Abstract
The CURB-65 (confusion, uremia, respiratory rate, blood pressure, age ≥ 65 years) score and the pneumonia severity index (PSI) are widely used and recommended in predicting 30-day mortality and the need for intensive care support in community-acquired pneumonia. This study aims to compare the performance of these two severity scores in both mortality prediction and the need for intensive care support. A systematic review and meta-analysis was carried out, following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) 2020 guidelines, and PubMed, Scopus, ScienceDirect, and Google Scholar were searched for articles published from 2012 to 2022. The reference lists of the included studies were also searched to retrieve possible additional studies. Twenty-five studies reporting prognostic information for CURB 65 and PSI were identified. ReviewManager (RevMan) 5.4.1 was used to produce risk ratios, and a random effects model was used to pool them. Both PSI and CURB-65 showed a high strength in identifying high-risk patients. However, CURB-65 was slightly better in early mortality prediction and had more sensitivity (96.7%) and specificity (89.3%) in predicting admission to intensive care support. Thus, CURB-65 seems to be the preferred tool in predicting mortality and the need for admission into intensive care support.
Keywords: psi criteria for pneumonia, methodological quality assessment, prognostic scoring methods, community-acquired pneumonia, systematic review and meta analysis, icu, mortality, curb 65, pneumonia severity index
Introduction and background
The CURB-65 (confusion, uremia, respiratory rate, blood pressure, age ≥ 65 years) score and the pneumonia severity index (PSI) are widely used in predicting 30-day mortality and the need for intensive care support in community-acquired pneumonia (CAP) [1]. As optimal care necessitates quick diagnosis of very ill patients and proper emphasis on hospital admission and ICU admission, prognostic scoring methods for CAP were established to evaluate the severity of the disease and categorize patients based on mortality risk [2].
Severity assessment methods have been created to direct treatment locations for patients with CAP and, in particular, identify individuals whose illness may be safely treated at home [3]. Moreover, the discovery of coronavirus disease 2019 (COVID-19) led to the use of these severity scores in stratifying COVID-19 patients into low-risk or high-risk at the time of hospital admission [4,5]. The PSI and CURB-65 are the two most widely used of these tools. Both products were created using statistical analysis of characteristics linked to 30-day mortality [3,6]. Such characteristics are translated into a severity score representing the patient's mortality risk and can be used to determine whether inpatient or outpatient care is best. Although 30-day mortality is undoubtedly significant, most CAP patients who pass away are older people with multiple comorbidities [7]. These challenges may be overcome by offering a reliable, validated classification of patients into low, middle, and high-risk groups based on severity scores.
The PSI, also known as the pneumonia Patient Outcomes Research Team (PORT) score, has been the subject of the most research. It was created in 1997 due to a study involving more than 50 000 CAP patients [8]. Patients were divided into five risk categories (I-V) using a 20-point scoring system based on their percentage risk of passing away within 30 days, as presented in Table 1.
Table 1. The 20-point scoring system .
| Class I (low risk) | Physical examination findings, no comorbidities or laboratory findings |
| Class II (low risk) | ≤70 points |
| Class III (low risk) | 71–90 points. |
| Class IV (moderate risk) | 91–130 points |
| Class V (high risk) | >130 total points |
Patients are then monitored according to their PSI/PORT results. Outpatient care is provided for patients with scores below 70. Patients who score between 71 and 90 may get outpatient care or be admitted for observation. Patients who score more than 90 must be admitted for optimal care, and those who score more than 130 should receive ICU therapy for the best results. The PSI has been used successfully in clinical practice to increase the use of outpatient treatment in CAP, and it is recommended by various national and international guidelines [9]. However, the PSI has its limitations. It is challenging to apply in a crowded emergency department due to the high number of factors which strongly weigh age and co-morbid diseases. Later, the Infectious Diseases Society of America advised using the PSI scoring system as a predictor for patients with community-acquired pneumonia [8].
The CURB-65 score, which gives one point each for confusion, urea >7 mM/L (19 mg/dL), respiration rate ≥ 30/min, systolic blood pressure < 90 mmHg, and/or diastolic blood pressure ≤ 60 mmHg, and age ≥ 65 yr, was developed by an international study carried out in Europe (Table 2) [10].
Table 2. CURB-65 score.
CURB-65: confusion, uremia, respiratory rate, blood pressure, age ≥ 65 years
| Variable | Value |
| Confusion | Mental Test Score ≤ 8, new disorientation in person, place or time |
| Urea | >7 mmol/L |
| Respiratory rate | ≥30/min |
| Blood pressure | Systolic < 90 mmHg, and/or diastolic ≤ 60 mmHg |
| Age | ≥ 65 years |
Since there are only five variables and one point is given for each, this score is much simpler to understand and apply than the PSI. To calculate the score, each parameter is worth one point, and 0 to 5 is the possible score. Patients with CURB-65 scores of 3 to 5 have a higher mortality risk than those scoring between 0 and 2 [9].
In addition to the PSI, CURB65 is now recommended by other national and international recommendations due to its widespread adoption. However, CURB-65 too has limitations. For instance, by dividing patients into only two categories (severe or non-severe), it fails to identify individuals with a low risk of mortality who would be good candidates for early hospital departure or home treatment. The CRB-65, a similar instrument not detecting blood urea, might also be applied in the community. In Europe, especially for hospitalized patients, the CRB-65 score is widely used and recommended for outpatient usage without monitoring blood urea [11].
Given patients’ low quality of life and prognosis, rigorous treatment in the intensive critical care unit is sometimes viewed as inappropriate when such patients are admitted to the hospital [12]. As a result, methods for forecasting mortality are more accurate than determining which patients will benefit from admission to the critical care unit.
Clinicians might exaggerate and understate the seriousness of CAP, making it challenging to determine which patients must be sent to the critical care unit. A significant part of healthcare costs is spent on patients admitted to the CCU [12]. Early identification of such patients could lead to better results, fewer incorrect non-admissions, and possibly shorter ICU stays. In addition, ICU admission criteria vary between countries and hospitals. Conflicting findings have been reported in studies comparing different scoring systems, with some believing the PSI to be superior [13] and others finding it has no advantage over CURB-65 [14]. According to studies using CRB-65, this more straightforward approach may be similar to PSI and CURB-65 for predicting 30-day mortality.
There are several articles on prognostic scales for various comorbidities. However, it is still unclear which one is better at predicting severity in terms of mortality and the requirement for ICU admission in hospitalized patients. This review was conducted to compare PSI and CURB-65 in the prediction of mortality and the need for intensive care support, evaluate the compatibility of these scores with other comorbidities, and determine which scoring system is better in both.
Review
Protocol and registration
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 guidelines [15]. We registered our protocol in the International Prospective Register of Systematic Reviews or PROSPERO.
Primary search
Three databases, PubMed/MEDLINE, Scopus, and ScienceDirect, were searched for relevant articles published between 2012 and October 2022 that presented information on mortality and the need for intensive care support concerning PSI and CURB-65 scores. A search string was developed for PubMed to conduct an e-databases search. The keyword search featured an all-text analysis to broaden the sensitivity of the search strategy. Our search was intended to capture articles presenting information on the comparative nature between PSI and CURB-65 scores on mortality and the need for intensive care support. The search strategies used for Scopus and ScienceDirect were slightly modified from the strategy used to search PubMed. The search string used in each database mentioned above is provided in Table 3.
Table 3. Search Strings .
| Database | Search string |
| PubMed | ("Pneumonia severity index" OR PSI OR "PORT Score") AND (CURB-65 OR ‘CURB 65’ OR ‘C.U.R.B.65’ OR ‘C-U-R-B-65’) AND (mortality OR death OR fatality OR dying OR carnage) AND (ICU OR "intensive care unit" OR "intensive treatment unit" OR "emergency unit" OR "critical care unit" OR "intensive therapy unit") |
| Scopus | (("Pneumonia severity index" OR PSI OR "PORT Score") AND (CURB-65 OR ‘CURB 65’ OR ‘C.U.R.B.65’ OR ‘C-U-R-B-65’) AND (mortality OR death OR fatality OR dying OR carnage) AND (ICU OR "intensive care unit" OR "intensive treatment unit" OR "emergency unit" OR "critical care unit" OR "intensive therapy unit")) AND PUBYEAR >1999 |
| ScienceDirect | ("Pneumonia severity index" OR PSI OR "PORT Score") AND (CURB-65 OR "CURB 65") AND (mortality OR death) AND (ICU OR "intensive care unit") |
Secondary search
In addition to the search conducted on the three databases, a direct search was done using the Google Scholar database. To allow the presentation of the most relevant results in the first pages, keywords representing mortality and Intensive care support (critical care unit, critical room, emergency unit, intensive treatment unit, loss of life, fatality, lethality, carnage, causality) were included in the search. The reference lists of the included studies were also searched for relevant additional articles.
Eligibility criteria
Two reviewers evaluated studies retrieved from the electronic databases using the inclusion and exclusion criteria. All studies had to meet the following pre-defined inclusion criteria: Original studies, including retrospective cohort studies, prospective cohort, and case-control studies; studies published in English; studies addressing mortality and the need for intensive unit support/admission, and presenting information for/of patients over 14 years of age. Studies that presented information of patients below 14 years of age were excluded. Studies that did not address mortality or the need for ICU but reported CURB 65 and PSI among CAP patients were excluded. Non-original articles like literature reviews, comments on published papers, letters to editors, conference papers, etc., non-peer reviewed, non-full text articles, and studies that did not report on any comparison between PSI and CURB 65 regarding mortality and ICU admission were excluded.
Review methods
Methodological Quality Assessment
The quality appraisal criteria used is a modification of the Newcastle-Ottawa Scale (NOS). The NOS was initially developed for cohort, case-control, and cross-sectional studies [16]. Hence, it had to be slightly modified to assess the quality of other study types. The criteria items and interpretation are described in Table 4.
Table 4. Criteria items and interpretation of quality assessment via Newcastle-Ottawa scale.
| Criteria | Description |
| Selection | Representativeness of the exposed cohort. Selection of the non-exposed cohort. Ascertainment of exposure. Demonstration that outcome of interest was not present at the start of the study. |
| Comparability | Comparability of cohorts based on design or analysis. |
| Outcome | Assessment of outcome. Was follow-up long enough for outcomes to occur. Adequacy of follow-up of cohorts. |
Data Extraction
Potentially eligible studies were individually screened using Zotero software. The selection featured a rigorous screening of titles, abstracts, and full texts. The full-text screening focused on presenting any form of data on the comparison between the PSI and CURB-65. After the selection of articles for inclusion, data was extracted into a predefined data descriptor table with the following fields: author, year of publication, country, study design (if presented), number of patients, age limit, mean age, mean duration of the hospital stay, mortality, sensitivity of PSI and CURB-65, and patients that were admitted in the ICU.
Synthesis of Results
Risk-of-bias appraisal was carried out through the robvis (Risk-Of-Bias VISualization) tool [17]. The heterogeneity was assessed across the included studies using a p-value and I2 statistics. A p-value having less than 0.10 was said to be evidence of heterogeneity. An I2 index between 50% and 70% was considered substantial heterogeneity, while an I2 value of more than 70% was regarded as the ultimate proof of study heterogeneity [18,19]. For calibration, the observed death rates from each trial were compared with the anticipated mortalities from the original derivation studies for PSI and CURB-65. The observed: and predicted risk ratios (RRs) are shown with 95% confidence intervals. The Review Manager (RevMan) Version 5.4 (2020; The Cochrane Collaboration) was used to produce RRs, and a random effects model was used to pool them. When the RR is more than 1, the observed mortality is more significant than predicted from the derivation study. An RR of less than 1 denotes that the number of deaths in the validation studies was lower than in the original derivation.
Results
Our search comparing PSI and CURB-65 retrieved 758 results from three primary databases. Of these, 122 articles were duplicates and were removed. Seven articles were removed because they were ineligible for inclusion as they did not contain any information on PSI and CURB-65 scores. The remaining articles were screened, and only 93 were sought for retrieval. We found no new additional articles for inclusion from Google Scholar and our search of the references of the included studies. The 93 articles were taken through the inclusion criteria, and only 25 studies were finally included in the review. Figure 1 represents the PRISMA flow chart summarizing the data screening procedure.
Figure 1. PRISMA flow chart illustrating the study selection procedure.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Quality Assessment Score
The quality assessment score according to the NOS is described in Table 5.
Table 5. Quality assessment score according to the Newcastle-Ottawa scale.
Selection: representativeness of studies (maximum score of 4); Comparability: comparability of studies based on the design or analysis or analysis (maximum score of 1); Outcome: assessment of outcome and follow-up (maximum score of 3); Studies with a total score of 6-8 were considered high quality while 1-5 were low-quality ones.
| Study ID | Selection | Comparability | Outcome | Total score |
| Alavi-Moghaddam et al., 2013 [20] | 4 | 1 | 3 | 8 |
| Ozkan et al., 2020 [21] | 4 | 1 | 3 | 8 |
| Bahlis et al., 2021 [2] | 4 | 1 | 3 | 8 |
| Ronda et al., 2021 [22] | 4 | 1 | 3 | 8 |
| Feng et al., 2021 [3] | 4 | 1 | 3 | 8 |
| Neto et al., 2021 [6] | 4 | 0 | 3 | 7 |
| Estella, 2015 [23] | 3 | 0 | 2 | 5 |
| Demirel, 2018 [24] | 1 | 1 | 3 | 5 |
| Holten et al., 2020 [25] | 4 | 1 | 3 | 8 |
| Olivia et al., 2021 [26] | 4 | 0 | 2 | 6 |
| Cupurdija et al., 2015 [27] | 4 | 1 | 3 | 8 |
| Anurag and Preetam, 2021 [5] | 4 | 1 | 3 | 8 |
| Ranzani et al., 2017 [28] | 4 | 1 | 2 | 7 |
| Günaydın et al., 2019 [29] | 4 | 0 | 3 | 7 |
| Tsai et al., 2021 [30] | 4 | 0 | 3 | 7 |
| Wen et al., 2020 [31] | 4 | 0 | 2 | 6 |
| Putot et al., 2016 [7] | 4 | 1 | 3 | 8 |
| Wang et al., 2020 [32] | 4 | 1 | 3 | 8 |
| Bloom et al., 2019 [33] | 4 | 0 | 1 | 5 |
| Williams et al., 2018 [34] | 4 | 0 | 3 | 7 |
| Kim et al., 2013 [10] | 4 | 1 | 2 | 7 |
| Aydin et al., 2019 [35] | 4 | 0 | 3 | 7 |
| Akpınar et al., 2019 [36] | 4 | 1 | 3 | 8 |
| Ito et al., 2017 [37] | 4 | 0 | 3 | 7 |
| Lee et al., 2013 [38] | 4 | 1 | 3 | 8 |
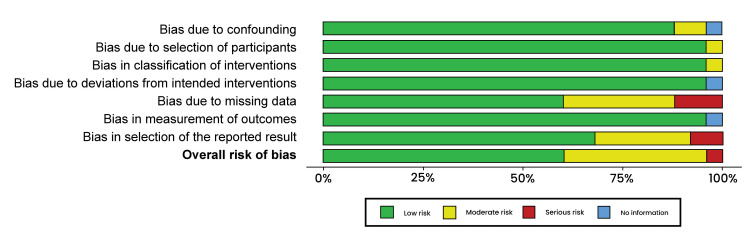
Risk-of-Bias Assessment
Non-randomized intervention studies were evaluated for risk of bias. Traffic light plots and summary plots were then generated (Figures 2, 3).
Figure 2. Traffic light plot.
Alavi-Moghaddam et al., 2013 [20], Ozkan et al., 2020 [21], Fuchs Bahlis et al., 2021 [2], Esteban Ronda et al., 2021 [22], Feng et al., 2021 [3], Lazar Neto et al., 2021 [6], Estella, 2015 [23], Demirel, 2018 [24], Holten et al., 2020 [25], Olivia et al., 2021 [26], Cupurdija et al., 2015 [27], Anurag and Preetam, 2021 [5], Ranzani et al., 2017 [28], Günaydın et al., 2019 [29], Tsai et al., 2021 [30], Wen et al., 2020 [31], Putot et al., 2016 [7], Wang et al., 2020 [32], Bloom et al., 2019 [33], Williams et al., 2018 [34], Kim et al., 2013 [10], Aydin et al., 2019 [35], Akpınar et al., 2019 [36], Ito et al., 2017 [37], Lee et al., 2013 [38]
Figure 3. Risk of bias summary.
Characteristics of Included Articles
All the studies were published between 2012 and 2021 and reported data from national registries gathered in different timelines (Table 6). There were nine retrospective studies, five prospective observational cohort studies, three studies were comparative, two population-based observational studies, and six were a combination of three prospective observational studies. The included studies covered a broad scope of countries across the globe. Out of 25 studies, only one study [5] did not report data comparing PSI and CURB-65 in mortality, and 19 studies [2,3,6,10,20-23,25,26,28,29,32-38] reported data on the need for intensive care support. The size of the studies varied from 24 patients [23] to up to 6874 in the cohort study of Spain [28]. Reported mortality rates varied from 4.5% to 44.72%. A few studies employed in-hospital mortality as their primary end measure, but most studies used 30-day mortality. Hospitalized patients made up the vast bulk of the included research. Most studies had a mix of inpatients and patients managed in the community. Alavi-Moghaddam et al. provided exhaustive data on the mortality rate and need for intensive care support, specificity, and sensitivity of both severity scores, PSI and CURB-65 [20]. This study was thus used as the data referencing point.
Table 6. Characteristics of included studies.
| Author and year | Study Design | Study region | Population | Age | Mean age | Mean duration of hospital stay | Mortality rate | sensitivity (PSI/CURB 65) | Need for ICU (PSI/CURB 65) |
| Alavi-Moghaddam et al., 2013 [20] | Observational comparative study | Iran | 200 | >18 years | 68 | 2-10.5 days | 36 died | 90%/96.7% | 52 patients (specificity: 78.7%/89.3%) |
| Ozkan et al., 2020 [21] | Comparative study | Turkey | 250 | > 18 years | 72.3 | 30 days | 27 died | 66.7%/88.9 | 80 patients |
| Fuchs Bahlis et al., 2021 [2] | Cohort Study | Brazil | 304 | ≥ 14 years | 67.1 | 7.2±7.4 days | 47 died | 3.7%/4.5% | 89 patients |
| Esteban Ronda et al., 2021 [22] | Retrospective observation study | Spain | 208 | ≥ 18 years | 63 | 6-13 days | 26 died | 84.62%/88.46% | 38 patients |
| Feng et al., 2021 [3] | Prospective cohort study | China | 239 | ≥ 18 years | 61.09 | 10 days | 22 died | - | 71 patients |
| Lazar Neto et al., 2021 [6] | Retrospective cohort study | Spain and Brazil | 1363 | ≥18 years | 61.05 | 7 days | 320 died | 59.9%/56.0% | 646 patients |
| Estella, 2015 [23] | Retrospective observation study | Spain | 24 | unspecified | unspecified | unspecified | 21.1% | CURB 65 scale of 1 (60%), 13.3% obtained 0 and 26.7% 2. PSI scale resulted class I in a 20%, class II 40%, 26.7% class IV, and 13.3% class V | 19 patients |
| Demirel, 2018 [24] | Prospective cross-sectional study | Turkey | unspecified | unspecified | 71±16.5 | unspecified | 21.8% | 90.9%/90.9% | unspecified |
| Holten et al., 2020 [25] | Prospective cohort study | Norway | 175 | ≥18 years | 59 | 14 days | 13 died | 71%/58% | 29 patients |
| Olivia et al., 2021 [26] | Retrospective single-center study | Italy | 224 | unspecified | unspecified | 28 days | 24 died | - | 26 patients |
| Cupurdija et al., 2015 [27] | Prospective cohort study | Serbia | 95 | ≥18 years | unspecified | 14 days | 5 died | 22%/29% | unspecified |
| Anurag & Preetam, 2021 [5] | Retrospective observational study | India | 122 | ≥11 years | 44.16 | 14 days | - | 47.6%/28.6% | unspecified |
| Ranzani et al., 2017 [28] | Cohort Study | Spain | 6874 | ≥18 years | 66.1 | 30 days | 442 died | 92%/78% | 950 patients |
| Günaydın et al., 2019 [29] | Case-control study | Turkey | 63 | ≥18 years | 72.05 | 30 days | 4 died | 85.2%/82.4% | 5 patients |
| Tsai et al., 2021 [30] | Retrospective cohort study | Australia | 203 | ≥18 years | unspecified | 30 days | 13 died | - | unspecified |
| Wen et al., 2020 [31] | Retrospective observational study | China | 223 | ≥18 years | unspecified | 30 days | 41 died | 66%/85% | unspecified |
| Putot et al., 2016 [7] | Retrospective cohort study | France | 217 | ≥75 years | unspecified | 1 year | 19.8% | 66%/58% | unspecified |
| Wang et al., 2020 [32] | Retrospective observational study | China | 123 | unspecified | unspecified | 180 days | 55 died | 8.1%/5.1% | 68 patients |
| Bloom et al., 2019 [33] | Comparative study | Germany | 276 | ≥60 years | unspecified | unspecified | unspecified | unspecified | 11 patients |
| Williams et al., 2018 [34] | Prospective cohort study | Australia | 618 | unspecified | unspecified | 30 days | 12.1% | 98%/94% | 75 patients |
| Kim et al., 2013 [10] | Prospective cohort study | Korea | 883 | ≥18 years | unspecified | 30 days | 40 died | 4.5%/2.3% | 80 patients |
| Aydin et al., 2019 [35] | Observational study | Turkey | 159 | ≥18 years | 66 | 28 days | 58 died | 8.6%/10.0% | 72 patients |
| Akpınar et al., 2019 [36] | Prospective observational study | Brazil | 155 | ≥18 years | 72.7 | 30 days | unspecified | 46.5%/36.1% | 42 patients |
| Ito et al., 2017 [37] | Prospective cohort study | Japan | 1834 | ≥15 years | 73.5 | 30 days | 122 died | 24.9%/17.9 | 95 patients |
| Lee et al., 2013 [38] | Comparative study | Korea | 208 | >65 years | 80 | 30 days | 21.1% | 40.0%/50.0% | 55 patients |
Results of Included Studies
Alavi-Moghaddam et al.’s study [20] was used to compare the data collected on the prediction of mortality and the need for ICU admission among patients from the other studies and as a data extraction guide for articles that generally focused on mortality. They established that the mortality was 18%, while the PSI and CURB 65 mortality/sensitivity predictions were 90% and 96.7%, respectively [20]. The mortality predictions were for the highest classes for both severity scores. These percentages showed that the patient's death was most likely. On the other hand, the prediction/specificity for ICU admission was 78.7% and 89.3%, respectively, for PSI and CURB 65 [20]. The CURB-65, however, seemed more specific in identifying the mortality risk in severe CAP. This study showed that 52 patients were admitted for critical care support. Eighteen studies were used in the meta-analysis to check the comparison of CURB 65 and PSI. The eighteen studies were further subdivided into two classes; the lowest class and the highest class. For PSI prediction, the lowest class was class I-II, while CURB 65 was class 0-1. As for the highest classes, PSI was class V, and CURB 65 was class 3-5. CURB-65 and PSI ratings both demonstrated a reasonable positive predictive value.
A comparison was made for the highest classes for both severity scores in 13 studies [6,7,20-22,25,27-29,31,34,37,38]. Ozkan et al.’s [21] study had 66.7%/88.9, Alavi-Moghaddam et al. [20] 96.7%/90%, Esteban Ronda et al. [22] 84.62%/88.46%, Lazar Neto et al. [6] 59.9%/56.0%, Holten et al. [25] 71%/58%, Cupurdija et al. [27] 22%/29%, Ranzani et al. [28] 92%/78%, Günaydın et al. [29] 85.2%/82.4%), Wen et al. [31] 66%/85%, Putot et al. [7] 66%/58%, Williams et al. [34], 98%/94%, Ito et al. [37] 24.9%/17.9, and Lee et al. [38] 40.0%/50.0% for PSI and CURB-65 mortality predictions, respectively. The mortality rate for PSI class V ranged from 60% to 96%. This meant there was a high likelihood of the death of patients. Using CURB-65 for the same articles, class 3-5 prediction was almost similar with slight differences, as shown in Figures 4, 5.
Figure 4. A forest plot of PSI scores risk ratios for class V.
PSI: Pneumonia Severity Index
Alavi-Moghaddam et al., 2013 [20], Ozkan et al., 2020 [21], Esteban Ronda et al., 2021 [22], Lazar Neto et al., 2021 [6], Holten et al., 2020 [25], Cupurdija et al., 2015 [27], Ranzani et al., 2017 [28], Günaydın et al., 2019 [29], Wen et al., 2020 [31], Putot et al., 2016 [7], Williams et al., 2018 [34], Ito et al., 2017 [37], Lee et al., 2013 [38]
Figure 5. A forest plot of CURB-65 score risk ratios for class 0-3.
Alavi-Moghaddam et al., 2013 [20], Ozkan et al., 2020 [21], Esteban Ronda et al., 2021 [22], Lazar Neto et al., 2021 [6], Holten et al., 2020 [25], Cupurdija et al., 2015 [27], Ranzani et al., 2017 [28], Günaydın et al., 2019 [29], Wen et al., 2020 [31], Putot et al., 2016 [7], Williams et al., 2018 [34], Ito et al., 2017 [37], Lee et al., 2013 [38]
CURB-65: confusion, uremia, respiratory rate, blood pressure, age ≥ 65 years
CURB-65 had mortality rates ranging from 58% to 90.9%. This was similar to the PSI predictions. Both severity scores showed a high strength in identifying high-risk patients. However, CURB-65 accurately predicted 30-day mortality compared to the PSI score. Also, CURB-65 seemed more effective than PSI at identifying patients at the most significant risk [20]. Heterogeneity for class V and class 3-5 was high (I2 = 98%).
The remaining five articles [2,10,23,32,35] were compared for mortality rates in the lowest classes; class I-II and class 0-1 for PSI and CURB 65, respectively. Bahlis et al. [2] had 3.7%/4.5%, Estella [23] 20%/13.3%, Wang et al. [32] 8.1%/5.1%, Kim et al. [10] 4.5%/2.3%, and Aydin et al. [35] 8.6%/10.0% mortality rates by PSI and CURB 65 prediction, respectively. The range for mortality rate in PSI scores was 3.7-24.9%. The range showed that the lesser scores in PSI severity, the less likelihood of death of patients; however, CURB-65 can be a good severity score in the lower classes compared to PSI. Similarly, the range showed that the patients may be discharged from the hospital and get treatment from their homes. CURB-65 varied slightly compared to PSI, ranging from 2.3% to 17.9%. The PSI can better identify patients who can be safely discharged and managed at home compared to the CURB-65 score, which is less likely to be used [18]. The comparison is illustrated in Figures 6-7, which show similarities between CURB-65 and PSI. CURB-65 offers a straightforward technique for recognizing patients with high mortality risk and who might profit from early ICU admission [28]. Results in Figure 6 showed substantial heterogeneity (I2 = 87%), while results in Figure 7 showed moderate heterogeneity (I2 = 64%).
Figure 6. A forest plot of PSI risk ratios for the lowest class (class I -II).
Fuchs Bahlis et al., 2021 [2], Estella, 2015 [23], Wang et al., 2020 [32], Kim et al., 2013 [10], Aydin et al., 2019 [35]
PSI: pneumonia severity index
Figure 7. A forest plot of CURB-65 risk ratios for the lowest class (class 0-1).
Fuchs Bahlis et al., 2021 [2], Estella, 2015 [23], Wang et al., 2020 [32], Kim et al., 2013 [10], Aydin et al., 2019 [35]
CURB-65: confusion, uremia, respiratory rate, blood pressure, age ≥ 65 years
CURB-65 had more sensitivity (96.7%) and specificity (89.3%) in predicting admission to intensive care support, as seen in Table 6.
Discussion
It's interesting to note that additional comparisons of the PSI and CURB-65 instruments have highlighted significant variations in benefits and restrictions. The requirement to identify patients with low mortality risk served as the foundation for the creation and validation of PSI. Therefore, this instrument may not be accurate for choosing the location of therapy and may underestimate the severity of the illness, especially in young patients without concomitant illnesses [1]. According to this review, when comparing the PSI and CURB-65 tools in the same group, both were effective at predicting death and spotting low-risk patients. For the opportunity costs associated with missed productivity, the CURB-65 and PSI ratings both demonstrated a reasonable positive predictive value. However, we could not find statistically significant relationships between the direct expenses of CAP treatment and clinical severity ratings. The CURB-65, however, seemed more specific in identifying the mortality risk in severe CAP [39,40]. Many inpatient and outpatient CAP patients were assessed using the PSI and the CURB-65 in a different investigation. The CURB-65 accurately predicted 30-day mortality, the requirement for mechanical ventilation, and perhaps the need for hospital admission [41]. The time to clinical stability was also connected with the CURB-65 score. CURB-65 seems to be more effective than PSI at identifying patients who are at the most significant risk. As a result, it may be better suited to direct investigations and the administration of broad-spectrum antibiotic therapy (as recommended by the British Thoracic Society (BTS) guidelines when these actions are directed explicitly at high-risk patients [42]. The PSI was good in predicting death but not the necessity for ICU admission. The CURB-65 tool was reported to be more accurate than the PSI for this site-of-care choice in the study by Capelastegui et al. but the authors also noted that it could not predict the requirement for ICU admission [41].
A study by Dhawan et al. supported PSI as the best available predictor for nursing home-acquired pneumonia (NHAP), while CURB-65 was an alternative indicator [43]. PSI has also been seen as the best indicator in predicting different clinical outcomes in the elderly with CAP compared to CURB-65 [44]. PSI's predictive efficacy differs depending on the cause of CAP in adults. According to Rello, PSI is better than CURB-65 and more effective in cases of mild bacterial infection [45]. The systematic application of objective criteria to pneumonia patients' site-of-care decision-making is emerging as a breakthrough in patient management. The PSI can identify patients who can be safely discharged and managed at home. Still, it can also understate severity, especially in young patients with severe respiratory failure who don't have any co-morbid conditions [46]. Besides, CURB-65 offers a straightforward technique that can recognize individuals at a high mortality risk and who might profit from early ICU admission.
Overall test performance did not differ significantly across these scores, indicating that physicians may select the scoring system that is most appropriate for their particular circumstances. Even though the tests' overall accuracy was comparable, there were some differences in the performance traits between the scores. A more considerable positive predictive value shows that CURB-65/CRB-65 may be preferable for identifying high-risk patients. Still, a low negative likelihood ratio suggests that PSI may be superior for identifying low-risk patients. It is challenging to determine the therapeutic significance of these discrepancies, though. Therefore, it is crucial that these tools accurately forecast the desired outcome. Our meta-analysis shows that the severity scores predict the 30-day mortality from CAP scores using PSI and CURB-65 with characteristics of moderate-good performance. The PSI is considerably more complicated than the CURB-65 because it calls for measuring 20 separate parameters, with varying points given for each [8].
Limitations
First, the heterogeneity of the included studies severely constrained our meta-analysis. Different outcome measures, such as 30-day or in-hospital mortality, were utilized in numerous studies that included inpatients and outpatients. Different study strategies were employed, including prospective observational studies, retrospective studies, population-based observation, and comparative research. Additionally, some studies presented the mortality rate in percentages. Consequently, converting the percentages to numbers for meta-analysis could have contributed to errors due to rounding off the decimals to whole numbers. Furthermore, the mortality rate for people with mild CAP may be higher as it included deaths from non-infectious and unknown causes.
Conclusions
This review attempted to provide a comparison of the PSI and CURB-65 on their abilities to predict mortality and the need for intensive care support. We formulated a research question and included relevant papers. Both narrative synthesis and meta-analysis were performed on the data taken from the included articles. Both severity scores have identical sensitivity, but the CURB-65 score was more specific than the PSI. Moreover, the CURB-65 score showed more sensitivity (89.3%) in ICU prediction than PSI (78.8%). It was seen that the two severity scores are the most preferred tools in the prediction of ICU admission and mortality. However, despite having comparable mortality, CURB-65 is highly preferred as it is easier to implement apart from everything else. Finally, even though these two scores are helpful tools, they cannot and should not be used in place of clinical judgment and medical examination. Ideally, the best strategy depends on doctors' experience and how well they apply their knowledge to the individual patients' scores to make the appropriate decision for ICU admission.
Acknowledgments
HAZ: Writing, critical review, and interpretation of data; BHA and ES: Conceptualization and design of the study, drafting the article; EHM: Analysis and interpretation of data and critical review; KB: Reviewing the article critically for important intellectual content and database search; WAEE: Acquisition of data and writing the article; AA: Critical review of the final article and analysis of data. All authors gave final approval of the article, and all authors are accountable for all aspects of the work.
The authors have declared that no competing interests exist.
References
- 1.Validity of pneumonia severity index and CURB-65 severity scoring systems in community acquired pneumonia in an Indian setting. Shah BA, Ahmed W, Dhobi GN, Shah NN, Khursheed SQ, Haq I. https://pubmed.ncbi.nlm.nih.gov/20364609/ Indian J Chest Dis Allied Sci. 2010;52:9–17. [PubMed] [Google Scholar]
- 2.Charlson comorbidity Index and other predictors of in-hospital mortality among adults with community-acquired pneumonia. Bahlis LF, Diogo LP, Fuchs SC. J Bras Pneumol. 2021;47:0. doi: 10.36416/1806-3756/e20200257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Serum interleukin-17 predicts severity and prognosis in patients with community acquired pneumonia: a prospective cohort study. Feng CM, Wang XM, Li MD, et al. BMC Pulm Med. 2021;21:393. doi: 10.1186/s12890-021-01770-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Performance of pneumonia severity index and CURB-65 in predicting 30-day mortality in patients with COVID-19. Satici C, Demirkol MA, Sargin Altunok E, et al. Int J Infect Dis. 2020;98:84–89. doi: 10.1016/j.ijid.2020.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Validation of PSI/PORT, CURB-65 and SCAP scoring system in COVID-19 pneumonia for prediction of disease severity and 14-day mortality. Anurag A, Preetam M. Clin Respir J. 2021;15:467–471. doi: 10.1111/crj.13326. [DOI] [PubMed] [Google Scholar]
- 6.Community-acquired pneumonia severity assessment tools in patients hospitalized with COVID-19: a validation and clinical applicability study. Lazar Neto F, Marino LO, Torres A, et al. Clin Microbiol Infect. 2021;27:1037–1038. doi: 10.1016/j.cmi.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.A new prognosis score to predict mortality after acute pneumonia in very elderly patients. Putot A, Tetu J, Perrin S, et al. J Am Med Dir Assoc. 2016;17:1123–1128. doi: 10.1016/j.jamda.2016.07.018. [DOI] [PubMed] [Google Scholar]
- 8.A prediction rule to identify low-risk patients with community-acquired pneumonia. Fine MJ, Auble TE, Yealy DM, et al. N Engl J Med. 1997;336:243–250. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 9.Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation study. Lim WS, van der Eerden MM, Laing R, et al. Thorax. 2003;58:377–382. doi: 10.1136/thorax.58.5.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mortality of community-acquired pneumonia in Korea: assessed with the pneumonia severity index and the CURB-65 score. Kim HI, Kim SW, Chang HH, et al. J Korean Med Sci. 2013;28:1276–1282. doi: 10.3346/jkms.2013.28.9.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.CRB-65 for the assessment of pneumonia severity: who could ask for more? Ewig S, Welte T. Thorax. 2008;63:665–666. doi: 10.1136/thx.2008.099028. [DOI] [PubMed] [Google Scholar]
- 12.SMART-COP: a tool for predicting the need for intensive respiratory or vasopressor support in community-acquired pneumonia. Charles PG, Wolfe R, Whitby M, et al. Clin Infect Dis. 2008;47:375–384. doi: 10.1086/589754. [DOI] [PubMed] [Google Scholar]
- 13.A prospective comparison of severity scores for identifying patients with severe community acquired pneumonia: reconsidering what is meant by severe pneumonia. Buising KL, Thursky KA, Black JF, MacGregor L, Street AC, Kennedy MP, Brown GV. Thorax. 2006;61:419–424. doi: 10.1136/thx.2005.051326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.The pneumonia severity index: a decade after the initial derivation and validation. Aujesky D, Fine MJ. Clin Infect Dis. 2008;47 Suppl 3:0–9. doi: 10.1086/591394. [DOI] [PubMed] [Google Scholar]
- 15.The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Page MJ, McKenzie JE, Bossuyt PM, et al. BMJ. 2021;372:0. doi: 10.1186/s13643-021-01626-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wells G, Shea B, O’Connell D, et al. The Ottawa Hospital: The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. [ Sep; 2022 ]. 2021. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 17.Risk-of-bias VISualization (robvis): an R package and Shiny web app for visualizing risk-of-bias assessments. McGuinness LA, Higgins JP. Res Synth Methods. 2021;12:55–61. doi: 10.1002/jrsm.1411. [DOI] [PubMed] [Google Scholar]
- 18.Severity assessment tools for predicting mortality in hospitalised patients with community-acquired pneumonia. Systematic review and meta-analysis. Chalmers JD, Singanayagam A, Akram AR, et al. Thorax. 2010;65:878–883. doi: 10.1136/thx.2009.133280. [DOI] [PubMed] [Google Scholar]
- 19.The significance of intracranial pressure monitoring for reducing mortality in patients with traumatic brain injury: a systematic review and meta-analysis. Han N, Yang F, Zhang X. Comput Math Methods Med. 2022;2022:1956908. doi: 10.1155/2022/1956908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pneumonia severity index compared to CURB-65 in predicting the outcome of community acquired pneumonia among patients referred to an Iranian emergency department: a prospective survey. Alavi-Moghaddam M, Bakhshi H, Rezaei B, Khashayar P. Braz J Infect Dis. 2013;17:179–183. doi: 10.1016/j.bjid.2012.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Comparison of pneumonia severity scores for patients diagnosed with pneumonia in emergency department. Kaya AE, Ozkan S, Usul E, Arslan ED. Indian J Med Res. 2020;152:368–377. doi: 10.4103/ijmr.IJMR_595_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Application of validated severity scores for pneumonia caused by SARS-CoV-2. Esteban Ronda V, Ruiz Alcaraz S, Ruiz Torregrosa P, et al. Med Clin (Engl Ed) 2021;157:99–105. doi: 10.1016/j.medcle.2021.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Usefulness of CURB-65 and pneumonia severity index for influenza A H1N1v pneumonia. Estella A. Monaldi Arch Chest Dis. 2012;77:118–121. doi: 10.4081/monaldi.2012.144. [DOI] [PubMed] [Google Scholar]
- 24.Lactate levels and pneumonia severity index are good predictors of in-hospital mortality in pneumonia. Demirel B. Clin Respir J. 2018;12:991–995. doi: 10.1111/crj.12616. [DOI] [PubMed] [Google Scholar]
- 25.Predicting severe COVID-19 in the emergency department. Holten AR, Nore KG, Tveiten CE, Olasveengen TM, Tonby K. Resusc Plus. 2020;4:100042. doi: 10.1016/j.resplu.2020.100042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.CURB-65 plus hypoalbuminemia: a new score system for prediction of the in-hospital mortality risk in patients with SARS-CoV-2 pneumonia. Oliva A, Borrazzo C, Mascellino MT, et al. Infez Med. 2021;29:408–415. doi: 10.53854/liim-2903-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Community-acquired pneumonia: economics of inpatient medical care vis-à-vis clinical severity. Cupurdija V, Lazic Z, Petrovic M, Mojsilovic S, Cekerevac I, Rancic N, Jakovljevic M. J Bras Pneumol. 2015;41:48–57. doi: 10.1590/S1806-37132015000100007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.New sepsis definition (Sepsis-3) and community-acquired pneumonia mortality. a validation and clinical decision-making study. Ranzani OT, Prina E, Menéndez R, et al. Am J Respir Crit Care Med. 2017;196:1287–1297. doi: 10.1164/rccm.201611-2262OC. [DOI] [PubMed] [Google Scholar]
- 29.The role of Endocan as a prognostic biomarker in community-acquired pneumonia. Gunaydin S, Kucuk M, Gunaydin UM. Pak J Med Sci. 2019;35:117–123. doi: 10.12669/pjms.35.1.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prediction accuracy of commonly used pneumonia severity scores in Aboriginal patients with severe community-acquired pneumonia: a retrospective study. Tsai D, Secombe P, Chiong F, Ullah S, Lipman J, Hewagama S. Intern Med J. 2023;53:51–60. doi: 10.1111/imj.15534. [DOI] [PubMed] [Google Scholar]
- 31.Performance and comparison of assessment models to predict 30-day mortality in patients with hospital-acquired pneumonia. Wen JN, Li N, Guo CX, Shen N, He B. Chin Med J (Engl) 2020;133:2947–2952. doi: 10.1097/CM9.0000000000001252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Admission C-reactive protein-to-albumin ratio predicts the 180-day mortality of AIDS-related pneumocystis pneumonia. Wang H, Chang Y, Cui ZZ, Liu ZJ, Ma SF. AIDS Res Hum Retroviruses. 2020;36:753–761. doi: 10.1089/AID.2020.0057. [DOI] [PubMed] [Google Scholar]
- 33.Utility of predictive tools for risk stratification of elderly individuals with all-cause acute respiratory infection. Bloom AS, Suchindran S, Steinbrink J, McClain MT. Infection. 2019;47:617–627. doi: 10.1007/s15010-019-01299-1. [DOI] [PubMed] [Google Scholar]
- 34.Utility of community-acquired pneumonia severity scores in guiding disposition from the emergency department: intensive care or short-stay unit? Williams JM, Greenslade JH, Chu KH, Brown AF, Lipman J. Emerg Med Australas. 2018;30:538–546. doi: 10.1111/1742-6723.12947. [DOI] [PubMed] [Google Scholar]
- 35.Viral prevalence, clinical profiles and comparison of severity scores for predicting the mortality of adults with severe acute respiratory infections. Aydın H, Doğan H, Özüçelik DN, Koçak M, Gül OA. Turk J Med Sci. 2019;49:862–871. doi: 10.3906/sag-1807-231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Do N-terminal pro-brain natriuretic peptide levels determine the prognosis of community acquired pneumonia? Akpınar EE, Hoşgün D, Akpınar S, Ateş C, Baha A, Gülensoy ES, Ogan N. J Bras Pneumol. 2019;45:0. doi: 10.1590/1806-3713/e20180417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prognostic factors in hospitalized community-acquired pneumonia: a retrospective study of a prospective observational cohort. Ito A, Ishida T, Tokumasu H, Washio Y, Yamazaki A, Ito Y, Tachibana H. BMC Pulm Med. 2017;17:78. doi: 10.1186/s12890-017-0424-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Comparison of severity predictive rules for hospitalised nursing home-acquired pneumonia in Korea: a retrospective observational study. Lee JC, Hwang HJ, Park YH, Joe JH, Chung JH, Kim SH. Prim Care Respir J. 2013;22:149–154. doi: 10.4104/pcrj.2013.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.External validation and recalibration of the CURB-65 and PSI for predicting 30-day mortality and critical care intervention in multiethnic patients with COVID-19. Elmoheen A, Abdelhafez I, Salem W, et al. Int J Infect Dis. 2021;111:108–116. doi: 10.1016/j.ijid.2021.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Combining information from prognostic scoring tools for CAP: an American view on how to get the best of all worlds. Niederman MS, Feldman C, Richards GA. Eur Respir J. 2006;27:9–11. doi: 10.1183/09031936.06.00130305. [DOI] [PubMed] [Google Scholar]
- 41.Validation of a predictive rule for the management of community-acquired pneumonia. Capelastegui A, España PP, Quintana JM, Areitio I, Gorordo I, Egurrola M, Bilbao A. Eur Respir J. 2006;27:151–157. doi: 10.1183/09031936.06.00062505. [DOI] [PubMed] [Google Scholar]
- 42.BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Lim WS, Baudouin SV, George RC, et al. Thorax. 2009;64 Suppl 3:0–55. doi: 10.1136/thx.2009.121434. [DOI] [PubMed] [Google Scholar]
- 43.Predictors of mortality for nursing home-acquired pneumonia: a systematic review. Dhawan N, Pandya N, Khalili M, Bautista M, Duggal A, Bahl J, Gupta V. Biomed Res Int. 2015;2015:285983. doi: 10.1155/2015/285983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Analysis of the severity and prognosis assessment of aged patients with community-acquired pneumonia: a retrospective study. Xiao K, Su LX, Han BC, et al. J Thorac Dis. 2013;5:626–633. doi: 10.3978/j.issn.2072-1439.2013.09.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Demographics, guidelines, and clinical experience in severe community-acquired pneumonia. Rello J. Crit Care. 2008;12:0. doi: 10.1186/cc7025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Diagnostic tests 4: likelihood ratios. Deeks JJ, Altman DG. BMJ. 2004;329:168–169. doi: 10.1136/bmj.329.7458.168. [DOI] [PMC free article] [PubMed] [Google Scholar]