Abstract
Purpose
Supracondylar humeral fractures (SCHFs) rank among the frequently observed fractures in children. Nonetheless, there exists a dearth of consensus regarding the optimal surgical approach. This meta-analysis aims to thoroughly evaluate and compare two distinct pinning techniques (cross pinning versus lateral pinning) for SCHFs, using data from Randomized controlled trials (RCTs).
Methods
Literature review was done using PubMed, CINAHL, Scopus, and The Cochrane Library for RCTs comparing the two pinning methods and providing information on at least one of the following: Loss of Baumann's angle, loss of carrying angle, elbow function assessed based on Flynn criteria, pin tract infection, and iatrogenic ulnar nerve injury. Random effect model was used to calculate standardized mean difference or Odds Ratio (OR) for the outcomes. Review Manager 5.4.1. was used to perform quality assessment and statistical analysis.
Results
A total of 22 RCTs were included. 20 studies reported data for iatrogenic ulnar nerve injury, the OR was calculated to be 3.76 (95% CI 1.75–8.06), showing a significantly lower risk of surgical ulnar nerve injury with the lateral technique. However, no significant difference was found between the pinning techniques in regard to the other outcomes.
Conclusion
In comparison to lateral pinning, the utilization of cross pinning technique exposes the patient to a heightened susceptibility of iatrogenic nerve injury. Therefore, it is recommended that surgeons prioritize the implementation of the lateral pinning technique whenever feasible, as it offers greater protection against iatrogenic ulnar nerve injury. For the other intraoperative and postoperative outcomes, both surgical techniques yield comparable results.
Keywords: Supracondylar distal humeral fracture, Elbow, Elbow fractures, Meta-analysis, Randomized controlled trial, Ulnar nerve, Orthopedic surgery
1. Introduction
Supracondylar humeral fractures (SCHFs) are frequently observed among pediatric patients and represent the most prevalent form of elbow fracture within this age group.1,2 This phenomenon can be attributed to the inherent characteristics of the pediatric skeleton, which includes a comparatively fragile metaphyseal sclerotin in the lower part of the humerus and a fragile bony ridge that separates the olecranon and coronoid fossa. Furthermore, the elbow joint's structural composition, prone to bending, contributes to the increased susceptibility to SCHFs. Notably, the majority of SCHFs occur as extension-type fractures, with the primary causative factor being a fall onto an outstretched hand.3 Classification of these fractures is commonly performed using Gartland's criteria.4
The preferred method of addressing SCHF primarily involves closed reductions and percutaneous pinning(s).5 However, in cases where there is a significant displacement and angulation of the fracture, open reduction with percutaneous pinning may be warranted. Currently, two techniques are commonly employed for percutaneous pinning: the lateral pinning method and the cross-pinning method.6 In the lateral pinning approach, the pins are inserted from the lateral aspect of the humerus, typically through the lateral epicondyle, and are directed towards the medial side of the bone. The pins traverse the fracture site, providing stability and maintaining proper alignment of the fractured fragments. In cross pinning approach, two pins are inserted from opposite sides of the humerus, typically from the lateral and medial aspects, and they intersect within the fracture site. The pins create a cross-like configuration, providing enhanced stability and alignment of the fractured fragments. It is important to note that while cross pinning theoretically offers a more stable configuration, it carries the potential hazard of iatrogenic ulnar nerve injuries, thus necessitating careful consideration and evaluation.7,8
Over the past decade, various systemic reviews and meta-analyses have been conducted with the aim of establishing a consensus regarding the optimal pinning technique following closed reduction. These studies primarily focused on Gartland type II and III displaced SCHFs.3,9, 10, 11, 12, 13, 14 The primary focus of this meta-analysis is to comprehensively compare the two pinning techniques exclusively using data derived from Randomized Controlled Trials (RCTs). RCTs are widely regarded as the benchmark in scientific research due to their ability to minimize author bias, thus providing the highest level of evidence. The selected outcomes for comparison in this study primarily focus on postoperative elbow functionality assessment, including measurements such as loss of carrying angle, Baumann's angle, and evaluation based on Flynn criteria. Furthermore, additional factors such as iatrogenic ulnar nerve injury and pin tract infection were also analyzed to offer a comprehensive evaluation.
2. Methods
This study is a systematic review and meta-analysis and does not require either ethical approval or patient consent. This article was completed as per PRSIMA guidelines.15 This systematic review was conducted based on a comprehensive, written protocol that prespecified the research question, search strategy, risk of bias assessment, and inclusion/exclusion criteria.
2.1. Search strategy
Four different electronic databases were used that is PubMed, Scopus, CINAHL, and the Cochrane library to perform the literature review. The literature review was performed from inception to May 2022. The terms used to form a search string for literature review were “Supracondylar fracture”, “Supra condylar fracture”, “supra-condylar fracture”, “humerus fracture”, “humeral fracture”, “children”, “pediatric”, and “pediatrics”. Boolean gates (“AND” and “OR”) were used to form the search string. Two independent authors performed the literature review, and any disagreement was solved by a third unbiased author. The same two authors also performed the data extraction, the data was extracted as per a predefined proforma, which included information such as author, year of publication, number of patients, mean age, grade of fracture, Flynn criteria, loss of carrying angle, Baumann's angle, iatrogenic ulnar nerve injuries, and number of pin tract infections. Any disagreement in data extraction between the authors was solved by a third unbiased author.
2.2. Selection criteria
The inclusion criteria were based on the PICOS method. Population: Pediatric population (age less than 15 years) with SCHF. Intervention: Cross pinning technique. Comparator: Lateral pinning technique. Outcomes: Loss of Baumann's angle, loss of carrying angle, elbow function assessed based on Flynn criteria, pin tract infection, and iatrogenic ulnar nerve injury. Study design: RCTs published in English language.
Studies with incomplete data that hindered a comprehensive assessment of the outcomes, studies with vague or ambiguous inclusion criteria that did not precisely define the characteristics of the participants, studies that included an adult population or failed to specify the cut-off age for the included participants, and studies that did not quantify the relevant outcomes of interest were excluded.
2.3. Outcomes
Baumann's angle was taken as the angle formed “between the long axis of the humerus and a line through the physis of the lateral condyle of the distal humerus”.16 Loss of carrying angle also known as cubitus varus, refers to a deformity or deviation of the elbow joint where the forearm deviates towards the body more than normal. It is characterized by a decreased or negative value of Baumann's angle. Flynn's criteria for grading the outcome for SCHF which incorporates both cosmetic and functional factors. Loss of Baumann's angle was defined as per the definition provided by the included studies. Cosmetic Factor: Excellent; No visible deformity (less than 5° loss of motion) or cosmetic concerns (less than 5° cubitus angle loss). Good; Minimal or barely noticeable deformity (6–10° loss of motion) that does not significantly affect appearance (6–10° cubitus angle loss). Fair; Noticeable deformity (11–15° loss of motion) that may affect appearance but is generally acceptable (11–15° cubitus angle loss). Poor; Significant deformity (more than 15° loss of motion) that visibly impacts appearance and may cause self-consciousness (more than 15° cubitus angle loss). Pin tract infection was defined as an infection that develops at the site of a pin or wire inserted into the humerus during either pinning techniques. Iatrogenic ulnar nerve injury was characterized as injury to ulnar nerve during the surgical intervention.
2.4. Statistical analysis
The statistical analysis was conducted on RevMan 5.4.1, the two kinds of data that were assessed were continuous and binary data. To analyze continuous data, a random-effects model utilizing the inverse variance statistical method was employed and the results were calculated with a standardized mean difference (SMD) with a 95% Confidence Interval (CI). To analyze binary data, a random-effects model was used to combine the results from multiple studies. The inverse variance method was applied to calculate the weights for each study, and the effect measure chosen to represent the binary outcomes was the Odds Ratio (OR) along with its corresponding 95% CI. For both types of data heterogeneity across the trials was calculated using Higgins I2, low heterogeneity was defined as “p > 0.1, I2 <50%”. Sensitivity analysis was used to define the reason for heterogeneity where necessary by removing each included study one at a time and reevaluating the result.
2.5. Quality assessment and publication bias
The evaluation of the level of quality was estimated by two independent authors using the Cochrane risk of bias 2.0 tool for RCTs in Review Manager 5.4.1. We assessed the publication bias using Begg's funnel plot.
3. Results
3.1. Demographics
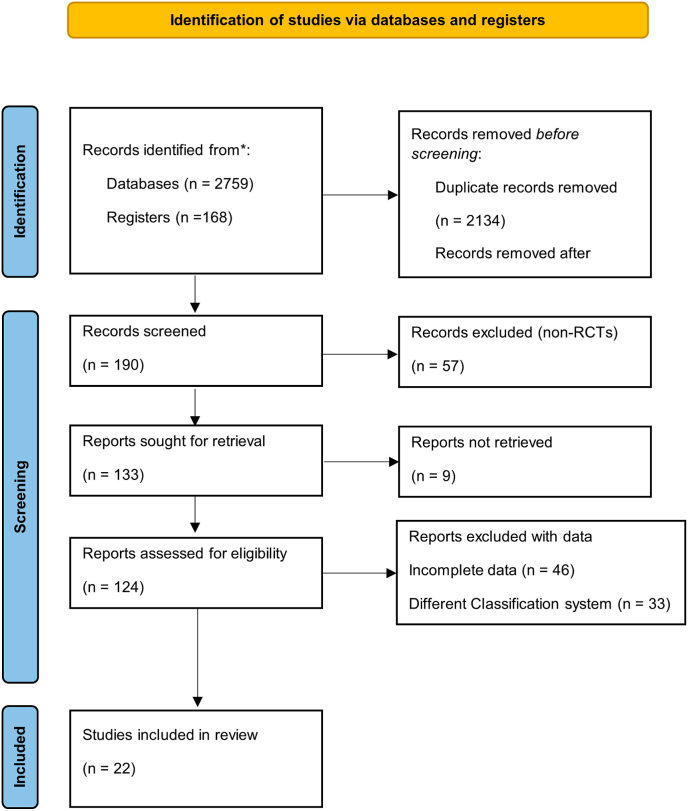
A total of 2927 articles were detected from the said databases and registers, after title and abstract screening 190 articles were left, whereas after full text review only 22 articles were found to follow our inclusion criteria1,17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37 and were hence included in this review (Fig. 1). The study encompassed a cohort of 1502 patients diagnosed with SCHF, with an average age of 6.5 years. While certain studies omitted explicit mention of the average age, they provided information regarding the age range of the participants. The majority of the patients had Gartland type II and Gartland type III SCHFs. The other demographic details were also comparable across the studies (Table 1).
Fig. 1.
PRISMA Flowchart. The PRIMSA diagram describes our search and selection process applied during the overview.
Table 1.
Demographics.
| Author Year | Number of patients (n) |
Age in years (SD) |
Gartland Fracture type |
Fracture type | |||
|---|---|---|---|---|---|---|---|
| CPG* | LPG** | CPG | LPG | CPG | LPG | ||
| Maity 2012 | 80 | 80 | 6.2 (1.8) | 6.1 (1.8) | II, III | II, III | Extension |
| Prashant 2016 | 31 | 31 | 8.55 | 8.25 | III | III | Extension |
| Karim 2016 | 30 | 30 | NA | NA | II, III | Extension | |
| Ducic 2016 | 71 | 67 | 6.7 (1.6) | 6.5 (1.8) | II, III | II, III | Extension |
| Naik 2017 | 29 | 28 | 6.3 (2.0) | 7.2 (2.2) | III | III | Extension |
| Kocher 2007 | 24 | 28 | 5.7 (1.6) | 6.1 (1.5) | III | III | Extension |
| Foaed 2004 | 28 | 27 | 5.8 | 5.8 | II, III | Extension | |
| Gaston 2010 | 57 | 47 | 6.2 | 5.7 | III | III | Extension |
| Tripuraneni 2009 | 20 | 20 | 5.5 | 4.3 | II, III | II, III | Extension |
| Anwar 2011 | 25 | 25 | 7.0 (1.3) | 7.0 (1.3) | II, III | Extension | |
| Patel 2018 | 31 | 29 | 6.2 (2.2) | 5.8 (3.4) | III | III | Extension |
| Afaque 2020 | 40 | 37 | 7.2 (0.8) | 6.8 (0.9) | II, III, IV | Extension | |
| Jain 2019 | 84 | 84 | NR | NR | II, III | Extension | |
| Shah 2013 | 100 | 100 | 6.5 (2.3) | 5.8 (1.8) | II, III | Extension | |
| Naveen 2017 | 20 | 20 | 7.4 (2.7) | 7.6 (2.5) | II, III | II, III | Extension |
| Ahmad 2020 | 35 | 35 | NR | I, II | I, II | Extension | |
| Dawood 2011 | 11 | 10 | 6.5 | III | III | Extension | |
| Aher 2018 | 30 | 30 | 7 | III | III | Extension | |
| Othman 2017 | 16 | 14 | 5.5 (2.8) | II, III | Extension | ||
| Kalia 2018 | 30 | 30 | 6.73 | II, III | Extension | ||
| Arun 2018 | 30 | 38 | 8.4 | III | III | Extension | |
| Gholap 2020 | 15 | 15 | 6.83 | III | III | Extension | |
CPG* = Cross Pinning Group, LPG** = Lateral pinning group, I = Gartland Type 1, II = Gartland type 2, III = Gartland type 3, IV = Gartland type 4, NR = Not reported.
3.2. Outcomes
3.2.1. Flynn criteria
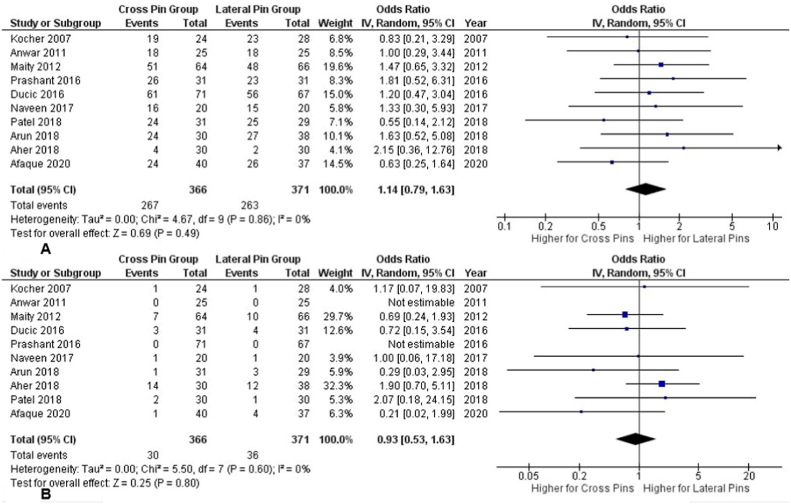
Ten studies17, 18, 19, 20,24, 25, 26,29,32,35 assessed Flynn criteria postoperatively on patients. Analysis was performed for “Excellent” and “Poor” outcomes. No significant difference between the two groups was observed for the "excellent" outcome, as indicated by the calculated OR of 1.14 (95% CI 0.79–1.63) and a Z-score of 0.69 (P = 0.49). There was no significant heterogeneity (P = 0.86, I2 = 0%) (Fig. 2A). No significant difference was observed between the two groups for the "poor" outcome, as indicated by the calculated OR of 0.93 (95% CI 0.53–1.63) and a Z-score of 0.25 (P = 0.80). Additionally, no significant heterogeneity was found between the studies (P = 0.60, I2 = 0%) (Fig. 2B).
Fig. 2.
Forest Plot (A) A Forest plot showing a comparison of the excellent outcome of Flynn's criteria between the cross entry and lateral entry groups. Odds Ratio was 1.14 (95% CI 0.79–1.63) showing no significant difference between the techniques. (B) A Forest plot showing a comparison of the poor outcomes of Flynn's criteria between cross entry and lateral entry groups. Odds Ratio was calculated as 0.93 (95% CI 0.53–1.63) showing no significant difference between the techniques.
3.2.2. Ulnar nerve injury
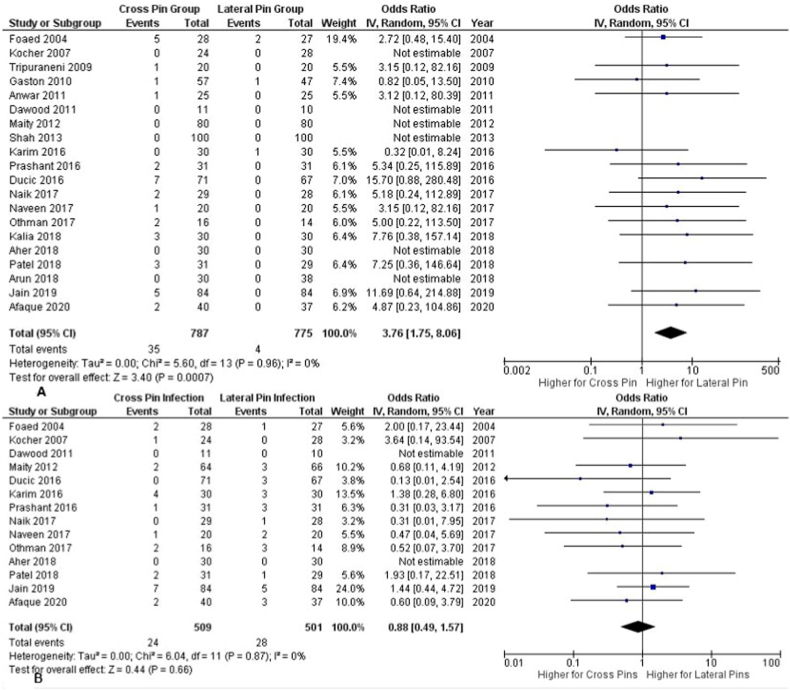
Twenty studies1,17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29,31, 32, 33, 34, 35,37 reported data for postoperative ulnar nerve injury. The OR was calculated to be 3.76 (95% CI 1.75–8.06), the Z-score for the overall effect was 3.40 (P = 0.0007), the results show a significant difference between the two interventions, showing that lateral pinning has a lesser incidence of iatrogenic ulnar nerve injury. No significant heterogeneity was found (P = 0.96, I2 = 0%) (Fig. 3A).
Fig. 3.
Forest Plot (A) A Forest plot showing a comparison of the ulnar nerve injury between the cross entry and the lateral entry groups. Odds Ratio was 3.76 (95% CI 1.75–8.06) showing a significant difference between the techniques (B) A Forest plot showing a comparison of the pin tract infection between the cross entry and the lateral entry groups. Odds Ratio was 0.88 (95% CI 0.49–1.57) showing a significant difference between the techniques.
3.2.3. Pin tract infection
Fourteen studies1,17, 18, 19, 20, 21,25, 26, 27,29,31, 32, 33,37 evaluated the data regarding postoperative pin tract infection. The calculated OR was 0.88 (95% CI 0.49–1.57), and the Z-score for the overall effect was 0.44 (P = 0.66), indicating no significant difference amongst the techniques. Furthermore, significant heterogeneity was not observed between the studies (P = 0.87, I2 = 0%) (Fig. 3B).
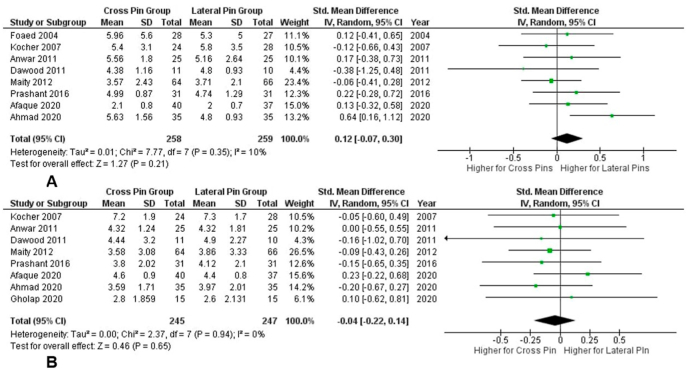
3.2.4. Loss of Baumann angle
Eight studies17,18,20,21,24,26,30,31 examined the loss in Baumann angle in patients after surgery. The SMD was calculated to be 0.12 (95% CI -0.07-0.30), and the Z-score for the overall effect was 1.27 (P = 0.21), indicating no significant difference between the two groups. Furthermore, significant heterogeneity was not detected between the studies (P = 0.35, I2 = 10%) (Fig. 4A).
Fig. 4.
Forest Plot (A) A Forest plot showing a comparison of the postoperative Baumann's angle between cross entry and lateral entry groups. Odds Ratio was 0.12 (95% CI -0.07-0.30) showing a significant difference between the techniques (B) A Forest plot showing a comparison of the postoperative loss of angle between cross entry and lateral entry groups. Odds Ratio was −0.04 (95% CI -0.22-0.14) showing a significant difference between the techniques.
3.2.5. Loss of carrying angle
Eight studies17,18,20,24,26,30,31,36 assessed the loss of carrying angle postoperatively. The calculated SMD was −0.04 (95% CI -0.22-0.14), and the Z-score for the overall effect was 0.46 (P = 0.65), indicating no significant difference between the two groups. Additionally, no significant heterogeneity was observed (P = 0.94, I2 = 0%) (Fig. 4B).
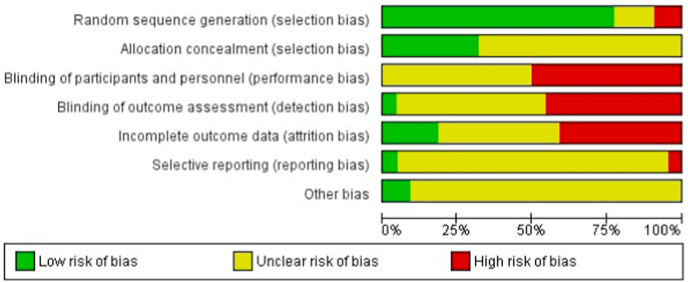
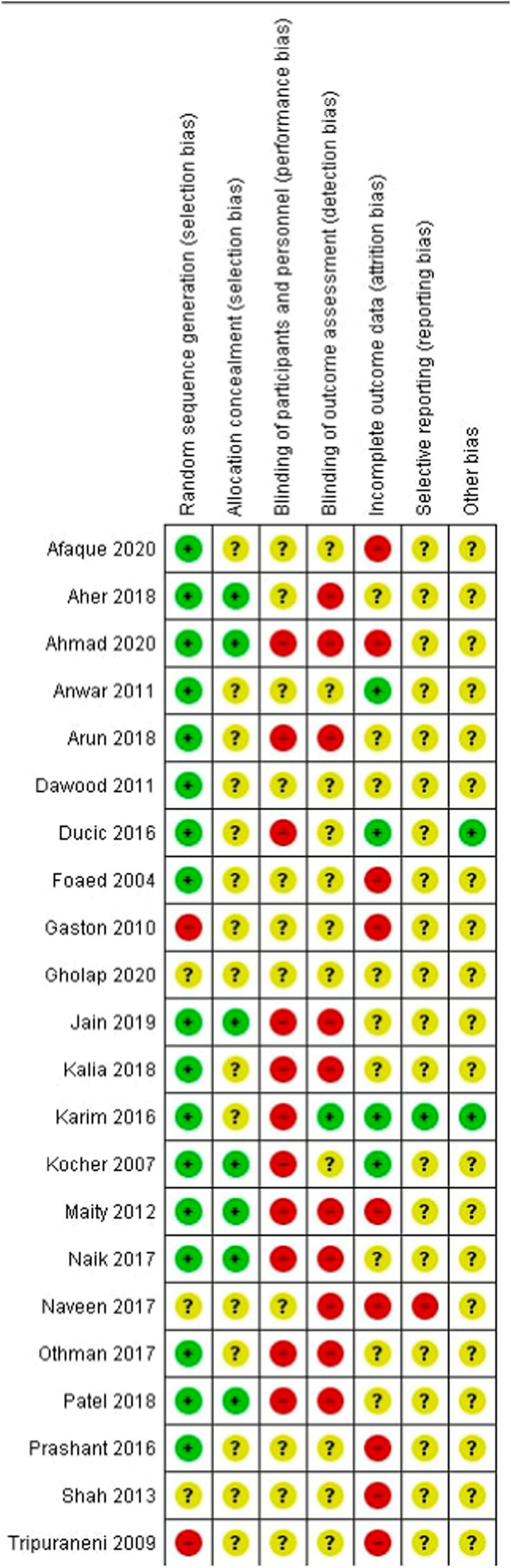
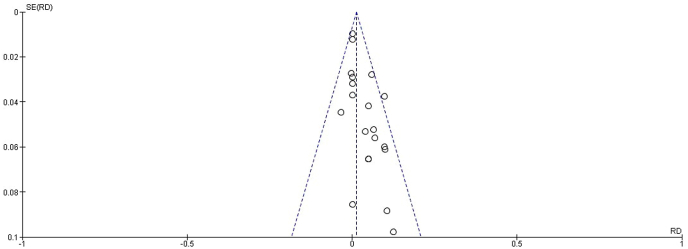
3.3. Quality assessment
While the majority of the studies indicated that their design was randomized, none of the articles provided a description of the method used to generate the allocation sequence. Overall, the risk of bias across the studies was unclear. The quality assessment results are summarized in Fig. 5, Fig. 6. There was no evidence of publication bias (Fig. 7).
Fig. 5.
Risk of bias graph. The risk of bias item estimation in all included studies is presented in percentage form.
Fig. 6.
The risk of bias in the included randomized controlled trials. +: no bias; −: bias; ? unknown bias.
Fig. 7.
Funnel plot of pooling ulnar nerve injury.
4. Discussion
In this study we analyzed 1502 patients, to quantify the outcomes of two percutaneous fixation techniques, namely the lateral pinning technique and cross pinning technique, and compare their intraoperative and postoperative results in the management of SCHF. Our results show that most of the postoperative and intraoperative outcomes associated with either pinning techniques are comparable with no significant difference. However, a noteworthy finding for our study was the significantly increased rate of ulnar nerve injury associated with the cross-pinning technique. It is important to note that iatrogenic ulnar nerve injury is one of the most common complications reported related to the pinning technique for SCHFs.
While the surgeons' preferences may vary based on their expertise, it is crucial to determine the most effective approach. Previous studies, including systematic reviews and meta-analyses,3,9, 10, 11, 12, 13, 14 have attempted to address the question of superiority between these techniques. Most of these studies have primarily focused on evaluating loss of range of motion and iatrogenic ulnar nerve injury. However, only a limited number of RCTs were included in these studies: Zhao et al.10 incorporated 7 RCTs with 521 patients, Carrazzone et al.12 considered 10 RCTs and 2 Quasi-RCTs comprising 930 patients, Kwok et al.13 examined 11 RCTs involving 900 patients, and Zhao et al., in 202138 analyzed 12 RCTs encompassing a total of 933 patients. The low number of RCTs can result in decreased statistical power, increased uncertainty in effect estimates, higher risk of publication bias, potential heterogeneity and limited generalizability, increased reliance on individual studies, and difficulty in conducting subgroup or sensitivity analyses. In contrast, the present study encompasses a larger sample size, including 22 RCTs with a total of 1502 patients. This extensive inclusion provides a clear and comprehensive analysis, reducing the risks of bias and heterogeneity. Additionally, the study's substantial sample size enhances its reliability by minimizing the potential for errors.
Our findings lend support to the efficacy of the lateral pinning technique, suggesting that both techniques are equally effective, but lateral pinning is notably safer for patients as it associated with a lower risk of ulnar nerve injuries. This aligns with the results of previous meta-analyses conducted by Na et al.3 and Woratanarat et al.,9 although it should be noted that their analyses included observational studies. In a separate study, Zhao et al.38 highlighted that utilizing the cross-pinning method through a mini-open incision decreases the chance of iatrogenic ulnar nerve injury. However, we did not perform a subgroup analysis in this particular area due to the limited number of studies available (only four studies1,17,20,37 reported this technique). Consequently, the results derived from such an analysis would have been heterogeneous and unreliable for application in a clinical setting. In another study, Kwok et al.13 reported that loss of fracture reduction was more prevalent in lateral pinning as compared to cross pinning. However, our study found no significant difference between the two pinning techniques in relation to this outcome. It is worth noting that the dissimilarity in results may be due to the inclusion of a larger number of RCTs in our current study, leading to a more precise and reliable analysis.
Lateral-only pinning was primarily associated with a notable drawback, which was diminished stability.39 In comparison to cross pinning, it had been observed that lateral-only pinning exhibited approximately 40% less rotational stability and a twofold increased likelihood of subsequent carrying angle deformity.40,41 However, recent studies have suggested that enhanced stability can be attained by implementing a divergent configuration with the lateral Kirschner wires.42 Moreover, optimal stability can be attained by implementing several strategies, including the placement of pins at a significant distance from each other, ensuring adequate bone contact in both fracture fragments, and utilizing bi-cortical pins instead of mono-cortical ones.43 A recent study demonstrated a higher failure rate was observed in cases where lateral-entry pins had a shorter distance (<5 mm) between the entry points or crossed at the fracture level. In contrast, patients with a proper pin configuration did not experience any failures.44 Hence, a lateral pinning approach with the correct technique to maximize stability in addition to the lower risk of ulnar nerve injury associated with lateral pinning makes this surgical technique a more favorable choice for the surgeon.
It is worth remembering that SCHF has a satisfactory result with either of the two pinning techniques. However, it is crucial to take the safety of both the techniques into account, for example, pin tract infection in severe cases can lead to major complications such as osteomyelitis and cellulitis which in turn leads to removal of the pin and intense antibiotic regimen. Similarly, the intensity of iatrogenic ulnar nerve injury can be variable but in severe cases it can lead to loss of function in hand.45 For a displaced, angulated, or unstable fractures cross pinning techniques can be preferred depending on the surgeon's expertise as it provides a more stability to the distal fractured segment.46,47 As mentioned earlier, the use of mini-open incision approach lacks sufficient literature so its benefits or detriments cannot be discussed with full confidence as of yet.
4.1. Strengths and limitations
This study possesses several notable strengths in comparison to the previously published literature. Notably, no prior meta-analyses that solely incorporated RCTs have exhibited a sample size as expansive as ours, which was made possible through an extensive review of relevant literature across multiple databases. Another strength lies in the significant sample size employed in our analysis, alongside the utilization of a random-effects model for assessing all outcomes, despite the low heterogeneity the utilization of a random-effects model ensures robustness of the result by taking into account the potential variability among studies beyond the observed heterogeneity, this can include clinical diversity such as basic demographics or different methodologies used by studies. Moreover, the exclusion of observational studies and quasi-RCTs has contributed to an overall improvement in the study's quality.
However, it is important to address several limitations inherent in our study. Firstly, variations were observed in the quantification of data across different studies, such as the utilization of Flynn's criteria or loss of Baumann's angle, with discrepancies arising from the presentation of values as mean and standard deviation or the pooling of all patient data into categorical ranges. Consequently, this data could not be effectively utilized for analysis. Secondly, although iatrogenic nerve injury was mentioned in 20 studies, only 10 studies quantified Flynn's criteria, and merely 8 studies quantified loss of Baumann's angle. This limitation affects the comprehensiveness of the analysis in these specific areas. Thirdly, a majority of the articles reviewed did not provide sufficient details regarding the randomization process, introducing a potential risk of bias. By acknowledging and addressing these limitations, we aim to provide a comprehensive and balanced evaluation of the study's findings and implications. Another limitation of this review is that we focused exclusively on studies published in the English language. As a result, relevant research conducted in non-English languages may not have been considered in our analysis. This language restriction could potentially lead to the omission of some findings.
4.2. Conclusion
In comparison to lateral pinning, the utilization of cross pinning technique exposes the patient to a heightened susceptibility of iatrogenic nerve injury. Therefore, it is recommended that surgeons prioritize the implementation of the lateral pinning technique whenever feasible, as it offers greater protection against iatrogenic ulnar nerve injury. Regarding other intraoperative and postoperative outcomes, such as loss of Baumann's angle and Flynn's criteria, both surgical techniques yield comparable results. However, due to an insufficiency of data, no definitive conclusions can be drawn regarding the mini-open incision approach in the context of cross pinning technique. Therefore, it is imperative that further RCTs be conducted to obtain more comprehensive insights into this particular aspect.
Funding
This research received no grant from any funding agency in the public, commercial or not-for-profit sectors.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author contribution
All authors have approved of the final article.
Declaration of competing interest
The authors declare that they have no conflict of interest.
Acknowledgements
None.
References
- 1.Abdel Karim M., Hosny A., Nasef Abdelatif N.M., et al. Crossed wires versus 2 lateral wires in management of supracondylar fracture of the humerus in children in the hands of junior trainees. J Orthop Trauma. Apr 2016;30(4):e123–e128. doi: 10.1097/bot.0000000000000473. [DOI] [PubMed] [Google Scholar]
- 2.Tripuraneni K.R., Bosch P.P., Schwend R.M., Yaste J.J. Prospective, surgeon-randomized evaluation of crossed pins versus lateral pins for unstable supracondylar humerus fractures in children. J Pediatr Orthop B. Mar 2009;18(2):93–98. doi: 10.1097/BPB.0b013e32832989ff. [DOI] [PubMed] [Google Scholar]
- 3.Na Y., Bai R., Zhao Z., et al. Comparison of lateral entry with crossed entry pinning for pediatric supracondylar humeral fractures: a meta-analysis. J Orthop Surg Res. Apr 3 2018;13(1):68. doi: 10.1186/s13018-018-0768-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gartland J.J. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. Aug 1959;109(2):145–154. [PubMed] [Google Scholar]
- 5.Patriota G., Assunção Filho C.A., Assunção C.A. What is the best fixation technique for the treatment of supracondylar humerus fractures in children? Rev Bras Ortop. Jun-Jul 2017;52(4):428–434. doi: 10.1016/j.rboe.2017.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Otsuka N.Y., Kasser J.R. Supracondylar fractures of the humerus in children. J Am Acad Orthop Surg. Jan 1997;5(1):19–26. doi: 10.5435/00124635-199701000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Zionts L.E., McKellop H.A., Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. J Bone Joint Surg Am. Feb 1994;76(2):253–256. doi: 10.2106/00004623-199402000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Lee S.S., Mahar A.T., Miesen D., Newton P.O. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. Jul-Aug 2002;22(4):440–443. [PubMed] [Google Scholar]
- 9.Woratanarat P., Angsanuntsukh C., Rattanasiri S., Attia J., Woratanarat T., Thakkinstian A. Meta-analysis of pinning in supracondylar fracture of the humerus in children. J Orthop Trauma. Jan 2012;26(1):48–53. doi: 10.1097/BOT.0b013e3182143de0. [DOI] [PubMed] [Google Scholar]
- 10.Zhao J.G., Wang J., Zhang P. Is lateral pin fixation for displaced supracondylar fractures of the humerus better than crossed pins in children? Clin Orthop Relat Res. Sep 2013;471(9):2942–2953. doi: 10.1007/s11999-013-3025-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dekker A.E., Krijnen P., Schipper I.B. Results of crossed versus lateral entry K-wire fixation of displaced pediatric supracondylar humeral fractures: a systematic review and meta-analysis. Injury. Nov 2016;47(11):2391–2398. doi: 10.1016/j.injury.2016.08.022. [DOI] [PubMed] [Google Scholar]
- 12.Carrazzone O.L., Mansur N.S.B., Matsunaga F.T., et al. Crossed versus lateral K-wire fixation of supracondylar fractures of the humerus in children: a meta-analysis of randomized controlled trials. J Shoulder Elbow Surg. 2021;30(2):439–448. doi: 10.1016/j.jse.2020.09.021. [DOI] [PubMed] [Google Scholar]
- 13.Kwok S.M., Clayworth C., Nara N. Lateral versus cross pinning in paediatric supracondylar humerus fractures: a meta‐analysis of randomized control trials. ANZ J Surg. 2021;91(5):980–985. doi: 10.1111/ans.16743. [DOI] [PubMed] [Google Scholar]
- 14.Kirzner N., Paul E., Moaveni A. Reverse shoulder arthroplasty vs BIO-RSA: clinical and radiographic outcomes at short term follow-up. J Orthop Surg Res. 2018;13(1):1–7. doi: 10.1186/s13018-018-0955-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arya S., Kaji A.H., Boermeester M.A. PRISMA reporting guidelines for meta-analyses and systematic reviews. JAMA Surg. Aug 1 2021;156(8):789–790. doi: 10.1001/jamasurg.2021.0546. [DOI] [PubMed] [Google Scholar]
- 16.Williamson D.M., Coates C.J., Miller R.K., Cole W.G. Normal characteristics of the Baumann (humerocapitellar) angle: an aid in assessment of supracondylar fractures. J Pediatr Orthop. 1992;12(5):636–639. [PubMed] [Google Scholar]
- 17.Maity A., Saha D., Roy D.S. A prospective randomised, controlled clinical trial comparing medial and lateral entry pinning with lateral entry pinning for percutaneous fixation of displaced extension type supracondylar fractures of the humerus in children. J Orthop Surg Res. Feb 15 2012;7:6. doi: 10.1186/1749-799x-7-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Prashant K., Lakhotia D., Bhattacharyya T.D., Mahanta A.K., Ravoof A. A comparative study of two percutaneous pinning techniques (lateral vs medial–lateral) for Gartland type III pediatric supracondylar fracture of the humerus. J Orthop Traumatol. 2016;17:223–229. doi: 10.1007/s10195-016-0410-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dučić S., Radlović V., Bukva B., et al. A prospective randomised non-blinded comparison of conventional and Dorgan's crossed pins for paediatric supracondylar humeral fractures. Injury. 2016;47(11):2479–2483. doi: 10.1016/j.injury.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 20.Kocher M.S., Kasser J.R., Waters P.M., et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children: a randomized clinical trial. JBJS. 2007;89(4):706–712. doi: 10.2106/JBJS.F.00379. [DOI] [PubMed] [Google Scholar]
- 21.Foead A., Penafort R., Saw A., Sengupta S. Comparison of two methods of percutaneous pin fixation in displaced supracondylar fractures of the humerus in children. J Orthop Surg. 2004;12(1):76–82. doi: 10.1177/230949900401200114. [DOI] [PubMed] [Google Scholar]
- 22.Gaston R.G., Cates T.B., Devito D., et al. Medial and lateral pin versus lateral-entry pin fixation for Type 3 supracondylar fractures in children: a prospective, surgeon-randomized study. J Pediatr Orthop. 2010;30(8):799–806. doi: 10.1097/BPO.0b013e3181f73d59. [DOI] [PubMed] [Google Scholar]
- 23.Tripuraneni K.R., Bosch P.P., Schwend R.M., Yaste J.J. Prospective, surgeon-randomized evaluation of crossed pins versus lateral pins for unstable supracondylar humerus fractures in children. J Pediatr Orthop B. 2009;18(2):93–98. doi: 10.1097/BPB.0b013e32832989ff. [DOI] [PubMed] [Google Scholar]
- 24.Anwar W., Rehman N., Iqbal M.J., Khan M.A. Comparison of the two methods of percutaneous K–wire fixation in displaced supracondylar fracture of humerus in children. J Postgrad Med Inst. 2011;25(4) [Google Scholar]
- 25.Patel I., Modi D.R., Sisodia K. Percutaneous fixation of displaced supracondylar fracture in children comparing lateral with MEDIALAND lateral PIN. Int J Sci Res. 2018;VII(V) doi: 10.36106/ijsr. [DOI] [Google Scholar]
- 26.Afaque S.F., Singh A., Maharjan R., Ranjan R., Panda A.K., Mishra A. Comparison of clinic-radiological outcome of cross pinning versus lateral pinning for displaced supracondylar fracture of humerus in children: a randomized controlled trial. Journal of clinical orthopaedics and trauma. 2020;11(2):259–263. doi: 10.1016/j.jcot.2019.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jain S., Agrawal S., Banshiwal R. Comparative study of posterior intrafocal with lateral pinning versus cross pinning for extension type supracondylar fracture humerus in children. National Journal of Clinical Orthopaedics. 2019;3(1):134–139. [Google Scholar]
- 28.Shah Z.A., Arif U. Displaced supracondylar humeral fractures;: treatment among children: crossed versus lateral pinning. Prof Med J. 2013;20(5):818–824. [Google Scholar]
- 29.Naveen P., Chaitanya P. A prospective study of crossed versus lateral only pinning in the treatment of displaced supracondylar fractures of the humerus in children. Int J Orthop Sci. 2017;3:400–404. [Google Scholar]
- 30.Ahmad M.M., Hussain H.U., Raza M.M., Ahmad S., Iqbal A.M., Iqbal U. Comparison of two methods of percutaneous pin fixation in displaced supracondylar fractures of the humerus in children: subcutaneous pin fixation. Medical Journal Of South Punjab. 2021;2(1) [Google Scholar]
- 31.Dawood W.F. Medial-lateral internal pin fixation compared to 2-lateral internal pin fixation in treatment of completely displaced supracondylar fractures of the humerus in children. Medical Journal of Tikrit University. 2011;2(172):61–66. [Google Scholar]
- 32.Aher D., Mishra R., Gohiya A. Comparative study of two techniques of percutaneous pinning of displaced supracondylar humerus fracture. Orthopaedic Journal of MP Chapter. 2018;24(1):3–7. [Google Scholar]
- 33.Othman M., Nahla A., El-Malt A. A comparative study of three percutaneous pinning techniques for paediatric supracondylar humeral fractures. ARC Journal of Orthopedics. 2017;2(2):11–19. [Google Scholar]
- 34.Kalia G., Singh N. Prospective randomised comparison study of 60 cases of type 2 and type 3 supracondylar fractures of humerus in children using conventional cross K wire fixation vs DORGAN’S lateral fixation. Indian J Appl Res. 2018;VIII(VII) [Google Scholar]
- 35.Arun K., Ramachandra K., Veerabhadra J., Suman N., Surya P., Nagadurga P. A prospective study of crossed versus lateral pinning for displaced extension-type supracondylar fractures of humerus. Int J Orthop Sci. 2018;4:737–740. [Google Scholar]
- 36.Gholap A., Wokhlu A., Gholap P. Gartlands type III supracondylar humerus fractures-cross k-wiring versus lateral k-wiring: a preliminary study. International Journal of Orthopaedics. 2020;6(1):1259–1262. [Google Scholar]
- 37.Naik L.G., Sharma G.M., Badgire K.S., Qureshi F., Waghchoure C., Jain V. Cross pinning versus lateral pinning in the management of type III supracondylar humerus fractures in children. J Clin Diagn Res. Aug 2017;11(8):Rc01–rc03. doi: 10.7860/jcdr/2017/28481.10351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhao H., Xu S., Liu G., Zhao J., Wu S., Peng L. Comparison of lateral entry and crossed entry pinning for pediatric supracondylar humeral fractures: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2021/06/09 2021;16(1):366. doi: 10.1186/s13018-021-02505-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mehserle W.L., Meehan P.L. Treatment of the displaced supracondylar fracture of the humerus (type III) with closed reduction and percutaneous cross-pin fixation. Journal of pediatric orthopedics. 1991;11(6):705–711. doi: 10.1097/01241398-199111000-00001. [DOI] [PubMed] [Google Scholar]
- 40.Brauer C.A., Lee B.M., Bae D.S., Waters P.M., Kocher M.S. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. 2007;27(2):181–186. doi: 10.1097/bpo.0b013e3180316cf1. [DOI] [PubMed] [Google Scholar]
- 41.Zionts L.E., McKellop H.A., Hathaway R. Torsional strength of pin configurations used to fix supracondylar fractures of the humerus in children. JBJS. 1994;76(2):253–256. doi: 10.2106/00004623-199402000-00013. [DOI] [PubMed] [Google Scholar]
- 42.Lee S.S., Mahar A.T., Miesen D., Newton P.O. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002;22(4):440–443. [PubMed] [Google Scholar]
- 43.Sankar W.N., Hebela N.M., Skaggs D.L., Flynn J.M. Loss of pin fixation in displaced supracondylar humeral fractures in children: causes and prevention. JBJS. 2007;89(4):713–717. doi: 10.2106/JBJS.F.00076. [DOI] [PubMed] [Google Scholar]
- 44.Hannonen J., Pokka T., Serlo W., Sinikumpu J.-J. Lateral-only kirschner-wire fixation of type-3 supracondylar humerus fractures in children with a special attention to technical issues. Scand J Surg. 2021;110(2):258–264. doi: 10.1177/1457496920908770. [DOI] [PubMed] [Google Scholar]
- 45.Slobogean B.L., Jackman H., Tennant S., Slobogean G.P., Mulpuri K. Iatrogenic ulnar nerve injury after the surgical treatment of displaced supracondylar fractures of the humerus: number needed to harm, a systematic review. J Pediatr Orthop. Jul-Aug 2010;30(5):430–436. doi: 10.1097/BPO.0b013e3181e00c0d. [DOI] [PubMed] [Google Scholar]
- 46.Brauer C.A., Lee B.M., Bae D.S., Waters P.M., Kocher M.S. A systematic review of medial and lateral entry pinning versus lateral entry pinning for supracondylar fractures of the humerus. J Pediatr Orthop. Mar 2007;27(2):181–186. doi: 10.1097/bpo.0b013e3180316cf1. [DOI] [PubMed] [Google Scholar]
- 47.Pavone V., Riccioli M., Testa G., et al. Surgical treatment of displaced supracondylar pediatric humerus fractures: comparison of two pinning techniques. Journal of Functional Morphology and Kinesiology. 2016;1(1):39–47. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.