Abstract
Objective:
To examine possible associations in inpatient healthcare expenditure and guideline changes in the surgical management of diverticulitis, in terms of both cost per discharge and total aggregate costs of care.
Background:
Medical costs throughout the healthcare system continue to rise due to increased prices for services, increased quantities of high-priced technologies, and an increase in the amount of overall services.
Methods:
We used a retrospective case-control design using the Healthcare Cost and Utilization Project National Inpatient Sample to evaluate cost per discharge and total aggregate costs of diverticulitis management between 2004 and 2015. The year 2010 was selected as the transition between the pre and postguideline implementation period.
Results:
The sample consisted of 450,122 unweighted (2,227,765 weighted) inpatient discharges for diverticulitis. Before the implementation period, inpatient costs per discharge increased 1.13% in 2015 dollars (95% confidence intervals [CI] 0.76% to 1.49%) per quarter. In the postimplementation period, the costs per discharge decreased 0.27% (95% CI –0.39% to –0.15%) per quarter. In aggregate, costs of care for diverticulitis increased 0.61% (95% CI 0.28% to 0.95%) per quarter prior to the guideline change, and decreased 0.52% (95% CI –0.87% to –0.17) following the guideline change.
Conclusions:
This is the first study to investigate any associations between evidence-based guidelines meant to decrease surgical utilization and inpatient healthcare costs. Decreased inpatient costs of diverticulitis management may be associated with guideline changes to reduce surgical intervention for diverticulitis, both in regards to cost per discharge and aggregate costs of care.
Keywords: diverticulitis, healthcare costs, healthcare utilization
Mini-abstract: We performed a retrospective case-control design using the Healthcare Cost and Utilization Project National Inpatient Sample to evaluate costs of diverticulitis management. Decreased inpatient costs of diverticulitis management may be associated with guideline changes to reduce surgical intervention for diverticulitis, both in regards to cost per discharge and aggregate costs of care.
Supplemental Digital Content is available in the text.
INTRODUCTION
Current healthcare spending in the United States averaged $3.6 trillion dollars in 2018, and currently approaches 19% of GDP.1 Rising healthcare expenditure can be categorized via two mechanisms: increased costs in unit per service and increased aggregate costs of care. Provider salaries, prices, and expensive technologies affect cost per unit of service, while the quantity of overall services is the main component of aggregate costs.2 Cutler and McClellan followed by Skinner et al showed demonstrated how new, more expensive medical technology in the treatment of myocardial infarction increased per-patient medical costs, 3,4 while Legoretta et al showed that despite a 25% decrease in the operative cost for laparoscopic cholecystectomy, a corresponding 60% increase in total surgical utilization increased aggregate costs by 11.4%.5 This increase in aggregate costs of care has also been shown in other areas of medicine, including in magnetic resonance imaging utilization, neonatology, cancer care, and ICU care.6
Diverticulitis is the most common gastrointestinal diagnosis requiring inpatient admission in US hospitals, with an increasing incidence in the population since 2000.7 Once thought to be a progressive disease following the first diverticulitis episode, early surgical intervention was favored.8 In 2006, however, the American Society of Colon and Rectal Surgeons (ASCRS) published its first set of standard guidelines regarding elective colectomy following an episode of diverticulitis and recommended an individualized decision making process for elective sigmoid colectomy rather than colectomy only based on number of attacks or patient factors such as age.9 These guidelines were based on long-term outcomes in diverticulitis management which questioned the validity of diverticulitis as a progressive disease and found treatment with immediate surgical colectomy unnecessary.10–13
Despite these recommendations, published literature demonstrated that the rate of elective colectomy for diverticulitis continued to increase even following the guideline change. This was, however, coupled with a significant decrease in the rate of emergent colectomies which ultimately led to an overall decrease in colectomies during the study period.14 No studies to date have examined associations of the 2006 surgical guideline changes on inpatient costs of care for diverticulitis. We sought to investigate if the change in surgical guidelines for diverticulitis management was associated with a decrease in either total aggregate cost or cost per discharge for diverticulitis.
METHODS
Study Design
We used a retrospective, case-control design using the Healthcare Cost and Utilization Project (HCUP) National Inpatient Sample (NIS) to evaluate cost per discharge and total aggregate costs of diverticulitis management before and following guideline implementation. To account for both lagged effects following the 2006 guideline change and additional publications verifying the initial results of the risks of recurrence of diverticulitis using data through 2009, we conservatively defined the pre-implementation period to years before 2010, and the post implementation period from 2010 and onwards. Table 1 highlights publications related to changes in surgical management for diverticulitis.
TABLE 1.
Changes in Surgical Management for Diverticulitis
| Year | Reference | Recomendations |
|---|---|---|
| 2005 | Chapman and Wolff13 | Prophylactic colectomy for reducing mortality and morbidity from complicated diverticulitis may be outmoded and needs to be reevaluated. Our study reveals that the majority of patients with complicated diverticulitis had no history of diverticulitis. Perforated diverticulitis, which carries the highest risk of mortality and morbidity, most commonly was the first manifestation of complicated diverticular disease. |
| 2005 | Broderick-Villa et al10 | Very few patients with acute diverticulitis treated nonoperatively have recurrence. The low recurrence rate argues against routine elective colectomy after successful nonoperative management of acute diverticulitis |
| 2006 | Chapman et al12 | In our current study, patients with fewer prior episodes of diverticulitis (1 or 2) presented more often with perforation compared with patients with >2 episodes of diverticulitis. Patients who had only 1 or 2 episodes of uncomplicated diverticulitis were at a higher risk for perforation than patients with >2 episodes. |
| 2006 | Rafferty et al 9 | The decision to recommend elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis. Most patients who present with complicated diverticulitis do so at the time of their first attack, therefore, a policy of elective colon resection after recovery from uncomplicated acute diverticulitis might not decrease the likelihood of later emergency surgery or overall mortality… the number of attacks of uncomplicated diverticulitis is not necessarily an overriding factor in defining the appropriateness of surgery. There is no clear consensus regarding whether younger patients (younger than aged 50 yrs) treated for diverticulitis are at increased risk of complications or recurrent attacks |
| 2008 | Comparato and Di Mario15 | Many authors have shown that patients treated nonoperatively have a low risk of recurrent disease and would be expected to do well without elective colectomy. Routine elective colectomy is rarely necessary in patients hospitalized with a first episode of uncomplicated acute diverticulitis, with or without an abscess, who are successfully treated nonoperatively. The recurrence rate in patients treated nonoperatively is low and therefore does not mandate elective colectomy. |
| 2010 | Eglinton et al16 | After an initial attack of uncomplicated diverticulitis, only 5.0% developed complicated diseaseSubsequent elective surgery to prevent recurrence and the development of complications should be used sparingly. |
| 2011 | Hall et al17 | Although diverticulitis recurrence is common following an initial attack that has been managed medically, complicated recurrence is uncommon. Patients who present with a family history of diverticulitis, long segment of involved colon, and/or retroperitoneal abscess are at higher risk for recurrent disease |
Bold indicates original guideline recommendations from the 2006 ASCRS Guidelines for new recommendations regarding elective sigmoid colectomy.
Data Source
The HCUP NIS is the largest, all-payer inpatient health care database in the United States. Before 2012, the NIS performed a stratified random sample of 20% of participating hospitals. In 2012, the NIS redesigned the sampling strategy to a stratified random sample of all discharge records, and updated sample weights were created for pre-2012 data to perform time trend analyses. There were substantial problems within the NIS following the transition between International Classification of Diseases, Ninth edition (ICD-9) to International Classification of Diseases, Tenth edition (ICD-10), thus we were forced to limit the analysis to only the ICD-9 time period from 2004 to the end of the third quarter of 2015.18 Discharge quarters were used as time periods as opposed to year, as 2015 contains only three discharge quarters. Our dataset contained four discharge quarters per year from 2004 to 2014 and three discharge quarters in 2015, for a total of 47 distinct quarters.
Patients 18 and older with an admission diagnosis of diverticulitis, based on ICD-9 diagnosis codes (562.11, 562.23) were included for analysis.19 Charge data for diverticulitis admissions were adjusted to 2015 dollars using the consumer price index20 and converted to costs using hospital-specific cost-to-charge ratios provided by HCUP.21 Due to the skewed distribution of costs and correlation of the error term, the variable was log-transformed, which improved the distribution.22
Clinical, patient, and hospital covariates were isolated for our multiple regression model. Clinical covariates included whether colectomy was performed during the admission, elective, length of stay, discharge disposition, and the number of procedures on the discharge record. Colectomy was identified using ICD-9 procedure codes (17.35, 17.36, 17.39, 45.75, 45.76, 45.79).19 “Elective” was a dummy variable identifying elective vs. urgent/emergent admissions. Patient covariates included age, race, insurance type, number of chronic diseases, the number of diagnoses on record, and median income quartile. Hospital covariates included region, bed size, teaching status, and the number of hospital discharges. Admissions that were missing variables for charges were deleted from the dataset, which decreased the total unweighted sample from 498,304 to 450,122 admissions (9.67%). Missing data were equally random pre and postimplementation period, and with our large sample size, we were comfortable using case-wise deletion.23
Statistical Analysis
Initial differences between groups were evaluated with t-tests, Wilcoxon tests, and chi-square tests, as appropriate. Due to the very large sample size of the cohorts, the statistical tests are likely overpowered, therefore, in addition to standard statistical tests, effect sizes were calculated and used as the primary interpretive statistic for meaningful differences.
To assess the change in the two different time periods, we implemented a segmented linear “hockey-stick” regression model using survey weighted data to measure the change in costs before and following the implementation time period, controlling for patient, clinical, and hospital factors. We then applied Duan’s retransformation method to convert from log back to original scale to determine change in dollars, controlling for independent variables. Comparisons of means on the transformed scale do not directly inform the comparison of means on the original scale, and back transformation of the results to the original scale is required due to the nature of the error term.24
To investigate aggregate costs of inpatient care, the retransformed values for costs per discharge in each discharge quarter over the study period were multiplied by the survey weighted total diverticulitis admissions in each discharge quarter to generate total aggregate costs per discharge quarter. These aggregate costs were log-transformed and a final segmented linear regression was performed. We repeated Duan’s retransformation to determine change in dollars in aggregate costs.
Sensitivity Analyses
We decided to perform two additional sensitivity analyses in order to further isolate the effects of surgical guidelines on both aggregate costs and cost per discharge. Our first analysis served as a negative control, using only medical admissions for diverticulitis to assess if medical, rather than surgical, factors contributed to the decrease in costs of diverticulitis. Our second sensitivity analysis used a washout period following the published guidelines in 2006 to allow for implementation. This was done to account for any potential bias regarding our choice of 2010 as the transition period. We compared changes in diverticulitis costs before 2006 and after 2011, the last publication year cited in the 2014 ASCRS Practice Parameter Guidelines for diverticulitis, the subsequent following set of guidelines after 2006.25 All data were analyzed using Stata software, version 15.1 (StataCorp). Statistical significance was assessed with two-sided tests using a threshold of P < 0.05.
RESULTS
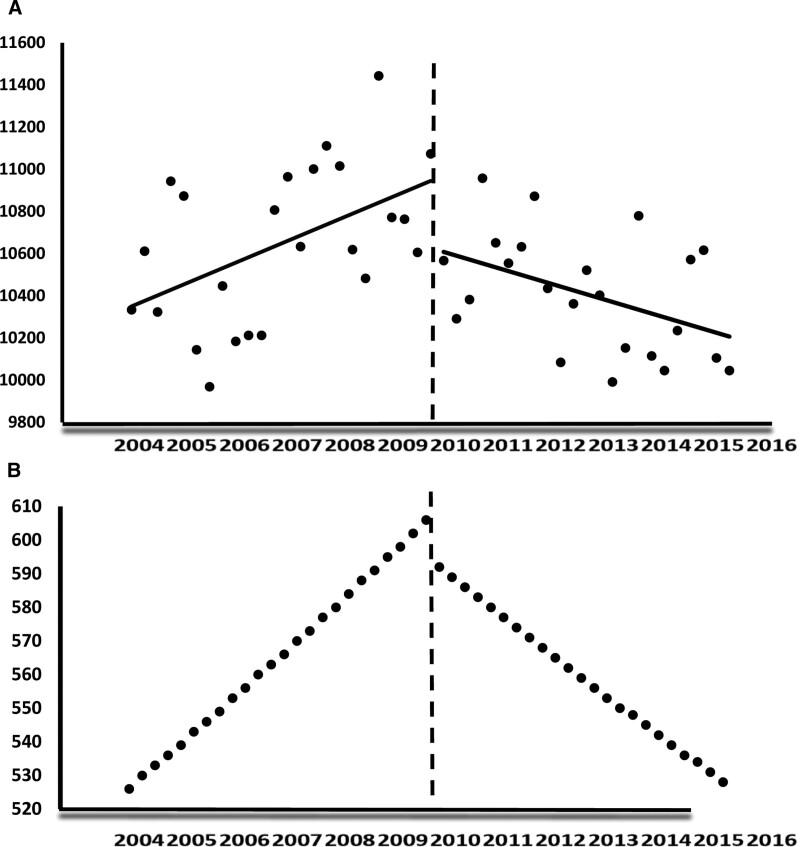
Survey-weighted, uncontrolled population trends of inpatient cost of diverticulitis, both in aggregate and cost per discharge are reported (Fig. 1). Both total cost per discharge and aggregate costs, by admission type (urgent surgical, elective surgical, and nonsurgical medical admissions), were also captured, and are available as Supplemental Appendix A, http://links.lww.com/AOSO/A50. The mean cost per discharge for elective colectomy admissions was $18,195 in 2015 dollars, while the mean cost per discharge for diverticulitis patients requiring emergent colectomy was $32,470 during the time period. The mean aggregate costs over the time period was $153 million for elective colectomy admissions and $213 million for emergent colectomy patients.
FIGURE 1.
Unadjusted, survey-weighted population level hospital costs, aggregate and costs per discharge.
Over the study period, there were 450,122 unweighted (2,227,765 weighted) observations of diverticulitis admissions. Unadjusted patient, clinical, and hospital characteristics in the sample are reported in Table 2. The proportion of colectomies per admission was 22.9% in the preimplementation period and 21.3% in the postmplementation period. The percentage of elective colectomies increased from 55.7% to 61.0% in the postimplementation period while the percentage of emergent colectomies decreased in the postimplementation period from 44% to 38.9%. All differences were statistically significant at P < 0.001, but all effect sizes were trivial/small. These results suggest that differences between groups, although statistically significant, may not be practically or clinically meaningful.
TABLE 2.
Patient, Hospital, Clinical Demographics, Pre and Postimplementation Period
| Preimplementation Period | Postimplementation Period | |
|---|---|---|
| Discharges (n) | 216,211 | 233,911 |
| Patient characteristics | ||
| Age (mean) | 59.81 | 59.72 |
| Sex (n, %) | ||
| Male | 91,829 (42.47) | 98,451 (42.09) |
| Female | 124,382 (57.53) | 135,460 (57.91) |
| Race (n, %) | ||
| White | 134,329 (62.13) | 168,533 (72.05) |
| Black | 11,313 (5.23) | 18,184 (7.77) |
| Hispanic | 15,421 (7.13) | 23,704 (10.13) |
| Asian | 1,463 (0.68) | 1,949 (0.83) |
| Native American | 684 (0.32) | 936 (0.40) |
| Other | 3,865 (1.79) | 5,109 (2.18) |
| Not reported/missing | 49,136 (22.73) | 15,496 (6.62) |
| Insurance status (n, %) | ||
| Private | 102,150 (47.25) | 101,480 (43.38) |
| Medicare | 85,417 (39.5) | 92,551 (39.57) |
| Medicaid | 10,634 (4.92) | 17,484 (7.47) |
| Self-pay | 10,739 (4.97) | 14,176 (6.06) |
| No charge | 1,422 (0.66) | 1,725 (0.74) |
| Other | 5,535 (2.56) | 6,297 (2.69) |
| Not reported/missing | 314 (0.15) | 198 (0.08) |
| Income quartile (n, %) | ||
| First | 48,103 (22.25) | 56,925 (24.34) |
| Second | 53,953 (24.95) | 58,097 (24.84) |
| Third | 53,827 (24.9) | 58,704 (25.10) |
| Fourth | 56,244 (26.01) | 56,276 (24.06) |
| Not reported/missing | 4,084 (1.89) | 3,909 (1.67) |
| Number of chronic diagnoses (mean) | 4.13 | 4.55 |
| Number of total diagnoses (mean) | 6.47 | 8.12 |
| Clinical characteristics | ||
| Colectomy (n, %) | 49,460 (22.88) | 49,749 (21.27) |
| Elective colectomies (n, %) | 27,548 (55.7) | 30,337 (60.98) |
| Urgent colectomies (n, %) | 21,763 (44) | 19,325 (38.85) |
| Not reported/missing | 149 (0.3) | 87 (0.17) |
| No. of procedures per admission (mean) | 1.17 | 1.11 |
| Length of stay (mean) | 5.20 | 4.76 |
| Disposition (n, %) | ||
| Normal discharge | 179,403 (82.98) | 194,377 (83.10) |
| Transfer to short-term care | 1,682 (0.78) | 1908 (0.82) |
| Skilled nursing facility | 13,153 (6.08) | 13452 (5.75) |
| Home health | 19,118 (8.84) | 21,473 (9.18) |
| Died | 1,545 (0.71) | 1,068 (0.46) |
| Left against medical advice | 1,239 (0.57) | 1,482 (0.63) |
| Unknown | 25 (0.01) | 16 (0.01) |
| Not reported/ missing | 46 (0.02) | 135 (0.06) |
| Hospital characteristics | ||
| Region (n, %) | ||
| Northeast | 38,311 (17.72) | 47,985 (20.51) |
| Midwest | 44,699 (20.67) | 56,563 (24.18) |
| South | 66,734 (30.87) | 93,167 (39.83) |
| West | 26, 921 (12.45) | 36,196 (15.47) |
| Not reported/ missing | 39,546 (18.29) | 0 (0) |
| Hospital size (n, %) | ||
| Small | 30,919 (14.30) | 41,135 (17.59) |
| Medium | 55,985 (25.89) | 67,084 (28.68) |
| Large | 128,612 (59.48) | 124,902 (53.40) |
| Not reported/missing | 695 (0.32) | 790 (0.34) |
| Teaching status (n, %) | ||
| Rural | 33,675 (15.58) | 32,131 (13.74) |
| Urban nonteaching | 107,286 (49.62) | 98,969 (42.31) |
| Urban teaching | 74,555 (34.48) | 102,021 (43.62) |
| Not reported/missing | 695 (0.32) | 790 (0.34) |
| Total discharges per hospital (mean) | 19,183 | 8809 |
Preimplementation period: 2004–009, Postimplementation period: 2010–2015.
Data obtained from the NIS. These data are provided by the AHRQ.
All differences were statistically significant at P < 0.001, all effect sizes were calculated as “small.”
AHRQ indicates Agency for Healthcare Research and Quality; NIS, National Inpatient Service.
The preimplementation period was associated with a +1.13% increase in cost per discharge, per quarter, when controlling for patient, clinical, and hospital factors (95% confidence intervals [CI] 0.76% to 1.49%, P < 0.001). The postimplementation period was associated with a –0.27% decrease in cost per discharge, per quarter (95% CI –0.39% to –0.15%, P < 0.001). When controlling for patient, clinical, and hospital factors, the change from the pre to postimplementation period was associated with a total 1.40 percentage point decrease in inpatient cost per discharge, per quarter (Table 3). When transformed, this equated to a +$196 increase in cost per discharge, per quarter in the preimplementation period and a –$86 decrease in cost per discharge in the postimplementation period.
TABLE 3.
OLS Estimates of the Effects of Guideline Changes on Inpatient Diverticulitis Costs, Quarterly
| Costs per Discharge, % Change | 95% Confidence Interval | Aggregate Costs, % Change | 95% Confidence Interval | |
|---|---|---|---|---|
| Preimplementation period | +1.13% | 0.76% to 1.49% | +0.61% | 0.28% to 0.94% |
| Postimplementation period | –0.27% | –0.39% to –0.15% | –0.52% | –0.87% to –0.17% |
| Total change from pre to postimplementation period | –1.40 | – | –1.13 | – |
| Change in Cost Per Discharge ($) | 95% Confidence Interval | Change in Aggregate Costs ($) | 95% Confidence Interval (Millions of Dollars) | |
| Preimplementation period* | +$196 | $50 to $342 | +$3.45 million | $3.43 to $3.48 |
| Postimplementation period† | –$86 | –$111 to –$61 | –$2.91 million | –$2.94 to –$2.89 |
| Total savings from pre to postimplementation period | –$282 | – | –$6.36 million | – |
All regressions use robust standard error; standard errors in parenthesis; cost per discharge contains patient, clinical, and hospital variables; aggregate costs generated from a segmented linear regression at the aggregate cost level per discharge quarter from 2004 to 2015. Dollar amounts in 2015 dollars. Unadjusted survey weighted estimates from the NIS; Y left axis is total aggregate costs (in millions of dollars); Y right axis is cost per discharge. All adjusted to 2015 dollars.
*Significant at the 0.05 level.
†Significant at the <0.01 level.
NIS indicates National Inpatient Sample.
The preimplementation period was associated with a +0.61% increase in aggregate costs (95% CI 0.28% to 0.94%). In the postimplementation period, aggregate costs decreased –0.52% per quarter (95% CI –0.87% to –0.17%). The aggregate cost increase per quarter in the preimplementation period was $3.45 million (95% CI $3.43 to $3.48), while the postimplementation period was associated with a decrease of $2.91 million (95% CI –$2.94 to –$2.89). At the aggregate level, the total savings associated with the postguideline implementation period was $6.36 million, per quarter, in 2015 dollars. Linear representation of costs per discharge and aggregate costs are shown in Figure 2A,B.
FIGURE 2.
A, Cost per discharge, adjusted; B, aggregate costs, adjusted (in millions).
Supplemental Appendix C, http://links.lww.com/AOSO/A52, reports coefficients for our cost per discharge model. Only the pre and postimplementation variables demonstrate the change in costs between pre and postimplementation period. The other independent variables are used as covariates in the model for costs per discharge. Colectomy had the greatest effect on average discharge cost, with colectomy increasing mean inpatient costs per discharge by 49.4% (95% CI 47.7% to 51.1%; P < 0.001). Medicaid and uninsured status (self-pay or no charge patients) as well as worsening income quartile was associated with increasing inpatient costs as compared to private insurance and the highest income quartile. Black, Hispanic, and Asian ethnicity was associated with higher costs as compared to white patients (P < 0.001).
Sensitivity Analyses
When evaluating costs of care for medical admissions, when controlling for patient, clinical and hospital factors, hospital costs increased 1.22% in the preimplementation time period (95% CI 0.83% to 1.60%, P < 0.001) and decreased –0.21% in the postimplementation period (95% CI –0.33% to –0.09%, P = 0.001). For aggregate costs, however, costs increased 1.17% (95% CI 0.74% to 1.60%) in the preimplementation period, but also increased 0.26% (95% CI –0.19% to 0.71%) through the postimplementation period, although this change was not statistically significant.
We did not see significant changes to the direction or statistical significance of the pre and postcoefficients when a washout period was used (comparing changes in costs from 2004 to 2006 to those from 2011 to 2015). Results of our sensitivity analysis are presented in Supplemental Appendix B, http://links.lww.com/AOSO/A51.
DISCUSSION
This is the first study demonstrating an association between surgical guideline changes recommending a decrease in surgical utilization and a decrease in both inpatient cost per discharge and aggregate costs of care. This work serves as a unique case study, as healthcare costs for most disease processes are increasing through one or both of these mechanisms.
Four main components of the 2006 published guidelines gave new recommendations meant to decrease elective sigmoid colectomy: (1) Elective sigmoid colectomy after recovery from acute diverticulitis should be made on a case-by-case basis, (2) most patients who present with complicated diverticulitis do so at the time of their first attack, therefore elective colon resection after recovery from uncomplicated acute diverticulitis might not decrease the likelihood of later emergency surgery or mortality, (3) the number of attacks of uncomplicated diverticulitis is not an overriding factor in defining the appropriateness of surgery, and (4) there is no clear consensus whether younger patients (younger than aged 50 years) treated for diverticulitis are at increased risk of complications or recurrent attacks.9
Despite wide acceptance of these guidelines among colorectal and general surgeons no published literature to date has demonstrated decreases in the rate of colectomy following guideline publication. Specifically, work by Strassle et al, which used the NIS database, showed that the rate of elective colectomies continued to increase while the rate of emergent surgical colectomies decreased following guideline publication. 14 Although the rate of elective colectomy for diverticulitis continued to increase following surgical guideline changes, it did not continue at the same slope. It is important to note that the magnitude of the slope decreased from 0.13/100,000 adults per year before the guideline change to 0.06/100,000 adults per year following the guideline change, a greater than 50% decrease in magnitude. This, coupled with a decrease in urgent/emergent colectomies, may serve as a potential important explanation for the results in our study. Because colectomy contributed to such a large proportion of discharge cost, these two factors could explain the decrease in cost in our study, despite the overall increasing rate of elective colectomies per year following implementation of surgical guidelines.
An important component of elective colectomy admissions is the increased use of minimal invasive surgical technologies, which has decreased the overall morbidity of surgical colectomy. This may lead to more patients willing to proceed with surgical resection and may explain the rise in elective colectomy for diverticulitis despite the recommended guideline changes. One study reported an average surgical cost of $10,589 vs $8,207 for laparoscopic surgery compared with the open approach. However, laparoscopic surgery resulted in a shorter hospital stay on average, and average total inpatient costs per discharge were decreased in laparoscopic patients ($11,528 for the laparoscopic approach vs $13,426 for the open approach).26 Unfortunately, our dataset did not code laparoscopic procedures before 2008. Although these procedures were able to be included for overall analysis, we were unable to control for laparoscopic or robotic procedures in our model.
Recent additional literature has investigated the prevalence of complicated diverticulitis in elective colon resections, which result in increased complexity of operation, longer operating times, and possibly can have an effect on costs of care. One recent study by Altinel et al reviewed complex diverticulitis patients between 2010 and 2016 undergoing elective colectomy. The authors showed surgical time was longer in complex diverticulitis patients (160 vs 181 minutes), and the patients were more likely to require diverting stomas and additional resections.27 Our study complements these findings, for despite potential increases in the number of total and more complicated elective procedures, inpatient costs overall did not increase during the time period.
Cost effects of guideline changes have been reported in the medical literature. An analysis regarding cost effects of guideline adherence in the use of hypertensive medications demonstrated that deviation from evidence-based guidelines for classes of antihypertensive medications resulted in both over prescription and over-utilization of more expensive and less effective medications. The authors presented an overall savings of $2.1 billion in 2001 dollars if appropriate guidelines were followed.28 Other cost-saving strategies for diverticulitis care have also been explored. Studies show that practitioners themselves can have important effects on hospital costs. Care by an integrated, multidisciplinary, digestive health service, or gastroenterologist-led inpatient service significantly reduced overall costs in patients admitted for diverticulitis as compared to nonintegrated or hospitalist inpatient services.29, 30
Limitations
Our study is retrospective using the NIS. Methodological concerns have been published concerning the NIS, with Khera et al demonstrating that out of 120 studies using NIS data, 85% had at least one methodological concern NIS.31 The authors highlight seven total research practices recommended by the AHRQ, and those specific to our work include as follows: regarding observations as discharge events rather than individual patients, avoiding using secondary diagnosis codes to infer in-hospital events, using survey-specific analysis that account for appropriate weighting, and accounting for changes in survey design beginning in 2012. We attempted to follow all of these documented practices, as our study uses appropriately survey weighted analyses on the individual discharge level, and accounts for the design in 2012 using weights provided by HCUP.
As acknowledged previously, we were unable to control for laparoscopic and robotic surgical procedures. Although these procedure codes were included in the cost variable, the ability to control for minimally invasive procedures would have strengthened our model and may have led to different coefficients in regards to the pre and postimplementation periods. Second, our study may not have captured outside factors that could have an effect on patient, clinical, and hospital covariates. For example, the NIS does not track patients over time in our dataset. If patients with more advanced disease were readmitted, this could have an effect on costs of care outside of our patient control variables. In addition, although we did adjust for inflation in our model, pricing changes and reimbursement rates of surgical and medical care may have had an effect on our results.
CONCLUSIONS
We present evidence that decreases in inpatient costs may have been associated with changes in surgical management guidelines for diverticular disease, both at the cost per discharge and aggregate level. This is unusual as healthcare expenditures in the care of most medical conditions are either increasing in regards to cost per unit of service or in aggregate. Although our data does not claim a causal relationship between costs and changes in surgical guidelines, it may imply that clinicians assessing their own practice patterns and adopting guidelines in limiting interventions can potentially affect inpatient healthcare expenditures.
ACKNOWLEDGMENTS
The authors would like to acknowledge Dr. Jan Blustein and John Billings at the NYU School of Public Service, who originally served as advisors for this work. None of the authors in this article have any conflict of interests to disclose.
Supplementary Material
Footnotes
Disclosure: The authors declare that they have nothing to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Hartman M, Martin AB, Benson J, et al. ; National Health Expenditure Accounts Team. National health care spending in 2018: growth driven by accelerations in medicare and private insurance spending. Health Aff (Millwood). 2020;39:8–17. [DOI] [PubMed] [Google Scholar]
- 2.Bodenheimer T. High and rising health care costs. Part 3: the role of health care providers. Ann Intern Med. 2005;142(12 Pt 1):996–1002. [DOI] [PubMed] [Google Scholar]
- 3.Cutler DM. Declining disability among the elderly. Health Aff (Millwood). 2001;20:11–27. [DOI] [PubMed] [Google Scholar]
- 4.Skinner JS, Staiger DO, Fisher ES. Is technological change in medicine always worth it? The case of acute myocardial infarction. Health Aff (Millwood). 2006;25:w34–w47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bodenheimer T. High and rising health care costs. Part 2: technologic innovation. Ann Intern Med. 2005;142:932–937. [DOI] [PubMed] [Google Scholar]
- 6.Baker L. Managed care, medical technology, and the well-being of society. Top Magn Reson Imaging. 2002;13:107–113. [DOI] [PubMed] [Google Scholar]
- 7.Reddy VB, Longo WE. The burden of diverticular disease on patients and healthcare systems. Gastroenterol Hepatol (N Y). 2013;9:21–27. [PMC free article] [PubMed] [Google Scholar]
- 8.Strate LL, Morris AM. Epidemiology, pathophysiology, and treatment of diverticulitis. Gastroenterology. 2019;156:1282–1298. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rafferty J, Shellito P, Hyman NH, et al. ; Standards Committee of American Society of Colon and Rectal Surgeons. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939–944. [DOI] [PubMed] [Google Scholar]
- 10.Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576–581; discussion 581–XXX583. [DOI] [PubMed] [Google Scholar]
- 11.Chapman J, Davies M, Wolff B, et al. Complicated diverticulitis: is it time to rethink the rules? Ann Surg. 2005;242:576–581; discussion 581– XXX–583.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chapman JR, Dozois EJ, Wolff BG, et al. Diverticulitis: a progressive disease? Do multiple recurrences predict less favorable outcomes? Ann Surg. 2006;243:876–830; discussion 880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chapman JR, Wolff BG. The management of complicated diverticulitis. Adv Surg. 2006;40:285–297. [DOI] [PubMed] [Google Scholar]
- 14.Strassle PD, Kinlaw AC, Chaumont N, et al. Rates of elective colectomy for diverticulitis continued to increase after 2006 guideline change. Gastroenterology. 2019;157:1679–1681 e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Comparato G, Di Mario F; NDSG. Recurrent diverticulitis. J Clin Gastroenterol. 2008;42:1130–1134. [DOI] [PubMed] [Google Scholar]
- 16.Eglinton T, Nguyen T, Raniga S, et al. Patterns of recurrence in patients with acute diverticulitis. Br J Surg. 2010;97:952–957. [DOI] [PubMed] [Google Scholar]
- 17.Hall JF, Roberts PL, Ricciardi R, et al. Long-term follow-up after an initial episode of diverticulitis: what are the predictors of recurrence? Dis Colon Rectum. 2011;54:283–288. [DOI] [PubMed] [Google Scholar]
- 18.Using Multiple Years of HCUP Data Tutorial. Healthcare Cost and Utilization Project (HCUP). Cited June 6, 2020. Available at: https://www.hcup-us.ahrq.gov/tech_assist/trends/508/508course_2019.jsp#updates. Accessed June 10, 2020.
- 19.Centers For Medicare & Medicaid Services. ICD-9-CM Diagnosis and Procedure Codes: Abbreviated and Full Code Titles. 2020. Cited January 5, 2020. Available at: https://www.cms.gov/Medicare/Coding/ICD9ProviderDiagnosticCodes/codes. Accessed January 5, 2020.
- 20.U.S. Bureau of Labor Statistics. Consumer Price Index, Medical Care. Cited June 2, 2020. 2020. Available at: http://data.bls.gov/cgi-bin/surveymost?cu. Accessed June 2, 2020.
- 21.Cost-to-Charge Ratio Files. Healthcare Cost and Utilization Project (HCUP). Available at: https://www.hcup-us.ahrq.gov/db/state/costtocharge.jsp. Accessed June 10, 2020.
- 22.Keene ON. The log transformation is special. Stat Med. 1995;14:811–819. [DOI] [PubMed] [Google Scholar]
- 23.Dong Y, Peng CY. Principled missing data methods for researchers. Springerplus. 2013;2:222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Duan N. Smearing estimate: a nonparametric retransformation method. J Am Stat Assoc. 1983;78:605–610. [Google Scholar]
- 25.Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57:284–294. [DOI] [PubMed] [Google Scholar]
- 26.Liberman MA, Phillips EH, Carroll BJ, et al. Laparoscopic colectomy vs traditional colectomy for diverticulitis. Outcome and costs. Surg Endosc. 1996;10:15–18. [DOI] [PubMed] [Google Scholar]
- 27.Altinel Y, Cavallaro PM, Ricciardi R, et al. Can we predict surgically complex diverticulitis in elective cases? Dis Colon Rectum. 2020;63:646–654. [DOI] [PubMed] [Google Scholar]
- 28.Fischer MA, Avorn J. Economic implications of evidence-based prescribing for hypertension: can better care cost less? JAMA. 2004;291:1850–1856. [DOI] [PubMed] [Google Scholar]
- 29.Arseneau KO, Yeaton P, Kahaleh M, et al. Effect of digestive health care services integration on resource use and outcomes in patients with digestive disorders. Clin Gastroenterol Hepatol. 2003;1:145–151. [DOI] [PubMed] [Google Scholar]
- 30.Zarling EJ, Piontek F, Klemka-Walden L, et al. The effect of gastroenterology training on the efficiency and cost of care provided to patients with diverticulitis. Gastroenterology. 1997;112: 1859–1862. [DOI] [PubMed] [Google Scholar]
- 31.Khera R, Angraal S, Couch T, et al. Adherence to methodological standards in research using the national inpatient sample. JAMA. 2017;318:2011–2018. [DOI] [PMC free article] [PubMed] [Google Scholar]