Abstract
Objective
Contact frequency with adult children plays a critical role in late-life depression. However, evidence on possible moderators of this association remains limited. Moreover, considering alterations in contact modes after the coronavirus disease-2019 pandemic, there is a need to investigate this association post-pandemic to develop effective therapeutic interventions.
Methods
This study included 7,573 older adults who completed the Living Profiles of the Older People Survey in Korea. Participants’ contact frequency and depressive symptoms were analyzed. Regression analysis was performed after adjusting for covariates. The moderating effects of variables were verified using a process macro.
Results
Multivariable logistic regression analysis revealed that infrequent face-to-face (odd ratio [OR]=1.86, 95% confidence interval [CI]=1.55–2.22) and non-face-to-face contact (OR=1.23, 95% CI=1.04–1.45) in the non-cohabitating adult children group was associated with a higher risk of late-life depression compared to that in the frequent contact group. Linear regression analysis indicated consistent results for face-to-face and non-face-to-face contact (estimate=0.458, standard error [SE]=0.090, p<0.001 and estimate=0.236, SE=0.074, p=0.001, respectively). Moderation analysis revealed that the association between late-life depression and frequency of face-to-face contact was moderated by age, household income quartiles, number of chronic diseases, physical activity frequency, presence of spouse, nutritional status, and whether the effect of frequency of non-face-to-face contact on late-life depression was increased by participation in social activity, frequent physical activity, and good cognitive function (p for interaction<0.05).
Conclusion
Frequent contact with non-cohabitating children lowers the risk of depression later in life. Several variables were identified as significant moderators of contact frequency and depression symptoms.
Keywords: Depression, Older adults, Non-cohabitating children, Social contact
INTRODUCTION
Late-life depression is associated with deterioration in function and quality of life among older adults and is emerging as a major global problem given the increase in the older adult population [1]. Late-life depression is a multidimensional disease that requires intervention using a biopsychosocial approach [2]. Several studies have reported that social support and interpersonal interactions improve depressive symptoms in late life [3-5]. Social engagements decrease in later adulthood due to retirement, health issues, and bereavement [6]. Recent reductions in family size and rapid simplification of generations have exacerbated this decrease. Thus, single older households are becoming a general type of household in late life emphasizing the need to promote social engagement to mitigate late-life depression [7].
Among the various forms of social engagement in late life, interactions with families are of particular importance. Several studies have demonstrated that older single households are more vulnerable to depression compared to households with family members [8,9], which supports the importance of familial interactions. Studies on the effects of interaction with families on late-life depression are being actively conducted. Previous studies have reported that depressive symptoms increase as the frequency of face-to-face contact with family members decreases [10], and the risk of depression is highest in older adults with a low frequency of face-to-face and phone calls with non-cohabitating adult children [11]. Another study reported that face-to-face contact has a unique impact on reducing late-life depression when social contact among older adults was classified as face-to-face or non-face-to-face [12].
Nevertheless, the majority of these studies were conducted before the 2010s. Accordingly, it is necessary to re-examine late-life depression considering the increased number of older single households and greater reduction in family size. In addition, no study to date has identified specific groups that are more strongly affected by the frequency of contact with non-cohabitating children, which has resulted in non-selective, less efficient intervention strategies. Considering the notable increase in depression among older adults whose frequency of face-to-face contact decreased after the coronavirus disease-2019 (COVID-19) outbreak and the observation that increased non-face-to-face contact frequency did not compensate for the decrease in face-to-face contact [13], there is an urgent need to investigate the effects of altered mode of contact with non-cohabitating children after the COVID-19 pandemic.
Therefore, this study aimed to assess the correlation between the frequency of face-to-face and non-face-to-face contact with non-cohabitating adult children and late-life depression after the COVID-19 pandemic. We hypothesized 10 possible moderators and evaluated the moderating effect of each moderator on the correlation. Identifying groups of older adults that are more affected by contact with their children will provide deeper understanding of the relationship between late-life depression and family contact in older adults, thus affording novel insights for intervention targets in the community.
METHODS
Participants
Participants were recruited from the Living Profiles of Older People Survey (LPOPS) conducted by the Ministry of Health Welfare and Family in 2020. LPOPS 2020 is a nationwide representative survey conducted from September 14, 2020 to November 20, 2020 across 17 cities and provinces in Korea. A stratified cluster sampling method based on geographic and demographic information was applied. This was a population survey of senior citizens aged 65 years or older living in general residential facilities. Participants were informed of the survey face-to-face by trained interviewers who visited the participants’ homes. After sufficient explanation was provided and consent was received, the survey was conducted using the Tablet-PC assisted personal interview method. Confidentiality and anonymity were guaranteed. We obtained permission to use the study data from the Korea Institute for Health and Social Affairs.
Individuals who met the following criteria were excluded from the analysis: no adult children, living with adult children, cognitive decline, disability affecting survey performance (brain lesions, hearing and/or speech impairments, and intellectual disability), missing main outcome data (Korean version of the short form of the Geriatric Depression Scale [SGDS-K] score), missing covariates, or main exposure. For cognitive decline, as the LPOPS 2020 is a community-based survey, this study circulated the mean and standard deviation (SD) from the survey population (n=10,097). The mean 2 SD of the survey was 13.011. This study defined participants with the Mini-Mental State Examination-Dementia Screening (MMSE-DS) score <13 points as having cognitive impairment, and these participants were excluded. In total, 7,573 participants were included in the final analysis (Figure 1).
Figure 1.
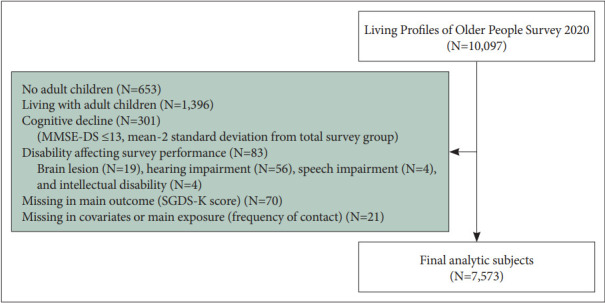
Flow chart of participants. MMSE-DS, Mini Mental State Examination-Dementia Screening; SGDS-K, Korean version of the 15-item Geriatric Depression Scale.
The study was approved by the Institutional Review Board of Ajou University Hospital (AJOUIRB-EX-2023-016). At the time of the survey, written informed consent was obtained from all participants.
Assessments and measurements
Depression
Late-life depression was the primary outcome of interest. To measure depression, the SGDS-K developed by Yesavage and Sheikh [14] and localized by Bae and Cho [15] was used. This scale consists of 15 questions and responses are designated “yes” or “no.” The SGDS-K scores range from 0 to 15 and are strongly correlated with the 30-item Korean version of the Geriatric Depression Scale [16]. A higher combined score indicates greater severity of depression. Positive questions were reversely converted to scores. A community-based study in Korea suggested that the optimal cutoff point for screening major depressive disorder was an SGDS-K score ≥8, and the sensitivity and specificity of the findings were 93.6% and 76.0%, respectively. The SGDS-K has satisfactory reliability (Cronbach’s α=0.90) and validity [14,15,17]. In this study, a binary divided variable based on an SGDS-K score of 8 points and continuous variable based on the total score were used for analysis.
Frequency of contact
The frequency of contact with non-cohabitating adult children was the primary exposure of interest and was assessed using written questions posed by trained interviewers. Participants were asked, “How often have you met your children living separately over the past year?” and “How often have you been in touch with your children living separately over the past year? (mutual response options were available for e-mail, letter, etc.).” Seven response options were available for the two questions, ranging from 1 (“more than 4 times a week”) to 7 (“hardly ever”).
Several studies have suggested accurate classification criteria for the frequency of social contact with non-cohabitating children; however, a previous study demonstrated that latelife depression increased as the frequency of visits/contact with children decreased [18]. In addition, talking on the phone more than once a week and having face-to-face contact at least once a month was associated with a lower risk of developing depression in older adults compared to that of those who lacked this contact [11]. However, this study was conducted before the COVID-19 outbreak. Considering the responses of the LPOPS survey, decreased frequency of face-to-face contact due to the COVID-19 pandemic and social distancing policies, and increased frequency of non-face-to-face contact, which is less burdensome [19-21], this study divided the frequency of contact using different standards. The frequency of face-to-face contact was classified as at least once every 3 months or less, and the frequency of non-face-to-face contact was classified as at least twice a week or less. The classification was determined dichotomously by assessing the number of contact frequencies corresponding to the 50th percentile, referring to studies conducted after the COVID-19 outbreak [13,22]. Based on this new classification, this study was able to identify intuitive and realistic intervention cutoff points for contact frequency and create a campaign with a public purpose.
Covariates
The covariates assessed in this study were age, sex, years of education, quartiles of household income, area of residence, current smoking, alcohol intake, number of chronic diseases diagnosed by physicians, cognitive function, presence of spouse, and the number of non-cohabitating adult children. The categories of alcohol intake and household income quartiles were derived based on the entire population of LPOPS study participants.
Residency was defined using the Korean administrative division system. The smallest subdivision level of the rural government, i.e., town (eup) or township (myeon), was defined as rural. The smallest subdivision level of the urban government, i.e., neighborhood (dong), was classified as urban.
The number of chronic diseases was counted when older adults responded that they had a physician-diagnosed disease. The questionnaire included seven cardiovascular diseases (hypertension, stroke, hyperlipidemia, angina pectoris, myocardial infarction, heart failure, and arrhythmia), two endocrine diseases (diabetes and thyroid disease), five musculoskeletal diseases (arthritis, osteoporosis, back pain, sciatica, and fracture or aftereffect of accident), three pulmonary diseases (chronic obstructive pulmonary disease, asthma, and tuberculosis), four cardiovascular diseases (cataracts, glaucoma, chronic otitis media, and senile hearing loss), oncologic diseases (all cancers), three gastrointestinal diseases (ulcer or gastritis, hepatitis, and liver cirrhosis), three genitourinary diseases (chronic kidney disease, benign prostate hyperplasia, and urinary incontinence), and other diseases (anemia and chronic dermatologic disease).
Cognitive function was measured using the MMSE-DS. Han et al. [23] standardized the MMSE-DS, thereby improving the limitations of the Korean version of MMSE, and prepared a cognitive function evaluation tool that accurately reflects the demographic and cultural characteristics of older adults in Korea. The reliability (Cronbach’s α=0.826) and validity of these tools have been verified [23]. The MMSE-DS includes items for orientation, memory registration and recollection, concentration, naming, language, understanding, and judgment. The scores ranged from 0 to 30, with higher scores indicating better cognitive function. In this study, the cutoff point of the MMSEDS for cognitive decline was defined as 13 or lower (mean minus 2 SD of the total participants). In this process, we did not use the existing suggested MMSE-DS cutoff values to define cognitive impairment. The reason we wanted to exclude patients with cognitive impairment was due to recall bias, and considering this, we determined that a somewhat stricter definition was necessary rather than a broad one.
Possible moderators
Ten possible moderators were suggested in this study: sex, age, quartiles of household income, total number of chronic diseases, participation in social activities, participation in religious activities, frequency of physical activity (days per week), cognitive function, presence of spouse, and nutritional status. Previous studies have reported that each of the 10 possible moderators is associated with social contact or depression. The effects of age, sex, and social interactions on the mental health of older adults are well-established. With regards to social interaction, religious activity has been reported to reduce depression [24] and social support from friends has been demonstrated to act as a buffer in relation to negative life events and depressive symptoms [12,25]. Previous studies have indicated that both friends and spouses are strongly associated with depression [26]. Further, reports suggest that social activity is closely related to physical activity, and several studies have demonstrated that physical activity itself is closely associated with mental health [27]. Further, health conditions are strongly related to depression in older adults, and social support from children may attenuate the symptoms [28]. Based on these results, health conditions can be subdivided into the total number of chronic diseases, cognitive function, and nutritional status [28-31]. In addition, the lower the income, the greater the effectiveness of depression-related social support for reducing depression [32]. Thus, these variables were considered to have moderating effects on the relationship between contact with non-cohabitating adult children and late-life depression. Based on above studies, three geriatric psychiatrists selected 10 possible moderators after in-depth discussions.
With regard to household income quartiles, number of chronic diseases, and cognitive function, definitions used for covariables were applied. Nutritional status was measured using the “Determine Your Nutrition Health” checklist developed by the Nutrition Screening Initiative (NSI). The total score was 21 points, which was calculated using 10 items of the NSI, (0 to 2 points, good; 3 to 5 points, moderate nutritional risk; and 6 or more points, high nutritional risk).
Statistical analysis
Descriptive statistics were computed. For each contact frequency group, categorical and continuous variables were compared using the chi-square test and t-test/analysis of variance for trends, respectively. For depression, two variables were used: a binary variable based on the SGDS-K score of 8 points and a continuous variable using the total score. After checking for multicollinearity, logistic regression and linear regression analyses were used to examine the association between the frequency of contact and risk of late-life depression. The Hosmer–Lemeshow test and Durbin–Watson statistics were used to confirm the goodness-of-fit of the regression model. Regression analysis using process macro v.4.0 (model 1; https://www.processmacro.org) was conducted to determine the interactional effects of the various possible moderators. Unadjusted and adjusted odds ratios (ORs) were calculated using 95% confidence intervals (CIs). A p<0.05 were considered statistically significant. Data were analyzed using Statistical Package for Social Sciences (IBM SPSS Statistics 28.0; IBM Corp., Armonk, NY, USA).
RESULTS
General characteristics of participants
The general characteristics of the participants according to frequency of the contact group are presented in Table 1. The mean age of participants was 73.2 (SD=6.3) years. Of participants, 41.4% were males and 58.6% were female. The mean number of years of education of the participants was 8.4 (SD=3.9) years. Household income was categorized into a quartile variable based on 10,097 persons in the first draft, with ratios of 26.8%, 27.8%, 27.2%, and 18.2% according to each income level. Of participants, 69.9% lived in urban areas, 11.1% were current smokers, and 37.6% were current drinkers. The mean number of chronic diseases was 1.8 (SD=1.5), and the mean MMSE-DS score was 25.0 (SD=4.0). Among the study participants, 63.4% had a spouse. The mean number of non-cohabitating adult children was 2.9 (SD=1.2). Significant baseline group differences were observed in the years of education, household income quartiles, area of residency, and alcohol intake in the frequent and less frequent face-to-face contact groups. In the frequent or less frequent non-face-to-face contact group, significant baseline group differences were observed in sex, household income quartiles, and area of residency.
Table 1.
Baseline characteristics of study participants by frequency of contact
| Variable | Total (N=7,573) | Face-to-face contact |
Non-face-to-face contact |
|||||
|---|---|---|---|---|---|---|---|---|
| ≥1 time/3 months (N= 6,233) | <1 time/3 months (N=1,340) | p | ≥2 times/week (N=2,421) | <2 times/week (N= 5,152) | p | |||
| Age (yr) | 73.2±6.3 | 73.2±6.3 | 73.6±6.0 | 0.081 | 73.2±6.6 | 73.3±6.1 | <0.001 | |
| Sex | 0.021 | <0.001 | ||||||
| Male | 3,133 (41.4) | 2,541 (40.8) | 592 (44.2) | 887 (36.6) | 2,246 (43.6) | |||
| Female | 4,440 (58.6) | 3,692 (59.2) | 748 (55.8) | 1,534 (63.4) | 2,906 (56.4) | |||
| Years of education (yr) | 8.4±3.9 | 8.4±3.9 | 8.1±4.1 | 0.153 | 8.4±4.1 | 8.3±3.8 | <0.001 | |
| Quartiles (Q) of household income | <0.001 | <0.001 | ||||||
| Q1, lowest | 2,028 (26.8) | 1,684 (27.0) | 344 (25.7) | 638 (26.4) | 1,390 (27.0) | |||
| Q2 | 2,109 (27.8) | 1,634 (26.2) | 475 (35.4) | 623 (25.7) | 1,486 (28.8) | |||
| Q3 | 2,059 (27.2) | 1,717 (27.5) | 342 (25.5) | 647 (26.7) | 1,412 (27.4) | |||
| Q4, highest | 1,377 (18.2) | 1,198 (19.2) | 179 (13.4) | 513 (21.2) | 864 (16.8) | |||
| Area of residency | <0.001 | <0.001 | ||||||
| Rural | 2,278 (30.1) | 1,784 (28.6) | 494 (36.9) | 632 (26.1) | 1,646 (31.9) | |||
| Urban | 5,295 (69.9) | 4,449 (71.4) | 846 (63.1) | 1,789 (73.9) | 3,506 (68.1) | |||
| Current smoker | 0.049 | <0.001 | ||||||
| Ex- or non-smoker | 6,734 (88.9) | 5,563 (89.3) | 1,171 (87.4) | 2,207 (91.2) | 4,527 (87.9) | |||
| Current smoker | 839 (11.1) | 670 (10.7) | 169 (12.6) | 214 (8.8) | 625 (12.1) | |||
| Alcohol intake | <0.001 | 0.007 | ||||||
| No drinking | 4,721 (62.3) | 3,809 (61.1) | 912 (68.1) | 1,559 (64.4) | 3,162 (61.4) | |||
| Once a week or less | 2,335 (30.8) | 1,994 (32.0) | 341 (25.4) | 724 (29.9) | 1,611 (31.3) | |||
| Two times a week or more | 517 (6.8) | 430 (6.9) | 87 (6.5) | 138 (5.7) | 379 (7.4) | |||
| Number of chronic diseases | 1.8±1.5 | 1.8±1.5 | 1.7±1.5 | 0.289 | 1.9±1.5 | 1.8±1.5 | 0.436 | |
| MMSE-DS score | 25.0±4.0 | 25.2±3.9 | 24.3±4.2 | <0.001 | 25.6±3.9 | 24.8±4.0 | 0.875 | |
| Presence of spouse | 4,805 (63.4) | 3,982 (63.9) | 823 (61.4) | 0.089 | 1,470 (60.7) | 3,335 (64.7) | 0.001 | |
| Number of non-cohabitating adult children | 2.9±1.2 | 2.9±1.2 | 2.9±1.3 | 0.004 | 2.9±1.2 | 2.9±1.2 | 0.414 | |
Values are presented as mean±standard deviation or number (%). MMSE-DS, Korean version of the Mini-Mental State Examination
Association between frequency of contact and risk of depression
Analysis of the frequency of contact between participants and their non-cohabitating adult children revealed that compared to the frequent contact group, the infrequent face-to-face and non-face-to-face contact groups had an adjusted OR of 1.86 (95% CI, 1.55–2.22, p=0.003) and 1.23 (95% CI, 1.04–1.45, p=0.015), respectively (Table 2).
Table 2.
Associations between frequency of contact and depression in older adults: results from logistic and linear regression models (N=7,573)
| Variable | Logistic regression model* |
Linear regression model |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | β | SE | p | |
| Frequency of face-to-face contact | ||||||
| ≥1 time/3 months | 1.00 | 1.00 | ||||
| <1 time/3 months | 1.86 | 1.55–2.22 | 0.003 | 0.458 | 0.090 | <0.001 |
| Frequency of non-face-to-face contact | ||||||
| ≥2 times/week | 1.00 | 1.00 | ||||
| <2 times/week | 1.23 | 1.04–1.45 | 0.015 | 0.236 | 0.074 | 0.001 |
in the logistic regression model, depression was defined as having a SGDS-K score of 8 or higher.
OR, odd ratio; CI, confidence interval; SE, standard error; SGDS-K, Korean version of the 15-item Geriatric Depression Scale
Linear regression analysis was performed by considering depression as a continuous variable (SGDS-K total score), and the results were consistent with the binary variable. When the contact frequency decreased, the SGDS-K score increased by 0.458 points (standard error [SE]=0.090, p<0.001) for face-to-face and 0.236 points (SE=0.074, p=0.001) for non-face-to-face contact, respectively (Table 2).
Interaction between possible moderators and relationship between frequency of contact and depression
The interaction effects of the 10 selected possible moderators were examined. The variables controlling for the effects of face-to-face and non-face-to-face contact frequency on depression in older adults differed. Variables that exhibited significant moderating effects in each item included age, quartiles of household income, number of chronic diseases, frequency of physical activity, presence of spouse, and nutritional status (NSI) for face-to-face contact frequency; and social activity participation, frequency of physical activity, and cognitive function (MMSE-DS score) for non-face-to-face contact frequency. To facilitate intuitive understanding, this interpretation is presented in Table 3.
Table 3.
Summary of moderation effects on relationship between frequency of face-to-face and non-face-to-face contact with SGDS-K score
| Possible moderators | Frequency of face-to-face contact |
Frequency of non-face-to-face contact |
||
|---|---|---|---|---|
| Interaction | Interpretation | Interaction | Interpretation | |
| Age | Yes | Older people are more affected | No | Not significant |
| Sex | No | Not significant | No | Not significant |
| Quartiles (Q) of household income | Yes | Lower incomes (Q1, 2) are affected | No | Not significant |
| Number of chronic diseases | Yes | Older adults with more chronic diseases are more affected | No | Not significant |
| Social activity participation | No | Not significant | Yes | Older adults participating in social activities are affected |
| Religious activity participation | No | Not significant | No | Not significant |
| Frequency of physical activity | Yes | Older adults frequently exercising are more affected | Yes | Older adults frequently exercising are more affected |
| MMSE-DS score | No | Not significant | Yes | Older adults with better cognitive functionare affected |
| Presence of spouse | Yes | Older adults with no spouse are affected | No | Not significant |
| NSI | Yes | Older adults with high nutritional risk (NSI ≥6) are affected | No | Not significant |
SGDS-K, Korean version of the 15-item Geriatric Depression Scale; MMSE-DS, Korean version of the Mini-Mental State Examination; NSI, Nutrition Screening Initiative
In the group of people who were older, had lower income, had more chronic diseases, exercised frequently, had no spouse, and had a high nutritional risk, the impact of frequent face-to-face contact on depression in older adults increased. Among individuals who participated in social activities, exercised frequently, and had good cognitive function, the frequency of non-face-to-face contact exerted a greater effect on depression. The values of the regression coefficients and standard estimates for the specific interaction effects of each variable are presented in Table 4.
Table 4.
Analysis of moderation effects on the relationship between frequency of face-to-face contact and non-face-to-face contact with SGDS-K scores (N=7,573)
| Variable | Frequency of face-to-face contact |
Variable | Frequency of non-face-to-face contact |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | SE | p | 95% CI | Coefficient | SE | p | 95% CI | ||||
| Age | Age | ||||||||||
| FTF | -2.381 | 1.092 | 0.029 | -4.520 to -0.241 | nFTF | 1.711 | 0.845 | 0.043 | 0.055 to 3.367 | ||
| Age | 0.006 | 0.008 | 0.450 | -0.009 to 0.021 | Age | 0.026 | 0.011 | 0.012 | 0.006 to 0.047 | ||
| Age×FTF | 0.039 | 0.015 | 0.009 | 0.010 to 0.068 | Age×nFTF | -0.020 | 0.012 | 0.077 | -0.043 to 0.002 | ||
| Gender | Gender | ||||||||||
| FTF | -0.062 | 0.297 | 0.835 | -0.644 to 0.520 | nFTF | 0.231 | 0.255 | 0.364 | -0.268 to 0.730 | ||
| Gender | 0.288 | 0.089 | 0.001 | 0.114 to 0.463 | Gender | 0.349 | 0.133 | 0.009 | 0.088 to 0.611 | ||
| Gender×FTF | 0.339 | 0.181 | 0.061 | -0.015 to 0.693 | Gender×nFTF | -0.006 | 0.151 | 0.967 | -0.302 to 0.290 | ||
| Quartiles of household incomea | Quartiles of household incomea | ||||||||||
| FTF | 1.073 | 0.177 | <0.001 | 0.727 to 1.419 | nFTF | 0.071 | 0.143 | 0.618 | -0.209 to 0.351 | ||
| W1 | 0.083 | 0.104 | 0.426 | -0.121 to 0.286 | W1 | -0.168 | 0.168 | 0.319 | -0.498 to 0.162 | ||
| W2 | -0.082 | 0.108 | 0.445 | -0.294 to 0.129 | W2 | -0.217 | 0.172 | 0.206 | -0.553 to 0.119 | ||
| W3 | -0.274 | 0.124 | 0.026 | -0.517 to -0.032 | W3 | -0.771 | 0.186 | <0.001 | -1.136 to -0.406 | ||
| W1×FTF | -0.350 | 0.235 | 0.137 | -0.810 to 0.111 | W1×nFTF | 0.326 | 0.201 | 0.105 | -0.068 to 0.721 | ||
| W2×FTF | -1.043 | 0.249 | <0.001 | -1.531 to -0.555 | W2×nFTF | -0.066 | 0.201 | 0.742 | -0.460 to 0.328 | ||
| W3×FTF | -1.517 | 0.296 | <0.001 | -2.098 to -0.936 | W3×nFTF | 0.412 | 0.219 | 0.060 | -0.018 to 0.841 | ||
| Number of chronic diseases (NCD) | Number of chronic diseases (NCD) | ||||||||||
| FTF | 0.186 | 0.139 | 0.182 | -0.087 to 0.459 | nFTF | 0.144 | 0.119 | 0.228 | -0.090 to 0.377 | ||
| NCD | 0.600 | 0.027 | <0.001 | 0.548 to 0.652 | NCD | 0.599 | 0.042 | <0.001 | 0.516 to 0.682 | ||
| NCD×FTF | 0.163 | 0.061 | 0.008 | 0.043 to 0.282 | NCD×nFTF | 0.042 | 0.050 | 0.405 | -0.057 to 0.140 | ||
| Social activity participation (SAP) | Social activity participation (SAP) | ||||||||||
| FTF | 0.991 | 0.319 | 0.002 | 0.365 to 1.616 | nFTF | 1.292 | 0.240 | <0.001 | 0.821 to 1.764 | ||
| SAP | 0.482 | 0.084 | <0.001 | 0.317 to 0.648 | SAP | 0.920 | 0.128 | <0.001 | 0.668 to 1.171 | ||
| SAP×FTF | -0.334 | 0.187 | 0.075 | -0.701 to 0.034 | SAP×nFTF | -0.699 | 0.148 | <0.001 | -0.989 to -0.409 | ||
| Religious activity participation (RAP) | Religious activity participation (RAP) | ||||||||||
| FTF | 0.897 | 0.281 | 0.001 | 0.346 to 1.449 | nFTF | 0.611 | 0.227 | 0.007 | 0.166 to 1.057 | ||
| RAP | -0.074 | 0.077 | 0.334 | -0.224 to 0.076 | RAP | 0.047 | 0.123 | 0.706 | -0.195 to 0.288 | ||
| RAP×FTF | -0.289 | 0.179 | 0.108 | -0.640 to 0.063 | RAP×nFTF | -0.265 | 0.148 | 0.074 | -0.555 to 0.026 | ||
| Frequency of physical activity (FPA) | Frequency of physical activity (FPA) | ||||||||||
| FTF | 0.222 | 0.123 | 0.072 | -0.020 to 0.464 | nFTF | 0.021 | 0.104 | 0.842 | -0.183 to 0.224 | ||
| FPA | -0.099 | 0.014 | <0.001 | -0.126 to -0.071 | FPA | -0.123 | 0.022 | <0.001 | -0.166 to -0.079 | ||
| FPA×FTF | 0.098 | 0.033 | 0.003 | 0.033 to 0.163 | FPA×nFTF | 0.065 | 0.027 | 0.016 | 0.012 to 0.118 | ||
| MMSE score (MMSE) | MMSE score (MMSE) | ||||||||||
| FTF | -0.531 | 0.538 | 0.324 | -1.586 to 0.524 | nFTF | -1.221 | 0.479 | 0.012 | -2.160 to -0.281 | ||
| MMSE | -0.120 | 0.011 | <0.001 | -0.142 to -0.099 | MMSE | -0.152 | 0.016 | <0.001 | -0.184 to -0.119 | ||
| MMSE×FTF | 0.041 | 0.022 | 0.060 | -0.002 to 0.083 | MMSE×nFTF | 0.057 | 0.019 | 0.002 | 0.020 to 0.094 | ||
| Existence of spouse (ES) | Existence of spouse (ES) | ||||||||||
| FTF | -0.676 | 0.271 | 0.013 | -1.207 to -0.145 | nFTF | 0.364 | 0.222 | 0.101 | -0.071 to 0.798 | ||
| ES | 0.275 | 0.089 | 0.002 | 0.100 to 0.451 | ES | 0.511 | 0.133 | <0.001 | 0.252 to 0.771 | ||
| ES×FTF | 0.820 | 0.185 | <0.001 | 0.458 to 1.182 | ES×nFTF | -0.093 | 0.151 | 0.541 | -0.389 to 0.204 | ||
| NSIbc | NSIbc | ||||||||||
| FTF | -0.014 | 0.107 | 0.895 | -0.225 to 0.196 | nFTF | 0.106 | 0.083 | 0.200 | -0.056 to 0.268 | ||
| W1 | 1.386 | 0.094 | <0.001 | 1.201 to 1.571 | W1 | 1.393 | 0.151 | <0.001 | 1.096 to 1.689 | ||
| W2 | 3.125 | 0.146 | <0.001 | 2.839 to 3.411 | W2 | 3.300 | 0.222 | <0.001 | 2.865 to 3.735 | ||
| W1×FTF | -0.001 | 0.211 | 0.996 | -0.415 to 0.413 | W1×nFTF | -0.004 | 0.178 | 0.982 | -0.353 to 0.345 | ||
| W2×FTF | 0.980 | 0.256 | <0.001 | 0.479 to 1.482 | W2×nFTF | 0.207 | 0.256 | 0.419 | -0.295 to 0.709 | ||
Interaction term is denoted by connecting two constructs with “×.”
the variables W1, W2, and W3 represent dummy variables. These variables indicate the relative position of quartiles compared to Quartile 1. Specifically, W1 corresponds to Quartile 2 compared to Quartile 1, W2 represents Quartile 3 compared to Quartile 1, and W3 denotes Quartile 4 compared to Quartile 1;
0≤NSI≤2: good nutrition score, 3≤NSI≤5: moderate nutritional risk, 6≤NSI: high nutritional risk;
the variables W1 and W2 represent dummy variables.
These variables indicate the relative position of other nutritional status to good nutritional status. Specifically, W1 corresponds to moderate nutritional risk status compared to good nutrition status, and W2 represents high nutritional risk compared to good nutrition status. SGDS-K, Korean version of 15-item Geriatric Depression Scale; SE, standard error; CI, confidence interval; FTF, face-to-face contact with non-cohabitating adult children; nFTF, non-face-to-face contact with non-cohabitating adult children; MMSE, Korean version of Mini Mental State Examination; NSI, Nutrition Screening Initiative
DISCUSSION
In this study, we observed that the frequency of face-to-face and non-face-to-face contact with non-cohabitating children was significantly associated with depression in later adulthood, even after adjusting for various co-variables. Increasing the frequency of face-to-face contact, rather than non-face-to-face contact, had a greater impact on lowering the risk of late-life depression. In addition, the types of possible moderators that controlled the effect of communication frequency with non-cohabitating children on late-life depression were different for face-to-face and non-face-to-face contact. Variables that moderated the effect of face-to-face contact frequency on depression included age, quartiles of household income, frequency of physical activity, presence of spouse, and nutritional status. In addition, social activity participation, frequency of physical activity, and cognitive function were variables that moderated the effect of non-face-to-face contact frequency on depression.
The results of this study demonstrated that both face-to-face and non-face-to-face contact with non-cohabitating adult children were significantly associated with depressive symptoms in late life. This is consistent with previous studies that addressed the effect of family contact on late-life depression. A study examining the frequency of contact with adult children and late-life depression reported that depressive symptoms increased as the frequency of contact decreased [26]. Similarly, an investigation performed by our group determined that the risk of depression increased with a decrease in face-to-face and non-face-to-face contact frequency with non-cohabitating adult children [11]. However, these studies may not be directly applicable for therapeutic interventions as they were conducted before the COVID-19 pandemic.
The COVID-19 pandemic and consequent social distancing measures have substantially altered the frequency of social contact as well as the mode of contact. A meta-analysis demonstrated that the frequency of social contact exhibited a substantial reduction after social distancing, and the frequency of older adults did not return to pre-COVID levels even after relaxation [33]. Similar observations were noted in a familial contact, with a 38% decrease in the frequency of face-to-face contact in older adults after the pandemic. In contrast, the frequency of non-face-to-face contact demonstrated a 16%–26% increase [13]. Considering these results, this study offers novel insight, as it was conducted after social distancing began.
The current study demonstrated that face-to-face and non-face-to-face contact were significantly associated with depressive symptoms. This suggests that face-to-face contact is as important as non-face-to-face contact during the COVID-19 pandemic. Therefore, careful consideration of face-to-face contact is needed in current conditions, whereby a substantial proportion of face-to-face contact is replaced by non-face-to-face contact [33]. Furthermore, the current findings emphasize the need for multidomain interventions that range from face-to-face to non-face-to-face, leading to improvements in depressive symptoms and avoidance of social isolation in community-dwelling older adults.
This study also investigated the moderators of the effects of face-to-face and non-face-to-face contact frequencies on late-life depression. Identifying moderators is critical given the need to specify the object of personalized community-based management or focused intervention. Strength of the current study is that it investigated the effects of 10 possible moderators based on a nationwide representative survey of older adults after COVID-19. We discuss the results and possible explanations below.
First, we identified that participation in social activity, exercising more frequently, and having good cognitive function had positive moderating effects on the relationship between the frequency of non-face-to-face contact with non-cohabitating adult children and late-life depression. This is because these individuals are more likely to be satisfied through social interaction. Obtaining energy through social interactions is referred to as extraversion, and it is well-established that these individuals need more social support to achieve psychological stability and stress [34-36]. Previous studies have demonstrated that extraverted individuals participate strongly in social activities and exercise [37]. In addition, individuals with better cognitive function participate more in social activities, which has a positive effect on mental health among older adults [30,31]. In summary, social interactions account for a larger proportion of psychological stability in older adults participating in social activities, exercising more frequently, and having better cognitive functions. Since non-face-to-face contact with non-cohabitating adult children is a key social activity [11], the influence of non-face-to-face contact frequency on depression is higher in this population. Additionally, as physical function improves with more frequent exercise, the desire for both face-to-face and non-face-to-face contact may increase. In participants with good or fair cognitive function, the frequency of non-face-to-face contact exerted a greater effect on depression. Considering that our study excluded participants with distinct cognitive impairment using relatively strict criteria, the somewhat insufficient effect of non-face-to-face contact in those with mildly reduced cognitive function may be attributed to the fact that these older adults may find device handling difficult, which could act as a stressor, or that when cognitive function is mildly impaired, sufficient qualitative communication may not be achieved through non-face-to-face contact, thus reducing its effect.
Second, older age, low quartiles of household income, a larger number of chronic illnesses, no spouse, and high nutritional risk had positive moderating effects on the relationship between face-to-face contact frequency with non-cohabitating adult children and late-life depression. As mentioned above, a common feature of older adults is that the family occupies a large portion of the entire social network. According to previous studies, social networks decrease with age, and the proportion of family members increases, whereas the proportion of non-family members (friends, workplace, neighbors, etc.) decreases [6,38]. In addition, previous studies have reported that higher income is associated with greater diversity and larger size of social networks [39]. Since individuals with lower income may have the opposite characteristics, it can be assumed that the family will occupy a larger portion of social interaction among lower-income individuals. Similarly, more chronic diseases or poorer nutritional status may be underscored by similar factors [40,41]. A previous study demonstrated that older adults without spouses relied more on their children, and the proportion of children in the family was even larger [42]. In other words, a smaller social network is associated with larger proportion of familial social contact and increased influence of relationships with children.
Moreover, instrumental help (meal provision, health habit management, hospital accompaniment, etc.) can be provided only via face-to-face contact, with the primary provider being the child [43]. Therefore, in older adults needing more instrumental support, such as due to older age, more chronic diseases, and poorer nutritional status, the frequency of face-to-face contact rather than non-face-to-face contact has a greater influence on late-life depression.
Several limitations of this study must be recognized. Firstly, the results might be affected by unmeasured confounders that could impact the association between the frequency of contact with non-cohabitating children and depression in later life. Secondly, the cross-sectional nature of the study hinders our ability to infer causality or establish the temporal relationships among the variables. Longitudinal investigations would be necessary to corroborate the directionality and causality of the relationships observed. Thirdly, the applicability of our findings may be constrained to the population, especially considering the distinctive conditions of the COVID-19 pandemic. Lastly, in the exclusion process, we did not use the existing suggested MMSE-DS cutoff values to define cognitive impairment. The reason we wanted to exclude patients with cognitive impairment was due to recall bias, and considering this, we determined that a somewhat stricter definition was necessary rather than a broad one.
In conclusion, it may be more cost-effective and therapeutic to encourage non-cohabitating adult children to contact older adults who receive greater satisfaction via social interactions or whose families account for a larger portion of their social network, particularly during the COVID-19 pandemic.
Footnotes
Availability of Data and Material
Data from the LPOPS study are available upon request to researchers who meet the criteria for access to confidential information. Access to data is permitted by Korea Institute for Health and Social Affairs.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Yujin Rho, Minji Kim, Jungeun Beon, Hyun Woong Roh. Data curation: Yujin Rho, Minji Kim, Jungeun Beon. Formal analysis: Yujin Rho, Minji Kim, Jungeun Beon, Hyun Woong Roh. Investigation: Yujin Rho, Minji Kim, Jungeun Beon, Hyun Woong Roh. Methodology: Yong Hyuk Cho, Sang Joon Son, Chang Hyung Hong, Hyun Woong Roh. Resources: Sang Joon Son, Chang Hyung Hong, Hyun Woong Roh. Software: Hyun Woong Roh. Supervision: Sang Joon Son, Chang Hyung Hong, Hyun Woong Roh. Validation: Sang Joon Son, Chang Hyung Hong, Hyun Woong Roh. Visualization: Yujin Rho, Minji Kim, Jungeun Beon. Writing—original draft: Yujin Rho, Minji Kim, Jungeun Beon, Hyun Woong Roh. Writing—review & editing: Yeojin Kim, Sunwoo Yoon, You Jin Nam, Sunhwa Hong, Yong Hyuk Cho, Sang Joon Son, Chang Hyung Hong, Hyun Woong Roh.
Funding Statement
This work was supported and funded by the grant from National Research Foundation of Korea (NRF), funded by the Ministry of Science and ICT (NRF-2019R1A5A2026045) and the grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HR21C1003, HI22C0724 and HR22C1734).
REFERENCES
- 1.Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003;58:249–265. doi: 10.1093/gerona/58.3.m249. [DOI] [PubMed] [Google Scholar]
- 2.Chang SC, Pan A, Kawachi I, Okereke OI. Risk factors for late-life depression: a prospective cohort study among older women. Prev Med. 2016;91:144–151. doi: 10.1016/j.ypmed.2016.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Roh HW, Hong CH, Lee Y, Oh BH, Lee KS, Chang KJ, et al. Participation in physical, social, and religious activity and risk of depression in the elderly: a community-based three-year longitudinal study in Korea. PLoS One. 2015;10:e0132838. doi: 10.1371/journal.pone.0132838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arean PA, Reynolds CF., 3rd The impact of psychosocial factors on latelife depression. Biol Psychiatry. 2005;58:277–282. doi: 10.1016/j.biopsych.2005.03.037. [DOI] [PubMed] [Google Scholar]
- 5.Schwarzbach M, Luppa M, Forstmeier S, König HH, Riedel-Heller SG. Social relations and depression in late life-a systematic review. Int J Geriatr Psychiatry. 2014;29:1–21. doi: 10.1002/gps.3971. [DOI] [PubMed] [Google Scholar]
- 6.Ajrouch KJ, Antonucci TC, Janevic MR. Social networks among blacks and whites: the interaction between race and age. J Gerontol B Psychol Sci Soc Sci. 2001;56:S112–S118. doi: 10.1093/geronb/56.2.s112. [DOI] [PubMed] [Google Scholar]
- 7.Mindel CH. Multigenerational family households: recent trends and implications for the future. Gerontologist. 1979;19:456–463. doi: 10.1093/geront/19.5_part_1.456. [DOI] [PubMed] [Google Scholar]
- 8.Taqui AM, Itrat A, Qidwai W, Qadri Z. Depression in the elderly: does family system play a role? A cross-sectional study. BMC Psychiatry. 2007;7:57. doi: 10.1186/1471-244X-7-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim H, Kwon S, Hong S, Lee S. Health behaviors influencing depressive symptoms in older Koreans living alone: secondary data analysis of the 2014 Korean longitudinal study of aging. BMC Geriatr. 2018;18:186. doi: 10.1186/s12877-018-0882-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Green MJ, Whitley E, Niedzwiedz CL, Shaw RJ, Katikireddi SV. Social contact and inequalities in depressive symptoms and loneliness among older adults: a mediation analysis of the English Longitudinal Study of Ageing. SSM Popul Health. 2021;13:100726. doi: 10.1016/j.ssmph.2021.100726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roh HW, Lee Y, Lee KS, Chang KJ, Kim J, Lee SJ, et al. Frequency of contact with non-cohabitating adult children and risk of depression in elderly: a community-based three-year longitudinal study in Korea. Arch Gerontol Geriatr. 2015;60:183–189. doi: 10.1016/j.archger.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 12.Macdonald B, Luo M, Hülür G. Daily social interactions and well-being in older adults: the role of interaction modality. J Soc Pers Relation. 2021;38:3566–3589. [Google Scholar]
- 13.Hawkley LC, Finch LE, Kotwal AA, Waite LJ. Can remote social contact replace in-person contact to protect mental health among older adults? J Am Geriatr Soc. 2021;69:3063–3065. doi: 10.1111/jgs.17405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yesavage JA, Sheikh JI. 9/Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol. 1986;5:165–173. [Google Scholar]
- 15.Bae JN, Cho MJ. Development of the Korean version of the Geriatric Depression Scale and its short form among elderly psychiatric patients. J Psychosom Res. 2004;57:297–305. doi: 10.1016/j.jpsychores.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Kim JY, Park JH, Lee JJ, Huh Y, Lee SB, Han SK, et al. Standardization of the Korean version of the Geriatric Depression Scale: reliability, validity, and factor structure. Psychiatry Investig. 2008;5:232–238. doi: 10.4306/pi.2008.5.4.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee SC, Kim WH, Chang SM, Kim BS, Lee DW, Bae JN, et al. The use of the Korean version of Short Form Geriatric Depression Scale (SGDSK) in the community dwelling elderly in Korea. J Korean Geriatr Psychiatry. 2013;17:37–43. [Google Scholar]
- 18.Ward R, Deane G, Spitze G. Life-course changes and parent-adult child contact. Res Aging. 2014;36:568–602. doi: 10.1177/0164027513510325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nguyen MH, Gruber J, Marler W, Hunsaker A, Fuchs J, Hargittai E. Staying connected while physically aprt: digital communication when face-to-face interactions are limited. New Media Soc. 2022;24:2046–2067. [Google Scholar]
- 20.Brzezinski A, Deiana G, Kecht V, Van Dijcke D. The COVID-19 pandemic: government vs. community action across the United States. INET Oxford Working Papers. 2020 Apr 18; 2020-06 [Epup]. https://ideas.repec.org/p/amz/wpaper/2020-06.html. [Google Scholar]
- 21.Newson N, Zhao Y, Zein ME, Sulik J, Dezecache G, Deroy O, et al. Digital contact does not promote wellbeing, but face-to-face contact does: a cross-national survey during the COVID-19 pandemic. New Media Soc. 2021 Dec 7; doi: 10.1177/14614448211062164. [Epub]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xie Y, Ma M, Wu W, Zhang Y, Zhang Y, Tan X. Dose-response relationship between intergenerational contact frequency and depressive symptoms amongst elderly Chinese parents: a cross-sectional study. BMC Geriatr. 2020;20:349. doi: 10.1186/s12877-020-01751-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Han JW, Kim TH, Jhoo JH, Park JH, Kim JL, Ryu SH, et al. A normative study of the Mini-Mental State Examination for Dementia Screening (MMSE-DS) and its Short form(SMMSE-DS) in the Korean elderly. J Korean Geriatr Psychiatry. 2010;14:27–37. [Google Scholar]
- 24.Balbuena L, Baetz M, Bowen R. Religious attendance, spirituality, and major depression in Canada: a 14-year follow-up study. Can J Psychiatry. 2013;58:225–232. doi: 10.1177/070674371305800408. [DOI] [PubMed] [Google Scholar]
- 25.Ruan H, Shen K, Chen F. Negative life events, social ties, and depressive symptoms for older adults in China. Front Public Health. 2022;9:774434. doi: 10.3389/fpubh.2021.774434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tosi M, Grundy E. Intergenerational contacts and depressive symptoms among older parents in Eastern Europe. Aging Ment Health. 2019;23:686–692. doi: 10.1080/13607863.2018.1442412. [DOI] [PubMed] [Google Scholar]
- 27.Larsen BA, Strong D, Linke SE. The association between family and friend integration and physical activity: results from the NHIS. Int J Behav Med. 2014;21:529–536. doi: 10.1007/s12529-013-9318-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hatfield JP, Hirsch JK, Lyness JM. Functional impairment, illness burden, and depressive symptoms in older adults: does type of social relationship matter? Int J Geriatr Psychiatry. 2013;28:190–198. doi: 10.1002/gps.3808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Arai K, Sakakibara H. [Malnutrition and social isolation among elderly residents of city public housing] Nihon Koshu Eisei Zasshi. 2015;62:379–389. doi: 10.11236/jph.62.8_379. Japanese. [DOI] [PubMed] [Google Scholar]
- 30.Brown CL, Robitaille A, Zelinski EM, Dixon RA, Hofer SM, Piccinin AM. Cognitive activity mediates the association between social activity and cognitive performance: a longitudinal study. Psychol Aging. 2016;31:831–846. doi: 10.1037/pag0000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fu C, Li Z, Mao Z. Association between social activities and cognitive function among the elderly in China: a cross-sectional study. Int J Environ Res Public Health. 2018;15:231. doi: 10.3390/ijerph15020231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brummett BH, Barefoot JC, Vitaliano PP, Siegler IC. Associations among social support, income, and symptoms of depression in an educated sample: the UNC alumni heart study. Int J Behav Med. 2003;10:239–250. doi: 10.1207/s15327558ijbm1003_04. [DOI] [PubMed] [Google Scholar]
- 33.Liu CY, Berlin J, Kiti MC, Del Fava E, Grow A, Zagheni E, et al. Rapid review of social contact patterns during the COVID-19 pandemic. Epidemiology. 2021;32:781–791. doi: 10.1097/EDE.0000000000001412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McHugh JE, Lawlor BA. Social support differentially moderates the impact of neuroticism and extraversion on mental wellbeing among community-dwelling older adults. J Ment Health. 2012;21:448–458. doi: 10.3109/09638237.2012.689436. [DOI] [PubMed] [Google Scholar]
- 35.Amirkhan JH, Risinger RT, Swickert RJ. Extraversion: a “hidden” personality factor in coping? J Pers. 1995;63:189–212. doi: 10.1111/j.1467-6494.1995.tb00807.x. [DOI] [PubMed] [Google Scholar]
- 36.Swickert RJ, Rosentreter CJ, Hittner JB, Mushrush JE. Extraversion, social support processes, and stress. Pers Individ Dif. 2002;32:877–891. [Google Scholar]
- 37.Quattrochi-Tubin SJ, Jason LA, Haworth Continuing Features Submission Worth repeating: the influence of introversion-extraversion on activity choice and satisfaction among the elderly. Activ Adapt Aging. 1983;4:19–28. [Google Scholar]
- 38.Wrzus C, Hänel M, Wagner J, Neyer FJ. Social network changes and life events across the life span: a meta-analysis. Psychol Bull. 2013;139:53–80. doi: 10.1037/a0028601. [DOI] [PubMed] [Google Scholar]
- 39.Pinquart M, Sörensen S. Influences of socioeconomic status, social network, and competence on subjective well-being in later life: a meta-analysis. Psychol Aging. 2000;15:187–224. doi: 10.1037//0882-7974.15.2.187. [DOI] [PubMed] [Google Scholar]
- 40.Ryan VC, Bower ME. Relationship of socioeconomic status and living arrangements to nutritional intake of the older person. J Am Diet Assoc. 1989;89:1805–1807. [PubMed] [Google Scholar]
- 41.Ell K. Social networks, social support and coping with serious illness: the family connection. Soc Sci Med. 1996;42:173–183. doi: 10.1016/0277-9536(95)00100-x. [DOI] [PubMed] [Google Scholar]
- 42.Hülür G, Elayoubi J, Nelson ME, Haley WE. Change in episodic memory with spousal loss: the role of social relationships. J Gerontol B Psychol Sci Soc Sci. 2022;77:683–694. doi: 10.1093/geronb/gbab231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Seeman TE, Berkman LF. Structural characteristics of social networks and their relationship with social support in the elderly: who provides support. Soc Sci Med. 1988;26:737–749. doi: 10.1016/0277-9536(88)90065-2. [DOI] [PubMed] [Google Scholar]


