Abstract
Objective:
The primary objective of this study was to assess trends in bowel preparation among patients who had elective colectomy between 2012 and 2018. The secondary objective was to assess patient and procedure-related factors predictive of bowel preparation use or lack thereof.
Background:
Numerous studies have demonstrated that bowel preparation before elective colorectal surgery can reduce the risk of postoperative complications. Studies of surgeon practices found 75% to 98% prescribe bowel preparation to their patients, although biases in the study design may lead to overestimation of bowel preparation practice.
Methods:
Cross-sectional study of the National Surgical Quality Improvement Program colectomy procedure targeted dataset. We included patients from 18 to 90 years old who underwent elective colectomy (n = 101,096). The primary outcomes were bowel preparation before elective colectomy, including oral antibiotic only, mechanical only, both oral and mechanical, or none.
Results:
Twenty percent of patients did not do any bowel preparation before elective colectomy. Almost all covariates were independently associated with any bowel preparation, although some were not clinically relevant. The odds that Black/African American or Hispanic patients had any bowel preparation were lower than that of White patients. Additionally, the odds minimally invasive colectomy patients completed any bowel preparation was 1.46 times that of open surgery patients.
Conclusions:
This study is the first of its kind to assess trends in bowel preparation using an objective dataset. Our study highlights disparities in bowel preparation. Further studies should focus on delineating the root cause of this disparity, identifying the barriers, and finding solutions.
Keywords: colectomy, bowel preparation, infection prevention, health disparity, NSQIP
Mini Abstract: The practice of bowel preparation is trending up with the evidence base, though a fifth of the sample did not complete any bowel preparation. We identified racial and ethnic disparities in completion of bowel preparation that needs to be explored and addressed in surgical practices.
Supplemental Digital Content is available in the text.
INTRODUCTION
Numerous randomized controlled trials and observational studies have demonstrated that oral antibiotic bowel preparation (OABP) before elective colorectal surgery, in combination with mechanical bowel preparation (MBP), can reduce the risk of postoperative complications.1–7 A meta-analysis of 38 randomized controlled trials found that MBP with OABP was associated with a lower risk of surgical site infection (SSI) when compared to MBP alone (odds ratio [OR] = 0.71, 95% Credible Interval [CrI] = 0.57, 0.88) or with no preparation (OR = 0.60, 95% CrI = 0.45, 0.79).1 Rollins et al7 also found a protective effect on the risk of SSI (risk ratio = 0.51, 95% confidence intervals [CI] = 0.55, 0.70, I2 = 0%) of OABP plus MBP when compared with MBP alone.
In addition to reducing the risk of SSIs, several studies have demonstrated that the combination of MBP and OABP can reduce the risk of anastomotic leak and postoperative ileus.8,9 These complications prolong hospitalization, decrease patients’ quality of life, and often require a return to the operating room.10 Reducing the incidence of these events not only reduces patient morbidity but also lowers healthcare costs. The American Society of Colon and Rectal Surgeons (ASCRS) Clinical Practice Guidelines encourage dual MBP and OABP for all elective colorectal surgeries unless specifically contraindicated.11 However, the extent to which bowel preparation methods have changed over time in conjunction with the evidence base is unclear.
Two studies previously assessed trends in bowel preparation with self-reported practices among members of the ASCRS. Zmora et al12 found that approximately 75.0% of participants (N = 515) routinely instructed patients to perform OABP, while more than 99.0% routinely instructed patients to perform MBP. A similar study from 2018 found that 83.2% of participants (N = 359) reported they instruct patients to perform OABP, while 98.6% routinely instruct patients to perform MBP, and 79.3% instruct patients to do both.13
While these studies are informative, biases in the study design may lead to the overestimation of bowel preparation practice. Thus, the primary objective of this study was to assess trends in bowel preparation by type among patients who had an elective colectomy between 2012 and 2018 using a large, validated dataset. We hypothesize that the proportion of patients that performed any bowel preparation increased over the last 6 years in accordance with the increase in the evidence base.
Our secondary objective was to explore patient and procedure-related factors predictive of bowel preparation use or lack thereof and identify groups or aspects of clinical care that can be targeted for improvement. This study not only provides a glimpse of the changes in clinical practice over time but also provides insight into the factors associated with bowel preparation among patients who had an elective colectomy. Importantly, the latter then allows identified disparities across patient groups to be addressed through health promotion or quality improvement programs.
METHODS
Study Design and Participants
We performed a cross-sectional study of the American College of Surgeons’ National Surgical Quality Improvement Program (NSQIP) colectomy procedure targeted (PT) datasets from 2012 to 2018. In 2012, 121 hospitals in the United States entered cases into the colectomy PT dataset with greater participation in subsequent years (Supplemental Table 1, http://links.lww.com/AOSO/A54).14 Large facilities used a systematic sampling strategy to select cases for inclusion, while small and rural hospitals reported all cases as described in the NSQIP user guide.15
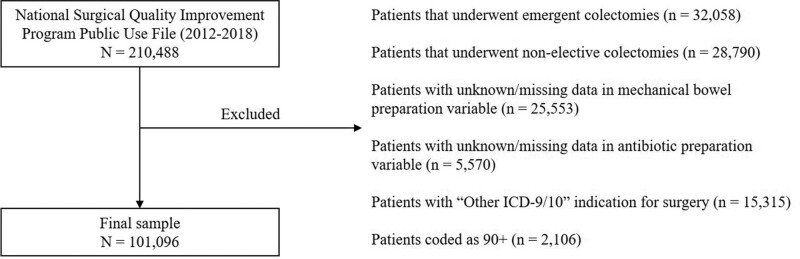
We included all patients in the PT datasets if they underwent an elective colectomy between 2012 and 2018. We excluded patients that required an emergent colectomy, had a nonelective colectomy, or had missing data for bowel preparation. We also excluded patients if the surgical approach was described as “unknown” or the indication for surgery was described as “Other—Enter ICD-9/10 for diagnosis.” We gained little information with these variables and their exclusion did not diminish the value of the analysis.16 Finally, we excluded patients who were coded as “90+” years old because NSQIP clusters these patients to prevent inadvertent identification (Fig. 1).15 This group represented only 1% of the total sample.
FIGURE 1.
Overview of sample selection from the NSQIP Colectomy Targeted dataset. NSQIP indicates National Surgical Quality Improvement Program.
This study was exempt from Nuvance Health’s Institutional Review Board review because we obtained the data from a public use file that was deidentified before acquisition. We followed all acquisition requirements from NSQIP including the user agreement contract. All authors contributed to the analysis and interpretation of results and approved publication of the manuscript in its entirety.
Variables
The variables included in our study were primarily selected from the PT datasets. We merged the PT datasets with the standard public use files using the case ID to capture demographics. The primary dependent variable was preoperative bowel preparation method, including no bowel preparation, MBP, OABP, or both. We created a categorical variable from the NSQIP variables for MPB and OABP (Table 1). We also created a dichotomous variable to reflect any versus no bowel preparation as the primary outcome variable in logistic regression analyses. We conducted a sensitivity analysis with a second dichotomous variable reflecting any bowel preparation as 0 = none or antibiotic only and 1 = mechanical only or both.
TABLE 1.
Descriptive Statistics for Elective Colectomy Patients Included in Analyses to Assess Trends and Determinants of Bowel Preparation Between 2012 and 2018 (N = 101,096)
| Characteristic | No Bowel Preparation (N = 21,165) | Any Bowel Preparation (N = 79,931) | P | |
|---|---|---|---|---|
| Operative year | 2012 | 1758 (8.3) | 5552 (7.0) | <0.01 |
| 2013 | 2336 (11.0) | 7163 (9.0) | ||
| 2014 | 3261 (15.4) | 8501 (10.6) | ||
| 2015 | 3623 (17.1) | 11,386 (14.2) | ||
| 2016 | 3720 (17.6) | 13,993 (17.5) | ||
| 2017 | 3087 (14.6) | 16,244 (20.3) | ||
| 2018 | 3380 (16.0) | 17,092 (21.4) | ||
| Age | <30 years old | 819 (3.9) | 2131 (2.7) | <0.01 |
| 30–39 years old | 1147 (5.4) | 4148 (5.2) | ||
| 40–49 years old | 2189 (10.3) | 9049 (11.3) | ||
| 50–59 years old | 4536 (21.4) | 19,590 (24.5) | ||
| 60–69 years old | 5452 (25.8) | 22,148 (27.7) | ||
| 70–79 years old | 4664 (22.1) | 16,149 (20.2) | ||
| 80–89 years old | 2358 (11.1) | 6716 (8.4) | ||
| Sex | Female | 10,804 (51.0) | 40,268 (50.4) | 0.08 |
| Male | 10,361 (49.0) | 39,663 (49.6) | ||
| Race | White | 14,038 (66.3) | 61,380 (76.8) | <0.01 |
| Black or African American | 1686 (8.0) | 6461 (8.1) | ||
| Other | 745 (3.5) | 3321 (4.2) | ||
| Unknown/not reported | 4696 (22.2) | 8769 (10.9) | ||
| Ethnicity | Not Hispanic | 15,792 (74.6) | 68,728 (86.0) | <0.01 |
| Hispanic | 980 (4.6) | 3719 (4.6) | ||
| Unknown/not reported | 4393 (20.8) | 7484 (9.4) | ||
| BMI | Normal weight (BMI = 18.5–24.9) | 6133 (29.0) | 21,642 (27.1) | <0.01 |
| Overweight (BMI = 25.0–29.9) | 7087 (33.5) | 27,052 (33.8) | ||
| Obese (BMI ≥ 30) | 7222 (34.1) | 29,468 (36.9) | ||
| Underweight (BMI < 18.5) | 723 (3.4) | 1769 (2.2) | ||
| Diabetes | Yes | 3339 (15.8) | 11,873 (14.9) | <0.01 |
| History of congestive heart failure | Yes | 150 (0.7) | 384 (0.5) | <0.01 |
| High BUN > 25* | Yes | 1200 (6.8) | 3828 (5.5) | <0.01 |
| Indication for surgery | Colon cancer | 10,762 (50.9) | 39,068 (48.9) | <0.01 |
| Nonmalignant polyp | 2911 (13.7) | 10,130 (12.7) | ||
| Chronic diverticular disease | 2962 (14.0) | 17,400 (21.8) | ||
| Colon cancer with obstruction | 733 (3.5) | 1778 (2.2) | ||
| Acute diverticulitis | 996 (4.7) | 4661 (5.8) | ||
| Crohn’s disease | 2015 (9.5) | 4988 (6.2) | ||
| Ulcerative colitis | 510 (2.4) | 1352 (1.7) | ||
| Volvulus | 189 (0.8) | 378 (0.5) | ||
| Bleeding | 75 (0.4) | 151 (0.2) | ||
| Entercolitis (eg, C. difficile) | 12 (0.1) | 25 (<0.1) | ||
| Surgical approach | Open | 5211 (24.6) | 14,614 (18.3) | <0.01 |
| Minimally invasive | 15,954 (75.4) | 65,317 (81.7) | ||
| Right colectomy | Yes | 6582 (31.1) | 17,485 (21.9) | <0.01 |
Data are N (%); P values are the result of Chi-square analyses.
*Missing data: N = 13,172 (13.0%).
BMI indicates body mass index; BUN, blood urea nitrogen.
We used operation year as the independent variable to assess trends in bowel preparation over time. We also included patient and procedure-related variables. These included age, sex, race, ethnicity, body mass index (BMI), preoperative diabetes, history of congestive heart failure, dialysis, indication for colectomy, laterality (right/left), and operative approach. Many categories for operative approach resulted in small cell sizes. We combined them to reflect an open or minimally invasive surgical approach with minimally invasive defined as laparoscopic, robotic, hybrid, endoscopic, single incision laparoscopic, natural orifice transluminal endoscopic surgery, and “other” minimally invasive surgery. We coded each patient given the initial approach; patients who had a laparoscopic colectomy that converted to open were coded as laparoscopic. We assumed that surgeons prepared their patients for the intended procedure rather than the result of decisions made during the operation.
We also created a variable to reflect kidney disease since it may be a deterrent for clinicians to prescribe a bowel prep. We deemed patients with preoperative blood urea nitrogen (BUN) measurements greater than 25 to have impaired kidney function.
Statistical Methods
We used StataSE version 16 with the default method of listwise deletion for missing data.17 For our first objective, we plotted the proportion of patients who completed each bowel preparation method by year to assess trends in bowel preparation over time. The response variable was constrained between 0 and 1, so we used a generalized linear model with a logit link, binomial family, and robust standard errors for these analyses.18 We transformed the response variables using an inverse logit function to generate predicted scores in the original units then performed linear regression.
For our second objective, we performed chi-square and the independent Student’s t-test (two-tailed α = 0.05) to identify relevant patient and procedure-related determinants of any bowel preparation to include in a multivariable model. We used backward, stepwise regression with change-in-estimate and likelihood ratio tests to determine the most parsimonious predictive model of bowel preparation given the hypothesized variables. Finally, we performed multivariable logistic regression of our full model to determine the odds of any bowel preparation while controlling for covariates and possible confounders. We selected the most prevalent group as the reference in nominal variables with no clear order (ie, indication). We confirmed that all of the assumptions of logistic regression were met before analysis. We used identical methods for the sensitivity analysis with the alternate definition for any bowel prep.
RESULTS
Participants
There were 101,096 patients in our sample, and we provide descriptive statistics in Table 1. Approximately 49.5% of patients used both MBP and OABP before elective colectomy, while almost 20% used none. The sample was approximately equal with regards to sex, and the majority were White (74.6%) and not Hispanic (83.6%). Few patients had a history of diabetes, congestive heart failure, or kidney disease. The most common indication for colectomy was colon cancer (49.3%), followed by chronic diverticular disease (20.1%) and nonmalignant polyp (12.9%). Additionally, the majority of patients had minimally invasive surgery (80.4%).
Trends in Bowel Preparation
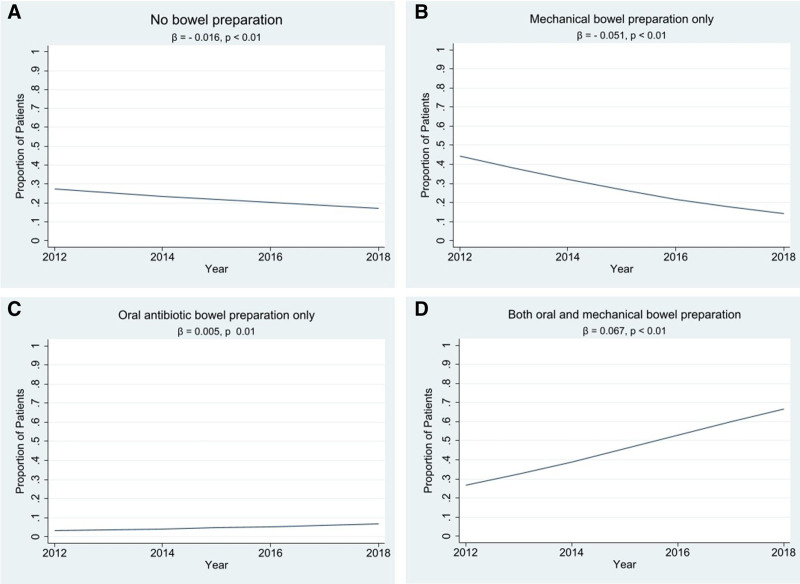
The proportion of patients who had no bowel preparation demonstrated a downward linear trend from 2012 to 2018 (Fig. 2A). There was a similar trend across time in the proportion of patients who only completed MBP, though the slope was much steeper (Fig. 2B). Alternatively, there was a small increase in the proportion of patients who had OABP only, with a statistically significant relationship between the two variables (Fig. 2C). There was a sharper linear increase in the proportion of patients who had both MBP and OABP across time (Fig. 2D).
FIGURE 2.
Trends of the proportion of patients who did no bowel preparation (A), mechanical bowel preparation only (B), oral antibiotic bowel preparation only (C), or both types of bowel preparation (D) from 2012 to 2018 among patients in the NSQIP database who had elective colectomy. NSQIP indicates National Surgical Quality Improvement Program.
Factors Associated With Bowel Preparation
Twenty percent of patients in the sample did not do any bowel preparation before elective colectomy. We found that many of the covariates were statistically significantly associated with any bowel preparation on crude analysis (Table 1), with the exception of sex, other race (compared with White), operative year 2013 and 2015 (compared with 2012), indication for surgery was enterocolitis and nonmalignant polyp (compared with colon cancer), and 40 to 49 years old compared with 60 to 69 years old.
None of the variables included in the full model demonstrated a change-in-estimate greater than 1%. However, likelihood ratio tests demonstrated that diabetes was excess and did not contribute significantly to the model. We included all other variables in the model, although the residuals for age violated the assumption of linearity. We converted age to a categorical variable in increments of 10 to accommodate this modeling issue.
Many of the covariates were independently associated with any bowel preparation in the multivariable model (Table 2). Male sex was statistically significantly associated with any bowel preparation, although the differences in odds were not clinically meaningful. The P value is likely an artifact of the very large sample size. Compared with 60 to 69 years old, young adults and patients over 80 were less likely to perform any bowel prep. Additionally, compared with 2012, patients undergoing elective colectomy in 2016 to 2018 had greater odds of completing bowel prep after controlling for indication, approach, and other covariates.
TABLE 2.
Multivariable Logistic Regression of Patient and Procedure-related Determinants of Any Bowel Preparation Among Patients in the NSQIP Database Who Underwent Elective Colectomy Between 2012 and 2018 (N = 87,481)*
| Any Bowel Preparation † | |||
|---|---|---|---|
| Characteristic | aOR | 95% CI | P |
| Operative year (2012) | Reference | – | – |
| 2013 | 1.05 | 0.97, 1.14 | 0.23 |
| 2014 | 0.92 | 0.85, 0.99 | 0.04 |
| 2015 | 1.04 | 0.97, 1.12 | 0.31 |
| 2016 | 1.28 | 1.19, 1.37 | <0.01 |
| 2017 | 1.84 | 1.71, 1.99 | <0.01 |
| 2018 | 1.04 | 1.10, 1.97 | <0.01 |
| Age (60–69 years old) | Reference | – | – |
| <30 years old | 0.86 | 0.77, 0.96 | <0.01 |
| 30–39 years old | 0.94 | 0.87, 1.03 | 0.17 |
| 40–49 years old | 0.97 | 0.91, 1.04 | 0.42 |
| 50–59 years old | 1.01 | 0.96, 1.06 | 0.66 |
| 70–79 years old | 0.90 | 0.86, 0.95 | <0.01 |
| 80–89 years old | 0.83 | 0.78, 0.88 | <0.01 |
| Sex (female) | Reference | – | – |
| Male | 1.05 | 1.01, 1.08 | <0.01 |
| Race (White) | Reference | – | – |
| Black or African American | 0.91 | 0.85, 0.97 | <0.01 |
| Other | 0.95 | 0.87, 1.04 | 0.26 |
| Unknown/not reported | 0.69 | 0.64, 0.73 | <0.01 |
| Ethnicity (Non-Hispanic) | Reference | – | – |
| Hispanic | 0.86 | 0.79, 0.93 | <0.01 |
| Unknown/not reported | 0.51 | 0.47, 0.55 | <0.01 |
| BMI [normal weight (BMI = 18.5–24.9)] | Reference | – | – |
| Overweight (BMI = 25.0–29.9) | 1.00 | 0.96, 1.05 | 0.96 |
| Obese (BMI ≥ 30) | 1.02 | 0.98, 1.07 | 0.37 |
| Underweight (BMI < 18.5) | 0.80 | 0.73, 0.89 | <0.01 |
| History of congestive heart failure | 0.78 | 0.64, 0.96 | 0.02 |
| High BUN > 25 | 0.86 | 0.80, 0.92 | <0.01 |
| Indication for surgery (colon cancer) | Reference | – | – |
| Colon cancer with obstruction | 0.64 | 0.58, 0.71 | <0.01 |
| Acute diverticulitis | 1.00 | 0.93, 1.09 | 0.84 |
| Bleeding | 0.62 | 0.46, 0.84 | <0.01 |
| Chronic diverticular disease | 1.27 | 1.21, 1.34 | <0.01 |
| Crohn’s disease | 0.71 | 0.66, 0.77 | <0.01 |
| Entercolitis (ie, C. difficile) | 0.67 | 0.31, 1.49 | 0.33 |
| Non-malignant polyp | 0.93 | 0.89, 0.99 | 0.01 |
| Ulcerative colitis | 0.60 | 0.54, 0.68 | <0.01 |
| Volvulus | 0.52 | 0.43, 0.64 | <0.01 |
| Surgical approach (open) | Reference | – | – |
| Minimally invasive | 1.31 | 1.26, 1.36 | <0.01 |
| Colectomy laterality (left) | Reference | – | – |
| Right | 0.74 | 0.71, 0.77 | <0.01 |
*Listwise deletion of variables with missing data reduced the total sample size, although not enough to decrement the power of the study.
†Any bowel prep = antibiotic only, mechanical only, and both.
aOR indicates adjusted odds ratio; BMI, body mass index; BUN, blood urea nitrogen; CI, confidence interval; NSQIP, National Surgical Quality Improvement Program.
The odds that Black or African American patients had any bowel preparation were 0.91 times that of White patients. Hispanic patients had lower odds of completing any bowel prep compared to non-Hispanic (aOR = 0.86, CI = 0.79, 0.93). Interestingly, patients with unknown race or ethnicity had even lower odds of any bowel preparation when compared with non-Hispanic patients (aOR = 0.51, CI = 0.47, 0.55). Patients with a history of congestive heart failure and high BUN also had reduced odds of completing any bowel preparation when compared with patients without these diseases.
The indication for the procedure was also strongly associated with any bowel preparation. Patients who had a colectomy due to chronic diverticular disease had 1.27 times the odds of completing any bowel preparation when compared with patients undergoing surgery for colon cancer. Importantly, all other indications for colectomy were associated with much lower odds of completing any bowel preparation when compared to colon cancer except acute diverticulitis (aOR = 1.0, 95% CI = 0.93, 1.09) and enterocolitis (aOR = 0.67, 95% CI = 0.31, 1.49), including colon cancer with obstruction, Crohn’s disease, nonmalignant polyp, ulcerative colitis, volvulus, and bleeding. Finally, the odds that patients who underwent a minimally invasive colectomy completed any bowel preparation were 1.31 times that of patients who had open surgery (95% CI = 1.26, 1.36), and the odds that a patient who underwent a right colectomy completed any bowel prep was 0.74 times that of a patient who underwent a left (95% CI = 0.71, 0.77).
Sensitivity Analysis
Antibiotic bowel preparation alone may not offer the same benefit as mechanical prep or a combination of both. We repeated the analyses above to compare the results between the primary definition (definition 1 = OABP, MBP, and both) and a definition that excludes OABP (definition 2 = MBP and both). The point estimates for the adjusted ORs were all on the same side of 1.0 with the exception of operative years 2013 and 2015 (Supplemental Table 2, http://links.lww.com/AOSO/A55). For all others, we draw similar conclusions as those from definition 1.
DISCUSSION
The purpose of this study was to determine if trends in bowel preparation for elective colectomies mirrored the increasing evidence base. We also sought to determine factors that were associated with bowel preparation before elective colectomy.
Overall, we found the trend in bowel preparation between 2012 and 2018 progressed with the evidence base. Each year a greater proportion of patients completed both OABP and MBP, while progressively fewer patients completed only MBP. However, there is still a concerning proportion of patients not doing any bowel preparation before elective colectomy, with dramatically lower odds of bowel preparation for indications other than colon cancer or chronic diverticular disease.
We found as few as 49.5% of patients completed both OABP and MBP. These numbers are markedly lower than the self-report studies from members of the ASCRS.12,13 McChesney et al13 reported as many as 98.6% of ASCRS members surveyed routinely use MBP, while Zmora et al reported 99%. The disparity between our study and these provider studies may be due to patient compliance with preoperative instructions. Bruns et al19 found that as few as 72.0% of patients in clinical trials for oral nutrition before colectomy complied with preoperative instructions. Similarly, Arrick et al20 found only 77.6% of patients performed preoperative carbohydrate loading before elective colectomy. Thus, it is not surprising that the proportion of surgeons who prescribe bowel preparation and the proportion of patients that complete it are different.
Importantly, the NSQIP instructions require abstractors to document if mechanical or antibiotic bowel prep was performed (not prescribed) in preparation for the operation, while the provider surveys asked surgeons if they prescribe them. However, it is possible there is some misclassification bias in the NSQIP data.
We recommend surgeons use mixed methods, including quantitative examination of bowel prep compliance in their practices and qualitative approaches to understand the determinants of compliance to develop evidence-based strategies to encourage bowel prep. Surgeons can then implement theory-based patient education initiatives to motivate patients to complete bowel preparation and prevent sequelae related to incomplete bowel prep.
The majority of the variables included in our multivariable analysis were significantly associated with bowel preparation use. Some of the significant findings are likely artifacts of the large sample size. However, factors such as ethnicity, race, indication for surgery, and surgical approach had narrow confidence intervals further away from 1.0. The degree of difference in the adjusted odds of any bowel prep across the indications for surgery are particularly concerning. It is possible differences in bowel preparation across indications are the result of surgeon hesitancy to prescribe a preparation for patients in whom they perceive a risk of intestinal perforation. This may help patients with an obstruction (ie, malignancy or volvulus) or in patients with severe inflammation such as Crohn’s or ulcerative colitis. Interestingly, we did not observe a decrease in bowel preparation in patients with acute or chronic diverticulitis.24–26
Importantly, we found that African American and Hispanic patients had significantly lower odds of completing any bowel preparation compared with White and non-Hispanic patients. Ours is not the first study to document these differences, although we are the first to describe them for colectomies. Kaye et al21 found racial/ethnic minority patients had 17 times the risk of not completing bowel preparation before laparoscopic renal surgery, while studies of colonoscopy preparation found African American patients less likely to perform bowel preparation compared with White patients.22,23 It is critical that future research investigates the cause of this disparity. Does it stem from insufficient patient education, lack of cultural competency, variations in health literacy, physician decision-making, or other causes? Surgeons may wish to examine their own practices for trends in bowel preparation to ensure all groups are equally likely to receive culturally appropriate instructions and follow up for bowel preparation.
We also found that surgical approach is an important predictor of bowel preparation after controlling for others. Patients who completed any bowel preparation had significantly higher odds of having minimally invasive surgery instead of open when compared with those who had no bowel preparation. Surgeons who anticipate increased maneuvering of the bowel in minimally invasive surgeries may more heavily encourage or require bowel preparation.24 Nonetheless, the literature shows all approaches benefit from bowel preparation. Surgeons may wish to examine their practices to ensure bowel preparation is done for all elective colectomies, not only the minimally invasive cases.
Limitations
There are several limitations to our study. First, the sample used in this study is not nationally representative, the sampling strategy across participating institutions is not consistent, and the participating institutions changed over time.27,28 It is important to interpret the temporal trends in this study within the scope of this limitation. Additionally, data are only entered into the NSQIP database by participating hospitals, and the sample demographics reveal a homogenous population. Inferences should only be made in the context of the sample characteristics. Another important limitation is that NSQIP deidentifies their data to the extent that statistical analyses cannot account for clustering of cases from the same hospital or surgeon.27 There is likely shared variance that is unaccounted for in the analyses, and the assumption that all observations are independent is violated for regression.
We excluded patients that had missing data for the bowel preparation variable and used listwise deletion for other missing data variables included in multivariable analysis (primarily BUN). This may lead to bias as there may be unique characteristics of these patients that we cannot account for in our analysis. Additionally, 13.3% of patients in the sample had “unknown” race and ethnicity. This was the second-largest group for the variable and also demonstrated a marked difference in odds of bowel preparation compared with White patients. We cannot draw conclusions or make recommendations for this group given the lack of specificity in this data. Further research should be done to clarify and prevent disparities in bowel preparation and surgical outcomes in minority groups.
In the NSQIP database, the completion of bowel prep is a binary variable. There is no way to distinguish patients who did not tolerate a bowel preparation and those who did not attempt one. Furthermore, the reasons behind a lack of bowel preparation may be nuanced: surgeon preference to avoid a bowel perforation, patient intolerance to large volume of liquid, partial consumption of the preparation, or lack of adherence to the instructed timing. Further prospective studies are required to delineate these patients and assess ways of addressing this deviation from current recommendations.
Finally, we excluded patients who had emergent or nonelective surgeries, as they would be less likely to complete bowel preparation. Despite these exclusions, ~1% of patients had indications more likely to be emergent or nonelective. It is possible procedures were incorrectly coded leading to a misclassification bias. We were unable to conduct our own quality verification on this data since we performed a retrospective analysis. However, the NSQIP user guide describes a robust inter-rater reliability audit process and reports only 2% disagreement on all variables.27 Therefore, we have confidence that the data are acceptably accurate, and the small proportion of potentially misclassified cases are unlikely to significantly impact the direction and magnitude of the results.
CONCLUSIONS
This study is the first of its kind to assess trends in bowel preparation over time using an objective dataset. The results are encouraging and demonstrate a progression of practices in line with the evidence base. However, it is important to further study the reasons patients may not complete bowel preparation to encourage best practices in colon surgery. Specifically, our study highlights disparities in bowel preparation completion between ethnic and racial minorities in comparison to White patients. Further studies should focus on delineating the root cause of this disparity in care and evaluate whether the barriers are a result of a lack of cultural competency, variations in health literacy, physician decision-making, or myriad other potential factors.
ACKNOWLEDGMENTS
We would like to acknowledge the faculty and staff in the Department of Surgery at Danbury Hospital and the Department of Research and Innovation at Nuvance Health.
Supplementary Material
Footnotes
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in the ACS NSQIP are the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or the conclusions derived by the authors.
Disclosure: The authors declare that they have nothing to disclose.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s Web site (www.annalsofsurgery.com).
REFERENCES
- 1.Toh JWT, Phan K, Hitos K, et al. Association of mechanical bowel preparation and oral antibiotics before elective colorectal surgery with surgical site infection: a network meta-analysis. JAMA Netw Open. 2018;1:e183226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kaslow SR, Gani F, Alshaikh HN, et al. Clinical outcomes following mechanical plus oral antibiotic bowel preparation versus oral antibiotics alone in patients undergoing colorectal surgery. BJS Open. 2018;2:238–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Luo J, Liu Z, Pei KY, et al. The role of bowel preparation in open, minimally invasive, and converted-to-open colectomy. J Surg Res. 2019;242:183–192. [DOI] [PubMed] [Google Scholar]
- 4.Murray AC, Kiran RP. Benefit of mechanical bowel preparation prior to elective colorectal surgery: current insights. Langenbecks Arch Surg. 2016;401:573–580. [DOI] [PubMed] [Google Scholar]
- 5.Scarborough JE, Mantyh CR, Sun Z, et al. Combined mechanical and oral antibiotic bowel preparation reduces incisional surgical site infection and anastomotic leak rates after elective colorectal resection: an analysis of colectomy-targeted ACS NSQIP. Ann Surg. 2015;262:331–337. [DOI] [PubMed] [Google Scholar]
- 6.Wexner SD, Yellinek S. Is preoperative bowel preparation needed before elective colectomy? Lancet. 2019;394:808–810. [DOI] [PubMed] [Google Scholar]
- 7.Rollins KE, Javanmard-Emamghissi H, Acheson AG, et al. The role of oral antibiotic preparation in elective colorectal surgery: a meta-analysis. Ann Surg. 2019;270:43–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haskins IN, Fleshman JW, Amdur RL, et al. The impact of bowel preparation on the severity of anastomotic leak in colon cancer patients. J Surg Oncol. 2016;114:810–813. [DOI] [PubMed] [Google Scholar]
- 9.Kiran RP, Murray AC, Chiuzan C, et al. Combined preoperative mechanical bowel preparation with oral antibiotics significantly reduces surgical site infection, anastomotic leak, and ileus after colorectal surgery. Ann Surg. 2015;262:416–25; discussion 423. [DOI] [PubMed] [Google Scholar]
- 10.Hammond J, Lim S, Wan Y, et al. The burden of gastrointestinal anastomotic leaks: an evaluation of clinical and economic outcomes. J Gastrointest Surg. 2014;18:1176–1185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Migaly J, Bafford AC, Francone TD, et al. ; Clinical Practice Guidelines Committee of the American Society of Colon and Rectal Surgeons. The American Society of Colon and rectal surgeons clinical practice guidelines for the use of bowel preparation in elective colon and rectal surgery. Dis Colon Rectum. 2019;62:3–8. [DOI] [PubMed] [Google Scholar]
- 12.Zmora O, Wexner SD, Hajjar L, et al. Trends in preparation for colorectal surgery: survey of the members of the American Society of Colon and Rectal Surgeons. Am Surg. 2003;69:150–154. [PubMed] [Google Scholar]
- 13.McChesney SL, Zelhart MD, Green RL, Nichols RL. Current U.S. pre-operative bowel preparation trends: a 2018 survey of the American Society of Colon and Rectal Surgeons members. Surg Infect. 2019;21:sur.2019.125. [DOI] [PubMed] [Google Scholar]
- 14.American College of Surgeons. ACS NSQIP Participant Use Data File. ACS National Surgical Quality Improvement Program. Available at: https://www.facs.org/quality-programs/acs-nsqip/participant-use. Accessed February 10, 2020. [Google Scholar]
- 15.American College of Surgeons. ACS NSQIP Participant Use Data File. ACS NSQIP. 2019. Available at: https://www.facs.org/quality-programs/acs-nsqip/participant-use. Accessed August 7, 2019. [Google Scholar]
- 16.Koskenvuo L, Lehtonen T, Koskensalo S, et al. Mechanical and oral antibiotic bowel preparation versus no bowel preparation for elective colectomy (MOBILE): a multicentre, randomised, parallel, single-blinded trial. Lancet. 2019;394:840–848. [DOI] [PubMed] [Google Scholar]
- 17.StataCorp LLC. Stata Statistical Software: Release 16. College Station, TX; 2019. [Google Scholar]
- 18.Baum C. Stata tip 63: modeling proportions. Stata J. 2008;8:299–303. [Google Scholar]
- 19.Bruns ERJ, Argillander TE, Van Den Heuvel B, et al. Oral nutrition as a form of pre-operative enhancement in patients undergoing surgery for colorectal cancer: a systematic review. Surg Infect (Larchmt). 2018;19:1–10. [DOI] [PubMed] [Google Scholar]
- 20.Arrick L, Mayson K, Hong T, et al. Enhanced recovery after surgery in colorectal surgery: impact of protocol adherence on patient outcomes. J Clin Anesth. 2019;55:7–12. [DOI] [PubMed] [Google Scholar]
- 21.Kaye JD, Richstone L, Cho JS, et al. Patient noncompliance before surgery. BJU Int. 2010;105:230–233. [DOI] [PubMed] [Google Scholar]
- 22.Appannagari A, Mangla S, Liao C, et al. Risk factors for inadequate colonoscopy bowel preparations in African Americans and whites at an urban medical center. South Med J. 2014;107:220–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mahmood S, Farooqui SM, Madhoun MF. Predictors of inadequate bowel preparation for colonoscopy: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2018;30:819–826. [DOI] [PubMed] [Google Scholar]
- 24.Ji D. Oral magnesium sulfate causes perforation during bowel preparation for fiberoptic colonoscopy in patients with colorectal cancer. J Emerg Med. 2012;43:716–717. [DOI] [PubMed] [Google Scholar]
- 25.Yamauchi A, Kudo SE, Mori Y, et al. Retrospective analysis of large bowel obstruction or perforation caused by oral preparation for colonoscopy. Endosc Int Open. 2017;5:E471–E476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Langdon DE. Colonic perforation with volume laxatives. Am J Gastroenterol. 1996;91:622–623. [PubMed] [Google Scholar]
- 27.American College of Surgeons National Surgical Quality Improvement Program. User Guide for the 2018 ACS NSQIP Participant Use Data File (PUF). 2019. Available at: https://www.facs.org/-/media/files/quality-programs/nsqip/nsqip_puf_userguide_2018.ashx. Accessed January 28, 2020.
- 28.Raval MV, Pawlik TM. Practical Guide to Surgical Data Sets: National Surgical Quality Improvement Program (NSQIP) and Pediatric NSQIP. JAMA Surg. 2018;153:764–765. [DOI] [PubMed] [Google Scholar]