Abstract
Background
In order to predict in-hospital mortality in ACS (Acute Coronary Syndrome) patients based solely on clinical examination, this study compares the shock index (heart rate divided by systolic blood pressure) variable in PADMA (PADjadjaran Mortality in Acute Coronary Syndrome) with the modified shock index (heart rate divided by mean arterial pressure) score. The predictive efficacy of the PADMA score in predicting in-hospital mortality in ACS patients has been in doubt up until recently.
Methods
All ACS patients above the age of 18 who were admitted to Dr. Hasan Sadikin Central General Hospital between January 2018 and January 2023 were included in this retrospective observational cohort study. This study did not involve any interventions, and verbal informed permission was obtained with the Hasan Sadikin Hospital Ethic Committee’s approval. Multivariate logistic regression was used to gather and evaluate patient demographic, comorbidity, and clinical presentation data in order to provide two scoring systems (probability and cut-off models) that can be used to predict in-hospital all-cause death. The Fisher Z test was used to assess the area under the curve (AUC) between the PADMA SI (shock index) and PADMA MSI (modified shock index).
Results
Killip classifications III and IV, tachycardia, a high shock index, and older age were found to be independent mortality predictors and were included to the PADMA MSI score by multivariate regression analysis of 1504 people. PADMA SI score >8 has a sensitivity of 67.92% and a specificity of 84.01% for predicting all-cause death. The range of the PADMA SI score is 0 to 19. The AUC between the PADMA MSI and PADMA SI scores did not differ significantly (p=0.022).
Conclusion
Similar to the PADMA SI score, the PADMA MSI score >8 demonstrated an accurate discriminative power to forecast in-hospital mortality though it did not have significant statistic difference.
Keywords: clinical examination-based risk score, in-hospital mortality, acute coronary syndrome, MSI, SI
Introduction
The term “acute coronary syndrome” (ACS) refers to a collection of clinical manifestations of coronary artery disorders (CAD), including unstable angina pectoris (UAP), ST elevation myocardial infarction (STEMI), and non-ST elevation myocardial infarction (NSTEMI).1,2 According to statistics from the American Heart Association (AHA) and the European Society of Cardiology (ESC), there were 370.000 deaths from CAD worldwide in 2013 and 1.8 fatalities each year on average.3 According to data from the Indonesian Ministry of Health in 2018, CAD is the second most common non-infectious disease-related cause of death in Indonesia.4 Therefore, the use of a risk stratification tool to forecast mortality risk in this population is essential for achieving an early prognosis and assisting clinicians in selecting the most effective therapy strategy.
GRACE (Global Registry of Acute Coronary Events), TIMI (Thrombolysis in Myocardial Infarction), Zwolle De Luca, PAMI (Primary Angioplasty in Myocardial Infarction), Addala, and Cadillac Halkin are a few prognostic techniques that have been discovered to predict the probability of mortality in ACS patients. Pramudyo et al established the PADMA (PADjadjaran Mortality in Acute Coronary Syndrome) score to gauge the likelihood of in-hospital mortality in ACS patients. This scoring method is straightforward, equivalent to the GRACE scoring system that has been developed from multinational registry,5 and it can be performed during the initial medical contact in all healthcare facilities because it simply relies on the patient’s history and clinical examination at admission.
Two new and practical indicators for predicting mortality and major adverse cardiac events (MACE) in ACS patients are the shock index (SI) and modified shock index (MSI). But when it came to predicting death in ACS, MSI appeared to have higher sensitivity and specificity.6 As a result, the goal of this study is to improve in-hospital mortality prediction in ACS patients by modifying the PADMA scoring system utilizing MSI in place of the SI.
Methods
Study Design and Patient Selection
All ACS patients hospitalized at Dr. Hasan Sadikin Central General Hospital between January 2018 and January 2023 were included in this retrospective observational, non-interventional, single-center cohort study. The study did not include any medical records with missing or incomplete data. The Dr. Hasan Sadikin Central General Hospital’s Medical Research Ethics Committee in West Java, Indonesia gave its approval to this study. For each patient admitted to the hospital with a diagnosis of ACS, the informed patient permission was verbally obtained at the start of the trial.
Definition of Variables and Outcome
Demographic (age, female [sex], body mass index) and initial clinical presentation (heart rate, systolic blood pressure, shock index), which is calculated as heart rate divided by systolic blood pressure, Killip classification, and ST-segment deviation on ECG (Electrocardiogram) variables were taken into account in the model, as well as history and cardiovascular risk factors (hypertension, diabetes, smoking, family history of cerebrovascular and coronary artery disease). These factors were all gathered from the patient’s medical files. The main outcome was in-hospital mortality, which was determined as any death from any cause that happened during the index hospitalization following an ACS occurrence.
Statistical Analyses
IBM Corp., Armonk, New York, produced SPSS version 25.0 for use in all statistical analyses. All category data were displayed as percentages and numbers. Numerical data, on the other hand, were shown as median and interquartile range or mean and standard deviation depending on whether the distribution was normal or not. The relationship between predictors and in-hospital mortality was examined using the Chi-square and Fisher’s tests. The adjusted odds ratio was used as the input for the logistic regression analysis to get the significant p-value (p 0.05). In logistic regression using a stepwise backward approach, all significant parameters were included. According to the regression coefficient (B) from the logistic regression multivariate studies, a number was given to each independent variable to build the scoring system. Area under the curve (AUC) for predicting the desired outcome was created using a receiver operating characteristics (ROC) analysis. Additionally, the sensitivity and specificity of the PADMA MSI score as well as the optimal cut-off were generated using the de long approach. The estimated likelihood of mortality for in-hospital death was calculated using the Granger model. In order to find diagnostic value, the scoring system evaluated the prior sample. Finally, we used the Fisher Z test to compare the area under the curve (AUC) of these scoring systems in order to assess the predictive significance of the PADMA MSI and PADMA SI scores.
Results
Table 1 provides a summary of the studies’ baseline characteristics. Most of the participants in this study—1504 participants—were male (76.1%) and under the age of 65 (72.3%). The majority of patients (7%) were not fat, and 57.1% of the participants smoked. Additionally, 64.7% of the patients had hypertension. The majority of those studied had no congestion (71.3%) and stable hemodynamics, with blood pressure greater than 100 mmHg (77.1%), a heart rate of less than 100 bpm (89.7%), and modified shock index (SI) 0.57 to 0.97 (62.4%). ST Elevation was found in over half of the ECGs (61.2%). Total of 159 patients (10.5%) died while they were still in the hospital. Higher mortality risk was significantly associated with old age, female sex, smoking, patients with a history of cerebrovascular disease, increased heart rate (HR), low systolic blood pressure (SBP), MSI < 0.56 and >0.97, high Killip classification (III and IV) and ST-segment elevation myocardial infarction (STEMI) (p 0.001).
Table 1.
Baseline Characteristic of the Study Participants
| Variable | Total n=1504 | Non-Survivor n=159 | Survivor n=1345 | P value |
|---|---|---|---|---|
| Gender | ||||
| Female | 360 (23.9) | 54 (34) | 306 (22.8) | 0.002 |
| Male | 1144 (76.1) | 105 (66) | 1039 (77.2) | |
| Age (years) | ||||
| Mean ± SD | 58 ± 11 | 65 ± 11 | 57 ± 11 | <0.001 |
| Usia (tahun) | ||||
| <65 | 1088 (72.3) | 76 (47.8) | 1012 (75.2) | <0.001 |
| 65–75 | 315 (20.9) | 51 (32.1) | 264 (19.6) | |
| >75 | 101 (6.7) | 32 (20.1) | 69 (5.1) | |
| BMI (kg/m2) | ||||
| Mean ± SD | 24.4 ± 3.5 | 23.9 ± 3.6 | 24.4 ± 3.5 | 0.084 |
| BMI (kg/m2) | ||||
| <30.0 | 1399 (93) | 153 (96.2) | 1246 (92.6) | 0.093 |
| ≥30.0 | 105 (7) | 6 (3.8) | 99 (7.4) | |
| Smoking | 859 (57.1) | 81 (50.9) | 778 (57.8) | 0.096 |
| Diabetes melitus | 378 (25.1) | 49 (30.8) | 329 (24.5) | 0.081 |
| Hypertension | 973 (64.7) | 106 (66.7) | 867 (64.5) | 0.582 |
| Family history of CAD | 190 (12.6) | 19 (11.9) | 171 (12.7) | 0.784 |
| History of cerebrovascular | 239 (15.9) | 29 (18.2) | 210 (15.6) | 0.392 |
| History of angina | 537 (35.7) | 63 (39.6) | 474 (35.2) | 0.276 |
| History of revascularization | 306 (20.3) | 25 (15.7) | 281 (20.9) | 0.126 |
| SBP (mmHg) | ||||
| Mean ± SD | 123 ± 24 | 110 ± 30 | 125 ± 22 | <0.001 |
| SBP (mmHg) | ||||
| ≤100 | 344 (22.9) | 69 (43.4) | 275 (20.4) | <0.001 |
| >100 | 1160 (77.1) | 90 (56.6) | 1070 (79.6) | |
| HR (beats per minute) | ||||
| Mean ± SD | 78 ± 21 | 81 ± 33 | 78 ± 20 | 0.004 |
| HR (beats per minute) | ||||
| ≤100 | 1349 (89.7) | 121 (76.1) | 1228 (91.3) | <0.001 |
| >100 | 155 (10.3) | 38 (23.9) | 117 (8.7) | |
| MSI | ||||
| Mean ± SD | 0.88 ± 0.29 | 1.01 ± 0.50 | 0.86 ± 0.25 | <0.001 |
| MSI | ||||
| <=0.56 | 126 (8.4) | 31 (19.5) | 95 (7.1) | |
| 0.57–0.97 | 938 (62.4) | 42 (26.4) | 896 (66.6) | |
| >0.97 | 440 (29.3) | 86 (54.1) | 354 (26.3) | |
| ACS | ||||
| STEMI | 920 (61.2) | 110 (69.2) | 810 (60.2) | 0.028 |
| NSTEMI/UAP | 584 (38.8) | 49 (30.8) | 535 (39.8) | |
| KILIP | ||||
| I | 1073 (71.3) | 58 (36.5) | 1015 (75.5) | <0.001 |
| II | 239 (15.9) | 25 (15.7) | 214 (15.9) | |
| III | 41 (2.7) | 13 (8.2) | 28 (2.1) | |
| IV | 151 (10) | 63 (39.6) | 88 (6.5) |
Abbreviations: BMI, body mass index; CAD, coronary artery disease; SBP, systolic blood pressure; HR, heart rate.
The results of the bivariate and multiple regression analyses are displayed in Table 2. Independence predictor in mortality were age 65–75 years [AOR=2.461 (95% CI=1.602–3.78); P<0.001], age >75 years [AOR=4.883 (95% CI=2.707–8.806); P<0.001], history of angina [AOR=1.73 (95% CI=1.114–2.688); P=0.015], history of revascularization [AOR=2.096 (95% CI=1.132–3.879); P=0.018], heart rate >100 bpm [AOR=1.426 (95% CI=0.834–2.439); P=0.195], MSI 0.57–0.97 [AOR= 4.399 (95% CI=2.474–7.823); P=0.001], MSI >0.97 [OR=2.967 (95% CI=1.824–4.825); P<0.001], Killip III [OR= 4.433 (95% CI=2.025–9.703); P<0.001], and Killip IV [OR=7.132 (95% CI=4.267–11.919); P<0.001].
Table 2.
Logistic Regression Analysis of in-Hospital Mortality Risk
| Variable | Crude OR (95% CI) | p-value | AOR (95% CI) | p-value |
|---|---|---|---|---|
| Gender | ||||
| Female | 1.746 (1.228–2.483) | 0.002 | 1.489 (0.937–2.366) | 0.092 |
| Male | 1 (ref) | 1 (ref) | ||
| Age (years) | ||||
| <65 | 1 (ref) | 1 (ref) | ||
| 65–75 | 2.572 (1.760–3.761) | <0.001 | 2.461 (1.602–3.78) | <0.001 |
| >75 | 6.175 (3.823–9.976) | <0.001 | 4.883 (2.707–8.806) | <0.001 |
| BMI (kg/m2) | ||||
| <30.0 | 1 (ref) | 1 (ref) | ||
| ≥30.0 | 0.494 (0.213–1.144) | 0.093 | 0.644 (0.26–1.597) | 0.342 |
| Smoking | 0.757 (0.545–1.052) | 0.096 | 1.102 (0.716–1.696) | 0.660 |
| Diabetes melitus | 1.376 (0.961–1.969) | 0.081 | 1.129 (0.732–1.742) | 0.582 |
| Hypertension | 1.103 (0.778–1.562) | 0.582 | 1.208 (0.792–1.844) | 0.380 |
| Family history of CAD | 0.932 (0.562–1.544) | 0.784 | 1.012 (0.541–1.892) | 0.970 |
| History of cerebrovascular | 1.206 (1.785–1.851) | 0.392 | 1.211 (0.681–2.154) | 0.514 |
| History of angina | 1.206 (0.861–1.689) | 0.276 | 1.73 (1.114–2.688) | 0.015 |
| History of revascularization | 0.706 (0.452–1.104) | 0.126 | 2.096 (1.132–3.879) | 0.018 |
| SBP (mmHg) | ||||
| ≤100 | 2.983 (2.122–4.193) | <0.001 | 1.081 (0.676–1.727) | 0.745 |
| >100 | 1 (ref) | 1 (ref) | ||
| HR (bpm) | ||||
| ≤100 | 1 (ref) | 1 (ref) | ||
| >100 | 3.296 (2.186–4.971) | <0.001 | 1.426 (0.834–2.439) | 0.195 |
| Modified score index (MSI) | ||||
| ≤0.56 | 6.961 (4.180–11.593) | <0.001 | 4.399 (2.474–7.823) | <0.001 |
| 0.57–0.97 | 1 (ref) | 1 (ref) | ||
| >0.97 | 5.183 (3.513–7.647) | <0.001 | 2.967 (1.824–4.825) | <0.001 |
| ACS | ||||
| STEMI | 1.483 (1.041–2.112) | 0.028 | 1.284 (0.848–1.944) | 0.238 |
| NSTEMI/UAP | 1 (ref) | 1 (ref) | ||
| KILIP | ||||
| I | 1 (ref) | 1 (ref) | ||
| II | 2.044 (1.251–3.342) | 0.004 | 1.361 (0.803–2.308) | 0.252 |
| III | 8.125 (3.999–16.510) | <0.001 | 4.433 (2.025–9.703) | <0.001 |
| IV | 12.528 (8.249–19.028) | <0.001 | 7.132 (4.267–11.919) | <0.001 |
Abbreviations: BMI, body mass index; CAD, coronary artery disease; SBP, systolic blood pressure; STEMI, ST-elevation myocardial infarction; NSTEMI, non-ST segment elevation myocardial infarction; UAP, unstable angina pectoris; OR, odds ratio; AOR, adjusted odds ratio; bpm: beat per minute.
Table 3 explains several independently predicted variables that were calculated as a new score system. Regression coefficient (B) from multivariate logistic regression is used to determine the score, which ranges from 0 to 19. Based to the findings, Killip II has the lowest score with 1 point, history of angina has the second-highest score with 2 points, and people between the ages of 65 and 75 have the lowest score with 7. Killip III has the highest score with 3 points, people over 75, and the MSI is between 0.56 and 0.97. Killip IV has the lowest score with 7 points.
Table 3.
Assessment of the Score Value from Each Independent Predictor Factor
| Variable | B | SE | B/SE |  |
Score |
|---|---|---|---|---|---|
| Age (years) | |||||
| <65 (ref) | |||||
| 65–75 | 0.952 | 0.214 | 4.45 | 3.42 | 3 |
| >75 | 1.676 | 0.288 | 5.82 | 4.48 | 4 |
| History of angina | 0.504 | 0.22 | 2.29 | 1.76 | 2 |
| No history of revascularization | 0.659 | 0.284 | 2.32 | 1.79 | 2 |
| Modified shock index | |||||
| ≤0.70 (ref) | |||||
| 0.71–1.00 | 1.557 | 0.289 | 5.39 | 4.15 | 4 |
| >1.00 | 1.232 | 0.219 | 5.63 | 4.33 | 4 |
| Killip class | |||||
| I (ref) | |||||
| II | 0.343 | 0.264 | 1.30 | 1.00 | 1 |
| III | 1.593 | 0.389 | 4.10 | 3.15 | 3 |
| IV | 2.031 | 0.234 | 8.68 | 6.68 | 7 |
Notes: Modified shock index is calculated by heart rate divided by mean arterial pressure.
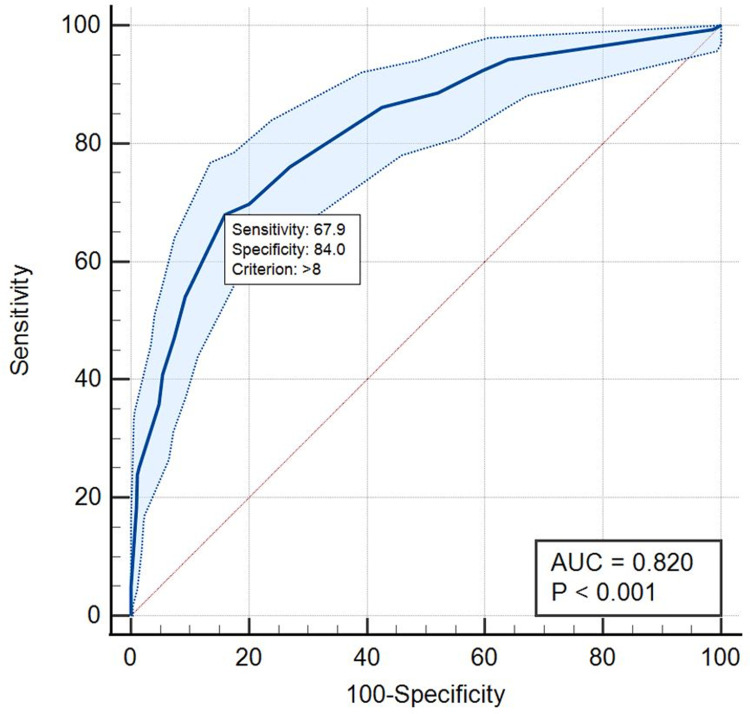
The scoring model for mortality events is presented in Table 4; the higher the score, the greater the likelihood of fatality, which shows a dose–response relationship. AUC, sensitivity, and specificity of this scoring system in predicting in-hospital mortality were identified with values of 0.820, 67.92%, and 84.01%, respectively, according to ROC analysis with a cut-off of >8 (Table 5 and Figure 1).
Table 4.
Scoring System Based on Patient’s Probability on Mortality Event
| Scoring | Probability (%) |
|---|---|
| 0 | 1.1 |
| 1 | 1.6 |
| 2 | 2.1 |
| 3 | 2.9 |
| 4 | 3.9 |
| 5 | 5.2 |
| 6 | 7.0 |
| 7 | 9.3 |
| 8 | 12.3 |
| 9 | 16.1 |
| 10 | 20.7 |
| 11 | 26.3 |
| 12 | 32.8 |
| 13 | 40.0 |
| 14 | 47.7 |
| 15 | 55.4 |
| 16 | 62.9 |
| 17 | 69.9 |
| 18 | 76.0 |
| 19 | 81.2 |
Table 5.
ROC Analysis as Mortality Scoring System Model
| Variable | AUC (95% CI) | p-value | Cut-off Value | Diagnostic Value |
|---|---|---|---|---|
| Score | 0.820 (0.800–0.839) | <0.001 | >8 | Sensitivity: 67.92% |
| Specificity: 84.01% | ||||
| PPV: 33.4% | ||||
| NPV: 95.7% | ||||
| LR+: 4.25 | ||||
| LR-: 0.38 |
Abbreviations: AUC, area under curve; PPV, positive predictive value; NPV, negative predictive value; LR, likelihood ratio.
Figure 1.
ROC curve score to predict mortality.
Data from February 2023 to June 2023 was used for validation cohort which consist of 156 patients. We found the sensitivity difference between derivation and validation cohort which are 67.92% and 38.46%, respectively. Specificity was slightly higher in validation group 90.91% compared to derivation group 84.01%.
A major finding from this analysis is that the scoring systems between derivation and cohort have different performance, sensitivity was lower in validation data but specificity was higher in validation data (Table 6). Validation cohort data might not be comparable to derivation data due to its limitation in sample volume.
Table 6.
Scoring System Model Validation Analysis on Mortality
| Variable | Diagnostic Value | Derivation (n=1504) | Validation (n=156) |
|---|---|---|---|
| Score>8 | Sensitivity | 67.92% | 38.46% |
| Specificity | 84.01% | 90.91% | |
| PPV | 33.4% | 27.8% | |
| NPV | 95.7% | 94.2% | |
| LR+ | 4.25 | 4.23 | |
| LR- | 0.38 | 0.68 |
Abbreviations: PPV, positive predictive value; NPV, negative predictive value; LR, likelihood ratio.
Additionally, using the PADMA SI score’s three risk categories (low risk: 0–2, moderate risk: 3–6, and high risk: 7–19), we ran the Granger model to predict the occurrence of mortality events. According to the PADMA MSI model, the probabilities of mortality at low, moderate, and high risk were 2.1%, 2.9–7.0%, and >7.0%, respectively (Table 7).
Table 7.
PADMA MSI Scoring System Based on Patient’s Probability on Mortality Event
| Risk Category (Tertiles) | PADMA MSI Score | Probability of Death |
|---|---|---|
| Low | 0−2 | <2.1 |
| Intermediate | 3−6 | 2.9–7.0 |
| High | 7−19 | >7.0 |
Abbreviation: PADMA, PADjadjaran Mortality in Acute coronary syndrome.
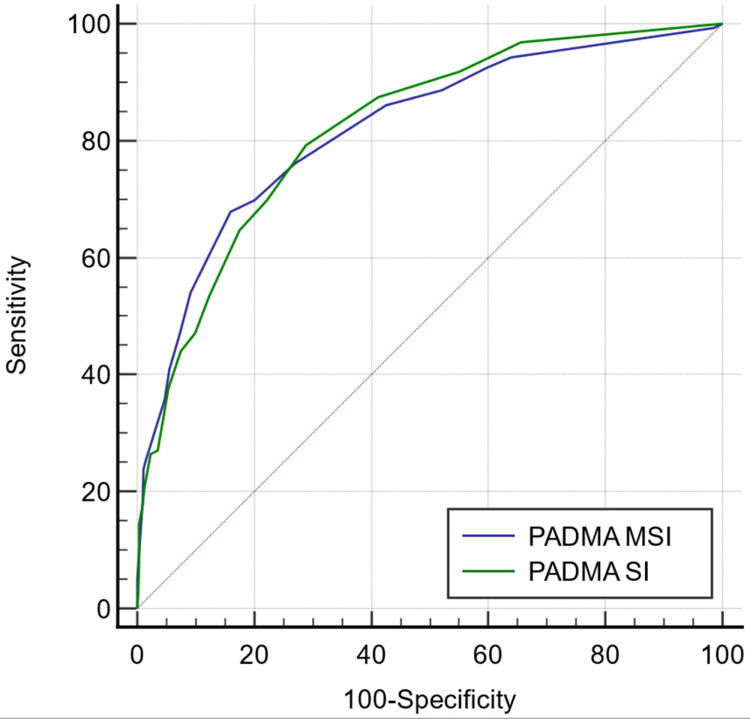
The ROC analysis revealed that predictive value between the PADMA MSI score and PADMA SI score was not significantly different for predicting the in-hospital mortality (p=0.388) (Table 8).
Table 8.
ROC Analysis Result Between PADMA MSI and PADMA Scoring System Based on Mortality
| Variable | AUC (95% CI) | AUC Difference (95% CI) | p-value |
|---|---|---|---|
| PADMA MSI score | 0.820 (0.800–0.839) | −0.022 (−0.073–0.029) | 0.388 |
| PADMA score | 0.842 (0.821–0.861) |
Abbreviations: PADMA, PADjadjaran Mortality in Acute coronary syndrome; AUC, area under curve.
Comparison of AUC of PADMA MSI score with PADMA SI risk scores to predict in-hospital mortality showed no significant statistical difference Figure 2.
Figure 2.
Comparison of AUC of PADMA MSI score with PADMA SI risk scores to predict in-hospital mortality.
Discussion
The following are the main conclusions of this cohort study. First, age, a history of cerebrovascular illness, heart rate, SI, and Killip class made up the PADMA SI score. These elements differ slightly from the PADMA MSI score, which substituted revascularization history and angina history for cerebrovascular disease. This is because the regression model’s mortality prediction was significant. The cause is still a mystery. Second, the correlation between PADMA scores and in-hospital mortality in ACS patients revealed that the mortality risk increased with each increase in score. Both the PADMA MSI and PADMA SI scores were divided into three risk categories: low, intermediate, and high. The likelihood of in-hospital mortality was 2.1; 2.9–7.0; >7.0; and 3%; 3%; and 6.8%; respectively. Thirdly, a high PADMA MSI score significantly increased the risk of in-hospital mortality using the cut-off of >8, with AUC, sensitivity, and specificity being 0.820, 67.82%, and 84.01%, respectively, compared to a PADMA score of 0.842, 82.78%, and 72.35%. Fourth, when it was used for estimating the likelihood of in-hospital death in ACS patients, the PADMA MSI score’s predictive value was on par with the PADMA SI scores. As a result, the PADMA MSI score may be an alternative prognosticator of in-hospital mortality in ACS patients. Two important elements of the PADMA MSI score are the patient’s demographics and hemodynamic condition at admission. Age, angina history, and revascularization history all reflect demographic status. In contrast, the Killip class, SI, and HR all indicate hemodynamic state. Given that each component of this system of scoring had a mechanism that was related to mortality, they were all statistically significant, independent, increased mortality in ACS patients, and were reasonable to be included.
The current study found that an older age was one of the independent predictors of mortality, with mortality risk being 2.5 times and 6 times higher for those aged 65 to 75 and >75 years than for those aged 65 years. According to previous two cohort studies, patients who were older (>65 years and >75 years) had a considerably higher chance of dying from ACS.7,8 Additionally, there are a number of reasons why elderly individuals with ACS tend to arrive with a high mortality risk. The cause is that elderly individuals are more likely to present with atypical ACS symptoms that delay diagnosis and treatment and have a higher risk of bleeding that makes revascularization therapies more challenging, such as comorbidities like hypertension and kidney diseases. These factors also increase the likelihood that ACS remains undiagnosed and untreated.9
In contrast to the PADMA SI score, which identified cerebrovascular illness as one of the characteristics predicting in-hospital death, the PADMA MSI score found that prior angina and prior revascularization were significant predictors of in-hospital mortality.10 This might be the result of angina, which is a symptom of ongoing ischemia and necessitates immediate revascularization, the main goal of treating ACS.
We altered the Shock Index (SI) to the Modified Shock Index (MSI) as a parameter in our study, which is another intriguing conclusion from our research. HR and MAP are the two key parts of the MSI. Numerous studies established a strong correlation between high MSI and a greater mortality risk in ACS groups. We classified MSI into three groups for this study: <0.56, 0.57–0.97, and >0.97. According to this study, patients with low MSI (0.56) and high MSI (>0.97) had a 6.9-fold and a 5-fold higher risk of mortality, respectively, compared to those with MSI (0.57–0.97). This result is consistent with the findings of other cohort studies, which showed that patients with ACS had a considerably higher risk of mortality when their MSI was <0.7 or >1.3.
In this study, compared to patients with low HR (<100), patients with high HR (>100) at admission had increased mortality that was approximately three times greater. High admission HR was independently associated with mortality in ACS patients, according to earlier investigations that supported this finding. Higher catecholamine levels in ACS patients were associated with lower ejection fraction, according to a study by Petterson et al. Additionally, sympathetic activation can trigger ischemia-induced ventricular fibrillation and result in sudden cardiac death. According to Yuksek et al, ACS patients who had raised HR were more likely to develop acute cardiac failure and had greater troponin and glucose levels.11,12
The PADMA MSI scoring system substitutes MSI for SI. According to a study by Vani et al, MSI has a sensitivity of 61.1% and a specificity of 73.7% for predicting hospital mortality as opposed to SI’s 49% and 85%.6 In addition, MSI and GRACE do not significantly differ when compared, with AUCs of 0.715 and 0.815, respectively.6 According to this study, the MSI had a normal value between 0.57 and 0.97. This might be caused by the intricate process of the RAAS’s (Renin-Angiotensin-Aldosterone System) hemodynamic response to ACS. Low mean arterial pressure and low heart rate result in high MSI, while the opposite is true for low heart rate and high mean arterial pressure. These two situations indicate impaired hemodynamics, which could aggravate conditions and increase mortality.
There are a few limitations on this study. Firstly, only one center was used for this study, and the sample size was small. Second, recall and selection bias may result from it, based on its retrospective design. Third, this scoring can only be used for predicting in-hospital mortality due to the significant loss to follow-up. Last but not least, a multi-center cohort study with many participants and a longer duration of follow-up is still required to further validate this scoring system in order to evaluate the relationship between the PADMA MSI score and mortality in ACS patients.
Conclusion
This study evaluated PADMA MSI score and PADMA with age, history of angina and revascularization, HR, MSI, and Killip class as well as other factors like age and Killip class to predict in-hospital mortality in ACS patients. This study demonstrated a dose–response relationship between the PADMA MSI score and in-hospital mortality. Additionally, similar to the PADMA score, this scoring system had a strong predictive value for predicting in-hospital mortality. As a result, there was no statistically significant difference between the PADMA MSI and PADMA SI scoring systems in terms of their ability to predict in-hospital mortality in ACS patients.
Acknowledgments
There are no acknowledgements in this review.
Funding Statement
There is no funding in this review.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from Raymond Bernardus (raymondbernardus@yahoo.com) on reasonable request.
Ethical Approval
This study conducted following the 1964 Declaration of Helsinki and its subsequent amendments. The study was approved by the Medical Research Ethics Committee of Dr. Hasan Sadikin General Hospital with ethical registration number LB.02.01/X.6.5/3/2022 and informed consent was obtained from all participants. Verbal consent was obtained.
Disclosure
Dr Miftah Pramudyo reports grants from inaACC, during the conduct of the study. The authors declare that they have no other conflicts of interest.
References
- 1.Kumar A, Cannon CP. Acute coronary syndromes: diagnosis and management, part I. Mayo Clin Proc. 2009;84:917–938. doi: 10.4065/84.10.917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dokter P, Kardiovaskular S, Ketiga E. Pedoman Tatalaksana Sindrom Koroner Akut Edisi Ketiga; 2015.
- 3.Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393 [DOI] [PubMed] [Google Scholar]
- 4.Kemenkes RI. Hasil Riset Kesehatan Dasar Tahun [Basic Health Research Result Year 2018]; 2018. Indonesian.
- 5.Tang EW, Wong CK, Herbison P. Global Registry of Acute Coronary Events (GRACE) hospital discharge risk score accurately predicts long-term mortality post acute coronary syndrome. Am Heart J. 2007;153:29–35. doi: 10.1016/j.ahj.2006.10.004 [DOI] [PubMed] [Google Scholar]
- 6.Pramudyo M, Marindani V, Achmad C, Putra ICS. Modified shock index as simple clinical independent predictor of in-hospital mortality in acute coronary syndrome patients: a retrospective cohort study. Front Cardiovasc Med. 2022;9:1–7. doi: 10.3389/fcvm.2022.915881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elbarouni B, Goodman SG, Yan RT, et al. Validation of the Global Registry of Acute Coronary Event (GRACE) risk score for in-hospital mortality in patients with acute coronary syndrome in Canada. Am Heart J. 2009;158:392–399. doi: 10.1016/j.ahj.2009.06.010 [DOI] [PubMed] [Google Scholar]
- 8.Shahawy S. Pathophysiology of Heart Disease; 2012.
- 9.Fox KAA, Goldberg RJ, Pieper KS, et al. Prediction of risk of death and myocardial infarction in the six months after presentation with acute coronary syndrome: prospective multinational observational study (grace). BMJ. 2006;333:1091. doi: 10.1136/bmj.38985.646481.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pramudyo M, Bijaksana TL, Yahya AF, Putra ICS. Novel scoring system based on clinical examination for prediction of in-hospital mortality in acute coronary syndrome patients: a retrospective cohort study. Open Hear. 2022;9:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cannon CP, Brindis RG, Chaitman BR, et al. 2013 ACCF/AHA Key data elements and definitions for measuring the clinical management and outcomes of patients with acute coronary syndromes and coronary artery disease: a report of the American college of cardiology foundation/American Heart Association. Circulation. 2013;127:1052–1089. doi: 10.1161/CIR.0b013e3182831a11 [DOI] [PubMed] [Google Scholar]
- 12.Yuksek U, Yaman B, Kemal H, Etikan L, Akpınar O, Duygu HCL. Increased discharge heart rate might be associated with increased short-term mortality after acute coronary syndrome. Acta Cardiol. 2021;7:1. [DOI] [PubMed] [Google Scholar]