Abstract
Objectives
Hypertension and uncontrolled high blood pressure (BP) are more prevalent among less-educated older adults than those with more schooling. However, these dichotomous indicators may fail to fully characterize educational disparities in BP, a continuous measure that predicts morbidity and mortality across much of its range. This study therefore focuses on the distribution of BP, assessing educational disparities across BP percentiles in addition to disparities in hypertension and uncontrolled BP.
Methods
Data are from the 2014–2016 Health and Retirement Study, a nationally representative survey of older U.S. adults (n = 14,498, ages 51–89). To examine associations between education, hypertension, and uncontrolled BP, I estimate linear probability models. To assess relationships between education and BP, I fit linear and unconditional quantile regression models.
Results
Less-educated older adults are not only more likely to have hypertension and uncontrolled BP than those with more schooling, they also have higher systolic BP across nearly the entire BP distribution. Educational disparities in systolic BP increase in magnitude across BP percentiles and are largest at the highest levels of BP. This pattern is observed for those with and without diagnosed hypertension, is robust to early-life confounders, and is only partially explained by socioeconomic and health-related circumstances in adulthood.
Discussion
Among older U.S. adults, the distribution of BP is compressed at lower, healthier levels for those with more education, and skewed toward the highest, most harmful levels among those with less education. Educational inequities in hypertension awareness and treatment efficacy may underlie these patterns. Implications for fundamental cause theory are discussed.
Keywords: Cardiovascular health, Education, Health disparities, Fundamental cause theory
Hypertension or high blood pressure (BP) is the number one risk factor for morbidity and mortality worldwide, elevating risk for heart disease, stroke, and other adverse cardiovascular events (Stanaway et al., 2018). Hypertension affects the majority of older U.S. adults, including 74.5% of those aged 60 and older (Ostchega et al., 2020). Although hypertension is treatable and BP can be reduced to targeted levels or “controlled” with lifestyle changes and medication, about half of hypertensive U.S. adults have uncontrolled high BP (Fryar et al., 2017; Whelton, 2015).
Prevalence of hypertension and uncontrolled BP is higher for U.S. adults of low socioeconomic status (SES), fueling SES disparities in morbidity and mortality (Dégano et al., 2017; Leng et al., 2015). In particular, the prevalence of hypertension and uncontrolled BP differ substantially by education (Gillespie & Hurvitz, 2013; Leng et al., 2015; Zacher et al., 2021). Among U.S. adults with a high school education or less, 47.0% have hypertension, compared with 38.5% of those with a college degree (Ostchega et al., 2020). While the mechanisms underlying these patterns are not fully understood, SES gradients in health, including disparities by education, are generally thought to result from unequal access to a multitude of health-supporting social, economic, cognitive, and behavioral resources (Cutler & Lleras-Muney, 2008; Link & Phelan, 1995; Zajacova & Lawrence, 2018). Early-life conditions, such as childhood SES and health, may also contribute to educational disparities in adult health (Jackson, 2009; Montez & Hayward, 2014). Whatever the causal processes underlying educational disparities in hypertension may be, characterizing these disparities is crucial for informing targeted interventions and monitoring progress toward health equity.
While the prevalence of both hypertension and uncontrolled BP is known to differ by education, less is known regarding whether and how the distribution of BP differs by education. This may be due in part to data limitations, as BP is less commonly collected in large social surveys than measures of diagnosed hypertension. It may also result from a commonly held view of health as the absence of disease versus its presence, with little in between. These barriers have lessened in recent years as large social surveys have begun to collect data on biomarkers, including BP (Harris & Schorpp, 2018). As continuous, objective, and dynamic measures of physiological function, biomarkers provide new opportunities for characterizing and studying health, such as evaluating distributions.
Characterizing the distribution of BP by education may provide valuable insights into health inequities. Increasing BP is associated with elevated risk of morbidity and mortality across much of its range, both below and above diagnostic thresholds for hypertension (Ettehad et al., 2016; Lewington et al., 2002). Disparities in the prevalence of hypertension and uncontrolled BP will therefore understate disparities in BP-related health risk if BP differences are evident among those with the same hypertension diagnostic or BP control statuses. Moreover, associations between BP and risk of morbidity and mortality vary across the BP distribution. A given increase in BP may have a larger impact on absolute risk of morbidity and mortality at BP’s higher levels than at its mean and lower levels (Flint et al., 2019; Lewington et al., 2002). Very low BP may also predict poor health (Mancia & Guido, 2014). It is therefore crucial to understand the direction and magnitude of disparities across the BP distribution, including its two extremes. In sum, the distribution of BP matters for morbidity and mortality, and variation in its shape by education cannot be discerned by examining hypertension and uncontrolled BP alone.
Examining the distribution of BP by education may also enrich theoretical perspectives on the social determinants of health, including fundamental cause theory (Link & Phelan, 1995). Fundamental cause theory posits that SES gradients in health stem from inequitable access to health-supporting resources. Consistent with this theory, studies suggest that health disparities depend on how advantageous SES-related resources are for a specific health outcome in a specific sociohistorical context, with the largest SES disparities observed when preventive methods or treatments exist, but are not universally utilized (Chang & Lauderdale, 2009; Clouston et al., 2016; Masters et al., 2015; Phelan & Link, 2005; Phelan et al., 2004). There are numerous evidence-based strategies for preventing and treating high BP, including maintaining a healthy weight, following a nutritious diet with reduced sodium and increased potassium, being physically active, limiting alcohol consumption, and, if hypertension is detected, taking medications (Carey et al., 2018). SES-related resources may support preventive behaviors and BP monitoring, and, if hypertension develops, may be used to seek out and adhere to the most efficacious treatment regimens. Ultimately, the use of SES-related resources may compress the distribution of BP to lower, healthier levels for people of high SES, whereas the BP distribution may be skewed toward the highest levels of BP among those of low SES. This hypothesis is consistent with evidence that body mass index (BMI) is compressed at lower values (Bann et al., 2020) and that mortality is compressed at older ages (Brown et al., 2012) for those of higher SES, while BMI is skewed toward higher levels and mortality is skewed toward younger ages for those of lower SES. Altogether, fundamental cause theory and prior research suggest that SES disparities in continuous health metrics that, like BP, are somewhat preventable or treatable will be largest at their least healthy levels, which SES-related resources can be deployed to avoid.
The current study characterizes differences in the distribution of BP by education in a nationally representative sample of older U.S. adults. After calculating descriptive statistics, I examine educational disparities in hypertension and uncontrolled BP. I then evaluate differences by education in the distribution of BP, using linear regression to examine educational disparities in mean BP and unconditional quantile regression (UQR) to estimate associations between education and BP’s 10th through 90th percentiles. Subsequent analyses examine patterns at very low and very high BP percentiles, assess educational disparities in BP within hypertension diagnostic and BP control statuses, and begin to explore the extent to which patterns are confounded by early-life factors or explained by socioeconomic circumstances and health-related risk factors in adulthood. Finally, sensitivity analyses evaluate the robustness of results to alternative measures of BP and education and to selective mortality.
Method
Data and Sample
Data are from the Health and Retirement Study (HRS), a biennial panel survey of older U.S. adults that is funded by the National Institute on Aging (grant U01AG009740) and conducted by the University of Michigan (Health and Retirement Study, 2019; RAND, 2019; Sonnega et al., 2014). The HRS began in 1992 and since 1998 has been nationally representative of the U.S. population aged 51 and older. To maintain its national representation of this age group, the HRS employs a steady-state design, replenishing the sample every 6 years with younger cohorts.
HRS personnel have collected BP and other physical measurements as part of enhanced face-to-face interviews since 2006 (Crimmins et al., 2008). Half of HRS households is eligible for enhanced face-to-face interviews each wave, and the other half is eligible in the following wave, such that physical measurements may be recorded every other wave. Physical measurements are not collected from those responding by proxy, residing in nursing homes, or interviewing by telephone.
Eligibility for the current study is limited to respondents who were invited to provide physical measurements in 2014 or 2016 and were aged 51–89 at the time (n = 16,103). Using listwise deletion, I drop 1,201 respondents (7.5%) with missing BP measures, 103 (0.6%) with missing information on hypertension diagnosis or treatment, and 301 (1.9%) with missing weighting variables, education, age, sex/gender, or race/ethnicity. The final analytic sample includes 14,498 respondents.
Measures
BP and related outcomes
BP was measured in millimeters of mercury (mmHg) three times at 45-s intervals by trained HRS personnel (Crimmins et al., 2008). To reduce error, I take the average of the three measurements. Main analyses focus on systolic BP, which is more strongly linked to morbidity and mortality than diastolic BP (Flint et al., 2019). I evaluate patterns for diastolic BP in sensitivity analyses.
I also consider three binary (1 = yes; 0 = no) measures of hypertension: diagnosed hypertension; measured hypertension; and diagnosed or measured hypertension. Diagnosed hypertension was assessed in each survey wave with a question asking, “Has a doctor ever told you that you have high blood pressure or hypertension?” Affirmative responses were carried through to subsequent waves. I determine measured hypertension status by comparing respondents’ BP to the recommended diagnostic threshold in 2014–2016 (Chobanian et al., 2003), coding those with a systolic BP of 140 mmHg or higher or a diastolic BP of 90 mmHg or higher as having measured hypertension. The third measure indicates that the respondent had either diagnosed or measured hypertension versus neither.
Finally, I create binary (1 = yes; 0 = no) measures of untreated BP and uncontrolled BP. Untreated BP is assessed in each survey wave by asking, “In order to lower your blood pressure, are you now taking any medication?” Those responding “No” are coded as having untreated BP. Uncontrolled BP is defined as having measured hypertension (i.e., BP 140/90 mmHg or higher). Analyses of untreated BP are restricted to respondents with diagnosed hypertension, and analyses of uncontrolled BP are restricted to those with diagnosed, treated hypertension.
Education
I measure education with highest degree attained in four categories: less than high school (the reference); high school or GED; associate’s or some college; and bachelor’s or higher. Sensitivity analyses draw on years of schooling as an alternative measure of education, expressed as a continuous variable ranging from 8 or fewer years to 17 years or more.
Covariates
To disentangle educational disparities in BP-related outcomes from disparities across other demographic characteristics, all regression analyses adjust for a small set of covariates. These include linear and squared terms for age, self-reported sex/gender (female; male), and self-reported race/ethnicity (non-Hispanic White; non-Hispanic Black; Hispanic; and Other). Each of these characteristics is known to be associated with both education and hypertension (Whelton, 2015).
Some analyses include additional covariates. Measures of potential early-life confounders include perceived childhood SES (poor; about average; pretty well off financially), maternal education (up to 8 years; 9–11 years; 12 years; more than 12 years; unknown), childhood health (poor/fair; good; very good; excellent), and region of birth (Northeast; Midwest; South; West; Outside the United States). Measures of socioeconomic circumstances and health-related risk factors in adulthood include marital status (married/partnered; divorced/separated; widowed; never married), total wealth quintile, BMI from measured height and weight where available (94.5%) or self-reports, frequency of vigorous physical activity (never; monthly or weekly; more than once per week), number of alcoholic drinks per week, smoking history (never smoked; formerly smoked; currently smokes), three binary diagnosis variables (ever diagnosed with diabetes, heart disease, stroke), health insurance type (private; public; none), and number of doctor visits in the past 2 years (0; 1–5; 6–11; 12–23; 24 or more).
Analysis
I begin by calculating descriptive statistics. I then estimate linear probability models of diagnosed or measured hypertension and uncontrolled BP on education, adjusting for demographic covariates including age, age-squared, sex/gender, and race/ethnicity. Next, I characterize demographics-adjusted differences in the distribution of BP by education, estimating associations between education and mean systolic BP using ordinary least squares (OLS) linear regression, and assessing relationships between education and the 10th, 25th, 50th, 75th, and 90th percentiles of systolic BP using UQR.
UQR models are designed to estimate associations between independent variables and unconditional distributional statistics of the dependent variable, such as quantiles (Firpo et al., 2009; Killewald & Bearak, 2014; Rios-Avila, 2020). UQR models are estimated in two steps. First, the dependent variable is transformed for the distributional statistic of interest—here, a particular quantile of systolic BP—using Equation 1, which estimates the recentered influence function (RIF). In the current study, is the value of systolic BP at quantile ; is the cumulative distribution function of systolic BP; is a function that equals 1 if systolic BP is less than or equal to and 0 otherwise; and is the density of systolic BP at . The second step in the estimation of a UQR model is to fit a linear OLS regression model with the estimated RIF as the dependent variable. The statistical package used to estimate UQR models for the current study carries out both steps, transforming the dependent variable and estimating an OLS regression model of the resulting RIF (Rios-Avila, 2020).
| (1) |
After examining patterns by education at the mean and 10th through 90th percentiles of systolic BP, I assess patterns at very low and very high levels of BP, specifically its 1st through 5th and 95th through 99th percentiles. Then, I examine whether relationships between education and systolic BP differ by hypertension diagnostic and BP control statuses by fitting stratified OLS and UQR models. Finally, in OLS and UQR models of systolic BP that incorporate additional sets of covariates, I examine the extent to which patterns by education are confounded by early-life factors or explained by adult socioeconomic circumstances and health-related risk factors. These analyses are restricted to the 13,965 respondents with full covariate data.
I also reestimate the main OLS and UQR models for three sets of sensitivity analyses. First, I examine whether patterns observed for systolic BP extend to diastolic BP. Second, I assess patterns when measuring education with years of schooling rather than highest degree attained. Third, to gauge the impact of selective mortality, I estimate models of systolic BP restricted to those aged 51–69.
In all analyses, two-sided p values below .05 are considered statistically significant. To ensure that the sample is nationally representative of older U.S. adults, I apply HRS-provided wave-specific, respondent-level weights for the physical measurement subsample throughout. Standard errors account for complex survey design and clustering with HRS-provided primary sampling unit and strata variables. Analyses are conducted in Stata 16.0 (StataCorp, 2019).
Results
Descriptive Statistics
Table 1 presents weighted descriptive statistics for variables in the main analysis. Additional descriptive statistics are provided in Supplementary Table 1. Respondents are, on average, 65.3 years old (standard deviation [SD] = 9.2) and 53.1% are female. Three in four (75.4%) identify as non-Hispanic White, 10.3% non-Hispanic Black, 9.7% Hispanic, and 4.6% another race/ethnicity. About 12.2% did not complete high school, 31.4% completed high school or earned a GED, 26.8% have an associate’s or some college education, and 29.6% have a bachelor’s or higher.
Table 1.
Weighted Descriptive Statistics
| Overall | By education | ||||
|---|---|---|---|---|---|
| Mean (SD) or % | Less than high school | High school or GED | Associate’s or some college | Bachelor’s or higher | |
| Systolic BP, mmHg | 127.80 (18.97) | 132.58 (24.40) | 129.35 (20.06) | 126.91 (18.03) | 125.01 (15.85) |
| Systolic BP percentiles, mmHg | |||||
| 10th percentile | 105.33 | 109.00 | 106.00 | 104.67 | 104.33 |
| 25th percentile | 114.67 | 118.00 | 116.00 | 114.33 | 112.67 |
| 50th percentile | 126.33 | 130.33 | 127.67 | 126.00 | 123.67 |
| 75th percentile | 138.67 | 145.33 | 140.33 | 137.67 | 136.00 |
| 90th percentile | 152.33 | 160.33 | 154.00 | 150.67 | 147.67 |
| Diastolic BP, mmHg | 78.57 (11.15) | 78.69 (13.96) | 78.79 (11.80) | 79.06 (11.01) | 77.84 (9.36) |
| Diagnosed hypertension | 56.18 | 68.19 | 61.51 | 55.73 | 46.00 |
| Measured hypertension | 27.36 | 34.62 | 29.65 | 26.47 | 22.74 |
| Diagnosed or measured hypertension | 64.16 | 75.73 | 69.73 | 63.77 | 53.84 |
| Untreated BP, among N = 8,917 with diagnosed hypertension | 12.50 | 12.41 | 11.03 | 14.39 | 12.58 |
| Uncontrolled BP, among N = 7,911 with diagnosed, treated hypertension | 33.19 | 38.64 | 33.62 | 31.76 | 30.78 |
| Education | |||||
| Less than high school | 12.19 | — | — | — | — |
| High school or GED | 31.36 | — | — | — | — |
| Associate’s or some college | 26.82 | — | — | — | — |
| Bachelor’s or higher | 29.62 | — | — | — | — |
| Age | 65.32 (9.21) | 67.68 (11.86) | 66.18 (9.83) | 64.17 (8.55) | 64.47 (7.76) |
| Female | 53.11 | 54.07 | 54.92 | 54.65 | 49.40 |
| Race/ethnicity | |||||
| Non-Hispanic White | 75.41 | 43.42 | 77.52 | 77.54 | 84.42 |
| Non-Hispanic Black | 10.27 | 18.12 | 10.61 | 10.94 | 6.07 |
| Hispanic | 9.69 | 33.76 | 8.41 | 7.13 | 3.47 |
| Other | 4.62 | 4.70 | 3.47 | 4.39 | 6.04 |
Notes: N = 14,498 unless stated otherwise. BP = blood pressure, measured in millimeters of mercury (mmHg); SD = standard deviation.
More than half of respondents (56.2%) have diagnosed hypertension, 27.4% have measured hypertension, and 64.2% have either diagnosed or measured hypertension. Among those with diagnosed hypertension, 12.5% are untreated while the large majority (87.5%) are currently taking BP-lowering medications. Among those diagnosed with hypertension and on treatment, 33.2% have uncontrolled BP. Mean systolic and diastolic BP are 127.8 (SD = 19.0) and 78.6 (SD = 11.2) mmHg, respectively, below diagnostic thresholds for hypertension when respondents were surveyed (140/90 mmHg; Chobanian et al., 2003), but approaching current guidelines (130/80 mmHg; Whelton et al., 2018).
Hypertension is dramatically more prevalent among respondents with less education. For example, the percentage with diagnosed or measured hypertension among those who did not complete high school (75.7%) is more than 20 points higher than that among college graduates (53.8%). Among those with diagnosed hypertension, the percentage who are untreated is similar across levels of education. However, among those diagnosed and on treatment, the percentage with uncontrolled BP is higher for the less-educated, reaching 38.6% among those who did not finish high school versus 30.8% of college graduates.
Mean systolic BP is highest among those who did not complete high school (132.6, SD = 24.4) and lowest among college graduates (125.0, SD = 15.9). Differences in the 10th through 90th percentiles of BP by education reveal three additional patterns. First, all evaluated percentiles of systolic BP are higher for the less-educated, such that the entire BP distribution is shifted upwards relative to those with more schooling. Second, the distribution of systolic BP is wider for those with less schooling, with 51.3 mmHg between the 10th (109.0) and 90th (160.3) percentiles of BP in the least-educated group, versus 43.3 mmHg (10th percentile: 104.3; 90th percentile: 147.7) in the most-educated group. Third, the distribution of systolic BP demonstrates a stronger positive skew for those with less schooling, with the largest educational disparity observed at BP’s 90th percentile. The difference between the least- and most-educated groups in the 10th percentile of systolic BP is just 4.7 mmHg, whereas the difference in the 50th percentile is 6.7, and the difference in the 90th is 12.7. In sum, the distribution of systolic BP among older U.S. adults is shifted upwards, more dispersed, and skewed toward the highest levels for those with less schooling, while it is compressed at lower, healthier levels for those with more schooling. Kernel density plots of systolic BP by education are presented in Supplementary Figure 1.
Demographics-Adjusted Associations Between Education and BP-Related Outcomes
Results from linear probability models of diagnosed or measured hypertension and uncontrolled BP in Table 2 demonstrate significant inverse associations with education when adjusting for demographic covariates. The adjusted probability of hypertension is 15.9 percentage points lower for those with a bachelor’s or higher compared to those who did not complete high school. Similarly, among diagnosed and treated hypertensive adults, the adjusted probability of uncontrolled BP is 7.1 percentage points lower for those with a bachelor’s or higher relative those with less than a high school education.
Table 2.
Coefficients and Standard Errors From Linear Probability Models of Diagnosed or Measured Hypertension and Uncontrolled BP
| Diagnosed or measured hypertension | Uncontrolled BP | |
|---|---|---|
| Education | ||
| Less than high school | Ref. | Ref. |
| High school or GED | −0.021 (0.016) | −0.043 (0.021)* |
| Associate’s or some college | −0.062 (0.018)** | −0.061 (0.024)* |
| Bachelor’s or higher | −0.159 (0.016)*** | −0.071 (0.025)** |
| Age | 0.016 (0.002)*** | −0.010 (0.003)** |
| Age-squared | −0.000 (0.000)** | 0.000 (0.000)*** |
| Female | −0.070 (0.010)*** | −0.053 (0.012)*** |
| Race/ethnicity | ||
| Non-Hispanic White | Ref. | Ref. |
| Non-Hispanic Black | 0.203 (0.011)*** | 0.081 (0.018)*** |
| Hispanic | 0.036 (0.020) | −0.013 (0.020) |
| Other | 0.042 (0.023) | 0.124 (0.034)*** |
| Constant | 0.544 (0.025)*** | 0.443 (0.034)*** |
| N | 14,498 | 7,911 |
Notes: Standard errors in parentheses. Age is centered at 51 years. Uncontrolled BP is evaluated among those with diagnosed, treated hypertension. BP = blood pressure; Ref = reference.
Two-sided significance tests: ***P < .001. **P < .01. *P < .05.
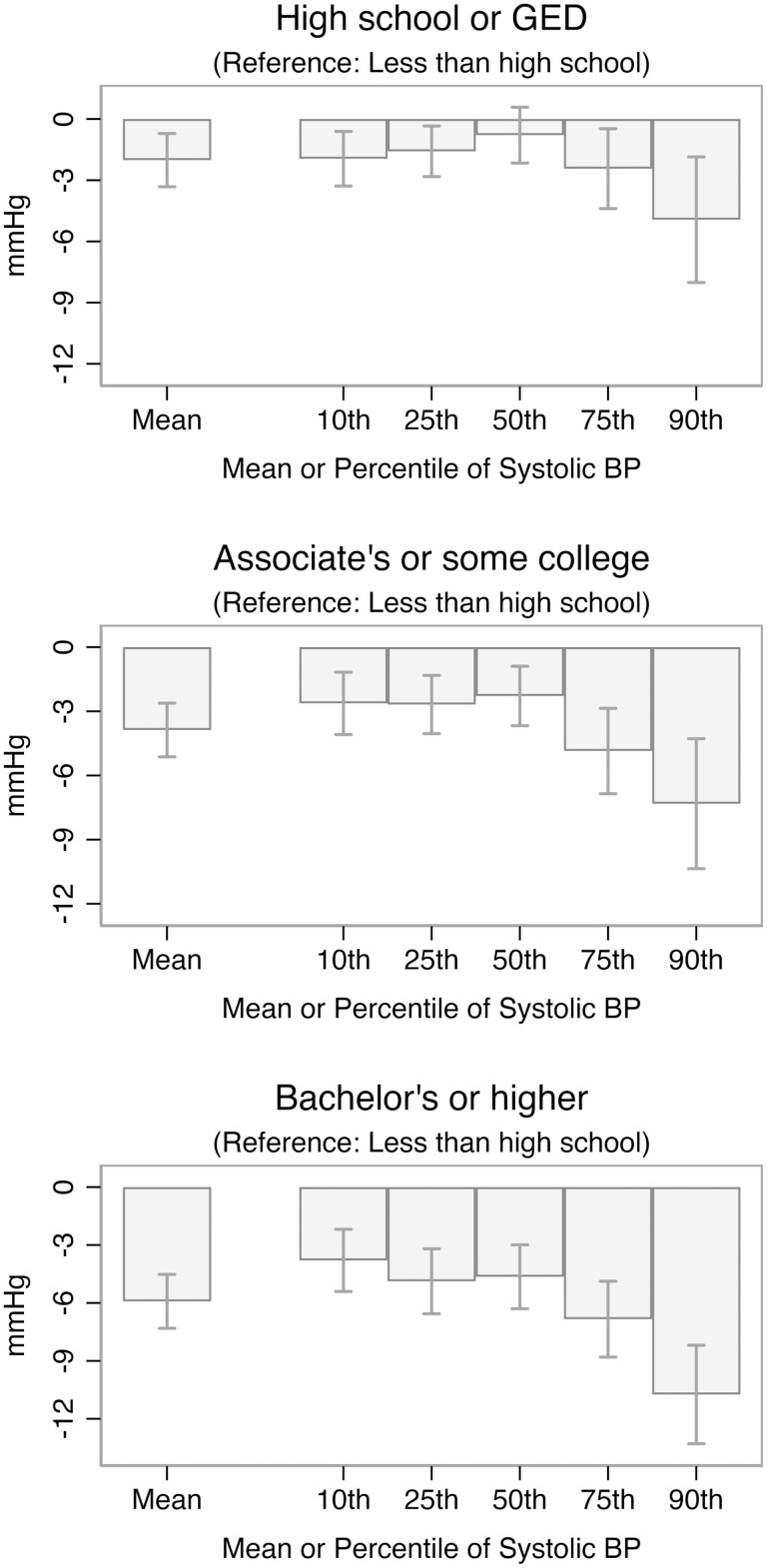
Table 3 and Figure 1 present results from demographics-adjusted OLS and UQR models of systolic BP’s mean and 10th through 90th percentiles on education. There are significant inverse associations between education and systolic BP at all evaluated points in the BP distribution, and the magnitude of this association increases across percentiles. For example, mean systolic BP is estimated to differ between the least- and most-educated groups by 5.9 mmHg, and the 10th, 25th, 50th, 75th, and 90th percentiles of systolic BP are estimated to differ between the least- and most-educated groups by 3.8, 4.9, 4.6, 6.8, and 10.7 mmHg, respectively. The estimated difference between the least- and most-educated groups in the 90th percentile of systolic BP is significantly larger in magnitude than the estimated difference at any lower percentile (all p < .05). Relatedly, the estimated relationship between each level of education, relative to less than high school, and the 90th percentile of systolic BP is significantly larger in magnitude than its estimated relationship with mean systolic BP (all p < .05). Again, results are indicative of a differential compression process, whereby the distribution of systolic BP is compressed at lower, healthier levels for more educated older adults, while it is shifted upwards and more dispersed with a stronger positive skew toward the highest, most harmful levels among those with less education.
Table 3.
Coefficients and Standard Errors From OLS Linear Regression and UQR Models of Systolic BP
| OLS | UQR | |||||
|---|---|---|---|---|---|---|
| Mean | 10th percentile | 25th percentile | 50th percentile | 75th percentile | 90th percentile | |
| Education | ||||||
| Less than high school | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| High school or GED | −2.02 (0.66)** | −1.95 (0.67)** | −1.58 (0.62)* | −0.79 (0.69) | −2.43 (0.98)* | −4.93 (1.55)** |
| Associate’s or some college | −3.87 (0.63)*** | −2.63 (0.73)** | −2.68 (0.69)*** | −2.28 (0.70)** | −4.86 (1.00)*** | −7.32 (1.53)*** |
| Bachelor’s or higher | −5.92 (0.70)*** | −3.80 (0.81) *** | −4.88 (0.84)*** | −4.64 (0.83)*** | −6.84 (0.99)*** | −10.74 (1.28)*** |
| Age | 0.34 (0.07)*** | 0.50 (0.11)*** | 0.42 (0.10)*** | 0.39 (0.09)*** | 0.36 (0.10)*** | 0.17 (0.17) |
| Age-squared | −0.00 (0.00) | −0.01 (0.00)** | −0.01 (0.00) | −0.00 (0.00) | 0.00 (0.00) | 0.01 (0.00) |
| Female | −5.92 (0.33)*** | −6.91 (0.54)*** | −6.94 (0.45)*** | −6.39 (0.39)*** | −6.06 (0.51)*** | −3.57 (0.83)*** |
| Race/ethnicity | ||||||
| Non-Hispanic White | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| Non-Hispanic Black | 5.28 (0.63)*** | 3.14 (0.66)*** | 3.61 (0.63)*** | 3.93 (0.74)*** | 6.89 (1.00)*** | 9.52 (1.31)*** |
| Hispanic | 1.14 (0.59) | −0.21 (0.90) | 0.80 (0.65) | 0.71 (0.62) | 1.17 (0.79) | 2.71 (1.46) |
| Other | 1.96 (0.97)* | −0.64 (1.67) | 1.11 (1.08) | 1.97 (1.00) | 3.08 (1.39)* | 4.97 (1.98)* |
| Constant | 129.04 (0.81)*** | 106.83 (0.95)*** | 116.20 (1.04)*** | 126.70 (1.14)*** | 139.85 (1.16)*** | 154.67 (1.98)*** |
| Systolic BP at percentile | 105.33 | 114.67 | 126.33 | 138.67 | 152.33 | |
Notes: N = 14,498. Standard errors in parentheses. Age is centered at 51 years. BP = blood pressure, measured in millimeters of mercury (mmHg); OLS = ordinary least squares; Ref = reference; UQR = unconditional quantile regression.
Two-sided significance tests: ***P < .001. **P < .01. *P < .05.
Figure 1.
Estimated associations between education (reference: less than high school) and systolic BP. Figure shows estimated coefficients and 95% confidence intervals on education variables (reference: less than high school) from OLS and UQR models of systolic BP that include age, age-squared, sex/gender, and race/ethnicity as covariates. Full numeric results are provided in Table 3. BP = blood pressure, measured in millimeters of mercury (mmHg); OLS = ordinary least squares; UQR = unconditional quantile regression.
Patterns at Very Low and Very High BP Percentiles
Supplementary Table 2 presents results from UQR models of systolic BP’s 1st through 5th percentiles. Significant inverse associations between education and systolic BP emerge at the 3rd percentile. As shown in Supplementary Table 3, there are also significant inverse associations between education and the 95th through 99th percentiles of systolic BP, similar to or larger in magnitude than those estimated at the 90th percentile.
Patterns by Hypertension Diagnostic and BP Control Statuses
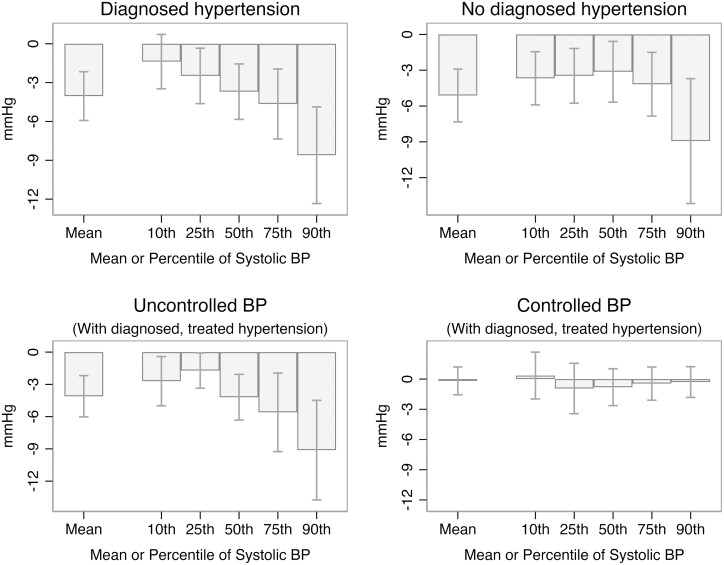
Figure 2 presents select results from stratified OLS and UQR models of systolic BP, with panels showing associations estimated for bachelor’s or higher, relative to less than high school, within subsamples defined by hypertension diagnostic and BP control statuses. Full numeric results are presented in Supplementary Tables 4 through 7. Both for those with and without diagnosed hypertension, there is a significant inverse relationship between education and systolic BP that increases in magnitude across the BP distribution, likely reflecting educational disparities in the prevalence of uncontrolled BP and undiagnosed hypertension. A similar pattern is observed among diagnosed, treated hypertensive adults with uncontrolled BP, signifying variation by education in the severity of uncontrolled BP. In contrast, among diagnosed, treated hypertensive adults with controlled BP, there are virtually no educational disparities in systolic BP at any point in the BP distribution.
Figure 2.
Estimated associations between bachelor’s or higher (reference: less than high school) and systolic BP, stratified by hypertension diagnostic and BP control statuses. Figure shows estimated coefficients and 95% confidence intervals on bachelor’s or higher (reference: less than high school) from stratified OLS and UQR models of systolic BP that include age, age-squared, sex/gender, and race/ethnicity as covariates. Full numeric results are provided in Supplementary Tables 4–7. BP = blood pressure, measured in millimeters of mercury (mmHg); OLS = ordinary least squares; UQR = unconditional quantile regression.
Adjusting for Potential Early-Life Confounders and Adult Socioeconomic and Health-Related Covariates
Supplementary Table 8 presents results from OLS and UQR models of systolic BP that incorporate potential early-life confounders as covariates. While estimated associations between education and systolic BP are occasionally reduced in magnitude relative to those estimated in models adjusting for basic demographic covariates only, no education coefficient is reduced by more than 15%. Furthermore, estimated associations between education and systolic BP remain significant at all points in the BP distribution, and continue to be largest in magnitude at the 90th percentile of systolic BP. Results suggest that measured early-life factors play a limited role in the differential distribution of systolic BP by education.
Results from models incorporating covariates reflecting socioeconomic circumstances and health-related risk factors in adulthood are presented in Supplementary Table 9. Education remains significantly inversely associated with systolic BP at all points in the BP distribution, and the magnitude of these associations remains largest at BP’s 90th percentile. However, associations between education and higher percentiles of systolic BP are reduced substantially compared to those estimated in models adjusting for demographics and early-life confounders only. Estimated associations between education and mean systolic BP are reduced by approximately one-quarter and those between education and systolic BP’s 75th and 90th percentiles are reduced by about one-third, whereas associations at lower BP percentiles are reduced by less than 10%. These findings implicate socioeconomic and health-related mechanisms in the shaping of the systolic BP distribution by education, including the extended tail toward the highest BP levels among the less-educated and its absence among those with more schooling.
Sensitivity Analyses
All three sets of sensitivity analyses reveal patterns that are consistent with the main results. First, analyses of diastolic BP return similar, albeit weaker, patterns as those observed for systolic BP (Supplementary Table 10). Second, consistent with results for highest degree attained, the estimated relationship between years of schooling and systolic BP is significant at all evaluated points in the BP distribution and increases in magnitude across BP percentiles (Supplementary Table 11). Third, results from analyses restricted to those aged 51–69 are substantively the same as those for the full sample, suggesting that selective mortality does not explain the study’s findings (Supplementary Table 12).
Discussion
In a nationally representative sample of older U.S. adults, I find that those with less education are more likely to experience hypertension and uncontrolled BP than those with more schooling, consistent with prior work (Gillespie & Hurvitz, 2013; Ostchega et al., 2020; Zacher et al., 2021). Weighted descriptive statistics indicate that 75.7% of older adults who did not complete high school have either diagnosed or measured hypertension compared with 53.8% of college graduates. Among the diagnosed, use of BP-lowering medication is widespread across education levels, with less than 15% untreated. However, uncontrolled BP remains common among those on treatment and varies by education, affecting 38.6% of those without a high school education versus 30.8% of college graduates. While educational disparities in these dichotomous measures are striking, this study builds on prior research by also documenting differences in the shape of the BP distribution by education, differences with meaningful consequences for morbidity and mortality and with implications for theoretical perspectives on the social determinants of health. Four findings warrant mention.
First, those with less education have significantly higher systolic BP than those with more schooling across nearly the entire range of BP, such that the distribution of systolic BP is shifted upwards toward higher, more harmful levels among those with less schooling. Significant disparities between the least- and most-educated groups emerge at the 3rd percentile of systolic BP and persist through the 99th. This is important because increasing BP elevates risk of morbidity and mortality both below and above diagnostic thresholds for hypertension (Ettehad et al., 2016; Lewington et al., 2002).
Second, the distribution of systolic BP is more dispersed and positively skewed among those with less education, with educational disparities increasing in magnitude across BP percentiles. The estimated difference in systolic BP between those with a bachelor’s or higher relative to those who did not complete high school, adjusting for demographic covariates, increases in magnitude from 3.8 mmHg at BP’s 10th percentile to 5.9 at its mean and 10.7 at its 90th percentile. This is cause for concern, as disparities may matter more for absolute risk of morbidity and mortality at higher levels of BP (Flint et al., 2019; Lewington et al., 2002).
Third, stratified models demonstrate that patterns observed in the full sample—higher systolic BP among the less-educated, with educational disparities increasing in magnitude across BP percentiles—are present for those with and without diagnosed hypertension and among diagnosed, treated hypertensive adults with uncontrolled BP. Among those diagnosed with hypertension, this pattern partially reflects differential progress toward BP control by education. Patterns for those without a hypertension diagnosis, on the other hand, likely reflect differential prevalence of undiagnosed hypertension by education, as well as educational disparities in BP among those with undiagnosed hypertension. This is consistent with prior work showing that undiagnosed hypertension is more common among those with less education (Zacher et al., 2021), precluding the use of BP-lowering medications for many who could benefit. For hypertensive adults with uncontrolled BP, results suggest that the extent to which BP is uncontrolled is more severe among the less-educated, perhaps due to differences in treatment assignment or adherence. Importantly, among hypertensive adults with controlled BP, there are virtually no educational disparities in systolic BP at any point in the BP distribution. Thus, when hypertension is clinically recognized and BP control is achieved, educational disparities are eliminated across the BP continuum. Reducing educational disparities in BP-related health risk will likely require expanding access to and utilization of routine preventive healthcare, where hypertension can be diagnosed and treatment plans formulated and revised as needed (Carey et al., 2018).
Finally, while this study does not identify the mechanisms responsible for the inverse relationship between education and BP, suggestive evidence can be discerned from models incorporating covariates reflecting potential early-life confounders and adult socioeconomic and health-related factors. Results do not change substantively when incorporating measures of childhood SES and health as covariates, suggesting that early-life factors play at most a limited role in shaping differences in the distribution of systolic BP by education. Adjusting for measures reflecting socioeconomic circumstances and health-related risk factors in adulthood also does not eliminate the robust relationship between education and systolic BP, although these measures do partially explain patterns at high BP percentiles. This suggests they may underlie the extended positive skew of the systolic BP distribution among the less-educated and the more compressed distribution among those with more schooling.
These findings are consistent with fundamental cause theory, which posits that SES gradients in health exist because those of higher SES can draw on their larger collection of resources to promote health through a variety of mechanisms (Link & Phelan, 1995). Another central tenet of fundamental cause theory is that SES is most strongly associated with health outcomes when preventive methods or treatments exist, but uptake of such methods or treatments is not yet universal, as it is in these cases that SES-related resources are most advantageous for health promotion (Chang & Lauderdale, 2009; Clouston et al., 2016; Masters et al., 2015; Phelan & Link, 2005; Phelan et al., 2004). This logic implies that SES disparities in continuous health metrics that, like BP, are affected by individual behavior (i.e., preventable) and modifiable with behavior change or medication (i.e., treatable) will be largest at the least healthy levels. SES-related resources may be deployed to support BP-lowering behaviors, such as maintaining a healthy weight and diet, engaging in physical activity, and reducing alcohol consumption (Carey et al., 2018). Resources may also promote access to and utilization of quality health care, facilitating earlier hypertension diagnosis and treatment initiation. Similarly, if hypertension is detected, SES-related resources may influence recommended treatments, adherence to recommendations, and how often treatment plans are revisited and refined. Ultimately, fundamental cause theory predicts precisely those patterns observed in the current study. Education-related resources can preclude the worst levels of BP from occurring, compressing the distribution of BP to lower, healthier levels for those with higher education, and leaving an extended positive skew toward the highest levels of BP among those with less schooling. Similar compression patterns by SES have been observed in prior work on the distribution of BMI (Bann et al., 2020) and longevity (Brown et al., 2012).
This study has several limitations. While I define measured hypertension and uncontrolled BP using BP measurements from a single HRS interview, clinical guidelines recommend multiple office visits to diagnose hypertension and to establish whether BP is controlled (Chobanian et al., 2003). That said, estimates of hypertension prevalence from the HRS are comparable to those from the National Health and Nutrition Examination Study, a major resource for monitoring hypertension in the United States (Fryar et al., 2017; Whelton, 2015).
Also, the current study is restricted to middle-aged and older U.S. adults. Selective mortality may affect results, possibly reducing estimated disparities in BP-related outcomes by education. However, results from sensitivity analyses limited to respondents aged 51–69 are consistent with those of the main analysis. Also, by characterizing the distribution of BP—a major risk factor for morbidity and mortality (Stanaway et al., 2018)—among middle-aged and older adults, this study generates important insights for anticipating future population health patterns. While BP-related outcomes have improved in recent decades (Whelton, 2015), high BP remains prevalent among middle-aged and older U.S. adults, and the most worrying levels of BP continue to be observed most often among those with less education. These findings are concerning in light of mounting evidence that U.S. midlife mortality is rising, that reductions in cardiovascular disease mortality have stalled, and that educational disparities in health are growing (Case & Deaton, 2021; Mehta et al., 2020).
Among this study’s strengths is its use of a biomarker—a continuous, objective, and dynamic measure of physiological function—to characterize differences by education in the distribution of a key health metric in a nationally representative sample of older U.S. adults. Results demonstrate that educational disparities in BP are pervasive across the BP distribution and are largest at its highest percentiles. As a result, the distribution of BP is shifted upwards, more dispersed, and skewed toward the highest, most harmful levels for those with less education, while it is compressed at lower, healthier levels for those with more schooling. Similar patterns may be found for other health outcomes that are amenable to prevention or treatment (e.g., blood sugar), and for other sociodemographic characteristics associated with access to health-supporting resources (e.g., race/ethnicity). To reduce educational disparities in BP and related morbidity and mortality among older U.S. adults, interventions are needed to enhance hypertension awareness and to promote progress toward BP control, as well as to support broad, sustained, and universal access to health-supporting resources more generally.
Supplementary Material
Acknowledgments
The author thanks Jason Beckfield, Alexandra Killewald, Susan Short, and Mary Waters for their feedback on early iterations of this work. The author is also grateful to attendees of the 2021 meetings of the Population Association of America for their insightful questions and comments.
Funding
This work was supported by the Population Studies and Training Center at Brown University, which receives funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health (grant number P2C HD041020). M. Zacher was supported by the National Institute on Aging of the National Institutes of Health (grant number K01AG078435). The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institutes of Health.
Conflict of Interest
None.
References
- Bann, D., Fitzsimons, E., & Johnson, W. (2020). Determinants of the population health distribution: An illustration examining body mass index. International Journal of Epidemiology, 49(3), 731–737. doi: 10.1093/ije/dyz245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, D. C., Hayward, M. D., Montez, J. K., Hummer, R. A., Chiu, C.-T., & Hidajat, M. M. (2012). The significance of education for mortality compression in the United States. Demography, 49(3), 819–840. doi: 10.1007/s13524-012-0104-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey, R. M., Muntner, P., Bosworth, H. B., & Whelton, P. K. (2018). Prevention and control of hypertension: JACC health promotion series. Journal of the American College of Cardiology, 72(11), 1278–1293. doi: 10.1016/j.jacc.2018.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case, A., & Deaton, A. (2021). Life expectancy in adulthood is falling for those without a BA degree, but as educational gaps have widened, racial gaps have narrowed. Proceedings of the National Academy of Sciences of the United States of America, 118(11), e2024777118. doi: 10.1073/pnas.2024777118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang, V. W., & Lauderdale, D. S. (2009). Fundamental cause theory, technological innovation, and health disparities: The case of cholesterol in the era of statins. Journal of Health and Social Behavior, 50(3), 245–260. doi: 10.1177/002214650905000301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chobanian, A. V., Bakris, G. L., Black, H. R., Cushman, W. C., Green, L. A., Izzo, J. L., Jones, D. W., Materson, B. J., Oparil, S., Wright, J. T., Roccella, E. J., Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute, & National High Blood Pressure Education Program Coordinating Committee. (2003). Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension, 42(6), 1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2 [DOI] [PubMed] [Google Scholar]
- Clouston, S. A. P., Rubin, M. S., Phelan, J. C., & Link, B. G. (2016). A social history of disease: Contextualizing the rise and fall of social inequalities in cause-specific mortality. Demography, 53(5), 1631–1656. doi: 10.1007/s13524-016-0495-5 [DOI] [PubMed] [Google Scholar]
- Crimmins, E., Guyer, H., Langa, K., Ofstedal, M. B., Wallace, R., & Weir, D. (2008). Documentation of physical measures, anthropometrics and blood pressure in the Health and Retirement Study [HRS Documentation Report]. Survey Research Center, University of Michigan. https://hrs.isr.umich.edu/sites/default/files/biblio/dr-011.pdf [Google Scholar]
- Cutler, D., & Lleras-Muney, A. (2008). Education and health: Evaluating theories and evidence. In Schoeni R. F., House J. S., Kaplan G. A., & Pollack H. (Eds.), Making Americans healthier: Social and economic policy as health policy (pp. 29–60). Russell Sage Foundation. [Google Scholar]
- Dégano, I. R., Marrugat, J., Grau, M., Salvador-González, B., Ramos, R., Zamora, A., Martí, R., & Elosua, R. (2017). The association between education and cardiovascular disease incidence is mediated by hypertension, diabetes, and body mass index. Scientific Reports, 7, 12370. doi: 10.1038/s41598-017-10775-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettehad, D., Emdin, C. A., Kiran, A., Anderson, S. G., Callender, T., Emberson, J., Chalmers, J., Rodgers, A., & Rahimi, K. (2016). Blood pressure lowering for prevention of cardiovascular disease and death: A systematic review and meta-analysis. The Lancet, 387(10022), 957–967. doi: 10.1016/s0140-6736(15)01225-8 [DOI] [PubMed] [Google Scholar]
- Firpo, S., Fortin, N. M., & Lemieux, T. (2009). Unconditional quantile regressions. Econometrica, 77(3), 953–973. doi: 10.3982/ECTA6822 [DOI] [Google Scholar]
- Flint, A. C., Conell, C., Ren, X., Banki, N. M., Chan, S. L., Rao, V. A., Melles, R. B., & Bhatt, D. L (2019). Effect of systolic and diastolic blood pressure on cardiovascular outcomes. New England Journal of Medicine, 381(3), 243–251. doi: 10.1056/nejmoa1803180 [DOI] [PubMed] [Google Scholar]
- Fryar, C. D., Ostchega, Y., Hales, C. M., Zhang, G., & Kruszon-Moran, D. (2017). Hypertension prevalence and control among adults: United States, 2015–2016 (NCHS Data Brief No. 289; p. 8). National Center for Health Statistics; [PubMed] [Google Scholar]
- Gillespie, C. D., & Hurvitz, K. A. (2013). Prevalence of hypertension and controlled hypertension—United States, 2007–2010. Morbidity and Mortality Weekly Report (MMWR), 62(3), 144–148. [PubMed] [Google Scholar]
- Harris, K. M., & Schorpp, K. M. (2018). Integrating biomarkers in social stratification and health research. Annual Review of Sociology, 44, 361–386. doi: 10.1146/annurev-soc-060116-053339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health and Retirement Study. (2019). RAND HRS longitudinal file 2016 (v1) public use dataset. Produced and distributed by the University of Michigan with funding from the National Institute on Aging (grant number NIA U01AG009740). University of Michigan. [Google Scholar]
- Jackson, M. I. (2009). Understanding links between adolescent health and educational attainment. Demography, 46(4), 671–694. doi: 10.1353/dem.0.0078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killewald, A., & Bearak, J. (2014). Is the motherhood penalty larger for low-wage women? A comment on quantile regression. American Sociological Review, 79(2), 350–357. doi: 10.1177/0003122414524574 [DOI] [Google Scholar]
- Leng, B., Jin, Y., Li, G., Chen, L., & Jin, N. (2015). Socioeconomic status and hypertension: A meta-analysis. Journal of Hypertension, 33(2), 221–229. doi: 10.1097/HJH.0000000000000428 [DOI] [PubMed] [Google Scholar]
- Lewington, S., Clarke, R., Qizilbash, N., Peto, R., Collins, R., & Prospective Studies Collaboration. (2002). Age-specific relevance of usual blood pressure to vascular mortality: A meta-analysis of individual data for one million adults in 61 prospective studies. Lancet (London, England), 360(9349), 1903–1913. doi: 10.1016/s0140-6736(02)11911-8 [DOI] [PubMed] [Google Scholar]
- Link, B. G., & Phelan, J. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 35, 80–94. doi: 10.2307/2626958 [DOI] [PubMed] [Google Scholar]
- Mancia, G., & Guido, G. (2014). Aggressive blood pressure lowering is dangerous: The J-curve. Hypertension, 63(1), 29–36. doi: 10.1161/HYPERTENSIONAHA.113.01922 [DOI] [PubMed] [Google Scholar]
- Masters, R. K., Link, B. G., & Phelan, J. C (2015). Trends in education gradients of “preventable” mortality: A test of fundamental cause theory. Social Science & Medicine, 127, 19–28. doi: 10.1016/j.socscimed.2014.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehta, N. K., Abrams, L. R., & Myrskylä, M. (2020). US life expectancy stalls due to cardiovascular disease, not drug deaths. Proceedings of the National Academy of Sciences of the United States of America, 117(13), 6998–7000. doi: 10.1073/pnas.1920391117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montez, J. K., & Hayward, M. D. (2014). Cumulative childhood adversity, educational attainment, and active life expectancy among U.S. adults. Demography, 51(2), 413–435. doi: 10.1007/s13524-013-0261-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostchega, Y., Fryar, C. D., Nwankwo, T., & Nguyen, D. T. (2020). Hypertension prevalence among adults aged 18 and over in the United States, 2017–2018 (NCHS Data Brief No. 364). National Center for Health Statistics. [PubMed] [Google Scholar]
- Phelan, J. C., & Link, B. G. (2005). Controlling disease and creating disparities: A fundamental cause perspective. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60(2), 27–33. doi: 10.1093/geronb/60.special_issue_2.s27 [DOI] [PubMed] [Google Scholar]
- Phelan, J. C., Link, B. G., Diez-Roux, A., Kawachi, I., & Levin, B. (2004). “Fundamental causes” of social inequalities in mortality: A test of the theory. Journal of Health and Social Behavior, 45(3), 265–285. doi: 10.1177/002214650404500303 [DOI] [PubMed] [Google Scholar]
- RAND. (2019). RAND HRS longitudinal file 2016 (v1). Produced by the RAND Center for the Study of Aging, with funding from the National Institute on Aging and the Social Security Administration. RAND. [Google Scholar]
- Rios-Avila, F. (2020). Recentered influence functions (RIFs) in Stata: RIF regression and RIF decomposition. The Stata Journal, 20(1), 51–94. doi: 10.1177/1536867x20909690 [DOI] [Google Scholar]
- Sonnega, A., Faul, J. D., Ofstedal, M. B., Langa, K. M., Phillips, J. W., & Weir, D. R. (2014). Cohort profile: The Health and Retirement Study (HRS). International Journal of Epidemiology, 43(2), 576–585. doi: 10.1093/ije/dyu067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanaway, J. D., Afshin, A., Gakidou, E., Lim, S. S., Abate, D., Abate, K. H., Abbafati, C., Abbasi, N., Abbastabar, H., Abd-Allah, F., & GBD 2017 Risk Factor Collaborators. (2018). Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 392(10159), 1923–1994. doi: 10.1016/S0140-6736(18)32225-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. (2019). Stata statistical software: Release 16. StataCorp LLC. [Google Scholar]
- Whelton, P. K. (2015). The elusiveness of population-wide high blood pressure control. Annual Review of Public Health, 36, 109–130. doi: 10.1146/annurev-publhealth-031914-122949 [DOI] [PubMed] [Google Scholar]
- Whelton, P. K., Carey, R. M., Aronow, W. S., Casey, D. E., Collins, K. J., Himmelfarb, C. D., DePalma, S. M., Gidding, S., Jamerson, K. A., Jones, D. W., MacLaughlin, E. J., Muntner, P., Ovbiagele, B., Smith, S. C., Spencer, C. C., Stafford, R. S., Taler, S. J., Thomas, R. J., Williams, K. A., & Wright, J. T. (2018). 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension, 71(6), e13–e115. doi: 10.1161/HYP.0000000000000065 [DOI] [PubMed] [Google Scholar]
- Zacher, M., Wang, J., & Short, S. E. (2021). The contributions of hypertension diagnosis and blood pressure control to subjective life expectancy in a representative sample of older U.S. adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 77(2), 378–388. doi: 10.1093/geronb/gbab022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zajacova, A., & Lawrence, E. M. (2018). The relationship between education and health: Reducing disparities through a contextual approach. Annual Review of Public Health, 39(1), 273–289. doi: 10.1146/annurev-publhealth-031816-044628 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.