Abstract
Background
Postoperative complications are associated with reduced long-term survival. We characterise healthcare use changes after sentinel postoperative complications.
Methods
We linked primary and secondary care records of patients undergoing elective surgery at four East London hospitals (2012–7) with at least 90 days follow-up. Complication codes (wound infection, urinary tract infection, pneumonia, new stroke, and new myocardial infarction) recorded within 90 days of surgery were identified from primary or secondary care. Outcomes were change in healthcare contact days in the 2 yr before and after surgery, and 2 yr mortality. We report rate ratios (RaR) with 95% confidence intervals and adjusted for baseline healthcare use and confounders using negative binomial regression.
Results
We included 49 913 patients (median age 49 yr [inter-quartile range {IQR}: 34–64]), 27 958 (56.0%) were female. Amongst 3883 (7.8%) patients with complications (median age 58 [IQR: 43–72]), there were 18.4 days per year in contact with healthcare before surgery and 25.3 days after surgery (RaR: 1.38 [1.37–1.39]). Patients without complications (median age 48 [IQR: 33–63]) had 12.3 days per year in contact with healthcare before surgery and 14.0 days after surgery (RaR: 1.14 [1.14–1.15]). The adjusted incidence rate ratio of days in contact with healthcare associated with complications was 1.67 (1.49–1.87). More patients (391; 10.1%) with complications died within 2 yr than those without (1428; 3.1%).
Conclusions
Patients with postoperative complications are older with greater healthcare use before surgery. However, their absolute and relative increases in healthcare use after surgery are greater than patients without complications.
Keywords: epidemiology, health services research, perioperative medicine, postoperative complications, primary care
More than 5 million procedures are performed in the NHS each year.1 Death after surgery is uncommon, affecting around one in 100 patients by 90 days.1,2 However, complications after surgery are much more common, affecting around one in 10 patients after inpatient surgery.3 The incidence of complications varies depending on the type of surgery, how complications are defined, and the way in which data are collected.
The commonest complications after surgery are infectious, such as surgical site infection and lower respiratory tract infection.4 5 Less frequent and more serious complications include myocardial infarction and acute kidney injury.6, 7, 8, 9, 10 Patients with complications after surgery have a greatly increased risk of death during their hospitalisation.3 However, even those who survive the immediate affects of the complication have substantially reduced long-term survival.8 11 12 In addition, patients with complications have greater healthcare costs and longer lengths of hospital stay.13 14 Given the increased length of stay associated with complications, it is likely that healthcare use is elevated.
Patients undergoing surgery are increasingly older.15 As patients age, they accumulate chronic diseases and therefore use more healthcare.16 17 They also have a higher risk of complications after surgery, as do patients having major surgical procedures.3 As such, it is important to understand and take account of differing baseline healthcare use between patients with complications and those without. We have demonstrated previously that patients at high risk of early postoperative death have greater healthcare use before surgery but experience disproportionate increases in healthcare use after surgery compared with patients who are not at high risk of death.18
The aim of this study was to determine the association between specified postoperative complications on long-term healthcare use, including primary and secondary care. Specifically, we took account of baseline healthcare use to provide both absolute and relative measures of change.
Methods
Study design
We described previously the design and conduct of this linked healthcare registry data study.18 We included patients who underwent surgery at any Barts Health NHS Trust hospital and were registered with a general practitioner (GP) in a clinical commissioning group (CCG) area covered by the Discovery Data Service. The local CCG areas were Tower Hamlets, Newham, City and Hackney, and Waltham Forest in London, UK. The Discovery Data Service contains primary care, secondary care, unscheduled care, and community mental health records for patients. Data are collected from direct clinical care databases, for example, primary care records come directly from the electronic health record. These data are collected for direct patient care, governance, quality improvement, and research. For the purposes of this study, we identified primary care records of patients who underwent surgery at a Barts Health NHS Trust hospital. Records were linked using an established pseudonymisation process. We received approval from the Health Research Authority (reference: 19/HRA/0319) and Discovery Data Service board (dated: 24 September 2019) for this analysis. Data were held within a data security and protection toolkit-compliant computing environment. We report findings in line with the Reporting of studies Conducted using Observational Routinely collected health Data statement (Supplementary Appendix B).19 We developed a statistical analysis plan before analysis. No sample-size calculation was performed for this analysis of routinely collected data.
Cohort identification
We selected patients undergoing surgery at a Barts Health NHS Trust hospital using a previously described list of Office of Population Censuses and Surveys Classification of Interventions and Procedures version 4.7 codes (OPCS 4 codes),1 which we refined to four character versions.2 These are typically performed in an operating theatre, under regional or general anaesthesia, or involve insertion of a stent/device. We identified the first procedure for each patient within secondary care records between 1 January 2012 and 1 January 2017 after a 5 yr washout period. We restricted to those registered with a relevant GP practice. We excluded organ donation procedures, operative deliveries, and emergency admissions. We excluded emergency admissions using admission method codes as recorded in secondary care records.20
Cohort construction
The hospital episode associated with the first procedure was the index surgical episode. We linked to inpatient admission, outpatient, emergency department attendance, and primary care records for the 2 yr before and after surgery. Primary care records were extracted from the Discovery Data Service and inpatient admissions; outpatient and emergency department attendances were extracted from the Cerner Millennium data warehouse. The Cerner Millennium data warehouse contains secondary care records within Barts Health NHS Trust hospitals, including procedures, diagnoses, and process measures (e.g. length of hospital stay). Death data were extracted from the NHS Spine. We restricted all primary and secondary care encounters to the period of primary care registration to ensure we considered each patient's unique risk time.
Outcome measures
The primary outcome measure was the change in healthcare use in the 2 yr before and after surgery, reported as a rate ratio between the days in contact per patient year for each time point. The secondary outcome measure was 2 yr survival.
Exposure
The primary exposure was the occurrence of first complication within 90 days of surgery. The following complications were defined using Read Codes in primary care records and International Classification of Diseases, 10th Revision (ICD-10) codes in secondary care records (codes are listed in Supplementary Appendix A).
-
(i)
Wound infection
-
(ii)
Urinary tract infection
-
(iii)
Pneumonia
-
(iv)
New stroke
-
(v)
New myocardial infarction
These common complications were selected as sentinel events to enable us to explore their association with changes in healthcare use. We did not seek to provide a comprehensive description of postoperative complications, as this is available elsewhere.3
Variables
Age was defined as the number of completed years at the start of the index surgical admission. Sex was recorded as male or female. Procedures were grouped by anatomical location to one of 18 categories based on the first two digits of the primary OPCS 4 code.21 We categorised procedures as either involving an overnight stay or day case based on length of hospital stay. We identified ethnicity from primary care records and aggregated these to five ethnic categories (South Asian, Black, White, other, and missing) that align with the UK 2011 census groupings.22 We divided the cohort into national quintiles of the English index of multiple deprivation (IMD 2019), as described previously.18 23 Chronic diseases were identified using a modified version of the Charlson score, using ICD-10 codes in secondary care records, and using Read Codes in primary care records, including relevant Quality Outcome Framework register codes.24 25 We captured diagnoses from prior episodes in secondary care with a two yr lookback file, and at any time before surgery in primary care. Presence of a diagnostic code in either primary or secondary care was sufficient for diagnosis. Time to complication was measured in days from the date of index surgical procedure until the date of first diagnosis, restricted to 90 days after surgery.
Statistical analysis
We report the characteristics of included patients, stratified by the presence or absence of a complication. We restricted to patients with complete follow-up (i.e. at least 90 days of postoperative primary care registration) and present the characteristics of patients with incomplete follow-up. We present the proportion of patients with complications at 90 days.
We present the change in healthcare use, stratified by the presence or absence of complications. Healthcare use is expressed as number of days in contact with primary or secondary care per patient year. We include inpatient admissions, emergency department attendances, outpatient clinic appointments, and primary care encounters. We restricted all healthcare encounters to patients' primary care registration period and used this as the denominator. We determined the crude rate by dividing the total number of encounters across all patients by the total number of days of registration. We multiplied the crude rate by 365 to provide the number of days in contact per patient year. We present the cumulative rate of death within 2 yr. We present the crude and adjusted hazard ratios for 2 yr death; we adjusted for age and sex in a Cox proportional hazards model. Events were right censored at the end of the registration window. We estimated when healthcare use returned to a new baseline by calculating proportion of patient days with healthcare contact in the final 5 months of the study (i.e. Months 19–24) and identified when healthcare use came within 10% of this new baseline.
We adjusted for potential confounders of the association between complications and subsequent healthcare use with a multivariable regression model. Because of the highly variable frequency of healthcare encounter events, we used a negative binomial model. The dependent variable was the rate of healthcare use per patient year, and the independent variables were presence of any complication, age (modelled with a restricted cubic spline with three degrees of freedom), sex, presence of any chronic diseases, and procedure category. We also included patients' healthcare use in the 2 yr before surgery, which we modelled using a restricted cubic spline with five degrees of freedom. We present the incidence rate ratio associated with complications before and after adjustment. For each complication, we computed the unadjusted and adjusted incidence rate ratios using a negative binomial regression model. The unadjusted incidence rate ratio included baseline healthcare only, and the adjusted incidence rate ratios also included sex and age.
To explore how postoperative complications might independently influence long-term healthcare need, we did a post hoc sensitivity analysis amongst patients who developed pneumonia within 90 days of surgery. We identified patients who developed pneumonia in either primary or secondary care records with relevant codes (Supplementary Appendix A). We matched individuals with a logistic regression model, including age, ethnicity, IMD quintile, sex, chronic diseases, procedure group, and inpatient or day-case surgery as the independent variables and pneumonia as the dependent variable. For each patient with pneumonia, the five most similar patients were sampled with replacement. We present the healthcare use and risk of death, stratified by the presence or absence of pneumonia. All analyses were performed using R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria) and associated packages.26
Results
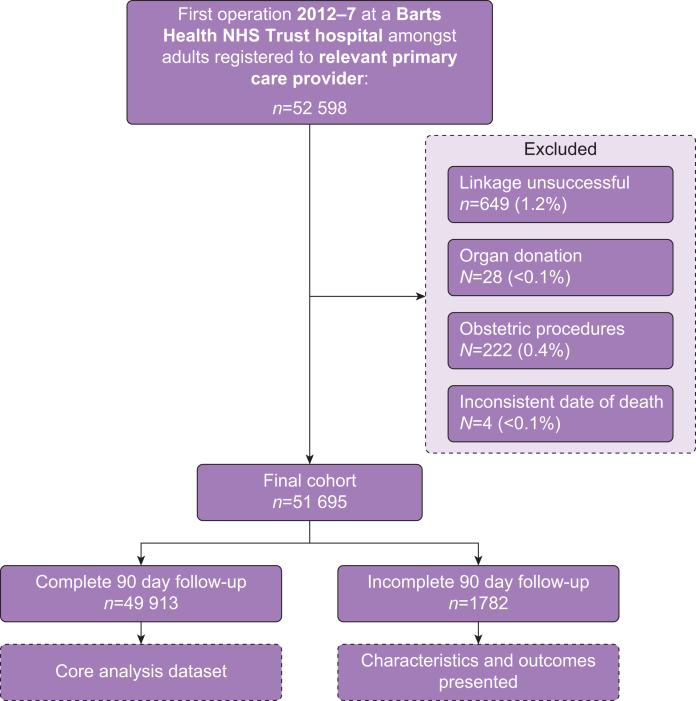
We identified 52 598 adults having their first elective procedure with a primary care provider in a relevant area, and linkage was successful for 51 949 records (98.8%). Of these, we excluded 28 (<0.1%) organ donation procedures, 222 obstetric procedures (0.4%), and four records with inconsistent date of death (<0.1%) (Fig 1). Of 51 695 eligible patients, 1782 (3.4%) had fewer than 90 days follow-up. These patients were excluded from the core analysis, and their characteristics and outcomes are summarised in Supplementary Tables 1 and 2. Aside from being younger (median age 38 [inter-quartile range {IQR}]: 28–56] yr) and having a lower burden of chronic disease (no diseases: 1108; 62.2%), the characteristics of excluded patients were similar to included patients. Excluded patients had a much lower rate of all complications (Supplementary Table 2).
Fig 1.
Flow of participant selection.
Characteristics of included patients
We included 49 913 patients with at least 90 days follow-up who had a median age of 49 yr (IQR: 34–64 yr), and 27 958 (56.0%) were female. Some 39 796 (79.7%) patients were in the lowest two quintiles of deprivation nationally, and the commonest ethnic category was White (23 539; 47.2%). Most procedures were female upper genitourinary tract procedures (5214; 10.4%), and 36 534 (73.2%) were performed on a day-case basis. The characteristics of patients, stratified by the occurrence of 90 day complications, are listed in Table 1.
Table 1.
Characteristics of included patients, stratified by the presence or absence of complications within 90 days of surgery. Data are presented as n (%) unless otherwise stated. Long-term diseases were captured from primary and secondary care data using Charlson index conditions. IQR, inter-quartile range; sd, standard deviation. ∗ numbers <7 suppressed for statistical disclosure control.
| All patients | Complication within 90 days |
||
|---|---|---|---|
| None | One or more | ||
| Number | 49 913 | 46 030 | 3883 |
| Age | |||
| Mean (sd) | 49.4 (18.2) | 48.8 (18.1) | 56.8 (17.8) |
| Median (IQR) | 49 (34–64) | 48 (33–63) | 58 (43–72) |
| Sex | |||
| Male | 21 955 (44) | 20 404 (44.3) | 1551 (39.9) |
| Female | 27 958 (56) | 25 626 (55.7) | 2332 (60.1) |
| Index of multiple deprivation (national quintile) | |||
| 1 (most deprived) | 14 274 (28.6) | 13 030 (28.3) | 1244 (32) |
| 2 | 25 522 (51.1) | 23 558 (51.2) | 1964 (50.6) |
| 3 | 7009 (14) | 6540 (14.2) | 469 (12.1) |
| 4 | 2278 (4.6) | 2126 (4.6) | 152 (3.9) |
| 5 (least deprived) | 756 (1.5) | 703 (1.5) | 53 (1.4) |
| Missing | 74 (0.1) | 73 (0.2) | (<0.1)∗ |
| Ethnic category | |||
| White | 23 539 (47.2) | 21 607 (46.9) | 1932 (49.8) |
| Asian | 13 482 (27) | 12 298 (26.7) | 1184 (30.5) |
| Black | 6593 (13.2) | 6173 (13.4) | 420 (10.8) |
| Other | 2674 (5.4) | 2520 (5.5) | 154 (4) |
| Missing | 3625 (7.3) | 3432 (7.5) | 193 (5) |
| Smoking status | |||
| Current | 10 982 (22) | 10 179 (22.1) | 803 (20.7) |
| Former | 12 810 (25.7) | 11 561 (25.1) | 1249 (32.2) |
| Never | 24 190 (48.5) | 22 410 (48.7) | 1780 (45.8) |
| Unknown | 1931 (3.9) | 1880 (4.1) | 51 (1.3) |
| Number of long-term diseases | |||
| 0 | 26 282 (52.7) | 25 024 (54.4) | 1258 (32.4) |
| 1 | 14 347 (28.7) | 13 151 (28.6) | 1196 (30.8) |
| 2 | 5836 (11.7) | 5106 (11.1) | 730 (18.8) |
| 3 | 2258 (4.5) | 1839 (4) | 419 (10.8) |
| >3 | 1190 (2.4) | 910 (2) | 280 (7.2) |
| Day-case or inpatient | |||
| Inpatient | 13 379 (26.8) | 11 458 (24.9) | 1921 (49.5) |
| Day case | 36 534 (73.2) | 34 572 (75.1) | 1962 (50.5) |
Incidence of complications
A specified complication occurred in 3883 patients within 90 days of surgery (7.8%). The commonest complication was urinary tract infection (n=1873; 3.8%), and new stroke was the least frequent (n=125; 0.3%) (Table 2). Patients with complications were older (median age 58 yr [IQR: 43–72]) than those without complications (median age 48 yr [IQR: 33–63]) (Table 1). One or more long-term diseases were suffered by 2625 (67.6%) patients who experienced complications compared with 21 006 (45.6%) of those without complications.
Table 2.
Incidence of first occurrence of specified complications within 30 or 90 days of surgery, and time to first occurrence, stratified by presence of relevant diagnostic code in primary or secondary care data. Data are presented as n (%) unless otherwise stated. Median times are in completed days and presented with inter-quartile range.
| Complication |
|||||
|---|---|---|---|---|---|
| Pneumonia | Wound infection | Urinary tract infection | New myocardial infarction | New stroke | |
| Number by 90 days | 1125 (2.3) | 897 (1.8) | 1871 (3.7) | 145 (0.3) | 124 (0.2) |
| Median time (IQR) | 30 (11–61) | 19 (11–34) | 31 (14–57) | 15 (5–45) | 35 (11–60.2) |
| Number by 30 days | 564 (1.1) | 630 (1.3) | 918 (1.8) | 99 (0.2) | 55 (0.1) |
Influence of complications on long-term healthcare use
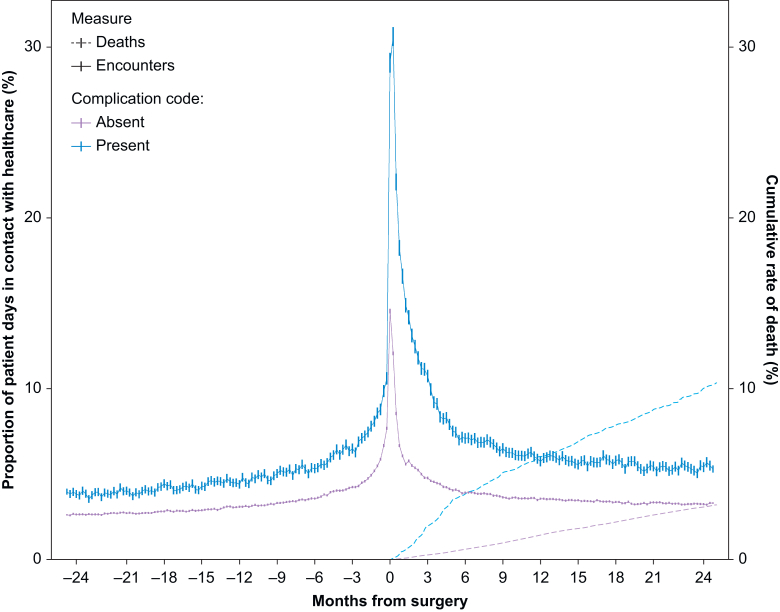
In the 2 yr before surgery, patients with complications had a higher burden of healthcare use (18.4 days per patient year [95% confidence interval {CI}: 18.3–18.5]) than patients without complications (12.3 days per patient year [95% CI: 12.3–12.3]). Data for the years after surgery exclude the number of days spent as an inpatient during the index hospital admission. In the 2 yr after surgery, patients with complications spent 25.3 days per patient year (95% CI: 25.2–25.4) in contact with a healthcare professional (rate ratio 1.38 [1.37–1.39]) (Table 3). Amongst patients without complications, 14.0 days per patient year (95% CI: 14.0–14.1) were spent in contact with a healthcare professional (rate ratio 1.14 [1.14–1.15]) (Fig 2). Most encounters were in primary care, but the largest increase occurred in hospital admissions or outpatient appointments (Table 3). Within the first 6 months after surgery, 44.9 days per patient year were spent in contact with a healthcare professional amongst patients with complications compared with 19.9 days amongst patients without complications (Supplementary Table 3). Healthcare use reached 10% of the final baseline at 47 weeks after surgery amongst those with complications compared with 36 weeks amongst those without (Supplementary Fig 1). We observed similar patterns of change in healthcare use across different ethnic categories (Supplementary Table 4). The healthcare use around surgery and the rate of death within 2 yr, stratified by type of complication, are listed in Supplementary Table 5.
Table 3.
Number of days in contact before and after surgery, stratified by type of encounter and presented by presence of complication codes. Data presented as encounters per patient year with associated 95% confidence intervals, unless otherwise stated. Before, 2 yr before surgery; after, 2 yr after surgery. ∗Excludes the days spent in hospital for index surgical admission. †P<0.05.
| Timing | Primary care encounters |
Secondary care encounters |
Total healthcare encounters |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Outpatient attendance |
Emergency department |
Hospital admissions |
|||||||||
| Before | After | Before | After | Before | After | Before | After∗ | Before | After∗ | Rate ratio | |
| All | 9.6 (9.6–9.6) | 9 (9–9.1) | 2.5 (2.4–2.5) | 3.9 (3.9–3.9) | 0.3 (0.3–0.3) | 0.4 (0.4–0.4) | 0.7 (0.7–0.7) | 2.8 (2.7–2.8) | 12.8 (12.7–12.8) | 14.9 (14.9–14.9) | 1.17 (1.16–1.17)† |
| Complication code | |||||||||||
| Absent | 9.3 (9.2–9.3) | 8.6 (8.6–8.6) | 2.4 (2.4–2.4) | 3.7 (3.7–3.7) | 0.3 (0.3–0.3) | 0.4 (0.4–0.4) | 0.6 (0.6–0.7) | 1.9 (1.9–1.9) | 12.3 (12.3–12.3) | 14.0 (14.0–14.1) | 1.14 (1.14–1.15)† |
| Present | 13.6 (13.5–13.7) | 14.6 (14.5–14.7) | 3.2 (3.2–3.3) | 5.5 (5.5–5.6) | 0.4 (0.4–0.4) | 0.8 (0.8–0.8) | 1.6 (1.6–1.6) | 5.6 (5.5–5.6) | 18.4 (18.3–18.5) | 25.3 (25.2–25.4) | 1.38 (1.37–1.39)† |
Fig 2.
Proportion of patients spending a day in contact with a healthcare professional in the 2 yr before and after surgery, and the cumulative rate of death, stratified by the presence of complication codes. Data aggregated by 7 day (week) windows, each of which has 95% confidence intervals.
Adjusted rate ratio of healthcare use after surgery
The unadjusted incidence rate ratio of healthcare use after surgery was 2.14 (95% CI: 2.08–2.21) amongst patients with complications compared with those without complications. The multivariable adjusted incidence rate ratio was 1.67 (95% CI: 1.49–1.87). The multivariable model is summarised in Supplementary Table 6. For an average patient aged 64 yr with preoperative healthcare use of 15 days in 2 yr, 23 (23–25) days would be expected in the 2 yr after surgery. A similar patient with a complication would expect 33 (31–34) days over the same period. The unadjusted and adjusted incidence rate ratios of healthcare use in the 2 yr after surgery, stratified by type of complication, are listed in Supplementary Table 5. There was a significant interaction between age and complications for patients aged under 58 yr, indicating complications have a greater relative influence in younger patients.
Death after complications
Overall, 1819 (3.6%) patients died within 2 yr. Amongst 3888 patients with complications, 391 (10.1%) died in 2 yr compared with 1428 of 46 025 (3.1%) patients without complications (Supplementary Table 3). The crude hazard ratio for death within 2 yr amongst those with complications was 3.4 (95% CI: 3.1–3.8). The age and sex adjusted hazard ratio for death within 2 yr was 2.3 (95% CI: 2.0–2.6).
Sensitivity analysis: propensity matched analysis of patients with pneumonia
Pneumonia within 90 days of surgery occurred amongst 1125 (2.3%) patients. Patients who developed pneumonia were significantly older (median age 62 yr [IQR: 49–74]) than those who did not develop pneumonia (median age 48 yr [IQR: 34–63]). Patients who developed pneumonia had a higher healthcare need before surgery (20.0 days [95% CI: 19.8–20.2 days]) compared with those who did not develop pneumonia (12.6 days [95% CI: 12.6–12.6 days]).
To account for the differing baseline, we did an exploratory propensity matched sensitivity analysis. We matched 5625 patients to the 1125 patients who developed pneumonia, and their characteristics are listed in Supplementary Table 7. The time spent in contact with a healthcare professional was 20.0 days per patient year (95% CI: 19.8–20.2) in the 2 yr before surgery and 32.6 days (32.4–32.8 days; rate ratio 1.63 [1.61–1.65]) after surgery amongst patients with pneumonia. Patients in the matched cohort spent 16.3 (16.3–16.4) days before and 22.8 (22.7–22.9 days; rate ratio 1.39 [1.39–1.40]) after surgery in contact with a healthcare professional. The rate of death by 2 yr was 9.7% amongst those in the matched cohort and 16.0% in the pneumonia cohort. Most of the increased healthcare need associated with pneumonia occurred in the first 6 months after the operation (pneumonia: 55.0 days per patient year vs matched group: 33.5 days) (Supplementary Table 8; Supplementary Fig 2). By the final 6 month period (Days 548–730 after surgery), patients with pneumonia had 22.2 days in contact compared with 17.8 amongst those without pneumonia.
Discussion
The principal finding of this large regional cohort study was that selected complications after elective surgery were associated with substantially greater healthcare use, both in absolute terms and relative to baseline healthcare use. By using precise linkage of hospital and primary care records, we were able to measure the temporal change in healthcare use before and after surgery. The increase in healthcare use after surgery amongst patients with complications was greatest in the first 6 months after surgery but persisted throughout the 2 yr period we examined. Patients with complications had a three-fold higher rate of death than those without. Whilst patients with complications were older, had a higher burden of comorbid disease, and had higher preoperative healthcare use, they suffered a disproportionate rise in healthcare use after complications. After adjusting for age comorbidity and differing preoperative healthcare use, our findings were unchanged. To further account for the differing characteristics of patients with complications, we explored a sentinel complication (pneumonia) in a propensity matched analysis. Patients experiencing postoperative pneumonia had persistently increased healthcare use after surgery and a three-fold higher rate of death than similar patients without pneumonia.
The overall rate of complications we observed was lower than in prior studies of mixed surgical populations. For example, in an international prospective cohort study of 44 000 patients undergoing inpatient elective surgery, complications were reported for 16.8% of patients within 30 days of surgery.3 However, one-third of these were unspecified complications, which we would not be able to capture through coding data alone. We pre-specified important postoperative complications that could be identified in both primary and secondary care using diagnostic codes. These were selected as common complications to explore the hypothesis that complications are associated with greater postoperative healthcare use. When we consider the complications we specified, the rate of pneumonia in the International Surgical Outcomes Study was 1.6% and amongst inpatients in our study was 4.4%. The increased incidence in our cohort is likely because of the longer follow-up in our study (90 days) and the inclusion of primary care data. Whilst many studies report 30 day infection, our findings would suggest that the rate of complications remains elevated over the subsequent 90 day period, which aligns with a recent study of patients in the USA.27 When we stratified by type of complication, the infectious complication associated with the greatest cumulative rate of death and increase in healthcare use was pneumonia. However, urinary tract infection and wound infection were both associated with increases in healthcare use of between one and two-thirds. Whilst our study is unable to establish a causal relationship between complications and long-term healthcare use given the potential for unmeasured confounding, it adds to the substantial literature demonstrating the poor long-term health outcomes associated with postoperative complications.8 12, 13, 14 27 Our data highlight the attention provided in primary care before and after surgery. Whilst the largest relative change in healthcare encounters was within secondary care, primary care still accounted for most encounters, even amongst patients with complications.
The occurrence of a postoperative complication is more strongly associated with long-term death than underlying chronic diseases.11 The findings of our adjusted death analysis align with a recent pooled analysis of two cohort studies we undertook.12 The influence of complications on long-term healthcare use after adjustment was relatively greater than all chronic diseases except for cancer. This is likely because of ongoing treatment of patients with cancer, including chemotherapy and radiotherapy, which would result in a consistent increase in healthcare need. However, patients with complications were older, had a higher burden of chronic disease, typically underwent cardiac or thoracic procedures, and had greater healthcare use before surgery. As such, the observed association may have been confounded because patients with complications were already predisposed to greater healthcare use before developing a complication. We explored this with both a multivariable regression and a propensity matched analysis amongst patients with pneumonia. An observational study, such as ours, cannot definitively determine if associations are causative. However, our findings suggest that some of the long-term harm experienced by high-risk patients may be mediated by complications. Most excess healthcare use amongst patients with pneumonia was in the first 6–12 months after surgery. These findings suggest that in addition to reduced long-term survival, patients with complications also have a higher burden of healthcare use after surgery. This increase is both greater in absolute terms than those without complications, and disproportionately higher relative to their preoperative baseline.
Strengths and weaknesses
This study has strengths. First, we used a robust linkage infrastructure to generate a detailed dataset of linked primary and secondary care records. Most healthcare in the UK is provided by primary care providers, and these records provide rich, detailed understanding of the surgical population. Specifically, capture of chronic diseases within primary care records is likely more complete than secondary care records, and we anticipate that more postoperative infections will be treated within primary care.28 29 Second, we used a reproducible definition of surgery based on OPCS codes that we have described and used previously. Third, we used a consistent risk-time measure based on GP registration. We excluded some 4% of records that had incomplete 90 day follow-up time. These patients had low rates of infection, which likely relates to their primary care registration being outside the Discovery Data Service coverage area in the immediate postoperative period. Fourth, we planned our analysis, including the specific complications we describe, and the method of determining risk-time.
This study also has some potential limitations. First, in any study of routinely collected data, there is a risk of information bias. However, the rates of complications we identified are comparable with other studies, and the influence of those complications on long-term survival was similar. Second, we included only the first operation per patient, which means some patients may have gone on to have subsequent procedures during the follow-up period. However, this enabled longitudinal follow-up before and after surgery, which was the key aim of our study. Third, misclassification of the primary exposure (complication) may occur if chronic diagnoses are confused for acute conditions. We minimised this by restricting complications to only those that occurred after surgery, which, in elective patients, should reliably capture only postoperative complications. We also reduced this risk by excluding patients with a prior diagnosis of stroke or myocardial infarction from our assessment of these rare, but important, cardiovascular complications. As such, we anticipate that our capture of cardiovascular complications represents an under-estimate. We selected a representative set of important complications based on previous epidemiological studies to explore the association between them and subsequent healthcare use. Our aim was not to describe the incidence of complications after surgery, particularly because some complications (e.g. bleeding) are likely to be poorly captured within routine coding data. The East London population also has a higher burden of chronic disease at a younger age, which may limit the external generalisability of our findings.
Future work and conclusions
Complications after surgery are associated with a substantial increase in healthcare need that is most prominent in the first 6 months after surgery. This increase in healthcare use is likely to be associated with substantial financial costs to the healthcare system and direct impairments to quality of life for patients. Whilst the extent to which complications can be prevented and their causative influence on long-term healthcare cannot be precisely established, this study provides further evidence that patients with short-term surgical complications suffer persistent long-term harm. Surgical complications thus represent a key target for both primary and secondary treatment interventions to improve long-term outcomes in perioperative medicine.
Authors’ contributions
Study design: all authors
Data collection/analysis: AJF, ABB
Data interpretation: all authors
Writing of first draft of paper: AJF, JRP
Revising of paper for important intellectual content: all authors
Approval of final version of paper: all authors
Access to data: AJF, JRP
Data guarantee: AJF, JRP
Acknowledgements
The authors would like to thank Leslie Everest (patient representative) for her time and thoughtful input to the design of this study, and Dr Kambiz Boomla and Dr Bhavi Trivedi for their assistance with study design and conduct. The authors acknowledge and thank all patients, clinicians, coders, and support staff involved in the generation and collection of data. The funding source had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Declarations of interest
AJF holds a National Institute for Health and Care Research Doctoral Research Fellowship (DRF-2018-11-ST2-062). RMP has received honoraria or research grants from Edwards Lifesciences, Intersurgical, and GlaxoSmithKline within the past 5 yr and holds editorial roles with the British Journal of Anaesthesia and the British Journal of Surgery. ABB and JRP report no relevant conflicts of interest.
Funding
National Institute for Health and Care Research Doctoral Research Fellowship (DRF-2018-11-ST2-062 to AJF)
Handling Editor: Phil Hopkins
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.bjao.2023.100142.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Abbott T.E.F., Fowler A.J., Dobbs T.D., Harrison E.M., Gillies M.A., Pearse R.M. Frequency of surgical treatment and related hospital procedures in the UK: a national ecological study using hospital episode statistics. Br J Anaesth. 2017;119:249–257. doi: 10.1093/bja/aex137. [DOI] [PubMed] [Google Scholar]
- 2.Fowler A.J., Wahedally M.A.H., Abbott T.E.F., et al. Death after surgery among patients with chronic disease: prospective study of routinely collected data in the English NHS. Br J Anaesth. 2022;128:333–342. doi: 10.1016/j.bja.2021.11.011. [DOI] [PubMed] [Google Scholar]
- 3.International Surgical Outcomes Study Group Global patient outcomes after elective surgery: prospective cohort study in 27 low-, middle- and high-income countries. Br J Anaesth. 2016;117:601–609. doi: 10.1093/bja/aew316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wan Y., Patel A., Achary C., Hewson R., Phull M., Pearse R. Postoperative infection and mortality following elective surgery in the International Surgical Outcomes Study (ISOS) Br J Surg. 2021;108:220–227. doi: 10.1093/bjs/znaa075. [DOI] [PubMed] [Google Scholar]
- 5.Bhangu A., Ademuyiwa A., Aguilera M., et al. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infect Dis. 2018;18:516–525. doi: 10.1016/S1473-3099(18)30101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prowle J.R., Forni L.G., Bell M., et al. Postoperative acute kidney injury in adult non-cardiac surgery: joint consensus report of the Acute Disease Quality Initiative and PeriOperative Quality Initiative. Nat Rev Nephrol. 2021;17:605–618. doi: 10.1038/s41581-021-00418-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaudery H., MacDonald N., Ahmad T., et al. Acute kidney injury and risk of death after elective surgery: prospective analysis of data from an international cohort study. Anesth Analg. 2019;128:1022–1029. doi: 10.1213/ANE.0000000000003923. [DOI] [PubMed] [Google Scholar]
- 8.STARSurg Collaborative Impact of postoperative acute kidney injury in patients undergoing major gastrointestinal surgery on 1-year survival and renal outcomes: a national multicentre cohort study. BJS Open. 2021;5:zrab134. doi: 10.1093/bjsopen/zrab134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abbott T.E.F., Pearse R.M., Archbold R.A., et al. A prospective international multicentre cohort study of intraoperative heart rate and systolic blood pressure and myocardial injury after noncardiac surgery: results of the VISION study. Anesth Analg. 2018;126:1936–1945. doi: 10.1213/ANE.0000000000002560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pandey A., Sood A., Sammon J.D., et al. Effect of preoperative angina pectoris on cardiac outcomes in patients with previous myocardial infarction undergoing major noncardiac surgery (data from ACS-NSQIP) Am J Cardiol. 2015;115:1080–1084. doi: 10.1016/j.amjcard.2015.01.542. [DOI] [PubMed] [Google Scholar]
- 11.Khuri S.F., Henderson W.G., DePalma R.G., Mosca C., Healey N.A., Kumbhani D.J. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:323–326. doi: 10.1097/01.sla.0000179621.33268.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fowler A.J., Wan Y.I., Prowle J.R., et al. Long-term mortality following complications after elective surgery: a secondary analysis of pooled data from two prospective cohort studies. Br J Anaesth. 2022;129:588–597. doi: 10.1016/j.bja.2022.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Straatman J., Cuesta M.A., de Lange-de Klerk E.S.M., van der Peet D.L. Hospital cost-analysis of complications after major abdominal surgery. Dig Surg. 2015;32:150–156. doi: 10.1159/000371861. [DOI] [PubMed] [Google Scholar]
- 14.Vonlanthen R., Slankamenac K., Breitenstein S., et al. The impact of complications on costs of major surgical procedures: a cost analysis of 1200 patients. Ann Surg. 2011;254:907–913. doi: 10.1097/SLA.0b013e31821d4a43. [DOI] [PubMed] [Google Scholar]
- 15.Fowler A.J., Abbott T.E.F., Prowle J., Pearse R.M. Age of patients undergoing surgery. Br J Surg. 2019;106:1012–1018. doi: 10.1002/bjs.11148. [DOI] [PubMed] [Google Scholar]
- 16.Hing E., Cherry D.K., Woodwell D.A. National Ambulatory medical care survey: 2004 summary. Adv Data. 2006;372:1–33. [PubMed] [Google Scholar]
- 17.Kuan V., Denaxas S., Gonzalez-Izquierdo A., et al. A chronological map of 308 physical and mental health conditions from 4 million individuals in the English National Health Service. Lancet Digit Health. 2019;1:e63–e77. doi: 10.1016/S2589-7500(19)30012-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fowler A.J., Trivedi B., Boomla K., Pearse R.M., Prowle J.R. Change in healthcare use after surgical treatment: observational study of routinely collected patient data from primary and secondary care. Br J Anaesth. 2022;129:889–897. doi: 10.1016/j.bja.2022.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Benchimol E.I., Smeeth L., Guttmann A., et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12 doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.HES data dictionary 2021. https://datadictionary.nhs.uk/supporting_information/hes_data_dictionary.html NHS Data Model and Dictionary. (Accessed 5 June 2023)
- 21.Fowler A.J., Dobbs T.D., Wan Y.I., et al. Resource requirements for reintroducing elective surgery during the COVID-19 pandemic: modelling study. Br J Surg. 2021;108:97–103. doi: 10.1093/bjs/znaa012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.2008. Harmonised concepts and questions for social data courses: primary standard—ethnic group.https://www.ons.gov.uk/methodology/classificationsandstandards/measuringequality/ethnicgroupnationalidentityandreligion/ Office for National Statistics. (Accessed 5 June 2023) [Google Scholar]
- 23.2019. England indices of deprivation.https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 Ministry of Housing Communities and Local Government. (Accessed 5 June 2023) [Google Scholar]
- 24.Metcalfe D., Masters J., Delmestri A., et al. Coding algorithms for defining Charlson and Elixhauser co-morbidities in Read-coded databases. BMC Med Res Methodol. 2019;19:115. doi: 10.1186/s12874-019-0753-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Armitage J.N., van der Meulen J.H. Identifying co-morbidity in surgical patients using administrative data with the Royal College of Surgeons Charlson Score. Br J Surg. 2010;97:772–781. doi: 10.1002/bjs.6930. [DOI] [PubMed] [Google Scholar]
- 26.2019. R: a language and environment for statistical computing.https://www.r-project.org/ R Core Team. (Accessed 5 June 2023) [Google Scholar]
- 27.Brown C.S., Montgomery J.R., Neiman P.U., et al. Assessment of potentially preventable hospital readmissions after major surgery and association with public vs private health insurance and comorbidities. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.5503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gallagher A.M., Williams T., Leufkens H.G.M., de Vries F. The impact of the choice of data source in record linkage studies estimating mortality in venous thromboembolism. PLoS One. 2016;11 doi: 10.1371/journal.pone.0148349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Williams R., van Staa T.-P., Gallagher A.M., Hammad T., Leufkens H.G.M., de Vries F. Cancer recording in patients with and without type 2 diabetes in the Clinical Practice Research Datalink primary care data and linked hospital admission data: a cohort study. BMJ Open. 2018;8 doi: 10.1136/bmjopen-2017-020827. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.