Abstract
Purpose
During the SARS-CoV-2 pandemic, various online instructional strategies in clinical skills training were piloted. The sudden transition to the remote platform circumvented the rigorous planning associated with curriculum reform. This study aimed to explore students’ and tutors’ perceptions of factors that promoted or hindered successful learning transfer and to propose a blended conceptual model to guide affective, cognitive, and psychomotor clinical skills training in the pre-clinical phase of medical education.
Methods
A mixed-method quasi-experimental study assessed third-year students’ transfer of clinical skills and knowledge following online learning in 2021. Students and their tutors completed online surveys that included open and closed-ended questions regarding factors influencing their experience of the adapted teaching methods. Descriptive statistical analysis was used for the quantitative data. Qualitative responses were thematically analyzed.
Results
One hundred fourteen students (48%) and seven tutors (100%) responded to the surveys. The questionnaires’ internal consistency and construct validity were determined using Cronbach’s α-Coefficient. There was an overall positive response (86%) to the acceptability of the online platform in clinical skills training. Using online simulations with targeted onsite practice was reported as effective in clinical skills training. Tutors perceived students as well-prepared for the skills laboratory. Five emergent themes, qualified by a linear model of asynchronous and synchronous online and onsite teaching with the evaluation of the instructional design and institutional support, informed the proposed blended learning guide for clinical skills training in the pre-clinical phase.
Conclusion
Blended clinical skills learning that included the flipped classroom concept was well-accepted. Virtual patients proved a convenient cognitive preparation tool for skills training and potentially optimized teaching delivery. The study found that the adapted teaching frameworks incorporating an online clinical skills component into a modified onsite curriculum augmented learners’ ability to transfer knowledge to the clinical skills laboratory. An integrated five-step blended model is proposed for future interventions.
Keywords: flipped classroom, psychomotor skills, COVID-19, learning transfer
Introduction
Medical education has faced several transitions in pedagogy, attempting to reconcile teaching with learning.1,2 Typically, rigorous scientific data precedes educational reform;3 however, the most recent shift to an online teaching methodology was sudden and unplanned.4,5 The impact of COVID-19 on universities globally6 was a catalyst in reframing the planning, teaching, and learning of medical education in the online arena. Despite the benefits of various blended learning strategies in other disciplines,7–9 changes to the medical curriculum have been slow,10,11 especially in clinical skills training.12,13 The loss of face-to-face (f2f), hands-on learning during the pandemic created an unprecedented opportunity14 to pilot teaching strategies previously considered superfluous.10 Medical schools implemented an interim online learning program to ensure the continuity of the curriculum during the lockdown restrictions when students and tutors had to stay at home to stop the spread of the virus. Irrespective of the temporary intent, the program’s merits and shortfalls inherently emerged,15 revealing the need for innovative teaching strategies.
The flipped classroom (FC) model using online, asynchronous, self-directed learning is practiced in medical education. Students independently study pre-shared resources to apply later in the classroom.16 However, the implementation of synchronous online teaching, where “live” interactions occurred between teachers and students in real-time over a web-based platform, was novel and vague,11 making its role in medical education uncertain.12
Clinical teaching comprises communication, physical examination, procedural, and patient management skills within the affective, cognitive, and psychomotor domains, respectively.17 Affective skills assess behavioral knowledge, cognitive skills assess comprehension, and psychomotor skills assess performance knowledge.18
Enoch et al19 evaluated the effectiveness of an adapted online clinical skills program and showed that students taught online were competent in these three domains of clinical skills. Although this single-center study included only third-year students and examined a limited number of clinical skills, the findings supported the systematic review and meta-analysis by Pei et al.20 The contributing factors for this successful transfer of learning are not well established.
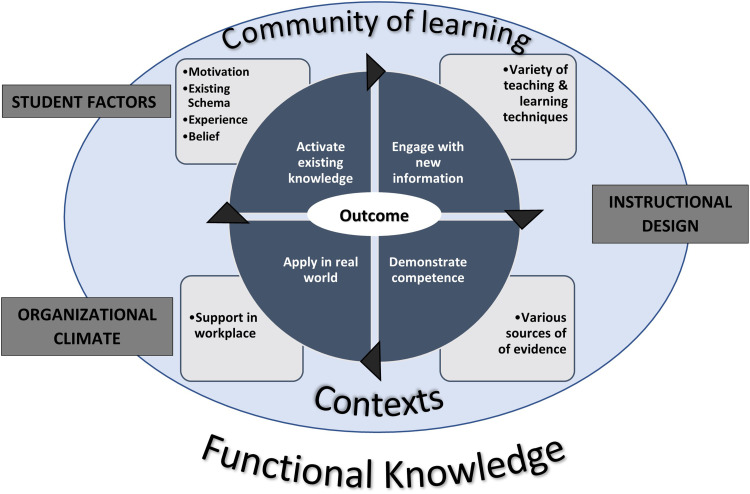
Botma et al21 developed a conceptual framework (Figure 1) for designing modular teaching to optimize the transfer of learning. It considers student characteristics, teaching design, and organizational impact on transferring knowledge in the traditional educational paradigm.
Figure 1.
A conceptual framework for educational design at a modular level to promote the transfer of learning - adapted from Botma et al (2015).21
This constructivist-based model consists of four steps – (i) activation of existing knowledge; (ii) engagement with new information; (iii) demonstration of competence; and (iv) application in real-world practice. Effective transfer rooted in understanding these concepts leads to long-term knowledge retention, which is essential for medical decision-making.8 To activate knowledge, the tutor identifies a baseline of foundational knowledge on which to construct new information. A student-centered approach with precise outcomes must be clearly defined to facilitate learner engagement. Students then develop an understanding of the newly acquired skill as the relevance of what is being taught meaningfully connects to pre-existing knowledge.22 A controlled clinical skills simulation laboratory23 supports the performance of these new skills aiding the transition to the clinical learning environment, where knowledge can be integrated holistically.
However, a comprehensive conceptual framework that provides an understanding of the underlying factors associated with online learning transfer to hands-on practice has not yet been established.24 According to Galoyan,24 this is due to three factors. First, the complex nature of transfer; second, the variables that affect transfer; and third, the limited knowledge of online instructional strategies to enhance transfer. The dissimilarity between the source learning context, be it online or in the clinical skills laboratory (CSL), and the bedside application context decreases the learning transfer of clinical skills training.23,25 Thus, the ability to transition skills learned in the pre-clinical years to the clinical setting has continued to challenge both students and tutors, even pre-pandemic.26,27
By assessing students’ and tutors’ perceptions of the adapted clinical skills teaching strategies during the pandemic, the enhancers and limitations to the transfer and retention of clinical knowledge and skills could be established.11,22,28 Improving these measures may progress pre-clinical medical education towards renewed teaching and learning strategies by incorporating the best of the online and onsite platforms.29 This study aimed to evaluate the factors that enhance the retention and transfer of clinical knowledge and skills from the adapted online teaching strategy and proposes a conceptual model to optimize undergraduate clinical skills training in an integrated blended educational approach.
Methods
Context and Setting
The study was conducted at the Nelson R Mandela School of Medicine (NRMSM), clinical skills department – University of KwaZulu-Natal (UKZN). Clinical skills are taught during the three pre-clinical years in the CSL, using simulated patients and models. From March 2020, due to the Covid-19 pandemic, an adapted online curriculum was implemented to support remote student learning in clinical skills’ affective, cognitive, and psychomotor domains.30 In preparation for clinical rotations, the 2021 third-year medical students were invited to participate in an onsite “Readiness Programme” (RP).19 They were formatively assessed at the CSL in a mock Objective Structured Clinical Examination (OSCE) on their ability to perform psychomotor (procedural and examination) skills following online training. This formative assessment was conducted as a 20-minute, one-on-one, directly observed session with a tutor who scored students’ competence in the obstetric examination and Pap Smear skills using a standard OSCE score sheet. After scoring, students were given feedback and an opportunity for correction and self-directed practice in other examination and procedural skills. All COVID-19 protocols were observed. A summative online OSCE was also conducted to assess affective (history-taking) and cognitive skills.
Research Design, Study Sample, and Data Collection
A mixed-methods quasi-experimental cross-sectional study was conducted with the 2021 third-year medical students (n=239) and their clinical skill tutors (n=7). This class experienced face-to-face, online, and blended teaching methods at different training junctures since admission to medical school. The research design involved quantitative and qualitative data collection using survey questionnaires. The two components were concurrently merged in the study to provide a more comprehensive understanding of the students’ and teachers’ responses. Participants anonymously shared uncensored perceptions that aptly captured their personal experiences of factors that promoted or limited the transfer of learning following online training.31 One hundred and fourteen medical students (n=114) and seven clinical tutors (n=7) consented and completed the questionnaires.
Instruments
Two questionnaires (Instruments A and B) were designed based on Botma et al’s21 conceptual framework to promote the transfer of learning.21 Instrument A investigated students’ perceptions, and Instrument B tutors’ perceptions of the factors that impacted the transfer of learning and students’ confidence to apply their clinical skills competently. Botma et al’s21 framework highlighted the following components which informed sections (ii–iv) of the questionnaire:- (i) demographic data, (ii) perceptions of students’ characteristics in the approach to online learning, (iii) perceptions of the learning design, (iv) perceptions of institutional support available during the online curriculum. A 6-point Likert scale was used to gather quantitative data where the participants indicated their level of agreement with a series of closed-ended statements related to sections (ii–iv) above. The scale ranged from a score of 1 = strongly disagree; 2 = disagree; 3 = slightly disagree; 4 = slightly agree; 5 = agree; 6 = strongly agree. Each statement could score a minimum of 1 and a maximum of 6 points.
Section (v) comprised six open-ended questions about the adaptations to the affective, cognitive, and psychomotor domains of clinical skills online training and the ability to apply those hands-on skills. This section also included questions about the acceptance of online learning, blended learning strategies, challenges experienced, and recommendations for the future. As this was a small-scale study, Instruments A and B were pretested with two students and one tutor, respectively, to determine the clarity of the questions.32 After minor adjustments, the instruments were made available electronically via Google Forms with links shared on the Learning Management System – Learn2021.
Ethical approval to conduct the study was granted by the UKZN Humanities and Social Sciences Research Ethics Committee [HSSREC/00003459/2021]. Written consent was obtained from all participants. The data are reported anonymously by replacing participant identities with codes, where prefixes “S” and “T” represent students and tutors, respectively.
Data Analysis
The quantitative data were statistically analyzed using the Statistical Package for the Social Sciences (SPSS) version 27 (IBM, USA) and reported anonymously. Cronbach’s α-Coefficient was used to test the construct validity of the questionnaire. Descriptive statistics were used to determine percentages and mean scores of the close-ended responses in Instruments A and B. Graphs were generated on Microsoft Excel spreadsheets using the mean response to a statement and reported in the results section below. Following calculations of the range between the Likert-scale categories, a mean of 4.5 out of 6 was selected to include only the upper limit of “Slightly Agree”, “Agree”, and “Strongly Agree” as a positive response to a statement. Each section of both questionnaires received a total score as a percentage based on the cumulative responses of students and tutors, respectively.
The qualitative data from the students’ and tutors’ responses to the open-ended questions were downloaded and thematically analyzed using the NVivo 12 Pro software. Each author read the written responses multiple times to familiarize themselves with the data, explore the information’s meaning in the study context, and systematically condense the data into the essential content using sequential steps. There was noteworthy consistency in the participants’ responses suggesting data saturation was achieved. The main author methodically examined the data concentrating on participants’ views of the transfer of learning using inductive coding to uncover patterns within the data. The remaining authors performed preliminary analysis or acted as second coders for the data. Initial codes tabled keywords and phrases to identify patterns in participants’ responses about factors that affected the transfer of learning. Similar codes were grouped, carefully reviewed, and inductively organized as themes. After some revision, the more representative final themes and sub-themes were agreed upon at a consensus meeting, and the relationship between the students’ and tutors’ perceptions of the factors impacting the transfer of learning was clarified.33 Thematic analysis is a powerful method for organizing and understanding the experiences and thoughts of a group across a large data set.31 The quantitative and qualitative data were analyzed separately and then triangulated.34 This was achieved by selecting specific quotations from both participant groups to support and extend the quantitative data in order to provide a comprehensive picture of the phenomenon under study.35
Results
The questionnaires’ internal consistency and construct validity were determined using Cronbach’s α-Coefficient. Reliability analysis reported an overall Cronbach’s alpha of 0.953 for the 53-statement student questionnaire (Instrument A) and 0.866 for the 29-statement tutor questionnaire (Instrument B).
There were two hundred and thirty-nine (n=239) students in the 2021 third-year class. One hundred and fourteen students consented to participate in the study and completed the questionnaire, representing a response rate of 48% (n=114). The sample population was demographically representative of the third-year cohort regarding age, sex, and race. 93.9% (n=107) of participants were 18 to 25 years in age, 60.5% (n=69) were female, 55.2% (n=63) African, 36% (n=41) Indian, 7% (n=8) Colored, 0.9% (n=1) white, and 0.9% (n=1) was Asian. 58.2% (n=59) were second-language English speakers, and 85.1% (97) entered the medical school from secondary schooling. In addition to the online curriculum, 65% of the participants (n=74) also participated in a formative onsite OSCE Readiness Programme (RP), where they demonstrated the online skills taught to a tutor.
Seven of the nine tutors that teach clinical skills to third-year medical students were invited to participate in the questionnaire. The two tutors (LE & RA) involved in the study were excluded from the surveys. All tutors (100% response rate) were involved in the traditional face-to-face and online curricula and had more than three years of teaching experience. 74% of the tutors participated in the formative onsite RP.
The responses of both students and tutors to the open-ended questions revealed five main themes and sub-themes (Tables 1–5) relating to factors impacting the transfer of learning, retention of clinical knowledge, and the ability to perform clinical skills in the CSL following the adapted curriculum. The quantitative data from the tutors’ and students’ close-ended questions and specific, prevalent views from their open-ended questions are represented simultaneously, thereby adding validity by incorporating a qualitative component into an otherwise quantitative study.36
Table 1.
Excerpts from student and tutor responses regarding asynchronous online learning
| Pre-reading |
|
| Self-motivated, self-directed |
|
| Quality of lecture delivery |
|
| Environmental factors |
|
| Device fatigue |
|
Table 2.
Excerpts from student and tutor responses regarding synchronous online learning
| Interactive student engagement |
|
| Foundational concepts through innovative teaching design |
|
| Spaced learning and consolidation of knowledge through constructive instructional design |
|
| Immediate feedback and remediation |
|
| Preparedness for demonstration of clinical skills |
|
Table 3.
Excerpts from student and tutor responses regarding synchronous onsite learning
| Appreciation for hands-on practice |
|
| Effectual transfer of skills |
|
| Personalized interaction, feedback, and remediation |
|
Table 4.
Excerpts from student responses regarding asynchronous onsite learning
| Self-directed and peer practice promotes retention and competence |
|
Table 5.
Excerpts from student and tutor responses regarding the evaluation of the program
| Continuous Assessments benefits students |
|
| Summative Assessments Identify knowledge and teaching gaps |
|
Strengths:
|
|
Opportunities:
|
|
Weaknesses:
|
|
Threats
|
|
Graphical representations (Figures 2–6) of the quantitative data as mean values and specific quotations from both participant groups that supported and extended the quantitative data are indicated in Tables 1–5 under the major themes and subthemes as factors that impacted clinical skills training in an integrated blended education approach.
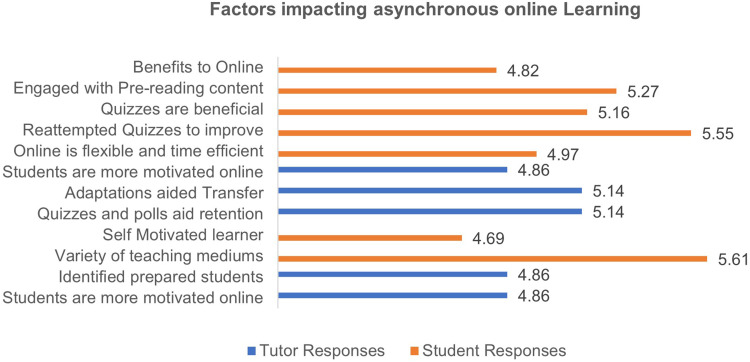
Figure 2.
Mean level of agreement of students and tutors with statements related to factors impacting asynchronous online learning.
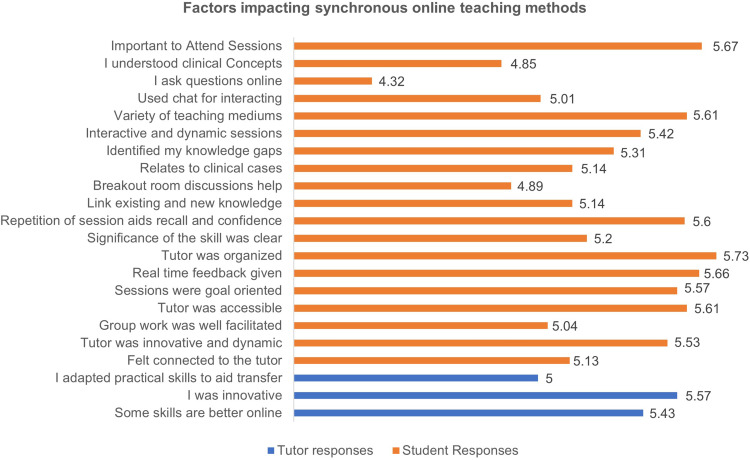
Figure 3.
Mean level of agreement of students and tutors with statements related to factors impacting synchronous online learning.
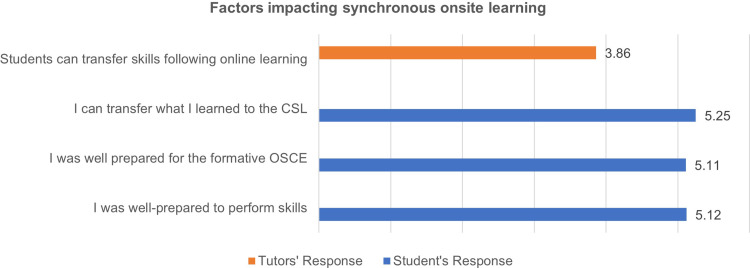
Figure 4.
Mean level of agreement of students and tutors with statements related to factors impacting synchronous onsite learning.
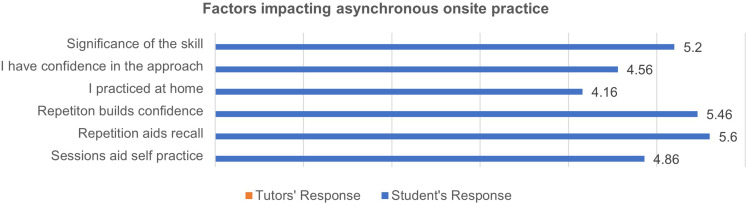
Figure 5.
Mean level of agreement of students and tutors with statements related to factors impacting asynchronous onsite learning.
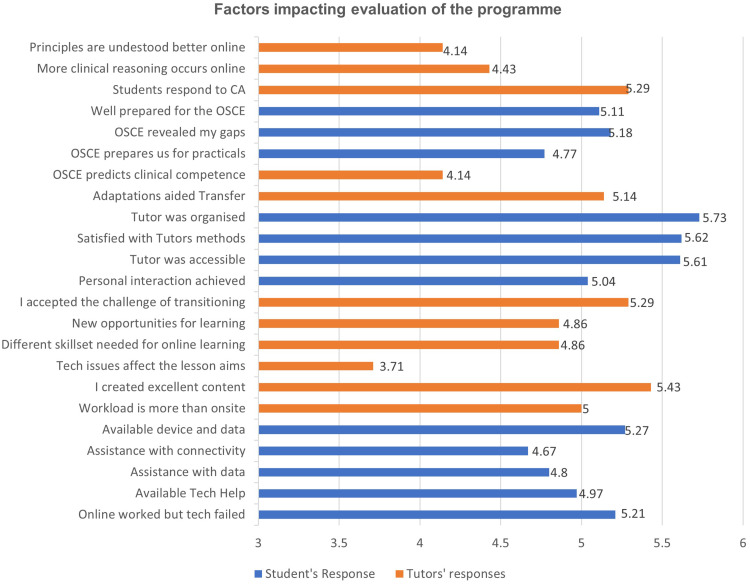
Figure 6.
Mean level of agreement of students and tutors with statements related to the evaluation of the program.
Theme 1: Asynchronous Online Teaching Material Aided and Motivated Students to Develop a Foundation to Construct New Knowledge
Figure 2 represents students and tutors’ mean level of agreement related to factors impacting asynchronous online learning, and Table 1 illustrates the representative quotes. There was an overall positive response (88.6%) to the acceptability of the online platform in learning clinical skills. Factors that promoted student preparation for lessons included pre-reading (5.27) and self-motivation to engage with the material (5.27). The quality of lecture delivery played an important role in processing the presented information. Tutors perceived that students were well-resourced for the synchronous online sessions (5.14). The student’s environment needed to suit a technology-based platform for adequate preparation. Prolonged screen time resulted in a “device fatigue” phenomenon (4.96%). Despite some challenges, there was an 80.7% positive response by students appreciating the online curriculum designed and curated by the clinical skills department, compared to other disciplines.
Theme 2: Synchronous Online Teaching Using Various Instructional Methods Improves Comprehension of Concepts
Figure 3 represents students, and tutors mean level of agreement related to factors impacting synchronous online teaching methods, and Table 2 illustrates the representative quotes. The online synchronous Zoom lectures and “practical” sessions were interactive, dynamic, goal-orientated, and well-facilitated (5.42). The content was relevant, and multimedia and discussions enhanced learning and retention. Examination, procedural, and history-taking skill teaching approaches offered better comprehension than traditional learning. Learners linked the pre-reading material and quizzes to the new knowledge taught (5.14). They identified their knowledge gaps during these sessions and appreciated the immediate remediation. Most tutors implemented innovative teaching designs, including novel teaching strategies, small group breakout room sessions, and simulations focused on the cognitive domain (5.57). Spaced learning helped students to reinforce their knowledge (5.60) and improve their confidence to attempt the skill (5.46). Communication skills were comparable to onsite practice (5.24); however, students were mindful of the limitations of the zoom platform.
Learners felt connected to their tutors (5.13) and peers on the online platform, and the feedback received stimulated self-directed learning and practice (5.66). Preparedness for their profession was a student concern since competence could only be determined by demonstrating the physical examinations and procedures skills learned to a tutor in the CSL on simulated or actual patients (4.50).
Theme 3: Synchronous Onsite Learning Consolidates Knowledge and Skills and Improves Students’ Confidence and Competence
Figure 4 shows students and tutors mean level of agreement related to factors impacting synchronous onsite learning, and Table 3 illustrates the representative quotes. Students viewed the onsite RP provided in the CSL as an opportunity to consolidate learning instead of an additional task, expressing an appreciation for the benefits of online learning (5.25). Students demonstrated competence in their ability to perform skills to their tutors. Learning most of the theoretical knowledge before the practical session allowed for deliberate practice in the skills lab (5.12). Although tutors were initially skeptical of the students’ ability to transfer skills from the online platform to the CSL (3.86), they were surprised and impressed with the participants’ performance in the Readiness Programme (RP). They felt that the online teaching strategies had benefitted students and allowed them to transfer the skills to a mannequin effectively. Interaction with tutors allowed students’ knowledge gaps to be identified, enabling immediate remediation and hands-on correction (5.18). Following the RP, the learners felt more confident and prepared to perform the skills in the future.
Theme 4: Asynchronous Onsite Hands-on Practice Reinforces Skills and Promotes the Retention of Knowledge
Figure 5 shows students’ mean level of agreement related to factors impacting asynchronous online practice, and Table 4 illustrates the representative quotes. Repeated exposure to the skills enhanced students’ understanding (5.60). University-residing students that engaged in self-directed practice to improve their capabilities felt that working with a peer was beneficial. However, students at home had a neutral response regarding opportunities to practice (4.16). The significance of the skills taught and the importance of practicing the skills to achieve competence was acknowledged (5.20). Many students felt confident to attempt to do the skills in the CSL (5.25) but relied on feedback to address gaps (4.56).
Theme 5: Evaluation of the Curriculum and Students’ Performance Through Continuous Assessments, Summative OSCEs, and Feedback by All Role Players Enhance Student Engagement and Student-Centered Learning
Students and tutors evaluated their experience of the adapted curriculum and offered specific feedback on recommendations for modular planning. Figure 6 represents their level of agreement with statements regarding the different components of the program, and Table 5 illustrates the students’ and tutors’ representative quotes.
Continuous Assessments
Students agreed that attempting online quizzes and participating in interactive “chats” during online teaching were beneficial (5.16). Initially, tutors were unsure that learners could grasp essential clinical skills principles using online learning alone (4.14). Therefore “continuous assessment” marks through quizzes and polls were used to incentivize students to learn and track their progress during the module (5.29).
Formative and Summative Assessments
Students advocated for implementing more formative assessments, like the RP, to consolidate knowledge and identify learning gaps in preparation for the summative OSCE (5.18). They considered summative OSCEs important and felt they were adequately prepared for the online examination during their third year (5.11). The consensus was that the online OSCE tested the theory well but did not guarantee the performance of the skill to the same quality. Tutors agreed with this sentiment and shared a neutral response regarding their ability to assess a student’s competence in a clinical skill based solely on an online OSCE (4.14).
Strengths and Opportunities That Promoted a Blended Learning Approach
Students proposed a blended learning approach for the future of medical education, with lectures and tutorials being online, and practical and practice sessions onsite. They advocated for structured one-on-one tutor-student interactions to optimize the time spent in the CSL. Tutors agreed that there was merit to having a system that combined online teaching with an onsite application (5.14).
Tutor support during the online training was perceived as 88.6% positive, and students strongly felt that their educators were well-prepared (5.73) and easily accessible to address queries. Key principles of the skills were understood, and they were allowed to perform tasks and demonstrate their knowledge with immediate feedback during teaching. Despite the remote teaching, students felt connected to tutors, experienced a sense of personal interaction with staff, and expressed appreciation and respect for the faculty (5.04).
Opportunities
Although the transition to online teaching was challenging and required learning a new skill set (4.86), tutors felt that the technical and staff support provided by the institution helped enable their smooth transition.
Technical training allowed tutors to upskill themselves (5.29), and they disagreed that technical issues were a major disruption to teaching (3.71). All tutors believed that the training assisted them in creating excellent online content and expanding their teaching approaches (5.43). Online learning highlighted the need and presented an opportunity for collaborative curriculum planning with improved inter-departmental communication for efficient content delivery. Students also noted that the blended learning platform had benefits not present in the traditional setting, like the interactive format and spaced delivery of new information.
Weaknesses and Threats to the Blended Learning Approach
Developing the online curriculum was more labor-intensive than the traditional setting (5.0). Students expressed fatigue with long online sessions and felt inadequate breaks were allocated. They felt overwhelmed with the volume of work and mentioned that the schedule was poorly planned. Another weakness was that students could choose not to participate by feigning network difficulties, which contributed negatively to the session.
Students were the least satisfied with technical support (75.4%). While devices and data were available, there were issues related to internet connectivity and data insufficiency. Technical support was not always accessible (4.67), meaning students were “left out” of discussions when their network or device failed. Students strongly agreed that online learning could work; however, technical issues and rolling electricity rationing disrupted network coverage and device power, compromising the experience (5.21). These infrastructural disturbances required additional planning to avoid interruptions in teaching delivery.
Discussion
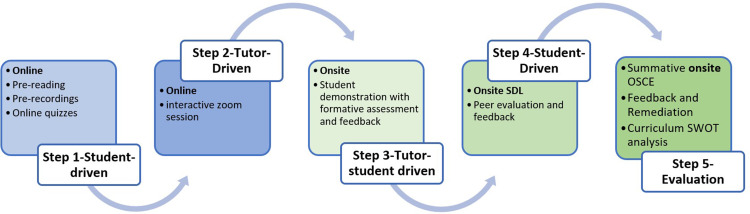
The effectiveness of blended teaching strategies is well supported in the literature;37,38 however, many challenges have contributed to the slow implementation of the pedagogical shift in medical education.39,40 This study evaluated students’ and their tutors’ perceptions of the enhancers and limitations of the online and blended teaching strategies implemented in pre-clinical training during the pandemic. Understanding the role of student characteristics, teaching design, and the organizational environment is integral to the constitution of blended learning strategies for transferring knowledge and designing modular themes. Our findings agreed with Saiyad et al41 who described twelve principles of good online-teaching practices for sustainable and effective teaching-learning outcomes. These principles include synchronous and asynchronous teacher-student interactions that promote cognitive development, teamwork, and active and self-directed learning, followed by formative and summative assessments with feedback opportunities. Tutors must manage their time well, set clear expectations for sessions, and use a variety of instructional approaches. Mentoring through guidance, facilitation, and setting learning goals to match curriculum objectives are also part of the strategy to optimize the online platform. Based on the findings of the current study and the literature, a five-step multimodal constructivist approach to clinical skills training in the pre-clinical years within a blended learning and teaching model is proposed (Figure 7).
Figure 7.
A proposed five-step multimodal blended learning and teaching approach to clinical skills training.
Student-Driven Online Asynchronous Learning and Teaching
The participants in this study expressed positive attitudes toward implementing online and blended learning. This FC concept emphasizes flexibility, a student-centered learning culture, well-curated pre-learning content, and a professional educator. Rahmani et al42 confirmed that in such a setting, the Teacher should assume the role of an education guide rather than an education source. The FC approach is highly dependent on the learner’s willingness to engage with the information presented, recognize the need for the learning, and be committed to using the knowledge beyond the initial learning session to ensure that long-term retention is achieved.8,43 Our students’ motivation to learn was a significant factor that guided their acceptance of the online platform. Students’ roles are generally diminished to recipients of knowledge rather than contributors to instructional design.10,44 However, students who are more engaged play a critical role in establishing a working curriculum,45 and learners in this study vocalized specific strategies which aided their training.
The student’s beliefs and value systems dictate how they perceive and learn. When these systems misalign with the institution, impediments may occur.44 Our students recognized how the learning environment and curriculum planning contributed to their ability to assimilate information and impacted the vigor with which they interacted with the teaching material. Lawrence et al45 reported that the conduct of a delivered course might not fulfill the learner’s expectations in terms of the content, the comparison to face-to-face delivery, or the time allocated for a session. Students in our study found that uploaded pre-recorded lectures were beneficial if they were well-paced, offered clear explanations that expanded their understanding, and allowed for repetition of the learning material, similar to findings by Van Duijn et al.46 The clinical tutors agreed that continuous assessment motivated students and prepared them well for interactive online sessions. Our learners described an acceptable lecture as concise, goal-oriented, and engaging, but lectures where tutors read off their slides were poorly received and decreased students’ enthusiasm. Our study participants responded positively to effectively planned lectures, which is important for satisfying the educators’ agenda and the students’ mindset.47 However, a well-executed lecture in a poorly structured timetable depreciated the positive effects, as found by Pokryszko-Dragan et al.48 Our students reported being overwhelmed by the volume of work since they had minimal breaks between back-to-back online lectures, leading to digital fatigue as hours were expended in front of their computers, decreasing their learning motivation. With this understanding, Step One of the proposed model was developed (Figure 7).
Step 1
Pre-reading material from uploaded voice-recorded lectures with specified learning goals and links to videos that demonstrate the application of the week’s scheduled skill is delivered asynchronously. Students further supplement their knowledge with the prescribed clinical textbooks or approved websites. Tutors also upload quizzes onto the learning management system, and students complete them for continuous assessment (CA), encouraging preparation and maximum productivity38 for the following steps.
Tutor-Driven Online Synchronous Learning and Teaching
The adaptations made to satisfy the online teaching of “practical” sessions were positively received by students in our study. They expressed appreciation for the innovation and creativity their clinical skills tutors had invested in leading their learning process. Incorporating multiple mediums like video clips, pictures, and role plays into the web-based zoom synchronous practical sessions are strategies to advance learning design.14 The Zoom chat and poll functions promoted participation and active engagement, developing learners’ competence.49,50 Group work in Zoom Breakout rooms encouraged peer discussions of clinical scenarios and enhanced their critical thinking, clinical reasoning, and knowledge retention.5 Other strategies to gain more insight into the skill included home-made models to understand the anatomy of an organ system before simulating the procedures. Simulation-based training has been described as a successful strategy to enhance engagement and learning.51,52 Increased engagement is an important indicator of students’ success, satisfaction, and knowledge retention in higher education.44 Traditional face-to-face lectures are associated with lower student participation rates.53 The Covid-19 pandemic offered opportunities for the clinical tutors in our setting to restructure and redesign traditional onsite classroom teaching strategies since direct translation to the online platform would not be effective.9,54 The interactive instructional teaching design and simulation-based teaching, like role-plays, are superior to didactic medical teaching practice in clinical skills.55 Students in our cohort were pleased with the communication skills simulation training using virtual simulated patients. They felt that role-playing online offered more opportunities for practicing a doctor-patient consultation and effectively achieved learning outcomes. The use of virtual patients proved to be a convenient cognitive preparation tool for skills training. However, they recognized difficulties in assessing the simulated patient’s non-verbal communication cues as a significant shortfall of the online platform. Step Two (Figure 7) was developed by the participants’ positive response to the online practical session and the specific benefits mentioned.
Step 2
Online interactive teaching-learning sessions are presented synchronously as case-based clinical scenarios on the Zoom platform after the students have completed activities in Step One. These Step Two sessions are goal orientated and form the foundation for conducting the systematic approach to the skill. The basic sciences are also effectively integrated into the session to aid the understanding and retention of root concepts. Students interact verbally, on the chat, and via polls to consolidate and test their knowledge, contributing to their CA. Tutors offer real-time feedback and ensure that the salient components of the session are comprehended and that learners are prepared for the implementation of skills in Step Three. During these sessions, students may be assigned to work individually or in breakout rooms to problem-solve cases.
Student-Tutor-Driven Onsite Synchronous Learning and Teaching
Although the online classroom offered a distinct advantage for comprehending theoretical knowledge,56,57 students and tutors were apprehensive that effective transfer of the “hands-on” skills would occur. Sahu et al55 reported that for augmented transfer, the expected competencies must be clearly stated for students to learn, practice, and demonstrate their basic clinical skills and knowledge to align their theoretical know-how with hands-on practice in the safety of the CSL.58 Our onsite RP alleviated performance anxiety as participating students and tutors found that significant transfer of learning had occurred and that students could perform the skills competently.19 Azizi et al59 agreed that online learning with targeted onsite practice is superior to either face-to-face or online learning methods alone and promotes a constructivist approach to instructional designs.21,25,60 Students’ online foundation links to knowledge acquired onsite. Tutors refine techniques, and students master their skills rather than learning them for the first time,56 with skills laboratory time being used more effectively. This meaningful student-tutor interaction, where learners’ skills are physically molded, informed Step Three of the model (Figure 7).
Step 3
In Step Three, shared responsibility for learning and teaching occurs onsite. Tutors demonstrate learned skills without further explanation, followed by student demonstration of the skill as part of a group or as individuals.30 Problem areas are identified, and the techniques can be re-emphasized or re-taught according to the needs of the learners. These sessions can be conducted as log book sessions, in which students’ performance competencies are formatively evaluated, supported by written feedback and hands-on correction, enhancing their learning.23
Student-Driven Onsite Self-Directed Learning and Practice with Peer Review
Group work in online and onsite platforms was also considered an effective strategy for increasing knowledge retention.61,62 Students who resided in the dormitories worked together to practice skills with each other.
At the CSL, the RP was followed by self-directed practice at various skill stations with a tutor available. Our students practiced examination skills and procedural skills using the knowledge gained from their online resources. The availability of a fully equipped CSL was viewed as an opportunity to implement their theoretical knowledge in a “hands-on” demonstration, an advantage sometimes taken for granted pre-pandemic.56 The CSL is the ideal safe space for students to practice clinical skills without fear of mistakes.55 In contrast to the adage of “see one, do one, teach one”, students are better encouraged to learn a skill, practice it many times, and then “do one”.63 Step Four (Figure 7) describes the opportunity for students to develop their skills further and test their knowledge as they participate in peer assessments.
Step 4
Following directly observed demonstration of their clinical competence, students engage in self-directed, onsite practice to consolidate knowledge using protocols, video demonstrations, and other resources, including self-directed peer assessment with feedback. The students are given access to the CSL to conduct the peer evaluation as a duly performed (DP) requirement. Self-directed formative logbook peer evaluation and feedback sessions can empower students to adopt the roles of a learner who demonstrates the skill and as an assessor who provides constructive criticism. When providing feedback, the written remarks encourage the peer examiner to go deeper into their own understanding of the skill.23
Tutor and Student-Driven Evaluation of the Curriculum
The success of the online and blended platforms depends on the institutional leaders, academic planners, tutors, and students.64 Our study participants mentioned the contribution and performance of all these role-players and critiqued different aspects of the program. Students were assessed online through CAs that comprised quizzes, answering in chats and polls, and verbal participation during zoom sessions. The directly observed onsite formative OSCE (RP) assessed the learner’s competence in performing psychomotor skills and indirectly evaluated the effectiveness of the adapted online teaching strategies. Tutors in the study mentioned that students were well-prepared to perform skills, despite their lack of exposure to onsite teaching in the CSL. Students, too, felt that significant learning transfer had occurred. Students further supported the implementation of more formative onsite assessments of their skills with feedback opportunities to gain confidence and competence. The summative online OSCE assessed behavioral knowledge through a communication skills history-taking role-play, followed by a viva voce examination of cognitive knowledge using clinical case vignettes. Tutors and students agreed that despite being adequately prepared for the OSCE, this format did not comprehensively assess the learner’s competence in the psychomotor domain. However, Remmen et al65 suggested that written tests are satisfactory alternatives to predict the student’s ability to demonstrate the skill.
Evaluation of the study participants perceptions further highlighted other aspects within the system that could shape the institutional paradigm in the future. Organizational reform to meet medical education needs can be complex and disruptive and does not always meet the expectations of the role players.2 Technical naivety was a hindrance, with educators needing to acquire new skills for online teaching delivery with minimal training initially. For some educators, the fear of technology and the additional work associated with online teaching created a mental resistance to adjusting and accepting an online presence in teaching. These findings were common concerns mentioned in the literature.10,38,66 However, the reality of a prolonged lockdown prompted active institutional involvement via the university teaching and learning office (UTLO) to upskill tutors. Our study showed that efforts made by NRMSM to mitigate the effects of the sudden transition to the online platform were well received by tutors. Students felt well supported by their tutors and thought they were adequately trained for their level within the limitations of the pandemic. Tutors, in turn, reported that the UTLO had technologically resourced them to navigate the online platform, despite the steep learning curve and early difficulties. Andersson et al47 concurred that an effective e-learning program should be intentionally designed with human resources and technology funding. Equally, students faced environmental challenges and needed to create a learning environment in their residences or dormitories that was conducive to knowledge acquisition. This included adequate internet connectivity, data, and devices.39 However, our students, like many others globally, felt this was poorly managed, and there was little to no support, causing a significant online classroom barrier.11,67,68
Therefore, students, tutors, coordinators, academic leaders, and administrators determine the program’s success and future. These role-players must scrutinize the curriculum’s strengths, weaknesses, opportunities, and threats (SWOT) at these different levels. Multiple perspectives will result in a 360-degree feedback loop that will enable continuous curricular re-evaluation, culminating in an organizational transformation that will adapt to the changing demands of students and instructors within the institution.2 This SWOT analysis may guide the development of a rigorous blended learning and teaching approach, as elaborated in Step Five (Figure 7) below.
Step 5
The last step involves evaluating the role-players using various assessment and feedback methods. A summative end-of-semester onsite assessment is conducted to evaluate the student’s overall performance and learning. Tutor feedback to the class and targeted remediation follow the results’ analysis.69 For curriculum design and tutor evaluations, students complete a survey at the end of modules and semesters regarding teaching and learning, with ratings, comments, and recommendations for improvements. The SWOT analysis of the module’s instructional design, institutional preparedness, and student factors must be undertaken to ensure that continuous improvements are implemented. Tutors’ evaluation of students’ competence and students’ evaluation of the curriculum and teaching design ensures a 360-degree feedback loop promoting quality assurance as a key institutional process.70
Limitations and Recommendations
Although this was a single-center research study, the challenges and promoters associated with the transfer and application of hands-on skills using the blended learning strategy supported the literature. The added benefit was that our students experienced more than a year of online learning. While our tutor response rate was excellent, the student response rate was lower than anticipated. The fourth wave of COVID-19 coincided with the Readiness Programme, which may have contributed to the lower response rate, as well as the proximity of the data collection questionnaire request to the final examination. Students that completed the study questionnaire may have had a more positive outlook, which may have skewed the study results. Finally, while the study questionnaire was guided by a recognized framework and pretested prior to use, the impact of researchers on the results must be considered. Future studies should incorporate a larger sample size and pilot the questionnaire with more participants to enhance face validity. To mitigate possible researcher biases, the quantitative data was concurrently merged with the qualitative data, allowing the reader to contextualize the findings fully. The proposed model to optimize the transfer of learning is in the early phase of development and requires implementation in the clinical skills training facility to determine its effectiveness. A longitudinal study assessing such a method’s outcomes will add value to the proposed model.
Conclusion
The benefits of online and blended learning are becoming apparent and potentially play a vital role in optimizing teaching delivery in medical education. Our study confirms that the traditional frameworks that guided learning transfer can be adapted to incorporate the online component and augment the learners’ use of the CSL, incorporating the best of the onsite and online teaching platforms. The successful implementation of a multimodal approach depends on all role players embracing and integrating a blended strategy to instill confidence in our students and reform the way we teach undergraduate clinical skills.
Abbreviations
FC, flipped classroom; CSL clinical skills laboratory; RP, readiness program; f2f, face-to-face.
Data Sharing Statement
The datasets analyzed during the current study are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Research involving human participants, human material, or human data must have been performed in accordance with the Declaration of Helsinki. Ethical approval for this study was granted by the University of KwaZulu-Natal’s ethics committee (approval number HSSREC/00003459/2021). Informed consent was obtained. The authors confirm that all methods were carried out in accordance with UKZN’s guidelines and regulations.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Trullàs JC, Blay C, Sarri E, Pujol R. Effectiveness of problem-based learning methodology in undergraduate medical education: a scoping review. BMC Med Educ. 2022;22(1). doi: 10.1186/s12909-022-03154-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gordon L, Cleland JA. Change is never easy: how management theories can help operationalise change in medical education. Med Educ. 2021;55(1):55–64. doi: 10.1111/medu.14297 [DOI] [PubMed] [Google Scholar]
- 3.Irby DM, Cooke M, O’Brien BC. Calls for reform of medical education by the Carnegie Foundation for the advancement of teaching: 1910 and 2010. Acad Med. 2010;85(2):220–227. doi: 10.1097/ACM.0B013E3181C88449 [DOI] [PubMed] [Google Scholar]
- 4.Bock A, Kniha K, Goloborodko E, et al. Effectiveness of face-to-face, blended and e-learning in teaching the application of local anaesthesia: a randomised study. BMC Med Educ. 2021;21(1):1–8. doi: 10.1186/s12909-021-02569-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eglseder K, Littleton A. Teaching clinical skills online: techniques, student feedback, and lesson learned. J Occup Ther Educ. 2021;5(2):11. doi: 10.26681/jote.2021.050211 [DOI] [Google Scholar]
- 6.Stambough JB, Curtin BM, Gililland JM, et al. The past, present, and future of orthopedic education: lessons learned from the COVID-19 pandemic. J Arthroplasty. 2020;35(7):S60–S64. doi: 10.1016/j.arth.2020.04.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gormley G, Collins K, Boohan M, Bickle I, Stevenson M. Is there a place for e-learning in clinical skills? A survey of undergraduate medical students’ experiences and attitudes. Med Teach. 2009;31(1):e6–12. doi: 10.1080/01421590802334317 [DOI] [PubMed] [Google Scholar]
- 8.Rosby V, Schmidt HG, Tan GJS, et al. Promotion of knowledge transfer and retention in year 2 medical students using an online training exercise. Adv Heal Sci Educ. 2021;26:1059–1074. doi: 10.1007/s10459-021-10037-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Turk B, Ertl S, Wong G, Wadowski PP, Löffler-Stastka H. Does case-based blended-learning expedite the transfer of declarative knowledge to procedural knowledge in practice? BMC Med Educ. 2019;19(1). doi: 10.1186/s12909-019-1884-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Regmi K, Jones L. A systematic review of the factors - enablers and barriers - affecting e-learning in health sciences education. BMC Med Educ. 2020;20(1):1–8. doi: 10.1186/s12909-020-02007-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khalil R, Mansour AE, Fadda WA, et al. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: a qualitative study exploring medical students’ perspectives. BMC Med Educ. 2020;20(1):285. doi: 10.1186/s12909-020-02208-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Botelho MG, Agrawal KR, Bornstein MM. An systematic review of e-learning outcomes in undergraduate dental radiology curricula—levels of learning and implications for researchers and curriculum planners. Dentomaxillofacial Radiol. 2019;48(1). doi: 10.1259/dmfr.20180027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen F, Lui AM, Martinelli SM. A systematic review of the effectiveness of flipped classrooms in medical education. Med Educ. 2017;51(6):585–597. doi: 10.1111/medu.13272 [DOI] [PubMed] [Google Scholar]
- 14.Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10(11):e042378. doi: 10.1136/bmjopen-2020-042378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thomas PA, Kern DE, Hughes MT, Chen BY. Curriculum Development for Medical Education: A Six-Step Approach. JHU press; 2015. [DOI] [PubMed] [Google Scholar]
- 16.Kraut AS, Omron R, Caretta-Weyer H, et al. The flipped classroom: a critical appraisal. West J Emerg Med. 2019;20(3):527–536. doi: 10.5811/WESTJEM.2019.2.40979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Michels MEJ, Evans DE, Blok GA. What is a clinical skill? Searching for order in chaos through a modified Delphi process. Med Teach. 2012;34(8):e573–81. doi: 10.3109/0142159X.2012.669218 [DOI] [PubMed] [Google Scholar]
- 18.Adams NE. Bloom’s taxonomy of cognitive learning objectives. J Med Libr Assoc. 2015;103(3):152–153. doi: 10.3163/1536-5050.103.3.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Enoch LC, Abraham RM, Singaram VS. A comparative analysis of the impact of online, blended, and face-to-face learning on medical students’ clinical competency in the affective, cognitive, and psychomotor domains. BMC Med Educ. 2022;22(1):753. doi: 10.1186/s12909-022-03777-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pei L, Wu H. Does online learning work better than offline learning in undergraduate medical education? A systematic review and meta-analysis. Med Educ Online. 2019;24(1). doi: 10.1080/10872981.2019.1666538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Botma Y, Van Rensburg GH, Coetzee IM, Heyns T. A conceptual framework for educational design at modular level to promote transfer of learning. Innov Educ Teach Int. 2015;52(5):499–509. doi: 10.1080/14703297.2013.866051 [DOI] [Google Scholar]
- 22.Prober CG, Khan S. Medical education reimagined: a call to action. Acad Med. 2013;88(10):1407–1410. doi: 10.1097/ACM.0b013e3182a368bd [DOI] [PubMed] [Google Scholar]
- 23.Abraham RM, Singaram VS. Using deliberate practice framework to assess the quality of feedback in undergraduate clinical skills training. BMC Med Educ. 2019;19(1):1–11. doi: 10.1186/s12909-019-1547-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Galoyan T, Betts K. Integrative transfer of learning model and implications for higher education. J Contin High Educ. 2021;69(3):169–191. doi: 10.1080/07377363.2020.1847970 [DOI] [Google Scholar]
- 25.Bossard C, Kermarrec G, Buche C, Tisseau J. Transfer of learning in virtual environments: a new challenge? Virtual Real. 2008;12(3):151–161. doi: 10.1007/s10055-008-0093-y [DOI] [Google Scholar]
- 26.Widyandana D, Majoor G, Scherpbier A. Transfer of medical students’ clinical skills learned in a clinical laboratory to the care of real patients in the clinical setting: the challenges and suggestions of students in a developing country. Educ Heal Chang Learn Pract. 2010;23(3):339. [PubMed] [Google Scholar]
- 27.Karim JA, Marwan YA, Dawas AM, Akhtar S. Self-confidence of medical students in performing clinical skills acquired during their surgical rotation assessing clinical skills education in Kuwait. Saudi Med J. 2012;33(12):1310–1316. [PubMed] [Google Scholar]
- 28.Ellman MS, Schwartz ML. Online learning tools as supplements for basic and clinical science education. J Med Educ Curric Dev. 2016;3:109–114. doi: 10.4137/JMecd.S18933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bordoloi R, Das P, Das K. Perception towards online/blended learning at the time of COVID-19 pandemic: an academic analytics in the Indian context. Asian Assoc Open Univ J. 2021;16(1):41–60. doi: 10.1108/aaouj-09-2020-0079 [DOI] [Google Scholar]
- 30.Abraham R. The need of the hour: adapting the delivery of clinical skills teaching remotely. Perspect Educ. 2021;39(2):82–94. doi: 10.18820/2519593x/pie.v39.i2.7 [DOI] [Google Scholar]
- 31.Kiger ME, Varpio L. Thematic analysis of qualitative data: AMEE guide No. 131. Med Teach. 2020;42(8):846–854. doi: 10.1080/0142159X.2020.1755030 [DOI] [PubMed] [Google Scholar]
- 32.Roopa S, Rani M. Questionnaire designing for a survey. J Indian Orthod Soc. 2012;46(December):273–277. doi: 10.5005/jp-journals-10021-1104 [DOI] [Google Scholar]
- 33.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706QP063OA [DOI] [Google Scholar]
- 34.Tonkin-Crine S, Anthierens S, Hood K, et al. Discrepancies between qualitative and quantitative evaluation of randomised controlled trial results: achieving clarity through mixed methods triangulation. Implement Sci. 2016;11(1):1–8. doi: 10.1186/s13012-016-0436-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang W, Creswell J. The use of mixing procedure of mixed methods in health services research. Med Care. 2013;51(8). doi: 10.1097/MLR.0B013E31824642FD [DOI] [PubMed] [Google Scholar]
- 36.Creswell JW, Creswell J. Steps in conducting a scholarly mixed methods study. DBER Speak Ser; 2013. Availble from: https://digitalcommons.unl.edu/dberspeakers/48. Accessed July 22, 2021.
- 37.Bloomfield JG, Jones A. Using e-learning to support clinical skills acquisition: exploring the experiences and perceptions of graduate first-year pre-registration nursing students - A mixed method study. Nurse Educ Today. 2013;33(12):1605–1611. doi: 10.1016/j.nedt.2013.01.024 [DOI] [PubMed] [Google Scholar]
- 38.Singh J, Steele K, Singh L. Combining the best of online and face-to-face learning: hybrid and blended learning approach for COVID-19, Post vaccine, & post-pandemic world. J Educ Technol Syst. 2021;50(2):140–171. doi: 10.1177/00472395211047865 [DOI] [Google Scholar]
- 39.Shahrvini B, Baxter SL, Coffey CS, MacDonald BV, Lander L. Pre-clinical remote undergraduate medical education during the COVID-19 pandemic: a survey study. BMC Med Educ. 2021;21(1):1–13. doi: 10.1186/s12909-020-02445-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gaur U, Majumder MAA, Sa B, Sarkar S, Williams A, Singh K. Challenges and opportunities of preclinical medical education: COVID-19 crisis and beyond. SN Compr Clin Med. 2020;2(11):1992–1997. doi: 10.1007/s42399-020-00528-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saiyad S, Virk A, Mahajan R, Singh T. Online teaching in medical training: establishing good online teaching practices from cumulative experience. Int J Appl Basic Med Res. 2020;10(3):149–155. doi: 10.4103/ijabmr.IJABMR_358_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rahmani A, Samira Zitouni K. Blended learning and flipped classroom’s application during post pandemic. Arab World English J. 2022;13(2):451–461. doi: 10.24093/awej/vol13no2.31 [DOI] [Google Scholar]
- 43.Gitonga J. Transfer of learning in Continuing Medical Education (CME): a conceptual model. Online Submiss; 2007.
- 44.Brown A, Lawrence J, Basson M, Redmond P. A conceptual framework to enhance student online learning and engagement in higher education. High Educ Res Dev. 2020;41(2):284–299. doi: 10.1080/07294360.2020.1860912 [DOI] [Google Scholar]
- 45.Lawrence J, Brown A, Redmond P, Basson M. Engaging the disengaged: exploring the use of course-specific learning analytics and nudging to enhance online student engagement. Student Success. 2019;10(2):47–58. doi: 10.5204/ssj.v10i2.1295 [DOI] [Google Scholar]
- 46.van Duijn AJ, Swanick K, Donald EK. Student learning of cervical psychomotor skills via online video instruction versus traditional face-to-face instruction. J Phys Ther Educ. 2014;28(1):94–102. [Google Scholar]
- 47.Andersson A, Grönlund Å. A conceptual framework for E-learning in developing countries: a critical review of research challenges. Electron J Inf Syst Dev Ctries. 2009;38(1):1–16. doi: 10.1002/j.1681-4835.2009.tb00271.x [DOI] [Google Scholar]
- 48.Pokryszko-Dragan A, Marschollek K, Nowakowska-Kotas M, Aitken G. What can we learn from the online learning experiences of medical students in Poland during the SARS-CoV-2 pandemic? BMC Med Educ. 2021;21(1):1–12. doi: 10.1186/S12909-021-02884-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mayer RE. Applying the science of learning to medical education. Med Educ. 2010;44(6):543–549. doi: 10.1111/j.1365-2923.2010.03624.x [DOI] [PubMed] [Google Scholar]
- 50.New K, Edwards C, Norris H. Meeting our students’ educational needs during a global pandemic: creating online clinical learning experiences. Teach Learn Nurs. 2022;17(1):126–129. doi: 10.1016/j.teln.2021.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Offiah G, Ekpotu LP, Murphy S, et al. Evaluation of medical student retention of clinical skills following simulation training. BMC Med Educ. 2019;19(1):263. doi: 10.1186/s12909-019-1663-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Anderson JDM, Warren JB. Using simulation to enhance the acquisition and retention of clinical skills in neonatology. Semin Perinatol. 2011;35(2):59–67. doi: 10.1053/j.semperi.2011.01.004 [DOI] [PubMed] [Google Scholar]
- 53.Riedel M, Eisenkolb G, Amann N, et al. Experiences with alternative online lectures in medical education in obstetrics and gynecology during the COVID-19 pandemic-possible efficient and student-orientated models for the future? Arch Gynecol Obstet. 2022;305:1041–1053. doi: 10.1007/s00404-021-06356-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sebbani M, Adarmouch L, Mansouri A, et al. Implementation of online teaching in medical education: lessons learned from students’ perspectives during the health crisis in Marrakesh, Morocco. Educ Res Int. 2021;2021:e5547821. doi: 10.1155/2021/5547821 [DOI] [Google Scholar]
- 55.Sahu P, Chattu V, Rewatkar A, Sakhamuri S. Best practices to impart clinical skills during preclinical years of medical curriculum. J Educ Health Promot. 2019;8(57):57. doi: 10.4103/jehp.jehp_354_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lala SG, George AZ, Wooldridge D, et al. A blended learning and teaching model to improve bedside undergraduate paediatric clinical training during and beyond the COVID-19 pandemic. African J Heal Prof Educ. 2021;13(1):18–22. [Google Scholar]
- 57.George PP, Papachristou N, Belisario JM, et al. Online eLearning for undergraduates in health professions: a systematic review of the impact on knowledge, skills, attitudes and satisfaction. J Glob Health. 2014;4(1):010406. doi: 10.7189/jogh.04.010406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Al-Elq AH. Medicine and clinical skills laboratories. J Family Community Med. 2007;14(2):59–63. [PMC free article] [PubMed] [Google Scholar]
- 59.Azizi SM, Roozbahani N, Khatony A. Factors affecting the acceptance of blended learning in medical education: application of UTAUT2 model. BMC Med Educ. 2020;20(1):367. doi: 10.1186/s12909-020-02302-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Taylor DCM, Hamdy H. Adult learning theories: implications for learning and teaching in medical education: AMEE Guide No. 83. Med Teach. 2013;35(11):1561–1572. doi: 10.3109/0142159X.2013.828153 [DOI] [PubMed] [Google Scholar]
- 61.Giacomino K, Caliesch R, Sattelmayer KM. The effectiveness of the Peyton’s 4-step teaching approach on skill acquisition of procedures in health professions education: a systematic review and metaanalysis with integrated meta-regression. PeerJ. 2020;8:e10129. doi: 10.7717/peerj.10129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ramnanan CJ, Pound LD. Advances in medical education and practice: student perceptions of the flipped classroom. Adv Med Educ Pract. 2017;8:63–73. doi: 10.2147/AMEP.S109037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ali NB, Pelletier SR, Shields HM. Innovative curriculum for second-year harvard-mit medical students: practicing communication skills with volunteer patients giving immediate feedback. Adv Med Educ Pract. 2017;8:337–345. doi: 10.2147/AMEP.S135172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Al-Wardy NM. Assessment methods in undergraduate medical education. Sultan Qaboos Univ Med J. 2010;10(2):203–209. [PMC free article] [PubMed] [Google Scholar]
- 65.Remmen R, Scherpbier A, van der Vleuten C, et al. Effectiveness of basic clinical skills training programmes: a cross-sectional comparison of four medical schools. Med Educ. 2001;35(2):121–128. [DOI] [PubMed] [Google Scholar]
- 66.Schlenz MA, Schmidt A, Wöstmann B, Krämer N, Schulz-Weidner N. Students’ and lecturers’ perspective on the implementation of online learning in dental education due to SARS-CoV-2 (COVID-19): a cross-sectional study. BMC Med Educ. 2020;20(1):354. doi: 10.1186/s12909-020-02266-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Abraham R. Turning constraints into opportunities: online delivery of communication skills simulation sessions to undergraduate medical students during the COVID-19 pandemic. Perspect Educ. 2021;39(4):57–71. doi: 10.18820/2519593X/PIE.V39.I4.5 [DOI] [Google Scholar]
- 68.Baticulon RE, Sy JJ, Alberto NRI, et al. Barriers to online learning in the time of COVID-19: a national survey of medical students in the Philippines. Med Sci Educ. 2021;31(2):615–626. doi: 10.1007/s40670-021-01231-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Engerer C, Berberat PO, Dinkel A, Rudolph B, Sattel H, Wuensch A. Integrating 360° behavior-orientated feedback in communication skills training for medical undergraduates: concept, acceptance and students’ self-ratings of communication competence. BMC Med Educ. 2016;16(1):1–8. doi: 10.1186/S12909-016-0792-0/FIGURES/1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sadler I, Reimann N, Sambell K. Feedforward practices: a systematic review of the literature. Assess Eval High Educ. 2022;47(1):1–16. doi: 10.1080/02602938.2022.2073434 [DOI] [Google Scholar]