Abstract
The “hotness” or “coldness” of the tumors are determined by the information of the cancer cells themselves, tumor immune characteristics, tumor microenvironment, and signaling mechanisms, which are key factors affecting cancer patients’ clinical efficacy. The switch mechanism of “hotness” and “coldness” and its corresponding pathological characteristics and treatment strategies are the frontier and hot spot of tumor treatment. How to distinguish the “hotness” or “coldness” effectively and clarify the causes, microenvironment state, and characteristics are very important for the tumor response and efficacy treatments. Starting from the concept of hot and cold tumor, this review systematically summarized the molecular characteristics, influencing factors, and therapeutic strategies of “hot and cold tumors,” and analyzed the immunophenotypes, the tumor microenvironment, the signaling pathways, and the molecular markers that contribute to “hot and cold tumors” in details. Different therapeutic strategies for “cold and hot tumors” based on clinical efficacy were analyzed with drug targets and proteins for “cold and hot tumors.” Furthermore, this review combines the therapeutic strategies of different “hot and cold tumors” with traditional medicine and modern medicine, to provide a basis and guidance for clinical decision‐making of cancer treatment.
Keywords: cancer, hotness and coldness of tumors, immune characteristics, signaling mechanism, therapeutic strategies, tumor microenvironment
The characteristics of coldness and hotness tumors are determined by the information of cancer cells and tumor microenvironments, which significantly affects cancer patients’ clinical efficacy. Different therapeutic strategies for cold and hot tumors based on clinical efficacy were analyzed through clinical drug targets, tumor microenvironments, and tumor stages. Coldness tumors can transform into hotness tumors through chemotherapy, radiotherapy, targeted therapy, and other therapies.

1. INTRODUCTION
Cancer morbidity and mortality have continued to rise significantly over the past few years. In 2020, there were 19.29 million new malignant tumor patients were diagnosed worldwide, with 9.96 million cancer‐related deaths. The cancer incidence rate increased significantly compared with 2018. In many countries, malignant tumors have become the leading cause of death. 1 With the development of society and technological advancements, precision medicine has gradually replaced conventional radiotherapy (RT) and surgical treatment of malignant tumors. 2 , 3 , 4 , 5 , 6 Precision cancer therapy is currently the most promising cancer treatment, including targeted therapy and immunotherapy. 7
Immunotherapy is a therapeutic modality that aims to regulate and eradicate tumors by reactivating and sustaining the antitumor immune cycle, as well as reinstating the body's innate antitumor immune response. It has become the fifth pillar of cancer treatment and mainly includes immune checkpoint inhibitors (ICIs), 8 adoptive cell transfer therapy, 9 , 10 , 11 tumor‐specific vaccines, cytokines (CKs), and small‐molecule immunological drugs. Of these, ICIs are currently the most widely used drugs in cancer immunotherapy.
Immunotherapy for tumors has been used for over 100 years, but the efficacy of immunotherapy varies even for patients with the same cancer type. 12 , 13 In 2009, Camus et al. 14 introduced the three primary immune features (“hot, variable, and cold”) that are evident in primary colorectal cancers (CRCs). This discovery led to a classification system that is based on the equilibrium between tumor evasion and immune coordination, with a 2‐year recurrence risk of 10, 50, and 80% for the three cancer types, respectively. Variable tumors can further be divided into two distinct patterns: “immune rejection” and “immunosuppressive.” 14 , 15 A global consensus immune scoring study validates the prediction of recurrence and survival risk based on these three main tumor subtypes (“hot, variable, and cold”). 16 , 17
ICI has been authorized to treat various tumors with demonstrated effectiveness. 18 Predictive indicators for immunotherapy, which are currently being researched, can be classified into two primary groups. Tumor immune microenvironments (TME) (e.g., tumor‐infiltrating lymphocytes (TILs), tertiary lymphoid structures [TLSs]) fall into the first category. 19 The second category is related to the molecular characteristics of the tumor cells (microsatellite instability/mismatch repair defects, tumor mutational load, neoantigen load, etc.). “Hot tumors” are characterized by a TME rich in TILs, PD‐L1 overexpression, genomic instability, and preexisting antitumor immune responses. 20 “Cold tumors” have the opposite characteristics. 21 Variable tumors are tumors in a variable state between cold and hot ones. It is generally accepted that ICIs alone are more effective against “hot tumors” while having no benefit in treating “cold” tumors or “variable” tumors, which require a combination of other therapies to recruit immune cells to the tumor tissue, that is, to convert a “cold tumor” or “variable” tumor to a “hot” tumor. The conversion of cold tumors and variable tumors to hot tumors is an important option to treat malignant tumors and ought to become a promising and clinically important area of research.
Cancer immunotherapy and ICIs have revolutionized cancer treatment with the development of hot and cold tumors. By taking the immune response of tumor patients as the target of anticancer treatment intervention, combined with chemotherapy, RT, targeted therapy, and other therapeutic methods, anticancer treatment has achieved remarkable and amazing effects, thus completely changing the treatment concept and method in the field of cancer.
The objective of this review is to conduct a comprehensive and in‐depth investigation into the immune mechanism underlying the formation and progression of cancer, examine the interplay between cancer and the immune system of the body, gain a comprehensive understanding of the potential mechanisms and intervention points that influence the emergence of “hot” and “cold” tumors, and offer anticancer concepts and potential strategies that involve combined immunity based on “hot and cold tumors.” We have reason to believe that the comprehensive use of an objective, standardized, and reasonable decision‐making method to guide cancer treatment requires a lot of clinical practice and evidence‐based medical evidence, which requires multidisciplinary collective efforts, but has great clinical value and practical significance.
2. CHARACTERISTICS OF COLD AND HOT TUMORS
The immune microenvironment and immune mechanisms differ between hot and cold tumors (Figure 1), mainly in the degree and type of immune cell infiltration, with different immune characteristics depending on the immune cell activity, and the heterogeneity of TME makes the tumor characteristics vary greatly between individuals (Figure 2).
FIGURE 1.
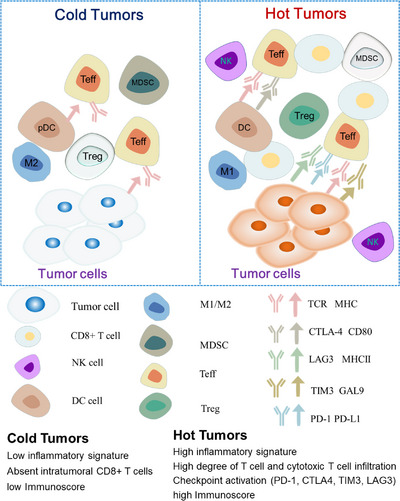
The differences of cold and hot tumors. The main cellular players and molecular interactions that affecting the cold tumor phenotype (left) and the hot tumor phenotype (right). Abbreviations are as follows: NK, natural killer cells; DC, dendritic cells; pDC, plasmacytoid dendritic cells; M1, macrophages of type 1; M2, macrophages of type 2; MDSC, myeloid‐derived suppressor cells; T eff, effector T cells; T reg, regulator T cells; TCR, T cell receptor; MHC, major histocompatibility complex; CTLA‐4, cytotoxic T‐lymphocyte‐associated protein 4; LAG3, lymphocyte‐activationgene‐3; TIM3, T cell immunoglobulin domain and mucin domain‐3; GAL9, galectin‐9; PD‐1, programmed cell death‐1; PD‐L1, programmed cell death‐ligand 1.
FIGURE 2.
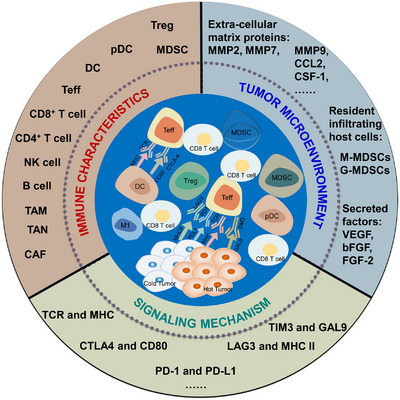
The immune microenvironment of hot and cold tumors. Tumors have many influencing factors in the tumor microenvironment, immune characteristics and signaling mechanisms, and hot and cold tumors present different characteristics, respectively.
2.1. Tumor microenvironment
The concept of TME was first introduced by Loannnides et al. 19 in 1993, specifically referring to the local environment of tumor occurrence and development, which mainly includes tumor cells, immune cell stromal cells and their secreted CKs, and extracellular matrix, which is formed through their interactions. The phenomenon of immune infiltration encompasses the presence of all immune cells within the TME, including but not limited to T cells, macrophages, natural killer (NK) cells, bone marrow‐derived suppressor cells (MDSCs), mast cells, neutrophils, B cells, and dendritic cells (DCs), and TLSs resulting from lymphoid neo‐organogenesis involving B cells, T cells, DCs, and lymphatic vessels. 22 , 23 , 24 It is important to note that certain cell types within the TME may exhibit both antitumor and protumor effects. For example, macrophages can differentiate into two simplified categories: M1 macrophages that are associated with acute inflammatory and antitumor activity, and M2 macrophages that are recruited for protumorous chronic inflammation. 25
2.2. Immune characteristics
TME is decisive for tumor heterogeneity, as tumor cells and their surrounding microenvironment are interdependent and influenced by each other. Tumor cells can release extracellular signals and influence TME to produce immune tolerance. Meanwhile, immune cells infiltrating the TME also kill tumor cells, preventing their proliferation and metastasis. The TME comprises two distinct mechanisms of immunosuppression: intrinsic immunosuppression, which may result from genetic alterations within the tumor and involves the activation of multiple oncogenic pathways, leading to the development of cold tumors; and locally adaptive immunosuppression, which gives rise to hot tumors characterized by a high degree of T‐cell infiltration, thereby providing a favorable milieu for effective ICI‐based mono‐ or combination therapy. 20 To enhance the efficacy of ICIs, it is imperative to devise strategies aimed at modulating the TME and shifting the tumor phenotype from cold to hot.
2.3. Signaling mechanism
TMEs with cold or hot tumors are characterized by the presence of sufficient immune cells, immune factors, or other immune factors. The immune microenvironment of cold tumors has fewer immune cells such as T cells and NK cells due to the activation of immunosuppressive pathways of immune checkpoints (ICs) such as PD‐1/PD‐L1 and CTLA‐4, and more immunosuppressive factors like interleukin 10 (IL‐10) and transforming growth factor beta, thus inhibiting the proliferation and activation of immune cells, while IC molecules such as PD‐L1 on the surface of tumor cells also inhibit the activation of immune cells. In contrast, the immune microenvironment of hot tumors is enhanced by the activation of immune activation pathways such as CD28/B7, CD40/CD40L, a higher number of immune cells, mainly including T cells, NK cells, and DCs, fewer immunosuppressive factors and a strong immune response. 26 The proliferation and activation of immune cells are stimulated by immune activating factors released from tumor cells, while IC molecules such as PD‐L1 on the surface of tumor cells are also attacked and cleared by immune cells.
3. FACTORS AFFECTING TUMOR HOTNESS AND COLDNESS
Presently, the terminology “hot” and “cold” is frequently employed to denote tumors that are infiltrated by T cells, those that are inflamed but not infiltrated, and those that are noninflamed. The differentiation between hot and cold tumors is predicated on the status of cytotoxic T cells within the tumors. In addition to the presence of TILs, other attributes, such as the expression of antiprogrammed death ligand 1 (PD‐L1) on immune cells associated with the tumor, potential genomic instability, and preexisting antitumor immune responses, have been identified as hallmarks of hot tumors (Figure 3).
FIGURE 3.
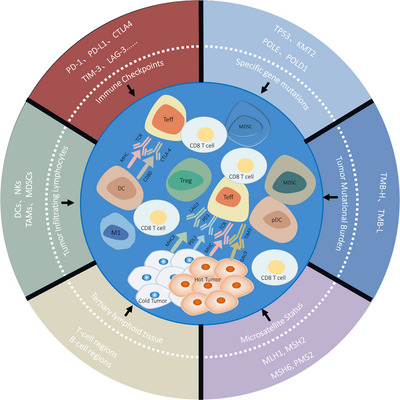
Factors influencing “hot and cold tumors.” “Hot and cold tumors” is a concept in comparison with the clinical efficacy of tumor treatment. Tumors that respond well to treatment are defined as hot tumors, and those that respond poorly are defined as cold tumors. There are many factors affecting tumor efficacy, including immune checkpoints (PD‐1, PD‐L1, CTL4, TIM‐3, LAG‐3), tumor infiltrating lymphocytes (TIL), tertiary lymphoid tissue (TLS), microsatellite status (MSI), tumor mutational burden (TMB), and specific gene mutations (SGM, e.g., TP53, KMT2, POLE, and POLD1). Abbreviations are as follows: TP53, tumor protein p53; KMT2, histone–lysine N‐methyltransferase 2; POLE, polymerase epsilon; POLD1, polymerase delta 1; MLH1, MutL homolog 1; MSH2, MutS homolog 2; MSH6, MutS homolog 6; PMS2, postmeiotic segregation increased 2.
3.1. Immune checkpoints
ICs (Table 1) 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 are inhibitory receptors expressed on T cells or other immune cells, including PD‐1, cytotoxic T‐lymphocyte‐associated protein‐4 (CTLA4), T cell immunoglobulin and mucin‐domain containing‐3 (TIM‐3), and lymphocyte activation gene‐3 (LAG‐3). Ligand molecules of IC have been found to be widely expressed in various types of tumor cells and may be involved in tumor immune escape through different mechanisms of action.
TABLE 1.
IC‐related drugs and their indications.
| Target | Drugs | Indications | References |
|---|---|---|---|
| Anti‐PD‐1 | Pembrolizumab | Non‐small cell lung cancer; melanoma; head and neck squamous cell cancer; classical Hodgkin lymphoma; primary mediastinal large B‐cell lymphoma; urothelial carcinoma; microsatellite instability‐high or mismatch repair deficient cancer; gastric cancer; esophageal cancer; cervical cancer; hepatocellular carcinoma; Merkel cell carcinoma; renal cell carcinoma; endometrial carcinoma; tumor mutational burden‐high cancer; cutaneous squamous cell carcinoma; triple‐negative breast cancer | 27 , 28 |
| Nivolumab | Melanoma; non‐small cell lung cancer; malignant pleural mesothelioma; renal cell carcinoma; classical Hodgkin lymphoma; squamous cell carcinoma of the head and neck; urothelial carcinoma; microsatellite instability‐high or mismatch repair deficient metastatic colorectal cancer; hepatocellular carcinoma; esophageal cancer; gastric cancer, gastroesophageal junction cancer, esophageal adenocarcinoma | 29 , 30 , 31 , 32 | |
| Dostarlimab | Mismatch repair deficient recurrent or advanced endometrial cancer | 33 , 34 | |
| Toripalimab | Melanoma; urothelial carcinoma; esophageal cancer; nasopharyngeal carcinoma | 35 , 36 | |
| Tislelizumab | Classical Hodgkin lymphoma; urothelial carcinoma; non‐small cell lung cancer; hepatocellular carcinoma; microsatellite instability‐high or mismatch repair deficient cancer; esophageal cancer; nasopharyngeal carcinoma | 37 , 38 | |
| Camrelizumab | Classical Hodgkin lymphoma; hepatocellular carcinoma; esophageal cancer; nasopharyngeal carcinoma; non‐small cell lung cancer | 39 , 40 | |
| Sintilimab | Classical Hodgkin lymphoma; non‐small cell lung cancer; hepatocellular carcinoma; esophageal squamous cancer; gastric cancer | 41 , 42 | |
| Penpulimab | Classical Hodgkin lymphoma | 43 , 44 | |
| Zimberelimab | Classical Hodgkin lymphoma | 45 , 46 | |
| Serplulimab | Microsatellite instability‐high or mismatch repair deficient cancer; non‐small cell lung cancer | 47 , 48 , 49 | |
| Pucotenlimab | Microsatellite instability‐high or mismatch repair deficient cancer; melanoma | 50 , 51 | |
|
Anti‐ PD‐L1 |
Atezolizumab | Non‐small cell lung cancer; small cell lung cancer; hepatocellular carcinoma; melanoma; alveolar soft part sarcoma | 52 , 53 |
| Durvalumab | Non‐small cell lung cancer; small cell lung cancer; biliary tract cancers; hepatocellular carcinoma | 54 , 55 | |
| Envafolimab | microsatellite instability‐high or mismatch repair deficient cancer | 56 , 57 | |
| Sugemalimab | Non‐small cell lung cancer | 58 , 59 , 60 | |
| Adebrelimab | Small cell lung cancer | 61 , 62 | |
| Anti‐CTLA4 | Ipilimumab | Unresectable or metastatic melanoma; adjuvant treatment of melanoma; advanced renal cell carcinoma; microsatellite instability‐high or mismatch repair deficient metastatic colorectal cancer; hepatocellular carcinoma; metastatic non‐small cell lung cancer; malignant pleural mesothelioma; esophageal cancer | 63 , 64 |
| Anti‐CTLA4/PD‐1 | Cadonilimab | Cervical cancer | 65 , 66 |
PD‐1 is a cell surface receptor that binds to PD‐L1 ligand in the TME to activate downstream signaling pathways to inhibit T cell activation, thereby causing tumor‐specific T cell failure and apoptosis. 67 , 68 PD‐1 is abundantly expressed in various cancers, resulting in the immune escape of tumor cells and promoting malignant tumor progression. 69 , 70 , 71 Combined action of PD‐1 and PD‐L1 suppresses host antitumor immunity, leading to tumor immune escape (Figure 4).
FIGURE 4.
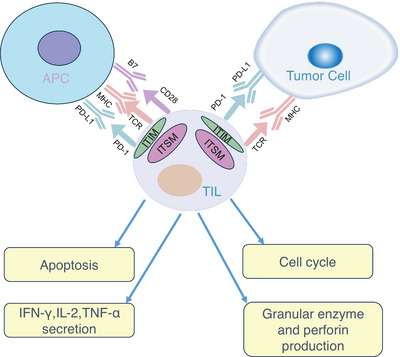
PD‐1 and PD‐L1 interactions affect TIL function in the tumor microenvironment. In the tumor microenvironment, PD‐L1, which can bind PD‐1, is aberrantly highly expressed on tumor cells and APC. Activation of PD‐1/PD‐L1 signaling induces phosphorylation of tyrosine residues in the PD‐1 cytoplasmic ITIM and ITSM structural domains and, by inducing apoptosis, inhibiting the production of granzyme and perforin, reducing the secretion of IFN‐γ, IL‐2, and TNF‐α reduces the antitumor activity of TILs and arrests the cell cycle. Abbreviations are as follows: TCR, T cell receptor; MHC, major histocompatibility complex; APC, antigen‐presenting cell; ITIM, immune receptor tyrosine‐based inhibitory motif; ITSM, immune receptor tyrosine‐based switch motif.
PD‐L1 is the most relevant predictive marker for the treatment efficacy of ICIs. 72 The main evaluation indicators include TPS (tumor cell proportion score), CPS (combined positive score), and IPS (immune cell proportion score). In contrast, the TPS score is less well established, while the CPS is a more stable and reproducible method of scoring PD‐L1. 73 A study finds the objective response to pembrolizumab in gastric cancer patients significantly correlates with CPS but not TPS. 74 Therefore, CPS perhaps is a more accurate index for PD‐L1 evaluation than TPS. According to the different CPS scores, tumors can be classified into three PD‐L1 expression‐based subtypes: CPS < 1 is considered no expression, which is equivalent to “cold” tumors; 1 ≤ CPS < 50 is considered low expression, which is equivalent to “variable” tumors; when CPS ≥50, the tumor is considered to be highly expressed, corresponding to a “hot” tumor. 75 , 76
CTLA‐4 is predominantly expressed on activated T cells and Tregs, functioning as a negative regulator for T cell activation. The use of CTLA‐4 inhibitors plays a significant role in T cell initiation and can facilitate T cell trafficking to “cold” tumors. TIM‐3 primarily serves to inhibit the activation and proliferation of T cells, thereby enabling immune evasion by tumor cells. Overexpression of TIM‐3 is linked to T cell dysfunction and exhaustion. LAG‐3, a cell surface protein of the immunoglobulin superfamily, acts similarly to CTLA4 and PD‐1 and negatively regulates T cell activation.
3.2. Tumor‐infiltrating lymphocytes
TILs are immune cells isolated from tumor tissue and contain both positive regulatory immune cells, such as DCs, CD8+ T cells, and NK cells, 77 , 78 and negative regulatory immune cells, such as tumor‐associated macrophages (TAMs), regulatory T cells, myeloid‐derived suppressor cells (MDSCs), tumor‐associated neutrophils (TANs), and son. 79 , 80 TILs are evaluated by HE staining, immunohistochemistry, multiplex immunofluorescence, flow cytometry, and so on. 81 , 82 , 83
In a study of 228 immunotherapy patients with mNSCLC, the patients were classified into four types based on levels of CD8+ TILs and PD‐L1, and significant differences in response to PD‐1/PD‐L1 monoclonal antibodies were found among the different immunotypes. For the patients with high expression of PD‐L1, ORR and PFS were significantly better in type I patients with high expression of TILs than in type III patients with low expression of TILs. 84 Another study of patients with stage II or stage III CRC found that patients with low TIL had poor disease‐free survival (DFS) and those with high TIL had a better prognosis, regardless of whether they were dMMR or pMMR. 85
3.3. Tertiary lymphoid tissue
TLS, the third type of lymphoid tissue distinct from primary lymphoid tissue (thymus and bone marrow) and secondary lymphoid tissue (spleen, lymph nodes, tonsils, etc.), consists of multiple immune cells, including T‐cell and B‐cell regions, 86 , 87 that promote immune cell infiltration into solid tumors. 88 TLS has been shown to predict the efficacy of ICIs in multiple tumor types and is independent of PD‐L1 status. 89 The first report of TLS appeared in a study in which samples from NSCLC patients were tested, and TLS (clusters of mature DCs and T cells) were found to be present at the infiltrative margins of NSCLC tumors at all stages and were described as tumor‐induced bronchial‐associated lymphoid tissue. 90
Many clinical studies have shown that TLS cell composition, density, and site correlate with improved clinical prognosis or benefit from immunotherapy in lung cancer, 91 , 92 ovarian cancer, 93 melanoma, 94 , 95 CRC, 96 head and neck cancer, 97 and oral squamous cell carcinoma. 98 However, it has also been shown that TLS is associated with poorer tumor prognosis, for example, in hepatocellular carcinoma; additionally, TLS is associated with tumor progression, poorer associated clinicopathological features, and poor prognosis. 99 , 100 Different stages of TLS differentiation within the tumor may play different roles in tumor immunity, with patients containing mature TLS presenting lower recurrence rates compared to those containing early TLS in CRC 96 , 101 and liver cancer. 100
3.4. Microsatellite status
Microsatellite (MS), also known as short series repeated sequence, is a simple repetitive sequence of less than 10 nucleotides in the DNA genome. 102 Mismatch Repair (MMR) genes include MLH1, MSH2, MSH6, and PMS2. 103 , 104 Microsatellite status (MSI) can be caused by MMR‐Foricient (D‐MMR) genetic mutations or expression abnormalities. 105 , 106 According to the number of mutation sites, MSI can be divided into MSI‐H, MSI‐L, and MSS. Among them, MSI‐L and MSS are often classified as a single category because of their highly similar clinical characteristics, which are equivalent to “cold tumors” or “variable tumors.” 107
In cancer treatment, dMMR and MSI‐H are considered as “hot tumors” because of their sensitivity to ICIS treatment. 108 , 109 The advanced MSI‐H solid tumors often respond well to immunotherapy. Some studies have shown that the benefit of ICI treatment for tumor patients is closely related to the levels of MSI and has nothing to do with specific cancer types. 110 Patients with dMMR/MSI‐H CRC can get better disease control through ICI treatment. 111 , 112 One study confirmed that the median follow‐up times for MSI‐H CRC and MSI‐H non‐CRC cancers were 7.4 months and 4.5 months, respectively, with ORRs of 26.2% and 42.9% and DCRs of 50.8% and 66.7%, both achieving safe and efficient treatment outcomes. 113 In studies of pembrolizumab for the treatment of non‐CRC patients with MSI‐H/dMMR, the ORR was 48% and the DCR 66% in patients with endometrial cancer 114 and 45.8% in patients with gastric cancer. 115 With a median PFS of 11.0 months, pembrolizumab showed potent antitumor activity, producing a durable response. The incidence of MSI‐H varied by cancer and was described in only about 5% of cancer patients, being more common in CRC, gastric cancers, and endometrial adenocarcinomas.
3.5. Tumor mutational burden
Tumor mutational burden (TMB) is the number of nonsynonymous mutations occurring in the tumor genome, reflecting the degree of genomic variation in the tumor. 116 TMB‐H (high) tumors have the potential to acquire more de novo antigens, which can improve tumor immunogenicity and response to ICI, 117 and TMB has become an important indicator for immunotherapy dosing. One study found a correlation between immunotherapy and TMB, with high TMB values predicting better treatment outcomes. 118 , 119
In June 2020, the United States Food and Drug Administration (US FDA)‐approved pembrolizumab for the treatment of unresectable or metastatic solid tumors with TMB‐H. 120 According to some studies, TMB predicts the efficacy of ICI in patients with malignant melanoma and NSCLC; patients with TMB ≥ 20 mutations/mb responded better to immunotherapy and had a longer DFS. 121 Pembrolizumab had better efficacy in patients with TMB‐H compared with patients with TMB‐L (low) (ORR, 30.3 vs. 6.7%). Another analysis of pan‐cancer study of 1600 patients also showed that TMB‐H was associated with higher response rates and longer OS with ICIs. 122 Therefore, the US FDA‐approved pembrolizumab for monotherapy in TMB‐H and unresectable or metastatic solid tumors with disease progression after prior therapy, regardless of cancer type. 123
3.6. Specific gene mutations
The TP53 gene is a carcinogenic suppression gene that maintains genome stability on the 17th chromosome and prevents genetic mutation. 124 , 125 TP53 mutation status may be a positive or negative predictor of response to tumor immunotherapy (e.g., a positive predictor in breast and lung adenocarcinomas and a negative predictor in gastric, colon, and head and neck squamous cell carcinomas). 126 TP53 mutations increased TAMs in the TME of lung, ovarian, pancreatic, and skin cancers, 127 involving multiple complex signaling pathways, including regulation of gene expression, protein stability, protein interactions, and posttranscriptional modifications, 19 causing changes in the secretion of chemokines and CKs, which in turn alter the immune microenvironment.
Cell adhesion molecules (CAMs), a class of proteins that mediate adhesion between cells and between cells and external structures, play an important role in tumor development and metastasis. Tumor endothelial cells (ECs) promote the adhesion of tumor cells to vascular ECs and inhibit the infiltration of T cells into the tumor bed by modulating CAMs (ICAM‐1 and VCAM‐1). Hot tumors are characterized by a high infiltration of various infiltrating lymphocytes (TILs), whereas cold tumors have fewer infiltrating lymphocytes and often show abnormal expression of CAMs on tumor‐associated vessels, thus preventing immune cells from entering the tumor. Clinical studies have demonstrated that upregulation of ICAM‐1 in the TME is associated with a good prognosis for patients with various cancers, suggesting enhanced immune surveillance of cancer. 128 , 129 , 130 , 131
In addition, several other studies have demonstrated that some specific gene mutations (e.g., KMT2, 132 POLE, and POLD1 133 ) can be used as independent predictors of survival benefit from treatment with pan‐tumoral ICIs.
4. TREATMENT STRATEGIES FOR HOT AND COLD TUMORS
In both cold and hot tumors, the focus of treatment is on activating the immune system and enhancing the ability of the immune system to kill tumor cells. The relevance of tumor classification criteria and the effectiveness of immunotherapy can guide the selection of different immunotherapy strategies for different types of tumors in clinical applications (Figure 5).
FIGURE 5.
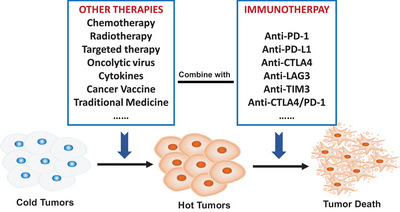
Therapeutic strategies for cold and hot tumors. For hot tumors with high PD‐L1 expression and MSI‐H, single immunotherapy can show amazing efficacy, while for cold tumors with low PD‐L1 expression and MSI‐L, single immunotherapy cannot achieve satisfactory efficacy. How to convert a cold tumor into a hot tumor is crucial. Combined immunotherapy strategy is an important method for cold tumor treatment, including immunotherapies combined with chemotherapy, targeted therapy, radiotherapy, double immunotherapy, oncolytic virus, cancer vaccine, cytokines, traditional medicine, intestinal flora, and so on, are all clinically available combination methods.
4.1. Hot tumors treatment strategies
“Hot” tumors provide fertile ground for immunotherapy through high levels of T‐cell infiltration, and ICIs can block the PD‐1/PD‐L1 pathway or CTLA‐4, normalizing the immune system and inhibiting tumor growth. The “hot tumor” treatment focuses on strengthening the immune system against the tumor and increasing the activity of the immune cells.
4.1.1. Anti‐PD‐1 monotherapy
In 2017, the US FDA‐approved nivolumab for the treatment of MSI‐H/dMMR mCRC patients who had progressed after prior chemotherapy. 112 Pembrolizumab is available as a first‐line treatment option for NSCLC patients without EGFR or ALK mutations and with PD‐L1 TPS ≥ 50%. 134 Cemiplimab was approved as a single‐agent first‐line treatment for patients with locally advanced or metastatic NSCLC with ≥50% PD‐L1 expression and no EGFR, ALK, or ROS1 mutations and who are not candidates for surgical resection or RT. 135 Sintilimab was approved as a single‐agent treatment for EGFR‐ and ALK‐negative patients with PD‐L1 TPS ≥ 50. 136 Toripalimab was effective in treating advanced UC patients with PD‐L1‐positive TMB‐H. 137 Camrelizumab monotherapy showed beneficial antitumor activity in patients with PD‐L1‐positive pulmonary sarcomatoid carcinoma. 138 Tislelizumab was used to treat adult patients with unresectable or metastatic MSI‐H/dMMR in advanced solid tumors. 139
4.1.2. Anti‐PD‐L1 monotherapy
Atezolizumab was approved in China as first‐line monotherapy for metastatic NSCLC with high PD‐L1 expression and no EGFR/ALK gene mutations. 140 A phase I/II clinical study of duravulumab for the first‐line treatment of NSCLC patients provided an ORR of 28.6% in PD‐L1‐positive patients. 141 In patients with MSI‐H/dMMR mCRC, avelumab (avelumab) outperformed second‐line standard therapy in terms of PFS. 142 Envafolimab has a better efficacy and safety profile in the treatment of patients with dMMR/MSI‐H tumors. 56
4.1.3. Anti‐PD‐1/CTLA4 bi‐specific antibody
There is enhanced antitumor efficacy of cadonilimab, a drug that blocks the ligands to bind on PD‐1 and CTLA‐4 65 with a 43.8% ORR and a median PFS of 6.34 months in PD‐L1‐positive cervical cancer patients (CPS ≥ 1). 143
4.2. Cold and variable tumors treatment strategies
Single immunotherapy can achieve good results in “hot” tumors, but few patients meet the treatment criteria, and the treatment costs are high. Moreover, the intricate nature of immunomodulatory signaling pathways implies that patients who exhibit initial sensitivity to ICI therapy may eventually experience resistance or relapse. 144 Consequently, it is imperative to explore methods that can enhance ICI sensitivity. The integration of targeted therapy, chemotherapy, and RT can potentially transform “cold” or “variable” tumors into “hot” ones, thereby augmenting the effectiveness of immunotherapy. Furthermore, novel and personalized immunotherapy approaches should be investigated to improve patients’ sensitivity and response rates to activated antitumor immune responses. 145
4.2.1. Combination of chemotherapy with PD‑1/PD‑L1 inhibitors
Chemotherapy is a commonly used treatment modality for cancer by targeting DNA replication and disrupting cellular metabolism. 146 Certain cytotoxic chemotherapeutic agents, such as anthracyclines and oxaliplatin, have been shown to induce immunogenic cell death (ICD), stimulate antitumor immune responses, 147 or directly eliminate immunosuppressive cells, and enhance the function of effector cells. 148 , 149 Appropriate combinations of chemotherapeutic agents and ICIs can enhance efficacy and produce a more durable antitumor response. 150 , 151
In 2016, the US FDA approved the use of pembrolizumab in combination with pemetrexed/carboplatin for the treatment of metastatic nonsquamous NSCLC, which effectively improved symptoms and increased PFS. 152 , 153 PD‐1 monoclonal antibody in combination with GEM (gemcitabine) has demonstrated efficacy in treating of hepatic metastases from pancreatic ductal adenocarcinoma enhanced the immune response and significantly prolonged OS in mice model. 154 One study evaluated changes in IC ligands and receptors on the cell surface of esophageal adenocarcinoma (OAC) before and after chemotherapy demonstrated that chemotherapy upregulated PD‐L1 and TIM‐3 on the surface of OAC cells to enhance the stem cell‐like phenotype and promote the conversion of “cold” to “hot” tumors, making them more sensitive to ICI treatment. 155
4.2.2. Combination of molecular targeting drugs with PD‑1/PD‑L1 inhibitors
Vascular endothelial growth factor (VEGF) regulates the growth of vascular ECs, causing immunosuppression. 156 Several studies have shown that blocking VEGF‐related pathways enhances the immune response, and the combined application of PD‐L1 monoclonal antibodies and VEGF inhibitors has shown good synergistic effects in clinical studies and is promising for the treatment of a variety of tumors. 157 PD‐L1 inhibitors in combination with VEGFR2 inhibitors can significantly downregulate PD‐1 and PD‐L1 expression levels, increase TILs, decrease Treg and MDSCs, and inhibit tumor growth. 158 , 159 Bevacizumab (bevacizumab), an antiangiogenic drug, increased T cell reversal of immunosuppressive infiltration and improved the antitumor activity of the PD‐L1 monoclonal antibody. 160 Atezolizumab in combination with Bevacizumab improved PFS and OS in patients with mNSCLC, and the combination significantly improved Atezolizumab sensitivity. 161
EGFR is a transmembrane tyrosine kinase receptor involved in tumor cell proliferation, invasion, and metastatic angiogenesis. 162 T‐cell apoptosis is reduced and IFN‐ production is increased by EGFR inhibitors (EGFR‐TKI). 163 Erlotinib, an EGFR‐TKI, reduces CD4 effector regulatory T‐cell infiltration in TME and is used in combination with PD‐1 monoclonal antibody to treat NSCLC, improving immunotherapy efficacy. 164 In EGFR/ALK‐positive and ALK‐rearranged patients, the addition of bevacizumab improved the clinical outcome of ICI. 165
Lenvatinib is a drug that helps transform TME and improve the anticancer effect of immune cells 166 by inhibiting both VEGFR and FGFR targets. 167 In September 2019, Lenvatinib in combination with pembrolizumab (the “cola combination”) received US FDA approval for patients with advanced endometrial cancer who have disease progression after systemic therapy that is not suitable for surgery or RT and who do not have MSI‐H or dMMR. 168 In a phase IB single‐arm study of first‐line treatment of advanced hepatocellular carcinoma, the “cola combination” improved tumor activity with an ORR of 76.7%, a CR rate of 10%, and a significant prolongation of patient OS. 169 In another phase II study, the ORR of “cola combination” was 21.4% and the mOS was 13.9 months in patients with inoperable stages III–IV melanoma who had progressed to resistance to previous immunotherapy, demonstrating good efficacy and a manageable safety profile. 170 Based on the positive results of these clinical studies, the “cola combination” has become a classic combination of immunotherapy and targeted therapy.
4.2.3. Dual IC blockade or costimulatory molecule agonist plus α‑PD‑1/PD‑L1
Dual immunotherapy, referring to the combination of immunotherapies targeting two different mechanisms or targets of action, is gradually gaining acceptance among clinicians and cancer patients as clinical studies on dual immunotherapy are conducted and the benefits of efficacy have been realized. 171 , 172 , 173 Nivolumab and Ipilimumab are PD‐1 antibody and CTLA‐4 antibody: one reduces excessive contact between T cells and cancer cells to prevent T cells from being misled by cancer cells, 174 and the other signals antigen‐presenting cells to activate T cells 174 , 175 for cancer cell killing. The combination of PD‐1 and CTLA‐4 inhibitors is mechanistically synergistic and complementary, 176 , 177 and Nivolumab and Ipilimumab are the only dual immunotherapies currently approved by the US FDA, 178 , 179 demonstrating better antitumor effects than single immunotherapies, especially in “cold tumors.” 171
There are also ICs that are still in clinical trials and have not yet been approved by the US FDA or NMPA. Lymphocyte‐activation gene 3 (LAG‐3) negatively regulates T‐cell effects by directly inhibiting helper T cells (Th) via MHCII. 180 , 181 In the EG7 lymphoma model, the combination of anti‐LAG3 and PD‐1 monoclonal antibodies had a 100% tumor clearance effect, whereas treatment with PD‐1 monoclonal antibodies alone resulted in a tumor clearance rate of only 50%. 182 Targeted inhibition of LAG3 and PD‐1 also showed significant tumor regression in the B16‐F10 recurrent melanoma model. Tim‐3 (T cell immunoglobulin domain and mucin domain‐3, TIM‐3) on effector T cells interacts with Galectin‐9 on tumor cells to induce T cell apoptosis and suppress immune responses. 183 TIL is a severely depleted phenotype that fails to proliferate to produce IL‐2, TNF, and IFN‐. It is TIM‐3 and PD‐1 positive. The combination of a TIM‐3 inhibitor and a PD‐1 monoclonal antibody can upregulate TIL expression to effectively control tumor growth in lung cancer mice, whereas the use of PD‐1 monoclonal antibodies alone led to resistance, promoting tumor progression. 184 , 185
4.2.4. Combination of RT with PD‑1/PD‑L1 inhibitors
Radiotherapy (RT) can enhance the efficacy of PD‐1 inhibitors by promoting T‐cell infiltration, increasing the number of TILs, inducing ICD, and enhancing the antitumor immune response. 186 , 187 , 188 On the one hand, it can induce damage‐associated molecular patterns (DAMPs) and CKs (especially IFN‐I) associated with ICD to recruit immune cells and promote DC function; on the other hand, DCs can capture their released tumor antigens and present them to T cells 189 , 190 as a way to stimulate systemic antitumor immunity.
Most radioimmunotherapy regimens are based on stereotactic body radiation therapy (SBRT), which can deliver ablative doses of radiation by means of image guidance and intensity modulation. 191 , 192 , 193 SBRT combined with durvalumab was superior to durvalumab alone in early‐stage NSCLC, and the major pathological response rate was significantly higher than in the durvalumab group. 194 Clinical studies have demonstrated that anti‐PD‐1 therapy significantly improves OS in patients with melanoma brain metastases treated with stereotactic radiotherapy. 195
4.2.5. Combination of oncolytic virus with PD‑1/PD‑L1 inhibitors
Oncolytic virus (OV) therapy elicits ICD and immune responses via the release of pathogen‐associated molecular patterns and DAMPs, 196 , 197 resulting in the destruction of cancer cells by targeting the tumor vascular system and inducing immunity, 198 , 199 increasing the sensitivity of tumor cells to immunotherapy (“warming up” the tumor), and enhancing the therapeutic effect.
Talimogene laherparepvec, the first US FDA‐approved oncolytic therapy, is a herpes simplex virus that expresses granulocyte‐macrophage colony‐stimulating factor. 200 In Talimogene combined with pembrolizumab in 21 patients with advanced melanoma, lysing virus therapy was found to improve immune efficacy by altering TME. 201 A phase 1 clinical trial of a herpes simplex virus type 1‐based lysozyme virus (HSV‐1‐G207) for the treatment of high‐grade gliomas in children showed that intratumoral injection of the lysozyme virus alleviated recurrent or progressive high‐grade gliomas in children, transforming “cold” tumors to “hot” tumors. 148 Poxvirus is a highly immunogenic vector for lytic immunotherapy, 202 , 203 and some studies have reported that poxvirus attracts effector T cells in mouse models of colorectal and ovarian cancer. 204 , 205 mJX‐594 (JX), a lysing cowpox virus, was found to be effective in restoring peritoneal immunity by Lee et al. 206 This virus promoted immune cell infiltration, inhibited peritoneal metastasis of colon cancer cells, and exerted stronger antitumor effects through combined immunotherapy. 206 t‐VEC, an OV for the treatment of malignant melanoma, provides a new strategy for melanoma treatment by upregulating the expression of inflammatory molecules, including PD‐L1, and enhancing immune efficacy. 207 Rotavirus vaccines have immunostimulatory and antitumor effects, 208 and when used in oncology, it can overcome resistance to PD‐L1 inhibitors and have synergistic effects with them. Rotaviruses have been used clinically and can be used for clinical sensitization of anti‐PD‐1/PD‐L1 therapy. 209
4.2.6. Combination of cancer vaccine with PD‑1/PD‑L1 inhibitors
Tumor vaccines control or eliminate tumors by increasing immunity and activating the patient's immune system, 210 , 211 The DNA vaccine contains the coding sequences of multiple neoantigens and is a universal and personalized cancer treatment. 212 , 213
Studies have shown that DNA vaccines combined with anti‐PD‐1 treatment significantly controlled tumor growth and achieved a 25% cure rate in MC38 colon cancer cell line‐inoculated hormonal mice, demonstrating the synergistic effect of tumor vaccines and ICIs. 214 The lmdd‐MPFG vaccine promotes the TAMs NF‐κB pathway and autophagy pathway in hepatocellular carcinoma cells by activating PD‐L1 expression, restoring T‐cell responses to PD‐1 inhibitors, and enabling local T‐cell resensitization to anti‐PD‐1 immunotherapy in tumors. 215 A study investigated Nivolumab in combination with a peptide vaccine as adjuvant therapy for patients with stages III and IV resected melanoma, demonstrating the combination significantly increased CD8+ T cell levels and enhanced treatment efficacy. 216 , 217
HER2Δ16 commands an important oncogenic signaling pathway; however, endogenous HER2Δ16+ breast cancers do not respond to single‐dose treatment of anti‐PD‐1. One mouse model study found that the use of anti‐PD‐1 in combination with Ad‐HER2Δ16‐KI improved survival, with approximately 30% of mice showing complete tumor regression as well as long‐term tumor‐free survival, and HER2Δ16 vaccine effectively induced HER2‐specific T cells in TME, enhancing the therapeutic effect. 218 One study created a liposomal nanoparticle encapsulated with TNF‐α that penetrated into and remained in tumor tissue for an extended period of time, promoting ICD, inducing the release of tumor‐specific antigens, promoting T‐cell infiltration, converting tumor cells into endogenous vaccines, therefore significantly improving antitumor immunity of PD‐1/PD‐L1 antibodies. 219 cMB305 (DC vaccine) in combination with atezolizumab activated antitumor‐specific immune responses in some patients with synovial sarcoma, demonstrating enhanced effect of CMB305 vaccine against PD‐L1 immunotherapy. 220
4.2.7. Combination of CK treatment with PD‑1/PD‑L1 inhibitors
CKs are low‐molecular‐weight soluble proteins induced by immunogens, mitogens, or other stimulants to be produced by a variety of cells. They are an essential part of the TMB, having an important role in tumor pathogenesis. 221
ALT‐803 (IL‐15 superagonist) in combination with ICI for refractory solid tumors enhances immune efficacy. 222 , 223 , 224 , 225 Phase Ib clinical trials of ALT‐803 in combination with nivolumab for NSCLC resulted in reactivation of antitumor activity. 226 In PD‐L1‐negative (<1%) nonsquamous NSCLC patients, only 9% achieved clinical efficacy with nivolumab alone, whereas the combination of ALT‐803 and nivolumab demonstrated a clinical efficacy of 30%, indicating that the utilization of IL‐2Rβγ agonists may serve as a potential solution to overcome resistance to ICI therapy. The activation of proinflammatory CKs such as IFN‐γ systemically stimulates an effector immune response, thereby facilitating the conversion of “cold” tumors to “hot” tumors. 227
Additional research has demonstrated that L19‐IL‐2 treatment significantly enhances the infiltration of immune cells (e.g., NK cells, T cells) into tumor tissue in mice compared to IL‐2 treatment and exhibits significantly stronger tumor growth inhibition, with L19‐IL‐2 showing good antitumor activity as a single or combination therapy for metastatic solid tumors in phase I clinical studies. 228 , 229
4.2.8. Combination of traditional Chinese medicine with PD‑1/PD‑L1 inhibitors
With modern traditional Chinese medicine (TCM) research at the molecular level, study attempts have been made to combine TCM to the effects on the PD‐1/PD‐L1 signaling pathway. 230 , 231 , 232 Recent studies have found that many TCM extracts/components such as paeoniflorin, 233 berberine, 234 cordycepin, 235 atractylenolide I, 236 can regulate lymphocyte PD‐1/PD‐L1 expression, modulate tumor immunity, and enhance antitumor effects by increasing the proliferation and killing effect of T lymphocytes such as CD4+.
There are also variable Chinese herbal compounds found to act on cells or CKs in the TMB to remodel the TMB and enhance the body's antitumor immune response. Zhong et al. 237 administered Guilu Erxian Jiao Decoction gavage to tumor‐bearing mice inoculated with the H22 hepatocellular carcinoma cell line, to find that such gavage inhibit tumor growth by reducing apoptosis of T‐lymphocytes through inhibition of PD‐1 expression. Ge Gen Scutellaria Tang has an overall regulatory effect on immune cells, inhibiting tumor progression by increasing the number of CD8+ T cells and NK cells. 238
4.2.9. Combination of intestinal microflora with PD‐1/PD‐L1 inhibitors
Several studies have also confirmed that intestinal flora can influence the efficacy of cancer immunotherapy. 239 , 240 For example, Bifidobacterium, Bacillus faecalis, Ackermannia, and Bacteroides fragilis, can enhance the function of DCs and T cells and contribute to a better immunotherapeutic response. 241 , 242 Oral administration of Bifidobacterium bifidum significantly reduced the growth rate of melanoma, promoted DC maturation and IFN‐γ production, and enhanced the antitumor effects of PD‐1 inhibitors, according to one study. 243
4.3. Research prospects and application perspectives for hot and cold tumors
With the extensive research and therapeutic applications of the concept of “hot and cold” tumors, the future treatment of malignant tumors will be based on gene expression, immunophenotype, and molecular typing of patients, alas gradually downplaying the importance of tumor location and pathological types, therefore ushering in a new conceptual and fundamental change in cancer treatment regime. “Hot tumors“ are more likely to occur in the bladder, head and neck, kidney, liver, melanoma, and non‐small cell lung cancers, while ”cold tumors“ are more likely in gliomas, ovarian, prostate, and pancreatic cancers. 244 Further studies of ”hot and cold” tumors are still needed, and its conceptual application in the field of tumor therapy is promising.
The “hot and cold” characteristics of tumors are similar to the “yin and yang” properties of TCM. 245 , 246 Just as “yin” and “yang” (Figure 6) are mutually rooted and transformed into each other, so can “hot” and “cold” tumors. According to Chinese medicine, the causative factors of malignant tumors, such as phlegm, stasis, and toxicity, are yin‐evil glued to each other and therefore called “yin in the body,” while the active growth and proliferation of tumors, invasion, metastasis, and other malignant behaviors are “yang in the body.” 247 Interestingly, TCM's understanding of the “yin” and “yang” properties of malignant tumors, analysis of the etiology and pathogenesis, as well as the differentiation and classification of malignant tumors have all reflected the “hot and cold” concept of malignant tumors. A lot of clinical and basic studies have been conducted on the treatment of “hot and cold” tumors in Chinese medicine, and some active ingredients and herbal compounds have been proven to be able to adjust “hotness and coldness” of the immune function of tumor patients via affecting immune organs, immune cells, and immune molecules. 248 By analyzing the “yin” and “yang” of “hot and cold” tumors, TCM treats “cold” tumors by “warming the yang and supporting the righteousness,” converting the tumor from being “cold” to “hot,” to activate the positive immunity of “cold tumors” to achieve effective clinical treatment of malignant tumors.
FIGURE 6.
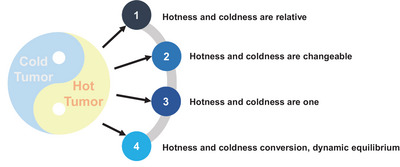
Holistic and yin‐yang properties of tumors. The “hot and cold tumor” is consistent with the “Yin and Yang” attribute in traditional Chinese medicine theory, which believes that “Yin and Yang” are two corresponding attributes of the human body, which are mutually used and dynamically balanced. “Tumor” also has Yin and Yang attributes, “hot and cold tumor” is relative, but also mutual root, can be transformed, can be normalized, dynamic balance.
The efficient application of immunotherapy in the era of precision medicine requires clear information on tumor gene mutation profiles and immunophenotypes. Various tumor immune markers are used for patient selection of ICI treatment, also guiding us in designing studies to combine basic research and clinical scenarios to transform ICI insensitive cancers into sensitive ones. This strategy, combined with developments in precision medicine and the use of next‐generation sequencing in molecular profiling of cancers, will take us into the era of personalized cancer immunotherapy, where multiple therapeutic approaches are combined to achieve durable remission in hard‐to‐treat cancers.
5. SUMMARY AND PROSPECT OF THE FUTURE
“Cold” and “hot” have attracted widespread interest because of their important impacts on cancer immunotherapy. 249 , 250 , 251 The “hot” conversion of “cold” tumors improves the efficacy of cancer immunotherapy. 252 The change of the relationship between tumor cells and immune cells leads to the process of cancer occurrence, development, invasion, and metastasis. TME, immune functions, organ metabolism mechanism, and signaling pathway are closely related to cancer development. Focusing on the changes of tumor immune microenvironment and immune function are the keys to improving the efficacy and survival rate of immunotherapy in advanced cancer patients. 253 A thorough examination of tumor tissue, blood samples, and clinical data of the host utilizing diverse diagnostic methodologies such as molecular, cellular, histological, imaging, and artificial intelligence can facilitate the identification of specific immunological characteristics of patients. 254 , 255 , 256 , 257 This approach represents a novel avenue for cancer immunotherapy, aimed at converting “cold” tumors into “hot” tumors, thereby creating a conducive environment for enhancing the effectiveness of immunotherapy, which has great potential for clinical application.
Although great progress has been made in recent years, limited by the spatial distribution of immune cells, cold tumors are often “insensitive” to immunotherapy, and ICI treatment is still limited in the treatment of cold and altered tumors. There is still a lot to learn about how to overcome the limitations of ICI in cold tumor therapy. Local immunomodulatory therapy, such as elevating the expression of tumor antigens, restoring antigen processing and presentation, and reprogramming TME, can promote T cell transport and enable T cells to infiltrate tumor more effectively, resulting in synergistic effect with ICI. 258 However, the existence of immune response and immune drug resistance is likely to limit the efficacy of a single ICI due to tumor‐mediated immunosuppression. The colder the tumor, the more it requires a combination of therapies to achieve significant results.
Multitargets drug therapy may represent the future of “hotness and coldness tumor” immunotherapy strategies. From the current situation, molecular drugs represented by targeted therapies and immunotherapies are important parts of cancer research. Targeted drugs prevent the growth of cancer cells by interacting with specific molecular targets necessary for cancer occurrence and tumor growth, while immunotherapy restarts and maintains the tumor‐immune cycle to restore the body's normal antitumor immune response, control and eliminate cancer cells. However, the mechanisms of cancer occurrence and progression are very complex, more than one related gene is involved, often rely on a variety of signaling pathways to maintain growth and survival, and there is crossover and compensation between signaling pathways, only inhibiting one (or the same type of) target has limited effect. For cancer patients, targeted therapy or immunotherapy that has a single‐target is prone to drug resistance, thus affecting the long‐term efficacy of cancer treatment, and multitarget therapy that inhibits multiple signaling pathways or multiple molecules in downstream of a pathway to achieve simultaneous treatment can effectively plan for this shortcoming. Therefore, the future research direction of “coldness and hotness tumor” is to combine the advantages of targeted therapy and immunotherapy, develop a single drug target to a multitarget direction, and enhance the immune response of “coldness tumor” effectively.
Targeted therapies for the precise treatment of cancer based on genetic mutations and Immunotherapy for individualized cancer treatment based on TME and tumor heterogeneity provide a variety of cancer therapies for the research of “hotness and coldness tumors.” Now we can fortunately see that under the precision and personalized combined treatment, some malignant tumors have become a slowly progressing disease, patients can survive for a long time, and malignant tumors have entered the era of “chronic disease.” With the existing drugs, it is very necessary to develop multitarget drugs that transform “coldness tumor” into “hotness tumor” to meet clinical needs. The natural drugs recorded in TCM may be the best treasure house to search for multitarget drugs. Whether it is plant drugs, animal drugs or mineral drugs, the rich and effective drug components provide important data for the research of multitarget drugs for cancer treatment.
AUTHOR CONTRIBUTIONS
Lianjie Wang, Hui Geng, and Yujie Liu contributed to the conception of the study and wrote the initial draft. Lei Liu, Yanhua Chen, Fanchen Wu, and Zhiyi Liu reviewed the manuscript and provided suggestions for revision. Shiliang Ling, Yan Wang, and Lihong Zhou helped perform the analysis with constructive discussions. All authors read and approved the final manuscript.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest regarding the publication of this paper.
ETHICS STATEMENT
Not applicable.
ACKNOWLEDGMENTS
We thank Sizhi Paul Gao, who is the senior research fellow from Memorial Sloan Kettering Cancer Center of USA, and Fuwen Yuan, who is the professor from Academy of Integrative Medicine, Shanghai University of Traditional Chinese Medicine, for their correction of language on this review.
Wang L, Geng H, Liu Y, et al. Hot and cold tumors: Immunological features and the therapeutic strategies. MedComm. 2023;4:e343. 10.1002/mco2.343
Contributor Information
Shiliang Ling, Email: sliang621@163.com.
Yan Wang, Email: bw0999@hotmail.com.
Lihong Zhou, Email: zlhtcm@hotmail.com.
DATA AVAILABILITY STATEMENT
Not applicable.
REFERENCES
- 1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: gLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209‐249. [DOI] [PubMed] [Google Scholar]
- 2. Tsimberidou AM, Fountzilas E, Nikanjam M, Kurzrock R. Review of precision cancer medicine: evolution of the treatment paradigm. Cancer Treat Rev. 2020;86:102019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mirnezami R, Nicholson J, Darzi A. Preparing for precision medicine. N Engl J Med. 2012;366(6):489‐491. [DOI] [PubMed] [Google Scholar]
- 4. Garraway LA, Verweij J, Ballman KV. Precision oncology: an overview. J Clin Oncol. 2013;31(15):1803‐1805. [DOI] [PubMed] [Google Scholar]
- 5. Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med. 2015;372(9):793‐795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Rubin MA. Health: make precision medicine work for cancer care. Nature. 2015;520(7547):290‐291. [DOI] [PubMed] [Google Scholar]
- 7. Janiaud P, Serghiou S, Ioannidis JPA. New clinical trial designs in the era of precision medicine: an overview of definitions, strengths, weaknesses, and current use in oncology. Cancer Treat Rev. 2019;73:20‐30. [DOI] [PubMed] [Google Scholar]
- 8. Duan J, Cui L, Zhao X, et al. Use of immunotherapy with programmed cell death 1 vs programmed cell death ligand 1 inhibitors in patients with cancer: a systematic review and meta‐analysis. JAMA Oncol. 2020;6(3):375‐384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lin H, Cheng J, Mu W, Zhou J, Zhu L. Advances in universal CAR‐T cell therapy. Front Immunol. 2021;12:744823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Ma S, Li X, Wang X, et al. Current progress in CAR‐T cell therapy for solid tumors. Int J Biol Sci. 2019;15(12):2548‐2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Newick K, O'Brien S, Moon E, Albelda SM. CAR T cell therapy for solid tumors. Annu Rev Med. 2017;68:139‐152. [DOI] [PubMed] [Google Scholar]
- 12. Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001;357(9255):539‐545. [DOI] [PubMed] [Google Scholar]
- 13. Coley WB II. Contribution to the knowledge of sarcoma. Ann Surg. 1891;14(3):199‐220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Camus M, Tosolini M, Mlecnik B, et al. Coordination of intratumoral immune reaction and human colorectal cancer recurrence. Cancer Res. 2009;69(6):2685‐2693. [DOI] [PubMed] [Google Scholar]
- 15. Chen DS, Mellman I. Elements of cancer immunity and the cancer‐immune set point. Nature. 2017;541(7637):321‐330. [DOI] [PubMed] [Google Scholar]
- 16. Galon J, Mlecnik B, Bindea G, et al. Towards the introduction of the ‘Immunoscore’ in the classification of malignant tumours. J Pathol. 2014;232(2):199‐209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pages F, Mlecnik B, Marliot F, et al. International validation of the consensus Immunoscore for the classification of colon cancer: a prognostic and accuracy study. Lancet. 2018;391(10135):2128‐2139. [DOI] [PubMed] [Google Scholar]
- 18. Miller KD, Nogueira L, Mariotto AB, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363‐385. [DOI] [PubMed] [Google Scholar]
- 19. Ioannides CG, Whiteside TL. T cell recognition of human tumors: implications for molecular immunotherapy of cancer. Clin Immunol Immunopathol. 1993;66(2):91‐106. [DOI] [PubMed] [Google Scholar]
- 20. Galon J, Bruni D. Approaches to treat immune hot, altered and cold tumours with combination immunotherapies. Nat Rev Drug Discov. 2019;18(3):197‐218. [DOI] [PubMed] [Google Scholar]
- 21. Sharma P, Allison JP. The future of immune checkpoint therapy. Science. 2015;348(6230):56‐61. [DOI] [PubMed] [Google Scholar]
- 22. Galon J, Costes A, Sanchez‐Cabo F, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science. 2006;313(5795):1960‐1964. [DOI] [PubMed] [Google Scholar]
- 23. Horjus Talabur Horje CS, Smids C, Meijer JW, et al. High endothelial venules associated with T cell subsets in the inflamed gut of newly diagnosed inflammatory bowel disease patients. Clin Exp Immunol. 2017;188(1):163‐173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Muniz LR, Pacer ME, Lira SA, Furtado GC. A critical role for dendritic cells in the formation of lymphatic vessels within tertiary lymphoid structures. J Immunol. 2011;187(2):828‐834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ley K. M1 means kill; M2 means heal. J Immunol. 2017;199(7):2191‐2193. [DOI] [PubMed] [Google Scholar]
- 26. Gajewski TF, Schreiber H, Fu YX. Innate and adaptive immune cells in the tumor microenvironment. Nat Immunol. 2013;14(10):1014‐1022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kwok G, Yau TC, Chiu JW, Tse E, Kwong YL. Pembrolizumab (Keytruda). Hum Vaccin Immunother. 2016;12(11):2777‐2789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Conforti F, Pala L, Bagnardi V, et al. Cancer immunotherapy efficacy and patients' sex: a systematic review and meta‐analysis. Lancet Oncol. 2018;19(6):737‐746. [DOI] [PubMed] [Google Scholar]
- 29. Finkelmeier F, Waidmann O, Trojan J. Nivolumab for the treatment of hepatocellular carcinoma. Expert Rev Anticancer Ther. 2018;18(12):1169‐1175. [DOI] [PubMed] [Google Scholar]
- 30. Smith KM, Desai J. Nivolumab for the treatment of colorectal cancer. Expert Rev Anticancer Ther. 2018;18(7):611‐618. [DOI] [PubMed] [Google Scholar]
- 31. Fulchiero E, Jimeno A. Nivolumab. Drugs Today (Barc). 2014;50(12):791‐802. [DOI] [PubMed] [Google Scholar]
- 32. Koppolu V, Rekha Vasigala VK. Checkpoint immunotherapy by nivolumab for treatment of metastatic melanoma. J Cancer Res Ther. 2018;14(6):1167‐1175. [DOI] [PubMed] [Google Scholar]
- 33. Cercek A, Lumish M, Sinopoli J, et al. PD‐1 blockade in mismatch repair‐deficient, locally advanced rectal cancer. N Engl J Med. 2022;386(25):2363‐2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Markham A. Dostarlimab: first approval. Drugs. 2021;81(10):1213‐1219. [DOI] [PubMed] [Google Scholar]
- 35. Zhang L, Hao B, Geng Z, Geng Q. Toripalimab: the first domestic anti‐tumor PD‐1 antibody in China. Front Immunol. 2021;12:730666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Keam SJ. Toripalimab: first global approval. Drugs. 2019;79(5):573‐578. [DOI] [PubMed] [Google Scholar]
- 37. Lee A, Keam SJ. Tislelizumab: first approval. Drugs. 2020;80(6):617‐624. [DOI] [PubMed] [Google Scholar]
- 38. Liu SY, Wu YL. Tislelizumab: an investigational anti‐PD‐1 antibody for the treatment of advanced non‐small cell lung cancer (NSCLC). Expert Opin Investig Drugs. 2020;29(12):1355‐1364. [DOI] [PubMed] [Google Scholar]
- 39. Markham A, Keam SJ. Camrelizumab: first global approval. Drugs. 2019;79(12):1355‐1361. [DOI] [PubMed] [Google Scholar]
- 40. Luo H, Lu J, Bai Y, et al. Effect of camrelizumab vs placebo added to chemotherapy on survival and progression‐free survival in patients with advanced or metastatic esophageal squamous cell carcinoma: the ESCORT‐1st randomized clinical trial. JAMA. 2021;326(10):916‐925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hoy SM. Sintilimab: first global approval. Drugs. 2019;79(3):341‐346. [DOI] [PubMed] [Google Scholar]
- 42. Zhang L, Mai W, Jiang W, Geng Q. Sintilimab: a promising anti‐tumor PD‐1 antibody. Front Oncol. 2020;10:594558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Dhillon S. Penpulimab: first approval. Drugs. 2021;81(18):2159‐2166. [DOI] [PubMed] [Google Scholar]
- 44. Song Y, Zhou K, Jin C, et al. Penpulimab for relapsed or refractory classical hodgkin lymphoma: a multicenter, single‐arm, pivotal phase I/II trial (AK105‐201). Front Oncol. 2022;12:925236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Markham A. Zimberelimab: first approval. Drugs. 2021;81(17):2063‐2068. [DOI] [PubMed] [Google Scholar]
- 46. Lin N, Zhang M, Bai H, et al. Efficacy and safety of GLS‐010 (zimberelimab) in patients with relapsed or refractory classical Hodgkin lymphoma: a multicenter, single‐arm, phase II study. Eur J Cancer. 2022;164:117‐126. [DOI] [PubMed] [Google Scholar]
- 47. Lee A. Serplulimab: first approval. Drugs. 2022;82(10):1137‐1141. [DOI] [PubMed] [Google Scholar]
- 48. Zhu Y, Liu K, Qin Q, Zhu H. Serplulimab plus chemotherapy as first‐line treatment for extensive‐stage small‐cell lung cancer: a cost‐effectiveness analysis. Front Immunol. 2022;13:1044678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Qin S, Li J, Zhong H, et al. Serplulimab, a novel anti‐PD‐1 antibody, in patients with microsatellite instability‐high solid tumours: an open‐label, single‐arm, multicentre, phase II trial. Br J Cancer. 2022;127(12):2241‐2248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Cao J, Wang B, Zhang J, Tao Z, Wang L, Hu X. Phase 1b clinical trial of pucotenlimab (HX008), a novel anti‐PD‐1 monoclonal antibody, combined with gemcitabine and cisplatin in the first‐line treatment of metastatic triple‐negative breast cancer. Front Oncol. 2022;12:837963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Dhillon S. Pucotenlimab: first approval. Drugs. 2022;82(15):1557‐1564. [DOI] [PubMed] [Google Scholar]
- 52. Markham A. Atezolizumab: first global approval. Drugs. 2016;76(12):1227‐1232. [DOI] [PubMed] [Google Scholar]
- 53. Reddy SM, Carroll E, Nanda R. Atezolizumab for the treatment of breast cancer. Expert Rev Anticancer Ther. 2020;20(3):151‐158. [DOI] [PubMed] [Google Scholar]
- 54. Syed YY. Durvalumab: first global approval. Drugs. 2017;77(12):1369‐1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Alvarez‐Argote J, Dasanu CA. Durvalumab in cancer medicine: a comprehensive review. Expert Opin Biol Ther. 2019;19(9):927‐935. [DOI] [PubMed] [Google Scholar]
- 56. Li J, Deng Y, Zhang W, et al. Subcutaneous envafolimab monotherapy in patients with advanced defective mismatch repair/microsatellite instability high solid tumors. J Hematol Oncol. 2021;14(1):95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Markham A. Envafolimab: first approval. Drugs. 2022;82(2):235‐240. [DOI] [PubMed] [Google Scholar]
- 58. Dhillon S, Duggan S. Sugemalimab: first approval. Drugs. 2022;82(5):593‐599. [DOI] [PubMed] [Google Scholar]
- 59. Zhou C, Wang Z, Sun Y, et al. Sugemalimab versus placebo, in combination with platinum‐based chemotherapy, as first‐line treatment of metastatic non‐small‐cell lung cancer (GEMSTONE‐302): interim and final analyses of a double‐blind, randomised, phase 3 clinical trial. Lancet Oncol. 2022;23(2):220‐233. [DOI] [PubMed] [Google Scholar]
- 60. Zhou Q, Chen M, Jiang O, et al. Sugemalimab versus placebo after concurrent or sequential chemoradiotherapy in patients with locally advanced, unresectable, stage III non‐small‐cell lung cancer in China (GEMSTONE‐301): interim results of a randomised, double‐blind, multicentre, phase 3 trial. Lancet Oncol. 2022;23(2):209‐219. [DOI] [PubMed] [Google Scholar]
- 61. Wang J, Zhou C, Yao W, et al. Adebrelimab or placebo plus carboplatin and etoposide as first‐line treatment for extensive‐stage small‐cell lung cancer (CAPSTONE‐1): a multicentre, randomised, double‐blind, placebo‐controlled, phase 3 trial. Lancet Oncol. 2022;23(6):739‐747. [DOI] [PubMed] [Google Scholar]
- 62. Yan W, Zhong WZ, Liu YH, et al. Adebrelimab (SHR‐1316) in combination with chemotherapy as perioperative treatment in patients with resectable stage II to III NSCLCs: an open‐label, multicenter, phase 1b trial. J Thorac Oncol. 2023;18(2):194‐203. [DOI] [PubMed] [Google Scholar]
- 63. Cameron F, Whiteside G, Perry C. Ipilimumab: first global approval. Drugs. 2011;71(8):1093‐1104. [DOI] [PubMed] [Google Scholar]
- 64. Korman AJ, Garrett‐Thomson SC, Lonberg N. The foundations of immune checkpoint blockade and the ipilimumab approval decennial. Nat Rev Drug Discov. 2022;21(7):509‐528. [DOI] [PubMed] [Google Scholar]
- 65. Keam SJ. Cadonilimab: first approval. Drugs. 2022;82(12):1333‐1339. [DOI] [PubMed] [Google Scholar]
- 66. Pang X, Huang Z, Zhong T, et al. Cadonilimab, a tetravalent PD‐1/CTLA‐4 bispecific antibody with trans‐binding and enhanced target binding avidity. MAbs. 2023;15(1):2180794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Boger C, Behrens HM, Mathiak M, Kruger S, Kalthoff H, Rocken C. PD‐L1 is an independent prognostic predictor in gastric cancer of Western patients. Oncotarget. 2016;7(17):24269‐24283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Yang B, Liu T, Qu Y, et al. Progresses and perspectives of anti‐PD‐1/PD‐L1 antibody therapy in head and neck cancers. Front Oncol. 2018;8:563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Jiang Y, Chen M, Nie H, Yuan Y. PD‐1 and PD‐L1 in cancer immunotherapy: clinical implications and future considerations. Hum Vaccin Immunother. 2019;15(5):1111‐1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Pardoll DM. The blockade of immune checkpoints in cancer immunotherapy. Nat Rev Cancer. 2012;12(4):252‐264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ai L, Chen J, Yan H, et al. Research status and outlook of PD‐1/PD‐L1 inhibitors for cancer therapy. Drug Des Devel Ther. 2020;14:3625‐3649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Rongshan C, Liyan X. Research progress of predictive markers for efficacy of immune checkpoint inhibitors for esophageal squamous cell carcinoma. Cancer Res Prevent Treat. 2022;49(12):1302‐1306. [Google Scholar]
- 73. Kulangara K, Zhang N, Corigliano E, et al. Clinical utility of the combined positive score for programmed death ligand‐1 expression and the approval of pembrolizumab for treatment of gastric cancer. Arch Pathol Lab Med. 2019;143(3):330‐337. [DOI] [PubMed] [Google Scholar]
- 74. Kulangara K, Hanks DA, Waldroup S, et al. Development of the combined positive score (CPS) for the evaluation of PD‐L1 in solid tumors with the immunohistochemistry assay PD‐L1 IHC 22C3 pharmDx. J Clin Oncol. 2017;35(15):e14589‐e14589. _suppl. [Google Scholar]
- 75. Yue‐jun W, Na‐na W, Miao‐miao Y, et al. Pathological study on expression and distribution of PD‐L1 protein in gastric cancer. Chinese J Clin Exp Pathol. 2019;35(09):1053‐1059. [Google Scholar]
- 76. Hogner A, Moehler M. Immunotherapy in gastric cancer. Curr Oncol. 2022;29(3):1559‐1574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Chang WJ, Du Y, Zhao X, Ma LY, Cao GW. Inflammation‐related factors predicting prognosis of gastric cancer. World J Gastroenterol. 2014;20(16):4586‐4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Johansson M, Denardo DG, Coussens LM. Polarized immune responses differentially regulate cancer development. Immunol Rev. 2008;222:145‐154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mossanen JC, Tacke F. Role of lymphocytes in liver cancer. Oncoimmunology. 2013;2(11):e26468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Wenya C, Shaoling R, Zhenguo Z. Research progress of tumor infiltrating lymphocytes in tumor immunity. Guangxi J Tradit Chinese Med. 2020;43(05):66‐68. [Google Scholar]
- 81. Hendry S, Salgado R, Gevaert T, et al. Assessing tumor‐infiltrating lymphocytes in solid tumors: a practical review for pathologists and proposal for a standardized method from the international immunooncology biomarkers working group: part 1: assessing the host immune response, TILs in invasive breast carcinoma and ductal carcinoma in situ, metastatic tumor deposits and areas for further research. Adv Anat Pathol. 2017;24(5):235‐251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Denkert C, Loibl S, Noske A, et al. Tumor‐associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol. 2010;28(1):105‐113. [DOI] [PubMed] [Google Scholar]
- 83. Ying L, Yan F, Meng Q, et al. Understanding immune phenotypes in human gastric disease tissues by multiplexed immunohistochemistry. J Transl Med. 2017;15(1):206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Shirasawa M, Yoshida T, Shimoda Y, et al. Differential immune‐related microenvironment determines programmed cell death protein‐1/programmed death‐ligand 1 blockade efficacy in patients with advanced NSCLC. J Thorac Oncol. 2021;16(12):2078‐2090. [DOI] [PubMed] [Google Scholar]
- 85. Williams DS, Mouradov D, Jorissen RN, et al. Lymphocytic response to tumour and deficient DNA mismatch repair identify subtypes of stage II/III colorectal cancer associated with patient outcomes. Gut. 2019;68(3):465‐474. [DOI] [PubMed] [Google Scholar]
- 86. Ruddle NH. Basics of inducible lymphoid organs. Curr Top Microbiol Immunol. 2020;426:1‐19. [DOI] [PubMed] [Google Scholar]
- 87. Munoz‐Erazo L, Rhodes JL, Marion VC, Kemp RA. Tertiary lymphoid structures in cancer ‐ considerations for patient prognosis. Cell Mol Immunol. 2020;17(6):570‐575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Da‐chuan Z, Wen‐ting H, Lei P, Yang H, Jing‐ting J, Qing L. Tertiary lymphoid structure in gastric cancer and its clinical significance. Chinese J Clin Exp Pathol. 2019;35(02):139‐143. [Google Scholar]
- 89. Helmink BA, Reddy SM, Gao J, et al. B cells and tertiary lymphoid structures promote immunotherapy response. Nature. 2020;577(7791):549‐555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Dieu‐Nosjean MC, Antoine M, Danel C, et al. Long‐term survival for patients with non‐small‐cell lung cancer with intratumoral lymphoid structures. J Clin Oncol. 2008;26(27):4410‐4417. [DOI] [PubMed] [Google Scholar]
- 91. Goc J, Germain C, Vo‐Bourgais TK, et al. Dendritic cells in tumor‐associated tertiary lymphoid structures signal a Th1 cytotoxic immune contexture and license the positive prognostic value of infiltrating CD8+ T cells. Cancer Res. 2014;74(3):705‐715. [DOI] [PubMed] [Google Scholar]
- 92. Silina K, Soltermann A, Attar FM, et al. Germinal centers determine the prognostic relevance of tertiary lymphoid structures and are impaired by corticosteroids in lung squamous cell carcinoma. Cancer Res. 2018;78(5):1308‐1320. [DOI] [PubMed] [Google Scholar]
- 93. Ukita M, Hamanishi J, Yoshitomi H, et al. CXCL13‐producing CD4+ T cells accumulate in the early phase of tertiary lymphoid structures in ovarian cancer. JCI Insight. 2022;7(12):e157215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Salem D, Chelvanambi M, Storkus WJ, Fecek RJ. Cutaneous melanoma: mutational status and potential links to tertiary lymphoid structure formation. Front Immunol. 2021;12:629519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Cabrita R, Lauss M, Sanna A, et al. Tertiary lymphoid structures improve immunotherapy and survival in melanoma. Nature. 2020;577(7791):561‐565. [DOI] [PubMed] [Google Scholar]
- 96. Posch F, Silina K, Leibl S, et al. Maturation of tertiary lymphoid structures and recurrence of stage II and III colorectal cancer. Oncoimmunology. 2018;7(2):e1378844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Ruffin AT, Cillo AR, Tabib T, et al. B cell signatures and tertiary lymphoid structures contribute to outcome in head and neck squamous cell carcinoma. Nat Commun. 2021;12(1):3349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Li K, Guo Q, Zhang X, et al. Oral cancer‐associated tertiary lymphoid structures: gene expression profile and prognostic value. Clin Exp Immunol. 2020;199(2):172‐181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Finkin S, Yuan D, Stein I, et al. Ectopic lymphoid structures function as microniches for tumor progenitor cells in hepatocellular carcinoma. Nat Immunol. 2015;16(12):1235‐1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Calderaro J, Petitprez F, Becht E, et al. Intra‐tumoral tertiary lymphoid structures are associated with a low risk of early recurrence of hepatocellular carcinoma. J Hepatol. 2019;70(1):58‐65. [DOI] [PubMed] [Google Scholar]
- 101. Prabhakaran S, Rizk VT, Ma Z, et al. Evaluation of invasive breast cancer samples using a 12‐chemokine gene expression score: correlation with clinical outcomes. Breast Cancer Res. 2017;19(1):71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Gadgil R, Barthelemy J, Lewis T, Leffak M. Replication stalling and DNA microsatellite instability. Biophys Chem. 2017;225:38‐48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103. Shinozuka K, Tang H, Jones RB, Li D, Nieto Y. Impact of polymorphic variations of gemcitabine metabolism, DNA damage repair, and drug‐resistance genes on the effect of high‐dose chemotherapy for relapsed or refractory lymphoid malignancies. Biol Blood Marrow Transplant. 2016;22(5):843‐849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Liu X, Meltzer SJ. Gastric cancer in the era of precision medicine. Cell Mol Gastroenterol Hepatol. 2017;3(3):348‐358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Le DT, Uram JN, Wang H, et al. PD‐1 blockade in tumors with mismatch‐repair deficiency. N Engl J Med. 2015;372(26):2509‐2520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Verma R, Agarwal AK, Sakhuja P, Sharma PC. Microsatellite instability in mismatch repair and tumor suppressor genes and their expression profiling provide important targets for the development of biomarkers in gastric cancer. Gene. 2019;710:48‐58. [DOI] [PubMed] [Google Scholar]
- 107. Kloor M, Staffa L, Ahadova A, von Knebel Doeberitz M. Clinical significance of microsatellite instability in colorectal cancer. Langenbecks Arch Surg. 2014;399(1):23‐31. [DOI] [PubMed] [Google Scholar]
- 108. Li K, Luo H, Huang L, Luo H, Zhu X. Microsatellite instability: a review of what the oncologist should know. Cancer Cell Int. 2020;20:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Chang L, Chang M, Chang HM, Chang F. Microsatellite instability: a predictive biomarker for cancer immunotherapy. Appl Immunohistochem Mol Morphol. 2018;26(2):e15‐e21. [DOI] [PubMed] [Google Scholar]
- 110. Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD‐1 blockade. Science. 2017;357(6349):409‐413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Overman MJ, Lonardi S, Wong KYM, et al. Durable clinical benefit with nivolumab plus ipilimumab in DNA mismatch repair‐deficient/microsatellite instability‐high metastatic colorectal cancer. J Clin Oncol. 2018;36(8):773‐779. [DOI] [PubMed] [Google Scholar]
- 112. Overman MJ, McDermott R, Leach JL, et al. Nivolumab in patients with metastatic DNA mismatch repair‐deficient or microsatellite instability‐high colorectal cancer (CheckMate 142): an open‐label, multicentre, phase 2 study. Lancet Oncol. 2017;18(9):1182‐1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Diaz LA, Marabelle A, Delord J‐P, et al. Pembrolizumab therapy for microsatellite instability high (MSI‐H) colorectal cancer (CRC) and non‐CRC. J Clin Oncol. 2017;35(15_suppl):3071‐3071. [Google Scholar]
- 114. O'Malley DM, Bariani GM, Cassier PA, et al. Pembrolizumab in patients with microsatellite instability‐high advanced endometrial cancer: results from the KEYNOTE‐158 study. J Clin Oncol. 2022;40(7):752‐761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Marabelle A, Le DT, Ascierto PA, et al. Efficacy of pembrolizumab in patients with noncolorectal high microsatellite instability/mismatch repair‐deficient cancer: results from the phase II KEYNOTE‐158 study. J Clin Oncol. 2020;38(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Zhang X, Shi M, Chen T, Zhang B. Characterization of the immune cell infiltration landscape in head and neck squamous cell carcinoma to aid immunotherapy. Mol Ther Nucleic Acids. 2020;22:298‐309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Alexandrov LB, Nik‐Zainal S, Wedge DC, et al. Signatures of mutational processes in human cancer. Nature. 2013;500(7463):415‐421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Snyder A, Makarov V, Merghoub T, et al. Genetic basis for clinical response to CTLA‐4 blockade in melanoma. N Engl J Med. 2014;371(23):2189‐2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Chan TA, Yarchoan M, Jaffee E, et al. Development of tumor mutation burden as an immunotherapy biomarker: utility for the oncology clinic. Ann Oncol. 2019;30(1):44‐56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120. Subbiah V, Solit DB, Chan TA, Kurzrock R. The FDA approval of pembrolizumab for adult and pediatric patients with tumor mutational burden (TMB) >/= 10: a decision centered on empowering patients and their physicians. Ann Oncol. 2020;31(9):1115‐1118. [DOI] [PubMed] [Google Scholar]
- 121. Goodman A, Kato S, Bazhenova L, et al. Comprehensive genomic profiling to identify tumor mutational burden (TMB) as an independent predictor of response to immunotherapy in diverse cancers. J Clin Oncol. 2017;35(15_suppl):e14508‐e14508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Lee M, Samstein RM, Valero C, Chan TA, Morris LGT. Tumor mutational burden as a predictive biomarker for checkpoint inhibitor immunotherapy. Hum Vaccin Immunother. 2020;16(1):112‐115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Marabelle A, Fakih M, Lopez J, et al. Association of tumour mutational burden with outcomes in patients with advanced solid tumours treated with pembrolizumab: prospective biomarker analysis of the multicohort, open‐label, phase 2 KEYNOTE‐158 study. Lancet Oncol. 2020;21(10):1353‐1365. [DOI] [PubMed] [Google Scholar]
- 124. Donehower LA, Soussi T, Korkut A, et al. Integrated analysis of TP53 gene and pathway alterations in the cancer genome atlas. Cell Rep. 2019;28(11):3010. [DOI] [PubMed] [Google Scholar]
- 125. Kastenhuber ER, Lowe SW. Putting p53 in context. Cell. 2017;170(6):1062‐1078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Li L, Li M, Wang X. Cancer type‐dependent correlations between TP53 mutations and antitumor immunity. DNA Repair (Amst). 2020;88:102785. [DOI] [PubMed] [Google Scholar]
- 127. Goodman AM, Kato S, Bazhenova L, et al. Tumor mutational burden as an independent predictor of response to immunotherapy in diverse cancers. Mol Cancer Ther. 2017;16(11):2598‐2608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Maeda K, Kang SM, Sawada T, et al. Expression of intercellular adhesion molecule‐1 and prognosis in colorectal cancer. Oncol Rep. 2002;9(3):511‐544. [PubMed] [Google Scholar]
- 129. Fujihara T, Yashiro M, Inoue T, et al. Decrease in ICAM‐1 expression on gastric cancer cells is correlated with lymph node metastasis. Gastric Cancer. 1999;2(4):221‐225. [DOI] [PubMed] [Google Scholar]
- 130. Ogawa Y, Hirakawa K, Nakata B, et al. Expression of intercellular adhesion molecule‐1 in invasive breast cancer reflects low growth potential, negative lymph node involvement, and good prognosis. Clin Cancer Res. 1998;4(1):31‐36. [PubMed] [Google Scholar]
- 131. Koyama S, Ebihara T, Fukao K. Expression of intercellular adhesion molecule 1 (ICAM‐1) during the development of invasion and/or metastasis of gastric carcinoma. J Cancer Res Clin Oncol. 1992;118(8):609‐614. [DOI] [PubMed] [Google Scholar]
- 132. Zhang P, Huang Y. Genomic alterations in KMT2 family predict outcome of immune checkpoint therapy in multiple cancers. J Hematol Oncol. 2021;14(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Wang F, Zhao Q, Wang YN, et al. Evaluation of POLE and POLD1 mutations as biomarkers for immunotherapy outcomes across multiple cancer types. JAMA Oncol. 2019;5(10):1504‐1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134. Reck M, Rodriguez‐Abreu D, Robinson AG, et al. Updated analysis of KEYNOTE‐024: pembrolizumab versus platinum‐based chemotherapy for advanced non‐small‐cell lung cancer with PD‐L1 tumor proportion score of 50% or greater. J Clin Oncol. 2019;37(7):537‐546. [DOI] [PubMed] [Google Scholar]
- 135. Sezer A, Kilickap S, Gumus M, et al. Cemiplimab monotherapy for first‐line treatment of advanced non‐small‐cell lung cancer with PD‐L1 of at least 50%: a multicentre, open‐label, global, phase 3, randomised, controlled trial. Lancet. 2021;397(10274):592‐604. [DOI] [PubMed] [Google Scholar]
- 136. Qz S‐YML, Yan H‐H, Bin G, et al. Sintilimab versus pembrolizumab in monotherapy or combination with chemotherapy as first‐line therapy for advanced non–small cell lung cancer: Results from phase 2, randomized clinical trial (CTONG1901).
- 137. Sheng X, Chen H, Hu B, et al. Safety, efficacy, and biomarker analysis of toripalimab in patients with previously treated advanced urothelial carcinoma: results from a multicenter phase II trial POLARIS‐03. Clin Cancer Res. 2022;28(3):489‐497. [DOI] [PubMed] [Google Scholar]
- 138. Zhao M, Liu X, Yuan C, et al. 16P Camrelizumab monotherapy or plus apatinib for PD‐L1‐positive advanced pulmonary sarcomatoid carcinoma: a single‐arm, open‐label, multicenter, phase II study. Ann Oncol. 2022;33:S36‐S37. [Google Scholar]
- 139. Li J, Xu Y, Zang A, et al. A phase 2 study of tislelizumab monotherapy in patients with previously treated, locally advanced unresectable ormetastatic microsatellite instability‐high/mismatch repair deficient solid tumors. J Clin Oncol. 2021;39(15):2569‐2569. _suppl. [Google Scholar]
- 140. Spigel D, de Marinis F, Giaccone G, et al. IMpower110: interim overall survival (OS) analysis of a phase III study of atezolizumab (atezo) vs platinum‐based chemotherapy (chemo) as first‐line (1L) treatment (tx) in PD‐L1–selected NSCLC. Ann Oncol. 2019;30:v915. [Google Scholar]
- 141. Joseph AS, Brahmer JR, Sarkis BA, et al. Safety and clinical activity of first‐line durvalumab in advanced NSCLC: updated results from a Phase 1/2 study. J Clin Oncol. 2017;35(15_suppl):e20504. [Google Scholar]
- 142. Taieb J, Andre T, El Hajbi F, et al. Avelumab versus standard second line treatment chemotherapy in metastatic colorectal cancer patients with microsatellite instability: the SAMCO‐PRODIGE 54 randomised phase II trial. Dig Liver Dis. 2021;53(3):318‐323. [DOI] [PubMed] [Google Scholar]
- 143. Wu X, Ji J, Lou H, et al. Efficacy and safety of cadonilimab, an anti‐PD‐1/CTLA4 bi‐specific antibody, in previously treated recurrent or metastatic (R/M) cervical cancer: a multicenter, open‐label, single‐arm, phase II trial (075). Gynecol Oncol. 2022;166:S47‐S48. [Google Scholar]
- 144. Kim JM, Chen DS. Immune escape to PD‐L1/PD‐1 blockade: seven steps to success (or failure). Ann Oncol. 2016;27(8):1492‐1504. [DOI] [PubMed] [Google Scholar]
- 145. Smyth MJ, Ngiow SF, Ribas A, Teng MW. Combination cancer immunotherapies tailored to the tumour microenvironment. Nat Rev Clin Oncol. 2016;13(3):143‐158. [DOI] [PubMed] [Google Scholar]
- 146. Kitao H, Iimori M, Kataoka Y, et al. DNA replication stress and cancer chemotherapy. Cancer Sci. 2018;109(2):264‐271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Gotwals P, Cameron S, Cipolletta D, et al. Prospects for combining targeted and conventional cancer therapy with immunotherapy. Nat Rev Cancer. 2017;17(5):286‐301. [DOI] [PubMed] [Google Scholar]
- 148. Gallego Perez‐Larraya J, Garcia‐Moure M, Labiano S, et al. Oncolytic DNX‐2401 virus for pediatric diffuse intrinsic pontine glioma. N Engl J Med. 2022;386(26):2471‐2481. [DOI] [PubMed] [Google Scholar]
- 149. Mathew M, Enzler T, Shu CA, Rizvi NA. Combining chemotherapy with PD‐1 blockade in NSCLC. Pharmacol Ther. 2018;186:130‐137. [DOI] [PubMed] [Google Scholar]
- 150. Liang H, Lin G, Wang W, et al. Feasibility and safety of PD‐1/L1 inhibitors for non‐small cell lung cancer in front‐line treatment: a Bayesian network meta‐analysis. Transl Lung Cancer Res. 2020;9(2):188‐203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151. Zhou Y, Chen C, Zhang X, et al. Immune‐checkpoint inhibitor plus chemotherapy versus conventional chemotherapy for first‐line treatment in advanced non‐small cell lung carcinoma: a systematic review and meta‐analysis. J Immunother Cancer. 2018;6(1):155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Langer CJ, Gadgeel SM, Borghaei H, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non‐squamous non‐small‐cell lung cancer: a randomised, phase 2 cohort of the open‐label KEYNOTE‐021 study. Lancet Oncol. 2016;17(11):1497‐1508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Gandhi L, Rodriguez‐Abreu D, Gadgeel S, et al. Pembrolizumab plus chemotherapy in metastatic non‐small‐cell lung cancer. N Engl J Med. 2018;378(22):2078‐2092. [DOI] [PubMed] [Google Scholar]
- 154. Ho TTB, Nasti A, Seki A, et al. Combination of gemcitabine and anti‐PD‐1 antibody enhances the anticancer effect of M1 macrophages and the Th1 response in a murine model of pancreatic cancer liver metastasis. J Immunother Cancer. 2020;8(2):e001367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155. Davern M, Donlon NE, Sheppard A, et al. Chemotherapy regimens induce inhibitory immune checkpoint protein expression on stem‐like and senescent‐like oesophageal adenocarcinoma cells. Transl Oncol. 2021;14(6):101062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156. Di Tacchio M, Macas J, Weissenberger J, et al. Tumor vessel normalization, immunostimulatory reprogramming, and improved survival in glioblastoma with combined inhibition of PD‐1, angiopoietin‐2, and VEGF. Cancer Immunol Res. 2019;7(12):1910‐1927. [DOI] [PubMed] [Google Scholar]
- 157. Gao F, Yang C. Anti‐VEGF/VEGFR2 monoclonal antibodies and their combinations with PD‐1/PD‐L1 inhibitors in clinic. Curr Cancer Drug Targets. 2020;20(1):3‐18. [DOI] [PubMed] [Google Scholar]
- 158. Amin A, Plimack ER, Ernstoff MS, et al. Safety and efficacy of nivolumab in combination with sunitinib or pazopanib in advanced or metastatic renal cell carcinoma: the CheckMate 016 study. J Immunother Cancer. 2018;6(1):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159. Zhao S, Ren S, Jiang T, et al. Low‐dose apatinib optimizes tumor microenvironment and potentiates antitumor effect of PD‐1/PD‐L1 blockade in lung cancer. Cancer Immunol Res. 2019;7(4):630‐643. [DOI] [PubMed] [Google Scholar]
- 160. McDermott DF, Huseni MA, Atkins MB, et al. Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat Med. 2018;24(6):749‐757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Reck M, Mok TSK, Nishio M, et al. Atezolizumab plus bevacizumab and chemotherapy in non‐small‐cell lung cancer (IMpower150): key subgroup analyses of patients with EGFR mutations or baseline liver metastases in a randomised, open‐label phase 3 trial. Lancet Respir Med. 2019;7(5):387‐401. [DOI] [PubMed] [Google Scholar]
- 162. Sigismund S, Avanzato D, Lanzetti L. Emerging functions of the EGFR in cancer. Mol Oncol. 2018;12(1):3‐20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Liu Z, Han C, Dong C, et al. Hypofractionated EGFR tyrosine kinase inhibitor limits tumor relapse through triggering innate and adaptive immunity. Sci Immunol. 2019;4(38):eaav6473. [DOI] [PubMed] [Google Scholar]
- 164. Sugiyama E, Togashi Y, Takeuchi Y, et al. Blockade of EGFR improves responsiveness to PD‐1 blockade in EGFR‐mutated non‐small cell lung cancer. Sci Immunol. 2020;5(43):eaav3937. [DOI] [PubMed] [Google Scholar]
- 165. Chen DS, Hurwitz H. Combinations of bevacizumab with cancer immunotherapy. Cancer J. 2018;24(4):193‐204. [DOI] [PubMed] [Google Scholar]
- 166. Yi C, Chen L, Lin Z, et al. Lenvatinib targets FGF receptor 4 to enhance antitumor immune response of anti‐programmed cell death‐1 in HCC. Hepatology. 2021;74(5):2544‐2560. [DOI] [PubMed] [Google Scholar]
- 167. Ikeda K, Kudo M, Kawazoe S, et al. Phase 2 study of lenvatinib in patients with advanced hepatocellular carcinoma. J Gastroenterol. 2017;52(4):512‐519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Makker V, Taylor MH, Aghajanian C, et al. Lenvatinib plus pembrolizumab in patients with advanced endometrial cancer. J Clin Oncol. 2020;38(26):2981‐2992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Finn RS, Ikeda M, Zhu AX, et al. Phase ib study of lenvatinib plus pembrolizumab in patients with unresectable hepatocellular carcinoma. J Clin Oncol. 2020;38(26):2960‐2970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Arance A, de la Cruz‐Merino L, Petrella TM, et al. Phase II LEAP‐004 study of lenvatinib plus pembrolizumab for melanoma with confirmed progression on a programmed cell death protein‐1 or programmed death ligand 1 inhibitor given as monotherapy or in combination. J Clin Oncol. 2022:JCO2200221. [DOI] [PubMed] [Google Scholar]
- 171. Wu K, Yi M, Qin S, Chu Q, Zheng X, Wu K. The efficacy and safety of combination of PD‐1 and CTLA‐4 inhibitors: a meta‐analysis. Exp Hematol Oncol. 2019;8:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172. Kim SY, Halmos B. Choosing the best first‐line therapy: nSCLC with no actionable oncogenic driver. Lung Cancer Manag. 2020;9(3):LMT36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Puri S, Shafique M. Combination checkpoint inhibitors for treatment of non‐small‐cell lung cancer: an update on dual anti‐CTLA‐4 and anti‐PD‐1/PD‐L1 therapies. Drugs Context. 2020;9:2019‐2019‐2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Topalian SL, Drake CG, Pardoll DM. Immune checkpoint blockade: a common denominator approach to cancer therapy. Cancer Cell. 2015;27(4):450‐461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Buchbinder EI, Desai A. CTLA‐4 and PD‐1 pathways: similarities, differences, and implications of their inhibition. Am J Clin Oncol. 2016;39(1):98‐106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Harjunpaa H, Guillerey C. TIGIT as an emerging immune checkpoint. Clin Exp Immunol. 2020;200(2):108‐119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Curran MA, Montalvo W, Yagita H, Allison JP. PD‐1 and CTLA‐4 combination blockade expands infiltrating T cells and reduces regulatory T and myeloid cells within B16 melanoma tumors. Proc Natl Acad Sci USA. 2010;107(9):4275‐4280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178. Hodi FS, Chesney J, Pavlick AC, et al. Combined nivolumab and ipilimumab versus ipilimumab alone in patients with advanced melanoma: 2‐year overall survival outcomes in a multicentre, randomised, controlled, phase 2 trial. Lancet Oncol. 2016;17(11):1558‐1568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Larkin J, Chiarion‐Sileni V, Gonzalez R, et al. Five‐year survival with combined nivolumab and ipilimumab in advanced melanoma. N Engl J Med. 2019;381(16):1535‐1546. [DOI] [PubMed] [Google Scholar]
- 180. Hannier S, Tournier M, Bismuth G, Triebel F. CD3/TCR complex‐associated lymphocyte activation gene‐3 molecules inhibit CD3/TCR signaling. J Immunol. 1998;161(8):4058‐4065. [PubMed] [Google Scholar]
- 181. Ferris RL, Blumenschein G Jr, Fayette J, et al. Nivolumab for recurrent squamous‐cell carcinoma of the head and neck. N Engl J Med. 2016;375(19):1856‐1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182. Huang RY, Eppolito C, Lele S, Shrikant P, Matsuzaki J, Odunsi K. LAG3 and PD1 co‐inhibitory molecules collaborate to limit CD8+ T cell signaling and dampen antitumor immunity in a murine ovarian cancer model. Oncotarget. 2015;6(29):27359‐27377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183. Goding SR, Wilson KA, Xie Y, et al. Restoring immune function of tumor‐specific CD4+ T cells during recurrence of melanoma. J Immunol. 2013;190(9):4899‐4909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Sun F, Guo ZS, Gregory AD, Shapiro SD, Xiao G, Qu Z. Dual but not single PD‐1 or TIM‐3 blockade enhances oncolytic virotherapy in refractory lung cancer. J Immunother Cancer. 2020;8(1):e000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185. Sakuishi K, Apetoh L, Sullivan JM, Blazar BR, Kuchroo VK, Anderson AC. Targeting Tim‐3 and PD‐1 pathways to reverse T cell exhaustion and restore anti‐tumor immunity. J Exp Med. 2010;207(10):2187‐2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Lim JY, Gerber SA, Murphy SP, Lord EM. Type I interferons induced by radiation therapy mediate recruitment and effector function of CD8(+) T cells. Cancer Immunol Immunother. 2014;63(3):259‐271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Wang X, Schoenhals JE, Li A, et al. Suppression of type I IFN signaling in tumors mediates resistance to anti‐PD‐1 treatment that can be overcome by radiotherapy. Cancer Res. 2017;77(4):839‐850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Deng L, Liang H, Burnette B, et al. Irradiation and anti‐PD‐L1 treatment synergistically promote antitumor immunity in mice. J Clin Invest. 2014;124(2):687‐695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189. Hwang WL, Pike LRG, Royce TJ, Mahal BA, Loeffler JS. Safety of combining radiotherapy with immune‐checkpoint inhibition. Nat Rev Clin Oncol. 2018;15(8):477‐494. [DOI] [PubMed] [Google Scholar]
- 190. Lhuillier C, Rudqvist NP, Elemento O, Formenti SC, Demaria S. Radiation therapy and anti‐tumor immunity: exposing immunogenic mutations to the immune system. Genome Med. 2019;11(1):40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Howells CC, Stinauer MA, Diot Q, et al. Normal liver tissue density dose response in patients treated with stereotactic body radiation therapy for liver metastases. Int J Radiat Oncol Biol Phys. 2012;84(3):e441‐446. [DOI] [PubMed] [Google Scholar]
- 192. Timmerman RD, Herman J, Cho LC. Emergence of stereotactic body radiation therapy and its impact on current and future clinical practice. J Clin Oncol. 2014;32(26):2847‐2854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193. Huang Q, Li F, Liu X, et al. Caspase 3‐mediated stimulation of tumor cell repopulation during cancer radiotherapy. Nat Med. 2011;17(7):860‐866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Altorki NK, McGraw TE, Borczuk AC, et al. Neoadjuvant durvalumab with or without stereotactic body radiotherapy in patients with early‐stage non‐small‐cell lung cancer: a single‐centre, randomised phase 2 trial. Lancet Oncol. 2021;22(6):824‐835. [DOI] [PubMed] [Google Scholar]
- 195. Ahmed KA, Stallworth DG, Kim Y, et al. Clinical outcomes of melanoma brain metastases treated with stereotactic radiation and anti‐PD‐1 therapy. Ann Oncol. 2016;27(3):434‐441. [DOI] [PubMed] [Google Scholar]
- 196. Garg AD, Agostinis P. Cell death and immunity in cancer: from danger signals to mimicry of pathogen defense responses. Immunol Rev. 2017;280(1):126‐148. [DOI] [PubMed] [Google Scholar]
- 197. Cai J, Lin Y, Zhang H, et al. Selective replication of oncolytic virus M1 results in a bystander killing effect that is potentiated by Smac mimetics. Proc Natl Acad Sci USA. 2017;114(26):6812‐6817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. VanSeggelen H, Tantalo DG, Afsahi A, Hammill JA, Bramson JL. Chimeric antigen receptor‐engineered T cells as oncolytic virus carriers. Mol Ther Oncolytics. 2015;2:15014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Kaufman HL, Kohlhapp FJ, Zloza A. Oncolytic viruses: a new class of immunotherapy drugs. Nat Rev Drug Discov. 2015;14(9):642‐662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200. Coffin R. Interview with Robert Coffin, inventor of T‐VEC: the first oncolytic immunotherapy approved for the treatment of cancer. Immunotherapy. 2016;8(2):103‐106. [DOI] [PubMed] [Google Scholar]
- 201. Ribas A, Dummer R, Puzanov I, et al. Oncolytic virotherapy promotes intratumoral t cell infiltration and improves anti‐PD‐1 immunotherapy. Cell. 2017;170(6):1109‐1119 e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202. Guo ZS, Lu B, Guo Z, et al. Vaccinia virus‐mediated cancer immunotherapy: cancer vaccines and oncolytics. J Immunother Cancer. 2019;7(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203. Kowalsky SJ, Liu Z, Feist M, et al. Superagonist IL‐15‐armed oncolytic virus elicits potent antitumor immunity and therapy that are enhanced with PD‐1 blockade. Mol Ther. 2018;26(10):2476‐2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Wang N, Wang J, Zhang Z, et al. A novel vaccinia virus enhances anti‐tumor efficacy and promotes a long‐term anti‐tumor response in a murine model of colorectal cancer. Mol Ther Oncolytics. 2021;20:71‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205. Liu Z, Ravindranathan R, Kalinski P, Guo ZS, Bartlett DL. Rational combination of oncolytic vaccinia virus and PD‐L1 blockade works synergistically to enhance therapeutic efficacy. Nat Commun. 2017;8:14754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206. Lee YS, Lee WS, Kim CW, et al. Oncolytic vaccinia virus reinvigorates peritoneal immunity and cooperates with immune checkpoint inhibitor to suppress peritoneal carcinomatosis in colon cancer. J Immunother Cancer. 2020;8(2):e000857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207. Bommareddy PK, Aspromonte S, Zloza A, Rabkin SD, Kaufman HL. MEK inhibition enhances oncolytic virus immunotherapy through increased tumor cell killing and T cell activation. Sci Transl Med. 2018;10(471):eaau0417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208. Melero I, Gato M, Shekarian T, et al. Repurposing infectious disease vaccines for intratumoral immunotherapy. J Immunother Cancer. 2020;8(1):e000443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209. Shekarian T, Sivado E, Jallas AC, et al. Repurposing rotavirus vaccines for intratumoral immunotherapy can overcome resistance to immune checkpoint blockade. Sci Transl Med. 2019;11(515):eaat5025. [DOI] [PubMed] [Google Scholar]
- 210. Shemesh CS, Hsu JC, Hosseini I, et al. Personalized cancer vaccines: clinical landscape, challenges, and opportunities. Mol Ther. 2021;29(2):555‐570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211. Ott PA, Hu Z, Keskin DB, et al. An immunogenic personal neoantigen vaccine for patients with melanoma. Nature. 2017;547(7662):217‐221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212. Kong X, Lu P, Liu C, et al. A combination of PD1/PDL1 inhibitors: the prospect of overcoming the weakness of tumor immunotherapy (Review). Mol Med Rep. 2021;23(5):362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213. Liu R, Zhou C, Wang D, et al. Enhancement of DNA vaccine potency by sandwiching antigen‐coding gene between secondary lymphoid tissue chemokine (SLC) and IgG Fc fragment genes. Cancer Biol Ther. 2006;5(4):427‐434. [DOI] [PubMed] [Google Scholar]
- 214. Tondini E, Arakelian T, Oosterhuis K, et al. A poly‐neoantigen DNA vaccine synergizes with PD‐1 blockade to induce T cell‐mediated tumor control. Oncoimmunology. 2019;8(11):1652539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215. Xu G, Feng D, Yao Y, et al. Listeria‐based hepatocellular carcinoma vaccine facilitates anti‐PD‐1 therapy by regulating macrophage polarization. Oncogene. 2020;39(7):1429‐1444. [DOI] [PubMed] [Google Scholar]
- 216. Weber JS, Kudchadkar RR, Yu B, et al. Safety, efficacy, and biomarkers of nivolumab with vaccine in ipilimumab‐refractory or ‐naive melanoma. J Clin Oncol. 2013;31(34):4311‐4318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217. Gibney GT, Kudchadkar RR, DeConti RC, et al. Safety, correlative markers, and clinical results of adjuvant nivolumab in combination with vaccine in resected high‐risk metastatic melanoma. Clin Cancer Res. 2015;21(4):712‐720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218. Crosby EJ, Acharya CR, Haddad AF, et al. Stimulation of oncogene‐specific tumor‐infiltrating t cells through combined vaccine and alphaPD‐1 enable sustained antitumor responses against established HER2 breast cancer. Clin Cancer Res. 2020;26(17):4670‐4681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219. Xia GQ, Lei TR, Yu TB, Zhou PH. Nanocarrier‐based activation of necroptotic cell death potentiates cancer immunotherapy. Nanoscale. 2021;13(2):1220‐1230. [DOI] [PubMed] [Google Scholar]
- 220. Chawla SP, Van Tine BA, Pollack SM, et al. Phase II randomized study of CMB305 and atezolizumab compared with atezolizumab alone in soft‐tissue sarcomas expressing NY‐ESO‐1. J Clin Oncol. 2022;40(12):1291‐1300. [DOI] [PubMed] [Google Scholar]
- 221. Ai L, Xu A, Xu J. Roles of PD‐1/PD‐L1 pathway: signaling, cancer, and beyond. Adv Exp Med Biol. 2020;1248:33‐59. [DOI] [PubMed] [Google Scholar]
- 222. Xu W, Jones M, Liu B, et al. Efficacy and mechanism‐of‐action of a novel superagonist interleukin‐15: interleukin‐15 receptor alphaSu/Fc fusion complex in syngeneic murine models of multiple myeloma. Cancer Res. 2013;73(10):3075‐3086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223. Wong HC, Jeng EK, Rhode PR. The IL‐15‐based superagonist ALT‐803 promotes the antigen‐independent conversion of memory CD8(+) T cells into innate‐like effector cells with antitumor activity. Oncoimmunology. 2013;2(11):e26442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224. Guo Y, Luan L, Patil NK, Sherwood ER. Immunobiology of the IL‐15/IL‐15Ralpha complex as an antitumor and antiviral agent. Cytokine Growth Factor Rev. 2017;38:10‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225. Redman JM, Steinberg SM, Gulley JL. Quick efficacy seeking trial (QuEST1): a novel combination immunotherapy study designed for rapid clinical signal assessment metastatic castration‐resistant prostate cancer. J Immunother Cancer. 2018;6(1):91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226. Wrangle JM, Velcheti V, Patel MR, et al. ALT‐803, an IL‐15 superagonist, in combination with nivolumab in patients with metastatic non‐small cell lung cancer: a non‐randomised, open‐label, phase 1b trial. Lancet Oncol. 2018;19(5):694‐704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227. Zheng X, Wu Y, Bi J, et al. The use of supercytokines, immunocytokines, engager cytokines, and other synthetic cytokines in immunotherapy. Cell Mol Immunol. 2022;19(2):192‐209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228. Schliemann C, Palumbo A, Zuberbuhler K, et al. Complete eradication of human B‐cell lymphoma xenografts using rituximab in combination with the immunocytokine L19‐IL2. Blood. 2009;113(10):2275‐2283. [DOI] [PubMed] [Google Scholar]
- 229. Wagner K, Schulz P, Scholz A, Wiedenmann B, Menrad A. The targeted immunocytokine L19‐IL2 efficiently inhibits the growth of orthotopic pancreatic cancer. Clin Cancer Res. 2008;14(15):4951‐4960. [DOI] [PubMed] [Google Scholar]
- 230. Lanyu C, Kaiwen H. Research progress of TCM improving tumor immunosuppressive microenvironment based on programmed death 1/programmed death ligand 1 signaling pathway. Chinese J Inform Tradit Chinese Med. 2020;27(02):135‐137. [Google Scholar]
- 231. Weihan T, Zhao J, Qian W, Fengming Y, Ran Y, Chuan Z. A study on properties and actions of Chinese medicinals of PD‐1/PD‐L1 inhibitor. New Chinese Med. 2020;52(12):206‐208. [Google Scholar]
- 232. Hongzhi C, Weilin L, Zhan G, Huiqing Z. Etiology and pathogeny analysis and treatment exploration in traditional Chinese medicine of immune‐related adverse reactions of PD‐1/1 inhibitors. World Chinese Med. 2021;16(09):1386‐1390+1399. [Google Scholar]
- 233. Nanyan W, Cuihua J, Meng G, Jian Z, Zhiqi Y, Ke P. Paeoniflorin inhibits programmed cell death‐1‐ligand 1 expression in HepG2 cells by regulating JAK/STAT3 signal pathway. J China Pharm Univ. 2019;50(02):213‐221. [Google Scholar]
- 234. Liu Y, Liu X, Zhang N, et al. Berberine diminishes cancer cell PD‐L1 expression and facilitates antitumor immunity via inhibiting the deubiquitination activity of CSN5. Acta Pharm Sin B. 2020;10(12):2299‐2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235. Qing A, Li‐wei H, Hong‐yan W, et al. Mechanismof cordycepin promotes tumor immunity by regulating PD‐1 receptor of CD4 T lymphocytes+. J Nanjing Univ Tradit Chinese Med. 2018;34(05):495‐498. [Google Scholar]
- 236. Xu H, Van der Jeught K, Zhou Z, et al. Atractylenolide I enhances responsiveness to immune checkpoint blockade therapy by activating tumor antigen presentation. J Clin Invest. 2021;131(10):e146832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237. Yazhen Z, Xianlei L, Jinhua L, Shengyou L. Study on Guilu Erxianjiao in inhibiting tumor growth of H22 tumor‐bearing mice by regulating PD‐1 expression. China Modern Doctor. 2018;56(36):1‐5. [Google Scholar]
- 238. Lv J, Jia Y, Li J, et al. Gegen Qinlian decoction enhances the effect of PD‐1 blockade in colorectal cancer with microsatellite stability by remodelling the gut microbiota and the tumour microenvironment. Cell Death Dis. 2019;10(6):415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239. Vetizou M, Trinchieri G. Anti‐PD1 in the wonder‐gut‐land. Cell Res. 2018;28(3):263‐264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240. Andrews MC, Vasanthakumar A. Gut microbiota ‐ a double‐edged sword in cancer immunotherapy. Trends Cancer. 2023;9(1):3‐5. [DOI] [PubMed] [Google Scholar]
- 241. Yi M, Jiao D, Qin S, Chu Q, Li A, Wu K. Manipulating gut microbiota composition to enhance the therapeutic effect of cancer immunotherapy. Integr Cancer Ther. 2019;18:1534735419876351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 242. Montalban‐Arques A, Katkeviciute E, Busenhart P, et al. Commensal Clostridiales strains mediate effective anti‐cancer immune response against solid tumors. Cell Host Microbe. 2021;29(10):1573‐1588 e7. [DOI] [PubMed] [Google Scholar]
- 243. Sivan A, Corrales L, Hubert N, et al. Commensal Bifidobacterium promotes antitumor immunity and facilitates anti‐PD‐L1 efficacy. Science. 2015;350(6264):1084‐1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244. Xiao‐yu Z, Jie L. Discussion on traditional Chinese medicine promoting the transformation of ‘cold' tumor to ‘hot' based on yin‐yang theory. China J Tradit Chinese Med Pharmacy. 2022;37(08):4356‐4359. [Google Scholar]
- 245. Li X, Shao C, Shi Y, Han W. Lessons learned from the blockade of immune checkpoints in cancer immunotherapy. J Hematol Oncol. 2018;11(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246. Jiansheng L, Fuchun S. Explaination to apoptosis of tumor cells by the theory of Yin and Yang of Chinese medicine. Liaoning J Tradit Chinese Med. 2010;37(06):1034‐1035. [Google Scholar]
- 247. Shumin Y, Zhenye X, Haibin D, Xiaozhen Z. Mechanism and advantages of traditional Chinese medicine in remodeling tumor microenvironment. Acad J Shanghai Univ Tradit Chinese Med. 2019;33(05):1‐7. [Google Scholar]
- 248. Qing S, Qing J, Qi L. Research on the clinical and mechanism of traditional Chinese medicine regulating tumor immunity. China J Tradit Chinese Med Pharmacy. 2018;33(10):4542‐4545. [Google Scholar]
- 249. Chen Q, Sun T, Jiang C. Recent advancements in nanomedicine for ‘cold’ tumor immunotherapy. Nanomicro Lett. 2021;13(1):92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250. Liu YT, Sun ZJ. Turning cold tumors into hot tumors by improving T‐cell infiltration. Theranostics. 2021;11(11):5365‐5386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251. Giustarini G, Pavesi A, Adriani G. Nanoparticle‐based therapies for turning cold tumors hot: how to treat an immunosuppressive tumor microenvironment. Front Bioeng Biotechnol. 2021;9:689245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252. Jeon MJ, Lee H, Lee J, et al. Development of potent immune modulators targeting stimulator of interferon genes receptor. J Med Chem. 2022;65(7):5407‐5432. [DOI] [PubMed] [Google Scholar]
- 253. Xiong W, Gao X, Zhang T, et al. USP8 inhibition reshapes an inflamed tumor microenvironment that potentiates the immunotherapy. Nat Commun. 2022;13(1):1700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254. Sun R, Limkin EJ, Vakalopoulou M, et al. A radiomics approach to assess tumour‐infiltrating CD8 cells and response to anti‐PD‐1 or anti‐PD‐L1 immunotherapy: an imaging biomarker, retrospective multicohort study. Lancet Oncol. 2018;19(9):1180‐1191. [DOI] [PubMed] [Google Scholar]
- 255. Lu S, Stein JE, Rimm DL, et al. Comparison of biomarker modalities for predicting response to PD‐1/PD‐L1 checkpoint blockade: a systematic review and meta‐analysis. JAMA Oncol. 2019;5(8):1195‐1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256. Fu Y, Jung AW, Torne RV, et al. Pan‐cancer computational histopathology reveals mutations, tumor composition and prognosis. Nat Cancer. 2020;1(8):800‐810. [DOI] [PubMed] [Google Scholar]
- 257. Wu TD, Madireddi S, de Almeida PE, et al. Peripheral T cell expansion predicts tumour infiltration and clinical response. Nature. 2020;579(7798):274‐278. [DOI] [PubMed] [Google Scholar]
- 258. Pelly VS, Moeini A, Roelofsen LM, et al. Anti‐inflammatory drugs remodel the tumor immune environment to enhance immune checkpoint blockade efficacy. Cancer Discov. 2021;11(10):2602‐2619. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


