Abstract
Objective
Internet gaming disorder (IGD) is an increasingly common behavioral addiction, with an estimated global prevalence of 3%. A variety of pharmacological treatments have been used to treat IGD, yet no review to date has synthesized clinical trials evaluating their efficacy. This systematic review therefore synthesized the literature reporting on clinical trials of pharmacological treatments for IGD.
Methods
We reviewed articles from MEDLINE, Embase, PubMed Central, CINAHL, and PsycINFO that were published as of March of 2022. A total of 828 articles were retrieved for review and 12 articles were included, reporting on a total of 724 participants.
Results
Most participants were male (98.6%), and all were currently living in South Korea. The most common drugs used to treat IGD were bupropion, methylphenidate, and a range of selective serotonin reuptake inhibitors. The Young Internet Addiction Scale was the most frequently used to measure gaming-related outcomes. All studies reported reduced symptoms of IGD from pre- to post-treatment. Across all clinical trials, IGD symptom reductions following the administration of pharmacological treatments ranged from 15.4% to 51.4%. A risk of bias assessment indicated that only four studies had a low risk of bias.
Conclusion
Preliminary results suggest that a wide array of pharmacological interventions may be efficacious in the treatment of IGD. Future studies using double-blind randomized controlled trial designs, recruiting larger and more representative samples, and controlling for psychiatric comorbidities are needed to better inform understanding of pharmacological treatments for IGD.
Keywords: Gaming disorder, Internet gaming disorder, Video game addiction, Pharmacological treatment
INTRODUCTION
Internet gaming disorder (IGD), now classified as an addictive disorder in the International Classification of Diseases 11th revision [1], is becoming increasingly common, with a recent large-scale meta-analysis indicating global prevalence as high as 3.1% [2]. IGD is characterized by impaired control over gaming, increasing priority given to gaming to the extent that gaming takes precedence over other life interests, and continuation or escalation of gaming despite the occurrence of negative consequences. While IGD falls under a larger umbrella of problematic internet use (PIU), research has identified IGD as unique and distinct from other forms of PIU, such as internet addiction [3,4]; whereas PIU spans a range of online behaviors, including online chatting and social media use, IGD refers specifically to excessive engagement and associated problems with online gaming.
Psychological and pharmacological treatments are the most common treatment options for IGD [5]. Psychological treatments for IGD have predominantly drawn on cognitive-behavioral therapy and have demonstrated good effectiveness in reducing symptoms [6]. Conversely, the types of pharmacological treatments used to treat IGD have varied considerably. Indeed, treatments have included psychostimulants [7], selective serotonin reuptake inhibitors (SSRIs) [8], serotonin and norepinephrine reuptake inhibitors [9], and non-selective inhibitors of dopamine and norepinephrine transporters [10]. To date, empirical research has yet to consolidate the effectiveness of these different drugs, precluding insight as to whether pharmacological treatment is generally effective in reducing symptoms of IGD, and if so, the types that may be most effective.
There is strong evidence to suggest that pharmacological treatments for IGD may be effective, stemming from research demonstrating the functional and structural neurobiological underpinnings of IGD [11]. For example, a recent systematic review found that individuals with IGD display increased activity in brain regions associated with reward, reduced activity in brain regions associated with impulse control, and reduced functional connectivity in brain networks implicated in motivation, reward, and executive function, and cognitive control [12]. This review also identified structural differences among individuals with IGD, with regard to reduced grey-matter volume and white-matter density [12]. Importantly, these neurobiological abnormalities are consistent with those observed in other addictive disorders, such as gambling disorder and substance use disorders—addictive disorders for which pharmacological treatments have demonstrated effectiveness [13-15].
Given increasing understanding of IGD as an addictive disorder and relatively high prevalence rates, an improved understanding of its potential pharmacological treatments is warranted. A previous systematic review [5] examining interventions for IGD identified eight studies that reported on clinical trials of pharmacological interventions for IGD, observing reductions in IGD symptoms following the administration of pharmacological treatments across studies. This review, however, did not focus specifically on pharmacological treatments, thus omitting search terms needed to identify pharmacological treatments and precluding a fulsome identification of relevant studies. As such, we conducted a systematic review of studies examining the effectiveness of pharmacological treatments in reducing symptoms of IGD.
METHODS
Search strategy
The search strategy for this review was developed in consultation with a librarian specializing in systematic reviews. Using MeSH terms, we searched the following databases: MEDLINE, Embase, PubMed Central, CINAHL, and PsycINFO. We included all terms related to IGD and problematic engagement in internet use and or video gaming (e.g., internet gaming disorder, video game addiction). We also included terms related to pharmacological treatment (e.g., pharmacotherapy, medication), as well as terms related to common classes of pharmacological treatments (e.g., selective serotonin reuptake inhibitors, norepinephrine-dopamine reuptake inhibitors) and specific pharmacological treatments (e.g., bupropion, methylphenidate). Terms related to IGD were combined with terms related to pharmacological treatments using Boolean operators. Searches were adapted to each database using appropriate MeSH terms and keywords for each database. We conducted our search on March of 2022 and did not limit results to a specific timeframe. A sample search strategy is provided in Supplementary Materials (in the online-only Data Supplement). The reference lists of the included articles were also screened to identify additional articles reporting on pharmacological treatments for IGD.
Eligibility criteria
We reviewed original articles involving human research participants that reported the use of a pharmacological intervention in the treatment of IGD. Our inclusion criteria were as follows: 1) studies included a sample comprised of people with IGD or gaming-related symptoms if reporting on PIU; 2) studies reported on a pharmacological intervention used in the treatment of IGD; 3) studies reported on at least one outcome measure related to IGD; and 4) studies were available in English, Portuguese, Spanish, or French. Theoretical papers, opinion pieces, commentaries, conference proceedings, case reports, and review papers were excluded, although reference lists of review papers were screened for relevancy.
Screening abstracts
Two authors screened each article independently for relevance based on title and abstract, with discrepancies resolved through consensus. Inter-rater reliability (IRR) between the two authors was near-perfect (Cohen’s kappa=0.85) [16]. Full texts were then retrieved for all included articles and were each independently screened by the two authors, again revealing near-perfect IRR (Cohen’s kappa=0.88). Discrepancies were resolved through consensus and consultation with a third author.
Data extraction
For each included article, the following information were extracted: 1) study design; 2) participant information including sample size, mean age, and sex; 3) instrument used to measure IGD; 4) pharmacological treatments used; 5) duration of treatment; and 6) main results.
Risk of bias
Included manuscripts were assessed by SJ and PP for risk of bias using the Cochrane Collaboration Risk of Bias (ROB-2) Tool [17] for randomized controlled trials and the Cochrane Risk of Bias In Non-Randomized Studies (ROBINS-I) [18] for open label trials. The ROB-2 evaluates the following criteria: random sequence generation, blinding of participants and research personnel, blinding of outcome measures, incomplete outcome data, and selective reporting of results, whereas the ROBINS-I evaluates bias in controlling for confounding variables, selection of participants, classification of interventions, deviations from intended intervention, missing data, measurement of outcomes, and selection of reported results. There was high IRR for each scale (IRR=100%; 90%, respectively). Disagreements were resolved by HSK.
RESULTS
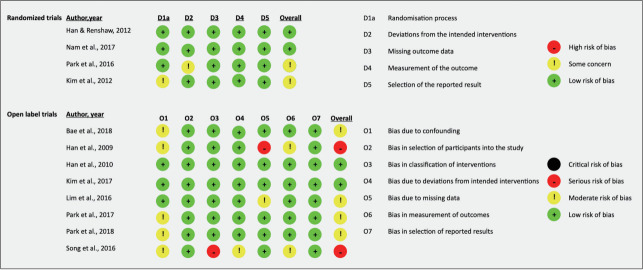
Our search generated 912 articles, of which 828 remained after the removal of duplicates (Figure 1). Of these 828 articles, 19 were retrieved for full-text review. A total of 12 articles met all eligibility criteria and were included in the present review.
Figure 1.
PRISMA flow diagram of the studies included in the present review (N=12). PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
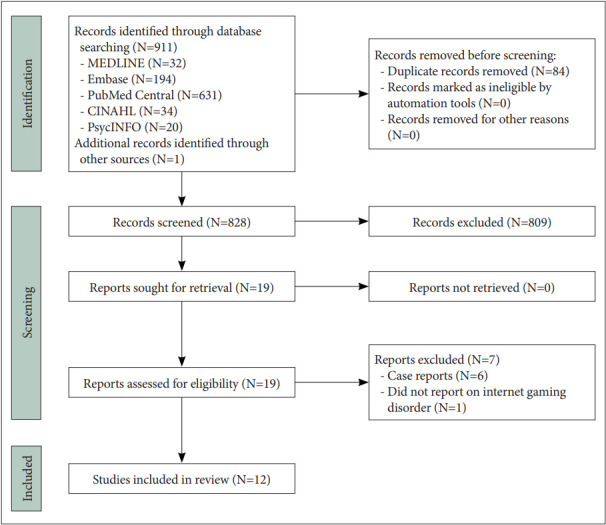
Risk of bias
With respect to randomized trials, two of the four included studies were rated as having low risk of bias whereas the remaining two had some concerns, due to the randomization process [19] and deviations from the intended intervention [7]. Comparatively, two of eight open label trials were rated as having low risk of bias, four as having some concerns, and two as having a serious risk of bias. Concerns of bias were primarily due to confounding, with serious concerns in classification of interventions in one study [8] and bias due to missing data in one study [20]. Further details are in Figure 2.
Figure 2.
Risk of bias assessment of the included studies (N=12) [7-10,19-26].
Summary of findings
Table 1 summarizes the main findings of the articles included in the present review. All articles were conducted in South Korea. All studies reported on clinical trials, of which eight were open clinical trials [8,9,19,21-25]; one was an open, uncontrolled clinical trial [20]; one was a prospective, randomized, controlled, single-blind clinical trial [7]; one was a prospective, controlled, double-blind clinical trial [26]; and one was a prospective, randomized, controlled, and double-blind clinical trial [10]. Across all studies, the total sample included 724 participants. Park et al. [7] reported a total of 86 participants in their abstract and 84 participants in their method section. For consistency, we assumed their sample size to be 84 across all our analyses. Of the 694 participants for whom sex was reported, 684 (98.6%) were male and 10 (1.4%) were female. Eight articles reported on samples of adults, three reported on samples of children and/or adolescents, and one reported on both adults and adolescents.
Table 1.
Summary of articles included for systematic review
| Study | Study design | Participants | GD measure | Treatment | Duration | Improvement in IGD Symptoms (%) | Key results |
|---|---|---|---|---|---|---|---|
| Bae et al. [9] (2018) | Open clinical trial | 16 male adults with internet gaming disorder (IGD; 25.3±5.2 yr), 15 male adults with internet-based gambling disorder (ibGD; 25.0±4.9 yr), 15 male adult healthy controls (25.7±4.7 yr) | Young’s Internet Addiction Scale (YIAS) | Bupropion | 12 weeks | IGD group: 20.5%; ibGD group: 4.7% | • After 12 weeks of treatment, IGD and ibGD symptoms decreased in both treatment groups |
| • In IGD group, functional connectivity (FC) within the posterior default mode network (DMN) and between the DMN and cognitive control network (CCN) decreased following treatment | |||||||
| • In IGD group, FC within the DMN was positively correlated with changes in the YIAS after treatment | |||||||
| • In the ibGD group, FC within the posterior DMN decreased while FC within the CCN increased following treatment | |||||||
| Han and Renshaw [10] (2012) | Prospective, randomized, controlled, double-blind clinical trial | 57 male adults with excessive online game play and major depressive disorder (MDD); 29 treatment group (21.2±8.0 yr), 28 placebo group (19.1±6.2 yr) | YIAS | Bupropion | 8 weeks | 36.8% 8 weeks, 40.7% 12 weeks | • YIAS scores and time playing online games were greatly reduced in bupropion group compared to placebo group |
| • Bupropion-associated reductions in online game play persisted during four-week post-treatment follow-up period | |||||||
| Han et al. [21] (2010) | Open clinical trial | 11 male adults with internet video game addiction (IA; 21.5±5.6 yr), 8 male adult healthy controls (20.3±4.1 yr) | YIAS | Bupropion sustained release (SR) | 6 weeks | 15.40% | • After 6 weeks of bupropion SR, craving for internet video game play, total game play time, and cue-induced brain activity in the dorsolateral prefrontal cortex were decreased in the IA group |
| Kim et al. [19] (2012) | Open clinical trial | 65 male adolescents with excessive online game play and MDD; 32 CBT-Bupropion group (16.2±1.4 yr), 33 Bupropion group (15.9±1.6 yr) | YIAS | Cognitive behavioral therapy (CBT) combined with Bupropion (CBT-Bupropion group) or Bupropion alone (Bupropion-alone group) | 8 weeks | CBT-Bupropion group: 51.4% 8 weeks, 49.1% 12 weeks; Bupropion group: 33.6% 8 weeks, 33.3% 12 weeks | • After 8 weeks, CBT-Bupropion group showed significantly greater decrease in YIAS scores and mean game playing time compared to Bupropion-alone group |
| • In both groups, changes in YIAS scores were positively correlated with changes in depression | |||||||
| • No changes in YIAS scores or total game playing time observed in either group during the 4-week post-treatment follow-up period | |||||||
| Nam et al. [26] (2017) | Prospective, controlled, double-blind clinical trial | 30 adults with IGD and MDD; 15 Bupropion group (22.9±1.9 yr), 15 Escitalopram group (23.9±1.6 yr) | YIAS | Bupropion SR or Escitalopram | 12 weeks | Not reported | • IGD and MDD symptoms in both groupsimproved after 12 weeks of treatment |
| • After treatment, FC within only the DMN in escitalopram decreased, while FC between DMN and salience network decreased in bupropion SR group | |||||||
| • Compared to escitalopram, bupropion SR was associated with significantly decreased FC within the salience network and between the salience network and the DMN | |||||||
| Song et al. [8] (2016) | Open clinical trial | 119 male adolescents and adults with IGD; 44 Bupropion group (20.0±3.62 yr), 42 Escitalopram group (19.8±4.2 yr), 36 Observation group (19.6±4.0 yr) | YIAS | Bupropion SR or Escitalopram | 6 weeks | Bupropion group: 34.9%; Escitalopram group: 24.0% | • After 6 weeks of treatment, both bupropion SR and escitalopram groups showed greater reductions in IGD symptoms compared to a control group who was observed in the community |
| • Bupropion group showed greater reductions in IGD symptoms compared to control group | |||||||
| Kim et al. [22] (2017) | Open clinical trial | 20 male adults with IGD (22.71±5.47 yr), 29 male adult healthy controls (23.97±4.36 yr) | Young’s Internet Addiction Test (Y-IAT) | Selective serotonin reuptake inhibitors: Escitalopram, Fluoxetine, or Paroxetine | 6 weeks | 21.50% | • From pre- to post-treatment, the IGD group exhibited a significant decrease in IGD symptoms |
| • Compared to healthy controls, the IGD group displayed increased resting-state electroencephalography (EEG) activity in the delta and theta bands at baseline, which normalized following treatment | |||||||
| • Decreased resting-state EEG activity in delta and theta bands from pre- to post-treatment was associated with decreased IGD symptoms | |||||||
| • Higher absolute theta activity at baseline predicted greater improvement in IGD symptoms following treatment, controlling for depressive and anxiety symptoms | |||||||
| Lim et al. [23] (2016) | Open clinical trial | 44 young adult males with IGD (19.159±5.216 yr), 40 young adult male healthy controls (21.375±6.307 yr) | Y-IAT | Selective serotonin reuptake inhibitors (not specified) | 6 months | 18.7% | • From pre- to post-treatment, the IGD group showed significant reductions in IGD severity, as well as increased quality of life, response inhibition, and executive functioning |
| • Low working memory functioning and high executive functioning at baseline predicted improvements in IGD symptoms among the IGD group from pre- to post-treatment | |||||||
| Park et al. [24] (2017) | Open clinical trial | 18 male adults with IGD (22.6±5.1 yr), 29 male adult healthy controls (24.7±3.8 yr) | Y-IAT | Selective serotonin reuptake inhibitors: Escitalopram, Fluoxetine, or Paroxetine | 6 months | 22.1% | • At baseline, IGD group displayed significantly lower P300 amplitudes and delayed latencies at the midline centro-parietal site compared to healthy group |
| • Significant reduction in IGD symptoms observed following 6 months of treatment | |||||||
| • No significant changes in the P300 indices observed from pre- to post-treatment | |||||||
| • No significant difference in ERPs was observed between responders and non-responders to 6-month treatment | |||||||
| • Reduced P300 amplitudes and delayed latencies may be candidate endophenotypes in the pathophysiology of IGD | |||||||
| Park et al. [25] (2018) | Open clinical trial | 30 male adults with IGD (23.27±5.15 yr), 32 male adults healthy controls (24.97± 3.70 yr) | Y-IAT | Selective serotonin reuptake inhibitors: Escitalopram, Fluoxetine, or Paroxetine | 6 months | 17.6% | • IGD group displayed increased beta and gamma intrahemispheric coherence and increased delta intrahemispheric coherence of the right hemisphere at baseline, compared to healthy controls |
| • IGD group displayed reduced IGD symptoms following treatment compared to baseline but continued to show increased beta and gamma intrahemispheric coherence compared to healthy controls | |||||||
| • IGD group did not display significant EEG coherence changes between the pre- and post-treatment assessments | |||||||
| Han et al. [20] (2009) | Open, uncontrolled clinical trial | 62 children (10 females) with ADHD who played internet video games (9.3±2.2 yr) | Young’s Internet Addiction Scale–Korean version (YIAS-K) | Methylphenidate (MPH) | 8 weeks | 23.70% | • After 8 weeks of treatment, YIAS-K scores and internet usage times significantly reduced compared to baseline |
| • Changes in YIAS-K scores were associated with changes in inattention and visual attention | |||||||
| Park et al. [7] (2016) | Prospective, randomized, controlled, single-blind clinical trial | 84 male adolescents with ADHD and IGD; 44 MPH group (16.9±1.6 yr), 40 ATM group (17.1±1.0 yr) | YIAS | MPH or Atomoxetine (ATM) | 12 weeks | MPH group: 32.8%; ATM group: 19.0% | • Both MPH and ATM reduced symptoms of IGD |
| • Changes in IGD symptoms were associated with changes in impulsivity | |||||||
| • No significant differences observed in IGD symptom or impulsivity reduction between MPH and ATM group |
GD, gaming disorder; ERP, event-related potential; ADHD, attention deficit hyperactivity disorder
Seven studies focused primarily on the treatment of IGD, totaling 63.6% (n=461) of participants with IGD across all articles. Five of the seven studies included participants with IGD and other psychiatric comorbidities (n=298), the most common of which were attention deficit hyperactivity disorder (ADHD) and major depressive disorder (MDD). Regarding pharmacological treatments, six articles reported the use of more than one drug in the treatment of IGD, although only three articles reported results separately for different drugs. The most common drug used to treat IGD was bupropion or bupropion sustained release, which was used in six articles and among 26.9% (n=195) of participants across all studies. Other drugs used included a range of SSRIs, such as fluoxetine, escitalopram, and paroxetine (6 articles; n=169, 23.3%); methylphenidate (2 articles; n=106, 14.6%); and atomoxetine (1 article; n=40, 5.5%).
The most widely used instrument to measure gaming-related symptoms was the Young Internet Addiction Scale (YIAS) [27]. This scale, developed to analyze PIU, was used in eight of the 12 articles. The remaining four studies measured gaming-related symptoms using the Young’s Internet Addiction Test [28]. Four studies also examined time spent gaming as an outcome, which was measured via self-report and verified by collateral information (usually provided by a parent or spouse).
Of the 12 articles included in the present review, all reported reduced IGD symptoms from pre- to post-treatment across participants who received pharmacological treatment. Across all clinical trials, symptom reductions among participants who received treatment for IGD-related symptoms ranged from 15.4% to 51.4%. When stratifying analyses by specific drug, atomoxetine promoted an 18.3% symptom reduction, bupropion promoted symptom reductions ranging from 15.4% to 51.4%, SSRIs promoted symptom reductions ranging from 17.6% to 24.0%, and methylphenidate promoted symptom reductions ranging from 23.7% to 25.7%. Three articles focused on individuals with IGD and comorbid MDD [10,19,26], all reporting improvements in both MDD and IGD symptoms (n=124, 17.1%). Similarly, of the two articles that focused on individuals with ADHD who engaged in gaming [7,20], reductions in both ADHD and IGD symptoms were reported from pre- to post-treatment (n=146, 20.2%).
DISCUSSION
The aim of the present review was to synthesize the existing literature on pharmacological treatments for IGD. Overall, there is preliminary support that a wide range of pharmacological treatments may be effective in reducing symptoms of IGD and its associated comorbidities, including ADHD and depression. Although promising, the present review identified several gaps in the literature that warrant future address.
First, only 1.4% of the total sample were females. This differs markedly from the global demographic composition of video game players, in which women represent roughly 50% of gamers worldwide [29-31]. Furthermore, the rates of IGD in women are increasing, with current prevalence rates of 4%–5% [2], suggesting a need to examine gender differences in the efficacy of pharmacological treatment for IGD. Secondly, all studies included in the present review were conducted in South Korea. This may reduce the generalizability of the findings to people with IGD in other countries due to cross-cultural differences in IGD. For example, there may exist physiological differences among people of East Asian descent that may impact the efficacy of pharmacological treatments for IGD. Indeed, studies have reported on neurogenetic variance by ethnicity, particularly in dopamine polymorphism, which is implicated in addictive behaviors and depression symptoms [32,33].
Interestingly, most participants presented with psychiatric comorbidities, with only 24.0% of the total sample presenting exclusively with IGD. This finding is consistent with previous studies that have shown that IGD often presents with other mental health comorbidities [34]. The presence of comorbidities may render difficulties disentangling the intervention effects of pharmacological treatments on multiple co-occurring disorders. For example, in studies in which the samples were comprised of patients with IGD and ADHD who were treated with psychostimulants, it is difficult to determine whether the reductions in IGD symptoms were a direct result of the intervention, or were caused indirectly through reductions in ADHD symptoms [7,20]. The same challenge was presented in studies examining the treatment of IGD in the presence of comorbid depressive symptoms [10,19,24,26] and anxiety symptoms [24]. That said, the inclusion of people with IGD and mental health comorbidities better reflects clinical reality and likely provides more generalizable results. Future studies that investigate whether different pharmacological treatments have differential outcomes based on comorbid psychopathology would be highly informative.
Bupropion was the most frequently used drug in the treatment of IGD. Given that IGD is conceptualized as a behavioral addiction and most frequently co-occurs with depression, anxiety, and ADHD, this was not surprising, as bupropion is the only pharmacological treatment that has demonstrated efficacy in the treatment of smoking [35]; depressive disorders [36]; anxiety symptoms [37]; and ADHD [38]. These findings may illuminate the neurobiological mechanisms of action of bupropion in IGD, given the shared pathophysiology of dysregulated dopaminergic signaling across these conditions [39-41] and the role of bupropion in regulating dopamine release [42,43]. Furthermore, previous studies have also found increased default mode network (DMN) connectivity to correspond with dysregulated dopamingergic and norepinephrinergic signaling [44] as well as greater addictive behaviors [45,46], including impulsivity and risk-taking [47]. Importantly, two studies included in this review that investigated bupropion treatment of IGD observed decreases in functional connectivity within DMN [9,26] while one found decreased connectivity between the DMN and cognitive control network in people with IGD, which correlated with changes in IGD and MDD symptoms [26], potentially indicating a mechanism of action for bupropion in the treatment of IGD via regulation of dopamine and norepinephrine [43]. Comparatively, two studies investigated the efficacy of an SSRI in individuals with IGD [22,26]; one found decreased connectivity of the DMN, but not between the DMN and cognitive control network, and efficacy was lower relative to bupropion [26]. The other found normalization of absolute delta and theta power that correlated with reductions in IGD symptoms [22]. Normalization of resting state delta and theta waves may have implications for decreased DMN activity [48] and reflect improvements in inhibitory control [22]. However, this treatment did not correlate with reductions in co-occurring psychiatric symptoms. Thus, the co-occurring psychiatric symptoms presenting in IGD may have relevant implications for the preferred treatment method.
Worth noting, no studies in the current review examined pharmacological treatments targeting craving. Naltrexone is an anti-craving pharmacological intervention that is effective in the treatment of alcohol use disorder [49] and opioid use disorder [50], due to its antagonist actions in the mu-opioid system, thereby reducing rewarding effects of exogenous agonists such as alcohol and opioids. Some studies have investigated the use of naltrexone in behavioral addictions, with one small meta-analysis finding statistically significant improvements of naltrexone relative to placebo in treatment of gambling, kleptomania, trichotillomania, and impulsive-compulsive disorders [51]. In addition, one case-study reported reductions in IGD symptoms after naltrexone was administered to a 15-year old male [52]. However, research in the application of naltrexone to behavioral addictions is in its infancy, with existing studies having substantial heterogeneity, no randomized controlled trials of naltrexone on IGD, lack of long-term follow-ups, and limited empirical evidence on mechanisms of action. Nonetheless, the potential utility of naltrexone in treating IGD is a promising avenue of further study; long-term randomized clinical trials are needed to assess its effects.
This review is limited by several studies that did not provide a clear description of instruments used to measure primary and secondary outcomes. Most studies used the YIAS as an outcome measure, which may be problematic as the YIAS was originally developed for diagnosing PIU. As such, future pharmacological studies of IGD would benefit from including scales that have been developed specifically for the measurement of IGD, such as the Ten-Item Internet Gaming Disorder Test [53]. Further, the majority of the included studies were rated as having at least some concern of bias, with two rated as having serious concern. Potential bias in study findings limits adequate comparison of pharmacological treatments for IGD and may reduce confidence in the validity of the findings. Other methodological limitations include small sample sizes, inability to rule out regression to the mean in open label trials and lack of long follow up periods. Thus, future studies should ensure rigorous methodology.
An additional limitation is that studies rarely described the type(s) of games played by participants (e.g., role-playing, first-person shooter). Gaming preference is a relevant consideration as some game types, such as massively multiplayer online role playing games (MMORPG), are more strongly related to IGD than others, irrespective of player characteristics [54]. In addition, psychological profiles associated with game types may differ. For example MMORPGs are associated with high social anxiety, escapism, impulsivity, and sensation-seeking [55], which may not be the case for other game-types (e.g., offline computer games, arcade games). Given the heterogeneity in IGD presentation with respect to both game-level and player-level differences, future studies should examine the type of games to inform the selection of optimal pharmacological treatments for IGD.
Relatedly, examining the reasons why people play video games (i.e., gaming motivations) may also help to inform the selection of optimal treatments. For example, if a primary motivation for an individual with IGD is to regulate their affect due to symptoms of depression and anxiety, then antidepressant and anti-anxiety medications may be warranted. On the other hand, if individuals are motivated by need for achievement/advance (i.e., increase rank/pass levels), and purchase microtransactions such as loot boxes which operate on an intermittent reward schedule, then naltrexone may be of benefit. Furthermore, for individuals whose primary motivation is for social-relationships or high social anxiety then cognitive behavioral interventions may be the optimal treatment. However, we caution that further research is needed to examine whether gaming motives may have utility in selecting the most optimal treatments in IGD.
In summary, the literature examining pharmacological interventions is in its infancy. Although limited, results are promising and suggest that a wide array of pharmacological interventions may be leveraged in the treatment of IGD. Additional research is needed to further our understanding of pharmacological treatments for IGD. In particular, future studies using the gold standard methodology (i.e., double-blind randomized controlled trials), recruiting adequate sample sizes, controlling for psychiatric comorbidities, and consisting of more representative samples would better inform our understanding of the potential pharmacological treatments for this increasingly prevalent disorder. Moreover, an important direction for future research will be to explore heterogeneity in IGD presentation and treatment response to inform the selection of optimal treatments.
Acknowledgments
We would like to thank Ms. Kelly Dermody for their assistance with the search strategy.
Footnotes
Availability of Data and Material
Data sharing not applicable to this article as no datasets were generated or analyzed during the study.
Conflicts of Interest
The authors have no potential conflicts of interest to disclose.
Author Contributions
Conceptualization: Rafael Richard Clorado de Sá, Hyoun Soo Kim, Hermano Tavares. Data curation: Sophie Coelho, Puneet Kaur Parmar, Hyoun Soo Kim. Formal analysis: Sophie Coelho, Puneet Kaur Parmar, Samantha Johnstone. Supervision: Hyoun Soo Kim, Hermano Tavares. Visualization: Sophie Coelho, Puneet Kaur Parmar. Writing—original draft: Rafael Richard Clorado de Sá, Sophie Coelho, Puneet Kaur Parmar, Samantha Johnstone. Writing—review & editing: Sophie Coelho, Puneet Kaur Parmar, Hyoun Soo Kim, Hermano Tavares.
Funding Statement
None
Supplementary Materials
The online-only Data Supplement is available with this article at https://doi.org/10.30773/pi.2022.0297.
REFERENCES
- 1.ICD-11 for Mortality and Morbidity Statistics [Internet] Available at: https://icd.who.int/browse11/l-m/en. Accessed August 1, 2022.
- 2.Stevens MW, Dorstyn D, Delfabbro PH, King DL. Global prevalence of gaming disorder: a systematic review and meta-analysis. Aust N Z J Psychiatry. 2021;55:553–568. doi: 10.1177/0004867420962851. [DOI] [PubMed] [Google Scholar]
- 3.Király O, Griffiths MD, Urbán R, Farkas J, Kökönyei G, Elekes Z, et al. Problematic internet use and problematic online gaming are not the same: findings from a large nationally representative adolescent sample. Cyberpsychol Behav Soc Netw. 2014;17:749–754. doi: 10.1089/cyber.2014.0475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moreno M, Riddle K, Jenkins MC, Singh AP, Zhao Q, Eickhoff J. Measuring problematic internet use, internet gaming disorder, and social media addiction in young adults: cross-sectional survey study. JMIR Public Health Surveill. 2022;8:e27719. doi: 10.2196/27719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zajac K, Ginley MK, Chang R. Treatments of internet gaming disorder: a systematic review of the evidence. Expert Rev Neurother. 2020;20:85–93. doi: 10.1080/14737175.2020.1671824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stevens MWR, King DL, Dorstyn D, Delfabbro PH. Cognitive-behavioral therapy for internet gaming disorder: a systematic review and meta‐analysis. Clin Psychol Psychother. 2019;26:191–203. doi: 10.1002/cpp.2341. [DOI] [PubMed] [Google Scholar]
- 7.Park JH, Lee YS, Sohn JH, Han DH. Effectiveness of atomoxetine and methylphenidate for problematic online gaming in adolescents with attention deficit hyperactivity disorder. Hum Psychopharmacol. 2016;31:427–432. doi: 10.1002/hup.2559. [DOI] [PubMed] [Google Scholar]
- 8.Song J, Park JH, Han DH, Roh S, Son JH, Choi TY, et al. Comparative study of the effects of bupropion and escitalopram on internet gaming disorder. Psychiatry Clin Neurosci. 2016;70:527–535. doi: 10.1111/pcn.12429. [DOI] [PubMed] [Google Scholar]
- 9.Bae S, Hong JS, Kim SM, Han DH. Bupropion shows different effects on brain functional connectivity in patients with internet-based gambling disorder and internet gaming disorder. Front Psychiatry. 2018;9:130. doi: 10.3389/fpsyt.2018.00130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Han DH, Renshaw PF. Bupropion in the treatment of problematic online game play inpatients with major depressive disorder. J Psychopharmacol. 2012;26:689–696. doi: 10.1177/0269881111400647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuss DJ, Pontes HM, Griffiths MD. Neurobiological correlates in internet gaming disorder: a systematic literature review. Front Psychiatry. 2018;9:166. doi: 10.3389/fpsyt.2018.00166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weinstein A, Lejoyeux M. Neurobiological mechanisms underlying internet gaming disorder. Dialogues Clin Neurosci. 2020;22:113–126. doi: 10.31887/DCNS.2020.22.2/aweinstein. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goslar M, Leibetseder M, Muench HM, Hofmann SG, Laireiter AR. Pharmacological treatments for disordered gambling: a meta-analysis. J Gambl Stud. 2019;35:415–445. doi: 10.1007/s10899-018-09815-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Grant JE, Odlaug BL, Schreiber LR. Pharmacological treatments in pathological gambling. Br J Clin Pharmacol. 2014;77:375–381. doi: 10.1111/j.1365-2125.2012.04457.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van den Brink W. Evidence-based pharmacological treatment of substance use disorders and pathological gambling. Curr Drug Abuse Rev. 2012;5:3–31. doi: 10.2174/1874473711205010003. [DOI] [PubMed] [Google Scholar]
- 16.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- 17.Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 18.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, Viswanathan M, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim SM, Han DH, Lee YS, Renshaw PF. Combined cognitive behavioral therapy and bupropion for the treatment of problematic on-line game play in adolescents with major depressive disorder. Comp Hum Behav. 2012;28:1954–1959. [Google Scholar]
- 20.Han DH, Lee YS, Na C, Ahn JY, Chung US, Daniels MA, et al. The effect of methylphenidate on internet video game play in children with attention deficit/hyperactivity disorder. Compr Psychiatry. 2009;50:251–256. doi: 10.1016/j.comppsych.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 21.Han DH, Hwang JW, Renshaw PF. Bupropion sustained release treatment decreases craving for video games and cue-induced brain activity in patients with internet video game addiction. Exp Clin Psychopharmacol. 2010;18:297–304. doi: 10.1037/a0020023. [DOI] [PubMed] [Google Scholar]
- 22.Kim YJ, Lee JY, Oh S, Park M, Jung HY, Sohn BK, et al. Associations between prospective symptom changes and slow-wave activity in patients with internet gaming disorder: a resting-state EEG study. Medicine (Baltimore) 2017;96:e6178. doi: 10.1097/MD.0000000000006178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lim JA, Lee JY, Jung HY, Sohn BK, Choi SW, Kim YJ, et al. Changes of quality of life and cognitive function in individuals with internet gaming disorder: a 6-month follow-up. Medicine (Baltimore) 2016;95:e5695. doi: 10.1097/MD.0000000000005695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Park M, Kim YJ, Choi JS. Sustained dysfunctional information processing in patients with internet gaming disorder: 6-month follow-up ERP study. Medicine (Baltimore) 2017;96:e7995. doi: 10.1097/MD.0000000000007995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park S, Ryu H, Lee JY, Choi A, Kim DJ, Kim SN, et al. Longitudinal changes in neural connectivity in patients with internet gaming disorder: a resting-state EEG coherence study. Front Psychiatry. 2018;9:252. doi: 10.3389/fpsyt.2018.00252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nam B, Bae S, Kim SM, Hong JS, Han DH. Comparing the effects of bupropion and escitalopram on excessive internet game play in patients with major depressive disorder. Clin Psychopharmacol Neurosci. 2017;15:361–368. doi: 10.9758/cpn.2017.15.4.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Young KS. Internet addiction: the emergence of a new clinical disorder. CyberPsychology Behav. 1998;1:237–244. [Google Scholar]
- 28.Young KS. Psychology of computer use: XL. Addictive use of the internet: a case that breaks the stereotype. Psychol Rep. 1996;79:899–902. doi: 10.2466/pr0.1996.79.3.899. [DOI] [PubMed] [Google Scholar]
- 29.Entertainment Software Association 2020 essential facts about the video game industry [Internet] Available at: https://www.theesa.com/resource/2020-essential-facts/. Accessed August 1, 2022.
- 30.Interactive Software Federation of Europe Videogames in Europe: consumer study. European summary report November 2012 [Internet] Available at: https://www.isfe.eu/wp-content/uploads/2018/11/euro_summary_-_isfe_consumer_study.pdf. Accessed August 1, 2022.
- 31.Pesquisa Game Brazil Understand the consumer behaviour of Latin American gamers [Internet] Available at: https://www.pesquisagamebrasil.com.br/pt/. Accessed August 1, 2022.
- 32.Abijo T, Blum K, Gondré-Lewis MC. Neuropharmacological and neurogenetic correlates of opioid use disorder (OUD) as a function of ethnicity: relevance to precision addiction medicine. Curr Neuropharmacol. 2020;18:578–595. doi: 10.2174/1570159X17666191118125702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Avinun R, Nevo A, Radtke SR, Brigidi BD, Hariri AR. Divergence of an association between depressive symptoms and a dopamine polygenic score in Caucasians and Asians. Eur Arch Psychiatry Clin Neurosci. 2020;270:229–235. doi: 10.1007/s00406-019-01040-x. [DOI] [PubMed] [Google Scholar]
- 34.González-Bueso V, Santamaría JJ, Fernández D, Merino L, Montero E, Ribas J. Association between internet gaming disorder or pathological video-game use and comorbid psychopathology: a comprehensive review. Int J Environ Res Public Health. 2018;15:668. doi: 10.3390/ijerph15040668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cahill K, Stevens S, Perera R, Lancaster T. Pharmacological interventions for smoking cessation: an overview and network meta‐analysis. Cochrane Database Syst Rev. 2013;5:CD009329. doi: 10.1002/14651858.CD009329.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thase ME, Haight BR, Richard N, Rockett CB, Mitton M, Modell JG, et al. Remission rates following antidepressant therapy with bupropion or selective serotonin reuptake inhibitors: a meta-analysis of original data from 7 randomized controlled trials. J Clin Psychiatry. 2005;66:974–981. doi: 10.4088/jcp.v66n0803. [DOI] [PubMed] [Google Scholar]
- 37.Trivedi MH, Rush AJ, Carmody TJ, Donahue RM, Bolden-Watson C, Houser TL, et al. Do bupropion SR and sertraline differ in their effects on anxiety in depressed patients? J Clin Psychiatry. 2001;62:776–781. doi: 10.4088/jcp.v62n1005. [DOI] [PubMed] [Google Scholar]
- 38.Moriyama TS, Polanczyk GV, Terzi FS, Faria KM, Rohde LA. Psychopharmacology and psychotherapy for the treatment of adults with ADHD—a systematic review of available meta-analyses. CNS Spectr. 2013;18:296–306. doi: 10.1017/S109285291300031X. [DOI] [PubMed] [Google Scholar]
- 39.Blum K, Chen AL, Braverman ER, Comings DE, Chen TJ, Arcuri V, et al. Attention-deficit-hyperactivity disorder and reward deficiency syndrome. Neuropsychiatr Dis Treat. 2008;4:893–918. doi: 10.2147/ndt.s2627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Belujon P, Grace AA. Dopamine system dysregulation in major depressive disorders. Int J Neuropsychopharmacol. 2017;20:1036–1046. doi: 10.1093/ijnp/pyx056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oprea DC, Moldovan MA, Chirija R, Bolos A. Behavioural addictions and the role of dopamine. Bull Integr Psychiatry. 2021;27:63–70. [Google Scholar]
- 42.Dannon PN, Lowengrub K, Musin E, Gonopolski Y, Kotler M. Sustained-release bupropion versus naltrexone in the treatment of pathological gambling: a preliminary blind-rater study. J Clin Psychopharmacol. 2005;25:593–596. doi: 10.1097/01.jcp.0000186867.90289.ed. [DOI] [PubMed] [Google Scholar]
- 43.Stahl SM, Pradko JF, Haight BR, Modell JG, Rockett CB, Learned-Coughlin S. A review of the neuropharmacology of bupropion, a dual norepinephrine and dopamine reuptake inhibitor. Prim Care Companion J Clin Psychiatry. 2004;6:159–166. doi: 10.4088/pcc.v06n0403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bymaster FP, Katner JS, Nelson DL, Hemrick-Luecke SK, Threlkeld PG, Heiligenstein JH, et al. Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder. Neuropsychopharmacology. 2002;27:699–711. doi: 10.1016/S0893-133X(02)00346-9. [DOI] [PubMed] [Google Scholar]
- 45.Regner MF, Saenz N, Maharajh K, Yamamoto DJ, Mohl B, Wylie K, et al. Top-down network effective connectivity in abstinent substance dependent individuals. PLoS One. 2016;11:e0164818. doi: 10.1371/journal.pone.0164818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Han DH, Kim SM, Bae S, Renshaw PF, Anderson JS. A failure of suppression within the default mode network in depressed adolescents with compulsive internet game play. J Affect Disord. 2016;194:57–64. doi: 10.1016/j.jad.2016.01.013. [DOI] [PubMed] [Google Scholar]
- 47.Hong JS, Kim SM, Bae S, Han DH. Impulsive internet game play is associated with increased functional connectivity between the default mode and salience networks in depressed patients with short allele of serotonin transporter gene. Front Psychiatry. 2018;9:125. doi: 10.3389/fpsyt.2018.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zacharias N, Musso F, Müller F, Lammers F, Saleh A, London M, et al. Ketamine effects on default mode network activity and vigilance: a randomized, placebo‐controlled crossover simultaneous fMRI/EEG study. Hum Brain Mapp. 2020;41:107–119. doi: 10.1002/hbm.24791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Murphy CE, 4th, Wang RC, Montoy JC, Whittaker E, Raven M. Effect of extended-release naltrexone on alcohol consumption: a systematic review and meta-analysis. Addiction. 2022;117:271–281. doi: 10.1111/add.15572. [DOI] [PubMed] [Google Scholar]
- 50.Syed YY, Keating GM. Extended-release intramuscular naltrexone (VIVITROL®): a review of its use in the prevention of relapse to opioid dependence in detoxified patients. CNS Drugs. 2013;27:851–861. doi: 10.1007/s40263-013-0110-x. [DOI] [PubMed] [Google Scholar]
- 51.Mouaffak F, Leite C, Hamzaoui S, Benyamina A, Laqueille X, Kebir O. Naltrexone in the treatment of broadly defined behavioral addictions: a review and meta-analysis of randomized controlled trials. Eur Addict Res. 2017;23:204–210. doi: 10.1159/000480539. [DOI] [PubMed] [Google Scholar]
- 52.Gour R, Hiral K, Srikanth R, Rathi PS. Use of naltrexone in internet gaming disorder. Indian J Psychiatry. 2022;64(Suppl 3):S682. [Google Scholar]
- 53.Király O, Böthe B, Ramos-Diaz J, Rahimi-Movaghar A, Lukavska K, Hrabec O, et al. Ten item internet gaming disorder test (IGDT10): measurement invariance and cross-cultural validation across seven language-based samples. Psychol Addict Behav. 2019;33:91–103. doi: 10.1037/adb0000433. [DOI] [PubMed] [Google Scholar]
- 54.King DL, Delfabbro PH, Perales JC, Deleuze J, Király O, Krossbakken E, et al. Maladaptive player-game relationships in problematic gaming and gaming disorder: a systematic review. Clin Psychol Rev. 2019;73:101777. doi: 10.1016/j.cpr.2019.101777. [DOI] [PubMed] [Google Scholar]
- 55.Park JH, Han DH, Kim BN, Cheong JH, Lee YS. Correlations among social anxiety, self-esteem, impulsivity, and game genre in patients with problematic online game playing. Psychiatry Investig. 2016;13:297–304. doi: 10.4306/pi.2016.13.3.297. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.