Abstract
Background.
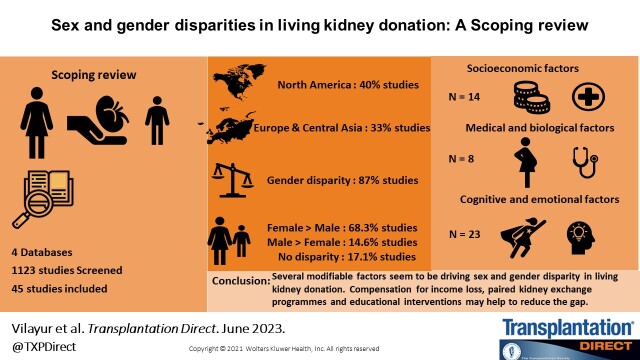
Women are more likely than men to be living kidney donors. We summarized the evidence concerning the reasons behind sex and gender disparities in living kidney donation (LKD).
Methods.
A scoping review of quantitative and qualitative evidence on reasons for sex and gender disparities in LKD was conducted from inception to March 2023.
Results.
Of 1123 studies screened, 45 were eligible for inclusion. Most studies were from North America, Europe, and Central Asia (n = 33, 73%). A predominance of women as living donors (55%–65%) was observed in 15 out of 18 (83%) studies. Reasons for sex and gender disparities in LKD included socioeconomic, biological, and cognitive or emotional factors. A gendered division of roles within the families was observed in most studies, with men being the primary income earner and women being the main caregiver. Fear of loss of income was a barrier to male donation. Human leukocyte antigen sensitization through pregnancy in female recipients precluded male partner donation, whereas female donation was supported by altruism and a positive attitude toward LKD.
Conclusions.
Sex imbalance in LKD is prevalent, with a predominance of women as living donors. Such disparities are driven by societal and cultural perceptions of gender roles, pregnancy-induced sensitization, and attitudes toward donation and at least some of these factors are modifiable. Donor compensation to support predonation assessments and income loss, implementation of innovative desensitization treatments, promotion of paired kidney exchange program, and targeted educational initiatives to promote equitable living donation may help to close the gender gap in LKD.
Global observational data has consistently shown that sex and gender disparities exist in living kidney donation, with women overrepresented as living donors.1-3 In high-income countries such as the United States, Canada, and Australia, approximately 60% of all living kidney donors are women.3-5 Similar findings are observed in lower-middle-income countries.6 These disparities are most marked in low-resource settings such as Bangladesh and Indonesia, where the proportion of women live donors, compared with men, has increased by 20% in the last decade, primarily driven by spousal donation.7,8
Despite the higher prevalence of nondialysis dependent chronic kidney disease among women,9 the global men-to-women kidney transplantation ratio is approximately 1.36.10 Sex disparity is even more pronounced in lower-middle-income countries such as India, Nepal, and Pakistan, where the probability of men receiving a kidney transplant is at least 10 times higher than women.10 More importantly, the proportion of women receiving a living kidney transplant from men is much lower than men receiving a living kidney transplant from women.11,12 That is, women predominantly give rather than receive a living donor kidney.
There are many potential reasons for the observed sex and gender disparities in living kidney donation, including factors across medical,1,13 socioeconomic,14 cultural, and cognitive or emotional15 domains. Root causes for the inequities may also differ between regions and countries. In countries such as India and Bangladesh, >70% of the living donors are women, and such disparities are driven largely by cultural and patriarchal norms16, whereas in countries such as the Philippines16 and Iran,17 financial drivers may be responsible for the observed disparity.8
Current observational data highlights the prevalence and magnitude of the existing sex and gender disparities in living kidney donation, but a comprehensive review evaluating the reasons behind this disparity across many settings is lacking. Through identification of the potential barriers and facilitators in the pathways to living kidney donation across sex and gender, we hope to inform the development of strategies to reduce this gap. In this scoping review, we aimed to identify and summarize all of the available evidence on the reasons behind the observed sex and gender disparities in living kidney donation globally. Understanding the reasons behind these disparities is critical to closing the gender gap and will guide the development of initiatives to promote equitable access to living donor kidney transplantation.
MATERIALS AND METHODS
We followed the Preferred Reporting Items for Systematic Review and Meta-Analyses extension for Scoping Reviews statement and the Joanna Briggs Institute Manual for Evidence Synthesis for the conduct and reporting of this review.18,19 Sex and gender data were taken as defined by the authors in the included studies. In this review, we used the term “gender” when the studies referred to the participants as being a woman, man, girl, boy, nonbinary, transgender, gender fluid, or queer. Sex is the biological assignment at birth, and therefore, the term “sex” was used if the studies referred to the participants as male, female, or intersex.20
Study Eligibility
We included all primary quantitative and qualitative studies published in peer-reviewed journal articles that examined the reasons for sex and gender disparities in living kidney donation. Studies were eligible if their populations were adult (aged ≥18 y) living kidney donors and/or potential donors of any gender or sex from all regions globally. Studies exploring the gender disparities in attitudes of the general adult population toward living kidney donation were also included. There were no time limits on publication dates. Non-English language publications were included if a translation was available. We excluded studies that examined only deceased donor transplantation, involved other living organ donors (eg, living liver donors), only included sex or gender disparities in outcomes of living kidney donation or described sex or gender disparities without considering reasons for disparities, only included sex or gender disparities in kidney recipients, were written in non-English languages with no translation available, or were case studies, case series, editorials, commentaries, review articles, and abstracts if the full text was not available.
Search Strategies
We searched MEDLINE, Embase, PsychINFO, and CINAHL databases. All databases were searched from inception to March 2023. The search strategy included keywords and MeSH terms for “sex or gender disparity” combined with terms for “living kidney donation” using appropriate Boolean Operators. The search strategies for each of the databases are included in the Appendix (Table S1, SDC, http://links.lww.com/TXD/A562). We also searched Google Scholar and the grey literature database “Grey Matters” to identify additional reports of relevance in this area. The references of the identified papers were also reviewed to determine additional publications relevant to the topic.
Two reviewers (E.V. and M.C.) independently performed title and abstract screening using the Covidence software,21 with discrepancies resolved through discussion with senior coauthors (G.W., A.v.Z., T.C., S.K., M.W., and A.F.). Twenty-five percent of the title and abstract screening was double-screened, and discrepancies were resolved through discussion. Duplicates were removed by Covidence, with additional duplicates identified and removed during screening. The full-text screening was performed solely by the author (E.V.). There was further discussion with senior researchers during full-text screening to ensure complete agreement between team members.
Data Extraction
We developed a data extraction form for this review using Covidence and extracted the relevant information from individual studies. Information extracted included (i) author; (ii) study title; (iii) y of publication; (iv) country of publication based on world bank classification of countries by regions; (v) study design; (vi) study methodology and analysis; (vii) aim of the study; (viii) study participants (living kidney donors or potential donors or general population); (ix) sample size; (x) participant characteristics including age range, gender proportion, employment, education, and income when available; (xi) proportion of successful and excluded donors when relevant; and (xii) proportion of men and women supporting donation or willing to donate in the general population-based studies.
Data Synthesis
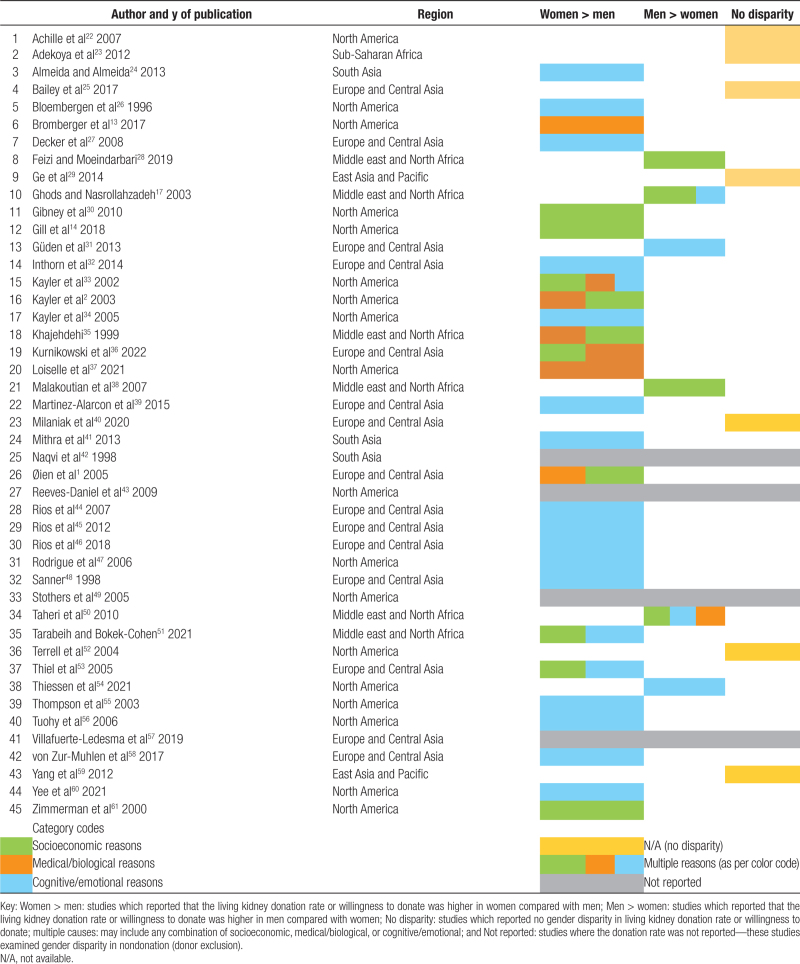
Descriptive statistics were used to synthesize and summarize the study characteristics and participant demographics. Studies were categorized based on 3 different aspects: the presence or absence of sex/gender disparities in living kidney donation, the presence or absence of sex/gender disparities in the willingness to donate, and reasons/factors associated with sex/gender disparity in living kidney donation. They are summarized in Table 1.
TABLE 1.
Summary of findings.
RESULTS
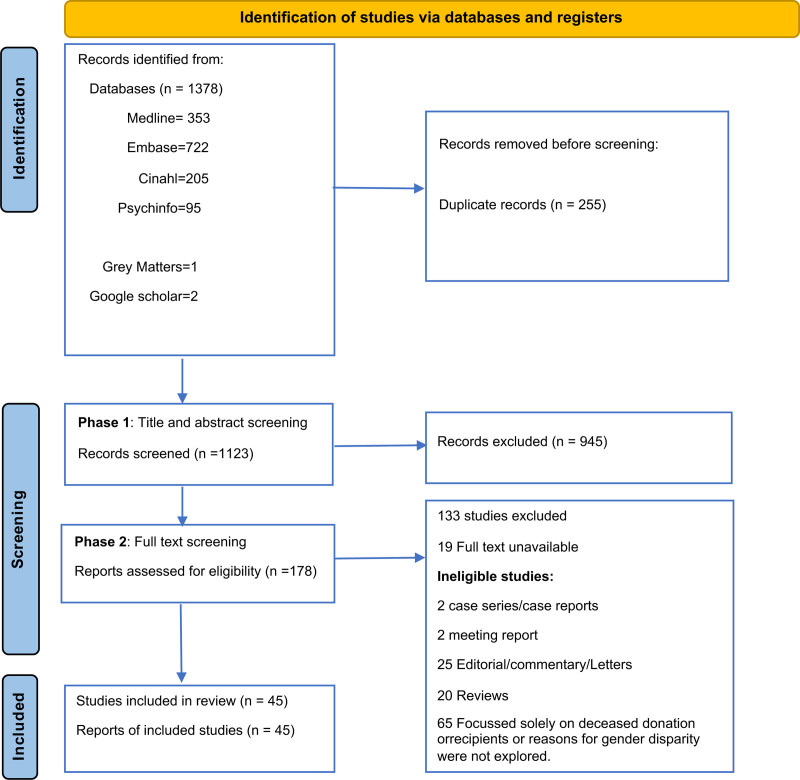
A total of 1378 studies were identified, of which 1123 remained for the title and abstract screening after duplicate removal. Of these, 178 proceeded to full-text screening, and 45 studies were eligible and included in the review (Figure 1).
FIGURE 1.
PRISMA flow diagram of study selection. PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analyses.
Study Characteristics
Detailed characteristics of each study are presented in Table S2 (SDC, http://links.lww.com/TXD/A562) and summarized across studies in Table 2. Most studies were from North America (n = 18, 40%), followed by Europe and Central Asia (n = 15, 33%). Most studies (n = 43, 96%) used quantitative methods (cross-sectional n = 34, ecological n = 2, cohort n = 6, case-control n = 1), whereas 1 mixed methods study focused on the perceptions of living donors in the adult population and assessed donor-risk tolerance.54 One qualitative study from the Middle East evaluated the perceptions of parents who were living kidney donors for their children with kidney failure (Table 2).42 None of the studies included nonbinary categories for gender.
TABLE 2.
Characteristics of included studies (n = 45).
| Description | N (%) |
|---|---|
| Publication y | |
| 2000 and before | 5 (11.1) |
| 2001–2010 | 18 (40.0) |
| 2011–2020 | 17 (37.8) |
| After 2020 | 5 (11.1) |
| Country (World Bank Region) | |
| North America | 18 (40) |
| Europe and Central Asia | 15 (33.3) |
| East Asia and the Pacific | 2 (4.4) |
| Middle East and North Africa | 6 (13.3) |
| South Asia | 3 (6.6) |
| Latin America and Caribbean | 0 (0) |
| Sub-Saharan Africa | 1 (2.2) |
| Sample size | |
| ≤500 | 16 (35.6) |
| 501–1000 | 13 (28.9) |
| 1001–5000 | 10 (22.2) |
| 5001–10 000 | 1 (2.22) |
| >10 000 | 5 (11.1) |
| Proportion of male participants | |
| <25% | 2 (4.4) |
| 26%–50% | 28 (62.2) |
| 51%–75% | 3 (6.7) |
| >75% | 4 (8.9) |
| Not specified | 8 (17.8) |
| Study design | |
| Cohort | 6 (13.3) |
| Cross-sectional | 34 (75.6) |
| Ecological | 2 (4.4) |
| Case-control | 1 (2.2) |
| Qualitative | 1 (2.2) |
| Mixed (qualitative and quantitative) | 1 (2.2) |
| Study population | |
| Living kidney donors | 15 (33.3) |
| Potential living donors | 11 (24.4) |
| General population | 16 (35.6) |
| Recipients/caregivers | 2 (4.4) |
| Living kidney donors/potential donors | 1 (2.2) |
Reasons and Factors Associated With Sex and Gender Disparities
Thirty-eight (87%) studies reported evidence of sex or gender disparity in living kidney donation, donor suitability, and the attitudes toward living kidney donation, whereas 7 (13%) studies reported the absence of these disparities (Table 1).22,23,25,29,40,52,59 A predominance of women as living kidney donors was observed in 15 of 18 studies (83%) where the donation rate was reported (Table 1).1,2,14,26,30,33-36,47,53,56-58,61 Women comprised of 55%–65% all living kidney donors in these studies. Only 3 studies reported a higher proportion of donations from men (>75%), all of which were from Iran.17,38,50 Four key reasons that influenced sex and gender disparities in living kidney donation were identified and categorized as socioeconomic, biological, and cognitive or emotional factors. Some studies identified >1 reason for sex and gender disparity and were categorized as multiple factors (Table 1).
Socioeconomic Factors
Fourteen studies indicated that socioeconomic factors were potential reasons for the observed gender and sex disparity in living kidney donation (Table 1).1,14,17,28,30,33,35,36,38,49-51,53,61 Economic factors centered around family income and the primary income-earning role of men were the key drivers in this category.
Four studies from North America identified socioeconomic factors as the leading cause of gender disparity.14,30,49,61 A population-based study from the United States, which included 52 690 living kidney donors between 2005 and 2015, found that the overall donation rate declined in men but not in women during the study period. When the population was stratified into income quartiles, the effects of income on changes in donation rate over time were much more pronounced in men compared with women. Profound gender disparity was observed where women were twice more likely to donate to men than receiving a kidney from men. The authors concluded that the financial implications of donation might significantly impact donations from men because a greater proportion of men were the primary household income earners.14 Six studies from the Middle East and North Africa suggested socioeconomic factors as an important cause of gender disparity in living kidney donation.17,28,35,38,51,62 A qualitative study from Israel involving parents of children with kidney failure found that mothers were the dominant donors for their children because of their self-sacrificing nature and to protect their husbands who were the sole income earners for the family.51 Similarly, a longitudinal cohort study conducted in Pakistan reported that social reasons were the predominant causes of refusal to donate among males because they were the income providers for the family.42
The availability of medical insurance also played a key role in living kidney donation. Men were less likely to be covered by health insurance; hence, a lower proportion of men were considered living donors. These findings were consistent across North America and Europe. A North American study involving 10 021 living kidney donors found that a higher percentage of male donors were uninsured compared with female donors (19.5% versus 16.5%).30 Similarly, a lower-than-expected living donation rate in Switzerland was seen among men compared with women (40% versus 60%). The authors hypothesized that the observed disparity may be explained by the lack of financial assistance to cover the out-of-pocket expenses during the donation process.53 A recent ecological study (n = 36 666 living kidney donors) reported that a higher proportion of donors were women (compared with men), and the donation rate from women was higher than the expected sex distribution in the general population in 10 out of 14 countries. The authors concluded that gender disparity in employment was a potential explanation behind gender disparity in living kidney donation.36 In the context of paid donation in Iran, men were more willing to sell their kidneys at a lower cost compared with women.28 Four out of the 5 quantitative studies conducted in Iran reported a significantly higher proportion of living kidney donors were men (>80%) compared with women17,28,38,50 except a single-center study (n = 78), which reported a higher donation rate from women compared with men.35
Thus, low socioeconomic factors and its correlates are important reasons for the observed sex and gender disparities in living kidney donation in both high- and low-income countries. The perceived societal role of men as primary income earners and hence the fear of income loss and the lack of insurance among men are significant barriers to male living donation. Lower employment rate among women and their perceived need to protect the primary income earner in the household have facilitated female donation.
Biological or Medical Reasons
Eight studies highlighted underlying health issues or barriers pertaining to biological sex as explanatory factors for sex and gender disparities in living kidney donation (Table 1). In particular, the reasons for the observed disparity were related to the donors’ general health and the recipients’ sensitization status.
An observational study from the United States that involved >500 potential live donors found that women were more likely to be excluded from donation because of incidental discovery of reduced kidney function during the assessment process.43 Other medical reasons identified included a higher proportion of substance use in men35-37 and a higher proportion of men with coexisting comorbidities such as hypertension, chronic kidney disease,1,50 and diabetes.42 Spousal donation from men to their female partners was also precluded by pregnancy-induced HLA sensitization and further exacerbated by blood transfusion or prior transplants.2,13
Although there is some evidence suggesting that underlying health and certain lifestyle factors are potential barriers to living kidney donation in men and women, sensitization of women is a critical barrier to male spousal donation.
Cognitive and Emotional Reasons
Twenty-three studies in total indicated cognitive and emotional factors as causes of sex or gender disparity in living kidney donation. Altruism is an essential driver for living kidney donation.
Fourteen studies involving the general population, potential kidney donors, or live donors across 5 countries (United States, India, Sweden, Spain, and Germany) have shown that a higher proportion of women exhibited greater willingness, initiative, and volunteerism toward living kidney donation compared with men (Table 1).24,27,32,34,39,41,44-46,48,55,58,60 In general, women were less willing to accept any financial compensation for living kidney donation, including health insurance coverage, compared with men.27,32,47 Women were also more likely to discuss with families about living kidney organ donation.45,55 Three observational studies found that a greater proportion of women were willing to offer their kidneys to families and strangers compared with men.27,32,60
The perceived risks and fear of complications associated with living donation were also considered a hindrance to living kidney donation. The fear of open surgery,40,56 mutilation,44,45 kidney failure,24 and infertility42 were some of the concerns raised by both women and men in high- and lower-middle-income countries. Some authors indicated that certain cultures perceive surgical scars as unacceptable in women.50 In some places within Pakistan, unmarried women were prohibited from donating.42
In Iran, a predominance of living donations from men was observed.17,38,50 This may be explained by the financial incentive to donate as a regulated compensated donation is permitted in Iran. Additionally, there was a preference to donate to potential recipients of the same gender.50 A single study exploring religious leaders’ attitudes in Turkey showed a higher willingness to donate among men compared with women.31
Emotional factors such as the closeness of the relationship to the recipient were an important determining factor for donation. Globally, mothers donated more often than fathers, and this finding was consistent even in countries such as those in the Middle East, where men predominate as living donors compared with women.1,17,26,50 In a multicenter study from North America, the authors concluded that parental relationship was associated with a higher willingness to accept risks of kidney failure postdonation.54
Thus, there is good evidence to suggest that certain cognitive and emotional factors are potential facilitators in female living kidney donation, whereas other emotional factors such as perceived surgical and medical risks are barriers to male donation. Closeness of the relationship between donor and recipient is an important facilitator in living kidney donation globally. Of note, there is considerable cultural variation in countries such as Iran where a preponderance of male donors was observed.
Studies Showing No Sex and Gender Disparities
Seven studies reported the absence of sex and gender disparities in living kidney donation or willingness to donate.22,23,25,29,40,52,59 A large multicenter cohort study showed that donor race, age, and relationship with the recipient were important predictors, but sex and gender were not identified as influential factors.25
DISCUSSION
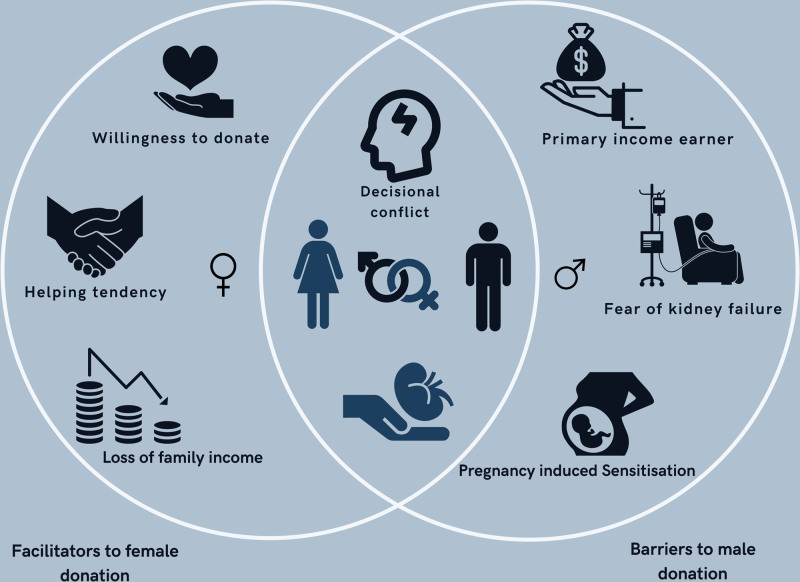
This scoping review summarizes all the published evidence concerning the reasons for sex and gender disparities in living kidney donation. There is clear evidence to suggest that women outnumber men as living kidney donors, with 83% of studies reporting donation rate showed a predominance of women as living donors. Across studies, approximately 55%–65% of living donors are women. This finding is largely consistent globally. There are many reasons for the observed inequality between men and women (Figure 2), but the key factors may include a higher full-time employment rate among men compared with women,36,61 men often being the primary income earner, the fear of income loss, and the lack of health insurance coverage and support during the process of living kidney donation.30,36,53,61
FIGURE 2.
Reasons for gender disparities in living kidney donation.
Of all the biological or medical reasons for gender disparity, pregnancy-induced HLA sensitization appears to be one of the most critical barriers to spousal donation by male partners.13 Despite men’s willingness to donate, women with previous pregnancies have high levels of donor specific HLA antibodies, which often precludes male spousal donation.2 Women were excluded from donation in a few instances because they have reduced estimated glomerular filtration rate.43 However, there was limited information to conclude whether the reduced kidney function was physiological or pathological. Altruism is a crucial driver for living kidney donation. Some studies have suggested specific characteristics such as being cooperative, self-sacrificing, and having strong concerns about the general well-being of others are some of the drivers for the observed higher rates of living kidney donation in women compared with men.41,46,58
Interventions to Reduce Sex and Gender Disparity in Living Kidney Donation
Our current study findings suggest several interventions that transplant programs may consider to address gender disparities in living kidney donation. There is now considerable evidence to suggest that socioeconomic, cultural, and emotional reasons are key drivers of gender disparity in living kidney donation. These factors could be potentially modifiable in society by policy changes and strategic planning.
Overcoming Socioeconomic Barriers
Universal health insurance coverage, provision of comprehensive income support for donors and reimbursement of all expenses associated with donation63 may alleviate the unforeseeable financial burden and out-of-pocket costs associated with the donation process. Legislative protection from job loss and insurance discrimination, tax credit on actual donor costs and other similar strategies to remove financial barriers to living kidney donation have been recommended at a consensus conference on best practices in living kidney donation held in Jun 2014 in Illinois, United States.64 Although such schemes have been implemented in some countries and recommended by experts in living kidney donation,65 instigating these strategies globally is a critical first step to reducing the inequities in living kidney donation.64 Implementing minimally invasive surgical techniques like laparoscopic donor nephrectomy would reduce hospital stay and facilitate early return to work, however, may not be easily implementable in lower-middle-income countries because of resource limitations.66 This could potentially reduce overall donor costs and loss of family income and hence increase live donation rate and balance the gender gap.67
Overcoming the Immunologic Barriers
Barriers to male spousal donation posed by pregnancy-induced sensitization may be addressed by enrolling incompatible donor-recipient pairs into paired kidney exchange programs. Political and legal barriers, cultural concerns regarding the concept of kidney exchange and prolonging cold ischemia time with kidney transportation may all be significant barriers in low-resource settings and may be overcome in future through strategic planning with involved stakeholders.68 In resource constrained settings, improving knowledge regarding kidney paired exchange program and engagement with established national programs may help guide the development of national paired kidney exchange programs. Enrolling HLA matched pairs in the paired exchange programs and considering ABO incompatible transplant is a potential option to improve transplant potential and opportunities for highly sensitized patients.69 Future research should consider implementation studies that assess the effectiveness and uptake of paired exchange programs to address the issues of HLA incompatibility in female recipients. Exploring the options of desensitization strategies using the available live donors with access to live donors is an alternative strategy where national paired kidney exchange programs are not available.70 Additionally, implementation of a molecular matching system program that allows matching at the epitope level may refine HLA matching and improve transplantation potential.71,72
Targeting Cognitive and Emotional Barriers
Targeted, individualized educational initiatives that are tailored to meet individuals’ needs and levels of health literacy may serve to clarify risk perceptions and enhance willingness to participate in living kidney donation among men.73 Trial-based evidence from North America and the Netherlands has shown that home-based family interventions may increase knowledge, communication, and live donation rates.74,75 Many women with kidney failure may struggle to initiate the conversations about kidney donation with their families. Therefore, family education and involvement from a social worker, or live donor champion, either from the hospital teams, a friend, or a community member, may alleviate some of the fears, and anxiety associated with living kidney donation.76 A multicomponent intervention including education and social network activation that addresses these issues in communication barriers and misinformation about living kidney donation is being trialed in the United Kingdom.77
Suggestions for Future Research
We suggest qualitative studies involving potential living donors, their respective recipients, and health providers should be conducted to further explore and understand the gender differences in the motivation and decisional conflict in living kidney donation. Using a codesign approach, novel interventions to support the male partners to donate, particularly from socioeconomically disadvantaged backgrounds, and target potential mediators of inequity, should be tested and evaluated in trial-based settings.
Strengths and Limitations
This scoping review has several strengths. We conducted a comprehensive and systematic search of 4 key scientific databases. Gray literature was also searched, given the complex nature of the topic. This scoping review examined the extent, range, and nature of the available evidence concerning sex and gender disparities in living kidney donation, with a specific focus on the underlying reasons and drivers. We extracted the available data systematically and classified studies based on country of origin, type of study, and the reasons for the disparities in each study. We found that very few large-scale studies identified the causes of donor exclusion and the reasons behind gender disparity in live donor attrition. The lack of trial-based quality evidence on effective strategies to improve the gender disparity in living kidney donation is a clear incentive to further explore novel initiatives that may be applicable in all settings, particularly in lower to lower-middle-income countries where the disparities are most marked.
This scoping review has some potential limitations. Across included studies, sex, and gender were not clearly and explicitly defined and there was a lack of studies on nonbinary people and other minority groups. Most studies were from North America (40%) and Europe (33%), with few publications from other parts of the world, which limits the generalizability of our study. Most studies were quantitative based on registry data and were therefore subject to the inherent risks of confounding and selection biases. In certain registry studies, the reasons behind observed gender disparities were hypothesized by authors based on limited data. The lack of granular data on social and cultural factors precluded a detailed assessment of the intersectionality between sex and gender and other social determinants of health that shapes biases and disparities in living kidney donation. There is a need for future qualitative studies to better understand the perspectives, experiences, barriers, and facilitators of living donation across different settings. We did not generate quantitative summary estimates across included studies, and a formal risk of bias assessment was not conducted, but these are not standard requirements of a scoping review.78 Furthermore, given the extent of the heterogeneity between studies, pooling the quantitative findings would not be feasible.
In conclusion, we have identified many reasons for the observed gender disparity in living kidney donation across both high- and low-resource settings. Our scoping review has highlighted the urgent need to engage with the relevant stakeholders, including potential donors, recipients, clinicians, and transplant coordinators, to better understand the potentially modifiable factors as well as other interactive factors that lie in the causal pathways to sex/gender disparity in living kidney donation. These may be features that are challenging to alter or adapt, such as socioeconomic position and health literacy, but knowledge of these critical elements will help the transplant community to guide research directions and priorities to close the gender inequity gap.
Supplementary Material
Footnotes
The authors declare no funding or conflicts of interest.
E.V. wrote the protocol, carried out all stages of review, and wrote the entire article. A.v.Z., S.K., and T.C. contributed to protocol methodology, revisions, and approved the final article. A.F. and M.W. contributed to protocol methodology and revisions and approved the final article. M.C. contributed to the first phase of title and abstract screening, revisions, and approved final article. G.W. contributed to protocol methodology, clinical content expertise, revisions, and approved the final article.
Supplemental digital content (SDC) is available for this article. Direct URL citations appear in the printed text, and links to the digital files are provided in the HTML text of this article on the journal’s Web site (www.transplantationdirect.com).
REFERENCES
- 1.Øien CM, Reisaeter AV, Leivestad T, et al. Gender imbalance among donors in living kidney transplantation: the Norwegian experience. Nephrol Dial Transplant. 2005;20:783–789. [DOI] [PubMed] [Google Scholar]
- 2.Kayler LK, Rasmussen CS, Dykstra DM, et al. Gender imbalance and outcomes in living donor renal transplantation in the United States. Am J Transplant. 2003;3:452–458. [DOI] [PubMed] [Google Scholar]
- 3.ANZDATA Registry. Australia and New Zealand Dialysis and Transplant Registry. Available at http:/www.anzdata.org.au. Accessed March 3, 2023.
- 4.Hart A, Lentine K, Smith J, et al. OPTN/SRTR 2019 annual data report: kidney. Am J Transplant. 2021;21:21–137. [DOI] [PubMed] [Google Scholar]
- 5.Canadian Institute for Health Information. Organ replacement in Canada: CORR annual statistics. Available at https://www.cihi.ca/en/organ-replacement-in-canada-corr-annual-statistics. Accessed April 06, 2023.
- 6.Kute VB, Chauhan S, Navadiya VV, et al. India: gender disparities in organ donation and transplantation. Transplantation. 2022;106:1293–1297. [DOI] [PubMed] [Google Scholar]
- 7.The Transplantation Society: Women in Transplantation. Gender disparity in transplant in Asia. Available at https://www.tts-wit.org/?id=27. Accessed February 12, 2022.
- 8.Kim Y, Ahmed E, Ascher N, et al. Meeting report: first state of the art meeting on gender disparity in kidney transplantation in the Asia-Pacific. Transplantation. 2021;105:1888–1891. [DOI] [PubMed] [Google Scholar]
- 9.Carrero JJ, Hecking M, Chesnaye NC, et al. Sex and gender disparities in the epidemiology and outcomes of chronic kidney disease. Nat Rev Nephrol. 2018;14:151–164. [DOI] [PubMed] [Google Scholar]
- 10.Bikbov B, Perico N, Remuzzi G; on behalf of the GBD Genitourinary Diseases Expert Group. Disparities in chronic kidney disease prevalence among males and females in 195 countries: analysis of the Global Burden of Disease 2016 Study. Nephron. 2018;139:313–318. [DOI] [PubMed] [Google Scholar]
- 11.Piccoli GB, Alrukhaimi M, Liu Z-H, et al. What we do and do not know about women and kidney diseases; questions unanswered and answers unquestioned: reflection on world kidney day and international woman’s day. BMC Nephrol. 2018;19:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jindal RM, Ryan JJ, Sajjad I, et al. Kidney transplantation and gender disparity. Review. Am J Nephrol. 2005;25:474–483. [DOI] [PubMed] [Google Scholar]
- 13.Bromberger B, Spragan D, Hashmi S, et al. Pregnancy-induced sensitization promotes sex disparity in living donor kidney transplantation. J Am Soc Nephrol. 2017;28:3025–3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gill J, Joffres Y, Rose C, et al. The change in living kidney donation in women and men in the United States (2005-2015): a population-based analysis. J Am Soc Nephrol. 2018;29:1301–1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rota-Musoll L, Brigidi S, Molina-Robles E, et al. An intersectional gender analysis in kidney transplantation: women who donate a kidney. BMC Nephrol. 2021;22:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Han M, Wong G, Kute VB, et al. ; Steering Committee Members of ASTREG-WIT-KT. Gender disparity in Asian-Pacific countries: an analysis of the ASTREG-WIT-KT registry. Transplantation. 2023;107:1–5. [DOI] [PubMed] [Google Scholar]
- 17.Ghods AJ, Nasrollahzadeh D. Gender disparity in a live donor renal transplantation program: assessing from cultural perspectives. Transplant Proc. 2003;35:2559–2560. [DOI] [PubMed] [Google Scholar]
- 18.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Int Med. 2018;169:467–473. [DOI] [PubMed] [Google Scholar]
- 19.Aromataris E, Munn Z. JBI manual for evidence synthesis. Joanna Briggs Institute. Available at https://synthesismanual.jbi.global. Accessed February 20, 2022.
- 20.American Psychological Association. Gender. Available at https://apastyle.apa.org/style-grammar-guidelines/bias-free-language/gender. Accessed October 26, 2022.
- 21.Covidence. Covidence software website. Available at https://www.covidence.org/. Accessed March 11, 2022.
- 22.Achille M, Soos J, Fortin MC, et al. Differences in psychosocial profiles between men and women living kidney donors. Clin Transplant. 2007;21:314–320. [DOI] [PubMed] [Google Scholar]
- 23.Adekoya AO, Desalu OO, Onakoya JA, et al. Willingness of Nigerians to donate a kidney. Niger. 2012;22:282–287. [PubMed] [Google Scholar]
- 24.Almeida N, Almeida A. Community attitudes toward kidney donation in india. Transplant Proc. 2013;45:1307–1309. [DOI] [PubMed] [Google Scholar]
- 25.Bailey PK, Tomson CRV, MacNeill S, et al. A multicenter cohort study of potential living kidney donors provides predictors of living kidney donation and non-donation. Kidney Int. 2017;92:1249–1260. [DOI] [PubMed] [Google Scholar]
- 26.Bloembergen WE, Port FK, Mauger EA, et al. Gender discrepancies in living related renal transplant donors and recipients. J Am Soc Nephrol. 1996;7:1139–1144. [DOI] [PubMed] [Google Scholar]
- 27.Decker O, Winter M, Brahler E, et al. Between commodification and altruism: gender imbalance and attitudes towards organ donation. A representative survey of the German community. J Gend Stud. 2008;17:251–255. [Google Scholar]
- 28.Feizi M, Moeindarbari T. Donor willingness to accept selling a kidney for transplantation: evidence from Iran. J Urol. 2019;201:235–236. [DOI] [PubMed] [Google Scholar]
- 29.Ge F, Kaczmarczyk G, Biller-Andorno N. Attitudes toward live and postmortem kidney donation: a survey of Chinese medical students. Exp Clin Transplant. 2014;12:506–509. [PubMed] [Google Scholar]
- 30.Gibney EM, Doshi MD, Hartmann EL, et al. Health insurance status of US living kidney donors. Clin J Am Soc Nephrol. 2010;5:912–916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Güden E, Çetinkaya F, Naçar M. Attitudes and behaviors regarding organ donation: a study on officials of religion in Turkey. J Relig Health. 2013;52:439–449. [DOI] [PubMed] [Google Scholar]
- 32.Inthorn J, Wohlke S, Schmidt F, et al. Impact of gender and professional education on attitudes towards financial incentives for organ donation: results of a survey among 755 students of medicine and economics in Germany. BMC Med Ethics. 2014;15:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kayler LK, Meier-Kriesche HU, Punch JD, et al. Gender imbalance in living donor renal transplantation. Transplantation. 2002;73:248–252. [DOI] [PubMed] [Google Scholar]
- 34.Kayler LK, Armenti VT, Dafoe DC, et al. Patterns of volunteerism, testing, and exclusion among potential living kidney donors. Health Care Women Int. 2005;26:285–294. [DOI] [PubMed] [Google Scholar]
- 35.Khajehdehi P. Living non-related versus related renal transplantation-its relationship to the social status, age and gender of recipients and donors. Nephrol Dial Transplant. 1999;14:2621–2624. [DOI] [PubMed] [Google Scholar]
- 36.Kurnikowski A, Krenn S, Lewandowski MJ, et al. Country-specific sex disparities in living kidney donation. Nephrol Dial Transplant. 2022;37:595–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Loiselle MM, Gulin S, Rose T, et al. The relationship between marijuana use and psychosocial variables in living kidney donor candidates. Clin Transplant. 2021;35:e14248. [DOI] [PubMed] [Google Scholar]
- 38.Malakoutian T, Hakemi MS, Nassiri AA, et al. Socioeconomic status of Iranian living unrelated kidney donors: a multicenter study. Transplant Proc. 2007;39:824–825. [DOI] [PubMed] [Google Scholar]
- 39.Martinez-Alarcon L, Ramis G, Gomez-Laguna J, et al. Attitude toward living kidney donation: differences between students from two Spanish universities. Transplant Proc. 2015;47:10–12. [DOI] [PubMed] [Google Scholar]
- 40.Milaniak I, Ruzyczka EW, Przybylowski P. Factors influencing decision making about living donation among medical students. Transplant Proc. 2020;52:1994–2000. [DOI] [PubMed] [Google Scholar]
- 41.Mithra P, Ravindra P, Unnikrishnan B, et al. Perceptions and attitudes towards organ donation among people seeking healthcare in tertiary care centers of coastal South India. Indian J Palliat Care. 2013;19:83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Naqvi SAA, Mazhar F, Ahmed R, et al. Limitation in selection of donors in a living-related renal transplant programme. Transplant Proc. 1998;30:2286–2288. [DOI] [PubMed] [Google Scholar]
- 43.Reeves-Daniel A, Adams PL, Daniel K, et al. Impact of race and gender on live kidney donation. Clin Transplant. 2009;23:39–46. [DOI] [PubMed] [Google Scholar]
- 44.Rios A, Martinez-Alarcon L, Ramirez P, et al. Irish residents in southeastern Spain: in search of favorable groups to encourage living kidney donation in Spain. Transplant Proc. 2007;39:2068–2071. [DOI] [PubMed] [Google Scholar]
- 45.Rios A, Febrero B, Lopez-Navas A, et al. Evaluation of attitude toward living organ donation among adolescents in Southeast Spain. Transplant Proc. 2012;44:1489–1492. [DOI] [PubMed] [Google Scholar]
- 46.Rios A, Lopez-Navas AI, Sanchez A, et al. Multivariate analysis of factors that influence the attitude of the Ecuadorian population resident in Spain toward living-related kidney donation. Transplant Proc. 2018;50:366–369. [DOI] [PubMed] [Google Scholar]
- 47.Rodrigue JR, Widows MR, Guenther R, et al. The expectancies of living kidney donors: do they differ as a function of relational status and gender? Nephrol Dial Transplant. 2006;21:1682–1688. [DOI] [PubMed] [Google Scholar]
- 48.Sanner MA. Giving and taking - to whom and from whom? People’s attitudes toward transplantation of organs and tissue from different sources. Clin Transplant. 1998;12:530–537. [PubMed] [Google Scholar]
- 49.Stothers L, Gourlay WA, Liu L. Attitudes and predictive factors for live kidney donation: a comparison of live kidney donors versus nondonors. Kidney Int. 2005;67:1105–1111. [DOI] [PubMed] [Google Scholar]
- 50.Taheri S, Alavian SM, Einollahi B, et al. Gender bias in Iranian living kidney transplantation program: a national report. Clin Transplant. 2010;24:528–534. [DOI] [PubMed] [Google Scholar]
- 51.Tarabeih M, Bokek-Cohen Y. The gendered body work of Muslim Arab mothers who donate a kidney to their children. J Pediatr Nurs. 2021;60:e68–e73. [DOI] [PubMed] [Google Scholar]
- 52.Terrell F, Mosley KL, Terrell AS, et al. The relationship between motivation to volunteer, gender, cultural mistrust, and willingness to donate organs among Blacks. J Natl Med Assoc. 2004;96:53–60. [PMC free article] [PubMed] [Google Scholar]
- 53.Thiel GT, Nolte C, Tsinalis D. Gender imbalance in living kidney donation in Switzerland. Transplant Proc. 2005;37:592–594. [DOI] [PubMed] [Google Scholar]
- 54.Thiessen C, Gannon J, Li S, et al. Quantifying risk tolerance among potential living kidney donors with the Donor-Specific Risk Questionnaire. Am J Kidney Dis. 2021;78:246–258. [DOI] [PubMed] [Google Scholar]
- 55.Thompson TL, Robinson JD, Kenny R. Gender differences in family communication about organ donation. Sex Roles. 2003;49:587–596. [Google Scholar]
- 56.Tuohy KA, Johnson S, Khwaja K, et al. Gender disparities in the live kidney donor evaluation process. Transplantation. 2006;82:1402–1407. [DOI] [PubMed] [Google Scholar]
- 57.Villafuerte-Ledesma HM, De Sousa-Amorim E, Peri L, et al. Impact of discards for living donor kidney transplantation in a transplant program. Transplant Proc. 2019;51:3222–3226. [DOI] [PubMed] [Google Scholar]
- 58.von Zur-Muhlen B, Yamamoto S, Wadstrom J. Few gender differences in attitudes and experiences after live kidney donation, with minor changes over time. Ann Transplant. 2017;22:773–779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang H, Wang Z, Li H, et al. Factors influencing attitudes of relatives of renal failure patients toward living kidney donation: central China. Transplant Proc. 2012;44:2921–2924. [DOI] [PubMed] [Google Scholar]
- 60.Yee E, Hosseini SM, Duarte B, et al. Sex disparities in organ donation: finding an equitable donor pool. J Am Heart Assoc. 2021;10:e020820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Zimmerman D, Donnelly S, Miller J, et al. Gender disparity in living renal transplant donation. Am J Kidney Dis. 2000;36:534–540. [DOI] [PubMed] [Google Scholar]
- 62.Tarabeih M, Bokek-Cohen Y. The double gender bias in parental kidney donation among Muslim Arab patients. Nurs Inq. 2021;28:1–10. [DOI] [PubMed] [Google Scholar]
- 63.Klarenbach S, Gill J, Knoll G, et al. Economic consequences incurred by living kidney donors: a Canadian multi-center prospective study. Am J Transplant. 2014;14:916–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Tushla L, Rudow DL, Milton J, et al. ; American Society of Transplantation. Living-donor kidney transplantation: reducing financial barriers to live kidney donation—recommendations from a consensus conference. Clin J Am Soc Nephrol. 2015;10:1696–1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Rodrigue JR, Kazley AS, Mandelbrot DA, et al. ; American Society of Transplantation. Living donor kidney transplantation: overcoming disparities in live kidney donation in the US-recommendations from a consensus conference. Clin J Am Soc Nephrol. 2015;10:1687–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cohen AJ, Williams DS, Bohorquez H, et al. Robotic-assisted laparoscopic donor nephrectomy: decreasing length of stay. Ochsner J. 2015;15:19–24. [PMC free article] [PubMed] [Google Scholar]
- 67.Schweitzer EJ, Wilson J, Jacobs S, et al. Increased rates of donation with laparoscopic donor nephrectomy. Ann Surg. 2000;232:392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Kute VB, Vanikar AV, Shah PR, et al. Increasing access to kidney transplantation in countries with limited resources: the Indian experience with kidney paired donation. Nephrology. 2014;19:599–604. [DOI] [PubMed] [Google Scholar]
- 69.Ferrari P, Hughes PD, Cohney SJ, et al. ABO-incompatible matching significantly enhances transplant rates in kidney paired donation. Transplantation. 2013;96:821–826. [DOI] [PubMed] [Google Scholar]
- 70.Heidt S, Claas FH. Transplantation in highly sensitized patients: challenges and recommendations. Expert Rev Clin Immunol. 2018;14:673–679. [DOI] [PubMed] [Google Scholar]
- 71.Heidt S, Haasnoot GW, van der Linden-van Oevelen MJH, et al. Highly sensitized patients are well served by receiving a compatible organ offer based on acceptable mismatches. Front Immunol. 2021;12:687254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lim WH, Wong G, Heidt S, et al. Novel aspects of epitope matching and practical application in kidney transplantation. Kidney Int. 2018;93:314–324. [DOI] [PubMed] [Google Scholar]
- 73.Waterman AD, Morgievich M, Cohen DJ, et al. ; American Society of Transplantation. Living donor kidney transplantation: improving education outside of transplant centers about live donor transplantation—recommendations from a consensus conference. Clin J Am Soc Nephrol. 2015;10:1659–1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ismail S, Luchtenburg A, Timman R, et al. Home-based family intervention increases knowledge, communication and living donation rates: a randomized controlled trial. Am J Transplant. 2014;14:1862–1869. [DOI] [PubMed] [Google Scholar]
- 75.Rodrigue J, Cornell D, Lin J, et al. Increasing live donor kidney transplantation: a randomized controlled trial of a home-based educational intervention. Am J Transplant. 2007;7:394–401. [DOI] [PubMed] [Google Scholar]
- 76.Garonzik-Wang JM, Berger JC, Ros RL, et al. Live donor champion: finding live kidney donors by separating the advocate from the patient. Transplantation. 2012;93:1147–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bailey PK, Caskey FJ, MacNeill S, et al. Investigating strategies to improve AccesS to Kidney transplantation (the ASK trial): a protocol for a feasibility randomised controlled trial with parallel process evaluation. Pilot Feasibility Stud. 2023;9:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Munn Z, Peters MD, Stern C, et al. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143. [DOI] [PMC free article] [PubMed] [Google Scholar]