method for pyrazinamide susceptibility testing of Mycobacterium tuberculosis in egg-yolk-enriched BACTEC 12A medium. Antimicrob Agents Chemother. 1988;32:125–127. doi: 10.1128/aac.32.1.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yajko D M, Nassos P S, Sanders C A, Gonzalez P C, Reingold A L, Horsburgh C R, Hopewell P C, Chin D P, Hadley W K. Comparison of four decontamination methods for recovery of Mycobacterium avium complex from stools. J Clin Microbiol. 1993;31:302–306. doi: 10.1128/jcm.31.2.302-306.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]