Abstract
Objective:
The study objective was to evaluate effects of the COVID-19 pandemic on rates of emergency department (ED) acute appendicitis presentation, management strategies, and patient outcomes.
Summary Background Data:
Acute appendicitis is the most commonly performed emergency surgery in the United States and is unlikely to improve without medical or surgical intervention. Dramatic reductions in ED visits prompted concern that individuals with serious conditions, such as acute appendicitis, were deferring treatment for fear of contracting COVID-19.
Methods:
Patients from 146 hospitals with diagnosed appendicitis and arrival between March 2016 and May 2020 were selected. Electronic medical records data were retrospectively reviewed to retrieve patient data. Daily admissions were averaged from March 2016 through May 2019 and compared with March 2020. April-specific admissions were compared across the 5-year pre-COVID-19 period to April 2020 to identify differences in volume, demographics, disease severity, and outcomes.
Results:
Appendicitis patient admissions in 2020 decreased throughout March into April, with April experiencing the fewest admissions. April 2020 experienced a substantial decrease in patients who presented with appendicitis, dropping 25.4%, from an average of 2030 patients (2016–2019) to 1516 in 2020. An even greater decrease of 33.8% was observed in pediatric patients (age <18). Overall, 77% of the 146 hospitals experienced a reduction in appendicitis admissions. There were no differences between years in percent of patients treated nonoperatively (P = 0.493) incidence of shock (P = 0.95), mortality (P = 0.24), or need for postoperative procedures (P = 0.81).
Conclusions:
Acute appendicitis presentations decreased significantly during the COVID-19 pandemic, while overall management and patient outcomes did not differ from previous years. Further research is needed focusing on putative explanations for decreased hospital presentations unrelated to COVID-19 infection and possible implications for surgical management of uncomplicated acute appendicitis.
Keywords: acute appendicitis, COVID-19, decreasing volumes, multicenter study
Mini-abstract: The COVID-19 pandemic was associated with fewer emergency department (ED) visits. Appendicitis is the most frequent general surgical condition presenting to EDs. Data analysis from a national hospital system revealed a 25.4% decrease in appendicitis admissions during April 2020 compared with previous years without significant changes in management or outcomes.
INTRODUCTION
The onset of the coronavirus disease (COVID-19) pandemic, caused by the severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) virus, has resulted in many dramatic effects on the US health care system.1 Early reports and publications noted dramatic reductions in emergency department (ED) visits and hospital admissions among non-COVID-19 related illnesses,2–5 and a significant drop in the rates of elective surgeries.4,6–8 As time passed, the number of COVID-19 infections and associated deaths increased as “shelter-in-place” requirements became nearly universal and the US declared COVID-19 a national emergency in March of 2020. Concerns began to emerge that individuals with serious conditions were deferring presentation to EDs and hospitals due to fear of contracting the virus.4,5,7
In the early phases of the pandemic, initial findings from the scientific literature reported patients with suspected appendicitis may have delayed seeking medical attention, thus presenting with advanced stages of the disease, or even dying at home.9,10 Acute appendicitis is the most commonly performed emergency surgery in the United States and is a condition unlikely to improve without medical or surgical intervention.11,12
The purpose of this study was to evaluate the effects of the COVID-19 pandemic on the rates of ED acute appendicitis presentation, management strategies, and patient outcomes. Based on the burgeoning scientific literature on this subject, expected outcomes during the COVID-19 pandemic included a decrease in acute appendicitis hospitalizations, increased presentations of advanced stages of the disease, increased complication rates, and higher rates of nonoperative management for uncomplicated acute appendicitis.
METHODS
Patients admitted to one of 155 hospitals within a large national network (HCA Healthcare) were reviewed for inclusion if they had a primary diagnosis of appendicitis [International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10 code K352-K38)] at discharge and hospital arrival between March 1, 2016, and May 31, 2020. To reduce the potential confounding rendered by the addition and removal of facilities, only patients admitted to one of the 146 network hospitals who remained members of the system for the entirety of the 5-year study were included. For inclusion, patients’ primary care team was required to be one of general surgery, medicine, pediatric, pediatric surgery, or gastroenterology. Patients were excluded if care teams included gynecology, medical oncology, and urology. Additionally, patients determined to have only undergone procedures unrelated to an appendicitis diagnosis were excluded. As the clinical management of appendicitis in adult (≥18 years) and pediatric (<18 years) patients may differ due to age-related guidelines and protocols, these groups were examined separately.
Electronic medical records extracted from a centralized electronic data warehouse were retrospectively reviewed to retrieve information concerning patient volume, demographics, current procedural terminology, and ICD-10 diagnoses and procedures, in addition to patient outcomes. Current procedural terminology and ICD-10 procedure codes were used to categorize each patient into groups according to how they were clinically managed. Categories included appendiceal surgery (laparoscopic and open appendectomy), other abdominal procedures related to appendicitis (percutaneous drain), or no surgical intervention. To examine any potential differences in severity of disease from year to year, rates of open appendectomy, percutaneous drainage, shock, mortality, and hospital length of stay (LOS) were analyzed. To describe trends in appendicitis admissions, average daily hospital admission rates were calculated for March 2016 through May 2019, and then compared with those in 2020 by plotting the average number of daily hospital admissions for 2016–2019 as compared to 2020 using a locally weighted scatter plot smoother curve. Admissions specific to the month of April, where “shelter-in-place” orders were assumed to be in full effect across the United States,13,14 were compared across the 5-year (2016–2019) pre-COVID-19 period to the 2020 COVID-19 period to identify differences in volume, demographics, severity of disease, and patient outcomes. Patient characteristics within the years evaluated were compared using univariate analyses, including Pearson χ2 for categorical variables and Wilcoxon rank-sum for continuous variables. A subgroup analysis was performed repeating all analyses for patients’ payor status, with emphasis placed on being uninsured. R software version 3.6.2 was used for all statistical analyses, and P values less than .05 were considered statistically significant. This research was determined to be exempt or excluded from Institutional Review Board oversight in accordance with current regulations and institutional policy.
RESULTS
The number of patients admitted with an appendicitis diagnosis in 2020 to the 146 hospitals decreased throughout March and into April, with April experiencing the fewest admissions (Fig. 1). There was a substantial decrease in the number of patients who presented with appendicitis in April 2020, as admissions with a diagnosis of acute appendicitis dropped 25.4%, from an average of 2030 patients (2016–2019) to 1516 in 2020 (Table 1). An even greater decrease (495/328, 33.8%) was observed in pediatric patients (age <18). Overall, 77% of the 146 hospitals experienced a reduction in appendicitis hospital admissions, with the decrease in volumes ranging from as little as 1.75% to as high as 84% in the network of facilities. Hospitals included in this analysis are described in Table 2. The majority of hospitals are located in the Southern Region (110/146), with 41 facilities located in Florida and 35 in Texas. The bed sizes of the included hospitals ranged from 28 to 996, with a median of 268.5 beds.
FIGURE 1.
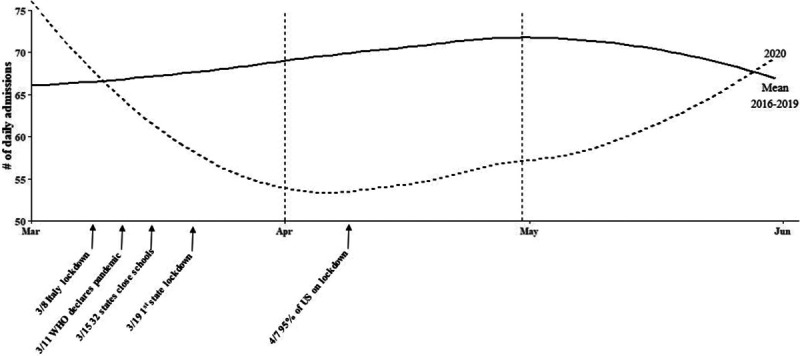
Daily number of patient arrivals with an appendicitis diagnosis within a network of 146 hospitals. WHO indicates World Health Organization.
TABLE 1.
Volume of Patient Appendicitis Admissions for April 2016–2020
| Patient Admissions | April 2016 | April 2017 | April 2018 | April 2019 | April 2020 | 2020 Percent Decrease Compared With 2016–2019 Mean (%) |
|---|---|---|---|---|---|---|
| No. Admissions | 2080 | 1973 | 2027 | 2043 | 1516 | 25.3 |
| Adults | 1549 | 1491 | 1553 | 1549 | 1188 | 22.6 |
| Pediatrics | 531 | 482 | 474 | 494 | 328 | 33.8 |
TABLE 2.
Characteristics of Hospitals by Region
| Midwest | Northeast | South | West | |
|---|---|---|---|---|
| Number of hospitals | 9 | 2 | 110 | 25 |
| Bed number Median (IQR) | 278 (99–358) | 153 (119.5–186.5) | 272.5 (171.5–383) | 265 (150–407) |
Patient demographic characteristics are described in Table 3. In April 2020, patients admitted for appendicitis were 65.8% white, 46.3% female, with a mean age of 41.6 for adults and 11.7 for pediatric patients. Patient characteristics, including age, race and gender, were found to be statistically similar to the referent April time frame of previous years (2016–2019). Patients admitted for appendicitis in April 2020 were found to have a statistically significant increase of 0.13 days in hospital LOS compared with previous years. When comparing nonoperative patients LOS in previous years to patients in 2020, no statistically significant difference was found. Appendicitis patients in 2020 were discharged home from the emergency room at a rate of 5.3% which was similar to previous years (4.5%). Reported rates of mortality and shock were found to be statistically similar across all years examined. Patients whose financial class was categorized as uninsured proved to be a small proportion of patients, making up 7.3% of all admitted patients in April 2020 (P < 0.001). The locally weighted scatter plot smoother curve visualization of daily admissions depicted a similar trend, and rates of declining volume year to year were found to be similar compared with the insured group of previous years (46.1% decrease), with similar rates of clinical management type (Fig. 1).
TABLE 3.
Patient Characteristics of Admitted Patients With Appendicitis by Year
| April 2016 (n = 2080) | April 2017 (n = 1973) | April 2018 (n = 2027) | April 2019 (n = 2043) | April 2020 (n = 1516) | P (2020 vs 2016-2019 Mean) | |
|---|---|---|---|---|---|---|
| Adult age, mean (SD), y | 41.1 (16.9) | 40.7 (16.8) | 42.0 (17.0) | 41.3 (16.8) | 41.6 (16.6) | .355 |
| Pediatric age, mean (SD), y | 11.4(3.9) | 11.3 (3.9) | 11.6 (3.9) | 11.4 (3.8) | 11.7 (4.1) | .215 |
| Race | ||||||
| White, No. (%) | 1357 (65.2) | 1297 (65.7) | 1321 (65.2) | 1339 (65.5) | 997 (65.8) | .937 |
| Black, No. (%) | 173 (8.3) | 158 (8.0) | 182 (9.0) | 149 (7.3) | 120 (7.9) | |
| Asian, No. (%) | 50 (2.4) | 47 (2.4) | 61 (3.0) | 39 (1.9) | 34 (2.2) | |
| Other, No. (%) | 438 (21.1) | 413 (20.9) | 400 (19.7) | 438 (21.4) | 311 (20.5) | |
| Gender | ||||||
| Male, No. (%) | 1140 (54.8) | 1049 (53.2) | 1074 (53) | 1105 (54.1) | 814 (53.7) | .625 |
| Uninsured, No. (%) | 257 (12.4) | 217 (11) | 179 (8.8) | 166 (8.1) | 111 (7.3) | <.001 |
| Mortality, No. (%) | 3 (0.1) | 1 (0.1) | 3 (0.1) | 4 (0.2) | 4 (0.3) | .244 |
| Hospital LOS, mean (SD), d | 1.5 (3.4) | 1.5 (3.6) | 1.4 (2.9) | 1.3 (3.0) | 1.4 (2.5) | <.001 |
| LOS nonoperative only, mean (SD), d | 0.9 (5.6) | 0.8 (3.3) | 0.6 (2.0) | 0.6 (2.3) | 0.6 (1.8) | .152 |
| Shock, No. (%) | 15 (0.7) | 8 (0.4) | 10 (0.5) | 11 (0.5) | 8 (0.5) | .946 |
LOS indicates length of stay.
The results of adult and pediatric management patterns of appendicitis cases by year are shown in Table 4. The rates of appendiceal surgical procedures performed in April 2020 were not found to be statistically different compared with previous years in the adult (90.8% vs 91.5%, P = 0.47), or pediatric group (73.8% vs 73.1%, P = 0.795).
TABLE 4.
Adult and Pediatric Management of Appendicitis Admissions by Year
| April 2016 (n = 2080) | April 2017 (n = 1973) | April 2018 (n = 2027) | April 2019 (n = 2043) | April 2020 (n = 1516) | P (2020 vs 2016-2019 Mean) | |
|---|---|---|---|---|---|---|
| Adult Management | ||||||
| Open surgery, No. (%) | 97 (6.3) | 82 (5.5) | 65 (4.2) | 63 (4.1) | 46 (3.9) | .097 |
| Laparoscopic surgery, No. (%) | 1335 (86.2) | 1295 (86.9) | 1336 (86.0) | 1345 (86.8) | 1033 (87.0) | .655 |
| Percutaneous drainage, No. (%) | 5 (0.3) | 5 (0.3) | 5 (0.3) | 3 (0.2) | 4 (0.3) | .801 |
| Medical/other, No. (%) | 112 (7.2) | 109 (7.3) | 147 (9.5) | 138 (8.9) | 105 (8.8) | .493 |
| Mean operative time, mean (SD) | 82.0 (37.9) | 65.9 (20.3) | 76.9 (36.0) | 77.3 (34.0) | 85.3 (41.8) | <.001 |
| Pediatric Management | ||||||
| Open Surgery, No. (%) | 22 (4.1) | 25 (5.2) | 12 (2.5) | 13 (2.6) | 4 (1.2) | .023 |
| Laparoscopic Surgery, No. (%) | 374 (70.4) | 340 (70.5) | 336 (70.9) | 326 (66.0) | 238 (72.6) | .257 |
| Percutaneous Drainage, No. (%) | 3 (0.6) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | .481 |
| Medical/Other, No. (%) | 132 (24.9) | 117 (24.3) | 126 (26.6) | 155 (31.4) | 86 (26.2) | .839 |
| Mean operative time, mean (SD) | 59.3 (9.5) | 78.2 (38.9) | 72.6 (42.2) | 75.5 (80.3) | 76.7 (26.7) | .003 |
Additional markers of severity were examined year to year. Mean operative time in 2020 procedures was found to be statistically significantly longer in the adult (85.3 min vs 77.0 min) and pediatric groups (76.7 min vs 74.0 min). Rates of readmission within 30 days for procedures related to the appendix were low across all years, with 2020 having slightly more than the average found in previous years (n = 16 vs n = 9, P = 0.004). Rates of postoperative abscess or percutaneous drainage on days following appendix surgery in 2020 occurred in less than 1% of patients, and rates were not found to be statistically different compared with previous years.
DISCUSSION
This large, multistate, trend analysis of 146 hospitals in a large community-based system demonstrated a significant decrease in the number of patients presenting for evaluation and management of appendicitis, without a significant change in rates of operative intervention. The frequency of advanced disease presentation could not be directly elucidated from the data, but proxy variables did not indicate a significant rate of unexpected disease progression. This is one of the first studies to contribute to the literature an evaluation of the effects of the COVID-19 pandemic on the volume of patients presenting to the ED with a primary diagnosis of appendicitis, and their associated management strategies and patient outcomes.
The COVID-19 pandemic drastically changed the way we function as a health care system in the United States.1 A moratorium was placed on elective procedures as hospitals and lawmakers urged the public to refrain from presenting to the ED except in the case of true emergency.15 Governors in almost all 50 states instituted “shelter-in-place” orders, closing schools, businesses, places of recreation, and preventing hospital visitation.14 These measures, along with community fear of contracting COVID-19 on presenting to a hospital, likely led to a significant decline in overall ED and hospital admissions.2,10,16 Nationwide, ED volumes were reported to be down 40–50%,2 with pediatric ED visits down 60%.17 Early April 2020 brought news reports across the United States describing record decreases in ED visits for life-threatening diseases such as myocardial infarction,5,8,18 stroke,5,8,19 and appendicitis.8,20,21 Anecdotal reports by news agencies quoted what many physicians were calling a “silent sub-epidemic” of patients who required emergency care but were refusing to present to a hospital. Patients seemed to be waiting until their disease had progressed to an advanced stage before seeking care, or worse, they were dying at home.10,22 Emergency medical services reported cardiac arrests were up 113% and the out of hospital mortality rate was up 164% in April 2020, with a simultaneous overall decrease in total emergency medical services responses.23 A possible explanation for these statistics is that patients refrained from presenting to the hospital until later in the course of progression of their disease. As these data originated mostly from anecdotal media reports, there were few scientific investigations to corroborate this theory.
To examine the effect of COVID-19 on hospital admissions not related to the SARS-CoV-2 virus, the volume of ED presentations and hospital admissions for acute appendicitis were evaluated. Appendicitis was chosen because it is the most common acute surgical condition of the abdomen and its treatment is available at essentially all hospitals in the United States.24 Acute appendicitis is believed to be caused by obstruction of the appendiceal lumen, either by a fecalith or lymphoid hyperplasia, leading to eventual ischemia and bacterial overgrowth.25 The standard of care for decades has been appendectomy, with newer literature suggesting the safety of antibiotic treatment for uncomplicated acute appendicitis.26 As appendicitis is unlikely to improve without medical and/or surgical intervention, the question arises whether COVID-19 and its effects on our social norms and behaviors might impact the disease process and incidence rate of acute appendicitis.
We demonstrated a significant decrease in overall appendicitis presentations to our large community hospital network during April of the early phase of the COVID-19 pandemic. Potential explanations for this decline include: an overall decrease in incidence of appendicitis related to adjustments in social behaviors associated with COVID-19; patients utilized primary care physicians/urgent care/telehealth services to receive antibiotic therapy for presumed appendicitis; appendicitis was overtreated or overdiagnosed prior to the emergence of COVID-19 in the United States, and some patients with early uncomplicated appendicitis could have spontaneously resolved; a number of patients were dying at home from appendicitis; or patients with appendicitis were misdiagnosed with COVID-19 associated gastrointestinal symptoms. To attempt to fully answer this question was beyond the capabilities and scope of this research. Beyond seasonal variations,27,28 acute appendicitis is not thought to be affected by environmental factors, consequently, there appears to be no scientific explanation for a link between the decrease in the incidence of appendicitis and the behavioral changes associated with the COVID-19 pandemic. We did not have access to databases for telehealth, urgent care, or primary care physician services; however, we assumed patients without health insurance were less likely to utilize these services, and were more likely to use the ED, should they seek care. Our analysis showed that uninsured patients represented a small portion of the total acute appendicitis admissions (7.3%), but there was no significant difference in the decrease in ED admission volume of uninsured compared with insured patients.
There have been multiple studies documenting the safety and success of nonoperative management of uncomplicated acute appendicitis without fecalith with acute failure rates ranging from 10% to 30%.29,30 In pediatric patients, nonoperative management is even more routine.31 The American College of Surgeons released a statement early in the course of the pandemic suggesting surgeons consider nonoperative management of uncomplicated acute appendicitis to decrease the risk of viral transmission.32 This recommendation was believed to potentially prolong hospital LOS and over-utilize hospital resources and has not been widely adopted.33,34 Italian experts published a protocol recommending all uncomplicated acute appendicitis be managed nonoperatively in an outpatient setting with daily follow-up telephone calls to patients.35 This recommendation appears to have been followed in Italy with one study reporting a 40% increase in nonoperative management.36 Against this background, with patients’ fear of contracting COVID-19 in the hospital, and the knowledge that endotracheal intubation and laparoscopic surgery were high exposure risks for health care workers, we expected rates of nonoperative medical management would increase during the COVID-19 pandemic. There were also suggestions that all procedures be performed using an open technique to decrease aerosolization and exposure risk.37 This study revealed management of acute appendicitis to be significantly different in 2020 compared with prior years among pediatric appendicitis patients. This may be related to surgeons deciding that a laparoscopic operation would most expediently allow discharge to home compared with nonoperative management or open appendectomy, as a step-wise decrease in pediatric open appendectomies can be observed from 2016 to 2020.
As appendicitis is unlikely to improve without medical intervention, increases in patients presenting with advanced appendicitis with perforation, abscess, and sepsis, and worsening outcomes were expected, however, this was not observed in our results. Of the variables used to examine any potential differences in the severity of disease from year to year, hospital LOS was shown to be statistically—but not clinically—significant. Despite the slight increase in LOS, this finding was interesting, as it was expected that patient and physician fear of COVID-19 exposure would provoke a decrease in hospital LOS. In subset analysis, patients managed nonoperatively had no significant difference in LOS. Furthermore, the rates of appendicitis discharged from the ED remained unchanged. Operative times were significantly longer by 8 minutes, which is likely not clinically significant and postoperative complications including readmission or need for percutaneous drainage were very low. The rates of open appendiceal surgical procedures performed in April 2020 were found to be statistically lower compared with previous years in the pediatric group, but this may not be contingent upon the COVID-19 pandemic, as this increasing trend away from open appendectomy was noted in previous years.
Limitations
Our study has several limitations. By design, the retrospective evaluation of a large database includes its inherent limitations. Hospitals within the network are located primarily in suburban areas, which were likely less affected by COVID-19 than large urban areas, and therefore may not represent the same patterns of acute appendicitis presentations or the same hospital resource shortages seen in several large urban areas. This issue with external validity lends itself to the fact that we cannot conclude that total incidence is decreased, as access to data from nearby hospitals outside our network, where patients may have presented, was not part of this analysis. Access to primary care/urgent care/telehealth data, which could potentially explain the decrease in ED/hospital presentations, was also not available. These factors also limit the evaluation of readmissions, as patients may have presented to another facility. As the electronic database was accessed retrospectively, the stage of disease in which patients presented was unknown, thus proxy variables were utilized, which may not be sensitive or specific for disease severity.
CONCLUSION
Acute appendicitis presentations in our large hospital network decreased significantly during the COVID-19 pandemic, while the overall management of acute appendicitis and patient outcomes did not differ from previous years. Potential reasons for the decline in acute appendicitis amidst the COVID-19 pandemic may be related to changes in social behavior, access to telemedicine, or spontaneous resolution without medical intervention. Further research is needed focusing on the putative explanations for the decline in hospital presentations not directly related to COVID-19 infection and the outcomes of these patients. Continued investigation is also warranted into the role of surgical intervention for the optimal treatment for patients with presumed uncomplicated acute appendicitis.
ACKNOWLEDGMENTS
The views expressed in this publication represent those of the authors and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
Footnotes
Disclosure: The authors declare that they have nothing to disclose.
This research was supported (in whole or in part) by HCA Healthcare and an HCA Healthcare affiliated entity.
M.G.R. coordinated/oversaw research process, led all meetings and directed protocol design discussion, wrote research protocol, contributed substantially to analysis/interpretation of data, worked with senior author to delegate article work/monitor author workload, wrote multiple sections of the article, guided article section write-up/revisions, ensured article coherence, edited/revised article per journal guidelines, accepted responsibility for final article content, provided consent to publish the final document, created/maintains all required documents for IRB approval, responds to journal editors/reviewers, maintained records of project work, which can be produced at any point for at least seven years postpublication. S.M.F., J.L.M., and R.W. attended meetings and contributed to design discussion, assisted with drafting protocol, contributed substantially to analysis/interpretation of data, wrote multiple sections of the article, conducted/assisted with analyses and interpretation, ensured coherence of article, edited/revised article per journal guidelines, accepted responsibility for final article content, provided consent to publish the final document, maintains records of project work, which can be produced at any point for at least seven years postpublication. J.M.G. attended meetings and contributed to design discussion, assisted with drafting protocol, wrote multiple sections of the article, ensured coherence of article, edited/revised article per journal guidelines, accepted responsibility for final article content, provided consent to publish the final document, maintained records of project work, which can be produced at any point for at least seven years postpublication. T.M.D. attended meetings and contributed to design discussion, assisted with drafting the protocol, contributed substantially to interpretation of data, conducted/assisted with analyses and interpretation, edited/revised article per journal guidelines, accepted responsibility for final article content, provided consent to publish the final document, maintained records of project work, which can be produced at any point for at least seven years postpublication. A.S. attended meetings and contributed to design discussion, assisted with drafting the protocol, contributed substantially to analysis/interpretation of data, conducted/assisted with analyses and interpretation, edited/revised article per journal guidelines, accepted responsibility for final article content, provided consent to publish the final document, maintained records of project work, which can be produced at any point for at least seven years postpublication. N.Y.W. Nina attended meetings and contributed to design discussion, assisted with drafting the protocol, contributed substantially to interpretation of data, conducted/assisted with analyses and interpretation, ensured coherence of article, edited/revised article per journal guidelines, accepted responsibility for final article content, provided consent to publish the final document, maintained records of project work, which can be produced at any point for at least seven years post publication. D.D.W. and Y.S. attended meetings and contributed to design discussion, assisted with drafting the protocol, contributed substantially to analysis/interpretation of data, conducted/assisted with analyses and interpretation, accepted responsibility for final article content, provided consent to publish the final document, maintained records of project work, which can be produced at any point for at least seven years postpublication. M.B. attended meetings and contributed to design discussion, assisted with drafting the protocol, contributed substantially to analysis/interpretation of data, mentored/ assisted other authors in their work, is the consultant to all members of the research team, worked with First Author to delegate article work/monitor author workload, ensured coherence of article, edited/revised article per journal guidelines, accepted responsibility for final article content, provided consent to publish the final document, and maintained records of project work, which can be produced at any point for at least seven years postpublication.
REFERENCES
- 1.Khusid JA, Weinstein CS, Becerra AZ, et al. Well-being and education of urology residents during the COVID-19 pandemic: results of an American National Survey. Int J Clin Pract. 2020; 74:e13559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hartnett KP, Kite-Powell A, DeVies J, et al. ; National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:699–704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prohaska TJ. Fewer patients showing up at ERs as hospitals prep for COVID-19 surge. The Buffalo News. March 27, 2020. Available at: https://buffalonews.com/news/local/fewer-patients-showing-up-at-ers-as-hospitals-prep-for-covid-19-surge/article_fb25d5db-b9e7-5f8d-b28a-6f8b175fb46c.html. Accessed July 17, 2020 [Google Scholar]
- 4.Love S. Even people without coronavirus are getting sicker right now. VICE. April 15, 2020Available at: https://www.vice.com/en_us/article/v74a54/even-people-without-coronavirus-are-getting-sicker-right-now. Accessed July 17, 2020 [Google Scholar]
- 5.Zavadsky M. Complete April data shows alarming 911 trends for EMS calls during the COVID-19 pandemic. J Emergency Services website. Updated May 5, 2020. Available at: https://www.jems.com/2020/05/05/calls-during-the-covid-19-pandemic/. Accessed July 17, 2020 [Google Scholar]
- 6.Hixenbaugh M. ‘All the hospitals are full’: In Houston, overwhelmed ICUs leave COVID-19 patients waiting in ER. NBC News. July 10, 2020Available at: https://www.nbcnews.com/news/us-news/all-hospitals-are-full-houston-overwhelmed-icus-leave-covid-19-n1233430. Accessed July 15, 2020 [Google Scholar]
- 7.Nelson J. Coronavirus sparks dramatic decline in overall ER visits, job losses for hospital workers. The Sun. April 14, 2020. Available at: https://www.sbsun.com/2020/04/14/coronavirus-sparks-dramatic-decline-in-overall-er-visits-job-losses-for-hospital-workers/. Accessed July 18, 2020 [Google Scholar]
- 8.Baum A, Schwartz MD. Admissions to veterans affairs hospitals for emergency conditions during the COVID-19 pandemic. JAMA. 2020; 324:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernstein L, Sellers F. Patients with heart attacks, strokes and even appendicitis vanish from hospitals. The Washington Post. April 19, 2020. Available at: https://www.washingtonpost.com/health/patients-with-heart-attacks-strokes-and-even-appendicitis-vanish-from-hospitals/2020/04/19/9ca3ef24-7eb4-11ea-9040-68981f488eed_story.html. Accessed July 17, 2020 [Google Scholar]
- 10.Lange SJ, Ritchey MD, Goodman AB, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January-May 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:795–800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gignoux B, Blanchet MC, Lanz T, et al. Should ambulatory appendectomy become the standard treatment for acute appendicitis? World J Emerg Surg. 2018; 13:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dixon F, Singh A. Acute appendicitis. Surgery (Oxford). 2020; 38:310–317 [Google Scholar]
- 13.Galvin G. Study: shelter-in-place orders prevented up to 370,000 coronavirus deaths. U.S. News. July 10, 2020. Available at: https://www.usnews.com/news/health-news/articles/2020-07-10/shelter-in-place-orders-prevented-up-to-370-000-coronavirus-deaths-study-says. Accessed July 18, 2020 [Google Scholar]
- 14.McGuireWoods Consulting. State governor’s “stay-at-home” and prohibition on elective procedures orders McGuireWoods. July 8, 2020. Available at: https://www.mcguirewoods.com/client-resources/Alerts/2020/7/state-governors-stay-at-home-prohibition-elective-procedures-orders. Accessed July 15, 2020 [Google Scholar]
- 15.American College of Surgeons website. COVID-19: executive orders by state on dental, medical, and surgical procedures. Updated June 8, 2020. Available at: https://www.facs.org/covid-19/legislative-regulatory/executive-orders. Accessed July 15, 2020
- 16.McFarling UL. ‘Where are all our patients?’ Covid phobia is keeping people with serious heart symptoms away from ERs. STAT News. April 23, 2020. Available at: https://www.statnews.com/2020/04/23/coronavirus-phobia-keeping-heart-patients-away-from-er/. Accessed July 17, 2020 [Google Scholar]
- 17.Westgard BC, Morgan MW, Vazquez-Benitez G, et al. An analysis of changes in emergency department visits after a state declaration during the time of COVID-19. Ann Emerg Med. 2020; 76:595–601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Solomon MD, McNulty EJ, Rana JS, et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020; 383:691–693 [DOI] [PubMed] [Google Scholar]
- 19.Uchino K, Kolikonda MK, Brown D, et al. Decline in stroke presentations during COVID-19 surge. Stroke. 2020; 51:2544–2547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Snapiri O, Rosenberg Danziger C, Krause I, et al. Delayed diagnosis of paediatric appendicitis during the COVID-19 pandemic. Acta Paediatr. 2020; 109:1672–1676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tankel J, Keinan A, Blich O, et al. The decreasing incidence of acute appendicitis during COVID-19: a Retrospective Multi-centre Study. World J Surg. 2020; 44:2458–2463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Baldas T. ER visits plummet amid pandemic: ‘more people are dying at home’. Detroit Free Press. May 5, 2020. Available at: https://www.freep.com/story/news/local/michigan/2020/05/05/er-visits-plummet-amid-pandemic-we-know-more-people-dying-home/3067993001/. Accessed July 15, 2020 [Google Scholar]
- 23.MedStar Mobile Healthcare. Alarming 9-1-1 trends for EMS calls during the COVID pandemic. MedStar Mobile Healthcare. May 5, 2020. Available at: https://www.medstar911.org/2020/05/05/alarming-9-1-1-trends-for-ems-calls-during-the-covid-19-pandemic/. Accessed July 18, 2020 [Google Scholar]
- 24.Pisano M, Capponi MG,, Ansaloni L. Kon K, Rai M, eds. Acute appendicitis: an open issue. Current Trends in Diagnostic and Therapeutic Options. Microbiology for Surgical Infections. 2014, Amsterdam Academic Press: 97–110 [Google Scholar]
- 25.Lamps LW. Appendicitis and infections of the appendix. Semin Diagn Pathol. 2004; 21:86–97 [DOI] [PubMed] [Google Scholar]
- 26.Salminen P, Paajanen H, Rautio T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015; 313:2340–2348 [DOI] [PubMed] [Google Scholar]
- 27.Zangbar B, Rhee P, Pandit V, et al. Seasonal variation in emergency general surgery. Ann Surg. 2016; 263:76–81 [DOI] [PubMed] [Google Scholar]
- 28.Fares A. Summer appendicitis. Ann Med Health Sci Res. 2014; 4:18–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Minneci PC, Sulkowski JP, Nacion KM, et al. Feasibility of a nonoperative management strategy for uncomplicated acute appendicitis in children. J Am Coll Surg. 2014; 219:272–279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smink D, Soybel DI. Post TW. Management of acute appendicitis in adults. UpToDate [database online]. 2004, Wolters Kluwer. Available at: http://www.uptodate.com. Updated April 17, 2020. Accessed July 17, 2020 [Google Scholar]
- 31.Gorter RR, van der Lee JH, Cense HA, et al. ; APAC Study Group. Initial antibiotic treatment for acute simple appendicitis in children is safe: short-term results from a multicenter, prospective cohort study. Surgery. 2015; 157:916–923 [DOI] [PubMed] [Google Scholar]
- 32.American College of Surgeons website. COVID-19 Guidelines for Triage of Emergency General Surgery Patients. Updated March 25, 2020. Available at: https://www.facs.org/covid-19/clinical-guidance/elective-case/emergency-surgery. Accessed July 17, 2020
- 33.Stahel PF. How to risk-stratify elective surgery during the Covid-19 pandemic? Patient Saf Surg. 2020; 14:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shabbir A, Menon RK, Somani J, et al. ELSA recommendations for minimally invasive surgery during a community spread pandemic: a centered approach in Asia from widespread to recovery phases. Surg Endosc. 2020; 34:3292–3297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Di Saverio S, Khan M, Pata F, et al. Laparoscopy at all costs? Not now during COVID-19 outbreak and not for acute care surgery and emergency colorectal surgery: a practical algorithm from a hub tertiary teaching hospital in Northern Lombardy, Italy. J Trauma Acute Care Surg. 2020; 88:715–718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fransvea P, Di Grezia M, La Greca A, et al. Are emergency surgical patients “collateral victims” of COVID-19 outbreak? Injury. 2020; 51:2330–2331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Moletta L, Pierobon ES, Capovilla G, et al. International guidelines and recommendations for surgery during Covid-19 pandemic: a systematic review. Int J Surg. 2020; 79:180–188 [DOI] [PMC free article] [PubMed] [Google Scholar]


