Abstract
The pharynx plays a significant role in swallowing and speech, and this is reflected in both its complex anatomy and degree of physiological motility. Patients who present with pharynx-related symptoms such as sore throat, globus, dysphagia or dysphonia will usually undergo visual and nasal endoscopic examination in the first instance. Imaging is frequently required to supplement clinical assessment and this typically involves MRI and CT. However, fluoroscopy, ultrasound and radionuclide imaging are valuable in certain clinical situations. The aforementioned complexity of the pharynx and the myriad of pathologies which may arise within it often make radiological evaluation challenging. In this pictorial review, we aim to provide a brief overview of cross-sectional pharyngeal anatomy and present the radiological features of a variety of pharyngeal pathologies, both benign and malignant.
INTRODUCTION
The pharynx is a hollow muscular tube which extends from the skull base to the inferior border of the cricoid cartilage, and is an integral part of the upper aerodigestive tract. It serves as a conduit for air, food and fluid, connecting the nasal and oral cavities to the larynx and oesophagus. It is divided into three main regions: the nasopharynx, oropharynx and hypopharynx (Figure 1a).
Figure 1.
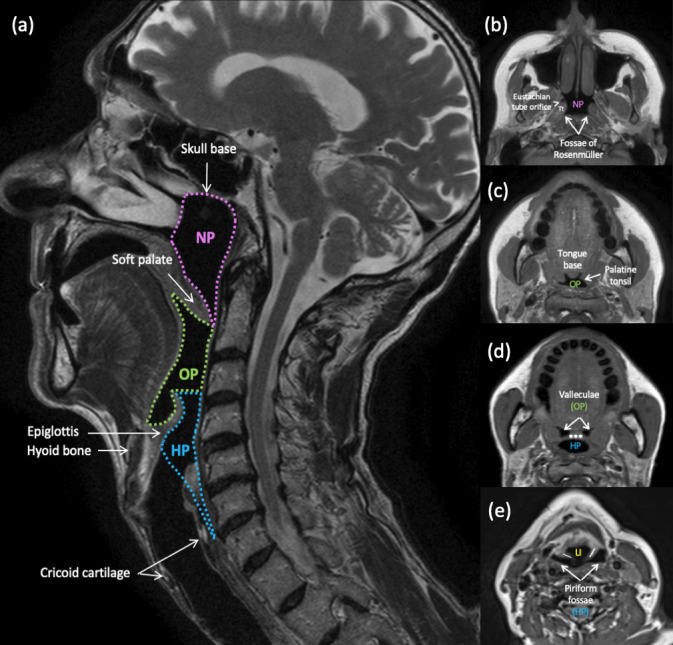
Pharyngeal anatomy. (a) Anatomical divisions of the pharynx and their boundaries. Sagittal T2-weighted MRI. Nasopharynx (NP): skull base to the free edge of the soft palate. Oropharynx (OP): free edge of the soft palate to the hyoid bone. Hypopharynx (HP): hyoid bone to the inferior border of the cricoid cartilage or cricopharyngeus muscle.(b-e) Important anatomical landmarks within each subdivison. Axial T1-weighted MR images through the pharynx. (b) Nasopharynx; Tt = torus tubarius; (c, d) Oropharynx; *** = epiglottis; (d,e) Hypopharynx; \ / = aryepiglottic folds; LI = laryngeal inlet. Note the complex anatomy at the oropharyngeal-hypopharyngeal-supraglottic junction, where from one cavity (OP), two separate cavities arise (HP and larynx).
The nasopharynx lies behind the nasal cavity and its lateral walls contain the pharyngeal orifices of the Eustachian tubes. The medial ends of the Eustachian tubes have cartilaginous extensions that form focal protrusions at the posterosuperior aspect of each orifice. These protrusions and their overlying nasopharyngeal mucosa are known as the tori tubarii. Immediately posterior to these lie the fossae of Rosenmüller (Figure 1b). The nasopharynx also contains several foci of mucosa-associated lymphoid tissue, namely, the paired tubal tonsils (located posterior to the Eustachian tube orifices) and the adenoid tonsil in its posterosuperior aspect. The oropharynx lies behind the oral cavity and caudal to the nasopharynx. It contains the paired lingual and palatine tonsils (Figure 1c and d), which, together with the tubal and adenoid tonsils, form Waldeyer’s ring of lymphoid tissue. The hypopharynx lies behind the larynx and caudal to the oropharynx, and is in continuity with the cervical oesophagus below (Figure 1d and e).
The pharynx can be assessed via direct visualisation and this is often facilitated by endoscopy. If clinical examination is inadequate or non-diagnostic, it can be further assessed using several imaging modalities. Both MRI and CT are widely used cross-sectional imaging modalities for the pharynx. They are extremely useful for detecting lesions which are deep to the pharyngeal mucosal surface or in clinical and endoscopic blind spots, such as the post-cricoid space and caudal hypopharynx. They also allow for accurate assessment of the size and extent of a lesion, which is of course key in tumour staging. Endoscopic ultrasound is occassionally used to detect submucosal lesions and guide biopsies. For investigation of dysphagia, dynamic fluoroscopic contrast swallow studies are particularly valuable in assessment of the pharyngeal phase of swallowing, and can aid in detecting mucosal lesions and other structural abnormalities.
Cysts
Benign cysts are common entities within the nasopharynx and oropharynx, often incidentally detected on imaging. They are usually asymptomatic unless large or infected. Typically, they appear as well-circumscribed, thin-walled, round or ovoid lesions on cross-sectional imaging. Their contents are usually of simple fluid density on CT. On MRI, they are usually T2-hyperintense, T1-hypointense and demonstrate facilitated diffusion (Figure 2). With increasing proteinaceous content, they may be of increased density on CT and increased T1 signal intensity on MRI. The main differential diagnoses to consider are cystic tumours, typically those of the minor salivary glands.
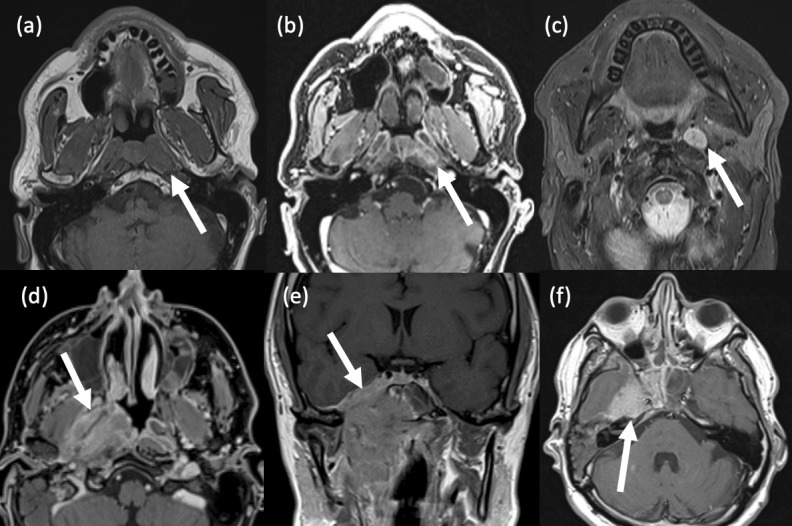
Figure 2.
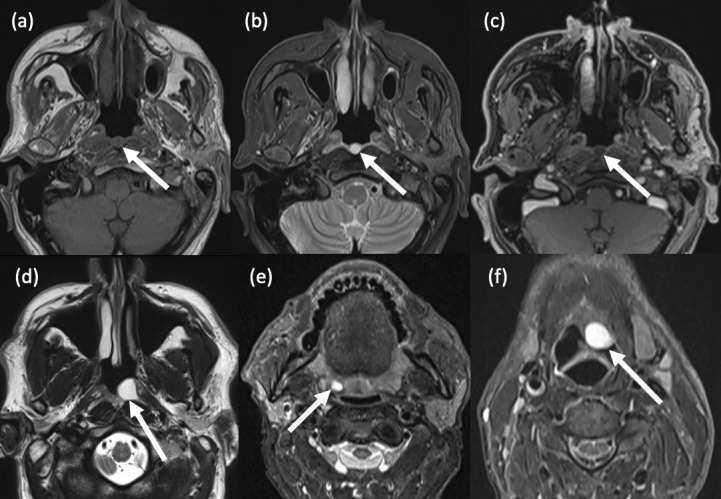
Pharyngeal cysts. (a-c) Tornwaldt cyst. (a) Axial T1-weighted TSE MRI shows a well-circumscribed, round, hypointense lesion in the posterior nasopharyngeal midline; (b) Axial T2-weighted TSE MRI shows homogeneous central hyperintensity; (c) Axial T1-weighted, fat suppressed, post-contrast MRI shows no enhancement within the lesion.(d) Nasopharyngeal mucous retention cyst. Axial T2-weighted TSE MRI shows a hyperintense cyst in the left fossa of Rosenmüller. (e) Tonsillar cyst. Axial STIR MRI shows an incidental small right palatine tonsillar retention cyst. (f) Vallecular cyst. A 60-year-old male presented with globus sensation and throat irritation for three weeks. Axial STIR MRI shows a large, well-defined cyst which expands the left vallecula and abuts the epiglottis.
A Tornwaldt cyst is a benign, midline developmental cyst which is situated in the posterosuperior nasopharynx and arises due to persistent communication between the pharynx and a notochordal remnant 1 (Figure 2a–c). Mucus retention cysts are more common and arise due to trapped mucus and secondary inflammation. They occur in the pharyngeal mucosal space, typically at the posterior nasopharyngeal wall and in the adenoidal and tonsillar crypts, less commonly in the valleculae 2 (Figure 2d–f). Though rare, another type of cyst which may arise from the lateral wall of the naso- or oropharynx is a branchial cleft cyst which can be differentiated pathologically by the presence of lymphoid tissue. 3
Benign lymphoid hyperplasia
Benign lymphoid hyperplasia refers to the rapid proliferation of lymphocytes within the lymphatic tissue of Waldeyer’s ring. When florid, it can result in a diagnostic conundrum due to overlapping clinical, radiological and histopathological features with malignancy, in particular, lymphoma. In the pharynx, the most commonly affected tissue is the adenoid tonsil. In normal circumstances, the adenoid enlarges during early childhood, reaching its maximum size by the age of 7 years, after which it usually involutes. 4 Its persistence or enlargement in adulthood is often secondary to recurrent viral or bacterial insults and/or exposure to irritants such as gastro-oesophageal reflux or smoking (Figure 3a–c). Similar aetiological factors can also contribute to benign lymphoid hyperplasia of the oropharyngeal tonsils (Figure 3d and e). Clinically, depending on the extent of involvement, benign pharyngeal lymphoid hyperplasia may cause symptoms of nasal obstruction, Eustachian tube dysfunction, globus, dysphagia and obstructive sleep apnoea.
Figure 3.
Benign lymphoid hyperplasia. (a,b) Nasopharyngeal lymphoid hyperplasia in a 41-year-old male smoker. (a) Axial T2-weighted MRI shows symmetrical mucosal thickening in the roof of the nasopharynx. (b) Axial T1-weighted, post-contrast MRI demonstrates a vertical stripe-like enhancing pattern (bright and dark). Tiny, non-enhancing cysts are also noted within the lymphoid tissue. (c) Focal adenoid tonsillar hyperplasia in an adolescent as demonstrated on axial T2-weighted MRI. (d,e) Oropharyngeal lymphoid hyperplasia. A 32-year old female presented with persistently enlarged, bilateral upper cervical lymph nodes. Axial T2-weighted STIR MR images show diffuse, symmetrical enlargement of both the (d) palatine and (e) lingual tonsils.
Radiologically, the condition typically manifests as symmetrical enlargement of any component of Waldeyer’s ring and is confined to the pharyngeal mucosal space (Figure 3). An alternating, vertical stripe-like pattern and an intact deep mucosal white line are classical findings on post-contrast T1-weighted MRI. Clinical correlation and biopsy are recommended in order to exclude malignancy if imaging findings are not typical. 5
Infections and abscesses
Acute pharyngitis is a very common, diffuse inflammatory disorder of the throat, which is usually viral in aetiology and typically results in sore throat, dysphagia and often reactive cervical adenopathy. It is usually self-limiting and no imaging is warranted. Tonsillitis is another common viral or bacterial condition that typically affects the palatine tonsils specifically. It usually occurs in children, teenagers and young adults, with the most common causative bacterial pathogen being group A beta-haemolytic streptococcus. 6 Again, acute tonsillitis is usually self-limiting. However, it can be complicated by peritonsillar abscess, otherwise known as quinsy, which forms when pus accumulates in the peritonsillar space (between the tonsillar capsule and the superior constrictor muscle). These are usually unilateral, associated with trismus and occur more frequently in younger patients, males and smokers (Figure 4). Drainage is the mainstay of treatment, along with antimicrobial treatment. Imaging is indicated in the event of airway compromise, large collection or clinical deterioration following conservative or surgical treatment. The full radiological extent of inflammation and any collection should be described, including any extension into deep neck spaces (the retropharyngeal and danger spaces in particular) 7,8 and any resultant airway obstruction.
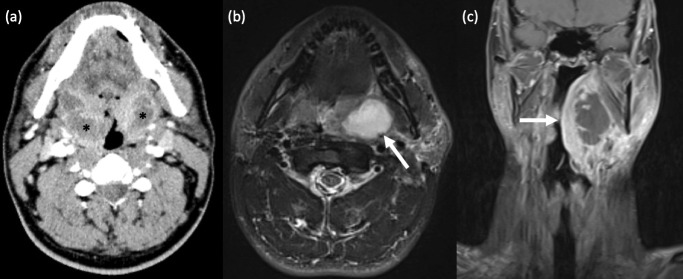
Figure 4.
Tonsillitis with peritonsillar abscess. (a) Bilateral peritonsillar abscesses. A 42-year old male had persistent parapharyngeal swelling following aspiration of only a right peritonsillar collection. Axial contrast-enhanced CT Neck revealed bilateral, peripherally enhancing, centrally hypodense peritonsillar collections, in keeping with abscesses, larger on the right. Unilateral peritonsillar abscess is more common. (b,c) Left peritonsillar abscess. (c) Axial T2-weighted STIR MRI shows a well-defined, left peritonsillar collection with homogenous, central hyperintensity. (d) Coronal T1-weighted, fat-suppressed, post-contrast MRI in the same patient demonstrates a left peritonsillar abscess with central non-enhancement and marked peripheral enhancement, and extension of diffuse inflammatory changes into the adjacent left parapharyngeal and submandibular spaces.
Thyroglossal tract pathology
Lingual thyroid
Ectopic thyroid tissue arises due to failure of the thyroid gland to migrate caudally from the foramen caecum at the tongue base to its usual position in the pre-tracheal neck (the path of the thyroglossal duct). It can form anywhere along this path, the most common site being the tongue base 9 (Figure 5). It is often asymptomatic and found incidentally, but may result in globus, dysphagia, dyspnoea, dysphonia and bleeding from ulceration. Ectopic thyroid tissue usually has the same imaging features as normal thyroid tissue, including high density on non-contrast CT and diffuse enhancement post-contrast. Similarly, it can also develop cysts, nodules, goitrous change and malignancy. In making the diagnosis of ectopic thyroid tissue, it is important to note the absence of the thyroid gland in its expected position in the lower neck. No treatment is required if the patient is asymptomatic and euthyroid.
Figure 5.
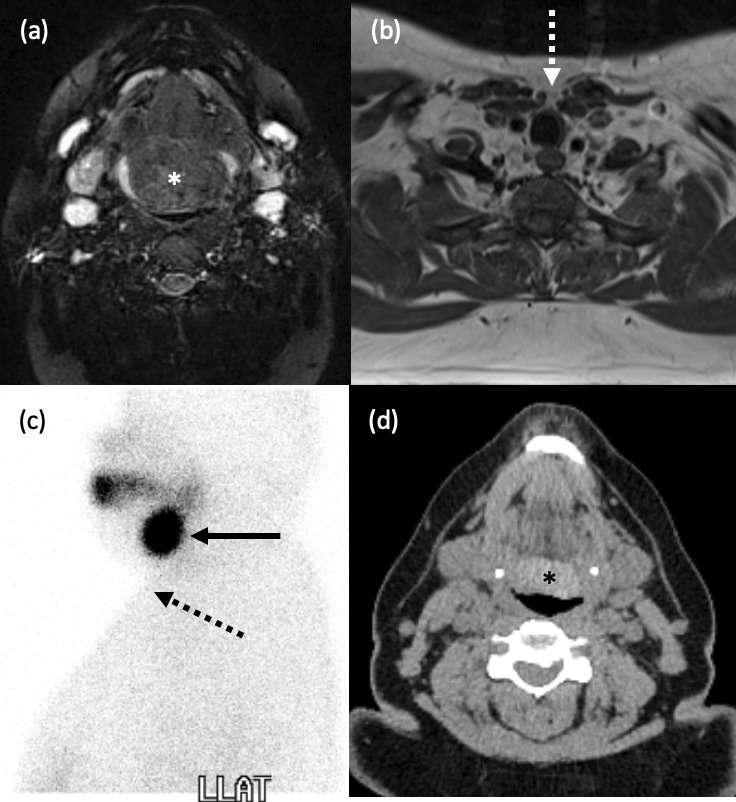
Lingual thyroid. (a-d) A 24-year old female presented with a large tongue base mass. (a) Axial T2-weighted, fat suppressed MRI demonstrates a lobulated, heterogeneous lesion at the base of the tongue (*). (b) Axial T1-weighted MRI confirmed the absence of any normal thyroid tissue in the pretracheal neck (white dashed arrow). (c) Left lateral view from a Tc-99m pertechnetate thyroid scintigraphy study shows intense uptake at the tongue base (black solid arrow), and none in the usual position (black dashed arrow). (d) Axial, unenhanced CT Neck over 10 years later in the same patient shows a hyperdense mass typical of thyroid tissue at the tongue base (*).
Thyroglossal duct cyst
Thyroglossal duct cysts form due to failure of closure of the midline embryological thyroglossal duct, which usually involutes by the 10th week of gestation. If any portion of the duct persists, secretion from the epithelial lining can result in inflammation and cyst formation. They are the most common congenital anomaly in the neck, with a population prevalence of 7% 10 , but can occur at the foramen caecum in the tongue base (Figure 6). As with ectopic thyroid tissue, they may also be complicated by malignancy, typically papillary thyroid carcinoma.
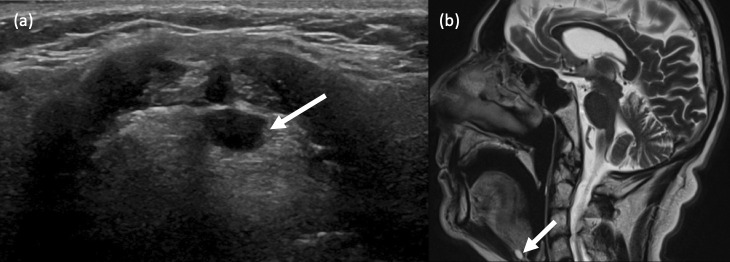
Figure 6.
Thyroglossal duct cysts. (a) A 32-year old female presented with a blood-speckled, white lump at the back of her tongue. B-mode ultrasound imaging revealed a well-defined, ovoid, anechoic lesion at the base of the tongue, in close proximity to the foramen caecum. Some posterior acoustic enhancement is also seen. (b) Sagittal T2-weighted MRI in a different patient who underwent an MRI Brain for investigation of headaches revealed an incidental, small, midline hyperintense cystic lesion at the tongue base, consistent with a thyroglossal duct cyst.
Pharyngeal diverticulum
A pharyngeal diverticulum is a sac-like outpouching of the hypopharynx, which usually occurs due to cricopharyngeal dysfunction. They may be posterior, posterolateral or lateral, with most protruding to the left. 11 A Zenker’s diverticulum is a particular subtype in which the hypopharyngeal wall herniates posteriorly through Killian’s dehiscence, a region of low resistance between the inferior pharyngeal constrictor muscle superiorly and the cricopharyngeus muscle inferiorly. In general, these diverticulae most commonly occur in elderly patients and typical symptoms include dysphagia, regurgitation, cervical borborygmi (gurgling noise on material passing through the pharynx), chronic cough and weight loss. Diagnosis is easily made via barium swallow studies (Figure 7). There is a small risk of developing a carcinoma within a pouch that is not surgically excised, and long-term follow-up is often undertaken in such cases.
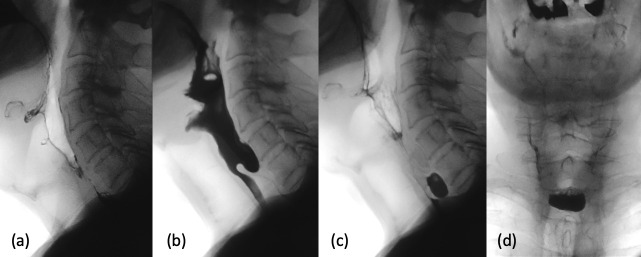
Figure 7.
Hypopharyngeal pouch. (a-d) An 88-year old male with a known hiatus hernia and family history of pharyngeal pouch presented with high dysphagia. (a-c) Serial lateral and (d) single AP views from his barium swallow study demonstrate a midline, posterior hypopharyngeal outpouching immediately above the well-delineated cricopharyngeus muscle, in keeping with a Zenker’s diverticulum.
Foreign bodies
Impaction of ingested foreign bodies is a common presentation to the emergency department. In children, coins and buttons are the most common culprits, whereas in adults, it is usually fish or meat bones which become lodged. Frequent sites of impaction are the oropharyngeal tonsils, tongue base, valleculae and piriform fossae. The majority can be detected on direct clinical inspection 12,13 . Lateral neck soft tissue radiographs are often used as diagnostic adjuncts and may show the radiopaque foreign body itself and/or secondary ‘softer’ signs, such as prevertebral soft tissue swelling and loss of the normal cervical lordosis 12 (Figure 8a). If both direct clinical inspection and plain radiography are inconclusive, and the clinical suspicion of impacted foreign body or associated complication remains high, contrast-enhanced CT scan of the neck is indicated (Figure 8b). While searching for foreign bodies in the pharynx on imaging, it is important to be mindful of normal calcifications within the pharynx, e.g. tonsilloliths. (Figure 8c).
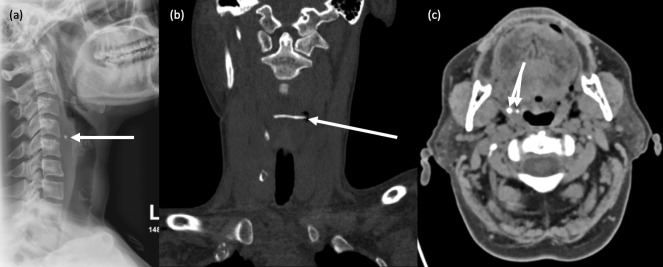
Figure 8.
Foreign bodies. (a,b) Impacted fishbone. A 36-year-old female presented with severe dysphagia and inability to move her neck following ingestion of fish. (a) Lateral neck soft tissue radiograph revealed a small radiopaque object anterior to the C4 vertebral body, with associated prevertebral soft tissue swelling. (b) Unenhanced coronal CT Neck confirmed the presence of a 28mm horizontally orientated fish bone lodged in the hypopharynx. (c) Benign calcifications. Axial CT Neck image in a different patient shows two right-sided tonsilloliths. It is important not to confuse these with foreign bodies.
Tumours
Benign pharyngeal tumours are generally uncommon but include minor salivary gland tumours (such as pleomorphic adenomas), nerve sheath tumours and lipomas (Figure 9). Juvenile nasopharyngeal angiofibroma (JNA) is a benign but locally aggressive and highly vascular tumour, which arises from either the nasopharynx, the posterior nasal cavity or the sphenopalatine foramen. It almost exclusively occurs in young males. Diagnostic imaging is imperative due to the risks associated with biopsy. It usually appears as a unilateral, heterogeneous, lobulated soft tissue mass on CT, with flow-voids on T2-weighted MRI and prominent enhancement post-contrast. Treatment is usually via endovascular embolisation and/or surgical resection. 14
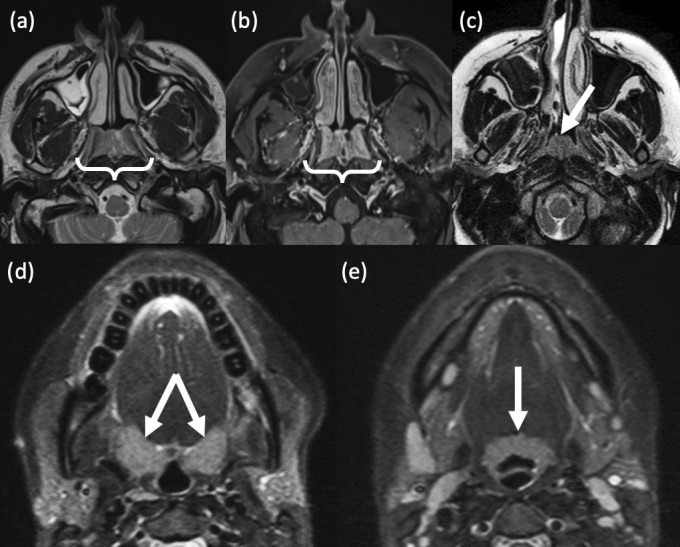
Figure 9.
Benign pharyngeal tumours. (a,b) Minor salivary gland pleomorphic adenoma. A 36-year old female presented with a lump in her soft palate. (a) Coronal T1-weighted, pre-contrast MRI shows a well-circumscribed, heterogeneous lesion within the right soft palate which is predominantly hypointense. Smaller lesions are often homogeneously hypointense. (b) Sagittal T2-weighted MRI shows a hypointense rim surrounding the lesion, which represents the fibrous capsule that is characteristic of pleomorphic adenomas. Histology confirmed pleomorphic adenoma with extensive epidermoid differentiation. (c) Minor salivary gland pleomorphic adenoma. A 61-year old male also presented with a soft palate swelling. Axial T1-weighted, fat-suppressed, post-contrast MRI reveals a well-defined, heterogeneously enhancing lesion in the soft palate. Another common feature of these tumours, which is also seen here, is its lobulated contour. (d-f) Schwannoma. A 17-year old male presented with a 1cm lesion in his right soft palate. (d) Axial T1-weighted, pre-contrast MRI shows a well-defined, ovoid lesion in the right soft palate which is isointense to muscle. Note also the thin, peripheral rind of fat (the so-called ‘split fat’ sign). (e) Axial T2-weighted, fat-suppressed MRI shows intralesional hyperintensity. (f) Axial T1-weighted, fat-suppressed, post-contrast MRI shows intense contrast enhancement, a typical imaging feature of schwannoma. Though not demonstrated in this case, the ‘fascicular’ sign may also be seen, i.e. multiple ring-like structures within the lesion which reflect fascicular bundles.
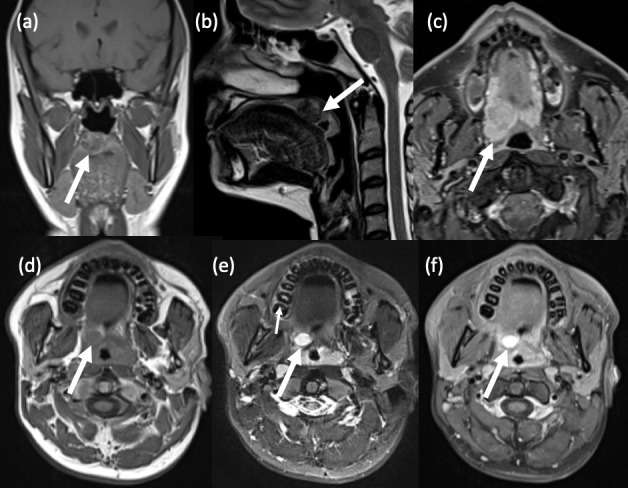
Malignant pharyngeal tumours are far more common, with squamous cell carcinoma (SCC) being the most prevalent. 15 The most significant risk factors for all keratinising SCCs of the pharynx are excessive smoking and alcohol consumption. In the nasopharynx, the histologically distinct, non-keratinising SCC is endemic in South China, typically occurs in males aged between 40 and 60 and is strongly associated with Epstein-Barr virus (EBV) infection. The most common site of nasopharyngeal SCC is the fossa of Rosenmüller and ipsilateral middle ear effusion secondary to Eustachian tube obstruction is common (Figure 10). Oropharyngeal SCCs (Figure 11) are unique in that there are two distinct prognostic types. 16 Human papilloma virus (HPV)-associated oropharyngeal SCC is more prevalent in younger age groups and is associated with frequent oral sex with multiple partners. Though it is often associated with more rapid growth and more pronounced locoregional and cystic nodal metastasis, it is deemed to be more treatable than its non-HPV–associated counterpart. Hypopharyngeal SCC is relatively less common (Figure 12) but carries the worst prognosis of all the pharyngeal SCCs due to its often late presentation. It occurs more frequently in the piriform fossae, where the prognosis tends to be better than for those which arise at the other hypopharyngeal subsites (the posterior pharyngeal wall and the post-cricoid space).
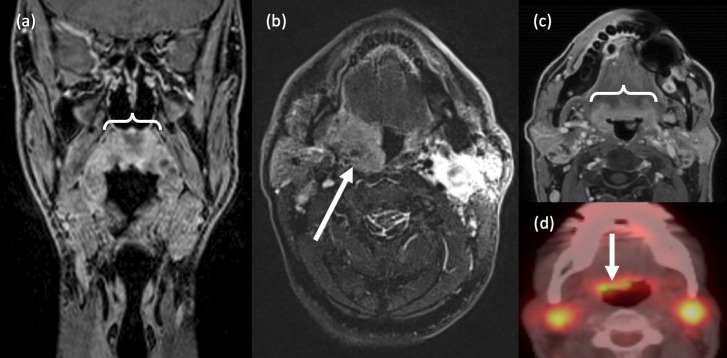
Figure 10.
Nasopharyngeal carcinoma. (a-c) Small NPC in the left fossa of Rosenmüller. A 66-year old male presented with a suspicious left nasopharyngeal lesion on nasendoscopy. (a) Axial T1-weighted STIR MRI shows asymmetrical enlargement of the left nasopharynx. (b) Axial T1-weighted post-contrast MRI shows heterogeneous enhancement. (c) Axial T2-weighted, fat-suppressed MRI shows an enlarged ipsilateral retropharyngeal node – a common region of nodal metastasis in NPC. (d-f) Invasive NPC. A 48-year old male presented with a large, highly suspicious right nasopharyngeal mass on nasendoscopy. (d) Axial fat-suppressed T1-weighted, post-contrast MRI shows an irregular, heterogeneously enhancing, right nasopharyngeal mass and middle ear effusion. (e) Coronal T1-weighted, post-contrast MRI shows the craniocaudal extent of the mass, with skull base invasion and intracranial extension. (f) Axial T1-weighted, post-contrast MRI Brain shows cranial invasion into the right middle cranial fossa.
Figure 11.
Oropharyngeal SCC. (a) Soft palate SCC. Coronal T1-weighted, post-contrast MRI shows a large, ill-defined, enhancing soft palate mass which extends laterally to the tonsillar pillars, more notably on the right. (b) Tonsillar SCC. Axial T2-weighted, fat-suppressed MRI shows a large right palatine tonsil mass. Histology confirmed a poorly undifferentiated SCC. (c,d) Base of tongue SCC. A 64-year old male who presented with cervical lymphadenopathy underwent a lymph node biopsy which confirmed metastatic SCC. (c) Axial T1-weighted, post-contrast MRI shows mild asymmetrical thickening at the lingual tonsils and right base of tongue. (d) Axial FDG-PET CT confirms abnormal uptake at the base of tongue on the right, as well as in bilateral cervical lymph nodes.
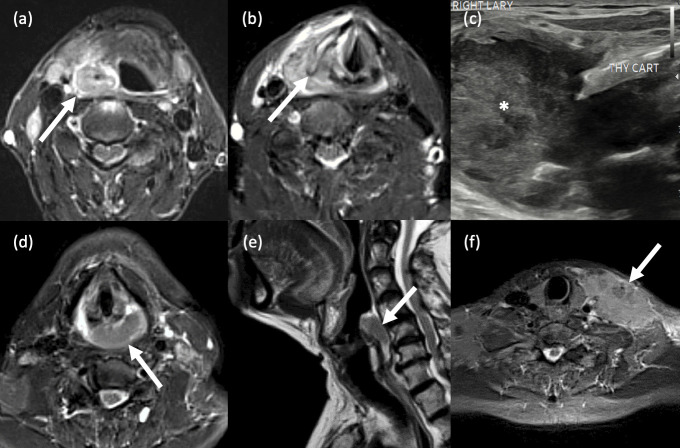
Figure 12.
Hypopharyngeal SCC. (a-c) Pyriform sinus SCC. Axial STIR MR images show (a) a large right hypopharyngeal mass lesion which is centred around the right piriform fossa, extends anterolaterally into the surrounding superficial soft tissues and; (b) anteromedially and caudally into the ipsilateral aryepiglottic fold and supraglottic larynx. The right thyroid cartilage is partially destroyed. (c) B-mode ultrasound imaging in the same patient shows a large, right-sided heterogeneous mass (*) abutting and protruding outwards beyond the destroyed right thyroid cartilage (labelled). (d-f) Posterior pharyngeal wall SCC. A 52-year old female presented with a 3-month history of dysphagia and weight loss. (d) Axial STIR MRI shows a large lesion in the mid and left posterior wall of the hypopharynx. (b) Sagittal T2-weighted MRI better demonstrates that the posterior wall is the subsite around which the mass is centred, in addition to its craniocaudal extent. (f) Axial STIR MRI in the same patient shows a large, irregular left lower cervical nodal mass (extranodal spread).
Extranodal lymphoma (Figure 13) is the most common non-epithelial malignancy of the head and neck, 17 accounting for approximately 10% of all malignant pharyngeal tumours. They are almost always of the non-Hodgkin’s type and typically occur within Waldeyer’s ring. Radiological features that favour pharyngeal lymphoma over carcinoma include lesion symmetry, relative homogeneity and diffuse mucosal spread which extends into adjacent fat planes but not into deeper structures. 18 They also demonstrate low apparent diffusion coefficient (ADC) values on diffusion-weighted MRI sequences due to their higher cellularity. In addition, involved neck nodes tend not to be necrotic, unlike in SCC.
Figure 13.
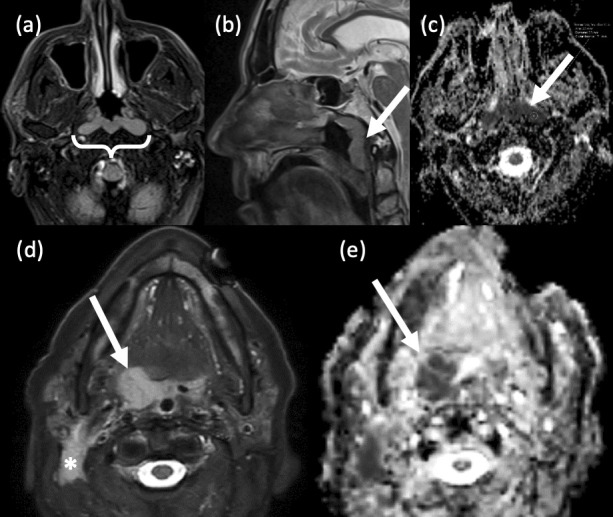
Pharyngeal lymphomas. (a-c) Nasopharyngeal lymphoma. A 69-year old male presented with a post-nasal space mass and bilateral cervical lymphadenopathy. (a) Axial T2-weighted, fat suppressed MRI reveals a bulky, symmetrical, slightly hyperintense mass in the roof of the nasopharynx. Extensive bilateral cervical lymphadenopathy was confirmed (not shown). (b) Sagittal T2-weighted, fat-suppressed MRI shows the craniocaudal extent of the mass, i.e. the entire length of the posterior nasopharynx. There is no evidence of skull base invasion. (c) Axial EPI DWI and relative ADC map show marked restricted diffusion and low ADC values. Histopathology confirmed diffuse large B cell lymphoma (DLBCL). (d,e) Oropharyngeal lymphoma. (d) Axial T2-weighted, fat-suppressed MRI reveals a relatively homogeneous right tonsillar lesion and an abnormal right level 2 lymph node (*). (e) Axial EPI DWI ADC imaging in the same patient shows well the restricted diffusion within the lesion.
Extrinsic compression of the pharynx
As is the case with other tubular structures in the body, symptoms which are commonly attributed to intraluminal pharyngeal pathology, such as nasal obstruction, globus and dysphagia may in fact be secondary to externally compressing anatomical structures or pathological processes (Figures 14 and 15). In such cases, clinical examination is usually limited and imaging and/or image-guided biopsy can be key in providing the diagnosis.
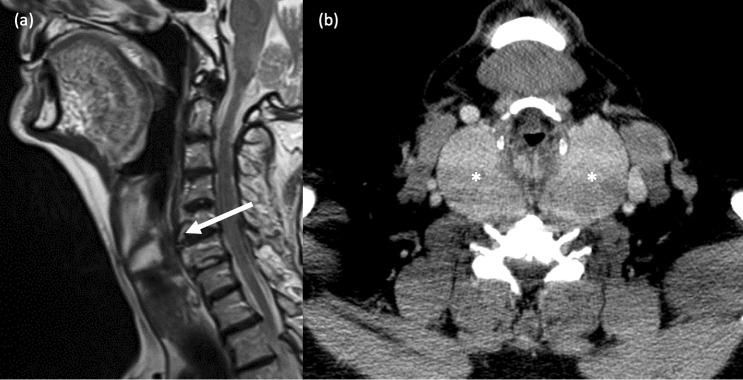
Figure 14.
Extrinsic compression of the naso- and oropharynx. (a) Prevertebral tuberculous collection. A 77-year old male presented with a 3-month history of odynophagia, neck pain and weight loss and a posterior nasopharyngeal ‘mass’ was seen on clinical examination. Sagittal T2-weighted MRI shows a well-circumscribed fluid collection posterior to the pharynx at the level of C1/C2, with subligamentous extension and breaching of the epidural space. (b) Left parotid deep lobe tumour. A 45-year old female presented with smooth left tonsillar enlargement and left level 2 cervical lymphadenopathy. Axial T2-weighted MRI shows a large, well-circumscribed mass in the deep lobe of the left parotid gland, which causes displacement of the oropharynx to the right. (c) Medialisation of the internal carotid artery. A 62-year old male presented with right sided oropharyngeal swelling. Axial T1-weighted, fat-suppressed, post-contrast MRI shows incidental medial deviation of a tortuous right common carotid artery and resultant indentation of the right posterolateral oropharyngeal wall.
Figure 15.
Extrinsic compression of the hypopharynx. (a) Cervical vertebral osteophytosis. An elderly patient presented with mild dysphagia. Sagittal T2-weighted MRI of the neck shows severe anterior osteophytosis of the C4-6 vertebral bodies resulting in indentation of the posterior hypopharyngeal wall. (b) Multinodular goitre. A 60-year old male with dysphagia and clinically obvious multinodular goitre required cross-sectional imaging prior to surgical intervention. Axial, contrast-enhanced CT Neck image shows a large, bilateral multinodular thyroid goitre (* *) causing marked compression of the hypopharynx.
CONCLUSION
A variety of benign and malignant lesions can arise within the pharynx. Many of these can be detected on clinical and endoscopic examination. However, cross-sectional imaging frequently provides useful additional information, and is often key in identifying clinically relevant lesions that have not been visualised. Incidental benign findings are also commonplace in pharyngeal imaging and it is important to have an awareness of these in order to avoid unnecessary further investigation. The radiologist should also be sure to look for extrinsic causes of pharynx-related clinical symptoms, such as normal anatomical variation or mass lesions in adjacent structures.
Contributor Information
Ishrat Rahim, Email: ishrat.rahim@nhs.net.
Angela Napolitano, Email: angela.napolitano90@gmail.com.
Chris Burd, Email: chris.burd@nhs.net.
Ravi Kumar Lingam, Email: ravi.lingam@nhs.net.
REFERENCES
- 1. Alshuhayb Z, Alkhamis H, Aldossary M, Almoumen Z, Aldhurais A, Alshuhayb B, et al. Tornwaldt Nasopharyngeal Cyst: case series and literature review. Int J Surg Case Rep 2020; 76: 166–69. doi: 10.1016/j.ijscr.2020.09.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ben Salem D, Duvillard C, Assous D, Ballester M, Krausé D, Ricolfi F. Imaging of Nasopharyngeal cysts and Bursae. Eur Radiol 2006; 16: 2249–58. doi: 10.1007/s00330-006-0238-x [DOI] [PubMed] [Google Scholar]
- 3. Flis DW, Wein RO. Nasopharyngeal Branchial cysts—diagnosis and management: A case series. J Neurol Surg B Skull Base 2013; 74: 50–53. doi: 10.1055/s-0032-1331020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bhatia KSS, King AD, Vlantis AC, Ahuja AT, Tse GM. Nasopharyngeal mucosa and Adenoids: appearance at MR imaging. Radiology 2012; 263: 437–43. doi: 10.1148/radiol.12111349 [DOI] [PubMed] [Google Scholar]
- 5. King AD, Wong LYS, Law BKH, Bhatia KS, Woo JKS, Ai Q-Y, et al. MR imaging criteria for the detection of Nasopharyngeal carcinoma: discrimination of early-stage primary tumors from benign hyperplasia. AJNR Am J Neuroradiol 2018; 39: 515–23. doi: 10.3174/ajnr.A5493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Georgalas CC, Tolley NS, Narula PA. Tonsillitis. BMJ Clin Evid 2014; 2014: 0503. [PMC free article] [PubMed] [Google Scholar]
- 7. Jameson MJ, Wintermark M, Raghavan P, May S. Radiologykey.com - Spaces of the Neck. 2016. Available from: https://radiologykey.com/spaces-of-the-neck
- 8. Kamalian S, Avery L, Lev MH, Schaefer PW, Curtin HD, Kamalian S. Nontraumatic head and neck emergencies. Radiographics 2019; 39: 1808–23. doi: 10.1148/rg.2019190159 [DOI] [PubMed] [Google Scholar]
- 9. Zander DA, Smoker WRK. Imaging of ectopic thyroid tissue and Thyroglossal duct cysts. Radiographics 2014; 34: 37–50. doi: 10.1148/rg.341135055 [DOI] [PubMed] [Google Scholar]
- 10. Garcia E, Osterbauer B, Parham D, Koempel J. The incidence of microscopic Thyroglossal duct tissue superior to the Hyoid bone. Laryngoscope 2019; 129: 1215–17. doi: 10.1002/lary.27291 [DOI] [PubMed] [Google Scholar]
- 11. Siddiq MA, Sood S, Strachan D. Pharyngeal pouch (Zenker’s Diverticulum). Postgrad Med J 2001; 77: 506–11. doi: 10.1136/pmj.77.910.506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Castán Senar A, Dinu LE, Artigas JM, Larrosa R, Navarro Y, Angulo E. Foreign bodies on lateral neck Radiographs in adults: imaging findings and common pitfalls. Radiographics 2017; 37: 323–45. doi: 10.1148/rg.2017160073 [DOI] [PubMed] [Google Scholar]
- 13. Virk JS, Pang J, Okhovat S, Lingam RK, Singh A. Analysing lateral soft tissue neck Radiographs. Emerg Radiol 2012; 19: 255–60. doi: 10.1007/s10140-012-1026-3 [DOI] [PubMed] [Google Scholar]
- 14. López F, Triantafyllou A, Snyderman CH, Hunt JL, Suárez C, Lund VJ, et al. Nasal juvenile Angiofibroma: Current perspectives with emphasis on management. Head Neck 2017; 39: 1033–45. doi: 10.1002/hed.24696 [DOI] [PubMed] [Google Scholar]
- 15. Stelow EB, Wenig BM. Update from the 4TH edition of the world health organization classification of head and neck tumours: Nasopharynx. Head and Neck Pathol 2017; 11: 16–22. doi: 10.1007/s12105-017-0787-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lechner M, Liu J, Masterson L, Fenton TR. HPV-associated oropharyngeal cancer: epidemiology, molecular biology and clinical management. Nat Rev Clin Oncol 2022; 19: 306–27. doi: 10.1038/s41571-022-00603-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hsueh C-Y, Yang C-F, Gau J-P, Kuan EC, Ho C-Y, Chiou T-J, et al. Nasopharyngeal lymphoma: A 22-year review of 35 cases. J Clin Med 2019; 8(): 1604. doi: 10.3390/jcm8101604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Liu X, Xie C, Mo Y, Zhang R, Li H, Huang Z-L, et al. Magnetic resonance imaging features of Nasopharyngeal carcinoma and Nasopharyngeal non-Hodgkin’s lymphoma: are there differences. Eur J Radiol 2012; 81: 1146–54. doi: 10.1016/j.ejrad.2011.03.066 [DOI] [PubMed] [Google Scholar]