OBJECTIVES:
Thoracic aortic injuries from intra-aortic balloon pump (IABP) are rare, and no publications exist in the context of patients awaiting heart transplantation. We present a single-institution case series involving five patients out of 107 who sustained thoracic aortic injuries following IABP placement awaiting heart transplantation. The goal of this study is to describe the characteristics of patients, presenting symptoms, treatment and the impact of these injuries on their suitability for transplantation.
DESIGN:
Retrospective, single-institution study through chart review of five patients with known thoracic aortic injuries following IABP placement awaiting heart transplant.
SETTING:
Tertiary care academic teaching hospital with all patients requiring cardiac ICU admission.
PATIENTS:
All five patients were diagnosed with advanced heart failure awaiting heart transplantation.
INTERVENTIONS:
Each patient had an IABP placed while awaiting transplant.
MEASUREMENTS AND MAIN RESULTS:
Five patients (4.6%) out of a total of 107 supported with IABP awaiting heart transplantation were identified with thoracic aortic injury. Three underwent transplantation and subsequently received thoracic endovascular aortic repair, and they are doing well with a mean follow-up of 6 months. One patient died acutely and the other did not require intervention.
CONCLUSIONS:
IABP-related aortic injuries may be more common in patients awaiting transplantation and that endovascular therapy is a suitable treatment modality with no immediate impact on transplantation outcomes. Pooled data from multiple centers may help identify patients risk profile to potentially design an algorithm that can more quickly identify these injuries.
Keywords: aorta, heart failure, heart transplantation, intra-aortic balloon pumping, thoracic endovascular aortic repair
KEY POINTS
Question: This study addresses several clinical questions, including how common thoracic aortic injuries occur following IABP placement, the characteristics of these patients, and how their transplant suitability was impacted.
Findings: This study was a single-institution retrospective chart review of five patients who were known to have sustained a thoracic aortic injury following IABP placement while awaiting heart transplant. These five patients represent a 4.6% prevalence of injury. Three patients successfully underwent transplant and thoracic endovascular aortic repair and are doing well with mean follow-up of 6 months.
Meaning: IABP-related aortic injuries may be more common in patients awaiting transplantation and that endovascular therapy appears to be a suitable treatment modality with no immediate impact on transplant outcomes.
The intra-aortic balloon pump (IABP) is the most common mechanical circulatory support device in use, owing to its wide availability, relative ease of deployment and a lower rate of complications (1). Since the heart allocation policy changes made in 2018, the prevalence of IABP implantation, which elevates the patient’s status to two, has tripled (2). Prior to the policy change, the reported rates of vascular complications with IABP, such as limb ischemia, femoral artery pseudoaneurysm, hematoma, hemorrhage, and mesenteric ischemia, ranged from 1% to 30% (3). Injuries to the aorta such as aortic rupture, aortic dissection, pseudoaneurysm, and intramural hematoma from IABP are rare. In a series of over five hundred patients with IABP support, only two patients developed aortic dissection (4). At our institution, five patients awaiting heart transplantation supported with IABP developed an aortic injury. We describe here the characteristics of these patients, presenting symptoms, diagnosis, treatment and their ability to proceed with heart transplantation.
METHODS
This study was conducted in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975. This study was approved by the Virginia Commonwealth University Institutional Review Board (IRB) and was granted a waiver for informed consent to collect and review the data. IRB Number: HM20025328 Approved October 25, 2022, intra-aortic balloon-related vascular injury.
From June 2019 to June 2022, 107 patients supported with IABP were listed for heart transplantation. Five out of these 107 patients (4.6%) developed thoracic aortic injuries from IABP use and are the focus of this report. All patients supported with IABP were admitted to the cardiac ICU for management of cardiogenic shock refractory to medical management. Each patient had undergone a left heart catheterization prior to index hospital admission without evidence of aortic injury. A summary of the patient characteristics is provided in Table 1.
TABLE 1.
Summary of General Patient Demographic Information
| Patient Characteristic | Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 |
|---|---|---|---|---|---|
| Gender | Female | Male | Female | Female | Male |
| Age | 65 | 46 | 34 | 54 | 35 |
| Body mass index | 22 | 28 | 22 | 26 | 27 |
| Diagnosis | NICM | NICM | NICM | NICM | NICM |
| IABP insertion site | LCFA | RCFA/LAx | RCFA/LAx/LCFA | RCFA | RCFA |
| Duration of IABP support (d) | 11 | 10 | 37 | 2 | 8 |
| Presenting sign/symptom | Chest pain | Recurrent transfusion requirement | Loss of radial pulse | Chest pain | Ongoing leukocytosis |
| Complication | Type A aortic dissection | Intramural hematoma | Distal aortic arch pseudo aneurysm | Pseudoaneurysm of the proximal descending thoracic aorta with intramural hematoma | Pseudoaneurysm of transverse aorta |
| Treatment | Advance cardiac life support after pulseless electrical activity arrest; deceased | None | TEVAR—26 × 100 mm Gore cTAG graft | TEVAR (April 1, 2022)—26 × 26 × 100 mm Medtronic Valiant TEVAR | TEVAR—26 × 26 × 100 mm Gore cTAG graft |
| Transplanted | No | No (total artificial heart) | Yes | Yes | Yes |
| Condition at last follow-up | Deceased | Deceased | Alive | Alive | Alive |
cTAG = conformable thoracic aortic graft, IABP = intra-aortic balloon pump, LAx = left axillary artery, LCFA = left common femoral artery, NICM = nonischemic cardiomyopathy, RCFA = right common femoral artery, TEVAR = thoracic endovascular aortic repair.
RESULTS
The average duration of IABP for the five patients was 13.5 ± 10 days. Two patients complained of chest discomfort; a third patient had a radial pulse examination change prompting further evaluation. The remaining two patients had no specific complaints but had laboratory findings that prompted imaging. The mean duration between the initial sign or symptom to diagnosis was 1.5 days. One patient who presented acutely with chest pain suffered pericardial tamponade secondary to retrograde type A aortic dissection rupture and died. Another patient had a descending aortic intramural hematoma that was monitored and did not require any intervention. Three of the five patients had aortic pseudoaneurysms located at the distal aortic arch, the anterior surface of the aortic arch, and the proximal descending thoracic aorta. They underwent thoracic endovascular aortic repair (TEVAR) within 2 weeks of diagnosis (mean time from diagnosis to TEVAR of 10 ± 3.201 d). Three of the five patients received heart transplantation. In two of these patients, the aortic injury was identified after the transplantation. Patients who underwent heart transplantation and were treated with TEVAR are alive and doing well with a mean follow-up of 6 months.
DISCUSSION
As a result of the changes to the heart transplant allocation system many patients are supported with IABP for a longer duration awaiting heart transplantation. The average duration of IABP support in our institution for patients not listed for heart transplantation is 4.5 days, compared with 13.5 days in our study cohort. While the reported prevalence of aortic injury from IABP in the literature is very low, it may relate to the shorter duration of support. Very limited data are available on the prevalence of aortic injury in patients supported with IABP awaiting heart transplantation. We report several key findings, acknowledging the low sample size of patients. First, since not all patients supported with IABP undergo surveillance CT angiograms, the prevalence of aortic injury in the subset of patients awaiting heart transplantation is likely higher than reported here and, in the literature. Second, patients with injuries to the thoracic aorta following IABP placement are not always symptomatic. Third, more common CT scan finding in these patients with injury is pseudo aneurysm. Last, endovascular treatment is effective.
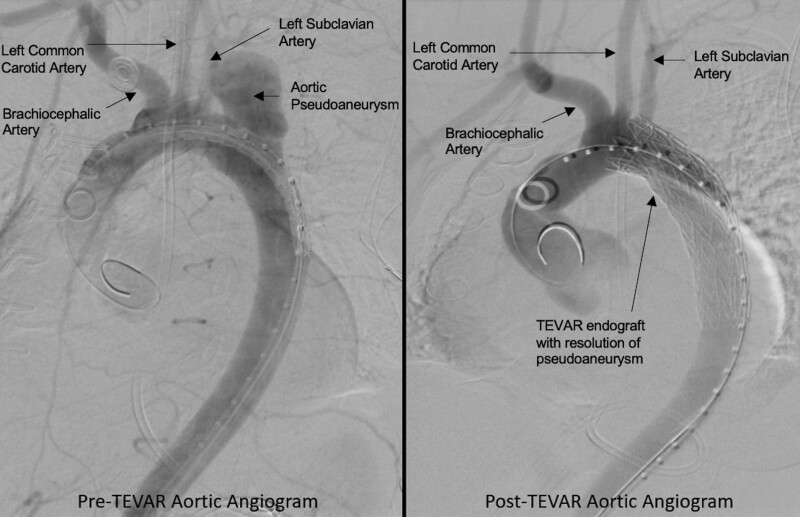
In this study, two patients had multiple IABPs placed from different sites due to position related device malfunction. Since these patients had no symptoms, it was difficult to ascertain from which access site the patient developed IABP-related injury. Three of the five patients underwent orthotopic heart transplantation. In one patient, the injury was identified the same day a heart became available for transplantation. Given the time constraints around the heart donor condition, the transplantation was done first then the TEVAR was performed. In the remaining two patients, the diagnosis was established on average 9 ± 4 days after transplantation. A follow-up CT scan in the three patients who underwent TEVAR showed resolution of the aortic injury (Fig. 1).
Figure 1.
Pre- and post-thoracic endovascular aortic repair (TEVAR) angiogram of a patient. On the left aortogram shows significant aortic arch pseudoaneurysm. The image on the right shows resolution of pseudoaneurysm following TEVAR procedure.
CONCLUSIONS
Due to the small number of patients, we could not identify a specific risk profile for the development of aortic injury. As most of these patients were asymptomatic, developing a screening tool to identify higher-risk patients who may need routine post-placement CT imaging could prove beneficial. Pooling data from multiple institutions in the future will be important to facilitate this. Ultimately, the aim will be to identify patients at higher risk for these types of injuries and have a clinical framework in place to better identify the injury, address it, and allow for safe transplantation.
Footnotes
This was an unfunded study conducted by the included authors.
The authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Ferguson JJ, Cohen M, Freedman RJ, et al. : The current practice of intra-aortic balloon counterpulsation: Results from the benchmark registry. J Am Coll Cardiol 2001; 38:1456–1462 [DOI] [PubMed] [Google Scholar]
- 2.Huckaby L, Seese LM, Mathier MA, et al. : Intra-aortic balloon pump bridging to heart transplantation: Impact of the 2018 allocation change. Circ Heart Fail 2020; 13:e006971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.de Jong MM, Lorusso R, Al Awami F, et al. : Vascular complications following intra-aortic balloon pump implantation: An updated review. Perfusion 2018; 33:96–104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arafa OE, Pedersen TH, Svennevig JL, et al. : Vascular complications of the intraaortic balloon pump in patients undergoing open heart operations: 15-year experience. Ann Thorac Surg 1999; 67:645–651 [DOI] [PubMed] [Google Scholar]
- 5.Valente S, Lazzeri C, Crudeli E, et al. : Intraaortic balloon pump: Incidence and predictors of complications in the Florence registry. Clin Cardiol 2012; 35:200–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Parissis H, Graham V, Lampridis S, et al. : IABP: History-evolution-pathophysiology-indications: What we need to know. J Cardiothorac Surg 2016; 11:122. [DOI] [PMC free article] [PubMed] [Google Scholar]