Abstract
It is well known that vascular factors and specific social determinants of health contribute to dementia risk and that the prevalence of these risk factors differs according to race and sex. In this review, we discuss the intersection of sex and race, particularly female sex and Black American race. Women, particularly Black women, have been underrepresented in Alzheimer’s disease clinical trials and research. However, in recent years, the number of women participating in clinical research has steadily increased. A greater prevalence of vascular risk factors such as hypertension and type 2 diabetes, coupled with unique social and environmental pressures, puts Black American women particularly at risk for the development of Alzheimer’s disease and related dementias. Female sex hormones and the use of hormonal birth control may offer some protective benefits, but results are mixed, and studies do not consistently report the demographics of their samples. We argue that as a research community, greater efforts should be made to not only recruit this vulnerable population, but also report the demographic makeup of samples in research to better target those at greatest risk for the disease.
Keywords: Biological sex, Dementia, Vascular, Alzheimer’s disease, Racial disparities, Ethnicity, Health disparities
Introduction
An estimated 6.2 million adults 65 years of age and older are living with Alzheimer’s disease (AD) and related dementias in the USA, and this burden is expected to more than double by 2060 [1, 2]. Increasing age is the largest risk factor for AD, and prevalence doubles every 5 years beyond the age of 65. Many studies have thoroughly reported on the increased prevalence of dementia in both Black Americans [3, 4] and women [5, 6]. About two-thirds of persons living with AD are women, and Black American adults are thought to have the highest risk of AD, with a 64% higher risk than non-Hispanic White adults (NHW) [2, 5]. Among people ages 65 and older, the African and Black American population, hereafter referred to as Black Americans, has the highest prevalence of AD and related dementias (13.8%), while the prevalence among NHW individuals is 10.3% [7–9]. That more women than men develop AD is primarily attributed to the fact that, on average, women live longer than men [10]. However, the extent to which sex differences in AD are solely due to the larger number of women or if other contributing factors are present is yet to be resolved, and findings related to this issue are mixed.
Before we begin a discussion of these factors, it is important that we define the terms we use in this review regarding sex and race. The term we use here refers to biological sex, and this review particularly covers the overlap between Black American race and female sex. Recently, scientists have called into question the use of the word “race” in scientific research, as the categories themselves are ill-defined with little genetic or cultural validity [11]. However, current use of census racial categories in the USA does have some utility in determining dementia risk, as individuals who self-report as Black American have an increased risk of developing AD compared to those who self-report as NHW [9]. In medical literature, race typically describes those who share phenotypic features and/or ancestral backgrounds. Race has a loose genetic interpretation, and the self-reported term we use here is more accurately described as an ethno-racial identity. The scope of this review is to outline the overlap of sex and race and how these factors may influence and interact with one another to generate the health disparities we see in this population.
Inclusion of Women and Black Americans in Research and Clinical Trials
Women and Black Americans have historically been underrepresented in clinical trials and other research studies in the field of AD. While AD risk factors, biomarkers, and clinical factors have been reported by sex in numerous studies, sex as a biological variable and differing effects by sex in randomized clinical trials (RCTs) are not well reported. While women have been included in clinical trials and psychosocial interventions, the rates of enrollment for women are significantly lower than the proportion of women living with AD [12, 13]. A systematic review of 56 RCTs found that 59% of participants were women, and women made up 58% of participants in RCT testing experimental drugs, even though women make up approximately 75% of the diagnosed AD population [5, 7]. These findings are similar to RCTs in other conditions that disproportionately affect females, such as stroke [14]. A study examining the role of sex in 9593 individuals (69% women) diagnosed with AD or mild cognitive impairment who screened for enrollment in an AD RCT found that men had significantly higher odds of meeting eligible criteria overall (OR = 1.26) and across several factors, including age (OR = 1.22), education (OR = 2.25), and medications (OR = 1.19) [12]. Men were more likely to be excluded based on comorbidities (OR = 0.86). To our knowledge, no meta-analysis or systematic reviews have reported the participation of women in observational aging or dementia studies. These figures would allow us to identify whether it is general research participation or specifically participation in RCTs that show these recruitment disparities.
Sex-stratified results in AD clinical trials and other research are not well reported in the literature. A systematic review of RCTs using established AD treatments found that of the 48 studies comprising 20,688 participants with AD, none reported data analyzed by sex and/or gender [15]. Of these studies, two studies published post hoc secondary analyses accounting for sex. These findings are surprising considering previous animal model studies demonstrating sex differences in the response to cholinesterase inhibitors and older clinical studies reporting differences in treatment effects based on APOE ε4genotype and sex interactions [16–18]. A study analyzing sex differences in psychosocial intervention studies found that only 62% of the 73 studies analyzed reported gender by group and women were underrepresented in the control groups [19]. Analyses by group were reported in 19% of the studies; however, significant differences by gender were found only among the studies (8%) with adequate representation of women based on prevalence [19]. In 2016, NIH issued a call to action for increased reporting and analysis of sex as a biological variable (SABV), and since this time, the analysis of SABV has increased [20]. Our hope is that these continued efforts will increase the recruitment and participation of women. It may be prudent for journals to require a statement about the analysis of SABV, where relevant, like the required data-sharing statements for most publications.
Many RCTs and observational studies of aging use cognition as a primary outcome measure [21]. Men and women have different cognitive advantages; men are typically better at motor and visuospatial tasks, while women perform better on verbal memory tasks [22, 23]. We must ensure that the cognitive tests we use as outcome measures are either broad enough to analyze and capture sex differences or tailor measures in cognitive batteries to the sex of participants.
Black Americans are enrolled in AD RCTs and other research at a lower rate, despite having the highest risk for the development of AD. We do indeed acknowledge the role that discrimination, particularly systemic racism, plays in the development of these risk factors and the role that mistrust of the scientific community plays in lower recruitment rates of minority populations [24–26]. A meta-analysis of 18 studies consisting of 5164 participants from the Alzheimer’s Disease Cooperative Study and the Alzheimer’s Disease Neuroimaging Initiative found that Black Americans made up 7% of participants diagnosed with AD, 4% of participants with mild cognitive impairment, and 11% of cognitively unimpaired controls [27]. Proposed factors contributing to the lack of diversity in AD clinical research include screening criteria, barriers to accessing expert care and diagnoses, logistical barriers to participation, lower motivation and interest, and a lack of trust [24, 28]. A study of six AD RCTs found that Black Americans had higher rates of screen failure for meeting cognitive criteria as compared to NHW individuals (30.7% vs. 16.2%, respectively; OR = 0.43). Analysis of 2716 individuals screened for elevated amyloid with neuroimaging found that Black Americans were more likely to be excluded than NHW individuals (OR = 0.59) [29]. A study of 5700 BA and 31,225 NHW participants across 39 Alzheimer’s Disease Research Centers in the National Alzheimer’s Coordinating Center (NACC) database found that, at baseline, Black American participants were less likely to be diagnosed with AD (27% vs. 36%, respectively) and were 35% less likely to be diagnosed with AD and related dementias than NHW participants [30]. Despite lower rates of AD diagnosis, Black American participants had more AD risk factors for the disease, greater cognitive impairment, and greater symptom severity than NHW participants. A meta-analysis found a higher prevalence of cardiovascular disorders (OR = 2.10), a significant AD risk factor, but lower rates of other disorders [27]. Analysis of pooled participants from the NACC database showed that Black Americans living with AD and other dementias have more cognitive deficits, neuropsychiatric symptoms, and functional dependence as compared to NHW participants. This study further demonstrated that there was a higher rate of dropouts among Black American participants as compared to NHW individuals (OR 1.60) [27].
Eligibility criteria in many random control trials disproportionately exclude Black Americans. Franzen et al. [31] looked at 101 drug trials targeting Aβ42 and neurofibrillary tangles and quantified the frequency of eligibility criteria related to medical conditions. Among those that could affect Black American enrollment included cardiovascular disease (71.3%), cerebrovascular disease (68.3%), cerebrovascular evidence on MRI (47.5%), and alcohol or drug abuse (58.4%). Rising evidence shows that not only do these conditions disproportionately affect Black Americans [24, 25] but they may also play a role, or have synergistic effects, in AD pathogenesis in racially diverse groups. Franzen et al. showed a large frequency of exclusionary eligibility criteria related to study procedures. These criteria and their frequency in drug trials are caregiver attendance (80.2%), caregiver consent (27.7%), language ability (34.7%), and education requirement (18.8%) [31, 32]. Furthermore, Black Americans tend to perform better on certain cognitive tasks and worse on others compared to NHW individuals. Culture has a well-documented effect on neuropsychological test performance [33, 34], and cognitively unimpaired Black Americans tend to score worse on neuropsychological tests than their NHW counterparts [35–37]. There has been a recent push for the development of culturally specific neuropsychological norms and tests that are more culturally specific and therefore more accurate [38, 39]. The Mini-Mental State Exam and the Montreal Cognitive Assessment are the most widely used tests of cognitive function both in the clinic and in Alzheimer’s research [40–42]. However, both of these tests show disparities in diagnostic accuracy across sex and race such that females typically score higher on the MoCA, and Black Americans typically score lower than what their current level of daily impairment would suggest [43–46]. New ethno-racial-specific norms for Black Americans and alternative cognitive tests such as the Fuld Object Memory test may yield less false-positive MCI and dementia diagnoses [47–49]. If we are to develop effective interventions in this critically at-risk population, it is imperative that we develop cognitive batteries and assessments that accurately capture baseline cognitive functioning and track response to potential interventions.
A study examining sources of recruitment and screen failures for an RCT in a diverse group (N = 5945) of older adults with pre-clinical AD found differences in recruitment sources, demographics, study partners, and study criteria [50]. Black American participants were more likely to be recruited internally at the primary study site as compared to NHW participants (69% vs. 43%, respectively), while external recruitment efforts, such as media and trusted organizations, were a larger recruitment source for NHW participants. The proportion of women was higher among Black American participants (70%) as compared to NHW participants (59%). Study partners, an individual with whom the participant had weekly contact and could provide information on daily life and cognitive function, differed by race. NHW participants were more likely to list spouse as study partner (58%), where friend/companion (29%) and spouse (27%) were listed at similar rates in Black American populations. Black American adults were more likely to be excluded due to screen failures than NHW individuals (46% vs. 26%, respectively). Black American participants were more frequently excluded based on cognitive criteria than NHW participants (31% vs. 16%, respectively), with failures among Black Americans more likely based on Clinical Dementia Rating scores and Logical Memory II scores. Overall, Black Americans had a lower likelihood of meeting eligibility as compared to their NHW counterparts, when controlling for sex, age, and education (OR = 0.43) [50]. We acknowledge that to fully distinguish the unique contributions of the ethno-racial group from those of sex, we must increase the recruitment and participation of Black American men. Reviewing and applying the methods outlined by those who have collected data in this population will be crucial for ongoing aging research [51–53]. A literature review examining consent rates in health research studies found that racial and ethnic minoritized populations were not less willing to participate in clinical research and that disparities in research are more likely due to characteristics of individual studies, such as enrollment criteria.
Other important factors related to research participation included study site location and accessibility, caregiving responsibilities, knowledge about research participation, and travel expenses [54]. The experiences of caregivers are diverse, especially between racial groups. Compared to NHW caregivers, Black American caregivers are 69% less likely to utilize respite, are more likely to provide more than 40 h a week of care, and are more likely to be adult children of individuals with dementia with other full-time jobs, and Black male caregivers are 3.3 times more likely to experience financial burden [55–57]. These racial disparities in caregivers may contribute to the lack of Black American participation in studies with caregiver attendance and consent as eligibility criteria. Caregivers may not be able to take time out of their weeks to participate in these studies, especially if they are longitudinal and each session lasts several hours.
In 2020, the US Food and Drug Administration released guidelines to increase diversity in clinical trial participation, with the key recommendation of broadening eligibility criteria [58]. Further work is needed focusing on increasing diversity in AD research, as diverse study populations representative of clinical populations are essential components in identifying effective treatments and decreasing disease burden. Recruitment and study participation bias likely results from an interplay between convenient sampling [59], a lack of networking with diverse populations that may be less likely to seek healthcare at early stages of AD [60], and greater mistrust toward the scientific and medical community within the Black American population [61]. Promising work under the community-based participatory research framework shows that community interaction can increase research participation and increase intervention adherence [62, 63]. Despite the lack of representative participation in RCTs, there is some research that investigates sex and ethno-racial differences in AD. The studies we review in this article are a combination of research that investigates Black Americans and women and some that specifically target or include an analysis of Black American women.
Social Determinants of Health and Their Contribution to AD Risk in Black American Women
Social disparities that contribute to AD risk include poverty, educational attainment, and healthcare discrimination. Black Americans represent 13.2% of the population in the USA but make up 23.8% of individuals living in poverty [64]. Black American women are more likely to be single mothers and come from single-parent households than other races and sex combinations in the USA [65]. Single motherhood is a predictor of greater stress and puts Black American women at risk for worse cardiovascular outcomes such as stroke and obesity [66–68]. Black American women are likely to be stuck in poverty (62%) compared to black men (50%) [69], which is related to lower educational attainment [70]. Greater education levels can preserve cognitive function by compensating for memory deficits by relying on skills from other cognitive domains, otherwise known as cognitive reserve [71]. Cognitive reserve is typically lower in Black Americans and women [72–74]. Historically, women and Black Americans have had lower educational achievements due to limited access to formal education. Fortunately, there is some evidence that as women gained progressively more access to formal education during the twentieth century, the risk of dementia among women began to decrease.
However, despite educational attainment, women and Black Americans still suffer from discrimination in the workplace and in healthcare [75, 76]. A wealth of research in reproductive care and aging healthcare suggests that Black American women face a disproportionate amount of discrimination from healthcare providers [75, 77, 78]. In addition to adding to the cumulative burden of stressful life events, discrimination in healthcare is associated with poorer health outcomes including utilization of care and lower medication adherence [77, 79]. Discrimination in daily life is associated with an increase in chronic stress and accelerated markers of aging [26, 27, 80]. In a study conducted exclusively on Black American women, racial centrality, or the importance of racial identity to an individual, and emotional suppression were associated with shorter telomere length, which is typically associated with advanced cellular aging [81]. Also worth mentioning is the recent work showing that Black American women are disproportionately affected by air pollution [82], and exposure to air pollution is associated with increased inflammation and an increased risk for AD [83, 84].
A unifying factor among all of these social determinants of health is that of allostatic load in that the stressors associated with poverty and stressful life events add to an individual’s burden of chronic stressors [81, 82]. Allostatic load is typically higher in Black Americans and women and is associated with a higher risk of dementia [85–89]. The overlap of gender and racial discrimination and the lack of financial mobility out of poverty for Black American women all contribute negatively to dementia risk. Future studies investigating allostatic load and aging in this population may better identify the biological outcomes related to cumulative stress as a means of capturing the burden of intersectionality.
Vascular Risk Factors and Inflammation in Black American Women
Vascular risk factors for AD such as hypertension, coronary artery disease, type 2 diabetes, and congestive heart failure are all more prevalent in Black American women than any other race by sex category [90–93]. While others have covered these factors to a greater extent [30, 94–96], it is important to note that, given the intersection of race and sex, few of these papers consider the interaction of these factors and the impact on dementia risk. Reasons for disparities in cardiovascular risk factors in Black American women are best explained using the biopsychosocial model: sex- and hormone-related inflammatory and cardiometabolic pathways synergistically interact with the social determinants of health discussed above and psychological factors that influence behavior.
Sex differences in vascular risk factors for AD have been covered extensively [97–99], but less work specifically investigates the overlap of Black American identity and female sex. Early large-scale studies investigating cardiovascular risk factors report that young women were less likely than men to develop and die from cardiovascular conditions such as hypertension [100, 101]. However, in post-menopausal women, the prevalence and impact of cardiovascular diseases mirror that of men. Some suggest that estrogen may be a protective factor against cardiovascular disease [102, 103], which is supported by animal models [104, 105]. Further adding to the complication of understanding hormonal interactions and their effect on vascular disease, hormone replacement therapy administered to post-menopausal women has either no impact on cardiovascular risk factors [106] or is associated with a decline in cardiovascular health [107]. Recently, the “timing hypothesis” has become more widely accepted which states that the harms of hormone replacement therapy can be reduced, and benefits increased, the closer therapy is delivered to the onset of menopausal symptoms [108]. A more thorough discussion of hormone replacement therapy with specific reference to dementia risk is included below. Relatively few studies have investigated hormone replacement therapy and cardiovascular risk factors in Black American women, and those that do are over 20 years old [109, 110]. To gauge the generalizability of the timing hypothesis, more research should be conducted specifically on Black American women using hormone replacement therapy.
Increased exposure to stress and higher allostatic load in Black American females as compared to NHW females likely contribute to the observed disparities in cardiovascular risk factors. Sex differences in immunological and inflammatory responses contribute to the development of cardiometabolic disease and AD [111–113]. Women have greater pro-inflammatory responses to stressors [114] as evidenced by the greater prevalence of auto-immune diseases and type 2 diabetes in women [115]. Sex-based differences in glucocorticoid responses to stress [105] and higher pro-inflammatory cytokines in women [116] contribute to greater acute immune responses to pathogens but can lead to chronic inflammation [114]. In studies investigating insulin resistance, a component of type 2 diabetes that is a marker of chronic inflammation, insulin resistance was higher and was related to oxidative stress in Black American women [117–119]. Negative social determinants of health more prevalent in Black Americans place women from this population uniquely susceptible to the effects of chronic stress and inflammation [120]. Sustained vascular dysfunction can lead to cerebrovascular disease such as stroke or transient ischemic attacks, both of which are risk factors for AD [121, 122]. Black American women have a higher risk of stroke than other races and sex combinations, and stroke is associated with a higher risk of developing dementia in Black Americans [123, 124]. Black Americans and women have higher levels of lipoprotein (a), a robust predictor of cerebrovascular disease higher in individuals who have experienced strokes [125, 126]. Cerebrovascular lesions in the form of white matter hyperintensities (WMH) also show sex and race differences and will be covered in greater depth in the section on neuroimaging [127, 128]. Whether this increased susceptibility to AD in Black Americans and in women is due to lifestyle or purely cardiometabolic sex differences is not understood, but it is likely a combination of both.
While sociocultural and biological factors increase allostatic load and negatively impact cardiovascular health, there is room for the introduction of positive behavioral changes that can help alleviate some of this burden. A recent analysis of US Behavioral Risk Factor Surveillance Survey data found that the largest population-attributable vascular risk factors for AD were midlife obesity and physical inactivity, and these risk factors were more prevalent in Black American women than in any other race and sex combination [91]. Black American women are less likely to adhere to medication recommendations for anti-hypertensive pharmacotherapy [129]. The role of hypertension in AD risk may be obfuscated by the lack of medication-use data and understanding of whether there is an underlying mechanistic difference according to the ethno-racial group that creates an increased vulnerability in Black Americans with hypertension to dementia, or whether it is lower medication adherence that contributes to this disparity is an important topic for future research. There are other health behaviors that contribute to increased vascular health that seem to be less prevalent in the Black American community including increased physical activity and reporting adherence to a healthy diet [130, 131]. Understanding barriers to increasing these should be a key focus of future research, so we can design and implement effective, culturally relevant interventions [132]. Fortunately, researchers have begun to work with communities to gain knowledge about the cultural and lifestyle aspects that influence cardiovascular risk and introduce interventions tailored to these communities [62, 133]. Increased efforts such as these and careful attention to the needs of the communities we wish to impact should decrease these health disparities.
Hormonal Contraception, Pregnancy, and Hormone Replacement Therapy in Black Americans
Hormonal contraceptives (HCs), particularly oral contraceptives (OCs), are one of the most extensively used drugs worldwide. Approximately 400 million women around the world use OCs, which are the most prescribed medication for women between the ages of 15 and 49 [134]. However, their effect on endogenous hormones, which are highly neuroactive, can vary widely. More extensive study is needed to investigate their modulatory effects on domains of cognition.
So far, a few studies have shown conflicting results on the effects of HCs on domains such as verbal fluency, visuospatial cognition, attention, and working memory [135, 136]. It appears that more agreement is found when accounting for the androgenic formulations of the contraceptives. To our knowledge, there are no significant studies or reviews that have analyzed the long-term effects of HCs on neurodegenerative diseases. However, one study published in the Journal of Women’s Health by Egan and Gleason analyzed the long-term effects of prolonged duration contraceptive use on cognitive abilities such as memory, verbal ability, learning, and visuospatial ability and concluded that “hormonal contraceptive use may have a protective cognitive effect even years after use is discontinued” [137].
Use of HCs differs across ethno-cultural groups. The most recent report by the National Center for Health Statistics (NCHS) included data about the current contraceptive status among women in the USA. The report revealed that 65.3% of women in the USA are currently using contraception. However, it noted a significant disparity in use across racial and ethnic groups, with NHW participants driving the total value with a reported use of 69.2% and Hispanic and non-Hispanic black individuals reporting only 60.5% and 61.4% use, respectively [138]. These results are not surprising: clinical studies have reported that both awareness and use of almost all types of contraceptives are significantly higher in NHW women compared to non-White women, with an exception being injectable hormones, which are used significantly more by non-White women [139]. It has been reported that these differences can be attributed to barriers to contraceptive access, such as cost [140], health insurance status [78], pharmacy-level access [141], legislation impediment [142], and clinician bias [143]. Throughout the years, HC research has suffered from a lack of representation. Considering the discovery of how small differences can produce varying cognitive effects, grouping HC users together without considering HC formulations (androgenic vs. anti-androgenic), HC mechanisms (OCs, IUDs, implants, and vaginal rings), or even differences across individuals creates a compelling barrier for the identification of new, significant knowledge, especially since these can influence cognitive function in potentially contradictory ways. Moreover, most studies on HCs have an underrepresented subject sample or simply fail to report the demographic information of their subjects [144].
Hypertensive disorders of pregnancy (HDP) include chronic hypertension that begins before pregnancy and continues during pregnancy and pregnancy-associated hypertension that begins during or after pregnancy, such as gestational hypertension, preeclampsia, and eclampsia [145]. These disorders have an incidence rate of 16%, meaning that close to 1 in 7 pregnancies are affected, and this number has been steadily increasing since 1990 [146]. HDP impact Black American, Latino, Asian/Pacific Islander, and Native American communities at higher rates, with an incidence of almost 1 in 5 [146]. Furthermore, medications used to prevent preeclampsia may not be as effective in Black Americans compared to NHW individuals [147], and residence in the USA in particular is associated with an increased risk of preeclampsia for Black pregnant women [148].
HDP have been known to cause heart attacks, strokes, intracerebral hemorrhage, and death and are a leading cause of death in pregnant people and their fetuses [145]. HDP are far more common in Black American women than in other ethno-racial groups [78, 149, 150]. Women with preeclampsia have lower cerebrovascular resistance, reduced vasodilation when inhaling CO2, and a higher cerebral perfusion pressure at baseline, even when hypertension is treated, when compared to women without a history of hypertensive conditions during pregnancy [151, 152]. Another study also found that the brains of women who died from eclampsia, a complication of preeclampsia caused by hypertension during pregnancy, had perivascular microhemorrhages, microinfarcts, and arteriolar vasculopathy, which the authors hypothesized was due to a lack of cerebral autoregulation [153]. Finally, a recent subset of studies proposed an association between preeclampsia and subjective cognitive failure [154]. These findings paved the way for researchers to start investigating the association between HDP and disorders of cognition, specifically dementia. Several clinical studies and retrospective reviews have investigated the association between HDP and disorders of cognition and found significant conclusions. Recent findings described the potential long-term neurological consequences that disorders of high blood pressure during pregnancy can have in later life. The extracellular vesicles (EVs) of women who have experienced severe preeclampsia have a substantially greater concentration of Aβ42 compared to the extracellular vesicles of their counterparts with non-hypertensive pregnancies. The difference in blood circulating levels of Aβ42 in women with conditions of preeclampsia is also significant compared to controls [155]. Also, individuals with a history of HDP show a 38% higher white matter hyperintensity volume compared to their counterparts with non-hypertensive pregnancies. The increased presence of Aβ42 in EVs and in circulation and the findings of white matter pathology during midlife point to dementia-related brain changes and thus a higher risk of accelerated cognitive decline [156].
The conclusions drawn from these studies are definitive: individuals who experience HDP are at a higher risk of cognitive decline in later life than individuals with normotensive pregnancies. Shedding light on these findings is critical for the well-being and cognitive maintenance of both pregnant individuals and fetuses [157]. The American College of Obstetrics and Gynecology and the American College of Cardiology recently released a collective announcement in which they advised obstetrics and primary care providers to work together to identify and treat pregnant individuals at risk of short- and long-term cerebrovascular damage [158].
The transition to menopause generates many neurological changes including changes to thermoregulation, sleep, and circadian rhythms and impairment in multiple cognitive domains [159]. Hormone replacement therapy is a common treatment for symptoms associated with menopause. Multiple reviews and studies have identified that hormone replacement therapy is also associated with an increased risk of dementia [160, 161]. However, two meta-analyses did find that the window in which hormone replacement therapy was administered did have an effect on dementia risk such that hormone replacement therapy administered during the peri-menopausal stages decreased dementia risk, lending credence to the “timing hypothesis” previously discussed [163–165]. APOE ε4 status may also affect dementia risk as one study found that hormone replacement therapy was associated with less cognitive decline in APOE ε4–negative women, but not in APOE ε4–positive women [166]. In one study that investigated different cognitive domains, long-term administration of estrogen only improved performance on the word recall test and actually decreased performance on a finger-tapping task and a paragraph memory task [162].
Unfortunately, little research has been conducted specifically on Black American women investigating the use of hormone replacement therapy in this population, or its effect on dementia risk. Most studies control for the ethno-racial group instead of analyzing it as a variable of interest. Some studies have found that the use of and adherence to prescribed hormone replacement therapy is lower in Black Americans and that quality of life is lower in Black American women using hormone replacement therapy [110, 167]. Given the interaction between vascular health, dementia risk, female sex, and hormone replacement therapy, future studies should investigate the use of hormone replacement therapy specifically in Black American women.
Alzheimer’s Disease Risk Genes in Black American Women
APOE ε4, a cholesterol transporter gene, is associated with the development of Aβ42 plaques and is the most widely recognized genetic risk factor for AD [168]. Numerous sex differences have been identified in the relationships between APOE ε4 and AD biomarkers. Women APOE ε4 carriers are at a greater risk of developing AD than males [169]. Women are more likely to have increased tau with the APOE ε4 genetic variant, with some identifying that this difference does not extend itself to the presentation of tangles upon autopsy and others identifying that heterozygous APOE ε4 females have more widespread tau deposition in vivo [169–171]. APOE ε4 may also diminish the effect of physical activity on cognitive reserve in women [172]. Cognitively normal elderly female APOE ε4 carriers present with brain hypometabolism, cortical thinning, and lower DMN connectivity compared to men [173, 174]. There is less conclusive evidence according to race with some studies reporting no difference or lower AD risk according to APOE ε4 status but greater APOE ε4 allele frequency in Black Americans [169, 175, 176]. Factors associated with resilience to the effects of positive APOE ε4 status may differ across ethno-racial groups [175]. In studies examining genetic race versus ethnicity, researchers frequently make comparisons between Black Americans and the Yoruba tribe, an ethnic group located in Ibadan, Nigeria [177]. Diet and lifestyle factors between Black Americans and the Yoruba tribe are very different, but these individuals share similar genetic ancestry [178]. These similarities are a means of exploring lifestyle factors and related epigenetics while somewhat controlling for ancestry. There are differential effects of APOE ε4 on the risk for AD between the Yoruba and Black American cohorts and differential effects of sex on AD risk between the Yoruba and Black American cohorts such that in Black Americans, only one copy of the APOE ε4 allele was necessary to increase dementia risk, but two copies of the APOE ε4 were necessary to increase dementia risk in the Yoruba [177]. Sex differences in the APOE ε4 variant may potentially explain the contradictions in results across studies, as the interaction of ethno-racial identity by sex is not typically analyzed or reported in demographic tables.
While genetics seem to play a smaller role in the development of AD than social and vascular factors, other risk genes and epigenetic modifications may contribute to the development of AD in Black American women. The ABCA7 gene exhibits sex and race disparities and is related to the lipid transportation process and regulation of cholesterol in the amyloid pathway [179]. A study on older Black Americans found that ABCA7 status can diminish the neuroprotective effect of aerobic fitness on cognitive flexibility [180]. In women, particular ABCA7 single-nucleotide polymorphisms were selectively associated with cognitive decline and dyslipidemia [181, 182]. Other risk genes specific to women include are related to both tau and amyloid pathology [183]. In support of the genetic inflammatory pathways as a potential explanation for the increased risk of Alzheimer’s disease in women, the genetic architecture associated with resilience in women contained genes that are associated with reduced risk for auto-immune diseases, suggesting that auto-immune processes contribute to AD risk in women [184].
Lifestyle and cultural factors can influence gene expression and are the focus of the field of epigenetics. Epigenetics involved in immune responses in the presence of chronic inflammation lead to AD, and AD itself can have epigenetic effects that modulate CNS immune function [185, 186]. This may explain why there seems to be a viscous downward spiral in inflammatory responses and neurodegeneration in the presence of AD [185]. Black Americans have lower genetic variation and epigenetic modification of cholesterol pathways indicating greater genetic vulnerability to the effects of dyslipidemia, while other studies have found that Black Americans have no difference in epigenetic pathways related to aging [187, 188]. Aroke et al. provide a comprehensive review of epigenetic factors associated with Black American ethno-racial identity with regard to chronic pain and inflammation and conclude that glucocorticoid stress receptor genes are altered in this population and are associated with depression, childhood stress, and low socio-economic status [189]. In a recent meta-analysis, Kunkle et al. conclude that while the endpoints of AD may be similar across races (AD pathology), the loci by which these pathologies emerge may differ in Black Americans involving genes associated with lipid dysregulation, brain metabolism, and intracellular trafficking [190]. Regarding sex, studies have identified that X-chromosome-linked gene expression has been implicated in heightened and prolonged inflammatory responses, yet one study found that women have slower rates of epigenetic aging [188, 191, 192]. Because genetic studies require a great number of participants, we think it prudent to recommend that future students analyze the overlap of sex and ethno-racial identity. This will help better characterize risk genes and potentially identify unique markers of AD specific to Black Americans.
Alzheimer’s Disease Fluid Biomarker Profile of Black American Women
The use of both plasma and cerebrospinal fluid (CSF) markers including Aβ42, total tau (t-tau), phospho-tau (p-tau), and neurofilament light chain (NFL) as diagnostic biomarkers of AD is increasing [193–195]. When considered together, Aβ and p-tau in CSF have increased sensitivity and specificity for the detection of AD [196]. NFL is a non-specific measure but a sensitive measure of neurodegeneration and can be measured in both plasma and CSF [197]. Gleason et al. summarized the race-based differences in fluid biomarkers in AD and found that the consensus across multiple studies is that Black Americans exhibit lower CSF t-tau and p-tau levels than their NHW counterparts even at similar levels of cognitive impairment and that this relationship may be partially explained by APOE ε4 status [198–200]. CSF and plasma Aβ42 results are less consistent, with some identifying no difference between Black Americans and NHW individuals and others identifying lower levels of Aβ42 [201, 202]. Diagnostic models of AD that predict dementia from levels of Aβ42 seem to be more reliable than models that use t- or p-tau and NFL in Black Americans [203, 204]. The CSF biomarker differences that we observe are likely a complex interplay between environmental and genetic factors. For example, there are genetic differences in levels of triggering receptor expressed on myeloid cells 2 (TREM2), a microglia mediator protein that handles the inflammatory immune response to Aβ42, that differ across ethno-racial groups [205, 206]. As the amyloid hypothesis is brought into question, as a field, we may need to shift our focus to tau, particularly in studies of racial disparities, as this protein exhibits the most consistent differences between ethno-racial groups.
Sex differences in fluid biomarkers of AD have not been as well characterized as ethno-racial differences in the literature. Mielke has comprehensively reviewed sex differences in fluid biomarkers of AD and has generally found no differences in CSF Aβ42 between men and women [207]. However, similar levels of fluid AD biomarkers may indicate a greater risk for dementia, and women may have as much as a 20-fold increase in dementia risk compared to a threefold higher risk in men [208]. Longitudinal studies have identified that in similar concentrations of Aβ42, women experience greater hippocampal atrophy, higher p-tau levels, and worse memory performance than men [209, 210].
As previously mentioned, women have heightened inflammatory responses as confirmed by plasma markers of pro-inflammatory cytokines, particularly TNF-alpha and IL-6 [211]. Although not as widely used as specific biomarkers of AD, cytokines allow us to examine levels of inflammation and immune activation, which we know to be crucial in the development of AD and exhibit sex differences [105, 111, 212–214]. In AD, levels of the inflammatory cytokine IL-β were related to worse memory performance in women but not in men [211]. Additionally, Black American women have higher levels of circulating pro-inflammatory cytokines, and inflammatory markers are associated with psychosocial factors such as late-life dissatisfaction and perceived discrimination [215–218]. Aβ42 and tau can activate microglia and create an inflammatory response in the brain, specific pro-inflammatory cytokines can cross the blood–brain barrier, and chronic exposure to plasma cytokines can increase blood–brain barrier permeability [219, 220]. Social, lifestyle, vascular, and sex-based immune factors could embroil Black American women in a downward spiral starting with increased systemic inflammation, which can cause CNS inflammation and trigger a metabolic cascade leading to AD pathology [221, 222].
Fluid biomarkers studies are limited by smaller sample sizes than the large population-based vascular studies mentioned previously, and these studies have limited power to analyze factorial categories of race and sex combinations [223, 224]. If authors are interested in ethno-racial differences, they will often include sex as a nuisance covariate and vice versa. Because we know that Black American women are uniquely vulnerable to the development of AD, we recommend that authors analyze sex differences in fluid biomarker studies and, when possible, analyze race and sex interactions. Furthermore, we recommend that authors report the makeup of their sample broken down into factorial categories of race and sex to assist with future meta-analyses that will ultimately be necessary to further characterize this population and fill this gap in the literature.
Racial and Sex Differences in Neuroimaging Biomarkers of AD
Racial differences in neuroimaging biomarkers of AD have been identified, but MRI studies specifically in this population are limited, especially for studies investigating the role of both sex and ethno-racial group. Most of the differences have been primarily identified in white matter hyperintensities (WMHs), which makes sense, given the vascular disparities present in this population. WMHs increase the risk of developing AD, and WMH volumes are typically higher in individuals with MCI and AD [225, 226]. A recent review by Carmichael and Newton identifies several MRI-related differences between Black Americans and NHW individuals in early, middle, and late life [227]. One important finding particularly relevant to AD is that WMH, not hippocampal volumes, more accurately predicts cognition in Black Americans [228]. Sex differences in WMH have also been identified such that women typically have greater WMH than men and that vascular risk factors may predict higher WMH in women than men [127, 229, 230]. Black Americans and NHW individuals do not consistently exhibit differences in brain atrophy patterns, but some differences have been identified in functional and structural neuroimaging. Amyloid-positive Black Americans have smaller cortical thickness than NHWs in the precuneus, and in a separate study, measures are inversely correlated with AD biomarkers (tau, Aβ42, and cognition) between NHW individuals and Black Americans specifically within the precuneus [47, 231]. Despite the utility of other neuroimaging modalities in the identification and tracking of AD, there has been relatively little research regarding the role of the ethno-racial group. Understanding the intersectionality of race and gender can help further elucidate the role of WMH in cognitive decline and whether its effects are additive or independent of AD pathology and whether the protective benefit of female sex against the deleterious effects of WMHs extends to the Black American population.
Alzheimer’s Disease Pathology in Black American Women
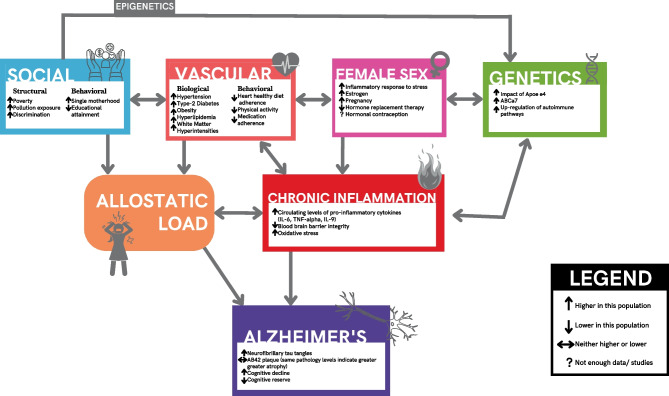
We have outlined sex and ethno-racial disparities in exposure to AD risk factors. AD pathology may differ according to sex and ethno-racial identity. Women typically have greater levels of tau pathology as measured ex vivo [232–234], in vivo using tau PET [209, 235], and in mouse models [236]. Studies investigating amyloid pathology have yielded mixed results with some reporting no difference between sexes and others reporting higher levels of Aβ42 among women [209, 237]. Despite these mixed findings in amyloid, many studies have identified a trend that similar unit increases in Aβ42 across men, and women are associated with worse clinical outcomes [209, 238, 239]. Black Americans typically do not show differences in Aβ42 pathology either in vivo or ex vivo when compared to other ethno-racial groups, but studies investigating ethno-racial differences in pathology are not as common as studies comparing sex differences, and Babulal et al. outlined this field as an area in immediate need of research attention [200, 240]. Importantly, Black Americans are more likely to have mixed pathology than NHW individuals with AD [241]. Considering that Black Americans have lower CSF tau levels, despite the increased prevalence of vascular and inflammatory risk factors, this suggests that the increase in systemic inflammation may synergistically interact with amyloid and tau to create similar clinical outcomes at lower levels of AD pathology. In their comprehensive review of pathology differences associated with female sex in Latinos and Black Americans, Royse et al. concluded that few studies include the interaction of race and sex, but those that analyze the interaction show that women have greater tau burden than men of the same race and that Black American women have increased rates of regional atrophy and worse cognition at the same levels of Aβ42 pathology [242]. We cannot overstate the importance of analyzing the interaction of the ethno-racial group and sex in AD pathology studies. If Black Americans generally have lower tau, but tau levels are increased in women compared to men, differences according to sex and the ethno-racial group will be entirely dependent on the demographic makeup of the sample. Analyzing this interaction will allow us to create generalizable diagnostic thresholds appropriate for sex and ethno-racial group (Fig. 1).
Fig. 1.
Flow diagram of mechanisms of Alzheimer’s disease risk and prevalence in Black American women
Conclusion
In this review, we outline existing research on ethno-racial and sex disparities in AD but also hope to illuminate the current gaps in the literature regarding the intersectionality of Black American identity and female sex. Social factors combined with sex-based propensities for inflammatory responses to stress that have negative cardiovascular consequences are likely the biggest contributors to AD risk in Black American women. Increased diversity in sexual and ethno-racial representation that captures this intersectionality will enable us to build models of disease and wellness that are accurate for the populations most at risk for AD. If we, as a field, hope to reduce the incidence of and develop interventions for AD, we must focus our sampling and recruitment and analysis efforts on those most impacted by the disease. Many reviews of studies on women and Black Americans call for more data collection. We wholeheartedly agree with this suggestion and are pleased that studies on minoritized populations have been made a priority by funding agencies and journals [243, 244]. While we certainly want to echo this sentiment, we also include a more nuanced list of recommendations based on the needs of this population.
Increased reporting and analysis of ethno-racial groups stratified by sex: studies should report demographic variables stratified by ethno-racial and sex categories. Even if a study is underpowered to analyze this interaction, this data will be incredibly useful for meta-analyses and studies that track the enrollment and participation of minorities in research.
Development of accurate biomarker thresholds: CSF and PET markers of amyloid and tau are now part of the standard biomarker-based definition of AD based on the NIA-AA framework, and we have discussed differences in both measures within Black Americans and women. We emphasize the need to develop both sex and ethno-racially appropriate cutoffs.
Increase in studies that investigate the heterogeneity of the Black diaspora: now that we have established that there are social, environmental, and behavioral factors that make women from minoritized populations uniquely at risk for AD, it will be increasingly important to move away from the concept of ethno-racial group to identify individual factors that lead to the “racialization” of certain groups upon which we can develop effective interventions. An individual growing up in urban areas of Chicago would certainly have different exposure, cultural, and lifestyle factors than someone who lives in rural Georgia, and there are well-established Black communities in both environments. Teasing apart exactly which variables contribute to ethno-cultural health disparities to develop appropriate interventions, rather than reinforce a biological-based racial divide, should be the goal of much of this research.
Development of culturally appropriate recruitment strategies and interventions: community-based participatory research has proven to be an effective strategy for community buy-in and adherence to interventions, particularly in Black American populations [63, 245, 246]. Culturally appropriate recruitment strategies increase participation and open a line of communication between researchers and the populations that they serve [247]. Examples include interventions and study designs that compensate for the increased caregiver burden in Black American women and limited access to transportation resources and use of less restrictive inclusion criteria so Black American women are less likely to be screened out of RCTs.
This is a short list of recommendations that we hope will increase the research representation of Black American women, who are uniquely vulnerable to the development of AD. This review brings to light significant gaps in research including the role of inflammation and exposure to negative social determinants of health on the development of dementia in Black American women, the use and role of hormone replacement therapy in peri- and post-menopausal Black American women, and the need for the validation of biomarker thresholds and cutoffs for Black American women. To reduce health disparities and develop effective interventions for AD, we must prioritize these areas of research.
Funding
This study was financially supported by the Foundation for the National Institutes of Health (5R01AG066203-04) acquired by Dr. Whitney Wharton.
Declarations
Conflict of Interest
None.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Martinkova J, Quevenco FC, Karcher H, Ferrari A, Sandset EC, Szoeke C, et al. Proportion of women and reporting of outcomes by sex in clinical trials for Alzheimer disease: a systematic review and meta-analysis. JAMA Netw Open. 2021;4(9):e2124124. doi: 10.1001/jamanetworkopen.2021.24124. [DOI] [PubMed] [Google Scholar]
- 2.2021 Alzheimer’s disease facts and figures. Alzheimer's & Dementia : The Journal of the Alzheimer's Association 2021;17(3):327–6. 10.1002/alz.12328. [DOI] [PubMed]
- 3.Barnes LL, Bennett DA. Alzheimer’s disease in African Americans: risk factors and challenges for the future. Health Aff Proj Hope. 2014;33(4):580–586. doi: 10.1377/hlthaff.2013.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brewster P, Barnes L, Haan M, Johnson JK, Manly JJ, Nápoles AM, et al. Progress and future challenges in aging and diversity research in the United States. Alzheimers Dement J Alzheimers Assoc. 2019;15(7):995–1003. doi: 10.1016/j.jalz.2018.07.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alzheimer’s Association. 2017 Alzheimer's disease facts and figures. Alzheimer's & Dementia: The Journal of the Alzheimer's Association 2017;13(4):325–3. 10.1016/j.jalz.2017.02.001. [DOI] [PubMed]
- 6.Mielke MM. Sex and gender differences in Alzheimer’s disease dementia. Psychiatr Times. 2018;35(11):14–17. [PMC free article] [PubMed] [Google Scholar]
- 7.Beam CR, Kaneshiro C, Jang JY, Reynolds CA, Pedersen NL, Gatz M. Differences between women and men in incidence rates of dementia and Alzheimer’s disease. J Alzheimers Dis. 2018;64(4):1077–1083. doi: 10.3233/JAD-180141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayeda ER, Glymour MM, Quesenberry CP, Whitmer RA. Inequalities in dementia incidence between six racial and ethnic groups over 14 years. Alzheimers Dement. 2016;12(3):216–224. doi: 10.1016/j.jalz.2015.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alzheimer’s Association. Race, ethnicity, and Alzheimer’s [Fact Sheet]. 2020; Available from: Retrieved June 17, from https://www.alz.org/news/2021/new-alzheimers-association-report-examines-racial.
- 10.Chêne G, Beiser A, Au R, Preis SR, Wolf PA, Dufouil C, et al. Gender and incidence of dementia in the Framingham Heart Study from mid-adult life. Alzheimers Dement. 2015;11(3):310–320. doi: 10.1016/j.jalz.2013.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weiner MF. Perspective on race and ethnicity in Alzheimer’s disease research. Alzheimers Dement J Alzheimers Assoc. 2008;4(4):233–238. doi: 10.1016/j.jalz.2007.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosende-Roca M, Abdelnour C, Esteban E, Tartari JP, Alarcon E, Martínez-Atienza J, et al. The role of sex and gender in the selection of Alzheimer patients for clinical trial pre-screening. Alzheimers Res Ther. 2021;13(1):95. doi: 10.1186/s13195-021-00833-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Olson NL, Albensi BC. Race- and sex-based disparities in Alzheimer’s disease clinical trial enrollment in the United States and Canada: an indigenous perspective. J Alzheimers Dis Rep. 2020;4(1):325–344. doi: 10.3233/ADR-200214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Carcel C, Woodward M, Balicki G, Koroneos GL, Sousa DA, Cordonnier C, et al. Trends in recruitment of women and reporting of sex differences in large-scale published randomized controlled trials in stroke. Int J Stroke. 2019;14(9):931–938. doi: 10.1177/1747493019851292. [DOI] [PubMed] [Google Scholar]
- 15.Canevelli M, Quarata F, Remiddi F, Lucchini F, Lacorte E, Vanacore N, et al. Sex and gender differences in the treatment of Alzheimer’s disease: a systematic review of randomized controlled trials. Pharmacol Res. 2017;115:218–223. doi: 10.1016/j.phrs.2016.11.035. [DOI] [PubMed] [Google Scholar]
- 16.Wang RH, Bejar C, Weinstock M. Gender differences in the effect of rivastigmine on brain cholinesterase activity and cognitive function in rats. Neuropharmacology. 2000;39(3):497–506. doi: 10.1016/S0028-3908(99)00157-4. [DOI] [PubMed] [Google Scholar]
- 17.Farlow MR, Lahiri DK, Poirier J, Davignon J, Schneider L, Hui SL. Treatment outcome of tacrine therapy depends on apolipoprotein genotype and gender of the subjects with Alzheimer’s disease. Neurology. 1998;50(3):669–677. doi: 10.1212/WNL.50.3.669. [DOI] [PubMed] [Google Scholar]
- 18.Haywood WM, Mukaetova-Ladinska EB. Sex influences on cholinesterase inhibitor treatment in elderly individuals with Alzheimer’s disease. Am J Geriatr Pharmacother. 2006;4(3):273–286. doi: 10.1016/j.amjopharm.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Baron S, Ulstein I, Werheid K. Psychosocial interventions in Alzheimer’s disease and amnestic mild cognitive impairment: evidence for gender bias in clinical trials. Aging Ment Health. 2015;19(4):290–305. doi: 10.1080/13607863.2014.938601. [DOI] [PubMed] [Google Scholar]
- 20.Arnegard ME, Whitten LA, Hunter C, Clayton JA. Sex as a biological variable: a 5-year progress report and call to action. J Womens Health. 2020;29(6):858–864. doi: 10.1089/jwh.2019.8247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coley N, Giulioli C, Aisen PS, Vellas B, Andrieu S. Randomised controlled trials for the prevention of cognitive decline or dementia: a systematic review. Ageing Res Rev. 2022;82:101777. doi: 10.1016/j.arr.2022.101777. [DOI] [PubMed] [Google Scholar]
- 22.Miller DI, Halpern DF. The new science of cognitive sex differences. Trends Cogn Sci. 2014;18(1):37–45. doi: 10.1016/j.tics.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 23.Upadhayay N, Guragain S. Comparison of cognitive functions between male and female medical students: a pilot study. J Clin Diagn Res JCDR. 2014;8(6):BC12–BC15. doi: 10.7860/JCDR/2014/7490.4449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Scharff DP, Mathews KJ, Jackson P, Hoffsuemmer J, Martin E, Edwards D. More than Tuskegee: understanding mistrust about research participation. J Health Care Poor Underserved. 2010;21(3):879–897. doi: 10.1353/hpu.0.0323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Greer TM, Brondolo E, Brown P. Systemic racism moderates effects of provider racial biases on adherence to hypertension treatment for African Americans. Health Psychol Off J Div Health Psychol Am Psychol Assoc. 2014;33(1):35–42. doi: 10.1037/a0032777. [DOI] [PubMed] [Google Scholar]
- 26.Yudell M, Roberts D, DeSalle R, Tishkoff S. Taking race out of human genetics. Science. 2016;351(6273):564. doi: 10.1126/science.aac4951. [DOI] [PubMed] [Google Scholar]
- 27.Kennedy RE, Cutter GR, Wang G, Schneider LS. Challenging assumptions about African American participation in Alzheimer disease trials. Am J Geriatr Psychiatry. 2017;25(10):1150–1159. doi: 10.1016/j.jagp.2017.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou Y, Elashoff D, Kremen S, Teng E, Karlawish J, Grill JD. African Americans are less likely to enroll in preclinical Alzheimer’s disease clinical trials. Alzheimers Dement N Y N. 2016;3(1):57–64. doi: 10.1016/j.trci.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Grill JD, Raman R, Ernstrom K, Aisen P, Karlawish J. Effect of study partner on the conduct of Alzheimer disease clinical trials. Neurology. 2013;80(3):282–288. doi: 10.1212/WNL.0b013e31827debfe. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lennon JC, Aita SL, Bene VAD, Rhoads T, Resch ZJ, Eloi JM, et al. Black and White individuals differ in dementia prevalence, risk factors, and symptomatic presentation. Alzheimers Dement. 2022;18(8):1461–1471. doi: 10.1002/alz.12509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franzen S, Smith JE, van den Berg E, Rivera Mindt M, van Bruchem-Visser RL, Abner EL, et al. Diversity in Alzheimer’s disease drug trials: the importance of eligibility criteria. Alzheimers Dement J Alzheimers Assoc. 2022;18(4):810–823. doi: 10.1002/alz.12433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fitzpatrick AL, Kuller LH, Ives DG, Lopez OL, Jagust W, Breitner JCS, et al. Incidence and prevalence of dementia in the Cardiovascular Health Study. J Am Geriatr Soc. 2004;52(2):195–204. doi: 10.1111/j.1532-5415.2004.52058.x. [DOI] [PubMed] [Google Scholar]
- 33.Agranovich AV, Puente AE. Do Russian and American normal adults perform similarly on neuropsychological tests?: preliminary findings on the relationship between culture and test performance. Arch Clin Neuropsychol. 2007;22(3):273–282. doi: 10.1016/j.acn.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 34.The impact of culture on neuropsychological test performance. In: International handbook of cross-cultural neuropsychology. Psychology Press; 2007.
- 35.Zsembik BA, Peek MK. Race Differences in cognitive functioning among older adults. J Gerontol Ser B. 2001;56(5):S266–S274. doi: 10.1093/geronb/56.5.S266. [DOI] [PubMed] [Google Scholar]
- 36.Werry AE, Daniel M, Bergström B. Group differences in normal neuropsychological test performance for older non-Hispanic White and Black / African American adults. Neuropsychology. 2019;33(8):1089–1100. doi: 10.1037/neu0000579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Campbell AL, Ocampo C, DeShawn RK, Lewis S, Combs S, Ford-Booker P, et al. Caveats in the neuropsychological assessment of African Americans. J Natl Med Assoc. 2002;94(7):591–601. [PMC free article] [PubMed] [Google Scholar]
- 38.Fujii D. Conducting a culturally informed neuropsychological evaluation. American Psychological Association 2017.
- 39.Barnes LL, Wilson RS, Li Y, Aggarwal NT, Gilley DW, McCann JJ, et al. Racial differences in the progression of cognitive decline in Alzheimer disease. Am J Geriatr Psychiatry [Internet]. 2005;13. Available from: 10.1097/00019442-200511000-00006. [DOI] [PubMed]
- 40.Schweizer TA, Al-Khindi T, Macdonald RL. Mini-Mental State Examination versus Montreal Cognitive Assessment: rapid assessment tools for cognitive and functional outcome after aneurysmal subarachnoid hemorrhage. J Neurol Sci. 2012;316(1):137–140. doi: 10.1016/j.jns.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Creavin ST, Wisniewski S, Noel‐Storr AH, Trevelyan CM, Hampton T, Rayment D, et al. Mini‐Mental State Examination [MMSE] for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev [Internet]. 2016 [cited 2023 Jun 5];[1]. Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011145.pub2/full. [DOI] [PMC free article] [PubMed]
- 42.Davis DH, Creavin ST, Yip JL, Noel-Storr AH, Brayne C, Cullum S. Montreal cognitive assessment for the detection of dementia. Cochrane Database Syst Rev [Internet]. 2021 [cited 2023 Jun 5];[7]. Available from: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD010775.pub3/full. [DOI] [PMC free article] [PubMed]
- 43.Engedal K, Gjøra L, Bredholt T, Thingstad P, Tangen GG, Ernstsen L, et al. Sex differences on Montreal Cognitive Assessment and Mini-Mental State Examination scores and the value of self-report of memory problems among community dwelling people 70 Years and above: The HUNT Study. Dement Geriatr Cogn Disord. 2021;50(1):74–84. doi: 10.1159/000516341. [DOI] [PubMed] [Google Scholar]
- 44.Rossetti HC, Lacritz LH, Hynan LS, Cullum CM, Van Wright A, Weiner MF. Montreal Cognitive Assessment performance among community-dwelling African Americans. Arch Clin Neuropsychol. 2017;32(2):238–244. doi: 10.1093/arclin/acw095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Espino DV, Lichtenstein MJ, Palmer RF, Hazuda HP. Ethnic differences in Mini-mental State Examination [MMSE] scores: where you live makes a difference. J Am Geriatr Soc. 2001;49(5):538–548. doi: 10.1046/j.1532-5415.2001.49111.x. [DOI] [PubMed] [Google Scholar]
- 46.Hawkins KA, Cromer JR, Piotrowski AS, Pearlson GD. Mini-Mental State Exam performance of older African Americans: effect of age, gender, education, hypertension, diabetes, and the inclusion of serial 7s subtraction versus “world” backward on score. Arch Clin Neuropsychol. 2011;26(7):645–652. doi: 10.1093/arclin/acr054. [DOI] [PubMed] [Google Scholar]
- 47.Howell JC, Watts KD, Parker MW, Wu J, Kollhoff A, Wingo TS, et al. Race modifies the relationship between cognition and Alzheimer’s disease cerebrospinal fluid biomarkers. Alzheimers Res Ther. 2017;9(1):88. doi: 10.1186/s13195-017-0315-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rideaux T, Beaudreau SA, Fernandez S, O’Hara R. Utility of the abbreviated Fuld Object Memory Evaluation and MMSE for detection of dementia and cognitive impairment not dementia in diverse ethnic groups. J Alzheimers Dis JAD. 2012;31(2):371–386. doi: 10.3233/JAD-2012-112180. [DOI] [PubMed] [Google Scholar]
- 49.Mast BT, Fitzgerald J, Steinberg J, MacNeill SE, Lichtenberg PA. Effective screening for Alzheimer’s disease among older African Americans. Clin Neuropsychol. 2001;15(2):196–202. doi: 10.1076/clin.15.2.196.1892. [DOI] [PubMed] [Google Scholar]
- 50.Raman R, Quiroz YT, Langford O, Choi J, Ritchie M, Baumgartner M, et al. Disparities by race and ethnicity among adults recruited for a preclinical Alzheimer disease trial. JAMA Netw Open. 2021;4(7):e2114364. doi: 10.1001/jamanetworkopen.2021.14364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bruce MA, Beech BM, Kermah D, Bailey S, Phillips N, Jones HP, et al. Religious service attendance and mortality among older Black men. PLoS ONE. 2022;17(9):e0273806. doi: 10.1371/journal.pone.0273806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Thorpe RJ, Whitfield KE. Advancing minority aging research. Res Aging. 2017;39(4):471–475. doi: 10.1177/0164027516672779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Forrester SN, Whitfield KE, Kiefe CI, Thorpe RJ. Navigating Black aging: the biological consequences of stress and depression. J Gerontol B Psychol Sci Soc Sci. 2022;77(11):2101–2112. doi: 10.1093/geronb/gbab224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wendler D, Kington R, Madans J, Van Wye G, Christ-Schmidt H, Pratt LA, et al. Are racial and ethnic minorities less willing to participate in health research? PLoS Med. 2006;3(2):e19–e19. doi: 10.1371/journal.pmed.0030019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Liu R, Chi I, Wu S. Caregiving burden among caregivers of people with dementia through the lens of intersectionality. Gerontologist. 2022;62(5):650–661. doi: 10.1093/geront/gnab146. [DOI] [PubMed] [Google Scholar]
- 56.Abramsohn EM, Jerome J, Paradise K, Kostas T, Spacht WA, Lindau ST. Community resource referral needs among African American dementia caregivers in an urban community: a qualitative study. BMC Geriatr. 2019;19(1):311. doi: 10.1186/s12877-019-1341-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fabius CD, Wolff JL, Kasper JD. Race differences in characteristics and experiences of Black and White caregivers of older Americans. Gerontologist. 2020;60(7):1244–1253. doi: 10.1093/geront/gnaa042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.U.S. Food and Drug Administration. Enhancing the diversity of clinical trial populations — eligibility criteria, enrollment practices, and trial designs guidance for industry. 2020.
- 59.Brodaty H, Mothakunnel A, de Vel-Palumbo M, Ames D, Ellis KA, Reppermund S, et al. Influence of population versus convenience sampling on sample characteristics in studies of cognitive aging. Ann Epidemiol. 2014;24(1):63–71. doi: 10.1016/j.annepidem.2013.10.005. [DOI] [PubMed] [Google Scholar]
- 60.Williams MM, Scharff DP, Mathews KJ, Hoffsuemmer JS, Jackson P, Morris JC, et al. Barriers and facilitators of African American participation in Alzheimer’s disease biomarker research. Alzheimer Dis Assoc Disord. 2010;24(Suppl):S24–S29. doi: 10.1097/WAD.0b013e3181f14a14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Jefferson AL, Lambe S, Cook E, Pimontel M, Palmisano J, Chaisson C. Factors associated with African-American and White elders’ participation in a brain donation program. Alzheimer Dis Assoc Disord. 2011;25(1):11–16. doi: 10.1097/WAD.0b013e3181f3e059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Wharton W, Jeong L, Ni L, Bay AA, Shin RJ, McCullough LE, et al. A pilot randomized clinical trial of adapted tango to improve cognition and psychosocial function in African American women with family history of Alzheimer’s disease [ACT trial] Cereb Circ - Cogn Behav. 2021;2:100018. doi: 10.1016/j.cccb.2021.100018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Morgan D, Crossley M, Stewart N, Kirk A, Forbes D, D’Arcy C, et al. Evolution of a community-based participatory approach in a rural and remote dementia care research program. Prog Community Health Partnersh Res Educ Action. 2014;8(3):337–345. doi: 10.1353/cpr.2014.0040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bureau UC. Inequalities persist despite decline in poverty for all major race and hispanic origin groups [Internet]. Census.gov. [cited 2023 May 31]. Available from: https://www.census.gov/library/stories/2020/09/poverty-rates-for-blacks-and-hispanics-reached-historic-lows-in-2019.html.
- 65.Bureau UC. Historical living arrangements of children [Internet]. Census.gov. [cited 2023 Jun 2]. Available from: https://www.census.gov/data/tables/time-series/demo/families/children.html.
- 66.van Hedel K, Mejía-Guevara I, Avendaño M, Sabbath EL, Berkman LF, Mackenbach JP, et al. Work-family trajectories and the higher cardiovascular risk of American women relative to women in 13 European countries. Am J Public Health. 2016;106(8):1449–1456. doi: 10.2105/AJPH.2016.303264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Young LE, Cunningham SL, Buist DSM. Lone mothers are at higher risk for cardiovascular disease compared with partnered mothers. Data from the National Health and Nutrition Examination Survey III [NHANES III] Health Care Women Int. 2005;26(7):604–621. doi: 10.1080/07399330591004845. [DOI] [PubMed] [Google Scholar]
- 68.Duriancik DM, Goff CR. Children of single-parent households are at a higher risk of obesity: a systematic review. J Child Health Care Prof Work Child Hosp Community. 2019;23(3):358–369. doi: 10.1177/1367493519852463. [DOI] [PubMed] [Google Scholar]
- 69.Winship S, Reeves RV, Guyot K. The inheritance of Black poverty: Technical Paper. 2018.
- 70.Ferguson H, Bovaird S, Mueller M. The impact of poverty on educational outcomes for children. Paediatr Child Health. 2007;12(8):701–706. doi: 10.1093/pch/12.8.701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stern Y. Cognitive reserve in ageing and Alzheimer’s disease. Lancet Neurol. 2012;11(11):1006–1012. doi: 10.1016/S1474-4422(12)70191-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Subramaniapillai S, Almey A, Natasha Rajah M, Einstein G. Sex and gender differences in cognitive and brain reserve: implications for Alzheimer’s disease in women. Front Neuroendocrinol. 2021;60:100879. doi: 10.1016/j.yfrne.2020.100879. [DOI] [PubMed] [Google Scholar]
- 73.Pa J, Aslanyan V, Casaletto KB, RenterÃa MA, Harrati A, Tom SE, et al. Effects of sex, APOE4, and lifestyle activities on cognitive reserve in older adults. Neurology. 2022 doi: 10.1212/WNL.0000000000200675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Fyffe DC, Mukherjee S, Barnes LL, Manly JJ, Bennett DA, Crane PK. Explaining differences in episodic memory performance among older African Americans and Whites: the roles of factors related to cognitive reserve and test bias. J Int Neuropsychol Soc JINS. 2011;17(4):625–638. doi: 10.1017/S1355617711000476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nong P, Raj M, Creary M, Kardia SLR, Platt JE. Patient-reported experiences of discrimination in the US health care system. JAMA Netw Open. 2020;3(12):e2029650. doi: 10.1001/jamanetworkopen.2020.29650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.SteelFisher GK, Findling MG, Bleich SN, Casey LS, Blendon RJ, Benson JM, et al. Gender discrimination in the United States: experiences of women. Health Serv Res. 2019;54(Suppl 2):1442–1453. doi: 10.1111/1475-6773.13217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Williams DR, Lawrence JA, Davis BA, Vu C. Understanding how discrimination can affect health. Health Serv Res. 2019;54(Suppl 2):1374–1388. doi: 10.1111/1475-6773.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Sutton MY, Anachebe NF, Lee R, Skanes H. Racial and ethnic disparities in reproductive health services and outcomes, 2020. Obstet Gynecol. 2021;137(2):225–233. doi: 10.1097/AOG.0000000000004224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Berger M, Sarnyai Z. “More than skin deep”: stress neurobiology and mental health consequences of racial discrimination. Stress. 2015;18(1):1–10. doi: 10.3109/10253890.2014.989204. [DOI] [PubMed] [Google Scholar]
- 80.Sawyer PJ, Major B, Casad BJ, Townsend SSM, Mendes WB. Discrimination and the stress response: psychological and physiological consequences of anticipating prejudice in interethnic interactions. Am J Public Health. 2012;102(5):1020–1026. doi: 10.2105/AJPH.2011.300620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Thomas MD, Mendez RM, Zhang Y, Wang Y, Sohail S, Chae DH, et al. Superwoman schema, racial identity, and cellular aging among African American women. Gerontologist. 2022;62(5):762–772. doi: 10.1093/geront/gnac005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Jbaily A, Zhou X, Liu J, Lee TH, Kamareddine L, Verguet S, et al. Air pollution exposure disparities across US population and income groups. Nature. 2022;601(7892):228–233. doi: 10.1038/s41586-021-04190-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Thomson EM. Air pollution, stress, and allostatic load: linking systemic and central nervous system impacts. J Alzheimers Dis. 2019;69(3):597–614. doi: 10.3233/JAD-190015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Peters, A. Ambient air pollution and Alzheimer’s disease: the role of the composition of fine particles. Proc. Natl. Acad. Sci. 2023;120:e2220028120. [DOI] [PMC free article] [PubMed]
- 85.Brody GH, Lei MK, Chen E, Miller GE. Neighborhood poverty and allostatic load in African American youth. Pediatrics. 2014;134(5):e1362–1368. doi: 10.1542/peds.2014-1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Guidi J, Lucente M, Sonino N, Fava GA. Allostatic load and its impact on health: a systematic review. Psychother Psychosom. 2021;90(1):11–27. doi: 10.1159/000510696. [DOI] [PubMed] [Google Scholar]
- 87.Schulz AJ, Mentz G, Lachance L, Johnson J, Gaines C, Israel BA. Associations between socioeconomic status and allostatic load: effects of neighborhood poverty and tests of mediating pathways. Am J Public Health. 2012;102(9):1706–1714. doi: 10.2105/AJPH.2011.300412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Richardson LJ, Goodwin AN, Hummer RA. Social status differences in allostatic load among young adults in the United States. SSM - Popul Health. 2021;1(15):100771. doi: 10.1016/j.ssmph.2021.100771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ehrlich KB, Yu T, Sadiq A, Brody GH. Neighborhood poverty, allostatic load, and changes in cellular aging in African American young adults: the moderating role of attachment. Attach Hum Dev. 2022;24(3):339–352. doi: 10.1080/14616734.2021.1976934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ebong I, Breathett K. The cardiovascular disease epidemic in African American women: recognizing and tackling a persistent problem. J Womens Health. 2020;29(7):891–893. doi: 10.1089/jwh.2019.8125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Nianogo RA, Rosenwohl-Mack A, Yaffe K, Carrasco A, Hoffmann CM, Barnes DE. Risk factors associated with Alzheimer disease and related dementias by sex and race and ethnicity in the US. JAMA Neurol. 2022;79(6):584–591. doi: 10.1001/jamaneurol.2022.0976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gillum RF. Epidemiology of hypertension in African American women. Am Heart J. 1996;131(2):385–395. doi: 10.1016/S0002-8703(96)90371-3. [DOI] [PubMed] [Google Scholar]
- 93.Toft-Nielsen F, Emanuelsson F, Benn M. Familial hypercholesterolemia prevalence among ethnicities-systematic review and meta-analysis. Front Genet. 2022;13:840797. doi: 10.3389/fgene.2022.840797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Brown MD, Gomez DH. Race, cardiovascular disease, and vascular health. Kinesiol Rev. 2021;11(1):43–53. doi: 10.1123/kr.2021-0061. [DOI] [Google Scholar]
- 95.de Bruijn RF, Ikram MA. Cardiovascular risk factors and future risk of Alzheimer’s disease. BMC Med. 2014;12(1):130. doi: 10.1186/s12916-014-0130-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Babulal GM, Quiroz YT, Albensi BC, Arenaza-Urquijo E, Astell AJ, Babiloni C, Bahar-Fuchs A, Bell J, Bowman GL, Brickman AM, Chételat G, Ciro C, Cohen AD, Dilworth-Anderson P, Dodge HH, Dreux S, Edland S, Esbensen A, Evered L, Ewers M, Fargo KN, Fortea J, Gonzalez H, Gustafson DR, Head E, Hendrix JA, Hofer SM, Johnson LA, Jutten R, Kilborn K, Lanctôt KL, Manly JJ, Martins RN, Mielke MM, Morris MC, Murray ME, Oh ES, Parra MA, Rissman RA, Roe CM, Santos OA, Scarmeas N, Schneider LS, Schupf N, Sikkes S, Snyder HM, Sohrabi HR, Stern Y, Strydom A, Tang Y, Terrera GM, Teunissen C, Melo van Lent D, Weinborn M, Wesselman L, Wilcock DM, Zetterberg H, O'Bryant SE; International Society to Advance Alzheimer's Research and Treatment, Alzheimer's Association. Perspectives on ethnic and racial disparities in Alzheimer's disease and related dementias: Update and areas of immediate need. Alzheimers Dement. 2019 Feb;15(2):292–312. 10.1016/j.jalz.2018.09.009. Epub 2018 Dec 13. PMID: 30555031; PMCID: PMC6368893. [DOI] [PMC free article] [PubMed]
- 97.Garcia M, Mulvagh SL, Merz CNB, Buring JE, Manson JE. Cardiovascular disease in women: clinical perspectives. Circ Res. 2016;118(8):1273–1293. doi: 10.1161/CIRCRESAHA.116.307547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lucà F, Abrignani MG, Parrini I, Di Fusco SA, Giubilato S, Rao CM, et al. Update on management of cardiovascular diseases in women. J Clin Med. 2022;11(5):1176. doi: 10.3390/jcm11051176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Dhaibar HA, Cruz-Topete D. Predisposition of women to cardiovascular diseases: a side-effect of increased glucocorticoid signaling during the COVID-19 pandemic? Front Glob Womens Health. 2021;16(2):606833. doi: 10.3389/fgwh.2021.606833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Kannel WB. The Framingham Study: historical insight on the impact of cardiovascular risk factors in men versus women. J Gend-Specif Med JGSM Off J Partnersh Womens Health Columbia. 2002;5(2):27–37. [PubMed] [Google Scholar]
- 101.Kander MC, Cui Y, Liu Z. Gender difference in oxidative stress: a new look at the mechanisms for cardiovascular diseases. J Cell Mol Med. 2017;21(5):1024–1032. doi: 10.1111/jcmm.13038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Matthews KA, Crawford SL, Chae CU, Everson-Rose SA, Sowers MF, Sternfeld B, et al. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol. 2009;54(25):2366–2373. doi: 10.1016/j.jacc.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Roeters van Lennep JE, Westerveld HT, Erkelens DW, van der Wall EE. Risk factors for coronary heart disease: implications of gender. Cardiovasc Res. 2002;53(3):538–549. doi: 10.1016/S0008-6363(01)00388-1. [DOI] [PubMed] [Google Scholar]
- 104.Xue B, Pamidimukkala J, Lubahn DB, Hay M. Estrogen receptor-α mediates estrogen protection from angiotensin II-induced hypertension in conscious female mice. Am J Physiol-Heart Circ Physiol. 2007;292(4):H1770–H1776. doi: 10.1152/ajpheart.01011.2005. [DOI] [PubMed] [Google Scholar]
- 105.Duma D, Collins JB, Chou JW, Cidlowski JA. Sexually dimorphic actions of glucocorticoids provide a link to inflammatory diseases with gender differences in prevalence. Sci Signal. 2010;3(143):ra74. doi: 10.1126/scisignal.2001077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Grady D, Herrington D, Bittner V, Blumenthal R, Davidson M, Hlatky M, et al. Cardiovascular disease outcomes during 6.8 years of hormone therapy: Heart and Estrogen/Progestin Replacement Study follow-up [HERS II] JAMA. 2002;288(1):49–57. doi: 10.1001/jama.288.1.49. [DOI] [PubMed] [Google Scholar]
- 107.Atkins D. Estrogen plus progestin was not effective for long-term secondary prevention of coronary heart disease in postmenopausal women. ACP J Club. 2003;138(1):6–7. doi: 10.7326/ACPJC-2003-138-1-006. [DOI] [PubMed] [Google Scholar]
- 108.Nudy M, Chinchilli VM, Foy AJ. A systematic review and meta-regression analysis to examine the ‘timing hypothesis’ of hormone replacement therapy on mortality, coronary heart disease, and stroke. IJC Heart Vasc. 2019;1(22):123–131. doi: 10.1016/j.ijcha.2019.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Nicholson WK, Brown AF, Gathe J, Grumbach K, Washington AE, Pérez-Stable EJ. Hormone replacement therapy for African American women: missed opportunities for effective intervention. Menopause N Y N. 1999;6(2):147–155. [PubMed] [Google Scholar]
- 110.McNagny SE, Jacobson TA. Use of postmenopausal hormone replacement therapy by African American women. The importance of physician discussion. Arch Intern Med. 1997;157(12):1337–1342. doi: 10.1001/archinte.1997.00440330073008. [DOI] [PubMed] [Google Scholar]
- 111.Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–638. doi: 10.1038/nri.2016.90. [DOI] [PubMed] [Google Scholar]
- 112.Zieneldien T, Kim J, Sawmiller D, Cao C. The immune system as a therapeutic target for Alzheimer’s disease. Life. 2022;12(9):1440. doi: 10.3390/life12091440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Henein MY, Vancheri S, Longo G, Vancheri F. The role of inflammation in cardiovascular disease. Int J Mol Sci. 2022;23(21):12906. doi: 10.3390/ijms232112906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chrousos GP. Stress and sex versus immunity and inflammation. Sci Signal. 2010;3(143):pe36. doi: 10.1126/scisignal.3143pe36. [DOI] [PubMed] [Google Scholar]
- 115.Ngo ST, Steyn FJ, McCombe PA. Gender differences in autoimmune disease. Front Neuroendocrinol. 2014;35(3):347–369. doi: 10.1016/j.yfrne.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 116.Wegner A, Benson S, Rebernik L, Spreitzer I, Jäger M, Schedlowski M, et al. Sex differences in the pro-inflammatory cytokine response to endotoxin unfold in vivo but not ex vivo in healthy humans. Innate Immun. 2017;23(5):432–439. doi: 10.1177/1753425917707026. [DOI] [PubMed] [Google Scholar]
- 117.Fisher G, Alvarez JA, Ellis AC, Granger WM, Ovalle F, Man CD, et al. Race differences in the association of oxidative stress with insulin sensitivity in African- and European-American women. Obes Silver Spring Md. 2012;20(5):972–977. doi: 10.1038/oby.2011.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Chow CC, Periwal V, Csako G, Ricks M, Courville AB, Miller BV, et al. Higher acute insulin response to glucose may determine greater free fatty acid clearance in African-American women. J Clin Endocrinol Metab. 2011;96(8):2456–2463. doi: 10.1210/jc.2011-0532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ellis AC, Alvarez JA, Granger WM, Ovalle F, Gower BA. Ethnic differences in glucose disposal, hepatic insulin sensitivity, and endogenous glucose production among African American and European American women. Metabolism. 2012;61(5):634–640. doi: 10.1016/j.metabol.2011.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Tan M, Mamun A, Kitzman H, Mandapati SR, Dodgen L. Neighborhood disadvantage and allostatic load in African American women at risk for obesity-related diseases. Prev Chronic Dis. 2017;22(14):E119. doi: 10.5888/pcd14.170143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Kuźma E, Lourida I, Moore SF, Levine DA, Ukoumunne OC, Llewellyn DJ. Stroke and dementia risk: a systematic review and meta-analysis. Alzheimers Dement. 2018;14(11):1416–1426. doi: 10.1016/j.jalz.2018.06.3061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Pluta R, Januszewski S, Czuczwar SJ. Brain ischemia as a prelude to Alzheimer’s disease. Front Aging Neurosci. 2021;18(13):636653. doi: 10.3389/fnagi.2021.636653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Jiménez MC, Manson JE, Cook NR, Kawachi I, Wassertheil-Smoller S, Haring B, et al. Racial variation in stroke risk among women by stroke risk factors. Stroke. 2019;50(4):797–804. doi: 10.1161/STROKEAHA.117.017759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Clark DG, Boan AD, Sims-Robinson C, Adams RJ, Amella EJ, Benitez A, et al. Differential impact of index stroke on dementia risk in African-Americans compared to Whites. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2018;27(10):2725–2730. doi: 10.1016/j.jstrokecerebrovasdis.2018.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Costello BT, Silverman ER, Doukky R, Braun LT, Aggarwal NT, Deng Y, et al. Lipoprotein[a] and increased cardiovascular risk in women. Clin Cardiol. 2016;39(2):96–102. doi: 10.1002/clc.22500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mukaz DK, Zakai NA, Cruz-Flores S, McCullough LD, Cushman M. Identifying genetic and biological determinants of race-ethnic disparities in stroke in the United States. Stroke. 2020;51(11):3417–3424. doi: 10.1161/STROKEAHA.120.030425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Alqarni A, Jiang J, Crawford JD, Koch F, Brodaty H, Sachdev P, et al. Sex differences in risk factors for white matter hyperintensities in non-demented older individuals. Neurobiol Aging. 2021;1(98):197–204. doi: 10.1016/j.neurobiolaging.2020.11.001. [DOI] [PubMed] [Google Scholar]
- 128.Boots EA, Castellanos KJ, Zhan L, Barnes LL, Tussing-Humphreys L, Deoni SCL, et al. Inflammation, cognition, and white matter in older adults: an examination by race. Front Aging Neurosci. 2020;12:387. doi: 10.3389/fnagi.2020.553998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Abel WM, Greer DB, Sue-Ling C, Kirkland TW. Antihypertensive medication adherence and persistence among Black women: a qualitative study. Nurse Pract. 2022;47(3):40–47. doi: 10.1097/01.NPR.0000819620.71567.0e. [DOI] [PubMed] [Google Scholar]
- 130.Bherer L, Erickson KI, Liu-Ambrose T. A review of the effects of physical activity and exercise on cognitive and brain functions in older adults. J Aging Res. 2013. [DOI] [PMC free article] [PubMed]
- 131.Agarwal P, Morris MC, Barnes LL. Racial differences in dietary relations to cognitive decline and Alzheimer’s disease risk: do we know enough? Front Hum Neurosci [Internet]. 2020 [cited 2022 Aug 16];14. Available from: https://www.frontiersin.org/articles/10.3389/fnhum.2020.00359. [DOI] [PMC free article] [PubMed]
- 132.Adinkrah E, Bazargan M, Wisseh C, Assari S. Adherence to hypertension medications and lifestyle recommendations among underserved African American middle-aged and older adults. Int J Environ Res Public Health. 2020;17(18):6538. doi: 10.3390/ijerph17186538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Jones HJ, Bakas T, Nared S, Humphries J, Wijesooriya J, Butsch KM. Co-designing a program to lower cardiovascular disease risk in midlife Black women. Int J Environ Res Public Health. 2022;19(3):1356. doi: 10.3390/ijerph19031356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Chadwick KD, Burkman RT, Tornesi BM, Mahadevan B. Fifty years of “the pill”: risk reduction and discovery of benefits beyond contraception, reflections, and forecast. Toxicol Sci Off J Soc Toxicol. 2012;125(1):2–9. doi: 10.1093/toxsci/kfr242. [DOI] [PubMed] [Google Scholar]
- 135.Mordecai KL, Rubin LH, Maki PM. Effects of menstrual cycle phase and oral contraceptive use on verbal memory. Horm Behav. 2008;54(2):286–293. doi: 10.1016/j.yhbeh.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 136.Griksiene R, Ruksenas O. Effects of hormonal contraceptives on mental rotation and verbal fluency. Psychoneuroendocrinology. 2011;36(8):1239–1248. doi: 10.1016/j.psyneuen.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 137.Egan KR, Gleason CE. Longer duration of hormonal contraceptive use predicts better cognitive outcomes later in life. J Womens Health. 2012;21(12):1259–1266. doi: 10.1089/jwh.2012.3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Daniels K. Current contraceptive status among women aged 15–49: United States, 2017–2019. 2020;(388):8. [PubMed]
- 139.Lin CJ, Maier J, Nwankwo C, Burley C, deBorja L, Aaraj YA, et al. Awareness and use of contraceptive methods and perceptions of long-acting reversible contraception among White and non-White women. J Womens Health 2002. 2021;30(9):1313–1320. doi: 10.1089/jwh.2020.8642. [DOI] [PubMed] [Google Scholar]
- 140.Kavanaugh ML, Pliskin E, Hussain R. Associations between unfulfilled contraceptive preferences due to cost and low-income patients’ access to and experiences of contraceptive care in the United States, 2015–2019. Contracept X. 2022;6(4):100076. doi: 10.1016/j.conx.2022.100076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Soon JA, Whelan AM, Yuksel N, Rafie S. Enhancing access to contraception through pharmacist prescribing across Canada. Can Pharm J Rev Pharm Can. 2021;154(6):356–362. doi: 10.1177/17151635211034534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Committee on healthcare for underserved women. Committee opinion number 615. Access to Contraception 2015. https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2015/01/access-to-contraception.
- 143.Kathawa CA, Arora KS. Implicit bias in counseling for permanent contraception: historical context and recommendations for counseling. Health Equity. 2020;4(1):326–329. doi: 10.1089/heq.2020.0025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Beltz AM, Moser JS. Ovarian hormones: a long overlooked but critical contributor to cognitive brain structures and function. Ann N Y Acad Sci. 2020;1464(1):156–180. doi: 10.1111/nyas.14255. [DOI] [PubMed] [Google Scholar]
- 145.Mammaro A, Carrara S, Cavaliere A, Ermito S, Dinatale A, Pappalardo EM, et al. Hypertensive disorders of pregnancy. J Prenat Med. 2009;3(1):1–5. [PMC free article] [PubMed] [Google Scholar]
- 146.Ford ND. Hypertensive disorders in pregnancy and mortality at delivery hospitalization — United States, 2017–2019. MMWR Morb Mortal Wkly Rep [Internet]. 2022 [cited 2022 Nov 19];71. Available from: https://www.cdc.gov/mmwr/volumes/71/wr/mm7117a1.htm. [DOI] [PMC free article] [PubMed]
- 147.Tolcher MC, Sangi-Haghpeykar H, Mendez-Figueroa H, Aagaard KM. Low-dose aspirin for preeclampsia prevention: efficacy by ethnicity and race. Am J Obstet Gynecol MFM. 2020;2(4):100184. doi: 10.1016/j.ajogmf.2020.100184. [DOI] [PubMed] [Google Scholar]
- 148.Boakye E, Kwapong YA, Obisesan O, Ogunwole SM, Hays AG, Nasir K, et al. Nativity-related disparities in preeclampsia and cardiovascular disease risk among a racially diverse cohort of US women. JAMA Netw Open. 2021;4(12):e2139564. doi: 10.1001/jamanetworkopen.2021.39564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Ghosh G, Grewal J, Männistö T, Mendola P, Chen Z, Xie Y, et al. Racial/ethnic differences in pregnancy-related hypertensive disease in nulliparous women. Ethn Dis. 2014;24(3):283–289. [PMC free article] [PubMed] [Google Scholar]
- 150.Minhas AS, Ogunwole SM, Vaught AJ, Wu P, Mamas MA, Gulati M, et al. Racial disparities in cardiovascular complications with pregnancy-induced hypertension in the United States. Hypertension. 2021;78(2):480–488. doi: 10.1161/HYPERTENSIONAHA.121.17104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Riskin-Mashiah S, Belfort MA. Preeclampsia is associated with global cerebral hemodynamic changes. J Soc Gynecol Investig. 2005;12(4):253–256. doi: 10.1016/j.jsgi.2005.01.002. [DOI] [PubMed] [Google Scholar]
- 152.Riskin-Mashiah S, Belfort MA, Saade GR, Herd JA. Cerebrovascular reactivity in normal pregnancy and preeclampsia. Obstet Gynecol. 2001;98(5 Pt 1):827–832. doi: 10.1097/00006250-200111000-00020. [DOI] [PubMed] [Google Scholar]
- 153.Richards A, Graham D, Bullock R. Clinicopathological study of neurological complications due to hypertensive disorders of pregnancy. J Neurol Neurosurg Psychiatry. 1988;51(3):416–421. doi: 10.1136/jnnp.51.3.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Basit S, Wohlfahrt J, Boyd HA. Pre-eclampsia and risk of dementia later in life: nationwide cohort study. BMJ. 2018;17(363):k4109. doi: 10.1136/bmj.k4109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Schuster J, Cheng SB, Padbury J, Sharma S. Placental extracellular vesicles and preeclampsia. Am J Reprod Immunol N Y N 1989. 2021;85(2):e13297. [DOI] [PMC free article] [PubMed]
- 156.DeBattista C. Executive dysfunction in major depressive disorder. Expert Rev Neurother. 2005;5(1):79–83. doi: 10.1586/14737175.5.1.79. [DOI] [PubMed] [Google Scholar]
- 157.Miller EC. Preeclampsia and cerebrovascular disease. Hypertension 2019;74:5–13. [DOI] [PMC free article] [PubMed]
- 158.Brown HL, Warner JJ, Gianos E, Gulati M, Hill AJ, Hollier LM, et al. Promoting risk identification and reduction of cardiovascular disease in women through collaboration with obstetricians and gynecologists: a presidential advisory from the American Heart Association and the American College of Obstetricians and Gynecologists. Circulation. 2018;137(24):e843–e852. doi: 10.1161/CIR.0000000000000582. [DOI] [PubMed] [Google Scholar]
- 159.Scheyer O, Rahman A, Hristov H, Berkowitz C, Isaacson RS, Diaz Brinton R, et al. Female sex and Alzheimer’s risk: the menopause connection. J Prev Alzheimers Dis. 2018;5(4):225–230. doi: 10.14283/jpad.2018.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Hershey L, Tarawneh R. Women need to be advised about the risks of long-term hormone replacement therapy. Neurology. 2022;99(17):733–734. doi: 10.1212/WNL.0000000000201337. [DOI] [PubMed] [Google Scholar]
- 161.Sung YF, Tsai CT, Kuo CY, Lee JT, Chou CH, Chen YC, et al. Use of hormone replacement therapy and risk of dementia: a nationwide cohort study. Neurology. 2022;99(17):e1835–e1842. doi: 10.1212/WNL.0000000000200960. [DOI] [PubMed] [Google Scholar]
- 162.Hogervorst E, Yaffe K, Richards M, Huppert FAH. Hormone replacement therapy to maintain cognitive function in women with dementia. Cochrane Database Syst Rev. 2009;2009(1):CD003799. doi: 10.1002/14651858.CD003799.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Wu M, Li M, Yuan J, Liang S, Chen Z, Ye M, et al. Postmenopausal hormone therapy and Alzheimer’s disease, dementia, and Parkinson’s disease: a systematic review and time-response meta-analysis. Pharmacol Res. 2020;155:104693. doi: 10.1016/j.phrs.2020.104693. [DOI] [PubMed] [Google Scholar]
- 164.Stute P, Wienges J, Koller AS, Giese C, Wesemüller W, Janka H, et al. Cognitive health after menopause: does menopausal hormone therapy affect it? Best Pract Res Clin Endocrinol Metab. 2021;35(6):101565. doi: 10.1016/j.beem.2021.101565. [DOI] [PubMed] [Google Scholar]
- 165.Whitmer RA, Quesenberry CP, Zhou J, Yaffe K. Timing of hormone therapy and dementia: the critical window theory revisited. Ann Neurol. 2011;69(1):163–169. doi: 10.1002/ana.22239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Yaffe K, Haan M, Byers A, Tangen C, Kuller L. Estrogen use, APOE, and cognitive decline: evidence of gene-environment interaction. Neurology. 2000;54(10):1949–1954. doi: 10.1212/WNL.54.10.1949. [DOI] [PubMed] [Google Scholar]
- 167.Christmas M, Janssen I, Joffe H, Upchurch D, Santoro N, Kravitz HM. Menopause hormone therapy and complementary alternative medicine, quality of life, and racial/ethnic differences: the Study of Women’s Health Across the Nation [SWAN] Menopause N Y N. 2022;29(12):1357–1364. doi: 10.1097/GME.0000000000002087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Alzheimer’s disease genetics fact sheet [Internet]. National Institute on Aging. [cited 2023 Jun 2]. Available from: https://www.nia.nih.gov/health/alzheimers-disease-genetics-fact-sheet.
- 169.Altmann A, Tian L, Henderson VW, Greicius MD. Sex modifies the APOE-related risk of developing Alzheimer’s disease. Ann Neurol. 2014;75(4):563–573. doi: 10.1002/ana.24135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Arnold M, Nho K, Kueider-Paisley A, Massaro T, Huynh K, Brauner B, et al. Sex and APOE ε4 genotype modify the Alzheimer’s disease serum metabolome. Nat Commun. 2020;11(1):1148. doi: 10.1038/s41467-020-14959-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Yan S, Zheng C, Paranjpe MD, Li Y, Li W, Wang X, et al. Sex modifies APOE ε4 dose effect on brain tau deposition in cognitively impaired individuals. Brain J Neurol. 2021;144(10):3201–3211. doi: 10.1093/brain/awab160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Park SY, Setiawan VW, White LR, Wu AH, Cheng I, Haiman CA, et al. Modifying effects of race and ethnicity and APOE on the association of physical activity with risk of Alzheimer’s disease and related dementias. Alzheimers Dement [Internet]. 2022 Apr 27 [cited 2022 Aug 3]. 10.1002/alz.12677. [DOI] [PMC free article] [PubMed]
- 173.Sampedro F, Vilaplana E, de Leon MJ, Alcolea D, Pegueroles J, Montal V, et al. APOE-by-sex interactions on brain structure and metabolism in healthy elderly controls. Oncotarget. 2015;6(29):26663–26674. doi: 10.18632/oncotarget.5185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Damoiseaux JS, Seeley WW, Zhou J, Shirer WR, Coppola G, Karydas A, et al. Gender modulates the APOE ε4 effect in healthy older adults: convergent evidence from functional brain connectivity and spinal fluid tau levels. J Neurosci. 2012;32(24):8254–8262. doi: 10.1523/JNEUROSCI.0305-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Barnes LL, Bennett DA. Cognitive resilience in APOE*ε4 carriers—is race important? Nat Rev Neurol. 2015;11(4):190–191. doi: 10.1038/nrneurol.2015.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Rajan KB, McAninch EA, Wilson RS, Weuve J, Barnes LL, Evans DA. Race, APOE ε4, and long-term cognitive trajectories in a biracial population sample. J Alzheimers Dis JAD. 2019;72(1):45–53. doi: 10.3233/JAD-190538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hendrie HC, Murrell J, Baiyewu O, Lane KA, Purnell C, Ogunniyi A, et al. APOE ε4 and the risk for Alzheimer disease and cognitive decline in African Americans and Yoruba. Int Psychogeriatr IPA. 2014;26(6):977–985. doi: 10.1017/S1041610214000167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Hendrie HC, Ogunniyi A, Hall KS, Baiyewu O, Unverzagt FW, Gureje O, et al. Incidence of dementia and Alzheimer disease in 2 communities Yoruba residing in Ibadan, Nigeria, and African Americans residing in Indianapolis, Indiana. JAMA. 2001;285(6):739–747. doi: 10.1001/jama.285.6.739. [DOI] [PubMed] [Google Scholar]
- 179.De Roeck A, Van Broeckhoven C, Sleegers K. The role of ABCA7 in Alzheimer’s disease: evidence from genomics, transcriptomics and methylomics. Acta Neuropathol [Berl] 2019;138(2):201–220. doi: 10.1007/s00401-019-01994-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Berg CN, Sinha N, Gluck MA. ABCA7 risk genotype diminishes the neuroprotective value of aerobic fitness in healthy older African Americans. Front Aging Neurosci [Internet]. 2019 [cited 2022 Oct 22];11. Available from: https://www.frontiersin.org/articles/10.3389/fnagi.2019.00073. [DOI] [PMC free article] [PubMed]
- 181.Nettiksimmons J, Tranah G, Evans DS, Yokoyama JS, Yaffe K. Gene-based aggregate SNP associations between candidate AD genes and cognitive decline. Age Dordr Neth. 2016;38(2):41. doi: 10.1007/s11357-016-9885-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Fu Y, He Y, Phan K, Pickford R, Kim YB, Dzamko N, et al. Sex-specific lipid dysregulation in the Abca7 knockout mouse brain. Brain Commun. 2022;4(3):fcac120. doi: 10.1093/braincomms/fcac120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Deming Y, Dumitrescu L, Barnes LL, Thambisetty M, Kunkle B, Gifford KA, et al. Sex-specific genetic predictors of Alzheimer’s disease biomarkers. Acta Neuropathol [Berl] 2018;136(6):857–872. doi: 10.1007/s00401-018-1881-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Eissman JM, Dumitrescu L, Mahoney ER, Smith AN, Mukherjee S, Lee ML, et al. Sex differences in the genetic architecture of cognitive resilience to Alzheimer’s disease. Brain J Neurol. 2022;145(7):2541–2554. doi: 10.1093/brain/awac177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Nikolac Perkovic M, Videtic Paska A, Konjevod M, Kouter K, Svob Strac D, Nedic Erjavec G, et al. Epigenetics of Alzheimer’s disease. Biomolecules. 2021;11(2):195. doi: 10.3390/biom11020195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Qin L, Xu Q, Li Z, Chen L, Li Y, Yang N, et al. Ethnicity-specific and overlapping alterations of brain hydroxymethylome in Alzheimer’s disease. Hum Mol Genet. 2020;29(1):149–158. doi: 10.1093/hmg/ddz273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Woo JG, Morrison JA, Stroop DM, Aronson Friedman L, Martin LJ. Genetic architecture of lipid traits changes over time and differs by race: Princeton Lipid Follow-up Study. J Lipid Res. 2014;55(7):1515–1524. doi: 10.1194/jlr.M049932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Horvath S, Gurven M, Levine ME, Trumble BC, Kaplan H, Allayee H, et al. An epigenetic clock analysis of race/ethnicity, sex, and coronary heart disease. Genome Biol. 2016;11(17):171. doi: 10.1186/s13059-016-1030-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Aroke EN, Joseph PV, Roy A, Overstreet DS, Tollefsbol TO, Vance DE, et al. Could epigenetics help explain racial disparities in chronic pain? J Pain Res. 2019;18(12):701–710. doi: 10.2147/JPR.S191848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Kunkle BW, Schmidt M, Klein HU, Naj AC, Hamilton-Nelson KL, Larson EB, et al. Novel Alzheimer disease risk loci and pathways in African American individuals using the African genome resources panel: a meta-analysis. JAMA Neurol. 2021;78(1):102–113. doi: 10.1001/jamaneurol.2020.3536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Mahady L, Nadeem M, Malek-Ahmadi M, Chen K, Perez SE, Mufson EJ. HDAC2 dysregulation in the nucleus basalis of Meynert during the progression of Alzheimer’s disease. Neuropathol Appl Neurobiol. 2019;45(4):380–397. doi: 10.1111/nan.12518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Chlamydas S, Markouli M, Strepkos D, Piperi C. Epigenetic mechanisms regulate sex-specific bias in disease manifestations. J Mol Med Berl Ger. 2022;100(8):1111–1123. doi: 10.1007/s00109-022-02227-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Molinuevo JL, Ayton S, Batrla R, Bednar MM, Bittner T, Cummings J, et al. Current state of Alzheimer’s fluid biomarkers. Acta Neuropathol [Berl] 2018;136(6):821–853. doi: 10.1007/s00401-018-1932-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Blennow K, Zetterberg H, Fagan AM. Fluid biomarkers in Alzheimer disease. Cold Spring Harb Perspect Med. 2012;2(9):a006221. doi: 10.1101/cshperspect.a006221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Anoop A, Singh PK, Jacob RS, Maji SK. CSF biomarkers for Alzheimer’s disease diagnosis. Int J Alzheimers Dis. 2010;23(2010):606802. doi: 10.4061/2010/606802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Hu WT, Chen-Plotkin A, Arnold SE, Grossman M, Clark CM, Shaw LM, et al. Novel CSF biomarkers for Alzheimer’s disease and mild cognitive impairment. Acta Neuropathol [Internet]. 2010;119. Available from: 10.1007/s00401-010-0667-0. [DOI] [PMC free article] [PubMed]
- 197.Gaetani L, Blennow K, Calabresi P, Filippo MD, Parnetti L, Zetterberg H. Neurofilament light chain as a biomarker in neurological disorders. J Neurol Neurosurg Psychiatry. 2019;90(8):870–881. doi: 10.1136/jnnp-2018-320106. [DOI] [PubMed] [Google Scholar]
- 198.Gleason CE, Zuelsdorff M, Gooding DC, Kind AJH, Johnson AL, James TT, et al. Alzheimer’s disease biomarkers in Black and non-Hispanic White cohorts: a contextualized review of the evidence. Alzheimers Dement [Internet]. 2021 Dec 6 [cited 2022 Aug 10]; Available from: https://onlinelibrary.wiley.com/doi/abs/10.1002/alz.12511. [DOI] [PMC free article] [PubMed]
- 199.Brickman AM, Manly JJ, Honig LS, Sanchez D, Reyes-Dumeyer D, Lantigua RA, et al. Plasma p-tau181, p-tau217, and other blood-based Alzheimer’s disease biomarkers in a multi-ethnic, community study. Alzheimers Dement J Alzheimers Assoc. 2021;17(8):1353–1364. doi: 10.1002/alz.12301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Morris JC, Schindler SE, McCue LM, Moulder KL, Benzinger TLS, Cruchaga C, et al. Assessment of racial disparities in biomarkers for Alzheimer disease. JAMA Neurol. 2019;76(3):264–273. doi: 10.1001/jamaneurol.2018.4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hajjar I, Yang Z, Okafor M, Liu C, Waligorska T, Goldstein FC, et al. Association of plasma and cerebrospinal fluid Alzheimer disease biomarkers with race and the role of genetic ancestry, vascular comorbidities, and neighborhood factors. JAMA Netw Open. 2022;5(10):e2235068–e2235068. doi: 10.1001/jamanetworkopen.2022.35068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Garrett SL, McDaniel D, Obideen M, Trammell AR, Shaw LM, Goldstein FC, et al. Racial disparity in cerebrospinal fluid amyloid and tau biomarkers and associated cutoffs for mild cognitive impairment. JAMA Netw Open. 2019;2(12):e1917363–e1917363. doi: 10.1001/jamanetworkopen.2019.17363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Schindler SE, Karikari TK, Ashton NJ, Henson RL, Yarasheski KE, West T, et al. Effect of race on prediction of brain amyloidosis by plasma Aβ42/Aβ40, phosphorylated tau, and neurofilament light. Neurology. 2022;99(3):e245–e257. doi: 10.1212/WNL.0000000000200358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Beydoun MA, Noren Hooten N, Beydoun HA, Maldonado AI, Weiss J, Evans MK, et al. Plasma neurofilament light as a potential biomarker for cognitive decline in a longitudinal study of middle-aged urban adults. Transl Psychiatry. 2021;21(11):436. doi: 10.1038/s41398-021-01563-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Jin SC, Carrasquillo MM, Benitez BA, Skorupa T, Carrell D, Patel D, et al. TREM2 is associated with increased risk for Alzheimer’s disease in African Americans. Mol Neurodegener [Internet]. 2015;10. Available from: 10.1186/s13024-015-0016-9. [DOI] [PMC free article] [PubMed]
- 206.Schindler SE, Cruchaga C, Joseph A, McCue L, Farias FHG, Wilkins CH, et al. African Americans have differences in CSF soluble TREM2 and associated genetic variants. Neurol Genet. 2021;7(2):e571. [DOI] [PMC free article] [PubMed]
- 207.Mielke MM. Consideration of sex differences in the measurement and interpretation of Alzheimer disease-related biofluid-based biomarkers. J Appl Lab Med. 2020;5(1):158–169. doi: 10.1373/jalm.2019.030023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Ferretti MT, Iulita MF, Cavedo E, Chiesa PA, Schumacher Dimech A, Santuccione Chadha A, et al. Sex differences in Alzheimer disease - the gateway to precision medicine. Nat Rev Neurol. 2018;14(8):457–469. doi: 10.1038/s41582-018-0032-9. [DOI] [PubMed] [Google Scholar]
- 209.Buckley RF, Mormino EC, Rabin JS, Hohman TJ, Landau S, Hanseeuw BJ, et al. Sex differences in the association of global amyloid and regional tau deposition measured by positron emission tomography in clinically normal older adults. JAMA Neurol. 2019;76(5):542–551. doi: 10.1001/jamaneurol.2018.4693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 210.Koran MEI, Wagener M, Hohman TJ. Sex differences in the association between AD biomarkers and cognitive decline. Brain Imaging Behav. 2017;11(1):205–213. doi: 10.1007/s11682-016-9523-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Caldwell JZK, Kinney JW, Ritter A, Salazar A, Wong CG, Cordes D, et al. Inflammatory cytokine levels implicated in Alzheimer’s disease moderate the effects of sex on verbal memory performance. Brain Behav Immun. 2021;95:27–35. doi: 10.1016/j.bbi.2020.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Su F, Bai F, Zhang Z. Inflammatory cytokines and Alzheimer’s disease: a review from the perspective of genetic polymorphisms. Neurosci Bull. 2016;32(5):469–480. doi: 10.1007/s12264-016-0055-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Morgan AR, Touchard S, Leckey C, O’Hagan C, Nevado-Holgado AJ, Barkhof F, et al. Inflammatory biomarkers in Alzheimer’s disease plasma. Alzheimers Dement. 2019;15(6):776–787. doi: 10.1016/j.jalz.2019.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Ferrucci L, Fabbri E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nat Rev Cardiol. 2018;15(9):505–522. doi: 10.1038/s41569-018-0064-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Williams A, Greene N, Kimbro KS. Increased circulating cytokine levels in African American women with obesity and elevated HbA1c. Cytokine. 2020;128:154989. doi: 10.1016/j.cyto.2020.154989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Wickrama KAS, Ralston PA, Ilich JZ. Lower life satisfaction and inflammation in African American adults: body adiposity mediation and sex moderation. J Pers Med. 2022;12(5):745. doi: 10.3390/jpm12050745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Byrd DR, Allen JO. Multiple forms of discrimination and inflammation in Black Americans: are there differences by sex? Soc Sci Med. 2023;1(321):115785. doi: 10.1016/j.socscimed.2023.115785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Brown MD, Feairheller DL, Thakkar S, Veerabhadrappa P, Park JY. Racial differences in tumor necrosis factor-α-induced endothelial microparticles and interleukin-6 production. Vasc Health Risk Manag. 2011;7:541–550. doi: 10.2147/VHRM.S22930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Yarlagadda A, Alfson E, Clayton AH. The blood brain barrier and the role of cytokines in neuropsychiatry. Psychiatry Edgmont. 2009;6(11):18–22. [PMC free article] [PubMed] [Google Scholar]
- 220.Banks WA, Kastin AJ, Broadwell RD. Passage of cytokines across the blood-brain barrier. NeuroImmunoModulation. 1996;2(4):241–248. doi: 10.1159/000097202. [DOI] [PubMed] [Google Scholar]
- 221.Xie J, Van Hoecke L, Vandenbroucke RE. The impact of systemic inflammation on Alzheimer’s disease pathology. Front Immunol. 2021;12:796867. doi: 10.3389/fimmu.2021.796867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Ising C, Venegas C, Zhang S, Scheiblich H, Schmidt SV, Vieira-Saecker A, et al. NLRP3 inflammasome activation drives tau pathology. Nature. 2019;575(7784):669–673. doi: 10.1038/s41586-019-1769-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Blazel MM, Lazar KK, Van Hulle CA, Ma Y, Cole A, Spalitta A, et al. Factors associated with lumbar puncture participation in Alzheimer’s disease research. J Alzheimers Dis. 2020;77(4):1559–1567. doi: 10.3233/JAD-200394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Witbracht MG, Bernstein OM, Lin V, Salazar CR, Sajjadi SA, Hoang D, et al. Education and message framing increase willingness to undergo research lumbar puncture: a randomized controlled trial. Front Med. 2020;18(7):493. doi: 10.3389/fmed.2020.00493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Nyquist PA, Bilgel MS, Gottesman R, Yanek LR, Moy TF, Becker LC, et al. Extreme deep white matter hyperintensity volumes are associated with African American race. Cerebrovasc Dis Basel Switz. 2014;37(4):244–250. doi: 10.1159/000358117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Brickman AM, Provenzano FA, Muraskin J, Manly JJ, Blum S, Apa Z, et al. Regional white matter hyperintensity volume, not hippocampal atrophy, predicts incident Alzheimer disease in the community. Arch Neurol. 2012;69(12):1621–1627. doi: 10.1001/archneurol.2012.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Carmichael O, Newton R. 1a - Brain MRI findings related to Alzheimer’s disease in older African American adults. In: Becker JT, Cohen AD, editors. Progress in molecular biology and translational science [Internet]. Academic Press; 2019 [cited 2022 Aug 16]. p. 3–23. [Brain Imaging; vol. 165]. Available from: https://www.sciencedirect.com/science/article/pii/S1877117319300614. [DOI] [PubMed]
- 228.Zahodne LB, Manly JJ, Narkhede A, Griffith EY, DeCarli C, Schupf NS, et al. Structural MRI predictors of late-life cognition differ across African Americans, Hispanics, and Whites. Curr Alzheimer Res. 2015;12(7):632–639. doi: 10.2174/1567205012666150530203214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.de Leeuw FE, de Groot JC, Achten E, Oudkerk M, Ramos L, Heijboer R, et al. Prevalence of cerebral white matter lesions in elderly people: a population based magnetic resonance imaging study. The Rotterdam Scan Study. J Neurol Neurosurg Psychiatry. 2001;70(1):9–14. doi: 10.1136/jnnp.70.1.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Lohner V, Pehlivan G, Sanroma G, Miloschewski A, Schirmer MD, Stöcker T, et al. Relation between sex, menopause, and white matter hyperintensities: the Rhineland Study. Neurology. 2022;99(9):e935–e943. doi: 10.1212/WNL.0000000000200782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Misiura MB, Howell JC, Wu J, Qiu D, Parker MW, Turner JA, et al. Race modifies default mode connectivity in Alzheimer’s disease. Transl Neurodegener. 2020;9(1):8. doi: 10.1186/s40035-020-0186-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 232.Oveisgharan S, Arvanitakis Z, Yu L, Farfel J, Schneider JA, Bennett DA. Sex differences in Alzheimer’s disease and common neuropathologies of aging. Acta Neuropathol [Berl] 2018;136(6):887–900. doi: 10.1007/s00401-018-1920-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Bennett DA, Schneider JA, Arvanitakis Z, Wilson RS. Overview and findings from the religious orders study. Curr Alzheimer Res. 2012;9(6):628–645. doi: 10.2174/156720512801322573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Corder EH. et al. The biphasic relationship between regional brain senile plaque and neurofibrillary tangle distributions: modification by age, sex, and APOE polymorphism. Ann. N. Y. Acad. Sci. 2004;1019:24–28. [DOI] [PubMed]
- 235.Buckley RF, O’Donnell A, McGrath ER, Jacobs HIL, Lois C, Satizabal CL, et al. Menopause status moderates sex differences in tau burden: a Framingham PET Study. Ann Neurol. 2022;92(1):11–22. doi: 10.1002/ana.26382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Jankowsky JL, Zheng H. Practical considerations for choosing a mouse model of Alzheimer’s disease. Mol Neurodegener. 2017;22(12):89. doi: 10.1186/s13024-017-0231-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Gottesman RF, Schneider ALC, Zhou Y, Chen X, Green E, Gupta N, et al. The ARIC-PET amyloid imaging study: brain amyloid differences by age, race, sex, and APOE. Neurology. 2016;87(5):473–480. doi: 10.1212/WNL.0000000000002914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Armstrong NM, Huang CW, Williams OA, Bilgel M, An Y, Doshi J, et al. Sex differences in the association between amyloid and longitudinal brain volume change in cognitively normal older adults. NeuroImage Clin. 2019;1(22):101769. doi: 10.1016/j.nicl.2019.101769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Caldwell JZK, Berg JL, Shan G, Cummings JL, Banks SJ. Sex moderates the impact of diagnosis and amyloid PET positivity on hippocampal subfield volume. J Alzheimers Dis. 2018;64(1):79–89. doi: 10.3233/JAD-180028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Babulal GM, Quiroz YT, Albensi BC, Arenaza-Urquijo E, Astell AJ, Babiloni C, et al. Perspectives on ethnic and racial disparities in Alzheimer’s disease and related dementias: update and areas of immediate need. Alzheimers Dement J Alzheimers Assoc. 2019;15(2):292–312. doi: 10.1016/j.jalz.2018.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Barnes LL, Leurgans S, Aggarwal NT, Shah RC, Arvanitakis Z, James BD, et al. Mixed pathology is more likely in black than white decedents with Alzheimer dementia. Neurology [Internet]. 2015;85. Available from: 10.1212/WNL.0000000000001834. [DOI] [PMC free article] [PubMed]
- 242.Royse SK, Cohen AD, Snitz BE, Rosano C. Differences in Alzheimer’s disease and related dementias pathology among African American and Hispanic women: a qualitative literature review of biomarker studies. Front Syst Neurosci. 2021;15:685957. doi: 10.3389/fnsys.2021.685957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Abdel-Rahman SM, Wimes MP, Curran T. A call to action: issuing a diversity and inclusion challenge to research organizations. Clin Transl Sci. 2021;14(6):2095–2098. doi: 10.1111/cts.13105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Mujuru P, Jean-Francois B, Pérez-Stable EJ. National institute on minority health and health disparities specialized centers of excellence on minority health and health disparities. Am. J. Prev. Med. 2022;63:S6–S7. [DOI] [PMC free article] [PubMed]
- 245.Portacolone E, Palmer NR, Lichtenberg P, Waters CM, Hill CV, Keiser S, et al. Earning the trust of African American communities to increase representation in dementia research. Ethn Dis. 2020;30(Suppl 2):719–734. doi: 10.18865/ed.30.S2.719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Shaw AR, Perales-Puchalt J, Moore T, Weatherspoon P, Robinson M, Hill CV, et al. Recruitment of older African Americans in Alzheimer’s disease clinical trials using a community education approach. J Prev Alzheimers Dis. 2022;9(4):672–678. doi: 10.14283/jpad.2022.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Cunningham-Erves J, Mayo-Gamble TL, Hull PC, Lu T, Barajas C, McAfee CR, et al. A pilot study of a culturally-appropriate, educational intervention to increase participation in cancer clinical trials among African Americans and Latinos. Cancer Causes Control CCC. 2021;32(9):953–963. doi: 10.1007/s10552-021-01449-7. [DOI] [PMC free article] [PubMed] [Google Scholar]