Summary
Controlling avoidable causes of cancer may save cancer-related healthcare costs and indirect costs of premature deaths and productivity loss. This study aimed to estimate the economic burden of cancer attributable to major lifestyle and environmental risk factors in Japan in 2015. We evaluated the economic cost of cancer attributable to modifiable risk factors from a societal perspective. We obtained the direct medical costs for 2015 from the National Database of Health Insurance Claims and Specific Health Checkups of Japan, and estimated the indirect costs of premature mortality and of morbidity due to cancer using the relevant national surveys in Japan. Finally, we estimated the economic cost of cancer associated with lifestyle and environmental risk factors. The estimated cost of cancer attributable to lifestyle and environmental factors was 1,024,006 million Japanese yen (¥) (8,460 million US dollars [$]) for both sexes, and ¥673,780 million ($5,566 million) in men and ¥350,226 million ($2,893 million) in women, using the average exchange rate in 2015 ($1 = ¥121.044). A total of ¥285,150 million ($2,356 million) was lost due to premature death in Japan in 2015. Indirect morbidity costs that could have been prevented were estimated to be ¥200,602 million ($1,657 million). Productivity loss was highest for stomach cancer in men (¥28,735 million/$237 million) and cervical cancer in women (¥24,448 million/$202 million). Preventing and controlling cancers caused by infections including Helicobacter pylori, human papillomavirus and tobacco smoking will not only be life-saving but may also be cost-saving in the long run.
Keywords: cost of illness, economic burden, cancer, population attributable fraction
Introduction
Cancer is a major public health issue, and has also been the leading cause of death in Japan since 1981 (1). Around 378,000 people died from cancer in 2020, and 999,000 cancer cases were newly diagnosed in 2019 (2). Recent statistics suggest that one in two Japanese people will be diagnosed with cancer during their lifetime (2). There is also wide agreement that many cancers are caused by lifestyle and environmental risk factors, which can be prevented if appropriate measures are taken (3).
The proportion of cancers that are associated with certain risk factors, such as lifestyle and environmental factors, is often referred to as the population attributable fraction (PAF). PAF is defined as the fraction of cancer attributable to a particular exposure that could be averted if the exposure were reduced to a theoretically minimal level. To date, several comprehensive assessments of the PAF of cancer have been reported in western countries (4-6) and in Asia (7). Further, updated findings on the disease burden of cancer associated with preventable risk factors in Japan were reported in 2022 (8), providing the PAF of major lifestyle and environmental risk factors.
Despite mounting evidence on disease burden, however, only a few studies have evaluated the economic burden cancer poses on society (9-12). According to the Estimates of National Medical Care Expenditure in fiscal year 2015, the direct medical and non-medical costs of all diseases amounted to 30,046 billion Japanese yen (248 billion US dollars as of 2015), of which cancer-related costs constituted 12% (13). Beyond direct costs, cancer incurs a heavy economic burden due to premature deaths, temporary work cessation during treatment, and permanent exit from the workforce. Preventing causes of cancer may save cancer-related healthcare costs and indirect costs of premature death and productivity loss. Hence, quantification of the avoidable costs of cancer is important in identifying the financial impact of cancer control policies.
Here, we aimed to estimate the economic burden of cancer attributable to major lifestyle and environmental risk factors using the latest data on population attributable fractions in Japan.
Materials and Methods
We evaluated the economic cost of cancer attributable to modifiable risk factors based on the prevalence-based cost-of-illness approach (14). We adopted a societal perspective for our analysis, which included direct healthcare costs, indirect morbidity costs and indirect mortality costs due to lifestyle and environmental risk factors.
Data sources
We obtained the number of cancer patients who received any type of healthcare service and the associated direct medical costs for 2015 from the aggregated datasets of the National Database of Health Insurance Claims and Specific Health Checkups of Japan (the NDB Japan) by the Ministry of Health, Labour and Welfare, which covers 99.9% of hospital or medical clinic claims nationwide. Details of the NDB Japan data can be found elsewhere (15,16). We classified sex- and age-specific number of patients and associated costs in 2015 by 20 cancer sites reported as the principal diagnosis according to the WHO International Classification of Diseases, 10th Revision (ICD-10) diagnosis codes. The list of ICD- 10 codes used in the current study is shown in Table 1. Because the NDB data and other public statistics were obtained in an aggregated format, ethical approval for this study was not necessary.
Table 1. Number of cancer patients by cancer site in Japan, 2015.
| Cancer site | ICD-10 | Number of patients |
|---|---|---|
| Both sexes, all cancers | C00-C97 | 4,045,940 |
| Men | ||
| All cancers | C00-C97 | 2,107,331 |
| Prostate | C61 | 551,195 |
| Stomach | C16 | 316,112 |
| Colon | C18 | 230,125 |
| Lung, trachea | C33-C34 | 211,306 |
| Bladder | C67 | 146,038 |
| Rectum | C19-C20 | 122,297 |
| Liver | C22 | 75,478 |
| Kidney and other urinary organs | C64-C66 C68 | 73,708 |
| Malignant lymphoma | C81-C85 C96 | 69,500 |
| Esophagus | C15 | 67,276 |
| Oral cavity and pharynx | C00-C14 | 47,589 |
| Pancreas | C25 | 37,090 |
| Leukemia | C91-C95 | 34,314 |
| Gallbladder and bile ducts | C23-C24 | 27,351 |
| Larynx | C32 | 26,669 |
| Women | ||
| All cancers | C00-C97 | 1,938,609 |
| Breast | C50 | 659,970 |
| Colon | C18 | 197,745 |
| Stomach | C16 | 154,807 |
| Lung, trachea | C33-C34 | 134,500 |
| Corpus uteri | C54 | 79,055 |
| Rectum | C19-C20 | 74,965 |
| Cervix uteri | C53 | 73,972 |
| Malignant lymphoma | C81-C85 C96 | 67,830 |
| Ovary | C56 | 60,852 |
| Bladder | C67 | 41,767 |
| Liver | C22 | 36,636 |
| Kidney and other urinary organs | C64-C66 C68 | 35,338 |
| Pancreas | C25 | 33,146 |
| Leukemia | C91-C95 | 28,457 |
| Gallbladder and bile ducts | C23-C24 | 22,383 |
| Oral cavity and pharynx | C00-C14 | 19,267 |
| Esophagus | C15 | 14,707 |
| Larynx | C32 | 2,163 |
The most up-to-date data on population attributable fraction (PAF) of cancer due to lifestyle and environmental risk factors in Japan is for 2015 (8), namely tobacco smoking (both active and passive) (17), alcohol drinking (18), excess bodyweight (19), physical inactivity (19), infectious agents (Helicobacter pylori [H. pylori], hepatitis C virus, hepatitis B virus, human papillomavirus [HPV], Epstein-Barr virus, and human T-cell leukemia virus type 1) (20), dietary intake (highly salted food (21), fruit, vegetables, dietary fiber (22), red and processed meat (23)), exogenous hormone use (24), never breastfeeding (25) and air pollution (26). All of the aforementioned factors are considered potentially modifiable via environmental policy, lifestyle change, population-based screening or through vaccination programs.
Direct medical costs
Direct medical costs denote the cost of resources consumed for treatment of the disease, and includes all costs of healthcare and medical examinations during hospitalization and outpatient visits, prescriptions and drugs. The cost of each cancer site attributable to modifiable risk factors was calculated using the following equation (27).
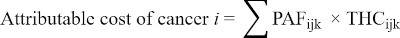
where:
Attributable cost of cancer i = direct medical costs of cancer site i attributable to lifestyle and environmental risk factors, including inpatient hospitalizations, outpatient visits, prescriptions and drugs
PAFijk = PAF of cancer incidence i due to lifestyle and environmental risk factors among people in 5-year age group j by gender k
THCijk = total direct medical costs for treating cancer i among people in age group j by gender k
Table 1 lists site-specific data on the number of patients extrapolated from the NDB Japan. A total of 2.1 million men and 1.9 million women received cancer treatment in 2015.
Indirect mortality costs
We also estimated the economic cost of potential work-life lost due to premature deaths from cancer, which are attributable to modifiable risk factors. Indirect mortality costs attributable to lifestyle and environmental risk factors were calculated by the net present value of future productivity using the following equation (27) :

where:
Indirect mortality cost of cancer i = indirect mortality costs from productivity losses due to premature deaths from cancer site i that are attributable to lifestyle and environmental risk factors
PAFijk = PAF of cancer mortality i due to lifestyle and environmental risk factors among people in 5-year age group j by gender k
NDEATHijk = number of deaths from cancer site i among people in age group j by gender k
PVLEjk = present value of potential lifetime earnings in age group j by gender k discounted at an annual rate of 3%
EMPjk = average employment rate among people in age group j by gender k
The number of cancer deaths during 2015 by cancer site, 5-year age group, and gender were obtained from the Cancer Statistics available on the Cancer Information Service website (2). This was then used to derive the remaining years of working life by subtracting the age at death from the retirement age of 65 years. Subsequently, we multiplied the remaining years of working life by the average annual income for the 5-year age group reported in the Basic Survey on Wage Structure 2015 (28) and adjusted the future earnings lost to the present values with a discount rate of 3% according to the WHO guide to cost-effectiveness (29).
Indirect morbidity costs
We estimated the indirect costs of cancer following the human capital approach (30). The indirect costs of cancer in this study denote the economic value of productivity loss associated with absenteeism due to hospitalization and receipt of healthcare treatment. The costs of indirect morbidity costs attributable to modifiable risk factors were calculated using the following equation (27).

where:
Indirect morbidity cost of cancer i = indirect morbidity costs from productivity losses due to cancer site i that are attributable to lifestyle and environmental risk factors
PAFijk = PAF of cancer incidence i due to lifestyle and environmental risk factors among people in 5-year age group j by gender k
TWLDijk = total annual work-loss days due to hospitalization and outpatient visits for cancer site i among people in age group j by gender k
ADWj = average daily wage among people in age group j
EMPjk = average employment rate among people in age group j by gender k
We estimated the indirect morbidity cost of cancer attributable to modifiable risk factors by multiplying the total number of work-loss days among patients aged 20 to 65 years by the average daily income and adjusted by the average employment rates of the corresponding age group. The number of work-loss days was estimated by multiplying the annual hospitalization days and outpatient visits for each cancer site reported in the Patient Survey 2014 (31) by the age-, gender- and site-specific number of patients. We estimated the average daily wage for the 5-year age group from the Basic Survey on Wage Structure 2015 (28). The average employment rates by gender and 5-year age group were obtained from the Labour Force Survey 2015 (32).
Further, we performed disaggregated estimation of the total economic costs of cancer by major five modifiable risk factors, namely active tobacco smoking (PAF: 15.2% of all cancer incidence), alcohol drinking (PAF: 6.2%), infectious agents (H. pylori, hepatitis C virus, hepatitis B virus, HPV, Epstein-Barr virus, and human T-cell leukemia virus type) (PAF: 16.6%), excess bodyweight (PAF: 0.7%), and physical inactivity (PAF: 1.3%) (8). These risk factors could be avoided if the exposure were either eliminated or reduced to the theoretical minimum risk exposure distribution. In this study, all the economic costs are presented in 2015 prices in Japanese yen (JPY), which was converted to US dollars (USD) using the annual average exchange rate of the same year (1 USD = 121.044 yen).
Results and Discussion
Total economic costs of cancer
In 2015, the total number of cancer patients who received any type of healthcare service and were reported to the NDB Japan was 4,045,940 persons (men, 2,107,331 persons; women, 1,938,609 persons). Prostate was the most common cancer site in men (551,195 persons), followed by stomach (316,112 persons) and colon (230,125 persons). In women, breast was the most common cancer site (659,970 persons), followed by colon (197,745 persons) and stomach (154,807 persons). Population attributable fraction of cancer incidence was highest in stomach cancer in men (85.05%) and cervical cancer in women (100%) (8).
Table 2 lists the total economic costs and associated cost components of cancer as of 2015. The overall estimated cost of cancer inclusive of direct medical costs, indirect mortality costs and indirect morbidity costs was ¥2,859,727 million ($23,626 million) for both sexes, ¥1,494,581 million ($12,347 million) in men, and ¥1,365,146 million ($11,278 million) in women. The direct medical costs of cancer, which include all costs of healthcare and medical examinations during hospitalization and outpatient visits, and prescriptions and drugs were highest in male prostate cancer (¥189,723 million /$1,567 million), and breast cancer in women (¥200,249 million/$1,654 million).
Table 2. Total economic costs of cancer by cancer site, Japan, 2015.
| Cancer Site | Direct medical costs* |
Indirect mortality costs* |
Indirect morbidity costs* |
Total costs* |
||||
|---|---|---|---|---|---|---|---|---|
| JPY | USD | JPY | USD | JPY | USD | JPY | USD | |
| Both sexes, all cancers | 1,520,487 | 12,561 | 726,943 | 6,006 | 612,297 | 5,058 | 2,859,727 | 23,626 |
| Men | ||||||||
| All cancers | 848,537 | 7,010 | 393,309 | 3,249 | 252,736 | 2,088 | 1,494,581 | 12,347 |
| Stomach | 79,565 | 657 | 49,565 | 409 | 33,794 | 279 | 162,923 | 1,346 |
| Lung, trachea | 101,021 | 835 | 68,795 | 568 | 23,303 | 193 | 193,118 | 1,595 |
| Colon | 76,649 | 633 | 37,361 | 309 | 29,233 | 242 | 143,243 | 1,183 |
| Liver | 34,089 | 282 | 30,573 | 253 | 8,679 | 72 | 73,341 | 606 |
| Leukemia | 45,636 | 377 | 20,782 | 172 | 12,738 | 105 | 79,156 | 654 |
| Rectum | 52,361 | 433 | 27,884 | 230 | 20,919 | 173 | 101,165 | 836 |
| Esophagus | 20,837 | 172 | 16,845 | 139 | 8,512 | 70 | 46,194 | 382 |
| Bladder | 25,655 | 212 | 4,422 | 37 | 12,756 | 105 | 42,833 | 354 |
| Oral cavity and pharynx | 15,985 | 132 | 14,960 | 124 | 11,835 | 98 | 42,780 | 353 |
| Kidney and other urinary organs | 21,925 | 181 | 9,712 | 80 | 13,524 | 112 | 45,161 | 373 |
| Pancreas | 24,510 | 202 | 33,786 | 279 | 5,565 | 46 | 63,861 | 528 |
| Larynx | 5,543 | 46 | 660 | 5 | 3,283 | 27 | 9,486 | 78 |
| Prostate | 189,723 | 1,567 | 2,312 | 19 | 19,051 | 157 | 211,087 | 1,744 |
| Malignant lymphoma | 33,136 | 274 | 14,394 | 119 | 16,930 | 140 | 64,459 | 533 |
| Gallbladder and bile ducts | 10,846 | 90 | 8,421 | 70 | 4,085 | 34 | 23,353 | 193 |
| Women | ||||||||
| All cancers | 671,950 | 5,551 | 333,634 | 2,756 | 359,561 | 2,971 | 1,365,146 | 11,278 |
| Stomach | 38,100 | 315 | 28,389 | 235 | 16,136 | 133 | 82,625 | 683 |
| Breast | 200,249 | 1,654 | 86,107 | 711 | 146,491 | 1,210 | 432,846 | 3,576 |
| Lung, trachea | 62,664 | 518 | 22,299 | 184 | 13,261 | 110 | 98,224 | 811 |
| Liver | 17,418 | 144 | 5,222 | 43 | 2,027 | 17 | 24,667 | 204 |
| Cervix uteri | 9,936 | 82 | 29,593 | 244 | 24,448 | 202 | 63,977 | 529 |
| Colon | 61,993 | 512 | 25,644 | 212 | 18,919 | 156 | 106,557 | 880 |
| Leukemia | 28,358 | 234 | 10,770 | 89 | 8,709 | 72 | 47,837 | 395 |
| Rectum | 27,082 | 224 | 11,606 | 96 | 10,539 | 87 | 49,227 | 407 |
| Corpus uteri | 12,330 | 102 | 9,602 | 79 | 16,736 | 138 | 38,669 | 319 |
| Esophagus | 4,600 | 38 | 4,188 | 35 | 1,651 | 14 | 10,440 | 86 |
| Pancreas | 20,453 | 169 | 14,657 | 121 | 3,130 | 26 | 38,239 | 316 |
| Malignant lymphoma | 27,281 | 225 | 6,656 | 55 | 12,353 | 102 | 46,290 | 382 |
| Oral cavity and pharynx | 4,885 | 40 | 4,872 | 40 | 3,663 | 30 | 13,420 | 111 |
| Bladder | 6,903 | 57 | 1,425 | 12 | 2,744 | 23 | 11,072 | 91 |
| Kidney and other urinary organs | 9,247 | 76 | 2,467 | 20 | 4,249 | 35 | 15,962 | 132 |
| Ovary | 18,528 | 153 | 27,826 | 230 | 14,277 | 118 | 60,631 | 501 |
| Gallbladder and bile ducts | 8,957 | 74 | 4,432 | 37 | 1,488 | 12 | 14,877 | 123 |
| Larynx | 386 | 3 | 114 | 1 | 338 | 3 | 838 | 7 |
*Data are millions of Japanese yen (JPY) and US dollars (USD).
Table 2 also summarizes the economic cost of potential work-life lost due to premature deaths from cancer, with a cut-off age of 65 (age of retirement in Japan). A total of ¥726,943 million ($6,006 million) was estimated to be lost due to premature death in Japan in 2015. Lung cancer incurred the highest indirect mortality cost in men (¥68,795 million/$568 million). In women, breast cancer caused the highest cost of indirect mortality (¥86,107 million/$711 million). The indirect morbidity costs, which means the annual productivity loss due to the absenteeism associated with cancer treatment, was estimated at ¥612,297 million/$5,058 million in 2015. The type of cancer that incurred the greatest productivity loss in men was stomach cancer (¥33,794 million/$279 million). In women, the highest productivity loss was seen in breast cancer (¥146,691 million/$1,210 million).
Economic costs of cancer attributable to modifiable risk factors
Table 3 lists the cost components of economic costs attributable to modifiable risk factors of cancer. The overall estimated cost of cancer inclusive of direct medical costs, indirect mortality costs and indirect morbidity costs that were attributable to lifestyle and environmental factors was ¥1,024,006 million ($8,460 million) for both sexes, ¥673,780 million ($5,566 million) in men, and ¥350,226 million ($2,893 million) in women. The direct medical costs of cancer associated with modifiable risk factors were highest in stomach cancer in both men (¥67,655 million /$559 million) and women (¥33,187 million/$274 million).
Table 3. Total economic costs attributable to modifiable risk factors, Japan, 2015.
| Cancer Site | Direct medical costs* |
Indirect mortality costs* |
Indirect morbidity costs* |
Total costs* |
||||
|---|---|---|---|---|---|---|---|---|
| JPY | USD | JPY | USD | JPY | USD | JPY | USD | |
| Both sexes, all cancers | 538,254 | 4,447 | 285,150 | 2,356 | 200,602 | 1,657 | 1,024,006 | 8,460 |
| Men | ||||||||
| All cancers | 368,460 | 3,044 | 195,574 | 1,616 | 109,746 | 907 | 673,780 | 5,566 |
| Stomach | 67,655 | 559 | 42,930 | 355 | 28,735 | 237 | 139,320 | 1,151 |
| Lung, trachea | 67,025 | 554 | 45,132 | 373 | 15,461 | 128 | 127,618 | 1,054 |
| Colon | 32,221 | 266 | 15,222 | 126 | 12,289 | 102 | 59,731 | 493 |
| Liver | 25,317 | 209 | 23,033 | 190 | 6,446 | 53 | 54,796 | 453 |
| Leukemia | 17,904 | 148 | 6,544 | 54 | 4,998 | 41 | 29,445 | 243 |
| Rectum | 17,871 | 148 | 9,267 | 77 | 7,140 | 59 | 34,278 | 283 |
| Esophagus | 17,163 | 142 | 13,718 | 113 | 7,011 | 58 | 37,893 | 313 |
| Bladder | 10,680 | 88 | 1,801 | 15 | 5,310 | 44 | 17,791 | 147 |
| Oral cavity and pharynx | 10,011 | 83 | 9,139 | 76 | 7,412 | 61 | 26,562 | 219 |
| Kidney and other urinary organs | 8,512 | 70 | 4,148 | 34 | 5,250 | 43 | 17,910 | 148 |
| Pancreas | 6,580 | 54 | 9,017 | 74 | 1,494 | 12 | 17,091 | 141 |
| Larynx | 4,268 | 35 | 498 | 4 | 2,528 | 21 | 7,294 | 60 |
| Prostate | 2,621 | 22 | 69 | 1 | 263 | 2 | 2,953 | 24 |
| Malignant lymphoma | 2,178 | 18 | 668 | 6 | 1,113 | 9 | 3,959 | 33 |
| Gallbladder and bile ducts | 332 | 3 | 226 | 2 | 125 | 1 | 684 | 6 |
| Women | ||||||||
| All cancers | 169,793 | 1,403 | 89,576 | 740 | 90,857 | 751 | 350,226 | 2,893 |
| Stomach | 33,187 | 274 | 25,570 | 211 | 14,055 | 116 | 72,812 | 602 |
| Breast | 27,992 | 231 | 12,190 | 101 | 20,477 | 169 | 60,658 | 501 |
| Lung, trachea | 20,820 | 172 | 6,962 | 58 | 4,406 | 36 | 32,188 | 266 |
| Liver | 12,199 | 101 | 3,793 | 31 | 1,419 | 12 | 17,411 | 144 |
| Cervix uteri | 9,936 | 82 | 29,593 | 244 | 24,448 | 202 | 63,977 | 529 |
| Colon | 9,382 | 78 | 3,870 | 32 | 2,863 | 24 | 16,116 | 133 |
| Leukemia | 8,242 | 68 | 2,723 | 22 | 2,531 | 21 | 13,495 | 111 |
| Rectum | 2,640 | 22 | 1,023 | 8 | 1,028 | 8 | 4,691 | 39 |
| Corpus uteri | 1,984 | 16 | 1,782 | 15 | 2,693 | 22 | 6,458 | 53 |
| Esophagus | 1,975 | 16 | 1,682 | 14 | 709 | 6 | 4,366 | 36 |
| Pancreas | 1,568 | 13 | 1,060 | 9 | 240 | 2 | 2,868 | 24 |
| Malignant lymphoma | 1,565 | 13 | 291 | 2 | 708 | 6 | 2,564 | 21 |
| Oral cavity and pharynx | 1,557 | 13 | 1,316 | 11 | 1,168 | 10 | 4,041 | 33 |
| Bladder | 659 | 5 | 115 | 1 | 262 | 2 | 1,035 | 9 |
| Kidney and other urinary organs | 277 | 2 | 63 | 1 | 127 | 1 | 466 | 4 |
| Ovary | 193 | 2 | 321 | 3 | 149 | 1 | 663 | 5 |
| Gallbladder and bile ducts | 78 | 1 | 36 | 0 | 13 | 0 | 126 | 1 |
| Larynx | 51 | 0 | 13 | 0 | 45 | 0 | 109 | 1 |
*Data are millions of Japanese yen (JPY) and US dollars (USD).
Table 3 also shows the indirect cost of mortality from cancer due to modifiable risk factors. A total of ¥285,150 million ($2,356 million) was lost due to premature death in Japan in 2015 which could have been potentially averted. Lung cancer incurred the highest indirect mortality cost in men (¥45,132 million/$373 million) and cervical cancer in women (¥29,593 million/$244 million). Similarly, the estimated indirect morbidity costs that could have been theoretically prevented were ¥200,602 million ($1,657 million) in 2015. Modifiable productivity loss was the highest in stomach cancer in men (¥28,735 million/$237 million), and cervical cancer in women (¥24,448 million/$202 million).
Table 4 presents the total economic costs of cancer attributable to each of the five modifiable risk factors for both sexes. The economic burden of cancer caused by infection was highest among all modifiable risk factors (¥478,774 million/$3,955 million), followed by active tobacco smoking (¥434,048 million/$3,586 million) and alcohol drinking (¥172,129 million/$1,422 million).
Table 4. Breakdown of total economic costs by major modifiable risk factors*, both sexes, Japan, 2015.
| Cancer Site | Active smoking |
Alcohol |
Infections |
Excess body weight |
Physical inactivity |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| JPY | USD | JPY | USD | JPY | USD | JPY | USD | JPY | USD | |
| All cancers | 434,048 | 3,586 | 172,129 | 1,422 | 478,774 | 3,955 | 19,041 | 157 | 33,726 | 279 |
| Oral cavity and pharynx | 19,951 | 165 | 13,049 | 108 | 6,933 | 57 | 0 | 0 | 0 | 0 |
| Esophagus | 28,435 | 235 | 29,784 | 246 | 0 | 0 | 162 | 1 | 0 | 0 |
| Stomach | 35,472 | 293 | 10,731 | 89 | 210,993 | 1,743 | 1,110 | 9 | 0 | 0 |
| Colon | 16,303 | 135 | 33,146 | 274 | 0 | 0 | 4,619 | 38 | 9,890 | 82 |
| Rectum | 12,456 | 103 | 21,562 | 178 | 0 | 0 | 3,082 | 25 | 6,991 | 58 |
| Liver | 24,401 | 202 | 26,145 | 216 | 60,655 | 501 | 3,102 | 26 | 0 | 0 |
| Gallbladder and bile ducts | 0 | 0 | 0 | 0 | 0 | 0 | 820 | 7 | 0 | 0 |
| Pancreas | 19,952 | 165 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Larynx | 6,486 | 54 | 2,667 | 22 | 0 | 0 | 0 | 0 | 0 | 0 |
| Lung, trachea | 138,553 | 1,145 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Breast | 0 | 0 | 27,186 | 225 | 0 | 0 | 1,904 | 16 | 22,159 | 183 |
| Cervix uteri | 9,241 | 76 | 0 | 0 | 63,977 | 529 | 0 | 0 | 0 | 0 |
| Corpus uteri | 0 | 0 | 0 | 0 | 0 | 0 | 270 | 2 | 5,896 | 49 |
| Ovary | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Prostate | 0 | 0 | 0 | 0 | 0 | 0 | 2,992 | 25 | 0 | 0 |
| Bladder | 18,809 | 155 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Kidney and other urinary organs | 17,596 | 145 | 0 | 0 | 0 | 0 | 1,029 | 9 | 0 | 0 |
| Malignant lymphoma | 0 | 0 | 0 | 0 | 6,531 | 54 | 0 | 0 | 0 | 0 |
| Leukemia | 14,873 | 123 | 0 | 0 | 28,072 | 232 | 0 | 0 | 0 | 0 |
*Data are millions of Japanese yen (JPY) and US dollars (USD). Note that the sum of the economic costs of all risk factors occasionally exceeds the total economic costs presented in Table 2 because of the co-prevalence of multiple risk factors in a person.
Discussion
This report draws on updated estimates of cancer burden attributable to modifiable factors in Japan in 2015 published by Inoue et al. (8). Because cancer constitutes 12% of the direct costs of healthcare in Japan as of 2015 (13), and 35.4% of the direct medical costs of cancer are associated with lifestyle and environmental factors, controlling the modifiable risk factors may save more than 4% of healthcare costs. Further, this study found that the indirect costs of cancer made up around 46.8% of the total costs. The indirect cost of morbidity in our study is analogous to that in a previous report in Japan in 2011, which estimated this cost to be around ¥295,900 million for men (33). On the other hand, our estimate of the indirect morbidity cost in women was higher (¥359,561 million) than their estimate (¥156,900 million) (33). This difference is because they used the sex- and age-specific average daily wage, whereas we used the age-specific average daily wage common for both men and women, to take account of the potential full earnings lost according to market value.
Our study found that there were around 1.1 times more male cancer patients than female patients in Japan in 2015, and that the total economic costs of cancer did not considerably differ between men and women. This is because female breast cancer, which is by far the most common female cancer in Japan, accounted for by far the greatest economic burden in terms of not only direct costs but also indirect mortality costs and indirect morbidity costs. Breast cancer begins to occur in working-age women in their 40s (2), and the indirect costs of cancer rise when premature deaths occur or patients receive treatment at a younger age. For the same reason, cervical cancer ranked second in indirect morbidity and mortality costs in women although the direct medical costs ranked only 12th among all the cancer sites investigated in this study.
It was not surprising to find that lung, stomach, colon and male prostate cancer incurred a heavy economic burden in terms of both direct medical costs and indirect costs, as these are the most commonly reported types of cancer in Japanese (2). Previous reports from the European Union are consistent with our findings - lung cancer showed the highest economic cost followed by breast cancer, colorectal cancer and prostate cancer but not stomach cancer (10). In Korea, where Helicobacter pylori infection is prevalent (34), the economic burden of cancer was heaviest in stomach cancer, followed by liver, lung, and colorectal cancers in 2015 (11).
Economic burden attributable to modifiable risk factors
According to our estimation, the economic burden of cancer was highest in cancers that are caused by infection, namely Helicobacter pylori (H.pylori) for stomach cancer (85%) and human papillomavirus (HPV) for cervical cancer in women (100%) (20). In other words, ¥210,993 million ($1,743 million) could have been saved if no infection from H.pylori had occurred, and ¥63,977 million ($529 million) could have been saved if no one had been infected by HPV in Japan. Further, active tobacco smoking constituted as much as 23.6% in men and 4.0% in women of the total population attributable fraction of cancer incidence in Japan in 2015 (17). This implies that a total of ¥434,048 million ($3,586 million) was lost in Japan due to tobacco smoking.
Limitations
Some limitations of this study warrant mention. First, we were not able to consider direct non-medical costs in our analysis. Access to medical facilities to receive treatment varies by geographic region in Japan, where islands are sparsely located, yet the NDB Japan data do not record the place of residence of patients. Therefore, we were unable to estimate distance to medical facilities. Second, although we considered productivity loss due to premature mortality and absenteeism from work, we were not able to estimate the impact of presenteeism (partial loss of productivity on days a patient did work) in our productivity loss estimation due to a paucity of data. Third, we were not able to estimate the informal care provided by family members, because data on the days and hours of informal care for each type of cancer were not available. Nonetheless, this study provides the first evidence on the direct medical costs, indirect morbidity and mortality costs, and costs associated with lifestyle and environmental factors in Japan from a societal perspective.
In conclusion, this study reported that the overall cost of cancer attributable to lifestyle and environmental factors was ¥1,024,006 million ($8,460 million) in Japan in 2015. Productivity loss associated with modifiable factors was highest in stomach cancer in men (¥28,735 million/$237 million) and cervical cancer in women (¥24,448 million/$202 million). Preventing and controlling cancers caused by infections, including H.pylori and HPV, and tobacco smoking will not only be life-saving but may also be cost-saving in the long run.
Funding
This study was supported by JSPS KAKENHI Grant Number 16H05244 and the National Cancer Center Research and Development Fund (2021-A-16).
Conflict of Interest
The authors have no conflicts of interest to disclose.
References
- 1. Ministry of Health, Labour and Welfare. Vital Statistics of Japan. https://www.e-stat.go.jp/stat-search/files?page=1&toukei=00450011&kikan=00450&tstat=000001028897&result_page=1 (accessed January 11, 2023). (in Japanese) .
- 2. National Cancer Center Japan. Cancer Statistics. Cancer Information Service, National Cancer Center, Japan (Vital Statistics of Japan, Ministry of Health, Labour and Welfare). https://ganjoho.jp/reg_stat/statistics/data/dl/index.html (accessed January 11, 2023). (in Japanese) .
- 3. Peto J. Cancer epidemiology in the last century and the next decade. Nature. 2001; 411:390-395. [DOI] [PubMed] [Google Scholar]
- 4. Doll R, Peto R. The causes of cancer: quantitative estimates of avoidable risks of cancer in the United States today. J Natl Cancer Inst. 1981; 66:1191-1308. [PubMed] [Google Scholar]
- 5. Soerjomataram I, Shield K, Marant-Micallef C, Vignat J, Hill C, Rogel A, Menvielle G, Dossus L, Ormsby JN, Rehm J, Rushton L, Vineis P, Parkin M, Bray F. Cancers related to lifestyle and environmental factors in France in 2015. Eur J Cancer. 2018; 105:103-113. [DOI] [PubMed] [Google Scholar]
- 6. Harvard Report on Cancer Prevention. Volume 1: Causes of human cancer. Cancer Causes Control. 1996; 7 Suppl 1:S3-S59. [DOI] [PubMed] [Google Scholar]
- 7. Wang JB, Jiang Y, Liang H, et al. Attributable causes of cancer in China. Ann Oncol. 2012; 23:2983-2989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Inoue M, Hirabayashi M, Abe SK, et al. Burden of cancer attributable to modifiable factors in Japan in 2015. Glob Health Med. 2022; 4:26-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Haga K, Matsumoto K, Kitazawa T, Seto K, Fujita S, Hasegawa T. Cost of illness of the stomach cancer in Japan - a time trend and future projections. Bmc Health Serv Res. 2013; 13:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Luengo-Fernandez R, Leal J, Gray A, Sullivan R. Economic burden of cancer across the European Union: a population-based cost analysis. Lancet Oncol. 2013; 14:1165-1174. [DOI] [PubMed] [Google Scholar]
- 11. Kim YA, Lee YR, Park J, Oh IH, Kim H, Yoon SJ, Park K. Socioeconomic Burden of Cancer in Korea from 2011 to 2015. Cancer Res Treat. 2020; 52:896-906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Matsumoto K, Haga K, Kitazawa T, Seto K, Fujita S, Hasegawa T. Cost of illness of breast cancer in Japan: trends and future projections. BMC Res Notes. 2015; 8:539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ministry of Health, Labour and Welfare. Estimates of National Medical Care Expenditure. 2015. https://www.mhlw.go.jp/english/database/db-hss/enmce.html (accessed January 11, 2023).
- 14. Larg A, Moss JR. Cost-of-illness studies: a guide to critical evaluation. Pharmacoeconomics. 2011; 29:653-671. [DOI] [PubMed] [Google Scholar]
- 15. Nishioka Y, Okada S, Noda T, Myojin T, Kubo S, Ohtera S, Kato G, Kuroda T, Ishii H, Imamura T. Absolute risk of acute coronary syndrome after severe hypoglycemia: A population-based 2-year cohort study using the National Database in Japan. J Diabetes Investig. 2020; 11:426-434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nakajima A, Sakai R, Inoue E, Harigai M. Prevalence of patients with rheumatoid arthritis and age-stratified trends in clinical characteristics and treatment, based on the National Database of Health Insurance Claims and Specific Health Checkups of Japan. Int J Rheum Dis. 2020; 23:1676-1684. [DOI] [PubMed] [Google Scholar]
- 17. Katanoda K, Hirabayashi M, Saito E, Hori M, Abe SK, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to tobacco smoke in Japan in 2015. GHM Open. 2021; 1:43-50. [Google Scholar]
- 18. Hirabayashi M, Sawada N, Abe SK, Saito E, Hori M, Katanoda K, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to consumption of alcohol in Japan in 2015. GHM Open. 2021; 1:51-55. [Google Scholar]
- 19. Hirabayashi M, Abe SK, Sawada N, Saito E, Hori M, Katanoda K, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to excess bodyweight and physical inactivity in Japan in 2015. GHM Open. 2021; 1:56-62. [Google Scholar]
- 20. Lin Y, Wang C, Kikuchi S, Akita T, Tanaka J, Abe SK, Hirabayashi M, Saito E, Hori M, Katanoda K, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to infection in Japan in 2015. GHM Open. 2021; 1:63-69. [Google Scholar]
- 21. Takachi R, Ishihara J, Abe SK, Hirabayashi M, Saito E, Hori M, Katanoda K, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to consumption of highly salted food in Japan in 2015. GHM Open. 2021; 1:85-90. [Google Scholar]
- 22. Ishihara J, Takachi R, Abe SK, Hirabayashi M, Saito E, Hori M, Katanoda K, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to insufficient vegetable, fruit and dietary fiber consumption in Japan in 2015. GHM Open. 2021; 1:70-75. [Google Scholar]
- 23. Abe SK, Takachi R, Ishihara J, Hirabayashi M, Saito E, Hori M, Katanoda K, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to excess red and processed meat consumption in Japan in 2015. GHM Open. 2021; 1:91-96. [Google Scholar]
- 24. Hirabayashi M, Nagata C, Abe SK, Sawada N, Saito E, Hori M, Katanoda K, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to exogenous hormone use in Japan in 2015. GHM Open. 2021; 1:97-101. [Google Scholar]
- 25. Hirabayashi M, Nagata C, Abe SK, Saito E, Hori M, Katanoda K, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to never breastfeeding in Japan in 2015. GHM Open. 2021; 1:102-105. [Google Scholar]
- 26. Hori M, Katanoda K, Ueda K, Nakaya T, Saito E, Abe SK, Hirabayashi M, Matsuda T, Inoue M; the Cancer PAF Japan Collaborators. Burden of cancer attributable to air pollution in Japan in 2015. GHM Open. 2021; 1:76-84. [Google Scholar]
- 27. Wu Q, Szatkowski L, Britton J, Parrott S. Economic cost of smoking in people with mental disorders in the UK. Tob Control. 2015; 24:462-468. [DOI] [PubMed] [Google Scholar]
- 28. Ministry of Health, Labour and Welfare. Basic Survey on Wage Structure. https://www.mhlw.go.jp/english/database/db-l/wage-structure.html (accessed January 11, 2023).
- 29. World Health Organization. Making choices in health: WHO guide to cost-effectiveness analysis. https://apps.who.int/iris/handle/10665/42699?locale-attribute=en& (accessed January 11, 2023).
- 30. Hanly P, Timmons A, Walsh PM, Sharp L. Breast and prostate cancer productivity costs: a comparison of the human capital approach and the friction cost approach. Value Health. 2012; 15:429-436. [DOI] [PubMed] [Google Scholar]
- 31. Ministry of Health, Labour and Welfare. Patient Survey 2014. https://www.mhlw.go.jp/toukei/saikin/hw/kanja/14/index.html (accessed January 11, 2023). (in Japanese) .
- 32. Statistics Bureau of Japan. Labour Force Survey 2015. https://www.e-stat.go.jp/en/stat-search/files?page=1&layout=datalist&toukei=00200531&tstat=000000110001&cycle=7&year=20150&month=0&tclass1=000001040276&tclass2=000001040283&tclass3=000001040284&result_back=1&tclass4val=0 (accessed January 11, 2023).
- 33. Fukuda K. Estimation of productivity loss due to cancer incidence. 2012-13 Ministry of Health, Labour and Welfare Research Grant Report. https://hospital.luke.ac.jp/about/approach/doc/ra21/2/research_activities_2_6.doc (accessed January 11, 2023). (in Japanese) .
- 34. Leja M, Grinberga-Derica I, Bilgilier C, Steininger C. Review: Epidemiology of Helicobacter pylori infection. Helicobacter. 2019; 24 Suppl 1:e12635. [DOI] [PubMed] [Google Scholar]


