Abstract
Background
Scedosporium apiospermum (SA) is commonly present in temperate climates. It can induce cutaneous and subcutaneous tissue infections as well as disseminated infections in immunocompromised or immunocompetent hosts. The eye is rarely involved. Keratomycosis is usually caused by plant-related injuries. Here, we describe a patient with a severe and sight-threatening corneal abscess caused by SA, which was associated with contact lens wear and was successfully treated with a combination of surgical and medical therapies.
Case Presentation:
An otherwise healthy 22-year-old woman, with history of contact lens wearing, was referred to the Ophthalmic Department of Bari University, Bari, Italy for evaluation of a corneal abscess and hypopyon in her left eye. Intensive topical and systemic antibiotic therapy was initiated after obtaining con- junctival swabs. Within 2 days, her ophthalmic condition had worsened, and her best-corrected visual acuity (BCVA) dropped to counting fingers. She underwent penetrating keratoplasty, after which her ophthalmic condition improved. Microbiological culture, obtained from the explanted cornea, revealed SA infection. This was addressed with specific topical and systemic therapy using voriconazole. Two weeks later, the con- dition of her left eye was stable, with mild corneal edema and no sign of acute graft rejection. Her BCVA improved to 20/25, and all medications were discontinued, except for the steroid eye drop. The patient was scheduled for a 1-month follow-up.
Conclusions:
Prompt identification of the etiological agent is mandatory to perform appropriate therapy in cases of keratomycosis. Surgery to remove the infected cornea is helpful in patients with deteriorating condition, in whom the initial medical therapy has failed. Topical and systemic antimycotic therapy, based on microbiological culture, is recommended as an adjunctive therapy for the surgical management of severe corneal mycotic abscesses.
Key Words: Scedosporium apiospermum, keratitis, contact lenses, keratomycosis, penetrating keratoplasty, voriconazole
INTRODUCTION
Contact lens wear is a risk factor for microbial keratitis. Along with ocular trauma, contact lens wear is one of the two major factors predisposing to this condition [1]. Furthermore, fungi can invade the contact lens matri [2].
Fungal keratitis was an uncommon cause of keratitis until 2005; compared to a 29% incidence in the 1990s, a 52% incidence was registered in the early 2000s [3]. Fungal keratitis mostly occurs after corneal trauma in agricultural workers, usually, but not always, after exposure to fungus-contaminated plant material [4]. Trauma may also be so negligible that the patient cannot remember it. Filamentous fungi are responsible for most cases of keratitis, whereas in compromised corneas, yeasts, such as Candida species, may cause infection [4].
Scedosporium apiospermum (SA) and its sexual state Pseudallescheria boydii, is a ubiquitous filamentous fungus commonly present in temperate climates, where it is found in brackish water and saltwater, sewage, soil, poultry and cattle manure, and bat feces [1]. It can colonize previously damaged bronchopulmonary trees and cause localized, locally invasive, or hematogenously disseminated infections [5]. These infections affect many tissues, including the skin, soft tissues, bone (mycetoma), heart (endocarditis), brain (meningoencephalitis, meningitis, and brain abscess), and eye, where it causes keratitis, chorioretinitis, and endophthalmitis. Disseminated infections typically affect immunocompromised hosts; however, even in immunocompetent individuals, cases of disseminated disease have been reported. The eye is rarely involved, but such keratomycosis is usually caused by plant-related injuries [5]. Although keratitis caused by SA is rare, several cases have been reported [6, 7]. Early diagnosis is of the utmost importance, since the immediate initiation of antifungal therapy may improve the final prognosis, along with anatomical and functional recovery [8]. Therapy usually includes topical and systemic voriconazole (VRCZ); nevertheless, therapeutic penetrating keratoplasty is often required [9, 10].
Here, we describe a patient with a severe and sight-threatening corneal abscess that was caused by SA and was associated with contact lens wear, and which was successfully treated with combined surgical and medical therapies.
CASE PRESENTATION
An otherwise healthy 22-year-old woman, who had accidentally worn her contact lenses over the course of one night, was referred to the Ophthalmic Department of Bari University, Bari, Italy for a 1-week history of ocular pain and photophobia in her left eye, which appeared red. The patient wore contact lenses to correct myopic refractive error. She had no history of trauma, and her drug and medical history were unremarkable. She was first referred to a private ophthalmologist, who had prescribed topical tetracycline and sulfamethylthiazole, both three times daily, and systemic azithromycin (250 mg, twice daily) at a private clinic. However, after 5 days of treatment, the patient came to our clinic because the symptoms had not improved.
Her best-corrected visual acuity (BCVA) was 20/50, using a Snellen chart. On the first detailed slit-lamp examination (SL9900 Slit Lamp, CSO, Florence, Italy), she exhibited full involvement of the anterior segment with severe conjunctival and ciliary congestion, along with a substantial paracentral corneal abscess in her left eye. The anterior chamber and underlying structures were not fully explorable because of the extent of the corneal lesion. There was no suspected scleral or intraocular extension of the infection. Her fellow eye examination was normal, with a BCVA of 20/20. The patient underwent B-scan ultrasonography (HiScan Touch Unit, Optikon, Rome, Italy) of the left eye, which revealed no signs of posterior pole involvement (vitritis, retinal detachment, etc.). Conjunctival swabs were then obtained, and specimens were collected and subjected to combined smear microscopy and culture. Since the patient was no longer in possession of her contact lenses, smear and culture of the contact lens and its container was not possible. Due to the serious conditions of the patient and the non-response to the previous treatment regimen, her medication was switched to intravenous ceftriaxone (Roche Pharma, Basel, Switzerland) 2 g once daily, along with a drop of 1% atropine (Farmigea, Pisa, Italy) 2 times daily, ofloacin (Allergan; Ocuflo; Dublin, Ireland) eye drops 4 times daily, and topical gentamicin (ribomicin eye drops; Farmigea, SPA, Pisa, Italy) 4 times daily.
Within 2 days of starting the new treatment regimen, the patient’s ophthalmic condition had worsened severely; her BCVA deteriorated and dropped to counting fingers. On slit lamp examination, the abscess had extended to two-thirds of the corneal surface, with fibrinous strands in the anterior chamber and no visible details. Conjunctival swabs showed the presence of Aspergillus spp. Because of the unrelenting deterioration, she was scheduled to undergo penetrating keratoplasty, which was performed on the same day.
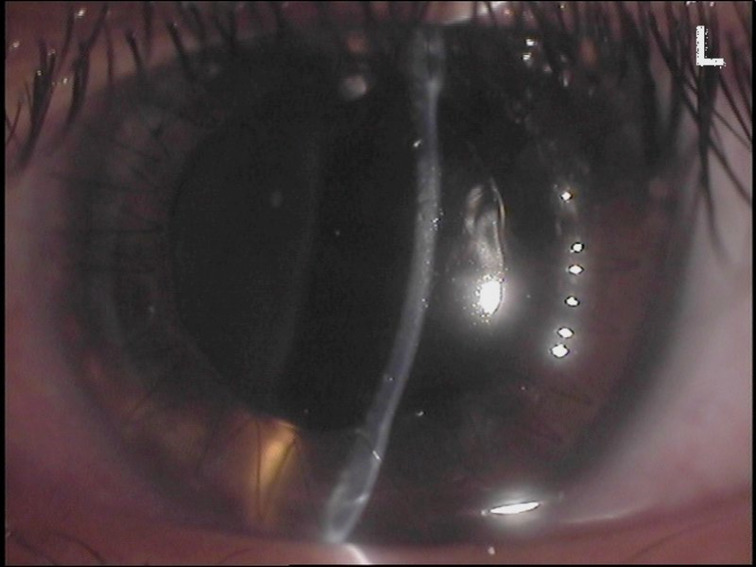
Microbiological examination of the explanted cornea revealed numerous SA colonies. On the advice of an infectious disease specialist, the patient’s therapy was adjusted to an hourly fortified antifungal eye drop (VRCZ 1 % solution; Vfend, Pfizer Inc., New York, NY, USA), and intravenous VRCZ, 6 mg/kg once, twice daily (Vfend; Pfizer Inc.). Within 1 week of discharge, the patient showed mild conjunctival hyperemia, the donor cornea was well positioned with a continuous nylon suture, and the anterior chamber was clear and showed normal depth. The dilated fundus examination results were normal. She continued therapy with hourly fortified VRCZ eye drops and oral itraconazole 100 mg twice daily (Janssen Pharmaceutica, Beerse, Belgium). Two weeks later, the condition of her left eye was stable, with mild corneal edema (Figure 1) and no sign of acute graft rejection. Her BCVA improved to 20/25, and all medications were discontinued, except for the steroid eye drop. The patient was scheduled for a 1-month follow-up.
Figure 1.
Slit photo of the patient’s left eye 2 weeks after penetrating keratoplasty. A full thickness corneal transplant has restored the patient’s anatomy. There is almost complete resolution of conjunctival reaction, the donor cornea is sutured with a continuous 10-0 nylon suture, and is clear, with fine Descemet’s folds inferiorly. The anterior chamber is clear with normal depth. The pupil shows pharmacological mydriasis.
This case report received ethical approval from the Ophthalmic Department of Bari University, Bari, Italy. Informed consent was obtained from this case report at the time of hospitalization.
DISCUSSION
Here, we have described a contact lens-related severe and sight-threatening keratitis caused by SA, which was successfully treated with combined surgical and medical therapies.
More than 70 species of fungi have been reported to cause mycotic keratitis; among these, Fusarium and Aspergillus are the most common. Furthermore, the presence of Candida spp. is related to contact lens wear and can contribute to filamentous keratitis or perforation [2, 11-14]. Characterization of the etiological agent of keratomycosis requires microbiological investigation; nevertheless, clinical history assessment and examination usually raise the suspicion of fungal involvement [15].
SA is a ubiquitous filamentous fungus that grows rapidly; however, definitive identification of SA requires at least 3–4 days of challenging identification. In vitro analyses of SA have shown that it has poor susceptibility to fluconazole and ketoconazole; however, it is susceptible to all other azoles, including VRCZ, miconazole, and albaconazole [9, 15]. Broad-spectrum ocular infections with a variable prognosis caused by SA have been reported in the literature [16- 35]; these infections involve the eyelids [19] up to the orbital apex [17]. It can affect both immunocompetent [19, 20, 23-26, 28, 30, 32] and immunocompromised [17, 18, 21, 22, 27, 29, 31, 33-35] hosts. Following previous studies on eye infections related to SA, it appears remarkable that most cases require penetrating keratoplasty to restore at least the anatomical structure of the eye [16, 20, 23, 26, 28, 30]. However, a few cases of SA-induced keratitis that were successfully treated with medical treatment alone have been reported [24, 29, 32, 33]. Even in an old immunodeficient patient with a severe ocular condition, such as endophthalmitis, early diagnosis, along with prompt and proper management, could result in a good prognosis [31].
The literature also indicates that the patients with SA-related eye infections are often over 60 years of age [18, 20-22, 25-28, 30, 31, 35]. The most severe cases involve a history of conditions that lead to immunodeficiency, allowing a faster and more destructive intraocular growth of SA [17, 21, 22, 27, 34, 35]. The pharmacological treatment of this infection includes mainly VRCZ, followed by amphotericin B, whereas surgical treatment involves penetrating keratoplasty or more aggressive techniques, such as enucleation/evisceration [16-35]. Table 1 summarizes the studies on patients’ demographics, treatment approaches, and the outcomes of ocular infections caused by SA.
Table 1.
Summary of case reports [16-19, 21-26, 28-35] or case series [20, 27] on Scedosporium apiospermum (SA) related ocular infections
| Author (Year of publication) | Characteristics of subjects | Main findings |
|---|---|---|
| Lenk et al. (2020) [ 16 ] | 44-year-old contact lens wearer. | Right eye keratitis; unsuccessful antimycotic treatment and corneal colla- gen crosslinking procedures necessitated keratoplasty. |
| Loh et al. (2018) [ 17 ] | 48-year-old male with DM. | Orbital apex syndrome subsequent to dental caries in the upper molars and pansinusitis, which were complicated with bilateral loss of vision. |
| Todokoro et al. (2018) [ 18 ] | 75-year-old immunocompromised male, re- ceived posterior subtenon triamcinolone ace- tonide injection to treat macular edema due to left eye branch retinal vein occlusion. | Infectious scleritis, successfully treated with topical and systemic VRCZ and repetitive surgical debridement. |
| Zoroquiain et al. (2017) [ 19 ] | 56-year-old healthy female. | Palpebral mycetoma treated with systemic VRCZ; resolved after 18 weeks. |
| Bui et al. 2016 [ 20 ] | Two female patients with SA induced exog- enous endophthalmitis. Case 1: 44-year-old healthy contact lens wearer, and case 2: 78-year- old with left eye advanced glaucoma, who had history of mitomycin C assisted trabeculecto- my. | Despite fulminant left eye involvement, both cases were managed with immediate surgical intervention, combined with intravitreal and systemic VRCZ postoperatively. Final BCVA was 20/20 in case 1, and hand motion in case 2. |
| Fernandez-Flores et al. (2016) [ 21 ] | 71-year-old immunocompromised male. | Left eye endophthalmitis with antecedent conjunctivitis, which evolved into phtisis bulbi, leading to globe removal. |
| Vanzzini-Zago et al. (2016) [ 22 ] | 69-year-old male with DM. | Blind painful right eye with endogenous endophthalmitis caused by Scedo- sporium boydii, which deteriorated despite medical treatment and resulted in enucleation. |
| Roy et al. (2016) [ 23 ] | 32-year-old healthy male with history of left eye trauma caused by plant matter. | Endophthalmitis secondary to keratomycosis, which was treated with com- bined keratoplasty, PPV, and intravitreal AB. Final vision was LP and the eye became phthisical. |
| Palanisamy et al. (2015) [ 24 ] | 30-year-old healthy female. | Left eye keratomycosis caused by the Graphium state of SA, successfully treated with topical natamycin, econazole, and itraconazole. |
| Jutley et al. (2015) [ 25 ] | 65-year-old immunocompetent female. | Right eye keratitis following phacoemulsification, successfully treated with systemic and topical VRCZ, topical natamycin, dexamethasone, and cyc- losporine. |
| Hayashi et al. (2014) [ 26 ] | 78-year-old healthy female. | Sclerokeratitis caused by SA and Aspergillus cibarius, treated with combined keratoplasty, systemic caspofungin/itraconazole, and both systemic and topical VRCZ. The final vision was the LP at the 7th month follow-up as the sclerokeratitis led to bullous keratopathy. |
| Moloney et al (2014) [ 27 ] | Four patients with an underlying malignancy (3 females, and 1 male, age range: 60‒78 years). | Scedosporium species detected in all patients; one was SA. All patients had endophthalmitis and received systemic VRCZ and topical antifungal treat- ment. Two patients underwent enucleation, one of them had SA-induced endophthalmitis, while the other two achieve a BCVA of LP and NLP. |
| Kepez Yildiz et al. (2014) [ 28 ] | 62-year-old immunocompetent female with right eye injury sustained during gardening. | Keratitis that required penetrating tectonic keratoplasty and lensectomy with continuation of anti-fungal therapy (topical VRCZ, vancomycin, cef- tazidime, and systemic VRCZ). Her final BCVA was 20/200 with aphakic correction. |
| Fadzillah et al. (2013) [ 29 ] | 47-year-old female with DM. | Left eye keratitis successfully treated with topical AB and VRCZ (BCVA: 20/30). |
| Kalkan Akçay et al. (2013) [ 30 ] | 61-year-old female with history of right eye foreign body trauma, with no known systemic disease or drug history. | Keratitis refractory to topical and systemic VRCZ along with topical nata- mycin; required keratoplasty but the patient refused. |
| Belenitsky et al. (2012) [ 31 ] | 83-year-old male with DM. | Right eye endophthalmitis treated with PPV and intravitreal VRCZ, with full recovery of vision (BCVA: 20/40). |
| Al-Badriyeh et al. (2009) [ 32 ] | 54-year-old immunocompetent female. | Right eye keratitis was treated with topical natamycin, but relapsed, and was then treated successfully with topical VRCZ (BCVA: 20/30). |
| Yoon et al. (2008) [ 33 ] | 54-year-old immunocompromised male. | Right eye SA-induced keratitis demonstrated by a molecular genetic meth- od and successfully treated with topical AB. |
| Jain et al. (2007) [ 34 ] | Three immunocompromised female patients with disseminated SA, left eye endogenous endophthalmitis, having ages of 59 years, 37 years, and 21 years (case 1, case 2, and case 3, respectively). | Case 1: eye deteriorated despite medical treatment and underwent limited exenteration, but the patient died 6 months later. Case 2: eye developed retinal detachment, which was treated with scleral buckling and PPV, but the patient died shortly thereafter. Case 3: received bilateral intravitreal in- jections of AB and PPV, followed by weekly intravitreal itraconazole, but no visual recovery was achieved, and she died shortly thereafter. |
| Chen et al. (2007) [ 35 ] | Two immunocompromised male patients (56 years and 62 years of age). | Left eye with endogenous endophthalmitis; treated with intravitreal and systemic VRCZ, but both patients underwent enucleation due to unrelent- ing ocular pain deterioration. |
Abbreviations: DM, diabetes mellitus; VRCZ, voriconazole; SA, Scedosporium apiospermum; BCVA, best corrected visual acuity; PPV, pars plana vitrectomy; AB, amphotericin B; LP, light perception; NLP, no light perception.
In our case, combined surgical and medical treatment with systemic and topical VRCZ, as well as oral itraconazole, induced complete remission. However, a pivotal therapeutic approach remains penetrating keratoplasty. Early detection of the pathogenic agent is critical for the optimal management of keratomycosis. However, in the absence of prompt microbiological assessments, surgery may be the only effective approach; yet, adjunctive antifungal therapy is essential.
A strength of this paper is that it describes a rare case of SA keratitis with a good anatomical outcome and functional recovery. Furthermore, it summarizes a broad spectrum of ocular infections caused by SA, with details of the treatment approach and management outcomes. However, it is limited by its nature, being a report of a single case, and a lack of molecular diagnostic methods, such as fungal polymerase chain reaction and sequencing. Another limitation of this work is the lack of a photographic document of the initial conditions of the patient, because the diagnosis of SA infection was delayed. Future studies with more cases and longer follow-up, along with assessment of various routes of administration and minimum inhibitory concentrations of VRCZ, and determination of the optimum route, dose, and duration of medical treatment in case of SA-induced keratomycosis, are required. Moreover, future studies using sophisticated laboratory evaluations, such as species- specific polymerase chain reaction and sequencing, will lead to the identification of elements that allow for an immediate differential diagnosis between SA and Aspergillus infections, and timely initiation of the appropriate antifungal treatment.
CONCLUSIONS
Rapid identification of the etiological agent is mandatory to ensure appropriate therapy in cases of keratomycosis. Surgery to remove the infected cornea is helpful in cases in which initial medical therapy fails. Topical and systemic antimycotic therapy, based on microbiological culture, is recommended as an adjunctive therapy for the surgical management of severe corneal abscess secondary to SA.
ETHICAL DECLARATIONS
Ethical approval:
This case report received ethical approval from the Ophthalmic Department of Bari University, Bari, Italy. Informed consent was obtained from the patient at the time of hospitalization.
Conflict on interests:
None.
FUNDING
None.
ACKNOWLEDGMENTS
We thank Ryan Chastain-Gross, Ph.D., from the Edanz Group (https://en-author-services.edanz.com/ac) for editing a draft of this manuscript, and Roberta Dima for helping in the collection of the data.
References
- 1.Keay L, Edwards K, Naduvilath T, Taylor HR, Snibson GR, Forde K, et al. Microbial keratitis predisposing factors and morbidity. Ophthalmology. 2006;113(1):109–16. doi: 10.1016/j.ophtha.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 2.ElMallah MK, Edward DP, McMahon TT. Filamentous fungal invasion of a methafilcon contact lens. Cornea. 2006;25(7):860–2. doi: 10.1097/01.ico.0000220772.04155.33. [DOI] [PubMed] [Google Scholar]
- 3.Tuli SS, Iyer SA, Driebe WT Jr. Fungal keratitis and contact lenses: an old enemy unrecognized or a new nemesis on the block? Eye Contact Lens. 2007;33(6 Pt 2):415–7; discussion 424-5. doi: 10.1097/ICL.0b013e318157e999. [DOI] [PubMed] [Google Scholar]
- 4.Klotz SA, Penn CC, Negvesky GJ, Butrus SI. Fungal and parasitic infections of the eye. Clin Microbiol Rev. 2000;13(4):662–85. doi: 10.1128/cmr.13.4.662-685.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cortez KJ, Roilides E, Quiroz-Telles F, Meletiadis J, Antachopoulos C, Knudsen T, et al. Infections caused by Scedosporium spp. Clin Microbiol Rev. 2008;21(1):157–97. doi: 10.1128/CMR.00039-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rynga D, Capoor MR, Varshney S, Naik M, Gupta V. Scedosporium apiospermum, an emerging pathogen in India: Case series and review of literature. Indian J Pathol Microbiol. 2017;60(4):550–555. doi: 10.4103/IJPM.IJPM_742_16. [DOI] [PubMed] [Google Scholar]
- 7.Diaz-Valle D, Benitez del Castillo JM, Amor E, Toledano N, Carretero MM, Diaz-Valle T. Severe keratomycosis secondary to Scedospo- rium apiospermum. Cornea. 2002;21(5):516–8. doi: 10.1097/00003226-200207000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Nulens E, Eggink C, Rijs AJ, Wesseling P, Verweij PE. Keratitis caused by Scedosporium apiospermum successfully treated with a cornea transplant and voriconazole. J Clin Microbiol. 2003;41(5):2261–4. doi: 10.1128/JCM.41.5.2261-2264.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steinbach WJ, Perfect JR. Scedosporium species infections and treatments. J Chemother. 2003;15 Suppl 2:16–27. doi: 10.1179/joc.2003.15.Supplement-2.16. [DOI] [PubMed] [Google Scholar]
- 10.Ramakrishnan S, Mandlik K, Sathe TS, Gubert J, Krishnan T, Baskaran P. Ocular infections caused by Scedosporium apiospermum: A case series. Indian J Ophthalmol. 2018;66(1):137–140. doi: 10.4103/ijo.IJO_524_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stapleton F, Carnt N. Contact lens-related microbial keratitis: how have epidemiology and genetics helped us with pathogenesis and prophylaxis. Eye (Lond). 2012;26(2):185–93. doi: 10.1038/eye.2011.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mahmoudi S, Masoomi A, Ahmadikia K, Tabatabaei SA, Soleimani M, Rezaie S, et al. Fungal keratitis: An overview of clinical and laboratory aspects. Mycoses. 2018;61(12):916–930. doi: 10.1111/myc.12822. [DOI] [PubMed] [Google Scholar]
- 13.Slowik M, Biernat MM, Urbaniak-Kujda D, Kapelko-Slowik K, Misiuk-Hojlo M. Mycotic Infections of the Eye. Adv Clin Exp Med. 2015;24(6):1113–7. doi: 10.17219/acem/50572. [DOI] [PubMed] [Google Scholar]
- 14.Thomas PA. Current perspectives on ophthalmic mycoses. Clin Microbiol Rev. 2003;16(4):730–97. doi: 10.1128/CMR.16.4.730-797.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mancini N, Ossi CM, Perotti M, Carletti S, Gianni C, Paganoni G, et al. Direct sequencing of Scedosporium apiospermum DNA in the diagnosis of a case of keratitis. J Med Microbiol. 2005;54(Pt 9):897–900. doi: 10.1099/jmm.0.46029-0. [DOI] [PubMed] [Google Scholar]
- 16.Lenk J, Raiskup F, Pillunat LE, Rossler S. [Scedosporium apiospermum-a rare pathogen of keratomycosis] Ophthalmologe. 2020;117(12):1225–1228. doi: 10.1007/s00347-020-01073-x. [DOI] [PubMed] [Google Scholar]
- 17.Loh UL, Tai PY, Hussein A, A Qamarruddin F. Scedosporium apiospermum: A Rare Cause of Aggressive Orbital Apex Syndrome. Cureus. 2018;10(12):e3743. doi: 10.7759/cureus.3743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Todokoro D, Hoshino J, Yo A, Makimura K, Hirato J, Akiyama H. Scedosporium apiospermum infectious scleritis following posterior subtenon triamcinolone acetonide injection: a case report and literature review. BMC Ophthalmol. 2018;18(1):40. doi: 10.1186/ s12886. doi: 10.1186/s12886-018-0707-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zoroquiain P, Alghamdi S, Arthurs B, Levin L, Sheppard DC, Ralph B, et al. Eyelid Mycetoma Masquerading as Sebaceous Carcinoma. Ophthalmic Plast Reconstr Surg. 2017;33(3S Suppl 1):S101–S104. doi: 10.1097/IOP.0000000000000657. [DOI] [PubMed] [Google Scholar]
- 20.Bui DK, Carvounis PE. Favorable Outcomes of Filamentous Fungal Endophthalmitis Following Aggressive Management. J Ocul Phar- macol Ther. 2016;32(9):623–630. doi: 10.1089/jop.2016.0055. [DOI] [PubMed] [Google Scholar]
- 21.Fernandez-Flores A, Lopez-Medrano R, Fuster-Foz C. Histopathological clues in the diagnosis of fungal infection by Scedosporium in a case of endophthalmitis starting as conjunctivitis. J Cutan Pathol. 2016;43(5):461–7. doi: 10.1111/cup.12689. [DOI] [PubMed] [Google Scholar]
- 22.Vanzzini-Zago V, Corredor-Casas S, Rodriguez-Reyes A, Hernandez-Hernandez F, Manzano-Gayosso P, Martinez RL, et al. Endoph- thalmitis of probable endogenous origin caused by Scedosporium boydii: A case report. Rev Iberoam Micol. 2016;33(2):122–5. doi: 10.1016/j.riam.2015.07.006. [DOI] [PubMed] [Google Scholar]
- 23.Roy R, Panigrahi PK, Pal SS, Mukherjee A, Bhargava M. Post-traumatic Endophthalmitis Secondary to Keratomycosis Caused by Scedosporium apiospermum. Ocul Immunol Inflamm. 2016;24(1):107–9. doi: 10.3109/09273948.2014.902078. [DOI] [PubMed] [Google Scholar]
- 24.Palanisamy M, Venkatapathy N, Rajendran V, Shobana CS. Keratomycosis Caused By Graphium eumorphum (Graphium State of Scedosporium apiospermum) J Clin Diagn Res. 2015;9(4):DD03–4. doi: 10.7860/JCDR/2015/12089.5802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jutley G, Koukkoulli A, Forbes J, Sharma V. Unusual case of Scedosporium apiospermum keratitis following phacoemulsification in a systemically well patient. J Cataract Refract Surg. 2015;41(1):230–3. doi: 10.1016/j.jcrs.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 26.Hayashi Y, Eguchi H, Toibana T, Mitamura Y, Yaguchi T. Polymicrobial sclerokeratitis caused by Scedosporium apiospermum and Aspergillus cibarius. Cornea. 2014;33(8):875–7. doi: 10.1097/ICO.0000000000000172. [DOI] [PubMed] [Google Scholar]
- 27.Moloney TP, Park J. Pseudallescheria endophthalmitis: four cases over 15 years in Queensland, Australia, and a review of the literature. Retina. 2014;34(8):1683–701. doi: 10.1097/IAE.0000000000000126. [DOI] [PubMed] [Google Scholar]
- 28.Kepez Yildiz B, Hasanreisoglu M, Aktas Z, Aksu G, Kocak BC, Akata F. Fungal keratitis secondary to Scedosporium apiospermum infection and successful treatment with surgical and medical intervention. Int Ophthalmol. 2014;34(2):305–8. doi: 10.1007/s10792-013-9777-8. [DOI] [PubMed] [Google Scholar]
- 29.Fadzillah MT, Ishak SR, Ibrahim M. Refractory Scedosporium apiospermum Keratitis Successfully Treated with Combination of Amphotericin B and Voriconazole. Case Rep Ophthalmol Med. 2013;2013:413953. doi: 10.1155/2013/413953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalkan Akcay E, Acikgoz ZC, Can ME, Celikbilek N, Dereli Can G, Cagil N. [Fungal keratitis caused by Scedosporium apiospermum: first report from Turkey] Mikrobiyol Bul. 2013;47(4):727–33. doi: 10.5578/mb.5262. [DOI] [PubMed] [Google Scholar]
- 31.Belenitsky MP, Liu C, Tsui I. Scedosporium apiospermum endopthalmitis treated early with intravitreous voriconazole results in recov- ery of vision. J Ophthalmic Inflamm Infect. 2012;2(3):157–60. doi: 10.1007/s12348-012-0063-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Badriyeh D, Leung L, Davies GE, Stewart K, Kong D. Successful salvage treatment of Scedosporium apiospermum keratitis with topical voriconazole after failure of natamycin. Ann Pharmacother. 2009;43(6):1139–42. doi: 10.1345/aph.1M008. [DOI] [PubMed] [Google Scholar]
- 33.Yoon S, Kim S, Lee KA, Kim H. [A case of Scedosporium apiospermum keratitis confirmed by a molecular genetic method] Korean J Lab Med. 2008;28(4):307–11. doi: 10.3343/kjlm.2008.28.4.307. [DOI] [PubMed] [Google Scholar]
- 34.Jain A, Egbert P, McCulley TJ, Blumenkranz MS, Moshfeghi DM. Endogenous Scedosporium apiospermum endophthalmitis. Arch Ophthalmol. 2007;125(9):1286–9. doi: 10.1001/archopht.125.9.1286. [DOI] [PubMed] [Google Scholar]
- 35.Chen FK, Chen SD, Tay-Kearney ML. Intravitreal voriconazole for the treatment of endogenous endophthalmitis caused by Scedospo- rium apiospermum. Clin Exp Ophthalmol. 2007;35(4):382–5. doi: 10.1111/j.1442-9071.2007.01493.x. [DOI] [PubMed] [Google Scholar]