Abstract
Objective
The primary objective of this review was to summarize systematic reviews and meta-analyses reporting on nonoperative management of lateral epicondyle tendinopathy.
Methods
An umbrella review of all published systematic reviews and meta-analyses was performed. Three databases were searched using the key words “tennis elbow,” “lateral epicondylitis,” “non-operative,” and “non-surgical modalities.” The search was limited to English-language systematic reviews and meta-analyses between the years of 2000 and 2022.
Results
There were 114 systematic reviews/meta-analyses, of which 35 met our inclusion criteria. These articles reviewed the following nonoperative management strategies: ultrasound, shockwave therapy, injection procedures, low-level laser therapy, joint mobilizations, exercise therapy, and electrophysical modalities. Exercise therapy was beneficial in decreasing pain regardless of dosage or type. Conflicting results were seen with ultrasound, laser, and shockwave therapy. Corticosteroid injections provided the most short-term pain relief, and platelet-rich plasma and autologous blood injections were most effective in the long term.
Conclusion
A variety of nonoperative interventions were found to be effective for short- and long-term pain relief as well as functional improvement, with most interventions indicating mixed results. Due to variations in study populations and study quality, results should be interpreted with caution.
Key Indexing Terms: Tennis Elbow, Conservative Treatment, Exercise Therapy, Physical Therapy Modalities, Injections
Introduction
Lateral epicondyle tendinopathy (LET), commonly known as “tennis elbow,” is a common disorder of the arm1 that was first reported by Runge in 1873.2 With a prevalence of between 1% and 5.2% in the general population, it is estimated that 1 million people in the United States develop new-onset LET each year.3 The usual symptoms associated with LET are pain over the lateral aspect of the elbow, pain and weakness on wrist extension, and pain when gripping objects. These symptoms can last for up to 2 years3,4 and can have detrimental effects on activities of daily living.
The main cause of LET is repetitive microtrauma to the origin of the extensor and supinator muscles of the forearm (primarily extensor carpi radialis brevis) on the humeral epicondyle.5, 6, 7, 8 These microtraumas are typically provoked by repetitive athletic or occupational tasks.5 While it is generally agreed that repetitive use can result in microtears/micro-ruptures, a consensus has not been reached regarding an inflammatory component of LET.9, 10, 11, 12 In fact, many studies are suggesting LET is a degenerative tendinous disease and recommend renaming it as a tendinosis4,8 or a tendinopathy13 instead of using the infllammatory term of lateral epicondylitis.
Current treatment guidelines recommend conservative care as first-line therapy,14,15 but there is no clear preferred conservative treatment method as ultrasound, exercise, manual therapies, electrical modalities, laser therapies, and various injection procedures are commonly used. Corticosteroid injections (CSI) were previously considered gold-standard treatment; however, this is becoming increasingly discouraged due to a high reoccurrence rate.16,17 More recently, providers are transitioning to platelet-rich plasma injections (PRP) or autologous blood (AB) injections for nonoperative options. Given the variety of nonoperative interventions available, an umbrella review methodology is ideal to synthesize systematic reviews and meta-analyses studying these interventions. The primary aim of this umbrella review was to summarize the available evidence in regard to nonoperative management of LET.
Methods
Umbrella reviews summarize evidence from multiple research syntheses, including systematic reviews and meta-analyses, and provide a synthesis of findings on a particular topic to determine whether the evidence base is consistent or contradictory.18 This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
The research question guiding this umbrella review was, what nonoperative management strategies have been reported for LET, and which strategies optimally improve pain and function? The nonoperative terms included in this review were guided by 2 articles19,20 investigating nonoperative treatments for LET.
A literature search of 3 databases (PubMed, CINAHL, and Cochrane Library of Systematic reviews) was conducted on October 7, 2022. A detailed description of the search strategy for each database can be found in the Supplementary Data. The search was limited to English language systematic reviews and meta-analyses including human participants with a date range of 2000 to present.
The following Population Intervention Comparison Outcome (PICO) question guided the inclusion/exclusion criteria: A population (P) of men and women over the age of 18 diagnosed with LET; Interventions (I) were nonoperative treatments,19,20 namely injections (CSI, botulinum [BT] toxin, saline, prolotherapy, PRP, and AB), exercise therapy, electric stimulation, extracorporeal shockwave therapy (ESWT), joint manipulation, and low-level light therapy; Comparison (C) between the different nonoperative treatments; Outcome (O) measures included verbal/visual analog scale, Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire, Patient-rated Tennis Elbow Evaluation (PRTEE), Upper Extremity Functional Index, and/or grip strength. Studies were excluded if: (1) LET was not the primary condition being evaluated; (2) published before 2000; (3) review papers published after 2000 which included clinical trials published prior to 2000; (4) not a systematic review or meta-analysis; (5) was not written or translated into English; and (6) did not investigate at least 1 of the interventions previously described.
All citations resulting from the search process described in the Supplementary Data were imported into the software program Covidence,21 which automatically removes duplicate citations. Two reviewers independently screened all citations for eligibility in 3 stages (title, abstract, and full text). Any consensus disagreements were discussed, with 1 author (B.A.) having the final decision. The following information was extracted and entered into a data table: title; authors; citation; aim; study design; start and end date; patient population; inclusion/exclusion criteria; number of studies; number of participants; qualitative description of results (systematic reviews); quantitative results (meta-analyses); and results summary.
The JBI Critical Appraisal Checklist for systematic reviews and research synthesis18 was used for bias assessment. Extraction and bias assessment was performed by 1 author (B.A.) and verified by the second author (W.K.). The JBI checklist contains 11 questions, with a yes/no answer for each. Questions 6 and 7 could not be adequately evaluated for the majority of studies, so each study was graded on a 0 to 9 scale (see Supplementary Data for checklist).
Results
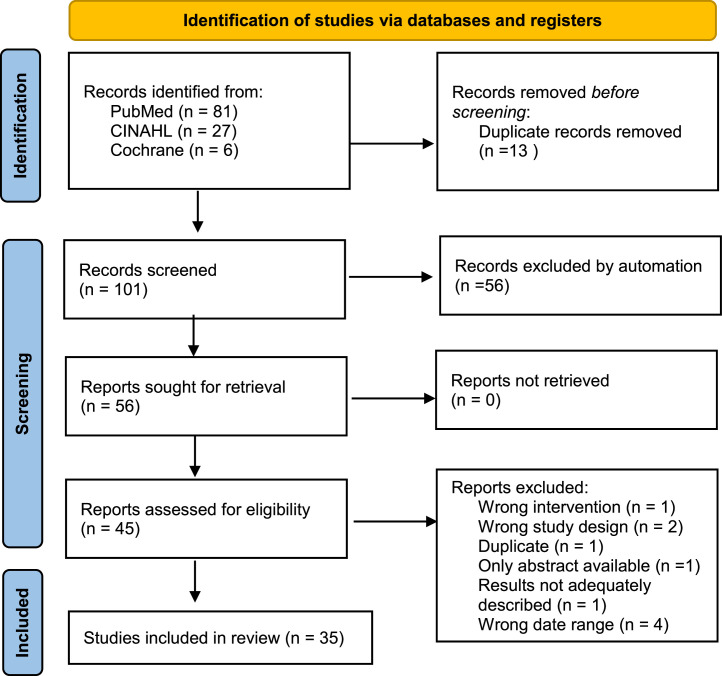
The initial search identified 114 articles, with 101 screened for inclusion and 35 included in the final review (Fig 1). The characteristics of these articles can be found in the Supplementary Data table and are summarized by intervention category below. Within the included studies22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56 the number of participants ranged from 20322 to 8656.23 The visual analog scale (VAS) was used in the majority of studies to evaluate pain-related outcomes. Only 3 studies24, 25, 26 did not include a functional outcome such as DASH, PRTEE, or grip strength. The JBI score of the included studies ranged from 5/9 to 9/9, with the majority indicating a low risk of bias. The most common interventions studied were PRP injections (11 studies), ESWT (8 studies), CSI (6 studies), and exercise therapy (6 studies).
Fig 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram.
Summary Description of Findings
Injection Therapies (PRP, AB, CSI, BT, Hyaluronic Acid, Peppering Technique, Prolotherapy, and Glycosaminoglycan Polysulfate)
Arirachakara et al27 (n = 10) compared PRP, AB, and CSI. PRP injections significantly improved pain and PRTEE score vs AB and steroid injections. CSI significantly improved DASH score and pressure pain threshold vs AB injection. AB injection had a significantly higher chance of adverse effects when compared with CSI. de Vos et al28 (n = 6) compared PRP, CSI, and AB using VAS, DASH, Liverpool elbow score (LPES), and PRTEE as outcome measures. The mean improvement across studies was 59.6%, however, the authors indicated there is currently strong evidence that PRP injections are not efficacious for chronic LET. Ahmad et al29 (n = 9) compared the use of PRP to CSI, blood injections, and bupivacaine. All groups demonstrated a decrease in pain and increase in function, with PRP performing best in this regard. While there was some debate over the efficacy of PRP vs CSI, 1 of the studies that had a larger cohort demonstrated that PRP was in fact superior to CSI. PRP showed improvement in pain scores for those that had previously failed physiotherapy (PT). Dong et al25 (n = 27) compared a variety of injections (AB, BT, CSI, glycosaminoglycan polysulfate, hyaluronic acid, peppering technique, prolotherapy [PRO], and PRP) using VAS as an outcome measure. They concluded that BT, PRP, and AB injections are good treatment options regarding VAS improvement in the intermediate term (6 months/26 weeks), but not CSI. Hyaluronic acid and PRO might be more effective, but their superiority must be confirmed by more evidence. Song et al22 (n = 7) evaluated outcomes with different BT injection sites. Using VAS and grip strength as outcome measures, injecting BT at one-third of the length of the forearm distal to the lateral epicondyle along the course of the posterior interosseous nerve demonstrated the most pain relief. Houck et al23 (n = 9) indicated AB and PRP showed a significantly greater improvement vs placebo between 8 and 52 weeks using a variety of outcome measures. Their meta-analysis concluded that CSI improves functional outcomes and pain relief in the short term, while AB and PRP are the most effective treatment options in the intermediate term. Huang et al30 (n = 8 LET, n = 12 plantar fasciitis) found CSI is superior to PRP in short-term pain improvement, with PRP showing statistically and clinically better improvement in long-term pain relief than CSI treatment (moderate quality evidence). There was no difference in short-term DASH score improvement between the 2 interventions. Kalichman et al31 (n = 4) found moderate benefit for BT injection on pain outcomes at 3 months, with no statistical or clinical difference in grip strength during this same follow-up period, although a trend was seen favoring BT. Li et al32 (n = 7) compared PRP to CSI using DASH, VAS, and modified Mayo performance index for elbow (MAYO) scores. Local CSI demonstrated a favorable outcome (DASH score) vs PRP treatments at 4 and 8 weeks after treatment. At long-term follow-up (24 weeks), PRP injections were associated with improved pain and function (VAS and DASH score) vs CSI. Kemp et al33 (n = 5) evaluated PRP, CSI, and AB using both pain and functional metrics. They report that PRP is more effective than CSI in the long term with regard to pain, function, disability, and pressure pain threshold. Krogh et al34 (n = 17) found that beyond 8 weeks, CSI was no more effective than placebo. Meta-analysis showed that AB, PRP, prolotherapy, and hyaluronic acid were all more effective than placebo. Lin et al35 (n = 6) evaluated BT and CSI vs the placebo group and found BT significantly reduced pain at 2 to 4 weeks, 8 to 12 weeks, and 16 weeks after injection. However, BT was significantly less effective than CSI at 2 to 4 weeks’ follow-up. CSI and BT were largely equivalent, except CSI was better at pain relief in early stages and did not decrease grip strength. No differences were observed at 8- to 12- or 16-week follow-up periods. Niemiec et al36 (n = 26) used a combination of functional and pain scales to evaluate PRP. Both VAS and PRTEE showed greater improvement between 4- and 52-week follow-up. DASH improvement varied between 27% (week 4) and 77% (year 2), and improvement in the MAYO score was seen throughout the 4- to 52-week follow-up periods. Rabago et al37 (n = 9) investigated PRO, polidocanol, AB, and PRP with VAS and grip strength as outcome measures. Ultrasound (US)–guided polidocanol treatment improved VAS, grip strength scores, and structural defects as visualized by US at 3 and 8 months. A single PRP injection improved symptoms by a mean of 81% at 27 weeks vs control. One RCT compared polidocanol with vasoconstrictive lidocaine/adrenaline injections; significant changes at 12-month follow-up were seen only after receiving an additional injection at 3 months. PRO was associated with a 90% improvement at 16 weeks (vs 22% for controls). Three studies reported an improvement in outcome measures with AB compared with control. Simental-Mendía et al38 (n = 10) found no significant difference in improvement with regard to pain and joint functionality (VAS, DASH, and PRTEE) between PRP and placebo injections. Tang et al39 (n = 20) investigated PRP, AB, and CSI using a combination of functional and pain scales. PRP was associated with more improvement in pain intensity and function in the long term than were the comparators. CSI was associated with the most improvement in short-term pain ratings. No significant strength differences were found between interventions. Acosta-Olivo et al.40 (n = 15) compared the use of saline (usually used as a placebo intervention) to no intervention by measuring VAS, DASH, and PRTEE and found that the saline injection resulted in a reduction of VAS with significant improvements in PRTEE and DASH scores.
Passive Modalities
Bjordal et al41 (n = 13) compared low level light therapy (LLLT) to placebo, and found LLLT (904 nm, 632 nm wavelength) to have better overall outcomes. Buchbinder et al42 (n = 12) evaluated EWST vs other treatments or placebo. Data from 6 trials could be pooled, which concluded that ESWT is no more effective than placebo for LET. One trial reported CSI was more effective than ESWT at 3 months as measured by 50% pain reduction and found mean pain scores at 6 weeks favored CSI over ESWT. Yoon et al43 (n = 12) compared ESWT with placebo using VAS and grip strength as outcome measures. ESWT was not associated with clinically important improvement in pain reduction and grip strength; however, radial ESWT showed better effects than the focused type of ESWT. Dingemanse et al44 (n = 22) evaluated the effectiveness of a variety of electrophysical modalities. There was some evidence that US is more effective than placebo on midterm follow-up, and US plus friction massage showed moderate evidence of improvement versus LLLT in the short term. On the contrary, moderate evidence was found in favor of LLLT over plyometric exercises at short-term follow-up. For all other modalities only limited, conflicting, or evidence of no difference in effect was found. Zheng et al45 (n = 9) focused on ESWT and LLLT vs placebo or sham and used functional and pain scales as outcome measures. They concluded that ESWT cannot effectively reduce the mean overall pain, but that more patients achieved a 50% pain reduction vs placebo. Three studies showed a clinically significant improvement in grip strength in the ESWT group compared with controls at 12 weeks. Karanasios et al46 (n = 16) examined ESWT vs US, LLLT, or sham. They found that ESWT presented no clinical benefits compared with sham or control treatment in pain intensity, grip strength, and elbow disability at all follow-up periods. ESWT performed better than LLLT when evaluating grip strength and better than US when evaluating pain intensity. Yan et al47 (n = 5) evaluated ESWT vs US using VAS and grip strength as outcomes. The ESWT group showed a significantly larger reduction in pain at 1-month follow-up, whereas the US group took 3 months to show similar improvement. ESWT had a better recovery of grip strength compared with the US group at 1 and 6 months. There was no significant difference in function scores between the 2 treatments at 3 months follow-up. Yao et al48 (n = 13) compared ESWT to a control group and used both VAS and grip strength as outcome measures. The pooled data showed significantly lower VAS scores in the ESWT group, although significant heterogeneity was observed among included studies. Patients in the ESWT group also significantly increased their grip strength scores.
Exercise and Manual Therapy
Keating et al26 (n = 18) focused on various types and dosage of exercises using VAS as the only outcome measure. The authors found that regardless of dosage, exercise is effective in reducing pain in LET; however, due to lack of comparison between dosing parameters, the optimal dosage is unclear. Hoogvliet et al49 (n = 13) focused on different types of exercise programs and mobilizations using both functional and pain-focused outcome measures. One high-quality study found a significant benefit in favor of stretching plus strengthening exercises on pain. Significant differences were found in grip strength at 6 months favoring eccentric exercise vs stretching but no significant results were seen at 3 and 12 months. Significant differences in favor of the Mulligan mobilization as an add-on to US were found on pain and weight test outcomes at the 3 months follow-up. Moderate evidence for a short-term effect of stretching plus strengthening exercises compared with US plus friction massage in the short term was found. Lucado et al50 (n = 27) investigated various mobilization techniques with functional and pain-related outcomes used. Mobilization with movement and Mill's manipulation techniques were found to be more beneficial than comparison groups at improving VAS at short and intermediate follow-up periods. No significant change was shown with respect to grip strength for mobilization with movement. Raman et al51 (n = 11) evaluated various resistance exercise regimens using VAS and grip strength among other functional tests as outcome measures. All exercise variations showed some degree of improvement in pain and function; however, no major differences were found between the types of exercises.
Combined Interventions
Buchbinder et al24 (n = 9) focused on ESWT and CSI vs placebo. The authors concluded that ESWT is no more effective than placebo for LET. Although 3 trials reported highly significant differences in favor of ESWT, these results became nonsignificant when combined with results of studies that reported no or minimal benefit over placebo. CSI was shown to have a greater impact on pain reduction after 3 months compared to ESWT. Chen and Baker52 (n = 8) investigated exercises in combination with other conservative therapies. In the short term, eccentric strengthening was found to be superior to other treatments at reducing pain and improving function with large effect sizes; however, no significant changes were noted in the intermediate timeframe. Cullinane et al53 (n = 12) compared eccentric strengthening alone and in combination with iontophoresis and US and stretching using both functional and pain measures as outcomes. Eccentric exercise programs used as an adjunct to other therapies were associated with decreased pain and improved function and grip strength vs baseline. Lian et al54 (n = 36) investigated ESWT, LLLT, CSI, PRP, and BT, using VAS and grip strength as outcome measures. Local CSI significantly reduced VAS only at short-term follow-up. Additionally, both LLLT and local BT injection were associated with significant pain relief at midterm follow-up. ESWT was the only therapy shown to have an effect at long-term follow-up, and LLLT was the only modality that improved grip strength. Barr et al55 (n = 5) evaluated CSI, physiotherapeutic interventions and a wait-and-see group and demonstrated that CSI was significantly more effective than PT for outcome measurements between 3 and 7 weeks. For intermediate term outcomes, 3 studies found PT significantly more effective. Karanasios et al56 (n = 21) investigated PT, CSI, exercises, mobilizations, and wait-and-see interventions using both functional and pain outcome measures. CSI had lower pain scores than other interventions only in the short term. No difference between eccentric and concentric exercise was found. Conflicting results were seen with mobilization plus PT regarding improvements in pain. Very low certainty evidence for improvement was found for an exercise intervention vs CSI in all outcomes at all follow-up occasions. In summary, interventions with an active treatment component performed better than passive interventions, but the effects are small.
Discussion
This umbrella review analyzed the literature to investigate the treatment effects of individual and combined nonoperative interventions in the management of patients with LET.
The majority of interventions in this review show inconsistent results. Four studies24,42,43,46 documented that ESWT was no more effective than placebo/control; this was contradicted by another study45 showing ESWT to be superior vs control. Exercise was beneficial in reducing pain and improving function; however, there was a lack of consensus regarding optimal dosage or type of exercise. Regarding injection therapies, CSI seems to be associated with optimal short-term outcomes while PRP and AB had better long-term results.
Practical Application
Injections
The general trend in the literature demonstrates that the use of CSI has a greater effect on pain and functional scores in the short term, whereas PRP has been shown to have more favorable long-term effects. Both AB and BT decrease pain and improve function. Botulinum injections one-third of the length of the forearm distal to lateral epicondyle demonstrated the most pain relief, and injecting 1 cm inferior from the lateral epicondyle produced the most improvement in grip strength. Lastly, although clinical effectiveness may be similar among injection procedures, cost-effectiveness favors AB and CSI over PRP.
Passive Modalities
No consensus exists as to the optimal passive modality. Low level light therapy was shown to outperform placebo, and shockwave therapy was shown to outperform LLLT, while 1 study noted no difference between shockwave and placebo. Ultrasound was shown to be inferior to shockwave. Therefore, while no consensus exists, the current evidence points toward using shockwave therapy for decreasing pain and improving function.
Exercise and Manual Therapy
No optimal dosage or exercise types have been established. Eccentric exercise was shown to be more beneficial compared with stretching only. The combination of exercise and stretching were more beneficial than US and friction massage. Active modalities were superior to passive modalities for decreasing pain. In short, exercise was shown to improve function and decrease pain.
Combined Interventions
Short-term pain relief favored CSI in comparison to all other passive or exercise modalities. For mid- and long-term outcomes, physiotherapeutic rehab, LLLT, BT, and ESWT were shown to have better improvement in pain scores when compared to injections. Eccentric exercise was shown to decrease pain and improve function when used as an adjunctive therapy. Conflicting evidence exists between the use of mobilization and PT, although any therapy was more beneficial when compared with a waiting group.
Limitations
Limitations to this umbrella review include the following: (1) some relevant articles may have been missed due to publication language eligibility, search strategy used, and date limits set; (2) the use of the same RCT in separate systematic reviews or meta-analyses could have influenced the results of this study; and (3) the diversity of populations, dosing of interventions, and methodological quality of the included studies all lead to complications in developing strong conclusions.
Conclusion
This umbrella review summarizes the results of systematic reviews and meta-analyses on the nonoperative management of LET conducted between the years 2000 and 2022. A wide range of management strategies exist, although the quality of evidence is lacking. A lack of demographic diversity limits the interpretation of different management strategies in different populations. The consistent use of both functional and pain outcome measures would help standardize results of clinical trials in the management of LET. Lastly, nonoperative vs operative management strategies should be further investigated, as direct evidence comparing these management strategies is lacking. Addressing these limitations would allow clinicians to have a better understanding of best practices for managing patients with LET.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.jcm.2023.04.004.
Funding Sources and Conflicts of Interest
No funding sources or conflicts of interest were reported for this study.
Contributorship Information
Concept development (provided idea for the research): W.K., B.A.
Design (planned the methods to generate the results): W.K., B.A.
Supervision (provided oversight, responsible for organization and implementation, writing of the manuscript): B.A.
Data collection/processing (responsible for experiments, patient management, organization, or reporting data): W.K., B.A.
Analysis/interpretation (responsible for statistical analysis, evaluation, and presentation of the results): W.K., B.A.
Literature search (performed the literature search): W.K., B.A.
Writing (responsible for writing a substantive part of the manuscript): W.K., B.A.
Critical review (revised manuscript for intellectual content, this does not relate to spelling and grammar checking): B.A.
Practical Applications.
-
•
Inconsistent results were reported for passive modalities (shockwave therapy, ultrasound, and laser).
-
•
Exercise was beneficial in reducing pain and improving function; however, there was a lack of consensus regarding optimal dosage or type of exercise.
-
•
Corticosteroid injections seemed to be associated with optimal short-term outcomes, and platelet rich plasma and autologous blood injections had better long-term results.
Alt-text: Unlabelled box
Appendix. Supplementary materials
References
- 1.Shiri R, Viikari-Juntura E, Varonen H, Heliovaara M. Prevalence and determinants of lateral and medial epicondylitis: a population study. Am J Epidemiol. 2006;164(11):1065–1074. doi: 10.1093/aje/kwj325. [DOI] [PubMed] [Google Scholar]
- 2.Runge F. On the Genesis and Treatment of Writer's Cramp [English translation from German] Berl Klin Wochenschr. 1873;10(1):245–248. [Google Scholar]
- 3.Sanders TL, Jr, Maradit Kremers H, Bryan AJ, Ransom JE, Smith J, et al. The epidemiology and health care burden of tennis elbow: a population-based study. Am J Sports Med. 2015;43(5):1066–1071. doi: 10.1177/0363546514568087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De Smedt T, de Jong A, Van Leemput W, Lieven D, Van Glabbeek F. Lateral epicondylitis in tennis: update on aetiology, biomechanics and treatment. Br J Sports Med. 2007;41(11):816–819. doi: 10.1136/bjsm.2007.036723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tosti R, Jennings J, Sewards JM. Lateral epicondylitis of the elbow. Am J Med. 2013;126(4) doi: 10.1016/j.amjmed.2012.09.018. 357.e1-6. [DOI] [PubMed] [Google Scholar]
- 6.Buchanan BK, Varacallo M. Tennis Elbow. [Updated 2022 Nov 7]. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing.
- 7.Lieber F. Physiological consequences of surgical lengthening of extensor carpi radialis brevis muscle-tendon junction for tennis elbow. J Hand Surg. 1994;19A:269–274. doi: 10.1016/0363-5023(94)90018-3. [DOI] [PubMed] [Google Scholar]
- 8.Vaquero-Picado A, Barco R, Antuna S. Lateral epicondylitis of the elbow. EFORT Open Rev. 2016;1(11):391–397. doi: 10.1302/2058-5241.1.000049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Faro F, Moriatis Wolf J. Lateral epicondylitis: review and current concepts. J Hand Surg. 2007;32(8):1271–1279. doi: 10.1016/j.jhsa.2007.07.019. [DOI] [PubMed] [Google Scholar]
- 10.Nirschl R. Elbow tendinosis/tennis elbow. Clin J Sport Med. 1992;11(4):851–870. [PubMed] [Google Scholar]
- 11.Doran A, Gresham G, Rushton N, Watson C. Tennis elbow. A clinicopathologic study of 22 cases followed for 2 years. Acta Orthop Scand. 1990;61(6):535–538. doi: 10.3109/17453679008993577. [DOI] [PubMed] [Google Scholar]
- 12.Bhabra G, Wang A, Ebert JR, Edwards P, Zheng M, et al. Lateral elbow tendinopathy: development of a pathophysiology-based treatment algorithm. Orthop J Sports Med. 2016;4(11):1–10. doi: 10.1177/2325967116670635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coombes B, Bisset L, Vicenzino B. Management of lateral elbow tendinopathy: one size does not fit all. J Orthop Sports Phys Ther. 2015;45(11):938–949. doi: 10.2519/jospt.2015.5841. [DOI] [PubMed] [Google Scholar]
- 14.Uygur E, Aktas B, Ozkut A, Erinc S, Yilmazoglu E. Dry needling in lateral epicondylitis: a prospective controlled study. Int Orthop. 2017;41(11):2321–2325. doi: 10.1007/s00264-017-3604-1. [DOI] [PubMed] [Google Scholar]
- 15.Huber L, Granado M. CINAHL Rehabilitation Guide EBSCO Publishing, (Ipswich, Massachusetts); 2021 Oct 22. Epicondylitis, Medial. [Google Scholar]
- 16.Coombes BK, Bisset L, Brooks P, Khan A, Vicenzino B. Effect of corticosteroid injection, physiotherapy, or both on clinical outcomes in patients with unilateral lateral epicondylalgia: a randomized controlled trial. JAMA. 2013;309(5):461–469. doi: 10.1001/jama.2013.129. [DOI] [PubMed] [Google Scholar]
- 17.Gosens T, Peerbooms JC, Van Laar W, Den Oudsten BL. Ongoing positive effect of platelet-rich plasma versus corticosteroid injection in lateral epicondylitis: A double-blind randomized controlled trial with 2-year follow-up. Am J Sports Med. 2011;39(6):1200–1208. doi: 10.1177/0363546510397173. [DOI] [PubMed] [Google Scholar]
- 18.Aromataris E, Fernandez R, Godfrey C, Holly C, Kahlil H, et al. Summarizing systematic reviews: methodological development, conduct and reporting of an umbrella review approach. Int J Evid Based Healthc. 2015;13(3):132. doi: 10.1097/XEB.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 19.Sims SEG, Miller K, Elfar JC, Hammert WC. Non-surgical treatment of lateral epicondylitis: a systematic review of randomized controlled trials. Hand. 2014;9(4):419–446. doi: 10.1007/s11552-014-9642-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lapner P, Alfonso A, Hebert-Davies J, Pollock JW, Marsh J, et al. Nonoperative treatment of lateral epicondylitis: a systematic review and meta-analysis. JSES Int. 2022;6(2):321–330. doi: 10.1016/j.jseint.2021.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Covidence systematic review software, Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org
- 22.Song B, Day D, Jayaram P. Efficacy of botulinum toxin in treating lateral epicondylitis-does injection location matter? A systematic review. Am J Phys Med Rehabil. 2020;99(12):1157–1163. doi: 10.1097/PHM.0000000000001511. [DOI] [PubMed] [Google Scholar]
- 23.Houck DA, Kraeutler MJ, Thornton LB, McCarty EC, Bravman JT. Treatment of lateral epicondylitis with autologous blood, platelet-rich plasma, or corticosteroid injections: a systematic review of overlapping meta-analyses. Orthop J Sports Med. 2019;7(3):1–9. doi: 10.1177/2325967119831052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Buchbinder R, Green SE, Youd JM, Assendelft WJJ, Barnsley L, et al. Shock wave therapy for lateral elbow pain. Cochrane Database Syst Rev. 2005;2005(4) doi: 10.1002/14651858.CD003524.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dong W, Goost H, Lin X-B, Burger C, Wang ZL, et al. Injection therapies for lateral epicondylalgia: A systematic review and Bayesian network meta-analysis. Br J Sports Med. 2016;50(15):900–908. doi: 10.1136/bjsports-2014-094387. [DOI] [PubMed] [Google Scholar]
- 26.Keating C, Bodnar R, Joseph J, Knapp S, Lepage M, et al. Effectiveness of painful loading in lateral elbow tendinopathy on pain outcome: a systemic review. Orthopaedic Physical Therapy Practice. 2020;32(4):208–214. [Google Scholar]
- 27.Arirachakaran A, Sukthuayat A, Sisayanarane T, Laoratanavoraphong S, Kanchanatawan W, et al. Platelet-rich plasma versus autologous blood versus steroid injection in lateral epicondylitis: systematic review and network meta-analysis. J Orthop Traumatol. 2016;17(2):101–112. doi: 10.1007/s10195-015-0376-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.de Vos RJ, Windt J, Weir A. Strong evidence against platelet-rich plasma injections for chronic lateral epicondylar tendinopathy: a systematic review. Br J Sports Med. 2014;48(12):952–956. doi: 10.1136/bjsports-2013-093281. [DOI] [PubMed] [Google Scholar]
- 29.Ahmad Z, Brooks R, Kang SN, Weaver H, Nunney I, et al. The effect of platelet-rich plasma on clinical outcomes in lateral epicondylitis. Arthroscopy. 2013;29(11):1851–1862. doi: 10.1016/j.arthro.2013.07.272. [DOI] [PubMed] [Google Scholar]
- 30.Huang K, Giddins G, Wu L-D. Platelet-rich plasma versus corticosteroid injections in the management of elbow epicondylitis and plantar fasciitis: an updated systematic review and meta-analysis. Am J Sports Med. 2020;48(10):2572–2585. doi: 10.1177/0363546519888450. [DOI] [PubMed] [Google Scholar]
- 31.Kalichman L, Bannuru RR, Severin M, Harvey W. Injection of botulinum toxin for treatment of chronic lateral epicondylitis: systematic review and meta-analysis. Semin Arthritis Rheum. 2011;40(6):532–538. doi: 10.1016/j.semarthrit.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 32.Li A, Wang H, Yu Z, Zhang G, Feng S, et al. Platelet-rich plasma vs corticosteroids for elbow epicondylitis: a systematic review and meta-analysis. Medicine. 2019;98(51):e18358. doi: 10.1097/MD.0000000000018358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kemp JA, Olson MA, Tao MA, Burcal CJ. Platelet-rich plasma versus corticosteroid injection for the treatment of lateral epicondylitis: a systematic review of systematic reviews. Int J Sports Phys Ther. 2021;16(3):597–605. doi: 10.26603/001c.24148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Krogh TP, Fredberg U, Stengaard-Pedersen K, Christensen R, Jensen P, et al. Treatment of lateral epicondylitis with platelet-rich plasma, glucocorticoid, or saline: a randomized, double-blind, placebo-controlled trial. Am J Sports Med. 2013;41(3):625–635. doi: 10.1177/0363546512472975. [DOI] [PubMed] [Google Scholar]
- 35.Lin Y-C, Wu W-T, Hsu Y-C, Han D-S, Chang K-V. Comparative effectiveness of botulinum toxin versus non-surgical treatments for treating lateral epicondylitis: a systematic review and meta-analysis. Clin Rehabil. 2018;32(2):131–145. doi: 10.1177/0269215517702517. [DOI] [PubMed] [Google Scholar]
- 36.Niemiec P, Szyluk K, Jarosz A, Iwanicki T, Balcerzyk A. Effectiveness of platelet-rich plasma for lateral epicondylitis: a systematic review and meta-analysis based on achievement of minimal clinically important difference. Orthop J Sports Med. 2022;10(4):1–10. doi: 10.1177/23259671221086920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rabago D, Best TM, Zgierska AE, Zeisig E, Ryan M, et al. A systematic review of four injection therapies for lateral epicondylosis: prolotherapy, polidocanol, whole blood and platelet-rich plasma. Br J Sports Med. 2009;43(7):471–481. doi: 10.1136/bjsm.2008.052761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Simental-Mendía M, Vilchez-Cavazos F, Álvarez-Villalobos N, Blazquiz-Saldana J, Pena-Martinez V, et al. Clinical efficacy of platelet-rich plasma in the treatment of lateral epicondylitis: a systematic review and meta-analysis of randomized placebo-controlled clinical trials. Clin Rheumatol. 2020;39(8):2255–2265. doi: 10.1007/s10067-020-05000-y. [DOI] [PubMed] [Google Scholar]
- 39.Tang S, Wang X, Wu P, et al. Platelet-rich plasma vs autologous blood vs corticosteroid injections in the treatment of lateral epicondylitis: a systematic review, pairwise and network meta-analysis of randomized controlled trials. PM R. 2020;12(4):397–409. doi: 10.1002/pmrj.12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Acosta-Olivo CA, Millán-Alanís JM, Simental-Mendía LE, Alvarez-Villalobos N, Vilchez-Cavazos F, et al. Effect of normal saline injections on lateral epicondylitis symptoms: a systematic review and meta-analysis of randomized clinical trials. Am J Sports Med. 2020;48(12):3094–3102. doi: 10.1177/0363546519899644. [DOI] [PubMed] [Google Scholar]
- 41.Bjordal JM, Lopes-Martins RAB, Joensen J, et al. A systematic review with procedural assessments and meta-analysis of low level laser therapy in lateral elbow tendinopathy (tennis elbow) BMC Musculoskelet Disord. 2008;9:1–15. doi: 10.1186/1471-2474-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buchbinder R, Green S, Youd J, Assendelft W, Barnsley L, et al. Systematic review of the efficacy and safety of shock wave therapy for lateral elbow pain. J Rheumatol. 2006;33(7):1351–1361. [PubMed] [Google Scholar]
- 43.Yoon SY, Kim YW, Shin I-S, Moon HI, Lee SC. Does the type of extracorporeal shock therapy influence treatment effectiveness in lateral epicondylitis? A systematic review and meta-analysis. Clin Orthop Relat Res. 2020;478(10):2324–2339. doi: 10.1097/CORR.0000000000001246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dingemanse R, Randsdorp M, Koes BW, Huisstede BMA. Evidence for the effectiveness of electrophysical modalities for treatment of medial and lateral epicondylitis: a systematic review. Br J Sports Med. 2014;48(12):957–965. doi: 10.1136/bjsports-2012-091513. [DOI] [PubMed] [Google Scholar]
- 45.Zheng C, Zeng D, Chen J, Liu S, Li J, et al. Effectiveness of extracorporeal shock wave therapy in patients with tennis elbow: a meta-analysis of randomized controlled trials. Medicine (Baltimore) 2020;99(30):e21189. doi: 10.1097/MD.0000000000021189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Karanasios S, Tsamasiotis GK, Michopoulos K, Sakellari V, Gioftsos G. Clinical effectiveness of shockwave therapy in lateral elbow tendinopathy: systematic review and meta-analysis. Clin Rehabil. 2021;35(10):1383–1398. doi: 10.1177/02692155211006860. [DOI] [PubMed] [Google Scholar]
- 47.Yan C, Xiong Y, Chen L, Endo Y, Hu L, et al. A comparative study of the efficacy of ultrasonics and extracorporeal shock wave in the treatment of tennis elbow: a meta-analysis of randomized controlled trials. J Orthop Surg Res. 2019;14(1):1–12. doi: 10.1186/s13018-019-1290-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yao G, Chen J, Duan Y, Chen X. Efficacy of extracorporeal shock wave therapy for lateral epicondylitis: a systematic review and meta-analysis. BioMed Res Int. 2020;2020 doi: 10.1155/2020/2064781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hoogvliet P, Randsdorp MS, Dingemanse R, Koes BW, Huisstede BMA. Does effectiveness of exercise therapy and mobilization techniques offer guidance for the treatment of lateral and medial epicondylitis? A systematic review. Br J Sports Med. 2013;47(17):1112–1119. doi: 10.1136/bjsports-2012-091990. [DOI] [PubMed] [Google Scholar]
- 50.Lucado AM, Dale RB, Vincent J, Day JM. Do joint mobilizations assist in the recovery of lateral elbow tendinopathy? A systematic review and meta-analysis. J Hand Ther. 2018;32(2):1–14. doi: 10.1016/j.jht.2018.01.010. [DOI] [PubMed] [Google Scholar]
- 51.Raman J, MacDermid J, Grewal R. Effectiveness of different methods of resistance exercises in lateral epicondylosis—a systematic review. J Hand Ther. 2012;25(1):5–25. doi: 10.1016/j.jht.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 52.Chen Z, Baker NA. Effectiveness of eccentric strengthening in the treatment of lateral elbow tendinopathy: a systematic review with meta-analysis. J Hand Ther. 2021;34(1):18–28. doi: 10.1016/j.jht.2020.02.002. [DOI] [PubMed] [Google Scholar]
- 53.Cullinane FL, Boocock MG, Trevelyan FC. Is eccentric exercise an effective treatment for lateral epicondylitis? A systematic review. Clin Rehabil. 2014;28(1):3–19. doi: 10.1177/0269215513491974. [DOI] [PubMed] [Google Scholar]
- 54.Lian J, Mohamadi A, Chan JJ, Hanna P, Hemmati D, et al. Comparative efficacy and safety of nonsurgical treatment options for enthesopathy of the extensor carpi radialis brevis: a systematic review and meta-analysis of randomized placebo-controlled trials. Am J Sports Med. 2019;47(12):3019–3029. doi: 10.1177/0363546518801914. [DOI] [PubMed] [Google Scholar]
- 55.Barr S, Cerisola FL, Blanchard V. Effectiveness of corticosteroid injections compared with physiotherapeutic interventions for lateral epicondylitis: a systematic review. Physiotherapy. 2009;95(4):251–265. doi: 10.1016/j.physio.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 56.Karanasios S, Korakakis V, Whiteley R, Vasilogeorgis I, Woodbridge S, et al. Exercise interventions in lateral elbow tendinopathy have better outcomes than passive interventions, but the effects are small: a systematic review and meta-analysis of 2123 subjects in 30 trials. Br J Sports Med. 2021;55(9):477–485. doi: 10.1136/bjsports-2020-102525. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.