Abstract
This narrative review aims to summarize non-pharmacological interventions for pain management in hemodialysis patients, assessing their potential benefits and limitations in enhancing patient well-being and quality of life. We reviewed the current literature on five primary non-pharmacological interventions: acupuncture, cognitive behavioral therapy, relaxation techniques, virtual reality, and alternative methods such as transcutaneous electrical nerve stimulation, music therapy, and aromatherapy. We analyzed the evidence regarding their effectiveness, feasibility, and optimal implementation strategies. The existing evidence supports the potential benefits of these interventions in managing pain and improving the well-being of hemodialysis patients. However, further high-quality research is needed to confirm their effectiveness, establish implementation best practices, and assess their long-term impact on patient outcomes. Non-pharmacological interventions hold promise for pain management in hemodialysis patients. Additional research is required to optimize these interventions and validate their effectiveness, contributing to comprehensive pain management strategies for this vulnerable patient population.
Keywords: pain management, hemodialysis, acupuncture, cognitive behavioral therapy, relaxation techniques, virtual reality
1. Introduction
Hemodialysis is a life-saving treatment for people with end-stage renal disease (ESRD) that involves the removal of toxins and excess fluids from the blood using an artificial kidney. Although hemodialysis is essential to maintain the health of ESRD patients, the process can cause significant pain and discomfort, leading to a lower quality of life [1,2]. Pain faced by hemodialysis patients can be categorized into three categories: (a) procedure-related pain, (b) access-related pain, and (c) pain secondary to renal disease or its complications [3,4]. Effective pain management is crucial during hemodialysis to improve patient compliance, enhance the overall treatment experience, and promote better physical, mental, and emotional well-being [5,6].
Inappropriate pain management can lead to nonadherence to treatment, increased healthcare costs, and reduced quality of life [7]. Furthermore, unmanaged pain can exacerbate existing co-morbidities and contribute to the development of new health problems such as depression, anxiety, and sleep disturbances [8]. Managing pain in hemodialysis patients is often challenging due to the complex nature of ESRD and the potential risks associated with pharmacological interventions. Commonly prescribed medications for pain management include opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and acetaminophen [9]. However, in 2016, the Centers for Disease Control and Prevention published guidelines that addressed the impact of opioids on patients suffering from chronic non-malignant pain, including ESRD. These guidelines recommended the reduction of dosages or discontinuation of opioid medications to alleviate the burden experienced by patients [10]. Moreover, those conventional medications do have other limitations, such as drug–drug interactions, the potential for addiction, gastrointestinal complications, and the need for dose adjustments due to decreased renal function [5]. Given that studies evaluating non-pharmacological approaches in patients with ESRD are scarce, in addition to the limitations of pharmacological approaches, this study was designed to review the available evidence on the effectiveness, feasibility, and accessibility of various non-pharmacological interventions (NPIs), including acupuncture, cognitive behavioral therapy, relaxation techniques, virtual reality, and other alternative methods in ESRD cases, and to evaluate their performance and application in clinical practice.
2. Methods
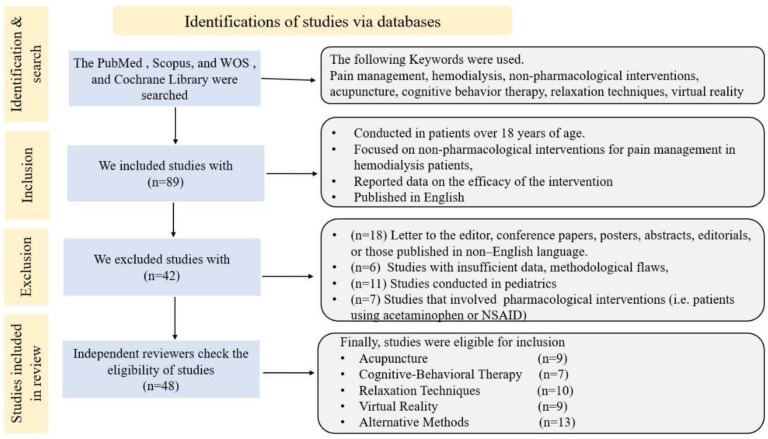
This narrative review aims to synthesize the evidence on NPIs for pain management in hemodialysis patients. The methods followed a simplified approach to ensure a comprehensive analysis of the available literature, consisting of the following steps: a strategy to locate pertinent publications was performed through digital repositories, encompassing databases such as PubMed, Scopus, Web of Science, and the Cochrane Library. The search strategy used a combination of keywords and subject headings related to NPIs, pain management, and hemodialysis patients. Keywords were combined using Boolean operators such as “AND” and “OR” to refine the search results. The search was carried out for articles published up to 2023. The study workflow is described in Figure 1. In this review, we primarily focused on studies that reported reductions in pain and improvements in quality of life (QOL) among hemodialysis patients. We excluded any studies that examined the effects of pharmacological drugs, as they were beyond the scope of our analysis. For each study included, we collected information about the authors’ names, year of publication, study type, population, and sample size. This review aimed to summarize the principal mechanism of NPI action and its role in the following: 1. Improving patients’ QOL and related stress; 2. reducing the pain scale; and 3. the specific type of pain for which it was employed, whether this was procedure-related pain, access-related pain, or pain secondary to renal disease and its complications.
Figure 1.
The study workflow.
3. Acupuncture
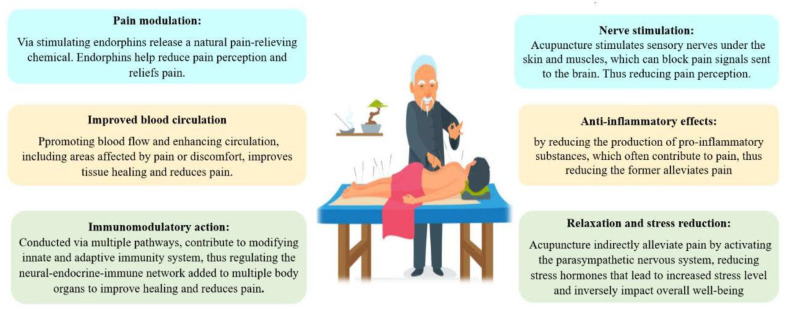
Acupuncture is a traditional Chinese medicine technique involving the insertion of thin needles into specific points on the body to stimulate the flow of energy (Qi) and restore balance [11,12,13]. The therapeutic effect is believed to be achieved through the modulation of multiple physiological systems and biochemical pathways, as shown in Figure 2, which describes how acupuncture contributes to pain reduction in ESRD [14,15,16].
Figure 2.
The main proposed pathways by which acupuncture interferes with pain intensity.
Several studies have investigated the efficacy of acupuncture for pain management in the hemodialysis group. A recent randomized control trial by Correia et al. [17] in 2022 was conducted on 67 male and female adult patients who presented decreased functional capacity associated with hemodialysis. The study concluded that patients undergoing hemodialysis demonstrated improvements in functional capacity and muscle strength after acupuncture treatment. Similarly, another study was conducted by Bullen et al. [18] on 101 patients with end-stage renal disease, but this time acupuncture was associated with a massage procedure. The conclusion of this study was an improvement in the overall health-related quality of life of the 101 patients, which is confirmed by a new study that revealed that acupuncture was found to enhance the health-related quality of life in individuals undergoing maintenance hemodialysis following their treatment [19]. In addition, a study by Tsai et al. [20] focused on the impact of acupuncture on the reduction of restless leg syndrome (RLS) in hemodialysis patients.
RLS is a common complication that can negatively affect sleep quality and overall well-being. The study revealed that acupuncture treatment significantly decreased RLS symptoms but did not enhance sleep quality in patients on hemodialysis [20]. A systematic review and meta-analysis of seven randomized controlled trials conducted in 2023 showed that acupuncture is a safe and effective treatment for uremic pruritus (UP) in patients undergoing hemodialysis [21].
A randomized control trial conducted in 2020 on 50 patients divided into two groups of 25 each to determine how acupuncture can reduce pain and improve the quality of life in hemodialysis patients [22]. The study concluded that there was a great improvement in the groups who underwent the procedure and had a remarkable improvement in their overall quality of life. Furthermore, a pilot study investigated the feasibility, safety, and potential benefits of acupuncture for the management of patients who have hemodialysis sessions [23]. Twenty-four participants received individualized acupuncture treatments twice a week for six weeks, and their symptoms were assessed using the MYMOP2 Questionnaire and KDQOL-SF™ Version 1.3. The results showed a significant improvement in the most bothersome symptoms and some quality-of-life subscales at 7 and 11 weeks [23]. Acupuncture combined with hemodialysis was also more effective in relieving pruritus than hemodialysis alone [24]. Adverse events were rare, and acupuncture was found to be a safe treatment modality for patients with UP who received hemodialysis. Furthermore, in the context of fatigue experienced by hemodialysis patients, Melo et al. [25] revealed that acupuncture can offer a positive influence. Their literature review found a significant reduction in reported fatigue levels in patients treated with acupuncture, demonstrating the potential role of acupuncture in managing this debilitating symptom. Furthermore, they found that acupuncture can reduce sleep problems and HRQOL in patients with CKD [25].
However, while these studies collectively suggest that acupuncture can have multifaceted benefits for hemodialysis patients, it is crucial to note that acupuncture must be performed by qualified professionals to ensure patient safety. As reiterated by Xu et al. [26], acupuncture-related adverse events can occur, although some of these events might be minor and transient when the procedure is conducted by adequately trained professionals in proper conditions. Zheng et al. [27] explored the potential of acupuncture for improving cardiovascular function in hemodialysis patients. In this study, acupuncture was associated with improvements in mild hypertension, one of the most common co-morbidities in these patients [27]. The exact mechanism through which acupuncture impacts cardiovascular function is still under investigation, but the findings suggest a promising avenue for further research [28]. Acupuncture’s multifaceted benefits make it a suitable intervention for pain secondary to renal disease or its complications [21,23,24]. However, more extensive and well-designed studies are required to solidify these findings and determine the optimal treatment parameters for this patient population.
4. Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy (CBT) is a goal-oriented psychotherapy that focuses on identifying and modifying maladaptive thoughts, emotions, and behaviors [29]. In the context of pain management, CBT aims to help patients develop effective coping strategies, improve pain tolerance, and improve self-efficacy [30]. CBT has been investigated for its potential to treat pain in hemodialysis patients. The systematic review and meta-analysis by Zegarow et al. [31] engaged in an exploration of cognitive behavioral therapy being employed as a psychological treatment strategy. It was reported that the lowering of the intensity of depressive symptoms in patients with hemodialysis. To improve patient well-being, they recommend considering incorporating cognitive behavior therapy as an extension to renal replacement therapy. This was in line with Zheng et al. [27] systematic review and meta-analysis that examined the benefits of CBT on depression and anxiety in hemodialysis patients. Furthermore, a randomized control trial conducted by Valsaraj et al. [32] on 67 chronic kidney diseases found that CBT is more effective than nondirective counseling in improving therapeutic adherence, as well as physiological and clinical parameters among CKD patients undergoing hemodialysis. At six months, the experimental group exhibited a significant reduction in interdialytic weight gain and blood pressure and an increase in adherence to dialysis, fluids, diet, and drugs [32].
A pilot study found that a tech-assisted cognitive behavioral therapy procedure for ESRD undergoing hemodialysis was feasible and well accepted [33]. While no significant changes in depression, fatigue, or pain were observed, preliminary results suggested that the intervention may improve physical health and pain. Additionally, a study explored the impact of a 12-week group CBT program, including mindfulness meditation, on the quality of life, mood, anxiety, perceived stress, and biochemical markers in seven ESRD patients undergoing hemodialysis and experiencing depression [34]. Measurements were taken at baseline and at weeks 8 and 12 using the WHOQOL-BREF, BDI-II, HAM-D, BAI, and PSS scales. Biochemical markers were measured at baseline and after 12 weeks. The results revealed significant improvements in quality of life, mood, anxiety, and perceived stress following the 12-week CBT program. In addition, serum creatinine levels significantly improved [34]. A randomized trial evaluated the impact of personal cognitive behavioral therapy in mitigating depressive symptoms and enhancing life quality for hemodialysis patients who exhibited pronounced depressive feelings [35]. A total of 59 patients from two New York dialysis centers completed the study and were assigned to a treatment-first group (n = 33) or a waitlist control group (n = 26). CBT was administered chairside during dialysis treatments for three months, with evaluations performed three and six months post-randomization. The treatment-first group experienced significantly greater reductions in depression scores (both self-reported and clinician-reported) compared to the waitlist group [35]. Furthermore, the treatment-first group showed greater improvements in quality of life and interdialytic weight gain. CBT has also shown positive results in improving the quality of sleep in patients undergoing hemodialysis [36]. CBT addresses the psychological aspects of pain [27,32].
In summary, CBT has shown potential for improving various aspects of well-being in hemodialysis patients, such as social support, quality of life, and mental health outcomes. Further research is needed, including exploring novel modalities such as Internet-based CBT, which could potentially enhance the accessibility and effectiveness of CBT interventions for this patient population. Another area to consider is establishing optimal implementation strategies and confirming CBT’s long-term benefits in hemodialysis patients.
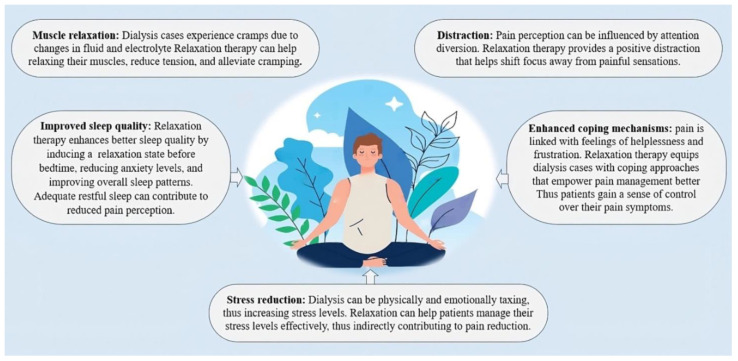
5. Relaxation Techniques
Relaxation techniques encompass a variety of non-invasive approaches designed to promote mental and physical relaxation, thus alleviating stress and fostering well-being [37]. Examples of relaxation techniques include progressive muscle relaxation (PMR), guided imagery, deep breathing exercises, and mindfulness meditation [38]. These mechanisms for alleviating discomfort, as depicted in Figure 3, each follow their own unique pathways.
Figure 3.
The main pathways by which relaxation techniques modify pain intensity.
Numerous studies have investigated the potential benefits of employing relaxation techniques for pain management in individuals undergoing hemodialysis [39]. A quasi-experimental (time series) study evaluated the effects of increasing muscle relaxation on the intensity of restless leg syndrome (RLS) among adult patients on maintenance hemodialysis [40]. Sixty patients with RLS were divided into two groups, the study group receiving progressive muscle relaxation therapy. Results showed that the severity of RLS significantly decreased in the study group, with improvements observed in sleep patterns, physical activities, emotional well-being, and social activities [40]. A clinical trial, organized under randomized control, explored the impact of directed mental visualization on depressive and anxious symptoms, as well as vital signs, among individuals undergoing hemodialysis [41]. Eighty patients were randomly allocated either to a group undergoing guided intervention or a control group. Results displayed that the guided intervention group endured significantly reduced values of anxiety and depression after the intervention compared to the control group. In addition, there was a reduction in respiratory rate and heart rate in the intervention group [41]. A similar study aimed to assess the effect of muscle relaxation on foot pain in hemodialysis patients [42]. Ninety patients were randomly divided into control and experimental groups, with the experimental group practicing Benson muscle relaxation twice a day for a month. The results showed a significant decrease in pain intensity in the intervention group compared to the control, suggesting that muscle relaxation can effectively reduce pain in hemodialysis patients.
In 2023, a novel cluster-randomized controlled study was executed to gauge the efficacy of the Benson Relaxation technique in alleviating pain and perceived stress in patients undergoing hemodialysis [43]. The intervention group performed Benson’s relaxation twice a day for 10 min for 8 weeks, while the control group received an educational session about Progressive Relaxation. The study found that Benson’s Relaxation significantly relieved perceived stress and pain among hemodialysis patients after 1 week and 1 month of practicing, but not after only 1 week. The later study had similar results to a study conducted in 2014 that showed similar findings [44].
A study by Heidari et al. [45] conducted on eight patients and separated into two groups found that relaxation training using the Benson technique twice a day for four weeks was effective in lowering anxiety and pain experienced by hemodialysis patients. The intervention group showed significant improvements compared to the control group, and there was a correlation between pain perception and stress/anxiety levels. Moreover, a randomized controlled experimental investigation was undertaken with the intent to assess the impact of progressive relaxation exercises (PREs) on discomfort, exhaustion, and life quality among individuals receiving hemodialysis [46]. The study included 48 intervention and 48 control patients. The outcomes indicated that the average comprehensive fatigue score and the average pain score diminished in the group undergoing the intervention following the implementation of PREs. Meanwhile, the average ratings for both physical and mental elements of life quality showed an uptick (p < 0.05). No change was observed in the control group. The study reported that PREs can improve pain, fatigue, and quality of life in patients with hemodialysis [46].
Similarly, another study included 100 patients who received PMR every day for four weeks [47]. The results showed a decrease in pain level from moderate to mild, and a significant difference in pain level between the intervention and control groups (p < 0.001). The study showed that NPIs, such as PMR, can effectively reduce pain in hemodialysis patients. These techniques, by promoting relaxation and reducing anxiety, can be instrumental in alleviating procedure-related pain experienced during hemodialysis [42,43,47].
Relaxation techniques show promising potential in managing pain and improving the well-being of hemodialysis patients. However, more high-quality research is needed to confirm the effectiveness of these approaches and determine best practices for their implementation.
6. Virtual Reality
Virtual reality (VR) is an immersive technology that allows users to experience a computer-generated environment using head-mounted displays and other sensory devices [48]. In the context of pain management, VR has been used as a distraction technique to divert attention away from pain, reducing its perception and emotional impact [49]. While the evidence is still sparse, it holds encouraging potential for employing virtual reality in managing pain for individuals receiving hemodialysis [50,51]. A randomized controlled study evaluated the effects of combining exercise training with VR on functionality and quality of life in patients on hemodialysis [52]. The intervention group showed improved functional capacity and quality of life in physical and specific domains [52]. There was no significant impact on depressive symptoms. Furthermore, a pilot trial study tested the safety, acceptability, and utility of VR during hemodialysis treatment sessions using a new VR program that provided mindfulness training and guided meditation [53]. Patients on hemodialysis (n = 20) experienced the program on two separate occasions, and the results showed significant decreases in treatment and/or motion-related symptoms after VR exposure, with high levels of immersion in the VR environment reported. VR programs may be a safe platform to improve the experience of dialysis patients.
Another study conducted in Spain by Romero et al. [54] investigated the effects of virtual reality exercise on the functional and psychological states of patients having chronic kidney failure (CKF) undergoing hemodialysis treatment. The study randomized 80 patients into two groups: an experimental group that will use no immersive VR for intradialytic exercise and a control group that will exercise with a static pedal. The study concluded that virtual reality exercise can improve adherence to exercise in hemodialysis patients, leading to better outcomes such as improved inflammatory state, functional capacity, psychological state, and cardiovascular health. Additionally, VR can make hemodialysis sessions more bearable for patients.
A scoping review aimed to identify the potential of virtual reality interventions to affect the level of participation in self-care and quality of life in hemodialysis patients [55]. The review included 12 articles that demonstrated significant improvement in physical activity levels and a reduction in fatigue in patients during hemodialysis, with no adverse events. The study reported that virtual reality interventions may improve the level of adherence and engagement with treatment. Despite these promising results, more extensive research is needed to establish the effectiveness and feasibility of VR as a non-pharmacological intervention in this population [55]. Given its potential as a distraction technique, VR can be particularly beneficial in addressing procedure-related pain during hemodialysis sessions [54,55].
A focus should be made on evaluating the optimal frequency and duration of VR interventions, determining the most effective VR content for pain management in hemodialysis patients, and exploring the potential long-term benefits of VR therapy to patients’ overall quality of life and psychological well-being.
7. Other Alternative Methods
In addition to the previously mentioned NPIs, several alternative methods have been examined to manage pain in hemodialysis patients. These non-pharmacological approaches include transcutaneous electrical nerve stimulation (TENS), music therapy, and aromatherapy. TENS is a non-invasive method that involves delivering mild electrical currents through electrodes placed on the skin to help alleviate pain [56].
In a randomized controlled trial (RCT) conducted by Yang et al. [57], it was observed that TENS significantly reduced pain intensity in hemodialysis patients with access-related pain and increased salivary flow rate [57]. TENS can be a valuable tool in addressing access-related pain in hemodialysis patients. In various contexts, music was demonstrated to have a significant impact on pain reduction [58]. There are several hypotheses regarding the mechanism that underlies the musical effect. By engaging the brain in the processing of musical stimuli, the brain’s capacity to process pain signals may be diminished; this is called the distraction effect [59]. Listening to pleasurable and comforting music can encourage relaxation and positive emotions, which may relieve pain by reducing stress and anxiety; this is called emotional regulation [60]. Lastly, through neurochemical modulation, music induces the release of endorphins, which can act as analgesics to minimize pain sensations [61,62]. A study examined the effect of listening to patient-selected music on the pain and anxiety levels of hemodialysis patients during vascular access operations [63]. The experimental group listened to their favorite music during their operations, while the control group did not. The experimental group had drastically reduced subjective pain levels, objective pain behaviors, and lower levels of subjective anxiety and anxiety states compared to the controls [63]. These results suggest that music medicine can be a useful clinical intervention to reduce pain and anxiety in hemodialysis patients [63]. Similarly, another study used eight music therapy sessions using specific techniques, and patients were evaluated before and after the intervention [64]. They showed a significant reduction in depression symptoms and an improvement in quality-of-life dimensions such as functional capacity, pain, general health, vitality, mental health, list of symptoms and problems, and overall health [64]. The distraction effect of music can be especially useful in mitigating procedure-related pain during the hemodialysis process [63,64].
Aromatherapy is a type of alternative medicine that employs plant-derived essential oils to promote physical and mental health. While aromatherapy is not a pain remedy, it effectively reduces pain levels and enhances overall comfort [65]. Aromatherapy’s pain-relieving mechanism remains unclear, but multiple hypotheses explain its effectiveness. Aromatherapy activates the limbic system in the brain, which is connected to the olfactory system [66]. This stimulation causes the release of endorphins, a natural painkiller [67]. The delightful aroma of essential oils may distract the mind from painful sensations by acting as a diversion. Lastly, some essential oils possess anti-inflammatory effects, thereby reducing inflammation and relieving pain in afflicted areas [68]. Furthermore, a quasi-experimental study investigated the influences of sweet orange aromatherapy on pain and anxiety in 50 hemodialysis patients [69]. The results showed that patients who received sweet orange aromatherapy had significantly lower pain and anxiety scores than those who received calm breathing. Aromatherapy has shown promise in reducing access-related pain, such as during needle insertions [65,66,69].
8. Discussion
The current study embarked on a quest to investigate numerous non-pharmacological interventions for alleviating pain in individuals undergoing hemodialysis. Five principal strategies were identified. Among these, acupuncture demonstrated considerable promise as a benign and efficacious supplementary therapy for managing pain, enhancing functional capacity and muscular strength, lessening symptoms of restless leg syndrome and uremic pruritus, and bettering the QOL of patients on hemodialysis [13,19]. Nonetheless, additional investigations are imperative to confirm these results and define the ideal parameters for treatment. Cognitive behavioral therapy also exhibited the potential to ameliorate diverse facets of wellness in hemodialysis patients, including social support, QOL, and mental health outcomes [70]. CBT proved successful in attenuating depressive symptom severity, enhancing therapy adherence, and diminishing depression [31]. Internet-based CBT could potentially enhance the accessibility and effectiveness of these interventions for this patient population. Relaxation techniques, encompassing progressive muscle relaxation, guided imagery, deep breathing exercises, and mindfulness meditation, appear to hold potential in managing pain, fatigue, stress, and sleep patterns, as well as in promoting well-being and QOL for hemodialysis patients [43]. Further high-quality studies are needed to substantiate the effectiveness of these strategies and establish optimal procedures for their application.
Emerging as an innovative immersive technology, virtual reality has demonstrated potential benefits in pain management for individuals undergoing hemodialysis. This includes improved exercise adherence, enhanced functional capacity, improved cardiovascular health and psychological state, and making hemodialysis sessions more tolerable [53,54]. VR interventions may also promote patient compliance and engagement in treatment without any reported adverse events. However, more comprehensive research is required to validate VR’s efficacy and practicality as a non-pharmacological intervention in this demographic. Other alternative methods have also been explored for pain management in hemodialysis patients. TENS may reduce pain intensity, and music therapy can potentially reduce pain and anxiety and improve quality of life [71]. Finally, aromatherapy may reduce pain and anxiety during needle insertion [72]. These non-pharmacological approaches have demonstrated potential benefits, although more research is needed to confirm their effectiveness and establish best practices for their implementation.
9. Timing of Interventions
The application of non-pharmacological interventions in the context of hemodialysis varies in terms of their timing. It is essential to understand when these interventions are typically administered to appreciate their efficacy and relevance to the hemodialysis process.
Acupuncture: This ancient Chinese therapeutic technique is often scheduled adjacent to the hemodialysis session. Patients usually undergo acupuncture either preceding, following their hemodialysis sessions, or during the sessions to harness its full therapeutic potential, aiding in pain management and enhancing overall well-being [18,25].
Cognitive behavioral therapy sessions are generally organized independently of the hemodialysis procedure. They can be conducted on days when patients are not undergoing dialysis or after a session to address any psychological distress. All the included studies in our narrative review were introduced during the hemodialysis sessions [31,32,33].
Relaxation techniques: Techniques such as progressive muscle relaxation, guided imagery, and deep breathing exercises can be integrated both during the hemodialysis to alleviate immediate discomfort and outside the session to promote holistic well-being [44,47].
Virtual reality: Employed predominantly as an immersive distraction method, virtual reality interventions are typically introduced during the hemodialysis session [52,53]. This helps divert the patient’s attention from the immediate discomfort and creates a calming environment.
Other alternative methods: The application timing for these methods can be similar. For instance, music therapy can be introduced during the hemodialysis session to provide a soothing ambiance; similarly, aromatherapy might be more effective when used during the session to induce a state of relaxation [63,69].
The studies that explored the benefits of different non-pharmacological interventions are summarized in Table 1.
Table 1.
Comparative analysis on the benefits of different non-pharmacological interventions in hemodialysis patients.
| Intervention | Authors; Year | Study Type | Participants | Perceived Benefits |
|---|---|---|---|---|
| Acupuncture | Kim et al. [16]; 2016 | Observational pilot | 24 hemodialysis patients | Reduction in pain related to hemodialysis |
| Correia et al. [17]; 2022 | Randomized control trial | 67 male and female adult patients who are experiencing decreased functional capacity associated with hemodialysis | Improvements in functional capacity and muscle strength | |
| Bullen et al. [18]; 2018 | Pre- and postintervention surveys | 101 patients who have end-stage renal disease | Improvement in the overall health-related quality of life | |
| Correia et al. [19]; 2023 | Randomized, controlled patient–assessor trial | 67 cases receiving maintenance HD | Enhancement of the health-related quality of life in individuals | |
| Çevik et al. [22]; 2020 | Randomized controlled trial | 50 patients divided into two groups of 25, each consisting of patients on hemodialysis [1] | Improved overall quality of life. Acupressure significantly reduces extremity pain according to the VAS pain score |
|
| Melo et al. [25]; 2020 | Systematic review | Nine selected studies that examined patients with chronic kidney disease | Reduction in reported fatigue; reduced sleep problems and HRQOL in patients with CKD | |
| Cognitive behavioral therapy (CBT) | Zegarow et al. [31]; 2020 | Meta-analysis | 226 patients with hemodialysis | Reduced intensity of depressive symptoms |
| Valsaraj et al. [32]; 2021 | Randomized controlled trial | 67 patients with chronic kidney disease | Improved therapeutic adherence, as well as physiological and clinical parameters among CKD patients undergoing hemodialysis | |
| Jakbowski et al. [33]; 2020 | Pilot study | 10 ESRD undergoing hemodialysis was feasible and well accepted | No significant changes in depression, fatigue, or pain were observed | |
| Sohn et al. [34]; 2018 | Pilot study | Seven ESRD patients undergoing hemodialysis and experiencing depression | Significant improvements in quality of life, mood, anxiety, and perceived stress following the 12-week CBT program. In addition, serum creatinine levels significantly improved | |
| Cukor et al. [35]; 2014 | Randomized reciprocal trial | 59 patients undergoing dialysis treatments for three months | Reductions in depression scores, greater improvements in quality of life and interdialytic weight gain |
|
| Relaxation techniques | Syam et al. [40]; 2022 | A quasi-experimental trial | 60 patients patients on maintenance hemodialysis |
Reduced severity of restless leg syndrome and improvements observed in sleep patterns, physical activities, and social activities |
| Beizaee et al. [41]; 2018 | Clinical trial organized under randomized control | 80 patients undergoing hemodialysis |
Reduced values of anxiety and depression | |
| Blouchi et al. [42]; 2015 | Random division into control and experimental groups | Ninety hemodialysis patients taking Benson muscle relaxation twice a day | A decrease in pain intensity in the intervention group compared to the control, suggesting that muscle relaxation can effectively reduce pain in hemodialysis patients | |
| Heidari et al. [45]; 2014 | Randomized controlled trial | 80 patients undergoing hemodialysis |
Lowered anxiety and pain experienced in hemodialysis patients | |
| Kaplan et al. [46]; 2014 | Randomized controlled experimental investigation | 48 intervention and 48 control patients undergoing hemodialysis |
Reduced fatigue score and average pain score and improved life quality | |
| Virtual reality | Maynard et al. [52]; 2019 | Randomized controlled trial | 20 intervention and 20 control patients undergoing hemodialysis | Improved functional capacity and some quality-of-life domains of hemodialysis patients |
| Hernandez et al. [53]; 2021 | Pilot study | 20 patients undergoing hemodialysis | Decrease in symptoms such as fatigue, nausea, lightheadedness, and headaches that often manifest during hemodialysis sessions | |
| Romero et al. [54]; 2023 | Randomized controlled trial | 40 intervention patients and 40 control patients | Improved adherence to exercise in hemodialysis patients leads to better outcomes, such as improved inflammatory state, functional capacity, psychological state, and cardiovascular health | |
| Transcutaneous electrical nerve stimulation | Yang et al. [57]; 2019 | Randomized controlled trial | 80 patients undergoing hemodialysis | Reduced pain intensity in hemodialysis patients with access-related pain and improved salivary flow rate |
| Music | Kim et al. [63]; 2021 | Randomized controlled trial | 32 intervention patients and 33 control patients | Reduced pain and anxiety levels of hemodialysis patients during vascular access operations |
| Hagemann et al. [64]; 2019 | Interventional study | 23 patients undergoing hemodialysis | Significant decrease in depression symptoms and improved quality of life across various dimensions, including functional capacity, pain, general health, vitality, mental health, and overall well-being | |
| Aromatherapy | Reyes et al. [69]; 2020 | A quasi-experimental | 50 patients undergoing hemodialysis | Sweet orange aromatherapy was effective in reducing pain and anxiety in hemodialysis patients |
| Yıldız et al. [72]; 2022 | Systematic review | Seven studies included in the review | Decreased pain during the fistula needle intervention |
10. Side Effects of Non-Pharmacological Interventions
Before implementing NPIs for pain management in hemodialysis, clinicians must evaluate each patient’s unique requirements and preferences. Monitoring for adverse side effects and promptly addressing them can contribute to the safety and efficacy of these interventions. We have summarized the more frequent side effects reported in the literature in Table 2.
Table 2.
The side effects of non-pharmacological interventions.
| No. | Non-Pharmacological Intervention | Reported Side Effects | Supporting Reference: 1st Author Name and Year |
|---|---|---|---|
| 1 | Acupuncture | Usually safe, but it can have mild side effects like bruises, bleeding, or pain where the needles were put in. Rarely, more major side effects like infections or organ damage can happen if you do not follow the right hygiene and approach. | |
| 2 | Cognitive behavioral treatment | It is safe and well tolerated by most people and has few bad effects. Some people may feel temporary pain or mental distress during treatment meetings as they face and deal with problems linked to their pain. |
|
| 3 | Relaxation techniques | These are generally safe and have no major side effects. But, some people may find it hard to fully relax or get frustrated if they do not reach the level of relaxation they aim for. | |
| 4 | Virtual reality | It is usually safe to use, but patients with motion sickness may feel dizzy or sick because of the way the virtual world moves. |
11. Study Limitations, Future Perspectives, and Further Research
Non-pharmacological interventions (NPIs) have gained popularity as an alternative or supplement to pharmacological treatments in recent years. While various studies have been conducted to investigate their usefulness, there are still significant gaps and deficiencies requiring further study.
While this review endeavored to offer an exhaustive overview of NPIs in the context of hemodialysis patients, it does come with certain constraints. Notably, individuals undergoing peritoneal dialysis were not encompassed in our analysis, marking a significant limitation. Additionally, the distinction between inpatient and outpatient status of the patients was not considered. Recognizing that the requirements and treatment modalities for hospitalized patients can substantially diverge from those receiving outpatient care presents another limitation of our study.
Much of the research has focused on the efficacy of specific NPIs; however, comparative studies that directly compare different treatments are needed to find the most effective pain management technique. The majority of NPI research focuses on short-term results. Future studies should focus on the long-term impacts to establish their viability and capacity to give long-term pain relief. Understanding the underlying processes through which NPIs relieve pain in hemodialysis patients is critical. Research should be conducted to understand better the physiological and psychological mechanisms of how NIP works to increase their efficiency [83]. When using NPIs in pain treatment, it is critical to consider patient preferences to ensure that they are acceptable and realistic in real-world situations. Since hemodialysis patients suffer discomfort from various underlying diseases, such as neuropathy or musculoskeletal difficulties, tailoring therapies should be considered [84,85]. More research has to look at whether adapting non-pharmacological therapies to specific patient characteristics improves pain management results. Another aspect to consider in NPIs is cost-effectiveness analysis, as some interventions endure upfront expenditures like training employees or acquiring equipment. Cost-effectiveness assessments can assist in establishing if these therapies are economically feasible in the long run when compared to pharmaceutical treatments [86]. The potential effects of combining NPIs are also worth exploring; future research in that area is warranted.
Finally, once the usefulness of NPIs has been shown, projects should concentrate on creating ways to incorporate them into routine clinical practice. Identifying challenges and facilitators, as well as defining criteria or protocols, can assist assure widespread acceptance and sustainability.
There is a lack of studies addressing the efficacy of analgesic medicine or comparisons between non-pharmacological interventions and an analgesic regimen. The current evidence regarding the efficacy and safety of NPIs seems promising; they are recommended and should always be available to hemodialysis patients. However, owing to the complexity of pain and the associated medical co-morbidities that most hemodialysis patients have, there is an urge for a cautious approach to managing pain.
12. Conclusions
In conclusion, a comprehensive review of the diverse NPIs for hemodialysis patients was performed. Preliminary data suggest the potential utility of these NPIs in mitigating pain and augmenting the QOL in this specific group of patients. However, a crucial need exists for high-quality research to validate their effectiveness, delineate optimal implementation methodologies, and investigate innovative approaches to enhance their reach and effectiveness.
It is essential to address the identified gaps in current knowledge. Progression in the domain of pain management for hemodialysis patients could potentially be driven by implementing comparative studies, analyzing long-term outcomes, and gaining insight into the precise mechanisms through which NPIs exert their effects. It is also important to consider patient preferences, evaluate cost-effectiveness, individualize interventions, and develop effective strategies for implementation. In the final analysis, a holistic, patient-centered approach to pain management, incorporating a variety of these NPIs, might be instrumental in addressing the unique needs of patients undergoing hemodialysis. This comprehensive strategy could lead to enhanced patient outcomes and improvement in the overall quality of healthcare provided to this specific patient group.
Author Contributions
A.C.P., W.N., L.A.T., A.L.B., C.M.M., L.M., C.E.F., V.V.L., A.L., A.A., A.M.I., R.M.L., I.I., E.C., S.I.C. and T.C. contributed equally with M.A.K.K. to this article. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were generated.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This research received no external funding.
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Davison S.N. Pain in hemodialysis patients: Prevalence, cause, severity, and management. Am. J. Kidney Dis. 2003;42:1239–1247. doi: 10.1053/j.ajkd.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 2.Thurlow J.S., Joshi M., Yan G., Norris K.C., Agodoa L.Y., Yuan C.M., Nee R. Global Epidemiology of End-Stage Kidney Disease and Disparities in Kidney Replacement Therapy. Am. J. Nephrol. 2021;52:98–107. doi: 10.1159/000514550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kafkia T., Chamney M., Drinkwater A., Pegoraro M., Sedgewick J. Pain in Chronic Kidney Disease: Prevalence, Cause and Management. J. Ren. Care. 2011;37:114–122. doi: 10.1111/j.1755-6686.2011.00234.x. [DOI] [PubMed] [Google Scholar]
- 4.dos Santos P.R., Mendonça C.R., Noll M., Borges C.C., Alves P.M., Dias N.T., Romeiro A.M.d.S., Barbosa M.A., Porto C.C. Pain in Hemodialysis Patients: Prevalence, Intensity, Location, and Functional Interference in Daily Activities. Healthcare. 2021;9:1375. doi: 10.3390/healthcare9101375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davison S.N., Jhangri G.S. Impact of Pain and Symptom Burden on the Health-Related Quality of Life of Hemodialysis Patients. J. Pain Symptom Manag. 2010;39:477–485. doi: 10.1016/j.jpainsymman.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Upadhyay C., Cameron K., Murphy L., Battistella M. Measuring pain in patients undergoing hemodialysis: A review of pain assessment tools. Clin. Kidney J. 2014;7:367–372. doi: 10.1093/ckj/sfu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kimmel P.L., Emont S.L., Newmann J.M., Danko H., Moss A.H. ESRD patient quality of life: Symptoms, spiritual beliefs, psychosocial factors, and ethnicity. Am. J. Kidney Dis. 2003;42:713–721. doi: 10.1016/S0272-6386(03)00907-7. [DOI] [PubMed] [Google Scholar]
- 8.Theofilou P. Quality of Life in Patients Undergoing Hemodialysis or Peritoneal Dialysis Treatment. J. Clin. Med. Res. 2011;3:132–138. doi: 10.4021/jocmr552w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hedayati S., Bosworth H., Kuchibhatla M., Kimmel P., Szczech L. The predictive value of self-report scales compared with physician diagnosis of depression in hemodialysis patients. Kidney Int. 2006;69:1662–1668. doi: 10.1038/sj.ki.5000308. [DOI] [PubMed] [Google Scholar]
- 10.Dowell D., Haegerich T.M., Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA. 2016;315:1624–1645. doi: 10.1001/jama.2016.1464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wilkinson J., Faleiro R. Acupuncture in pain management. Contin. Educ. Anaesth. Crit. Care Pain. 2007;7:135–138. doi: 10.1093/bjaceaccp/mkm021. [DOI] [Google Scholar]
- 12.Dhond R.P., Yeh C., Park K., Kettner N., Napadow V. Acupuncture modulates resting state connectivity in default and sensorimotor brain networks. Pain. 2008;136:407–418. doi: 10.1016/j.pain.2008.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu X., Wang X., Ma H., Zhang W. Mechanisms underlying acupuncture therapy in chronic kidney disease: A narrative overview of preclinical studies and clinical trials. Front. Nephrol. 2022;2:1006506. doi: 10.3389/fneph.2022.1006506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang M., Liu W., Ge J., Liu S. The immunomodulatory mechanisms for acupuncture practice. Front. Immunol. 2023;14:1147718. doi: 10.3389/fimmu.2023.1147718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ma Q. Somatotopic organization of autonomic reflexes by acupuncture. Curr. Opin. Neurobiol. 2022;76:102602. doi: 10.1016/j.conb.2022.102602. [DOI] [PubMed] [Google Scholar]
- 16.Kim K.H., Lee M.S., Kim T.-H., Kang J.W., Choi T.-Y., Lee J.D. Acupuncture and related interventions for symptoms of chronic kidney disease. Cochrane Database Syst. Rev. 2016;2016:CD009440. doi: 10.1002/14651858.CD009440.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Carvalho M.C., de Azevedo J.N., Azevedo P., Pires C., Laranjeira M., Machado J.P. Effect of Acupuncture on Functional Capacity in Patients Undergoing Hemodialysis: A Patient-Assessor Blinded Randomized Controlled Trial. Healthcare. 2022;10:1947. doi: 10.3390/healthcare10101947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bullen A., Awdishu L., Lester W., Moore T., Trzebinska D. Effect of Acupuncture or Massage on Health-Related Quality of Life of Hemodialysis Patients. J. Altern. Complement. Med. 2018;24:1069–1075. doi: 10.1089/acm.2018.0030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Carvalho M.C., de Azevedo J.N., Azevedo P., Pires C., Machado J.P., Laranjeira M. Effectiveness of Acupuncture on Health-Related Quality of Life in Patients Receiving Maintenance Hemodialysis. Healthcare. 2023;11:1355. doi: 10.3390/healthcare11091355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tsai L.-H., Chen C.-M., Lin L.-M., Tsai C.-C., Han Y., See L.-C. Acupressure reduces the severity of restless legs syndrome in hemodialysis patients: A cluster-randomized crossover pilot study. Biomed. J. 2022;45:533–541. doi: 10.1016/j.bj.2021.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang L., Li Y., Xiao X., Shi Y., Xu D., Li N., Deng Y. Acupuncture for Uremic Pruritus: A Systematic Review and Meta-Analysis. J. Pain Symptom Manag. 2022;65:e51–e62. doi: 10.1016/j.jpainsymman.2022.08.017. [DOI] [PubMed] [Google Scholar]
- 22.Çevik B., Taşcı S. The effect of acupressure on upper extremity pain and quality of life in patients hemodialysis treatment: A Randomized Controlled Trial. Complement. Ther. Clin. Pr. 2020;39:101128. doi: 10.1016/j.ctcp.2020.101128. [DOI] [PubMed] [Google Scholar]
- 23.Kim K., Kim T., Kang J., Lee M., Kim J., Shin M., Jung S., Kim A., Kang K., Choi S., et al. P02.176. Acupuncture for symptom management in hemodialysis patients: A prospective, observational pilot study. BMC Complement. Altern. Med. 2012;12:P232. doi: 10.1186/1472-6882-12-S1-P232. [DOI] [PubMed] [Google Scholar]
- 24.Lu P.-H., Lai C.-C., Chiu L.-Y., Wang J.-Y., Lu P.-H. Comparative efficacy of Chinese herbal medicines for dialysis patients with uremic pruritus: A systematic review and network meta-analysis. Front. Pharmacol. 2023;14:1064926. doi: 10.3389/fphar.2023.1064926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Melo G.A.A., Aguiar L.L., Silva R.A., Pereira F.G.F., da Silva F.L.B., Caetano J. Effects of acupuncture in patients with chronic kidney disease: A systematic review. Rev. Bras. Enferm. 2020;73:e20180784. doi: 10.1590/0034-7167-2018-0784. [DOI] [PubMed] [Google Scholar]
- 26.Xu M., Yang C., Nian T., Tian C., Zhou L., Wu Y., Li Y., Deng X., Li X., Yang K. Adverse effects associated with acupuncture therapies: An evidence mapping from 535 systematic reviews. Chin. Med. 2023;18:1–10. doi: 10.1186/s13020-023-00743-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zheng H., Li J., Li Y., Zhao L., Wu X., Chen J., Li X., Huang Y., Chang X., Liu M., et al. Acupuncture for patients with mild hypertension: A randomized controlled trial. J. Clin. Hypertens. 2019;21:412–420. doi: 10.1111/jch.13490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lin J.-H., Shih C.-H., Kaphle K., Wu L.-S., Tseng W.-Y., Chiu J.-H., Lee T.-C., Wu Y.-L. Acupuncture Effects on Cardiac Functions Measured by Cardiac Magnetic Resonance Imaging in a Feline Model. Evid.-Based Complement. Altern. Med. 2010;7:169–176. doi: 10.1093/ecam/nem187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ince L.P. Cognitive Therapy and the Emotional Disorders. Am. J. Psychother. 1977;31:633–634. doi: 10.1176/appi.psychotherapy.1977.31.4.633. [DOI] [Google Scholar]
- 30.Ehde D.M., Dillworth T.M., Turner J.A. Cognitive-behavioral therapy for individuals with chronic pain: Efficacy, innovations, and directions for research. Am. Psychol. 2014;69:153–166. doi: 10.1037/a0035747. [DOI] [PubMed] [Google Scholar]
- 31.Zegarow P., Manczak M., Rysz J., Olszewski R. The influence of cognitive-behavioral therapy on depression in dialysis patients—Meta-analysis. Arch. Med. Sci. 2020;16:1271–1278. doi: 10.5114/aoms.2019.88019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Valsaraj B.P., Bhat S.M., Prabhu R., Kamath A. Follow-Up Study on the Effect of Cognitive Behaviour Therapy on Haemodialysis Adherence: A randomised controlled trial. Sultan Qaboos Univ. Med. J. 2021;21:e58–e65. doi: 10.18295/squmj.2021.21.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jakubowski K.P., Jhamb M., Yabes J., Gujral S., Oberlin L.E., Bender F.H., Steel J.L. Technology-assisted cognitive-behavioral therapy intervention for end-stage renal disease. Transl. Behav. Med. 2020;10:657–663. doi: 10.1093/tbm/ibz077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sohn B.K., Oh Y.K., Choi J.-S., Song J., Lim A., Lee J.P., An J.N., Choi H.-J., Hwang J.Y., Jung H.-Y., et al. Effectiveness of group cognitive behavioral therapy with mindfulness in end-stage renal disease hemodialysis patients. Kidney Res. Clin. Pr. 2018;37:77–84. doi: 10.23876/j.krcp.2018.37.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cukor D., Halen N.V., Asher D.R., Coplan J.D., Weedon J., Wyka K.E., Saggi S.J., Kimmel P.L. Psychosocial Intervention Improves Depression, Quality of Life, and Fluid Adherence in Hemodialysis. J. Am. Soc. Nephrol. 2014;25:196–206. doi: 10.1681/ASN.2012111134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. NCT01159197. Cognitive-Behavioral Therapy for Sleep Disturbance in Patients Undergoing Hemodialysis. [(accessed on 18 July 2023)]; Available online: https://clinicaltrials.gov/show/NCT01159197.
- 37.Principles and Practice of Stress Management. 3rd ed. The Guilford Press; New York, NY, USA: 2007. [(accessed on 1 May 2023)]. Available online: https://psycnet.apa.org/record/2007-14796-000. [Google Scholar]
- 38.Whitehouse W., Orne E., Orne M. Encyclopedia of Stress. 2nd ed. Elsevier; Amsterdam, The Netherlands: 2007. Relaxation Techniques; pp. 345–350. [DOI] [Google Scholar]
- 39.Gorji M.A.H., Ardebil M.D., Mahdavi A., Gorji A.M.H., Yazdani J. Implementing benson′s relaxation training in hemodialysis patients: Changes in perceived stress, anxiety, and depression. N. Am. J. Med. Sci. 2013;5:536–540. doi: 10.4103/1947-2714.118917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Syam N.M., Desoky G.M., Ahmed H., Eldesoky M. Effects of Progressive Muscle Relaxation Technique on Severity of Restless Legs Syndrome Among Patients on Maintenance Hemodialysis. Orig. Artic. Egypt. J. Health Care. 2022;13:102–120. doi: 10.21608/ejhc.2022.249361. [DOI] [Google Scholar]
- 41.Beizaee Y., Rejeh N., Heravi-Karimooi M., Tadrisi S.D., Griffiths P., Vaismoradi M. The effect of guided imagery on anxiety, depression and vital signs in patients on hemodialysis. Complement. Ther. Clin. Pr. 2018;33:184–190. doi: 10.1016/j.ctcp.2018.10.008. [DOI] [PubMed] [Google Scholar]
- 42.Blouchi T., Kianmehr M., Tavakolizade J., Basiri-Moghadam M., Biabani F. Effect of Muscle Relaxation on Hemodialysis Patients’ Pain. Intern. Med. Today. 2015;21:75–80. doi: 10.18869/acadpub.hms.21.2.75. [DOI] [Google Scholar]
- 43.Abu Maloh H.I.A., Chong S.C., Ismail S.I.F., Soh K.G., Abu Maloh D.I., Al Yateem N., AbuRuz M.E. The Effectiveness of Benson’s Relaxation Technique on Pain and Perceived Stress Among Patients Undergoing Hemodialysis: A Double-Blind, Cluster-Randomized, Active Control Clinical Trial. Clin. Nurs. Res. 2023;32:288–297. doi: 10.1177/10547738221112759. [DOI] [PubMed] [Google Scholar]
- 44.Rambod M., Sharif F., Pourali-Mohammadi N., Pasyar N., Rafii F. Evaluation of the effect of Benson’s relaxation technique on pain and quality of life of haemodialysis patients: A randomized controlled trial. Int. J. Nurs. Stud. 2014;51:964–973. doi: 10.1016/j.ijnurstu.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 45.Heidarigorji A., Davanloo A.A. The efficacy of relaxation training on stress, anxiety, and pain perception in hemodialysis patients. Indian J. Nephrol. 2014;24:356–361. doi: 10.4103/0971-4065.132998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Serin E.K., Ovayolu N., Ovayolu Ö. The Effect of Progressive Relaxation Exercises on Pain, Fatigue, and Quality of Life in Dialysis Patients. Holist. Nurs. Pr. 2020;34:121–128. doi: 10.1097/HNP.0000000000000347. [DOI] [PubMed] [Google Scholar]
- 47.Al Hasbi H., Chayati N., Makiyah S.N.N. Progressive muscle relaxation to reduces chronic pain in hemodialysis patient. Medisains. 2020;17:62. doi: 10.30595/medisains.v17i3.5823. [DOI] [Google Scholar]
- 48.Riva G., Wiederhold B.K., Mantovani F. Neuroscience of Virtual Reality: From Virtual Exposure to Embodied Medicine. Cyberpsychol. Behav. Soc. Netw. 2019;22:82–96. doi: 10.1089/cyber.2017.29099.gri. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hoffman H.G., Chambers G.T., Meyer W.J., Arceneaux L.L., Russell W.J., Seibel E.J., Richards T.L., Sharar S.R., Patterson D.R. Virtual Reality as an Adjunctive Non-pharmacologic Analgesic for Acute Burn Pain During Medical Procedures. Ann. Behav. Med. 2011;41:183–191. doi: 10.1007/s12160-010-9248-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maddox T., Fitzpatrick T. Virtual Reality in Chronic Kidney Disease Education and Training. Nephrol. Nurs. J. 2022;49:329–381. doi: 10.37526/1526-744X.2022.49.4.329. [DOI] [PubMed] [Google Scholar]
- 51.Burrows B., Wilund K., Hernandez R. Fully immersive virtual reality for hemodialysis patients: Is it safe? Blood Purif. 2020;49:250–251. [Google Scholar]
- 52.Maynard L.G., de Menezes D.L., Lião N.S., de Jesus E.M., Andrade N.L.S., Santos J.C.D., Júnior W.M.d.S., Bastos K.d.A., Filho J.A.S.B. Effects of Exercise Training Combined with Virtual Reality in Functionality and Health-Related Quality of Life of Patients on Hemodialysis. Games Health J. 2019;8:339–348. doi: 10.1089/g4h.2018.0066. [DOI] [PubMed] [Google Scholar]
- 53.Hernandez R., Burrows B., Browning M.H., Solai K., Fast D., Litbarg N.O., Wilund K.R., Moskowitz J.T. Mindfulness-based Virtual Reality Intervention in Hemodialysis Patients: A Pilot Study on End-user Perceptions and Safety. Kidney360. 2021;2:435–444. doi: 10.34067/KID.0005522020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Meléndez-Oliva E., Sánchez-Romero E.A., Segura-Ortí E., Gil-Gómez J.-A., Soto-Goñi X.A., Poveda-Pagán E.J. Effect of a Virtual Reality Exercise on Patients Undergoing Haemodialysis: A Randomised Controlled Clinical Trial Research Protocol. Int. J. Environ. Res. Public Health. 2023;20:4116. doi: 10.3390/ijerph20054116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Omonaiye O., Smyth W., Nagle C. Impact of virtual reality interventions on haemodialysis patients: A scoping review. J. Ren. Care. 2021;47:193–207. doi: 10.1111/jorc.12362. [DOI] [PubMed] [Google Scholar]
- 56.Vance C.G.T., Dailey D.L., Chimenti R.L., Van Gorp B.J., Crofford L.J., Sluka K.A. Using TENS for Pain Control: Update on the State of the Evidence. Medicina. 2022;58:1332. doi: 10.3390/medicina58101332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Yang L.Y., Chen H.M., Su Y.C., Chin C.C. The effect of transcutaneous electrical nerve stimulation on increasing salivary flow rate in hemodialysis patients. Oral Dis. 2019;25:133–141. doi: 10.1111/odi.12948. [DOI] [PubMed] [Google Scholar]
- 58.Linnemann A., Kappert M.B., Fischer S., Doerr J.M., Strahler J., Nater U.M. The effects of music listening on pain and stress in the daily life of patients with fibromyalgia syndrome. Front. Hum. Neurosci. 2015;9:434. doi: 10.3389/fnhum.2015.00434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Thakare A., Jallapally A., Agrawal A., Salkar P. Music in Health and Diseases. IntechOpen; Rijeka, Croatia: 2022. Music Therapy and Its Role in Pain Control. [DOI] [Google Scholar]
- 60.Ginsberg J.P., Raghunathan K., Bassi G., Ulloa L. Review of Perioperative Music Medicine: Mechanisms of Pain and Stress Reduction Around Surgery. Front. Med. 2022;9:821022. doi: 10.3389/fmed.2022.821022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Colebaugh C.A., Wilson J.M., Flowers K.M., Overstreet D., Wang D., Edwards R.R., Chai P.R., Schreiber K.L. The Impact of Varied Music Applications on Pain Perception and Situational Pain Catastrophizing. J. Pain. 2023;24:1181–1192. doi: 10.1016/j.jpain.2023.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Chai P.R., Gale J.Y., Patton M.E., Schwartz E., Jambaulikar G.D., Taylor S.W., Edwards R.R., Boyer E.W., Schreiber K.L. The Impact of Music on Nociceptive Processing. Pain Med. 2020;21:3047–3054. doi: 10.1093/pm/pnaa070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kim S., Jeong H. Effects of Patient-Selected Music Listening on the Pain and Anxiety of Patients Undergoing Hemodialysis: A Randomized Controlled Trial. Healthcare. 2021;9:1437. doi: 10.3390/healthcare9111437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hagemann P.M.S., Martin L.C., Neme C.M.B. The effect of music therapy on hemodialysis patients’ quality of life and depression symptoms. Braz. J. Nephrol. 2019;41:74–82. doi: 10.1590/2175-8239-jbn-2018-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Farrar A.J., Farrar F.C. Clinical Aromatherapy. Nurs. Clin. N. Am. 2020;55:489–504. doi: 10.1016/j.cnur.2020.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jankowska M., Rogalska J., Wyszkowska J., Stankiewicz M. Molecular Targets for Components of Essential Oils in the Insect Nervous System—A Review. Molecules. 2018;23:34. doi: 10.3390/molecules23010034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fung T.K.H., Lau B.W.M., Ngai S.P.C., Tsang H.W.H. Therapeutic Effect and Mechanisms of Essential Oils in Mood Disorders: Interaction between the Nervous and Respiratory Systems. Int. J. Mol. Sci. 2021;22:4844. doi: 10.3390/ijms22094844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Agarwal P., Sebghatollahi Z., Kamal M., Dhyani A., Shrivastava A., Singh K.K., Sinha M., Mahato N., Mishra A.K., Baek K.-H. Citrus Essential Oils in Aromatherapy: Therapeutic Effects and Mechanisms. Antioxidants. 2022;11:2374. doi: 10.3390/antiox11122374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Reyes M.C.G.M., Ribay K.G.L., Paragas E.D. Effects of sweet orange aromatherapy on pain and anxiety during needle insertion among patients undergoing hemodialysis: A quasi-experimental study. Nurs. Forum. 2020;55:425–432. doi: 10.1111/nuf.12447. [DOI] [PubMed] [Google Scholar]
- 70.Mo P.K.H., Wong E.L.Y., Yeung N.C.Y., Wong S.Y.S., Chung R.Y., Tong A.C.Y., Ko C.C.Y., Li J., Yeoh E.-K. Differential associations among social support, health promoting behaviors, health-related quality of life and subjective well-being in older and younger persons: A structural equation modelling approach. Health Qual. Life Outcomes. 2022;20:38. doi: 10.1186/s12955-022-01931-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cheng J., Zhang H., Bao H., Hong H. Music-based interventions for pain relief in patients undergoing hemodialysis: A PRISMA-compliant systematic review and meta-analysis. Medicine. 2021;100:e24102. doi: 10.1097/MD.0000000000024102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Yıldız A., Şahan S. Effect of aromatherapy on the pain of arteriovenous fistula puncture in patients on hemodialysis: A systematic review. J. Health Res. 2021;36:1187–1197. doi: 10.1108/JHR-05-2021-0280. [DOI] [Google Scholar]
- 73.Nielsen A., Dusek J.A., Taylor-Swanson L., Tick H. Acupuncture Therapy as an Evidence-Based Nonpharmacologic Strategy for Comprehensive Acute Pain Care: The Academic Consortium Pain Task Force White Paper Update. Pain Med. 2022;23:1582–1612. doi: 10.1093/pm/pnac056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Dusek J.A., Kallenberg G.A., Hughes R.M.D., Storrow A.B., Coyne C.J., Vago D.R., Nielsen A., Karasz A., Kim R.S., Surdam J., et al. Acupuncture in the emergency department for pain management: A BraveNet multi-center feasibility study. Medicine. 2022;101:e28961. doi: 10.1097/MD.0000000000028961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nees T.A., Riewe E., Waschke D., Schiltenwolf M., Neubauer E., Wang H. Multidisciplinary Pain Management of Chronic Back Pain: Helpful Treatments from the Patients’ Perspective. J. Clin. Med. 2020;9:145. doi: 10.3390/jcm9010145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Driscoll M.A., Edwards R.R., Becker W.C., Kaptchuk T.J., Kerns R.D. Psychological Interventions for the Treatment of Chronic Pain in Adults. Psychol. Sci. Public Interest. 2021;22:52–95. doi: 10.1177/15291006211008157. [DOI] [PubMed] [Google Scholar]
- 77.Arcoraci V., Barbieri M.A., Rottura M., Nobili A., Natoli G., Argano C., Squadrito G., Squadrito F., Corrao S., on behalf of the REPOSI Investigators Kidney Disease Management in the Hospital Setting: A Focus on Inappropriate Drug Prescriptions in Older Patients. Front. Pharmacol. 2021;12:749711. doi: 10.3389/fphar.2021.749711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Kesik G., Ersoy N.A. The effect of nonpharmacologic interventions for muscle cramps and restless-leg syndrome in hemodialysis patients: A meta-analysis of randomized controlled trials. Ther. Apher. Dial. 2023;27:636–654. doi: 10.1111/1744-9987.13968. [DOI] [PubMed] [Google Scholar]
- 79.Hargrove N., El Tobgy N., Zhou O., Pinder M., Plant B., Askin N., Bieber L., Collister D., Whitlock R., Tangri N., et al. Effect of Aerobic Exercise on Dialysis-Related Symptoms in Individuals Undergoing Maintenance Hemodialysis. Clin. J. Am. Soc. Nephrol. 2021;16:560–574. doi: 10.2215/CJN.15080920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Ghanbari A., Shahrbabaki P.M., Dehghan M., Mardanparvar H., Abadi E.K.D., Emami A., Sarikhani-Khorrami E. Comparison of the Effect of Reflexology and Swedish Massage on Restless Legs Syndrome and Sleep Quality in Patients Undergoing Hemodialysis: A Randomized Clinical Trial. Int. J. Ther. Massage Bodyw. 2022;15:1–13. doi: 10.3822/ijtmb.v15i2.705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Martin J.L., Saredakis D., Hutchinson A.D., Crawford G.B., Loetscher T. Virtual Reality in Palliative Care: A Systematic Review. Healthcare. 2022;10:1222. doi: 10.3390/healthcare10071222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hsieh C.-H., Li D. Understanding how virtual reality forest experience promote physiological and psychological health for patients undergoing hemodialysis. Front. Psychiatry. 2022;13:1007396. doi: 10.3389/fpsyt.2022.1007396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gerogianni G. Factors Affecting Pain in Hemodialysis and Non-pharmacological Management. Cureus. 2023;15:e35448. doi: 10.7759/cureus.35448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Jira L., Weyessa N., Mulatu S., Alemayehu A. Knowledge and Attitude Towards Non-Pharmacological Pain Management and Associated Factors Among Nurses Working in Benishangul Gumuz Regional State Hospitals in Western Ethiopia, 2018. J. Pain Res. 2020;13:2917–2927. doi: 10.2147/JPR.S265544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Bello A.K., Okpechi I.G., Osman M.A., Cho Y., Htay H., Jha V., Wainstein M., Johnson D.W. Epidemiology of haemodialysis outcomes. Nat. Rev. Nephrol. 2022;18:378–395. doi: 10.1038/s41581-022-00542-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Andronis L., Kinghorn P., Qiao S., Whitehurst D.G.T., Durrell S., McLeod H. Cost-Effectiveness of Non-Invasive and Non-Pharmacological Interventions for Low Back Pain: A Systematic Literature Review. Appl. Health Econ. Health Policy. 2016;15:173–201. doi: 10.1007/s40258-016-0268-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated.