Abstract
Platelet transfusions (PTx) are the principal approach for treating neonatal thrombocytopenia, a common hematological abnormality affecting neonates, particularly preterm infants. However, evidence about the outcomes associated with PTx and whether they provide clinical benefit or harm is lacking. The aim of this systematic review and meta-analysis is to assess the association between PTx in preterm infants and mortality, major bleeding, sepsis, and necrotizing enterocolitis (NEC) in comparison to not transfusing or using different platelet count thresholds for transfusion. A broad electronic search in three databases was performed in December 2022. We included randomized controlled trials, and cohort and case control studies of preterm infants with thrombocytopenia that (i) compared treatment with platelet transfusion vs. no platelet transfusion, (ii) assessed the platelet count threshold for PTx, or (iii) compared single to multiple PTx. We conducted a meta-analysis to assess the association between PTx and mortality, intraventricular hemorrhage (IVH), sepsis, and NEC and, in the presence of substantial heterogeneity, leave-one-out sensitivity analysis was performed. We screened 625 abstracts and 50 full texts and identified 18 reports of 13 eligible studies. The qualitative analysis of the included studies revealed controversial results as several studies showed an association between PTx in preterm infants and a higher risk of mortality, major bleeding, sepsis, and NEC, while others did not present a significant relationship. The meta-analysis results suggest a significant association between PTx and mortality (RR 2.4, 95% CI 1.8–3.4; p < 0.0001), as well as sepsis (RR 4.5, 95% CI 3.7–5.6; p < 0.0001), after a leave-one-out sensitivity analysis. There was also found a significant correlation between PTx and NEC (RR 5.2, 95% CI 3.3–8.3; p < 0.0001). As we were not able to reduce heterogeneity in the assessment of the relationship between PTx and IVH, no conclusion could be taken.
Conclusion: Platelet transfusions in preterm infants are associated to a higher risk of death, sepsis, and NEC and, possibly, to a higher incidence of IVH. Further studies are needed to confirm these associations, namely between PTx and IVH, and to define the threshold from which PTx should be given with less harm effect.
|
What is Known: • Platelet transfusions are given to preterm infants with thrombocytopenia either to treat bleeding or to prevent hemorrhage. • Lack of consensual criteria for transfusion. | |
|
What is New: • A significant association between platelet transfusions and mortality, sepsis, and NEC. |
Supplementary Information
The online version contains supplementary material available at 10.1007/s00431-023-05031-y.
Keywords: Platelets, Transfusions, Preterm, Death, Sepsis, Necrotizing enterocolitis
Introduction
Thrombocytopenia is a hematological abnormality commonly found in newborns, characterized by a platelet count (PC) inferior to 150 × 109/L. This condition mainly affects preterm infants and critically ill neonates and it occurs due to decreased platelet production or increased consumption, or both [1]. Some common causes include fetal growth restriction (FGR), sepsis, and necrotizing enterocolitis (NEC) [1, 2]. Thrombocytopenia has been identified as a risk factor for frequent complications of prematurity, such as intraventricular hemorrhage (IVH), despite its correlation with bleeding still being uncertain [3, 4].
Platelet transfusions (PTx) remain the principal approach for treating neonatal thrombocytopenia. They are administered, generally, in two situations: to treat thrombocytopenic hemorrhage or prophylactically to prevent hemorrhage, the latter corresponding to the biggest proportion of transfusions [5, 6]. Prophylactic platelet transfusions are given to many infants even in the absence of bleeding, once their platelet counts fall below a certain threshold, aiming to prevent major hemorrhage [7, 8]. However, there is currently no consensus on the specific platelet count threshold that indicates a transfusion for a newborn [3]. These decisions are often based on physicians’ preferences, expert advice, or consensus-driven recommendations [9], and there is a lack of strong and consensual scientific evidence about whether platelet transfusions provide clinical benefit or harm to preterm infants with thrombocytopenia. Indeed, the relationship between platelet count and bleeding risk is complex in preterm infants, and the role of platelet transfusions in reducing bleeding risk is unclear [10].
This systematic review and meta-analysis aims to evaluate the risks and benefits of PTx in preterm infants compared to not transfusing or using different platelet count thresholds for transfusion. The primary outcomes in study are mortality and major bleeding (including IVH and other hemorrhage) and the secondary outcomes include sepsis and NEC.
Methods
Study design
We performed this systematic review and meta-analysis according to the Cochrane Handbook [11] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [12].
Eligibility criteria
We included randomized controlled trials (RCT), cohort studies, and case control studies of preterm infants with thrombocytopenia that (i) compared treatment with platelet transfusion versus no platelet transfusion, (ii) assessed the platelet count threshold for PTx, or (iii) compared single to multiple PTx. We defined preterm neonates as those born before 37 weeks of gestation, and neonatal thrombocytopenia as platelet count below 150 × 109/L, diagnosed during the first 28 days of life. Studies that involved both term and preterm infants were included if preterm infants represented at least 75% of the sample or if it was possible to extract separate results for preterm newborns. We considered the following outcomes: mortality of the infant or bleeding episodes post-PTx (including any grade of IVH or other hemorrhage), as primary outcomes; and morbidity, including sepsis (clinical or identified agent in hemoculture) and any stage of NEC, as secondary outcomes.
Studies including infants with congenital malformations, chromosomal anomalies, or treated with extracorporeal membrane oxygenation (ECMO) were excluded. Studies in which transfusion was not restricted to platelets were also excluded.
Search strategy
We performed a broad electronic search in three databases, namely MedLine (via Ovid), ISI Web of Science, and Scopus, to identify relevant original articles published up to December 15, 2022, without language or date restrictions. The details of the search strategy are provided in Supplementary Information 1 (Suppl1).
Selection process
The search results were exported to the reference management software EndNote X7, where duplicate articles were removed. The remaining articles were then uploaded to Rayyan, a web tool used for systematic reviews, and any lasting duplicates were excluded.
Two reviewers independently screened the articles initially by titles and abstracts and disagreements were resolved by consensus. The full-text versions of the articles that passed the initial screening were retrieved and assessed for eligibility by the same two reviewers, independently. Any disagreements were resolved by consensus and, if necessary, a third reviewer was consulted for discussion.
Data extraction and critical appraisal of individual studies
Data extraction was accomplished by two researchers using a purposely built Excel form. The following information was extracted from each study: author, year of publication, study design; number of preterm newborns, gender, gestational age, and birth weight of the total sample and in each group; available data about the intervention (total and mean number of transfusions, threshold, and PTx criteria per group); and the incidence of the outcomes: mortality, IVH, other bleeding events, sepsis, and NEC. Two tables were created based on the study objectives: one for studies that compared receiving vs. not receiving PTx and another for studies comparing different thresholds of transfusion or single with multiple PTx.
To assess the quality of the studies and the potential sources of bias, we used the Cochrane risk-of-bias tool, version 2 [11], for randomized controlled trials and the Newcastle–Ottawa Scale (NOS) for observational studies. The 9-point NOS is divided into three main categories: selection, comparability, and exposure [13]. Studies that scored a total of 7–9 stars were considered of “good quality,” 4–6 of “fair quality,” and 0–3 of “poor quality.”
Data synthesis
We conducted meta-analysis assessing the association between PTx and mortality, IVH, sepsis, and NEC based on relative risks (RR) retrieved or calculated from included primary studies. We used a random-effects model weighting for the restricted maximum likelihood approach to estimate the pooled RRs. In each meta-analysis, only primary studies with the same design were included (i.e., we did not include observational and experimental studies in the same analysis). Inter-study heterogeneity was assessed using the I2 statistic and the Cochran Q statistic. An I2 > 50% and a Cochran Q statistic p value less than 0.1 were considered to represent substantial heterogeneity and, in the presence of substantial heterogeneity, leave-one-out sensitivity analysis was conducted. Data analysis was performed using software R (version 4.0), with use of meta package.
Results
Study selection
Our search returned a total of 1100 articles. After removing duplicates, 625 reports were screened by title and abstract, leading to the exclusion of 573 articles. The remaining 50 full-text articles retrieved were thoroughly analyzed for eligibility, and 18 reports from 13 studies met the inclusion criteria and were ultimately included in this review. Suppl2 illustrates the screening and selection process.
Overview of the included studies
Our review includes 10 reports [14–23] from 8 studies that assessed the effects of PTx in preterm infants, comparing transfused infants vs. non-transfused infants. The characteristics of each study (population and interventions) are presented in Suppl3, and the corresponding outcomes are listed in Table 1. We included 5 additional reports [24–28] from 3 studies that compared different transfusion thresholds and 3 reports [29–31] from 2 studies comparing single vs. multiple transfusions. Table 2 provides demographic and intervention information for each study, while Table 3 outlines the assessed outcomes. A total of 7 reports from the 3 RCT conducted on this topic were included [14–16, 25–28].
Table 1.
Outcomes studied and comparison between transfused and non-transfused groups
| Author, year | N | n |
Mortality n (%) |
IVH n (%) |
Other hemorrhage n (%) |
Sepsis n (%) |
NEC n (%) |
Findings | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| G1 | G2 | G1 | G2 | G1 | G2 | G1 | G2 | G1 | G2 | G1 | G2 | |||
|
Andrew |
152 | 78 | 74 | 16(20.5) | 11(14.9) | - | - |
22(28.2) a |
19(25.7) a | - | - |
3 (3.8) |
1 (1.4) |
No association between PTx and intracranial hemorrhage (p = 0.73) |
| Christensen 2006 [17] | 283 | 129 | 154 | 29(22.5) | 18(11.7) | - | - | - | - | - | - | - | - | Significant association between PTx and mortality rate (p < 0.01) |
| Baer 2007 [18] | 1600 | 494 | 1106 | 81(16.4) | 22(2.0) | 99(20.0)b | 44(4.0b | - | - | 143(28.9) | 77(7.0) | 54(10.9) | 22(2.0) |
Significant association between PTx and mortality and greater increase with a higher number of transfusions (p < 0.001) Significant association between PTx and IVH (p < 0.001) |
| Bonifacio 2007 [19] | 82 | 60 | 22 | 29(48.3) | 4(18.2) | 37(61.7) | 7(31.8) | - | - | 34(56.7) | 10(45.5) | - | - | No association between PTx and mortality, IVH, or sepsis |
|
Sparger 2016 [20] |
972 | 212c | 190c | - | - | 97(45.8)c |
39 (20.5)c |
42 (19.8)c,d |
6 (3.2)c,d |
- | - | - | - |
Significant association between PTx and IVH (p = 0.005) and other bleeding (p < 0.001) After adjusting for relevant variables, no significant association between PTx and IVH |
| Alhamad 2022 [21] | 154 | 77 | 77 | 30(39.0) | 15(19.5) | 59(76.6) | 71(92.2) | - | - | - | - |
1 (1.3) |
0 (0.0) |
No association between PTx frequency and threshold and mortality rate |
| Chen 2002 [22] | 1221 | 94 | 1127 | 18(19.1) |
62 (5.5) |
50(53.2) | 213(18.9) | - | - | 16(17.0) |
35 (3.1) |
1 (1.1) |
5 (0.4) |
Significant association between PTx and mortality (HR 1.48; 95%CI 1.13–1.93; p = .004) No association between PT and IVH |
| Raja 2022 [23] | 540 | 105 | 435 | - | - | 14(13.3)b |
7 (1.6) b |
- | - | - | - | - | - | Significant association between PTx and all grades of IVH (OR: 4.3, 95% CI: 2.3–8.2) and severe IVH (OR: 41, 95% CI: 14.0–146.6) |
n number of infants, IVH Intraventricular Hemorrhage, NEC Necrotizing Enterocolitis, G1 Group 1—received platelet transfusion, G2 Group 2—did not receive platelet transfusion PTx Platelet Transfusion, HR Hazard Ratio, CI Confidence Interval, OR Odds Ratio -, outcomes not studied
aIntracranial hemorrhage
bOnly grade 3 or 4 IVH
cNumber in patient-days, during the first 7 days of life with a platelet count < 100 × 109/L, in whom the outcomes were studied. Absolute numbers of patients in each group: Group 1, 231; Group 2, 741
dPulmonary, gastrointestinal, genitourinary, wound, or other hemorrhage (not including IVH)
Table 2.
Demographic and intervention data in studies comparing preterm infants who received platelet transfusions from different platelet count thresholds or different numbers of platelet transfusions
| Author, year | Study design | N | Group description | n |
Male n (%) |
Gestational age, weeks (mean ± SD) |
Birth weight, grams (mean ± SD) |
Intervention details |
|---|---|---|---|---|---|---|---|---|
|
Garcia |
Retrospective cohort | 61 | G1: Received more than 1 PTx | 54 | 37 (68.5) | 32.6 ± 3.7 | 1720 ± 752 |
Criteria for PTx: 1. PC < 20 × 109/L 2. PC < 50 × 109/L with active bleeding |
| G2: Received only 1 PTx | 7 | 6 (85.7) | 33.6 ± 6.2 | 1675 ± 1052 | ||||
| Del Vecchio 2001 [31] | Retrospective cohort | 114 | G1: Received more than 1 PTx | 59 | 29 (49.2) | 30.1 ± 5.8 | 1408 ± 990 | Total number of transfusions: 371 |
| G2: Received only 1 PTx | 55 | 21 (38.2) | 30.8 ± 5.2 | 1568 ± 943 | ||||
| von Lindern 2012 [24] | Retrospective cohort | 679 | G1: Liberal transfusion group | 326 | 172 (52.8) | 28.9 ± 1.9 | 1259 ± 326 |
Criteria for PTx: 1. PC < 30 × 109/L in clinically stable infants 2. PC < 50 × 109/L in unstable infants, before planned surgery, or both 3. < 100 × 109/L in cases of active bleeding, at the start of an exchange transfusion or both Mean number of transfusions ± SD: 1.1 ± 3.0 |
| G2: Restrictive transfusion group | 353 | 195 (55.2) | 28.9 ± 1.9 | 1270 ± 353 |
Criteria for PTx: PC < 50 × 109/L in the presence of: - Major bleeding, massive petechiae, and bruising - Need for surgery, invasive procedures, or indomethacin treatment for PDA Prophylactic PTx not given if infants had severe thrombocytopenia but no clinical signs of bleeding Mean number of transfusions ± SD: 0.2 ± 0.7 |
|||
|
Curley |
RCT | 660 | G1: Liberal transfusion group | 329 | 205 (62.3) | 26.6 (24.9–28.9) a | 728 (600–940) a |
PTx given at PC thresholds of 50 × 109/L 90% of the infants (296) received at least 1 PTx |
| G2: Restrictive transfusion group | 331 | 191 (57.7) | 26.7 (24.9–28.7) a | 743 (605–990) a |
PTx given at PC thresholds of 25 × 109/L 53% of the infants (177) received at least 1 PTx |
|||
|
Kumar 2019 [28] |
RCT | 44 | G1: Liberal transfusion group | 22 | 11 (50.0) | 29.3 ± 2.4 | 1075 ± 308 |
Infants received PTx to maintain PC > 100 × 109/L until one of the following: 1. PDA closed 2. 120 h after randomization |
| G2: Restrictive transfusion group | 22 | 13 (59.1) | 30.0 ± 2.0 | 1149 ± 303 |
Standard criteria for transfusion: 1. PC < 20 × 109/L 2. Clinical bleed 3. PC < 50 × 109/L + requiring a major non-neurosurgical procedure 4. PC < 100 × 109/L + requiring a neurosurgical procedure |
N Total number of infants in the study, n number of infants per group, SD Standard Deviation, G1 Group 1, G2 Group 2, RCT Randomized Controlled Trial, PTx Platelet Transfusion, PC Platelet Count, PDA Patent Ductus Arteriosus
aMedian (interquartile range)
Table 3.
Outcomes studied and comparison between groups who received platelet transfusions from different platelet count thresholds or different numbers of platelet transfusions
| Author, year | N | n |
Mortality n (%) |
IVH n (%) |
Other hemorrhage n (%) |
Sepsis n (%) |
NEC n (%) |
Findings | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| G1 | G2 | G1 | G2 | G1 | G2 | G1 | G2 | G1 | G2 | G1 | G2 | |||
|
Garcia 2001 |
61 | 54 | 7 | 12 (22.2) | 3 (42.9) | 21 (38.9) |
4 (57.1) |
- | - | 24 (44.4) |
4 (57.1) |
10 (18.5) |
0 (0.0) |
No association between the increasing number of PTx given and mortality |
| Del Vecchio 2001 [31] | 114 | 59 | 55 | † | † | - | - | - | - | - | - | - | - | Significant increase in mortality rate in infants who received > 4 PTx vs. those who received 1 PTx (RR 2.9; p < 0.0001). Significant increase in infants who received 1 PTx vs. all the other infants in the NICU who did not receive any (RR 10.4; p < 0.0001) |
| von Lindern 2012 [24] | 679 | 326 | 353 | 22 (6.7) | 25 (7.1) | 63 (19.5) a | 75 (22.7) a | - | - | 98 (30.1) | 89(25.2) | 9(2.8) | 14(4.0) | No significant difference in the incidence of IVH between liberal and restrictive transfusion groups (p = 0.31) |
|
Curley 2019 |
660 | 329b | 331b |
G1: 85(26.2)c G2: 61 (18.5)c |
181(55.9) | 175(53.7)d | 42(13.0) | 54 (16.6)d |
Significant increase in mortality and major bleeding in preterm infants in the liberal transfusion group vs. restrictive group (OR 1.57; 95%CI 1.06 -2.32; p = 0.02) No significant differences in sepsis and NEC between groups |
|||||
| Kumar 2019 [28] | 44 | 22 | 22 | 8 (36.4) |
9 (40.9) |
9 (40.9) |
2 (9.1) |
- | - |
8 (36.3) |
2 (9.1) |
- | - |
Significant association between liberal transfusion and any grade of IVH vs. restrictive transfusion (p = 0.034) No significant differences between liberal and restrictive transfusion groups in grade III or IV IVH or mortality |
n number of infants, IVH Intraventricular Hemorrhage, NEC Necrotizing Enterocolitis, G1 Group 1, G2 Group 2, PTx Platelet Transfusion, RR relative Risk, NICU Neonatal Intensive Care Unit, OR, Odds Ratio, CI Confidence Interval, -, outcomes not studied, † outcome studied but unavailable number and percentage of infants who developed the outcome
aPercentage calculated for a total number of infants who had a cranial ultrasound scan: 323 infants in group 1 and 330 in group 2
b5 infants in group 1 and 2 infants in group 2 did not have primary outcomes reported and were excluded in the phase of outcomes analysis due to palliative care (3); randomization error (2); and issues with consenting process (2): Group 1, 324; Group 2, 329
cDeath and major bleeding were accessed together, as the primary outcome of the study
dPercentage calculated for a total number of 326 infants in group 2
To perform the meta-analyses, only studies comparing PTx vs. non-transfusion were included [17–19, 21, 22]. Some studies comparing transfused vs. non-transfused infants were not included in the meta-analyses: Andrew et al. [14–16] for being the sole RCT; Sparger et al. [20] because outcome values were presented in patient-days; Raja et al. [23] and Del Vecchio et al. [31] due to the unavailability of number and percentage of infants with outcome events. In addition, studies assessing liberal vs. restrictive transfusion or different number of PTx were excluded due to methodological heterogeneity.
No studies assessing the association between PTx and retinopathy of prematurity (ROP), patent ductus arteriosus (PDA), or bronchopulmonary dysplasia (BPD) met the inclusion criteria or had extractable data.
Risk of bias assessment
The three RCT included in the analysis were evaluated for bias risk and the two most recent trials [25–28] showed a low risk, while that of Andrews et al. [14–16] was found to have some potential risk of bias, due to deviations from the intervention in the control group, in case of major bleeding or platelet count below 50 × 109/L.
Concerning the ten observational studies included, seven [18–22, 24, 31] scored 7 stars or higher, being classified as “good quality,” while three [17, 23, 29, 30] scored 4 to 6 stars and were categorized as “fair quality.”
Detailed assessments of the risk of bias within each study are presented in Supplementary Information: Suppl4 for RCT and Suppl5 for observational studies.
Mortality
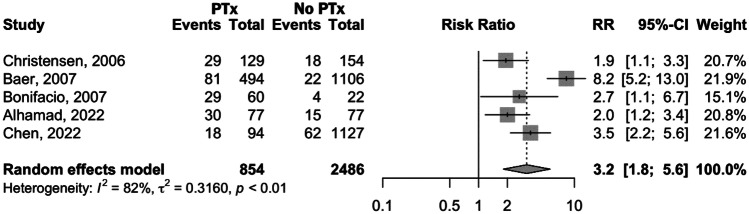
Among the studies that compared preterm infants who received PTx with those who did not, five [17–19, 21, 22] assessed the relationship between receiving PTx and mortality. Three studies [17, 18, 22] found a significant increase in mortality rate in the transfused group in comparison to the non-transfused one. In contrast, two studies [19, 21] did not find a significant association between PTx and mortality, even though the mortality rate was higher among patients who received PTx. The forest plot in Fig. 1 illustrates the comparison between transfused and non-transfused groups. The results show a significantly higher mortality in the PTx group [relative risk (RR) 3.2, 95% confidence interval (CI) 1.8–5.6; p < 0.0001] than in the non-transfused group. Significant heterogeneity was present across the studies (I2 = 82%, p < 0.01), so a leave-one-out sensitivity analysis was conducted to identify potential sources of heterogeneity in the quantitative analysis. Regardless of which study is removed, there is always a significantly higher risk of death in the transfused group (Suppl6). Heterogeneity decreases substantially to 12% when Baer et al. [18] is removed, indicating that this study is the primary source of heterogeneity. Upon omitting this study, the risk of death is 2.4 times higher in the transfused group vs. the non-transfused one (95% CI 1.8–3.4; p < 0.0001).
Fig. 1.
Forest plot comparing mortality in preterm infants who received platelet transfusions and those who did not receive platelet transfusions
Regarding the evaluation of different transfusion thresholds, PlaNeT-2 Trial [25–27] found a significant increase in mortality and major bleeding in the liberal transfusion group when compared to the restrictive approach. Likewise, Del Vecchio et al. [31] reported that the risk of death was significantly higher in patients who receive more than four transfusions vs. those who receive solely one or no PTx. Kumar et al. [28], however, did not observe a higher mortality rate in the liberal PTx group vs. the restrictive one. Garcia et al. [29; 30] also did not identify an association between giving multiple PTx to preterm infants and a higher mortality rate in comparison to solely one platelet transfusion.
Intraventricular hemorrhage and other bleeding events
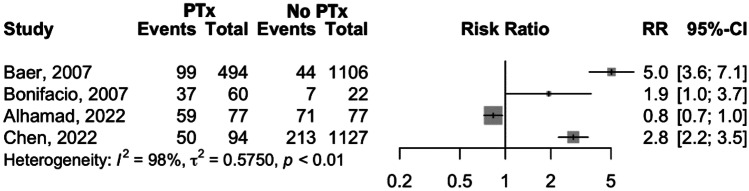
The influence of PTx in the occurrence of new-onset IVH was studied in five articles [18–20, 22, 23] that compared the outcome in transfused and non-transfused infants. While two studies [19, 22] did not find a significant correlation between PTx and IVH, Baer et al. [18] observed a significant increase of IVH events in transfused newborns. Similarly, Sparger et al. [20] found a significant association, not only for IVH but also for other bleeding events; however, after two multivariable regression models, the relationship weakened and was no longer significant. In contrast, even after adjusting for possible confounders, in Raja et al. [23], PTx were found to be a significant predictor of severe IVH (p < 0.001), with odds ratio (OR) of 4.3 for developing any grade of IVH (95% CI: 2.3–8.2) and 41 for grade III or IV (95% CI 14.0–146.6). Andrew et al. [14–16] evaluated the incidence of intracranial hemorrhage (ICH) and did not find a correlation between PTx and ICH. Quantitative assessment for IVH is shown in Fig. 2 and because of the high degree of heterogeneity observed (I2 = 98%, p < 0.01), which was not resolved by leave-one-out sensitivity analysis, the meta-analytical effect measure is not presented.
Fig. 2.
Forest plot comparing IVH incidence in preterm infants who received platelet transfusions and those who did not receive platelet transfusions
In relation to liberal vs. restrictive transfusion, the two RCT [25–28] reported a significantly higher incidence of IVH in the liberal transfusion group but von Linder et al. [24] did not observe differences between groups.
Morbidity: sepsis and necrotizing enterocolitis
None of the studies included in this systematic review had the primary objective of assessing the effects of PTx on sepsis, NEC, or other newborn diseases besides bleeding. Although several studies provide data on the association between PTx and sepsis, only Bonifacio et al. [19] and Curley et al. [25–27] performed statistical analyses, reporting a non-significant correlation between PTx and sepsis, and liberal transfusion and sepsis, respectively. With regard to NEC, Curley et al. [25–27] also did not observe a significant relationship.
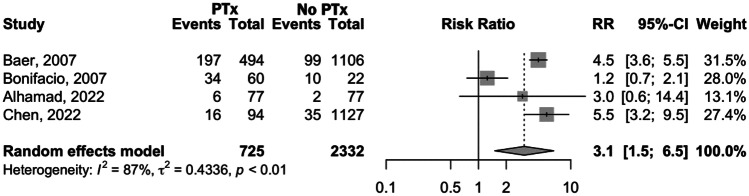
Despite that, we conducted a meta-analysis for both outcomes using data present in several studies [18, 19, 21, 22]. The forest plot for sepsis in presented in Fig. 3 that shows a significantly higher incidence in PTx-receiving group than in the non-transfused group [RR 3.1, 95% CI 1.5–6.5; p < 0.0001]. Due to significant heterogeneity across the studies (I2 = 87%, p < 0.01), a leave-one-out sensitivity analysis was conducted (Suppl7) and, when omitting Bonifacio et al. [19], heterogeneity was no longer present and a significant association between PTx and sepsis remained (RR 4.5, 95% CI 3.7–5.6; p < 0.0001).
Fig. 3.
Forest plot comparing sepsis incidence in preterm infants who received platelet transfusions and those who did not receive platelet transfusions
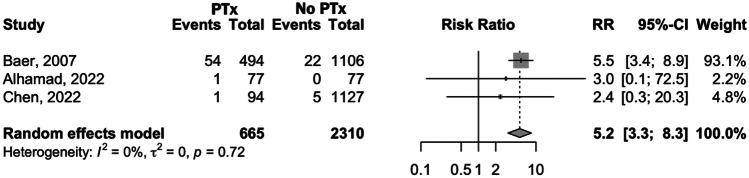
The forest plot for NEC, illustrated in Fig. 4, shows that the risk of developing NEC in the PTx group was significantly higher than in the non-transfused group (RR 5.2, 95% CI 3.3–8.3; p < 0.0001), with no heterogeneity detected (I2 = 0%; p = 0.72).
Fig. 4.
Forest plot comparing NEC incidence in preterm infants who received platelet transfusions and those who did not receive platelet transfusions
Discussion
The qualitative analysis of the studies included in this systematic review has revealed the controversial nature of the topic and the lack of consistent evidence about the effects of PTx in preterm infants. In fact, several studies have shown an association between PTx in thrombocytopenic preterm infants and a higher risk of mortality, major bleeding, sepsis, and NEC, while others did not show a significant relationship. The same happens with studies assessing different thresholds (i.e., the deleterious effect of transfusion at higher thresholds). These discrepancies may be partly attributed to methodological differences across the studies (e.g., demographic characteristics, interventions applied, and measured outcomes). These methodological disparities pose challenges when comparing the studies and drawing definitive conclusions.
Our meta-analysis aimed to assess the potential relationships between PTx and the outcomes in study. Despite the presence of high heterogeneity, significant risk-associations were found between PTx and adverse outcomes. A leave-one-out sensitivity analyses for mortality and sepsis outcomes allowed for decreased heterogeneity. Motives of such heterogeneity are already mentioned above. Based on these results, PTx in preterm infants are associated to increased risk of mortality, sepsis, and NEC. Evidence regarding the association between PTx and IVH is too heterogeneous and a meta-analysis could not be conducted.
Mortality and intraventricular hemorrhage and other bleeding events
The results related to mortality are in agreement with those of the largest RCT conducted to date on the effects of different transfusion thresholds in mortality and the development of major bleeding. The PlaNeT-2 trial [25–27] demonstrated that administering prophylactic PTx at a lower threshold (PC below 25 × 109/L) resulted in lower mortality rates and hemorrhage episodes in infants than transfusions at a higher threshold (PC below 50 × 109/L). The liberal transfusion group received more PTx and had more adverse events than the restrictive one. Another RCT was conducted by Kumar et al. [28], which not only aimed principally to assess the relation between PTx and patent ductus arteriosus (PDA), but also found that IVH events were significantly higher in the liberal transfusion group.
It is well-known that platelets have an imperative role in primary hemostasis. However, in newborn infants, particularly those born prematurely, platelets tend to be less active, which can result in longer bleeding and clotting times compared to healthy neonates born at full-term [5]. As preterm infants have a greater likelihood of bleeding, especially IVH, neonatologists frequently administer platelet transfusions in thrombocytopenic newborns without bleeding signs in an attempt to prevent bleeding and reduce the risk of further complications [32]. Unfortunately, and despite the theoretical benefit that PTx should have, no trials have yet conclusively demonstrated a protective effect of PTx on bleeding risk in preterm neonates with severe thrombocytopenia [2]. In fact, the studies reviewed in this analysis showed either a higher or similar risk of adverse effects between the transfused vs. non-transfused group but never an improvement in the health outcomes of the transfused group because of the intervention. The mechanisms underlying the deleterious effects of PTx are still unknown but some possible explanations are the use of transfusion products from adult donors, whose platelets are hyperreactive and pro-inflammatory in comparison to newborns’ ones and also the rapid expansion of blood volume due to the PTx, which can be the cause of bleeding [33].
As PTx can result in unfavorable consequences, it is still unclear what specific threshold provides a greater benefit over risk. Curley et al. [25–27] and Kumar et al. [28] suggest that a lower threshold should be used. However, further randomized controlled trials are necessary to determine the exact PC threshold at which transfusion is beneficial and should be performed. This will help prevent harm to newborns, avoid unnecessary costs, and prevent overuse of blood bank resources [5].
Morbidity
Sepsis and NEC were the two outcomes in study concerning morbidity of the newborn because sufficient data could be extracted from the included articles for comparison. However, there was limited data available on the outcomes of ROP, PDA, and BPD, so these outcomes were not included in the analysis. Further research to assess the consequences of PTx in the occurrence of these outcomes would be useful.
Strengths and limitations
Our review has several strengths, including a broad search strategy, as well as the inclusion of both RCTs and observational studies, which have an adequate risk of bias assessment, strengthening the results obtained. We also present and compare the results of studies with different objectives: transfusion vs. no transfusion; different transfusion thresholds and single vs. multiple transfusions. To our knowledge, it is the first meta-analysis conducted on this specific topic.
One limitation of this review is the retrospective nature of the majority of non-randomized studies, which are generally considered to be of lower quality compared to RCT. However, we still included these studies as they can provide valuable insights. To address this potential limitation, we conducted a risk of bias analysis as part of our study methodology. Another limitation is that temporal ambiguity presents a complex challenge, making it difficult to establish causality between outcomes and PTx, as opposed to the underlying thrombocytopenia. In addition, the fragility of the preterm population and the presence of confounding factors, such as comorbidities associated with newborns, make it difficult to draw definitive conclusions because there are events that cannot be fully eliminated when studying humans and, particularly, neonates. For example, common causes of thrombocytopenia, like sepsis and NEC [1; 2], may be a consequence of PTx rather than the primary cause. Likewise, it is possible that a higher number of PTx are administered due to the presence of IVH or other hemorrhage, rather than bleeding being caused by the transfusions. To minimize these confounding effects, in every included study, we ensured that the outcomes were not present before the intervention. However, the non-randomized design of some studies introduces the potential for selection bias, whereby infants who received PTx may have had higher levels of morbidity, which could have influenced the occurrence of adverse outcomes. Additionally, there is missing data from the original studies regarding the index of severity of illness and causes of death. Furthermore, the meta-analyses’ results may be limited by the relatively small number of studies that met the inclusion criteria, as well as their heterogeneity. A Leave-one-out sensitivity analyses for mortality and sepsis showed a decrease in heterogeneity without affecting our meta-analytical results, which supports the robustness and reliability of our findings. A meta-regression could not be done due to the small number of studies.
Conclusion
Platelet transfusions in preterm infants are associated to a higher risk of death, sepsis, and NEC and, possibly, to a higher incidence of IVH. Further studies are needed to confirm these associations, namely between PTx and IVH, and to define the threshold from which PTx should be given with less harmful effect. Preferably, RCTs should be conducted in preterm infants, comparing the outcomes of transfused and non-transfused patients at defined and comparable thresholds. Furthermore, it would be valuable to assess outcomes based on the number of transfusions received.
Supplementary Information
Below is the link to the electronic supplementary material.
Abbreviations
- BPD
Bronchopulmonary dysplasia
- CI
Confidence interval
- ECMO
Extracorporeal membrane oxygenation
- FGR
Fetal growth restriction
- I2
I-square
- ICH
Intracranial hemorrhage
- ISI
Institute of Scientific Information
- IVH
Intraventricular hemorrhage
- NEC
Necrotizing enterocolitis
- NOS
Newcastle-Ottawa Scale
- OR
Odds ratio
- PC
Platelet count
- PDA
Patent ductus arteriosus
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- PTx
Platelet transfusions
- RCT
Randomized controlled trial
- ROP
Retinopathy of prematurity
- RR
Relative risk
Authors’ contributions
HG and FFL developed the idea. RJV conducted literature searches. HSR and AA screened the articles for eligibility, collected the data using an Excel form, and assessed the risk of bias. HSR and AA performed the qualitative analysis and RJV performed the quantitative one. HSR wrote the first draft of the manuscript and all the authors commented on previous versions of the manuscript. All the authors approved the final version of the manuscript before submission for publication.
Funding
Open access funding provided by FCT|FCCN (b-on).
Declarations
Ethics approval
Since this study is a systematic review of previous published studies, the ethical approval was not required.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gunnink SF, Vlug R, Fijnvandraat K, van der Bom JG, Stanworth SJ, Lopriore E. Neonatal thrombocytopenia: etiology, management and outcome. Expert Rev Hematol. 2014;7:387–395. doi: 10.1586/17474086.2014.902301. [DOI] [PubMed] [Google Scholar]
- 2.Fustolo-Gunnink SF, Huisman EJ, van der Bom JG, van Hout FMA, Makineli S, Lopriore E, Fijnvandraat K. Are thrombocytopenia and platelet transfusions associated with major bleeding in preterm neonates? A systematic review. Blood Rev. 2019;36:1–9. doi: 10.1016/j.blre.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 3.Sola-Visner M, Bercovitz RS. Neonatal platelet transfusions and future areas of research. Transfus Med Rev. 2016;30:183–188. doi: 10.1016/j.tmrv.2016.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Roberts IA, Murray NA. Neonatal thrombocytopenia. Curr Hematol Rep. 2006;5:55–63. [PubMed] [Google Scholar]
- 5.Cremer M, Sallmon H, Kling PJ, Bührer C, Dame C. Thrombocytopenia and platelet transfusion in the neonate. Semin Fetal Neonatal Med. 2016;21:10–18. doi: 10.1016/j.siny.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 6.Christensen RD. Advances and controversies in neonatal ICU platelet transfusion practice. Adv Pediatr. 2008;55:255–269. doi: 10.1016/j.yapd.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 7.Dohner ML, Wiedmeier SE, Stoddard RA, Null D, Jr, Lambert DK, Burnett J, Baer VL, Hunt JC, Henry E, et al. Very high users of platelet transfusions in the neonatal intensive care unit. Transfusion. 2009;49:869–872. doi: 10.1111/j.1537-2995.2008.02074.x. [DOI] [PubMed] [Google Scholar]
- 8.Moore CM, Curley AE. Neonatal platelet transfusions: starting again. Transfus Med Rev. 2021;35:29–35. doi: 10.1016/j.tmrv.2021.06.003. [DOI] [PubMed] [Google Scholar]
- 9.Josephson CD, Su LL, Christensen RD, Hillyer CD, Castillejo MI, Emory MR, Lin Y, Hume H, Easley K, et al. Platelet transfusion practices among neonatologists in the United States and Canada: results of a survey. Pediatrics. 2009;123:278–285. doi: 10.1542/peds.2007-2850. [DOI] [PubMed] [Google Scholar]
- 10.Stanworth SJ. Thrombocytopenia, bleeding, and use of platelet transfusions in sick neonates. Hematology Am Soc Hematol Educ Program. 2012;2012:512–516. doi: 10.1182/asheducation-2012.1.512. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (2022) Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022). In: Cochrane (ed)
- 12.Moher D, Liberati A, Tetzlaff J, Altman DG (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed]
- 13.Wells GA SB, O'Connell D, Peterson J, Welch V, Losos M, Tugwell P (2023) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. (https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp). Accessed 13 February 2023
- 14.Andrew M, Vegh P, Caco C, Kirpalani H, Jefferies A, Ohlsson A, Watts J, Saigal S, Milner R, et al. A randomized, controlled trial of platelet transfusions in thrombocytopenic premature infants. J Pediatr. 1993;123:285–291. doi: 10.1016/s0022-3476(05)81705-6. [DOI] [PubMed] [Google Scholar]
- 15.Andrew MC, Vegh C, Kirplani P, Jefferies H, Ohlsson A, Watts A, Saigal J, Milner S, Wang RE. Benefits of platelet transfusions in premature-infants - a randomized controlled trial. Thromb Haemost. 1991;65:721–721. [Google Scholar]
- 16.Andrew M, Caco C, Vegh P, Kirpalani H, Jefferies A, Ohlsson A, Watts J, Saigal S, Milner R, Wang E. A multicenter randomized controlled trial of platelet infusions in premature-infants. Pediatr Res. 1991;29:A272–A272. doi: 10.1016/s0022-3476(05)81705-6. [DOI] [PubMed] [Google Scholar]
- 17.Christensen RD, Henry E, Wiedmeier SE, Stoddard RA, Sola-Visner MC, Lambert DK, Kiehn TI, Ainsworth S. Thrombocytopenia among extremely low birth weight neonates: data from a multihospital healthcare system. J Perinatol. 2006;26:348–353. doi: 10.1038/sj.jp.7211509. [DOI] [PubMed] [Google Scholar]
- 18.Baer VL, Lambert DK, Henry E, Snow GL, Sola-Visner MC, Christensen RD. Do platelet transfusions in the NICU adversely affect survival? Analysis of 1600 thrombocytopenic neonates in a multihospital healthcare system. J Perinatol. 2007;27:790–796. doi: 10.1038/sj.jp.7211833. [DOI] [PubMed] [Google Scholar]
- 19.Bonifacio L, Petrova A, Nanjundaswamy S, Mehta R. Thrombocytopenia related neonatal outcome in preterms. Indian J Pediatr. 2007;74:269–274. doi: 10.1007/s12098-007-0042-x. [DOI] [PubMed] [Google Scholar]
- 20.Sparger KA, Assmann SF, Granger S, Winston A, Christensen RD, Widness JA, Josephson C, Stowell SR, Saxonhouse M, et al. Platelet transfusion practices among very-low-birth-weight infants. JAMA Pediatr. 2016;170:687–694. doi: 10.1001/jamapediatrics.2016.0507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alhamad FA, Hussien A, Alqahtani F. Association between platelet transfusion and mortality rate among preterm neonates in the Eastern Province, Saudi Arabia. Med Arch. 2022;76:278–282. doi: 10.5455/medarh.2022.76.278-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen C, Wu S, Chen J, Wu J, Mei Y, Han T, Yang C, Ouyang X, Wong MCM et al (2022) Evaluation of the association of platelet count, mean platelet volume, and platelet transfusion with intraventricular hemorrhage and death among preterm infants. JAMA Netw Open 5:e2237588. 10.1001/jamanetworkopen.2022.37588 [DOI] [PMC free article] [PubMed]
- 23.Raja KM, Hussey-Gardner B, Gopalakrishnan M, Sundararajan S. Association of platelet transfusion and severe intraventricular hemorrhage in very low birth weight infants. J Investig Med. 2022;70:1089–1089. [Google Scholar]
- 24.von Lindern JS, Hulzebos CV, Bos AF, Brand A, Walther FJ, Lopriore E. Thrombocytopaenia and intraventricular haemorrhage in very premature infants: a tale of two cities. Arch Dis Child Fetal Neonatal Ed. 2012;97:F348–352. doi: 10.1136/fetalneonatal-2011-300763. [DOI] [PubMed] [Google Scholar]
- 25.Curley A, Stanworth SJ, Willoughby K, Fustolo-Gunnink SF, Venkatesh V, Hudson C, Deary A, Hodge R, Hopkins V, et al. Randomized trial of platelet-transfusion thresholds in neonates. N Engl J Med. 2019;380:242–251. doi: 10.1056/NEJMoa1807320. [DOI] [PubMed] [Google Scholar]
- 26.Curley A, Venkatesh V, Stanworth S, Clarke P, Watts T, New H, Willoughby K, Khan R, Muthukumar P, et al. Platelets for neonatal transfusion - study 2: a randomised controlled trial to compare two different platelet count thresholds for prophylactic platelet transfusion to preterm neonates. Neonatology. 2014;106:102–106. doi: 10.1159/000358481. [DOI] [PubMed] [Google Scholar]
- 27.Fustolo-Gunnink SF, Fijnvandraat K, van Klaveren D, Stanworth SJ, Curley A, Onland W, Steyerberg EW, de Kort E, d'Haens EJ, et al. Preterm neonates benefit from low prophylactic platelet transfusion threshold despite varying risk of bleeding or death. Blood. 2019;134:2354–2360. doi: 10.1182/blood.2019000899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kumar J, Dutta S, Sundaram V, Saini SS, Sharma RR, Varma N (2019) Platelet transfusion for PDA closure in preterm infants: a randomized controlled trial. Pediatrics 143. 10.1542/peds.2018-2565 [DOI] [PubMed]
- 29.Garcia MG, Duenas E, Sola MC, Hutson AD, Theriaque D, Christensen RD. Epidemiologic and outcome studies of patients who received platelet transfusions in the neonatal intensive care unit. J Perinatol. 2001;21:415–420. doi: 10.1038/sj.jp.7210566. [DOI] [PubMed] [Google Scholar]
- 30.Garcia MG, Chevuru SC, Saxonhouse MA, Theriaque DW, Hutson AD, Christensen RD, Sola MC. Effect of implementing platelet transfusion guidelines in a neonatal intensive care unit. Pediatr Res. 2002;51:308A–309A. [Google Scholar]
- 31.Del Vecchio A, Sola MC, Theriaque DW, Hutson AD, Kao KJ, Wright D, Garcia MG, Pollock BH, Christensen RD. Platelet transfusions in the neonatal intensive care unit:factors predicting which patients will require multiple transfusions. Transfusion. 2001;41:803–808. doi: 10.1046/j.1537-2995.2001.41060803.x. [DOI] [PubMed] [Google Scholar]
- 32.Davenport P, Sola-Visner M (2021) Hemostatic challenges in neonates. Front Pediatr 9:627715. 10.3389/fped.2021.627715 [DOI] [PMC free article] [PubMed]
- 33.Davenport P, Sola-Visner M (2022) Platelets in the neonate: not just a small adult. Res Pract Thromb Haemost 6:e12719. 10.1002/rth2.12719 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.