Abstract
Background:
Cardiovascular diseases, specifically acute myocardial infarction (AMI), are the leading cause of death worldwide. In this review, we explain the characteristics of AMI in Iran.
Methods:
We searched PubMed, Google, and Google Scholar for articles containing myocardial infarction, STEMI, and MI+ Iran in English and Persian words.
Results:
The age-standardized incidence rate of MI was 73.3 per 100 000. The mean±SD age of patients was 61.20±13.40 years. In-hospital mortality of patients with AMI in the IMIR was 12.1%. Concerning AMI complications reported in the IMIR, 5.8% of patients experienced ventricular tachycardia, and 2.5% experienced ventricular fibrillation. The 1-year mortality rate in the IPACE2 study was 4.3%.
Conclusion:
Only a few national studies are available in Iran regarding patients with AMI. A federal surveillance program continuously monitoring and tracking coronary events is essential to improve the general population’s health.
Keywords: Myocardial infarction, ST-elevation myocardial infarction, Iran
Introduction
Cardiovascular diseases, including ischemic heart disease, stroke, heart failure, and peripheral arterial disease, constitute the leading cause of mortality and are a significant contributor to reduced quality of life the world over.1 In 2019, cardiovascular diseases were the underlying cause of 9.6 million deaths among men and 8.9 million deaths among women, approximately one-third of all deaths globally.2
As a subtype of ischemic heart disease, acute myocardial infarction (AMI) is the most common cause of death.3 From the epidemiological point of view, the incidence of MI in a population can be used as a proxy for the prevalence of coronary artery disease in that population.4
In this review, we explain the characteristics of AMI in Iran, a country with a population of about 75 million people in 2011.5 We searched PubMed, Google, and Google Scholar for articles containing myocardial infarction, STEMI, and MI+ Iran in English and Persian.
The age-standardized incidence rate of MI was reported at 73.3 per 100 000 in the whole country (95% confidence interval [CI], 72.30% to 74.30%) based on the Iranian Myocardial Infarction Registry (IMIR) in 2012, which varied from 24.5 to 152.5 per 100 000 across 31 provinces.6
The prevalence of hypertension in patients with coronary artery disease was reported 44.0% (95% CI, 38.00% to 49.00%): 67.0% in women (95% CI, 53.00% to 82.00%) and 42.0% in men (95% CI, 39.00% to 46.00%). The highest prevalence of hypertension was in patients with AMI (50.0%; 95% CI, 8.00% to 93.00%).7 Additionally, in a large population study on 20 750 patients with MI, 35.5% had hypertension, 26.2% were smokers, 17.8% had dyslipidemia, and 22.2% had type 2 diabetes mellitus.8 A summary of the reported risk factors in patients with AMI based on different studies is presented in Table 1.
Table 1.
Iranian studies on acute myocardial infarction according to location, years, mean age, sex, and risk factors*
| Author | Origin of the Population | Year | Type of Study | N | Mean age (year±SD) | Male | Diabetes mellitus | Dyslipidemia | Hypertension | Smoker |
|---|---|---|---|---|---|---|---|---|---|---|
| Ahmadi8 | 31 Provinces | 2012–2013 | Cross-sectional | 20750 | 61.20±13.40 | 72.4 | 22.2 | 17.8 | 35.5 | 26.2 |
| Hosseini30 | 1 hospital in Tehran | 2003–2007 | Retrospective | 2028 † | 60.60±12.50 | 75.0 | 32.3 | 46.7 | 42.8 | 33.2 |
| Sezavar17 | 5 hospitals in Tehran and Shiraz | 2017 | Prospective, observational | 162 † | 61.00±12.00 | 75.0 | 20.0 | 39.0 | 65.0 | 15.0 |
| Nozari21 | 1 hospital in Tehran | 2015–2019 | Observational | 2823 † | 59.60±11.60 | 79.5 | 40.5 | 53.3 | 46.6 | NA |
| Kassaian18 | 11 hospitals in Tehran, Mashhad, Tabriz, Isfahan, and Shiraz | 2011–2012 | Prospective | 463 † | 58.80±11.30 | 80.1 | 25.9 | 34.9 | 39.5 | 51.9 |
| Safi29 | 1 hospital in Tehran | 2001–2005 | Cross-sectional | 180 | 56.00±2.10 | 80.0 | 19.4 | 43.9 | 29.4 | 50.6 |
| Ghaffari27 | NA | 1993–2012 | Cross-sectional, descriptive, analytical | 600 | 60.03±11.61 | 73.3 | 15.7 | 11.3 | 39.3 | 43.5 |
| Beyranvand26 | 1 hospital in Tehran | 2003–2004 | Cohort | 132 | 59.20±13.10 | 76.5 | 21.2 | NA | 28 | 32.6 |
| Donyavi35 | 1 hospital in Tehran | 2005–2006 | Retrospective | 1283 | 62.40±12.30 | 74.0 | 35.1 | 53.2 | 45.2 | 67.6 |
| Poorhosseini16 | 1 hospital in Tehran | 2016–2018 | Cross-sectional | 2103 † | 59.49±11.79 | 76.4 | 31.2 | 41.8 | 40.5 | 35.1 |
| Saadatagah33 | 1 hospital in Tehran | 2006–2017 | Retrospective | 8295 † | 60.40±12.50 | 77.5 | 30.1 | 39.3 | 43.4 | 42.7 |
Data are presented as n (%).
ST-elevation myocardial infarction patients
The mean±SD age of patients was 61.20±13.40 years,6 with the mean age at MI incidence being significantly lower in men than in women.6,9–11 A summary of the reported mean age in patients with AMI according to different studies is shown in Table 1. Most patients with AMI were illiterate (46.3%) or had only primary school education (23.8%) in a large study in 2012.8 The geographical distribution of MI studies from 1994 through 2018 is illustrated in Figure 1.
Figure 1.
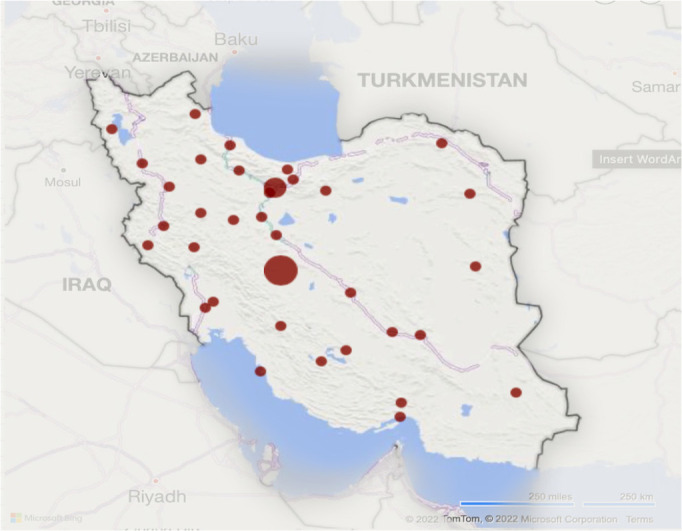
The image depicts the geographical distribution of Iranian studies on acute myocardial infarction.
Chest pain was the most common manifestation of patients with AMI.10,12–17 Small studies covered different periods across the country, from symptom onset to medical contact or arrival at the hospital. Only a minority of patients with AMI (35.7%) arrived at the hospital during the first hour of symptom onset, 7.9% 24 hours after symptom onset in Bandar Abbas,12 and 69.0% 2 hours after symptom onset in Kashan.15 In other articles, the mean (±SD) pre-hospital delay was 7.40 (±16.25) hours in Gilan,14 127.00 (±174.00) minutes in Kashan,13 265.60 minutes (among patients with acute coronary syndromes),18 149.00 (±120.00) minutes in Isfahan,19 and 146.00±20.00 minutes in Tehran among patients transferred in Emergency Medical System (EMS) ambulances.20 The median time of hospital arrival, according to various articles, was 279 (interquartile range [IQR], 120 to 630) minutes,16 258 (IQR, 108 to 574) minutes,21 3 (min-max: 0.5148) hours,22 and 244 (IQR, 109 to 565) minutes23 in Tehran.
According to several studies, prehospital delays were correlated with educational level. Patients with a higher level of education had a lower rate of prehospital delays12,16 and vice versa.13,14 The most common causes of delays were unawareness of coronary artery disease12 and waiting for improvement.15
A minority of patients with MI came to the hospital in EMS ambulances: 23.5% (n=227) in Bandar Abbas,12 17.3% (n=162) in Rasht,14 25.4% (n=248)13 and 10.0% (n=200) in Kashan,15 and 9.3% (n=2103),16 18.5% (n=2823),21 and 12.7% (n=1493)23 in Tehran.
In Tehran, among 513 patients with STEMI transported by the EMS, the mean time from the onset of symptoms to calling EMS was 61.00±19.00 minutes, and the mean transportation time from the patient’s place to the hospital was 34.00±12.00 minutes.20
AMI is classified as STEMI or non-STEMI based on the presence or absence of ST-segment elevation on the electrocardiogram.24 The ratio of STEMI among patients with AMI was 75.8%25 and 79.5%.26 The ratio among patients with coronary syndromes was 52.0%17 and 25.7%.18
The frequency of thrombolytic therapy among patients with AMI rose over time: 1.0% between 1993 and 1999, 13.0% between 1993 and 2003, 26.5% between 2003 and 2012,27 and 52.0% between 2000 and 2009.11 In addition, the frequency of thrombolytic therapy among patients with STEMI was 58.1% between 2003 and 2004,26 52.7% between 2009 and 2011,22 46.3% between 2011 and 2012,18 and 73.3% between 2012 and 2013.25
Streptokinase was the main thrombolytic drug in the past.10,18,22,26,27 Nonetheless, in recent years, it has been replaced with reteplase (Retelies, OSVAH Pharmaceutical CO, Tehran).
According to various articles, the median door-to-needle time was 30 (range: 6–330) minutes22 and 44 minutes, 20 with a mean (±SD) time of 45.60 (±41.10) minutes18 and 64.00 (±74.00) minutes.19
Primary percutaneous coronary intervention (PPCI) has increased rapidly in recent years. Many hospitals (n=31) are involved in a national program called “247”, which means the capability of doing PPCI over 24 hours, 7 days a week.28
The door-to-balloon time was reported in a few studies. The median door-to-balloon time was 30 (range: 60–300) minutes,22 53 minutes in the Iranian Project for Assessment of Coronary Events 2 (IPACE2) study,18 and 55 (IQR, 40 to 92) minutes in a study on 2823 patients. Further, a door-to-balloon time of 90 minutes or less was noted in most patients (74.0%).21 In a study on 180 patients, the door-to-balloon time was less than 90 minutes in only 39.0%.29 On the other hand, the median door-to-device time was 64 (41–100) minutes in a study on 11 563 patients who underwent PPCI in 247 centers. Additionally, 68.0% of the patients had a door-to-device time of 90 minutes or less.28 The in-hospital mortality rate of patients with AMI in the IMIR was 12.1%: 11.0% in males and 15.0% in females. Furthermore, the female/male fatality ratio was 1.36 (95% CI, 1.20 to 1.40), and the mortality rate was 13.3% in patients with STEMI and 8.1% in those with non-STEMI.8,25 In a study using data from the Cardiovascular Disease Registry of Tehran Heart Center from 2003 through 2007, in-hospital mortality was 5.8% in 2028 patients with STEMI.30
The fatality rate of patients with AMI has decreased over time, as shown in the Isfahan Registry, including 12 900 patients admitted with their first AMI during 10 years from 2000 through 2009. The registry showed a 28-day case fatality rate reduction, from 11.2% to 7.9%: from 9.2% to 6.7% in men and from 16.1% to 10.9% in women, indicating a 29.4% reduction in the case fatality rate: 27.1% in men and 32.2% in women.31
Among patients who underwent PPCI, the mortality rate was 6.6%.29 In a study on patients older than 75, the inhospital mortality rate was 17.0%: 2.4% in patients without cardiogenic shocks and 83.0% in those with cardiogenic shocks.32 In other studies, in-hospital mortality rates were 18.5%,28 5.4%,33 and 15.1%34 (Table 2).
Table 2.
Iranian studies on acute myocardial infarction according to location, years, treatment, and mortality
| Study | Year | N | Origin of the Population | Thrombolytic | Primary PCI | Door –to-Needle time (mean±SD) (min) | Door-to-Balloon Time (mean±SD) (min) | In-hospital Mortality | 1 M Mortality |
|---|---|---|---|---|---|---|---|---|---|
| Abdolazim 9 | 1999–2009 | 14426 | Isfahan | NA | NA | NA | NA | 6.7 (7 D Mortality) | 8.5 |
| Mohammadian 10 | 2000–2009 | 12900 | Isfahan | NA | NA | NA | NA | NA | 9.3 |
| Ghadimi 33 | 2002–2003 | 139 | Tehran | 35.9 | 6.4 | NA | NA | 15.1 | 17.3 |
| Hosseini 30 | 2003–2007 | 2028 | Tehran | NA | NA | NA | NA | 5.8 | NA |
| Saadatagah 33 | 2006–2017 | 8295 | Tehran | 36.6 | 28.0 | 31.00±15.00 | 70.00±25.00 | 5.4 | NA |
| Alishahi Tabriz 20 | 2007–2010 | 513 | Tehran | 100 | NA | 44 | NA | NA | NA |
| Donyavi 35 | 2008 | 664 | Tehran | NA | NA | NA | NA | NA | NA |
| Kassaian 18 | 2011–2012 | 463 | 5 Major cities | 46.3 | 17.3 | 45.60±41.10 | 82.80±112.50 | NA | NA |
| Ahmadi 25 | 2012 | 20750 | 31 provinces of Iran | NA | NA | NA | NA | 12.1 | NA |
| Nozari 21 | 2020 | 2823 | Tehran | 0 | 100 | NA | Median: 55 (IQR 40–92) | 1.6 | NA |
| Abdi 28 | 2021 | 11563 | 31 Centers | NA | 100 | NA | Median: 64 (41–100) | NA | NA |
The complications of AMI have not been reported thoroughly. In the IMIR, ventricular tachycardia occurred in 1198 patients (5.8%) and ventricular fibrillation in 511 (2.5%). The frequencies of ventricular tachycardia and ventricular fibrillation were significantly higher in deceased patients (10.5% vs 5.1% and 5.5% vs 2.0%, respectively; P=0.001).25
The duration of hospitalization showed a significant reduction, as shown in a multicenter study over 20 years from 1993 through 2012, from a mean duration of 11.36±6.48 days to 6.35±3.56 days.27
Data regarding long-term mortality are scarce. According to various articles, short-term (28 d) survival rates were 91.5% (93.0% in males and 86.8% in females)9 and 90.9% (92.5% in males and 86.7% in females).10 Most deaths occurred during the first week after the events.9
One-year mortality of 132 patients with AMI (20.0% non-STEMI) stood at 6.1% and readmission rates at 14.3%.26 The 1-year mortality rate in the IPACE2 study was 4.3% (71.4% cardiac causes).18 The 2-year mortality rate in 664 out of 1283 patients with AMI who could be followed up was 24.7% in a study on 139 patients with AMI in 2002.35
Ghadimi et al34 reported 1-, 6-, and 12-month cumulative mortality rates of 17.3%, 20.1%, and 21.6%, respectively (Table 2).
In a small study, the rates of adherence to prescribed β-blockers, ASA, angiotensin-converting enzyme inhibitors, and statins 1 year after discharge were 74.2%, 98.5%, 71.2%, and 67.4%, respectively.26
Conclusion
Few extensive national studies have been conducted on patients with AMI in Iran. Having a national program for gathering data on patients with AMI throughout the country will help to overcome this shortage.
A national surveillance program that continuously monitors and tracks coronary events is essential to improve the general population’s health. In addition, such a program may be used as an indicator of the effectiveness of community-based interventions by showing the outcome of intervention programs on the population.
Notes:
This paper should be cited as: Beyranvand MR, Manhoobi H, Shahraz S, Kolahi AA. Myocardial Infarction in Iran: Epidemiology, Management, and Prognosis. J Teh Univ Heart Ctr 2023;18(2):82-86.
References
- 1.Mensah GA, Roth GA, Fuster V. The Global Burden of Cardiovascular Diseases and Risk Factors: 2020 and Beyond. J Am Coll Cardiol 2019;74:2529–2532. [DOI] [PubMed] [Google Scholar]
- 2.Roth GA, Mensah GA, Fuster V. The Global Burden of Cardiovascular Diseases and Risks: A Compass for Global Action. J Am Coll Cardiol 2020;76:2980–2981. [DOI] [PubMed] [Google Scholar]
- 3.Roth GA, Johnson C, Abajobir A, Abd-Allah F, Abera SF, Abyu G, Ahmed M, Aksut B, Alam T, Alam K, Alla F, Alvis-Guzman N, Amrock S, Ansari H, Ärnlöv J, Asayesh H, Atey TM, Avila-Burgos L, Awasthi A, Banerjee A, Barac A, Bärnighausen T, Barregard L, Bedi N, Belay Ketema E, Bennett D, Berhe G, Bhutta Z, Bitew S, Carapetis J, Carrero JJ, Malta DC, Castañeda-Orjuela CA, Castillo-Rivas J, Catalá-López F, Choi JY, Christensen H, Cirillo M, Cooper L, Jr, Criqui M, Cundiff D, Damasceno A, Dandona L, Dandona R, Davletov K, Dharmaratne S, Dorairaj P, Dubey M, Ehrenkranz R, El Sayed Zaki M, Faraon EJA, Esteghamati A, Farid T, Farvid M, Feigin V, Ding EL, Fowkes G, Gebrehiwot T, Gillum R, Gold A, Gona P, Gupta R, Habtewold TD, Hafezi-Nejad N, Hailu T, Hailu GB, Hankey G, Hassen HY, Abate KH, Havmoeller R, Hay SI, Horino M, Hotez PJ, Jacobsen K, James S, Javanbakht M, Jeemon P, John D, Jonas J, Kalkonde Y, Karimkhani C, Kasaeian A, Khader Y, Khan A, Khang YH, Khera S, Khoja AT, Khubchandani J, Kim D, Kolte D, Kosen S, Krohn KJ, Kumar GA, Kwan GF, Lal DK, Larsson A, Linn S, Lopez A, Lotufo PA, El Razek HMA, Malekzadeh R, Mazidi M, Meier T, Meles KG, Mensah G, Meretoja A, Mezgebe H, Miller T, Mirrakhimov E, Mohammed S, Moran AE, Musa KI, Narula J, Neal B, Ngalesoni F, Nguyen G, Obermeyer CM, Owolabi M, Patton G, Pedro J, Qato D, Qorbani M, Rahimi K, Rai RK, Rawaf S, Ribeiro A, Safiri S, Salomon JA, Santos I, Santric Milicevic M, Sartorius B, Schutte A, Sepanlou S, Shaikh MA, Shin MJ, Shishehbor M, Shore H, Silva DAS, Sobngwi E, Stranges S, Swaminathan S, Tabarés-Seisdedos R, Tadele Atnafu N, Tesfay F, Thakur JS, Thrift A, Topor-Madry R, Truelsen T, Tyrovolas S, Ukwaja KN, Uthman O, Vasankari T, Vlassov V, Vollset SE, Wakayo T, Watkins D, Weintraub R, Werdecker A, Westerman R, Wiysonge CS, Wolfe C, Workicho A, Xu G, Yano Y, Yip P, Yonemoto N, Younis M, Yu C, Vos T, Naghavi M, Murray C. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol 2017;70:1–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, White HD, Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction . Fourth Universal Definition of Myocardial Infarction (2018). Circulation 2018;138:e618–e651. [DOI] [PubMed] [Google Scholar]
- 5.Noroozian M. The elderly population in iran: an ever growing concern in the health system. Iran J Psychiatry Behav Sci 2012;6(2):1–6. [PMC free article] [PubMed] [Google Scholar]
- 6.Ahmadi A, Soori H, Mehrabi Y, Etemad K, Samavat T, Khaledifar A. Incidence of acute myocardial infarction in Islamic Republic of Iran: a study using national registry data in 2012. East Mediterr Health J 2015;21:5–12. [DOI] [PubMed] [Google Scholar]
- 7.Fakhri M, Sarokhani D, Ghiasi B, Dehkordi AH. Prevalence of Hypertension in Cardiovascular Disease in Iran: Systematic Review and Meta-Analysis. Int J Prev Med 2020;11:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmadi A, Soori H, Mehrabi Y, Etemad K, Khaledifar A. Epidemiological pattern of myocardial infarction and modelling risk factors relevant to in-hospital mortality: the first results from the Iranian Myocardial Infarction Registry. Kardiol Pol 2015;73:451–457. [DOI] [PubMed] [Google Scholar]
- 9.Abdolazimi M, Khosravi A, Sadeghi M, Mohammadian-Hafshejani A, Sarrafzadegan N, Salehiniya H, Golshahi J. Predictive factors of short-term survival from acute myocardial infarction in early and late patients in Isfahan and Najafabad, Iran. ARYA Atheroscler 2016;12:59–67. [PMC free article] [PubMed] [Google Scholar]
- 10.Mohammadian M, Hosseini S, Salehiniya H, Sadeghi M, Sarrafzadegan N, Roohafza HR, Khazaei S, Soltani S, Sarrafkia A, Golshahi J, Mohammadian-Hafshejani A. Prognostic factors of 28 days survival rate in patients with a first acute myocardial infarction based on gender in Isfahan, Iran (2000–2009). ARYA Atheroscler 2015;11:332–340. [PMC free article] [PubMed] [Google Scholar]
- 11.Hosseini K, Mortazavi SH, Sadeghian S, Ayati A, Nalini M, Aminorroaya A, Tavolinejad H, Salarifar M, Pourhosseini H, Aein A, Jalali A, Bozorgi A, Mehrani M, Kamangar F. Prevalence and trends of coronary artery disease risk factors and their effect on age of diagnosis in patients with established coronary artery disease: Tehran Heart Center (2005–2015). BMC Cardiovasc Disord 2021;21:477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farshidi H, Rahimi S, Abdi A, Salehi S, Madani A. Factors Associated With Pre-hospital Delay in Patients With Acute Myocardial Infarction. Iran Red Crescent Med J 2013;15:312–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dianati M, Mosavi GA, Hajibagheri A, Alavi NM. The pre-hospital delay in seeking treatment in patients with acute myocardial infarction referring to a central hospital in Kashan, Iran. Indian J Med Sci 2010;64:448–454. [PubMed] [Google Scholar]
- 14.Momeni M, Salari A, Shafighnia S, Ghanbari A, Mirbolouk F. Factors influencing pre-hospital delay among patients with acute myocardial infarction in Iran. Chin Med J (Engl) 2012;125:3404–3409. [PubMed] [Google Scholar]
- 15.Taghaddosi M, Dianati M, Fath Gharib Bidgoli J, Bahonaran J. Delay and its related factors in seeking treatment in patients with acute myocardial infarction. ARYA Atheroscler 2010;6:35–41. [PMC free article] [PubMed] [Google Scholar]
- 16.Poorhosseini H, Saadat M, Salarifar M, Mortazavi SH, Geraiely B. Pre-Hospital Delay and Its Contributing Factors in Patients with ST-Elevation Myocardial Infarction; a Cross sectional Study. Arch Acad Emerg Med 2019;7:e29. [PMC free article] [PubMed] [Google Scholar]
- 17.Sezavar SH, Hassanzadeh M, Akhlagh Moayed D, Tabandeh M, Ghasemi M, Abdi S, Firoozi I, Golbidi P, Pourjafari M, Taslimi N, Akhlaghi AA, Hashemian M. Current practice of percutaneous coronary intervention on patients with acute coronary syndrome in Iran: A prospective observational study. Med J Islam Repub Iran 2020;34:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kassaian SE, Masoudkabir F, Sezavar H, Mohammadi M, Pourmoghaddas A, Kojuri J, Ghaffari S, Sanaati H, Alaeddini F, Pourmirza B, Mir E, IPACE2 Registry Investigators . Clinical characteristics, management and 1-year outcomes of patients with acute coronary syndrome in Iran: the Iranian Project for Assessment of Coronary Events 2 (IPACE2). BMJ Open 2015;5:e007786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moeini M, Mahmoudian SN, Khalifezadeh A, Pour AH. Reviewing time intervals from onset of the symptoms to thrombolytic therapy in patients with ST segment elevation myocardial infarction (STEMI). Iran J Nurs Midwifery Res 2010;15(Suppl 1):379–385. [PMC free article] [PubMed] [Google Scholar]
- 20.Alishahi Tabriz A, Sohrabi MR, Kiapour N, Yazdani S. Factors Associated with Delay in Thrombolytic Therapy in Patients with ST-Elevation Myocardial Infarction. J Tehran Heart Cent 2012;7:65–71. [PMC free article] [PubMed] [Google Scholar]
- 21.Nozari Y, Geraiely B, Alipasandi K, Jalali A, Omidi N, Aghajani H, Hajizeinali A, Alidoosti M, Pourhoseini H, Salarifar M, Amirzadegan A, Nematipour E, Nomali M. Time to Treatment and In-Hospital Major Adverse Cardiac Events Among Patients With ST-Segment Elevation Myocardial Infarction Who Underwent Primary Percutaneous Coronary Intervention (PCI) According to the 24/7 Primary PCI Service Registry in Iran: Protocol for a Cross-Sectional Study. JMIR Res Protoc 2019;8:e13161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Khalili H, Talasaz AH, Jenab Y, Salarifar M. Clinical characteristics and risk assessment of ST-segment elevation myocardial infarction patients of an Iranian referral center. J Cardiovasc Med (Hagerstown) 2012;13:708–715. [DOI] [PubMed] [Google Scholar]
- 23.Salarifar M, Askari J, Saadat M, Geraiely B, Omid N, Poorhosseini H, Amirzadegan A, Hajzeinali A, Alidoosti M, Aghajani H, Nozari Y, Nematipoor E. Strategies to Reduce the Door-to-Device Time in ST-Elevation Myocardial Infarction Patients. J Tehran Heart Cent 2019;14:18–27. [PMC free article] [PubMed] [Google Scholar]
- 24.Anderson JL, Morrow DA. Acute Myocardial Infarction. N Engl J Med 2017;376:2053–2064. [DOI] [PubMed] [Google Scholar]
- 25.Ahmadi A, Khaledifar A, Sajjadi H, Soori H. Relationship between risk factors and in-hospital mortality due to myocardial infarction by educational level: a national prospective study in Iran. Int J Equity Health 2014;13:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beyranvand MR, Emami MA, Aliasgari A, Kolahi AA. One-Year Outcome of Patients with Acute Myocardial Infarction. J Tehran Heart Cent 2007;2:229–232. [Google Scholar]
- 27.Ghaffari S, Hakim H, Pourafkari L, Asl ES, Goldust M. Twenty-year route of prevalence of risk factors, treatment patterns, complications, and mortality rate of acute myocardial infarction in Iran. Ther Adv Cardiovasc Dis 2013;7:117–122. [DOI] [PubMed] [Google Scholar]
- 28.Abdi S, Haji Aghajani M, Janbabaei G, Noohi F, Kermanchi J, Salarifar M, Geraiely B, Sadeghipour P, Kazemi-Saleh D, Firouzi A, Soleimani A, Mortazavi SH. 24/7 Primary Percutaneous Coronary Intervention as a National Program. Crit Pathw Cardiol 2021;20:81–87. [DOI] [PubMed] [Google Scholar]
- 29.Safi M, Rajabi Moghadam H, Sadeghi R, Saadat H, Namazi MH, Vakili H, Hassantash SA, Motamedi MR. Primary Percutaneous Coronary Intervention in Patients with Acute Myocardial Infarction. J Tehran Heart Cent 2009;4:45–48. [Google Scholar]
- 30.Hosseini SK, Soleimani A, Karimi AA, Sadeghian S, Darabian S, Abbasi SH, Ahmadi SH, Zoroufian A, Mahmoodian M, Abbasi A. Clinical features, management and in-hospital outcome of ST elevation myocardial infarction (STEMI) in young adults under 40 years of age. Monaldi Arch Chest Dis 2009;72:71–6. [DOI] [PubMed] [Google Scholar]
- 31.Mohammadian M, Hosseini S, Sadeghi M, Sarrafzadegan N, Salehiniya H, Roohafza H, Khazaei S, Mohammadian-Hafshejani A. Trends of 28 days case fatality rate after first acute myocardial infarction in Isfahan, Iran, from 2000 to 2009. ARYA Atheroscler 2015;11:233–243. [PMC free article] [PubMed] [Google Scholar]
- 32.Noohi F, Hashemi I, Sanati HR, Peighambari MM, Kiavar M, Maadani M, Bassiri HA, Zahedmehr A, Shakerian F, Firouzi A, Kiani R, Abdi S. In-hospital and six-month outcomes of elderly patients undergoing primary percutaneous coronary intervention for acute ST-elevation myocardial infarction. ARYA Atheroscler 2016;12:28–34. [PMC free article] [PubMed] [Google Scholar]
- 33.Saadatagah S, Ghodsi S, Omidi N, Poorhosseini H, Salarifar M, Sadeghian S, Alidoosti M, Kassaian SE, Aghajani H, Mortazavi SH, Hosseini K, Geraiely B. Twelve-Year History of STEMI Management in Tehran Heart Center: Concomitant Reduction of In-Hospital Mortality and Hospitalization Length. Arch Iran Med 2020;23:514–521. [DOI] [PubMed] [Google Scholar]
- 34.Ghadimi H, Bishehsari F, Allameh F, Bozorgi AH, Sodagari N, Karami N, Yaghoubi M, Emami S, Ghadimi F, Haerizadeh BF, Sanati A. Clinical characteristics, hospital morbidity and mortality, and up to 1-year follow-up events of acute myocardial infarction patients: the first report from Iran. Coron Artery Dis 2006;17:585–591. [DOI] [PubMed] [Google Scholar]
- 35.Donyavi T, Naieni KH, Nedjat S, Vahdaninia M, Najafi M, Montazeri A. Socioeconomic status and mortality after acute myocardial infarction: a study from Iran. Int J Equity Health 2011;10:9. [DOI] [PMC free article] [PubMed] [Google Scholar]


