Abstract
The United States is in the midst of a childhood obesity epidemic that disproportionately impacts underserved and diverse populations. In this study, in-depth qualitative interviews were conducted with 16 low-income, single, female, parent/guardians of an overweight or obese 3- to 8-year-old from socioeconomically disadvantaged backgrounds. Following the tenets of the thematic analysis approach, interviews focused on identifying risk and protective factors influencing parental and child health behaviors associated with child weight status. Results from the interviews are organized according to the Socioecological Framework to help identify risk and protective factors at various system levels. Findings from this investigation have relevance for family therapists as they can inform clinical and advocacy-focused interventions with disadvantaged families affected by childhood obesity.
Keywords: Family, Qualitative, Health
INTRODUCTION
The childhood obesity epidemic in the U.S. constitutes one of the most considerable public health challenges facing the nation, particularly affecting underserved (e.g., socioeconomically disadvantaged) and diverse populations (Ogden, Carroll, Fryar, & Flegal, 2015). Childhood obesity is multifactorial in nature, with contextual adversity having a considerable impact on the etiology and maintenance of this problem (Harrison et al., 2011; Russell-Mayhew, McVey, Bardick, & Ireland, 2012). In addition to deleterious physical (e.g., type 2 diabetes, asthma) and psychological (e.g., low self-esteem, loneliness) effects on children and families (van Grieken, Renders, Wijtzes, Hirasing, & Raat, 2013), the ramifications of the epidemic are widespread. For example, national estimates indicate that the annual cost for the U.S. economy associated with obesity is approximately $254 billion (Levi et al., 2014).
According to meta-analytic data, critical protective factors against childhood obesity include positive parental involvement, effective parenting practices, and nutritional family habits (Kitzmann et al., 2010). However, there remains a need to further evaluate prevention and treatment approaches focused on childhood obesity (Oude Luttikhuis et al., 2009). With regard to solutions, an area in need of further exploration refers to examining the ways in which family dynamics and parent–child interactions constitute relevant protective factors for at risk children and youth (Pocock, Trivedi, Willis, Bunn, & Magnusson, 2010). Empirical evidence indicates that selecting the parent–child dyad as the unit of intervention for childhood obesity interventions constitutes a more effective approach than a child-only focus (Kitzman-Ulrich et al., 2010). Furthermore, it is critical to promote applied lines of research aimed at understanding the life experiences of underserved diverse populations affected by this problem, as well as identifying the most effective culturally relevant approaches to support them (Van Rinsum, Gerards, Rutten, van de Goor, & Kremers, 2017).
Systemic Factors Associated with Childhood Obesity
This study is informed by the ecological systems framework (Bronfenbrenner, 1986), which delineates five environmental systems with which individuals interact. These systems include, starting at closest proximity and moving outward, the microsystem, mesosystem, exosystem, macrosystem, and chronosystem. Each of these systems is characterized by roles, rules, and norms that influence psycho-social development. Systems frameworks are particularly relevant for understanding the multiplicity of factors impacting underserved and ethnic minority populations affected by childhood obesity. For example, the framework is particularly useful to understand how historical challenges and injustices are associated with negative health outcomes (Brotman et al., 2012).
The ecological systems framework was used in this investigation to inform a research design aimed at identifying specific factors associated with the etiology and maintenance of childhood obesity. By identifying factors that influence obesity at various eco-systemic levels, we hope to offer relevant contributions to the intervention literature, particularly as it refers to enhancing services for underserved and diverse individuals and families affected by childhood overweight and obesity.
Risk factors
Singh, Siahpush, and Kogan (2010) reported that rates of childhood obesity among children from single, female parent/guardian households, although not exclusively living in poverty, rose from 18.9% in 2003 to 21.9% in 2007. More recent reviews (e.g., Chung et al., 2016) suggest that children from lower socioeconomic groups disproportionately experience overweight and obesity. Children living in poor families are also less likely to engage in physical activity due to neighborhood safety concerns or lack of access to recreational facilities (Ding, Sallis, Kerr, Lee, & Rosenberg, 2011). Thus, it is important to identify how various systems within the socioecological framework interact to influence a child’s weight status. For example, chronic adversity and perceived discrimination are hypothesized to increase the risk of obesity because financial and contextual challenges are likely to result in increased levels of stress for adults as well as negative impacts on overall family stability. These factors can lead to child distress and psychological and emotional overload, with the end result of disrupting children’s homeostasis and increasing the likelihood of unhealthy weight gain (Hemmingsson, 2014).
Macrosystem
Ethnic minority populations continue to be impacted by significant barriers to health and mental health services throughout the U.S. Thus, there is a critical need to understand how contextual adversity is associated with risk factors and barriers impeding adherence to healthy eating habits. For example, fast food often represents a key coping mechanism to cope with financial limitations and time constraints, particularly as it refers to challenges experienced by low-income populations (Lucan, Barg, & Long, 2010). Thus, health disparities must be examined by carefully considering the deleterious impact of chronic adversity, poverty, historical segregation, and discrimination (Bleich, Thorpe, Sharif-Harris, Fesahazion, & Laveist, 2010; Stewart & Menning, 2009).
Exosystem
In the current literature review, no existing studies were identified focused on risk factors associated with the exosystem level, which indicates the need to expand existing frameworks according to the life experiences and risk/protective factors that are most relevant in the lives of families impacted by childhood obesity.
Mesosystem
Porter, Bean, Gerke, and Stern (2010) identified that low-income ethnic minority families are at high risk for having overweight and obese children, particularly if families are affected by long work schedules, transportation barriers, dangerous neighborhoods, and neighborhood segregation. These researchers found that these risk factors were important determinants of unhealthy cooking styles, insufficient time for meal preparation due to busy schedules, and dislike for the taste of healthy food.
Intergenerational transmission of health behaviors
Empirical studies indicate that parents’ experiences in their families of origin influence the ways in which they feed their children as well as the type of interactions they establish during mealtimes (Berge et al., 2017; Trofholz, Thao, et al., 2018). Researchers have also reported that frequency of meals and meal expectations in adolescence predicted family meal patterns 15 years later (Watts, Berge, Loth, Larson, & Neumark-Sztainer, 2018). Furthermore, parental health beliefs and knowledge of healthy lifestyles and eating patterns have been shown to be influenced by family of origin experiences (Pocock et al., 2010).
Microsystem
Unregulated emotional eating resulting from family conflict has been found to contribute to high calorie intake (Kelly et al., 2016). Owen, Sharp, Shield, and Turner (2009) found that children in families in which feelings of guilt resulting from overeating were not acknowledged were at an increased risk for experiencing distress. In addition, these families were at risk of unsuccessfully engaging in problem-solving behaviors associated with unhealthy eating patterns. Furthermore, in the context of childhood overweight and obesity, feeding styles are conceptualized as specific subtypes of parenting (Blissett, 2011). Specifically, authoritarian feeding styles usually involve restricted access to food and strict rules regarding food consumption. Permissive feeding styles lack rules or expectations about the quality or quantity of diet. Due to the negative impacts of contextual adversity, low-income and multi-stressed families are likely to engage in authoritarian or permissive styles as a response to adapt to intense adversity. For example, families may frequently consume fast food due to exhaustion associated with long working hours and their difficulty to access financial resources or time to prepare healthy foods (Blissett, 2011). In addition, childhood obesity is associated with biological and neuro-chemical brain changes associated with eating high-calorie and sugar-saturated foods that characterize fast food (Francis & Stevenson, 2013).
Protective Factors
Protective factors associated with the prevention of childhood overweight and obesity continue to be understudied, particularly as it refers to meso- and macrosystems (Redsell et al., 2015; Sigman-Grant, Hayes, VanBrackle, & Fiese, 2015). In the literature review conducted for this study, there was a scarcity of studies explicitly focused on identifying protective factors in the macro-, meso-, and exosystems.
Mesosystem
There is a notorious gap of empirical studies focused on identifying protective factors at the mesosystem level. In the current literature review, the only protective factor identified at the mesosystem level consisted of social support provided by family members as sources of social support for childcare responsibilities and meal preparation (Lindsay, Sussner, Greaney, & Peterson, 2009).
Microsystem
Highly relevant protective factors have been reported in the literature at the microsystem level. For example, financial stability constitutes a critical factor that determines the extent to which families can consume healthy foods on a regular basis, as well as having sufficient time for food preparation. Authoritative parenting styles also constitute a relevant protective factor as they are associated with healthy eating and promotion of child exercise (Silventoinen, Rokholm, Kaprio, & Sørensen, 2010). Additional family-level protective factors include supportive family dynamics (Gruber & Haldeman, 2009), adequate parental sense of self-efficacy (West, Sanders, Cleghorn, & Davies, 2010), and parental knowledge about healthy behaviors (Vereecken & Maes, 2010). Furthermore, clear family rules, emotional support, and parental encouragement have been found to be key determinants of healthy family behavioral eating patterns (Gruber & Haldeman, 2009). Studies also show that parents have an instrumental role in modeling healthy behaviors such as not soothing children with food, having positive family interactions with food, allowing children to try new and healthy foods, and talking positively about body image (Golley, Hendrie, Slater, & Corsini, 2011; Schwartz, Scholtens, Lalanne, Weenen, & Nicklaus, 2011).
Existing Qualitative Research
Qualitative research informed by a socio-ecological lens to study childhood obesity remains scarce, regardless of its potential to inform family therapy interventions (Bradbury et al., 2018). In fact, qualitative research exploring childhood obesity and affected families has historically focused on the study of microsystemic factors, such as precursors or barriers to healthy eating.
Macrosystem
In the current literature review, no existing qualitative studies focused on macrosystem factors were identified. Due to the critical importance of macrosystem factors in the lives of underserved and diverse families affected by childhood obesity, the current research protocol was carefully designed to address this gap in the literature.
Exosystem
Existing qualitative research aimed at identifying exosystem factors is scarce although existing studies point to the negative impact of long work schedules and neighborhood safety concerns as risk factors due to lack of sufficient time for food preparation and cumulative stress experienced by parents (Lindsay, Wallington, Lees, & Greaney, 2018).
Mesosystem
There is a considerable paucity of qualitative studies aimed at identifying risk and protective factors at the mesosystem level. Addressing this gap in research is highly relevant as researchers hypothesize that mesosystem level factors are likely to constitute critical barriers and facilitators for the successful implementation of childhood weight management programs (Kelleher, Harrington, Shiely, Perry, & McHugh, 2017), particularly as it refers to the influence of family-related factors that constitute precursors or barriers for successfully engaging families in childhood obesity interventions and related health services (Banks, Cramer, Sharp, Shield, & Turner, 2014).
Microsystem
Existing qualitative research focused on the microsystem level is primarily focused on the family unit. For example, studies have centered on investigating family dynamics at mealtimes (Berge, Hanson, & Draxten, 2016), parental perspectives of feeding practices with siblings (Berge, Trofholz, Schulte, Conger, & Neumark-Sztainer, 2016), mealtime characteristics of families who have frequent or infrequent family meals (Berge et al., 2018), maternal perceptions of their role during family meals (Trofholz, Schulte, & Berge, 2018), and parent and child division of feeding responsibilities (Loth, Nogueira de Brito, Neumark-Sztainer, Fisher, & Berge, 2018).
In the face of the existing gaps in the qualitative research literature, such as the scarcity of data related to macro-, exo-, and mesosystems, the main objectives of this study were to: (i) utilize a qualitative methodology to expand a multi-systemic understanding of risk and protective factors impacting underserved populations affected by childhood overweight and obesity, and (ii) provide family therapists and researchers with first-person accounts of female parents/guardians who are socioeconomically disadvantaged and whose children are overweight and obese. We expect that research findings can inform prevention and clinical interventions implemented by family therapists committed to helping this population.
METHOD
Participants
Sixteen low-income, single, female parents/guardians, residing in a midwestern city, participated in this investigation. Parents/guardians were eligible to participate if they met the following eligibility criteria: (i) single marital status, (ii) female parent/guardian, (iii) had at least one 3- to 8-year-old child. This age range was selected because as children become adolescents, the quality of their diet tends to decline (Larson & Story, 2009), (iv) a child with a BMI ≥85th percentile, which was determined according to the CDC’s online BMI calculator for children, and (v) an annual household income that met or exceeded federal poverty guidelines.
Parents/guardians ranged in age from 29 to 60 years (M = 37, SD = 9.7), and children’s BMI percentile ranged from 85 to 99. Nine parents/guardians were African American, followed by Hispanic (n = 3), non-Hispanic White (n = 2), and multi-ethnic (n = 2). Forty-three percent of parents/guardians completed some level of college education. Thirty-eight percent of parents/guardians were currently unemployed or receiving disability. Parents/guardians spent approximately 33% of their monthly income on food and approximately 4% on recreation. Additional participant information is included in Table 1.
TABLE 1.
Descriptive Information of Study Participants
| Demographic Factors | Summary Statistic |
|---|---|
| Caregiver age (mean, std) | 37 (9.7) |
| Child age (mean, std) | 5.8 (1.6) |
| Relation of respondent to child (%) | |
| Mother | 81 |
| Grandmother | 19 |
| Child overweight (%) | 81 |
| Child obese (%) | 19 |
| Race/ethnicity (%) | |
| White | 19 |
| Black/African American | 69 |
| Hispanic | 13 |
| Education level (%) | |
| Less than 9th grade | 6 |
| Less than 12th grade | 13 |
| High school graduate | 13 |
| Some college | 44 |
| Associate’s degree | 6 |
| Bachelor’s degree | 19 |
| Employment status (%) | |
| Unemployed/Disabled | 37 |
| Part-time | 25 |
| Self-employed | 6 |
| Full-time not in area of interest | 6 |
| Full-time in area of interest | 25 |
| % of monthly income spent on food (mean, std) | 32.6 (13.5) |
| % of monthly income spent on recreation (mean, std) | 4.4 (5.4) |
Procedures
Recruitment and data collection
Between May and October of 2015 participants were recruited in collaboration with healthcare centers offering services to low-income and disadvantaged populations. Specifically, the first author initially met with healthcare providers who work primarily with low-income patients. These professionals were offered a description of the study and inclusion and exclusion criteria to participate in the study. Next, potential participants were identified by healthcare providers based on demographic information of income and child age, weight, and height. Health professionals called potential participants and explored their interest to participate in the study. Potential participants contacted the first author, who verified eligibility criteria. If eligible, participants were offered a description of the purpose of the study and data collection procedures. Parents/guardians were compensated $30 for their participation in the study.
Qualitative data were collected by conducting semi-structured, face-to-face individual interviews (Ritchie, 2003), which included the completion of eco-maps. An eco-map is a graphical representation that describes all of the systems with which an individual interacts (e.g., family and extended social support networks; Hartman, 1995). Participants were asked to identify people, services, and entities in their support system and were asked to explain how central or auxiliary those supports were on a variety of issues, including the engagement in health promotion behaviors for them and their children.
Interviews were initiated by establishing rapport with participants and completing consent procedures, followed by a discussion of guiding research questions (Hill & Lambert, 2004). The interview protocol focused on four areas: (i) parental socio-historical and ethnocultural history, (ii) family interactions, (iii) family financial resources, and (iv) participants’ identified risk and protective factors regarding access to food and health promotion behaviors (e.g., physical activity). Research questions were designed to build upon themes previously identified in the literature and to expand a contextual understanding of such themes, while also highlighting the voices of research participants.
The research questions guiding this investigation were: (i) How do parents/guardians’ interactions with multiple systems in their lives (e.g., socio-historical contexts, family relations, sources of financial support), influence childhood overweight and obesity?; (ii) How do parents/guardians understand the impact of multiple systems according to the cultural diversity they represent (e.g., being a member of an ethnic minority population)?; and (iii) According to the participants’ narratives, what are key areas of intervention for family therapists committed to supporting families impacted by childhood overweight and obesity? Specific interview protocol questions are included as a Supplemental Table (S1). This study was approved by the corresponding institutional review board (IRB).
Data Analysis
NVivo 10 software (QSR International, 2012) was utilized to import and code the transcribed interviews. A thematic analysis approach was used to identify, analyze, and report patterns of data according to specific themes. Thematic analysis followed a semantic and latent approach (Braun & Clarke, 2006). A semantic approach consists of identifying themes exclusively found in explicit meaning of data (Vaismoradi, Turunen, & Bondas, 2013). In a subsequent step, data were examined according to latent analysis to identify and examine the underlying ideas, assumptions, and unique conceptualizations (Braun & Clarke, 2006). More specifically, we followed Braun and Clarke’s (2006) six-phase analytic guide consisting of the following steps: (i) becoming familiar with the data, (ii) generating initial codes, (iii) searching for themes, (iv) reviewing the themes, (v) defining themes, and (vi) creating the manuscript.
The lead author was the primary coder, with the second author reviewing half of the coded transcripts at random to ensure accuracy. The coding scheme was shared with co-authors, one of whom is an expert in child obesity and diet-related health disparities. The third author is an expert in qualitative research in the area of childhood obesity. Co-authors assisted with the overall research design, including the selection of research questions and interview guide. Co-authors also confirmed that current findings corresponded with existing literature, including their own studies, indicating a wide array of contextual challenges experienced by low-income families affected by child obesity. Co-authors also assisted data analyses by helping to understand the depth of the data. For example, co-authors analyzed collected data in light of challenges they have experienced in related studies focused on populations affected by child obesity. Examples of similar challenges included barriers to engage mothers and caregivers to attend interventions, often due to overwhelming responsibilities and lack of basic resources, such as lack of transportation. Co-authors also supported the data analytic process on highly relevant themes such as the fact that mothers in their studies also report struggling with their own weight issues and are unable or unwilling to change their own eating related behaviors.
In summary, co-authors had a critical role for establishing trustworthiness of the data by ensuring rigor of implementation of the research design, rigor of data analyses, and interpretation of qualitative findings within the context of their previous experiences with similar vulnerable populations. The first author also maintained an audit trail and memo describing key methodological decisions. Final findings were confirmed by conducting short follow-up interviews with participants as recommend by member checking procedures (Morrow, 2005).
RESULTS
Results are reported according to the specific dimensions of Bronfenbrenner’s (1986) Ecological Systems Framework, which differentiates multiple systems in the lives of individuals ranging from those having a direct influence (e.g., microsystem) to the larger context (macrosystem). To increase clarity of presentation, participants’ quotes are supplemented by the parent’s/guardian’s age, ethnic self-identification, and number of children residing in the household, respectively. Names of participants have been replaced with pseudonyms to ensure anonymity. All findings are derived from interviews conducted with the 16 participants in this study. Results are organized and presented according to the ecological systems framework, which identifies risk and protective factors at various levels of the framework (i.e., macrosystem, mesosystem, and the microsystem). No themes corresponding to the exosystem or chronosystem were identified in the data. Figure 1 provides an overview of study findings.
FIGURE 1.
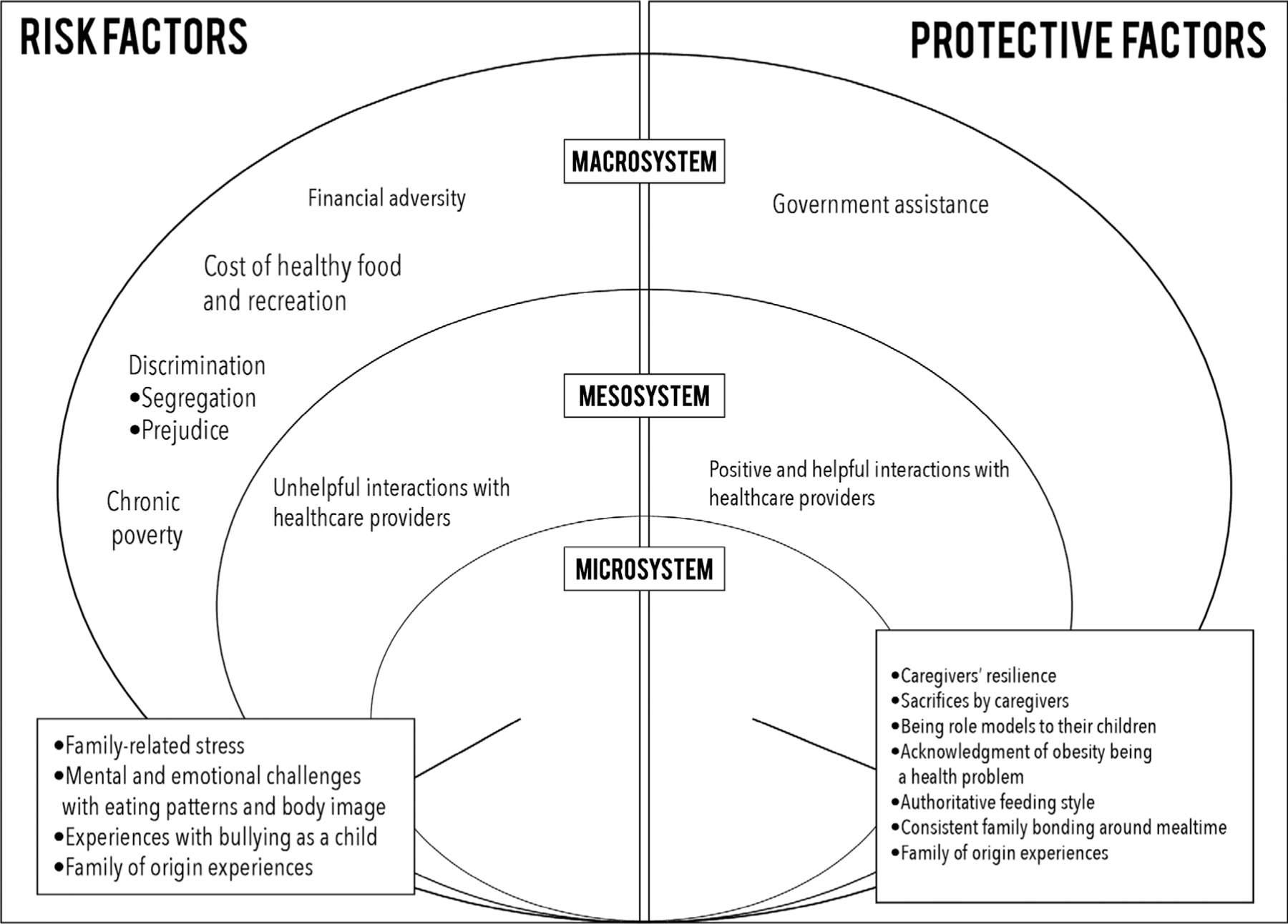
Risk and protective factors in health.
Macrosystem
Macrosystems refer to larger systems that impact the lives of individuals through larger contextual variables such as economic factors, community resources, health policies, and socio-cultural issues such as racism or prejudice towards low-income individuals (Bronfenbrenner, 1986). Risk factors identified at this level focused on discriminatory experiences according to the following sub-themes: segregation and prejudice, financial adversity, cost of healthy food and recreation, and chronic poverty. Government assistance was the only protective factor identified by participants at this level.
Risk factors
Discrimination
Eleven participants mentioned experiencing discrimination associated with attempting to access resources focused on healthy foods and recreational activities. For example, Honesty (43, White, 2) shared that she feels she is treated differently because of “being overweight, not necessarily color or anything, I think just being overweight … Then the kids have their friends that are like, ‘why is your mom like that,’ so I think that affects my kids.”
Segregation and prejudice
Ten parents/guardians expressed how segregation and prejudice have a deleterious effect on their lives. Angela (33, African, 3) shared her experience with regard to racism as a barrier to accessing healthy food:
We went to the farmers’ market that’s in a White neighborhood. As soon as we walked into the table with the fruit and stuff the lady was like, “We don’t take food stamps.” I’m not using food stamps I got my debit card out, why would you just automatically assume that I’m using food stamps?
Financial adversity
Twelve participants reported how financial adversity impacts their ability to access healthy food, recreational activities, and health services. Dee (36, Hispanic, 2) affirmed:
Resources are more available depending on what class you’re rated. I consider myself to be a middle-class person but I’m not. The reason I consider myself middle class is because I work. I go out there and look for it, it’s just not enough.
Lisa (29, African American/White, 1) discussed how financial challenges limit her health care options, “As far as medical care, I can’t go to the good doctors. … I can’t afford it. I feel like it’s not reachable to me because there’s not enough to go around.”
Cost of healthy food and recreation
Ten participants shared that healthy food is not affordable to them due to financial limitations. Minty (29, African American, 1) expressed:
I think that healthy food is affordable, but unhealthy food is cheap. I don’t think we think about it in that way. It’s the lifestyle that I may be condemned to at the time and may not allow me to afford it.
Amy (32, African American, 5) discussed her grocery shopping experience as one characterized by having to make compromises on the quality of food that she purchases. She shared:
We go to the grocery store and you buy a bag of oranges that are $3.99 and you want the big nice oranges but those are $6.99 a pound. We’d love to get those, but that’s not an option because the bag comes with many more even though they are not as appealing or good, but this is what I can afford and this will feed everyone.
In addition, 11 parents/guardians mentioned that the cost of recreational facilities hinders their ability to regularly gain access to activities that promote physical activity. Jazmyne (48, American Indian/White, 5) expressed, “I can’t afford to do a lot of stuff I’d like to with my children, like take them to Cedar Point or things like that.” Quana (28, African American, 3) expanded on these issues, “My children don’t get to do a lot of things, like camping or swimming lessons, because they cost money and I don’t have a lot of money.”
Dee (36, Hispanic, 2) also reflected:
Since I became a single parent, I haven’t been able to have a gym membership. When we had two incomes in the home, we had a Y membership. We would go swimming and I would go work out and they would go to a kid zone. We miss that.
Chronic poverty
All participants expressed that chronic poverty has become a permanent challenge to their health and well-being. As Amy (32, African American, 5) explained, “I definitely buy the less healthy stuff because it is cheaper than buying the healthier stuff and I have a big family.” Chasidy (29, African American, 2) agreed:
I am always on the budget and as of right now, I don’t have food stamps for the rest of the month, so I am using cash for us to buy food. I buy foods that can get us until I get more.
Ellena (41, Hispanic, 4) described similar struggles:
On a good week, we can go grocery shopping and I don’t have to think about how much we are going to spend and what specifically we are going to buy. If money is the issue, then it’s just basics.
Protective factors
Government assistance
Fourteen parents/guardians reported relying on government welfare programs and spoke of their ability to afford healthier foods because of the assistance they receive. Though parents/guardians stated that food assistance was helpful, only two expressed that their food stamps support was sufficient to meet their needs. For example, Monica (60, Hispanic, 2) shared, “Sometimes [the assistance] doesn’t last the entire month and it leaves me like half of the month with nothing.” Of concern, this was the only macrosystemic protective factor identified by families.
Mesosystem
Mesosystems refer to interactions among systems that have a direct influence in the lives of individuals. In the case of childhood obesity, these factors have a crucial role in increasing levels of risk for vulnerable families (Bronfenbrenner, 1986). Unhelpful interactions with healthcare providers were the only risk factor identified at the mesosystem level. Positive interactions with healthcare providers were the only protective factor identified at this level.
Risk factor
Unhelpful interactions with healthcare providers
Eight parents/guardians considered that healthcare professionals did not take the time to corroborate if the information they provided to participants was relevant. Angela (33, African, 3) shared that the “information from the dietician wasn’t helpful … she was just telling me stuff that I was already doing, but you can’t watch the portion sizes with a 5-month to 1-year-old baby, if she’s being breastfed.” Dee (36, Hispanic, 2) reported a similar challenge, “I always felt seeing a nutritionist is a waste of time. I think I’m very well informed, I just don’t have the means.”
Lisa (29, African American/White, 1) discussed the challenges to make health information relevant to her life, “[the information] would be beneficial for like a month and then I would go back, discuss it with them after trying that and it fails. I don’t know what changes to make. I don’t know what to do.” Both Minty (29, African American, 1) and Edna (52, African American, 2) discussed how the healthcare provider’s lack of understanding of their context created mistrust and would lead them to rely on family for help and information. Edna stated that she “just disregarded” the feedback she was given by her doctor.
An additional concern raised by parents/guardians referred to the way in which healthcare providers informed the parents/guardians of their children’s weight status. Jazmyne (48, American Indian/White, 5) shared her frustration by saying, “they said she was obese and that upset me.” She continued to explain how not only the label upset her, but that “they said it in front of my daughter” and her daughter “almost started crying.”
Protective factor
Positive and helpful interactions with healthcare providers
Eight participants reported that their interactions with healthcare providers were helpful. Ellena (41, Hispanic, 4) shared, “At times they are helpful with suggesting things that we can do. I have not run into anybody at the doctors that gave us anything negative. It is mostly positive.” Quana (28, African American, 3) talked about the helpful information she received from her local WIC office, “It’s good because they give you a lot of good ideas about cooking with the kids and what’s healthy and what’s not. It’s good they did it.”
Microsystem
Microsystems refer to the most proximal level of influence for families (Bronfenbrenner, 1986). Risk factors identified by participants at this level included: family of origin experiences, stress, mental and emotional challenges of mothers/guardians regarding their own eating patterns and body image, and parents/guardians’ experiences of bullying as a child. Protective factors included: family of origin experiences, parents/guardians’ resilience, parents/guardians’ sacrifices, parents/guardians’ beliefs of being a role model for their children, the belief that childhood obesity is a health problem, authoritative feeding styles, and consistent family bonding during mealtime.
Risk factors
Family of origin experiences
Seven parents/guardians disclosed that they adopted unhealthy behaviors from their families of origin, which have influenced their own parenting practices with their children. For example, Edna (52, African American, 2) learned to overlook hunger cues as a way of coping with the fear of poverty and starvation. She affirmed, “We had to eat everything that was on our plate. I try to do the same thing and make sure that they eat every portion that’s on their plate and that they are full once they finish.” Quana (28, African American, 3) shared that she continues eating habits with her own children that she did not enjoy as a child. She said:
My mom made us drink milk for every meal. I didn’t like it. After a certain time, we couldn’t get anything to drink, but water. I try and do … everything she did to me with my kids. It doesn’t work really but I still try to stick to it and try to make them do it.
Family-related stress
Fourteen participants expressed experiencing some type of family-related stress on a daily basis, which decreases the quality of interactions with their children, as Ellena (41, Hispanic, 4) acknowledged, “At times, if I find my children arguing, my stress level goes up and I yell at them. … I don’t like that.” Jada (27, African American, 1) provided a similar reflection, “Sometimes you get loud or take it out on the kids, but it’s not their fault.” Lisa (29, African American/White, 1) added, “I try not to yell at my son because he doesn’t really deserve that, but the yelling becomes the factor a lot more.”
Mental and emotional challenges associated with eating patterns and body image
All participants revealed having some level of dissatisfaction with either their own eating patterns, physical activity habits, or body image. Amy (32, African American, 5) reflected on these struggles:
I have such a love/hate relationship with food. It is definitely one of the hardest things to do in my life because I have been gaining weight since I was in fourth grade and I love food but then I hate it.
Thirteen parents/guardians also disclosed their discomfort with their own weight and eight identified themselves as “emotional eaters” or “stress snackers.” Honesty (43, White, 2) explained:
When I get nervous, I eat. I have a child that’s the same way and I think that has a lot to do with some of the obesity in some of the other kids too. … They don’t know how to deal with it and that’s their comfort zone.
Experiences with bullying as a child
Thirteen participants disclosed experiences of being bullied as children due to their weight. Amy (32, African American, 5) shared her experience:
I never knew I was obese growing up and in fourth grade I started being called the “fat girl,” being bullied about my weight, that’s when I noticed that I am a big person. I didn’t notice it because mostly everybody in our family was big at that time. It wasn’t until school it was like “I am the fat kid.” It was hard.
Jada (27, African American, 1) shared a similar experience, “Being overweight kind of hurt me. Now I hope my son doesn’t have to go through what I went through. I’m trying to change a lot of things, but it’s a big challenge.”
Protective factors
Family of origin experiences
All parents/guardians shared family of origin experiences that have positively influenced the way they interact with their children regarding healthy eating and physical activity. With regard to eating practices, parents/guardians reported fond memories of family gatherings during meals. For example, Angela (33, African, 3) shared, “Everyone had to eat dinner together at the table, just eat as much as you can, you didn’t have to clean your plate. We eat the same way now.”
Regarding physical activity traditions that parents/guardians want to pass down to their children, Nikki (32, White, 5) said, “I was in sports. I played basketball and volleyball, but I wasn’t pushed to do it, I did it on my own. … My daughter is in basketball and volleyball. My son wants to do soccer and football.”
Participants also reflected about family of origin challenges that they are determined to correct and that represent a contrast with their families of origin. For example, Jada (27, African American, 1) shared, “Everybody in my family was overweight. I wish there were more boundaries with portions and certain types of foods to be healthy and stay fit.” Dee (36, Hispanic, 2) provided an additional example:
In my family, we had to finish what was on our plate in order to even get up from the table and we didn’t get our drinks until we were done eating. I actually didn’t like that as a child, so I don’t make my kids finish everything and I do give them a drink before their meals.
With regard to food insecurity, Ellena (41, Hispanic, 4) reflected, “We did not have much to eat when we were growing up. So, I always make sure that my kids don’t suffer the way I did.” Similarly, Dee (36, Hispanic, 2) shared, “we went to bed without food for 2 days, twice in my life. I always strive to provide. I’m always looking for resources … because I don’t want them to go through what I went through.”
Participants also discussed issues of physical activity. For example, Lisa (29, African American/White, 1) expressed, “I didn’t play any sports at all as a kid. I was kind of lazy. With my son, I do the opposite. He plays every sport you can think of.” Jazmyne (48, American Indian/White, 5) reported doing activities with her children that she wished her parents would have done with her, “I like to take the kids for walks in the woods and stuff. … My parents never did that.”
Caregivers’ resilience
Fifteen parents/guardians shared how their sense of resilience and use of their support system helps them persevere and overcome life challenges. For example, Chasidy (29, African American, 2) described the importance of her attitude when facing challenges, “Staying positive. I don’t like to be around negativity or drama.” Honesty (43, White, 2) discussed the benefit of utilizing her support system, “Talking to people and telling people some of my problems helps a lot. It relieves a lot of stress because you’re not keeping it bottled up inside.”
The majority of participants (n = 15) discussed ways in which they were proactive to access healthy foods and remain physically active. Minty (29, African American, 1) commented on this issue, “I just volunteered at a food drive. I got a ton of food from that.” Others discussed utilizing free activities throughout their community, as Jada (27, African American, 1) affirmed:
I try to find free things to do. There’s a lot of free things, I take advantage of that. I’ll go to the museum where it’s free for students. I go to the water park where it’s free.
Sacrifices by caregivers
Eight participants explicitly discussed sacrificing their own food intake and leisure activities to ensure the well-being of their children. Towana (41, African American, 2) shared her experience, “It’s not that we don’t eat. I might not eat as much because I’m going to make sure my kids eat.” Minty (29, African American, 1) added, “I think every mom puts their child first, so, sometimes moms don’t get to eat what they want to eat.” Ellena (41, Hispanic, 4) shared how her “kids come first” in terms of the family food consumption and that she’ll “figure out [what food she will eat] somehow.” Nikki (32, White, 5) discussed the importance of making sure that her children do not feel different because of her income:
I’m in the lower class, poor, so we don’t have a lot of things. I don’t do my hair or nails because my kids insist on having designer clothes and shoes. I get it for them and I go without. I don’t care what people think about me, as long as my kids are good.
Being role models to their children
All participants reflected on the importance of being role models for their children. For example, Nikki (32, White, 5) shared that she “would like to go to the gym and get in shape to show to my kids that it’s fun.” Amy (32, African American, 5) further elaborated on this issue, “I am changing what I am doing and bettering my own health. … Since April I have lost 48 pounds.” Ellena (41, Hispanic, 4) shared her strategy of inviting her children to be active with her, “I ask them to come and join me if I am going for a walk.”
Parents/guardians also reflected on areas for self-improvement, as Towana (41, African American, 2) affirmed, “Your kids usually eat what you eat and if I don’t want to eat my green vegetables, why would they?” However, parents/guardians also discussed the challenges associated with trying to make healthy decisions. Dee (36, Hispanic, 2) described her struggle, “I hide when I don’t make good decisions. I can’t eat my snack until they are in bed so they can’t see me stressed out eating my snack. I’m supposed to lead by example.” Other participants shared a similar challenge, as Honesty (43, White, 2) said, “I eat unhealthy snacks when my kids are at school.”
Identifying obesity as a health problem
Fifteen participants said they believe childhood obesity is a problem in their community. In addition, eleven parents/guardians disclosed their discomfort with their children’s weight. Chasidy (29, African American, 2) shared, “My concern was his eating habits, but that has slowed down. He knows that he can’t eat certain things or a lot of whatever it is. I just watch how he eats.”
Dee (36, Hispanic, 2) expressed her motivation for having bariatric surgery: “I don’t want my kids to go through that and to get to that point to feel like surgery is the only way out.” Honesty (43, White, 2) said, “Because high blood pressure and diabetes runs in the family and her being a sugar bug. I worry about stuff like that.”
Authoritative feeding style
Thirteen women expressed their desire to embrace authoritative feeding styles. For example, Amy (32, African American, 5) shared that her children have “zero” influence over what she buys at the grocery store because if she let them, “they would pick waffles, pop tarts, chips, and donuts.” Dee (36, Hispanic, 2) shared her strategy for dealing with begging children in the grocery store, “they’ll beg first, then if I keep saying no they’ll start stomping and I sometimes ignore them and keep going through the grocery isle.” Tasha (32, African American, 3) also shared, “they’re only allowed to get one or two snacks from the store.”
Consistent family bonding during mealtimes
Participants provided multiple examples associated with their commitment to be consistent with their children with regard to mealtimes and exposure to healthy foods. Minty (29, African American, 1) reflected on this issue, “The average child may not be eating a plate of brussel sprouts, but I promise, you’ll really like this. You should try this.”
Thirteen parents/guardians reported eating at least one meal a day as a family and all participants reported eating together at least 4 days per week. Parents/guardians also framed mealtimes as an opportunity to bond with their children and hear about their daily experiences, as Edna (52, African American, 2) said, “We just talk about how their day went by.”
Additionally, all participants reported the benefits associated with the bonding experience of preparing meals with family members, as Amy (32, African American, 5) described:
I try to switch it up [meal preparation] so they can learn everything because that’s how my mom did with both me and my sister. If you were in charge of lettuce for salad last time, then I want you to flour the chicken with me this time. If you seasoned the food last time, you are going to set the table and get the tomatoes out and cut them up. I try to get them all doing different things so they can move around and know.
DISCUSSION
Current findings highlight the salient role of contextual risk and protective factors as it refers to the etiology and maintenance of childhood overweight and obesity. In fact, the primary and most concerning finding refers to qualitative narratives indicating that the majority of risk factors reported by participants were identified at the macrosystem level. In contrast, few protective factors were identified at the same level, which corroborates how health disparities affecting low-income and disadvantaged populations are closely related to chronic poverty, income inequality, and barriers to health promotion resources (e.g., limited access to facilities for physical activity, neighborhood safety, limited lighting for evening activities, parks isolated from traffic; Devís-Devís, Beltrán-Carrillo, & Peiró-Velert, 2015).
Findings indicating that the majority of risk factors were identified at the macrosystem level correspond with research informed by socio-ecological models, which facilitate a systemic understanding of the etiology of childhood obesity (Bradbury et al., 2018). Thus, according to current results, oppressive macro-level factors constitute salient precursors of childhood obesity, which considerably call into question dominant perspectives that over-emphasize micro-level risk factors. Research results also highlight the need for mental health professionals, especially family therapists and other systemic-oriented health professionals, to carefully examine the role of context in the etiology and maintenance of childhood obesity, which extend beyond the immediate family system.
Despite the considerable influence of contextual risk factors, it is also essential to highlight the extraordinary sense of resilience of parents/guardians. For example, within their limited resources, parents/guardians expressed their strong commitment and resolve to offer a new legacy to their children with regard to creating healthy eating habits, as well as engaging them in healthy behaviors. Parents/guardians also provided detailed accounts of personal sacrifices for the sake and well-being of their children. Thus, current qualitative data highlight the need to continuously identify the many coping mechanisms that populations exposed to systemic oppression utilize in their efforts to adapt to contextual adversity and offer a better future to their children (Burt, Simons, & Gibbons, 2012).
IMPLICATIONS FOR PRACTICE
The Need for Advocacy-Focused Approaches
Several risks factors identified in this study were associated with the pernicious effects of historical marginalization and limited impact of welfare and government-sponsored programs. These findings indicate the high need for family therapists to embrace advocacy approaches in addition to therapeutic interventions, particularly because advocacy-focused interventions have been demonstrated to be particularly effective for supporting families exposed to intense adversity (Sullivan, Bybee, & Allen, 2002). With regard to current findings, caregivers were keenly aware of the contextual challenges they face that prevent them from embracing healthier lifestyles. Thus, family therapists can have a key role in serving as advocate for families as they strive to access the resources they need to better cope with contextual adversity.
Current findings also highlight important lessons according to principles that constitute the foundation of community-based participatory research (CBPR), as applied to clinical practice. Specifically, CBPR principles indicate that the research process should be strengths-based and collaborative in nature. In prevention and clinical practice, such a focus is essential to help families address barriers that will allow them to adopt healthy lifestyles (Berge, Jin, et al., 2016; Davison, Jurkowski, Li, Kranz, & Lawson, 2013). Close adherence to these CBPR principles has been confirmed to be a key factor for success in obesity prevention and clinical interventions (Berge, Jin, et al., 2016; Davison et al., 2013).
Current findings also indicate the relevance for family therapists to inform clinical practice according to advocacy approaches, particularly because living healthy lifestyles is closely related to having access to resources that will support these life goals. For example, half of the participants in this study could not identify resources in the community to help them improve their children’s health. Even if such resources exist in communities and are advertised, advocacy approaches are highly needed as families experiencing intense adversity are very likely to need support when attempting to access such resources, particularly if parents/guardians have been exposed to past experiences of discrimination from healthcare providers. Thus, family therapists can serve as advocates by discussing with families alternatives for interacting with healthcare providers, including offering families to facilitate or support the communication with health care providers with the goal of offering integrative treatments (Chandler, 2010; Fiese, Hammons, & Grisby-Toussaint, 2012). In essence, rather than receiving referral information for services, research on advocacy approaches indicates that families exposed to contextual adversity can greatly benefit from interactions with mental health professionals who will have an active role in helping them access the resources they need to better cope with adversity (Trickett et al., 2011). These reflections are particularly relevant when considering that empirical research indicates that stigma among health care providers continues to inform stereotypes that blame individuals for their overweight and obesity (Pagnini, King, Booth, Wilkenfeld, & Booth, 2009; Ruelaz et al., 2007). The fact that eight parents/guardians reported feeling judged or blamed by their healthcare providers confirms this body of literature.
Interventions Focused on Health Promotion
With regard to health promotion implications, current research results correspond with research findings highlighting the need for interventions aimed at exploring, validating, and de-constructing parental feelings of guilt and shame associated with their children’s overweight and obesity (Resnicow, Davis, & Rollnick, 2006). This is a critical area of intervention because although parental feelings of guilt and shame are critical precursors of childhood obesity, existing family- and parent-focused health interventions tend to primarily consist of cognitive and behavioral interventions (e.g., Epstein, Paluch, & Raynor, 2001; Golley, Perry, Magarey, & Daniels, 2007; Kalavainen, Korppi, & Nuutinen, 2007).
Furthermore, the empirical literature indicates that a nurturing emotional climate during mealtimes constitutes an important protective factor against childhood overweight and obesity (e.g., Saltzman, Pineros-Leano, Liechty, Bost, & Fiese, 2016; Saltzman, Bost, Musaad, Fiese, & Wiley, 2018). This constitutes a key area of intervention for family therapists as clinicians can help parents/guardians enhance skills aimed at ensuring that family meal times are characterized by nurturing interactions among family members. For those families that cannot have regular family mealtimes due to job constraints, it is essential for family therapists to help them brainstorm alternatives to facilitate close and nurturing family interactions associated with food, such as weekend mealtimes.
Current findings also indicate the need to help families identify the ways in which childhood obesity can be related to detrimental family legacies. Thus, family therapists can address challenging family backgrounds while also highlighting to parents the unique opportunity they have to offer new legacies to their children such as having family routines consisting of healthy interactions with food, adequate calorie consumption, and regular exercise.
Finally, conceptualizing childhood overweight and obesity as influenced by macrosystem factors can significantly reduce feelings of shame and guilt experienced by parents/guardians. In fact, highlighting to families how contextual challenges constitute key factors that force families to engage in unhealthy eating as a coping and survival mechanism constitutes a highly relevant alternative to individual-based approaches that solely focus on promoting “individual responsibility and self-efficacy,” which constitutes an approach that is likely to perpetuate oppression among families impacted by legacies of social injustice.
POLICY IMPLICATIONS
One of the most relevant findings from this investigation refers to the fact that the majority of risk factors identified by participants refer to macro-level issues that have a detrimental impact on their lives. In contrast, research participants only identified one protective factor at the macro-level. These findings highlight that the U.S. continues to lag behind with regard to having a welfare infrastructure capable of providing basic services to the most vulnerable members of society, in contrast to more progressive societies in which health care services constitutes a basic right to all individuals (Basu, Andrews, Kishore, Panjabi, & Stuckler, 2012).
Of particular concern, as expressed by Lebow (2018), current federal initiatives are increasingly focused on reducing critical welfare programs that are essential for the well-being of families affected across generations by the detrimental legacies of poverty, oppression, and systemic segregation (U.S. Office of Management and Budget, 2018). More than ever, we face as family therapists a challenge to critically examine our professional identity as it is not enough to limit our scope of action to interventions in clinical settings, but to extend our area of impact to influence social justice policies at local, regional, and national levels. As proposed by Smith, Chambers, and Bratini (2009), childhood obesity is a clear example of a health crisis in which “oppression is the pathogen.”
Following this order of ideas, it is critical to remember that policy promotion is not restricted to major initiatives at the federal level. In fact, the core of policy impact can be found in systemic changes at local levels (Cerna, 2013). For example, there are successful examples of municipalities in the U.S. that integrate federal and local resources to effectively promote subsidized affordable prices of healthy foods to low-income families, incentives to farmers, increased taxes of unhealthy foods, and promotion of free obesity prevention programs (Chriqui, 2013; Frieden, Dietz, & Collins, 2010). Furthermore, policy efforts must be informed by acknowledging that not all populations in the U.S. are affected equally by overweight and obesity, with ethnic minority status and poverty being key determinants of health across the U.S. (Caprio et al., 2008).
LIMITATIONS OF THE STUDY AND FUTURE RESEARCH DIRECTIONS
Important limitations of this study must be noted. First, the selection criteria did not include parental recognition of childhood obesity as a requisite for participation. This constitutes a considerable limitation as four participants were reluctant to identify their children as being affected by this problem. This may very well be associated with the fact that the data collector was Euro-American and trust could have been a factor for these and other families to being reluctant to engage in full disclosure about their life experiences. In addition, the challenges reported by parents/guardians related to healthcare services were circumscribed to available government services in the target community. Thus, it may be possible that a similar study may provide contrasting results if participants are selected from healthcare organizations with a strong history of serving disadvantaged ethnic minority communities.
With regard to future directions for research, we offer specific recommendations. First, interactions with healthcare providers in this study were identified as both protective and risk factors. This constitutes a meaningful finding and an area of relevant research inquiry, particularly as it refers to the need to more clearly identify the characteristics of providers that position them as barriers to or facilitators of support by families affected by childhood obesity.
Similarly, there is great need for health services research aimed at investigating the health care processes that affected families consider are most beneficial to help them engage in healthy lifestyles. In fact, although important advancements have been achieved in the field of implementation science in the health sciences, implementation scientists continue to highlight that research focused on health disparities in health services delivery continues to be seriously underdeveloped (Cabassa & Baumann, 2013).
Finally, promoting new lines of services research can be achieved by implementing studies grounded in CBPR principles with co-leadership from families affected by childhood obesity. Thus, studies aimed at evaluating cultural relevance of services for childhood obesity can include mothers/guardians as key collaborators during various phases of the research process, including the design of protocols, selection of culturally relevant data collection methodologies, and evaluation approaches capable of capturing relevant life and family experiences related to the promotion of healthy lifestyles.
CONCLUSION
Current findings indicate the need to elevate the voices of those impacted by health disparities as participants in this study identified salient risk factors beyond the immediate family system. Embracing a broad systemic perspective is essential to develop more contextually relevant family therapy interventions to effectively support families that have been subject to legacies of discrimination and exclusion. In essence, the main call for action proposed by the resilient participants in this study refers to the need for family therapists to serve not only as experts in relationship functioning, but equally important, as social justice advocates.
Supplementary Material
Footnotes
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
REFERENCES
- Banks J, Cramer H, Sharp DJ, Shield JPH, & Turner KM (2014). Identifying families’ reasons for engaging or not engaging with childhood obesity services: A qualitative study. Journal of Child Health Care, 18, 101–110. [DOI] [PubMed] [Google Scholar]
- Basu S, Andrews J, Kishore S, Panjabi R, & Stuckler D (2012). Comparative performance of private and public healthcare systems in low- and middle-income contries: A systematic review. PLoS Medicine, 9, e001244. 10.1371/journal.pmed.1001244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Draxten M, Trofholz A, Hanson-Bradley C, Justesen K, & Slattengren A (2018). Similarities and differences between families who have frequent and infrequent family meals: A qualitative investigation of low-income and minority households. Eating Behaviors, 29, 99–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Hanson C, & Draxten M (2016). Perspectives about family meals from racially/ethnically and socioeconomically diverse households with and without an overweight/obese child. Childhood Obesity, 12, 368–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Jin S, Hanson-Bradley C, Doty J, Jagaraj K, Braaten K, & Doherty W (2016). Play it forward!: A community-based participatory research approach to childhood obesity prevention. Families, Systems, and Health, 34, 15–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Miller J, Watts A, Larson N, Loth KA, & Neumark-Sztainer D (2017). Intergenerational transmission of family meal patterns from adolescence to parenthood: Longitudinal associations with parents’ dietary intake, weight-related behaviors and psychosocial well-being. Public Health Nutrition, 21, 299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berge JM, Trofholz A, Schulte A, Conger K, & Neumark-Sztainer D (2016). A qualitative investigation of parents’ perspectives about feeding practices with siblings among racially/ethnically and socioeconomically diverse households. Journal of Nutrition Education and Behavior, 48, 496–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bleich SN, Thorpe RJ, Sharif-Harris H, Fesahazion R, & Laveist TA (2010). Social context explains race disparities in obesity among women. Journal of Epidemiology & Community Health, 64, 465–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blissett J (2011). Relationships between parenting style, feeding style and feeding practices and fruit and vegetable consumption in early childhood. Appetite, 57, 826–831. [DOI] [PubMed] [Google Scholar]
- Bradbury D, Chisholm A, Watson PM, Bundy C, Bradbury N, & Birtwistle S (2018). Barriers and facilitators to health care professionals discussing child weight with parents: A meta-synthesis of qualitative studies. British Journal of Health Psychology, 23, 519–774. 10.11111/bjhp.12312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, & Clarke V (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3, 77–101. [Google Scholar]
- Bronfenbrenner U (1986). Ecology of the family as a context for human development: Research perspectives. Developmental Psychology, 22, 723–742. [Google Scholar]
- Brotman LM, Dawson-McClure S, Huang K-Y, Theise R, Kamboukos D, Wang J, Petkova E, & Ogedegbe G (2012). Early childhood family intervention and long-term obesity prevention among high-risk minority youth. Pediatrics, 129(3), e621–e628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burt CH, Simons RL, & Gibbons FX (2012). Racial discrimination, ethic-racial socialization, and crime: A micro-sociological model of risk and resilience. American Sociological Review, 77, 648–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabassa LJ, & Baumann AA (2013). A two-way street: Bridging implementation science and cultural adaptations of mental health treatments. Implementation Science, 8, 90–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caprio S, Daniels SR, Drewnowski A, Kaufman FR, Palinkas LA, Rosenbloom AL et al. (2008). Influence of race, ethnicity, and culture on childhood obesity: Implications for prevention and treatment. Diabetes Care, 31, 2211–2221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerna L (2013). The nature of policy change and implementation: A review of different theoretical approaches Paris: OECD/CERI. Retrieved from http://www.oecd.org/edu/ceri/The%20Nature%20of%20Policy%20Change%20and%20Implementation.pdf. [Google Scholar]
- Chandler D (2010). The underutilization of health services in the Black community: An examination of causes and effects. Journal of Black Studies, 40, 915–931. [Google Scholar]
- Chriqui JF (2013). Obesity prevention policies in U.S. states and localities: Lessons from the field. Current Obesity Reports, 2, 200–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung A, Backholer K, Wong E, Palermo C, Keating C, & Peeters A (2016). Trends in child and adolescent obesity prevalence in economically advanced countries according to socioeconomic position: A systematic review. Obesity Reviews, 17, 276–295. [DOI] [PubMed] [Google Scholar]
- Davison KK, Jurkowski JM, Li K, Kranz S, & Lawson HA (2013). A childhood obesity intervention developed by families for families: Results from a pilot study. International Journal of Behavioral Nutrition and Physical Activity, 10, 3. 10.1186/1479-5868-10-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devís-Devís J, Beltrán-Carrillo V, & Peiró-Velert C (2015). Exploring socio-ecological factors influencing active and inactive Spanish students in years 12 and 13. Sport, Education and Society, 3, 361–380. [Google Scholar]
- Ding D, Sallis JF, Kerr J, Lee S, & Rosenberg DE (2011). Neighborhood environment and physical activity among youth: A review. American Journal of Preventative Medicine, 41, 442–455. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Paluch RA, & Raynor HA (2001). Sex differences in obese children and siblings in family-based obesity treatment. Obesity Research, 9, 746–753. [DOI] [PubMed] [Google Scholar]
- Fiese BH, Hammons A, & Grisby-Toussaint D (2012). Family mealtimes: A contextual approach to understanding childhood obesity. Economics & Human Biology, 10, 365–374. [DOI] [PubMed] [Google Scholar]
- Francis H, & Stevenson R (2013). The longer-term impacts of Western diet on human cognition and the brain. Appetite, 63, 119–128. [DOI] [PubMed] [Google Scholar]
- Frieden TR, Dietz W, & Collins J (2010). Reducing childhood obesity through policy change: Acting now to prevent obesity. Health Affairs, 29, 357–363. [DOI] [PubMed] [Google Scholar]
- Golley RK, Hendrie GA, Slater A, & Corsini N (2011). Interventions that involve parents to improve children’s weight-related nutrition intake and activity patterns: What nutrition and activity targets and behaviour change techniques are associated with intervention effectiveness? Obesity Reviews, 12(2), 114–130. [DOI] [PubMed] [Google Scholar]
- Golley RK, Perry RA, Magarey A, & Daniels L (2007). Family-focused weight management program for five- to nine-year-olds incorporating parenting skills training with healthy lifestyle information to support behavior modification. Nutrition & Dietetics, 64, 144–150. [Google Scholar]
- Gruber KJ, & Haldeman LA (2009). Using the family to combat childhood and adult obesity. Preventing Chronic Disease, 6, A106. [PMC free article] [PubMed] [Google Scholar]
- Harrison K, Bost KK, McBride BA, Donovan SM, Grigsby-Toussaint DS, Kim J et al. (2011). Toward a developmental conceptualization of contributors to overweight and obesity in childhood: The Six-Cs Model. Child Development Perspectives, 5, 50–58. [Google Scholar]
- Hartman A (1995). Diagrammatic assessment of family relationships. Families in Society: The Journal of Contemporary Human Services, 1, 111–122. [Google Scholar]
- Hemmingsson E (2014). A new model of the role of psychological and emotional distress in promoting obesity: Conceptual review with implication for treatment and prevention. Obesity Reviews, 15, 769–779. [DOI] [PubMed] [Google Scholar]
- Hill CE, & Lambert MJ (2004). Methodological issues in studying psychotherapy processes and outcomes. In Lambert MJ (Ed.), Bergin and Garfield’s handbook of psychotherapy and behavior change, 5th ed. (pp. 84–135). New York: John Wiley & Sons. [Google Scholar]
- Kalavainen MP, Korppi MO, & Nuutinen OM (2007). Clinical efficacy of group-based treatment for childhood obesity compared with routinely given individual counseling. International Journal of Obesity, 31, 1500–1508. [DOI] [PubMed] [Google Scholar]
- Kelleher E, Harrington JM, Shiely F, Perry IJ, & McHugh SM (2017). Barriers and facilitators to the implementation of a community-based, multidisciplinary, family-focused childhood weight management programme in Ireland: A qualitative study. British Medical Journal Open, 7. 10.1136/bmjopen-2017-016459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly NR, Tanofsky-Kraff M, Vannucci A, Ranzenhofer LM, Altschul AM, Schvey NA et al. (2016). Emotion dysregulation and loss-of-control eating in children and adolescents. Health Psychology, 35, 1110–1119. 10.1037/hea0000389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzmann KM, Dalton WT, Stanley CM, Beech BM, Reeves TP, Buscemi J et al. (2010). Lifestyle interventions for youth who are overweight: A meta-analytic review. Health Psychology, 29, 91–101. [DOI] [PubMed] [Google Scholar]
- Kitzman-Ulrich H, Wilson D, George S, Lawman H, Segal M, & Fairchild A (2010). The integration of a family systems approach for understanding youth obesity, physical activity, and dietary programs. Clinical Child and Family Psychology Review, 13, 231–253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson N, & Story M (2009). A review of environmental influences on food choices. Annals of Behavioral Medicine, 38, s56–s73. [DOI] [PubMed] [Google Scholar]
- Levi J, Segal LM, & St. Laurent R, & Rayburn J, (2014). State of obesity: Better policies for a healthier America: 2014 Princeton, NJ: Robert Wood Johnson Foundation. [Google Scholar]
- Lindsay AC, Sussner KM, Greaney ML, & Peterson KE (2009). Influence of social context on eating, physical activity, and sedentary behaviors of Latina mothers and their preschool-age children. Health Education & Behavior, 36, 81–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindsay AC, Wallington SF, Lees FD, & Greaney ML (2018). Exploring how the home environment influences eating and physical activity habits of low-income, Latino children of predominantly immigrant families: A qualitative study. International Journal of Environmental Research and Public Health, 15, 978. 10.3390/ijerph15050978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loth KA, Nogueira de Brito J, Neumark-Sztainer D, Fisher JO, & Berge JM (2018). A qualitative exploration into the parent-child feeding relationship: How parents of preschoolers divide the responsibilities of feeding with their children. Journal of Nutrition Education and Behavior, 50, 655–667. 10.1016/j.jned.2018.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucan SC, Barg FK, & Long JA (2010). Promoters and barriers to fruit, vegetable, and fast-food consumption among urban, low-income African Americans: A qualitative approach. American Journal of Public Health, 100, 631–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrow SL (2005). Quality and trustworthiness in qualitative research in counseling psychology. Journal of Counseling Psychology, 52, 250–260. [Google Scholar]
- Ogden CL, Carroll MD, Fryar CD, & Flegal KM (2015). Prevalence of obesity among adults and youth: United States, 2011–2014. NCHS data brief, no 219 Hyattsville, MD: National Center for Health Statistics. [PubMed] [Google Scholar]
- Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O’Malley C, Stolk RP et al. (2009). Interventions for treating obesity in children. Evidence-Based Child Health: A Cochrane Review Journal, 4, 1571–1729. [DOI] [PubMed] [Google Scholar]
- Owen S, Sharp D, Shield J, & Turner K (2009). Children’s and parents’ views and experiences of attending a childhood obesity clinic: A qualitative study. Primary Healthcare Research & Development, 10, 236–244. [Google Scholar]
- Pagnini D, King L, Booth S, Wilkenfeld R, & Booth M (2009). The weight of opinion on childhood obesity: Recognizing complexity and supporting collaborative action. International Journal of Pediatric Obesity, 4, 233–241. [DOI] [PubMed] [Google Scholar]
- Pocock M, Trivedi D, Willis W, Bunn F, & Magnusson J (2010). Parental perceptions regarding healthy behaviours for preventing overweight and obesity in young children: A systematic review of qualitative studies. Obesity Reviews, 11, 338–353. [DOI] [PubMed] [Google Scholar]
- Porter J, Bean M, Gerke C, & Stern M (2010). Psychosocial factors and perspectives on weight gain and barriers to weight loss among adolescents enrolled in obesity treatment. Journal of Clinical Psychology in Medical Settings, 17, 98–102. [DOI] [PubMed] [Google Scholar]
- QSR International (2012). NVivo qualitative data analysis software (Version 10). [Computer software]
- Redsell SA, Edmonds B, Swift JA, Siriwardena AN, Weng S, Nathan D et al. (2015). Systematic review of randomized controlled trials of interventions that aim to reduce the risk, either directly or indirectly, of overwight and obesity in infancy and early childhood. Maternal and Child Nutrition, 12, 24–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnicow K, Davis R, & Rollnick S (2006). Motivational interviewing for pediatric obesity: Conceptual issues and evidence review. Journal of the American Dietetic Association, 106, 2024–2033. [DOI] [PubMed] [Google Scholar]
- Ritchie J (2003). The applications of qualitative methods to social research. In Ritchie J & Lewis J (Eds.), Qualitative research practice (pp. 24–46). Thousand Oaks, CA: Sage. [Google Scholar]
- Ruelaz A, Diefenbach P, Simon B, Lanto A, Arterburn D, & Shekelle P (2007). Perceived barriers to weight management in primary care: Perspectives of patients and providers. Society of General Internal Medicine, 22, 518–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell-Mayhew S, McVey G, Bardick A, & Ireland A (2012). Mental health, wellness, and childhood overweight/obesity. Journal of Obesity, 2012, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saltzman JA, Bost KK, Musaad SMA, Fiese BH, Wiley AR, & The STRONG Kids Team (2018). Predictors and outcomes of mealtime emotional climate in families with preschoolers. Journal of Pediatric Psychology, 43, 195–206. [DOI] [PubMed] [Google Scholar]
- Saltzman JA, Pineros-Leano M, Liechty JM, Bost KK, & Fiese BH (2016). Eating, feeding, and feeling: Emotional responsiveness mediates longitudinal associations between maternal binge eating, feeding practices, and child weight. International Journal of Behavioral Nutrition and Physical Activity, 13, 89. 10.1186/s12966-016-0415-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz C, Scholtens PA, Lalanne A, Weenen H, & Nicklaus S (2011). Development of healthy eating habits early in life: Review of recent evidence and selected guidelines. Appetite, 57, 796–807. [DOI] [PubMed] [Google Scholar]
- Sigman-Grant M, Hayes J, VanBrackle A, & Fiese B (2015). Family resiliency: A neglected perspective in addressing obesity in young children. Childhood Obesity, 11. 10.1089/chi.2014.0107 [DOI] [PubMed] [Google Scholar]
- Silventoinen K, Rokholm B, Kaprio J, & Sørensen TIA (2010). The genetic and environmental influences on childhood obesity: A systematic review of twin and adoption studies. International Journal of Obesity, 34, 29–40. [DOI] [PubMed] [Google Scholar]
- Singh GK, Siahpush M, & Kogan MD (2010). Rising social inequalities in US childhood obesity, 2003–2007. Annals of Epidemiology, 20(1), 40–52. [DOI] [PubMed] [Google Scholar]
- Smith L, Chambers DA, & Bratini L (2009). When oppression is the pathogen: The participatory development of socially just mental health practice. American Journal of Orthopsychiatry, 79, 159–168. [DOI] [PubMed] [Google Scholar]
- Stewart SD, & Menning CL (2009). Family structure, nonresident father involvement, and adolescent eating patterns. Journal of Adolescent Health, 45(2), 193–201. [DOI] [PubMed] [Google Scholar]
- Sullivan CM, Bybee DI, & Allen NE (2002). Findings from a community-based program for battered women and their children. Journal of Interpersonal Violence, 17, 915–936. [Google Scholar]
- Trickett EJ, Beehler S, Deutsch C, Green LW, Hawe P, McLeroy K et al. (2011). Advancing the science of community-level interventions. American Journal of Public Health, 101, 1410–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trofholz AC, Schulte AK, & Berge JM (2018). A qualitative investigation of how mothers from low income households perceive their role during family meals. Appetite, 126, 121–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trofholz AC, Thao MS, Donley M, Smith M, Isaac H, & Berge JM (2018). Family meals then and now: A qualitative investigation of intergenerational transmission of family meal practices in a racially/ethnically diverse and immigrant population. Appetite, 121, 163–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Office of Management and Budget (2018). Budget of the U.S. government Retrieved from https://www.whitehouse.gov/wp-content/uploads/2018/02/budget-fy2019.pdf
- Vaismoradi M, Turunen H, & Bondas T (2013). Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nursing & Health Sciences, 15(3), 398–405. [DOI] [PubMed] [Google Scholar]
- van Grieken A, Renders CM, Wijtzes AI, Hirasing RA, & Raat H (2013). Overweight, obesity and underweight is associated with adverse psychosocial and physical health outcomes among 7-year-old children: The “Be active, eat right” study. PLoS ONE, 8, e67383. 10.1371/journal.pone.0067383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Rinsum CE, Gerards SMPL, Rutten GM, van de Goor IAM, & Kremers SPJ (2017). Health brokers: How can they help deal with the wickedness of public health problems? BioMed Research International, 2017, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vereecken C, & Maes L (2010). Young children’s dietary habits and associations with the mothers’ nutritional knowledge and attitudes. Appetite, 54, 44–51. [DOI] [PubMed] [Google Scholar]
- Watts A, Berge J, Loth K, Larson N, & Neumark-Sztainer D (2018). The transmission of parent food and mealtime practices from adolescence to adulthood: Longitudinal findings from Project EAT-IV. Journal of Nutrition Education Behavior, 50, 141–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West F, Sanders M, Cleghorn G, & Davies P (2010). Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behavior Research and Therapy, 48, 1170–1179. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


