CS‐74‐CAB
Ventricular tachycardia from a right apical coarse trabeculation
Fengyuan Yu; Lijie Mi; Min Tang
Fuwai Hospital, China
A 31‐year‐old male was admitted for asymptomatic ventricular tachycardia (VT) for 2 years, as revealed by Holter. Echocardiography was normal. The earliest ventricular activation was mapped at the right apex, with a satisfying pace‐mapping. Electroanatomic mapping and intracardiac echocardiography discovered the target was inside a recess. The VT disappeared after ablated with 30 W. Reconstruction of post‐ablation cardiac CT revealed a right apical occupying lesion (2.6 × 9.5 mm). Together with cardiac MRI, it was considered to be a coarse trabeculation and separated the adjacent space into recesses. Low density was detected on the trabeculation, arguably edema from the ablation. The patient remained free of VT 3 months after ablation. VT from the right apex or big trabeculation was rarely reported. Cardiac occupancy needs to be differentiated from neoplasms. However, the continuity with other trabeculation and non‐specific density supported the diagnosis of trabeculation in this case.

CS‐84‐CAB
A case of entrapment of quadripolar catheter within advisor HD grid catheter
June Namgung; Jae‐Jin Kwak
Inje University Ilsan Paik Hospital, Goyang‐si, South Korea
Complications of device entrapment during catheter ablation have been reported occasionally. The Advisor HD grid is a confined cellular structure, so other catheters can get stuck during catheter ablation. There is such a possibility, so the phrase to be careful is specified in the manual. A 67‐year‐old male patient experienced a 6Fr. quadripolar catheter getting caught in the HD grid during atrial fibrillation. The catheter was safely and successfully removed and the arrhythmia procedure was successfully completed. Therefore, we discussed what to be careful about to prevent these complications.
CS‐113‐CAB
A late‐onset coronary artery spasm triggered ventricular fibrillation after radiofrequency catheter ablation for atrial fibrillation in a young patient
Fengxiang Zhang; Xinguang Chen; Yangming Mao
The First Affiliated Hospital with Nanjing Medical University, Nanjing, China
A 44‐year‐old man with symptomatic drug‐refractory persistent AF accepted ablation. He suffered restlessness and disconsciousness 2 h after atria intensive stepwise ablation including complete isolation of four pulmonary veins (PV), posterior wall box line, tricuspid and mitral isthmus line, the coronary sinus and superior vena cava isolation and attempted six direct current (DC) cardioversions. Electrocardiogram (ECG) demonstrated a ST‐segment elevation in the inferior leads (II, III, and aVF) with AF rhythm (Figure 1A). Then ventricular tachycardia (VT) and ventricular fibrillation (VF) occurred. Amiodarone was intravenous infused after the procedure. Coronary vasospasm (CV) was suspected after ST‐segment elevation in the inferior leads, and then VT/VF occurred. He had recurrent VF and was treated by DC defibrillation. Meanwhile, cardiopulmonary resuscitation was performed, and an emergency temporary pacemaker was successfully placed in the right ventricular. Coronary angiography revealed severe vasospasm of the proximal, middle and distal segments of right coronary artery (RCA) (Figure 1C). Nitroglycerin (200 μg) was intracoronary administered, which greatly relieved the spasm. There were no residual obstructions with air bubbles or thrombus of RCA (Figure 1D). Subsequently, blood pressure and general condition stabilized. ECG did not show subsequent abnormal Q wave or ST‐T changes (Figure 1B). He recovered without any neurological sequelae, and was discharged.
CS‐123‐CAB
A delayed victory over the summit
Yuen Hoong Phang; Kenneth Kay Leong Khoo; Ahmad Faiz Ezanee; Chee Wei Leong; Fatin Nabilah Azizan; Saravanan Krishinan; Kantha Rao Narasamuloo
Hospital Sultanah Bahiyah, Alor Setar, Malaysia
Background: LV summit is a common site of LV‐origin PVC. Catheter ablation (CA) is curative, but its location poses multiple challenges to successful ablation. The resolution of PVC is often the endpoint.
Case: 61 years gentleman with symptomatic PVC of 42% burden, planned for CA under 3D Ensite system.
Twelve leads PVC morphology as shown, was suggestive of LV in origin.
A coronary angiogram was done to visualize the coronary arteries and veins. We proceeded to map the left system via retrograde manner through RFA.
The earliest point was noted over LCC with LAT −41 ms, but there was a discrepancy of −30 ms comparing Bipolar to Unipolar signals. Ablation was performed but PVC recurred after a repeat of LCA angiogram. Coronary sinus was engaged using Agilis Steerable Catheter with Terumo wire support due to proximal location of valve of Vieussens. AIV LAT noted −19 ms. Ablation was done and consolidated below LCC and AMC regions.
Despite extensive ablation surrounding the summit, PVC albeit reduced in burden, was still recurrent. We decided to stop as adequate ablation has be made. PVC resolved after 18 h.
Decision Making and Conclusion: Locating the site of PVC is crucial for successful ablation.
Coronary angiogram is useful to mark LCA and coronary veins, especially in center without ICE.
Ablation of epicardial LV summit requires multi‐directional RFA energy—LCC, AIV, and AMC.
Complete resolution of PVC may not be required and stopping the procedure to leave for observation maybe considered if adequate targeted RFAs are done.

CS‐172‐CAB
Demonstration of pseduo‐VAAV during EPS in a case of a wide complex tachycardia
Mohanaraj Jayakumar; Kantha Rao Narasamuloo; Saravanan Krishinan
Hospital Sultanah Bahiyah, Ministry of Health Malaysia, Alor Setar, Malaysia
Regular wide complex tachycardias (WCT) can be VT or SVT with aberrancy. In this case, we demonstrate a case of WCT which turns out to be SVT and our approach to the case.
Forty‐five years old gentleman, presented with palpitations. Admitted to the ED and noted to have WCT. The tachycardia terminated with adenosine 12 mg. From the ECG, we can actually deduce it's SVT according to the algorithms like Vereckei and Brugada. Echocardiography ruled out structural heart disease. Coronary angiography revealed normal coronaries.
Patient agreed for EPS and three wire study was performed. The WCT was induced during catheter manipulation, which showed LBBB, short RP with TCL of 370 ms. PVC on His showed no A‐A advancement. Entrainment showed VAAV response. However, upon careful observation noted the returned A was similar to the pacing cycle length hence it is concluded to be pseudo VAAV. PPI–TCL (591–372) ms = 219 ms, and SA–VA (453–249) ms = 204 ms.
Hence, it was concluded to be an AVNRT and the slow pathway was ablated and modified. During follow up, patient is no longer on medications and his symptoms are no longer there.
This shows proper observations of an ECG and the response during EPS will guide to proper diagnosis and treatment.

CS‐236‐CAB
The possibility of identification of epicardial connection between the right pulmonary vein carina and right atrium with analyzing the unipolar electrogram using TRUE ref technology
Koyo Sato; Masanao Takeya; Tomofumi Nakamura; Yuuto Teshima; Yasuhide Ookawa
Nagoya Heart Center, Nagoya, Japan
A 62‐year‐old man underwent circumferential pulmonary vein isolation (PVI) and Ganglionated Plexi ablation for persistent atrial fibrillation. After circumferential PV antrum ablation was performed, complete PVI was not obtained on the right PVs. We created a gap map with CARTO mapping system using OCTARAY catheter. The gap map showed the site of earliest activation was the right‐sided PV carina apart from the isolation line. The earliest activation site shows that the unipolar electrogram using TRUE ref technology was earlier than the bipolar electrogram, and the unipolar electrogram might be suggested the epicardial connection between right PV antrum and right atrium. To identify whether the conduction from the right PV carina connected to adjacent structures, an activation maps of both atriums were obtained during pacing from the right inferior PV. This revealed that the site of earliest activation was the posterior right atrium (RA) and implied a direct connection between the right‐sided PVs and RA. The first radiofrequency (RF) application in the posterior RA resulted in only temporary isolation of the right‐sided PVs with bi‐directional block. Therefore, we performed a second set of RF applications to the earliest activation site of right PV carina. PVI was obtained after initiating the second set of applications and no further reconnection was observed.
CS‐239‐CAB
Intracardiac echocardiography guided PVC ablation
Mohanaraj Jayakumar; Hartini Yusoff
Ministry of Health Malaysia, Kajang, Malaysia
Sixty year old Malaysian lady presented with history of palpitations. Noted to have high PVC burden from Holter screening. From the ECG, noted to have left superior axis PVC.
Her ECHO showed grossly normal and coronary angiography revealed normal coronaries. She was counselled for PVC ablation under ThermoCool SmartTouch DF Curve (Carto) 3D guidance.
ICE catheter was used to guide the mapping catheter and fluoro was not used. While mapping the PVC from left midposteroseptal region, noted fragmented signal and good QS unipolar signal. Pace mapping at that region revealed 93% morphology match from clinical PVC. ICE catheter revealed the location of the catheter at posteroseptal papillary muscle of mitral valve.
Ablation was performed and noted runs of VT with similar morphology to the PVC. The are was consolidated with more ablations. Post ablation, the PVC no longer seen.
This case highlights that ICE can help to guide ablation and without the need for fluoro and pinpoint the location of ablation.

CS‐246‐CAB
Successful radiofrequency ablation of incision‐induced atrial tachycardia arising from orthotopic heart transplantation: A case report
Jianhua Li 1; Min Tang2
1Jinling Hospital, Nanjing University School of Medicine, Nanjing, China; 2Fuwai Hospital, Chinese Academy of Medical Sciences, Beijing, China
Objectives: Atrial arrhythmias, including atrial tachycardia (AT) are commonly observed after orthotopic heart transplantation (OHT). Here, we present a case of a 64‐year‐old man with AT originated from OHT‐related incision by electrophysiological study, and radiofrequency (RF) ablation was successfully applied.
Materials and Methods: A 64‐year‐old man who underwent OHT (bicaval technique) in November 2010 for rheumatic heart disease. Dual chamber permanent pacemaker was implanted in May 2012 due to sick sinus syndrome. Cavotricuspid isthmus dependent atrial flutter was confirmed by electrophysiological examination in May 2021, linear tricuspid isthmus ablation was then performed and sinus rhythm was recovered. The patient was admitted to emergency room with complaints of palpitation in August 2022. Rapid AT was revealed by electrocardiogram examination. Subsequently, endomyocardial biopsy result showed negative for rejection. Attempts at rhythm control with antiarrhythmic medications and cardioversion had failed. Recurrent symptomatic palpitations occurred after 6 months and AT with rapid ventricular rate was recorded. The patient then underwent an electrophysiological study and catheter ablation.
Results: Echocardiogram revealed normal cardiac function of transplanted heart. Three‐dimensional mapping results showed that AT was originated from sidewall at the junction of right atrial appendage and superior vena cava, which was associated with incision of OHT. Fractionated atrial electrograms could be found, and tachycardia was terminated when ablation catheter oppressed this site instantly. After a low power and short ablation, no AT was induced.
Conclusion: The current work presented a case of AT arising from the incision of OHT. We identified ablation are effective in incision‐associated AT.

CS‐248‐CAB
Ventricular tachycardia ablation with prosthetic aortic and mitral valve
Lee Karl Thien; Ming Yoong Low; Sharmila Shanmugam; Iskandar Mirza Amran; Surinder Kaur Khelae
National Heart Institute, Kuala Lumpur, Malaysia
Background: Sixty‐seven‐year‐old gentleman presented with palpitations. Co‐morbid include prior aortic (AVR) and mitral valve replacement (MVR) for chronic rheumatic heart disease, non‐ischemic cardiomyopathy, dual chamber implantable cardioverter defibrillator (ICD) for primary prevention, atrial fibrillation with prior atrio‐ventricular nodal (AVN) ablation.
Case: Sustained slow ventricular tachycardia (VT) recurred despite amiodarone, overdrive pacing and electrical cardioversion. Device interrogation of ICD (His lead and right ventricle [RV] lead) showed possible conducted supraventricular tachycardia (SVT) despite previous AVN ablation. Electrocardiogram (ECG) of tachycardia was suspicious of right bundle branch (RBB) reentrant VT. Proceeded with VT ablation under EnSite system mapping of RV.
Decision‐making: Occasional conducted SVT seen, His bundle and RBB ablated. Clinical VT induced, earliest at RV septum and ablated. Different VT induced mapped to posterior right ventricular outflow tract (RVOT). Ablation terminated VT. Likely origin of VT was from left ventricular outflow tract given history of AVR, successfully ablated from RVOT.

CS‐250‐CAB
Combining with intracardiac echocardiography and radiofrequency catheter ablation of focal right atrial tachycardia in dextrocardia
Shuai Shang; Yankai Guo; Baopeng Tang
Department of Pacing and Electrophysiology, The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
Background: Atrial fibrillation ablation for a patient with dextrocardia.
Case: A female patient, 66 years old, 12‐lead ECG (Figure A) indicates sinus rhythm, 24 h ambulatory ECG indicates atrial tachycardia. Chest radiographs (Figure B) and cardiac CTA (Figure D) suggest dextrocardia. The echocardiogram (Figure C) showed the patient had a mirror dextrocardia.
Decision‐making: We performed atrial fibrillation ablation for her under the guidance of intracardiac echocardiography. The patient recovered well after surgery.
Conclusion: During the operation, ICE, fluoroscopic image, and Carto three‐dimensional mapping system can be combined to guide catheter positioning better and adjust catheter operation to ensure smooth operation and reduce operation time and complications.

CS‐251‐CAB
A case report of successful ablation for dual epicardial left ventricle origin ventricular premature contractions utilizing by 2Fr electrode catheter inserted to coronary sinus
Norihiro Enomoto 1; Makoto Takei2; Toru Mese1; Takanori Tamaru1; Kenji Suzuki2; Hideki Nishimura1; Toshiyuki Takahashi2; Yutaka Okada1
1Eiju General Hospital, Taito‐ku, Japan; 2Saiseikai Central Hospital, Minato‐ku, Japan
Catheter ablation is considerable choice for high VPC burden patients with chronic heart failure (CHF); however, an epicardial origin of cardiac arrhythmia reduces the success rate. Such a case deeper inserted CS electrode catheter is often effective.
Case is 70s male CHF patient and ICD was implanted due to NSVT with EF 23%. VPC ablation was chosen to control CHF because of 37.1% VPCs (42 706/115 152) under taking optimized medications.
Two types VPCs were mainly documented (Figure). Both VPCs were inferior axis but surmised origins were different. VPC mapping resulted in VPC1 from epicardial lateral LV and VPC2 from epicardial anterior LV. Activation and pace mapping utilized by 2Fr electrode catheter into AIV revealed a firmly conclusion. Ablations at endocardial LV nearest from CS landmark successfully eliminated VPC1 and VPC2.
We experienced an effective 2Fr CS electrode catheter use in multiple epicardial LV origin VPCs case.

CS‐279‐CAB
Long RP tachycardia after short RP tachycardia ablation—A case report
Andrianus Oktovianto 1; Mohammad Iqbal2
1Dr. M. Soewandhie General Hospital Surabaya, Surabaya, Indonesia; 2Dr. Hasan Sadikin Central General Hospital, Bandung, Indonesia
Background: Short RP and long RP SVT have a different mechanisms of arrhythmia that poses a significant challenge to electrophysiologists during ablation. We present a case of female with PJRT after typical AVNRT ablation.
Case: A 21 year old female was referred for frequent recurrent palpitations for the past 6 years. The ECG showed SVT of 185 bpm, a short RP interval suggesting typical AVNRT. SVT induced by atrial extra‐stimulus test with AH jump. V entrainment exhibited V‐A‐V response. HRVPB showed no atrial advancement. We decided to perform slow pathway (SP) ablation. Confirming a successful ablation by pacing maneuver induced another SVT of 140 bpm with long RP interval. Long VA interval and eccentric atrial activation was observed with earliest site on right posteroseptal. Ventricle extra‐stimulus test revealed decrement properties. The ΔAH interval of <20 ms was suggesting that SVT due to PJRT. Subsequent ablation was applied to the earliest site of atrial activation. Finally, tachycardia was not induced with aggressive pacing.
Decision‐making: Distinguishing possible mechanism of long RP tachycardia may be challenging, particularly a concealed posteroseptal accessory pathway with decrement property. A comparison of AH interval during pacing and tachycardia provides a maneuver to establish the mechanism.
Conclusion: The coexistence of typical AVNRT and PJRT is uncommon arrhythmia and has rarely been reported. This case highlights the diagnostic defiance and importance of simple and reliable diagnostic maneuver for the rapid differentiation.
CS‐300‐CAB
First hybrid AF ablation in Asia with combined LAA clip and vein of Marshall ablation
Wood Hay Ian Ling 1; Max K. H. Wong2; Daniel Tai‐Leung Chan2; Katherine Y. Y. Fan1
1Grantham Hospital, Hong Kong SAR; 2Queen Mary Hospital, Hong Kong SAR
A 56‐year old man underwent pulmonary vein ablation in 2014 for symptomatic AFib and maintained on flecainide 50 mg BD. AFib recurrence in 2023. Holter showed persistent AFib. Echocardiogram showed normal biventricular function and biatrial size. He underwent epicardial AFib ablation with a subxiphoid approach. Epicardial lesions were created around the right and left PV antrum, across the posterior wall using the vacuum‐assisted, unipolar radiofrequency device (Epi‐Sense, AtriCure, OH). Left atrial appendage clipping and ablation of the vein of Marshall were performed thorascopically in the same procedure. The total procedure time was 3 h 5 min. The patient cardioverted to sinus rhythm during the procedure. Staged catheter ablation was performed 1 month later. Complete pulmonary vein and posterior wall isolation were demonstrated (see Figure). The total procedure time was 90 min, total LA dwell time was 25 min.

CS‐301‐CAB
Catheter ablation for persistent atrial fibrillation in a patient with heart of stone
Yingjian Deng; Faguang Zhou; Dong Chang
Xiamen Cardiovascular Hospital of Xiamen University, Xiamen, China
Myocardial calcification is a rare condition, with only a few reports in the literature. For the first time, we report a case of symptomatic persistent atrial fibrillation (AF) with diffuse myocardial calcification who underwent radiofrequency ablation and recovered well. Atrial septal puncture guided by fluoroscopy is difficult due to the calcification of the atrial septa. Electroanatomic mapping of the atrium showed areas of low voltage in the region of calcification. AF was terminated after circumferential pulmonary vein isolation, and no recurrence was observed during the 1‐year follow‐up.
Catheter ablation is a reasonable procedure to maintain the sinus rhythm for such patients. Calcification may play an important role in the maintenance of AF; however, ablation of these regions might be ineffective and dangerous. For patients with diffuse calcification, we recommend intracardiac echocardiography, which can provide a real‐time visualization of cardiac structures to guide atrial septal puncture and catheter ablation.

CS‐326‐CAB
Catheter ablation of left ventricular tachycardia in a patient with mechanical aortic and mitral valves
Hailei Liu; Youmei Shen; Weizhu Ju; Minglong Chen
The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
Background: In patients with mechanical aortic and mitral valves (MAMV) implantation, ablation of ventricular tachycardia (VT) originating from left ventricle (LV) is challenging.
Case: A 53‐year‐old woman presented with recurrent palpitation with dizziness for 10 years, yet aggravated for 3 days with electrocardiograms indicating sustained ventricular tachycardia (VT) originating from LV. She had a history of rheumatic heart disease, with MAMV implanted. VT repeated and sustained after intravenous administration of antiarrhythmic drugs, sedatives and sympathetic ganglion block.
Decision‐making: Catheter ablation for VT was preferred and LV access is the most challenging step. We took the following steps to access LV from right atrium: (1) Advance an intracardiac cardiography catheter and a deflectable sheath to the mid‐right atrium; (2) A large‐curve‐preformed transseptal needle was advanced into the dilator; (3) Clockwise torque of the sheath to obtain contact with the right atrium adjacent to the infero‐septal LV; (4) Puncture by advancing the needle, and confirm the LV access by contrast injection and a guidewire to the apex; (5) Advance the sheath into LV under the guidance of the transseptal needle. A sustained VT episode spontaneously occurred during ablation and was eliminated by ablating the target at the anterior wall. Substrate‐based ablation was performed and VT was non‐inducible thereafter. The patient refused ICD implantation. At the 3‐month follow‐up, the patient had no recurrent VT.
Conclusion: Trans‐right atrial access through blunt separation to ablate VT originating from LV is an effective and reproducible approach in patients with MAMV.
CS‐332‐CAB
Tricuspid isthmus ablation with linear pulsed‐field ablation
Xinzhong Li; Jianyong Li; Senlin Huang; Hairuo Lin; Xiaobo Huang; Yuegang Wang
Nanfang Hospital, Southern Medical University, Guangzhou, China
Pulsed‐field ablation with annular or petal‐shaped catheters has been used for electrical isolation of pulmonary veins in atrial fibrillation. However, the application of linear pulse‐field power in the treatment of atrial flutter has not been reported. Here we report a case of tricuspid isthmus dependent atrial flutter treated with a linear pulsed‐field catheter.
Case Report: Atrial flutter was indicated by electrocardiogram in a 71‐year‐old patient with a history of coronary artery bypass. A pulsed‐field ablation was scheduled with the linear ablation catheter (PulseLine, PL03F07N, EnChannel Medical Guangzhou Inc) (panel A) and pulsed electric field instrument (NanoAblate, PG‐01; EnChannel Medical Guangzhou, Inc.). The electroanatomical mapping and entrainment maneuvers in tachycardia suggest the typical cavo‐tricuspid isthmus (CTI) dependent atrial flutter (panel B). The nitroglycerin (5 μg/min) was administrated, then one pulsed‐field application in linear configuration at the tricuspid isthmus terminated the flutter (panel C). One additional application achieved bidirectional CTI block by atrial activation during septal and lateral atrial pacing (panels D and E).

CS‐334‐CAB
A case of re‐entrant atrial tachycardia post Senning procedure
Mathan Munusamy; Azlan Hussin; Marhisham Che Mood; Hasri Samion
National Heart Institute Kuala Lumpur, Kuala Lumpur, Malaysia
Background: Congenitally corrected transposition of great arteries (CCTGA) is a complex congenital heart lesion which has inherent risks of arrhythmias due to its unique electrophysiological properties. The risk of tachycardia is greatly increased especially after surgical correction.
Case: We present a case of an 8 year old boy with an underlying complex congenital lesion (congenitally corrected transposition of great arteries with pulmonary atresia) who had undergone surgical correction with Senning‐Rastelli procedure at age of 3. He presented with a 3 year history of recurrent and medication refractory narrow complex tachycardia and symptoms include palpitation and syncope. Multiple combinations of anti‐arrhythmics were tried due to limited experience in field of complex congenital ablation. He remained home‐bound due to the severity and we decided to undertake a challenging ablation. As part of his preparation to undergo the ablation, we performed a cardiac computed tomography and a 3‐dimensional reconstructed model of the heart to assess coronary sinus anatomy and feasibility of trans‐baffle puncture.
Decision‐making: Electrophysiology study was performed and oesophageal echocardiogram guided baffle puncture was performed. Mapping was performed with Advisor HD‐Grid catheter and 3D electroanatomical (Ensite NavX) mapping systems, revealing a re‐entrant tachycardia with earliest signals traced to the pulmonary venous atrium and early meets late pattern was mapped to the cavo‐mitral isthmus. Targeted ablation in this region successfully terminated the tachycardia. The patient is now 8 months symptom free without any anti‐arrhythmics.
Conclusion: Ablation procedures in complex congenital heart lesion is possible with 3D electroanatomical mapping and meticulous planning.
CS‐337‐CAB
Right bundle branch block and junctional rhythm seen during ablation in the right ventricle outflow tract: A case report
Si Jia Pu 1,2; Wei Dong Lin1; Yu Mei Xue1,2; Hai Deng1
1Guangdong Cardiovascular Institute, Guangdong Provincial People's Hospital, Guangzhou, China; 2School of Medicine, South China University of Technology, Guangzhou, China
Background: We present a case of radiofrequency catheter ablation on a 16‐year‐old girl with premature ventricular complexes (PVC) who had a prior history of transcatheter closure for peri‐membranous ventricular septal defects in Guangdong Provincial People's Hospital.
Case: A 16‐year‐old girl with a metallic occluder in the membranous ventricular septum underwent ablation for PVC. Right bundle branch block and junctional rhythm were recorded during ablation in the right ventricle outflow tract. His bundle potential as well as the high‐frequency potential generated by electrical interference was observed when mapping the margin of the occluder. Damage to the His‐Purkinje system (HPS), related to the possible anatomical variation of HPS and the uncontrolled radiofrequency energy heated up by the metallic device, underlies the phenomena.
Decision‐making: For safety reasons, we attempted ablation at the right coronary cusp and it worked eventually, presenting an alternative ablation strategy.
Conclusion: The case cautions electrophysiologists that ablation in a relatively remote position is feasible and worthy of consideration in patients with metallic occluders.
CS‐352‐CAB
Coronary spasm induced by cryoablation of atrial fibrillation: A case report
Huasheng Lv; Zilalai Ainiwaer, Yanmei Lu
Xinjiang Medical University Affiliated First Hospital, China
The patient, a 61 year old male, was admitted on December 4, 2021 with intermittent palpitations and chest tightness for 7 years, worsening for 2 months. The patient experienced intermittent palpitations 7 years ago and was diagnosed with “paroxysmal atrial fibrillation” in an external hospital. This time, they were admitted for atrial fibrillation catheter ablation. The patient had smoked for 20 years and denied the history of hypertension and diabetes. Two months ago, coronary angiography showed that the anterior descending artery was interrupted with diffuse stenosis, 40% of the most severe stenosis, and no other abnormalities were found. Upon admission, no abnormalities were found in the blood test. Echocardiography: EF62.14%. Transesophageal three‐dimensional echocardiography showed no thrombus. ECG shows atrial fibrillation rhythm (Figure ①). After completing preoperative preparation, transcatheter cryoablation of the heart was performed at 13:30 on December 8, 2021. The surgery ended at 15:00 without any complications and was safely returned to the ward. At 16:29, the patient suddenly experienced squeezing pain in the precordium while lying still. The bedside 12 lead ECG showed that the ST segment of lead V2–V6 was significantly elevated (Figure ②), and the pain improved for 3–5 min. At 16:40, ECG was rechecked, indicating a sinus rhythm (Figure ③). After that, there was no pain in precordium and ECG changes. The diagnosis considers the induction of coronary artery spasm by cryoablation.

CS‐365‐CAB
A case of ischemic macro‐reentrant ventricular tachycardia: Usefulness of overdrive pacing maneuver
Jina Choi 1,2; Youngjin Cho1,2; Il‐Young Oh1,2; Ji Hyun Lee1,2
1Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam‐si, Republic of Korea; 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Republic of Korea
Background: Our report aims to provide insight into electrophysiologic (EP) approach and electrogram guided ablation strategy, emphasizing the utility of pacing maneuver in an case of ischemic ventricular tachycardia (VT).
Case: A 83‐year‐old male patient with ischemic cardiomyopathy presented with ventricular tachycardia. During the EP study, a VT was induced by programmed electrical stimulation. The VT was successfully eliminated by the radiofrequency ablation at the place with the mid‐diastolic potentials during the tachycardia (Figure 1).
Decision‐making: Subsequent series of overdrive pacing maneuvers demonstrated progressive fusion with fixed post‐pacing interval, suggesting macroreentrant mechanism. Furthermore VT termination by non‐propagated PVC was also observed during the ventricular pacing maneuver at the target lesion.
Conclusion: In conclusion, overdrive pacing maneuver is not only useful to identify the mechanism but also helps to facilitate mapping. By identifying the critical isthmus using pacing maneuver could allow minimal successful ablation, avoiding potential complications by unnecessary ablations.

CS‐367‐CAB
Lightning before the thunder
Manuel Jared Theo Jimenez; Marie Kirk Patrich Maramara; Michael‐Joseph Agbayani; Jorge Sison; Mariel Barcelon‐Cruz
Manila Med ‐ Medical Center Manila, Paco, Philippines
Sudden cardiac arrest (SCA) affects a number of persons worldwide. In the US, there are about 350 000 cases of occurring annually. Although numerous etiologies are possible, majority of these patients are found to have a primary coronary heart disease. Other possible causes of OHCA may also be due to primary electric disorders, among which would be abnormal tachyarrhythmias, Long QT‐Syndrome (LQTS), and Wolff–Parkinson–White (WPW) syndrome. This is a case of a 49‐year‐old male, hypertensive, dyslipidemic, was brought in due to sudden cardiac arrest. He was immediately brought to the hospital and successfully resuscitated within 27 min of ACLS/BLS. Initial rhythm post resuscitation showed atrial fibrillation in controlled rate with anterolateral wall ST‐Elevation. During the course of his admission, multiple episodes of supraventricular tachycardia (SVT) occurred almost every day. Each SVT episode was managed with medical or electrical cardioversion, whenever warranted. Subsequent ECG taken later on during admission showed pre‐excitation in the inferior, and lateral leads. Due to the recurrent SVT episodes, despite maximal cardioversion therapy, an electrophysiologic study was then performed confirming an accessory pathway located in the anterior tricuspid annulus, with orthodromic AV reciprocating tachycardia after which followed by successful ablation with resolution of the pre‐excitation and SVT. Further work‐up was pursued for the coronary artery status with a coronary angiogram done, succeeding the ablation. Results showed three vessel coronary artery disease and successful angioplasty was performed in the LAD. Patient was eventually sent home with modest improvement with his neurologic status.
CS‐370‐CAB
The curious case of left bundle branch morphology tachycardia, what is the mechanism?
Harsh Kumar Pandey 1; Narayanan Namboodiri2; Krishna Kumar Mohanan Nair2; Ajit Kumar Valaparambil2
1Sri Jayadeva Institute for Cardiovascular Sciences and Research, Mysuru, India; 2Sree Chitra Tirunal Institute for Medical Sciences and Technology (SCTIMST), Thiruvananthapuram, India
Background: 10%–15% of cases of Ebstein's anomaly are associated with multiple accessory pathways.
Case Report: An 8‐year‐old girl, with a known case of Ebstein's anomaly with the WPW syndrome, was referred for electrophysiologic evaluation and RF ablation because of frequent symptomatic episodes of the two types of sustained supraventricular tachycardia.
Decision‐making: During the EP study, different EP maneuvers help in differentiating between typical and atypical accessory pathways. The typical accessory pathways do not exhibit decremental conduction properties. Whereas, in the atypical accessory pathway (Atrio fascicular Mahaim), both PR interval and QRS duration changed due to decremental conduction property in the Mahaim fiber.
Conclusion: Ebstein's anomaly is associated with multiple pathways.
Characteristics of typical and atypical pathway help in its localization and ablation.

CS‐386‐CAB
Successful ablation of coexisting pleomorphic ventricular tachycardia and Mahaim‐type AVRT with the same trigger
Emin Evren Ozcan; Oguzhan Ekrem Turan; Reşit Yiğit Yilancioğlu
Dokuz Eylul University Heart Rhythm Management Centre, Izmir, Turkey
Background: Wide QRS complex tachycardia (WCT) is a diagnostic challenge as it can be caused by different mechanisms. We present the patient who diagnosed with tachycardiomyopathy related to two different WCTs were induced by RVOT PVCs.
Case: A 46‐year‐old woman with flecainide‐resistant WCT and tachycardiomyopathy underwent an electrophysiological study. Pleomorphic ventricular tachycardia (VT) and Mahaim‐type antidromic atrioventricular reentrant tachycardia (AVRT) were observed, both induced by right ventricular outflow tract (RVOT) premature ventricular complexes (PVCs). Echocardiography showed reduced left ventricular function.
Decision Making: Atrial incremental pacing showed progressive prolongation of the A‐H interval, concomitant shortening of the H–V interval, and progressive preexcitation of QRS complexes with LBBB morphology, confirming Mahaim‐type AVRT with negative HV and A‐V‐A responses in tachycardia. The ablation strategy targeted the constant RVOT PVC trigger. Endocardial mapping localised the PVC origin at the RVOT and its elimination successfully abolished pleomorphic VT. Ablation targeted the right atrial free wall of the tricuspid annulus, resulting in the absence of sustained tachycardia or pleomorphic VT (Figure 1).
Conclusions: Accurate diagnosis by the conventional electrophysiological study was essential for successful ablation and resolution of the tachycardiomyopathy.

CS‐389‐CAB
Three cases of atrial tachycardia associated with the sinus venosa region
Nao Yasuda 1; Fumiya Uchida3; Masafumi Kato4; Soichiro Maeda2; Kato Toshiaki2; Yoshifumi Awaji2
1Nagoya Ekisaikai Hospital, Department of Clinical Engineering, Nagoya, Japan; 2Nagoya Ekisaikai Hospital, Department of Cardiology, Nagoya, Japan; 3Mie Heart Center, Department of Clinical Laboratory, Taki‐Gun, Japan; 4Mie Heart Center, Department of Cardiology, Taki‐Gun, Japan
Background: The Sinus Venosa (SV) is located in the posteromedial right atrium (RA) and is considered the boundary between the tissues derived from the true embryonic RA and sinus venosus. Only a few reports suggests a connection between atrial tachycardia (AT) and SV. This study presents three cases of complex AT associated with the SV.
Cases: An 80‐year‐old female with paroxysmal atrial fibrillation (AF) and AT underwent radiofrequency catheter ablation (RFCA). Activation mapping (AM) for AT showed two functional block lines from SVC to IVC in Crista Terminalis (CT) and SV region, indicating a macroreentrant circuit around the CT gap. Linear ablation between these lines successfully terminated the AT.
An 80‐year‐old female with a history of RFCA for persistent AF developed AT. AM revealed a functional block in the SV region, with excitement propagation circling around the block. The successful ablation site was where the fractionated electrograms were recorded adjacent to the block.
A 60‐year‐old male, with a history of repeated RFCA for longstanding AF developed AT. AM suggested Bi‐AT. Initially, it showed delayed activation through the SV region, transmitting from the RA to the left atrium (LA) via the septum, ascending along the LA septum, returning to the RA via the Bachman Bundle, descending along the lateral side of the RA, and returning to the SV region. The ablation of the conduction pathway between the RA and LA successfully terminated the AT.
Conclusion: The SV might play an important role in complex AT involving the RA.
CS‐390‐CAB
Displaced endocardial catheter location during the ablation of ventricular arrhythmia originated from a septal perforating vein
Chhayroud Heng; Hui Nam Pak; Chun Hwang
Yonsei University Health System, Seoul, South Korea
Background: Catheter ablation of ventricular arrhythmia (VA) originating from the left ventricular summit (LVS) is known to be difficult due to the complicated anatomical constraint. Mapping a septal perforating vein may play an essential role in subepicardial or intramural VA from LVS, providing the anatomical endocardial ablation target.
Case: We report a successful endocardial ablation of premature ventricular contraction (PVC) from the LVS by a single (RF) energy delivery targeting the micro‐catheter in the septal perforating vein.
Decision‐making: We observed sudden septal displacement of the endocardial catheter during the 2nd consolidation radiofrequency (RF) energy delivery (45 W, Contact force 24 g). Therefore, we changed the catheter position reducing the contract force, and finished the procedure successfully.
Conclusion: Displacement of the ablation tag from the endocardial surface may suggest impending steam‐pop during high‐power endocardial ablation for intra‐mural or subepicardial VA.
CS‐417‐CAB
Accurate ablation of atrial fibrillation with real‐time ICE measurement: A case report
Hao Su
Anhui Provincial Hospital, He Fei City, China
Background: Atrial fibrillation is a common arrhythmia with main complications including embolism, heart failure and cognitive impairment. If the thickness of the ablation site can be accurately measured to guide ablation, the complications of ablation will be greatly reduced.
Case: A 51‐year‐old male patient with “repeated palpitation for 2 years” was admitted to hospital and diagnosed as arrhythmia, paroxysmal atrial fibrillation, and hypertension.
Decision‐making: Relevant examinations were completed, contraindications were excluded, and catheter ablation of atrial fibrillation was planned. During the operation, the intracardiac echocardiography (ICE) catheter was regulated in the cardiac chamber so that the ultrasonic fan surface was perpendicular to the above nine fixation points, and the thickness of the atrial muscle in this part was measured successively (Figure 1). The guiding ablation index (AI) of the anterior wall, posterior wall, top, bottom and left pulmonary vein ridge, anterior and inferior margin, top, bottom and posterior wall of the right pulmonary vein was obtained based on the myocardial thickness measured by ultrasound (Figure 2).
Conclusion: A customized AI approach based on real‐time atrial muscle thickness measurements should improve the success rate of first isolation, shorten the time to PVI, and reduce surgery‐related complications and long‐term atrial fibrillation recurrence compared to an approach based on an empirical row target AI value.

CS‐419‐CAB
Pulsed electric field ablation for treatment of typical atrial flutter: A case report
Hao Su
Anhui Provincial Hospital, He Fei City, China
Background: Pulsed electric field is an emerging energy source for ablation of arrhythmia in recent years. It is often used for ablation of pulmonary veins in patients with atrial fibrillation. Compared to radiofrequency and cryoablation, pulsed field ablation (PFA) was superior to ablation for rapid and specific damage to the myocardium without damaging adjacent structures.
Case: A 65‐year‐old male patient was admitted to hospital with paroxysmal palpitation for 1 year. The dynamic electrocardiogram indicated sinus rhythm and paroxysmal atrial flutter. He had a history of hypertension, atrial flutter, cardiac insufficiency and uremia, and was treated with dialysis for a long time.
Decision‐making: The patient had renal failure and cardiac insufficiency. After physician discussion, the situation strongly indicated the necessity for the patient to undergo PFA to avoid intraoperative use of contrast media and cold saline perfusion.
Conclusion: For patients with renal failure and cardiac dysfunction, FAD can reduce the risk.

CS‐424‐CAB
A case of successful Purkinje de‐network for electrical storm after acute myocardial infarction
Takafumi Sasaki; Masao Takahashi; Marie Miura; Minami Suzuki; Seiya Komine; Taku Kanzaki; Masataka Sunagawa; Wataru Tsuno; Yoshiaki Mizunuma; Koichiro Yamaoka; Hirofumi Kujiraoka; Tomoyuki Arai; Kiyotaka Yoshida; Rintaro Hojo; Takaaki Tsuchiyama; Seiji Fukamizu
Department of Cardiology, Tokyo Metropolitan Hiroo Hospital, Shibuya, Japan
Background: Ventricular fibrillation (VF) storm after myocardial infarction (AMI) is a fatal situation and may not be controlled even with deep sedation, drug therapy, and sympathetic ganglion block. Recently, the usefulness of VF triggers ablation for electrical storms after AMI has been reported.
Case: The patient was a 79‐year‐old woman. She was transported to our hospital 36 h after the onset of her chest symptoms. Coronary angiography revealed total occlusion of the left anterior descending branch #6 and percutaneous coronary angioplasty was performed. One week later, VF occurred, and we defibrillated and started continuous infusion of amiodarone and deep sedation. However, the electrical storm was not suppressed and emergency ablation was performed.
Decision‐making: At first, substrate mapping was performed. There was no obvious slow conduction zone but a low voltage area (<0.5 mV) from the anterior wall septum to the apex. Purkinje potentials were observed around the septum. Delayed potentials were recorded from the apex to the middle of the anterior wall. The ablation strategy was to perform with endpoints of Purkinje de‐networking, in addition to the triggered PVCs' ablation recognized. After the procedure, the patient had no recurrence of VF.
Conclusion: We experienced a case of successful Purkinje de‐network for VF storm after AMI.
CS‐456‐CAB
The first cardioneural ablation at Ramathibodi Hospital for sinus node dysfunction in patient with sinus node dysfunction and paroxysmal atrial fibrillation
Naorn Pattanajidvilai; Tachapong Ngamukos
Mahidol University, Bangkok, Thailand
Background: Recent studies suggest that cardioneural ablation might be another treatment for SND.
Case: A 50‐year‐old male athlete visited the OPD due to palpitation. He was not taking any medications due to sinus bradycardia of 44 bpm. His maximal heart rate during the exercise stress test was 208 bpm and paroxysmal AF without any discernible ST‐T shift. His echocardiogram revealed no structural heart abnormalities. He was still having paroxysmal AF and sinus bradycardia 35 bpm despite 4 weeks of detraining. Therefore we decided to performed cardioneural ablation and PVI ablation for sinus bradycardia.
Decision‐making: The parasympathetic ganglion plexi were located where AEGM showed high‐amplitude fractionated electrogram or low‐amplitude fractionated electrogram during sinus rhythm which predominated at anterior RSPV ostium. Radiofrequency ablation in this area resulted in baseline heart rate increased to 55 bpm. PVI ablation was subsequently completed.
Conclusion: Post‐procedural ECG revealed sinus rhythm 60 bpm and the rhythm persisted at the 1‐month follow‐up.

CS‐466‐CAB
A case of new type bi‐atrial tachycardia
Yoshiaki Mizunuma; Rintaro Hojo; Marie Miura; Minami Suzuki; Seiya Komine; Wataru Tsuno; Takafumi Sasaki; Koichiro Yamaoka; Hirofumi Kujiraoka; Tomoyuki Arai; Kiyotaka Yoshida; Masao Takahashi; Takaaki Tsuchiyama; Seiji Fukamizu
Tokyo Metropolitan Hiroo Hospital, Shibuya, Japan
Background: There are several known types of bi‐atrial tachycardia (bi‐AT) circling both atria.
Case: Eighty‐one‐year‐old woman with a twice ablation history of pulmonary vein isolation and posterior wall isolation and anterior line for persistent atrial fibrillation. Catheter ablation was performed for recurrence of AT. The AT1 (tachycardia cycle length 250 ms) propagated clockwise in the right atrium (RA) and left atrial (LA) roof. Post pacing interval was matched only in Bachmann bundle (BB) attachment (Figure green dots). The epicardial conduction from the LA to RA was detected with Rhythmia mapping system (Figure blue dot line).
Decision Making: The AT1 was terminated by radiofrequency application (Figure pink tag). Additional application for the BB attachment to the LA roof. After ablation, BB conduction (the RA to the LA) was disappeared in the activation map.
Conclusion: We report a case of bi‐AT with BB and epicardial roof in circuit.

CS‐470‐CAB
Successful Purkinje de‐networking using a novel high‐resolution mapping catheter for ventricular fibrillation storm in a patient with ischemic cardiomyopathy supported by Impella device
Yuhei Kasai; Takayuki Kitai; Junji Morita; Takuya Okada; Ryo Horita; Daisuke Hachinohe; Tsutomu Fujita
Sapporo Heart Center, Sapporo Cardiovascular Clinic, Sapporo, Japan
Background: Sudden cardiac death resulting from ventricular fibrillation (VF) remains a significant concern, with Purkinje fibers identified as potential sources for VF initiation and maintenance.
Case: A 58‐year‐old woman with ischemic cardiomyopathy underwent catheter ablation due to recurrent VF episodes despite deep sedation with Propofol and pharmacological therapy using Amiodarone and Landiolol.
Decision‐making: Based on the slight change in morphology of triggered premature ventricular contractions, we performed Purkinje de‐networking instead of focal ablation. Given the necessity of Impella CP for maintaining hemodynamic stability, the Octaray mapping catheter was used to quickly identify the Purkinje network that triggers VF. The use of the Ripple map, independent of annotations, enabled precise identification of the branching point of the left anterior and posterior fascicles and prevention of left bundle branch block.
Conclusion: Utilizing the Octaray mapping catheter and analyzing the Ripple map can be valuable for quick and safe purkinje de‐networking for VF.

CS‐479‐CAB
Zero‐fluoroscopy ablation of frequent premature ventricular complex in a pregnant woman: First case in Soetomo General Hospital Surabaya, Indonesia
Yusuf Azmi; Budi Baktijasa Dharmadjati; Rerdin Julario; Muhammad Rafdi Amadis; Ragil Nur Rosyadi
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Airlangga – Soetomo General Hospital, Surabaya, Indonesia
Background: Arrhythmias during pregnancy pose a dilemma for the treating physician. Owing to radiation exposure and other uncertain risks for the mother and fetus, catheter ablation has rarely been performed and is often delayed until the postpartum period.
Case: Thirty‐four‐year‐old woman primigravida in the 26th week of pregnancy was presented to our department with drug‐resistant and poorly tolerated frequent premature ventricular contraction (PVC). The patient had structurally normal hearts without a known history of cardiovascular disease.
Decision‐making: We describe the case of a pregnant woman who presented with posteroseptal right ventricular outflow tract (RVOT) of PVC origin who underwent catheter ablation with a zero‐radiation approach. The patient successfully underwent zero‐fluoroscopy ablation guided by the Ensite NavX system, a non‐fluoroscopic navigation. Multiple radiofrequency ablations were accomplished using a 30‐W flexible ablation catheter at 45°C for 60–120 s in the posteroseptal RVOT. Accelerated VT was observed and a further 30 min observation showed no PVCs. The patient was then discharged the following day and the antiarrhythmic medication was discontinued. No episode of PVC was observed during follow‐up.
Conclusion: Catheter ablation of frequent PVC in pregnant patient can be safely and effectively performed with a completely zero‐fluoroscopy approach guided by the Ensite NavX system. In the case of a drug refractory, arrhythmia during pregnancy catheter ablation may be considered.
CS‐490‐CAB
Incessant AVNRT with tachycardia induced cardiomyopathy and conduction system dysfunction
Mohammad Sidqi Aulia; Giky Karwiky; Chaerul Achmad; Mohammad Iqbal
Universitas Padjadjaran, Indonesia
Background: Atrioventricular nodal reentrant tachycardia (AVNRT) is a common paroxysmal supraventricular arrhythmia, can rarely lead to cardiomyopathy and post‐AVNRT ablation abnormalities, including sinus and AV nodal dysfunction.
Case: A 70‐year‐old male was referred for syncope lasting less than 30 s, followed by full recovery of consciousness, preceded by sudden onset of palpitations without identifiable triggers. These palpitations had been occurring intermittently for 5 months, lasting up to 1 h with 2–3 episodes daily, with no chest pain or shortness of breath. A 12‐lead ECG showed sinus bradycardia with first‐degree AV block and SVT with RBBB Aberrancy. Echocardiography showed dilated chambers and reduced left ventricular systolic function (LVEF Biplane's 38%).
Decision‐making: The Electrophysiology (EP) Study, showed sinus rhythm, prolonged PR interval, intermittent SVT with RBBB aberrancy. V pacing demonstrated VA decremental conduction. Atrial extrastimulus testing revealed AH jump then induced SVT with VA interval 0 ms. Atrial pacing demonstrated SA and AV nodal dysfunction. Slow pathway ablation was performed, and no more tachycardia afterward. Post‐ablation ECG showed sinus AV nodal dysfunction, leading to a decision for Dual Chamber Left bundle Pacing implantation. Follow up after 1 month of ablation and pacemaker implantation, patient was asymptomatic and left ventricular systolic function was improved to 50%.
Conclusion: This case emphasizes the rarity of AVNRT‐induced cardiomyopathy and conduction system dysfunction, highlighting the diagnostic challenges and the importance of comprehensive treatment in managing incessant AVNRT complications.
Keywords: cardiomyopathy, incessant AVNRT, left bundle pacing, sinus AV nodal dysfunction.

CS‐530‐CAB
Do not forget the roots: Successful ablation of atrial flutter in a complex congenital heart disease patient simply using entrainment mapping
Lijie Mi; Hongda Zhang; Lei Ding; Min Tang
Fuwai Hospital, National Center for Cardiovascular Diseases, State Key Laboratory of Cardiovascular Disease, Chinese Academy of Medical Sciences, and Peking Union Medical College, Beijing, China
Background: Postoperative atrial flutter (AFL) patients with congenital heart disease (CHD) tend to be tough for ablation. Abnormal anatomy often makes additional difficulty for catheter placement and operation.
Case: A 40‐year‐old female with single atrium and pulmonary hypertension received repair surgery of endocardium cushion. She occurred consistent AFL after the surgery and asked for ablation. The pre‐procedure imaging showed heterotaxy syndrome, including polysplenia, inferior vena cava (IVC) interruption, left atrial isomerism, and scoliosis. During the procedure, we struggled but failed to insert the fixed or steerable decapolar catheter into the CS via the right internal jugular vein, finally, it was placed over RAA for a relatively stable position. The AFL cycle length was 280 ms. Because of the large size of RA and restricted operation, both right subclavian and femoral venous access (interrupted IVC → expansive azygos vein → SVC → RA) were obtained for mapping with a ThermoCool SmartTouch catheter. High‐density mapping electrodes were not used to avoid catheter collision.
Decision‐making: Substrate and activation mapping showed a scar and suspected isthmus in the posterolateral wall of RA, we performed entrainment there but the PPI‐TCL ranged from 80 to 100 ms. No special or fractionated potentials were found. Therefore, we performed entrainment at different sites and the PPI was 15 ms at a site near to CTI. Ablation of CTI via the subclavian access terminated the AFL successfully. No recurrence of tachycardia was reported during the 3 months after the procedure.
Conclusion: Traditional entrainment mapping is still significant in complex tachycardia patients, especially those with abnormal anatomical structures.

CS‐553‐CAB
Comparison of endocardial unipolar potentials and epicardial bipolar potentials in left atrial posterior wall isolation using epicardial mapping: Two cases
Tomoyuki Arai; Komine Seiya; Sunagawa Masataka; Tsuno Wataru; Miura Marie; Mizunuma Yoshiaki; Sasaki Takafumi; Kujiraoka Hirofumi; Yamaoka Koichiro; Takahashi Masao; Hojo Rintaro; Fukamizu Seiji
Tokyo Metropolitan Hiroo Hospital, Tokyo, Japan
Background: Whether conventional left atrial posterior wall (LAPW) isolation for atrial fibrillation form a transmural isolation is controversial. Although some studies show unipolar voltage map indicate transmural isolation for atrium, it is unclear whether unipolar map show atrial epicardial voltage and cutoff value.
Cases: We evaluated two cases which underwent pulmonary vein isolation and LAPW isolation and was added to perform atrial epicardial mapping. In a case which were completed transmural isolation to epicardial LAPW, endocardial unipolar potentials was less than 1.0 mV (Figure A). In another case which was not completed transmural isolation to epicardial LAPW, endocardial unipolar potentials was more than 1.0 mV (Figure B).
Decision‐making: Endocardial unipolar potentials were more than 1.0 mV at LAPW may indicate the no transmural isolation and may relate AF recurrence.
Conclusion: Endocardial unipolar potentials were less than 1.0 mV at LAPW may indicate the transmural isolation.

CS‐565‐CAB
Pathological ventricular tachycardia electrical storm after ECMO treatment: Three cases with different prognosis
Zidun Wang; Minglong Chen
The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
Three case on pathological ventricular tachycardia electrical storm after ECMO treatment.
Case 1: After ECMO treatment for ischemic cardiomyopathy, the repeated VT electrical storm occurred. Patient did not have the opportunity to undergo radio‐frequency ablation, and unfortunately passed away.
This case make us consider the “Timing” of ablation in such patients.
Case 2: After ECMO treatment for dilated cardiomyopathy, VT electrical storm occurred before weaning. The patient underwent VT ablation with ECMO support. The operation was successful, the prognosis was good, and the ICD was electively implanted after discharge.
This case make us consider the “Procedure” of ablation in such patients.
Case 3: After ECMO treatment for ischemic cardiomyopathy, the repeated VT electrical storm occurred. The patient underwent VT ablation with ECMO support. The operation was successful; however, the prognosis was bad. Patient unfortunately passed away.
This case make us consider the “Endpoint” of ablation in such patients.

CS‐603‐CAB
More than just PVI: Our initial experience in “Marshall's plan” for long standing persistent atrial fibrillation
Ignatius Yansen; Simon Salim; Daniel Tanubudi; Muhammad Yamin
EKA Hospital, Tangerang Selatan, Indonesia
Background: Complete isolation of the pulmonary veins is the foundation of catheter ablation of atrial fibrillation. However, only 50%–60% of patients remain in sinus rhythm at 2 years, particularly those with long‐standing persistent atrial fibrillation. Marshall's plan ablation consists of three steps and not limited to PVI alone. The technique focuses on anatomical targets (substrate) that have been recognized individually as important for the initiation or maintenance of atrial fibrillation but have not been targeted collectively or systematically.
Case: A 58‐year‐old, physically active male was advised by his I‐watch due to an arrhythmia (atrial fibrillation). He did had shortness of breath during physical activity, and 3‐days Holter revealed persistent atrial fibrillation. His echocardiogram revealed a dilated LA (47 mm) and global normokinetic.
Decision‐making: Patient was refer for radiofrequency ablation. We decided to follow the Marshall's plan steps as follows:
1. Coronary sinus ablation using irrigated catheter and vein of Marshall (CS‐VOM) musculature alcohol ablation
2. Pulmonary vein isolation
3. Anatomical isthmuses (mitral, roof, and cavotricuspid isthmus) ablation.
After ablation, patient was converted to sinus rhythm. Amiodarone was prescribed for 3 months, and he is still in sinus rhythm using Holter 9 months later.
Conclusion: Although this patient had long‐standing persistent AF, our initial experience with the Marshall's plan ablation lesion set (VOM ethanol infusion, PVI, and prespecified linear lesions) resulted in freedom from arrhythmia recurrence at 9 months.
CS‐606‐CAB
Long RP tachycardia with 2:1 block: What is the mechanism?
Ramdeo Yadave
Batra Hospital, Delhi, India
Clinical Presentation: Forty year old male presented with recurrent palpitations.
ECG during Palpitations showed long RP tachycardia.
Baseline ECG showed no preexcitation.
Echo showed structurally and functionally normal heart.
Taken up for EPS and RF ablation.
Summary and Conclusion: On ventricular extra 2:1 regular narrow QRS tachycardia induced which exclude Bypass tract mediated tachycardia.
Now we have to differentiate from AT to AVNRT with 2:1 conduction.
With one ventricular extra tachycardia become 1:1 due recovery of infra Hisian block because of peeling back of refractoriness and its long RP tachycardia. SA –VA time was more than 85 m. Tachycardia induction on V extra was VA and not VAAV rather VAAV occurred after VA which exclude atrial tachycardia.
Successful slow pathway ablation done with loss of dual AV nodal physiology and no more tachycardia was inducible.
CS‐608‐CAB
Long RP tachycardia: What is the mechanism
Ramdeo Yadave
Batra Hospital, Delhi, India
Thirty nine year old male presented with paroxysmal palpitations.
ECG during palpitations showed regular narrow QRS Tachycardia with long RP. Baseline ECG showed no preexcitation.
Echo showed structurally and functionally normal heart.
Taken up for EPS and RF ablation.
Summary and Conclusion: This long RP tachycardia was easily induced by VPC or Ventricular extra beat with long RP with earliest A at PCS.
On V extra during His refractory repeatedly terminate tachycardia without A excludes AT and confirms AVRT.
The AH during tachycardia is shorter than sinus rhythm suggest NVRT as fused captured beat terminate tachycardia and also reset tachycardia.
By single RF applications in the Right posteroseptal region terminated the tachycardia with V without A.
Over 6 month of follow up no recurrence of tachycardia.
CS‐613‐CAB
Radiofrequency ablation of focal atrial tachycardia emanating from the non‐coronary aortic cusp in a 36‐year old post‐kidney transplant patient
Mark Adorada 1; Erdie Fadreguilan2
1Philippine Heart Center, Quezon City, Philippines; 2Philippine Heart Center, Quezon City, Philippines
Background: Successful ablation of focal atrial tachycardia originating from the non‐coronary cusp is rarely encountered.
Case: A young patient with chronic kidney disease who underwent kidney transplant presented with 1‐year history of intermittent symptomatic supraventricular tachycardia. After written informed consent was obtained, an electrophysiologic study was undertaken. Atrial tachycardia was reproducibly induced by atrial pacing with earliest atrial activation at the coronary sinus catheter 9‐10. The tachyarrhythmia could not be entrained by ventricular overdrive pacing. Right atrium and coronary sinus activation maps were constructed using Carto (Biosense Webster, Thermacool Smarttouch). Local activation mapping during atrial tachycardia was carried‐out. The earliest activation region was located at the atrial septum. A 90 s radiofrequency was delivered but it failed to terminate the atrial tachycardia.
Decision‐making: Suspecting it was coming from adjacent site, mapping of the aortic coronary cusps was performed retrogradely via the right femoral artery. Earliest atrial activation signals were noted at the non‐coronary cusp region. Radiofrequency application of 26–31 W for a total of 180 s, opposite of corresponding earliest atrial activation at the right atrium, successfully abolished the atrial tachycardia without complication. Unsuccessful ablation of atrial tachycardia coming from the atrial septum suggests possible origin from non‐coronary aortic cusp. Furthermore, ablation of the right atrial septum must be done with caution since it carries substantial risk of heart block while ablation to the non‐coronary aortic cusp is less dangerous.
Conclusion: Symptomatic focal atrial tachycardia emanating from the non‐coronary cusp can be safely and effectively treated using radiofrequency ablation.

CS‐616‐CAB
Catheter ablation strategy for atrial fibrillation in patients with partial anomalous pulmonary venous return
Ishizue Naruya; Fukaya Hidehira; Ogiso Sho; Murayama Yusuke; Saito Daiki; Nakamura Hironori; Kishihara Jun; Oikawa Jun; Niwano Shinichi; Ako Junya
Kitasato University, Sagamihara/Minamiku/Kitasato, Japan
Background: Partial anomalous pulmonary venous return (PAPVR) is one of the rare congenital heart diseases. The ablation strategy for atrial fibrillation (AF) with PAPVR was not established.
Case: Case 1: A 62‐year‐old man diagnosed with paroxysmal AF. Pre‐procedural computed tomography (CT) scanning revealed that the right superior pulmonary vein (RSPV) did not connect to the left atrium (LA). The anomalous RSPV was draining to the superior vena cava (SVC). Thus, he was diagnosed with PAPVR. The encircling PV isolation was performed on the left PV and inferior right PV. Besides, the anomalous RSPV and SVC were also isolated because abnormal potentials and ectopies were observed inside them.
Case 2: A 57‐year‐old man diagnosed with persistent AF. Pre‐procedural CT scanning revealed that the left superior pulmonary vein (LSPV) did not connect to the LA. The anomalous LSPV was draining to the innominate vein. The encircling PV isolation was performed on the right PV and left inferior PV. Since the electrical potentials were not observed in abnormal LSPV, we did not perform the LSPV isolation.
Decision‐making: The ablation strategy for anomalous PV was determined by the presence or absence of electrical potentials.
Conclusion: We experienced two cases of AF complicated with PAPVR, treated with different strategies.
CS‐617‐CAB
Successful catheter ablation in patient with Ebstein anomaly and Wolff–Parkinson–White syndrome using surrogate electroanatomic mapping
Mark Adorada; Erdie Fadreguilan
Philippine Heart Center, Quezon City, Philippines
Background: Catheter ablation in patients with Ebstein Anomaly and Wolff–Parkinson–White (WPW) Syndrome remains challenging due to complex anatomy with generally low success rates.
Case: A 22‐year old male with Ebstein Anomaly and WPW Syndrome presented with symptomatic paroxysmal tachyarrhythmia and was scheduled for catheter ablation. Right coronary artery and right atrial angiogram were performed. Placement of diagnostic decapolar catheter in the coronary sinus os failed after several attempts due to distorted anatomy. Instead, a 20‐electrode diagnostic halo catheter was utilized for electroanatomic mapping of tricuspid annulus. An electrophysiologic study was done with orthodromic atrioventricular reentrant tachycardia rapidly induced. Localization of accessory pathway was identified at the right posteroseptal tricuspid annulus with earliest atrial signals noted on electrodes 1 and 2. Radiofrequency energy was applied over the target area for a total of 360 s with loss of pre‐excitation. Post‐ablation, no arrhythmia was induced with absence of ventriculo‐atrial conduction. Procedure concluded without reported complication.
Decision‐making: Several anatomic challenges presented during conventional catheter ablation. Coronary angiogram was done to demonstrate extent of coronary artery branches to avoid injury during radiofrequency application. Right atrial angiogram was carried‐out to help demonstrate true atrioventricular groove and the extent of downward displacement of the valve leaflets. Utilization of different conventional methods attributed to success rate of the procedure. Patient remained asymptomatic up to date without recurrence.
Conclusion: Catheter ablation in patients with Ebstein Anomaly and Wolff–Parkinson–White Syndrome remains a challenge, however; the use of conventional method with surrogate electroanatomic mapping can still be successful.

CS‐619‐CAB
Successful management of left atrial‐esophageal fistula following ablation in a patient with prior aortic stent placement: Left atrial patch closure and temporary esophageal stent placement
Kenji Kuroki; Yuya Tanaka; Koji Sudo; Chisa Asahina; Akira Sato
University of Yamanashi, Chuo, Japan
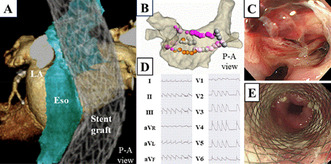
A 70‐year‐old female with an aortic stent graft after total arch replacement (A) underwent a second ablation procedure for atrial fibrillation. Posterior wall isolation was performed, in addition to re‐isolation of the right pulmonary veins (B). Seven days after discharge, she was readmitted due to chest pain, and esophageal ulcer was identified (C). On the 11th day of hospitalization, she suddenly developed hemiparesis, and CT scan revealed air in the mediastinum and left atrium, leading to a diagnosis of transient ischemic attack caused by a left atrial‐esophageal fistula. Because transient ST elevation was also observed that night (D), emergent left atrial patch closure and esophageal stent placement were simultaneously performed the following day (E). The postoperative course was uneventful with the esophageal stent removed on postoperative day 41. In cases of left atrial‐esophageal fistula with multiple complications, hybrid treatment involving surgical intervention and temporary esophageal stent placement is considered effective.
CS‐625‐CAB
High burden of premature ventricular complexes in a 37‐year old patient with left ventricular non‐compaction cardiomyopathy
Mark Adorada; Erdie Fadreguilan
Philippine Heart Center, Quezon City, Philippines
Background: Left ventricular non‐compaction is a rare congenital cardiomyopathy that predisposes patient to high risk of malignant arrhythmias.
Case: A 37‐year old female, known case of left ventricular non‐compaction cardiomyopathy (LVNC) presented with 4‐years history of palpitation accompanied with chest discomfort. Further work‐up was done including 24‐h Holter showing 25% burden of premature ventricular complexes (PVCs). Patient remained symptomatic despite on anti‐arrhythmic medication and was then advised for radiofrequency ablation. Local activation mapping during premature ventricular depolarization correlated with pace mapping showed earliest PVC activation (40 ms earlier than surface ECG) at the left ventricular summit. Radiofrequency application was performed for a total of 160 s with no recurrence of PVCs after 30‐min observation.
Decision‐making: Up to date, there is no established guideline regarding management of patients with LVNC presenting with clinically significant PVCs. Radiofrequency ablation and/or implantable cardioverter defibrillator device implantation are the probable therapeutic options. In our case, we performed radiofrequency ablation which rendered the patient asymptomatic up to this time.
Conclusion: Catheter ablation of PVCs originating from the left ventricular summit was successfully done in a patient with LVNC with no reported recurrence of palpitation.

CS‐626‐CAB
Papillary muscle pre potentials can guide successful ablation papillary muscle arrhythmias
Soumen Devidutta; Harish Mohan
Apollo Hospitals, Hyderabad, India
Background: A 30‐year‐old man presented with frequent PVCs (morphology suggestive of posterior papillary muscle origin), moderate MR, moderate LV dysfunction (non‐ischemic), and shortness of breath, NYHA III.
Case: Electroanatomic mapping of LV was done by retro aortic route. Activation map revealed an early spot at the base of posteromedial papillary muscle. Initial energy there only transiently suppressed the PVCs.
Decision making: Further mapping led to a nearby spot with very early pre potentials leading the local activation by over 57 ms. The unipolar was also sharp QS. Ablation there immediately suppressed the PVCs with dissociation of the prepotentials from the PVCs. ICE image showed the ablation catheter at the base of postero medial papillary muscle. Ablation guided by early local activation but without a prepotential may only transiently suppress the papillary muscle PVCs and it often reemerges from a nearby exit. Sites with early prepotentials coupled with local activation are at the PVC source and can guide successful elimination.
Conclusion: Early pre potentials leading local activation which are likely papillary muscle potentials and can lead to successful ablation of papillary muscle arrhythmias.

CS‐627‐CAB
Fragmented antegrade Purkinje potential ablation of idiopathic left posterior fascicular ventricular tachycardia in an adolescent
Tengyang Wang; Ji Wei; Xiaofeng Guo
Fujian Children's Hospital, Fuzhou, China
Background: Left posterior fascicular ventricular tachycardia catheter ablation remains challenging in the pediatric population. Re‐entry of the Purkinje network emanating from the left fascicles has been considered to be the underlying mechanism of Left posterior fascicular ventricular tachycardia.
Case: A 13 year‐old boy with 1‐year recurrent ventricular tachycardia history visited our hospital for treatment. We performed electrophysiological examination to this adolescent, ventricular tachycardia can be induced by program stimulation, P1 and P2 potentials were recorded during ventricular tachycardia. Fragmented antegrade Purkinje potential was recorded during sinus rhythm.
Decision‐making: We ablated fragmented antegrade Purkinje potential region. After the ablation, program stimulation could not Induced ventricular tachycardia. We did not detect ventricular tachycardia in this patient during follow‐up.
Conclusion: This case highlights the importance of fragmented antegrade Purkinje potential in left posterior fascicular ventricular tachycardia. The fragmented antegrade Purkinje potential may be used for guiding successful ablation in pediatric left posterior fascicular ventricular tachycardia.

CS‐632‐CAB
A case of successful ablation of cavotricuspid isthmus‐dependent atrial flutter after four times of failed ablation
Hongda Zhang; Lei Ding; Lijie Mi; Min Tang
Fuwai Hospital, Beijing, China
Introduction: The most common type of atrial flutter (AFL) is the cavotricuspid isthmus (CTI) dependent typical atrial flutter. Ablation of this type of AFL is associated with a high success rate. However, it sometimes can be challenging.
Case: A 45‐year‐old man with persistent AFL was admitted to our center for a fourth ablation procedure. The first time he was diagnosed with typical AFL was 6 months after the corrective surgery for the atrial septal defect, which was 14 years ago. He underwent the first radiofrequency ablation the same year and the AFL did not recur until 7 years ago. Then he had another three unsuccessful ablation procedures in the following years. This time the diagnosis was still counterclockwise CTI‐dependent atrial flutter as verified by activation mapping. Ablation of the gaps in the CTI line terminated the AFL but failed to achieve CTI conduction block. After extensive ablation for another 20 min, CTI conduction block still could not be achieved. Then we used a balloon of the Swan‐Ganz catheter to occlude the hepatic vein. During the occlusion, bidirectional CTI conduction was blocked after only several radiofrequency applications. The patient was free of AFL during the following 1‐year follow‐up.
Discussion: It is not always easy to block the CTI conduction. Anatomically, the left hepatic vein is just underneath the CTI, and the blood flow could decrease the lesion size and make ablation more difficult.
Conclusion: Occlusion of the hepatic vein could be used to facilitate ablation of challenging cases of CTI‐dependent AFL.

CS‐635‐CAB
Is it enough to perform slow pathway modification using 3D electroanatomical mapping to prevent AV block in octogenarian? What did we miss?
Theovano Oktavio 1; Michael Elias Santoso1; Theovano Oktavio1; Evan Jim Gunawan2; Ahmad Handayani2; Beny Hartono2; Dian Larasati1; Muhammad Munawar2
1Sam Ratulangi University, Manado, Indonesia; 2Binawaluya Heart Hospital, Jakarta, Indonesia
Background: Slow pathway modification is the preferred ablation method for typical AVNRT. AV block may occur about 1%–2.3%. Here we present a case of typical AVNRT ablation using 3D electroanatomical mapping with complication TAVB.
Case: A 86‐year old female with palpitation since 2 years ago spontaneously terminated. X‐ray showed cardiomegaly, echocardiography revealed normal heart chamber and ejection fraction, moderate aortic and mitral stenotic was found. Electrocardiography and electrophysiology study showed slow/fast AVNRT, PR interval 202 ms, AH interval 92 ms, HA interval 40 ms, AV conduction 2:1 was found. Ablation procedure using 4 mm non‐irrigating catheter, marking of the His using Carto 3D.
Decision‐making: His site was marked, AV signal 1:3 and no His signal was found in ablation catheter, ablation was performed near CS ostium and 15.1 mm from His site. Unfortunately, TAVB was found in <10 s of RFA with 30 W, 350°C, 40 s. 5 mg dexamethasone was administered, temporary pacemaker was implanted. The next 2 days, TAVB still exist so dual chamber permanent pacemaker was implanted.
Conclusion: AV block may appear as a direct damage to the AV node, displacement of the slow or fast pathway. In this case may be due to displacement of fast pathway. Even using 3D mapping, we need to use His catheter to calculate the A(H)‐A(Md) interval to prevent the incidence of AV block.
Keywords: 3D mapping AVNRT ablation, AV block slow pathway modification, AVNRT ablation.
CS‐638‐CAB
Catheter ablation of idiopathic premature ventricular complexes originating from the septal insertion of moderator band
Mark Adorada; Jemelee Hernandez‐Albano
Philippine Heart Center, Philippines
Background: Arrhythmias originating from the moderator band (MB) in the right ventricle have been increasingly recognized in the absence of identifiable structural heart disease.
Case: A 59‐year old female presented with 7‐month history of chest heaviness and palpitation that became persistent despite medication. Diagnostic work‐up was done including 24‐h Holter which showed frequent premature ventricular complexes (PVCs). Patient was then advised to undergo radiofrequency ablation. Local activation mapping during PVCs showed earliest activation at the septal insertion of the moderator band with PASO Score of 95.9%. Catheter ablation was successfully carried‐out without untoward complication.
Decision‐making: Documented PVCs were initially suspected to be coming from the tricuspid annulus. However during pace mapping, origin was traced at the septal insertion of the moderator band. This finding was strengthened by intraprocedural echocardiography that was able to visualize the intracardiac structures of interest. Ablation of MB was challenging due to thickened surrounding myocardial tissue that requires aggressive radiofrequency application and the need for catheter stability in order to maintain consistent contact.
Conclusion: Catheter ablation of PVCs originating from the MB poses a great challenge; however, it can be highly successful and lifesaving.

CS‐678‐CAB
An unusual anatomy of coronary sinus in patient with Wolff–Parkinson–White syndrome and stretched patent foramen ovale with atrial septal aneurysm undergoing accessory pathway ablation
Fandi Ahmad; Sunu Budhi Raharjo; Sebastian Andy Manurung; Chandara Rith; Dony Yugo Hermanto; Dicky Armein Hanafy; Yoga Yuniadi
Division of Arrhythmia, Department of Cardiology and Vascular Medicine, Faculty of Medicine Universitas Indonesia/National Cardiovascular Center Harapan Kita, Jakarta, Indonesia
Background: The coronary sinus (CS) is an important vascular structure that allows access to the coronary veins in multiple interventional procedures including ablation catheter. The success of the procedure is supported by the knowledge of the CS anatomy, particularly the recognition of its anomalies and other existing structural heart disease.
Case Illustration: We report a rare case describing the accidental finding of an abnormal septal anatomy structure in a 46‐year old woman with Wolff–Parkinson–White (WPW) syndrome undergoing right posteroseptal accessory pathway ablation. We found a difficulty when inserting the decapolar catheter to CS during ablation procedure. Finally, we had successfully inserted the catheter to the CS, but in the unusual form as it shown on fluoroscopic view. Transoesophageal echocardiography was performed, it showed a stretched patent foramen ovale (PFO) left to right shunt and atrial septal aneurysm with hyperkinetic interatrial septum. These findings suggesting the possibility cause of the unusual anatomy of the CS.
Conclusion: This case highlights the importance of understanding the CS anatomy and its variations during performing the catheter ablation procedure. Another diagnostic modalities, like cardiac MRI and MSCT may be needed for further detailed evaluation of CS anatomy.
Keywords: accessory pathway ablation, atrial septal aneurysm, coronary sinus, stretched patent foramen ovale.
CS‐679‐CAB
Pericardial effusion in the late phase after catheter ablation for atrial fibrillation
Kenichi Tokutake; Satoko Shiomi; Ryutaro Sakurai; Yoshito Yamazaki; Takuya Matsumoto; Hidenori Sato; Hirotsuna Oseto; Masaaki Yokoyama; Mika Kato; Seigo Yamashita; Michifumi Tokuda; Michihiro Yoshimura; Teiichi Yamane
The Jikei University School of Medicine, Tokyo, Japan
Background: Pericardial effusion is known as one of the complications of atrial fibrillation (AF) catheter ablation, and delayed pericardial effusion can rarely occur.
Case: A 67‐year‐old male patient. Catheter ablation for AF was performed. During the placement of the coronary sinus catheter, injury of the coronary vein occurred (Figure). After the procedure, a small amount of pericardial effusion was observed. The following day, there was no worsening of pericardial effusion and the patient was discharged.
Decision‐making: On the 58th day after the procedure, pericardial effusion was detected (Figure), and 450 mL pericardial drainage was performed. Subsequently, there was no recurrence of pericardial effusion and the patient was discharged. However, on the 100th day after the procedure, pericardial effusion was observed again, and 400 mL pericardial drainage was performed. Since then, the patient has been progressing without pericardial effusion.
Conclusion: We experienced a case involving pericardial effusion, which required two pericardial drainages in the late phase.

CS‐681‐CAB
Ablation of atrial arrhythmia in a patient with complex congenital heart disease
Preetam Krishnamurthy 1; Sachin Yalagudri2; Muthiah Subramanian2; Daljeet Kaur Saggu2; Calambur Narasimhan2
1Sri Ramachandra Institute for Higher Education and Research, Chennai, India; 2AIG Hospitals, Hyderabad, India
Background: Atrial arrhythmia is a common cause for failure of Fontan circulation. Here we discuss a challenging case of atrial arrhythmia in a patient with complex congenital heart disease.
Case: Firty‐year‐year‐old male, diagnosed to have double outlet right ventricle, with malposed great arteries and severe pulmonary stenosis, post Classical Fontan at 12 years age, presented with congestive cardiac failure, was found to have atrial flutter 2:1 AV conduction refractory to medications and cardioversion. Hence, ablation was planned using CARTO Mapping system with Pentaray mapping. An atrial screw in lead was used for stable atrial reference. The Fontan circuit was initially mapped, and areas of slow conduction were identified using coherence mapping and entrained. Sites with PPI‐TCL = 0 was tagged and ablated. Tachycardia terminated during ablation and further consolidation lesions were given along the isthmus. Patient symptomatically improved on follow up.
Decision Making: Refractory atrial arrhythmia can result in Fontan Failure and needs early ablation. Ablation in complex congenital heart disease is challenging since access to the pulmonary venous atrium is difficult. Since coronary sinus could not be cannulated, an atrial screw in lead was used, which provided stable reference for mapping. Access to the pulmonary venous atrium involves baffle puncture or complex retrograde access – both of which are high risk interventions and could be avoided since majority of the atrial flutter circuit could be mapped in the Fontan circuit.
Conclusion: Atrial arrhythmia ablation in complex congenital heart disease requires is challenging. Access to pulmonary venous atrium is not always required.
CS‐704‐CAB
A novel approach for identification of P1 potential in idiopathic left ventricular tachycardia—Estimation on characteristics of the circuit
Takahide Kadosaka 1; Taro Temma1; Kotaro Nishino1; Jiro Koya1; Daishiro Tatsuta1; Hiroyuki Natsui1; Motoki Nakao1; Masaya Watanabe2; Toshihisa Anzai1
1Department of Cardiovascular Medicine, Faculty of Medicine and Graduate School of Medicine, Hokkaido University, Sapporo, Japan; 2Department of Cardiovascular Medicine, Caress Sapporo Hokko Memorial Hospital, Sapporo, Japan
Background: Verapamil‐sensitive fascicular ventricular tachycardia (F‐VT) is the most common type of idiopathic left ventricular tachycardia (ILVT) in Asian young male patients. Although verapamil sensitive F‐VT is known as a reentry tachycardia, characteristics of its circuits is not fully elucidated.
Case: A 68‐year‐old man without structural heart disease was referred to our department for treatment of wide QRS tachycardia. During tachycardia, the 12‐lead ECG showed a right bundle branch block QRS morphology with a superior axis deviation. Intravenous injection of verapamil (5 mg) prolonged the tachycardia cycle length from 375 to 440 ms without termination. We performed electrophysiological study in conscious state. Multielectrode catheter was positioned in the left ventricular posterior septum. During sinus rhythm, left fascicular potentials following His‐bundle potential was recorded, but a delayed potential was not. However, S1–S2 stimulation from the right ventricular apex revealed a fractionated delayed potential. Interestingly, typical P1 and P2 potentials were recorded during the tachycardia from the electrodes where a delayed potential was observed. Radiofrequency application onto the site successfully terminated the VT.
Decision‐making: We could identify the P1 potentials by S1‐S2 stimulations before ablation and they showed polarity reverse at the middle of posterior septum. That may show the entrance of its circuit. This method has the potential to identify the ablation site even in cases tachycardia is difficult to induce or sustain.
Conclusion: We could identify the circuit of ILVT conducting S1–S2 stimulation and we will discuss the characteristics of its circuit from the polarity of the P1 potential.
CS‐719‐CAB
Fluoroscopy guided only cryoablation in paroxysmal atrial fibrillation
Ignatius Yansen 1,2; Simon Salim1,3; Muhammad Yamin1,3; Daniel Tanubudi1
1EKA Hospital, Tangerang, Indonesia; 2Tangerang District Hospital, Tangerang, Indonesia; 3Cipto Mangunkusumo National General Hospital, Central Jakarta, Indonesia
Background: Catheter ablation of atrial fibrillation (AF) is predicated on complete isolation of the pulmonary veins. Cryoablation or point‐by‐point radiofrequency ablation is used to perform electrical isolation. Cryoablation is comparable to RFA in terms of efficacy and safety, yet this procedure is faster. Cryoablation has become the primary treatment for paroxysmal AF. Recently, we perform this procedure using fluoroguided only methods.
Case: A physically active 53‐year‐old male with symptomatic palpitations once or twice per month. Holter monitoring reveals that he suffers from paroxysmal atrial fibrillation. While AF was present, he did experience shortness of breath during physical activity. His echocardiogram revealed normal dimensions of the heart and global normokinetics.
Decision‐making: Referral for ablation was made. We decided to perform cryoablation using the following fluoro‐only steps:
1. Patient was put in conscious sedation.
2. Transeptal procedure with SL1 long sheath, BRK needle using fluoroguided only using pigtail catheter in aorta as land mark for anteroinferior septal puncture (Figure 1A)
3. PVI using cryoballoon in all PV ostium. Direct isolation was observed directly during ablation (Figure 1B)
4. The puncture wound was then occluded using a figure‐of‐eight technique.
The patient was sent home the day following ablation, amiodarone was prescribed for 3 months, and holter monitoring was performed 3 months later.
Conclusion: Pulmonary vein isolation continues to be the primary treatment for paroxysmal atrial fibrillation. Cryoablation guided solely by fluoroscopy is a simple and feasible treatment for paroxysmal atrial fibrillation.
CS‐732‐CAB
First case of pulsed field ablation for pulmonary vein isolation in a patient with implantable upper‐airway neurostimulator to treat severe obstructive sleep apnea
Kars Neven 1,2; Stefan Hartl1,2; Anna Füting1,2; Nico Reinsch1,2
1Alfried Krupp Hospital, Essen, Germany; 2Witten/Herdecke University, Witten, Germany
Background: Pulsed field ablation (PFA) is a novel energy technology for AF. Obstructive sleep apnea (OSA) is an independent risk factor for AF and for PAP intolerant patients with moderate to severe OSA, hypoglossal neurostimulator implantation in a subcutaneous pocket in the right infraclavicular region to enable tongue protrusion is an option. A sensing electrode is placed in an intercostal space to detect inspiratory effort and a stimulation electrode is placed on the hypoglossal nerve. PFA seems to be safe in patients with CIEDs, but no experience with a hypoglossal neurostimulator has been reported.
Case: A 63‐year old male patient with paroxysmal AF (EHRA 3, CHA2DS2‐VASc 1, history of AF 120 months, BMI 29 kg/m2) and severe OSA (AHI 48/h) and a hypoglossal neurostimulator (Inspire Medical Systems) was scheduled for PFA‐PVI. The neurostimulator was turned off prior to PVI. PVI was performed under conscious sedation. All PV were isolated using a pentaspline ablation catheter (Farapulse). Total procedure time was 78 min, fluoroscopy time 31 min, and dose area product 10.65 Gy · cm2. No complications or desaturations occurred. Post‐ablation, neurostimulator functionality was normal. Flexible laryngoscopy demonstrated unimpaired patency at the level of the tongue during awake hypoglossal stimulation. During follow‐up, no arrhythmia recurrences were reported.
Conclusions: PFA for PVI was feasible and safe in a patient with an implantable hypoglossal neurostimulator and did not adversely affect the neurostimulator. Further studies are needed.
FIGURE RAO 30° fluoroscopic view showing the ablation catheter in flower configuration at the RSPV, in proximity to the neurostimulator.

CS‐743‐CAB
Focal ventricular tachycardia in established coronary artery disease: An entity rarely encountered
Jaskaran Singh Gujral 1; Sreenivas Reddy2
1Government Medical College and Hospital, Chandigarh, Chandigarh, India; 2Government Medical College and Hospital, Chandigarh, Chandigarh, India
Background: Scar Related Re‐entry is the most common mechanism of VT in structural heart disease. However, VT with focal origin may be rarely encountered in this subset.
Case: A 50‐year‐old gentleman with history of old inferior wall myocardial infarction, presented with one episode of self‐limiting syncope preceded by palpitations. Echocardiography was suggestive of akinetic inferior wall with moderate left ventricular dysfunction (40%–45%). The ECG (Figure 1A) recorded immediately after a repeat episode was suggestive of frequent runs of NSVT with inferior axis and right bundle branch morphology with early transition in V2. The patient was planned for Radiofrequency ablation after the occurrence of amiodarone induced sinus bradycardia requiring temporary pacemaker insertion.
Decision Making: Electroanatomic mapping of the left ventricle was performed using Ensite Precision (Abbot) system, using HD Grid catheter. Patient was having salvos of non‐sustained ventricular tachycardia which converted to sustained VT after isoprenaline infusion. Activation map (Figure 1B) was suggestive of earliest site of activation near anterolateral papillary muscle. The electrogram at the earliest site of activation was 37 ms ahead of the PVC onset (Figure 1C). Application of radiofrequency energy at the earliest site promptly terminated the VT (Figure 1D). No clinical tachycardia could be induced despite aggressive programmed extra‐stimulation with isoprenaline infusion till VERP.
Conclusion: It is essential to be cognizant that even in the presence of coronary artery disease, VT may be focal in origin. In such patients, VT may be targeted in an approach akin to idiopathic VT.
CS‐745‐CAB
Simultaneous dual tachycardia—A case report
Noha Elbanhawy1; Aruna Arujuna 1,2
1Lancashire Cardiac Centre, Victoria Hospital, Fylde Coast, Lancashire, UK; 2King's College London, UK
Background: Here we describe our observation of a simultaneous atrial and ventricular tachycardia on Holter and further investigated with an EP Study.
Case: The Holter recording of a 60 year old‐(M) patient captured both a narrow and broad complex tachycardia.
In the EP Lab the following observation was made:
1. Atrial pacing and Isoprenaline induced spontaneous broad complexes possibly Outflow Tract VEs, which rapidly degenerated into a sustained wide complex tachycardia similar to the Holter findings with periods of VA dissociation
2. Broad complex (BCT) start a second narrow complex tachycardia (NCT).
3. Broad complexes interrupted NCT in couplets occasionally with fusion of the initial ventricular beats but the NCT continued unperturbed.
4. Slow‐fast AVNRT diagnosed based on concentric sequence of retrograde atrial activation, with the earliest atrial electrogram recorded at the His, a short ventriculoatrial (VA) interval (VAHBE = 48 ms), the inability to pre‐excite the atria with His synchronous PVCs, a shorter HA interval during tachycardia (HA = 50 ms) than during ventricular pacing (HA = 70 ms). The presence of dual AV nodal pathway physiology with critical AH delay prior to the isoprenaline infusion
5. Following slow‐pathway ablation, only a broad complex tachycardia was inducible—3‐D mapping confirmed RVOT postero‐septal focus 34 ms pre‐surface QRS.
Decision Making: With NCT frequently induced we opted to start with slow pathway modification. Targeting both arrhythmia substrates was our goal since both were distinct (PVCs persisted after slow pathway modification).
Conclusion: When double tachycardia is observed a step‐wise approach is required.
CS‐755‐CAB
Catheter ablation from coronary sinus ostium for typical atrioventricular nodal reentrant tachycardia
Gaku Hatayama; Satoshi Miyazawa
Sendai Cardiovascular Center, Japan
Objectives: Slow pathway (SP) ablation is an established therapeutic approach for slow‐fast atrioventricular nodal reentrant tachycardia (AVNRT). Usually, radiofrequency energy is delivered at the inferior or mid part of the triangle of Koch to eliminate SP conduction. However, it is difficult to deliver sufficient energy at these areas in the vicinity of the conduction system in some cases.
This study aims to evaluate the efficacy and the safety of SP ablation from the ostium of the coronary sinus (CSos).
Materials and Methods: A total of 32 patients who were diagnosed as typical AVNRT by electrophysiology study in Sendai Cardiovascular Center were enrolled. Conventional SP ablation was performed along the tricuspid annulus (TA) in all patients. Additional application was delivered from CSos and case effective junctional rhythm was not observed during index application. Furthermore, it was considered a high risk to bring an atrioventricular block with additional ablation closer to the site of the conduction system along the tricuspid annulus. A total of eight patients underwent CSos ablation.
Results: Effective junctional rhythm was observed during application, with which cycle length was 626 ± 93 ms. Slow pathway conduction was eliminated and clinical tachycardia was not inducible by programmed stimulation at the end of the procedure in all patients. AH and HV duration were not affected by application from CSos. No adverse events were observed including conduction disturbance.
Conclusion: SP ablation from CSos was considered to be effective and safe.
CS‐757‐CAB
Successful ablation via endocardial approach for right atrial appendage accessory connection to right ventricle participating in rare reciprocating tachycardia utilizing dual accessory pathways
Jason Tan; Chatyapa S. Sriprom; Supaluck Kanjanauthai
Pediatric Cardiology, Pediatric Department, Faculty of Medicine Siriraj Hospital, Bangkok, Thailand
Background: Rare cases of right atrial appendage (RAA) accessory pathway (AP) ablation via endocardial approach were described.
Case: Ten‐year old boy who has normal structural heart presented with wide complex tachycardia (WCT). Figure showed baseline EKGs had two different delta wave patterns. WCT morphology was RBBB with superior axis. Multiple adenosine administrations failed to terminate WCT. Electrophysiologic study found inducible orthodromic reciprocating tachycardia (ORT) utilizing retrograde activation via RAA AP. Interestingly, during second inducible tachycardia as WCT (pre‐excited tachycardia) antegrade HIS activation (HV 0–12 ms) was found fusing with antegrade activation via left‐sided AP and retrogradely up RAA AP. EP findings were likely consistent with AP to AP tachycardia in this adenosine‐insensitive WCT.
Decision‐making: RF ablation (RFA) targeted at RAA pocket resulted in VA dissociation and change pre‐excitation pattern. Second set of RFA eliminated antegrade only left‐posterior AP.
Conclusion: First to describe endocardial ablation of RAA AP which participating in reciprocating tachycardia via dual accessory pathway.

CS‐774‐CAB
Extracorporeal membrane oxygenation assisted radiofrequency ablation for scar‐related ventricular tachycardia
Dongdong Que; Liyun Feng; Xudong Song; Pingzhen Yang
Zhujiang Hospital, Southern Medical University, Guangzhou City, China
Background: Despite the superiority of precisely illustrating the critical isthmus, activation mapping tends to cease abruptly in scar‐related ventricular tachycardia (VT) due to unstable haemodynamics. Extracorporeal membrane oxygenation (ECMO) provides a safe mapping environment.
Case: A 51‐year‐old man was admitted for recurrent syncope and a synchronized electrical cardioversion was delivered because of documented VT together with hypotensive shock. The VT was with complete right bundle branch block and left axis deviation. Coronary artery angiography and cardiac structure were normal.
Decision‐making: Given the unstable VT, ECMO assisted radiofrequency ablation was recommended. With the 3‐dimensional (3D) electroanatomic system (Boston Scientific), the left ventricular endocardium was mapped with the Orion basket catheter in sinus rhythm demonstrating normal substrate and voltage. Low voltage areas with late potential (LP) were located at the lateral posterior wall near the basis of the epicardium. With the Orion basket catheter bursting at the LP area, the other VT with complete right bundle branch block and right axis deviation was successfully induced after the implementation of ECMO. Regardless of the deteriorated blood pressure, epicardial remapping delineated a precise type‐8 reentry at the area of LP. The VT quitted after the first attempt ablation at the exit of the reentry and homogenizing ablation was further proceeded covering the area of LP, ultimately.
Decision‐making Conclusion: ECMO enables activation mapping in scar‐related VT and homogenizing ablation of LP is necessitated because of various reentries possibly assembled by remaining myocardium.
CS‐830‐CAB
Entrapment of ablation catheter in right pulmonary veins requiring surgical intervention: A rare complication in pulmonary vein isolation
Jonathan Lipton 1; Stephanie Cruise1; Simon Pitt1; Rajiv Sharma1
1Royal Hobart Hospital, Hobart, Australia; 2University of Tasmania, Hobart, Australia
Background: Pulmonary vein isolation (PVI) is a commonly performed and safe procedure, but can rarely be complicated by the need for cardiothoracic surgery.
Case: A 61‐year‐old male underwent redo PVI for symptomatic atrial fibrillation (AF). The procedure was conducted under general anesthesia, and transesophageal echocardiography (TEE) guided double transseptal access was obtained. Ensite‐X mapping system, along with a HD‐grid mapping catheter and DF‐curve TactiFlex ablation catheter, was used for mapping and ablation to address reconnection of the right pulmonary veins. During the catheter retraction from the right inferior pulmonary vein, resistance was encountered. TEE revealed a thin echodense structure connecting the catheter tip to the vein, and further traction resulted in tenting of the vein. This finding indicated entrapment/entanglement of the catheter tip in venous tissue.
Cardiothoracic consultation was sought, and surgical removal was recommended. Cardiopulmonary bypass was established, left atrial access obtained, and the catheter, entangled in fragile pulmonary venous tissue, was carefully removed. Manufacturer analysis found no catheter defects, and the patient made a full recovery.
This is the first reported case of pulmonary vein entrapment involving the TactiFlex ablation catheter. Pulmonary vein catheter entrapment is a rare complication in left atrial ablation, typically occurring during rotation of a curved catheter, and usually necessitates surgical intervention, although transvenous removal with traction and rotation has been described.
Conclusion: Catheter entrapment within a pulmonary vein is a rare complication characterized by inability to retract the catheter. Diagnosis is confirmed by TEE and can guide management, which usually involves surgical removal.
CS‐843‐CAB
Radiofrequency ablation for atrial fibrillation in a patient with dextrocardia and interruption of the inferior vena cava
Shengjie Wu; Fangyi Xiao
The First Affiliated Hospital of Wenzhou Medical University, China
Background: Mirror Dextrocardia with interruption of inferior vena cava (I‐IVC) is an extremely rare disease, while the experience of radiofrequency ablation for AF in this population is even less.
Case: A 57‐year‐old man with symptomatic persistent AF was referred to hospital. The preoperative examination indicated situs inversus dextrocardia with I‐IVC. The femoral vein connected with the azygos vein and flowed into the superior vena cava (SVC), while the jugular vein flowed into the SVC normally. An intracardiac echocardiography (ICE) and CS electrode were introduced via the femoral vein and a VIZIGO sheath was placed into internal jugular vein. After 3D anatomical reconstruction by ICE, transseptal puncture was performed under ICE using a J‐tip guidewire with 30 W electric cutting by high‐frequency electric knife. A “σ”‐shape of ablation catheter was restructured to ablate the anterior wall of the right pulmonary vein because of lacking sufficient operating space. Then electrical cardioversion was performed and SVC was ablated. At 3‐month post‐ablation, the patient was asymptomatic without recurrence of arrhythmia.
Decision‐making: (1) Compared to the transhepatic or retrograde aortic approach, transseptal access using a superior approach is more safety and feasibility using the existing equipment; (2) transseptal puncture can be performed precisely and efficiently under ICE using a J‐tip guidewire and high‐frequency electric knife; (3) The abnormal anatomy of azygos vein and SVC may trigger atrial fibrillation, so SVC ablation was performed.
Conclusion: Radiofrequency ablation for AF in patients with mirror dextrocardia and I‐IVC can be performed safety and efficiently using ICE and VIZIGO sheath via an SVC access.
CS‐847‐CAB
Unusual premature ventricular complex location mimicking right ventricular outflow tract origin
Danlu Liang; Cameron Mccormack; Aidan Holmes; Tina Lin
Austin Health, Heidelberg, Australia
Background: RVOT PVCs are common, with ECG demonstrating LBBB‐morphology, inferior‐axis. We describe a case of RVOT‐appearing PVCs on ECG; however, mapping showed an unusual location at the annulus adjacent to RVOT.
Case: Twenty‐nine‐year‐old woman presents with symptomatic RVOT‐appearing PVCs on ECG (Figure 1A) with 42% PVC burden on holter. TTE revealed structurally normal heart. She was managed on flecainide with ongoing palpitations and underwent ablation.
Decision‐making: Activation mapping was earliest at annulus (Figure 1B) but His‐signals were present. A position was found with earliest ventricular activation preceding QRS by 30 ms (blue dot) which did not show His‐signals and 30 W radiofrequency was applied for 60 s with immediate suppression of ectopy and no heart‐block.
Conclusion: This case highlights an uncommon and difficult PVC location adjacent to His and RVOT base with ECG mimicking RVOT origin. Electrophysiology‐study is gold‐standard to diagnose, and vigilance must be maintained to ensure local His‐signals are absent when ablating.

CS‐848‐CAB
Supraventricular tachycardia in Wolff–Parkinson–White syndrome in a pediatric patient—Case report
Luqman Hakim Andira 1; Dara Ninggar Ghassani1; Muhammad Rifqi Arya Putra2; Rerdin Julario1
1Department of Cardiology and Vascular Medicine, Faculty of Medicine ‐ Airlangga University ‐ Soetomo General Hospital, Surabaya, East Java, Indonesia, Surabaya, Indonesia; 2Faculty of Medicine ‐ Airlangga University ‐ Soetomo General Hospital, Surabaya, East Java, Indonesia
Background: Wolff–Parkinson–White (WPW) syndrome is a congenital cardiac preexcitation syndrome due to abnormal cardiac electrical conduction through accessory pathways (AP) that can result in life‐threatening arrhythmias. Some accessory pathways will not manifest the described typical electrocardiogram (ECG) findings. Patients with WPW are frequently susceptible to paroxysmal supraventricular tachycardia (SVT). Atrioventricular Re‐entrant Tachycardia (AVRT) is the most common cause of SVT in young children. Catheter ablation offers a potential cure for WPW syndrome.
Case: A 12‐year‐old boy was referred for electrophysiology opinion following the finding of documented SVT and a history of recurrent palpitation for 1 year without specific trigger. ECG showed normal sinus rhythm and echocardiogram was normal. Followingly, he underwent electrophysiology study (EPS). Ventricle overdrive pacing showed VAV pattern, PPI–TCL <115 ms and AV fusion at CS 1–2. Other pacing maneuver revealed: WP retrograde 265 ms, AVN ERP retrograde 270 ms, WP antegrade 340 ms, AVN ERP antegrade <290 ms, and WP retrograde 275 ms.
Decision‐making: Radiofrequency ablation (RFA) is a treatment of choice when the EPS result revealed a WPW, specifically a LLAP WPW. After multiple RFA, there was AV dissociation, then we performed ventricular pacing and AV dissociation remained. We investigated SNRT and CSNRT, the results were within normal limits.
Conclusion: RFA is a highly successful approach for patient with WPW syndrome and it can prevent the risk of SCD from arrhythmia.

CS‐850‐CAB
Subvalvular catheter approach for ablation of a challenging right sided accessory pathway
Vijay Shekar 1
Apollo Hospitals, Tiruchirapalli, India
Background: Conventional approach to catheter ablation of right‐sided accessory pathways (APs) can be challenging and may require alternate strategies in select cases.
Case: A 31 year‐old male presented with palpitations and syncope. Patient underwent cardioversion for pre excited atrial fibrillation. Baseline ECG showed preexcitation suggestive of right sided AP. During electrophysiology study, the AP was localized to 6–7 o'clock position of the tricuspid annulus. Conventional catheter ablation failed to eliminate the AP. Ablation was successfully accomplished using a sub valvular catheter approach and adopting open window mapping strategy.
Decision‐making: The sub valvular approach was chosen, as the conventional approach failed to reach the ventricular insertion of the AP. This approach also ensured good catheter stability and contact. The open window mapping strategy aided in precise localization of the AP.
Conclusion: Adopting novel mapping (open window) techniques and alternate catheter approach (sub valvular) during ablation helps improve the procedural outcomes of challenging right sided APs.

CS‐873‐CAB
Bipolar ablation for recurrent and failed orthodromic AVRT due to right lateral accessory pathway
Suresh Allamsetty
Medicover Hospital, Visakhapatnam, India
Background: Mapping and ablation of right free wall accessory pathways (AP) is more difficult because of absence of venous structure paralleling the tricuspid annulus and because of catheter instability.
Case: A 34 year old male presented with recurrent palpitations since 1 year. He had history of ablation of AP in the past. Baseline ECG showed preexcitation. He underwent EP study and orthodromic AVRT was induced due to right lateral AP. Ablation of right lateral AP was attempted using initially with non‐irrigated ablation catheter and as there was no effect flexibility irrigated ablation catheter was used for ablation. There was no AVRT induced but preexcitation persisted. He was kept on Flecainide and metoprolol. Again after 1 month he came with persistent palpitations since 2 days.
Decision Making: Long sheath was used for ablation, superior approach using jugular approach and using half normal saline for irrigated ablation catheter was tried. All the above methods were futile. Hence bipolar ablation set up was done. Ablation catheter from jugular route was connected to the anodal end of ablator via an 85 641 ablation cable and the cathode port of ablator was connected to the jumper cable via a custom made cable for grounding. Jumper cable was connected to the junction box. The other end of the jumper cable was connected to the catheter via femoral approach through an Inquiry decapolar cable and the circuit was completed. Successful RFA of AP was done.
Conclusion: Bipolar RFA is feasible for difficult APs with good success rate.

CS‐874‐CAB
Polymorphic PVC induced cardiomyopathy: Atrium as a vantage point
Darshan Krishnappa; Deepak Padmanabhan; C. N. Manjunath
Sri Jayadeva Institute of Cardiovascular Sciences and Research, India
Background: High burden PVCs are a frequent cause of left ventricular systolic dysfunction (LVSD). While most frequently monomorphic, some patients have polymorphic PVCs which adversely impact ablation outcomes.
Case: A 68 year old male presented with history of palpitations. On evaluation he was noted to have bigeminal PVCs on his ECG while echocardiogram showed LVSD with an EF of 30%. 24 h holter showed a PVC burden of 28% with two dominant PVC morphologies‐PVC1 and PVC2 (Figure A,B).
PVC1 was mapped in the GCV/AIV and aortic sinuses. Earliest activation was in the LCC and ablation here led to suppression of PVC1. PVC2 was then mapped (Figure B) in the LV. Earliest activation was in the postero‐superior process of the LV. Ablation here led to a change in the PVC morphology (PVC3) which had a similar axis but was now broader and notched. Activation mapping of PVC3 (Figure C) in the LV and right atrium (RA) now showed earliest activation in the RA in the region of the slow pathway. Ablation in the RA led to complete suppression of PVC2/3. Postoperative period was uneventful with no PVC seen.
Decision Making: Mapping of neighbouring sites—the GCV/AIV and the aortic sinuses for PVC1 and in case of PVC2 the RA (triangle of Koch region) and the postero‐superior process of LV. Epicardial sites in certain regions cannot be accessed via pericardial access but instead need to be approached from vantage points of neighbouring structures.
Conclusion: Knowledge of vantage points is essential while mapping and ablating PVCs of epicardial/intramural origin.

CS‐87‐CIED
The first leadless pacemaker implantation for symptomatic sinus node dysfunction and second supra‐hisian atrial ventricular block for old dementia patient and colon cancer with colostomy
Minh Hoang Quang; Van Tran Dai Quynh
FV Hospital, Ho Chi Minh, Viet Nam
Background: Dizziness, near‐syncope is difficult to define due to intrinsic bradycardia or cause by vaso vagal.
Case: The 88 year male patient had history of colon cancer. He noted sinus bradycardia with symptom a lot of time at home. Every time like that, he also had flash abdominal pain.
This admission, he had episode of dizziness, near‐syncope and also abdominal pain, blood pressure machine showed slow heart rate 38 bpm at home and ECG showed sinus bradycardia (Panel A).
The abdominal CT scan and blood test was performed immediately and showed normal (Panel B).
The sinus bradycardia continue screening with ECG stress test was performed to prove the chronotrop incompetence, the maximum heart rate (HR) on exertion 102 bpm, % maximum predicted HR get 77% on treadmill.
Moreover, the indication electrophysiology study for syncope was performed and showed maximum corrected SNRT 3070 ms at 300 ms and second degree AV suprahisian block 2:1 at 460 ms RA pacing (Panel C).
The final diagnosis was symptomatic sinus node dysfunction. The pacemaker implantation was indicated and the choice of leadless pacemaker.
The procedure was performed and implanted at apical septal with good parameter 0.88 V/0.24 ms, 590 Ohm (Figure 3).
Decision‐making: The colostomy on the dementia patient is easy to make risk of infection because the bad habit colostomy touching. So after the pacemaker indication, the choosing leadless pacemaker implantation was performed using shared decision‐making.
Conclusion: The leadless pacemaker implantation should be considered for old patient colon cancer with colostomy.

CS‐99‐CIED
A permanent pacemaker patient with positional syncope
Syed Haseeb Raza Naqvi; Madiha Fatima; Pir Sheeraz Ali; Faisal Qadir
Mukhtar A. Sheikh Hospital, Pakistan
Background: Post‐pacemaker implantation complications lead to significant morbidity and mortality in patients with syncope.
Case: A 60 year old lady was admitted in cardiology service with hypertensive heart failure symptoms. She had history of a VVI permanent pacemaker implantation 7 years back for complete heart block. Pacemaker was interrogated 8 months back and revealed appropriate pacemaker function. She was stabilized with medical therapy. ECG showed paced rhythm at 60 beats/min and echocardiography was normal.
On third day of hospitalization she developed episode of brief syncope in the morning while she was sitting up on bed. The patient's pacemaker device was interrogated at bedside; parameters came out to be normal. Sensing could not be evaluated because of pacemaker dependency.
Interestingly, when the patient sat up on bed to give history, she complained of dizziness and an intermittent high grade AV block with loss of pacing was seen on the bedside cardiac monitor. She lied on the bed immediately with resumption of normal pacing. Further device interrogation showed chronic escalation of lead impedance trends to maximum values >4000 ohm in the last 1 month, consistent with lead fracture. Bedside provocative maneuvers were positive for intermittent ventricular oversensing with inhibition of pacing.
Decision Making: New DDD pacemaker was implanted from the right side. The old pacemaker generator was explanted and the old fractured lead was capped. The patient was discharged home the following day. She was doing well at 1 month follow‐up.
Conclusion: Integration of posture to syncope should never be missed to diagnose syncope related complications.
CS‐118‐CIED
Leadless pacemaker implantation through jugular vein: An exceptional bailout strategy in inaccessible conventional route
Tommy Daindes; Faten Aqilah Aris; Hisham Md Shahrom; Rohith Stanislaus; Azlan Hussin
Institut Jantung Negara, Kuala Lumpur, Malaysia
Background: The leadless pacing system is usually implanted through a common femoral vein (CFV). We present the feasibility of the right internal jugular vein (RIJV) as an alternative route through the two cases below.
Cases: Case‐1: A 16‐year‐old girl came with an infected DDDR PPM implanted 6 months before admission. After 2 weeks of IV antibiotics, the old device was extracted. A week later the Leadless Pacemaker system was implanted. Measurement of both CFVs showed inadequate size (Ꝋ6.7–7.0 mm). The procedure proceeded through the RIJV (Ꝋ15.3 mm) using standard pre‐dilatation tools. Leadless Pacemaker attached in mid‐RV septum uneventfully with satisfying electrical parameters, unless the high threshold (3.38 V at 0.24 ms).
Case‐2: An 82‐year‐old female with Symptomatic Sinus Bradycardia came for elective Leadless Pacemaker Implantation. During the Procedure, the wire was unable to pass IVC through both CFVs. Venogram showed IVC stenosis and the procedure continued with the RIJV approach. Standard pre‐dilatation was performed and Leadless Pacemaker system was successfully implanted in the low‐RV septum with good electrical parameters achieved.
Decision‐making: Case‐1: The RIJ approach is the only choice left regarding anatomical handicaps. Despite the high threshold, the limited availability of attachment sites as a consequence of previous device infection makes the achieved electrical parameters acceptable.
Case‐2: The RIJ approach may become a good alternative in patients with impassable IVC, proven with good electrical parameters.
Conclusion: Nowadays, the CFV is still the mainstream approach for Leadless Pacemaker Implantation. However, the RJIV approach may become an alternative with similar technical steps and comparable electrical outcomes.

CS‐134‐CIED
Patent foramen ovale can lead to inadvertent misplacement of pacing leads
Michael Tierney; Jorge Moragues; Sukhmandeep Sangha; Judy Al Ahmad; Ivan Subiakto
Wollongong Hospital, Wollongong, Australia
Background: Inadvertent lead malposition in the left heart (ILMLH) is a rare complication of cardiac implantable electronic device insertion. In a cohort of 2000 patients it occurred in 0.34% of implantations. It can lead to serious complications such as systemic embolism, which is the presentation of ILMLH in 57% of cases. If ILMLH occurs, prevention of systemic embolism with lead revision or lifelong anticoagulation has high rates of complications, thus intraoperative identification of ILMLH is imperative.
Case: A 61‐year old female underwent dual‐chamber permanent pacemaker insertion for sick sinus syndrome. During right ventricular (RV) lead insertion there was suspicion of ILMLH because the lead trajectory occurred more superior than the anticipated tricuspid annulus and the lead crossed the left lateral spine border. Intravenous insertion was confirmed by identifying the sheath J‐wire in the inferior vena cava. After intraoperative repositioning a classical RV fluoroscopic lead trajectory resulted. Initial ILMLH (ventricular) was confirmed with analysis of the pre‐and‐post repositioning QRS morphology and lead parameters.
Decision Making: Careful multiple‐angle fluoroscopic examination of the RV lead allowed intraoperative identification and correction of ILMLH. The majority of ILMLH is due to patent foramen ovale (PFO) though rarely can be secondary to undiagnosed complex congenital heart disease. This patient's echocardiogram demonstrated an aneurysmal interatrial septum and suspected PFO.
Summary: This rare case demonstrates that ILMLH can happen inadvertently and can be avoided by routine multiple‐angle fluoroscopy. When there is suspicion of ILMLH immediate repositioning can confirm malposition and avoids serious consequences such as systemic embolism.
CS‐175‐CIED
Left‐sided implant of central sleep apnea device with traditional pacing leads facilitated by 3D‐mapping
Rahul Doshi; Amy Kleinhans
Honorhealth, Scottsdale, USA
Background: Phrenic nerve stimulation (PNS) for the treatment of central sleep apnea (CSA) is most often achieved with left pericardiophrenic (PCP) vein electrode. The alternate superior vena cava stimulation electrode is used in >20% of implants and is associated with higher thresholds with less stable capture. Alternative options when both are not effective are lacking.
Case Presentation: 71 years/old with severe CSA and had prior successful Remede phrenic nerve stimulator with left PCP lead. He did well until generator replacement with resultant lead fracture. He underwent removal with right stimulation electrode implant with elevated capture thresholds and ineffective treatment confirmed by sleep study. The patient was referred for system revision. He underwent right sided device/lead removal with an attempt to locate the PCP vein via the inferior pericardiophrenic vein. He was brought for left‐sided implant with active fixation pacing leads.
Left‐sided implantation was performed with a subcutaneous pocket and axillary access in the usual fashion. Mapping for the right phrenic nerve was performed from the right femoral vein with a deflectable quadripolar catheter and a 3D‐mapping system. This served as a guide for two 6‐Fr active fixation pacing leads via a deflectable splitable sheath. PNS was achieved with strong diaphragmatic excursion ranged from 4 to 6 mA and impedance 500–600 ohm. The patient has been followed >1 year with stable thresholds and good response.
Conclusion: PNS for CSA treatment can be achieved via traditional active fixation pacing leads with 3D‐mapping and is an option for patients who require system revision.
CS‐234‐CIED
Three cases of transvenous pacemaker infection in which infected device removal and leadless pacemaker Micra implantation were performed simultaneously
Tomoko Tada; Shigetoshi Sakabe; Soichiro Kobayashi; Hokuto Yamagishi; Tatsuya Mori; Kenji Nakamura; Masahide Horiguchi; Takeshi Takamura; Katsuyuki Tone; Kenichi Maeno; Tetsuya Seko; Atsunobu Kasai
Japanese Red Cross Ise Hospital, Ise, Japan
Background: Temporary extracorporeal pacing in device‐related infections in pacing‐dependent patients leads to pacing failure and prolonged hospitalization. On the other hand, the Micra registry has reported no problems with the implantation of Micra at the same time as the removal of an infected transvenous pacemaker (TVM).
Cases: TVM removal and Micra transplantation were performed in three patients. Case 1 was a woman in her 80 s with TVM infection secondary to lower leg cellulitis, in which methicillin‐susceptible Staphylococcus aureus (MSSA) was cultured; antimicrobial chemotherapy was started before TVM removal and Micra implantation, which was completed with wound healing. Case 2 was a male hemodialysis patient in his 60 s who was on Minocycline (MINO) due to an artificial vascular infection caused by methicillin‐resistant Staphylococcus aureus (MRSA); 1 year later, he developed an infection at the TVM implantation site; the removal of TVM and a Micra transplantation were performed simultaneously. The patient continues to be on MINO and is doing well. Case 3 was a woman with hemodialysis in her 70 s who developed a TVM infection caused by MRSA after a refractory knee synovial infection; TVM removal and Micra implantation were carried out on the same day, but the knee infection did not resolve, and the patient died of multi‐organ failure.
Decision‐making: The goal was to reduce the harmful effects of temporary extracorporeal pacing, such as infection, dislodgement, and prolonged hospitalization.
Conclusion: Removal of the infected TVM and transplantation of Micra simultaneously can be effective if the infection is adequately controlled.
CS‐244‐CIED
Staged total device protection of patients with atrial fibrillation: A case report
Chaodi Cheng 1; Yanjiang Wang1; Liang Shi1; Ying Tian2; Xingpeng Liu1
1Chaoyang Hospital, Capital Medical University, Beijing, China; 2Department of Cardiology, Beijing Tiantan Hospital, Beijing, China
Background: In atrial fibrillation (AF) patients, left atrial appendage occlusion (LAAO) is an alternative to anticoagulation to offset the risk of bleeding, and atrioventricular node (AVN) ablation combined with physiological pacing is considered one of the last resorts for rate and rhythm control.
Case: An 81‐year‐old female presented with symptomatic persistent atrial flutter (AFL) despite two AF catheter ablations. Her past medical history was notable for hypertension, ischemic stroke, chronic anemia caused by upper Gastrointestinal bleeding, and venous thromboembolism. CHA2DS2‐Vasc and HAS‐BLED scores were both high (6 and 3, respectively).
Decision‐making: LAAO was performed alternative to anticoagulation. Because of severe symptomatic AFL (Figure 1A) after optimal pharmacological management, she was indicated for AVN ablation and his bundle pacing.
Conclusion: We provide a staged “total protection” strategy for refractory AF treatment including initial ablations, LAAO implantation and HBP to balance risk.

CS‐249‐CIED
A case of endocardial dissection caused by Micra implantation
Shuai Shang; Jianghua Zhang; Baopeng Tang
Department of Pacing and Electrophysiology, The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
Background: A case of endocardial dissection caused by a device cup of the Micra transcatheter pacing system was suspected in a 77‐year‐old female.
Case: Right ventriculography was performed, showing that the endocardium was intact and that no abnormality was found. The delivery catheter was guided to the right mid‐ventricular septum, the right and left anterior oblique to ensure that the device cup was placed on the ventricular septum, and the contrast agent was injected to identify the location where the Micra was to be released, showing contrast agent residuals. The cup was pocket‐shaped with a large mouth and small tail, with an opening diameter of approximately 25 mm. The position was adjusted to the middle of the septum, and reimaging showed that the contrast medium was extravasated into the pericardial space. The Micra release cup was adjusted and sent to the high septum, and the Micra was released here. Approximately 20 min after the release of the Micra, the patient's blood pressure began to drop to 74/59 mmHg, and fluoroscopy showed that her cardiac shadow beat was weakened. Considering pericardial tamponade, we performed pericardiocentesis and drainage of approximately 100 mL of bloody pericardial effusion, after which the patient's vital signs remained stable.
Decision‐making: In the case, the endocardial rupture may have occurred at the edge of the Micra release cup at the time of positioning, and the rapid injection of the contrast medium here caused the endocardial tear and dissection due to its impact, so residual contrast medium appeared here.
CS‐294‐CIED
CRT implantation in a patient with left superior vena cava drain into the right atrium without passing through the coronary veins
Vien Hoang Long; Pham Tran Linh; Nguyen Thi Le Thuy; Nguyen Duy Tuan
Vietnam National Heart Institute, Viet Nam
Background: Pacemaker implantation in patients with LSVC often presents many challenges, particularly with CRT.
Case: A 52‐year‐old male patient diagnosed with severe heart failure due to dilated cardiomyopathy since May 2020 has been treated with Sacubitril/Valsartan 100 mg/day, metoprolol 25 mg/day, spironolactone 25 mg/day, and furosemide 40 mg/day. After 6 months of optimal treatment, the patient's follow‐up examination revealed an ejection fraction (EF) was 23%, Dd: 78 mm, Ds: 65 mm and moderate mitral regurgitation. The patient was recommended to undergo cardiac resynchronization therapy (CRT) device implantation. However, during the procedure of implanting the CRT device via the left subclavian vein, the presence of LSVC was detected.
Decision‐making: Particularly in this patient, when performing contrast angiography via the usual hand injection, the presence of the coronary sinus was not visualized. We decided to repeat the angiography using a 5F Pigtail catheter with the assistance of an automated contrast injector, which revealed the trace of the coronary sinus (with a relatively small size). The LSVC drained into the right atrium without passing through the coronary veins We utilized the JR4 catheter and the Asahi 165 extension guidewire for support and to position the LV lead.
Conclusion: The presence of the LSVC is one of the anatomical variations that can pose challenges and complexities in the implantation of pacemakers, defibrillators, or cardiac resynchronization therapy devices. In such cases, it is necessary to be prepared and select appropriate supportive tools.

CS‐304‐CIED
Delayed wound dehiscence with mucoid discharge of subcutaneous implantable cardioverter‐defibrillator at the subxiphoid area: Subcutaneous silk suture reaction without infection or allergy
Han‐Joon Bae; Se Hun Kim; Sung‐Eun Kim; Young Soo Lee
Daegu Catholic University, Daegu, South Korea
Background: Subcutaneous ICD (S‐ICD) offer a theoretical advantage over trans‐venous ICDs (TV‐ICD) by lowering the risk of systemic infection and endocarditis. The superficial skin and soft tissue infection rates are more highly reported.
Case: An 18‐year‐old male with arrest underwent S‐ICD (Boston Scientific). The prophylactic antibiotic was administered according to protocol. The device was implanted using a three‐incision technique.
One month later, he complained of a skin defect in the subxiphoid area. The patient was admitted with mucoid secretion at the subxiphoid area. The wound culture has not reported any bacteria. Although two times of revisions were performed, poor wound healing was continuously observed. Finally, the device was removed, and a new TV‐ICD was implanted on the left chest.
However, 3 weeks later, mucoid discharge was drained, and the device was exposed. wound culture, and blood analysis were all in a normal range.
Decision‐making: He had no allergies to any materials except to a cat. Finally, previously used materials including metal and silk sutures were placed under the skin in order to identify the cause. After 2 weeks, mucoid discharge was seen only in the pocket where the silk suture was placed. In the end, another TV‐ICD was implanted on the right chest without silk. The device wound healed well without any inflammation or infection signs for over 6 month‐follow periods.
Conclusion: Silk reaction should be included in the differential diagnosis of patients who present wound breakdown or apparent wound infection.

CS‐308‐CIED
The Bornean's cheetah for CIED infection
Stephanie Yen Li Chang; Zhao Ming Lee; Jhi Hui Foo
Cardiology Department, Hospital Queen Elizabeth II, Kota Kinabalu, Malaysia
Background: CITA (continuous, in situ‐targeted, ultrahigh concentration of antibiotics) treatment for infected subcutaneous device pocket is safe and effective for patients of high‐risk lead extraction or those opted for less invasive intervention.
Case: A 90‐year‐old gentleman with 10‐year single‐chamber pacemaker for pacing dependent complete heart block had pocket infection after box change, and failed response to 25 days of systemic antibiotics. He was started on total 14‐day CITA with vancomycin and gentamicin. His infection resolved and was discharged well.
Decision Making: The initial decisions were lead extraction/device removal with new implant or MICRA implantation plus box removal without lead extraction. We decided to proceed with CITA due to high risk of lead extraction. It is a less invasive approach and mitigated the risk of surgery.
Conclusion: This is the first successful CITA for infected CIED reported in Asia. However, more studies are needed to verify the efficacy of CITA.

CS‐321‐CIED
Successful cardiac resynchronization therapy defibrillator implantation with shock lead placement in the left bundle branch area
Kenta Yoshida; Mitsuru Yoshino; Tokuma Kawabata; Hironobu Sumiyoshi; Ryuki Chatani; Atsushi Sakata; Hiroshi Tasaka; Kazushige Kadota
Kurashiki Central Hospital, Japan
Background: Cardiac resynchronization therapy (CRT) with biventricular pacing (BVP) is a well‐established therapy. Left bundle branch area (LBBA) pacing has been shown to be a safe and more physiological alternative to BVP, and left bundle branch pacing‐optimized cardiac resynchronization therapy has been shown to provide better electrical resynchronization than BVP‐CRT alone. However, shock lead placement in the LBBA in CRT‐D implantation has not been described.
Case: The patient was a 76‐year‐old woman with dilated cardiomyopathy on optimal medical therapy, and her baseline electrocardiogram was in sinus rhythm with a left bundle branch block pattern (QRS duration 160 ms). Her left ventricular ejection fraction was 32.0%, and her physical status was New York Heart Association class III. Holter monitoring showed frequent multifocal ventricular premature beats and non‐sustained ventricular tachycardia. CRT‐D implantation was performed due to worsening heart failure symptoms.
Decision‐making: Since the Agilis HisPro catheter has two 90° deflections, we reshaped it between the first and second deflection and added a septal curve. This allowed us to screw the shock lead deep into the ventricular septum and achieve QRS narrowing of the right ventricular pace (127 ms). The time from stimulus to left ventricular activation was 84 ms. The coronary sinus lead and right atrial lead were placed in the conventional manner. Finally, a defibrillation threshold test confirmed successful treatment. No adverse events occurred after the procedure.
Conclusion: Reshaping the Agilis HisPro catheter enabled shock lead placement in the LBBA.
CS‐343‐CIED
Ankylosing spondylitis combining severe bradycardia treated with leadless pacemaker implantation—A case report
Yongqiang Fan; Jianghua Zhang; Zukela Tuerhong; Shuai Shang; Xianhui Zhou; Yaodong Li; Qiang Xing; Yankai Guo; Jiasuoer Xiaokereti; Yanmei Lu; Baopeng Tang
Xinjiang Medical University Affiliated First Hospital, China
Background: Traditional intravenous pacing implantation is difficult in patients with thoracic malformation and cardiac compression combined with severe bradycardia.
Case Presentation: We present a case of an 80‐year‐old man who underwent leadless pacemaker implantation. For ankylosing spondylitis, the patient cannot lie flat. The traditional subclavian vein approach is not easy to perform, therefore we decided to implant a leadless pacemaker. The implantation process is smooth without complications.
Conclusions: Therefore, implantation of leadless pacemaker is a method to treat severe bradycardia patients with thoracic malformation and cardiac compression.
CS‐364‐CIED
Delayed pacemaker generator pocket primary infection due to Burkholderia cepacia
Marie Kirk Patrich Maramara; Kaye Eunice Lustestica; Kevin Enriquez; Michael Joseph Agbayani
Philippine Heart Association, Philippines
Background: Staphylococcus sp. is responsible for the majority of CIED infection cases, pacemaker pocket infections caused by Burkholderia cepacia are rare, and only a few cases have been reported in the literature.
Case: A 57‐year‐old woman presented with swelling, tenderness, and pain at her pacemaker pocket site, which had persisted for 7 months despite multiple antibiotic treatments. She had a medical history of hypertension, diabetes and third degree AV block and had undergone dual chamber pacemaker implantation in 2021. Upon admission, a physical examination revealed swelling, tenderness and ulceration at the pacemaker pocket site. The patient was started on Vancomycin and Ceftazidime, and the pulse generator and leads were removed. A temporary pacemaker was inserted since the patient was pacer dependent. Blood cultures showed negative results, but after 5 days, B. cepacia was grown from the pocket pus, which was sensitive to Cotrimoxazole and Ceftazidime. Vancomycin was shifted to Cotrimoxazole. After 7 days of infected pulse generator and lead removal and 3 days on Cotrimoxazole, a pacemaker insertion on the contralateral side was done. Decrease in swelling and tenderness of the infected site on follow up was noted.
Conclusion: The patient in the case had underlying diabetes mellitus, which could have been a contributing risk factor for the CIED infection. The infection may have also been caused by an outbreak of nosocomial infections related to B. cepacia contamination of various solutions and disinfectants. Treatment of the infection in the patient involved a combination of appropriate antibiotics and complete device extraction.
CS‐377‐CIED
Utility of non‐conventional fluoroscopic images to implant a transvenous permanent pacemaker in patients with situs solitus dextrocardia and CCTGA
Deebaj Nadeem; Maqsood Alam; Faisal Qadir; Muhammad Mohsin
National Institute of Cardiovascular Diseases, Karachi, Pakistan
Case: 52 years lady presented with fever and dyspnea for 1 week. ECG showed sinus rhythm, complete atrioventricular dissociation, junctional escape 40 bpm, atrial rate 100 bpm and prominent R wave from V1 to V6. CXR showed dextrocardia. Echocardiography confirmed situs solitus dextrocardia and congenitally corrected transposition of great arteries with no associated abnormality. Temporary pacemaker lead was placed due to symptoms. The left axillary vein was accessed twice. The ventricular lead was advanced through the superior vena cava using a straight stellate into the right atrium and later into the right ventricular outflow tract over a stellate with a distal curvature, later withdrawn to the right venous ventricle (morphologic LV) and advanced into the apical‐septum. Position was confirmed by right anterior oblique view; however, it appeared to be pointing away from the septum and towards the lateral wall. Intravenous contrast was rapidly injected, and cine films were acquired in the RAO views to delineate ventricular septum and lateral wall. Ventricular lead was readjusted in RAO view to apical‐septum area using a double curvature (Proximal larger and distal small curve). A second 7F introducer was advanced over the guide wire. Atrial lead was advanced into the right atrium and screwed in place in RA appendage. Both lead parameters were satisfactory. A dual chamber pulse generator connected and pocket closed. A post‐procedural 12‐lead ECG showed paced rhythm.
Conclusion: Permanent pacemaker was successfully implanted in a challenging anatomy using venous angiography and fluoroscopy without the need of expensive imaging modality.

CS‐385‐CIED
An uncommon cause for rescue conduction system pacing: Epicardial substrate for ventricular tachycardia
Emin Evren Ozcan; Oguzhan Ekrem Turan; Reşit Yiğit Yilancioglu
Dokuz Eylul University Heart Rhythm Management Centre, İzmir Balcova, Turkey
Background: Cardiac resynchronisation therapy (CRT) is a mainstay of treatment for medically refractory congestive heart failure (CHF). Although rare, the proarrhythmic effects of CRT necessitate alternative methods. Conduction system pacing (CSP) may be an alternative salvage method in failed CRT cases due to proarrhythmic effects.
Case: A 64‐year‐old man with ischaemic cardiomyopathy presented with dyspnoea and NHYA 2–3. He had a history of secondary prevention ventricular ICD implantation and prior ablation for ischaemic ventricular tachycardia (LV posterobasal). Due to the left bundle branch block with reduced EF and frequent inappropriate shocks, CRT‐D upgrade and AV node ablation were recommended.
Decision Making: Although the patient's coronary sinus venous anatomy was appropriate, sustained VT was induced each time by pacing from that region. Late potentials during sinus rhythm and induction of VTs with a long pace‐QRS interval during the threshold test revealed that the pacing site was above the epicardial substrate. LBBAP was performed because there was no alternative vein. Dual chamber‐ICD was used with a LBBAP lead in the atrial portion and a RV ICD lead in the RV portion with appropriate device settings. AV node ablation was performed 1 week later.
Conclusion: CRT may have proarrhythmic effects. LBBAP may serve as a rescue therapy option when appropriate localisation is challenging.

CS‐393‐CIED
Non invasive LV dP/dt echo optimized QRS duration in HOT‐CRT patient
Andrianus Oktovianto 1; Giky Karwiky2; Mohammad Iqbal2; Chaerul Achmad2
1Dr. M. Soewandhie General Hospital Surabaya, Surabaya, Indonesia; 2Dr. Hasan Sadikin Central General Hospital, Bandung, Indonesia
Background: Usefulness of echocardiogram parameter for prediction of the response of the patients to HOT‐CRT is underdebate. We present a case the effect of improvement in LVdP/dt on secondary mitral regurgitation in male receiving HOT‐CRT for severe HF.
Case: A 63 year old male was hospitalized for intractable HF NYHA FC III. The ECG showed LBBB with QRSd of 185 ms. He had reduced LVEF of 24%, dyskinetic base anteroseptal with moderate MR. Laboratory tests revealed urea 170.9 mg/dL and creatinine 2.73 mg/dL. The patient underwent HOT‐CRT. The His‐RV delay was programmed to 40 ms. Acute responses measured by QRSd and LV dP/dt by echocardiography were recorded immediately after implantation. We compared the QRSd and dP/dt changes in BVP (with Q‐LV proximal 196 ms) only, HBP only and HOT‐CRT. Maximal QRS narrowing and increase in LV dP/dt was achieved by HOT‐CRT (120 ms and 1043 mmHg/s) compared to BVP (160 ms) or HBP only (140 ms and 693 mmHg/s) respectively. The patient had improvement in NYHA FC 1 and LVEF 28% also decrease in urea 34.7 mg/dL and creatinine 0.85 mg/dL within 3 days.
Decision‐making: The LV dP/dt as a surrogate of LV mechanical synchrony after HOT‐CRT implantation can be useful for prediction of the acute response of the patient to HOT‐CRT. There was linear correlation between QRSd and LVdP/dt.
Conclusion: The LV dP/dt by echocardiography provides a non invasive parameter to determine acute response of HOT‐CRT.
CS‐426‐CIED
Utilization of non‐peal‐away sheath for lead implantation in a case with multiple retained leads and strong adhesions
Ryo Nakada, Maki Ono, Akira Mizukami
Kameda Medical Center, Japan
Background: Implantation of leads to patients with multiple leads and strong adhesions can be challenging.
Case: The patient is a 73‐year‐old woman with one epicardial, and five transvenous leads. The epicardial lead was inserted in 1983 for sick sinus syndrome, two transvenous leads in 1988, two transvenous leads in 1993 for lead failure, and LV lead for CRT‐P upgrade in 2020 for cardiac dysfunction. She was hospitalized with acute pericarditis and pericardial effusion, with LV pacing failure due to increased threshold and worsening heart failure. Lead extraction was difficult due to strong adhesions, even for the LV lead, and lead implantation was performed. We punctured the left subclavian vein and inserted a guide wire. However, strong adhesion of the left subclavian vein was observed, and we were unable to insert a peel‐away introducer, even after dilation with non peal‐away Terumo sheath.
Decision‐making: As it was possible to insert the non peal‐away Terumo sheath, we excised the port and side tube of the sheath, and the tube‐like sheath was inserted with the dilator. We succeeded in inserting the lead into the sheath and peel‐away of the sheath was performed with a slitter.
Conclusion: We report that a rigid non‐peel away type sheath can be used for lead insertion in cases with strong adhesions.
CS‐431‐CIED
Subclavian venoplasty via left brachial vein access in a patient requiring device upgrade due to pacing induced cardiomyopathy
Faten Aqilah Aris; Rohith Stanislaus; Hisham Md Shahrom; Tommy Daindes; Azlan Hussin
National Heart Institute, Kuala Lumpur, Malaysia
Introduction: Pacing induced cardiomyopathy is a well known complication that tends to occur in patients who have a high pacing requirement in the right ventricle. Subclavian vein stenosis caused by venous access during initial procedure is also a well known complication. Patients may remain asymptomatic in‐spite of having stenosis as collateral circulation is established over time.
Case: A 70 year old lady with history complete heart block after Aortic Valve replacement in 2012. Following implant, she was well until recently, she was admitted for heart failure. Echocardiogram noted that her ejection fraction was reduced 43%. Retrospectively, we noted that she had 100% right ventricular pacing since 2012.
A diagnosis of pacing induced cardiomyopathy was made and she was counselled for a device upgrade to a Cardiac Resynchronization Therapy with Pacemaker (CRT‐P).
Prior to start of procedure, we performed a venogram which revealed total occlusion of the left subclavian artery. Left brachial vein punctured with venogram. Long CTO of left subclavian vein crossed with terumo (0.35) wire with glide cath support. We were unable to pass down 6.0 mm balloon. Catheter changed to trailblazer catheter for insertion of V18 wire. Sequential pre‐dilatation done with 3.0 mm then 6.0 mm balloon. Device upgrade was then done smoothly.
Decision Making: Brachial vein approach was chosen as the anatomical trajectory offers the guidewires with better support.
Conclusion: This case highlight the important of venogram prior to device upgrade as it allows the operator to plan the procedure prior to pocket creation thus reduced risk of infection.
CS‐438‐CIED
Cardiac resynchronization therapy from an iliac approach in a patient without superior access
Lei Xu; Yangang Su; Shengmei Qin; Junbo Ge
Shanghai Institute of Cardiovascular Diseases, Department of Cardiology, Zhongshan Hospital, Fudan University, Shanghai, China
Background: Cardiac resynchronization therapy has been shown to benefit patients with heart failure and left bundle branch block. When the superior venous access is not feasible, cardiac resynchronization therapy implantation is challenging.
Case: A 50‐year‐old man with a history of dilated cardiomyopathy and complete left bundle branch block was referred to our hospital for cardiac resynchronization therapy. The angiography showed that both left and right brachiocephalic veins were occluded. Cardiac resynchronization therapy was finally implanted via the iliac vein. Follow‐up echocardiography showed improved cardiac function and the pacing system was working properly.
Decision‐making: CRT can be implanted via the iliac vein approach when the superior venous access is not feasible. Compared with the femoral vein, the advantage of iliac access is that the leads can be unaffected by lower limb activities.
Conclusion: The iliac vein access is feasible for CRT implantation with good stability, which can be an alternative way to avoid unnecessary risk associated with thoracotomy and epicardial lead placement.
CS‐449‐CIED
“Top down” approach to Aveir leadless pacemaker implant in a small right atrium
Wood Hay Ian Ling; Jeffrey Chun Yin Lee; Katherine Y. Y. Fan
Grantham Hospital, Hong Kong SAR
A 84‐year old woman underwent Aveir VR Leadless Pacemaker for symptomatic slow AFib. The procedure was performed under local anaesthesia with right femoral vein access. Delivery catheter could not be deflected in the RA. Right atrium (RA) angiography showed a posterior pointing IVC and a small RA (RA ESA 10 cm2). A 6‐Fr MPA catheter was brought down via the right jugular vein by the second operator. A super‐stiff wire was left within the catheter to enhance torqueability. It was intubated into the Aveir delivery catheter in mid RA. The protective sleeve was pushed forward and put into the lock position to minimize direct interaction with the pacemaker. Coordinated manipulation involving forward‐push of the MPA catheter, pull‐back of the Aveir delivery catheter together with the application of the deflection lever successfully delivered and subsequent implant of the Aveir pacemaker onto the RV septum.

CS‐476‐CIED
A case report: Loss of synchrony after AV nodal ablation in previous successful HOT CRT patient with chronic atrial fibrillation
Ayundari Tahyra; Karwiky Giky; Mohammad Iqbal; Chaerul Achmad
Universitas Padjajaran, Bandung, Indonesia
Case Presentation: Cardiac resynchronization therapy (CRT) is indicated in advanced heart failure patient with LBBB ECG pattern to improve electrical resynchronization. Cardiomyopathy is a common cause of atrial fibrillation (AF). CRT is preferred to maintenance ventricular synchrony in patient with permanent AF, HFrEF undergoing AV Nodal ablation (AVNA). We present a case report of a 50‐year‐old man who underwent AV nodal ablation due to chronic AF with history of HOT‐CRT implantation. We highlight the complications that might be encountered.
A 50 year‐old man with a known history of HOT‐CRT implantation due to mixed typed cardiomyopathy with LBBB ECG pattern was evaluated by echocardiography and showed improved ventricle synchrony after implantation. During follow up biventricular pacing was shown only 80% despite maximal dose of rate drugs so we decided to undergoing AVNA. After multiple attempts, TAVB was not seen, noted ECG become RBBB. Ablation failed to ablate AV nodal. Procedure decided to stopped, when evaluated by echocardiography showed dyssynchrony. AVNA has been advocated to ensure complete synchronized biventricular capture. The electrical coupling of ventricle was altered after AVN ablation and caused electrical dyssynchrony. RBBB in this patient could be explained by the His bundle longitudinal dissociation after radiofrequency injury. Thus, this patient was then scheduled to undergo lead revision for HOT/LOT‐CRT implantation in the attempt improve electrical synchrony.
Conclusion: AVN ablation for patient with persistent AF despite medical therapy with history of HOT‐CRT implantation was quite challenging. During ablation procedure there are complication that we must be aware of.
Keywords: AV nodal ablation, electrical dyssynchrony, HOT‐CRT.
CS‐478‐CIED
Safety of left bundle branch area pacing lead extraction due to Pseudomonas infection: A case report
Margareta Ginanti; Giky Karwiky; Chaerul Achmad; Mohammad Iqbal
Universitas Padjajaran, Bandung, Indonesia
Background: The increasing number of CIED over last two decades led to higher incidence of CIED‐related complications, notably infections. LBBAP lead extraction has potential safety issue due to deep lead implantation in the septum. Treatment for CIED‐related infections comprised of lengthy antibiotic use and complete device removal.
Case: A 64‐year‐old female patient presented to the emergency department following a syncopal episode. The patient's vital signs were within normal limits; however, her ECG showed TAVB with ventricular escape rhythm and an inferior wall OMI. The patient was subsequently treated with LBAPP. The patient returned 2 weeks later, complaining of pain in the site of implantation with a yellowish discharge. Pseudomonas aeruginosa was identified in the pus culture.
Decision‐making: The patient underwent LBBAP lead extraction and re‐implantation, wound care, and antibiotic therapy. The patient tolerated the procedure well, without complications. Previous analysis of infected leads demonstrated that bacteria coated the leads and formed a “biofilm”, making the infection resistant to antibiotics. Hence, leaving the device in place increases risk of recurrent infection, device‐related endocarditis, and mortality, thus highlighting the importance of device extraction. The primary challenge associated with lead extraction is tissue binding sites along the lead's path and the interface between the lead tip and endocardium, which may cause rupture when the lead is pulled. Nonetheless, this case report showed that the removal of LBBAP was safe, possibly when performed within 1–2 months of implantation.
Conclusion: LBBAP extraction and re‐implantation is safe and effective in patient presenting with Pseudomonas infected lead.
CS‐502‐CIED
Dual chamber pacemaker implantation in a patient with persistent left superior vena cava with left‐sided inferior vena cava and absent right superior vena cava
Chengming Ma; Jingyi Bai; Xiaohong Yu; Siting Feng
First Affiliated Hospital of Dalian Medical University, Dalian, China
Background: Persistent Left Superior Vena Cava (PLSVC) is a rare congenital vascular anomaly that may occur with complex anatomical deformities.
Case: A 52‐year‐old female presented with recurrent palpitation and amaurosis for 3 years and suffered syncope due to sinus arrest. She received a metal mitral valve replacement. The computed tomography showed a PLSVC with the absence of the right superior vena cava (RSVC) and a left‐sided IVC with hemiazygos continuation drained to the PLSVC. The hepatic veins independently drained into the right atrium.
Decision‐making: Due to the sinus node dysfunction with accompanying symptoms, permanent pacing was recommended. During the implantation, venography showed PLSVC draining into the coronary sinus, and the right brachiocephalic vein continued to the left jugular vein, ultimately draining into the CS. With the above vascular anatomical variations, ventricular and atrial electrodes were eventually advanced through the PLSVC. After ventricular lead entering the right atrium formed a loop, facilitating the passage through the tricuspid orifice. Then a specialized J‐shaped stylet was used to gain a satisfactory site for fixation. The atrial active lead was fixed to the right atrial appendage. The pacing threshold, sensing threshold, and impedance of both leads were optimal. X‐ray fluoroscopy showed stabilization of the pacemaker electrode position. The symptoms improved significantly, and amaurosis disappeared during follow‐up. Stable and favorable pacing and sensing parameters were confirmed during device follow‐up.
Conclusion: PLSVC during pacemaker implantation is not uncommon, the operator should be familiar with its anatomic variants and with the technical alternatives to overcome difficulties.
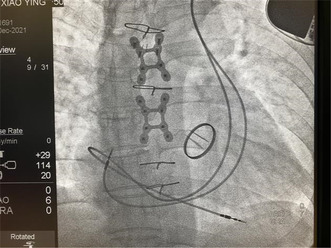
CS‐512‐CIED
Challenges in managing complete heart block as a manifestation of intracardiac mass in gravida young woman: A case report
Ina Marita; Giky Karwiky; Mohammad Iqbal; Chaerul Achmad
Department of Cardiology and Vascular Medicine, Universitas Padjadjaran, Dr. Hasan Sadikin General Hospital, Bandung, Indonesia
Background: While the management may be straightforward in patients with TAVB and cardiac mass; this might not be the case in pregnant patients. We have to weighted the risk and benefit of performing fluoroscopy‐based procedure due to the harmful effect of radiation to fetus. Delaying PPM implantation should be considered to minimize the risk. We presented a case in which we decided to perform left bundle pacing (LBP) in pregnant woman using minimal fluoroscopy technique after delaying the procedure with acceptable risk to the fetus.
Case Presentation and Decision Making: A 26‐year‐old G2P1A0 female at 5–6 weeks of gestation presented with recurrent syncope and near syncope since 2 months ago. ECG revealed Total AV Block with junctional escape rhythm (HR 40 beat/min, QRS duration 0.11 ms). Echocardiography showed hypoechoic mass at interventricular septum. Cardiac MRI examination showed mass (46 × 26 mm) with heterogenous enhancement at basal region of interventricular septum suggestive of lipoma causing RV compression. The patient underwent LBP (DDDR mode) at 20 weeks of gestation with minimal fluoroscopy time (6 min). ECG post‐procedure showed narrow QRS complex (0.10 ms). There was no incidence of syncope on follow‐up.
Conclusion: Management in pregnant TAVB patients should also consider the wellbeing of the fetus, thus it might be important to delay PPM implantation after considering the risk and benefit. Left bundle pacing should be prioritized in infrahisian block.
Keywords: intracardiac mass, left bundle pacing, total AV block, pregnancy, young patient.

CS‐546‐CIED
Permanent pacemaker implantation through persistent left superior vena cava
Abdul Mueed; Reema Qayoom; Ifrah Uroos; Ghulam Kubra
National Institute of Cardiovascular Diseases, Karachi, Pakistan
The left superior vena cava is a persistent embryo‐genetic variant, occurring in 0.3%–0.5% of individuals in which the venous blood of the upper half of the body is drained through a left vena cava into the coronary sinus and/or through the atrio‐ventricular groove in the right atrium. We present a case of incidental finding of persistent left superior vena cava (PLSVC) in a 70 years female who was being implanted with a single chamber pacemaker for complete heart block.
Case Presentation: 70 year old female patient known to have hypertension for last 15 year compliant to medication came to emergency room with complains of shortness of breath and dizziness for last 15 days. Electrocardiogram (ECG) showed complete heart block for which she was placed on temporary intravenous pacing through right subclavian venous approach. Work up was done for which no reversible cause was noted. Impression of senile deterioration of conducting tissue was made. Single chamber pacemaker implantation was planned. Lead was placed through the left subclavian vein. Access was performed via direct puncture; the guide‐wire was advanced through left subclavian vein to persistent left superior vena cava and coronary sinus to right atrium. This was incidental finding which was confirmed during the procedure through venogram from left upper limb. Lead (Medtronic CapSureFix MRI active fixation 58 cm lead, Minneapolis, USA) was actively fixed in right ventricle apex with alpha loop configuration.
CS‐571‐CIED
To open or not to open: Implanter's dilemma
Simon Salim1; Muhammad Yamin1; Rubiana Sukardi2; Angga Pramudita1; Catur Wulanningsari2; Rohmad Widiyanto2
1Division of Cardiology, Department of Internal Medicine, Faculty of Medicine, Universitas Indonesia, Jakarta, Indonesia; 2Integrated Cardiac Centre ‐ Dr. Cipto Mangunkusumo National General Hospital, Jakarta, Indonesia
Background: This case study explores the dilemma faced by implanters when managing infections in implantable cardiac devices (ICDs). Specifically, it focuses on a patient undergoing hemodialysis who experienced an early infection of a dual chamber ICD.
Case Presentation: A 67‐year‐old man with a history of cardiac resuscitation had a dual chamber ICD implanted. Three days later, he reported pain and a slight hematoma near the implantation site. Despite a conservative treatment plan and negative blood culture results, the patient returned 3 weeks later with increased swelling and signs of pocket infection. Consequently, the ICD was removed.
Decision‐making: Current guidelines recommend a conservative approach and close monitoring for CIED‐related infections after a period of Staphylococcus antibiotics and negative blood cultures. However, the WRAP‐IT study indicated that acute implant site hematoma had an 11‐fold increased risk of developing a serious infection. In this case, although a prolonged course of antibiotics was administered and the patient was discharged, the infection still occurred.
Conclusion: Delayed extraction of the CIED, defined as removal after the seventh hospital day, was associated with increased 1‐year mortality in patients with bacteremia or local pocket infection. Given the patient's high‐risk factors, including hemodialysis and central vein access, a more aggressive approach might have been beneficial. Implanters must carefully weigh the risks and benefits to make an informed decision regarding the management of CIED infections in individual patients.
CS‐573‐CIED
Simultaneous left bundle branch area pacing and implantable cardioverter defibrillator lead implantation: A case report
Muhammad Yamin 1; Simon Salim1; Rubiana Sukardi2; Angga Pramudita1; Catur Wulanningsari2; Rohmad Widiyanto2
1Division of Cardiology, Department of Internal Medicine, Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia; 2Integrated Cardiac Centre ‐ Dr. Cipto Mangunkusumo National General Hospital, Jakarta, Indonesia
Background: A case of LBB Area Pacing and ICD as an alternative for Cardiac Resynchronization Therapy with a Defibrillator (CRTD) in patients with heart failure.
Case Presentation: The EF of a 49‐year‐old man with heart failure reduced EF and LBBB had his symptoms worsened and EF gradually decreased from 34% to 24%. CS was difficult to cannulate during CRTD implantation, and the branches were unsuitable.
Decision‐making: Due to technical limitations, we chose to install the ICD lead first in the RV apex and the CRTD generator with a cap in the LV port. The following week, the patient underwent a second procedure to implant LBB Area Pacing (LBBaP) as an alternative for CRT using 3830 leads and a C304‐His catheter that was manually recurved for LBBaP. The LBBaP lead was then inserted into the device's LV port. LV‐only pacing was programmed into the device to facilitate LBBaP. Three months after the procedure, the patient's complaints improved with HFrEF NYHA FC I, despite the fact that his EF remains at 25%.
Conclusion: LBBaP is a good alternative for CRT and can be combined with ICD.
CS‐575‐CIED
Stress‐induced cardiomyopathy after uncomplicated permanent pacemaker implantation
Jiyeon Seo
Hongik Hospital, Seoul, South Korea
Introduction: Stress‐induced cardiomyopathy (SCMP) after permanent pacemaker (PPM) implantation is rare. We report an additional case which was initially misdiagnosed as another disease due to atypical symptoms.
Case Presentation: A 79‐year‐old woman with dizziness and dyspnea for 1 month visited Cardiology Department. She had a history of hypertension, dyslipidemia, diabetes‐mellitus and stage IV chronic kidney disease. We confirmed complete atrioventricular block. Left ventricular ejection fraction (LVEF) was normal. PPM implantation was successfully performed without complications. The next day she felt very well without symptoms. On the second day, she suddenly developed a fever and complained severe left neck pain. She had cough, sputum and general weakness without chest pain. C‐reactive protein level increased and blood pressure was decreased. We started antibiotics considering respiratory infection. We also checked implantation site, but there were no signs of infection. Echocardiography showed decreased LVEF (30%), akinesia of apical and medium segments of LV wall with preserved kinetics of basal segments (Figure 1). There was no significant stenosis at coronary angiography. We confirmed SCMP and prescribed sacubitril‐valsartan, bisoprolol and furosemide. After 10 days, she was discharged with improved symptoms.
Conclusion: Our case emphasizes that even successful implantation of PPM without complications can be a potential risk of SCMP. In the absence of typical cardiac symptoms after PPM implantation, a poor general condition may also be considered as a sign of SCMP. Therefore, it is necessary to monitor the patient for few days after PPM implantation.

CS‐586‐CIED
Case report: Undersensing helps in the diagnosis of the pacemaker lead perforation in the free wall of the right ventricular
Duy Linh Nguyen 1; Dinh Phong Phan1; Tuan Viet Nguyen2
1Vietnam National Heart Institute, Ha Noi, Vietnam; 2Thanh Hoa Province General Hospital, Thanh Hoa, Vietnam
A 66‐year‐old male patient was implanted with a dual‐chamber DDDR‐mode pacemaker due to symptomatic sinus node dysfunction (SND). After 2 months, the patient presented with persistent dull chest pain, was ruled out of the usual causes by coronary angiography, gastrointestinal endoscopy, and a chest CT scan, and did not respond to analgesics. On the ECG, the right ventricular lead showed undersensing and overpacing. This symptom raises the diagnosis of a right ventricular free wall rupture complication. An MSCT scan confirmed the patient's diagnosis. The results showed the lead tip penetrating the right ventricular free wall. Ultimately, the right ventricular lead was safely withdrawn with the help of echocardiography. This lead was implanted in the right ventricular outflow tract with the characteristic thick muscle to avoid recurrent complications.
CS‐598‐CIED
Hyperkalemia caused QRS double counting and inappropriate shocks—case report of a patient with hemodialysis and ICD implantation
Rong He; Yuanwei Liu; Fei She; Jing Yang; Ping Zhang
Beijing Tsinghua Changgung Hospital, School of Clinical Medicine, Tsinghua University, China
Background: Oversensing and inappropriate implantable cardioverter‐defibrillator (ICD) shocks remain common challenges. Taller T wave peaks and QRS wave widening in hyperkalemia can induce ICD oversensing and inappropriate shocks.
Case: A 54‐year‐old man with ischemic cardiomyopathy, reduced left ventricular ejection fraction (28%), and chronic kidney disease stage V, was referred for an ICD implantation as a primary prevention for sudden cardiac death. A dual chamber ICD (Abbott, Fortify DR CD2231‐40) was implanted in July 2017. Ventricular tachycardia (VT)‐1, VT‐2, and ventricular fibrillation (VF) zones was set at rate cutoffs of 160, 181, and 214 bpm, respectively. Ten months later, the patient experienced nine ICD shocks during sexual activity.
Decision‐making: Interrogation of the ICD revealed significantly wide and fractionated endocardial ventricular electrogram, which doubled the QRS counting, resulting in a slow VT (about 150 bpm) detected in the VF zone. Serum potassium level after hemodialysis was still 7.0 mmol/L. We prolonged ICD sensing refractory periods from 44 to 80 ms to avoid the QRS double counting immediately. Furthermore, the hemodialysis protocol was enhanced to avoid hyperkalemia induced inappropriate ICD shock. During the follow‐up, the serum potassium level was stable. No QRS double counting, inappropriate ICD shocks, and VT/VF episodes were reported till the date of the report completion.
Conclusion: Proper adjustment of sense parameters may be an immediate reasonable solution in hyperkalemia‐associated ICD oversensing and inappropriate shocks. Therefore, rapid determinating the cause of hyperkalemia and maintaining stable serum potassium levels are critical for the long‐term cardiac management in these patients.

CS‐614‐CIED
Pacemaker implantation in a patient with persistent left superior vena cava (PLSVC)
Jian Hao Sim; Gurudevan Mahadevan; Richard Chay Shien Long; Jin Kiang Cheng; Kim Fong Ng
Hospital Sultanah Aminah; Johor Bahru, Malaysia
Background: Persistent left superior vena cava (PLSVC) is a rare congenital vascular malformation of the thoracic venous return, whereby the left anterior cardinal vein failed to regress.
Case: Sixty‐year old Indian lady, with hypertension and Type II Diabetes Mellitus, presented with symptomatic complete heart block, necessitating a temporary transvenous pacemaker insertion via the right femoral vein. During permanent pacemaker implantation via the left cephalic vein, we had difficulty in advancing the guidewire through the midline to the intended location in the right ventricle. Careful analysis and venography demonstrated that our patient has PLSVC. With gentle manoeuvres, permanent pacemaker leads were placed at the correct anatomical locations successfully.
Decision‐making: Cephalic vein cut down provides a high rate of success with reduced risk of complications. We employed venography, which proved useful in confirming PLSVC during cardiovascular interventional procedures.
Conclusion: PLSVC has significant implications and needs to be considered during interventional procedures.

CS‐620‐CIED
Shall we reposition the atrial lead?
Sze Man Yuen; Ho Ling Tsoi; Tin Lam Lip; Wei Sze Eleanor Lee; Kwok Hing Yiu
North District Hospital, Hong Kong, Hong Kong SAR
A 70‐year‐old lady was admitted for recurrent syncope. Her past medical history included hypertension and paroxysmal atrial fibrillation. Electrocardiogram showed 6 s of sinus pause.
The dual‐chamber pacemaker was implanted. Immediate post‐operative atrial lead threshold was 0.5 V@0.4 ms. Continuous cardiac monitoring revealed atrial noncapture even though the programmed amplitude and pulse width was 3.5 V@0.4 ms. Next day interrogation of the device showed atrial threshold was 5 V@0.4 ms at AAI 60 bpm while it improved to 0.5 V@0.4 ms at AAI 90 bpm.
The pacemaker was programmed to DDD 80 bpm to maintain atrioventricular synchronisation. Four weeks later, the atrial pacing threshold improved to 0.7 V@0.4 ms at 60 bpm.
Acute rise in atrial capture threshold might occur particularly in female patients with sick sinus syndrome. Identification of this phenomenon may avoid unnecessary reintervention.
CS‐621‐CIED
Fluoroless emergency externalized temporary pacemaker insertion in pregnant patient with complete heart block
Mark Adorada; Jemelee Hernandez‐Albano
Philippine Heart Center, Philippines
Background: Minimizing radiation exposure among pregnant patients presenting with symptomatic atrioventricular block needing emergent pacemaker insertion is of paramount importance for safety health measures.
Case: A 30‐year old female on her 26 weeks age of gestation with no other comorbidity, presented with recurrent loss of consciousness prompting emergency consult. Baseline 12‐L ECG showed sinus rhythm, complete atrioventricular block with episodes of bradycardia‐induced ventricular tachycardia on telemetry monitoring. An emergency externalized temporary pacemaker insertion was performed and the procedure concluded without any untoward complication.
Decision‐making: Following the clinical recommendation for managing patients with bradycardia and cardiac conduction delay, temporary pacing is used to acutely treat bradycardia causing hemodynamically significant instability presenting with life‐threatening arrhythmias. Vascular access was made using the right internal jugular vein under the guidance of portable ultrasound. In contrast to conventional temporary transvenous pacing using the femoral vein, we avoid exposing the abdominal area that needs fluoroscopy as the pacing wire being advanced into the heart. Transthoracic echocardiography was utilized during deployment of the pacemaker lead. A very short single shot of fluoroscopy of less than 1 s corresponding to 0.82 mGy was only utilized at the end of the procedure for final checking of lead placement.
Conclusion: Performing an emergency externalized temporary pacing to pregnant women with symptomatic bradycardia can be done safely and considered life‐saving.
CS‐623‐CIED
Paradoxical worsening of heart failure post TAVI managed with apical pacing
Preetam Krishnamurthy; Muralidharan Thoddi Ramamurthy; Nagendra Boopathy Senguttvan; Akshay Prashanth; Divya Sridhar; Vinodkumar Balakrishnan
Sri Ramachandra Institute for Higher Education and Research, Chennai, India
Background: Left ventricular outflow tract obstruction and first‐degree AV block can worsen heart failure post TAVI (Trans‐Aortic Valve Implantation) and can be effectively treated with pacemaker.
Case: 78‐year‐old female was diagnosed with symptomatic severe aortic stenosis and moderate degenerative calcific mitral stenosis. Post procedure, patient developed first degree atrio‐ventricular block with left bundle branch block. Patient developed worsening dyspnoea secondary to significant left ventricular outlet obstruction (LVOTO) post valve implantation and elevated mitral valve gradients (Mean Mitral Diastolic Gradient—Baseline 5 mmHg, Post TAVI—16 mmHg). Holter done showed AV Wenckebach at heart rate 100/min and EP study showed HV 63 ms. In view of worsening AV block and Mitral Doppler showing significant AV fusion, pacemaker was implanted. The ventricular lead was screwed in apical septum. Post procedure, after optimizing the AV interval and maintaining complete paced rhythm, the LVOTO reduced and mitral gradients reduced to 5 mmHg. Patient symptomatically improved post pacemaker implantation.
Decision‐making: First degree AV block can cause impaired diastolic filling and worsening heart failure post valve implantation. Additionally, in our patient post valve implantation, patient developed LVOTO. By pacing the patient from apical septum and optimizing the AV interval, LVOTO was reduced, and Mitral Diastolic Gradients improved. Pacing also allowed usage of beta blockade to reduce the LVOTO further.
Conclusion: Paradoxical worsening of heart failure post TAVI can be attributed to the impaired diastolic filling secondary to AV block and dynamic LVOTO. Both the conditions can be effectively treated by apical pacing.
CS‐647‐CIED
A case report on atrial single‐chamber pacing + Micra AV implantation
Jianhong Tao; Yi Jia Tang
Sichuan Provincial People's Hospital, Chengdu, China
Background: The use of transvenous pace‐leads is associated with the risk of tricuspid valve dysfunction, mainly due to injury of the tricuspid valve during implantation or operation, including perforation, tear, avulsion, and rupture of the papillary muscle or chordae tendinae. The use of transvalved electrodes should be avoided in patients with severe tricuspid regurgitation.
Case Summary: A 69‐year‐old female with a history of exertional dyspnea and peripheral edema for 4 years, and a history of syncope for 9 months was studied. The cause of syncope was considered to be Sick Sinus Syndrome. Echocardiography suggested tricuspid valve downward displacement with severe insufficiency and atrial septal defect. The patient was considered a candidate for surgical intervention. To avoid aggravating tricuspid insufficiency by pacing lead through the tricuspid valve and hindering subsequent surgical treatment of tricuspid valve disease, atrial pacing with an AAI lead and Micra atrioventricular (AV) was chosen for maintaining atrioventricular synchrony after multi‐disciplinary discussion.
Conclusion: This is the first case of new implantation of single‐chamber atrial pacing + leadless ventricular pacing with Micra AV for tricuspid valve displacement malformation and severe tricuspid regurgitation.
CS‐661‐CIED
Permanent endocardial pacing stabilized the heart rhythm and facilitated physical growth in a 4.0 kg infant with high‐degree atrioventricular block
Juan Huang 1; Fen Li2; Wei Ji2; Xiao Feng Guo1
1Fujian Children's Hospital, Fuzhou/Jin‐An, China; 2Shanghai Children's Medical Center, Shanghai/Pudong New Area, China
Background: Pacemaker implantation is the standard treatment for symptomatic atrioventricular block (AVB) in children. Permanent endocardial pacing in low birthweight infants has been controversial.
Case: We present a case of a 2.8 kg infant diagnosed with high‐degree AVB, which showed a progressive trend, the average ventricular rate was 50 beats/min, accompanied by left ventricular enlargement and signs of inadequate systemic perfusion. We performed temporary pacemaker implantation, followed by permanent endocardial pacemaker implantation when the child's weight increased to 4.0 kg. A 5.6F electrode was inserted into the right ventricular septum, with the pulse generator embedded under the pectoralis major. The pacing mode was set to VVI, with a pacing rate of 90 beats/min.
Decision‐making: We took a risk and attempted permanent endocardial pacemaker implantation due to the lack of epicardial electrodes and the unstable circulation of the child. However, we must consider the high risks of complications associated with low birth weight. It is necessary to conduct a thorough evaluation of the vascular conditions of the child before the operation and use intraoperative transesophageal echocardiography to monitor the valves and cardiac function during operation. Six‐month follow‐up showed good pocket tissue healing, stable cardiac rhythm, and weight gain of up to 8.0 kg.
Conclusion: Permanent endocardial pacemaker implantation appears feasible in 4 kg infants, aiming to relieve symptoms and promote early growth. Nonetheless, caution is required given the risks associated with low birth weight, and individualized, precise treatment is essential to minimize complications.
CS‐662‐CIED
Ventricular premature complex worsened cardiomyopathy in a patient with rheumatoid arthritis ‐ the unusual suspect
Preetam Krishnamurthy1; Muralidharan Thoddi Ramamurthy 1; Calambur Narasimhan2; Vinodkumar Balakrishnan1; Divya Shridhar1; Muthiah Subramanian2
1Sri Ramachandra Institute for Higher Education and Research, Chennai, India; 2AIG Hospital, Gachibowli, Hyderabad, India
Background: Rheumatoid arthritis related inflammatory cardiomyopathy is uncommon. Early treatment of the disease can reverse the cardiomyopathy.
Case: 58‐year‐old female, known case of rheumatoid arthritis, with small joint involvement was on methotrexate therapy. She presented with complaints of palpitations with NYHA class III dyspnea. On evaluation was found to have severe left ventricular dysfunction (EF 25%) with significant ventricular premature complex of multiple morphologies (40% burden) with baseline first degree AV block (300 ms), narrow QRS which precluded initiation of beta blockers. Cardiac FDG‐PET scan done showed significant uptake in the lateral wall of the left ventricle suggesting inflammatory myocarditis. Coronary evaluation was normal. Since patient had pacing requirement with severe LV dysfunction, CRT‐D device was implanted. Later, high dose steroid therapy (methylprednisolone 15 mg/kg) was initiated. At 2 months follow up, patient LV function improved to 45% and patient symptomatically improved with significant reduction in VPC burden.
Decision Making: Patients presenting with VPC of multiple morphology should be evaluated for inflammatory pathology. In view of significant first‐degree AV block which precluded beta blockade and also worsened diastolic filling, pacing was required with defibrillator. Hence CRT‐D device was implanted. The steroid therapy had a dual role—to improve the left ventricular function and to suppress the VPC burden which in turn improved the LV function by improved biventricular pacing.
Conclusion: Though the most common cause of cardiomyopathy in rheumatoid arthritis is ischemic, inflammatory pathology should be evaluated and treated as a reversible cause.
CS‐668‐CIED
Rapid degradation of left ventricular function after permanent right ventricular pacing in patients with high‐grade atrioventricular block
Dion Setiawan; Setyasih Anjarwani; Ardian Rizal; Indra Prasetya
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Brawijaya, Malang, Indonesia
Background: Permanent right ventricular pacing (RVP) is a standard treatment for high‐grade atrioventricular (AV) block. Chronic and high‐burden RVP can cause pacing‐induced cardiomyopathy (PICM). We describe a case of a PICM with a significant decrease in LV systolic function in less than 2 years after RVP. Conduction system pacing (CSP) was scheduled on the patient.
Case: A 56‐year‐old Asian female with a history of RVP due to a high degree AV block came with acute decompensated heart failure. On arrival, she looked restless and had difficulty breathing. Physical examination showed bilateral leg edema, and rhonchi were heard bilaterally. Laboratory tests revealed leukositosis of 33.760/mm3, and increased NT pro BNP level of 9.233 pg/L. An electrocardiogram (ECG) showed atrial flutter with ventricular pacing rhythm 60 bpm RVOT origin. Chest x‐ray revealed pulmonary edema, infiltrates, and cardiomegaly with a single lead PPM seen at RVOT. Evaluation of her PPM showed high burden RVP 99.5%. Echocardiogram showed all chamber dilatation, global hypokinetic, and reduced ejection fraction (EF) from 62% to 26% in less than 2 years.
Decision‐making: Coronary angiography was performed, which showed non‐significant coronary artery stenosis. His‐Bundle pacing (HBP) was scheduled to reduced LV dyssynchrony and improve LV function.
Conclusion: Single‐chambered pacemakers create ventricular dyssynchrony, which can cause structural and molecular changes leading to cardiomyopathy. With early intervention, these changes can be reversible. Therefore, timely check‐ups and awareness are necessary for patients on RVP.
CS‐672‐CIED
Efficacy of wearable defibrillator in patients with Fabry disease prior to implantable cardioverter defibrillator implantation
Takuya Matsumoto; Kenichi Tokutake; Ui Takato; Yoshito Yamazaki; Ryutaro Sakurai; Satoko Shiomi; Hidenori Sato; Hirotsuna Oseto; Seigo Yamashita; Michifumi Tokuda; Storu Miyanaga; Yoshimura Michihiro; Teiichi Yamane
The Jikei University Hospital, Shinbashi, Japan
Background: Fabry disease can potentially lead to fatal ventricular arrhythmias; although immediate implantation of an implantable cardioverter‐defibrillator (ICD) may not always be feasible.
Case: A 47 years old man with Fabry disease experienced ventricular fibrillation during enzyme replacement therapy for Fabry disease. Cardiopulmonary resuscitation and external defibrillation were performed, resulting in the restoration of spontaneous circulation. Although ICD implantation was strongly recommended, the patient initially declined to undergo the procedure.
Decision‐making: The patient was discharged with the use of a wearable cardioverter‐defibrillator (LifeVest®). The patient experienced loss of consciousness while outside and received a shock from the wearable device (Figure). Subsequently, the patient consented to the ICD implantation, which was successfully performed.
Conclusion: We present this case to emphasize the efficacy of using a wearable cardioverter‐defibrillator to terminate ventricular fibrillation in patients with Fabry disease prior to ICD implantation.

CS‐674‐CIED
Cardiac resynchronization therapy—Defibrillator implantation in a 63‐year old patient with persistent left superior vena cava Schummer's type IIIb
Mark Adorada 1; Gladys Ruth David1; Eden Gabriel1
1Philippine Heart Center, Philippines
Background: The presence of persistent left superior vena cava (PLSVC) poses technical challenge when detected incidentally during cardiac resynchronization therapy‐defibrillator (CRT‐D) implantation.
Case: A 63‐year old female, diagnosed with symptomatic heart failure due to dilated cardiomyopathy, was advised to undergo CRT‐D implantation. Left‐sided venography showed PLSVC draining to the inferior vena cava. Right‐sided venography showed passage of dye to the right atrium. Due to anticipation of difficult access on the left side, we made use of the right subclavian vein for the placement of the right ventricular and right atrial electrodes positioned in the right ventricular apex and right atrial appendage respectively. The left ventricular lead was placed using epicardial approach via left thoracotomy.
Decision‐making: In PLSVC Schummer's Type IIIb, the right SVC is not connected to PLSVC. Access to the right heart was performed via the right subclavian vein that allowed easier route. In order to avoid untoward complication brought about by placement of left ventricular lead through the coronary sinus that may lead to lack of pacing or coronary sinus perforation and cardiac tamponade, epicardial approach was performed instead. Proper lead placement with good parameters, preventing dislodgement and minimizing radiation exposure were also considered.
Conclusion: CRT‐D implantation was successfully done in the presence of PLSVC with the left ventricular lead placed via epicardial approach.
CS‐675‐CIED
The role of LBB area pacing (LBBAP) in progressive cardiac conduction disease (PCCD) leading cardiomyopathy: A case series
Ria Ristianis; Giky Karwiky; Mohammad Iqbal; Chaerul Achmad
Universitas Padjadjaran, Bandung, Indonesia
Background: Progressive Cardiac Conduction Disease (PCCD) is associated with increased risk of heart failure and cardiovascular mortality that may develop bundle branch block leading progressive AV Block. LBB area pacing (LBBAP) may be appropriate for achieving resynchronization and improving EF as an approach managing those cases. This is a rare inherited cardiac disease and mainly associated with genetic disorder; however, we were unable to perform the genetic testing.
Case: Here we show two cases of PCCD:
First case, a 67‐year‐old female was referred for fatigue and suffered heart failure for 1 year. A 12‐lead ECG was performed a high‐degree AV block 2:1 with complete LBBB. Echocardiography showed LV enlargement, reduced LV systolic function (LVEF 34% BP) and regional wall motion abnormalities (RWMA).
Second case, a 71‐year‐old female was referred with ECG showed sinus bradycardia with an episode of AVB 2:1 and intermittent episodes of complete LBBB also PVC origin RVOT. Echocardiography revealed dilated LV, severely reduced LV systolic function (LVEF 29% BP) with RWMA. In these cases, we perform LBBAP providing synchronization.
Decision‐making: Genetic mutations associated with cardiomyopathy have been identified in familial PCCD. Prolonged presence of LBBB in PCCD causes dyssynchrony and reduces LV ejection fraction (LVEF). Placement of LBBAP in these patients may have a positive impact on improving QRS duration and LVEF recovery. QRS shortening is associated with better clinical outcomes in PCCD patients.
Conclusion: LBBAP is feasible and effective in treatment of PCCD patients. Determining the cause of PCCD through genetic testing can be challenging.
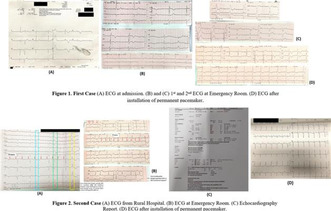
CS‐697‐CIED
Achieving left bundle branch pacing with standard non‐deflectable sheath via a persistent left superior vena cava
Jerome Reymatias; Jie Ying Lee; Toon Wei Lim; Wee Tiong Yeo; Swee‐Chong Seow; Kevin Ming Wei Leong
National University Heart Centre, Singapore
Background: A persistent left‐sided superior vena cava (PLSVC) can pose a technical challenge and barrier to left bundle branch pacing (LBBp). Techniques to overcome this anatomical challenge are desirable given the increasing use of LBBp over His and right ventricular pacing.
Case Presentation: A dual chamber pacemaker was implanted in a 65‐year‐old woman for symptomatic sinus node dysfunction with a PLSVC and a right‐sided breast mass. Non‐selective LBBp via a non‐stylet lead via a C315 and extended hook coronary sinus (CS) sheath (Medtronic) was achieved (Figure 1).
Decision Making: Possible future right‐sided radiotherapy influenced implant site. Equipment availability guided choice of equipment/vendor. The C315 sheath does not provide the correct shape to engage the septum orthogonally. The Medtronic CS extendable hook was utilized to provide the additional support and angulation needed.
Conclusion: We present an implant technique, not described previously, utilizing standard non‐deflectable sheaths via the PLSVC to achieve LBBp.

CS‐722‐CIED
Bradycardia‐dependent rise in atrial capture threshold after pacemaker implantation for a patient with sick sinus syndrome
Wai Lun Mak; Tsz Ho Chan; Lap Shing Chan; Shung Yee Wong; Chi Wing Wong
Pok Oi Hospital, Hong Kong SAR
A 69 year old woman was admitted to our hospital with intermittent lightheadedness for 2 weeks. Holter study showed sinus pauses of 3.6 s associated with symptoms. A dual‐chamber pacemaker with passive fixation lead at right atrial appendage was implanted. The initial atrial capture threshold was 1.0 V at 0.4 ms pulse width (measured at 80 bpm). The sensing and impedance values were both within normal range (2.9 mV and 501 ohm).
Patient reported recurrence of lightheadedness 1 week after discharge. Pacemaker interrogation revealed a marked rise in atrial capture threshold to 5.0 V at 1.5 ms at 70 bpm. Chest radiograph showed no apparent dislodgement of the atrial lead. Different threshold at different pacing rate was tested. We observed that the atrial lead threshold decreased with higher pacing rate. At 80 bpm, the threshold was 2.5 V at 1.0 ms. The pacemaker was programmed with base rate of 80 bpm.
The patient attended follow up again 1 month after implant. Her symptom was much improved. The atrial lead threshold dropped to 1.75 V at 0.4 ms at 70 bpm. At 75 bpm, threshold further dropped to 1.0 V at 0.4 ms. The base rate was adjusted to 75 bpm.
At 2 months, threshold returned to 1.5 V at 0.4 ms at 60 bpm and 1.0 V at 0.4 ms at 70 bpm. The base rate was further adjusted to 70 bpm.
In conclusion, bradycardia‐dependent rise in atrial capture threshold can occur transiently early after pacemaker implantation for sick sinus syndrome. It is important to be aware of this phenomenon to avoid unnecessary re‐intervention.
CS‐730‐CIED
Outcomes of Brugada syndrome patients in the Philippines who underwent ICD implantation
Paula Victoria Catherine Cheng; Giselle Gervacio
Philippine General Hospital, Manila, Philippines
Brugada syndrome is an inheritable channelopathy that can present with a coved‐type ST‐segment elevation on leads V1–V3. Patients can be asymptomatic or present with life‐threatening arrhythmias. This syndrome is particularly common in the Southeast Asian region, including the Philippines. In those who are at high risk for cardiac arrest or who have documented ventricular arrhythmias or survived cardiac arrest, implantable cardiac defibrillators are the only proven effective therapy to detect and treat these arrhythmias. In this case series, we present seven Brugada syndrome patients who have undergone implantation after experiencing either ventricular arrhythmias or have survived cardiac arrest. Among these patients, three presented with appropriate shocks for ventricular arrhythmias. Of these three patients, one patient had ventricular fibrillation storm and another presented with recorded supraventricular tachycardia for which he eventually underwent an EP study. Majority of the patients, however, did not have any events during their follow up period. While ICDs are proven to prevent sudden cardiac death from potentially lethal arrhythmias in Brugada syndrome patients, a large percentage of patients do not experience events after implantation. Further studies may be warranted to identify precipitating factors for these arrhythmias and factors which prevent them.
CS‐762‐CIED
Adolescent with sudden cardiac death high risks benefit from home automated external defibrillator: A case report
Yuanhao Jin; Ruohan Chen; Yan Dai; Keping Chen
State Key Laboratory of Cardiovascular Disease, National Center for Cardiovascular Diseases, Fuwai Hospital, Beijing, China
Background: Early identification and defibrillation are crucial for cardiac arrest. Home Automated external defibrillator (AED) are effective in the treatment of cardiac arrest.
Case: First admission: The patient is a 12‐year‐old male who was first admitted to the hospital on August 29, 2022. Three years ago, the patient experienced transient loss of consciousness while exercising. He had no previous record of heart diseases. His brother died suddenly at the age of 14. The electrocardiogram (ECG) suggested early repolarization phenomenon (Figure). Echocardiogram, coronary CT angiogram were normal on admission. ICD was recommended. The patient's guardians declined. They prepared AED at home. Three years later, the patient had a sudden twitching of the extremities while resting. The AED revealed ventricular fibrillation, and successfully defibrillated.
Decision Making: Considering that the patient was 12 years old and had no current need for pacing, a subcutaneous ICD was implanted.
The patient returned 2 weeks after being discharged due to repeated ICD shocks. The ECG showed atrial fibrillation and ventricular arrhythmia induced by premature ventricular beats falling in the T‐wave vulnerable phase. All episodes were associated with increased early repolarization after prolongation of the R–R interval. A bedside temporary right ventricle pacemaker was implanted. Pacing rate of 80 beats per minute successfully terminate the electrical storm. The patient received a dual‐chamber permanent pacemaker implantation. The patient returned to our clinic 6 month later without occurrence of ventricular arrhythmias.
Conclusion: SCD high risk people benefit from home AED.

CS‐771‐CIED
Potential for optimizing CRT with a novel, portable, wireless phonocardiogram
Nobunari Tomura 1; Keitaro Senoo2; Kohei Kawai1; Masahiro Makino1; Jun Munakata1; Satoshi Shimoo1; Hibiki Iwakoshi1; Tetsuro Nishimura1; Hirokazu Shiraishi1; Satoaki Matoba1
1Department of Cardiovascular Medicine, Graduate School of Medical Science, Kyoto Prefectural University of Medicine, Kyoto, Japan; 2Department of Cardiac Arrhythmia Research and Innovation, Graduate School of Medical Science, Kyoto Prefectural University of Medicine, Kyoto, Japan
Background: The splitting of the second heartbeat (S2) in the phonocardiogram correlates with interventricular dyssynchrony, but the test was burdensome. A novel, portable, wireless phonocardiogram was introduced to the market in Japan and we tested its use in CRT optimization.
Case: An 86‐year‐old man received CRT implantation for heart failure with reduced ejection fraction. Phonocardiogram was recorded at 4LSB in a supine position. We compared the relationship between cardiac output on echocardiogram and S2 interval on phonocardiogram among RV pacing and biventricular pacing from various polarities of LV lead. As a result, S2 interval was narrowest when left ventricular outflow tract velocity time integral (LVOT‐VTI) was greatest.
Decision‐making: The pacing polarity that maximized LVOT‐VTI on echocardiogram coincided with the polarity at which S2 interval on the phonocardiogram appeared minimal.
Conclusion: This novel phonocardiogram may simplify CRT optimization without the need for echocardiogram by providing a user‐friendly visualization of cardiac output.

CS‐813‐CIED
Use of ‘mother‐and‐child’ technique in conduction system pacing for cardiac sarcoidosis
Jonathan Caleb Quek 1; Chi Ming Kelvin Chua1; Thuan Tee Daniel Chong1,2; Kah Leng Ho1; Tien Siang Eric Lim1; Chi Keong Ching1; Hooi Khee Teo1
1National Heart Centre Singapore, Singapore; 2Sengkang General Hospital, Singapore
Background: Conduction system pacing is rapidly gaining ground as it can curtail the risk of pacing induced cardiomyopathy that is seen in RV pacing. This is advantageous in patients at‐risk of developing heart failure.
Case: A 60‐year‐old gentleman presented with multiple episodes of near syncope. He has a history of transthyretin cardiac amyloidosis (LVEF 48%) treated with Tafamidis. Electrocardiography showed complete heart block. He was counselled for a dual‐chamber pacemaker implantation with left bundle branch area pacing to prevent worsening heart failure.
Decision‐making: Initial attempts to deploy the Medtronic SelectSecure 3830 lead failed as the thickened septum made lead penetration difficult. Reattempted using a self‐modified Medtronic Extended Hook sheath using the ‘mother‐and‐child’ technique typically used in coronary angioplasty. The lead was advanced until RSR pattern arose on unipolar tip pacing. Contrast showed septum embedment of electrode.
Conclusion: The ‘mother‐and‐child’ technique may facilitate the successful deployment of the Medtronic SelectSecure lead.

CS‐828‐CIED
A challenging dual chamber pacemaker implantation in persistent left superior vena cava: When knowledge of anatomy and adequate implantation technique have an important role
Fandi Ahmad; Sunu Budhi Raharjo; Sebastian Andy Manurung; Chandara Rith; Dony Yugo Hermanto; Dicky Armein Hanafy; Yoga Yuniadi
Faculty of Medicine Universitas Indonesia—National Cardiovascular Center Harapan Kita, Jakarta, Indonesia
Background: Persistent left superior vena cava (PLSVC) is a rare congenital malformation and generally asymptomatic. It is usually discovered incidentally during a pacemaker implantation through the left axillary vein approach.
Case Illustration: We report a case of the incidental finding of PLSVC in a 57‐year old man with total AV block undergoing dual chamber pacemaker implantation. After achieving access through the left axillary vein, the guide wire repeatedly coursed on the left side of the mediastinum, rather than crossing the midline. We confirmed from cephalic vein access and the guidewire still could not be advanced into the normal expected course of SVC, raising suspicion of PLSVC. Then guide wire was advanced to PLSVC and coronary sinus to right atrium and finally reach into inferior vena cava. A ventricular lead was successfully passed and fixed into the RVOT area with alpha loop configuration and an atrial lead was then passed through and directly fixed into right atrial appendage. Both atrial and ventricular sensing and pacing parameters were excellent and post‐procedure fluoroscopy showed satisfactory lead positioning.
Conclusion: Pacemaker implantation in patients with PLSVC is technically challenging. Good knowledge of cardiac structure anatomy and adequate implantation technique are needed to achieve a good result in this such rare case.
Keywords: dual chamber pacemaker implantation, persistent left superior vena cava, total AV block.
CS‐840‐CIED
Excessive prolonged PR interval in a patient with worsening shortness of breath: A case report
Jin Jian Tang; Yan Juan Zhang; Ming‐Fang Li
Department of Cardiology, The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
Background: Patients with excessively prolonged PR interval may have impaired cardiac function.
Case: A 72‐year‐old man presented to the cardiology department with a history of worsening shortness of breath and chest tightness over the past 3 years. He had no history of smoking, hypertension, diabetes mellitus, or cardiovascular diseases. During his physical examination, his blood pressure was measured at 108/71 mmHg, and his heart rate was 68 bpm. The electrocardiogram (ECG) showed sinus rhythm with a prolonged PR interval of 400 ms. Echocardiogram revealed mild mitral valve regurgitation with mital E‐A fusion during ventricular diastole. His ventricular systolic function was found to be normal, but the level of NT‐proBNP was mildly elevated.
Decision‐making: The symptoms of this patient can be attributed to the cardiac dysfunction caused by delayed conduction in the atrioventricular node, reflected by excessively prolonged PR interval. Delayed conduction in the atrioventricular node significantly reduces the effective filling period of ventricular diastolic phase and leads to cardiac dysfunction. To address this, the patient received left bundle branch pacing to shorten the atrioventricular conduction time. After pacemaker implantation, his PR interval was reduced to 180 ms, and his E and A peaks returned to normal. Four months later, his symptoms were remarkably relieved. During the 2‐year follow‐up, he remained clinically stable.
Conclusion: In patients with excessively prolonged PR interval, prompt decision‐making regarding cardiac pacing therapy can help improving clinical symptoms and enhance the patient's quality of life.
CS‐859‐CIED
Two different venous access techniques leading to single pacing lead transection
Danlu Liang 1; Gareth Wynn2; Alistair Royse2,3; Jacinta Brown1; Han Lim1,3
1Austin Health, Heidelberg, Australia; 2Royal Melbourne Hospital, Parkville, Australia; 3University of Melbourne, Parkville, Australia
Background: Friction between clavicle and first‐rib can damage CIED‐leads placed via medial venous access. We describe a case of complete lead transection where both medial and lateral venous approaches were employed.
Case: 75‐year‐old man presented with pectoral muscle‐twitching 3‐years after Medtronic dual‐chamber pacemaker insertion. RV and RA‐leads were inserted via medial subclavian and lateral axillary approach, respectively. A sudden increase in RV impedances and threshold, decrease in R‐Wave amplitude and polarity switch correlated with symptom timing. CXR revealed complete RV‐lead transection at the subclavian‐vein. RA‐lead was intact.
Decision‐making: Distal RV‐lead was extracted using femoral approach with Needle's‐Eye Snare (CookMedical®). Proximal portion was removed by traction. New RV‐lead was implanted via cephalic‐vein. Medial subclavian access leads course between the clavicle and first‐rib making them unprotected and vulnerable to trauma before entering the vein. Lateral entry may avoid subclavian crush.
Conclusion: Implanters should consider lateral venous access approaches to minimise subclavian crush syndrome risk.

CS‐867‐CIED
Use of cardiac contractility modulation in a patient with chronic heart failure and renal dysfunction: A case report
Zhao Yijiang; Rong He; Lei Bi; Lingyun Kong; Kexin Zhang; Yuanwei Liu; Jing Yang; Ping Zhang
Beijing Tsinghua Chang Gung Hospital, Beijing, China
CCM (Cardiac Contractility Modulator) represents an emerging effective and safe HF device therapy for the treatment of HFrEF patients.
A 54‐year‐old female patient was admitted to the cardiology department in our hospital for exertional dyspnea and edema. Her past medical history is end‐stage kidney disease.
At clinical admission, the patient was in class NYHA III. ECG showed sinus rhythm, QRS <120 ms. LVEF was 25%. CRE value was 850.0 μmol/L indicating an eGFR of 4.4 mL/min/1.73 m2, NT‐proBNP was 153,322 pg/mL, and hs‐TnT was 0.074 ng/mL↑. The Minnesota Living with Heart Failure Questionnaire (MLHFQ) score was 21 points.
After admission, we optimized drug treatment for her three times a week. However, the level of BNP and CRE was still deteriorating. According to ESC guidelines on the management of chronic and acute HF, the patient was eligible to both ICD and CCM. To reduce HF‐related hospitalizations and to improve quality of life, we decided to implant a CCM therapy device after a patient‐clinician discussion.
At 3‐month follow‐up, the patient already experienced significant improvements in terms of LVEF (from 25% to 39%), MLWHFQ score (21–73), distance of 6‐min walk test (from 343 to 470 m), a smaller size of heart, and no HF‐related hospitalizations.
In our report, it showed that the use of CCM therapy as a standalone device could also be a good choice for HFrEF patients with end‐stage kidney disease, which led to improved quality of life, systolic function of ventricle, and function of kidney, and a reduction in HF‐related hospitalizations.

CS‐871‐CIED
A rare case of cardiovascular implantable electronic device (CIED) infection presenting as tricuspid valve endocarditis in an adult Filipino male: A case report
Lloyd Christopher Lim; Marie Kirk Patrich Maramara; Azel Paolo Bondoc; Giselle Gervacio; Richard Henry Tiongco
Division of Cardiovascular Medicine, Department of Medicine, University of the Philippines‐Philippine General Hospital, Manila, Philippines
Background: We present a case of an adult male with a dual chamber pacemaker who presented with a 2‐month history of on and off fever, diagnosed as CIED infection with tricuspid valve endocarditis, necessitating extraction of tricuspid valve vegetation, extraction of pacemaker leads and pulse generator, and epicardial permanent pacemaker insertion.
Case: A 58‐year old male, hypertensive and diabetic, is a known case of third degree AV block since 2018 presenting as syncope, underwent dual chamber pacemaker implantation with subsequent PTCA of the proximal to mid‐LAD due to three‐vessel coronary artery disease, with subsequent RV lead replacement after 3 years due to lead fracture. Patient had no symptoms in the interim until 2 months prior to admission when he started to have on–off low‐grade fever episodes associated with development of Janeway lesions on his palms. Baseline 12L ECG on admission showed ventricular paced rhythm. Transthoracic echocardiogram revealed a 13 mm × 14 mm tricuspid valve vegetation with concentric left ventricular remodeling and adequate systolic function. Three sets of blood cultures were consistently positive for growth of Staphylococcus epidermidis; hence impression was CIED infection with tricuspid valve endocarditis.
Decision‐making: Patient successfully underwent tricuspid valve vegetectomy, extraction of pacemaker leads and pulse generator, and epicardial permanent pacemaker implantation, with no residual vegetation in the tricuspid valve leaflets. Vancomycin was completed for 6 weeks with negative blood cultures.
Conclusion: Complete CIED explantation is recommended for complete resolution of infective endocarditis secondary to a CIED with timing of reimplantation dependent on negative blood cultures.

CS‐899‐CIED
Recurrent Cardiac Arrest as the Transient Manifestation of Neuromyelitis Optica Spectrum Disorder: a Case Report
Jingwen Zhang1,2; Ge Wang1,2; Haiying Li1,2
1Division of Cardiac Arrhythmia, Cardiac and Vascular Center, The University of Hong Kong‐Shenzhen Hospital, Shenzhen, China; 2Clinical, Translational and Basic Research Laboratory, The University of Hong Kong‐Shenzhen Hospital, Shenzhen, China
Background: Recurrent cardiac arrest as the transient manifestation of neuromyelitis optica spectrum disorder has rarely been reported.
Case presentation: A 44 ‐year‐old male was clinically presented with a vicous cycle as violent vomiting followed by intermittent epilepsy accompanied with recurrent cardiac arrest, with the longest RR interval recorded as 9 seconds. And this cycle repeat for 20‐30 times per day. He showed no damage on muscle strength, tendon reflexes, thermal, pain and vibration sensations. Bladder and rectal disturbances were not found. And his optic neuritis were normal after 2 weeks of the disease course. He was finally been able to be diagnosed as NMOSD based on the positive serum autoantibodies for Aquaporin 4 antibody (AQP4), while cranial magnetic resonance image detected at the dorsal aspect of the medulla oblongata come back negative. Anti‐nuclear antibody (ANA) (1:100) and anti‐SSA positive (++++) combined with positive ophthalmologic examination on tear secretion test indicated that he also has Sjögren’s syndrome. The patient was immediately implanted a temporary pacemaker for life support. Meanwhile he was treated with one course of an intravenous methylprednisolone pulse for 1000mg per day and one course of immunoglobulin 20g per day lasting for 5 days. A week later, He was been able to remove the pacemaker for his 24‐hour ambulatory electrocardiogram come back negative. He regained healthy and got discharged when his recurrent vomit ceasing with cardiac arrest as well. One year follow up showed that the patient has got fully recovered with no sign of neurological sequelae.
Conclusion: The case present a young male with recurrent autonomic nervous system lesion as the main manifestation of NMOSD. Recurrent cardiac arrest was used to be severe but also got fully recovered rapidly after only one course of immune therapy. This indicate not only one new spectrum of NMOSD, but also pointed out that it is not necessary to implant a permanent pacemaker in case of recurrent cardiac arrest detected in the initial course of NMOSD. Keywords: Cardiac arrest, Pacemaker implantation, Neuromyelitis optica spectrum disorder, Autonomic nervous system, Case report
.
CS‐73‐CAR
Epicardial pacing: Insight of late superior vena cava thromboembolism induced pacemaker lead fracture in a young woman
Subiyanto Fong; Theovano Oktavio; Benny Setiadi
Sam Ratulangi University, Manado, Indonesia
Background: Delayed superior vena cava (SVC) thromboembolism after pacemaker implantation is a rare but fatal outcome. We present a case of SVC thromboembolism induced pacemaker lead fracture in young woman resulted in implantation of epicardial pacing.
Case Presentation: A 35‐year old woman presented with presyncope. Patient's had pacemaker implanted for 10 years which never been interrogated as she felt asymptomatic. Heart rate was 35 beats/minute, blood pressure at 108/66 mmHg. Electrocardiogram showed uncaptured total AV Block, echocardiography showed normal heart function and structures. Pacemaker malfunction was suspected as culprit. During attempted urgent permanent pacemaker replacement procedure, the pacemaker lead was found fractured and the wire failed to cross SVC, the procedure then aborted. Later, patient's CTA (computed tomography angiography) scan showed near total occlusion at SVC with collateral flow from chest wall veins and intra lumen thrombus at right proximal jugular vein. Epicardial pacing placement and extraction of old pacemaker through thoracostomy was performed. Post procedure, patient was stable without complaint.
Decision‐making: Pacemaker implantation may cause venous endothelial injury releasing coagulation factors, hence, venous thromboembolism. Development of collateral flow decreases flow in the affected venous segment which extent the thrombus formations causing lead fracture induced pacemaker malfunction. Epicardial pacing is the choice in venous occlusion as presented in this case.
Conclusion: Routine control of pacemaker device and early screening for thrombus is a must. Epicardial pacing can be done in venous access occlusion case.
CS‐93‐CAR
High‐grade atrioventricular block in adolescent: A report of atypical presentation of acute rheumatic fever
Jian‐Gang Ang; Hazleena Mohamed Hasnan; Yew Fung Kwan; Jo‐Ven Chang; Kengeswary Raja; Sabapathy Diagarajan; Gurpreet Pal Singh Jugindar Singh; Tai Meng Chen; Zarrin Kang; Nor Hanim Mohd Amin
Hospital Raja Permaisuri Bainun, Ipoh, Malaysia
Background: Acute rheumatic fever is an autoimmune inflammatory process involving the heart, joints, central nervous system, subcutaneous tissue and skin. Here we present a case of acute rheumatic fever with atypical presentation.
Case: A 15‐year‐old boy presented with chest pain. There was a recent history of fever, back pain and knee pain for 5 days. He had no skin rash or abnormal movement. Examination showed no joint abnormality and no heart murmur. The electrocardiogram showed high‐grade atrioventricular block with ventricular standstill. An echocardiogram showed mild mitral regurgitation. Erythrocyte sedimentation rate and antistreptolysin‐O titer were raised with 65 mm/h and 800 IU. Troponin level was not raised, rheumatic factor and antinuclear antibodies were negative. A temporary pacemaker was inserted as he subsequently complained of giddiness. Thus, we treated him as acute rheumatic fever. High dose aspirin was started. He made a good recovery and his heart rhythm returned to sinus rhythm 3 days after treatment. The temporary pacemaker was subsequently removed.
Decision‐making: Prolonged atrioventricular conduction i.e. first degree atrioventricular block is a well‐recognized feature of acute rheumatic fever. The incidence of higher degrees of atrioventricular block is low. It is usually transient and reverses to sinus rhythm over the course of days. Role of steroids in carditis for acute rheumatic fever is controversial. However, our patient showed marked clinical improvement on high dose aspirin alone.
Conclusion: In conclusion, high‐grade atrioventricular block can occur in acute rheumatic fever, albeit rarely. Adolescents present with acquired heart block deserve a work‐up for rheumatic fever.
CS‐133‐CAR
Cough syrup addiction: A patient's slippery slope to ventricular tachycardia
Michael Tierney 1; Pratap Shetty1; Judy Al Ahmad1; Sukhmandeep Sangha1; Una Ionmhain2,3; Ivan Subiakto1
1Wollongong Hospital, Wollongong, Australia; 2Liverpool Hospital, Sydney, Australia; 3New South Wales Poisons Information Centre, Sydney, Australia
Background: Cough syrup and loperamide are both weak opioids. Loperamide abuse is rarely described to cause QTc prolongation and ventricular tachycardia (VT).
Case: A 29‐year old man presented with abdominal pain, palpitations and witnessed conscious monomorphic VT after ingesting 200 loperamide tablets. He had ingested this due to restricted access to cough syrup. After spontaneous reversion to sinus rhythm his ECG demonstrated QRS 200 ms, QTc 612 ms and anterolateral T‐wave inversion. During admission he had a polymorphic VT arrest, requiring electrical cardioversion, without any other reversible cause besides significant QTc prolongation. After ceasing loperamide his QRS and QTc normalised at day 5, in keeping with the half‐life reduction of N‐desmethyl‐loperamide (loperamide metabolite). Anterolateral T‐wave inversion persisted.
Decision Making: This case demonstrates the diagnostic dilemma of excluding another predisposing cause of VT. There was suspicion of a further predisposing cause as coincidentally during this admission the patient's brother died of sudden cardiac death with autopsy findings suggestive of dilated cardiomyopathy. Whilst our patient's echocardiography and cardiac MRI demonstrated mildly impaired left ventricular systolic function (EF 42%) and segmental non‐compaction (NC:C 2.7) ultimately his cardiomyopathy and channelopathy genetic panel was negative. Flecainide challenge and exercise stress test were also reassuring. No further arrhythmia occurred after cessation of loperamide and commencing bisoprolol.
Summary: This rare case demonstrates that overdose of loperamide can lead to life threatening arrhythmia from prolongation of QTc, even without contributing factors such as inherited cardiomyopathy or channelopathy. Excluding contributing aetiologies was of critical importance to avoid unnecessary defibrillator implantation.
CS‐145‐CAR
Atypical atrial flutter‐fibrillation and obstructive sleep apneu interconnection
Dya Andryan; Dony Yugo Hermanto
National Cardiovascular Center Harapan Kita, Faculty of Medicine Universitas Indonesia, Jakarta, Indonesia
Background: Atrial fibrillation (AF) is the most common sustained cardiac arrhythmia worldwide, while obstructive sleep apneu (OSA) is one of overlooked AF comorbid. The following case describes cases of AF‐OSA connection, as well as its importance.
Case: Mrs AT, 42 year old came to the arrhythmia outpatient clinic with complaints of palpitations got worse the past 1 year. The patient had a history of palpitations similar to before in mid‐2018. The patient underwent 3D ablation in June 2020 with the results of Multifocal atrial tachycardia with partial success of ablation. After the ablation procedure, the palpitations are still felt by the patient.
Patient was known has obstructive sleep apnea (OSA) as the Afib comorbid. Patient was diagnosed with atypical atrial flutter‐fibrillation with OSA.
Decision‐making: Patient was planned for 3D AFib Ablation as well as referral to sleep specialist. Circumferential isolation of right carina and right PV were delivered, conclude this is case of right pulmonary vein of atrial flutter. For her OSA, Patient underwent polysomnography, revealed the patient had severe obstructive sleep apnea syndrome. The Apnea‐hypopnea index (AHI) was 50.3/h (normal 0–5/h), with lowest oxygen 76% during sleep. Patient then underwent CPAP therapy.
Post ablation ECG showed sinus rhythm with QRS rate 66×/min, with reduce intensity of symptom. Her heart rate variability reduced from her smartphone tracking, as well as clinical improvement from the patient.
Conclusion: OSA is an important but overlooked risk factor for AF. It is important to treat AF in holistic way.

CS‐169‐CAR
The lightning strike: Unusual link between ventricular arrhythmias and sarcoidosis
Faten Aqilah Aris; Tommy Daindes; Rohith Stanislaus; Muhammad Izzad Johari; Hisham M. D. Shahrom; Azlan Hussin
National Heart Institute, Kuala Lumpur, Malaysia
Background: Sarcoidosis is a multisystem inflammatory disease characterized by granuloma formation usually affect lungs and lymph nodes. Ventricular tachycardia (VT) is one of the frequent presentation of cardiac sarcoidosis. We report a case of patient diagnosed with sarcoidosis presented with VT storm.
Case: A 33 years old lady presented for elective endoscopy appointment noted to have tachycardia (180 bpm). ECG showed VT. She was treated as stable VT and given IV amiodarone but failed to terminate her VT. Echocardiogram showed ejection fraction of 45% with hypokinetic at inferolateral wall. She was cardioverted after fail medication. Cardiac MRI showed subepicardial myocardial fibrosis with inflammation and edema at the basal to apical lateral and basal to mid inferior walls which suggestive myocarditis with a differential of sarcoidosis. Blood investigations were normal including inflammatory markers. CT scan of Neck, Chest, Abdomen and Pelvis showed hepatosplenomegaly with generalized lymphadenopathy. Despite started on high dose steroid she continue to have recurrent VT thus implantable cardioverter was implanted. Liver biopsy showed non caseating granuloma consistent with sarcoidosis. She was treated with immunosuppression and has not had any VT episode.
Decision Making: Cardiac MRI was done with the intention to aid in catheter ablation but revealed features of inflammation and possible sarcoidosis. VT was incessant to medication thus implantable cardioverter was implanted prior to referral to hematologist.
Conclusion: VT is a rare presentation of sarcoidosis, accurate diagnosis need high index of suspicious. Ventricular arrhythmia in sarcoidosis is difficult to control. Treatment include steroid, immunosuppression, implantable cardioverter and catheter ablation.

CS‐188‐CAR
A case of cardiac sarcoidosis with complete atrioventricular block in which the heart rate was relatively maintained, improved with steroid using FDG‐PET as an index
Taishi Hirahara; Yoshimitsu Tsurumaki; Hiroshi Wada; Midori Sato; Norifumi Kubo
JCHO Saitama Medical Center, Saitama, Japan
The common therapy for cardiac sarcoidosis is steroid, but if activity cannot be confirmed, there are side effects of steroid, it is controversial whether to administer them. We report a case of cardiac sarcoidosis with complete atrioventricular block (C‐AVB) without pacemaker indication. The patient is a 61‐year‐old man. A physical examination revealed C‐AVB, and he was referred to our hospital. Echocardiography showed normal cardiac function. Holter ECG showed C‐AVB throughout the day, but average heart rate preserved. Because he had previously suspected pulmonary sarcoidosis, cardiac sarcoidosis was suspected. Laboratory data showed a slight increase of ACE at first time only. Cardiac MRI showed delayed enhancement localized to the basal interventricular septum. C‐AVB was associated with cardiac sarcoidosis, but heart rate was preserved. Although cardiac function is currently preserved, it is possible that cardiac sarcoidosis may progress in the future. We recommended him to take steroid, but he did not take it because of possible side effect. But later shortness of breath appeared and BNP slightly increased. Because current activity of sarcoidosis was unclear, FDG‐PET was performed to determine the activity. As a result, there was partial uptake in the lungs and heart. Pulmonary and cardiac sarcoidosis were suspected. In addition, bronchoscopic lung biopsy pathologically diagnosed sarcoidosis. Based on the results, we determined activity existed and steroid was started. A year later C‐AVB improved to first‐degree atrioventricular block, and BNP improved.
We report a case of cardiac sarcoidosis with C‐AVB without pacemaker indication, FDG‐PET revealed activity of sarcoidosis and taking steroid improved atrioventricular conduction.
CS‐196‐CAR
Not just slow, tackling Torsades de Pointes in bradycardia
Chandra James Kurniawan; Benny Mulyanto Setiadi; Lily Wongso; Sheila Adiwinata
Sam Ratulangi university/Prof. Dr. R.D. Kandou Hospital, Manado, North Sulawesi, Indonesia
Background: Torsades de Pointes (TdP), a polymorphic ventricular tachycardia which associated with prolonged QT interval is a potential fatal tachyarrhythmia. Inverse relationship between heart rate and repolarization time makes bradycardia as one of the major factors predisposing to TdP.
Case: We reported two cases of TdP in patient with bradycardia. First, 68 years old male was admitted to our hospital due to loss of consciousness three times a day which initially preceded by palpitation. ECG showed sinus bradycardia 50 bpm with double‐peaked T wave morphology and QT interval prolongation (Qtc 633 ms). Second, 86 years old female was admitted due to three episodes of presyncope within a month. ECG showed sinus bradycardia 43 bpm with second degree AV block Mobitz II, with prolonged QT interval (Qtc 640 ms). Both patient had no history of QT‐prolonging medications.
Decision‐making: Complete blood count, thyroid function and electrolyte were in normal range. Echocardiography showed normal biventricular function without structural abnormalities. Inhospital 24 h holter monitoring was done and revealed TdP with 180 bpm which fortunately self‐terminated. Dual chamber permanent pacemaker was implanted. Patients had no complaint, pacing was seen >95% of the time and QT interval no more prolonged. Both patients had no further syncope episodes.
Conclusion: Bradycardia and pauses induced prolonged QT interval might predispose to TdP. Recognition of potentially lethal ECG in bradycardia patients such as T wave notching and prolonged QT had a predictive value for TdP. Combination of permanent pacemaker implantation with beta‐blockers could become a major role of treatments.
CS‐227‐CAR
Current status of emergent ventricular arrhythmia catheter ablation: Where are we now?
Tommy Daindes; Faten Aqilah Aris; Hisham Md Shahrom; Rohith Stanislaus; Azlan Hussin
Institut Jantung Negara, Kuala Lumpur, Malaysia
Background: Catheter Ablation (CA) in the acute management of VA is known as a challenging procedure. We outline the role of comprehensive management in successful procedures through the following cases.
Cases: Case‐1: A 62‐year‐old male came with monomorphic VT 1 week after LAD PCI for Acute MI. After several cardioversion, anti‐arrhythmic infusion, deep sedation, and angiography with acute stent thrombosis management, VT still occurred and emergent CA was performed. Three‐dimensional mapping showed a deceleration zone at the basal anteroseptal LV (just below the left bundle/His). CA is performed. No more VT after the procedure and the patient was discharged after ICD implantation a week later.
Case‐2: A 62‐year‐old female was referred with resuscitated VF after uneventful LAD PCI. Angiography showed a patent LAD stent. Cardioversions and anti‐arrhythmic infusions had been given but VF persisted. The patient was knocked down and emergent 3D mapping was performed, showing the area of interest at the posteromedial papillary muscle of the LV. Supported by intra‐cardiac echocardiography, CA is performed. Several Non‐Sustained VF keeps showing 2 days after the procedure but then decrease significantly. The patient was discharged after ICD implantation 10 days later.
Decision‐making: Sedating the patient while correcting the reversible cause of VA and performing emergent CA under cutting‐edge 3D mapping system and ICE guidance outstandingly improves the procedure outcome. Post‐procedural ICU monitoring and pre‐discharge ICD implantation assures the best practice for patients.
Conclusion: Comprehensive management undoubtedly plays a significant role in the successful emergent CA of ventricular arrhythmias.

CS‐280‐CAR
Syncope in a patient with an implantable cardioverter‐defibrillator
Justin Phan 1,2,3; Bruce Walker1,2; Rajesh Subbiah1,2,3
1St Vincent's Hospital Sydney, Darlinghurst, Australia; 2University of New South Wales, Sydney, Australia; 3Victor Chang Cardiac Research Institute, Darlinghurst, Australia
Background: A 66‐year‐old man with atrial flutter, severe cardiomyopathy and implantable defibrillator (Medtronic) was admitted with cardiogenic syncope.
Case: The patient was admitted for cardiac monitoring, which showed a symptomatic episode of non‐sustained VT at 170 beats per minute (bpm). This was not observed in the device arrhythmia log despite a monitor zone of 150–182 bpm.
Decision‐making: During atrial flutter, Medtronic defibrillators do not record episodes of non‐sustained VT in the monitor zone. This patient's syncope was likely due to VT at a rate below the treatment zone. Atrial over‐drive pacing was performed to revert the patient to sinus rhythm. The treatment zone was lowered to 160 bpm and no further syncope occurred.
Conclusion: Syncope in patient with an implantable defibrillator should prompt an evaluation for VT below the treatment zone. An important interaction exists with VT detection in patients with atrial tachy‐arrhythmias.

CS‐349‐CAR
Obstructive sleep apnea as overlooked risk factor for arrhythmia and stroke: Case report
Hendyono Lim; Hardi Hutabarat; Indah Sukmawati
Siloam Hospitals Lippo Village, Tangerang, Indonesia
Background: Obstructive sleep apnea (OSA) increases risk of stroke through multiple mechanism, also reported increased after stroke. (1) Nocturnal hypoxemia caused by OSA leads to cardiac remodelling and conduction rhythm disorders, leads to new onset cardiac arrhythmia included ventricular tachycardia (VT), mostly atrial fibrillation. (2) Unfortunately, awareness of OSA still low among stroke and cardiac arrhythmia patients, thus screening for OSA is underestimate.
Case Illustration: Male 63 years old with prior history of uncontrolled hypertension and smoking admitted with sudden weakness left side extremities. According to his wife, patient is snoring while sleeping with frequent episodes of periodic apnea. Electrocardiography confirmed sinus rhythm with right bundle branch block. Brain MRI confirmed multiple acute lacunar infarctions with severe bilateral middle cerebral artery stenosis. Holter monitor confirmed episode of paroxysmal atrial fibrillation, frequent PVCs and short ventricular tachycardia during sleep at night (Figure 1), and frequent premature ventricular extrasystole during daytime. Patient was advised to do polysomnography to confirm the severity of hypoxia episodes.
Discussion: It was described that repeated intermittent episodes of hypoxia caused by OSA triggered arrhythmogenesis. Number of studies already reported increased risk of AF in the presence of OSA, along with ventricular ectopy and ventricular arrhytmias. Current AF guideline recommended OSA screening and treatment, to prevent occurrence of AF along with stroke. (3) Polysomnography is the gold standard to confirmed OSA, combine with holter monitoring might provide better strategies in arrhytmias work‐up and treatment.

CS‐375‐CAR
Misleading causality between complete heart block and acute kidney injury: Rarely, it's other way round
Phrycilia Limen; Elias Michael; Billy Untu; Benny Setiadi
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Sam Ratulangi University, Manado, Indonesia
Background: Complete heart block is a life‐threatening condition in which at some cases explained as manifestation of acute kidney injury (AKI), whereas the reports of contrariwise case are very limited. We report a case of AKI due to a complete heart block which was never diagnosed before.
Case Presentation: A 67‐years old man presented in emergency ward with dizziness for 2 weeks. Electrocardiography showed complete heart block with ventricular rate 26 bpm. He was then proceeded for urgent temporary pacemaker (TPM) insertion. Creatinine level was 5.1 mg/dL and potassium 7.2 mEq/L though the patient has no history of renal disease with baseline creatinine level 1.3 mg/dL. After TPM insertion the creatinine level decreased to 1.7 mg/dL and potassium to 5.0 mEq/L. Electrophysiology study was performed several days after in which 440 ms incremental atrial pacing showed prolonged HV intervals, confirming the block site is on the infra‐Hissian area. The patient was planned for permanent pacemaker.
Discussion: Arrhythmia may reduce cardiac output temporarily, thereby attenuating kidney perfusion once renal autoregulation fails. Complete heart block is a life‐threatening condition and acute kidney injury (AKI) which is usually caused by renal hypo‐perfusion is associated with adverse outcomes. Patients with AKI resulted from complete heart block are likely to recover once pacemaker was implanted.
Conclusion: Acute kidney injury (AKI) induced by complete heart block is a rare condition and sometimes the general comprehension between AKI and complete heart block causality might lead to a mistreatment. The renal injury could recover after the pacemaker implantation.
CS‐415‐CAR
Torsade de pointes caused by coronary vasospasm combined with long QT syndrome: a case report
Hinh Nguyen Van; Tho Pham The; Ly Nguyen Thi Kieu; Son Pham Truong
108 Military Central Hospital, Hai Ba Trung District, Việt Nam
Coronary vasospasm and QT prolongation can lead to a fatal arrhythmia.
A 53‐year‐old male with a history of smoking (more than 20 pack years), and no other medications or significant diseases, was referred to the hospital due to chest pain and four episodes of syncope over 2 months. During the episode, the patient had atypical chest pain, palpitation for 1 min, then loss of consciousness over 2–3 min with pale skin, no convulsion, and subsequently recovered without paralysis. The patient was admitted to the hospital after fully recovering and no significant finding on physical examination. The ECG showed transient ST elevation at inferior leads (II, III, aVF) then ST became normal after 10 min, corrected QT interval of 510 ms. The laboratory test revealed the normal level of high‐sensitive troponin T, isozyme MB of creatinine kinase, and the normal electrolyte level. Echocardiography was normal and coronary angiography showed no significant stenosis but inducible coronary vasospasm by acetylcholine. The 24‐h Holter ECG at the time of syncope showed ST‐elevation for 1 min, then induced monomorphic ventricular tachycardia and subsequently torsade de pointes before spontaneously recovering. The genetic test showed positive KCNQ1 mutations.
The patient was diagnosed with coronary vasospasm and congenital long QT syndrome and treated with coronary vasodilators, including non‐dihydropyridine calcium channel blockers (diltiazem 60 mg twice daily), and nitroglycerin sublingual spray. An implantable cardiac defibrillator was successfully implanted for secondary prevention.
In conclusion, coronary vasospasm, and long QT syndrome should be investigated in patients with unexplained syncope.

CS‐430‐CAR
Catheter ablation combining cardiac resynchronization therapy for cardiomyopathy induced by persistent atrial fibrillation and complete left bundle branch block: A case report
Ning Chen; Mingfang Li; Hongwu Chen; Kai Gu; Minglong Chen
The First Affiliated Hospital of Nanjing Medical University, Nanjing, China
Arrhythmia‐induced cardiomyopathy (AIC) was diagnosed retrospectively by eliminating arrhythmia. We presented a case of 63‐year‐old man with dilated cardiomyopathy, persistent atrial fibrillation (PAF) and complete left bundle branch block (CLBBB). The suspicion of coronary artery disease was excluded. Cardiac magnetic resonance showed no scar. Patient underwent catheter ablation and cardiac resynchronization therapy (CRT). The indication for CRT was CLBBB with QRS duration to 183 ms and reduced left ventricular ejection fraction of 32%. Catheter ablation was for preservation of atrial systolic function and reduction of stroke risk. During follow‐up, the structure and function of left ventricular were reversed progressively post operation with no recurrence of PAF. Therefore, the patient was diagnosed with dual AIC induced by PAF and CLBBB. For patients with severely heart failure complicated by PAF and CLBBB, catheter ablation combining CRT was long‐term effective in condition of younger age, shorter course and lower scar load.

CS‐436‐CAR
The monitor alarm induced type 2 long QT syndrome of KCNH2 mutation
Hong Pan; Zichao Su; Jingting Mai; Yuling Zhang
Sun Yat‐sen Memorial Hospital, Sun Yat‐sen University, Guangzhou City, China
Background: A recurrent syncope patient with long QT interval and torsades de pointes (Tdp) during hospitalization due to monitor alarm was successfully treated. KCNH2 mutation was found by genetic test.
Case: The patient had recurrent syncope for 20 years, usually triggered by sudden fright such as door knock or alarm ring. Before each episode, the patient felt palpitations followed by complete loss of consciousness. Fifteen days ago, another episode of syncope occurred and no abnormalities were found in 24‐h Holter monitoring. The patient had no history of taking any special medications and no family history of sudden death or syncope. Admission electrocardiogram revealed a markedly prolonged QT interval (620 ms) with biphasic T waves. During hospitalization, the patient was startled by the monitor alarm while asleep and suddenly had a syncope episode and loss of consciousness, which lasted for 20–30 s and resolved spontaneously. Cardiac monitoring captured the episode of Tdp.
Decision‐making: Episode management: potassium and magnesium supplementation, atrial temporary pacing with rate of 90 bpm.
Long‐term Treatment: implantation of implantable cardioverter‐defibrillator, long‐term use of metoprolol.
Genetic Test: KCNH2 mutation (+).
Diagnosis: Arrhythmia: long QT syndrome (KCNH2 mutation +).
Teaching Points: Patients with multiple 24 h Holter recording without abnormal heart rhythm, but considering cardiogenic syncope, should carefully inquire the clues of medical history and undergo long‐term Holter (>72 h) to capture the abnormal heart rhythm during the episode.
Conclusion: LQTS is prone to misdiagnosis. The treatment needs to pay attention to both rescue and long‐term management. Genetic testing is an important indicator.
CS‐494‐CAR
Cardiac infiltration of diffuse large B‐cell lymphoma manifesting as sustained ventricular tachycardia: A case report
Wei Chen2; Kun Huang 1; Dening Liao1
1Changzheng Hospital: Shanghai Changzheng Hospital, Shanghai, China; 2Shanghai Jingan District Zhabei Central Hospital, Shanghai, China
Background: Cardiac tumors are rare. The symptoms of cardiac metastases vary depending on the degree of myocardial infiltration. Arrhythmias, such as atrioventricular block, atrial flutter or fibrillation, ectopy, or ventricular tachycardia, can be present, especially when the conduction system has been infiltrated.
Case: We present a 77‐year‐old man suffer from suspected cardiac infiltration of diffuse large B‐cell lymphoma manifesting as sustained ventricular tachycardia. Neither antiarrhythmic drugs nor defibrillation can terminate VT episodes. The ECG showed sustained wide QRS tachycardia with left bundle branch block (LBBB) morphology and QRS complex positive in lead I and aVL, which inferred the tachy‐arrhythmia would originated from the anterior wall of the right ventricle, this was consistent with the exact location of the tracer high‐uptake on prior PET‐CT.
Decision‐making: Chemotherapy was started urgently, the electrical‐storm was eliminated within 48 h and did not recur during 3 months of follow up.
Conclusion: In patients afflicted with advanced malignancies and malignant arrhythmias, particularly lymphoma, if antiarrhythmic medications and electronic cardioversions are not effective for the management of arrhythmias, cardiac infiltration should be taken into account as a possible cause of arrhythmias. PET‐CT and anti‐tumor interventions warrant consideration as a viable approach to detecting and mitigating arrhythmic episodes.

CS‐527‐CAR
TBX20 mutation in a middle‐aged male with early repolarization and recurrent ventricular tachycardia and fibrillation
Rongjie Lin; Yuling Zhang; Jingfeng Wang
Sun Yat‐sen Memorial Hospital of Sun Yat‐sen University, China
Background: Patients with early repolarization may experience malignant arrhythmias, but the mechanism is not clear.
Case: A 53 year old male was admitted due to recurrent syncope in the past 20 years, which worsened for half a month. The electrocardiogram showed early repolarization changes in leads II, III, and aVF, and there were no abnormalities in brain MRI, electroencephalogram, echocardiography, and cardiac MRI. There were no abnormalities in cardiac, liver, kidney and thyroid function. Recurrent syncope occurred in the patient, and holter ECG monitoring showed that the syncope was related to recurrent ventricular tachycardia and ventricular fibrillation induced by premature ventricular beats with short coupling interval. In order to determine the cause, we performed gene sequencing. No gene mutation related to ion channel was found, but we noticed that the patient had TBX20 mutation.
Decision‐making: An ICD was implanted and metoprolol was given, and the patient had no more malignant arrhythmias.
Conclusion: The case showed a mutation in TBX20. TBX20 is a conserved member of the T‐box gene family that encodes key transcription factors and is expressed in the heart, eyes, and limbs of the human fetus. In recent years, a number of studies have shown that TBX20 is related to the maturation and contraction of myocardium, and plays an important role in myocardial reprogramming. Therefore, this case suggests that TBX20 gene mutations may cause cardiac electrical remodeling, leading to the occurrence of malignant arrhythmias, and this gene may be a potential therapeutic target for early repolarization.
CS‐555‐CAR
A rare case of ventricular tachycardia in a child with a normal heart
Muhammad Hafiz Mahruzza Putra; Ali Nafiah Nasution; Hilfan Ade Putra Lubis; Grace Nikensari; Inke Nadia Diniyanti Lubis; Anggia Chairuddin Lubis; Cut Aryfa Andra; Sophia Khairina Khaidirman
Universitas Sumatera Utara, Medan, Indonesia
Background: Ventricular tachycardia (VT) is rarely seen in children. It is a serious form of arrhythmia that can be life threatening. Therefore, prompt diagnosis and treatment are very important to avoid serious complication and sudden cardiac death.
Case: A 12‐year‐old girl was admitted to the emergency room at H. Adam Malik Hospital, Medan, Indonesia, with palpitation 1 h prior to admission. She had history of fever a day before and had consumed several drugs (paracetamol, antihistamine) all at once to reduce her fever. She had no history of previous syncope or poor feeding, and no profound family history. On admission, her hemodynamic was stable and ECG showed wide QRS tachycardia at 200 beats per minute and revealed VT. Chest X‐ray, laboratory tests and echocardiography findings were all normal.
Decision‐making: 150 mg of amiodarone was administered via IV bolus for 30 min. Following treatment, ECG reverted to sinus tachycardia with right axis deviation, and the patient remained stable. Amiodarone was continued for maintenance over 24 h, and the patient was discharged the following day. The etiology of VT in this patient could not be determined.
Conclusion: We reported a case of VT in a healthy pediatric patient. Although uncommon, it can be life‐threatening. It is challenging to identify the cause of VT in this patient, and A 24‐h holter monitoring and magnetic resonance imaging should be considered to determine the right etiology.
CS‐558‐CAR
Ventricular tachycardia induced by propafenone in an infant patient
Tengyang Wang; Wei Ji; Xiao Feng Guo
Fujian Children's Hospital, Fuzhou, China
Background: Propafenone is a class 1C antiarrhythmic drug used in the second‐line management of supraventricular and ventricular arrhythmias. Aggravation of arrhythmia by propafenone is rare, but may be life‐threatening due to drug‐induced ventricular tachycardia.
Case: A 5‐month‐old infant with history of multifocal atrial tachycardia visited our hospital for feeding difficulty. The patient was taking propafenone 37.5 mg (5.3 mg/kg) q8h and metoprolol 6.25 mg (0.9 mg/kg) q8h regularly. Clinical examination showed heart rate 206 beats/min, and electrocardiogram revealed ventricular tachycardia.
Decision‐making: We gave the patient synchronized electrical cardioversion. After cardioversion, electrocardiogram showed multifocal atrial tachycardia with prolonged Q‐T interval. We replaced propafenone with amiodarone, and did not observe ventricular tachycardia in this patient afterward.
Conclusion: This case highlights the possibility of propafenone leading to ventricular tachycardia in the treatment of multifocal atrial tachycardia. Propafenone may lead to Q‐T prolongation and increase the risk of ventricular tachycardia occurrence. And Q‐T prolongation can be overlooked in patients with multifocal atrial tachycardia.

CS‐581‐CAR
Transesophageal overdrive pacing in special patients with paroxysmal supraventricular tachycardias
Quoc Cuong Truong 1; Quang Khanh Truong2; Gia Huy Tran3
1Thong Nhat Hospital, Ho Chi Minh, Viet Nam; 2Thong Nhat Hospital, Viet Nam; 3Thong Nhat Hospital, Viet Nam
Background: We describe two complex cases of paroxysmal supraventricular arrhythmia to review the role of transesophageal overdrive pacing in the interruption of tachycardia. In these cases depend on clinical features such as pregnancy, and resistance to antiarrhythmic drugs that make them difficult to treat.
Case: Case 1: A 30‐year‐old female with a primary pregnancy in 17 weeks was admitted emergency for palpitations, her blood pressure was 90/60 mmHg, heart rate was 180 bpm with narrow QRS complex. She has not got any medical history. That time after Covid‐19 pandemic, we did not got any anti‐arrhythmic drugs, except direct current cardiac shock.
Case 2: A 26‐year‐old female was admitted emergency for palpitations, her heart rate was 178 bpm with narrow QRS complex, blood pressure was 110/70 mmHg, none of medical history. At the emergency department, she was bolus intravenous with a full dose of adenosine but not interrupt tachycardia.
Decision‐making: These cases were converted by transesophageal overdrive atrial pacing and reversed to sinus rhythm.
Conclusion: Transesophageal overdrive atrial pacing is a low‐cost, simple and safe procedure that can be performed at the bedside and can do many times, especially in patients, whose condition makes difficult the usage of medicines.

CS‐607‐CAR
Short coupled PVC induced torsade de pointes and VF
Ramdeo Yadave
Batra Hospital, Delhi, India
Sixty nine year old female underwent SOL lesion surgery of brain 3 months back presented with history of recurrent syncope.
She underwent Echo which showed no RWMA and LVEF 60%.
CAG showed normal coronaries. Electrolytes were within normal range.
Twenty‐four hours Holter showed short coupled VPCs induced TDP Polymorphic VT and VF spontaneously recovering to NSR.
Her baseline ECG is normal without QT prolongation.
She was admitted in CCU where she is having recurrent cardiac arrest nine times requiring cardiac defibrillation.
Monitor during cardiac arrest showed VF.
Summary and Conclusion: She received about 50 DC cardioversion in CCU in 2 days time. Failed with all the initial antiarrhythmic drugs such as Amiodarone, Betablocker, and Maxilletine and Lidocaine IV.
Therefore did Vascular US guided Bupivacaine inj of Left stellate ganglion which led to stoppage of any VT or VF and even short coupled VPCs.
Started high dose Verapamil 80 mg six hourly daily along with 150 mg of Flecainide twice daily.
Then I put her Dual chamber ICD and discharged within 2 days.
CS‐609‐CAR
Moderator band VT and VF
Ramdeo Yadave
Batra Hospital, Delhi, India
Thirty two year old male presented with recurrent pre‐syncope and palpitations.
ECG showed VPCs with LBBB and LAD with late transition after V4.
Twenty‐four hours Holter showed frequent VPCs and NSVT and couplets and triplets with 42% VPCs load.
Echo showed structurally and functionally normal heart.
MRI of heart showed no late gadolinium enhancement.
PET CT was done by Dr. Narsimhan Sir. which was normal.
Put on Amiodarone 200 twice daily along with Metoprolol 25 mg twice daily.
Repeat Holter after 3 weeks of medications VPCs reduced to 5%.
ECG showed VPCs with LBBB and LAD with late transition after V4.
Twenty‐four hours Holter showed frequent VPCs and NSVT and couplets and triplets with 42% VPCs load.
Echo showed structurally and functionally normal heart.
MRI of heart showed no late gadolinium enhancement.
PET CT was done by Dr. Narsimhan Sir. which was normal.
Put on Amiodarone 200 twice daily along with Metoprolol 25 mg twice daily.
Repeat Holter after 3 weeks of medications VPCs reduced to 5%.
Summary and Conclusion: The morphology of VPCs suggestive of Moderator band VT. This may degenerate to VF.
ICD should be recommended for this.
This VT can be ablated from either septal part of moderator band or lateral part of it at the attachment of MB to anterior papillary muscle of RV.
This patient ultimately received ICD for documented reversible VF.
He will need Ablation of VPCs again if he will get recurrent shock.
CS‐618‐CAR
Symptomatic bradycardia from sinus node disease in an elderly patient with myasthenia gravis
Mark Adorada
Philippine Heart Center, Quezon City, Philippines
Background: Symptomatic bradycardia attributed from sinus node disease as predominant cardiac manifestation in patients with Myasthenia Gravis is rarely reported.
Case: A 65‐year old female patient diagnosed with Myasthenia Gravis (MG), maintained on Pyridostigmine and Azathioprine, presented with symptomatic bradycardia complaining of persistent non‐rotatory dizziness and near‐syncope prompting hospital admission. Baseline 12‐L ECG showed sinus bradycardia. Holter monitoring revealed sinus pauses matched with clinical evidence of chronotropic incompetence. After thorough evaluation was made, patient underwent dual chamber permanent pacemaker implantation with dramatic clinical improvement.
Decision‐making: Myasthenia patients may experience varied symptomatology including wide fluctuations in heart rate and blood pressure. Clinical dilemma recognized if sinus node disease experienced by the patient was part of the autoimmune disorder or a separate entity that has to be addressed individually. On the other hand, intake of anticholinesterase as treatment for MG may also cause bradycardia but rarely reported to produce clinical symptoms based on literature. Overlap of manifestations such as fatigue, dyspnea and poor exercise intolerance between MG and cardiac disease may lead to under recognition of underlying cardiac problem. Permanent pacing was justified due to: (1) presence of symptomatic bradycardia, (2) in patient who developed symptomatic bradycardia as a consequence of guideline‐directed therapy for which continued treatment is warranted to increase heart rate and improve symptoms.
Conclusion: Symptom overlap with an autoimmune disorder may result in failure to recognize underlying cardiac manifestation. Conduction system disorder such as sinus node dysfunction is rarely encountered in Myasthenia patients.
CS‐640‐CAR
A case of LMNA‐related atrial cardiomyopathy
Yuxi Wang; Wenjie Yu; Pingzhen Yang
Zhujiang Hospital, Guangzhou, China
Background: Atrial arrhythmia in young people may be associated with atrial cardiomyopathy and muscular dystrophy.
Case: A 29‐year‐old man presented to our department complaining of palpitation for a year. 12‐lead ECG showed atrial flutter (A). He was otherwise healthy but with a unique gait of toe walking. Troponin‐T and creatine kinase were elevated. Due to his abnormal gait and lab test results, a genetic test was performed which revealed LMNA‐gene mutation, a mutation associated with muscular dystrophy.
Decision‐making: An electrophysiology study was scheduled and the bipolar voltage map showed extremely low voltage throughout the posterior wall of RA, which confirmed the diagnosis of atrial cardiomyopathy (B). Sinus rhythm was restored after cardioversion which showed a separated P wave (C), suggesting relatively slow conduction within the atria.
Conclusion: Early onset atrial arrhythmia may be the initial presentation of muscular dystrophy; thus appropriate assessment may help to uncover the primary cause.

CS‐645‐CAR
Serial electrocardiographic changes during provocative testing with low dose oral flecainide in a patient with suspected Brugada syndrome
Iznaeny Rahma 1,2; Muzakkir Amir1,2
1Department of Cardiology and Vascular Medicine, Faculty of Medicine, University of Hasanuddin, Makassar, Indonesia; 2Wahidin Sudirohusodo Hospital, Makassar, Indonesia
Background: Brugada syndrome (BrS) is characterized by coved ST‐segment elevation (STE) in right precordial leads that predisposes to sudden cardiac death (SCD). The electrocardiographic (ECG) signature is dynamic and often concealed but can be unmasked by potent sodium channel blockers such as Flecainide.
Case: A 21‐year‐old asymptomatic man was referred to our clinic as part of army education recruitment medical check‐up. His electrocardiography (ECG) showed saddle‐back STE in V2, suggestive of Brugada pattern. Family history of BrS was unknown and the physical examination was unremarkable.
Decision Making: Due to limited resources, we performed provocative testing using lower‐dose oral Flecainide (300 mg) to clarify the diagnosis. The result was positive with coved STE developed in leads V1–V3 30 min after drug administration and reached maximal positivity at 3.5 h (Figure 1).
Conclusion: Provocative testing with low dose oral flecainide is an effective alternative method to unmask type‐1 Brugada ECG.

CS‐650‐CAR
Ganglionic plexus ablation in the management of long QT syndrome
Yuxi Wang; Pingzhen Yang
Zhujiang Hospital, Guangzhou, China
Background: Ganglionic plexus ablation in combination with beta‐blockers may be a novel approach in the management of LQTS.
Case: A 25‐year‐old female patient with genetic test confirmed LQT2 who refused any form of electronic device insertion and surgical sympathectomy. Base line ECG showed QTc of 6 of 593 ± 11 ms (A). Beta‐blocker administration failed to effectively eradicate arrhythmia episodes as her symptom including syncope, palpitation and dyspnea appeared increasingly frequent.
Decision‐making: We performed anterior right GP ablation from the aspect of both superior vena cava and left atrium (B). After the ablation procedure, QT interval of this patient shortened to 450 ± 10 ms as expected with increased heart rate (C). Combined with maximally tolerated beta blockers, this patient reported no episodes of syncope and revealed stable shortened QT interval at follow‐up.
Conclusion: GP ablation with beta‐blocker use proved to be a promising approach in shortening QT interval and decreasing the risk to develop fatal arrhythmia in congenital LQTS.

CS‐666‐CAR
Ventricular standstill as a lethal consequence of aortic valve endocarditis
Dion Setiawan; Valerinna Yogibuana; Cholid Tri Tjahjono; Ardian Rizal
Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Brawijaya, Malang, Indonesia
Background: Infective endocarditis is associated with myocardial abscesses leading to conduction abnormalities. Ventricular standstill is when the heart experiences absent ventricular activity despite normal atrial functioning. We present a case of aortic valve endocarditis with myocardial abscess. The patient experienced episodes of ventricular standstill accompanied by loss of consciousness, requiring implantation of a pacemaker.
Case: A 38‐year‐old male with a history of rheumatic heart disease came with persistent shortness of breath. On arrival, he appeared feverish and cachectic. Physical examination revealed an early diastolic murmur at the right parasternal border. Laboratory tests revealed leukocytosis, increased C‐reactive protein level, and a positive rheumatoid factor. Electrocardiogram (ECG) showed sinus rhythm with first‐degree atrioventricular (AV) block, and an echocardiogram revealed vegetation at the aortic valve, along with interventricular septum and annular aortic abscess. Repeat blood cultures grew Streptococcus gordonii. After 14 days of antibiotic treatment, blood cultures showed a negative result, and fever and shortness of breath resolved. The next day, his ECG monitor showed episodes of P waves without accompanying QRS complexes. He experienced loss of consciousness, and his condition rapidly deteriorated. He is in cardiac arrest before we can implant a temporary pacemaker.
Decision‐making: Aortic valve endocarditis is associated with conduction abnormalities due to its proximity to the AV‐node. Therefore, daily ECGs are warranted in patients with aortic valve endocarditis.
Conclusion: Implantation of pacemaker should not be delayed if hemodynamically unstable arrhythmias are found. Early surgical intervention is necessary.

CS‐711‐CAR
Low‐dose flecainide as an alternative in Brugada syndrome provocative test: A case report
Nooryasni Muchlis 1; Muzakkir Amir1,2
1Department of Cardiology and Vascular Medicine, Faculty of Medicine, Hasanuddin University, Makassar, Indonesia; 2Dr. Wahidin Sudirohusodo Hospital, Makassar, Indonesia
Background: Brugada syndrome (BrS) is a genetic disorder that predisposes life‐threatening heart rhythm abnormalities, which can be suspected through a provocative test. The clinical utility of low‐dose flecainide 300 mg as a provocative test was proven in previous studies, while the early consensus recommends oral flecainide 400 mg.
Case: A 51‐year‐old man was diagnosed with pulseless ventricular tachycardia and got 200 J defibrillation. Hypertension and Smoking were coronary risk factors. Coronary angiography (CAG) was performed and showed no significant stenosis. Besides, an electrophysiology study was also performed with no inducible tachyarrhythmias and normal function of the sinoatrial node and the atrioventricular node.
Decision‐making: Normal CAG and nodes function led us to undergo provocative testing. Even though the early consensus recommended the only oral dose for this test is flecainide 400 mg, we decide using a low dose of flecainide 300 mg according to previous case reports that succeeded in unmasking the electrocardiographic pattern of Brugada. Our consideration was its limitation of availability in our center. During the provocative test, the development of Saddle Back Type ST elevation in V1 and V2 (upper right‐sided lead) in the 30th minute gradually increased without premature ventricular beats or another arrhythmia.
Conclusion: Whereas some studies show the effectiveness of 400 mg oral flecainide, using a low‐dose of flecainide 300 mg is an effective alternative method if there is any limitation of its availability. This case report supports the previous studies that using a low‐dose of flecainide as provocative testing is an alternative if intravenous drug preparation is unavailable.
CS‐713‐CAR
Potential effects of artemisin as an anti‐arrhythmic drug in a 23‐year‐old man with Brugada syndrome and malaria
Ahmad Thotuching; Muzakkir Amir
Unhas, Makassar, Indonesia
Background: Since Brugada syndrome was first described by the Brugada brothers in 1992, extensive studies have been conducted on this disease's pathophysiology, clinical manifestation, natural course, and risk stratification. Jeong et al. reported that artemisinin effectively suppressed ventricular tachyarrhythmia and recovered the action potential dome of the right ventricular epicardium in canine experimental model.
Case: A 23‐year‐old man came with complaints of palpitations for the last 4 months accompanied by syncope. He also complained of fever since a week before admission. The patient had a history of malaria while on duty in Papua, an endemic area of malaria, around 1 year before admission. On clinical examination the suspicion led to the diagnosis of Brugada syndrome. Provocation test was performed with flecainide 300 mg orally. Then, flecainide provocative test showed a positive result.
Decision Making: We decided to administer our patient with Artemisinin‐based Combination Therapies for Malaria. After administration of therapy, the patient reported no palpitations nor syncope attacks. However, we decided to implant an Implantable Cardioverter Defibrillator to prevent sudden death in our patient with symptomatic Brugada syndrome.
Conclusion: Our case showed that artemisinin could be an effective treatment option for Brugada Syndrome. However, Implantable cardioverter defibrillator is the mainstay of therapy to prevent sudden death in Brugada syndrome.

CS‐715‐CAR
Dangerous precursors of Torsades de pointes
Zhenyu Dong; Yanmei Lu; Baopeng Tang
The First Affiliated Hospital of Xinjiang Medical University, China
This case report describes a young woman with recurrent syncope who was diagnosed with Takotsubo cardiomyopathy. The patient presented with prolonged QT interval and T‐wave humps on electrocardiogram (ECG), indicating an increased risk of Torsades de Pointes (TdP) arrhythmia. The ECG also revealed macrovolt T‐wave alternans. The patient experienced syncope while hospitalized, and TdP was observed on ECG monitoring, leading to immediate electrical cardioversion. Treatment included intravenous magnesium sulfate, potassium chloride, and Lidocaine. Echocardiography showed left ventricular hypokinesis, supporting the diagnosis of Takotsubo cardiomyopathy. After symptomatic treatment, the patient's symptoms improved, and follow‐up ECG and ultrasound returned to normal. T‐wave humps are associated with sympathetic nerve overactivation and early afterdepolarizations, indicating an increased risk of arrhythmias. Physicians should be aware of this ECG pattern in patients with Takotsubo cardiomyopathy.

CS‐721‐CAR
A rare case of giant cardiac mass manifesting as palpitations: A diagnostic challenge
Zhenyu Dong; Yanmei Lu; Baopeng Tang
The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
We present a rare case of a 30‐year‐old woman who presented with a 1‐month history of dyspnea and palpitations. The patient had a history of hepatic echinococcosis resection at the age of 9, but was otherwise healthy. Electrocardiogram findings indicated atrial fibrillation. Contrast‐enhanced CT revealed a massive pericardial mass measuring 10 cm × 9.8 cm, with peripheral curvilinear wall calcification surrounding the non‐enhancing mass. The patient underwent successful tumor resection, and subsequent pathology reports confirmed the presence of echinococcosis. While the liver is the most commonly affected organ in hydatid disease, cardiac involvement is a rare variant, accounting for only 0.5%–2% of cases. Clinical manifestations of cardiac echinococcosis can vary from asymptomatic to severe cardiac failure. Therefore, cardiac echinococcosis should be considered as a differential diagnosis in patients with hepatic echinococcosis presenting with cardiac masses. At the 7‐year follow‐up, the patient showed excellent recovery.
figure.jpg (could not be inserted).
CS‐727‐CAR
Nonsustained ventricular tachycardia in acute myocarditis mimicking myocardial infarction
Marie Aisen Kathrina Cabujat‐Bumanglag; Frederick Philip Gloria; Jhobeleen De Leon; Tam Adrian Aya‐Ay; Paulo Gabriel Godisan; Chelsea Colleen Paris
Philippine General Hospital, Manila, Philippines
Myocarditis is a challenging diagnosis due to the diverse range of clinical presentations including non‐sustained ventricular tachycardia, which is associated with increased cardiovascular mortality.
This case report describes a case of a 31‐year‐old male without comorbidities presenting with new onset chest pain, ST elevation on II, III, aVF, V3–V6, and premature ventricular complexes on ECG.
He eventually developed non‐sustained monomorphic ventricular tachycardia, hence given Amiodarone, and later on shifted to Lidocaine. Coronary angiogram revealed angiographically normal arteries. Echocardiography showed multisegmental wall motion abnormalities with mildly depressed ejection fraction. Cardiac MRI demonstrated myocardial edema, hyperemia and non‐ischemic late gadolinium enhancement in characteristic regions of the left ventricle, fulfilling three out of three of the Lake Louise criteria for acute myocarditis. Viral panel showed negative results, while thyroid function tests showed elevated FT4 and low TSH. Patient was sent home on Carvedilol, Colchicine, and Methimazole. There was no recurrence of the ventricular arrhythmia on follow‐up. He was monitored for symptomatic and hemodynamically tolerated ventricular arrhythmia in the chronic phase, as this would necessitate secondary prevention of sudden cardiac death.
Acute myocarditis can present with life‐threatening arrhythmias and must be considered in young adults presenting with chest pain. Key principles of management include arrhythmia control, heart failure management, and treatment of underlying condition. Antiarrhythmics may be used in the acute phase; however, its efficacy in chronic myocarditis may be limited. Monitoring for recurrence of ventricular arrhythmia is therefore crucial to assess the need for device implantation.
CS‐733‐CAR
A 51‐year‐old man with cardioinhibitory syncope: How to diagnose?
Mezly Hetharia; Muzakkir Amir
Unhas, Makassar, Indonesia; Department of Cardiology and Vascular Medicine, Faculty of Medicine, University of Hasanuddin. Dr. Wahidin Sudirohusodo General Hospital, Makassar
Background: Tilt Table Testing is recognized as a valuable diagnostic tool for the identification of patients with unknown origin syncope. The type of response to tilt‐testing could guide patient management. However, the proper management for patients with cardioinhibitory syncope with asystole has been the subject of much debate.
Case: A 51‐year‐old man patient was admitted to the hospital with a history of syncope after prolonged standing. It was not preceded by any prodromal symptoms. Vital signs and physical examination showed normal results. Electrocardiogram showed atrial fibrillation normoventricular response. Tilt table test was performed in our patient and showed significant decrease in blood pressure up to 55/40 mmHg and heart rate up to 32 times/min which followed immediately by asystole for ±5 s resulting in syncope.
Decision Making: The patient was diagnosed with cardioinhibitory syncope type 2B. Holter monitoring showed episodes of second degree‐sinoatrial exit block type I and bradycardia‐tachycardia. Then, We decided to implant dual chamber pacemaker to prevent recurrence of syncope.
Conclusion: Tilt table test remains a valid cornerstone test modality for syncope and should be considered in patients that have had several unexplained falls. However, Cardiac pacing is the most effective therapy to prevent syncopal recurrences when syncope is due to documented bradycardia.

CS‐734‐CAR
Atrioventricular synchronous leadless pacemaker‐induced takotsubo cardiomyopathy: A rare complication
Koji Sudo; Kenji Kuroki; Chisa Asahina; Yuya Tanaka; Akira Sato
University of Yamanashi, Yamanashi, Japan
Takotsubo cardiomyopathy (TCM) is showing a transient cardiomyopathy with typical form of left ventricular apical ballooning with ST elevation in 12‐lead electrocardiogram (ECG). An 84‐year‐old woman was referred to our hospital for consideration of permanent pacemaker implantation because of complete atrioventricular block with heart failure. Therefore, we performed an atrioventricular synchronous leadless pacemaker implantation. The day after implantation, 12‐lead ECG showed negative T wave (A), and transthoracic echocardiography revealed apical wall hypokinesis (B). A coronary computed tomography showed no significant stenotic lesions in the coronary arteries. In addition, myocardial scintigraphy with dual nuclides showed TCM pattern (C). Echocardiography performed 30‐day after discharge revealed that the LV systolic function had improved to 68% without heart failure. TCM induced by leadless pacemaker implantation is a rare case. Although spontaneous recovery is generally expected, it could be necessary to recognize that this is one of the complications of leadless pacemaker implantation.

CS‐738‐CAR
Brash syndrome: An often overlooked condition in elderly patient
Andriany Qanitha 1,2; Muzakkir Amir1
1Department of Cardiology and Vascular Medicine, Faculty of Medicine, Universitas Hasanuddin, Makassar, Indonesia; 2Department of physiology, Faculty of Medicine, Universitas Hasanuddin, Makassar, Indonesia
Background: BRASH syndrome is a relatively newly recognized and under‐reported clinical entity characterized by bradycardia, renal dysfunction, atrioventricular node blocking agent (AVNB), shock, and hyperkalemia. We report a case of BRASH syndrome that was resistant to usual medical treatment and necessitated transvenous pacing, and vasopressor support.
Case: A 79‐year‐old male with hypertension treated with bisoprolol, chronic kidney disease stage 4, and atrial fibrillation presented to the hospital due to shortness of breath, lethargy, and weakness experienced over the past 2 days, which gradually worsened into shock. The patient exhibited symptomatic bradycardia with an irregular heart rate (HR) of 34 BPM. Initial laboratory results indicated renal impairment, hyperkalemia, anemia, and thrombocytopenia. The initial ECG revealed atrial fibrillation slow ventricular rhythm, with an average HR of 30 BMP, ICLBBB, and extensive anterior wall ischemia. A chest X‐ray showed cardiomegaly, atherosclerosis of the aorta, and bilateral pleural effusion. Transthoracic echocardiogram showed normal systolic and diastolic function, along with moderate mitral regurgitation. The BRASH syndrome describes a consequential cycle in which the atrioventricular node blocking (AVNB) agent induces bradycardia and hyperkalemia. Consequently, this cycle results in decreased cardiac output and renal hypoperfusion.
Decision‐making: Permanent transvenous pacemaker was placed due to persistent bradycardia with hemodynamic instability. Vasoactive medications and potassium‐lowering medicines were administered. Renal function improved, and the heart rate stabilized at 70 beats per minute (bpm).
Conclusion: Prompt diagnosis and appropriate management involving the use of a transvenous pacemaker and measures to improve renal function are essential to improve BRASH outcomes in elderly.
CS‐781‐CAR
An orthodox case presentation—The mystery of conducted premature atrial contraction in 2:1 conduction atrioventricular block: Phase 4 block or gap phenomenon?
Muhammad Rizky Felani 1; Fajar Hamonangan Panjaitan1; Dony Yugo Hermanto2; Sunu Budhi Raharjo2; Dicky Armein Hanafy2; Yoga Yuniadi2
1Cardiology Resident (NCCHK), Palembang, Indonesia; 2Staff of Arrhythmia Division, Cardiology and Vascular Department, National Cardiovascular Center Harapan Kita (NCCHK), Jakarta, Indonesia
Background: Permanent pacemaker implantation for 2:1 atrioventricular block (AVB) is based on block location and symptom. Infrahisian block is a strong indication for pacemaker implantation.
Case Illustration: A 69‐year‐old male patient with long standing hypertension came to emergency department of National Cardiovascular Center Harapan Kita (NCCHK) due to recurrent dizziness and easily fatigue. Electrocardiography revealed bradycardia with 2:1 AVB.
Decision Making: During holter recordings, every premature atrial contraction (PAC) could be conducted to the ventricle. This phenomenon seemed odd in 2:1 AVB. The most possible underlying mechanism for this condition might be related to the phase 4 block that happened within the his‐purkinje system (HPS). Phase 4 block allows shorter P wave cycle length to be conducted while blocking the longer one, caused by a drift in resting membrane potential. This phenomenon usually happens in HPS disease. Another possible mechanism is gap phenomenon, a prolongation in proximal conduction in AV node, although it seems unlikely to be the cause in our case. Atropine test showed acceleration of P wave without any improvement in AV nodal conduction, thus the diagnosis was infrahisian block. Electrophysiology (EP) study still need to be done to discover the orthodox phenomena of this infrahisian block finding and pacemaker implantation for its definitive treatment.
Summary: Holter ECG allowed for diagnosis of an infrahisian block and atropine test as a part of more accurate diagnostic approach proved that the mechanism of the AVB was due to HPS disease.
Keywords: 2:1 AV block, atrial premature contraction, infrahisian block.

CS‐788‐CAR
Brugada syndrome and hypokalemia: The deadly duet
Kinanti Pravdani
Brugada syndrome is a cause of sudden death among young adults. Here, we present a case of Brugada syndrome with severe hypokalemia leading to cardiac arrest.
A 21‐year‐old woman presented to the hospital with weakness, profuse watery diarrhea, nausea and vomiting. Her late brother died from sudden death at 23 years old. She denied previous syncope or palpitations episodes. She has a fever with tetraparesis with 4/5 strength in all extremities.
Laboratory results showed leukocytosis, hyponatremia, and severe hypokalemia 1.31 mmol/L, with a normal‐sized heart from chest X‐ray.
ECG revealed normal sinus rhythm with RBBB‐type ST elevation on V1 consistent with type 1 Brugada pattern and ST depression in V2–V6 and a long QT interval of 560 ms.
She was then admitted to intermediate care and given IVFD, potassium replacement, antibiotics, and antidiarrheal drugs, while awaiting referral for AICD placement. Within 6 h of admission, she became unresponsive and developed ventricular fibrillation (VF). She was resuscitated and intubated. She underwent multiple cardiac arrest (four times) within the hour. ECG showed ventricular tachycardia and asystole all over again. Despite attempted CPR and defibrillation, the patient died.
Patients with distinct Brugada pattern with concomitant severe hypokalemia should be given immediate potassium replacement. Otherwise AICD placement is the sole effective method for averting sudden cardiac death from VT.
The combination of Brugada syndrome and severe hypokalemia poses a life‐threatening condition that must be treated immediately. It is essential to carefully consider the limited resources available and the urgency required in handling these cases.
CS‐809‐CAR
Ventricular tachycardia in a young man with symptoms of angina and an ischemic ECG: Is it always acute coronary syndrome?
Lutfi Hafiz Zunardi 1; Ardian Rizal1,2; Mohammad Saifur Rohman1,2
1Saiful Anwar General Hospital, Malang, Indonesia, Malang, Indonesia; 2Department of Cardiology and Vascular Medicine, Faculty of Medicine, Brawijaya University, Malang, Indonesia
Background: Ventricular tachycardia (VT), a potentially fatal arrhythmia, is the primary cause of sudden cardiac fatalities. Ischemic heart disease is the underlying condition that most frequently causes ventricular tachycardia. Understanding the pathogenesis of VT and underlying structural heart disease is crucial for the proper management of VT and the avoidance of sudden cardiac death. The ability to differentiate between the many types and causes and to treat them correctly is a critical competency for emergency physicians.
Case Illustration: A 33‐year‐old man, a smoker, was brought to the emergency department presenting with acute onset Angina, hypotension, cold acral and decrease of consciousness. ECG shows signs of VT. The patient was assessed as suspected of ACS. The patient was managed successfully with electrical Cardioversion, and continuous with amiodarone I. Patient reverted to sinus rhythm with T inverted. Patient was given O2, IV fluid, tab Aspilet (300 mg), clopidogrel (300 mg). With these interventions used in quick succession, the patient was reversed to hemodynamic stability, did not have further episodes of VT. patient was assessed with very high‐risk NSTACS criteria. The patient underwent immediate invasive coronary angiography (ICA) with minor disease.
Conclusion: Patients with clinical angina and an ischemic ECG suggestive of ACS are at high risk for VT, but the fact is that ACS or IHD are not always the cause of VT. The underlying cause must be investigated further after acute termination. Even if ICA show that coronary arteries are normal, a confirmation diagnosis may require an invasive electrophysiological examination.
CS‐837‐CAR
Appearances are deceptive: Heart failure with LBBB: CRT or EP STUDY?
Suresh Allamsetty
1Medicover Hospitals MVP Branch, Visakhapatnam, India; 2Apollo Hospital, Visakhapatnam, India
Background: Arrhythmic etiology must be ruled out in a patient with heart failure.
Case: A 40 years old male presented with shortness of breath class III since 3 months. ECG showed LBBB (Figure 1). Echo was suggestive of global LV Hypokinesia and severe LV dysfunction. As he had heart failure inspite of taking GDMT, he was advised CRT P/D implantation elsewhere.
Decision Making: ECG showed short PR interval. Hence without going for CRT implantation, patient was taken up for EP study. AVRT was easily induced and RFA of parahisian pathway was done successfully. Post RFA the LV ejection fraction improved. After 1 month of RFA patient had normal LV systolic function.
Conclusion: High index of suspicion is required in a patient with heart failure to rule out arrhythmia induced arrhythmia induced cardiomyopathy given the potential of LV recovery. An aggressive proactive approach to arrhythmia treatment is required in Cardiomyopathy.

CS‐870‐CAR
Massive atrial thrombus dislodgement in patients with atrial fibrillation—A scary and deadly risk
Jiasuoer Xiaokereti; Baopeng Tang
The First Affiliated Hospital of Xinjiang Medical University, Department of Cardiac Electrophysiology, Urumqi, China
A 77‐year‐old female was admitted with a complaint of persistent bilateral lower extremity pain for 3 h, accompanied by slight numbness in both lower extremities and limited walking. The patient was diagnosed with “persistent atrial fibrillation with a large left atrial thrombus (44 × 36 mm, Figure A, B)” 1 month ago. The emergency vascular ultrasound indicating thrombosis of the lower abdominal aorta, and no significant blood flow signal was seen in the lumen of the bilateral iliac arteries, external iliac arteries, posterior tibial arteries, and left anterior tibial artery (Figure C–G). On the same day, percutaneous abdominal aortic thrombectomy was performed. During the operation, both femoral arteries were freed, the wall of the common femoral artery was cut transversely, and an arterial thrombectomy catheter was placed into the proximal end of the artery, but the thrombus was not removed after repeated thrombectomy. A 5F sheath was placed in the femoral artery, and two balloons were placed in the sheath to dilate the occluded segment of the abdominal aorta at the same time (Figure H–K). One week after the operation, the patient's pain in both lower extremities was still not relieved, and considering the insufficient blood supply to the distal lower extremities. Therefore, abdominal aortic embolization was performed. The postoperative pathological analysis indicated that the mass was an intra‐arterial thrombus (Figure C).



