Abstract
It is becoming increasingly apparent that poor housing quality affects indoor air quality, significantly impacting on respiratory health in children and young people. Exposure to damp and/or mould in the home, cold homes and the presence of pests and pollutants all have a significant detrimental impact on child respiratory health. There is a complex relationship between features of poor-quality housing, such as being in a state of disrepair, poor ventilation, overcrowding and being cold, that favour an environment resulting in poor indoor air quality. Children living in rented (private or public) housing are more likely to come from lower-income backgrounds and are most at risk of living in substandard housing posing a serious threat to respiratory health. Children have the right to safe and adequate housing, and research has shown that either rehousing or making modifications to poor-quality housing to improve indoor air quality results in improved respiratory health. Urgent action is needed to address this threat to health. All stakeholders should understand the relationship between poor-quality housing and respiratory health in children and act, working with families, to redress this modifiable risk factor.
Educational aims
The reader should understand how housing quality and indoor air quality affect respiratory health in children.
The reader should understand which children are at most risk of living in poor-quality housing.
The reader should understand what policy recommendations have been made and what actions need to be undertaken to improve housing quality and respiratory health in children and young people.
Tweetable abstract
Poor-quality housing negatively impacts the quality of the air that children breathe in their living environment, which is detrimental to their respiratory health. Urgent action is needed to improve housing quality to improve child respiratory health. https://bit.ly/3pshb34
Introduction
In the United Nations Convention on the Rights of the Child (UNCRC), article 27 states that every child has the right to “a standard of living adequate for the child's physical, mental, spiritual, moral and social development” [1]. Further to this, the committee has since committed to evaluating “clean air” in the forthcoming general comment on the UNCRC [2]. In 2019, the UNICEF UK Child Friendly Cities and Communities Team in their “Children's rights in the new normal” campaign laid out recommendations to councils and partners regarding provision of “safe and well-maintained” housing for children and young people (CYP) in relation to article 27 of the UNCRC [3]. Despite this, and the growing evidence of the impact of housing quality on child health, children are still dying from inadequate and unsafe housing and resultant poor-quality air. In 2020, the death of 2-year-old Awaab Ishak in the UK due to mould exposure in his home [4] was a potent and sobering reminder to healthcare professionals of the impact of our patients’ physical environment and the air that they breathe. The inquest into his death concluded that he sadly passed away due to a severe respiratory condition due to prolonged exposure to mould in his home environment [4].
Our understanding of how the quality of the air that we breathe affects our (respiratory) health has increased over the past few decades. What is becoming increasingly apparent is that indoor air quality (IAQ) is an important determinant of respiratory health, particularly for CYP. CYP are extremely vulnerable in terms of effects on respiratory health due to exposure to air pollution [5] as their respiratory and immune systems still undergoing development, leaving them prone to respiratory sequelae and being poorly protected against the hazardous exposure to pollutants [6]. Moreover, children have relatively high respiratory rates [7] and inspire a larger volume of air relative to their body surface area [5], compared with adults. CYP also spend the majority of their time indoors and it is estimated that CYP spend only ∼68 min per day playing outside on average [8]. What has also become apparent is that the quality of the housing in which children and their families live significantly affects the quality of the air that they breathe, and this has a significant negative impact on their respiratory health [8]. It is estimated in the UK that 3.6 million CYP live in poor-quality housing [8]. Throughout this review, we will highlight elements that contribute to housing and IAQ and the effects on respiratory health in CYP, describing which CYP are at most risk. We will then discuss existing policy recommendations to improve housing and IAQ for CYP and what has already been done to address this and discuss the urgent actions that need to be taken next.
What do we mean by “poor-quality housing” and how does it contribute to IAQ?
Poor-quality housing in the UK is generally defined under the “Decent Homes Standard”; if a home cannot provide reasonable thermal comfort, is in a state of disrepair, lacks modern facilities, or has any category 1 housing health and safety rating system hazards (including damp and/or mould that may pose an immediate threat to life), it is deemed unsuitable for living in [9]. Whilst the overall number of decent homes in the UK has improved over the years, almost a quarter of privately rented homes failed this standard in 2021 (compared with a national average of 14% of all homes) [10]. However, the Decent Homes Standard provides a bare minimum of acceptability [9], and therefore will not identify most homes with poor air quality. In the UK, a relatively old housing stock is associated with high rates of structural issues, poor insulation, poor energy efficiency and poor ventilation. The interrelationship between poor-quality housing and IAQ is complex. Elements of poor-quality housing, such as the presence of mould, serves as a direct indoor air pollutant with negative effects on respiratory health [8]. Other elements of housing, such as homes being in a state of disrepair (including leaks) and poor ventilation result in higher levels of moisture and damp, serving as a medium in which biological pollutants such as mould and house dust mites (HDMs) can thrive, having detrimental impacts on IAQ and contributing to indoor air pollution (IAP).
IAP is affected by both indoor and outdoor factors. Sources of IAP can come from outside (e.g. traffic-related air pollution, industrial processes and activity at landfill sites) or from within the home, as described in the joint Royal College of Paediatrics and Child Health and Royal College of Physicians (UK) report “The inside story” [8]. Exposure to IAP depends on the source of pollution and how air is exchanged between inside and outside the home. Focussing specifically on factors of the housing itself (indoor factors), the design of homes/buildings plays an important role; for example, homes designed with open plan kitchens have higher levels of air pollution throughout the home [8, 11]. Different pollutants can also be released from building and construction materials as well as materials use to decorate and manufacture furniture [8]. Flame retardants have also been shown to be linked to health effects [12]. The ventilation within buildings and homes significantly affects IAP. The general principle is to exchange air from inside to outside to reduce the concentration of indoor air pollutants. This can be achieved through opening windows and doors, or by ventilation systems. Some ventilation systems have filters, but it is only high-quality filters that may help in preventing air pollutants from outside entering the home. Within the home, there are numerous processes of normal day-to-day living which contribute to IAP by emitting pollutants such as volatile organic compounds (VOCs), particulate matter (PM), nitrogen oxides (NOx) and carbon monoxide (CO) [8]. Pollutants emitted during cooking processes can be mitigated with adequate and effective ventilation in the form of extractor fans and cooker hoods, however, the filters need to be cleaned regularly for them to remain effective. Cooking with gas hobs, stoves and grills emits higher concentrations of nitrogen dioxide and CO [13]. Burning fuel for a source of heat (e.g. open fires and wood-burning stoves) releases a mixture of gases including CO and as well as VOCs and PM [8].
Higher levels of moisture and dampness on surfaces and in materials precipitates a proliferation of microorganisms, including moulds (and other fungi) and bacteria [14]. Moisture can enter the home from outside, particularly if leaks or flooding are present, and from activities of daily living within the home. Activities of daily living such as showering or dying laundry indoors introduces moisture into the atmosphere and alongside this, cold flooring and walls can enable condensation to be formed. As well as promoting mould growth, moisture promotes increasing numbers of HDMs. Increasing humidity also has a detrimental impact on IAQ as it increases the likelihood of damp and can also precipitate release of formaldehyde from building materials [15]. While activities of daily living can introduce moisture, the Energy Follow Up Survey (EFUS) commissioned by the British government in 2017 found that there was no difference in behaviours such as drying clothes inside, airing the home or bathroom ventilation between the households reporting damp and/or mould compared with those without [16]. The effect of moisture both entering the home from outside and created within the home is potentiated by inadequate ventilation, which traps higher levels of moisture in the home. This moisture then precipitates into condensation on cold surfaces. Cold homes are therefore particularly at risk of damp.
Air that we exhale also affects IAQ. We breathe out carbon dioxide and VOCs which alter the air quality and contribute to air moisture levels. Overcrowding, particularly with low levels of ventilation, potentiates the impact the inhabitants of a home have on IAQ. A study of 567 homes representative of mainland France showed that levels of PM2.5 (particulate matter with aerodynamic diameter <2.5 μm) were 68% higher in high density households compared with low density households, as well as finding significant increases in concentrations of VOCs [17].
How does poor housing and IAP contribute to poor respiratory health in children?
We have described factors that contribute to poor-quality housing which in turn affects IAQ, but how does this affect the respiratory health of CYP? Children who live in poor-quality housing in England are more likely to report poorer health and experience worse respiratory health. This is particularly pronounced in children living in private and social rented housing compared with children living in owner-occupied homes [18]. 22% of the modifiable factors contributing to child deaths in England from April 2019 to March 2020 were due to the child's physical environment, including overcrowding and unsuitable housing (including the presence of damp, mould and being in a state of disrepair). Risk to life from the home environment particularly impacted children living in the highest levels of deprivation, where 35% of all child deaths had identifiable modifiable risk factors compared with 24% of deaths in the wealthiest areas [19].
Whilst there is a wealth of literature regarding outdoor air pollution and effects on respiratory health, evidence regarding the impact of IAP specifically is sparser. As aforementioned, there is a complex relationship between different factors relating to housing quality and IAQ. In the following sections we will describe the effects of exposure to various housing conditions and pollutants on respiratory health in CYP.
Damp and mould
Two systematic reviews have shown a clear association between the presence of damp and mould in the home and risk of wheezing and asthma in infancy and older childhood [20, 21]. Dick et al. [20] in their systematic review of 135 papers consistently found a correlation between visible presence of mould in the home and developing asthma before the age of 9 years (OR 1.5), and an increased risk of wheezing at age 2 years with visible damp or mould (OR 1.4). Cohort studies found children who were exposed to damp in early life were significantly more likely to develop asthma at age 3 years (OR 7.1) [20]. In older children, Castro-Rodriguez et al. [21] in their systematic review with meta-analysis showed that children living in a home with damp or mould were 50% more likely to have asthma or wheezing. Studies from across the globe have shown that up to 14% of childhood asthma is attributable to living in a home with damp or mould [22–24]. A case–control study in New Zealand including 640 children demonstrated that the presence of damp or mould in the home is associated with an increased risk of hospitalisation with pneumonia [25]. A further prospective case–control study in New Zealand assessed the impact of housing quality, with assessors blinded to outcomes using the Respiratory Hazard Index (RHI), on risk of hospital admission from a respiratory tract infection [26]. They showed that a higher RHI was associated with an increased risk for hospitalisation. The damp–mould index showed a dose–response relationship with admission for a respiratory tract infection. They also estimated that by reducing this harmful exposure, the admission rate would have been reduced by 19% [26]. Furthermore, in their data looking at 891 homes in New Zealand using the RHI, they found a dose–response relationship where per each unit increase in the RHI score there was an 11% increased risk of having an episode of wheeze over the last year and an 11% increased risk of having an asthma attack in the last year, after adjusting for crowding index, age, sex and household smoking [27]. In the houses of poorest quality, if the children were moved to better-quality housing there would be an estimated 33% reduction in respiratory symptoms [27]. In their questionnaire-based cross-sectional study, Dales et al. [28] showed that presence of damp or mould in the home was associated with an increased risk of respiratory symptoms. In their meta-analysis with the Institute of Medicine (USA), Fisk et al. [29] showed that in buildings with reported damp or mould there was an associated OR of 2.04 for upper respiratory tract symptoms, OR of 1.65 for cough, OR of 1.66 for wheeze and OR of 1.45 for current asthma compared with buildings without damp or mould. Exposure to mould in the living environment can result in respiratory morbidity by allergic and non-allergic pathways. Mould components such as microbial VOCs and β-glucans could exert pro-inflammatory responses, but by non-IgE-mediated mechanisms. Thus, mould in the living environment can act as an allergen or an irritant to the airways [30].
Overcrowding
Overcrowding occurs when there is a mismatch between household size and dwelling size, and in the UK is defined by either the “room standard” (evaluating the number and sex of occupants sleeping in the same room) or the “space standard” (evaluating the number of occupants against either the number of rooms or floor space). Importantly, this definition focuses on privacy rather than the air quality risks of overcrowding and dismisses the impact overcrowding has on children [31]: children under the age of 10 years either do not count in the room standard or count as less than one person in the space standard. Overcrowding impacts respiratory health by increasing rates of transmission of respiratory infections. A systematic review led by the World Health Organization in 2018 found high certainty evidence that overcrowding increases the risk of respiratory infections and acute respiratory illness, in particular tuberculosis, influenza and respiratory syncytial virus (RSV) in both adult and paediatric populations [32].
Overcrowding also increases the levels of moisture and air pollutants in a home, and this is particularly prevalent in households with a younger average age. A Swedish study reviewing data from apartment buildings, using mathematical simulations of differing occupancy level, found that increasing occupancy correlated to increasing moisture supply [33]. As discussed throughout this review, increased levels of moisture correlate with increased risk of mould. Indeed, a systematic review in 2021 found that overcrowded homes were associated with an increased presence of mould, allergens, pests and increased use of biocides [34]. Causality was difficult to ascertain as: 1) definitions of overcrowding differed between countries; and 2) both overcrowding and poor housing are inextricably linked to socioeconomic deprivation.
Whilst beyond the scope of this review, overcrowding also negatively impacts mental health and educational achievement, and increases the risk of behavioural problems and accidental injury and burns for CYP.
Cold homes
Cold homes happen due to energy inefficient housing stock without proper insulation, and inefficient, expensive or underused heating systems. The implications of cold homes for child health are relatively underexplored in comparison to the effects of cold temperatures on adult health. A national longitudinal study of children in Ireland found that infants living in “affordability related” cold homes were 41% more likely to experience any respiratory illness and 47% more likely to have wheeze [35]. In this study, the association between cold homes and respiratory ill health decreased for older children aged ≥9 years [35]. Cold indoor temperatures have a direct impact on respiratory health, and an indirect impact through increasing risk of damp. Viral survivability improves in colder temperatures, with virus transmission, particularly for RSV and influenza, peaking at temperatures around 5°C in temperate countries such as the UK. Moreover, cold air can impact respiratory tract defences by reducing mucous clearance and causing bronchoconstriction. Colder temperatures may also impact child lung function. In a prospective cohort study of 286 children with asthma in New Zealand, lower bedroom temperatures had a small but significant association with reduction in lung function. This was particularly prevalent at temperatures below a threshold of between 9°C and 11°C [36].
PM and other pollutants
Table 1 demonstrates the sources of PM and other pollutants within the home environment. In a prospective cohort study of 150 children aged 2–6 years diagnosed with asthma in the USA, it was shown that increasing concentrations of PM2.5 and PM2.5–10 (particulate matter with aerodynamic diameter 2.5–10 μm) were associated with increased asthma symptoms and need for reliever medication use [37]. Furthermore, it has been demonstrated in asthmatic children that increasing concentrations of PM2.5 in the home are associated with poorer lung function (decreased percent predicted forced expiratory volume in 1 s/forced vital capacity (FVC) and forced expiratory flow at 25–75% of FVC), and in the same study population, no such association was seen with outdoor concentrations of PM2.5 [38]. Exposure to indoor and outdoor PM2.5 is associated with increased respiratory-related infant mortality [39], and is also related to delayed lung growth [40]. A case–control study in Australia demonstrated that VOC concentrations in the homes of asthmatic children are higher compared with non-asthmatic controls [41]. Looking at patients enrolled in a bronchopulmonary dysplasia registry in the USA, 75% of infants were exposed to at least one type of combustible source of air pollution which was associated with a need for hospitalisation due to respiratory illness [42].
TABLE 1.
Sources of indoor particulate matter
| Outdoor particulate matter (industry, traffic, etc.) |
| Cooking (gas versus induction, cooker hoods) |
| Fireplaces (wood and coal) |
| Combustion heating |
| Smoking or e-cigarette/vaping devices |
| Dust |
| Biological matter (mould spores, house dust mites, pet dander, pest droppings) |
| Scented candles/incense |
| Aerosols (from cleaning, air fresheners, etc.) |
Information from [8].
Poor ventilation
Homes with poor ventilation increase exposure to indoor air pollutants by increasing their concentrations and the length of exposure time. Poor ventilation within homes has been shown to be associated with increased risk of asthma exacerbations and respiratory tract infections in children [43]. Improving ventilation in homes reduces the concentration of HDMs and particulates that can exacerbate respiratory symptoms. It has also been shown that children living in homes with adequate ventilation are at a significantly lower risk of suffering from respiratory tract infections [44].
HDM
Exposure to HDMs has long been described as associated with the prevalence of asthma and as a trigger of symptoms and acute asthma attacks. Exposure to HDM allergen, particularly in atopic children, increases the risk of allergic sensitisation [45], which in turn is an independent risk factor for developing asthma with a dose–response relationship [46, 47]. It has also been demonstrated in asthmatic children with evidence of sensitisation to HDM that exposure to higher levels of HDM is associated with a greater degree of airway hyperresponsiveness [46, 48].
Pests
The presence of pests including cockroaches and rats poses a serious risk for children with asthma, particularly in those living in substandard housing [49]. Across eight inner-city regions in the USA, it has been shown that for children with asthma having evidence of allergic sensitisation to cockroach allergen and being exposed to high levels of this allergen meant they were 3.5 times more likely to be hospitalised with asthma and more likely to make unscheduled healthcare visits due to asthma, as well as having significantly more days of wheezing and missed school days [50]. Presence of reported rats is associated with an increased risk of current asthma diagnosis in children [51]. Exposure to mouse antigen in those sensitised is associated with emergency healthcare use due to asthma [52].
Housing in a state of disrepair (including holes in ceilings or walls, leaks and water damage) has been shown to be associated with increased levels of cockroach allergen [53]. Substandard public housing in Boston (USA), which was in a state of disrepair was found to have higher levels of cockroach allergen [54]. Neighbourhood socioeconomic status (SES) level was found to be lowest for families living in public housing and this housing was more likely to be inhabited by families of ethnic minorities. Moreover, children living in public housing were found to be more likely to have asthma [51].
Which children are at most risk of poor respiratory health due to poor-quality housing?
CYP are more likely to live in poor-quality housing than families with no dependent children [16]. The UK EFUS survey in 2017 found that 39% of households with dependent children reported damp and mould compared with 23% of households without children [16]. Lone parent households were particularly at risk, with 48% of respondents experiencing damp and/or mould [16]. Similarly, the 2022 English Housing Survey (EHS) found that overcrowding disproportionately impacts children in England, with 68% of overcrowded households containing dependent children [55]. In this section, we will review which children are more likely to be exposed to poor IAQ through living in poor-quality homes, and which children are clinically most susceptible to the impact of poor IAQ.
Low-income families
Families with low income are at particular risk of the effects of poor housing quality and its contribution to adverse respiratory health. First, low-income families are more likely to live in areas of high outdoor pollution, despite creating the least air pollution: 66% of all carcinogenic air pollutants produced in England are emitted into the most deprived areas of the country [56], where it then enters homes and contributes to IAP. Secondly, low-income families have increased exposure to air pollutants created indoors, as they are more likely to live in non-decent homes (as per the Decent Homes Standard) [57], and are more likely to live in flats in high density, multi-unit buildings and therefore have higher exposure to pollutants from neighbouring households [58]. Families living below the poverty threshold in England are twice as likely as the national average to live in damp, overcrowded homes [59], and 16 times more likely than the wealthiest quintile [60]. Thirdly, children from low-income families are likely to spend more time at home than their wealthier counterparts, as their families face barriers to accessing after school clubs and extracurricular activities [58].
Home ownership status
Children in renting households are at higher risk of living in homes with poor air quality than children whose family own their home. Renting families may have less control over repairs or modifications to the home, and landlords may not fully understand or appreciate the potential health effects for the family caused by poor-quality housing or have the impetus to dedicate costs needed for home improvements. In the UK, Citizen's Advice found in 2018 that renters who complained about damp or mould in their home had an almost 50% risk of being evicted in the 6 months following the complaint [61]. In 2021–2022, the EHS found that 11% of privately rented homes were estimated to have damp, over twice as high as rates in social housing (4%) and five-times higher than rates in owner-occupied homes (2%) [10]. Overcrowding in homes is also a rising risk to children in rented properties in the UK. Overcrowding in rented properties (both social and private) has almost doubled in the past 20 years. 8% of social housing, 5% of private rentals and just 1% of owner-occupied homes were deemed overcrowded in 2021; however, current estimates are probably an underestimate as the EHS and census data do not consider bedroom size and include communal areas such as living rooms.
Young children
Throughout this review, we have discussed why CYP are a very vulnerable group in terms of the impact of poor housing quality on respiratory health. When considering exposure to damp and/or mould, it has been demonstrated that younger children are more vulnerable to effects on respiratory health [20, 27]. Being housed in a cold home was found to be a greater risk to respiratory health for children under 9 years of age [35] and living in overcrowded housing a greater risk for children under 10 years of age as, in the UK, they are not counted in the room standard, or count as less than one person in the space standard.
Antenatal determinants of poor respiratory health
When considering children at risk of poorer respiratory health due to the contribution of poor-quality housing, it is important to first consider antenatal determinants of lung development and the environment in which the mother lives when she is pregnant. Evidence assessing the effects of intrauterine exposure to IAP specifically is lacking. In terms of IAP originating from sources within the home, Lee et al. [62] demonstrated that per unit increase in prenatal CO exposure in expectant mothers, there were poorer lung function measures in their children. As described above, IAQ is affected by numerous factors, including outdoor pollutants entering the home. Intrauterine exposure to PM is associated with reduced lung function in the newborn [63] and preschool period [64]. Children born to mothers who were exposed to higher levels of PM during their pregnancy have a higher risk of wheezing at in infancy [65] and increased risk of asthma in childhood [66]. Furthermore, intrauterine exposure to PM is also associated with increased risk of respiratory tract infections in childhood [67]. In these studies, exposure is based on PM associated with outdoor air pollution, mainly traffic-related air pollution [62].
How can we address respiratory ill health associated with poor-quality housing?
First and foremost, it is imperative that all stakeholders appreciate the relationship between housing quality and respiratory health in children, including medical and healthcare professionals, councils and government, building industries, housing associations and landlords or providers of accommodation (table 2). As highlighted at the beginning of this review, a relatively old and energy inefficient housing stock in England contributes to poor housing, and poorly installed/single measure retrofitting to address energy efficiency can inadvertently exacerbate health impacts of inadequate ventilation [69]. Whilst beyond the scope of this review, incorporating gold standards such as Passivhaus low energy design/retrofitting standards into UK Building Regulations will contribute to a much more health- and eco-friendly housing stock [68]. It is also imperative that all stakeholders understand the inequalities in terms of exposure to poor-quality housing.
TABLE 2.
Multilevel action to address housing-associated child health
| In healthcare |
| Ensure housing and living environment incorporated into all aspects of clinical care |
| Specialist clinics designed to address housing issues and how these relate to poorer (respiratory) health outcomes (e.g. Alder Hey Children's Hospital (UK) Clean Air Clinic) |
| Research linking health and environmental data, specifically focussed on antenatal and child health |
| In the building industry |
| Affordable new homes and retrofitting in keeping with gold standards [68] |
| At local council and government level |
| Better regulation of housing standards and tenants' rights |
| Joined health and housing departments |
| UNICEF child's rights impact assessments for housing policies [3] |
UNICEF: United Nations Children's Fund.
Lockdown restrictions during the coronavirus disease 2019 pandemic highlighted huge inequalities in housing and the impact this had on CYP. In response, UNICEF UK published the “Children's rights in the new normal” report series, identifying how local authorities should build back better for CYP [3]. Using a child rights-based approach in all aspects of housing policies and planning is at the heart of UNICEF's recommendations, including use of a child rights impact assessment. The report specifically identifies marginalised communities of children, particularly those living in unregulated accommodation (such as unaccompanied asylum-seeking CYP, care leavers and homeless 16–17 year-olds) [3].
As discussed, families who rent their homes are most at risk of living in poor-quality homes. As such, nongovernmental organisations such as Shelter (in the UK) have been campaigning for better rights for tenants for a number of years. In 2022, the government announced the Renters Reform Bill and the Social Housing Regulations Bill. However, the Social Housing Regulations Bill was tabled in February 2023 to focus on “Awaab's law” to specifically address the issue of damp and mould in social housing.
Research has shown that addressing poor-quality housing by either rehousing or making modifications to the home results in improved respiratory health outcomes in CYP. For example, in the USA, home repairs to remediate damp, poor ventilation and poor heating resulted in improved respiratory symptoms [70]. A further intervention whereby families who rented their home were moved to “asthma-friendly” homes with features such as moisture-proof exteriors, ventilation and heating systems and interior finishes designed to not allow accumulation of dust resulted in improved nocturnal symptoms in children with asthma [71]. An initiative whereby structured assessments were made within homes and improvements to damp/mould, heating and ventilation were shown to result in improved quality of life, reduction in symptoms and reduction in costs associated with hospitalisation due to asthma [72]. The Community Asthma Prevention Programme in Philadelphia (USA) incorporated a community-based approach to education and interventions to remediate exposures to asthma triggers in the home. Partnerships were formed with home repair companies to make structural changes to reduce the exposure of indoor asthma triggers caused by structural deficiencies such as holes in ceilings and walls, and leaks. After these repairs, the number reporting presence of pests such as rats and cockroaches significantly decreased as did reports of asthma symptoms and healthcare utilisation due to asthma [73].
Putting it all together
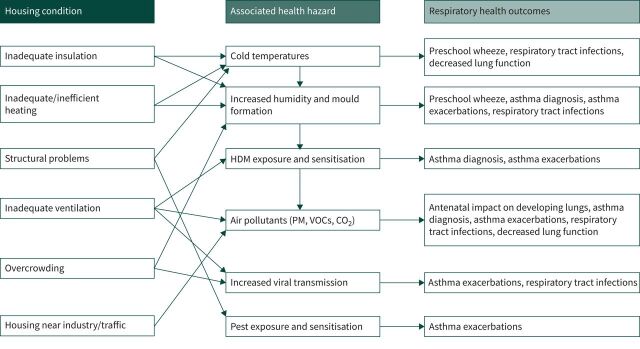
Throughout this review we have highlighted the determinants of IAQ and how this relates to housing quality and how poor housing quality contributes significantly to poorer respiratory health in children (figure 1). The story does not necessarily start in childhood, however, as there is compelling, albeit limited, evidence suggesting that the effects of poor air quality on respiratory health in children starts in utero. We must also consider not only the homes that children live in, but the homes of pregnant women too. Children at risk of poor respiratory health due to poor housing quality include those who are from lower-income backgrounds and younger children.
FIGURE 1.
How poor housing impacts paediatric respiratory health. HDM: house dust mite; PM: particulate matter; VOCs: volatile organic compounds; CO2: carbon dioxide.
As described above and as demonstrated in table 2, there is need for multilevel action to address the issue of poor-quality housing for CYP. For clinicians this means that there is a need for assessments of housing and IAQ in routine clinical assessments. Specialist clinics for CYP who have significant health issues which are felt to be related to the environment in which they live have been developed in the UK, the first of which is based at Alder Hey Children's Hospital (Liverpool, UK). Here, a specialist assessment of how poor-quality housing and IAQ contributes to their respiratory morbidity means that families can take away detailed reports to support them with seeking improvements or better-quality housing with either their private landlords or council-managed accommodation. As clinicians we are not legal experts; however, what we can do is link, in an evidence-based way, the exposure (poor-quality housing) to the detrimental health outcomes that these CYP face.
Further research into how interventions for families that live in poor-quality housing can remediate problems to improve respiratory health needs to be undertaken. Significant changes need to be undertaken at governmental and council level to ensure that accommodation provided by housing associations/councils and by landlords is of a quality that will not contribute to poorer respiratory health. This is in keeping with the UNCRC and UNICEF's guidance on the child's right to have adequate housing for their physical development [1, 3]. Stakeholders should also work with families to empower them if they report difficulties with their home, supporting them to address these issues.
Key points
Poor-quality housing results in poor indoor air quality, which significantly negatively affects respiratory health in children and young people.
Children and young people from lower-income backgrounds are most at risk of living in poor-quality housing.
Addressing the threat of living in poor-quality housing, through either rehousing or modifications within the home, results in improved respiratory outcomes for children.
Urgent action is needed from all stakeholders to understand the effect of poor-quality housing on respiratory health in children and take action to redress these issues.
Footnotes
Conflict of interest: K.A. Holden was Co-Principal Investigator for a feasibility study on use of Rensair Ltd air purifiers in homes of children with asthma (he received no payments or donations for conducting this study and the air purifiers were not donated). A.R. Lee reports receiving grants from HDRUK, and NHS England Health and Wellbeing Fund, outside the submitted work; and support for attending a meeting received from Asthma and Lung UK travel grant, outside the submitted work. D.B. Hawcutt reports receiving grants from NIHR, outside the submitted work; payment for expert testimony (no further details provided), disclosure made outside the submitted work; is Chair of RCPCH/NPPG joint standing committee on medicines, and a member of MHRA expert advisory groups, disclosures made outside the submitted work. I.P. Sinha was Co-Principal Investigator for a feasibility study on use of Rensair Ltd air purifiers in homes of children with asthma (he received no payments or donations for conducting this study and the air purifiers were not donated).
Support statement: No funding was received for this work, and it is supported by the NIHR Alder Hey Clinical Research Facility. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
References
- 1.United Nations . Convention on the Rights of the Child. Geneva, United Nations, 1989. https://www.ohchr.org/en/instruments-mechanisms/instruments/convention-rights-child [Google Scholar]
- 2.Global Action Plan . UN acknowledges children's demand for right to clean air. Date last updated: 17 November 2021. www.globalactionplan.org.uk/news/un-acknowledges-children-s-demand-for-right-to-clean-air
- 3.UNICEF UK . Children's rights in the new normal: 5. housing. Date last updated: February 2022. www.unicef.org.uk/child-friendly-cities/wp-content/uploads/sites/3/2022/02/5.-Housing_UNICEF-UK-New-Normal-series.pdf
- 4.BBC News . Awaab Ishak: Mould in Rochdale flat caused boy's death, coroner rules. Date last updated: 15 November 2022. www.bbc.co.uk/news/uk-england-manchester-63635721
- 5.Sly PD, Flack F. Susceptibility of children to environmental pollutants. Ann N Y Acad Sci 2008; 1140: 163–183. doi: 10.1196/annals.1454.017 [DOI] [PubMed] [Google Scholar]
- 6.Heinrich J, Slama R. Fine particles, a major threat to children. Int J Hyg Environ Health 2007; 210: 617–622. doi: 10.1016/j.ijheh.2007.07.012 [DOI] [PubMed] [Google Scholar]
- 7.Kim JJ. Ambient air pollution: health hazards to children. Pediatrics 2004; 114: 1699–1707. doi: 10.1542/peds.2004-2166 [DOI] [PubMed] [Google Scholar]
- 8.Royal College of Paediatrics and Child Health, Royal College of Physicians . The inside story: Health effects of indoor air quality on children and young people. London, Royal College of Paediatrics and Child Health, 2020. www.rcpch.ac.uk/sites/default/files/2020-01/the-inside-story-report_january-2020.pdf [Google Scholar]
- 9.UK Government, Department for Levelling Up, Housing and Communities and Ministry of Housing, Communities and Local Government . Decent Homes Standard: review. Date last updated: 8 February 2021. www.gov.uk/guidance/decent-homes-standard-review
- 10.UK Government, Department for Levelling Up, Housing and Communities . English Housing Survey 2021 to 2022: headline report. Date last updated: 15 December 2022. www.gov.uk/government/statistics/english-housing-survey-2021-to-2022-headline-report
- 11.O'Leary C, de Kluizenaar Y, Jacobs P, et al. Investigating measurements of fine particle (PM2.5) emissions from the cooking of meals and mitigating exposure using a cooker hood. Indoor Air 2019; 29: 423–438. doi: 10.1111/ina.12542 [DOI] [PubMed] [Google Scholar]
- 12.Hoffman K, Lorenzo A, Butt CM, et al. Exposure to flame retardant chemicals and occurrence and severity of papillary thyroid cancer: a case-control study. Environ Int 2017; 107: 235–242. doi: 10.1016/j.envint.2017.06.021 [DOI] [PubMed] [Google Scholar]
- 13.Raw GJ, Coward SKD, Brown VM, et al. Exposure to air pollutants in English homes. J Expo Sci Environ Epidemiol 2004; 14: S85–S94. doi: 10.1038/sj.jea.7500363 [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization, Regional Office for Europe . WHO guidelines for indoor air quality: dampness and mould. Copenhagen, World Health Organization, Regional Office for Europe, 2009. https://apps.who.int/iris/handle/10665/164348 [PubMed] [Google Scholar]
- 15.Haghighat F, De Bellis L. Material emission rates: literature review, and the impact of indoor air temperature and relative humidity. Build Environ 1998; 33: 261–277. doi: 10.1016/S0360-1323(97)00060-7 [DOI] [Google Scholar]
- 16.UK Government, Department for Energy Security and Net Zero and Department for Business, Energy and Industrial Strategy . Energy Follow Up Survey (EFUS) 2017 reports. Date last updated: 17 September 2021. www.gov.uk/government/publications/energy-follow-up-survey-efus-2017-reports
- 17.Brown T, Dassonville C, Derbez M, et al. Relationships between socioeconomic and lifestyle factors and indoor air quality in French dwellings. Environ Res 2015; 140: 385–396. doi: 10.1016/j.envres.2015.04.012 [DOI] [PubMed] [Google Scholar]
- 18.Barnes M, Cullinane C, Scott S, et al. People living in bad housing – numbers and health impacts. Date last updated: October 2013. https://england.shelter.org.uk/professional_resources/policy_and_research/policy_library/people_living_in_bad_housing_-_numbers_and_health_impacts
- 19.Odd D, Stoianova S, Sleap V, et al. Child Mortality and Social Deprivation: National Child Mortality Database Programme Thematic Report. Data from April 2019 to March 2020. Date last updated: May 2021. https://ncmd.info/wp-content/uploads/2021/05/NCMD-Child-Mortality-and-Social-Deprivation-report_20210513.pdf
- 20.Dick S, Friend A, Dynes K, et al. A systematic review of associations between environmental exposures and development of asthma in children aged up to 9 years. BMJ Open 2014; 4: e006554. doi: 10.1136/bmjopen-2014-006554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Castro-Rodriguez JA, Forno E, Rodriguez-Martinez CE, et al. Risk and protective factors for childhood asthma: what is the evidence? J Allergy Clin Immunol Pract 2016; 4: 1111–1122. doi: 10.1016/j.jaip.2016.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bjerg A, Rönmark E. Asthma in school age: prevalence and risk factors by time and by age. Clin Respir J 2008; 2: Suppl., 123–126. doi: 10.1111/j.1752-699X.2008.00095.x [DOI] [PubMed] [Google Scholar]
- 23.Cibella F, Cuttitta G, La Grutta S, et al. Proportional Venn diagram and determinants of allergic respiratory diseases in Italian adolescents. Pediatr Allergy Immunol 2011; 22: 60–68. doi: 10.1111/j.1399-3038.2010.01097.x [DOI] [PubMed] [Google Scholar]
- 24.Knibbs LD, Woldeyohannes S, Marks GB, et al. Damp housing, gas stoves, and the burden of childhood asthma in Australia. Med J Aust 2018; 208: 299–302. doi: 10.5694/mja17.00469 [DOI] [PubMed] [Google Scholar]
- 25.Grant CC, Emery D, Milne T, et al. Risk factors for community-acquired pneumonia in pre-school-aged children. J Paediatr Child Health 2012; 48: 402–412. doi: 10.1111/j.1440-1754.2011.02244.x [DOI] [PubMed] [Google Scholar]
- 26.Ingham T, Keall M, Jones B, et al. Damp mouldy housing and early childhood hospital admissions for acute respiratory infection: a case control study. Thorax 2019; 74: 849–857. doi: 10.1136/thoraxjnl-2018-212979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Keall MD, Crane J, Baker MG, et al. A measure for quantifying the impact of housing quality on respiratory health: a cross-sectional study. Environ Health 2012; 11: 33. doi: 10.1186/1476-069X-11-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dales RE, Zwanenburg H, Burnett R, et al. Respiratory health effects of home dampness and molds among canadian children. Am J Epidemiol 1991; 134: 196–203. doi: 10.1093/oxfordjournals.aje.a116072 [DOI] [PubMed] [Google Scholar]
- 29.Fisk WJ, Lei-Gomez Q, Mendell M. Meta-analyses of the associations of respiratory health effects with dampness and mold. Indoor Air 2007; 17: 284–296. doi: 10.1111/j.1600-0668.2007.00475.x [DOI] [PubMed] [Google Scholar]
- 30.Flamant-Hulin M, Annesi-Maesano I, Caillaud D. Relationships between molds and asthma suggesting non-allergic mechanisms. A rural-urban comparison. Pediatr Allergy Immunol 2013; 24: 345–351. doi: 10.1111/pai.12082 [DOI] [PubMed] [Google Scholar]
- 31.Holgate S, Grigg J, Arshad H, et al. Health effects of indoor air quality on children and young people. In: Harrison RM, ed. Environmental Pollutant Exposures and Public Health. Cambridge, The Royal Society of Chemistry, 2020; pp. 151–188. [Google Scholar]
- 32.World Health Organization . WHO housing and health guidelines: recommendations to promote healthy housing for a sustainable and equitable future. Date last updated: 23 November 2018. www.who.int/publications/i/item/9789241550376
- 33.Mjörnell K, Johansson D, Bagge H. The effect of high occupancy density on IAQ, moisture conditions and energy use in apartments. Energies (Basel) 2019; 12: 4454. doi: 10.3390/en12234454 [DOI] [Google Scholar]
- 34.Lorentzen JC, Johanson G, Björk F, et al. Overcrowding and hazardous dwelling condition characteristics: a systematic search and scoping review of relevance for health. Int J Environ Res Public Health 2022; 19: 15542. 10.3390/ijerph192315542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mohan G. Young, poor, and sick: the public health threat of energy poverty for children in Ireland. Energy Res Soc Sci 2021; 71: 101822. doi: 10.1016/j.erss.2020.101822 [DOI] [Google Scholar]
- 36.Pierse N, Arnold R, Keall M, et al. Modelling the effects of low indoor temperatures on the lung function of children with asthma. J Epidemiol Community Health 2013; 67: 918–925. doi: 10.1136/jech-2013-202632 [DOI] [PubMed] [Google Scholar]
- 37.McCormack MC, Breysse PN, Matsui EC, et al. Indoor particulate matter increases asthma morbidity in children with non-atopic and atopic asthma. Ann Allergy Asthma Immunol 2011; 106: 308–315. doi: 10.1016/j.anai.2011.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Isiugo K, Jandarov R, Cox J, et al. Indoor particulate matter and lung function in children. Sci Total Environ 2019; 663: 408–417. doi: 10.1016/j.scitotenv.2019.01.309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Woodruff TJ, Parker JD, Schoendorf KC. Fine particulate matter (PM2.5) air pollution and selected causes of postneonatal infant mortality in California. Environ Health Perspect 2006; 114: 786–790. doi: 10.1289/ehp.8484 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gauderman WJ, Avol E, Gilliland F, et al. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med 2004; 351: 1057–1067. doi: 10.1056/NEJMoa040610 [DOI] [PubMed] [Google Scholar]
- 41.Rumchev K. Association of domestic exposure to volatile organic compounds with asthma in young children. Thorax 2004; 59: 746–751. doi: 10.1136/thx.2003.013680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rice JL, McGrath-Morrow SA, Collaco JM. Indoor air pollution sources and respiratory symptoms in bronchopulmonary dysplasia. J Pediatr 2020; 222: 85–90.e2. doi: 10.1016/j.jpeds.2020.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Edwards RT, Neal RD, Linck P, et al. Enhancing ventilation in homes of children with asthma: cost-effectiveness study alongside randomised controlled trial. Br J Gen Pract 2011; 61: e733–e741. doi: 10.3399/bjgp11X606645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Qian Z. Factor analysis of household factors: are they associated with respiratory conditions in Chinese children? Int J Epidemiol 2004; 33: 582–588. doi: 10.1093/ije/dyg278 [DOI] [PubMed] [Google Scholar]
- 45.Lau S, Falkenhorst G, Weber A, et al. High mite-allergen exposure increases the risk of sensitization in atopic children and young adults. J Allergy Clin Immunol 1989; 84: 718–725. doi: 10.1016/0091-6749(89)90300-X [DOI] [PubMed] [Google Scholar]
- 46.Peat JK, Tovey E, Toelle BG, et al. House dust mite allergens. A major risk factor for childhood asthma in Australia. Am J Respir Crit Care Med 1996; 153: 141–146. doi: 10.1164/ajrccm.153.1.8542107 [DOI] [PubMed] [Google Scholar]
- 47.Sporik R, Chapman MD, Platts-Mills TA. House dust mite exposure as a cause of asthma. Clin Exp Allergy 1992; 22: 897–906. doi: 10.1111/j.1365-2222.1992.tb02062.x [DOI] [PubMed] [Google Scholar]
- 48.Custovic A, Taggart S, Francis H, et al. Exposure to house dust mite allergens and the clinical activity of asthma. J Allergy Clin Immunol 1996; 98: 64–72. doi: 10.1016/S0091-6749(96)70227-0 [DOI] [PubMed] [Google Scholar]
- 49.Wang J, Visness CM, Calatroni A, et al. Effect of environmental allergen sensitization on asthma morbidity in inner-city asthmatic children. Clin Exp Allergy 2009; 39: 1381–1389. doi: 10.1111/j.1365-2222.2009.03225.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rosenstreich DL, Eggleston P, Kattan M, et al. The role of cockroach allergy and exposure to cockroach allergen in causing morbidity among inner-city children with asthma. N Engl J Med 1997; 336: 1356–1363. doi: 10.1056/NEJM199705083361904 [DOI] [PubMed] [Google Scholar]
- 51.Northridge J, Ramirez OF, Stingone JA, et al. The role of housing type and housing quality in urban children with asthma. J Urban Health 2010; 87: 211–224. doi: 10.1007/s11524-009-9404-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Matsui EC, Eggleston PA, Buckley TJ, et al. Household mouse allergen exposure and asthma morbidity in inner-city preschool children. Ann Allergy Asthma Immunol 2006; 97: 514–520. doi: 10.1016/S1081-1206(10)60943-X [DOI] [PubMed] [Google Scholar]
- 53.Rauh VA, Chew GR, Garfinkel RS. Deteriorated housing contributes to high cockroach allergen levels in inner-city households. Environ Health Perspect 2002; 110: Suppl. 2, 323–327. doi: 10.1289/ehp.02110s2323 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Peters JL, Levy JI, Rogers CA, et al. Determinants of allergen concentrations in apartments of asthmatic children living in public housing. J Urban Health 2007; 84: 185–197. doi: 10.1007/s11524-006-9146-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wilson W, Barton C. Overcrowded housing (England). Date last updated: 15 June 2021. https://researchbriefings.files.parliament.uk/documents/SN01013/SN01013.pdf
- 56.Marmot M. Fair society, healthy lives: the Marmot Review: strategic review of health inequalities in England post-2010 . The Marmot Review, 2010. https://www.parliament.uk/globalassets/documents/fair-society-healthy-lives-full-report.pdf
- 57.The Health Foundation . Inequalities between groups of people living in non-decent homes. Date last updated: 27 April 2023. www.health.org.uk/evidence-hub/housing/housing-quality/inequalities-in-who-lives-in-non-decent-homes
- 58.Ferguson L, Taylor J, Zhou K, et al. Systemic inequalities in indoor air pollution exposure in London, UK. Build Cities 2021; 2: 425–448. doi: 10.5334/bc.100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Balogun B, Rankl F, Wilson W. Health inequalities: Cold or damp homes. London, House of Commons Library, 2023. https://researchbriefings.files.parliament.uk/documents/CBP-9696/CBP-9696.pdf [Google Scholar]
- 60.The Health Foundation . Overcrowding is highest for those with low incomes. Date last updated: 13 May 2020. www.health.org.uk/news-and-comment/charts-and-infographics/overcrowding-is-highest-for-those-with-low-incomes
- 61.Sharma R. Why are private renters still waiting for reform? Date last updated: 13 February 2023. https://blog.shelter.org.uk/2023/02/private-renters-waiting-for-reform/
- 62.Lee AG, Kaali S, Quinn A, et al. Prenatal household air pollution is associated with impaired infant lung function with sex-specific effects. Evidence from GRAPHS, a cluster randomized cookstove intervention trial. Am J Respir Crit Care Med 2019; 199: 738–746. doi: 10.1164/rccm.201804-0694OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Latzin P, Roosli M, Huss A, et al. Air pollution during pregnancy and lung function in newborns: a birth cohort study. Eur Respir J 2009; 33: 594–603. doi: 10.1183/09031936.00084008 [DOI] [PubMed] [Google Scholar]
- 64.Jedrychowski WA, Perera FP, Maugeri U, et al. Effect of prenatal exposure to fine particulate matter on ventilatory lung function of preschool children of non-smoking mothers. Paediatr Perinat Epidemiol 2010; 24: 492–501. doi: 10.1111/j.1365-3016.2010.01136.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jedrychowski WA, Perera FP, Maugeri U, et al. Intrauterine exposure to polycyclic aromatic hydrocarbons, fine particulate matter and early wheeze. Prospective birth cohort study in 4-year olds. Pediatr Allergy Immunol 2010; 21: e723–e732. doi: 10.1111/j.1399-3038.2010.01034.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Deng Q, Lu C, Li Y, et al. Exposure to outdoor air pollution during trimesters of pregnancy and childhood asthma, allergic rhinitis, and eczema. Environ Res 2016; 150: 119–127. doi: 10.1016/j.envres.2016.05.050 [DOI] [PubMed] [Google Scholar]
- 67.Jedrychowski WA, Perera FP, Spengler JD, et al. Intrauterine exposure to fine particulate matter as a risk factor for increased susceptibility to acute broncho-pulmonary infections in early childhood. Int J Hyg Environ Health 2013; 216: 395–401. doi: 10.1016/j.ijheh.2012.12.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Energy Saving Trust . What is Passivhaus? The gold standard in energy efficiency. Date last updated: 25 July 2022. https://energysavingtrust.org.uk/passivhaus-what-you-need-know/
- 69.The London Assembly . Turning up the heat on cold, damp and mouldy homes. Date last updated: 27 February 2019. www.london.gov.uk/programmes-strategies/turning-heat-cold-damp-and-mouldy-homes
- 70.Turcotte DA, Alker H, Chaves E, et al. Healthy homes: in-home environmental asthma intervention in a diverse urban community. Am J Public Health 2014; 104: 665–671. doi: 10.2105/AJPH.2013.301695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kercsmar CM, Dearborn DG, Schluchter M, et al. Reduction in asthma morbidity in children as a result of home remediation aimed at moisture sources. Environ Health Perspect 2006; 114: 1574–1580. doi: 10.1289/ehp.8742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Takaro TK, Krieger J, Song L, et al. The breathe-easy home: the impact of asthma-friendly home construction on clinical outcomes and trigger exposure. Am J Public Health 2011; 101: 55–62. doi: 10.2105/AJPH.2010.300008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Bryant-Stephens TC, Strane D, Robinson EK, et al. Housing and asthma disparities. J Allergy Clin Immunol 2021; 148: 1121–1129. doi: 10.1016/j.jaci.2021.09.023 [DOI] [PMC free article] [PubMed] [Google Scholar]