Abstract
The increasing morbidity and mortality of life-threatening Pneumocystis pneumonia (PCP) in immunocompromised people poses a global concern, prompting the World Health Organization to list it as one of the 19 priority invasive fungal diseases, calling for increased research and public health action. In response to this initiative, we provide this review on the epidemiology of PCP in non-HIV patients with various immunodeficient conditions, including the use of immunosuppressive agents, cancer therapies, solid organ and stem cell transplantation, autoimmune and inflammatory diseases, inherited or primary immunodeficiencies, and COVID-19. Special attention is given to the molecular epidemiology of PCP outbreaks in solid organ transplant recipients; the risk of PCP associated with the increasing use of immunodepleting monoclonal antibodies and a wide range of genetic defects causing primary immunodeficiency; the trend of concurrent infection of PCP in COVID-19; the prevalence of colonization; and the rising evidence supporting de novo infection rather than reactivation of latent infection in the pathogenesis of PCP. Additionally, we provide a concise discussion of the varying effects of different immunodeficient conditions on distinct components of the immune system. The objective of this review is to increase awareness and knowledge of PCP in non-HIV patients, thereby improving the early identification and treatment of patients susceptible to PCP.
Keywords: Pneumocystis, non-HIV/AIDS, immunocompromised, epidemiology, primary immunodeficiency, immunodepleting monoclonal antibodies, organ transplantation
1. Introduction
Pneumocystis jirovecii is an atypical opportunistic fungus that can cause life-threatening Pneumocystis pneumonia (PCP) in immunodeficient patients. Prior to the advent of the HIV/AIDS epidemic, PCP was predominantly reported in premature or malnourished infants and patients with cellular immunodeficiencies due to conditions such as hematological malignancies, T cell deficiency, and other severe diseases requiring corticosteroid treatment [1,2]. In the 1980s, the high morbidity of PCP in HIV-infected patients overshadowed its prevalence in non-HIV patients. Since the late 1990s, the broad utilization of prophylaxis and subsequent combination antiretroviral therapy (cART) has significantly reduced the PCP incidence in HIV-infected patients, but PCP has continued to affect individuals with other immunodeficient conditions [3,4]. In fact, some studies have reported an increase in PCP incidence among these patients [5,6]. It has been estimated recently that healthcare associated with PCP in the United States alone costs $475–$686 million annually, ranking among the top three or four most serious fungal diseases [7,8,9].
Compared to PCP in HIV-infected patients, PCP in a non-HIV immunosuppressed population has a shorter incubation period, a higher risk of respiratory failure and mortality, and a more rapid disease progression, making it more difficult to diagnose in a timely manner [10,11,12,13,14]. Given the serious threat PCP poses to immunodeficient patients, it is important for clinicians and health care workers to be aware of the new trends in the epidemiology of PCP and to identify potential susceptible patients at the earlier stage in order to initiate appropriate and timely prophylaxis or treatment.
Despite the growing public health implications of PCP, this and other invasive fungal diseases have received little attention and few resources, with limited access to quality diagnostics and treatment. This situation has recently prompted the World Health Organization (WHO) to list PCP as one of the 19 priority invasive fungal diseases, calling for increased research efforts and public health action [15]. In response to this important initiative, we contributed this review, with a focus on the changing epidemiology of PCP among non-HIV patients.
2. The Infectious Agent and Infection Chain of PCP
P. jirovecii, the pathogen responsible for PCP in humans, belongs to the genus Pneumocystis, which is closely related to the genera Schizosaccharomyces, Taphrina, and Saitoella of the subphylum Taphrinomycotina within the phylum Ascomycota phylum [16]. This genus encompasses a large group of phylogenetically closely related yet clearly distinct organisms that are potentially capable of infecting all mammalian species with a very strong, though probably not strict, host specificity. Currently, only six Pneumocystis species have been formally named, including P. jirovecii (infecting humans or Homo sapiens) [17,18], P. murina (house mice or Mus musculus) [19], P. carinii (Brown or Norway rats or Rattus norvegicus) [20], P. wakefieldiae (Brown or Norway rats or Rattus norvegicus) [21], P. oryctolagi (rabbits or Oryctolagus cuniculus) [22], and P. canis (dogs or Canis lupus familiaris) [23]. Long-term cultivation of Pneumocystis remains unsuccessful, which impedes research on many aspects of this pathogen, particularly its life cycle, transmission, immune evasion, and drug resistance and susceptibility.
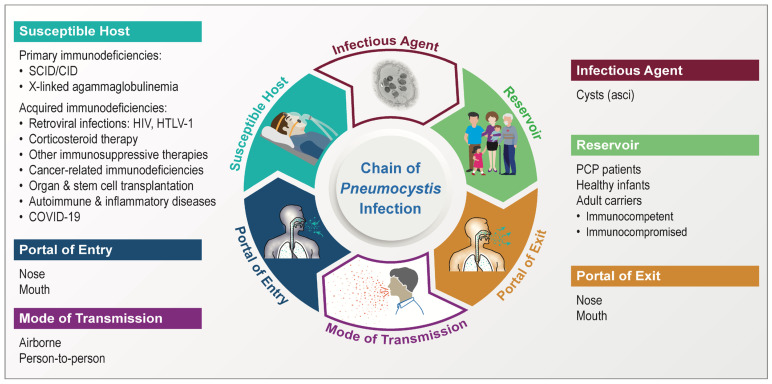
Despite great difficulty in studying Pneumocystis, recent advances in genetics have facilitated our understanding of the basic biology and epidemiology of this pathogen, including its chain of infection, as summarized in Figure 1.
Figure 1.
Pneumocystis infection chain. The infectious agent is exemplified by the cyst (also known as ascus) of P. murina in infected mouse lungs revealed by transmission electron microscopy at a magnification of 5000×. The cyst is characterized by a thick wall with double electron-dense layers enclosing eight intracystic bodies or spores. For the primary immunodeficiencies (under the Susceptible Host), only a limited number of conditions are listed as examples to enhance visual clarity, with more details described in Section 4.5.
Studies with animal models have confirmed that cysts (also known as asci) serve as the infectious agent [24]. Other life stages, including the trophic form, presumably cannot serve as the infectious agent due largely to the lack of a protective cell wall, which prevents their survival, even for a short transient period, in a natural environment outside the lungs of the host [16]. It is now evident that human infection with P. jirovecii is not of zoonotic origin, as strongly supported by the pathogen’s high-degree of host-species specificity and consistent failure in experimental cross-species infections.
No natural environmental reservoir has been identified, while there is overwhelming evidence indicating that humans themselves serve as carriers or reservoirs of this pathogen [16]. Potential human reservoirs include PCP patients and individuals, including children (particularly infants) and adults with either weakened or competent immunity, who are either colonized or have subclinical infection with P. jirovecii. There is no doubt that the respiratory tract serves as both the portal of exit and entry for Pneumocystis infection. The mode of transmission is now generally believed to be airborne through person-to-person contact. Efficient transmission likely requires proximity to an infected host––for example, in the same room [25,26].
PCP primarily affect individuals with impaired immunity. Susceptible individuals include those with various congenital or acquired immunodeficiencies, as detailed below. Excluded from this review are the acquired immunodeficiencies caused by HIV and other retroviruses, including human T-lymphotrophic virus (HTLV).
3. Increased Incidence of PCP in Patients without HIV/AIDS
Over the past two decades, there has been an increase in the incidence of PCP in non-HIV patients based on large-scale national studies. According to the national surveillance data in England, the annual PCP incidence in non-HIV patients rose from 3.15 cases per million general population between 2000 and 2005 to 5.13 cases between 2006 and 2010 [27]. In France, a study of 604 PCP cases in a single hospital from 2005 to 2013 showed an increase in the proportion of PCP cases from 63% to 85% in non-HIV patients and a decrease from 37% to 15% in HIV-infected patients [14]. In Germany, a multi-center, longitudinal population-base study of 12,455 PCP cases from 2014 to 2019 (including 2,124 HIV-related and 10,331 non-HIV-related) showed a significant decrease in annual HIV-related PCP cases from 346 to 331, while the number of non-HIV-related PCP cases increased substantially from 1511 to 1841 [28].
The increase in PCP incidence is attributed to a variety of factors, including the more aggressive use of immunosuppressive agents, increased implementation of organ and stem cell transplantation, application of more sensitive diagnostic methods, and improved awareness of PCP by physicians (reviewed in references [23,29,30,31,32,33]. The true incidence of PCP at present is difficult to determine due to the increased use of prophylaxis, which may lead to underestimation of the actual incidence.
4. Immunodeficient Conditions and Risk Factors for PCP
4.1. Immunosuppressive Agents
Various immunosuppressive or immunomodulatory agents have long been recognized as important risk factors for the development of PCP in non-HIV patients (Table 1). These agents can cause significant immunosuppression, primarily of cellular immunity, which is thought to be the major defense against Pneumocystis. Among the most significant immunosuppressive agents contributing to the occurrence of PCP in non-HIV patients are corticosteroids, which are widely used to treat various underlying conditions, including cancers, autoimmune and inflammatory diseases, and organ and stem cell transplantation, as described below. Several studies have shown that ~90% of PCP patients without HIV infection received corticosteroid therapy, usually in combination with other immunosuppressive agents [3,4,34]. Initially, only long-term and high-dose corticosteroid use was identified as a high risk for PCP, but recent studies suggest that intermittent corticosteroid therapy is also an important risk factor for developing PCP [35]. However, underlying conditions are a more important risk factor for PCP; for example, asthma patients (usually not immunocompromised) treated with steroids are typically not at risk for PCP.
In addition to corticosteroids, traditional immunosuppressive or chemotherapeutic agents associated with the development of PCP include various antimetabolites (methotrexate), alkylating agents (cyclophosphamide), anticalcineurins (cyclosporine and tacrolimus), and inhibitors of a mammalian target of rapamycin (mTOR) (sirolimus and everolimus) (Table 1). Beginning in the 1970s, these chemotherapeutic agents have been frequently reported as risk factors predisposing patients to PCP following their use to treat underlying disorders, primarily hematological malignancies, solid organ transplantation rejection, and rheumatoid arthritis. Subsequently, these drugs were gradually extended to other underlying disease conditions, thereby placing new disease categories at risk for PCP. Since the early 2000s, new immunotherapeutic agents that are utilized in the treatment of various diseases, particularly a wide array of monoclonal antibodies targeting TNFα and other cytokines [36] as well as lymphocyte antigens, have been further recognized as risk factors for PCP (Table 1).
Table 1.
Drugs associated with the development of PCP.
| Drugs | Mechanisms of Action |
Chemical Properties | Approved Applications | References * |
|---|---|---|---|---|
| Corticosteroids ** | Suppression of inflammation, leukocyte migration and activation; induction of apoptosis | Steroid hormones | Various diseases | [4,32,37] |
| Inhibitors of DNA/RNA synthesis | ||||
| Temozolomide | Inhibit DNA and cellular replication | Alkylating agent/imidazotetrazine | Brain cancer, astrocytoma, and glioblastoma multiforme | [38,39] |
| Cyclophosphamide | Inhibit DNA and cellular replication | Alkylating agent/phosphoramide mustard | Lymphoma, multiple myeloma, leukemia, ovarian cancer, breast cancer, small cell lung cancer, neuroblastoma, and sarcoma; organ transplant rejection | [40,41] |
| Bleomycin | Induce DNA strand breaks | Nonribosomal peptide | Lymphoma, testicular cancer, ovarian cancer, and cervical cancer | [42,43] |
| Fluorouracil | DNA synthesis inhibitor | Antimetabolite/pyrimidine analog | Various cancers | [43,44] |
| Cytarabine | DNA synthesis inhibitor | Antimetabolite | Leukemia and lymphoma | [43,45] |
| Methotrexate | DNA/RNA synthesis inhibitor | Antimetabolite/antifolate | Cancers, autoimmune diseases, and ectopic pregnancy | [43,46] |
| Azathioprine | Purine synthesis inhibitor | Antimetabolite/Purine analog | Rheumatoid arthritis, Crohn’s disease, ulcerative colitis, and kidney transplant rejection | [43,47,48] |
| Cladribine | Purine synthesis inhibitor | Antimetabolite/Purine analog | Leukemia and lymphoma | [43,49] |
| Fludarabine | Purine synthesis inhibitor | Antimetabolite/Purine analog | Leukemia and lymphoma | [43,50,51,52] |
| Inhibitors of immune functions | ||||
| Rituximab | B-cell signaling inhibitor | Anti-CD20 monoclonal antibody | Autoimmune diseases, Hematological cancers | [53,54] |
| Alemtuzumab | Deplete CD52-bearing B and T cells | Anti-CD52 monoclonal antibody | Hematological cancers, multiple sclerosis, and organ transplant rejection | [43,52,55] |
| Abatacept | T-cell signaling inhibitor | Recombinant protein | Rheumatoid arthritis, juvenile idiopathic arthritis, and psoriatic arthritis | [56,57] |
| Belatacept | T-cell signaling inhibitor | Recombinant protein | Organ transplant rejection | [58,59,60] |
| Tocilizumab | Anti–IL-6 receptor | Anti-IL6 receptor monoclonal antibody | Rheumatoid arthritis, juvenile rheumatoid arthritis | [61,62,63] |
| Adalimumab | TNFα inhibitor | Anti-TNFα monoclonal antibody | Rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, Crohn’s disease, ulcerative colitis, chronic psoriasis, hidradenitis suppurativa, and juvenile idiopathic arthritis | [64,65] |
| Etanercept | TNFα inhibitor | Recombinant protein | Rheumatoid arthritis, juvenile rheumatoid arthritis and psoriatic arthritis, plaque psoriasis and ankylosing spondylitis | [43,66,67] |
| Golimumab | TNFα inhibitor | Anti-TNFα monoclonal antibody | Rheumatoid arthritis, psoriatic arthritis, ankylosing spondylitis, ulcerative colitis, and rheumatoid arthritis | [68,69] |
| Infliximab | TNFα inhibitor | Anti-TNFα monoclonal antibody | Crohn’s disease, ulcerative colitis, psoriasis, psoriatic arthritis, and ankylosing spondylitis | [43,70,71] |
| Cyclosporine | Calcineurin inhibitor | Anticalcineurin | Autoimmune diseases, and organ transplant rejection | [43,72,73,74] |
| Tacrolimus | Calcineurin inhibitor | Anticalcineurin/macrolide lactone | Organ transplant rejection, eczema, uveitis, and vitiligo | [75,76,77] |
| Everolimus | Inhibitor of mammalian target of rapamycin (mTOR) | Derivative of sirolimus | Organ transplant rejection, kidney cancer, breast cancer, and subependymal giant cell astrocytoma | [78,79,80] |
| Sirolimus (rapamycin) | Inhibitor of mammalian target of rapamycin (mTOR) | Macrolide compound | Organ transplant rejection, lymphangioleiomyomatosis | [43,81,82,83] |
* For the association of the drug with the risk of PCP. ** Including prednisone, prednisolone, dexamethasone, hydrocortisone, etc.
Of special note is the risk of PCP associated with the growing use of a class of monoclonal antibodies targeting the CD20 antigen on B lymphocytes, including rituximab, ofatumumab, obinutuzumab, veltuzumab, and ocrelizumab. Among them, rituximab is the first generation of this class (approved in 1997), and it is frequently used to treat certain lymphomas and leukemias as well as various autoimmune diseases. It is the first known immunosuppressive agent associated with the development of PCP resulting primarily from suppression of B cell function, as has been documented in more than 100 reports worldwide [35,53,54,84,85], while there are only sparse reports of PCP in patients receiving the newer generation of anti-CD20 agents [86]. A range of 1.5–13% incidence rates of PCP has been reported in patients treated with rituximab for various underlying diseases, such as hematologic malignancies, rheumatic diseases, and solid organ transplantation [53,84,85,87]. Among these studies is one showing a 10% incidence of PCP in patients with hematologic malignancies who were treated with rituximab but without concomitant chemotherapy or significant glucocorticoid exposure [53]. These high incidences, together with the results of animal studies [88], support the important role of B cells in the host’s immune defense against PCP.
There are multiple monoclonal antibody agents used to suppress organ transplantation rejection that can increase the risk of PCP, including alemtuzumab, belatacept, cyclosporine, tacrolimus, everolimus, and sirolimus [52,55,58,89,90]. There are also multiple monoclonal antibody agents used to treat rheumatoid arthritis that can increase the risk of PCP, including abatacept, tocilizumab, adalimumab, etanercept, and golimumab.
4.2. Cancers
Cancers are one of the earliest identified underlying conditions associated with PCP, as first reported in late 1950s in patients with leukemia and Hodgkin’s disease [91,92]. Hematological malignancies (including various leukaemias and lymphomas as well as multiple myeloma) remain the most common underlying diseases predisposing patients to PCP, accounting for ~30–80% of PCP cases among non-HIV patients [10,29,31]. Solid tumors are also closely associated with the development of PCP among non-HIV patients, accounting for 7.9–26% of cases [93,94,95,96,97,98,99,100]. A single-center retrospective study of PCP in solid tumors in Japan showed lung cancer to be the most common underlying tumor (30%), followed by breast cancer (15%) [101].
Multiple factors may contribute to the development of PCP in these cancer patients, including cancer-induced immune dysfunction, chronic use of corticosteroid therapy and other chemotherapies and immunotherapies, and radiation therapy [101,102]. There are studies demonstrating that PCP can be effectively prevented by chemoprophylaxis, as evidenced by the absence of PCP in 80 high-risk patients receiving trimethoprim-sulfamethoxazole compared to the occurrence of PCP in 21% (17/80) of patients receiving a placebo [103].
4.3. Solid Organ and Stem Cell Transplantation
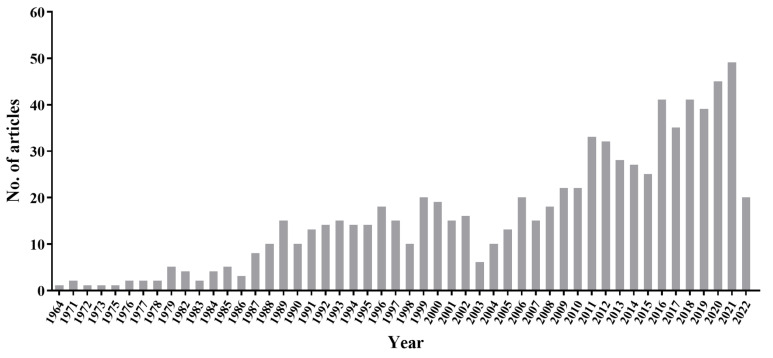
The first case of PCP in a transplant recipient was reported in 1964 from the United States in a boy following renal transplantation [47]. A search of PubMed using keywords “Pneumocystis AND Transplant” in “Title/Abstract” resulted in 751 articles from 1964 to 2022, with 75% of them published over the past two decades (Figure 2). Most of the recent cases were reported from outbreaks, as discussed below in Section 5.
Figure 2.
The number of reports on PCP in transplant recipients from 1964 to 2022 based on search of PubMed using keywords “Pneumocystis AND Transplant” or “Pneumocystis AND Transplantation” in “Title/Abstract”.
PCP is an important and dangerous cause of morbidity and mortality in transplant recipients, especially those with delayed diagnosis or no prophylaxis. Studies of transplant recipients without prophylaxis have reported a PCP incidence of 5–16%, depending on the type of transplanted organ, the transplant center, and the immunosuppressive regimens utilized (reviewed in references [10,104]). The highest incidences (10–40%) occurred among lung, combined lung-heart, and kidney transplant recipients [105,106,107]. Without prophylaxis, the first 6 months after solid organ transplantation have the highest risk for developing PCP, presumably due to intensified immune suppression to prevent graft rejection during this period. Nonetheless, PCP cases may still occur beyond 12 months after transplantation despite a full course of prophylaxis [108].
The occurrence of PCP after transplantation is associated with many additional risk factors, such as older ages, concomitant cytomegalovirus (CMV) infection, low CD4 cell counts, hypogammaglobulinemia, BK polyomavirus-related diseases, and human leukocyte antigen mismatches, as has been extensively reviewed [109,110,111].
4.4. Autoimmune and Inflammatory Diseases
PCP has been reported as a complication of a great variety of autoimmune and inflammatory diseases (AIIDs), including at least 19 individual diseases, as listed in Table S1 [4,40,70,97,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136,137,138,139,140,141,142]. Among them, the most frequently reported diseases associated with PCP are granulomatosis with polyangiitis (GPA, formerly known as Wegener’s granulomatosis), systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and inflammatory bowel disease (IBD, including Crohn’s disease and ulcerative colitis) [32,123,143]. Some AIIDs are caused by inherited genetic defects, as discussed below in the Primary Immunodeficiencies section.
GPA is a rare necrotizing vasculitis characterized by necrotizing granulomas and pauci-immune vasculitis that most commonly affects small- to medium-sized vessels in the respiratory tract and kidneys. The first case of PCP associated with GPA was reported in 1960 from a female American adult [92]. Based on multiple systematic reviews of data reported worldwide, GPA appears to be the most common AIID associated with PCP, with an estimated incidence of 6–20% [32,144,145]. The frequency of PCP in GPA in the United States and France is estimated to be 60–89 and 120 cases per 10,000 patients per year, respectively [114,124,146]. Godeau et al. [124] reported that GPA is more commonly associated with PCP (35%) than SLE (18%) and dermatomyositis (15%) among AIIDs. The main risk factors for developing PCP in GPA patients include the use of glucocorticoids and other immunosuppressive agents (such as cyclophosphamide and infliximab).
SLE patients are immunodeficient as part of their disease pathogenesis and as a result of their treatment, and are thus prone to opportunistic infections. The occurrence of PCP in SLE patients has been frequently reported since 1975 [147]. Based on the most recent review of 18 large-scale studies worldwide, the overall incidence of PCP in SLE patients is estimated to be 0.17% [148]. Most of these patients received high-dose corticosteroids and other chemotherapeutic and immunotherapeutic agents, and their disease course was complicated by lupus nephritis and lymphopenia, with low CD4 cell counts [122,149]. Pulmonary infections, especially CMV and Pneumocystis, are closely associated with increased mortality in SLE patients.
Based on reports from the 1990s from France [124] and the United States [114], the incidence of PCP among patients with RA was estimated to be 1–2 cases per 10,000 patients/year. Recent reports have shown a similar incidence in the UK [112] and a decrease incidence (0.6–4.0 PCP cases/100,000 RA patients/year) in the United States [113]. In contrast, a higher incidence of PCP has been reported from Japan among patients with RA, especially those receiving various newly developed immunotherapeutic agents, including TNFα inhibitors, T cell signaling inhibitors, and anti-IL-6 receptor antibody, with an incidence of 0.1–0.4% and mortality of 10.1–22.2% [115,116,117,150]. PCP incidence in RA is associated with multiple risk factors, such as older age, male sex, coexisting lung diseases, and therapy with methotrexate and corticosteroids [116,118,119]. Additionally, several studies have shown a relatively normal lymphocyte and CD4 cell counts in RA patients with PCP, suggesting the possibility of a different mechanism than T cell deficiency in the development of PCP in these patients [120,151].
IBD represents a group of intestinal disorders that cause chronic inflammation of the digestive tract. The two most common types of IBD are Crohn’s disease and ulcerative colitis. Almost all PCP cases in IBD patients were reported after the 1990s. The reported incidence of PCP in IBD varies from 0.03% [140] to 0.3% [136]. Based on the most recent review by Lawrence et al. [137], there have been a total of ~90 PCP cases in IBD patients reported from ~30 studies across the world. Among these patients, 88% received corticosteroids as IBD treatment, 44% received TNF inhibitors, 42% received thiopurines, and 15% received cyclosporine or tacrolimus. While CD4 cell counts were not available for most of these patients, 86% of them were lymphopenic. Once PCP has developed, the mortality rate of patients with IBD is high (18%) and strongly associated with low serum albumin levels [139].
4.5. Primary or Congenital Immunodeficiencies in Children
PCP is a significant cause of morbidity and mortality in immunocompromised children. In fact, it was the epidemic of interstitial plasma cell pneumonia in premature infants and malnourished children in the mid-20th century in Europe that led to the first recognition of Pneumocystis as a human pathogen [152,153]. Infants are at a higher risk for infection than healthy older children and adults because their immune systems are not fully developed, with limited or weakened innate and adaptive immune responses to pathogens [154,155]. Premature birth and malnourishment, along with the use of corticosteroids and other immunosuppressive agents as part of their treatment, can further compromise the immune system and increase their susceptibility to infection, including P. jirovecii infection [153,156,157,158,159,160].
The high susceptibility of infants and children to P. jirovecii is supported by the high seroprevalence of anti-Pneumocystis antibodies in healthy children early in life [161,162], and the high prevalence (100%) of P. jirovecii colonization detected by PCR in immunocompetent infants [163].
Various primary or hereditary immunodeficient diseases caused by genetic defects in germline variants in single genes can also increase the risk of PCP in children. In some early studies, primary immunodeficiency constitutes the most frequent underlying diseases associated with PCP in infants [164]. We provided a comprehensive list of primary immunodeficient diseases associated with PCP (Table 2 and Table S2 [86,165,166,167,168,169,170,171,172,173,174,175,176,177,178,179,180,181,182,183,184,185,186,187,188,189,190,191,192,193,194,195,196,197,198,199,200,201,202,203,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219]). There have been a total of 485 primary immunodeficient diseases or inborn errors of immunity (IEI) recognized by the International Union of Immunological Societies Expert Committee, which are classified into 10 major categories, including immunodeficiencies affecting cellular and humoral immunity, combined immunodeficiencies with associated or syndromic features, predominantly antibody deficiencies, diseases of immune dysregulation, congenital defects of phagocyte number or function, defects in intrinsic and innate immunity, autoinflammatory disorders, complement deficiencies, bone marrow failure, and phenocopies of inborn errors of immunity [220]. Out of these 485 diseases, 44 from nine categories (without the last one) have been associated with PCP, including 13 (30%) from immunodeficiencies affecting cellular and humoral immunity, and another 13 (30%) from combined immunodeficiencies with associated or syndromic features. More than half of the 44 diseases associated with PCP were reported in the past 5 years (Table S2). While individually rare, the cumulative number of individuals with these inherited diseases poses a significant health burden due to their prevalence of 1–5 cases per 1000 people and an annual increase in ~20 new types of genetic defect [220]. Children with these diseases may require long-term immunosuppressive therapy or stem cell transplantation, which can further increase their risk of developing PCP.
Table 2.
Primary immunodeficiencies associated with PCP.
| Immunodeficiency Category (according to the Classification by the Inborn Errors of Immunity Committee 2022 [220]) | Genetic Defects |
|---|---|
|
|
| T-B+ SCID | IL2RG, JAK3, ADA |
| CID generally less profound than SCID | CARD11, CD40, CD40LG, DOCK8, IKBKB, IKZF1, IL21R, MALT1, RFXANK, ZAP70 |
|
|
| DNA repair defects other than those in Category I | DNMT3B, ZBTB24 |
| Hyper IgE syndromes (HIES) | STAT3 |
| Defects of vitamin B12 and folate metabolism | MTHFD1, SLC46A1, TCN2 |
| Anhidrotic ectodermodysplasia with immunodeficiency | IKBKB, IKBKG |
| Calcium channel defects | ORAI1 |
| Other combined immunodeficiencies with syndromic features | IKZF3, KMT2A, SKIV2L, SP110 |
|
|
| Agammaglobulinemia | BTK |
| Common variable immune deficiency | NFKB1 |
|
|
| Regulatory T cell defects | CTLA4 |
|
|
| Defects of motility | CFTR |
| Defects of respiratory burst | CYBB, G6PD |
| Other non-lymphoid defects | GATA2 |
|
|
| Predisposition to severe viral infection | NOS2 |
| Predisposition to mucocutaneous candidiasis | IL17RA, STAT1 |
| Other inborn errors of immunity related to leukocytes | IRF4 |
|
IFIH1, IL36RN, TNFRSF1A |
|
C7 |
|
RTEL1, TERC, TP53 |
Details on genetic defects and references for PCP in patients with the genetic defects shown are provided in Supplemental Table S2. This table excludes genetic defects without reports of PCP clinical cases. SCID, severe combined immunodeficiencies; CID, combined Immunodeficiencies; CVID, common variable immune deficiency. T-B+, decreased T cell counts, and normal B cell counts but loss of function.
A serial cross-sectional study of US pediatric hospital discharges (aged 0–18 years) from 1997–2012 identified 1902 PCP cases. Cases with HIV infection decreased from 285 in 1997 to 29 cases in 2012, whereas hematologic malignancy and primary immunodeficiency became more prominent. All-cause in-hospital mortality was 12% and was particularly high among cases with hematopoietic stem cell transplant (32%) [221].
A recent single-center study of hospitalized children (<3 years old) in France found that 11% (32/279) of them were infected with P. jirovecii, with the highest positivity rate found in children with cardiopulmonary pathologies (22%), followed by SCID (19%), hyaline membrane disease (16%), asthma (9%), and acute leukaemia (6%) [222]. Of the infected children, 40% were considered colonization cases while 56% had confirmed PCP, mainly associated with SCID and other congenital diseases.
4.6. COVID-19
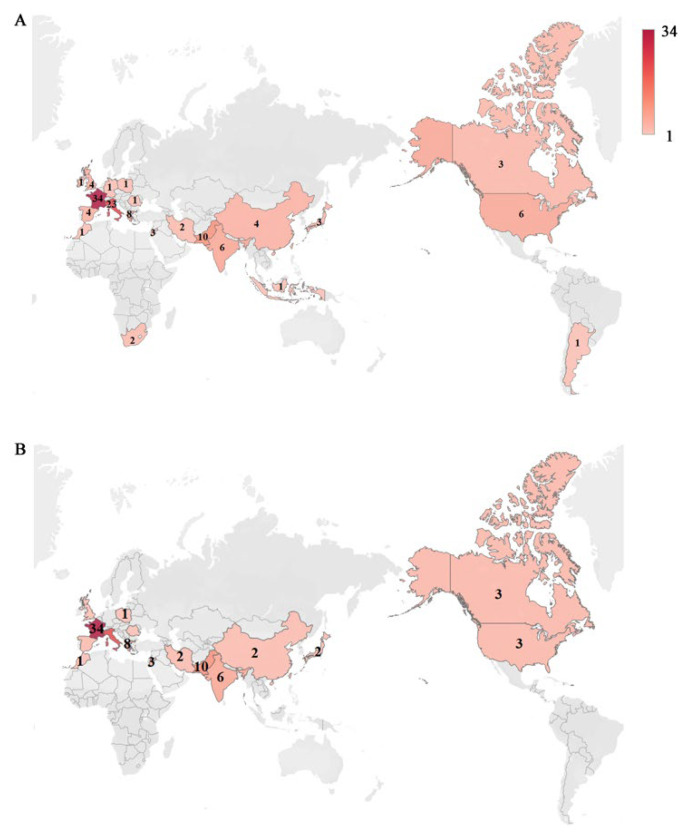
COVID-19, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), can weaken the host’s immune system and increase the risk of secondary infections with bacterial and fungal pathogens, including P. jirovecii [223,224,225]. There have been approximately 100 reports of coinfection of P. jirovecii in COVID-19 patients, with some of them reviewed recently by Gioia et al. [226] and Khodadadi et al. [227]. The largest number of coinfection cases (in non-HIV/AIDS) was reported from France (34 cases), followed by Italy (22 cases) and Pakistan (10 cases) (Figure 3 and Table S3 [15,224,225,226,228,229,230,231,232,233,234,235,236,237,238,239,240,241,242,243,244,245,246,247,248,249,250,251,252,253,254,255,256,257,258,259,260,261,262,263,264,265,266,267,268,269,270,271]).
Figure 3.
Heatmaps depicting the incidences of co-infection with P. jirovecii and SARS-CoV-2. (A) The total incidences of co-infection with P. jirovecii and SARS-CoV-2 in patients regardless of HIV/AIDS. (B) The incidences of co-infection with P. jirovecii and SARS-CoV-2 in patients without HIV/AIDS. The number on the map represents the reported number of cases. Details on statistics and related references for all cases are provided in Supplemental Table S3.
While there is evidence of significant depletion of CD4 T cells in COVID-19 patients [272] and CD4 cell deficiency is the most important driving factor for the development of PCP, as seen in AIDS, the incidence of PCP in COVID-19 appears to be far lower than that reported in AIDS. This may reflect the differences in T cell deficiency between COVID-19 and AIDS. AIDS is a chronic disease; its T cell deficiency is usually progressive and irreversible if untreated. In contrast, COVID-19 is primarily an acute illness; its T cell deficiency is generally temporary, reversible, and less severe, and, in most cases, T cell numbers and function improve as the patient recovers from the infection [273,274,275,276,277,278,279]. Another potential difference is that AIDS primarily targets CD4 T cells while COVID-19 appears to affect CD8 T cells more than CD4 T cells in mild cases of COVID-19, as evidenced by a greater reduction or cytotoxic response of CD8 T cells compared with CD4 T cells in these cases in several studies [280,281,282,283], though this trend was not supported by other studies [284,285].
While it is clear that the incidence of PCP is much lower in COVID-19 than that in AIDS, the incidence of PCP in COVID-19 seems to be underestimated for various reasons [223,226,286], including the difficulties in distinguishing between these two diseases due to their similarities in clinical symptoms and manifestations, the lack of awareness or attention to PCP, and the lack of access to sensitive diagnostic tests for PCP, particularly during the challenging pandemic era. A study using a highly sensitive qPCR assay identified a prevalence of 9% of P. jirovecii infection in critically ill COVID-19 patients [228], supporting the possibility of a high prevalence of PCP in COVID-19 patients and highlighting the importance of using a sensitive, pathogen-specific diagnostic method. Early diagnosis of PCP is crucial for the timely treatment of patients because coinfection with PCP may increase the severity and mortality of COVID-19 [286,287].
There are multiple potential risk factors for the development of PCP in COVID-19, including cytokine storm, damage to the airway epithelial barrier, mechanical ventilation, admissions to intensive care units (ICU), use of glucocorticoids and other immunosuppressive agents, underlying diseases (pulmonary diseases, acute respiratory distress syndrome, and kidney disease), and prolonged hospitalization [224,227,287]. Nonetheless, in some cases, it may be challenging to determine whether the onset of PCP in COVID-19 patients is solely due to COVID-19-induced immune defects, the administration of immunosuppressive agents during COVID-19 treatment, or underlying conditions prior to COVID-19 infection [288]. Further research is needed to better understand the role of these risk factors and thus help to develop appropriate and effective strategies to prevent or reduce the risk of PCP in COVID-19, ultimately improving patient outcomes.
4.7. Other Underlying Conditions
In addition to the underlying diseases described above, other conditions associated with a high risk of P. jirovecii infection, though not necessarily PCP, include chronic lung diseases, nephrotic diseases, diabetes mellitus, dermatologic diseases, CMV infection, BK polyomavirus-related infections, and surgical operation [109,289,290,291]. The prevalence of P. jirovecii in these conditions is highly variable depending on the patient populations. A large-scale national study of 4293 PCP patients in Japan has revealed diabetes mellitus to be the second most common underlying condition (30%) after hematologic malignancy (31%) for PCP in adults [291]. Patients with various chronic lung diseases, such as chronic obstructive pulmonary disease (COPD), interstitial lung disease (ILD), severe asthma (SA), and cystic fibrosis (CF) have a high prevalence of Pneumocystis, with most of them presumably representing colonization rather than active infection, as further discussed below.
4.8. Effects of Different Immunocompromised Conditions on Immune Functions
The host immune response plays a vital role in the development of PCP, which entails intricate interactions among numerous components, as has been extensively reviewed in recent publications by Charpentier et al. [292] and Otieno-Odhiambo et al. [293]. Immunocompetent individuals are capable of controlling and clearing Pneumocystis without experiencing symptoms, whereas immunodeficient individuals may develop severe and potentially life-threatening pneumonia. The risk for PCP depends on the interplay between epidemiologic exposure to P. jirovecii and the nature and severity of specific immunocompromised conditions. Immunocompromised conditions vary in their effects on specific components of the immune system and in the degree to which they impact its functioning. Some conditions have a broad impact on the entire immune system, while others selectively affect only particular components.
In early reported sporadic PCP cases associated with immunodeficient diseases, humoral immunodeficiency is observed more frequently than cellular immunodeficiency, leading to speculation that humoral immunodeficiency plays a primary role in driving the occurrence of PCP [294]. However, the remarkably high incidence of PCP outbreaks during the AIDS epidemic in 1980s, together with evidence from animal models, underscores the paramount significance of cellular immunodeficiency (particularly CD4 T cell deficiency) in the pathogenesis and development of PCP [292,293]. Patients with CD4 T cell counts lower than 200 cells/µL have a high risk for PCP [295].
Among all known non-HIV/AIDS immunocompromised conditions, glucocorticoid therapy, widely utilized in the treatment of almost all immunocompromised diseases, stands out as the predominant risk factor for PCP. Glucocorticoids inhibit both cellular and humoral immunity as well as innate immunity [296], so they appear to play a triple role in predisposing patients to the development of PCP. Immunodepleting monoclonal antibody agents, increasingly employed to treat cancers and AIIDs, have variable impacts on specific components of the immune system depending on their specific target; they may predominantly impair innate immunity (e.g., eculizumab and etanercept), cellular immunity (alemtuzumab, abatacept, and belatacept) or humoral immunity (rituximab and Epratuzumab), respectively [297,298]. Most of the chemotherapeutic agents used to treat cancers and AIIDs primarily suppress the production of white blood cells, particularly neutrophils, which are an essential component of innate immunity. Approximately half of the cancer patients undergoing chemotherapy develop neutropenia [299]. Neutropenia can lead to a weakened immune system and increased susceptibility to P. jirovecii infection [300].
For cancer patients, in addition to the immunosuppressive and chemotherapeutic agents discussed above, radiation therapy, especially when targeting the bone marrow or the lymph nodes, can damage all components of the immune system and impair their ability to function effectively [301]. Furthermore, many cancers, particularly blood cancers (e.g., leukemia, lymphoma), can cause extensive disruption of haematopoiesis and directly compromise the immune response [302,303]. Cancer cells may evade immune detection or inhibit immune cell function [304], thus impairing the body’s ability to mount an effective immune response against infections.
All organ transplant recipients require the use of immunosuppressive agents, which have varying effects on different components of the immune system, as discussed above. In solid organ transplantation, the primary goal of immune suppression is to suppress the T cell response and thus prevent organ rejection [305]. In stem cell transplantation, immune suppression usually targets both T cells and other components of the immune system, including B cells and natural killer cells, to prevent rejection of the transplanted stem cells and reduce the risk of graft-versus-host disease. Immune suppression in solid organ transplantation is generally more intensive and long-term compared to stem cell transplantation. As immunosuppression leaves the transplant recipients susceptible to various infections, success in transplantation requires careful management of the balance between the risks of graft rejection and the increased susceptibility to various infections, including PCP [289].
Primary immunodeficiency can affect all components of the immune system. More than half (60%) of all known primary immunodeficient diseases associated with PCP involve impairment of both cellular and humoral immunity (Table S2). Less than 10% of them predominantly affect humoral or innate immunity alone.
COVID-19 primarily targets the respiratory tract, leading to lung tissue damage and triggering overexaggerated and dysregulated pro-inflammatory and inflammatory responses. These effects extend beyond the innate defense system and have a broad impact on the adaptive immune system [306]. Patients with severe COVID-19 have marked reductions in the number of CD4 T cells, CD8 T cells, B cells, and natural killer cells, often accompanied by exhausted T cells that exhibit diminished proliferative capacity and over-production of pro-inflammatory cytokines [307]. Alongside the use of corticosteroids and other immunomodulatory agents, the defective immunity in COVID-19 patients creates an opportunity for the development of invasive fungal diseases, including PCP [308].
5. PCP Outbreaks
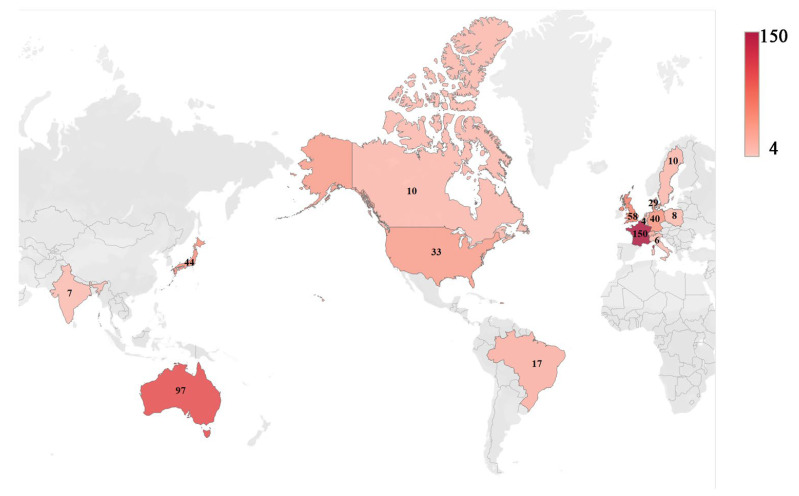
Despite the lack of a clearly identified virulence factor, PCP outbreaks occur periodically across the globe. Over the past two decades, there is an increasing trend of PCP outbreaks in immunocompromised patients without HIV/AIDS, particularly in transplant recipients, as recently reviewed by Delliere et al. [309]. The largest number of cases involved in PCP outbreaks was reported in France (150 cases), followed by Australia (97 cases) and the UK (58 cases) (Figure 4, Table S4 [58,77,107,310,311,312,313,314,315,316,317,318,319,320,321,322,323,324,325,326,327,328,329,330,331,332,333,334,335,336,337,338,339,340,341,342,343]).
Figure 4.
Heatmap depicting the incidences of PCP outbreaks in transplant patients. The number on the map represents the reported number of cases regardless of whether genotyping analysis was conducted. Details on statistics and related references for all cases are provided in Supplemental Table S4.
Types of transplantation associated with PCP outbreaks include both solid organ (kidney, heart, liver, lung, intestine, and pancreas) and hematopoietic stem cell (or bone marrow) transplantation. Outbreaks in solid organ transplant recipients account for approximately 80% of all documented PCP outbreaks [23]. These outbreaks have been documented in over a dozen countries, with the majority of cases occurring in Europe and predominantly affecting renal transplant recipients.
There has been an intense effort to investigate the epidemiology, contributing factors, and clinical management strategies of these outbreaks [23,109,309]. The transmission mode of PCP outbreaks in transplant patients has been extensively investigated by nearly 30 molecular epidemiological studies, as summarized in Table 3.
Table 3.
Published genotyping studies of PCP outbreaks in transplant patients.
| First Author [Reference] |
Year of Report |
Country | No. of Patients |
Transplanted Organs |
No. of P. jirovecii Strains/Clusters |
|---|---|---|---|---|---|
| Olsson [312] | 2001 | Sweden | 10 | Kidney | 3 |
| Hocker [313] | 2005 | Germany | 7 | Kidney | 5 |
| de Boer [314] | 2007 | Netherlands | 8 | Kidney | >5 |
| Schmoldt [315] | 2008 | Germany | 16 | Kidney | 1 |
| Yazaki [316] | 2009 | Japan | 27 | Kidney | 1 |
| Arichi [317] | 2009 | Japan | 9 | Kidney | 5 |
| Gianella [318] | 2010 | Switzerland | 20 | Kidney | 1 |
| Wynckel [319] | 2011 | France | 17 | Kidney | 2 |
| Thomas [321] | 2011 | UK | 21 * 11 * |
Kidney Kidney |
>5 >5 |
| Pliquett [322] | 2012 | Germany | 17 | Kidney | 3 |
| Brunot [323] | 2012 | France | 7 | Kidney | 1 |
| Rostvet [326] | 2013 | Denmark | 29 | Kidney, liver | 3 |
| Debourgogne [327] | 2014 | France | 13 | Kidney | 2 |
| Gits-Muselli [329] | 2015 | France | 6 | Kidney | 1 |
| Desoubeaux [330] | 2016 | France | 4 | Liver | 1 |
| Mulpuru [331] | 2016 | Canada | 10 | Kidney | 1 |
| Urabe [332] | 2016 | Japan | 8 | Kidney | 1 |
| Inkster [333] | 2017 | UK | 24 | Kidney | 2 |
| Vindrios [107] | 2017 | France | 7 | Heart | 1 |
| Robin [334] | 2017 | France | 12 | Stem cell | 5 |
| Frealle [335] | 2017 | France | 5 | Kidney | 2 |
| Alanio [336] | 2017 | France | 13 | Kidney | 1 |
| Belgium | 5 | Kidney | 1 | ||
| UK | 2 | Kidney | 1 | ||
| Wintenberger [337] and Charpentier [338] | 2017 | France | 12 | Lung, kidney, heart, liver | 9 |
| Nevez [339] | 2018 | France | 22 | Kidney | 1 |
| Ricci [340] | 2018 | Brazil | 17 | Kidney | 5 |
| Veronese [341] | 2018 | Italy | 6 | Heart | 2 |
| Szydlowicz [342] | 2019 | Poland | 8 | Kidney | >5 |
| Hosseini-Moghaddam [343] | 2020 | France | 10 | Heart, kidney, liver | 1 |
| Azar [58] | 2022 | USA | 19 | Kidney | 5 |
This is a simplified presentation to enhance visualization, with additional details (including duration of outbreaks and genotyping methods) provided in Supplemental Table S4. * Involved in two separate outbreaks in different hospitals.
In most of these studies, PCP outbreaks are linked to a predominant strain, often even a single strain, of P. jirovecii [23,344]. Strikingly, three outbreaks from distant renal transplant centers in Switzerland and Germany were linked to a single P. jirovecii strain [345,346]. These observations strongly suggest that the transplant recipients were infected by recent acquisition of P. jirovecii through person-to-person transmission. Nevertheless, some studies have demonstrated the presence of coinfections with up to seven P. jirovecii strains per patient or multiple distinct P. jirovecii strains in the same outbreaks [58,338,340].
Despite the relatively high prevalence of these outbreaks, the driving forces behind them remain unknown. The question of whether the outbreaks resulted from the introduction of specific P. jirovecii strains with enhanced virulence for transplant patients or from specific conditions that increase patients’ susceptibility to infection, such as certain immunosuppressive or rejection treatment regimens, still needs to be investigated. A better understanding of the infection mechanism and the transmission mode is expected to inform appropriate strategies for clinical management and control of PCP in transplant recipients, as discussed below.
6. Pneumocystis Colonization
Pneumocystis colonization is defined as the presence of Pneumocystis organisms in the respiratory tract (usually identified by PCR and less frequently by microscopy) without causing symptoms of acute pneumonia [33,347]. There has been increasing effort in addressing the prevalence and significance of Pneumocystis colonization, with ~80% (227/282) of PubMed reports related to this subject being published after 2010.
The reported prevalence of colonization varies greatly among current reports (0–100%), dependent largely on patients’ immune status, underlying health conditions, and ages, as well as the detection methods [33]. In general, immunocompromised patients have a higher colonization prevalence, as high as 68% in HIV-infected patients [348] and 44% in non-HIV patients received corticosteroids, compared to immunocompetent individuals (as high as 24% in adults [349]). In HIV-infected patients, severe immunosuppression (CD4 cell count ≤ 50/μL) and lack of prophylaxis increase the odds of colonization. An exceptionally high prevalence of 100% in immunocompetent individuals was reported from a study of seemingly healthy adults in Chile who died suddenly or violently using nested-PCR and a large weight of autopsied lung tissues [350].
Patients with various chronic lung diseases represent another exception to the immunocompetent population, as studies have reported a high prevalence of Pneumocystis colonization in these patients, ranging from 34% to 100%, although the sample size in some of these studies was very small [351,352,353].
Furthermore, children, particularly infants, represent a unique exception to the immunocompetent population, as their immune systems are not fully developed, which makes them more susceptible to Pneumocystis colonization, with a prevalence ranging from 32% to 100% [164,354,355].
Despite the widespread colonization in both immunocompetent and immunodeficient individuals, many questions remain unanswered regarding its mechanisms and clinical significance. The size of the colonized healthy population is expected to be substantially larger than that of the colonized immunodeficient population; this hypothesis is potentially supported by the immune evasion mechanism associated with the large major surface glycoprotein family, which is thought to be operative in immunocompetent hosts [356,357]. Nonetheless, it remains uncertain if colonization in some cases, especially in the early stage, may represent subclinical or self-limited infection, as studies of Pneumocystis-infected healthy animals have demonstrated mild pathological changes in the lungs [358,359]. Distinguishing between subclinical infection and colonization as well as latency discussed below is difficult based on the current data, and it may also depend on how these terms are defined, particularly in terms of the level of damage to the host and the host immune response, as discussed for other pathogens [360]. It also remains undetermined if Pneumocystis colonization could play a role in the progression of some chronic pulmonary diseases, particularly COPD, as hypothesized in some studies [33]. It would be necessary to determine whether colonization contributes to these diseases or is a result of certain levels of damage to the lungs due to these diseases.
Another potentially important role of colonization is that colonized patients may serve as reservoirs for transmission, as discussed above (in Section 2).
7. Reactivation of a Latent Infection Versus Acquisition of a New Infection
One of the key questions regarding the pathogenesis of PCP is whether it arises from the reactivation of a latent infection, as initially hypothesized, or from de novo acquisition of a new infection, as postulated more recently. While the reactivation hypothesis is a long-standing one, it is very difficult to prove this hypothesis as it would ideally require determining the genotypes of a strain acquired earlier in life (e.g., during primary infection as an infant) and a subsequent strain causing clinical PCP many years later. In addition, this hypothesis has been challenged by increasing evidence supporting the possibility of de novo infection. First, multiple animal studies have shown that no Pneumocystis organism or DNA can be detected in animals after recovery from experimental infection, implying that the host immune response can completely clear Pneumocystis without the organism transitioning to a latent state [358,361].
Second, several studies of patients with recurrent PCP have found genetically distinct strains between different episodes in the same patients [362,363], supporting the fact that reactivation though other cases in these studies showed identical strains between different episodes, and thereby supporting recent infection for the latter episodes.
Third, there are ample reports of detection of sulfa resistance-associated gene mutations in the dihydropteroate synthase gene of P. jirovecii from patients without prior exposure to sulfa drugs [364,365,366], suggesting de novo infection transmitted from patients with prior sulfa exposure, although the possibility of unidentified sulfa exposure cannot be ruled out.
Forth, there were over 20 outbreaks of PCP in transplant recipients (including three outbreaks from distant renal transplant centers in Switzerland and Germany) that were linked to a single or a few strains based on molecular typing, as listed in Table 3. This is very strong evidence for de novo infection via person-to-person transmission rather than reactivation of a latent infection. Of note, several studies have identified coinfections with up to seven P. jirovecii strains in the same transplant patients [58,338,340]. This may suggest a continuous acquisition of new strains from different infected individuals over time rather than reactivation of multiple latent strains.
In-depth understanding of the infection mechanisms is expected to inform appropriate strategies for clinical management and prevention of PCP. Theoretically, if reactivation of latent infection is the primary mechanism, it would not be necessary to implement respiratory isolation of PCP patients other than prophylaxis to protect susceptible individuals. If de novo infection is the primary mechanism, it would be important to prevent infected patients from spreading P. jirovecii to others, particularly to immunocompromised individuals [23], though all outbreaks would be stopped by widespread prophylaxis. Validation of these postulations is highly challenging due to the difficulty of tracking whether or not patients had a previous infection and, if so, when it occurred.
8. Prevention of PCP
At present, there is no vaccine for PCP, and respiratory isolation (by avoiding placement in the same room with PCP patients) is only recommended for susceptible patients in healthcare settings per the current USA CDC guidelines [367]. Chemical prophylaxis is highly effective in preventing PCP in high-risk immunocompromised patients without HIV/AIDS, which is similar to HIV/AIDS patients. Guidelines and the consensuses of experts for the prophylaxis of PCP in various immunocompromised conditions in different countries are listed in Table 4.
Table 4.
Guidelines and expert consensuses for the prophylaxis of PCP and other opportunistic infections in immunocompromised patients without HIV/AIDS.
| Countries | Release Years | Immunocompromised Conditions | References |
|---|---|---|---|
| Asia | 2021 | Systemic lupus erythematosus | [368] |
| Australia | 2014 | Haematological malignancies and stem cell transplantation | [369] |
| Europe | 2016 | Haematological malignancies and stem cell transplantation | [52] |
| Europe | 2022 | Autoimmune inflammatory rheumatic diseases | [370] |
| Europe | 2018 | Relapsed or refractory lymphocytic leukemia patients | [371] |
| Germany | 2021 | Haematopoietic stem cell transplantation, solid tumors, and autoimmune disorders | [372] |
| Japan | 2019 | Use of methotrexate in rheumatoid arthritis | [373] |
| Spain | 2022 | Autoimmune rheumatic diseases | [374] |
| UK | 2017 | Solid tumors in children | [375] |
| UK | 2020 | Anti-neutrophil cytoplasm antibody-associated vasculitis patients receiving Rituximab for maintenance | [376] |
| USA | 2019 | Solid organ transplantation | [111] |
| USA | 2018 | Cancers | [377] |
The first-line agent for prophylaxis is the traditional trimethoprim-sulfamethoxazole combination (cotrimoxazole). Alternative choices include dapsone, pyrimethamine-leucovorin, atovaquone, and pentamidine. Details on dosages and duration about these drugs are available from the Guidelines listed in Table 4.
9. Concluding Remarks
As a life-threatening opportunistic infection, PCP not only incurs significant healthcare costs [7] but also has profound impacts on the health and overall well-being of individuals with weakened immunity worldwide. PCP in non-HIV patients is often more severe and challenging to diagnose than PCP in HIV/AIDS patients. It is important for clinicians and health care workers to be aware of and identify various immunodeficient conditions and risk factors for PCP at an earlier stage in order to initiate timely and efficient prophylaxis or treatment. In addition, given the increasing reports of drug resistance in other fungal and bacterial infections, there is a clear need to increase efforts to investigate the epidemiology and significance of genetic mutations associated with drug resistance in PCP, as advocated recently by the WHO [15].
Acknowledgments
We greatly appreciate the assistance in electron microscopy analysis of P. murina-infected mouse lung tissues (shown in Figure 1) by Joseph Kovacs, M.D, Critical Care Medicine Department, Clinical Center; Christopher Bleck, and Erin Stempinski, Electron Microscopy Core Facility, National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, Maryland, USA. We also appreciate the assistance in graphic design by Belinda Lai from Lai Design, Fairfax, Virginia, USA.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/jof9080812/s1, Table S1: Incidence and risk factors of PCP in patients with autoimmune and inflammatory diseases (AIIDs); Table S2: Occurrence of PCP in primary immunodeficiencies or inborn errors of immunity classified by the International Union of Immunological Societies Expert Committee; Table S3: Reports of co-infection with P. jirovecii and SARS-CoV-2 in patients with or without HIV/AIDS; Table S4: Reports of PCP outbreaks in transplant patients.
Author Contributions
Conceptualization, T.X. and L.M.; literature search and review, T.X., X.K. and L.M.; writing—original draft preparation, T.X. and X.K.; writing—review and editing, T.X. and L.M.; visualization, T.X. and L.M.; supervision, L.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors have no conflict of interest in this study.
Funding Statement
This project was funded in part by the National Natural Scientific Foundation of China (Grant. No. 32200168), the Basic Research Projects of Natural Sciences in Shanxi Province (Grant. No. 20210302124039), Central Public-interest Scientific Institution Basal Research Fund (Grant. No. 2020-PT320-005), and federal funds from the Intramural Research Program of the United States National Institutes of Health Clinical Center.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Gajdusek D.C. Pneumocystis carinii as the cause of human disease: Historical perspective and magnitude of the problem: Introductory remarks. Natl. Cancer Inst. Monogr. 1976;43:1–11. [PubMed] [Google Scholar]
- 2.Walzer P.D., Perl D.P., Krogstad D.J., Rawson P.G., Schultz M.G. Pneumocystis carinii pneumonia in the United States. Epidemiologic, diagnostic, and clinical features. Ann. Intern. Med. 1974;80:83–93. doi: 10.7326/0003-4819-80-1-83. [DOI] [PubMed] [Google Scholar]
- 3.Sepkowitz K.A. Pneumocystis carinii pneumonia among patients with neoplastic disease. Semin. Respir. Infect. 1992;7:114–121. [PubMed] [Google Scholar]
- 4.Yale S.H., Limper A.H. Pneumocystis carinii pneumonia in patients without acquired immunodeficiency syndrome: Associated illness and prior corticosteroid therapy. Mayo Clin. Proc. 1996;71:5–13. doi: 10.4065/71.1.5. [DOI] [PubMed] [Google Scholar]
- 5.Arend S.M., Kroon F.P., van’t Wout J.W. Pneumocystis carinii pneumonia in patients without AIDS, 1980 through 1993. An analysis of 78 cases. Arch. Intern. Med. 1995;155:2436–2441. doi: 10.1001/archinte.1995.00430220094010. [DOI] [PubMed] [Google Scholar]
- 6.Mansharamani N.G., Garland R., Delaney D., Koziel H. Management and outcome patterns for adult Pneumocystis carinii pneumonia, 1985 to 1995: Comparison of HIV-associated cases to other immunocompromised states. Chest. 2000;118:704–711. doi: 10.1378/chest.118.3.704. [DOI] [PubMed] [Google Scholar]
- 7.Benedict K., Jackson B.R., Chiller T., Beer K.D. Estimation of direct healthcare costs of fungal diseases in the United States. Clin. Infect. Dis. 2019;68:1791–1797. doi: 10.1093/cid/ciy776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rayens E., Norris K.A. Prevalence and healthcare burden of fungal infections in the United States, 2018. Open Forum Infect. Dis. 2022;9:ofab593. doi: 10.1093/ofid/ofab593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rokas A. Evolution of the human pathogenic lifestyle in fungi. Nat. Microbiol. 2022;7:607–619. doi: 10.1038/s41564-022-01112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cordonnier C., Cesaro S., Maschmeyer G., Einsele H., Donnelly J.P., Alanio A., Hauser P.M., Lagrou K., Melchers W.J., Helweg-Larsen J., et al. Pneumocystis jirovecii pneumonia: Still a concern in patients with haematological malignancies and stem cell transplant recipients. J. Antimicrob. Chemother. 2016;71:2379–2385. doi: 10.1093/jac/dkw155. [DOI] [PubMed] [Google Scholar]
- 11.Bollee G., Sarfati C., Thiery G., Bergeron A., de Miranda S., Menotti J., de Castro N., Tazi A., Schlemmer B., Azoulay E. Clinical picture of Pneumocystis jiroveci pneumonia in cancer patients. Chest. 2007;132:1305–1310. doi: 10.1378/chest.07-0223. [DOI] [PubMed] [Google Scholar]
- 12.Asai N., Motojima S., Ohkuni Y., Matsunuma R., Nakashima K., Iwasaki T., Nakashita T., Otsuka Y., Kaneko N. Early diagnosis and treatment are crucial for the survival of Pneumocystis pneumonia patients without human immunodeficiency virus infection. J. Infect. Chemother. 2012;18:898–905. doi: 10.1007/s10156-012-0441-4. [DOI] [PubMed] [Google Scholar]
- 13.Festic E., Gajic O., Limper A.H., Aksamit T.R. Acute respiratory failure due to Pneumocystis pneumonia in patients without human immunodeficiency virus infection: Outcome and associated features. Chest. 2005;128:573–579. doi: 10.1378/chest.128.2.573. [DOI] [PubMed] [Google Scholar]
- 14.Bienvenu A.L., Traore K., Plekhanova I., Bouchrik M., Bossard C., Picot S. Pneumocystis pneumonia suspected cases in 604 non-HIV and HIV patients. Int. J. Infect. Dis. 2016;46:11–17. doi: 10.1016/j.ijid.2016.03.018. [DOI] [PubMed] [Google Scholar]
- 15.Chakravarthy K.K., Cherukuri B., Anne S., Shankar T.U., Mohan Reddy G.M., Guttikonda N. An unusual case of severe Pneumocystis jiroveci pneumonia (PJP) presenting as “recurrent cytokine storm’’ following COVID-19 infection. J. Assoc. Physicians India. 2021;69:78. [PubMed] [Google Scholar]
- 16.Ma L., Cisse O.H., Kovacs J.A. A molecular window into the biology and epidemiology of Pneumocystis spp. Clin. Microbiol. Rev. 2018;31:e00009–e00018. doi: 10.1128/CMR.00009-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Frenkel J.K. Pneumocystis jiroveci n. sp. from man: Morphology, physiology, and immunology in relation to pathology. Natl. Cancer Inst. Monogr. 1976;43:13–30. [PubMed] [Google Scholar]
- 18.Redhead S.A., Cushion M.T., Frenkel J.K., Stringer J.R. Pneumocystis and Trypanosoma cruzi: Nomenclature and typifications. J. Eukaryot. Microbiol. 2006;53:2–11. doi: 10.1111/j.1550-7408.2005.00072.x. [DOI] [PubMed] [Google Scholar]
- 19.Keely S.P., Fischer J.M., Cushion M.T., Stringer J.R. Phylogenetic identification of Pneumocystis murina sp. nov., a new species in laboratory mice. Microbiology. 2004;150:1153–1165. doi: 10.1099/mic.0.26921-0. [DOI] [PubMed] [Google Scholar]
- 20.Frenkel J.K. Pneumocystis pneumonia, an immunodeficiency-dependent disease (IDD): A critical historical overview. J. Eukaryot. Microbiol. 1999;46:89S–92S. [PubMed] [Google Scholar]
- 21.Cushion M.T., Keely S.P., Stringer J.R. Molecular and phenotypic description of Pneumocystis wakefieldiae sp. nov., a new species in rats. Mycologia. 2004;96:429–438. doi: 10.1080/15572536.2005.11832942. [DOI] [PubMed] [Google Scholar]
- 22.Dei-Cas E., Chabe M., Moukhlis R., Durand-Joly I., Aliouat E.M., Stringer J.R., Cushion M., Noel C., de Hoog G.S., Guillot J., et al. Pneumocystis oryctolagi sp. nov., an uncultured fungus causing pneumonia in rabbits at weaning: Review of current knowledge, and description of a new taxon on genotypic, phylogenetic and phenotypic bases. FEMS Microbiol. Rev. 2006;30:853–871. doi: 10.1111/j.1574-6976.2006.00037.x. [DOI] [PubMed] [Google Scholar]
- 23.Ma L., Cissé O.H., Kovacs J.A., Pneumocystis canis C Weissenbacher-Lang ex L. Ma, O.H. Cissé & J.A. Kovacs, sp. nov. Index Fungorum no. 450 at 2020. [(accessed on 20 July 2023)]. Available online: http://www.indexfungorum.org/Publications/Index%20Fungorum%20no.450.pdf.
- 24.Cushion M.T., Linke M.J., Ashbaugh A., Sesterhenn T., Collins M.S., Lynch K., Brubaker R., Walzer P.D. Echinocandin treatment of Pneumocystis pneumonia in rodent models depletes cysts leaving trophic burdens that cannot transmit the infection. PLoS ONE. 2010;5:e8524. doi: 10.1371/journal.pone.0008524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cisse O.H., Ma L., Jiang C., Snyder M., Kovacs J.A. Humans are selectively exposed to Pneumocystis jirovecii. MBio. 2020;11:e03138-19. doi: 10.1128/mBio.03138-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choukri F., Menotti J., Sarfati C., Lucet J.C., Nevez G., Garin Y.J., Derouin F., Totet A. Quantification and spread of Pneumocystis jirovecii in the surrounding air of patients with Pneumocystis pneumonia. Clin. Infect. Dis. 2010;51:259–265. doi: 10.1086/653933. [DOI] [PubMed] [Google Scholar]
- 27.Maini R., Henderson K.L., Sheridan E.A., Lamagni T., Nichols G., Delpech V., Phin N. Increasing Pneumocystis pneumonia, England, UK, 2000-2010. Emerg. Infect. Dis. 2013;19:386–392. doi: 10.3201/eid1903.121151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kolbrink B., Scheikholeslami-Sabzewari J., Borzikowsky C., von Samson-Himmelstjerna F.A., Ullmann A.J., Kunzendorf U., Schulte K. Evolving epidemiology of Pneumocystis pneumonia: Findings from a longitudinal population-based study and a retrospective multi-center study in Germany. Lancet Reg. Health-Eur. 2022;18:100400. doi: 10.1016/j.lanepe.2022.100400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu Y., Su L., Jiang S.J., Qu H. Risk factors for mortality from Pneumocystis carinii pneumonia (PCP) in non-HIV patients: A meta-analysis. Oncotarget. 2017;8:59729–59739. doi: 10.18632/oncotarget.19927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Reid A.B., Chen S.C., Worth L.J. Pneumocystis jirovecii pneumonia in non-HIV-infected patients: New risks and diagnostic tools. Curr. Opin. Infect. Dis. 2011;24:534–544. doi: 10.1097/QCO.0b013e32834cac17. [DOI] [PubMed] [Google Scholar]
- 31.Roux A., Gonzalez F., Roux M., Mehrad M., Menotti J., Zahar J.R., Tadros V.X., Azoulay E., Brillet P.Y., Vincent F., et al. Update on pulmonary Pneumocystis jirovecii infection in non-HIV patients. Med. Mal. Infect. 2014;44:185–198. doi: 10.1016/j.medmal.2014.01.007. [DOI] [PubMed] [Google Scholar]
- 32.Ghembaza A., Vautier M., Cacoub P., Pourcher V., Saadoun D. Risk factors and prevention of Pneumocystis jirovecii neumonia in patients with autoimmune and inflammatory diseases. Chest. 2020;158:2323–2332. doi: 10.1016/j.chest.2020.05.558. [DOI] [PubMed] [Google Scholar]
- 33.Morris A., Norris K.A. Colonization by Pneumocystis jirovecii and its role in disease. Clin. Microbiol. Rev. 2012;25:297–317. doi: 10.1128/CMR.00013-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sepkowitz K.A., Brown A.E., Telzak E.E., Gottlieb S., Armstrong D. Pneumocystis carinii pneumonia among patients without AIDS at a cancer hospital. JAMA. 1992;267:832–837. doi: 10.1001/jama.1992.03480060078034. [DOI] [PubMed] [Google Scholar]
- 35.Calero-Bernal M.L., Martin-Garrido I., Donazar-Ezcurra M., Limper A.H., Carmona E.M. Intermittent courses of corticosteroids also present a risk for Pneumocystis pneumonia in non-HIV patients. Can. Respir. J. 2016;2016:2464791. doi: 10.1155/2016/2464791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Baddley J.W., Cantini F., Goletti D., Gomez-Reino J.J., Mylonakis E., San-Juan R., Fernandez-Ruiz M., Torre-Cisneros J. ESCMID study group for infections in compromised hosts (ESGICH) consensus document on the safety of targeted and biological therapies: An infectious diseases perspective (Soluble immune effector molecules [I]: Anti-tumor necrosis factor-alpha agents) Clin. Microbiol. Infect. 2018;24((Suppl. 2)):S10–S20. doi: 10.1016/j.cmi.2017.12.025. [DOI] [PubMed] [Google Scholar]
- 37.Hu Y., Wang D., Zhai K., Tong Z. Transcriptomic analysis reveals significant B lymphocyte suppression in corticosteroid-treated hosts with Pneumocystis pneumonia. Am. J. Respir. Cell Mol. Biol. 2017;56:322–331. doi: 10.1165/rcmb.2015-0356OC. [DOI] [PubMed] [Google Scholar]
- 38.Climans S.A., Grunfeld E., Mason W.P., Chan K.K.W. Effectiveness and safety of Pneumocystis pneumonia prophylaxis for patients receiving temozolomide chemoradiotherapy. Neuro Oncol. 2022;24:1738–1748. doi: 10.1093/neuonc/noac072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Vos F.Y., Gijtenbeek J.M., Bleeker-Rovers C.P., van Herpen C.M. Pneumocystis jirovecii pneumonia prophylaxis during temozolomide treatment for high-grade gliomas. Crit. Rev. Oncol. Hematol. 2013;85:373–382. doi: 10.1016/j.critrevonc.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 40.Sen R.P., Walsh T.E., Fisher W., Brock N. Pulmonary complications of combination therapy with cyclophosphamide and prednisone. Chest. 1991;99:143–146. doi: 10.1378/chest.99.1.143. [DOI] [PubMed] [Google Scholar]
- 41.Lee J.Y., Kang M., Suh K.J., Kim J.W., Kim S.H., Kim J.W., Kim Y.J., Song K.H., Kim E.S., Kim H.B., et al. Pneumocystis jirovecii pneumonia in diffuse large B-cell lymphoma treated with R-CHOP. Mycoses. 2021;64:60–65. doi: 10.1111/myc.13184. [DOI] [PubMed] [Google Scholar]
- 42.Browne M.J., Hubbard S.M., Longo D.L., Fisher R., Wesley R., Ihde D.C., Young R.C., Pizzo P.A. Excess prevalence of Pneumocystis carinii pneumonia in patients treated for lymphoma with combination chemotherapy. Ann. Intern. Med. 1986;104:338–344. doi: 10.7326/0003-4819-104-3-338. [DOI] [PubMed] [Google Scholar]
- 43.Carmona E.M., Limper A.H. Update on the diagnosis and treatment of Pneumocystis pneumonia. Ther. Adv. Respir. Dis. 2011;5:41–59. doi: 10.1177/1753465810380102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hardy R., Cummings C., Faulkner M., Obianyo I. Pneumocystis carinii pneumonia following 5-fluorouracil administration. J. Natl. Med. Assoc. 1987;79:1205–1209. [PMC free article] [PubMed] [Google Scholar]
- 45.Hughes W.T., Feldman S., Aur R.J., Verzosa M.S., Hustu H.O., Simone J.V. Intensity of immunosuppressive therapy and the incidence of Pneumocystis carinii pneumonitis. Cancer. 1975;36:2004–2009. doi: 10.1002/cncr.2820360912. [DOI] [PubMed] [Google Scholar]
- 46.Havele S.A., Ellis A., Chaitoff A., Khanna U., Parambil J., Langford C.A., Fernandez A.P. Safety of trimethoprim-sulfamethoxazole for Pneumocystis jirovecii pneumonia prophylaxis in patients taking methotrexate. J. Am. Acad. Dermatol. 2021;84:166–168. doi: 10.1016/j.jaad.2020.04.040. [DOI] [PubMed] [Google Scholar]
- 47.Rifkind D., Starzl T.E., Marchioro T.L., Waddell W.R., Rowlands D.T., Jr., Hill R.B., Jr. Transplantation Pneumonia. JAMA. 1964;189:808–812. doi: 10.1001/jama.1964.03070110010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Seddik M., Melliez H., Seguy D., Viget N., Cortot A., Colombel J.F. Pneumocystis jiroveci (carinii) pneumonia after initiation of infliximab and azathioprine therapy in a patient with Crohn’s disease. Inflamm. Bowel Dis. 2005;11:618–620. doi: 10.1097/01.MIB.0000164002.32735.c2. [DOI] [PubMed] [Google Scholar]
- 49.Obeid K.M., Aguilar J., Szpunar S., Sharma M., del Busto R., Al-Katib A., Johnson L.B. Risk factors for Pneumocystis jirovecii pneumonia in patients with lymphoproliferative disorders. Clin. Lymphoma Myeloma Leuk. 2012;12:66–69. doi: 10.1016/j.clml.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 50.Schilling P.J., Vadhan-Raj S. Concurrent cytomegalovirus and Pneumocystis pneumonia after fludarabine therapy for chronic lymphocytic leukemia. N. Engl. J. Med. 1990;323:833–834. doi: 10.1056/NEJM199009203231216. [DOI] [PubMed] [Google Scholar]
- 51.Byrd J.C., Hargis J.B., Kester K.E., Hospenthal D.R., Knutson S.W., Diehl L.F. Opportunistic pulmonary infections with fludarabine in previously treated patients with low-grade lymphoid malignancies: A role for Pneumocystis carinii pneumonia prophylaxis. Am. J. Hematol. 1995;49:135–142. doi: 10.1002/ajh.2830490207. [DOI] [PubMed] [Google Scholar]
- 52.Maertens J., Cesaro S., Maschmeyer G., Einsele H., Donnelly J.P., Alanio A., Hauser P.M., Lagrou K., Melchers W.J., Helweg-Larsen J., et al. ECIL guidelines for preventing Pneumocystis jirovecii pneumonia in patients with haematological malignancies and stem cell transplant recipients. J. Antimicrob. Chemother. 2016;71:2397–2404. doi: 10.1093/jac/dkw157. [DOI] [PubMed] [Google Scholar]
- 53.Martin-Garrido I., Carmona E.M., Specks U., Limper A.H. Pneumocystis pneumonia in patients treated with rituximab. Chest. 2013;144:258–265. doi: 10.1378/chest.12-0477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rutter M., Chakravorty M., Lanyon P.C., Courtney P. Pneumocystis jirovecii following rituximab. Rheumatology. 2021;60:iii70–iii72. doi: 10.1093/rheumatology/keab040. [DOI] [PubMed] [Google Scholar]
- 55.Martin S.I., Marty F.M., Fiumara K., Treon S.P., Gribben J.G., Baden L.R. Infectious complications associated with alemtuzumab use for lymphoproliferative disorders. Clin. Infect. Dis. 2006;43:16–24. doi: 10.1086/504811. [DOI] [PubMed] [Google Scholar]
- 56.Ospina F.E., Agualimpia A., Bonilla-Abadia F., Canas C.A., Tobon G.J. Pneumocystis jirovecii pneumonia in a patient with rheumatoid arthritis treated with abatacept. Case Rep. Rheumatol. 2014;2014:835050. doi: 10.1155/2014/835050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mease P.J., Gottlieb A.B., van der Heijde D., FitzGerald O., Johnsen A., Nys M., Banerjee S., Gladman D.D. Efficacy and safety of abatacept, a T-cell modulator, in a randomised, double-blind, placebo-controlled, phase III study in psoriatic arthritis. Ann. Rheum. Dis. 2017;76:1550–1558. doi: 10.1136/annrheumdis-2016-210724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Azar M.M., Cohen E., Ma L., Cisse O.H., Gan G., Deng Y., Belfield K., Asch W., Grant M., Gleeson S., et al. Genetic and epidemiologic analyses of an outbreak of Pneumocystis jirovecii pneumonia among kidney transplant recipients in the United States. Clin. Infect. Dis. 2022;74:639–647. doi: 10.1093/cid/ciab474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Haidinger M., Hecking M., Memarsadeghi M., Weichhart T., Werzowa J., Horl W.H., Saemann M.D. Late onset Pneumocystis pneumonia in renal transplantation after long-term immunosuppression with belatacept. Transpl. Infect. Dis. 2009;11:171–174. doi: 10.1111/j.1399-3062.2009.00366.x. [DOI] [PubMed] [Google Scholar]
- 60.Bertrand D., Chavarot N., Gatault P., Garrouste C., Bouvier N., Grall-Jezequel A., Jaureguy M., Caillard S., Lemoine M., Colosio C., et al. Opportunistic infections after conversion to belatacept in kidney transplantation. Nephrol. Dial. Transplant. 2020;35:336–345. doi: 10.1093/ndt/gfz255. [DOI] [PubMed] [Google Scholar]
- 61.Kameda H., Tokuda H., Sakai F., Johkoh T., Mori S., Yoshida Y., Takayanagi N., Taki H., Hasegawa Y., Hatta K., et al. Clinical and radiological features of acute-onset diffuse interstitial lung diseases in patients with rheumatoid arthritis receiving treatment with biological agents: Importance of Pneumocystis pneumonia in Japan revealed by a multicenter study. Intern. Med. 2011;50:305–313. doi: 10.2169/internalmedicine.50.4508. [DOI] [PubMed] [Google Scholar]
- 62.Schiff M.H., Kremer J.M., Jahreis A., Vernon E., Isaacs J.D., van Vollenhoven R.F. Integrated safety in tocilizumab clinical trials. Arthritis Res. Ther. 2011;13:R141. doi: 10.1186/ar3455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vallabhaneni S., Chiller T.M. Fungal Infections and New Biologic Therapies. Curr. Rheumatol. Rep. 2016;18:29. doi: 10.1007/s11926-016-0572-1. [DOI] [PubMed] [Google Scholar]
- 64.Watanabe K., Sakai R., Koike R., Sakai F., Sugiyama H., Tanaka M., Komano Y., Akiyama Y., Mimura T., Kaneko M., et al. Clinical characteristics and risk factors for Pneumocystis jirovecii pneumonia in patients with rheumatoid arthritis receiving adalimumab: A retrospective review and case-control study of 17 patients. Mod. Rheumatol. 2013;23:1085–1093. doi: 10.3109/s10165-012-0796-5. [DOI] [PubMed] [Google Scholar]
- 65.Desales A.L., Mendez-Navarro J., Mendez-Tovar L.J., Ortiz-Olvera N.X., Cullen G., Ocampo J., Lemus W., Tun A.E., Mayoral-Zavala A., Dehesa-Violante M. Pneumocystosis in a patient with Crohn’s disease treated with combination therapy with adalimumab. J. Crohn’s Colitis. 2012;6:483–487. doi: 10.1016/j.crohns.2011.10.012. [DOI] [PubMed] [Google Scholar]
- 66.Tanaka M., Sakai R., Koike R., Komano Y., Nanki T., Sakai F., Sugiyama H., Matsushima H., Kojima T., Ohta S., et al. Pneumocystis jirovecii pneumonia associated with etanercept treatment in patients with rheumatoid arthritis: A retrospective review of 15 cases and analysis of risk factors. Mod. Rheumatol. 2012;22:849–858. doi: 10.3109/s10165-012-0615-z. [DOI] [PubMed] [Google Scholar]
- 67.Takeuchi T., Kameda H. The Japanese experience with biologic therapies for rheumatoid arthritis. Nat. Rev. Rheumatol. 2010;6:644–652. doi: 10.1038/nrrheum.2010.154. [DOI] [PubMed] [Google Scholar]
- 68.Tragiannidis A., Kyriakidis I., Zundorf I., Groll A.H. Invasive fungal infections in pediatric patients treated with tumor necrosis alpha (TNF-alpha) inhibitors. Mycoses. 2017;60:222–229. doi: 10.1111/myc.12576. [DOI] [PubMed] [Google Scholar]
- 69.Tanaka Y., Senoo A., Fujii H., Baker D. Evaluation of golimumab for the treatment of patients with active rheumatoid arthritis. Expert. Opin. Drug Metab. Toxicol. 2016;12:319–326. doi: 10.1517/17425255.2016.1146682. [DOI] [PubMed] [Google Scholar]
- 70.Kaur N., Mahl T.C. Pneumocystis jiroveci (carinii) pneumonia after infliximab therapy: A review of 84 cases. Dig. Dis. Sci. 2007;52:1481–1484. doi: 10.1007/s10620-006-9250-x. [DOI] [PubMed] [Google Scholar]
- 71.Harigai M., Koike R., Miyasaka N. Pneumocystis Pneumonia Under Anti-Tumor Necrosis Factor Therapy (PAT) Study, Group. Pneumocystis pneumonia associated with infliximab in Japan. N. Engl. J. Med. 2007;357:1874–1876. doi: 10.1056/NEJMc070728. [DOI] [PubMed] [Google Scholar]
- 72.Markus M.B. Cyclosporin A and Pneumocystis pneumonia. Med. J. Aust. 1985;143:91. doi: 10.5694/j.1326-5377.1985.tb122820.x. [DOI] [PubMed] [Google Scholar]
- 73.Franson T.R., Kauffman H.M., Jr., Adams M.B., Lemann J., Jr., Cabrera E., Hanacik L. Cyclosporine therapy and refractory Pneumocystis carinii pneumonia. A potential association. Arch. Surg. 1987;122:1034–1035. doi: 10.1001/archsurg.1987.01400210072010. [DOI] [PubMed] [Google Scholar]
- 74.Faure E., Lionet A., Kipnis E., Noel C., Hazzan M. Risk factors for Pneumocystis pneumonia after the first 6 months following renal transplantation. Transpl. Infect. Dis. 2017;19:e12735. doi: 10.1111/tid.12735. [DOI] [PubMed] [Google Scholar]
- 75.Matsuoka K., Saito E., Fujii T., Takenaka K., Kimura M., Nagahori M., Ohtsuka K., Watanabe M. Tacrolimus for the Treatment of Ulcerative Colitis. Intest. Res. 2015;13:219–226. doi: 10.5217/ir.2015.13.3.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Escher M., Stange E.F., Herrlinger K.R. Two cases of fatal Pneumocystis jirovecii pneumonia as a complication of tacrolimus therapy in ulcerative colitis—A need for prophylaxis. J. Crohn’s Colitis. 2010;4:606–609. doi: 10.1016/j.crohns.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 77.Miguel Montanes R., Elkrief L., Hajage D., Houssel P., Fantin B., Francoz C., Dreyfuss D., Ricard J.D., Durand F. An outbreak of Pneumocytis jirovecii pneumonia among liver transplant recipients. Transpl. Infect. Dis. 2018;20:e12956. doi: 10.1111/tid.12956. [DOI] [PubMed] [Google Scholar]
- 78.Hu Y.N., Lee N.Y., Roan J.N., Hsu C.H., Luo C.Y. High-dose calcineurin inhibitor-free everolimus as a maintenance regimen for heart transplantation may be a risk factor for Pneumocystis pneumonia. Transpl. Infect. Dis. 2017;19:e12709. doi: 10.1111/tid.12709. [DOI] [PubMed] [Google Scholar]
- 79.Loron M.C., Grange S., Guerrot D., Di Fiore F., Freguin C., Hanoy M., Le Roy F., Poussard G., Etienne I., Legallicier B., et al. Pneumocystis jirovecii pneumonia in everolimus-treated renal cell carcinoma. J. Clin. Oncol. 2015;33:e45–e47. doi: 10.1200/JCO.2013.49.9277. [DOI] [PubMed] [Google Scholar]
- 80.Nakamura M., Matsunuma R., Yamaguchi K., Hayami R., Tsuneizumi M. Pneumocystis pneumonia and acute kidney injury induced by everolimus treatment in a patient with metastatic breast cancer. Case Rep. Oncol. 2020;13:170–175. doi: 10.1159/000505909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Shetty A.K. Pneumocystis jirovecii pneumonia: A potential complication of sirolimus therapy. J. Paediatr. Child. Health. 2019;55:484. doi: 10.1111/jpc.14392. [DOI] [PubMed] [Google Scholar]
- 82.Russell T.B., Rinker E.K., Dillingham C.S., Givner L.B., McLean T.W. Pneumocystis jirovecii pneumonia during sirolimus therapy for kaposiform hemangioendothelioma. Pediatrics. 2018;141:S421–S424. doi: 10.1542/peds.2017-1044. [DOI] [PubMed] [Google Scholar]
- 83.Ghadimi M., Mohammadpour Z., Dashti-Khavidaki S., Milajerdi A. m-TOR inhibitors and risk of Pneumocystis pneumonia after solid organ transplantation: A systematic review and meta-analysis. Eur. J. Clin. Pharmacol. 2019;75:1471–1480. doi: 10.1007/s00228-019-02730-0. [DOI] [PubMed] [Google Scholar]
- 84.Kolstad A., Holte H., Fossa A., Lauritzsen G.F., Gaustad P., Torfoss D. Pneumocystis jirovecii pneumonia in B-cell lymphoma patients treated with the rituximab-CHOEP-14 regimen. Haematologica. 2007;92:139–140. doi: 10.3324/haematol.10564. [DOI] [PubMed] [Google Scholar]
- 85.Park J.W., Curtis J.R., Jun K.I., Kim T.M., Heo D.S., Ha J., Suh K.S., Lee K.W., Lee H., Yang J., et al. Primary prophylaxis for Pneumocystis jirovecii pneumonia in patients receiving rituximab. Chest. 2022;161:1201–1210. doi: 10.1016/j.chest.2021.11.007. [DOI] [PubMed] [Google Scholar]
- 86.Jones J.A., Robak T., Brown J.R., Awan F.T., Badoux X., Coutre S., Loscertales J., Taylor K., Vandenberghe E., Wach M., et al. Efficacy and safety of idelalisib in combination with ofatumumab for previously treated chronic lymphocytic leukaemia: An open-label, randomised phase 3 trial. Lancet Haematol. 2017;4:e114–e126. doi: 10.1016/S2352-3026(17)30019-4. [DOI] [PubMed] [Google Scholar]
- 87.Barreto J.N., Ice L.L., Thompson C.A., Tosh P.K., Osmon D.R., Dierkhising R.A., Plevak M.F., Limper A.H. Low incidence of pneumocystis pneumonia utilizing PCR-based diagnosis in patients with B-cell lymphoma receiving rituximab-containing combination chemotherapy. Am. J. Hematol. 2016;91:1113–1117. doi: 10.1002/ajh.24499. [DOI] [PubMed] [Google Scholar]
- 88.Lund F.E., Hollifield M., Schuer K., Lines J.L., Randall T.D., Garvy B.A. B cells are required for generation of protective effector and memory CD4 cells in response to Pneumocystis lung infection. J. Immunol. 2006;176:6147–6154. doi: 10.4049/jimmunol.176.10.6147. [DOI] [PubMed] [Google Scholar]
- 89.Mikulska M., Lanini S., Gudiol C., Drgona L., Ippolito G., Fernandez-Ruiz M., Salzberger B. ESCMID Study Group for Infections in Compromised Hosts (ESGICH) Consensus Document on the safety of targeted and biological therapies: An infectious diseases perspective (Agents targeting lymphoid cells surface antigens [I]: CD19, CD20 and CD52) Clin. Microbiol. Infect. 2018;24((Suppl. 2)):S71–S82. doi: 10.1016/j.cmi.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 90.Lau A.Y., Lui G.C.Y., Chan K.P., Au C., Mok V.C.T., Ziemssen T. Pneumocystis pneumonia in a patient treated with alemtuzumab for relapsing multiple sclerosis. Mult. Scler. Relat. Disord. 2020;38:101503. doi: 10.1016/j.msard.2019.101503. [DOI] [PubMed] [Google Scholar]
- 91.Dustin P., Jr., Maurus R. Fatal pneumopathy caused by “Pneumocystis carinii” in a leukemic child treated with prednisone. Bull. L’academie R. Med. Belg. 1959;24:566–579. [PubMed] [Google Scholar]
- 92.Symmers W.S. Generalized cytomegalic inclusion-body disease associated with Pneumocystis pneumonia in adults. A report of three cases. with Wegener’s granulomatosis. thrombotic purpura, and Hodgkin’s disease as predisposing conditions. J. Clin. Pathol. 1960;13:1–21. doi: 10.1136/jcp.13.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lemiale V., Debrumetz A., Delannoy A., Alberti C., Azoulay E. Adjunctive steroid in HIV-negative patients with severe Pneumocystis pneumonia. Respir. Res. 2013;14:87. doi: 10.1186/1465-9921-14-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Gaborit B.J., Tessoulin B., Lavergne R.A., Morio F., Sagan C., Canet E., Lecomte R., Leturnier P., Deschanvres C., Khatchatourian L., et al. Outcome and prognostic factors of Pneumocystis jirovecii pneumonia in immunocompromised adults: A prospective observational study. Ann. Intensive Care. 2019;9:131. doi: 10.1186/s13613-019-0604-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hardak E., Neuberger A., Yigla M., Berger G., Finkelstein R., Sprecher H., Oren I. Outcome of Pneumocystis jirovecii pneumonia diagnosed by polymerase chain reaction in patients without human immunodeficiency virus infection. Respirology. 2012;17:681–686. doi: 10.1111/j.1440-1843.2012.02158.x. [DOI] [PubMed] [Google Scholar]
- 96.Roblot F., Godet C., Le Moal G., Garo B., Faouzi Souala M., Dary M., De Gentile L., Gandji J.A., Guimard Y., Lacroix C., et al. Analysis of underlying diseases and prognosis factors associated with Pneumocystis carinii pneumonia in immunocompromised HIV-negative patients. Eur. J. Clin. Microbiol. Infect. Dis. 2002;21:523–531. doi: 10.1007/s10096-002-0758-5. [DOI] [PubMed] [Google Scholar]
- 97.Fillatre P., Decaux O., Jouneau S., Revest M., Gacouin A., Robert-Gangneux F., Fresnel A., Guiguen C., Le Tulzo Y., Jego P., et al. Incidence of Pneumocystis jiroveci pneumonia among groups at risk in HIV-negative patients. Am. J. Med. 2014;127:1242.e11–1242.e17. doi: 10.1016/j.amjmed.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 98.Kim S.J., Lee J., Cho Y.J., Park Y.S., Lee C.H., Yoon H.I., Lee S.M., Yim J.J., Lee J.H., Yoo C.G., et al. Prognostic factors of Pneumocystis jirovecii pneumonia in patients without HIV infection. J. Infect. 2014;69:88–95. doi: 10.1016/j.jinf.2014.02.015. [DOI] [PubMed] [Google Scholar]
- 99.Roblot F., Le Moal G., Kauffmann-Lacroix C., Bastides F., Boutoille D., Verdon R., Godet C., Tattevin P., Groupe d’Etudes et de Recherche en Infectiologie Clinique du Centre Ouest Pneumocystis jirovecii pneumonia in HIV-negative patients: A prospective study with focus on immunosuppressive drugs and markers of immune impairment. Scand. J. Infect. Dis. 2014;46:210–214. doi: 10.3109/00365548.2013.865142. [DOI] [PubMed] [Google Scholar]
- 100.Kofteridis D.P., Valachis A., Velegraki M., Antoniou M., Christofaki M., Vrentzos G.E., Andrianaki A.M., Samonis G. Predisposing factors, clinical characteristics and outcome of Pneumonocystis jirovecii pneumonia in HIV-negative patients. J. Infect. Chemother. 2014;20:412–416. doi: 10.1016/j.jiac.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 101.Takeda K., Harada S., Hayama B., Hoashi K., Enokida T., Sasaki T., Okamoto K., Nakano K., Ohkushi D. Clinical characteristics and risk factors associated with Pneumocystis jirovecii infection in patients with solid tumors: Study of thirteen-year medical records of a large cancer center. BMC Cancer. 2021;21:987. doi: 10.1186/s12885-021-08727-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lee E.H., Kim E.Y., Lee S.H., Roh Y.H., Leem A.Y., Song J.H., Kim S.Y., Chung K.S., Jung J.Y., Kang Y.A., et al. Risk factors and clinical characteristics of Pneumocystis jirovecii pneumonia in lung cancer. Sci. Rep. 2019;9:2094. doi: 10.1038/s41598-019-38618-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Hughes W.T., Kuhn S., Chaudhary S., Feldman S., Verzosa M., Aur R.J., Pratt C., George S.L. Successful chemoprophylaxis for Pneumocystis carinii pneumonitis. N. Engl. J. Med. 1977;297:1419–1426. doi: 10.1056/NEJM197712292972602. [DOI] [PubMed] [Google Scholar]
- 104.Fishman J.A. Prevention of infection due to Pneumocystis carinii. Antimicrob. Agents Chemother. 1998;42:995–1004. doi: 10.1128/AAC.42.5.995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gordon S.M., LaRosa S.P., Kalmadi S., Arroliga A.C., Avery R.K., Truesdell-LaRosa L., Longworth D.L. Should prophylaxis for Pneumocystis carinii pneumonia in solid organ transplant recipients ever be discontinued? Clin. Infect. Dis. 1999;28:240–246. doi: 10.1086/515126. [DOI] [PubMed] [Google Scholar]
- 106.Martin S.I., Fishman J.A., Practice ASTIDCo Pneumocystis pneumonia in solid organ transplantation. Am. J. Transplant. 2013;13((Suppl. 4)):272–279. doi: 10.1111/ajt.12119. [DOI] [PubMed] [Google Scholar]
- 107.Vindrios W., Argy N., Le Gal S., Lescure F.X., Massias L., Le M.P., Wolff M., Yazdanpanah Y., Nevez G., Houze S., et al. Outbreak of Pneumocystis jirovecii Infection Among Heart Transplant Recipients: Molecular Investigation and Management of an Interhuman Transmission. Clin. Infect. Dis. 2017;65:1120–1126. doi: 10.1093/cid/cix495. [DOI] [PubMed] [Google Scholar]
- 108.Hosseini-Moghaddam S.M., Shokoohi M., Singh G., Dufresne S.F., Boucher A., Jevnikar A., Prasad G.V.R., Shoker A., Kabbani D., Hebert M.J., et al. A multicenter case-control study of the effect of acute rejection and cytomegalovirus infection on Pneumocystis pneumonia in solid organ transplant recipients. Clin. Infect. Dis. 2019;68:1320–1326. doi: 10.1093/cid/ciy682. [DOI] [PubMed] [Google Scholar]
- 109.Permpalung N., Kittipibul V., Mekraksakit P., Rattanawong P., Nematollahi S., Zhang S.X., Steinke S.M. A comprehensive evaluation of risk factors for Pneumocystis jirovecii pneumonia in adult solid organ transplant recipients: A systematic review and meta-analysis. Transplantation. 2021;105:2291–2306. doi: 10.1097/TP.0000000000003576. [DOI] [PubMed] [Google Scholar]
- 110.Brakemeier S., Pfau A., Zukunft B., Budde K., Nickel P. Prophylaxis and treatment of Pneumocystis jirovecii pneumonia after solid organ transplantation. Pharmacol. Res. 2018;134:61–67. doi: 10.1016/j.phrs.2018.06.010. [DOI] [PubMed] [Google Scholar]
- 111.Fishman J.A., Gans H.A.S.T. Pneumocystis jiroveci in solid organ transplantation: Guidelines from the American Society of transplantation Infectious Diseases Community of Practice. Clin. Transplant. 2019;33:e13587. doi: 10.1111/ctr.13587. [DOI] [PubMed] [Google Scholar]
- 112.Bruce E.S., Kearsley-Fleet L., Watson K.D., Symmons D.P., Hyrich K.L. Risk of Pneumocystis jirovecii pneumonia in patients with rheumatoid arthritis treated with inhibitors of tumour necrosis factor alpha: Results from the British Society for Rheumatology Biologics Register for Rheumatoid Arthritis. Rheumatology. 2016;55:1336–1337. doi: 10.1093/rheumatology/kew200. [DOI] [PubMed] [Google Scholar]
- 113.Louie G.H., Wang Z., Ward M.M. Trends in hospitalizations for Pneumocystis jiroveci pneumonia among patients with rheumatoid arthritis in the US: 1996–2007. Arthritis Rheum. 2010;62:3826–3827. doi: 10.1002/art.27735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ward M.M., Donald F. Pneumocystis carinii pneumonia in patients with connective tissue diseases: The role of hospital experience in diagnosis and mortality. Arthritis Rheum. 1999;42:780–789. doi: 10.1002/1529-0131(199904)42:43.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 115.Mori S., Sugimoto M. Pneumocystis jirovecii pneumonia in rheumatoid arthritis patients: Risks and prophylaxis recommendations. Clin. Med. Insights Circ. Respir. Pulm. Med. 2015;9:29–40. doi: 10.4137/CCRPM.S23286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Sonomoto K., Tanaka H., Nguyen T.M., Yoshinari H., Nakano K., Nakayamada S., Tanaka Y. Prophylaxis against pneumocystis pneumonia in rheumatoid arthritis patients treated with b/tsDMARDs: Insights from 3,787 cases in FIRST registry. Rheumatology. 2021;61:1831–1840. doi: 10.1093/rheumatology/keab647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mimori T., Harigai M., Atsumi T., Fujii T., Kuwana M., Matsuno H., Momohara S., Takei S., Tamura N., Takasaki Y., et al. Safety and effectiveness of 24-week treatment with iguratimod, a new oral disease-modifying antirheumatic drug, for patients with rheumatoid arthritis: Interim analysis of a post-marketing surveillance study of 2679 patients in Japan. Mod. Rheumatol. 2017;27:755–765. doi: 10.1080/14397595.2016.1265695. [DOI] [PubMed] [Google Scholar]
- 118.Hashimoto A., Suto S., Horie K., Fukuda H., Nogi S., Iwata K., Tsuno H., Ogihara H., Kawakami M., Komiya A., et al. Incidence and Risk Factors for Infections Requiring Hospitalization, Including Pneumocystis Pneumonia, in Japanese Patients with Rheumatoid Arthritis. Int. J. Rheumatol. 2017;2017:6730812. doi: 10.1155/2017/6730812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Yukawa K., Nagamoto Y., Watanabe H., Funaki M., Iwahashi M., Yamana J., Sasaki R., Yamana S. Risk Factors for Pneumocystis jirovecii pneumonia in patients with rheumatoid arthritis and a prophylactic indication of trimethoprim/sulfamethoxazole. J. Clin. Rheumatol. 2018;24:355–360. doi: 10.1097/RHU.0000000000000731. [DOI] [PubMed] [Google Scholar]
- 120.Tokuda H., Sakai F., Yamada H., Johkoh T., Imamura A., Dohi M., Hirakata M., Yamada T., Kamatani N., Kikuchi Y., et al. Clinical and radiological features of Pneumocystis pneumonia in patients with rheumatoid arthritis, in comparison with methotrexate pneumonitis and Pneumocystis pneumonia in acquired immunodeficiency syndrome: A multicenter study. Intern. Med. 2008;47:915–923. doi: 10.2169/internalmedicine.47.0702. [DOI] [PubMed] [Google Scholar]
- 121.Mecoli C.A., Saylor D., Gelber A.C., Christopher-Stine L. Pneumocystis jiroveci pneumonia in rheumatic disease: A 20-year single-centre experience. Clin. Exp. Rheumatol. 2017;35:671–673. [PubMed] [Google Scholar]
- 122.Hsu H.C., Chang Y.S., Hou T.Y., Chen L.F., Hu L.F., Lin T.M., Chiou C.S., Tsai K.L., Lin S.H., Kuo P.I., et al. Pneumocystis jirovecii pneumonia in autoimmune rheumatic diseases: A nationwide population-based study. Clin. Rheumatol. 2021;40:3755–3763. doi: 10.1007/s10067-021-05660-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Li Y., Ghannoum M., Deng C., Gao Y., Zhu H., Yu X., Lavergne V. Pneumocystis pneumonia in patients with inflammatory or autoimmune diseases: Usefulness of lymphocyte subtyping. Int. J. Infect. Dis. 2017;57:108–115. doi: 10.1016/j.ijid.2017.02.010. [DOI] [PubMed] [Google Scholar]
- 124.Godeau B., Coutant-Perronne V., Le Thi Huong D., Guillevin L., Magadur G., De Bandt M., Dellion S., Rossert J., Rostoker G., Piette J.C., et al. Pneumocystis carinii pneumonia in the course of connective tissue disease: Report of 34 cases. J. Rheumatol. 1994;21:246–251. [PubMed] [Google Scholar]
- 125.Lertnawapan R., Totemchokchyakarn K., Nantiruj K., Janwityanujit S. Risk factors of Pneumocystis jeroveci pneumonia in patients with systemic lupus erythematosus. Rheumatol. Int. 2009;29:491–496. doi: 10.1007/s00296-008-0721-6. [DOI] [PubMed] [Google Scholar]
- 126.Wang Z.G., Liu X.M., Wang Q., Chen N.F., Tong S.Q. A retrospective study of patients with systemic lupus erythematosus combined with Pneumocystis jiroveci pneumonia treated with caspofungin and trimethoprim/sulfamethoxazole. Medicine. 2019;98:e15997. doi: 10.1097/MD.0000000000015997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gupta D., Zachariah A., Roppelt H., Patel A.M., Gruber B.L. Prophylactic antibiotic usage for Pneumocystis jirovecii pneumonia in patients with systemic lupus erythematosus on cyclophosphamide: A survey of US rheumatologists and the review of literature. J. Clin. Rheumatol. 2008;14:267–272. doi: 10.1097/RHU.0b013e31817a7e30. [DOI] [PubMed] [Google Scholar]
- 128.Yeo K.J., Chen H.H., Chen Y.M., Lin C.H., Chen D.Y., Lai C.M., Chao W.C. Hydroxychloroquine may reduce risk of Pneumocystis pneumonia in lupus patients: A Nationwide, population-based case-control study. BMC Infect. Dis. 2020;20:112. doi: 10.1186/s12879-020-4826-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Lahiff C., Khiaron O.B., Nolan N., Chadwick G.A. Pneumocystis carinii pneumonia in a patient on etanercept for psoriatic arthritis. Ir. J. Med. Sci. 2007;176:309–311. doi: 10.1007/s11845-007-0087-x. [DOI] [PubMed] [Google Scholar]
- 130.Jobanputra P. Polyarteritis nodosa. Diagnostic challenges in a patient with cutaneous vasculitis, psoriasis, psoriatic arthritis and pancytopenia: Fatal progression after treatment with G-CSF. Oxf. Med. Case Reports. 2016;2016:86–90. doi: 10.1093/omcr/omw025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wen Y.K., Chen M.L. Remission of nephrotic membranous glomerulonephritis after high-dose trimethoprim-sulfamethoxazole treatment for pneumocystis jiroveci pneumonia. Clin. Nephrol. 2007;68:99–103. doi: 10.5414/CNP68099. [DOI] [PubMed] [Google Scholar]
- 132.Yang C.Y., Yang A.H., Yang W.C., Lin C.C. Risk factors for Pneumocystis jiroveci pneumonia in glomerulonephritis patients receiving immunosuppressants. Intern. Med. 2012;51:2869–2875. doi: 10.2169/internalmedicine.51.6774. [DOI] [PubMed] [Google Scholar]
- 133.Hernandez Roca J.J., Pelaez Ballesta A., Lara G., Soto S., Mene Fenor E. Diffuse alveolar hemorrhage associated with Henoch-Schonlein purpura and Pneumocystis jirovecii infection: A case report. Rev. Clin. Esp. 2015;215:e1–e4. doi: 10.1016/j.rce.2014.07.011. [DOI] [PubMed] [Google Scholar]
- 134.Bungo M.W., Beetham W.P., Jr. Arthritis rounds. Pneumocystis carinii associated with polyarteritis and immunosuppressive therapy. Arthritis Rheum. 1977;20:1142–1146. doi: 10.1002/art.1780200516. [DOI] [PubMed] [Google Scholar]
- 135.Sabbagh S.E., Neely J., Chow A., DeGuzman M., Lai J., Lvovich S., McGrath T., Pereira M., Pinal-Fernandez I., Roberts J., et al. Risk factors associated with Pneumocystis jirovecii pneumonia in juvenile myositis in North America. Rheumatology. 2021;60:829–836. doi: 10.1093/rheumatology/keaa436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Cotter T.G., Gathaiya N., Catania J., Loftus E.V., Jr., Tremaine W.J., Baddour L.M., Harmsen W.S., Zinsmeister A.R., Sandborn W.J., Limper A.H., et al. Low risk of pneumonia from Pneumocystis jirovecii infection in patients with inflammatory bowel disease receiving immune suppression. Clin. Gastroenterol. Hepatol. 2017;15:850–856. doi: 10.1016/j.cgh.2016.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lawrence S.J., Sadarangani M., Jacobson K. Pneumocystis jirovecii pneumonia in pediatric inflammatory bowel disease: A case report and literature review. Front. Pediatr. 2017;5:161. doi: 10.3389/fped.2017.00161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Schwartz J., Stein D.J., Feuerstein J.D. Comprehensive national inpatient Sample data reveals low but rising Pneumocystis jiroveci pneumonia risk in inflammatory bowel disease patients. Ann. Gastroenterol. 2022;35:260–266. doi: 10.20524/aog.2022.0713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Yoshida A., Kamata N., Yamada A., Yokoyama Y., Omori T., Fujii T., Hayashi R., Kinjo T., Matsui A., Fukata N., et al. Risk factors for mortality in Pneumocystis jirovecii pneumonia in patients with inflammatory bowel disease. Inflamm. Intest. Dis. 2019;3:167–172. doi: 10.1159/000495035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Long M.D., Farraye F.A., Okafor P.N., Martin C., Sandler R.S., Kappelman M.D. Increased risk of pneumocystis jiroveci pneumonia among patients with inflammatory bowel disease. Inflamm. Bowel Dis. 2013;19:1018–1024. doi: 10.1097/MIB.0b013e3182802a9b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Nam K., Park S.H., Lee J., Jo S., Kim S.O., Noh S., Park J.C., Kim J.Y., Kim J., Ham N.S., et al. Incidence and risk factors of Pneumocystis jirovecii pneumonia in Korean patients with inflammatory bowel disease. J. Gastroenterol. Hepatol. 2020;35:218–224. doi: 10.1111/jgh.14832. [DOI] [PubMed] [Google Scholar]
- 142.Lawrance I.C., Radford-Smith G.L., Bampton P.A., Andrews J.M., Tan P.K., Croft A., Gearry R.B., Florin T.H. Serious infections in patients with inflammatory bowel disease receiving anti-tumor-necrosis-factor-alpha therapy: An Australian and New Zealand experience. J. Gastroenterol. Hepatol. 2010;25:1732–1738. doi: 10.1111/j.1440-1746.2010.06407.x. [DOI] [PubMed] [Google Scholar]
- 143.Baulier G., Issa N., Gabriel F., Accoceberry I., Camou F., Duffau P. Guidelines for prophylaxis of Pneumocystis pneumonia cannot rely solely on CD4-cell count in autoimmune and inflammatory diseases. Clin. Exp. Rheumatol. 2018;36:490–493. [PubMed] [Google Scholar]
- 144.Falagas M.E., Manta K.G., Betsi G.I., Pappas G. Infection-related morbidity and mortality in patients with connective tissue diseases: A systematic review. Clin. Rheumatol. 2007;26:663–670. doi: 10.1007/s10067-006-0441-9. [DOI] [PubMed] [Google Scholar]
- 145.Sowden E., Carmichael A.J. Autoimmune inflammatory disorders, systemic corticosteroids and Pneumocystis pneumonia: A strategy for prevention. BMC Infect. Dis. 2004;4:42. doi: 10.1186/1471-2334-4-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Ognibene F.P., Shelhamer J.H., Hoffman G.S., Kerr G.S., Reda D., Fauci A.S., Leavitt R.Y. Pneumocystis carinii pneumonia: A major complication of immunosuppressive therapy in patients with Wegener’s granulomatosis. Am. J. Respir. Crit. Care Med. 1995;151:795–799. doi: 10.1164/ajrccm/151.3_Pt_1.795. [DOI] [PubMed] [Google Scholar]
- 147.Decker J.L., Klippel J.H., Plotz P.H., Steinberg A.D. Cyclophosphamide or azathioprine in lupus glomerulonephritis. A controlled trial: Results at 28 months. Ann. Intern. Med. 1975;83:606–615. doi: 10.7326/0003-4819-83-5-606. [DOI] [PubMed] [Google Scholar]
- 148.Harder M.Z., Razzaque M.A., Shazzad M.N., Haq S.A., Ahmed S., Ahmed S.N. Pneumocystis jiroveci pnemonia in systemic lupus erythematosus: A case report. Int. J. Med. Health Res. 2017;3:84–86. [Google Scholar]
- 149.Weng C.T., Liu M.F., Weng M.Y., Lee N.Y., Wang M.C., Lin W.C., Ou C.Y., Lai W.W., Hsu S.C., Chao S.C., et al. Pneumocystis jirovecii pneumonia in systemic lupus erythematosus from southern Taiwan. J. Clin. Rheumatol. 2013;19:252–258. doi: 10.1097/RHU.0b013e31829d5017. [DOI] [PubMed] [Google Scholar]
- 150.Mori S., Sugimoto M. Pneumocystis jirovecii infection: An emerging threat to patients with rheumatoid arthritis. Rheumatology. 2012;51:2120–2130. doi: 10.1093/rheumatology/kes244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Iikuni N., Kitahama M., Ohta S., Okamoto H., Kamatani N., Nishinarita M. Evaluation of Pneumocystis pneumonia infection risk factors in patients with connective tissue disease. Mod. Rheumatol. 2006;16:282–288. doi: 10.3109/s10165-006-0502-6. [DOI] [PubMed] [Google Scholar]
- 152.Gajdusek D.C. Pneumocystis carinii; etiologic agent of interstitial plasma cell pneumonia of premature and young infants. Pediatrics. 1957;19:543–565. [PubMed] [Google Scholar]
- 153.Goldman A.S., Goldman L.R., Goldman D.A. What caused the epidemic of Pneumocystis pneumonia in European premature infants in the mid-20th century? Pediatrics. 2005;115:e725–e736. doi: 10.1542/peds.2004-2157. [DOI] [PubMed] [Google Scholar]
- 154.Semmes E.C., Chen J.L., Goswami R., Burt T.D., Permar S.R., Fouda G.G. Understanding early-life adaptive immunity to guide interventions for pediatric health. Front. Immunol. 2020;11:595297. doi: 10.3389/fimmu.2020.595297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Donald K., Finlay B.B. Early-life interactions between the microbiota and immune system: Impact on immune system development and atopic disease. Nat. Rev. Immunol. 2023 May 03; doi: 10.1038/s41577-023-00874-w. [DOI] [PubMed] [Google Scholar]
- 156.Montes-Cano M.A., Chabe M., Fontillon-Alberdi M., de-Lahorra C., Respaldiza N., Medrano F.J., Varela J.M., Dei-Cas E., Calderon E.J. Vertical transmission of Pneumocystis jirovecii in humans. Emerg. Infect. Dis. 2009;15:125–127. doi: 10.3201/eid1501.080242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Szydlowicz M., Krolak-Olejnik B., Vargas S.L., Zajaczkowska Z., Paluszynska D., Szczygiel A., Matos O., Hendrich A.B., Kicia M. Pneumocystis jirovecii colonization in preterm newborns with respiratory distress syndrome. J. Infect. Dis. 2022;225:1807–1810. doi: 10.1093/infdis/jiab209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Rojas P., Friaza V., Garcia E., de la Horra C., Vargas S.L., Calderon E.J., Pavon A. early acquisition of Pneumocystis jirovecii colonization and potential association with respiratory distress syndrome in preterm newborn infants. Clin. Infect. Dis. 2017;65:976–981. doi: 10.1093/cid/cix454. [DOI] [PubMed] [Google Scholar]
- 159.Basiaga M.L., Ross M.E., Gerber J.S., Ogdie A. Incidence of Pneumocystis jirovecii and adverse events associated with Pneumocystis prophylaxis in children receiving glucocorticoids. J. Pediatric Infect. Dis. Soc. 2018;7:283–289. doi: 10.1093/jpids/pix052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Terblanche A.J., Green R.J., Rheeder P., Wittenberg D.F. Adjunctive corticosteroid treatment of clinical Pneumocystis jiroveci pneumonia in infants less than 18 months of age—A randomised controlled trial. S. Afr. Med. J. 2008;98:287–290. [PubMed] [Google Scholar]
- 161.Peglow S.L., Smulian A.G., Linke M.J., Pogue C.L., Nurre S., Crisler J., Phair J., Gold J.W., Armstrong D., Walzer P.D. Serologic responses to Pneumocystis carinii antigens in health and disease. J. Infect. Dis. 1990;161:296–306. doi: 10.1093/infdis/161.2.296. [DOI] [PubMed] [Google Scholar]
- 162.Wakefield A.E., Stewart T.J., Moxon E.R., Marsh K., Hopkin J.M. Infection with Pneumocystis carinii is prevalent in healthy Gambian children. Trans. R. Soc. Trop. Med. Hyg. 1990;84:800–802. doi: 10.1016/0035-9203(90)90087-U. [DOI] [PubMed] [Google Scholar]
- 163.Beard C.B., Fox M.R., Lawrence G.G., Guarner J., Hanzlick R.L., Huang L., del Rio C., Rimland D., Duchin J.S., Colley D.G. Genetic differences in Pneumocystis isolates recovered from immunocompetent infants and from adults with AIDS: Epidemiological Implications. J. Infect. Dis. 2005;192:1815–1818. doi: 10.1086/497381. [DOI] [PubMed] [Google Scholar]
- 164.Walzer P.D., Schultz M.G., Western K.A., Robbins J.F. Pneumocystis carinii pneumonia and primary immune deficiency diseases. Natl. Cancer Inst. Monogr. 1976;43:65–74. [PubMed] [Google Scholar]
- 165.Gray P.E., Logan G.J., Alexander I.E., Poulton S., Roscioli T., Ziegler J. A novel intronic splice site deletion of the IL-2 receptor common gamma chain results in expression of a dysfunctional protein and T-cell-positive X-linked Severe combined immunodeficiency. Int. J. Immunogenet. 2015;42:11–14. doi: 10.1111/iji.12166. [DOI] [PubMed] [Google Scholar]
- 166.Sato T., Okano T., Tanaka-Kubota M., Kimura S., Miyamoto S., Ono S., Yamashita M., Mitsuiki N., Takagi M., Imai K., et al. Novel compound heterozygous mutations in a Japanese girl with Janus kinase 3 deficiency. Pediatr. Int. 2016;58:1076–1080. doi: 10.1111/ped.13070. [DOI] [PubMed] [Google Scholar]
- 167.Pan Y., Pan H., Lian C., Wu B., Lin J., Huang G., Cui B. Case Report: Mutations in JAK3 causing severe combined immunodeficiency complicated by disseminated Bacille Calmette-Guerin disease and Pneumocystis pneumonia. Front. Immunol. 2022;13:1055607. doi: 10.3389/fimmu.2022.1055607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Hershfield . Adenosine Deaminase Deficiency. In: Adam M.P., Mirzaa G.M., Pagon R.A., Wallace S.E., Bean L.J.H., Gripp K.W., Amemiya A., editors. GeneReviews((R)) University of Washington; Seattle, WA, USA: 2017. [Google Scholar]
- 169.Stepensky P., Keller B., Buchta M., Kienzler A.K., Elpeleg O., Somech R., Cohen S., Shachar I., Miosge L.A., Schlesier M., et al. Deficiency of caspase recruitment domain family, member 11 (CARD11), causes profound combined immunodeficiency in human subjects. J. Allergy Clin. Immunol. 2013;131:477–485.e1. doi: 10.1016/j.jaci.2012.11.050. [DOI] [PubMed] [Google Scholar]
- 170.Fuchs S., Rensing-Ehl A., Pannicke U., Lorenz M.R., Fisch P., Jeelall Y., Rohr J., Speckmann C., Vraetz T., Farmand S., et al. Omenn syndrome associated with a functional reversion due to a somatic second-site mutation in CARD11 deficiency. Blood. 2015;126:1658–1669. doi: 10.1182/blood-2015-03-631374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Al-Saud B.K., Al-Sum Z., Alassiri H., Al-Ghonaium A., Al-Muhsen S., Al-Dhekri H., Arnaout R., Alsmadi O., Borrero E., Abu-Staiteh A., et al. Clinical, immunological, and molecular characterization of hyper-IgM syndrome due to CD40 deficiency in eleven patients. J. Clin. Immunol. 2013;33:1325–1335. doi: 10.1007/s10875-013-9951-9. [DOI] [PubMed] [Google Scholar]
- 172.Levy J., Espanol-Boren T., Thomas C., Fischer A., Tovo P., Bordigoni P., Resnick I., Fasth A., Baer M., Gomez L., et al. Clinical spectrum of X-linked hyper-IgM syndrome. J. Pediatr. 1997;131:47–54. doi: 10.1016/S0022-3476(97)70123-9. [DOI] [PubMed] [Google Scholar]
- 173.Brunet B.A., Rodriguez R. Unusual presentation of combined immunodeficiency in a child with homozygous DOCK8 mutation. Ann. Allergy Asthma Immunol. 2017;119:294–295. doi: 10.1016/j.anai.2017.07.011. [DOI] [PubMed] [Google Scholar]
- 174.Nielsen C., Jakobsen M.A., Larsen M.J., Muller A.C., Hansen S., Lillevang S.T., Fisker N., Barington T. Immunodeficiency associated with a nonsense mutation of IKBKB. J. Clin. Immunol. 2014;34:916–921. doi: 10.1007/s10875-014-0097-1. [DOI] [PubMed] [Google Scholar]
- 175.Salt B.H., Niemela J.E., Pandey R., Hanson E.P., Deering R.P., Quinones R., Jain A., Orange J.S., Gelfand E.W. IKBKG (nuclear factor-kappa B essential modulator) mutation can be associated with opportunistic infection without impairing Toll-like receptor function. J. Allergy Clin. Immunol. 2008;121:976–982. doi: 10.1016/j.jaci.2007.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Boutboul D., Kuehn H.S., Van de Wyngaert Z., Niemela J.E., Callebaut I., Stoddard J., Lenoir C., Barlogis V., Farnarier C., Vely F., et al. Dominant-negative IKZF1 mutations cause a T, B, and myeloid cell combined immunodeficiency. J. Clin. Invest. 2018;128:3071–3087. doi: 10.1172/JCI98164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Kuehn H.S., Boisson B., Cunningham-Rundles C., Reichenbach J., Stray-Pedersen A., Gelfand E.W., Maffucci P., Pierce K.R., Abbott J.K., Voelkerding K.V., et al. Loss of B Cells in Patients with Heterozygous Mutations in IKAROS. N. Engl. J. Med. 2016;374:1032–1043. doi: 10.1056/NEJMoa1512234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Yamashita M., Morio T. Inborn errors of IKAROS and AIOLOS. Curr. Opin. Immunol. 2021;72:239–248. doi: 10.1016/j.coi.2021.06.010. [DOI] [PubMed] [Google Scholar]
- 179.Deal C., Thauland T.J., Stiehm E.R., Garcia-Lloret M.I., Butte M.J. Intact B-Cell Signaling and Function With Host B-Cells 47 Years After Transplantation for X-SCID. Front. Immunol. 2020;11:415. doi: 10.3389/fimmu.2020.00415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Sonoda M., Ishimura M., Eguchi K., Yada Y., Lenhartova N., Shiraishi A., Tanaka T., Sakai Y., Ohga S. Progressive B cell depletion in human MALT1 deficiency. Clin. Exp. Immunol. 2021;206:237–247. doi: 10.1111/cei.13662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Clarridge K., Leitenberg D., Loechelt B., Picard C., Keller M. Major Histocompatibility Complex Class II Deficiency due to a Novel Mutation in RFXANK in a Child of Mexican Descent. J. Clin. Immunol. 2016;36:4–5. doi: 10.1007/s10875-015-0219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Sharifinejad N., Jamee M., Zaki-Dizaji M., Lo B., Shaghaghi M., Mohammadi H., Jadidi-Niaragh F., Shaghaghi S., Yazdani R., Abolhassani H., et al. Clinical, Immunological, and Genetic Features in 49 Patients With ZAP-70 Deficiency: A Systematic Review. Front. Immunol. 2020;11:831. doi: 10.3389/fimmu.2020.00831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Barata L.T., Henriques R., Hivroz C., Jouanguy E., Paiva A., Freitas A.M., Coimbra H.B., Fischer A., da Mota H.C. Primary immunodeficiency secondary to ZAP-70 deficiency. Acta Med. Port. 2001;14:413–417. [PubMed] [Google Scholar]
- 184.Walkovich K., Vander Lugt M. ZAP70-Related Combined Immunodeficiency. In: Adam M.P., Mirzaa G.M., Pagon R.A., Wallace S.E., Bean L.J.H., Gripp K.W., Amemiya A., editors. GeneReviews((R)) University of Washington; Seattle, WA, USA: 2021. [Google Scholar]
- 185.Schroeder M.L., Triggs-Raine B., Zelinski T. Genotyping an immunodeficiency causing c.1624-11G>A ZAP70 mutation in Canadian Mennonites. BMC Med Genet. 2016;17:50. doi: 10.1186/s12881-016-0312-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Gossling K.L., Schipp C., Fischer U., Babor F., Koch G., Schuster F.R., Dietzel-Dahmen J., Wieczorek D., Borkhardt A., Meisel R., et al. Hematopoietic Stem Cell Transplantation in an Infant with Immunodeficiency, Centromeric Instability, and Facial Anomaly Syndrome. Front. Immunol. 2017;8:773. doi: 10.3389/fimmu.2017.00773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Banday A.Z., Jindal A.K., Kaur A., Kumar Y., Nameirakpam J., Patra P.K., Rawat A. A young girl with hypogammaglobulinemia and granulomatous hepatitis caused by a novel mutation in ZBTB24 gene: A case based analysis. Immunobiology. 2020;225:151912. doi: 10.1016/j.imbio.2020.151912. [DOI] [PubMed] [Google Scholar]
- 188.Garty B.Z., Ben-Baruch A., Rolinsky A., Woellner C., Grimbacher B., Marcus N. Pneumocystis jirovecii pneumonia in a baby with hyper-IgE syndrome. Eur. J. Pediatr. 2010;169:35–37. doi: 10.1007/s00431-009-0973-5. [DOI] [PubMed] [Google Scholar]
- 189.Lan J., Zhang Y., Song M., Cai S., Luo H., OuYang R., Yang P., Shi X., Long Y., Chen Y. Omalizumab for STAT3 Hyper-IgE Syndromes in Adulthood: A Case Report and Literature Review. Front Med. 2022;9:835257. doi: 10.3389/fmed.2022.835257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Keller M.D., Ganesh J., Heltzer M., Paessler M., Bergqvist A.G., Baluarte H.J., Watkins D., Rosenblatt D.S., Orange J.S. Severe combined immunodeficiency resulting from mutations in MTHFD1. Pediatrics. 2013;131:e629–e634. doi: 10.1542/peds.2012-0899. [DOI] [PubMed] [Google Scholar]
- 191.Kishimoto K., Kobayashi R., Sano H., Suzuki D., Maruoka H., Yasuda K., Chida N., Yamada M., Kobayashi K. Impact of folate therapy on combined immunodeficiency secondary to hereditary folate malabsorption. Clin. Immunol. 2014;153:17–22. doi: 10.1016/j.clim.2014.03.014. [DOI] [PubMed] [Google Scholar]
- 192.Pongphitcha P., Sirachainan N., Khongkraparn A., Tim-Aroon T., Songdej D., Wattanasirichaigoon D. A novel TCN2 mutation with unusual clinical manifestations of hemolytic crisis and unexplained metabolic acidosis: Expanding the genotype and phenotype of transcobalamin II deficiency. BMC Pediatr. 2022;22:233. doi: 10.1186/s12887-022-03291-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Dupuis-Girod S., Corradini N., Hadj-Rabia S., Fournet J.C., Faivre L., Le Deist F., Durand P., Doffinger R., Smahi A., Israel A., et al. Osteopetrosis, lymphedema, anhidrotic ectodermal dysplasia, and immunodeficiency in a boy and incontinentia pigmenti in his mother. Pediatrics. 2002;109:e97. doi: 10.1542/peds.109.6.e97. [DOI] [PubMed] [Google Scholar]
- 194.Mendez-Echevarria A., Gonzalez-Granado L.I., Allende L.M., De Felipe B., Teresa D.R., Calvo C., Perez-Martinez A., Raquel R.G., Neth O. Fatal Pneumocystis jirovecii and Cytomegalovirus Infections in an Infant With Normal TRECs Count: Pitfalls of Newborn Screening for Severe Combined Immunodeficiency. Pediatr. Infect. Dis. 2019;38:157–160. doi: 10.1097/INF.0000000000002058. [DOI] [PubMed] [Google Scholar]
- 195.Kuehn H.S., Chang J., Yamashita M., Niemela J.E., Zou C., Okuyama K., Harada J., Stoddard J.L., Nunes-Santos C.J., Boast B., et al. T and B cell abnormalities, pneumocystis pneumonia, and chronic lymphocytic leukemia associated with an AIOLOS defect in patients. J. Exp. Med. 2021;218:e20211118. doi: 10.1084/jem.20211118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Silverman L.B., McLean T.W., Gelber R.D., Donnelly M.J., Gilliland D.G., Tarbell N.J., Sallan S.E. Intensified therapy for infants with acute lymphoblastic leukemia: Results from the Dana-Farber Cancer Institute Consortium. Cancer. 1997;80:2285–2295. doi: 10.1002/(SICI)1097-0142(19971215)80:12<2285::AID-CNCR10>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 197.Hosking L.M., Bannister E.G., Cook M.C., Choo S., Kumble S., Cole T.S. Trichohepatoenteric Syndrome Presenting with Severe Infection and Later Onset Diarrhoea. J. Clin. Immunol. 2018;38:1–3. doi: 10.1007/s10875-017-0460-0. [DOI] [PubMed] [Google Scholar]
- 198.Wang T., Ong P., Roscioli T., Cliffe S.T., Church J.A. Hepatic veno-occlusive disease with immunodeficiency (VODI): First reported case in the U.S. and identification of a unique mutation in Sp110. Clin. Immunol. 2012;145:102–107. doi: 10.1016/j.clim.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 199.Marquardsen F.A., Baldin F., Wunderer F., Al-Herz W., Mikhael R., Lefranc G., Baz Z., Rezaee F., Hanna R., Kfir-Erenfeld S., et al. Detection of Sp110 by Flow Cytometry and Application to Screening Patients for Veno-occlusive Disease with Immunodeficiency. J. Clin. Immunol. 2017;37:707–714. doi: 10.1007/s10875-017-0431-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Alibrahim A., Lepore M., Lierl M., Filipovich A., Assaad A. Pneumocystis carinii pneumonia in an infant with X-linked agammaglobulinemia. J. Allergy Clin. Immunol. 1998;101:552–553. doi: 10.1016/S0091-6749(98)70363-X. [DOI] [PubMed] [Google Scholar]
- 201.Mandola A.B., Sharfe N., Nagdi Z., Dadi H., Vong L., Merico D., Ngan B., Reid B., Roifman C.M. Combined immunodeficiency caused by a novel homozygous NFKB1 mutation. J. Allergy Clin. Immunol. 2021;147:727–733.e2. doi: 10.1016/j.jaci.2020.08.040. [DOI] [PubMed] [Google Scholar]
- 202.Siddiqi A.E., Liu A.Y., Charville G.W., Kunder C.A., Uzel G., Sadighi Akha A.A., Oak J., Martin B., Sacha J., Lewis D.B., et al. Disseminated Pneumocystis jirovecii Infection with Osteomyelitis in a Patient with CTLA-4 Haploinsufficiency. J. Clin. Immunol. 2020;40:412–414. doi: 10.1007/s10875-020-00748-z. [DOI] [PubMed] [Google Scholar]
- 203.Ferec C., Cutting G.R. Assessing the Disease-Liability of Mutations in CFTR. Cold Spring Harb. Perspect. Med. 2012;2:a009480. doi: 10.1101/cshperspect.a009480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Pedersen F.K., Johansen K.S., Rosenkvist J., Tygstrup I., Valerius N.H. Refractory Pneumocystis carinii infection in chronic granulomatous disease: Successful treatment with granulocytes. Pediatrics. 1979;64:935–938. doi: 10.1542/peds.64.6.935. [DOI] [PubMed] [Google Scholar]
- 205.Lu Y.W., Chen T.C. Use of trimethoprim-sulfamethoxazole in a patient with G6PD deficiency for treating Pneumocystis jirovecii pneumonia without haemolysis: Case report and literature review. J. Clin. Pharm. Ther. 2020;45:1483–1485. doi: 10.1111/jcpt.13220. [DOI] [PubMed] [Google Scholar]
- 206.Zhang Z., Li Q., Shen X., Liao L., Wang X., Song M., Zheng X., Zhu Y., Yang Y. The medication for pneumocystis pneumonia with glucose-6-phosphate dehydrogenase deficiency patients. Front. Pharmacol. 2022;13:957376. doi: 10.3389/fphar.2022.957376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Gonzalez-Lara M.F., Wisniowski-Yanez A., Perez-Patrigeon S., Hsu A.P., Holland S.M., Cuellar-Rodriguez J.M. Pneumocystis jiroveci pneumonia and GATA2 deficiency: Expanding the spectrum of the disease. J. Infect. 2017;74:425–427. doi: 10.1016/j.jinf.2017.01.005. [DOI] [PubMed] [Google Scholar]
- 208.Drutman S.B., Mansouri D., Mahdaviani S.A., Neehus A.L., Hum D., Bryk R., Hernandez N., Belkaya S., Rapaport F., Bigio B., et al. Fatal Cytomegalovirus Infection in an Adult with Inherited NOS2 Deficiency. N. Engl. J. Med. 2020;382:437–445. doi: 10.1056/NEJMoa1910640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Somekh I., Lev A., Barel O., Lee Y.N., Hendel A., Simon A.J., Somech R. Exploring genetic defects in adults who were clinically diagnosed as severe combined immune deficiency during infancy. Immunol. Res. 2021;69:145–152. doi: 10.1007/s12026-021-09179-3. [DOI] [PubMed] [Google Scholar]
- 210.Yang Q., Yu C., Wu Y., Cao K., Li X., Cao W., Cao L., Zhang S., Ba Y., Zheng Y., et al. Unusual Talaromyces marneffei and Pneumocystis jirovecii coinfection in a child with a STAT1 mutation: A case report and literature review. Front. Immunol. 2023;14:1103184. doi: 10.3389/fimmu.2023.1103184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Consortium I.R.F.I., Fornes O., Jia A., Kuehn H.S., Min Q., Pannicke U., Schleussner N., Thouenon R., Yu Z., de Los Angeles Astbury M., et al. A multimorphic mutation in IRF4 causes human autosomal dominant combined immunodeficiency. Sci. Immunol. 2023;8:eade7953. doi: 10.1126/sciimmunol.ade7953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Zeleznik M., Soltirovska Salamon A., Debeljak M., Goropevsek A., Sustar N., Kljucevsek D., Ihan A., Avcin T. Case report: Pneumocystis jirovecii pneumonia in a severe case of Aicardi-Goutieres syndrome with an IFIH1 gain-of-function mutation mimicking combined immunodeficiency. Front. Immunol. 2022;13:1033513. doi: 10.3389/fimmu.2022.1033513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Podlipnik S., de la Mora L., Alsina M., Mascaro J.M., Jr. Pneumocystis jirovecii pneumonia in a patient with pustular psoriasis with an IL-36RN deficiency treated with infliximab: Case report and review of the literature. Australas. J. Dermatol. 2017;58:e44–e47. doi: 10.1111/ajd.12489. [DOI] [PubMed] [Google Scholar]
- 214.Pryhuber G.S., Huyck H.L., Bhagwat S., O’Reilly M.A., Finkelstein J.N., Gigliotti F., Wright T.W. Parenchymal cell TNF receptors contribute to inflammatory cell recruitment and respiratory failure in Pneumocystis carinii-induced pneumonia. J. Immunol. 2008;181:1409–1419. doi: 10.4049/jimmunol.181.2.1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Tillant D., Albanese J., Tomachot L., Durbec O., Granthil C. Purpura fulminans and C7 deficiency complicated by Pneumocystis carinii pneumonia. Ann. Fr. Anesth. Reanim. 1991;10:394–397. doi: 10.1016/S0750-7658(05)80816-0. [DOI] [PubMed] [Google Scholar]
- 216.Ziv A., Werner L., Konnikova L., Awad A., Jeske T., Hastreiter M., Mitsialis V., Stauber T., Wall S., Kotlarz D., et al. An RTEL1 Mutation Links to Infantile-Onset Ulcerative Colitis and Severe Immunodeficiency. J. Clin. Immunol. 2020;40:1010–1019. doi: 10.1007/s10875-020-00829-z. [DOI] [PubMed] [Google Scholar]
- 217.Borie R., Kannengiesser C., Sicre de Fontbrune F., Boutboul D., Tabeze L., Brunet-Possenti F., Lainey E., Debray M.P., Cazes A., Crestani B. Pneumocystosis revealing immunodeficiency secondary to TERC mutation. Eur. Respir. J. 2017;50 doi: 10.1183/13993003.01443-2017. [DOI] [PubMed] [Google Scholar]
- 218.Sharman J.P., Brander D.M., Mato A.R., Ghosh N., Schuster S.J., Kambhampati S., Burke J.M., Lansigan F., Schreeder M.T., Lunin S.D., et al. Ublituximab plus ibrutinib versus ibrutinib alone for patients with relapsed or refractory high-risk chronic lymphocytic leukaemia (GENUINE): A phase 3, multicentre, open-label, randomised trial. Lancet Haematol. 2021;8:e254–e266. doi: 10.1016/S2352-3026(20)30433-6. [DOI] [PubMed] [Google Scholar]
- 219.Davids M.S., Brander D.M., Kim H.T., Tyekucheva S., Bsat J., Savell A., Hellman J.M., Bazemore J., Francoeur K., Alencar A., et al. Ibrutinib plus fludarabine, cyclophosphamide, and rituximab as initial treatment for younger patients with chronic lymphocytic leukaemia: A single-arm, multicentre, phase 2 trial. Lancet Haematol. 2019;6:e419–e428. doi: 10.1016/S2352-3026(19)30104-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Tangye S.G., Al-Herz W., Bousfiha A., Cunningham-Rundles C., Franco J.L., Holland S.M., Klein C., Morio T., Oksenhendler E., Picard C., et al. Human inborn errors of immunity: 2022 update on the classification from the International Union of Immunological Societies Expert Committee. J. Clin. Immunol. 2022;42:1473–1507. doi: 10.1007/s10875-022-01289-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Inagaki K., Blackshear C., Hobbs C.V. Pneumocystis Infection in Children: National trends and characteristics in the United States, 1997-2012. Pediatr. Infect. Dis. J. 2019;38:241–247. doi: 10.1097/INF.0000000000002119. [DOI] [PubMed] [Google Scholar]
- 222.Menu E., Driouich J.S., Luciani L., Morand A., Ranque S., L’Ollivier C. Detection of Pneumocystis jirovecii in hospitalized children less than 3 years of age. J. Fungi. 2021;7:546. doi: 10.3390/jof7070546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Chong W.H., Saha B.K., Chopra A. Narrative review of the relationship between COVID-19 and PJP: Does it represent coinfection or colonization? Infection. 2021;49:1079–1090. doi: 10.1007/s15010-021-01630-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Gentile I., Viceconte G., Lanzardo A., Zotta I., Zappulo E., Pinchera B., Scotto R., Schiano Moriello N., Foggia M., Giaccone A., et al. Pneumocystis jirovecii pneumonia in non-HIV patients recovering from COVID-19: A single-center experience. Int. J. Environ. Res. Public. Health. 2021;18:11399. doi: 10.3390/ijerph182111399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Viceconte G., Buonomo A.R., Lanzardo A., Pinchera B., Zappulo E., Scotto R., Schiano Moriello N., Vargas M., Iacovazzo C., Servillo G., et al. Pneumocystis jirovecii pneumonia in an immunocompetent patient recovered from COVID-19. Infect. Dis. 2021;53:382–385. doi: 10.1080/23744235.2021.1890331. [DOI] [PubMed] [Google Scholar]
- 226.Gioia F., Albasata H., Hosseini-Moghaddam S.M. Concurrent infection with SARS-CoV-2 and Pneumocystis jirovecii in immunocompromised and immunocompetent individuals. J. Fungi. 2022;8:585. doi: 10.3390/jof8060585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Khodadadi H., Ahmadpour E., Nami S., Mohammadi R., Hosseini H., Behravan M., Morovati H. Global prevalence, mortality, and main risk factors for COVID-19 associated pneumocystosis: A systematic review and meta-analysis. Asian Pac. J. Trop. Med. 2022;15:431–441. doi: 10.4103/1995-7645.359784. [DOI] [Google Scholar]
- 228.Alanio A., Delliere S., Voicu S., Bretagne S., Megarbane B. The presence of Pneumocystis jirovecii in critically ill patients with COVID-19. J. Infect. 2021;82:84–123. doi: 10.1016/j.jinf.2020.10.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Blaize M., Mayaux J., Luyt C.E., Lampros A., Fekkar A. COVID-19-related respiratory failure and lymphopenia do not seem associated with pneumocystosis. Am. J. Respir. Crit. Care Med. 2020;202:1734–1736. doi: 10.1164/rccm.202007-2938LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Bretagne S., Sitbon K., Botterel F., Delliere S., Letscher-Bru V., Chouaki T., Bellanger A.P., Bonnal C., Fekkar A., Persat F., et al. COVID-19-associated pulmonary aspergillosis, fungemia, and pneumocystosis in the intensive care unit: A retrospective multicenter observational cohort during the first French pandemic wave. Microbiol. Spectr. 2021;9:e0113821. doi: 10.1128/Spectrum.01138-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Gerber V., Ruch Y., Chamaraux-Tran T.N., Oulehri W., Schneider F., Lindner V., Greigert V., Denis J., Brunet J., Danion F. Detection of Pneumocystis jirovecii in patients with severe COVID-19: Diagnostic and therapeutic challenges. J Fungi. 2021;7:585. doi: 10.3390/jof7080585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Mouren D., Goyard C., Catherinot E., Givel C., Chabrol A., Tcherakian C., Longchampt E., Vargaftig J., Farfour E., Legal A., et al. COVID-19 and Pneumocystis jirovecii pneumonia: Back to the basics. Respir. Med. Res. 2021;79:100814. doi: 10.1016/j.resmer.2021.100814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Castelnuovo F., Tiecco G., Storti S., Fumarola B., Brianese N., Bertelli D., Castelli F. Pneumocystis jirovecii pneumonia in breast cancer mimicking SARS-CoV-2 pneumonia during pandemic. Infez. Med. 2021;29:614–617. doi: 10.53854/liim-2904-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Cattaneo L., Buonomo A.R., Iacovazzo C., Giaccone A., Scotto R., Viceconte G., Mercinelli S., Vargas M., Roscetto E., Cacciatore F., et al. Invasive fungal infections in hospitalized patients with COVID-19: A non-intensive care single-centre experience during the first pandemic waves. J. Fungi. 2023;9 doi: 10.3390/jof9010086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.De Francesco M.A., Alberici F., Bossini N., Scolari F., Pascucci F., Tomasoni G., Caruso A. Pneumocystis jirevocii and SARS-CoV-2 co-infection: A common feature in transplant recipients? Vaccines. 2020;8 doi: 10.3390/vaccines8030544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Patrucco F., Airoldi C., Falaschi Z., Bellan M., Castello L.M., Filippone F., Matranga S., Masellis S., Smeriglia A., Solidoro P., et al. Mycotic infection prevalence among patients undergoing bronchoalveolar lavage with search of SARS-CoV-2 after two negative nasopharyngeal swabs. J. Breath. Res. 2021;15 doi: 10.1088/1752-7163/ac2290. [DOI] [PubMed] [Google Scholar]
- 237.Farinacci D., Ciccullo A., Borghetti A., Visconti E., Tamburrini E., Izzi I.M., Cauda R., Di Giambenedetto S., Pallavicini F. People living with HIV in the COVID-19 era: A case report. AIDS Res. Hum. Retroviruses. 2021;37:253–254. doi: 10.1089/aid.2020.0149. [DOI] [PubMed] [Google Scholar]
- 238.Niamatullah H., Nasir N., Jabeen K., Rattani S., Farooqi J., Ghanchi N., Irfan M. Post-COVID-19 Pneumocystis pneumonia cases from Pakistan: An observational study. Access Microbiol. 2023;5:acmi000406. doi: 10.1099/acmi.0.000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Baraboutis I.G., Gargalianos P., Aggelonidou E., Adraktas A., Collaborators Initial real-life experience from a designated COVID-19 centre in Athens, Greece: A proposed therapeutic algorithm. SN Compr. Clin. Med. 2020;2:689–693. doi: 10.1007/s42399-020-00324-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Sreenath K., Batra P., Vinayaraj E.V., Bhatia R., SaiKiran K., Singh V., Singh S., Verma N., Singh U.B., Mohan A., et al. Coinfections with other respiratory pathogens among patients with COVID-19. Microbiol. Spectr. 2021;9:e0016321. doi: 10.1128/Spectrum.00163-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Alebna P.L., Bellamy S., Tabur T.A., Mangia A. Rare case of persistently depressed T lymphocyte subsets after SARS-CoV-2 infection. Am. J. Case Rep. 2022;23:e937760. doi: 10.12659/AJCR.937760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242.Bhat P., Noval M., Doub J.B., Heil E. Concurrent COVID-19 and Pneumocystis jirovecii pneumonia in a severely immunocompromised 25-year-old patient. Int. J. Infect. Dis. 2020;99:119–121. doi: 10.1016/j.ijid.2020.07.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Menon A.A., Berg D.D., Brea E.J., Deutsch A.J., Kidia K.K., Thurber E.G., Polsky S.B., Yeh T., Duskin J.A., Holliday A.M., et al. A case of COVID-19 and Pneumocystis jirovecii coinfection. Am. J. Respir. Crit. Care Med. 2020;202:136–138. doi: 10.1164/rccm.202003-0766LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Merchant E.A., Flint K., Barouch D.H., Blair B.M. Co-infection with coronavirus disease 2019, previously undiagnosed human immunodeficiency virus, Pneumocystis jirovecii pneumonia and cytomegalovirus pneumonitis, with possible immune reconstitution inflammatory syndrome. IDCases. 2021;24:e01153. doi: 10.1016/j.idcr.2021.e01153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 245.Rubiano C., Tompkins K., Sellers S.A., Bramson B., Eron J., Parr J.B., Schranz A.J. Pneumocystis and severe acute respiratory syndrome Coronavirus 2 coinfection: A case report and review of an emerging diagnostic dilemma. Open Forum Infect. Dis. 2021;8:ofaa633. doi: 10.1093/ofid/ofaa633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Shah N., Dahi P.B., Ponce D.M., Sauter C.S., Shaffer B.C., Chung D.J., Politikos I., Lin R.J., Giralt S.A., Papanicolaou G., et al. Hematopoietic cell transplantation is feasible in patients with prior COVID-19 infection. Transplant. Cell Ther. 2022;28:55.e51–55.e55. doi: 10.1016/j.jtct.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Cai S., Sun W., Li M., Dong L. A complex COVID-19 case with rheumatoid arthritis treated with tocilizumab. Clin. Rheumatol. 2020;39:2797–2802. doi: 10.1007/s10067-020-05234-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Guo W., Wang M., Ming F., Tang W., Liang K. The diagnostic trap occurred in two COVID-19 cases combined Pneumocystis pneumonia in patient with AIDS. Res. Sq. 2020 doi: 10.21203/rs.3.rs-53350/v1. [DOI] [Google Scholar]
- 249.Peng J., Ni M., Du D., Lu Y., Song J., Liu W., Shen N., Wang X., Zhu Y., Vallance B.A., et al. Successful treatment of a kidney transplant patient with COVID-19 and late-onset Pneumocystis jirovecii pneumonia. Ann. Clin. Microbiol. Antimicrob. 2021;20:83. doi: 10.1186/s12941-021-00489-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Alvarez H., Ruiz-Mateos E., Juiz-Gonzalez P.M., Vitalle J., Vieitez I., Vazquez-Friol M.D.C., Torres-Beceiro I., Perez-Gomez A., Gallego-Garcia P., Estevez-Gomez N., et al. SARS-CoV-2 evolution and spike-specific CD4+ T-cell response in persistent COVID-19 with severe HIV immune suppression. Microorganisms. 2022;10 doi: 10.3390/microorganisms10010143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Amparo-Vicente M., Morte E. Pneumonia by Pneumocystis jirovecii after COVID-19 in non-HIV patient. Rev. Chilena Infectol. 2022;39:357–360. doi: 10.4067/s0716-10182022000200357. [DOI] [PubMed] [Google Scholar]
- 252.Blanco J.L., Ambrosioni J., Garcia F., Martinez E., Soriano A., Mallolas J., Miro J.M., Investigators C.-I.H. COVID-19 in patients with HIV: Clinical case series. Lancet HIV. 2020;7:e314–e316. doi: 10.1016/S2352-3018(20)30111-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Quintana-Ortega C., Remesal A., Ruiz de Valbuena M., de la Serna O., Laplaza-Gonzalez M., Alvarez-Rojas E., Udaondo C., Alcobendas R., Murias S. Fatal outcome of anti-MDA5 juvenile dermatomyositis in a paediatric COVID-19 patient: A case report. Mod. Rheumatol. Case Rep. 2021;5:101–107. doi: 10.1080/24725625.2020.1832755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Nguyen H., Salkeld J., Agarwal S., Goodman A. compassionate use of REGN-COV2 in the treatment of COVID-19 in a patient with impaired humoral immunity. Clin. Infect. Pract. 2021;12:100089. doi: 10.1016/j.clinpr.2021.100089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Coleman H., Snell L.B., Simons R., Douthwaite S.T., Lee M.J. Coronavirus disease 2019 and Pneumocystis jirovecii pneumonia: A diagnostic dilemma in HIV. AIDS. 2020;34:1258–1260. doi: 10.1097/QAD.0000000000002571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Kelly S., Waters L., Cevik M., Collins S., Lewis J., Wu M.S., Blanchard T.J., Geretti A.M. Pneumocystis pneumonia, a COVID-19 mimic, reminds us of the importance of HIV testing in COVID-19. Clin. Med. 2020;20:590–592. doi: 10.7861/clinmed.2020-0565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 257.Wenlock R.D., Brown C.S., Iwuji C., Vera J.H. Can I go back to work? A case of persistent SARS-CoV-2 with advanced untreated HIV infection. Int. J. STD AIDS. 2022;33:209–211. doi: 10.1177/09564624211051631. [DOI] [PubMed] [Google Scholar]
- 258.Alsayed A.R., Talib W., Al-Dulaimi A., Daoud S., Al Maqbali M. The first detection of Pneumocystis jirovecii in asthmatic patients post-COVID-19 in Jordan. Bosn. J. Basic. Med. Sci. 2022;22:784–790. doi: 10.17305/bjbms.2022.7335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Adachi E., Saito M., Koga M., Tsutsumi T., Yotsuyanagi H. Favorable Outcome following sotrovimab monoclonal antibody in a patient with prolonged SARS-CoV-2 omicron infection with HIV/AIDS. Intern. Med. 2022;61:3459–3462. doi: 10.2169/internalmedicine.0485-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Takahashi T., Saito A., Kuronuma K., Nishikiori H., Chiba H. Pneumocystis jirovecii pneumonia associated with COVID-19 in patients with interstitial pneumonia. Medicina. 2022;58:1151. doi: 10.3390/medicina58091151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Moradians V., Shateri Amiri B., Bahadorizadeh L., Gholizadeh Mesgarha M., Sadeghi S. Concurrent COVID-19 and Pneumocystis carinii pneumonia in a patient subsequently found to have underlying hairy cell leukemia. Radiol. Case Rep. 2022;17:3238–3242. doi: 10.1016/j.radcr.2022.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Tehrani S., Ziaie S., Kashefizadeh A., Fadaei M., Najafiarab H., Keyvanfar A. Case Report: Pneumonia in a patient with combined variable immunodeficiency: COVID-19 or Pneumocystis pneumonia? Front. Med. 2022;9:814300. doi: 10.3389/fmed.2022.814300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.Broadhurst A.G.B., Lalla U., Taljaard J.J., Louw E.H., Koegelenberg C.F.N., Allwood B.W. The diagnostic challenge of Pneumocystis pneumonia and COVID-19 co-infection in HIV. Respirol. Case Rep. 2021;9:e00725. doi: 10.1002/rcr2.725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Parker A., Shaw J., Karamchand S., Lahri S., Schrueder N., Chothia M.Y., Mowlana A., Lalla U., Allwood B.W., Koegelenberg C.F.N., et al. HIV and SARS-CoV-2 co-infection: The diagnostic challenges of dual pandemics. S Afr. Med. J. 2020;110:473–475. doi: 10.7196/SAMJ.2020.v110i6.14825. [DOI] [PubMed] [Google Scholar]
- 265.Jeican I.I., Inisca P., Gheban D., Tabaran F., Aluas M., Trombitas V., Cristea V., Crivii C., Junie L.M., Albu S. COVID-19 and Pneumocystis jirovecii pulmonary coinfection-the first case confirmed through autopsy. Medicina. 2021;57 doi: 10.3390/medicina57040302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 266.Skonieczny P., Heleniak Z., Szostakiewicz M., Kuziemski K., Debska-Slizien A. Coinfection of COVID-19 and pneumocystosis in a patient after kidney transplantation. Pol. Arch. Intern. Med. 2021;131:566–567. doi: 10.20452/pamw.15996. [DOI] [PubMed] [Google Scholar]
- 267.Yehouenou Tessi R.T., Onka B., El Bakkari A., Jerguigue H., Latib R., Omor Y. An etiology of ground–glass images during COVID-19: Pneumocystis jiroveci pneumonia. SAGE Open Med. Case Rep. 2022;10:2050313X221091391. doi: 10.1177/2050313X221091391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 268.Mang S., Kaddu-Mulindwa D., Metz C., Becker A., Seiler F., Smola S., Massmann A., Becker S.L., Papan C., Bals R., et al. Pneumocystis jirovecii pneumonia and severe acute respiratory syndrome Coronavirus 2 coinfection in a patient with newly diagnosed HIV-1 infection. Clin. Infect. Dis. 2021;72:1487–1489. doi: 10.1093/cid/ciaa906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Larzabal F.J., Vilela A., Brusca S., Saluzzi I., Ghergo G.E., Angiono M.A. Simultaneous diagnosis and favorable evolution of infection with Pneumocystis jirovecii, SARS-CoV-2 and advanced HIV. Medicina. 2020;80:554–556. [PubMed] [Google Scholar]
- 270.Connolly S.P., McGrath J., Sui J., Muldoon E.G. Rare, disseminated Kaposi sarcoma in advanced HIV with high-burden pulmonary and skeletal involvement. BMJ Case Rep. 2021;14:e245448. doi: 10.1136/bcr-2021-245448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Anggraeni A.T., Soedarsono S., Soeprijanto B. Concurrent COVID-19 and Pneumocystis jirovecii pneumonia: The importance of radiological diagnostic and HIV testing. Radiol. Case Rep. 2021;16:3685–3689. doi: 10.1016/j.radcr.2021.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Giamarellos-Bourboulis E.J., Netea M.G., Rovina N., Akinosoglou K., Antoniadou A., Antonakos N., Damoraki G., Gkavogianni T., Adami M.E., Katsaounou P., et al. Complex immune dysregulation in COVID-19 patients with severe respiratory failure. Cell Host Microbe. 2020;27:992–1000.e3. doi: 10.1016/j.chom.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Zhou Y., Fu B., Zheng X., Wang D., Zhao C., Qi Y., Sun R., Tian Z., Xu X., Wei H. Pathogenic T-cells and inflammatory monocytes incite inflammatory storms in severe COVID-19 patients. Natl. Sci. Rev. 2020;7:998–1002. doi: 10.1093/nsr/nwaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Liu R., Wang Y., Li J., Han H., Xia Z., Liu F., Wu K., Yang L., Liu X., Zhu C. Decreased T cell populations contribute to the increased severity of COVID-19. Clin. Chim. Acta. 2020;508:110–114. doi: 10.1016/j.cca.2020.05.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Rydyznski Moderbacher C., Ramirez S.I., Dan J.M., Grifoni A., Hastie K.M., Weiskopf D., Belanger S., Abbott R.K., Kim C., Choi J., et al. Antigen-specific adaptive immunity to SARS-CoV-2 in acute COVID-19 and associations with age and disease severity. Cell. 2020;183:996–1012. doi: 10.1016/j.cell.2020.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 276.Silva M.J.A., Ribeiro L.R., Lima K.V.B., Lima L. Adaptive immunity to SARS-CoV-2 infection: A systematic review. Front. Immunol. 2022;13:1001198. doi: 10.3389/fimmu.2022.1001198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.Haunhorst S., Bloch W., Javelle F., Kruger K., Baumgart S., Drube S., Lemhofer C., Reuken P., Stallmach A., Muller M., et al. A scoping review of regulatory T cell dynamics in convalescent COVID-19 patients—Indications for their potential involvement in the development of Long COVID? Front. Immunol. 2022;13:1070994. doi: 10.3389/fimmu.2022.1070994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Biswas B., Chattopadhyay S., Hazra S., Hansda A.K., Goswami R. COVID-19 pandemic: The delta variant, T-cell responses, and the efficacy of developing vaccines. Inflamm. Res. 2022;71:377–396. doi: 10.1007/s00011-022-01555-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 279.Liu K., Yang T., Peng X.F., Lv S.M., Ye X.L., Zhao T.S., Li J.C., Shao Z.J., Lu Q.B., Li J.Y., et al. A systematic meta-analysis of immune signatures in patients with COVID-19. Rev. Med. Virol. 2021;31:e2195. doi: 10.1002/rmv.2195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Jiang M., Guo Y., Luo Q., Huang Z., Zhao R., Liu S., Le A., Li J., Wan L. T-cell subset counts in peripheral blood can be used as discriminatory biomarkers for diagnosis and severity prediction of coronavirus disease 2019. J. Infect. Dis. 2020;222:198–202. doi: 10.1093/infdis/jiaa252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Mathew D., Giles J.R., Baxter A.E., Oldridge D.A., Greenplate A.R., Wu J.E., Alanio C., Kuri-Cervantes L., Pampena M.B., D’Andrea K., et al. Deep immune profiling of COVID-19 patients reveals distinct immunotypes with therapeutic implications. Science. 2020;369:eabc8511. doi: 10.1126/science.abc8511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 282.Wang F., Nie J., Wang H., Zhao Q., Xiong Y., Deng L., Song S., Ma Z., Mo P., Zhang Y. Characteristics of peripheral lymphocyte subset alteration in COVID-19 pneumonia. J. Infect. Dis. 2020;221:1762–1769. doi: 10.1093/infdis/jiaa150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Westmeier J., Paniskaki K., Karakose Z., Werner T., Sutter K., Dolff S., Overbeck M., Limmer A., Liu J., Zheng X., et al. Impaired cytotoxic CD8(+) T cell response in elderly COVID-19 patients. MBio. 2020;11:e02243-20. doi: 10.1128/mBio.02243-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Moss P. The T cell immune response against SARS-CoV-2. Nat. Immunol. 2022;23:186–193. doi: 10.1038/s41590-021-01122-w. [DOI] [PubMed] [Google Scholar]
- 285.Shen X.R., Geng R., Li Q., Chen Y., Li S.F., Wang Q., Min J., Yang Y., Li B., Jiang R.D., et al. ACE2-independent infection of T lymphocytes by SARS-CoV-2. Signal Transduct. Target. Ther. 2022;7:83. doi: 10.1038/s41392-022-00919-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Szydlowicz M., Matos O. Pneumocystis pneumonia in the COVID-19 pandemic era: Similarities and challenges. Trends Parasitol. 2021;37:859–862. doi: 10.1016/j.pt.2021.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Casalini G., Giacomelli A., Ridolfo A., Gervasoni C., Antinori S. Invasive fungal infections complicating COVID-19: A Narrative Review. J. Fungi. 2021;7:921. doi: 10.3390/jof7110921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Mina S., Yaakoub H., Annweiler C., Dubee V., Papon N. COVID-19 and fungal infections: A double debacle. Microbes Infect. 2022;24:105039. doi: 10.1016/j.micinf.2022.105039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Burghi G., Biard L., Roux A., Valade S., Robert-Gangneux F., Hamane S., Maubon D., Debourgogne A., Le Gal S., Dalle F., et al. Characteristics and outcome according to underlying disease in non-AIDS patients with acute respiratory failure due to Pneumocystis pneumonia. Eur. J. Clin. Microbiol. Infect. Dis. 2021;40:1191–1198. doi: 10.1007/s10096-020-04118-w. [DOI] [PubMed] [Google Scholar]
- 290.Ling C., Qian S., Wang Q., Zeng J., Jia X., Liu J., Li Z. Pneumocystis pneumonia in non-HIV children: A 10-year retrospective study. Clin. Respir. J. 2018;12:16–22. doi: 10.1111/crj.12467. [DOI] [PubMed] [Google Scholar]
- 291.Shoji K., Michihata N., Miyairi I., Matsui H., Fushimi K., Yasunaga H. Recent epidemiology of Pneumocystis pneumonia in Japan. J. Infect. Chemother. 2020;26:1260–1264. doi: 10.1016/j.jiac.2020.07.006. [DOI] [PubMed] [Google Scholar]
- 292.Charpentier E., Menard S., Marques C., Berry A., Iriart X. Immune response in Pneumocystis infections according to the host immune system status. J. Fungi. 2021;7:625. doi: 10.3390/jof7080625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 293.Otieno-Odhiambo P., Wasserman S., Hoving J.C. The contribution of host cells to Pneumocystis immunity: An Update. Pathogens. 2019;8:52. doi: 10.3390/pathogens8020052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Burke B.A., Good R.A. Pneumocystis carinii infection. Medicine. 1973;52:23–51. doi: 10.1097/00005792-197301000-00002. [DOI] [PubMed] [Google Scholar]
- 295.Masur H., Ognibene F.P., Yarchoan R., Shelhamer J.H., Baird B.F., Travis W., Suffredini A.F., Deyton L., Kovacs J.A., Falloon J., et al. CD4 counts as predictors of opportunistic pneumonias in human immunodeficiency virus (HIV) infection. Ann. Intern. Med. 1989;111:223–231. doi: 10.7326/0003-4819-111-3-223. [DOI] [PubMed] [Google Scholar]
- 296.Strehl C., Ehlers L., Gaber T., Buttgereit F. Glucocorticoids-all-rounders tackling the versatile players of the immune system. Front. Immunol. 2019;10:1744. doi: 10.3389/fimmu.2019.01744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Isaacs D. Infectious risks associated with biologics. Adv. Exp. Med. Biol. 2013;764:151–158. doi: 10.1007/978-1-4614-4726-9_12. [DOI] [PubMed] [Google Scholar]
- 298.Roberts M.B., Fishman J.A. Immunosuppressive agents and infectious risk in transplantation: Managing the “Net State of Immunosuppression”. Clin. Infect. Dis. 2021;73:e1302–e1317. doi: 10.1093/cid/ciaa1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Hashiguchi Y., Kasai M., Fukuda T., Ichimura T., Yasui T., Sumi T. Chemotherapy-induced neutropenia and febrile neutropenia in patients with gynecologic malignancy. Anticancer. Drugs. 2015;26:1054–1060. doi: 10.1097/CAD.0000000000000279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Classen A.Y., Henze L., von Lilienfeld-Toal M., Maschmeyer G., Sandherr M., Graeff L.D., Alakel N., Christopeit M., Krause S.W., Mayer K., et al. Primary prophylaxis of bacterial infections and Pneumocystis jirovecii pneumonia in patients with hematologic malignancies and solid tumors: 2020 updated guidelines of the Infectious Diseases Working Party of the German Society of Hematology and Medical Oncology (AGIHO/DGHO) Ann. Hematol. 2021;100:1603–1620. doi: 10.1007/s00277-021-04452-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 301.Ruckert M., Flohr A.S., Hecht M., Gaipl U.S. Radiotherapy and the immune system: More than just immune suppression. Stem Cells. 2021;39:1155–1165. doi: 10.1002/stem.3391. [DOI] [PubMed] [Google Scholar]
- 302.Hiam-Galvez K.J., Allen B.M., Spitzer M.H. Systemic immunity in cancer. Nat. Rev. Cancer. 2021;21:345–359. doi: 10.1038/s41568-021-00347-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Mortaz E., Tabarsi P., Mansouri D., Khosravi A., Garssen J., Velayati A., Adcock I.M. Cancers related to immunodeficiencies: Update and perspectives. Front. Immunol. 2016;7:365. doi: 10.3389/fimmu.2016.00365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Gonzalez H., Hagerling C., Werb Z. Roles of the immune system in cancer: From tumor initiation to metastatic progression. Genes. Dev. 2018;32:1267–1284. doi: 10.1101/gad.314617.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Duncan M.D., Wilkes D.S. Transplant-related immunosuppression: A review of immunosuppression and pulmonary infections. Proc. Am. Thorac. Soc. 2005;2:449–455. doi: 10.1513/pats.200507-073JS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Hasan A., Al-Ozairi E., Al-Baqsumi Z., Ahmad R., Al-Mulla F. Cellular and humoral immune responses in COVID-19 and immunotherapeutic approaches. Immunotargets Ther. 2021;10:63–85. doi: 10.2147/ITT.S280706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Mazzoni A., Salvati L., Maggi L., Annunziato F., Cosmi L. Hallmarks of immune response in COVID-19: Exploring dysregulation and exhaustion. Semin. Immunol. 2021;55:101508. doi: 10.1016/j.smim.2021.101508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Morton C.O., Griffiths J.S., Loeffler J., Orr S., White P.L. Defective antifungal immunity in patients with COVID-19. Front. Immunol. 2022;13:1080822. doi: 10.3389/fimmu.2022.1080822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 309.Delliere S., Gits-Muselli M., Bretagne S., Alanio A. Outbreak-causing fungi: Pneumocystis jirovecii. Mycopathologia. 2020;185:783–800. doi: 10.1007/s11046-019-00408-w. [DOI] [PubMed] [Google Scholar]
- 310.Hardy A.M., Wajszczuk C.P., Suffredini A.F., Hakala T.R., Ho M. Pneumocystis carinii pneumonia in renal-transplant recipients treated with cyclosporine and steroids. J. Infect. Dis. 1984;149:143–147. doi: 10.1093/infdis/149.2.143. [DOI] [PubMed] [Google Scholar]
- 311.Hennequin C., Page B., Roux P., Legendre C., Kreis H. Outbreak of Pneumocystis carinii pneumonia in a renal transplant unit. Eur. J. Clin. Microbiol. Infect. Dis. 1995;14:122–126. doi: 10.1007/BF02111870. [DOI] [PubMed] [Google Scholar]
- 312.Olsson M., Eriksson B.M., Elvin K., Strandberg M., Wahlgren M. Genotypes of clustered cases of Pneumocystis carinii pneumonia. Scand. J. Infect. Dis. 2001;33:285–289. doi: 10.1080/003655401300077324. [DOI] [PubMed] [Google Scholar]
- 313.Hocker B., Wendt C., Nahimana A., Tonshoff B., Hauser P.M. Molecular evidence of Pneumocystis transmission in pediatric transplant unit. Emerg. Infect. Dis. 2005;11:330–332. doi: 10.3201/eid1102.040820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.de Boer M.G., Bruijnesteijn van Coppenraet L.E., Gaasbeek A., Berger S.P., Gelinck L.B., van Houwelingen H.C., van den Broek P., Kuijper E.J., Kroon F.P., Vandenbroucke J.P. An outbreak of Pneumocystis jiroveci pneumonia with 1 predominant genotype among renal transplant recipients: Interhuman transmission or a common environmental source? Clin. Infect. Dis. 2007;44:1143–1149. doi: 10.1086/513198. [DOI] [PubMed] [Google Scholar]
- 315.Schmoldt S., Schuhegger R., Wendler T., Huber I., Sollner H., Hogardt M., Arbogast H., Heesemann J., Bader L., Sing A. Molecular evidence of nosocomial Pneumocystis jirovecii transmission among 16 patients after kidney transplantation. J. Clin. Microbiol. 2008;46:966–971. doi: 10.1128/JCM.02016-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Yazaki H., Goto N., Uchida K., Kobayashi T., Gatanaga H., Oka S. Outbreak of Pneumocystis jiroveci pneumonia in renal transplant recipients: P. jiroveci is contagious to the susceptible host. Transplantation. 2009;88:380–385. doi: 10.1097/TP.0b013e3181aed389. [DOI] [PubMed] [Google Scholar]
- 317.Arichi N., Kishikawa H., Mitsui Y., Kato T., Nishimura K., Tachikawa R., Tomii K., Shiina H., Igawa M., Ichikawa Y. Cluster outbreak of Pneumocystis pneumonia among kidney transplant patients within a single center. Transplant. Proc. 2009;41:170–172. doi: 10.1016/j.transproceed.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 318.Gianella S., Haeberli L., Joos B., Ledergerber B., Wuthrich R.P., Weber R., Kuster H., Hauser P.M., Fehr T., Mueller N.J. Molecular evidence of interhuman transmission in an outbreak of Pneumocystis jirovecii pneumonia among renal transplant recipients. Transpl. Infect. Dis. 2010;12:1–10. doi: 10.1111/j.1399-3062.2009.00447.x. [DOI] [PubMed] [Google Scholar]
- 319.Wynckel A., Toubas D., Noel N., Toupance O., Rieu P. Outbreak of pneumocystis pneumonia occurring in late post-transplantation period. Nephrol. Dial. Transplant. 2011;26:2417. doi: 10.1093/ndt/gfr159. [DOI] [PubMed] [Google Scholar]
- 320.Phipps L.M., Chen S.C., Kable K., Halliday C.L., Firacative C., Meyer W., Wong G., Nankivell B.J. Nosocomial Pneumocystis jirovecii pneumonia: Lessons from a cluster in kidney transplant recipients. Transplantation. 2011;92:1327–1334. doi: 10.1097/TP.0b013e3182384b57. [DOI] [PubMed] [Google Scholar]
- 321.Thomas S., Vivancos R., Corless C., Wood G., Beeching N.J., Beadsworth M.B. Increasing frequency of Pneumocystis jirovecii pneumonia in renal transplant recipients in the United Kingdom: Clonal variability, clusters, and geographic location. Clin. Infect. Dis. 2011;53:307–308. doi: 10.1093/cid/cir329. [DOI] [PubMed] [Google Scholar]
- 322.Pliquett R.U., Asbe-Vollkopf A., Hauser P.M., Presti L.L., Hunfeld K.P., Berger A., Scheuermann E.H., Jung O., Geiger H., Hauser I.A. A Pneumocystis jirovecii pneumonia outbreak in a single kidney-transplant center: Role of cytomegalovirus co-infection. Eur. J. Clin. Microbiol. Infect. Dis. 2012;31:2429–2437. doi: 10.1007/s10096-012-1586-x. [DOI] [PubMed] [Google Scholar]
- 323.Brunot V., Pernin V., Chartier C., Garrigue V., Vetromile F., Szwarc I., Delmas S., Portales P., Basset D., Mourad G. An epidemic of Pneumocystis jiroveci pneumonia in a renal transplantation center: Role of T-cell lymphopenia. Transplant. Proc. 2012;44:2818–2820. doi: 10.1016/j.transproceed.2012.09.089. [DOI] [PubMed] [Google Scholar]
- 324.Chapman J.R., Marriott D.J., Chen S.C., MacDonald P.S. Post-transplant Pneumocystis jirovecii pneumonia--a re-emerged public health problem? Kidney Int. 2013;84:240–243. doi: 10.1038/ki.2013.212. [DOI] [PubMed] [Google Scholar]
- 325.Nankivell B.J., Firacative C., Kable K., Chen S.C., Meyer W. Molecular epidemiology linking multihospital clusters of opportunistic Pneumocystis jirovecii pneumonia. Clin. Infect. Dis. 2013;57:1058–1059. doi: 10.1093/cid/cit413. [DOI] [PubMed] [Google Scholar]
- 326.Rostved A.A., Sassi M., Kurtzhals J.A., Sorensen S.S., Rasmussen A., Ross C., Gogineni E., Huber C., Kutty G., Kovacs J.A., et al. Outbreak of Pneumocystis pneumonia in renal and liver transplant patients caused by genotypically distinct strains of Pneumocystis jirovecii. Transplantation. 2013;96:834–842. doi: 10.1097/TP.0b013e3182a1618c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Debourgogne A., Favreau S., Ladriere M., Bourry S., Machouart M. Characteristics of Pneumocystis pneumonia in Nancy from January 2007 to April 2011 and focus on an outbreak in nephrology. J. Mycol. Med. 2014;24:19–24. doi: 10.1016/j.mycmed.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 328.Chandola P., Lall M., Sen S., Bharadwaj R. Outbreak of Pneumocystis jirovecii pneumonia in renal transplant recipients on prophylaxis: Our observation and experience. Indian. J. Med. Microbiol. 2014;32:333–336. doi: 10.4103/0255-0857.136594. [DOI] [PubMed] [Google Scholar]
- 329.Gits-Muselli M., Peraldi M.N., de Castro N., Delcey V., Menotti J., Guigue N., Hamane S., Raffoux E., Bergeron A., Valade S., et al. New short tandem repeat-based molecular typing method for Pneumocystis jirovecii reveals intrahospital transmission between patients from different wards. PLoS ONE. 2015;10:e0125763. doi: 10.1371/journal.pone.0125763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Desoubeaux G., Dominique M., Morio F., Thepault R.A., Franck-Martel C., Tellier A.C., Ferrandiere M., Hennequin C., Bernard L., Salame E., et al. epidemiological outbreaks of Pneumocystis jirovecii pneumonia are not limited to kidney transplant recipients: Genotyping confirms common source of transmission in a liver transplantation unit. J. Clin. Microbiol. 2016;54:1314–1320. doi: 10.1128/JCM.00133-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 331.Mulpuru S., Knoll G., Weir C., Desjardins M., Johnson D., Gorn I., Fairhead T., Bissonnette J., Bruce N., Toye B., et al. Pneumocystis pneumonia outbreak among renal transplant recipients at a North American transplant center: Risk factors and implications for infection control. Am. J. Infect. Control. 2016;44:425–431. doi: 10.1016/j.ajic.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 332.Urabe N., Ishii Y., Hyodo Y., Aoki K., Yoshizawa S., Saga T., Murayama S.Y., Sakai K., Homma S., Tateda K. Molecular epidemiologic analysis of a Pneumocystis pneumonia outbreak among renal transplant patients. Clin. Microbiol. Infect. 2016;22:365–371. doi: 10.1016/j.cmi.2015.12.017. [DOI] [PubMed] [Google Scholar]
- 333.Inkster T., Dodd S., Gunson R., Imrie L., Spalding E., Packer S., Deighan C., Daly C., Coia J., Imtiaz T., et al. Investigation of outbreaks of Pneumocystis jirovecii pneumonia in two Scottish renal units. J. Hosp. Infect. 2017;96:151–156. doi: 10.1016/j.jhin.2016.11.005. [DOI] [PubMed] [Google Scholar]
- 334.Robin C., Alanio A., Gits-Muselli M., la Martire G., Schlemmer F., Botterel F., Angebault C., Leclerc M., Beckerich F., Redjoul R., et al. Molecular demonstration of a Pneumocystis outbreak in stem cell transplant patients: Evidence for transmission in the daycare center. Front. Microbiol. 2017;8:700. doi: 10.3389/fmicb.2017.00700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Frealle E., Valade S., Guigue N., Hamane S., Chabe M., Le Gal S., Damiani C., Totet A., Aliouat E.M., Nevez G., et al. Diffusion of Pneumocystis jirovecii in the surrounding air of patients with Pneumocystis colonization: Frequency and putative risk factors. Med. Mycol. 2017;55:568–572. doi: 10.1093/mmy/myw113. [DOI] [PubMed] [Google Scholar]
- 336.Alanio A., Gits-Muselli M., Guigue N., Desnos-Ollivier M., Calderon E.J., Di Cave D., Dupont D., Hamprecht A., Hauser P.M., Helweg-Larsen J., et al. Diversity of Pneumocystis jirovecii across Europe: A multicentre observational study. EBioMedicine. 2017;22:155–163. doi: 10.1016/j.ebiom.2017.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.Wintenberger C., Maubon D., Charpentier E., Rendu J., Pavese P., Augier C., Malvezzi P., Camara B., Mallaret M.R., Bouillet L., et al. Grouped cases of pulmonary pneumocystosis after solid organ transplantation: Advantages of coordination by an infectious diseases unit for overall management and epidemiological monitoring. Infect. Control Hosp. Epidemiol. 2017;38:179–185. doi: 10.1017/ice.2016.274. [DOI] [PubMed] [Google Scholar]
- 338.Charpentier E., Garnaud C., Wintenberger C., Bailly S., Murat J.B., Rendu J., Pavese P., Drouet T., Augier C., Malvezzi P., et al. Added Value of Next-generation sequencing for multilocus sequence typing analysis of a Pneumocystis jirovecii pneumonia outbreak1. Emerg. Infect. Dis. 2017;23:1237–1245. doi: 10.3201/eid2308.161295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 339.Nevez G., Le Gal S., Noel N., Wynckel A., Huguenin A., Le Govic Y., Pougnet L., Virmaux M., Toubas D., Bajolet O. Investigation of nosocomial Pneumocystis infections: Usefulness of longitudinal screening of epidemic and post-epidemic Pneumocystis genotypes. J. Hosp. Infect. 2018;99:332–345. doi: 10.1016/j.jhin.2017.09.015. [DOI] [PubMed] [Google Scholar]
- 340.Ricci G., Santos D.W., Kovacs J.A., Nishikaku A.S., de Sandes-Freitas T.V., Rodrigues A.M., Kutty G., Affonso R., Silva H.T., Medina-Pestana J.O., et al. Genetic diversity of Pneumocystis jirovecii from a cluster of cases of pneumonia in renal transplant patients: Cross-sectional study. Mycoses. 2018;61:845–852. doi: 10.1111/myc.12823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 341.Veronese G., Ammirati E., Moioli M.C., Baldan R., Orcese C.A., De Rezende G., Veronese S., Masciocco G., Perna E., Travi G., et al. Single-center outbreak of Pneumocystis jirovecii pneumonia in heart transplant recipients. Transpl. Infect. Dis. 2018;20:e12880. doi: 10.1111/tid.12880. [DOI] [PubMed] [Google Scholar]
- 342.Szydlowicz M., Jakuszko K., Szymczak A., Piesiak P., Kowal A., Kopacz Z., Wesolowska M., Lobo M.L., Matos O., Hendrich A.B., et al. Prevalence and genotyping of Pneumocystis jirovecii in renal transplant recipients-preliminary report. Parasitol. Res. 2019;118:181–189. doi: 10.1007/s00436-018-6131-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Hosseini-Moghaddam S.M., Dufresne P.J., Hunter Gutierrez E., Dufresne S.F., House A.A., Humar A., Kumar D., Jevnikar A.M. Long-lasting cluster of nosocomial pneumonia with a single Pneumocystis jirovecii genotype involving different organ allograft recipients. Clin. Transplant. 2020;34:e14108. doi: 10.1111/ctr.14108. [DOI] [PubMed] [Google Scholar]
- 344.Yiannakis E.P., Boswell T.C. Systematic review of outbreaks of Pneumocystis jirovecii pneumonia: Evidence that P. jirovecii is a transmissible organism and the implications for healthcare infection control. J. Hosp. Infect. 2016;93:1–8. doi: 10.1016/j.jhin.2016.01.018. [DOI] [PubMed] [Google Scholar]
- 345.Hauser P., Rabodonirina M., Nevez G. Pneumocystis jirovecii genotypes involved in Pneumocystis pneumonia outbreaks among renal transplant recipients. Clin. Infect. Dis. 2013;56:165–166. doi: 10.1093/cid/cis810. [DOI] [PubMed] [Google Scholar]
- 346.Sassi M., Ripamonti C., Mueller N.J., Yazaki H., Kutty G., Ma L., Huber C., Gogineni E., Oka S., Goto N., et al. Outbreaks of Pneumocystis pneumonia in 2 renal transplant centers linked to a single strain of Pneumocystis: Implications for transmission and virulence. Clin. Infect. Dis. 2012;54:1437–1444. doi: 10.1093/cid/cis217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 347.Pifer L.L., Niell H.B., Morrison B.J., Counce J.D., Jr., Freeman J.M., Woods D.R., Neely C.L. Pneumocystis carinii antigenemia in adults with malignancy, infection, or pulmonary disease. J. Clin. Microbiol. 1984;20:887–890. doi: 10.1128/jcm.20.5.887-890.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Davis J.L., Welsh D.A., Beard C.B., Jones J.L., Lawrence G.G., Fox M.R., Crothers K., Morris A., Charbonnet D., Swartzman A., et al. Pneumocystis colonisation is common among hospitalised HIV infected patients with non-Pneumocystis pneumonia. Thorax. 2008;63:329–334. doi: 10.1136/thx.2007.088104. [DOI] [PubMed] [Google Scholar]
- 349.Medrano F.J., Montes-Cano M., Conde M., de la Horra C., Respaldiza N., Gasch A., Perez-Lozano M.J., Varela J.M., Calderon E.J. Pneumocystis jirovecii in general population. Emerg. Infect. Dis. 2005;11:245–250. doi: 10.3201/eid1102.040487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Ponce C.A., Gallo M., Bustamante R., Vargas S.L. Pneumocystis colonization is highly prevalent in the autopsied lungs of the general population. Clin. Infect. Dis. 2010;50:347–353. doi: 10.1086/649868. [DOI] [PubMed] [Google Scholar]
- 351.de la Horra C., Varela J.M., Fernandez-Alonso J., Medrano F.J., Respaldiza N., Montes-Cano M.A., Calderon E.J. Association between human-Pneumocystis infection and small-cell lung carcinoma. Eur. J. Clin. Invest. 2004;34:229–235. doi: 10.1111/j.1365-2362.2004.01317.x. [DOI] [PubMed] [Google Scholar]
- 352.Morris A., Sciurba F.C., Lebedeva I.P., Githaiga A., Elliott W.M., Hogg J.C., Huang L., Norris K.A. Association of chronic obstructive pulmonary disease severity and Pneumocystis colonization. Am. J. Respir. Crit. Care Med. 2004;170:408–413. doi: 10.1164/rccm.200401-094OC. [DOI] [PubMed] [Google Scholar]
- 353.Vidal S., de la Horra C., Martin J., Montes-Cano M.A., Rodriguez E., Respaldiza N., Rodriguez F., Varela J.M., Medrano F.J., Calderon E.J. Pneumocystis jirovecii colonisation in patients with interstitial lung disease. Clin. Microbiol. Infect. 2006;12:231–235. doi: 10.1111/j.1469-0691.2005.01337.x. [DOI] [PubMed] [Google Scholar]
- 354.Vargas S.L., Hughes W.T., Santolaya M.E., Ulloa A.V., Ponce C.A., Cabrera C.E., Cumsille F., Gigliotti F. Search for primary infection by Pneumocystis carinii in a cohort of normal, healthy infants. Clin. Infect. Dis. 2001;32:855–861. doi: 10.1086/319340. [DOI] [PubMed] [Google Scholar]
- 355.Vera C., Aguilar Y.A., Velez L.A., Rueda Z.V. High transient colonization by Pneumocystis jirovecii between mothers and newborn. Eur. J. Pediatr. 2017;176:1619–1627. doi: 10.1007/s00431-017-3011-z. [DOI] [PubMed] [Google Scholar]
- 356.Ma L., Chen Z., Huangda W., Kutty G., Ishihara M., Wang H., Abouelleil A., Bishop L., Davey E., Deng R., et al. Genome analysis of three Pneumocystis species reveals adaptation mechanisms to life exclusively in mammalian hosts. Nat. Commun. 2016;7:10740. doi: 10.1038/ncomms10740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Ma L., Chen Z., Huang D.W., Cisse O.H., Rothenburger J.L., Latinne A., Bishop L., Blair R., Brenchley J.M., Chabe M., et al. Diversity and complexity of the large surface protein family in the compacted genomes of multiple Pneumocystis species. MBio. 2020;11:e02878-19. doi: 10.1128/mBio.02878-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 358.Vestereng V.H., Bishop L.R., Hernandez B., Kutty G., Larsen H.H., Kovacs J.A. Quantitative real-time polymerase chain-reaction assay allows characterization of Pneumocystis infection in immunocompetent mice. J. Infect. Dis. 2004;189:1540–1544. doi: 10.1086/382486. [DOI] [PubMed] [Google Scholar]
- 359.Weissenbacher-Lang C., Blasi B., Bauer P., Binanti D., Bittermann K., Ergin L., Hogler C., Hogler T., Klier M., Matt J., et al. Detection of Pneumocystis and morphological description of fungal distribution and severity of infection in thirty-six mammal species. J. Fungi. 2023;9:220. doi: 10.3390/jof9020220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Casadevall A., Pirofski L.A. The damage-response framework of microbial pathogenesis. Nat. Rev. Microbiol. 2003;1:17–24. doi: 10.1038/nrmicro732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Chen W., Gigliotti F., Harmsen A.G. Latency is not an inevitable outcome of infection with Pneumocystis carinii. Infect. Immun. 1993;61:5406–5409. doi: 10.1128/iai.61.12.5406-5409.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Keely S.P., Stringer J.R., Baughman R.P., Linke M.J., Walzer P.D., Smulian A.G. Genetic variation among Pneumocystis carinii hominis isolates in recurrent pneumocystosis. J. Infect. Dis. 1995;172:595–598. doi: 10.1093/infdis/172.2.595. [DOI] [PubMed] [Google Scholar]
- 363.Tsolaki A.G., Miller R.F., Underwood A.P., Banerji S., Wakefield A.E. Genetic diversity at the internal transcribed spacer regions of the rRNA operon among isolates of Pneumocystis carinii from AIDS patients with recurrent pneumonia. J. Infect. Dis. 1996;174:141–156. doi: 10.1093/infdis/174.1.141. [DOI] [PubMed] [Google Scholar]
- 364.de la Horra C., Friaza V., Morilla R., Delgado J., Medrano F.J., Miller R.F., de Armas Y., Calderon E.J. Update on dihydropteroate synthase (DHPS) mutations in Pneumocystis jirovecii. J. Fungi. 2021;7:856. doi: 10.3390/jof7100856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 365.Deng X., Zhuo L., Lan Y., Dai Z., Chen W.S., Cai W., Kovacs J.A., Ma L., Tang X. Mutational analysis of Pneumocystis jirovecii dihydropteroate synthase and dihydrofolate reductase genes in HIV-infected patients in China. J. Clin. Microbiol. 2014;52:4017–4019. doi: 10.1128/JCM.01848-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Ma L., Borio L., Masur H., Kovacs J.A. Pneumocystis carinii dihydropteroate synthase but not dihydrofolate reductase gene mutations correlate with prior trimethoprim-sulfamethoxazole or dapsone use. J. Infect. Dis. 1999;180:1969–1978. doi: 10.1086/315148. [DOI] [PubMed] [Google Scholar]
- 367.Siegel J.D., Rhinehart E., Jackson M., Chiarello L., Health Care Infection Control Practices Advisory C. 2007 guideline for isolation precautions: Preventing transmission of infectious agents in health care settings. Am. J. Infect. Control. 2007;35:S65–S164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 368.Mok C.C., Hamijoyo L., Kasitanon N., Chen D.Y., Chen S.C., Yamaoka K., Oku K., L’i M.T., Zamora L. The Asia-Pacific League of Associations for Rheumatology consensus statements on the management of systemic lupus erythematosus. Lancet Rheumatol. 2021;3:e517–e531. doi: 10.1016/S2665-9913(21)00009-6. [DOI] [PubMed] [Google Scholar]
- 369.Chen S.C., Sorrell T.C., Chang C.C., Paige E.K., Bryant P.A., Slavin M.A. Consensus guidelines for the treatment of yeast infections in the haematology, oncology and intensive care setting, 2014. Intern. Med. J. 2014;44:1315–1332. doi: 10.1111/imj.12597. [DOI] [PubMed] [Google Scholar]
- 370.Fragoulis G.E., Nikiphorou E., Dey M., Zhao S.S., Courvoisier D.S., Arnaud L., Atzeni F., Behrens G.M., Bijlsma J.W., Bohm P., et al. 2022 EULAR recommendations for screening and prophylaxis of chronic and opportunistic infections in adults with autoimmune inflammatory rheumatic diseases. Ann. Rheum. Dis. 2022;82:742–753. doi: 10.1136/ard-2022-223335. [DOI] [PubMed] [Google Scholar]
- 371.Reinwald M., Silva J.T., Mueller N.J., Fortun J., Garzoni C., de Fijter J.W., Fernandez-Ruiz M., Grossi P., Aguado J.M. ESCMID study group for infections in compromised hosts (ESGICH) consensus document on the safety of targeted and biological therapies: An infectious diseases perspective (Intracellular signaling pathways: Tyrosine kinase and mTOR inhibitors) Clin. Microbiol. Infect. 2018;24((Suppl. 2)):S53–S70. doi: 10.1016/j.cmi.2018.02.009. [DOI] [PubMed] [Google Scholar]
- 372.Christopeit M., Schmidt-Hieber M., Sprute R., Buchheidt D., Hentrich M., Karthaus M., Penack O., Ruhnke M., Weissinger F., Cornely O.A., et al. Prophylaxis, diagnosis and therapy of infections in patients undergoing high-dose chemotherapy and autologous haematopoietic stem cell transplantation. 2020 update of the recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Medical Oncology (DGHO) Ann. Hematol. 2021;100:321–336. doi: 10.1007/s00277-020-04297-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Kameda H., Fujii T., Nakajima A., Koike R., Sagawa A., Kanbe K., Tomita T., Harigai M., Suzuki Y., Japan College of Rheumatology Subcommittee on the Guideline for the Use of Methotrexate in Patients with Rheumatoid Arthritis Japan College of Rheumatology guideline for the use of methotrexate in patients with rheumatoid arthritis. Mod. Rheumatol. 2019;29:31–40. doi: 10.1080/14397595.2018.1472358. [DOI] [PubMed] [Google Scholar]
- 374.Rua-Figueroa Fernandez de Larrinoa I., Carreira P.E., Brito Garcia N., Diaz Del Campo Fontecha P., Pego Reigosa J.M., Gomez Puerta J.A., Ortega-Castro R., Tejera Segura B., Aguado Garcia J.M., Torre-Cisneros J., et al. Recommendations for prevention of infection in systemic autoimmune rheumatic diseases. Reumatol. Clin. 2022;18:317–330. doi: 10.1016/j.reumae.2021.04.003. [DOI] [PubMed] [Google Scholar]
- 375.Proudfoot R., Phillips B., Wilne S. Guidelines for the prophylaxis of Pneumocystis jirovecii pneumonia (PJP) in children with solid tumors. J. Pediatr. Hematol. Oncol. 2017;39:194–202. doi: 10.1097/MPH.0000000000000771. [DOI] [PubMed] [Google Scholar]
- 376.Tieu J., Smith R., Basu N., Brogan P., D’Cruz D., Dhaun N., Flossmann O., Harper L., Jones R.B., Lanyon P.C., et al. Rituximab for maintenance of remission in ANCA-associated vasculitis: Expert consensus guidelines. Rheumatology. 2020;59:e24–e32. doi: 10.1093/rheumatology/kez640. [DOI] [PubMed] [Google Scholar]
- 377.Taplitz R.A., Kennedy E.B., Bow E.J., Crews J., Gleason C., Hawley D.K., Langston A.A., Nastoupil L.J., Rajotte M., Rolston K.V., et al. Antimicrobial prophylaxis for adult patients with cancer-related immunosuppression: ASCO and IDSA clinical practice guideline update. J. Clin. Oncol. 2018;36:3043–3054. doi: 10.1200/JCO.18.00374. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Not applicable.