Abstract
Objectives
This study examined short- and long-term psychological adjustment to parental bereavement in later life for mothers and fathers.
Methods
Using 9 waves of data from the United States (1998–2014 Health and Retirement Study), I estimated trajectories of mothers’ and fathers’ depressive symptoms surrounding child death in later life, highlighting gender differences in adjustment. Moderation analyses were performed to uncover heterogeneous trajectories across parental characteristics.
Results
Mothers were more likely to experience child death and reported higher depressive symptoms prior to parental bereavement than fathers. Mothers and fathers who lost a child reported an increase in depressive symptoms that diminished over time. The short-term elevation in depressive symptoms was marginally greater for mothers than fathers, but depressive symptoms declined at a faster rate for mothers than fathers in the years following the death. These counterbalancing changes resulted in mothers and fathers returning to their respective prebereavement levels of depressive symptoms between 2 and 4 years postbereavement. Parental age moderated trajectories distinctly by gender, and the presence of surviving children buffered the impact of child death on depressive symptoms for mothers but not fathers.
Discussion
Mothers more often experience child death in later life and their adjustment process differs from that of fathers, underscoring the salience of gender in shaping how older parents respond to the death of a child. Older parents and mothers without surviving children are vulnerable to prolonged elevations in depressive symptoms following the death of a child in later life.
Keywords: Life course, Parental bereavement, Population heterogeneity, Psychological adjustment
Child death is a stressful life event for all who experience it. Children are expected to outlive their parents, so when a child dies, the natural order of life is disrupted. Most research to date focuses on child death that occurs prior to midlife when parents and children are younger (e.g., Donnelly et al., 2020; Rogers et al., 2008; Umberson et al., 2020). However, given increases in age at first birth and life expectancy over the past several decades, people are becoming parents later and remaining parents longer, which means the risk of exposure to child death is moving up the age gradient and lengthening at later ages.
Alburez-Gutierrez and colleagues (2021) recently estimated that women born in 1985 will be the first cohort to experience child death more often at retirement ages (after age 65) than at reproductive ages (before age 50), reversing an enduring global trend. Projections for women born in later cohorts are even more pronounced. For instance, on average, North American or European women born in 2000 who survive to age 100 will be around 15 times more likely to experience the death of a child in their retirement years than in their reproductive years (Alburez-Gutierrez et al., 2021). In the United States, the disproportionate rise in “deaths of despair”—those related to substance abuse and suicide—among midlife adults with low socioeconomic status portends an increase in the number of older parents who experience the death of an adult child in later life (Case & Deaton, 2021). Sustained declines in fertility and mortality foretell an overall decrease in the number of parents who experience child death at any age over the next several decades (Alburez-Gutierrez et al., 2021), but a rise in “deaths of despair” among midlife children and a persistent gender gap in life expectancy could partially offset this decline among older parents, especially for mothers in lower-income families in the United States (Case & Deaton, 2021). If current demographic trends persist, although parental bereavement will become less normative at all ages, its incidence will be increasingly concentrated among mothers in later life (Alburez-Gutierrez et al., 2021). Uncovering the public health implications of losing a child as an older parent can facilitate the provision of effective grief support to bereaved parents and by extension promote successful aging more broadly. Yet, research on parental bereavement during the second half of life is surprisingly scant, and little is known about potential gender differences in parental adjustment to child death in later life.
Drawing on prospective, population-based data from the 1998–2014 Health and Retirement Study (HRS), I examine trajectories of psychological well-being surrounding parental bereavement in later life. Using growth curve models, I map population-level trajectories of depressive symptoms before, during, and after the death of a child experienced by parents aged 50 and older in the United States. Child death earlier in the life course has been shown to exert a greater psychological impact on mothers compared with fathers (Li et al., 2005; Rogers et al., 2008; Rostila et al., 2018), but whether these gender differentials persist in later in life is not well understood. I explore variation in the short- and long-term psychological impact of child death in later life by parental gender. Bereavement is not a monolithic experience, and thus population-level trajectories may smooth over the varied experiences of bereaved parents. Therefore, I conduct moderation analyses for mothers and fathers using an array of potentially relevant factors captured in the HRS. This study draws attention to an understudied life event—parental bereavement in later life—and produces for the first time population-level trajectories of depressive symptoms for bereaved mothers and fathers starting before a child’s death spanning over a decade following the loss. Moderation analyses elucidate subpopulations of older parents who may be especially vulnerable to a child’s death, helping to guide timely support from grief counselors and health care practitioners.
The Significance of Child Death in Later Life
Two tenets of the life course perspective—the timing of life course events and the reciprocal nature of family relationships (i.e., linked lives)—illuminate the importance of this perspective in understanding how the characteristics of older adulthood may shape adjustment to the death of a child when experienced in later life (Elder et al., 2003). A life course perspective on stress underlines the shifting landscape of life events through which people transition as they age and emphasizes the consideration of the timing of these events when examining late-life adjustment to stress (Pearlin & Skaff, 1996). At various life stages, people manifest stress differently and their social support systems differ in scope and composition (Pearlin, 1989).
Losing a child likely operates as a major turning point in older adulthood because of the linked lives of parents and children during this stage of life (Elder et al., 2003). Intergenerational ties are considered among the most enduring and influential of all social relationships. As parents and children age together, their lives become intimately interwoven and the parental role takes on new meaning (Rossi & Rossi, 1990). Older parents and their children share values and attitudes and often become sources of mutual support later in life (Seltzer & Bianchi, 2013), differentiating child death in later life from child death earlier in the life course when children are younger and more dependent. The rupture of the reciprocal parent–child relationship when parents and children are older may prove to be especially detrimental for parental well-being because they lose a mutually supportive relationship. Furthermore, younger parents may be inclined to give birth to a new child after child death (Finnäs et al., 2018), but older parents do not have the same opportunity for parity progression. Prior studies provide a sense of how parents adjust to child death more generally, but research with a singular focus on psychosocial adjustment to parental bereavement in later life is critical to our understanding of a life event that increasingly is concentrated in old age.
Parental Depressive Symptoms Following Child Death
The death of a child is a profoundly traumatic event and often is considered the worst life experience one can endure (e.g., Miller & Rahe, 1997). Child death is an off-time event that disturbs the natural order of life (Pearlin & Skaff, 1996). Upon losing a child, bereaved parents experience a period of intense emotional suffering that can last for many years following the loss (Stroebe et al., 2007), but whether this trauma manifests in short- versus long-term changes in depressive symptoms has been debated in the literature. Bonanno and colleagues (2005) measured bereaved parents’ depressive symptoms shortly after child death at 4- and 18-month postloss. Over half of bereaved parents in their sample showed resilience to the death, reporting similar levels of depressive symptoms to nonbereaved parents at both time points. However, 48% of bereaved parents reported higher depressive symptoms than nonbereaved controls at both the 4- and 18-month assessments. Kreicbergs et al. (2004) assessed the risk of depression between bereaved and nonbereaved parents over a 9-year period and found that bereaved parents endured a greater risk of depression than nonbereaved parents lasting up to 6 years after the death. In contrast, two other studies documented longer-term gaps in depressive symptoms between bereaved and nonbereaved parents spanning up to 20 years postbereavement (Rogers et al., 2008; Song et al., 2010).
These conflicting findings likely are related to differences in methodologies across studies, particularly discrepant measures of the timing of child death and parents’ depressive symptoms and a lack of preloss assessments. Most studies group together bereaved parents of all ages, young and old. Inconsistent measurement of the timing of child death vis-à-vis bereaved parents’ depressive symptoms across these studies makes it difficult to generalize their findings to child death experienced in later life. Past research also tends to measure child death retrospectively and compare postloss depressive symptoms between bereaved and nonbereaved parents. Given that bereaved parents typically report higher depressive symptoms than their nonbereaved counterparts even prior to child loss (Bolton et al., 2014; Floyd et al., 2013), this analytic strategy overlooks the role of selection into parental bereavement. Therefore, although past studies document differences in depressive symptoms by parental bereavement status, most cannot speak directly to bereaved parents’ individual adjustment to child death. Accounting for prebereavement depressive symptoms using prospective assessments before and after the loss is critical for accurately describing how the transition to parental bereavement shapes depressive symptoms over time (Bolton et al., 2014; Floyd et al., 2013; Maccallum et al., 2015).
Among the prior studies that include prebereavement information, only two studies based in the United States consider the association between parental bereavement specifically experienced in later life and depressive symptoms, and their findings were mixed. Floyd and colleagues (2013) examined pre- to postbereavement depressive symptoms of Wisconsin parents who experienced the death of a child at any time between 1992/1994 and 2004/2006. In these waves of the Wisconsin Longitudinal Survey (WLS), parents had a mean age of 54 and 65, respectively. The results revealed that, net of prebereavement differences in depressive symptoms, bereaved parents whose child died within the past 18 months reported higher levels of depressive symptoms than their nonbereaved counterparts. For the majority of bereaved parents, however, levels of depressive symptoms did not differ from the nonbereaved control group after 18 months after the loss. That is, parents endured a short-term depressive response after child death followed by a recovery over time. Maccallum et al. (2015) applied latent growth mixture modeling to HRS data to identify four discrete classes of depressive symptoms trajectories among those who either experienced widowhood or child death, assessed at one prebereavement time point and three postbereavement time points spanning 6 years total. The results from this analysis showed that the majority of bereaved parents (64.3%) exhibited “little or no depression at any time point [before or after child death]” (Maccallum et al., 2015, p. 72). In comparison, only 14% of bereaved parents reported a rise in depressive symptoms in the years following the loss characterized by a short-term increase followed by an eventual decline by the third time point.
These two studies offer insights on how older parents adjust to child death, but each has notable limitations that the present study overcomes. The WLS sample used by Floyd et al. (2013) is only generalizable to a particular cohort of older adults in Wisconsin and virtually all of the WLS sample (99%) identifies themselves as White with relatively high incomes (mean = $72,386 in 1992/1994 dollars) and education (all were high school graduates, 33% of whom earned postsecondary degrees). However, Black parents and parents with less than a high school education tend to experience child death at higher levels than White parents and those with more education, respectively (Mellencamp, 2019; Umberson et al., 2017). In addition, bereaved parents in Maccallum et al.’s (2015) analysis predominately were mothers (88%), raising questions about whether their results can be generalized to men given such a small sample of bereaved fathers (n = 64). Considering the limitations and disparate findings across past studies, it is difficult to extrapolate from them a population-level trajectory of depressive symptoms of mothers and fathers who experience parental bereavement in later life. The present study addresses these gaps by measuring within-parent changes in depressive symptoms before and after child death, and by including ample numbers of fathers, racially/ethnically minoritized parents, and parents with varying levels of education and economic resources.
Variation in Adjustment to Child Death
Adaptation to stress is shaped by other risks and protective factors that may serve as vulnerabilities or sources of resilience for individuals before and after experiencing a stressful life event (Pearlin, 1989). Research on child death to date has identified a range of salient factors that shape parental adjustment to this traumatic event. Racially/ethnically minoritized parents (Umberson & Donnelly, 2021; Youngblut et al., 2013), mothers (see the next section), and parents with fewer socioeconomic resources (Cacciatore et al., 2016) are at a greater risk of psychological distress than their respective counterparts following the death of a child. In contrast, interpersonal resources, namely social support and the presence of surviving children, ameliorate the impact of child death on psychological well-being (Infurna & Luthar, 2017; Li et al., 2005; Wijngaards-de Meij et al., 2005). The cause of a child’s death and parents’ intrapersonal characteristics both shape the experience of parental bereavement. An expected death related to a child’s long-term illness is particularly difficult for parents prior to the loss (Floyd et al., 2013), whereas an unexpected, sudden death is associated with intense grief reactions and depressive episodes postbereavement (Floyd et al., 2013; Wijngaards-de Meij et al., 2005). High self-efficacy and a strong sense of purpose in life also tend to promote resilience in bereaved persons as these intrapersonal characteristics aid in emotion regulation following loss (Floyd et al., 2013; Stroebe et al., 2007).
Past literature tends to focus on child death prior to midlife, so whether these characteristics operate similarly for the adjustment to child death in later life is unclear. The experience of other bereavement, such as the prior loss of a child or the death of other family members, and parental health have received less attention as potential moderators in the association between parental bereavement and psychological well-being. These factors warrant consideration given their connection with life course stress processes. Multiple forms of bereavement may compound stress over the life course, making it harder to adjust to a child’s death, but may also impart salient coping mechanisms that can be drawn upon in the face of child death. Poor parental health and negative health behaviors (e.g., heavy alcohol use and smoking) may serve as indicators of the lifelong wear and tear of cumulative stress on the body which could negatively affect one’s adjustment to child death in later life (Pearlin, 1989; Pearlin & Skaff, 1996). To explore the characteristics associated with variation in depressive symptoms trajectories surrounding child death in later life, I conduct moderation analyses using a host of risks and protective factors available in the HRS, including sociodemographic characteristics, socioeconomic resources, social support, the presence of surviving children, parental health (and health behaviors), the experience of past child death, and exposure to other family bereavement.
The Role of Parental Gender
As women live longer than men, they also are more likely to be confronted with bereavement in old age. Sometimes referred to as the “feminization of bereavement” (Williams et al., 2006), the gender disparity in exposure to family death in later life is most evident for spousal loss. However, increasing ages at first birth coupled with women’s greater survival to advanced ages likely also puts women at a heightened risk of experiencing child death in later life compared with men (Alburez-Gutierrez et al., 2021). Most prior research has found that mothers experience greater psychological distress than fathers in response to child loss earlier in the life course. Compared to bereaved fathers, bereaved mothers are at a greater risk for short- and long-term depression (Kreicbergs et al., 2004; Rogers et al., 2008; Wijngaards-de Meij et al., 2005), are more likely to be hospitalized for psychiatric disorders (Li et al., 2005), and more frequently use antidepressants following the loss (Rostila et al., 2018). Scholars offer two explanations for these differentials.
First, women may be more psychologically vulnerable to adverse life events like the death of a child. The gender gap in depressive symptoms across the life course is a well-documented finding in mental health research and is explained, in part, by women’s higher rates of chronic conditions, lower socioeconomic status, and higher rates of spousal loss (Acciai & Hardy, 2017). Differential exposure to these health-related, socioeconomic, and psychosocial risk factors likely shapes both pre- and postbereavement psychological contexts distinctly for mothers and fathers. Second, greater maternal investments in child rearing and kin-keeping may nurture closer relationships between children and their mothers than their fathers across the life course (Rosenthal, 1985; Silverstein et al., 2006), and thus the death of a child may mean the loss of a more salient parent–child relationship for mothers compared with fathers. Psychological adjustment to “deaths of despair” (Case & Deaton, 2021) likely also differs for mothers and fathers. Child deaths due to suicide and substance abuse may disproportionately affect mothers’ well-being as some studies find mothers are more susceptible to guilt and self-blame associated with their children’s problems than fathers (Rossi & Rossi, 1990; Ryff et al., 1996).
Prior research on the death of a child in later life (i.e., Floyd et al, 2013; Maccallum et al., 2015) found that mothers who lost a child reported higher prebereavement depressive symptoms than their male counterparts, yet no notable gender differences in postbereavement depressive symptoms were uncovered. Nonetheless, the primacy of the mother–child bond endures well into old age as older mothers report more interactions with and transfers to their children as well as greater parent–child relationship quality compared with older fathers (Kalmijn, 2019; Ward, 2008), suggesting that child death in later life may have a greater impact on depressive symptoms for mothers than fathers as is documented earlier in the life course.
The Present Study
Recent demographic projections portend a shift in the life course timing of parental bereavement. Delayed onset of parenthood implies that exposure to child death will become concentrated primarily in later life (Alburez-Gutierrez et al., 2021), yet psychological adjustment to the death of a child during this life stage remains poorly understood, and whether mothers and fathers display disparate trajectories of psychological adjustment to the death of a child in later life is unclear. In addition, little is known about whether and how various parental characteristics and bereavement contexts shape psychological reactions to child death during this stage of the life course. Elucidating how older parents adjust to the death of a child and uncovering what factors buffer against its detrimental impact are paramount to providing timely support to vulnerable parents following this life event and to promoting healthy aging in general.
Using nine waves of nationally representative panel data from the HRS, I estimate population-level trajectories of depressive symptoms prior to, during, and after child death in later life, paying close attention to gender differences in the short-term impact and long-term recovery, to illustrate how mothers and fathers adjust to the traumatic loss of a child during the second half of the life course. I posit that, regardless of gender, bereaved parents endure an immediate rise in depressive symptoms at child death that will dissipate over time. I also hypothesize that, compared with bereaved fathers, bereaved mothers will experience a greater short-term elevation and a slower subsequent recovery in depressive symptoms levels after the loss. Several factors that may moderate the association between child death and parents’ depressive symptoms are considered in the analyses, including sociodemographic characteristics, socioeconomic and interpersonal resources, parental health, and other experiences of bereavement.
Method
Data came from the 1998–2014 HRS, harmonized for public use by the RAND Corporation. The HRS is a longitudinal, nationally representative study of American adults over age 50 and their spouses/partners. Most HRS baseline interviews are conducted face-to-face with roughly 18,000 respondents per wave. The biennial study began in 1992 and combined with the Asset and Health Dynamics of the Oldest Old study in 1998 with the addition of two new birth cohorts. After 1998, a new birth cohort has been added every 6 years as refreshers to ensure the sample remains generalizable to the population ages 51 and older. HRS samples were selected using a multistage clustered area probability sample design, and oversampled Blacks, Hispanics, and Floridians to ensure generalizability. Baseline response rates for new cohorts averaged around 73%, while reinterview response rates ranged from 85% to 90% between 1998 and 2014 (HRS Sample Sizes and Response Rates, 2017). In addition, the HRS provides final person weights to adjust for the unequal probability of selection for individuals (Ofstedal et al., 2011). The wide range of topics covered by the HRS allows for the inclusion of baseline and time-varying controls related to both depressive symptoms and exposure to child death. Unfortunately, parents’ intrapersonal characteristics and cumulative exposure to life course stress are available only in a leave-behind questionnaire given to a subset of respondents every 4 years, and the cause of a child’s death is not recorded in the HRS, precluding the inclusion of these variables in the present study.
Sample Selection
Drawing on data from the RAND Family Data File 1992–2014 (V1), I began with 29,198 respondents aged 50 and older who reported having at least one living biological child at their baseline wave in 1998–2014. Next, I excluded respondents with a sample weight equal to 0 or missing across all waves (n = 1,124) as well as those who never reported on depressive symptoms during their observation (n = 1,159). Finally, I selected the 1,207 mothers and 662 fathers who reported the death of a biological child during their observation period (6.42% of mothers vs 4.41% of fathers, p < .001). Parents who experienced multiple child deaths at different time points (<10% of bereaved parents) were censored at the wave in which they reported the second death. This strategy ensured to capture parents’ first experience of child death during their observation in the HRS.
Measures
Depressive symptoms were measured at each wave using a sum of eight items that the respondent reported experiencing during the week preceding the interview, answering yes or no to feeling depressed, feeling sad, feeling lonely, feeling that everything was an effort, being unable to get going, having restless sleep, being unhappy, and not enjoying life. Responses were summed, with values ranging from 0 to 8. This measure is an abridged version of the Center for Epidemiological Studies—Depression scale (Radloff, 1977).
Child death was measured using a time-varying indicator of whether the respondent reported a child deceased but alive at the previous time point (1 = yes, 0 = no). This measurement strategy ensured that all respondents were prospectively observed for at least one wave of data prior to the experience of child death. Once the death was reported, the respondent was coded 1 for the remainder of their observation period. Time since death was a time-varying indicator of the number of years that had passed since child death, coded as 0 at the wave in which a child was reported deceased, adding 2 years with each subsequent wave. For example, if the respondent experienced child death in 2000, this variable was coded as 0 in 2000, 2 in 2002, 4 in 2004, and so on.
Several sociodemographic characteristics were also included. Age was measured in years at the baseline wave. Racially/ethnically minoritized captured whether the respondent self-identified as a race–ethnicity other than non-Hispanic White (1 = yes, 0 = no). Partnership status was gauged at each wave, coded 1 if the respondent was married or cohabiting, and 0 otherwise. Surviving children was a time-invariant measure capturing whether the respondent reported at least one other living biological child at the time of a child’s death (1 = yes, 0 = no).
Socioeconomic resources consisted of two measures. Education was captured at the respondent’s baseline wave using their continuous years of schooling. Wealth was a logged time-varying measure of the respondent’s total nonhousing wealth in the previous year.
Interpersonal resources included three time-varying variables. Friends nearby indicated whether the respondent had any good friends living nearby (1 = yes, 0 = no), family nearby captured whether they had any relatives living nearby (1 = yes, 0 = no), and share of children in weekly contact measured the proportion of biological children with whom the respondent had at least weekly contact in the past 12 months, either in person, or by phone, mail, or e-mail.
Three health characteristics were captured. Chronic conditions was a time-varying sum of the respondent’s doctor-diagnosed health conditions, including cancer, heart disease, lung disease, stroke, high blood pressure, diabetes, arthritis, and psychiatric disorders. This variable ranged from 0 to 8. Heavy alcohol use was a time-varying binary measure that reflected whether the respondent consumed three or more alcoholic drinks on at least 1 day each week in the last 3 months (1 = yes, 0 = no), and smoker was a time-varying measure that captured whether the respondent currently smoked cigarettes at a given wave (1 = yes, 0 = no).
Finally, to account for the experience of other bereavement, the respondent’s exposure to other family deaths was measured using two variables. Prior child death was measured at baseline denoting whether the respondent had experienced the death of any biological child prior to their first HRS interview. This variable was constructed using information about the respondent’s number of children ever born and their reported number of living biological children at baseline. If the respondent’s number of children ever born exceeded the number of children living at baseline, they were coded as having experienced child death before age 50 (1 = yes, 0 = no; Donnelly et al., 2020). Concurrent family death was a time-varying measure indicating whether the respondent experienced the death of other family members during their observation, including the death of a spouse, parent, or sibling at each wave (1 = yes, 0 = no).
Multiple imputation using chained equations was used to impute missing values across independent variables (White et al., 2011). All respondent characteristics, including the dependent variable, were included as auxiliary variables in the chained equations. Ten random, multiply-imputed data sets were created and used in the analyses.
Analytic Strategy
Multiple analyses were estimated using Stata 17. First, I compared bereaved parents’ characteristics across gender to illustrate how the contexts preceding the death of a child in later life differed for mothers and fathers. Second, consistent with prior research examining depressive symptoms trajectories following major life events in later life (e.g., Lin et al., 2019; Sasson & Umberson, 2014), I estimated growth curve models to map trajectories of parental depressive symptoms before and after the death of a child. Within-person depressive symptoms trajectories showed, on average, whether and how child death in later life affected depressive symptoms among individual parents over time, with each parent serving as their own control. Separate models were estimated for mothers and fathers. Then, to formally test gender differences in depressive symptoms trajectories surrounding parental bereavement, I pooled mothers and fathers together in one model and introduced a series of interaction terms between parental gender and the focal child death variables. Finally, because parental adjustment to the loss of a child can vary based on parental characteristics, I conducted within-gender moderation analyses to explore heterogeneity in depressive symptoms trajectories following child death in later life. In separate models, all time-invariant and time-varying covariates were interacted with the focal child death variables to uncover significant moderating effects on the short- and long-term adjustment in depressive symptoms for bereaved mothers and fathers. The reduced-form specification for the primary growth curve models is shown below.
Within-person depressive symptoms trajectories are approximated as a linear function of time (Timeit), with each respondent (parent) i’s depressive symptoms Y changing over time t (in years). Coefficient γ 00 is the intercept, indicating depressive symptoms of person i at baseline. Coefficient γ 10 denotes the rate of change in person i’s depressive symptoms over time. Three additional covariates were added to allow trajectories of depressive symptoms to be estimated once respondents experienced the death of a child. ChildDeathit is a time-varying variable that captures the respondent i’s exposure to child death at time t, coded as 1 if the respondent experienced this loss and 0 if they did not.
If π 2i is nonsignificant, it would demonstrate that parents, on average, do not report an appreciable increase in depressive symptoms after child death. Conversely, if π 2i is positively significant, it would indicate that parents do endure an elevation in depressive symptoms immediately following the death of a child. PostDeathit indicates the number of years that had passed at time t since child death for respondent i, coded 0 in the time preceding the year in which the child was reported deceased and 2 years added for each subsequent wave. This variable captures any additional change in depressive symptoms at each time point following child death unaccounted for by normative changes in depressive symptoms associated with aging which are controlled for by Timeit. Its squared term, PostDeathit2, was included to account for nonlinear changes in depressive symptoms following child death. Given a significant elevation in depressive symptoms following child death, π 3i being negatively significant would indicate a negative postbereavement slope. In other words, a negative slope would suggest that bereaved parents’ elevated depressive symptoms generally decrease with years since bereavement net of normative aging processes. Therefore, depressive symptoms eventually would return prebereavement levels, indicating a short-term trajectory. If π 3i is positively significant or nonsignificant, it would evince the contrary. That is, elevated depressive symptoms following bereavement do not dissipate with time net of normative aging processes, suggesting that bereaved parents’ depressive symptoms follow a longer-term, or chronic trajectory.
Furthermore, xmi represents time-invariant covariates that may be associated with between-person variation in depressive symptoms intercepts, and coefficient vector γ 0m specifies the average change in the intercept across these covariates: parent’s gender, age, racially/ethnically minoritized, surviving children, education, and prior child death, all measured at baseline. xit is a vector of time-varying covariates, including partnership status, wealth, family and friends nearby, parent–child contact, chronic conditions, heavy alcohol use, smoking, and concurrent family deaths, and their coefficients are represented as π ki. Lastly, ζ 0i and ζ 1i represent the between-person variance for depressive symptoms intercepts and rates of change, respectively, and ε ij is the within-person variance.
For the first analysis, baseline descriptive statistics were calculated using baseline sample weights to adjust for the unequal probability of selection and nonresponse. For the primary growth curve and moderation analyses, I applied normalized wave-specific sample weights at Level 1 and baseline sample weights at Level 2 (Heeringa et al., 2017). Given that respondents with poorer health are more likely to drop out of longitudinal surveys or die compared with their healthier counterparts, I accounted for differential attrition and mortality by including eight wave-specific dropout indicators (1 = dropout at a given wave, 0 = remain in study) in the models (Lin et al., 2019; Muthén et al., 2011).
Results
To highlight how prebereavement contexts differed for mothers versus fathers who lost a child in later life, Table 1 shows the variation in bereaved parents’ characteristics and resources by gender. As anticipated, a greater share of mothers than fathers in the HRS experienced the death of a child (6.42% vs 4.41%, p < .001). In line with prior research, average baseline depressive symptoms were higher among bereaved mothers than fathers before the death of a child. Mothers were less likely to be partnered and also reported fewer socioeconomic resources at baseline compared with their male counterparts. While the percentage of parents reporting friends and family living nearby did not differ by gender, mothers reported being in weekly contact with a greater share of their children than fathers. In addition, mothers had a greater number of chronic conditions but were less likely to be heavy alcohol users compared with fathers. Lastly, the experience of prior child death was more often reported by mothers than fathers.
Table 1.
Weighted Means (SD) or Percentages of Bereaved Parents’ Baseline Characteristics by Gender (N = 1,869)
| Bereaved mothers | Bereaved fathers | Difference | |
|---|---|---|---|
| Dependent variable | |||
| Depressive symptoms | 2.08 (2.19) | 1.32 (1.88) | *** |
| Sociodemographic characteristics | |||
| Age | 65.94 (10.22) | 64.91 (9.67) | |
| Racially/ethnically minoritized | 29.02 | 28.08 | |
| Partnered | 51.72 | 81.31 | *** |
| Socioeconomic resources | |||
| Education (in years) | 11.32 (3.16) | 11.78 (3.34) | ** |
| Wealth (in 1998 dollars) | $18,200 | $34,000 | *** |
| Interpersonal resources | |||
| Any surviving children | 93.63 | 94.60 | |
| Friends nearby | 69.02 | 66.82 | |
| Family nearby | 34.04 | 30.69 | |
| Share of children in weekly contact | 0.70 (0.33) | 0.63 (0.35) | ** |
| Health characteristics | |||
| Chronic conditions | 1.64 (1.25) | 1.46 (1.31) | ** |
| Heavy alcohol user | 3.25 | 10.77 | *** |
| Smoker | 16.85 | 20.02 | |
| Other bereavement | |||
| Prior child death | 19.73 | 13.21 | ** |
| Concurrent family death | 22.59 | 22.53 | |
| Weighted percentage of parents in HRS | 6.42% of mothers | 4.41% of fathers | *** |
| Unweighted n | 1,207 | 662 |
Notes: Weighted percentage of parents in Health and Retirement Study (HRS) refers to the weighted percentage of mothers and fathers who experienced the death of a child during their observation in the 1998–2014 HRS, calculated prior to removing nonbereaved parents from the sample. SD = standard deviation.
**p < .01. ***p < .001.
Child Death and Depressive Symptoms Trajectories
Table 2 displays the estimates from discontinued growth curve models predicting changes in depressive symptoms for mothers and fathers separately. The first column shows estimates for mothers. Prior to a child’s death, mothers’ depressive symptoms declined slightly over time (−0.03 per year, p < .001). Once child death was reported, bereaved mothers suffered an immediate, 0.41-point increase in depressive symptoms (p < .001), followed by a curvilinear negative slope over time (p < .001), indicating an eventual recovery to prebereavement levels.
Table 2.
Coefficients From Growth Curve Models Predicting Changes in Depressive Symptoms Over Time
| Mothers | Fathers | Difference | |
|---|---|---|---|
| Focal independent variables | |||
| Time (in years) | −0.03*** | −0.02* | |
| Child death | 0.41*** | 0.21** | † |
| Time since child death | −0.15*** | −0.07* | * |
| Time since child death2 | 0.01*** | 0.01† | |
| Sociodemographic characteristics | |||
| Age (at baseline) | −0.03*** | −0.02* | |
| Racially/ethnically minoritized | −0.04 | 0.17 | |
| Partnered | −0.47*** | −0.88*** | |
| Socioeconomic resources | |||
| Education (in years) | −0.09*** | −0.08*** | |
| Wealth (logged) | −0.04*** | 0.01 | |
| Interpersonal resources | |||
| Any surviving children | −0.49† | −0.25 | |
| Friends nearby | −0.07 | −0.05 | |
| Family nearby | −0.06 | 0.08 | |
| Share of children in weekly contact | −0.05 | −0.09 | |
| Health characteristics | |||
| Chronic conditions | 0.30*** | 0.22*** | |
| Heavy alcohol user | −0.36 | 0.14 | |
| Smoker | 0.06 | 0.02 | |
| Other bereavement | |||
| Prior child death | 0.18 | −0.13 | |
| Concurrent family death | 0.23*** | 0.09 | |
| Variance components | |||
| Within-person | 1.49 | 1.20 | |
| Intercept (1) | 1.46 | 1.15 | |
| Slope (2) | 0.08 | 0.08 | |
| Covariance between (1) and (2) | −0.25 | −0.40 | |
| Intercept | 5.35*** | 3.63*** |
Notes: Eight wave-specific, dichotomous indicators were included in the models to account for attrition from the study. Difference refers to significant gender interactions with focal independent variables from pooled model (not shown).
† p < .10. *p < .05. **p < .01. ***p < .001.
Other covariates also were significantly associated with depressive symptoms for bereaved mothers. On average, mothers who were older and partnered reported fewer depressive symptoms, and socioeconomic resources were inversely related to depressive symptoms. The presence of surviving children was marginally associated with lower depressive symptom levels for mothers. Chronic conditions and experiencing the death of a parent, sibling, or spouse were associated with elevated depressive symptoms for mothers.
The second column shows estimates for bereaved fathers. Fathers’ depressive symptoms declined slightly over time leading up the death of a child (−0.02 per year, p < .05). At child death, bereaved fathers reported a significant, 0.21-point increase in depressive symptoms (p < .01) followed by a negative postbereavement slope (p < .05) with a marginal curvilinear effect (p < .10). Fathers’ characteristics were associated with depressive symptoms in similar patterns to mothers with two exceptions. Neither wealth nor the experience of another family member significantly affected bereaved fathers’ depressive symptoms net of controls.
On average, both mothers and fathers who lost a child in later life reported an acute trajectory of depressive symptoms characterized by an immediate elevation in symptoms at the death followed by a recovery over time. Significant differences in these adjustment trajectories by parental gender are presented in the final column in Table 2. The rate of change in depressive symptoms leading up to the death of a child was the same for mothers and fathers as denoted by no significant gender difference in depressive symptoms over time (p > .05). Upon reporting a child’s death, the immediate elevation in depressive symptoms was marginally greater for mothers than fathers (p < .10). However, in the years following the death, the negative depressive symptoms slope was steeper for mothers than fathers (p < .05), indicating a faster rate of recovery for mothers.
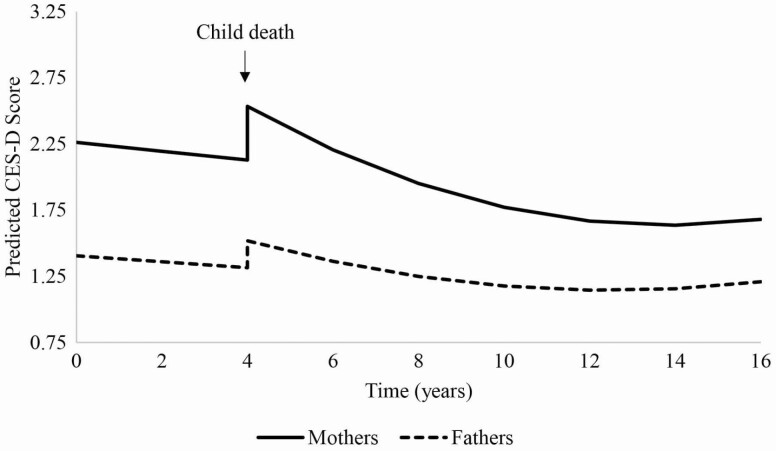
To help visualize the results presented in Table 2 and to approximate the average number of years it took for bereaved mothers and fathers to recover to prebereavement well-being, I plotted the predicted depressive symptoms trajectories for mothers and fathers in Figure 1 using Stata’s margins command, anchoring child death at Year 4 and holding control variables at their means. Both bereaved mothers and fathers reported a decline in depressive symptoms leading up to the death of a child. At child death, bereaved mothers endured a marginally greater rise in depressive symptoms than bereaved fathers. However, postbereavement decreases in depressive symptoms were steeper for bereaved mothers than fathers. On average, these counterbalancing changes in depressive symptoms resulted in both bereaved mothers and fathers returning to their respective prebereavement levels of depressive symptoms between 2 and 4 years postbereavement.
Figure 1.
Bereaved parents’ depressive symptoms trajectories, 1998–2014 Health and Retirement Study. CES-D = Center for Epidemiological Studies—Depression.
Moderation Analyses
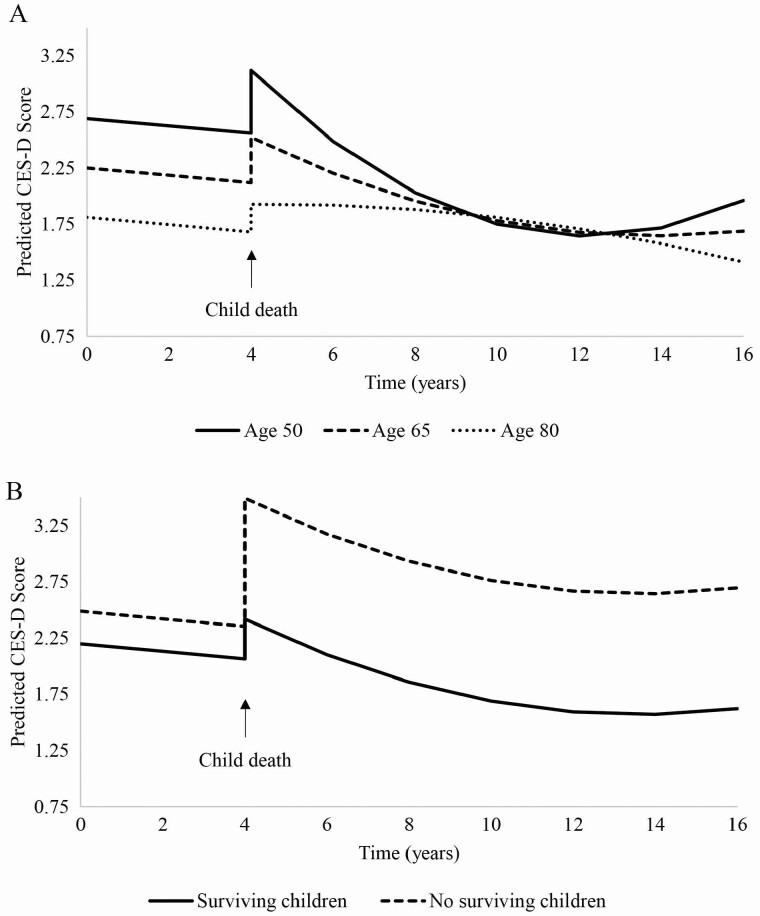
Within-gender moderation analyses were performed to uncover potential heterogeneity in depressive symptoms trajectories surrounding child death. All parental covariates were interacted with the focal child death variables in individual interaction models. Significant findings from these analyses are shown in Supplementary Table 1. Only two characteristics significantly influenced bereaved mothers’ depressive symptoms trajectories (p < .05). First, mothers’ age was associated with a slower rate of recovery after child death but did not moderate short-term elevations in depressive symptoms at child death. Figure 2, panel A shows depressive symptoms trajectories for mothers at three different baseline ages. On average, postbereavement depressive symptoms slopes flattened with increasing ages, suggesting that the older mothers were when they experienced the death of a child, the longer they took to recover to prebereavement depressive symptoms levels. Second, having surviving children considerably reduced mothers’ elevation in depressive symptoms immediately following a child’s death but was not associated with their rate of recovery thereafter. Figure 2, panel B shows depressive symptoms trajectories by whether mothers had other living children at the time of a child’s death. The presence of surviving children significantly reduced the short-term elevation in mothers’ depressive symptoms at child death. Given the comparatively greater magnitude in elevation in depressive symptoms, mothers without surviving children never fully recovered to their prebereavement levels, on average, indicating chronic elevations in depressive symptoms.
Figure 2.
Bereaved mothers’ depressive symptoms trajectories by (A) age and (B) presence of surviving children, 1998–2014 Health and Retirement Study. CES-D = Center for Epidemiological Studies—Depression.
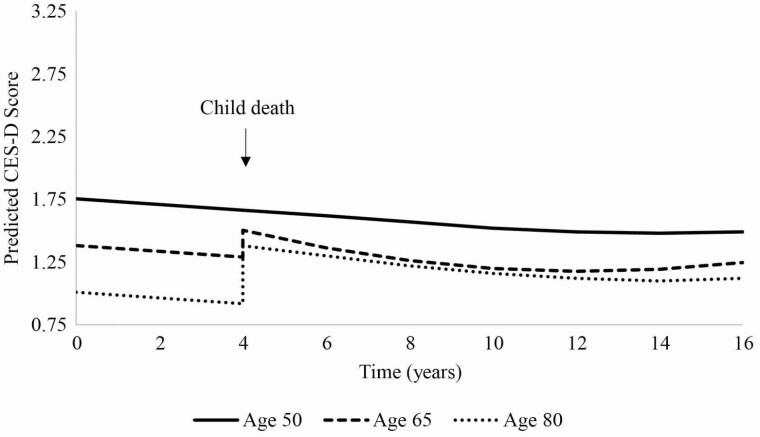
Turning to bereaved fathers, age was the only significant moderator of depressive symptoms surrounding child death (p < .05) as shown in Supplementary Table 1. Fathers’ age was associated with greater elevations in short-term depressive symptoms following the death of a child but was not associated with postbereavement slopes. Figure 3 illustrates this finding. At child death, the magnitude of elevation in fathers’ depressive symptoms grew larger with age, and the greater short-term elevations for older fathers translated to longer periods of recovery to prebereavement levels of depressive symptoms.
Figure 3.
Bereaved fathers’ depressive symptoms trajectories by age, 1998–2014 Health and Retirement Study. CES-D = Center for Epidemiological Studies—Depression.
Discussion
For the majority of parents, relationships with their children are among the most salient in their lives (Elder et al., 2003), and parents do not expect to outlive their children in the normative life course (Pearlin & Skaff, 1996). Accordingly, child death is often regarded as the most traumatic form of family bereavement (Miller & Rahe, 1997). Shifts in the timing of parenthood and gains in life expectancy suggest that parental bereavement is becoming a traumatic life event increasingly concentrated in the second half of life (Alburez-Gutierrez et al., 2021), yet how older parents psychologically adjust to the death of a child in later life is unclear.
Using nationally representative panel data from the 1998–2014 HRS, I mapped population-level trajectories of depressive symptoms before, during, and after the death of a child for mothers and fathers aged 50 and older in the United States. I also explored potential heterogeneity in adjustment trajectories across various parental characteristics. Findings suggest that, at the population level, mothers and fathers who experience the death of a child in later life endure a significant elevation in depressive symptoms at the death followed by a steady decline to prebereavement levels over the next few years. Although child death is one of the worst experiences imaginable, the immediate impact of the loss on older parents’ depressive symptoms diminishes over time, on average.
Several notable gender differences in adjustment to this traumatic event were uncovered. First, congruent with the notion of the “feminization of bereavement” in old age which is well-documented for widowhood (Williams et al., 2006), findings suggest that child death is another form of bereavement more often experienced by women than men over the age of 50 (6.42% of mothers vs 4.41% of fathers). Women’s greater survival to advanced ages likely explains most of this differential (Alburez-Gutierrez et al., 2021), but underreporting of child deaths by fathers in national surveys cannot be ruled out given the greater prevalence of father–child estrangement across the life course, especially following divorce (Blake, 2017). Second, in line with the limited research on child death in later life (Floyd et al., 2013; Maccallum et al., 2015), mothers went on to lose a child reported more depressive symptoms than their male counterparts prior to the death. Gender gaps in depressive symptoms in later life are explained, in part, by women’s greater exposure to lifetime risk factors for psychological distress compared with men (Acciai & Hardy, 2017). Yet, after controlling for chronic conditions, socioeconomic resources, partnership status, and the experience of prior child death, mothers still had significantly higher levels of depressive symptoms at baseline than fathers. Future research should attempt to parse out how other gendered pathways, such as differential exposure to cumulative life course stress or variation in intrapersonal characteristics, may explain bereaved mothers’ worse psychological well-being even prior to losing a child in later life (Floyd et al., 2013; Kiely et al., 2019).
Third, bereaved mothers endured a greater elevation in depressive symptoms at child death compared with bereaved fathers (p < .10). Although only marginally significant, this finding suggests that parental bereavement in later life is more detrimental for mothers than fathers, at least in the short term. This finding aligns with the notions that, compared with men, women’s depressive symptoms are more sensitive to stressful life events (Rosenfield & Mouzon, 2013), and child death in later life may mean the loss of a stronger, more salient parent–child relationship for mothers than fathers (Kalmijn, 2019; Ward, 2008). Fourth, bereaved mothers reported a faster decline in depressive symptoms after the loss of a child than bereaved fathers. In other words, child death exerted a more enduring relative impact on depressive symptoms for bereaved fathers than mothers. Following bereavement, women tend to confront and express their emotions, whereas men tend to hide and avoid them (Stroebe et al., 2001), and emotion-focused coping has been found to diminish stress and reduce depressed mood, especially among women (Carver & Connor-Smith, 2010; Howerton & Van Gundy, 2009). In addition, bereaved mothers in this study were more likely to experience the prior death of a child and the concurrent death of other family members, so it is possible that they developed coping strategies salient to a faster recovery from loss.
Moderation analyses uncovered heterogeneity in depressive symptoms trajectories across two significant factors: parental age and the presence of surviving children. Following the death of a child, parental age was associated with a slower long-term recovery in depressive symptoms for mothers and a higher short-term elevation in depressive symptoms for fathers. Although age did not emerge as a significant moderator in prior research, the result is not surprising given that age moderates psychological adjustment to spousal loss in a similar way (Onrust et al., 2007). Greater frailty at older ages may leave parents less equipped to adjust to the stress of child death in both the short term and long term (Pearlin & Skaff, 1996). Contemplating their own mortality, older parents also tend to report considerable difficulties coping with the loss of child, reporting feelings of survivor’s guilt alongside fears that the child will “die forever” when they themselves eventually pass away (Rubin & Malkinson, 2001).
The presence of surviving children was as a significant buffer for mothers but not fathers who lost a child in later life. Mothers with surviving children reported smaller short-term elevations in depressive symptoms after child loss than mothers without surviving children. This finding is in line with prior research examining child death earlier in the life course (Li et al., 2005; Wijngaards-de Meij et al., 2005). Engaging with surviving children is a constructive and adaptive way bereaved parents respond to child loss (Gerrish & Bailey, 2020), and this may be particularly true for mothers in later life who are beyond their childbearing years. Given the salience of the maternal role, relationships with surviving child relationships likely impart a stronger sense of purpose and meaning in life for bereaved mothers than bereaved fathers. Mothers who had no surviving children at the time of child death suffered from chronic increases in depressive symptoms after child death, on average, suggesting that childless bereaved mothers are uniquely vulnerable to prolonged psychological distress arisen from the death of a child in later life. Compared with fathers, mothers more often turn to their children for instrumental and emotional support in later life (Kalmijn, 2019). The loss of this key source of preferred support for aging mothers may help to explain the gender differential in depressive symptoms among bereaved parents without surviving children.
This study demonstrates the importance of examining trajectories of depressive symptoms surrounding parental bereavement across multiple time points separately for women and men. Both bereaved mothers and fathers reported a short-term recovery to their respective prebereavement levels of depressive symptoms between 2 and 4 years following the loss, but their trajectories were distinctive. By measuring depressive symptoms immediately following the death of a child and thereafter over time, this study uncovered differences in the immediate and protracted impacts of child death by parental gender. Bereaved mothers had greater initial elevations in depressive symptoms after child death but a faster postbereavement recovery, whereas bereaved fathers suffered smaller immediate increases in depressive symptoms with a slower decline over time. These counterbalancing changes in depressive symptoms by gender culminated in similar adjustment periods for bereaved mothers and fathers, but without multiple postbereavement time points, the nuances in their short- versus long-term processes would be blurred.
Limitations of the study should be noted. First, the HRS interviews respondents every two years. Because depressive symptoms were measured in the wave at which a child was reported deceased, bereaved parents may have begun to recover by the time they were interviewed if child death occurred early in the 2-year interview window. Furthermore, child death is selective of those with poor health and is associated with a greater risk of mortality (Donnelly et al., 2020). Older parents with the worst psychological well-being prior to and after child death may have refused to answer questions about their psychological well-being or could have died prior to responding to the survey entirely. Therefore, the elevations in depressive symptoms at child death may be conservative estimates. Second, some factors that may be associated with psychological adjustment to child death in later life, such as the cause of death and parents’ intrapersonal resources and exposure to life course trauma, are not readily available in the HRS but likely contribute to heterogeneity in depressive symptoms that was not captured in the overall trajectories presented in this study. Third, depressive symptoms are only one of many psychological dimensions of bereavement. Future research should consider how child death shapes other dimensions of health and health behaviors for mothers versus fathers, as stress may manifest distinctively based on gender (Rosenfield & Mouzon, 2013). Finally, it is possible that bereaved mothers and fathers in the sample were partnered with one another. Individual-level weighting was performed to weight the sample to noninstitutionalized individuals in the United States, but it is possible that nonindependence of depressive symptoms could occur in bereaved couple households. As a sensitivity check, I estimated all analyses using only information from parents without a partner at baseline (not shown). Results mirrored those from the whole sample of parents, suggesting that nonindependence did not appreciably shape depressive symptoms surrounding child death for mothers or fathers. Future studies should incorporate within-couple comparisons of adjustment to child death in later life.
This study advances research on parental bereavement by producing the first population-level trajectories of depressive symptoms for mothers and fathers who lose a child in later life. Findings from this study have important implications for grief counseling and support for aging parents. Mothers bear a disproportionate exposure to parental bereavement in later life and tend to suffer worse depressive outcomes in response to this life event in the short run compared with fathers. Child death may have a more enduring impact on the depressive symptoms of fathers after the death of a child, on average, underscoring the need for sustained support for these men in the years following their loss. Vulnerable subpopulations of older bereaved parents include mothers and fathers in advanced ages and mothers without other living children, all of whom are susceptible to enduring psychological distress arisen from child death in later life. This study serves as a vital basis from which future research can stem to investigate how parental bereavement experienced in later life manifests through distinct pathways to health and well-being for mothers and fathers.
Supplementary Material
Funding
This work was supported in part by the Center for Family and Demographic Research, Bowling Green State University, which has core funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (P2CHD050959).
Conflict of Interest
None declared.
Acknowledgments
Thank you to Dr. I-Fen Lin for her guidance and feedback on early versions of this paper.
References
- Acciai, F., & Hardy, M. (2017). Depression in later life: A closer look at the gender gap. Social Science Research, 68, 163–175. doi: 10.1016/j.ssresearch.2017.08.003 [DOI] [PubMed] [Google Scholar]
- Alburez-Gutierrez, D., Kolk, M., & Zagheni, E. (2021). Women’s experience of child death over the life course: A global demographic perspective. Demography, 58(5), 1715–1735. doi: 10.1215/00703370-9420770 [DOI] [PubMed] [Google Scholar]
- Blake, L. (2017). Parents and children who are estranged in adulthood: A review and discussion of the literature. Journal of Family Theory & Review, 9(4), 521–536. doi: 10.1111/jftr.12216 [DOI] [Google Scholar]
- Bolton, J. M., Au, W., Leslie, W. D., Martens, P. J., Enns, M. W., Roos, L. L., Katz, L. Y., Wilcox, H. C., Erlangsen, A., Chateau, D., Walld, R., Spiwak, R., Seguin, M., Shear, K., & Sareen, J. (2014). Parents bereaved by offspring suicide: A population-based longitudinal case-control study. JAMA Psychiatry, 70(2), 158–167. doi: 10.1001/jamapsychiatry.2013.275 [DOI] [PubMed] [Google Scholar]
- Bonanno, G. A., Moskowitz, J. T., Papa, A., & Folkman, S. (2005). Resilience to loss in bereaved spouses, bereaved parents, and bereaved gay men. Journal of Personality and Social Psychology, 88(5), 827–843. doi: 10.1037/0022-3514.88.5.827 [DOI] [PubMed] [Google Scholar]
- Cacciatore, J., Killian, M., & Harper, M. (2016). Adverse outcomes in bereaved mothers: The importance of household income and education. SSM—Population Health, 2, 117–122. doi: 10.1016/j.ssmph.2016.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver, C. S., & Connor-Smith, J. (2010). Personality and coping. Annual Review of Psychology, 61, 679–704. doi: 10.1146/annurev.psych.093008.100352 [DOI] [PubMed] [Google Scholar]
- Case, A., & Deaton, A. (2021). Deaths of despair and the future of capitalism. Princeton University Press. [Google Scholar]
- Donnelly, R., Umberson, D., Hummer, R. A., & Garcia, M. A. (2020). Race, death of a child, and mortality risk among aging parents in the United States. Social Science & Medicine, 249, 112853. doi: 10.1016/j.socscimed.2020.112853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elder, G. H., Jr., Johnson, M. K., & Crosnoe, R. (2003). The emergence and development of life course theory. In Mortimer J. T. & Shanahan M. J. (Eds.), Handbook of the life course (pp. 3–19). Kluwer Academic/Plenum Publishers. doi: 10.1007/978-0-306-48247-2_1 [DOI] [Google Scholar]
- Finnäs, F., Rostila, M., & Saarela, J. (2018). Divorce and parity progression following the death of a child: A register-based study from Finland. Population Studies, 72(1), 41–51. doi: 10.1080/00324728.2017.1337918 [DOI] [PubMed] [Google Scholar]
- Floyd, F. J., Mailick Seltzer, M., Greenberg, J. S., & Song, J. (2013). Parental bereavement during mid-to-later life: Pre- to postbereavement functioning and intrapersonal resources for coping. Psychology and Aging, 28(2), 402–413. doi: 10.1037/a0029986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerrish, N. J., & Bailey, S. (2020). Maternal grief: A qualitative investigation of mothers’ responses to the death of a child from cancer. OMEGA: Journal of Death and Dying, 81(2), 197–241. doi: 10.1177/0030222818762190 [DOI] [PubMed] [Google Scholar]
- Heeringa, S. G., West, B. T., & Berglund, P. A. (2017). Applied survey data analysis (2nd ed.). Chapman and Hall/CRC. [Google Scholar]
- Howerton, A., & Van Gundy, K. (2009). Sex differences in coping styles and implications for depressed mood. International Journal of Stress Management, 16(4), 333–350. doi: 10.1037/a0016843 [DOI] [Google Scholar]
- HRS Sample Sizes and Response Rates. (2017). Health and Retirement Study. https://hrs.isr.umich.edu/sites/default/files/biblio/ResponseRates_2017.pdf [Google Scholar]
- Infurna, F. J., & Luthar, S. S. (2017). Parents’ adjustment following the death of their child: Resilience is multidimensional and differs across outcomes examined. Journal of Research in Personality, 68, 38–53. doi: 10.1016/j.jrp.2017.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmijn, M. (2019). The effects of ageing on intergenerational support exchange: A new look at the hypothesis of flow reversal. European Journal of Population, 35(2), 263–284. doi: 10.1007/s10680-018-9472-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiely, K. M., Brady, B., & Byles, J. (2019). Gender, mental health and ageing. Maturitas, 129, 76–84. doi: 10.1016/j.maturitas.2019.09.004 [DOI] [PubMed] [Google Scholar]
- Kreicbergs, U., Valdimarsdóttir, U., Onelöv, E., Henter, J. I., & Steineck, G. (2004). Anxiety and depression in parents 4–9 years after the loss of a child owing to a malignancy: A population-based follow-up. Psychological Medicine, 34(8), 1431–1441. doi: 10.1017/s0033291704002740 [DOI] [PubMed] [Google Scholar]
- Li, J., Laursen, T. M., Precht, D. H., Olsen, J., & Mortensen, P. B. (2005). Hospitalization for mental illness among parents after the death of a child. New England Journal of Medicine, 352(12), 1190–1196. doi: 10.1056/nejmoa033160 [DOI] [PubMed] [Google Scholar]
- Lin, I. F., Brown, S. L., Wright, M. R., & Hammersmith, A. M. (2019). Depressive symptoms following later-life marital dissolution and subsequent repartnering. Journal of Health and Social Behavior, 60(2), 153–168. doi: 10.1177/0022146519839683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maccallum, F., Galatzer-Levy, I. R., & Bonanno, G. A. (2015). Trajectories of depression following spousal and child bereavement: A comparison of the heterogeneity in outcomes. Journal of Psychiatric Research, 69, 72–79. doi: 10.1016/j.jpsychires.2015.07.017 [DOI] [PubMed] [Google Scholar]
- Mellencamp, K. A. (2019). Parental bereavement in mid- to late-life: The death of a child after age 50. Family Profiles, FP-19-18. Bowling Green, OH: National Center for Family & Marriage Research. doi: 10.25035/ncfmr/fp-19-18 [DOI] [Google Scholar]
- Miller, M. A., & Rahe, R. H. (1997). Life changes scaling for the 1990s. Journal of Psychosomatic Research, 43(3), 279–292. doi: 10.1016/s0022-3999(97)00118-9 [DOI] [PubMed] [Google Scholar]
- Muthén, B., Asparouhov, T., Hunter, A. M., & Leuchter, A. F. (2011). Growth modeling with nonignorable dropout: Alternative analyses of the STAR*D antidepressant trial. Psychological Methods, 16(1), 17–33. doi: 10.1037/a0022634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ofstedal, M. B.,Weir, D. R., Chen, K.-T., & Wagner, J. (2011). Updates to HRS sample weights (HRS Report No. DR-013). University of Michigan Survey Research Center. http://hrsonline.isr.umich.edu/sitedocs/userg/dr-013.pdf [Google Scholar]
- Onrust, S., Cuijpers, P., Smit, F., & Bohlmeijer, E. (2007). Predictors of psychological adjustment after bereavement. International Psychogeriatrics, 19(5), 921–934. doi: 10.1017/S1041610206004248 [DOI] [PubMed] [Google Scholar]
- Pearlin, L. I. (1989). The sociological study of stress. Journal of Health and Social Behavior, 30(3), 241–256. doi: 10.2307/2136956 [DOI] [PubMed] [Google Scholar]
- Pearlin, L. I., & Skaff, M. M. (1996). Stress and the life course: A paradigmatic alliance. Gerontologist, 36(2), 239–247. doi: 10.1093/geront/36.2.239 [DOI] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rogers, C. H., Floyd, F. J., Seltzer, M. M., Greenberg, J., & Hong, J. (2008). Long-term effects of the death of a child on parents’ adjustment in midlife. Journal of Family Psychology, 22(2), 203–211. doi: 10.1037/0893-3200.22.2.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenfield, S., & Mouzon, D. (2013). Gender and mental health. In Aneshensel C. S., Phelan J. C., & Bierman A. (Eds.), Handbook of the sociology of mental health (pp. 277–296). Kluwer Academic/Plenum Publishers. doi: 10.1007/978-94-007-4276-5_14 [DOI] [Google Scholar]
- Rosenthal, C. J. (1985). Kinkeeping in the familial division of labor. Journal of Marriage and Family, 47(4), 965–974. doi: 10.2307/352340 [DOI] [Google Scholar]
- Rossi, A. S., & Rossi, P. H. (1990). Of human bonding: Parent–child relations across the life course. Routledge. [Google Scholar]
- Rostila, M., Mäki, N., & Martikainen, P. (2018). Does the death of a child influence parental use of psychotropic medication? A follow-up register study from Finland. PLoS One, 13(5), e0195500. doi: 10.1371/journal.pone.0195500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin, S. S., & Malkinson, R. (2001). Parental response to child loss across the life cycle: Clinical and research perspectives. In Stroebe M. S., Hansson R. O., Stroebe W., & Schut H. (Eds.), Handbook of bereavement research: Consequences, coping, and care (pp. 219–240). American Psychological Association. doi: 10.1037/10436-009 [DOI] [Google Scholar]
- Ryff, C. D., Schmutte, P. S., & Lee, Y. H. (1996). How children turn out: Implications for parental self-evaluation. In Ryff C. D. & Seltzer M. M. (Eds.), The parental experience in midlife. University of Chicago Press. [Google Scholar]
- Sasson, I., & Umberson, D. J. (2014). Widowhood and depression: New light on gender differences, selection, and psychological adjustment. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69(1), 135–145. doi: 10.1093/geronb/gbt058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seltzer, J. A., & Bianchi, S. M. (2013). Demographic change and parent–child relationships in adulthood. Annual Review of Sociology, 39, 275–290. doi: 10.1146/annurev-soc-071312-145602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein, M., Gans, D., & Yang, F. M. (2006). Intergenerational support to aging parents: The role of norms and needs. Journal of Family Issues, 27(8), 1068–1084. doi: 10.1177/0192513x06288120 [DOI] [Google Scholar]
- Song, J., Floyd, F. J., Seltzer, M. M., Greenberg, J. S., & Hong, J. (2010). Long‐term effects of child death on parents’ health‐related quality of life: A dyadic analysis. Family Relations, 59(3), 269–282. doi: 10.1111/j.1741-3729.2010.00601.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe, M., Schut, H., & Stroebe, W. (2007). Health outcomes of bereavement. The Lancet, 370(9603), 1960–1973. doi: 10.1016/s0140-6736(07)61816-9 [DOI] [PubMed] [Google Scholar]
- Stroebe, M., Stroebe, W., & Schut, H. (2001). Gender differences in adjustment to bereavement: An empirical and theoretical review. Review of General Psychology, 5(1), 62–83. doi: 10.1037/1089-2680.5.1.62 [DOI] [Google Scholar]
- Umberson, D., & Donnelly, R. (2021). The Death of a Child and Parents’ Psychological Distress in Mid to Later Life: Racial/Ethnic Differences in Exposure and Vulnerability. The Journals of Gerontology: Series B, 77(8), 1561-1570. doi: 10.1093/geronb/gbab206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson, D., Donnelly, R., Xu, M., Farina, M., & Garcia, M. A. (2020). Death of a child prior to midlife, dementia risk, and racial disparities. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(9), 1983–1995. doi: 10.1093/geronb/gbz154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson, D., Olson, J. S., Crosnoe, R., Liu, H., Pudrovska, T., & Donnelly, R. (2017). Death of family members as an overlooked source of racial disadvantage in the United States. Proceedings of the National Academy of Sciences of the United States of America, 114(5), 915–920. doi: 10.1073/pnas.1605599114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward, R. A. (2008). Multiple parent–adult child relations and well-being in middle and later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 63(4), S239–S247. doi: 10.1093/geronb/63.4.s239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, I. R., Royston, P., & Wood, A. M. (2011). Multiple imputation using chained equations: Issues and guidance for practice. Statistics in Medicine, 30(4), 377–399. doi: 10.1002/sim.4067 [DOI] [PubMed] [Google Scholar]
- Wijngaards-de Meij, L., Stroebe, M., Schut, H., Stroebe, W., van den Bout, J., van der Heijden, P., & Dijkstra, I. (2005). Couples at risk following the death of their child: Predictors of grief versus depression. Journal of Consulting and Clinical Psychology, 73(4), 617–623. doi: 10.1037/0022-006X.73.4.617 [DOI] [PubMed] [Google Scholar]
- Williams, B. R., Baker, P. S., Allman, R. M., & Roseman, J. M. (2006). The feminization of bereavement among community-dwelling older adults. Journal of Women & Aging, 18(3), 3–18. doi: 10.1300/J074v18n03_02 [DOI] [PubMed] [Google Scholar]
- Youngblut, J. M., Brooten, D., Cantwell, G. P., Del Moral, T., & Totapally, B. (2013). Parent health and functioning 13 months after infant or child NICU/PICU death. Pediatrics, 132(5), e1295–e1301. doi: 10.1542/peds.2013-1194 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.