Abstract
Hand hygiene is a crucial measure in the prevention and control of infections, and there is a growing awareness among individuals who are making a conscious effort to maintain hand cleanliness. With the advent of the SARS-CoV-2 outbreak, the demand for hand hygiene products has also gradually shifted towards those with antimicrobial properties. Among these products, hand sanitizer gels (HSGs) have gained considerable popularity as an efficient method of hand cleaning, due to their rapid drying and sustained antimicrobial efficacy. Concurrently, there has been a growing interest in novel HSGs that offer additional functions such as skin whitening, moisturizing, and anti-inflammatory effects. These novel HSGs effectively address concerns associated with the ingestion of antimicrobial ingredients and demonstrate reduced skin irritation, thereby alleviating hand dermatological issues. This review provides an extensive overview of the application scenarios, classification, and challenges associated with HSGs while emphasizing the emergence of novel components with biological functions, aiming to contribute to the advancement of hand hygiene practices and offer novel insights for the development of novel HSGs with outstanding antimicrobial properties with other multiple biological functions and desirable biosafety profiles.
Keywords: hand sanitizer gels, antimicrobial properties, biological functions, hand hygiene
1. Introduction
Hand hygiene plays a crucial role in preventing infections and controlling the spread of diseases, as hands serve as a major medium for the transmission of pathogenic microorganisms [1,2]. Notably, over half of respiratory viruses and enterovirus infections, along with bacterial infections, are transmitted through hand-to-mouth contact among people living in close contact [3,4,5]. Therefore, hand hygiene is crucial in preventing infections and controlling the spread of epidemics, which can ultimately safeguard human life and health [6,7]. In response to the global COVID-19 pandemic, the demand for hand cleaning products with antimicrobial properties has surged [8,9]. Instant hand sanitizers (IHSs) have gained significant popularity due to their effectiveness in reducing hand pathogens, along with their convenience, accessibility, and wide consumer acceptance [10,11]. Compared to traditional soaps and wipes, IHSs are considered more convenient and efficient in reducing bacterial counts [12]. Consequently, using IHSs as an alternative to disposable wipes before meals is considered more convenient and efficient [13]. As the importance of hand hygiene continues to be emphasized, promoting the use of IHSs as an integral part of everyday routines can significantly contribute to reducing the transmission of infectious diseases and improving overall public health.
IHSs typically contain active functional ingredients, as well as inactive carrier ingredients, such as excipients, humectants, fragrances, and colorants [14,15]. They are available in various forms, including gels, liquids, sprays, and foams [16]. Each formulation has its own characteristics and considerations: (I) The low viscosity of the liquid form makes it more challenging to use effectively [17]; (II) The spray formulation of IHSs offers broader coverage, allowing for convenient application to larger surfaces. However, it requires a valve mechanism and poses a safety risk due to the flammability of ethanol. Extra precautions must be taken to avoid accidents and ensure proper storage [18]; (III) The high humidity of the foam formulation can reduce its antimicrobial properties and prolong the drying time, leading to discomfort [19]. In comparison, hand sanitizer gels (HSGs) are a popular choice due to their rapid drying time and continuous antimicrobial efficacy [20]. Additionally, HSGs form a protective layer at the application site, providing a longer period of protection on the skin. It is essential to rub HSGs thoroughly to ensure complete coverage of the hand skin (see Table 1) [21,22]. It is important to consider factors such as ease of use, safety, antimicrobial efficacy, and user comfort when selecting the most suitable IHSs for personal hygiene practices. This review will take HSGs as the main character to introduce their research progress in the field of hand hygiene.
Table 1.
Different formulations of IHS and feature comparison.
| The Formulations of IHS | Inactive Ingredients | Characteristics | Ref. |
|---|---|---|---|
| Liquid formulations | Humectant, fragrance, colorant. | Widely available, but with low viscosity and hard to dispense. | [17] |
| Spray formulations | Valve actuation, humectant, fragrance, colorant. | Higher flammability risk at room temperature. | [18] |
| Foam formulations | Foaming agent, humectant, fragrance, colorant. | Longer drying time, difficult to eliminate the feeling of dissimilarity and more expensive than gel. | [19,23] |
| Gel formulations | Emollients, thickeners, neutralizers, chelators, fragrances, and dyes or colorants. | With better antimicrobial action and fast drying time, formation of a protective layer on the application site. |
[20,22] |
Since the onset of the pandemic, many countries have emphasized the implementation of non-pharmaceutical preventive measures, prominently including the intensive use of HSGs [24]. Additionally, the critical role of hand sanitizers in reducing the transmission of infectious diseases such as COVID-19 has led to a surge in global demand for HSGs since 2020, resulting in a remarkable 600-fold increase in market production [25,26]. Consequently, there has been a significant decrease in the incidence of infectious diseases in recent times [27]. This surge in market sales of HSGs has spurred the refinement of their applications, resulting in the development of a wide range of novel products with specific biological functions. These products have been designed to meet the varying needs of different consumer groups.
Herein, we focus on the research progress of HSGs in hand hygiene, highlighting the application scenarios, challenges, and possible solutions, as well as the outlook for the future application of biological functions. By making informed decisions, individuals can enhance their hand hygiene routine and contribute to the prevention of infections and the control of disease transmission.
2. Application Scenarios for HSGs
Hand hygiene products that are widely accepted for use should have good sensory characteristics, which include a pH value similar to that of the skin, as well as appropriate viscosity and spreadability [22], as depicted in Figure 1a. Additionally, it is important not to develop an allergic reaction to the skin. The majority of hand hygiene products contain high levels of alcohol, which can cause skin irritation and dryness, as well as harm the environment [28]. Therefore, it is essential to find hand hygiene products that are safe and environmentally friendly. Products with poor sensory characteristics can reduce the frequency with which it is necessary to wash your hands [29]. The components of HSGs are biocompatible with each other at an excellent level, and the most abundant component is the thickening agent, mainly using carbomer, which is extensively used for skin and eye wound healing [30,31]. Simultaneously, carbomer has high viscosity at low concentrations and has the advantages of a wide viscosity range, great flowability, compatibility with many active ingredients, high transparency, good thermal stability, and high consumer acceptance [32,33].
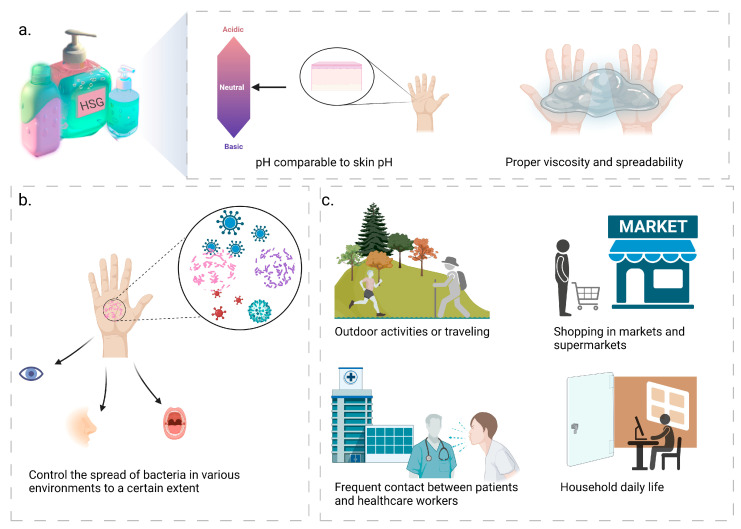
Figure 1.
Hand sanitizer gels (HSGs) possess favorable sensory characteristics, exert a certain degree of control over bacterial transmission, and can be applied in various scenarios. (a) Hand hygiene products with good sensory properties, including pH similar to skin, as well as appropriate viscosity and spreadability; (b) HSGs can control the spread of bacteria in various environments to a certain extent and significantly reduce the transfer of microorganisms, thus effectively reducing respiratory and gastrointestinal infections; (c) The versatility of HSGs extends to multiple scenarios, embracing outdoor activities, supermarket shopping, health centers, domestic routines and other scenarios.
HSGs can be utilized in a wide variety of situations, owing to its effectiveness in minimizing respiratory and gastrointestinal infections based on its ability to control to a certain extent the spread of bacteria in a range of environments and to significantly reduce the transfer of microorganisms [34,35,36], as illustrated in Figure 1b,c. (I) When engaging in outdoor activities or traveling, the compact size of the HSGs allows for convenient and hygienic hand cleaning without the necessity of additional water sources and towels, thus avoiding infections and contagious diseases caused by the presence of pollutants and bacteria [37], making HSGs suitable for travel, camping, and other activities [10]; (II) during shopping in markets and supermarkets, customers frequently touch surfaces such as cart handles and shelves, resulting in bacterial contamination and transmission through hand-to-mouth and other hand-to-face touching behaviors [37,38]. In pursuit of creating a safe, healthy, and hygienic environment, HSGs offer a convenient alternative to hand soaps and other cleaning methods. They effectively eliminate hand bacteria, ensuring personal cleanliness [39]; (III) frequent contact between patients and healthcare workers can lead to the spread of bacteria in health centers such as hospitals, clinics, and pharmacies, where HSGs are more effective, act faster and can be made available at the point of patient care [40]. Studies have also shown that HSGs are generally better tolerated by the skin than soap and water [41]; (IV) family members use mobile phones, keyboards and other electronic devices daily. It is possible to spread bacteria to the hands by touching these devices [42]. In addition to furniture, doorknobs, and other common items, family members can also spread bacteria from one item to another. Therefore, using HSGs is a quick, efficient, and convenient way to help maintain good hand hygiene and prevent the spread of bacteria [34,43].
3. Classification of HSGs
HSGs can be classified into two categories based on their active ingredients: Alcohol-based HSGs (ABHSGs) and Non-alcohol-based HSGs (NABHSGs). Both types are effective in inhibiting microorganisms on the hands and no significant difference in efficacy has been observed between them [44]. Nevertheless, the mechanisms of action for these two HSGs types differ [14].
3.1. ABHSGs
ABHSGs exert rapid antimicrobial effects by denaturing and deactivating microorganisms on the hands through their interaction with membrane proteins, thus acting as effective antimicrobial agents [1]. However, the alcohol-based components present in ABHSGs can often adversely affect the lipid structure of epidermal keratinocytes, resulting in side effects such as hand dryness and cracking [45].
Typically, commercially available ABHSGs contain primary ingredients such as ethanol (ranging from 60% to 95% concentration), isopropanol, or a combination of both [29,46]. Additional ingredients like hydrogen peroxide, water, and notably, glycerol as emollients, can be incorporated into the product to reduce irritation and minimize the occurrence of contact dermatitis [47]. ABHSGs have been demonstrated to eliminate most microorganisms present on the hands, and the alcohol group within the product acts as a potent antimicrobial agent against a broad spectrum of bacteria, viruses, and fungi, including methicillin-resistant Staphylococcus aureus, E. coli, H1N1, and the Ebola virus [48,49,50]. The World Health Organization has confirmed that corresponding concentrations of these alcohols effectively inactivate SARS-CoV-2 [51]. Ethanol is particularly effective against non-enveloped viruses, making it the primary active ingredient in most HSG products [52,53]. The antimicrobial activity of ABHSGs largely depends on the percentage concentration of alcohol-based substances [54]; if the content falls below 60% v/v, product quality may be compromised [16]. In response to the COVID-19 pandemic, the FDA has recommended increasing the concentration of isopropanol to 91% v/v and ensuring that the ethanol concentration does not exceed 94.9% v/v [46].
ABHSGs typically achieve their full antimicrobial activity within 15 s [55]. In accordance with EN1500 guidelines, approximately 3 mL of ABHSGs should be applied to the hands for approximately 30 s to ensure their effectiveness against microorganisms [29,56]. Nonetheless, factors such as the amount of ABHSGs applied, the duration of application, and hand size can influence the reduction of microbial load, the extent of hand surface coverage, and the drying time [57,58]. A significant correlation has been observed between hand area and the number of detected CFUs [59]. Larger hand surfaces necessitate a greater amount of ABHSGs to guarantee complete coverage, which, in turn, prolongs the required duration of hand friction. This could decrease the acceptability, practicality, and ultimately, the sterilization efficacy of ABHSGs [60].
3.2. NABHSGs
The efficacy of NABHSGs in reducing the incidence and transmission of bacterial infections has been demonstrated [61]. The antimicrobial function of NABHSGs is primarily mediated through the presence of cationic surfactants, such as quaternary ammonium compounds (QACs) [62]. These compounds exhibit a broad spectrum of antimicrobial properties due to their hydrophilic and hydrophobic components, specifically the positively charged ammonium cations in their hydrophilic part [37,63]. The presence of both hydrophilic and hydrophobic components enhances their surface activity and the ability to form liposomes, thereby increasing their antibacterial capacity [64,65]. Furthermore, ingredients such as aloe vera, glycerol, and vitamin E can be incorporated into NABHSGs to reduce skin irritation and enhance their moisturizing effects [22].
Benzalkonium chloride (BAK), a representative of QACs, exhibits excellent sterilization performance within 30 s and has been widely employed in medical institutions and cleaning supplies as a non-alcohol-based functional antimicrobial agent for NABHSGs [66,67]. Compared to alcohol, QACs offer several advantages for hand disinfection: (1) they are non-toxic, less irritating to the skin, and non-flammable [68]; (2) the combination of ABHSGs and NABHSGs (primarily referring to benzalkonium chloride) generates a synergistic effect that enhances the antimicrobial range and efficacy of the alcohol group while also providing an immediate and long-lasting antimicrobial effect [69]. Therefore, the identification of various QACs components with antimicrobial activity and good biocompatibility could potentially address future challenges associated with alcohol demand and side effects.
4. Application Challenges of HSGs
4.1. Antimicrobial Functional Ingredients
Since the onset of the COVID-19 pandemic, there has been a significant surge in sales of ABHSGs [70]. To meet the challenge of increased demand and raw material shortages, many countries have permitted manufacturers and medical institutions to develop and produce hand sanitizers independently. Unfortunately, this has led to a situation where some manufacturers fail to adhere to proper quality control measures or use denatured alcohol, resulting in a notable increase in substandard hand sanitizer products in the market [47,71,72,73]. Furthermore, the fermentation and distillation processes employed by manufacturers, along with the impact of production equipment and the environment, may introduce impurities such as benzene and acetaldehyde into hand sanitizers, exacerbating public health concerns [74,75]. Consequently, it is recommended that users critically evaluate the antimicrobial functional ingredients in hand sanitizer formulas and carefully review product labels to avoid potential allergens based on their personal sensitivities before use [76], as shown in Figure 2.
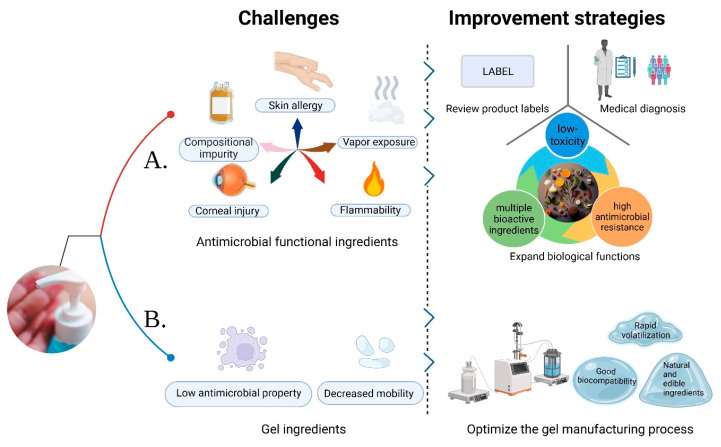
Figure 2.
Application challenges and the corresponding improvement strategies of hand sanitizer gels (HSGs). (A) The challenges of antimicrobial functional ingredients at present and the corresponding improvement measures are put forward; (B) The current challenges associated with gel ingredients are identified, along with proposed measures for their improvement.
Common antimicrobial components found in regular hand sanitizer products (such as ABHSGs) can cause corneal epithelial cell destruction at high concentrations, leading to eye diseases. Prolonged contact with hands may also increase the risk of local adverse reactions, such as contact dermatitis and atopic dermatitis [77]. In recent years, clinical cases involving adverse effects from ABHSGs have been on the rise, particularly among children [78,79]. Children tend to use hand sanitizers more frequently than adults [80], and face an increased risk of ingestion and exposure problems after using informal ABHSGs, underscoring the importance of adult supervision during use [78,81]. Additionally, healthcare workers who apply ABHSGs before handling newborns may heighten the risk of neonatal exposure to ethanol vapor, potentially causing neuronal damage and leading to neurodevelopmental delay and behavioral issues. However, the impact of such low-dose ethanol exposure on neonatal brain development is currently unclear [82,83]. Furthermore, isopropanol ingestion can result in common health problems. Accidental inhalation or dermal exposure may cause poisoning, although it usually does not lead to serious health hazards [84]. Repeated exposure of microbes to disinfectants, antibiotics, and other genotoxic chemicals leads to the development of resistance, becoming a significant global concern, particularly burdening healthcare professionals [85]. Triclosan serves as a prime example, having been used as an antimicrobial component in NABHSGs over the past decades, but evidence indicates its potential for environmental impact and antibiotic resistance [86]. Therefore, excessive and prolonged use of HSGs also entails potential risks. Furthermore, the impact of ethanol, isopropanol, and other ingredients on the environment has long been a topic of concern [87]. These compounds can volatilize or seep into soil and groundwater, significantly affecting aquatic organisms [88]. Thus, while addressing potential issues associated with the long-term use of HSGs, it is crucial to emphasize effective management of good hygiene practices.
To maintain hand hygiene, particularly among children and healthcare workers, frequent hand washing is crucial. Therefore, it is important to select an emollient that effectively strengthens the skin barrier. Research indicates that BAK, an antiseptic ingredient, provides immediate and long-term antimicrobial effects, and the addition of emollients typically does not diminish its effectiveness [89]. Furthermore, BAK tends to be less irritating to the skin and rarely causes allergic reactions [63]. In cases where adverse reactions, such as hand rashes, arise from using ABHSGs, it is recommended to either switch to hand sanitizers containing BAK or seek medical treatment [90]. It is important to note that ethanol and isopropanol, commonly found in ABHSGs, are volatile and combustible substances that could cause fires when used near flames or exposed to high temperatures [16,18,91]. As such, the inclusion of novel safe antimicrobial ingredients can offer a safer alternative with an improved safety profile.
4.2. Gel Ingredients
The stability of the gel is related to the pH of the compound, with a lower pH resulting in decreased mobility. Considering that ethanol and isopropanol have different polarities, and isopropanol exhibits a significantly lower polarity compared to ethanol, a greater amount of triethanolamine must be incorporated into isopropanol to produce a stable polymer with carbomer [92]. Studies have demonstrated that anionic thickeners (such as carbomer or acrylate) notably impair the antimicrobial persistence of ABHSGs on the skin. As an alternative, non-ionic polymer thickeners like hydroxypropyl cellulose may be considered to replace carbomer and improve antimicrobial persistence [93]. In addition, by optimizing the manufacturing process of the gel, it is possible to explore materials with good biocompatibility, fast volatilization, and even completely natural edible ingredients in HSGs, which not only contribute to the stability of the gel, but also provide enhanced biocompatibility, leading to faster volatilization. This exploration opens up the possibility of reducing reliance on synthetic ingredients and instead adopting entirely natural and edible ingredients. The trend towards using natural and edible ingredients in hand hygiene products is in line with consumers’ growing preference for environmentally friendly and safe options.
5. Novel Antimicrobial Ingredients of HSGs
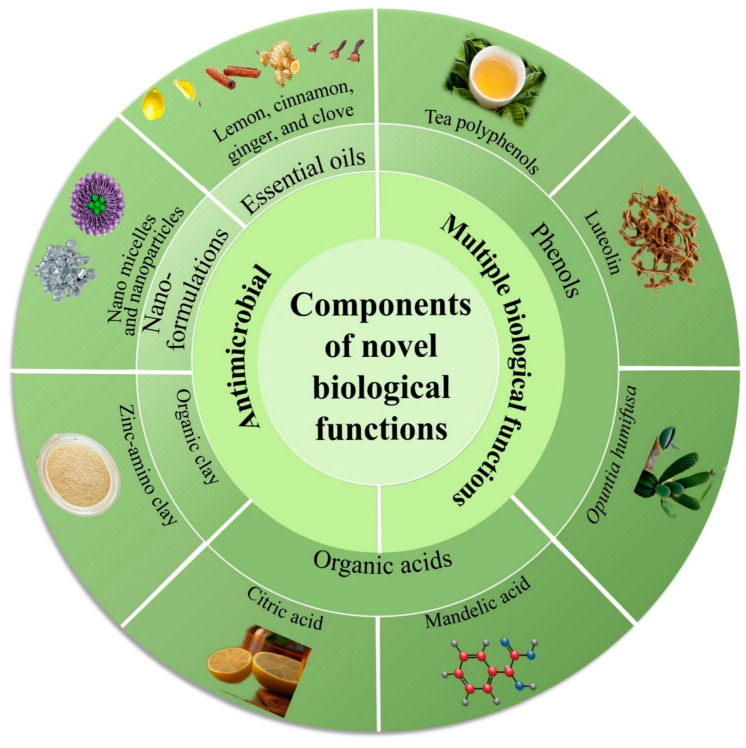
Due to various biocompatibility issues associated with antimicrobial components in traditional HSGs, there has been a notable shift towards the use of novel HSGs [88,90], as illustrated in Figure 3. Novel HSGs are embracing the use of natural and safe antimicrobial substances, such as essential oils, phenols, organic acids, and others, aiming to reduce or even completely replace traditional ingredients like ethanol or isopropanol. Additionally, NABHSGs represented by cationic surfactants have gained attention as an alternative [94]. The research community and consumers have also exhibited a growing interest in antimicrobial agents such as organic clay and nanoformulations. These agents not only provide antimicrobial effects but also offer certain anti-inflammatory and whitening properties, as shown in Figure 4. This dual functionality has contributed to their increasing popularity among researchers and consumers alike [95,96].
Figure 3.
Novel components of hand sanitizer gels (HSGs) possess antimicrobial properties and exhibit multiple biological functions.
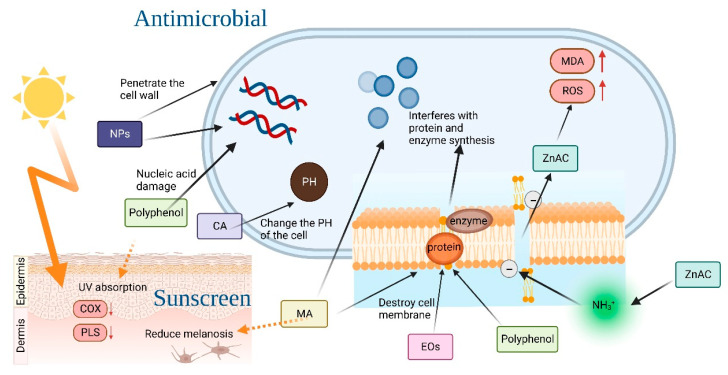
Figure 4.
The antimicrobial mechanisms of essential oils, phenols, and organic acids, as well as the skin whitening and anti-inflammatory mechanisms of phenols and Mandelic acid (MA).
5.1. Essential Oils
Natural substances with antimicrobial activity have been extensively investigated and studied [97]. Among these, natural plant essential oils (EOs) have been found to affect the synthesis of bacterial lipid membranes, including certain proteins and enzymes on the membrane surface, due to their lipid-soluble nature. This makes the bacterial membranes more permeable and reduces the protein content of the bacterium, while increasing the hydrophobicity of the bacterial cell surface, affecting various cellular processes that ultimately lead to cell death [22]. Furthermore, EOs have a stronger impact on the cell wall of gram-positive bacteria than on the cell membrane [98]. By combining representative EOs, namely lemon, cinnamon, ginger, and clove, the novel NABHSGs can be developed with superior antimicrobial properties compared to 60% ethanol, as demonstrated by the synergistic action of the main components limonene, cinnamaldehyde, turmeric, and eugenol [99,100,101]. Additionally, M. Ismail et al. prepared a novel HSG with pepper essential oil, clove essential oil, and a small amount of ethanol. This novel HSG reduces the exposure risk of isopropanol and alcohol on the skin and exhibits good drug diffusion and antibacterial properties [102].
The utilization of natural substances, particularly essential oils, in the development of novel HSGs presents a promising approach to enhance their antimicrobial efficacy while minimizing potential risks associated with traditional antimicrobial components. By leveraging the synergistic effects and unique properties of these natural substances, researchers are able to explore novel avenues for the formulation of safer and more effective HSGs.
5.2. Phenols
Tea polyphenols have multiple biomedical functions, with active components like epigallocatechin gallate (EGCG) and epigallocatechin-3-gallate-palmitate (EC16) directly damaging the cell membrane, altering cell structure, and affecting the proteins and DNA of microorganisms to exhibit antimicrobial effects. In particular, EC16, the main component of tea polyphenol palmitate, has emerged as a novel safe and non-toxic HSG component [103,104]. Research by M. Xi et al. has found luteolin (LUT) to be a highly promising antimicrobial functional component of hand sanitizers. LUT increases cell membrane permeability to inhibit bacterial growth, causing significant and irreversible damage to bacterial structure and leading to K+ extravasation. Additionally, LUT has strong antioxidant and free radical scavenging abilities, protecting cells from damage. As a novel HSG component, LUT not only exhibits antimicrobial effects, but also absorbs both ultraviolet A (UVA) and ultraviolet B (UVB) radiation, reducing their adverse effects on the skin. LUT can effectively mitigate the generation of reactive oxygen species (ROS) in the skin induced by ultraviolet (UV) radiation through mechanisms such as stabilizing free radicals, inhibiting pro-oxidant enzymes, and inducing antioxidant enzymes. Furthermore, LUT demonstrates effective inhibition of pro-inflammatory signaling pathways induced by UV radiation by targeting pro-inflammatory cytokines like IL-6, or COX-2, or NF-κB-dependent pathways [105,106].
Opuntia humifusa extract (OHE) is high in total polyphenols and flavonoids, giving it antioxidant and antimicrobial activity, as well as high moisture retention capabilities [107]. OHE stimulates the expression of epidermal hyaluronic acid synthases (HAS) and regulates the synthesis of hyaluronic acid (HA), thereby reducing the expression of the hyaluronidase transcript and contributing to skin hydration [25]. Additionally, OHE has whitening and anti-wrinkle effects. A study by Park et al. [108] demonstrated that OHE could regulate the ability of the skin to produce HA induced by UVB. OHE also inhibited the compensatory increase of HA, hyaluronic acid-binding protein (HABP), and CD44 protein expression under UV irradiation, all while reducing HAS percutaneous water loss and erythema. This suggests that OHE may protect the skin from the harmful effects of UVB radiation.
5.3. Organic Acids
Organic acids (OAs) act as broad-spectrum antimicrobial substances, inhibiting the growth of microorganisms through various mechanisms, and show synergistic antimicrobial effects with alcohol. Citric acid (CA), for instance, can alter the pH value of cells, thereby interfering with the normal metabolism of bacteria and exerting antimicrobial effects [109,110]. Using organic acids, alone, as antimicrobial ingredients in hand sanitizers is also significant. Mandelic acid (MA) has been identified as an antimicrobial component of NABHSGs, playing an antimicrobial role by affecting the bacterial cell membrane and inhibiting bacterial protein synthesis. Results of experiments by Pavlína Egner et al. suggest that MA has stronger antimicrobial properties and better stability than alcohol groups [111]. In addition to its antimicrobial properties, MA can also be employed as an active ingredient to reduce pigmentation and prevent skin erythema, sunburn, and skin cancer caused by ultraviolet rays. Lower concentrations of MA promote the regeneration of cells in different layers of the skin, reducing damage to the skin barrier and dehydration of the stratum corneum, thereby leading to maintenance of optimal pH values and a revamp of photoaging [112].
By harnessing the potential of these organic acids, researchers can develop novel HSGs that provide improved antimicrobial activity while promoting skin health and overall well-being.
5.4. Organic Clay
Zinc-amino clay (ZnAC) is a type of organic clay characterized by its strong antimicrobial properties and minimal toxic side effects. In an aqueous solution, ZnAC-HSG can interact with negatively charged bacterial lipid membranes through electrostatic interactions involving the quaternary ammonium (-NH3+) groups of organically modified clay. This interaction disrupts the permeability of the phospholipid bilayer and cell membrane, leading to an increased uptake of ZnAC by bacterial cells. Subsequently, intracellular ROS concentration rises, malondialdehyde (MDA) production is significantly increased, and ultimately, cell death occurs due to bacterial membrane disruption [25].
Moreover, the presence of organic clay in the sunscreen enhances the viscosity of its oil phase, resulting in the formation of a uniformly distributed film that improves the sunscreen’s ability to absorb ultraviolet rays. Consequently, sunscreen products containing HSGs with organic clay components exhibit enhanced sun protection and whitening effects [113].
5.5. Nanoformulations
Nanoformulations have emerged as a promising approach for enhancing the stability and biocompatibility of antimicrobial agents, leading to their increasing adoption in novel NABHSGs. For instance: (Ⅰ) Rhamnolipid nano-micelles exhibit antimicrobial activity comparable to NABHSGs, while maintaining non-cytotoxic properties. The inclusion of (biological) surfactants enhances the hydrophobicity of degrading microorganisms, thereby rendering the hydrophobic matrix more accessible to cells [114]. In comparison to ABHSGs, Rhamnolipid nano-micelles are safer and exhibit minimal impact on the skin [115,116]. Not only do Rhamnolipid nano-micelles possess antimicrobial properties, but they also hold potential as a therapeutic agent for COVID-19 treatment in future research [117]; (Ⅱ) nanoparticles, measuring between 1 and 1000 nm in size, have been reported to exhibit antimicrobial activity against both viruses and bacteria [118]. Silver nanoparticles, in particular, are excellent materials in the biomedical field [119,120]. Synthesized from plant extracts, silver nanoparticles are not only safe in composition but also demonstrate potent antimicrobial effects [121]. Their high surface area-to-volume ratio enables them to penetrate bacterial cell walls, alter membrane structures, and even eliminate target cells. Silver nanoparticles exert their effects through the release of silver ions, increased cell membrane permeability, generation of reactive oxygen species, and interference with DNA replication [120]. For instance, moss and eucalyptus leaf extracts have been employed in the preparation of silver nanoparticles [122]. The eucalyptus leaf extract exhibited an inhibitory effect on bacterial biofilm formation and demonstrated more favorable antimicrobial effects [123,124]. Furthermore, chitosan serves as a coating on the surface of silver nanoparticles, acting as a stabilizer to prevent agglomeration and enhance the effectiveness of nanoparticles as antimicrobial agents. This property results in natural plant silver nanoparticles exhibiting superior stability and more potent antimicrobial effects [121]. The primary antimicrobial mechanism of zinc oxide nanoparticles (ZnO-NPs) involves the generation of ROS, which can target multiple sites, such as proteins, nucleic acids, lipids, and enzymes [125]. Compared to traditional ABHSGs, ZnO-NPs demonstrate enhanced antimicrobial activity and greater safety, along with high biocompatibility [118].
Although the systemic toxicity of nanoformulations as nanoscale materials has not been reported, some studies have shown that nanoformulations can easily interfere with biomolecules, cells, and organs [126]. Researchers are also concerned about the ability of nanoformulations to cross the blood–brain barrier via trans-synaptic transport, and accumulate in the brain [127]. Another issue with nanoformulations is that they pose a potential hazard to marine life if released into the environment, so future safety assessments for nanoformulations must be carried out to ensure they are safe for humans and the environment [128].
The utilization of nanoformulations in NABHSGs offers a promising avenue for developing hand hygiene products with improved antimicrobial efficacy, stability, and safety profiles. These advancements align with the growing demand for effective and safe hand hygiene solutions. Further research in this area can explore the optimization of nanoformulations, integration with natural active substances, and their potential applications in preventing the spread of infections and controlling disease transmission.
6. Future Research on HSGs
In the future, research in the field of novel HSGs should align with the increasing demands for safety and functionality among consumers [129]. The focus of such research may revolve around two main areas: Firstly, there is a need to screen natural components that possess low toxicity and demonstrate high antimicrobial performance. These components can be utilized as novel ingredients in HSGs [130]. Additionally, exploring the combination of multiple bioactive ingredients may further enhance the biological activities of HSGs. This approach allows for the development of multifunctional HSGs that not only sanitize hands effectively but also offer supplementary benefits [131]; secondly, optimizing the manufacturing processes of HSGs is crucial. This involves investigating gel materials that exhibit good biocompatibility, ensuring they are suitable for frequent use on the skin [132]. Rapid volatilization of the gel upon application can enhance the user experience and convenience. Moreover, exploring purely natural and edible components as gel materials holds the potential to increase the safety and acceptability of HSGs, addressing consumers’ growing concerns about environmental and health impacts [133].
By addressing these research directions, we can continuously improve and innovate the performance of HSGs, thereby enhancing their practicality among consumers. Novel HSGs will be better equipped to meet the public’s demand for safe, efficient, and eco-friendly hand cleaning solutions, contributing significantly to disease prevention and personal health maintenance [6]. These efforts will drive further advancements in the field of hand hygiene and provide us with more innovative and effective hand cleaning solutions.
7. Conclusions
Hand hygiene plays a key role in preventing and controlling infections, especially with the SARS-CoV-2 outbreak, which has seen a surge in demand for hand hygiene products. In this review, we provide a comprehensive overview of the various application scenarios, classifications, and challenges associated with HSGs. In addition, we highlight the emergence of novel ingredients with biological functions, which offer promising opportunities for advances in hand hygiene practice. By exploring multiple biological functions and ensuring ideal biosafety, future research could lead to the development of novel HSGs with excellent antimicrobial properties. Nevertheless, it is essential that we account for the potential risks of HSGs, such as the development of antimicrobial resistance and the impact of HSGs on the environment, while balancing their potential benefits. Better management and responsible hygiene practices should be promoted to ensure sustainable and effective hand hygiene solutions. In conclusion, this review provides valuable insights into hand hygiene and encourages further research and development of HSGs. As we continue to explore new possibilities and innovations in our human health goals, we remain committed to creating a safer, healthier, and more hygienic environment for all.
Abbreviations
| IHSs | Instant hand sanitizers |
| HSGs | Hand sanitizer gels |
| ABHSGs | Alcohol-based hand sanitizer gels |
| NABHSGs | Non-alcohol-based hand sanitizer gels |
| QACs | Quaternary ammonium compounds |
| BZK | Benzalkonium chloride |
| EOs | Essential oils |
| EGCG | Epigallocatechin gallate |
| EC16 | Epigallocatechin-3-gallate-palmitate |
| LUT | Luteolin |
| UVA | Ultraviolet A |
| UVB | Ultraviolet B |
| UV | Ultraviolet |
| ROS | Reactive oxygen species |
| OHE | Opuntia humifusa extract |
| HAS | Hyaluronic acid synthases |
| HA | Hyaluronic acid |
| HABP | Hyaluronic acid-binding protein |
| OAs | Organic acids |
| CA | Citric acid |
| MA | Mandelic acid |
| ZnAC | Zinc-amino clay |
| MDA | Malondialdehyde |
| ZnO-NPs | Zinc oxide nanoparticles |
Author Contributions
Conceptualization, D.S., L.L. and Q.Y.; validation, M.C., W.W. and T.L.; formal analysis, D.S. and L.J.; writing—original draft preparation, Y.M. and J.Y.; writing—review and editing, Y.M., J.M. and H.Y.; funding acquisition, J.M. All authors have read and agreed to the published version of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Funding Statement
This work was Supported by the Graduate Scientific Research Foundation of Wenzhou University (3162023003048, 3162023003049, 3162023003051 and 3162023004076).
Footnotes
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
References
- 1.Del Campo R., Martínez-García L., Sánchez-Díaz A.M., Baquero F. Biology of Hand-to-Hand Bacterial Transmission. Microbiol. Spectr. 2019;7:1. doi: 10.1128/microbiolspec.MTBP-0011-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Edmonds-Wilson S.L., Nurinova N.I., Zapka C.A., Fierer N., Wilson M. Review of Human Hand Microbiome Research. J. Dermatol. Sci. 2015;80:3–12. doi: 10.1016/j.jdermsci.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Baquero F., Saralegui C., Marcos-Mencía D., Ballestero L., Vañó-Galván S., Moreno-Arrones Ó.M., Del Campo R. Epidermis as a Platform for Bacterial Transmission. Front. Immunol. 2021;12:774018. doi: 10.3389/fimmu.2021.774018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weber T.P., Stilianakis N.I. Fomites, Hands, and the Transmission of Respiratory Viruses. J. Occup. Environ. Hyg. 2021;18:1–3. doi: 10.1080/15459624.2020.1845343. [DOI] [PubMed] [Google Scholar]
- 5.Lukashev A.N., Vakulenko Y.A., Turbabina N.A., Deviatkin A.A., Drexler J.F. Molecular Epidemiology and Phylogenetics of Human Enteroviruses: Is There a Forest behind the Trees? Rev. Med. Virol. 2018;28:e2002. doi: 10.1002/rmv.2002. [DOI] [PubMed] [Google Scholar]
- 6.Stadler R.N., Tschudin-Sutter S. What Is New with Hand Hygiene? Curr. Opin. Infect. Dis. 2020;33:327–332. doi: 10.1097/QCO.0000000000000654. [DOI] [PubMed] [Google Scholar]
- 7.Howard G., Bartram J., Brocklehurst C., Colford J.M., Costa F., Cunliffe D., Dreibelbis R., Eisenberg J.N.S., Evans B., Girones R., et al. COVID-19: Urgent Actions, Critical Reflections and Future Relevance of ‘WaSH’: Lessons for the Current and Future Pandemics. J. Water Health. 2020;18:613–630. doi: 10.2166/wh.2020.162. [DOI] [PubMed] [Google Scholar]
- 8.Foddai A.C.G., Grant I.R., Dean M. Efficacy of Instant Hand Sanitizers against Foodborne Pathogens Compared with Hand Washing with Soap and Water in Food Preparation Settings: A Systematic Review. J. Food Prot. 2016;79:1040–1054. doi: 10.4315/0362-028X.JFP-15-492. [DOI] [PubMed] [Google Scholar]
- 9.Guidry J.P.D., O’Donnell N.H., Austin L.L., Coman I.A., Adams J., Perrin P.B. Stay Socially Distant and Wash Your Hands: Using the Health Belief Model to Determine Intent for COVID-19 Preventive Behaviors at the Beginning of the Pandemic. Health Educ. Behav. 2021;48:424–433. doi: 10.1177/10901981211019920. [DOI] [PubMed] [Google Scholar]
- 10.Opatz T., Senn-Bilfinger J., Richert C. Thoughts on What Chemists Can Contribute to Fighting SARS-CoV-2—A Short Note on Hand Sanitizers, Drug Candidates and Outreach. Angew. Chem. Int. Ed. Engl. 2020;59:9236–9240. doi: 10.1002/anie.202004721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Selam M.N. Hand Sanitizers Marketed in the Streets of Addis Ababa, Ethiopia, in the Era of COVID-19: A Quality Concern. Risk Manag. Healthc. Policy. 2020;13:2483–2487. doi: 10.2147/RMHP.S284007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ory J., Zingg W., de Kraker M.E.A., Soule H., Pittet D. Wiping Is Inferior to Rubbing: A Note of Caution for Hand Hygiene with Alcohol-Based Solutions. Infect. Control Hosp. Epidemiol. 2018;39:332–335. doi: 10.1017/ice.2017.307. [DOI] [PubMed] [Google Scholar]
- 13.Rai H., Knighton S., Zabarsky T.F., Donskey C.J. Comparison of Ethanol Hand Sanitizer versus Moist Towelette Packets for Mealtime Patient Hand Hygiene. Am. J. Infect. Control. 2017;45:1033–1034. doi: 10.1016/j.ajic.2017.03.018. [DOI] [PubMed] [Google Scholar]
- 14.Jing J.L.J., Pei Yi T., Bose R.J.C., McCarthy J.R., Tharmalingam N., Madheswaran T. Hand Sanitizers: A Review on Formulation Aspects, Adverse Effects, and Regulations. Int. J. Environ. Res. Public Health. 2020;17:3326. doi: 10.3390/ijerph17093326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Golin A.P., Choi D., Ghahary A. Hand Sanitizers: A Review of Ingredients, Mechanisms of Action, Modes of Delivery, and Efficacy against Coronaviruses. Am. J. Infect. Control. 2020;48:1062–1067. doi: 10.1016/j.ajic.2020.06.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saha T., Khadka P., Das S.C. Alcohol-Based Hand Sanitizer—Composition, Proper Use and Precautions. Germs. 2021;11:408–417. doi: 10.18683/germs.2021.1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Abuga K., Nyamweya N. Alcohol-Based Hand Sanitizers in COVID-19 Prevention: A Multidimensional Perspective. Pharm. J. Pharm. Educ. Pract. 2021;9:64. doi: 10.3390/pharmacy9010064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Selam M.N., Bayisa R., Ababu A., Abdella M., Diriba E., Wale M., Baye A.M. Increased Production of Alcohol-Based Hand Rub Solution in Response to COVID-19 and Fire Hazard Potential: Preparedness of Public Hospitals in Addis Ababa, Ethiopia. Risk Manag. Healthc. Policy. 2020;13:2507–2513. doi: 10.2147/RMHP.S279957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Edmonds-Wilson S., Campbell E., Fox K., Macinga D. Comparison of 3 in Vivo Methods for Assessment of Alcohol-Based Hand Rubs. Am. J. Infect. Control. 2015;43:506–509. doi: 10.1016/j.ajic.2015.01.025. [DOI] [PubMed] [Google Scholar]
- 20.Filipe H.A.L., Fiuza S.M., Henriques C.A., Antunes F.E. Antiviral and Antibacterial Activity of Hand Sanitizer and Surface Disinfectant Formulations. Int. J. Pharmaceut. 2021;609:121139. doi: 10.1016/j.ijpharm.2021.121139. [DOI] [PubMed] [Google Scholar]
- 21.Suchomel M., Fritsch F., Kampf G. Bactericidal Efficacy of Two Modified WHO-Recommended Alcohol-Based Hand Rubs Using Two Types of Rub-in Techniques for 15 s. J. Hosp. Infect. 2021;111:47–49. doi: 10.1016/j.jhin.2021.03.011. [DOI] [PubMed] [Google Scholar]
- 22.Booq R.Y., Alshehri A.A., Almughem F.A., Zaidan N.M., Aburayan W.S., Bakr A.A., Kabli S.H., Alshaya H.A., Alsuabeyl M.S., Alyamani E.J., et al. Formulation and Evaluation of Alcohol-Free Hand Sanitizer Gels to Prevent the Spread of Infections during Pandemics. Int. J. Environ. Res. Public Health. 2021;18:6252. doi: 10.3390/ijerph18126252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yüksel Y.T., Sonne M., Nørreslet L.B., Gundersen G., Fazli M.M., Agner T. Skin Barrier Response to Active Chlorine Hand Disinfectant-An Experimental Study Comparing Skin Barrier Response to Active Chlorine Hand Disinfectant and Alcohol-Based Hand Rub on Healthy Skin and Eczematous Skin. Ski. Res. Technol. 2022;28:89–97. doi: 10.1111/srt.13096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Advice for the Public on COVID-19—World Health Organization. [(accessed on 20 October 2022)]. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public.
- 25.Hoang H.T., Van Tran V., Bui V.K.H., Kwon O.-H., Moon J.-Y., Lee Y.-C. Novel Moisturized and Antimicrobial Hand Gel Based on Zinc-Aminoclay and Opuntia humifusa Extract. Sci. Rep. 2021;11:17821. doi: 10.1038/s41598-021-97363-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Choi K., Sim S., Choi J., Park C., Uhm Y., Lim E., Kim A.Y., Yoo S.J., Lee Y. Changes in Handwashing and Hygiene Product Usage Patterns in Korea before and after the Outbreak of COVID-19. Environ. Sci. Eur. 2021;33:79. doi: 10.1186/s12302-021-00517-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Galvin C.J., Li Y.-C.J., Malwade S., Syed-Abdul S. COVID-19 Preventive Measures Showing an Unintended Decline in Infectious Diseases in Taiwan. Int. J. Infect. Dis. IJID Off. Publ. Int. Soc. Infect. Dis. 2020;98:18–20. doi: 10.1016/j.ijid.2020.06.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rundle C.W., Presley C.L., Militello M., Barber C., Powell D.L., Jacob S.E., Atwater A.R., Watsky K.L., Yu J., Dunnick C.A. Hand Hygiene during COVID-19: Recommendations from the American Contact Dermatitis Society. J. Am. Acad. Dermatol. 2020;83:1730–1737. doi: 10.1016/j.jaad.2020.07.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Boyce J.M., Pittet D., Healthcare Infection Control Practices Advisory Committee. HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force Guideline for Hand Hygiene in Health-Care Settings Recommendations of the Healthcare Infection Control Practices Advisory Committee and the HICPAC/SHEA/APIC/IDSA Hand Hygiene Task Force. Society for Healthcare Epidemiology of America/Association for Professionals in Infection Control/Infectious Diseases Society of America. MMWR Recomm. Rep. Morb. Mortal. Wkly. Rep. 2002;51:1–45. quiz CE1-4. [PubMed] [Google Scholar]
- 30.Guo X., Huang S., Sun J., Wang F. Comparison of the Cytotoxicities and Wound Healing Effects of Hyaluronan, Carbomer, and Alginate on Skin Cells in Vitro. Adv. Ski. Wound Care. 2015;28:410–414. doi: 10.1097/01.ASW.0000467303.39079.59. [DOI] [PubMed] [Google Scholar]
- 31.Fresno Contreras M.J., Ramírez Diéguez A., Jiménez Soriano M.M. Rheological Characterization of Hydroalcoholic Gels—15% Ethanol—Of Carbopol Ultrez 10. II Farm. 2001;56:437–441. doi: 10.1016/S0014-827X(01)01057-6. [DOI] [PubMed] [Google Scholar]
- 32.Berardi A., Perinelli D.R., Bisharat L., Sabbatini B., Bonacucina G., Tiboni M., Palmieri G.F., Cespi M. Factors Affecting the Rheological Behaviour of Carbomer Dispersions in Hydroalcoholic Medium: Towards the Optimization of Hand Sanitiser Gel Formulations. Int. J. Pharm. 2022;616:121503. doi: 10.1016/j.ijpharm.2022.121503. [DOI] [PubMed] [Google Scholar]
- 33.Islam M.T., Rodríguez-Hornedo N., Ciotti S., Ackermann C. Rheological Characterization of Topical Carbomer Gels Neutralized to Different PH. Pharm. Res. 2004;21:1192–1199. doi: 10.1023/B:PHAM.0000033006.11619.07. [DOI] [PubMed] [Google Scholar]
- 34.Tamimi A.H., Carlino S., Edmonds S., Gerba C.P. Impact of an Alcohol-Based Hand Sanitizer Intervention on the Spread of Viruses in Homes. Food Environ. Virol. 2014;6:140–144. doi: 10.1007/s12560-014-9141-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tamimi A.H., Maxwell S., Edmonds S.L., Gerba C.P. Impact of the Use of an Alcohol-Based Hand Sanitizer in the Home on Reduction in Probability of Infection by Respiratory and Enteric Viruses. Epidemiol. Infect. 2015;143:3335–3341. doi: 10.1017/S0950268815000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Munoz-Figueroa G.P., Ojo O. The Effectiveness of Alcohol-Based Gel for Hand Sanitising in Infection Control. Br. J. Nurs. Mark Allen Publ. 2018;27:382–388. doi: 10.12968/bjon.2018.27.7.382. [DOI] [PubMed] [Google Scholar]
- 37.Zhao P., Li Y. Modeling and Experimental Validation of Microbial Transfer via Surface Touch. Environ. Sci. Technol. 2021;55:4148–4161. doi: 10.1021/acs.est.0c04678. [DOI] [PubMed] [Google Scholar]
- 38.L’Huillier A.G., Tapparel C., Turin L., Boquete-Suter P., Thomas Y., Kaiser L. Survival of Rhinoviruses on Human Fingers. Clin. Microbiol. Infect. Off. Publ. Eur. Soc. Clin. Microbiol. Infect. Dis. 2015;21:381–385. doi: 10.1016/j.cmi.2014.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Edmonds S.L., Mann J., McCormack R.R., Macinga D.R., Fricker C.M., Arbogast J.W., Dolan M.J. SaniTwice: A Novel Approach to Hand Hygiene for Reducing Bacterial Contamination on Hands When Soap and Water Are Unavailable. J. Food Prot. 2010;73:2296–2300. doi: 10.4315/0362-028X-73.12.2296. [DOI] [PubMed] [Google Scholar]
- 40.Lotfinejad N., Peters A., Tartari E., Fankhauser-Rodriguez C., Pires D., Pittet D. Hand Hygiene in Health Care: 20 Years of Ongoing Advances and Perspectives. Lancet Infect. Dis. 2021;21:e209–e221. doi: 10.1016/S1473-3099(21)00383-2. [DOI] [PubMed] [Google Scholar]
- 41.Vermeil T., Peters A., Kilpatrick C., Pires D., Allegranzi B., Pittet D. Hand Hygiene in Hospitals: Anatomy of a Revolution. J. Hosp. Infect. 2019;101:383–392. doi: 10.1016/j.jhin.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 42.Finger J.A.F.F., Lima E.M.F., Coelho K.S., Behrens J.H., Landgraf M., Franco B.D.G.M., Pinto U.M. Adherence to Food Hygiene and Personal Protection Recommendations for Prevention of COVID-19. Trends Food Sci. Technol. 2021;112:847–852. doi: 10.1016/j.tifs.2021.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sandora T.J., Taveras E.M., Shih M.-C., Resnick E.A., Lee G.M., Ross-Degnan D., Goldmann D.A. A Randomized, Controlled Trial of a Multifaceted Intervention Including Alcohol-Based Hand Sanitizer and Hand-Hygiene Education to Reduce Illness Transmission in the Home. Pediatrics. 2005;116:587–594. doi: 10.1542/peds.2005-0199. [DOI] [PubMed] [Google Scholar]
- 44.Montville R., Chen Y., Schaffner D.W. Risk Assessment of Hand Washing Efficacy Using Literature and Experimental Data. Int. J. Food Microbiol. 2002;73:305–313. doi: 10.1016/S0168-1605(01)00666-3. [DOI] [PubMed] [Google Scholar]
- 45.Feingold K.R. Thematic Review Series: Skin Lipids. The Role of Epidermal Lipids in Cutaneous Permeability Barrier Homeostasis. J. Lipid Res. 2007;48:2531–2546. doi: 10.1194/jlr.R700013-JLR200. [DOI] [PubMed] [Google Scholar]
- 46.Singh D., Joshi K., Samuel A., Patra J., Mahindroo N. Alcohol-Based Hand Sanitisers as First Line of Defence against SARS-CoV-2: A Review of Biology, Chemistry and Formulations. Epidemiol. Infect. 2020;148:e229. doi: 10.1017/S0950268820002319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dear K., Grayson L., Nixon R. Potential Methanol Toxicity and the Importance of Using a Standardised Alcohol-Based Hand Rub Formulation in the Era of COVID-19. Antimicrob. Resist. Infect. Control. 2020;9:129. doi: 10.1186/s13756-020-00788-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ho H.J., Poh B.-F., Choudhury S., Krishnan P., Ang B., Chow A. Alcohol Handrubbing and Chlorhexidine Handwashing Are Equally Effective in Removing Methicillin-Resistant Staphylococcus aureus from Health Care Workers’ Hands: A Randomized Controlled Trial. Am. J. Infect. Control. 2015;43:1246–1248. doi: 10.1016/j.ajic.2015.06.005. [DOI] [PubMed] [Google Scholar]
- 49.Wolfe M.K., Gallandat K., Daniels K., Desmarais A.M., Scheinman P., Lantagne D. Handwashing and Ebola Virus Disease Outbreaks: A Randomized Comparison of Soap, Hand Sanitizer, and 0.05% Chlorine Solutions on the Inactivation and Removal of Model Organisms Phi6 and E. coli from Hands and Persistence in Rinse Water. PLoS ONE. 2017;12:e0172734. doi: 10.1371/journal.pone.0172734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Nyamadzawo A., Nishio J., Okada S., Nyamakura R. Effect of Using Portable Alcohol-Based Handrub on Nurses’ Hand Hygiene Compliance and Nasal Carriage of Staphylococcus aureus in a Low-Income Health Setting. Am. J. Infect. Control. 2020;48:473–479. doi: 10.1016/j.ajic.2020.02.007. [DOI] [PubMed] [Google Scholar]
- 51.Andal V., Lakshmipathy R., Jose D. Effect of Sanitizer on Obliteration of SARS-CoV2/COVID 19: A Mini Review. Mater. Today Proc. 2022;55:264–266. doi: 10.1016/j.matpr.2021.07.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ochwoto M., Muita L., Talaam K., Wanjala C., Ogeto F., Wachira F., Osman S., Kimotho J., Ndegwa L. Anti-Bacterial Efficacy of Alcoholic Hand Rubs in the Kenyan Market, 2015. Antimicrob. Resist. Infect. Control. 2017;6:17. doi: 10.1186/s13756-017-0174-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kramer A., Arvand M., Christiansen B., Dancer S., Eggers M., Exner M., Müller D., Mutters N.T., Schwebke I., Pittet D. Ethanol Is Indispensable for Virucidal Hand Antisepsis: Memorandum from the Alcohol-Based Hand Rub (ABHR) Task Force, WHO Collaborating Centre on Patient Safety, and the Commission for Hospital Hygiene and Infection Prevention (KRINKO), Robert Koch Institute, Berlin, Germany. Antimicrob. Resist. Infect. Control. 2022;11:93. doi: 10.1186/s13756-022-01134-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kratzel A., Todt D., V’kovski P., Steiner S., Gultom M., Thao T.T.N., Ebert N., Holwerda M., Steinmann J., Niemeyer D., et al. Inactivation of Severe Acute Respiratory Syndrome Coronavirus 2 by WHO-Recommended Hand Rub Formulations and Alcohols. Emerg. Infect. Dis. 2020;26:1592–1595. doi: 10.3201/eid2607.200915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kampf G., Hollingsworth A. Comprehensive Bactericidal Activity of an Ethanol-Based Hand Gel in 15 Seconds. Ann. Clin. Microbiol. Antimicrob. 2008;7:2. doi: 10.1186/1476-0711-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Guilhermetti M., Marques Wiirzler L.A., Castanheira Facio B., da Silva Furlan M., Campo Meschial W., Bronharo Tognim M.C., Botelho Garcia L., Luiz Cardoso C. Antimicrobial Efficacy of Alcohol-Based Hand Gels. J. Hosp. Infect. 2010;74:219–224. doi: 10.1016/j.jhin.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 57.Gammon J., Hunt J. COVID-19 and Hand Hygiene: The Vital Importance of Hand Drying. Br. J. Nurs. Mark Allen Publ. 2020;29:1003–1006. doi: 10.12968/bjon.2020.29.17.1003. [DOI] [PubMed] [Google Scholar]
- 58.Voniatis C., Bánsághi S., Ferencz A., Haidegger T. A Large-Scale Investigation of Alcohol-Based Handrub (ABHR) Volume: Hand Coverage Correlations Utilizing an Innovative Quantitative Evaluation System. Antimicrob. Resist. Infect. Control. 2021;10:49. doi: 10.1186/s13756-021-00917-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ren S., Ni X., Xu H., Den J., Wang Y., Sun J., Kong Q., Zha J., Jin H., Zhao H., et al. The Relationship between Hand Area and Hand Contamination. Am. J. Infect. Control. 2011;39:66–68. doi: 10.1016/j.ajic.2010.06.014. [DOI] [PubMed] [Google Scholar]
- 60.Price L., Gozdzielewska L., Alejandre J.C., Jorgenson A., Stewart E., Pittet D., Reilly J. Systematic Review on Factors Influencing the Effectiveness of Alcohol-Based Hand Rubbing in Healthcare. Antimicrob. Resist. Infect. Control. 2022;11:16. doi: 10.1186/s13756-021-01049-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.la Fleur P., Jones S. Non-Alcohol Based Hand Rubs: A Review of Clinical Effectiveness and Guidelines. Canadian Agency for Drugs and Technologies in Health; Ottawa, ON, Canada: 2017. CADTH Rapid Response Reports. [PubMed] [Google Scholar]
- 62.Soltani M., Ravine T.J., Davis J.H. Novel Boronium Salt Exhibits Substantial Antibacterial Activity When Compared to a Commercial Quaternary Ammonium Disinfectant. Bioorg. Med. Chem. Lett. 2021;36:127808. doi: 10.1016/j.bmcl.2021.127808. [DOI] [PubMed] [Google Scholar]
- 63.Sadakane K., Ichinose T. Effect of the Hand Antiseptic Agents Benzalkonium Chloride, Povidone-Iodine, Ethanol, and Chlorhexidine Gluconate on Atopic Dermatitis in NC/Nga Mice. Int. J. Med. Sci. 2015;12:116–125. doi: 10.7150/ijms.10322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Dev Kumar G., Mishra A., Dunn L., Townsend A., Oguadinma I.C., Bright K.R., Gerba C.P. Biocides and Novel Antimicrobial Agents for the Mitigation of Coronaviruses. Front. Microbiol. 2020;11:1351. doi: 10.3389/fmicb.2020.01351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Obłąk E., Piecuch A., Rewak-Soroczyńska J., Paluch E. Activity of Gemini Quaternary Ammonium Salts against Microorganisms. Appl. Microbiol. Biotechnol. 2019;103:625–632. doi: 10.1007/s00253-018-9523-2. [DOI] [PubMed] [Google Scholar]
- 66.Herdt B.L., Black E.P., Zhou S.S., Wilde C.J. Inactivation of SARS-CoV-2 by 2 Commercially Available Benzalkonium Chloride-Based Hand Sanitizers in Comparison with an 80% Ethanol-Based Hand Sanitizer. Infect. Prev. Pract. 2021;3:100191. doi: 10.1016/j.infpip.2021.100191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Schrank C.L., Minbiole K.P.C., Wuest W.M. Are Quaternary Ammonium Compounds, the Workhorse Disinfectants, Effective against Severe Acute Respiratory Syndrome-Coronavirus-2? Acs Infect. Dis. 2020;6:1553–1557. doi: 10.1021/acsinfecdis.0c00265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ogilvie B.H., Solis-Leal A., Lopez J.B., Poole B.D., Robison R.A., Berges B.K. SARS-CoV-2Alcohol-Free Hand Sanitizer and Other Quaternary Ammonium Disinfectants Quickly and Effectively Inactivate SARS-CoV-2. J. Hosp. Infect. 2021;108:142–145. doi: 10.1016/j.jhin.2020.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Thaddeus N., Francis E., Jane O., Obumneme A., Okechukwu E. Effects of Some Common Additives on the Antimicrobial Activities of Alcohol-Based Hand Sanitizers. Asian Pac. J. Trop. Med. 2018;11:222. doi: 10.4103/1995-7645.228437. [DOI] [Google Scholar]
- 70.Hakimi A.A., Armstrong W.B. Hand Sanitizer in a Pandemic: Wrong Formulations in the Wrong Hands. J. Emerg. Med. 2020;59:668–672. doi: 10.1016/j.jemermed.2020.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Emami A., Javanmardi F., Keshavarzi A., Pirbonyeh N. Hidden Threat Lurking behind the Alcohol Sanitizers in COVID-19 Outbreak. Dermatol. Ther. 2020;33:e13627. doi: 10.1111/dth.13627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Gloekler L.E., de Gandiaga E.J., Binczewski N.R., Steimel K.G., Massarsky A., Kozal J., Vincent M., Zisook R., LaGuardia M.J., Dotson S., et al. Evaluation of the Safety and Efficacy of Hand Sanitizer Products Marketed to Children Available during the COVID-19 Pandemic. Int. J. Environ. Res. Public. Health. 2022;19:14424. doi: 10.3390/ijerph192114424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Baye A.M., Ababu A., Bayisa R., Abdella M., Diriba E., Wale M., Selam M.N. Perspectives of Compounding Pharmacists on Alcohol-Based Hand Sanitizer Production and Utilization for COVID-19 Prevention in Addis Ababa, Ethiopia: A Descriptive Phenomenology Study. PLoS ONE. 2021;16:e0250020. doi: 10.1371/journal.pone.0250020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Chan A.P.L., Chan T.Y.K. Methanol as an Unlisted Ingredient in Supposedly Alcohol-Based Hand Rub Can Pose Serious Health Risk. Int. J. Environ. Res. Public. Health. 2018;15:1440. doi: 10.3390/ijerph15071440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Matatiele P., Southon B., Dabula B., Marageni T., Poongavanum P., Kgarebe B. Assessment of Quality of Alcohol-Based Hand Sanitizers Used in Johannesburg Area during the COVID-19 Pandemic. Sci. Rep. 2022;12:4231. doi: 10.1038/s41598-022-08117-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Aschenbrenner D.S. Is That Hand Sanitizer Safe? Am. J. Nurs. 2020;120:23. doi: 10.1097/01.NAJ.0000718612.75996.e3. [DOI] [PubMed] [Google Scholar]
- 77.Basak D., Deb S. Sensitivity of SARS-CoV-2 towards Alcohols: Potential for Alcohol-Related Toxicity in Humans. Life. 2021;11:1334. doi: 10.3390/life11121334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Martin G.C., Le Roux G., Guindolet D., Boulanger E., Hasle D., Morin E., Vodovar D., Vignal C., Gabison E., Descatha A., et al. Pediatric Eye Injuries by Hydroalcoholic Gel in the Context of the Coronavirus Disease 2019 Pandemic. JAMA Ophthalmol. 2021;139:348–351. doi: 10.1001/jamaophthalmol.2020.6346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Akbas E., Korkmaz I., Palamar M., Barut Selver O. Shifting Trends in Demographic Features of Chemical Eye Injuries during COVID-19 Pandemic. Int. Ophthalmol. 2022;42:2127–2132. doi: 10.1007/s10792-022-02211-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lopez T.K., Jones K., Roseberry-Lincoln A., Zidek A., MacKinnon L., Marro L. Adult and Children’s Use of Hand Sanitizer during a Pandemic—An Observational Study. J. Expo. Sci. Environ. Epidemiol. 2022 doi: 10.1038/s41370-022-00479-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Babić Ž., Turk R., Macan J. Toxicological Aspects of Increased Use of Surface and Hand Disinfectants in Croatia during the COVID-19 Pandemic: A Preliminary Report. Arh. Hig. Rada I Toksikol. 2020;71:261–264. doi: 10.2478/aiht-2020-71-3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gharpure R., Miller G.F., Hunter C.M., Schnall A.H., Kunz J., Garcia-Williams A.G. Safe Use and Storage of Cleaners, Disinfectants, and Hand Sanitizers: Knowledge, Attitudes, and Practices among U.S. Adults during the COVID-19 Pandemic, May 2020. Am. J. Trop. Med. Hyg. 2021;104:496–501. doi: 10.4269/ajtmh.20-1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Hsieh S., Sapkota A., Wood R., Bearer C., Kapoor S. Neonatal Ethanol Exposure from Ethanol-Based Hand Sanitisers in Isolettes. Arch. Dis. Child. Fetal Neonatal Ed. 2018;103:F55–F58. doi: 10.1136/archdischild-2016-311959. [DOI] [PubMed] [Google Scholar]
- 84.Ghosh A., Mahintamani T., Balhara Y.P.S., Roub F.E., Basu D., Bn S., Mattoo S.K., Mishra E., Sharma B. Disulfiram Ethanol Reaction with Alcohol-Based Hand Sanitizer: An Exploratory Study. Alcohol Alcohol. Oxf. Oxfs. 2021;56:42–46. doi: 10.1093/alcalc/agaa096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lu J., Guo J. Disinfection Spreads Antimicrobial Resistance. Science. 2021;371:474. doi: 10.1126/science.abg4380. [DOI] [PubMed] [Google Scholar]
- 86.Daverey A., Dutta K. COVID-19: Eco-Friendly Hand Hygiene for Human and Environmental Safety. J. Environ. Chem. Eng. 2021;9:104754. doi: 10.1016/j.jece.2020.104754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Assefa D., Melaku T. Commercial Hand Sanitizers Use amid COVID-19 Pandemic: The Concerns of Antimicrobial Resistance. Infect. Drug Resist. 2021;14:2183–2185. doi: 10.2147/IDR.S317767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Mahmood A., Eqan M., Pervez S., Alghamdi H.A., Tabinda A.B., Yasar A., Brindhadevi K., Pugazhendhi A. COVID-19 and Frequent Use of Hand Sanitizers; Human Health and Environmental Hazards by Exposure Pathways. Sci. Total Environ. 2020;742:140561. doi: 10.1016/j.scitotenv.2020.140561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Gaonkar T.A., Geraldo I., Caraos L., Modak S.M. An Alcohol Hand Rub Containing a Synergistic Combination of an Emollient and Preservatives: Prolonged Activity against Transient Pathogens. J. Hosp. Infect. 2005;59:12–18. doi: 10.1016/j.jhin.2004.06.030. [DOI] [PubMed] [Google Scholar]
- 90.Loh E.D.W., Yew Y.W. Hand Hygiene and Hand Eczema: A Systematic Review and Meta-Analysis. Contact Dermat. 2022;87:303–314. doi: 10.1111/cod.14133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Dahmardehei M., Khadem Rezaiyan M., Safarnejad F., Ahmadabadi A. An Unprecedented Increase in Burn Injuries Due to Alcohol-Based Hand Sanitizers during the COVID-19 Outbreak. Med. J. Islam. Repub. Iran. 2021;35:107. doi: 10.47176/mjiri.35.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Kolman M., Smith C., Chakrabarty D., Amin S. Rheological Stability of Carbomer in Hydroalcoholic Gels: Influence of Alcohol Type. Int. J. Cosmet. Sci. 2021;43:748–763. doi: 10.1111/ics.12750. [DOI] [PubMed] [Google Scholar]
- 93.Kaiser N., Klein D., Karanja P., Greten Z., Newman J. Inactivation of Chlorhexidine Gluconate on Skin by Incompatible Alcohol Hand Sanitizing Gels. Am. J. Infect. Control. 2009;37:569–573. doi: 10.1016/j.ajic.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 94.Alghamdi H.A. A Need to Combat COVID-19; Herbal Disinfection Techniques, Formulations and Preparations of Human Health Friendly Hand Sanitizers. Saudi J. Biol. Sci. 2021;28:3943–3947. doi: 10.1016/j.sjbs.2021.03.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Jain V.M., Karibasappa G.N., Dodamani A.S., Prashanth V.K., Mali G.V. Comparative Assessment of Antimicrobial Efficacy of Different Hand Sanitizers: An in Vitro Study. Dent. Res. J. 2016;13:424–431. doi: 10.4103/1735-3327.192283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.David O., Olatunji F., Alese M., Babalola T., Alese O. Antimicrobial Activity, Safety and Acceptability of Formulated Ginger-Fortified Hand Sanitizer Gel. Int. J. Trop. Dis. Health. 2017;22:1–11. doi: 10.9734/IJTDH/2017/28352. [DOI] [Google Scholar]
- 97.Parham S., Kharazi A.Z., Bakhsheshi-Rad H.R., Nur H., Ismail A.F., Sharif S., RamaKrishna S., Berto F. Antioxidant, Antimicrobial and Antiviral Properties of Herbal Materials. Antioxidants. 2020;9:1309. doi: 10.3390/antiox9121309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Nazzaro F., Fratianni F., De Martino L., Coppola R., De Feo V. Effect of Essential Oils on Pathogenic Bacteria. Pharmaceuticals. 2013;6:1451–1474. doi: 10.3390/ph6121451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Egner P., Pavlačková J., Sedlaříková J., Pleva P., Mokrejš P., Janalíková M. Non-Alcohol Hand Sanitiser Gels with Mandelic Acid and Essential Oils. Int. J. Mol. Sci. 2023;24:3855. doi: 10.3390/ijms24043855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Chouhan S., Sharma K., Guleria S. Antimicrobial Activity of Some Essential Oils-Present Status and Future Perspectives. Medicines. 2017;4:58. doi: 10.3390/medicines4030058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Wang X., Shen Y., Thakur K., Han J., Zhang J.-G., Hu F., Wei Z.-J. Antibacterial Activity and Mechanism of Ginger Essential Oil against Escherichia Coli and Staphylococcus aureus. Molecules. 2020;25:3955. doi: 10.3390/molecules25173955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Ismail M., Penlap V., Mbacham W.F., Kamdem S.L.S. Improvement of the Efficacy an WHO Alcohol-Based Hand Rub Formulation by Reducing Isopropanol Content and Associating Syzygium Aromarticum and Piper Nigrum Essential Oils. J. Appl. Life Sci. Int. 2019;21:1–11. doi: 10.9734/jalsi/2019/v21i330105. [DOI] [Google Scholar]
- 103.Dickinson D., Tufo M.D., Liu E., Shao X., Hsu S. Bactericidal and Fungicidal Activities of Novel ProtecTeaV Formulations—Alcohol-Based Hand Hygiene and Surface Disinfectant Prototypes Containing Epigallocatechin-3-Gallate-Palmitate (EC16) Microbiol. Infect. Dis. Wilmington Del. 2021;5 doi: 10.33425/2639-9458.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Dickinson D., Marsh B., Shao X., Liu E., Sampath L., Yao B., Jiang X., Hsu S. Virucidal Activities of Novel Hand Hygiene and Surface Disinfectant Formulations Containing EGCG-Palmitates (EC16) Am. J. Infect. Control. 2022;50:1212–1219. doi: 10.1016/j.ajic.2022.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Gendrisch F., Esser P.R., Schempp C.M., Wölfle U. Luteolin as a Modulator of Skin Aging and Inflammation. BioFactors Oxf. Engl. 2021;47:170–180. doi: 10.1002/biof.1699. [DOI] [PubMed] [Google Scholar]
- 106.Xi M., Hou Y., Wang R., Ji M., Cai Y., Ao J., Shen H., Li M., Wang J., Luo A. Potential Application of Luteolin as an Active Antibacterial Composition in the Development of Hand Sanitizer Products. Molecules. 2022;27:7342. doi: 10.3390/molecules27217342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Silva-Hughes A.F., Wedge D.E., Cantrell C.L., Carvalho C.R., Pan Z., Moraes R.M., Madoxx V.L., Rosa L.H. Diversity and Antifungal Activity of the Endophytic Fungi Associated with the Native Medicinal Cactus Opuntia humifusa (Cactaceae) from the United States. Microbiol. Res. 2015;175:67–77. doi: 10.1016/j.micres.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 108.Park K., Choi H.-S., Hong Y.H., Jung E.Y., Suh H.J. Cactus Cladodes (Opuntia humifusa) Extract Minimizes the Effects of UV Irradiation on Keratinocytes and Hairless Mice. Pharm. Biol. 2017;55:1032–1040. doi: 10.1080/13880209.2017.1286357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Burel C., Kala A., Purevdorj-Gage L. Impact of PH on Citric Acid Antimicrobial Activity against Gram-Negative Bacteria. Lett. Appl. Microbiol. 2021;72:332–340. doi: 10.1111/lam.13420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ionidis G., Hübscher J., Jack T., Becker B., Bischoff B., Todt D., Hodasa V., Brill F.H.H., Steinmann E., Steinmann J. Development and Virucidal Activity of a Novel Alcohol-Based Hand Disinfectant Supplemented with Urea and Citric Acid. Bmc Infect. Dis. 2016;16:77. doi: 10.1186/s12879-016-1410-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Halla N., Fernandes I.P., Heleno S.A., Costa P., Boucherit-Otmani Z., Boucherit K., Rodrigues A.E., Ferreira I.C.F.R., Barreiro M.F. Cosmetics Preservation: A Review on Present Strategies. Molecules. 2018;23:1571. doi: 10.3390/molecules23071571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bruce S., Roberts W., Teller C., Colvan L. The Effects of a Daily Skincare Regimen on Maintaining the Benefits Obtained from Previous Chemical Resurfacing Treatments. J. Drugs Dermatol. 2016;15:1145–1150. [PubMed] [Google Scholar]
- 113.Yamaguchi K., Maeda M., Masaki H., Iwabuchi T. Oil Thickening with Organoclay Enhances the Ultraviolet Absorption Ability of Sunscreen on a Skin-Mimicking Substrate. J. Oleo Sci. 2021;70:721–730. doi: 10.5650/jos.ess20309. [DOI] [PubMed] [Google Scholar]
- 114.Banat I.M., Franzetti A., Gandolfi I., Bestetti G., Martinotti M.G., Fracchia L., Smyth T.J., Marchant R. Microbial Biosurfactants Production, Applications and Future Potential. Appl. Microbiol. Biotechnol. 2010;87:427–444. doi: 10.1007/s00253-010-2589-0. [DOI] [PubMed] [Google Scholar]
- 115.Ali A.M., Hill H.J., Elkhouly G.E., Bakkar M.R., Raya N.R., Stamataki Z., Abo-Zeid Y. Rhamnolipid Nano-Micelles Inhibit SARS-CoV-2 Infection and Have No Dermal or Eye Toxic Effects in Rabbits. Antibiotics. 2022;11:1556. doi: 10.3390/antibiotics11111556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Abo-Zeid Y., Bakkar M.R., Elkhouly G.E., Raya N.R., Zaafar D. Rhamnolipid Nano-Micelles versus Alcohol-Based Hand Sanitizer: A Comparative Study for Antibacterial Activity against Hospital-Acquired Infections and Toxicity Concerns. Antibiotics. 2022;11:605. doi: 10.3390/antibiotics11050605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Bakkar M.R., Faraag A.H.I., Soliman E.R.S., Fouda M.S., Sarguos A.M.M., McLean G.R., Hebishy A.M.S., Elkhouly G.E., Raya N.R., Abo-zeid Y. Rhamnolipids Nano-Micelles as a Potential Hand Sanitizer. Antibiotics. 2021;10:751. doi: 10.3390/antibiotics10070751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ismail A., Raya N.R., Orabi A., Ali A.M., Abo-zeid Y. Investigating the Antibacterial Activity and Safety of Zinc Oxide Nanoparticles versus a Commercial Alcohol-Based Hand-Sanitizer: Can Zinc Oxide Nanoparticles Be Useful for Hand Sanitation? Antibiotics. 2022;11:1606. doi: 10.3390/antibiotics11111606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Annamalai J., Nallamuthu T. Green Synthesis of Silver Nanoparticles: Characterization and Determination of Antibacterial Potency. Appl. Nanosci. 2016;6:259–265. doi: 10.1007/s13204-015-0426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Yin I.X., Zhang J., Zhao I.S., Mei M.L., Li Q., Chu C.H. The Antibacterial Mechanism of Silver Nanoparticles and Its Application in Dentistry. Int. J. Nanomed. 2020;15:2555–2562. doi: 10.2147/IJN.S246764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wulandari I.O., Pebriatin B.E., Valiana V., Hadisaputra S., Ananto A.D., Sabarudin A. Green Synthesis of Silver Nanoparticles Coated by Water Soluble Chitosan and Its Potency as Non-Alcoholic Hand Sanitizer Formulation. Materials. 2022;15:4641. doi: 10.3390/ma15134641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Sugumar S., Ghosh V., Nirmala M.J., Mukherjee A., Chandrasekaran N. Ultrasonic Emulsification of Eucalyptus Oil Nanoemulsion: Antibacterial Activity against Staphylococcus aureus and Wound Healing Activity in Wistar Rats. Ultrason. Sonochem. 2014;21:1044–1049. doi: 10.1016/j.ultsonch.2013.10.021. [DOI] [PubMed] [Google Scholar]
- 123.Ghosh S., Nandi S., Basu T. Nano-Antibacterials Using Medicinal Plant Components: An Overview. Front. Microbiol. 2021;12:768739. doi: 10.3389/fmicb.2021.768739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Aleksic Sabo V., Knezevic P. Antimicrobial Activity of Eucalyptus Camaldulensis Dehn. Plant Extracts and Essential Oils: A Review. Ind. Crops Prod. 2019;132:413–429. doi: 10.1016/j.indcrop.2019.02.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sirelkhatim A., Mahmud S., Seeni A., Kaus N.H.M., Ann L.C., Bakhori S.K.M., Hasan H., Mohamad D. Review on Zinc Oxide Nanoparticles: Antibacterial Activity and Toxicity Mechanism. Nano-Micro Lett. 2015;7:219–242. doi: 10.1007/s40820-015-0040-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Palacios-Hernandez T., Diaz-Diestra D.M., Nguyen A.K., Skoog S.A., Vijaya Chikkaveeraiah B., Tang X., Wu Y., Petrochenko P.E., Sussman E.M., Goering P.L. Cytotoxicity, Cellular Uptake and Apoptotic Responses in Human Coronary Artery Endothelial Cells Exposed to Ultrasmall Superparamagnetic Iron Oxide Nanoparticles. J. Appl. Toxicol. JAT. 2020;40:918–930. doi: 10.1002/jat.3953. [DOI] [PubMed] [Google Scholar]
- 127.Lebda M.A., Sadek K.M., Tohamy H.G., Abouzed T.K., Shukry M., Umezawa M., El-Sayed Y.S. Potential Role of α-Lipoic Acid and Ginkgo Biloba against Silver Nanoparticles-Induced Neuronal Apoptosis and Blood-Brain Barrier Impairments in Rats. Life Sci. 2018;212:251–260. doi: 10.1016/j.lfs.2018.10.011. [DOI] [PubMed] [Google Scholar]
- 128.Liao C., Li Y., Tjong S.C. Bactericidal and Cytotoxic Properties of Silver Nanoparticles. Int. J. Mol. Sci. 2019;20:449. doi: 10.3390/ijms20020449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Nisbar N.D., Jamal Khair S.K., Bujang N.B., Mohd Yusop A.Y. Determination of Ethanol, Isopropyl Alcohol and Methanol in Alcohol-Based Hand Sanitiser to Ensure Product Quality, Safety and Efficacy. Sci. Rep. 2023;13:9478. doi: 10.1038/s41598-023-36283-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Fallica F., Leonardi C., Toscano V., Santonocito D., Leonardi P., Puglia C. Assessment of Alcohol-Based Hand Sanitizers for Long-Term Use, Formulated with Addition of Natural Ingredients in Comparison to WHO Formulation 1. Pharmaceutics. 2021;13:571. doi: 10.3390/pharmaceutics13040571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ramaiah G.B., Tegegne A., Melese B. Developments in Nano-Materials and Analysing Its Role in Fighting COVID-19. Mater. Today Proc. 2021;47:4357–4363. doi: 10.1016/j.matpr.2021.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Bisht B., Lohani U.C., Kumar V., Gururani P., Sinhmar R. Edible Hydrocolloids as Sustainable Substitute for Non-Biodegradable Materials. Crit. Rev. Food Sci. Nutr. 2022;62:693–725. doi: 10.1080/10408398.2020.1827219. [DOI] [PubMed] [Google Scholar]
- 133.Ahmad Raus R., Wan Nawawi W.M.F., Nasaruddin R.R. Alginate and Alginate Composites for Biomedical Applications. Asian J. Pharm. Sci. 2021;16:280–306. doi: 10.1016/j.ajps.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.