Abstract
Chronic graft-versus-host disease (cGvHD) remains a prominent barrier to allogeneic hematopoietic stem cell transplantion as the leading cause of nonrelapse mortality and significant morbidity. Tremendous progress has been achieved in both the understanding of pathophysiology and the development of new therapies for cGvHD. Although our field has historically approached treatment from an empiric position, research performed at the bedside and bench has elucidated some of the complex pathophysiology of cGvHD. From the clinical perspective, there is significant variability of disease manifestations between individual patients, pointing to diverse biological underpinnings. Capitalizing on progress made to date, the field is now focused on establishing personalized approaches to treatment. The intent of this article is to concisely review recent knowledge gained and formulate a path toward patient-specific cGvHD therapy.
Introduction
Chronic graft-versus-host disease (cGvHD) remains the leading cause of long-term morbidity and mortality after allo hematopoietic stem cell transplantation (alloHSCT).1,2 Significant progress has been made in understanding cGvHD pathophysiology,3,4 leading to preclinical testing and clinical translation of agents that are now Food and Drug Administration (FDA)-approved for steroid-resistant disease,5, 6, 7 as well as the potential development of new approaches for prophylaxis and first-line treatment. As a result of the National Institutes of Health (NIH)-supported cGvHD consensus development project, disease definition, clinical features and severity, and criteria for treatment response have been established.8,9 The 2020 NIH consensus development project refined various aspects of cGvHD biology, clinical spectra, current status, and mapped future advancements in therapy.10 The goal of the present article is to summarize how recent understandings of cGvHD mechanisms may facilitate personalized treatment and prevention strategies.
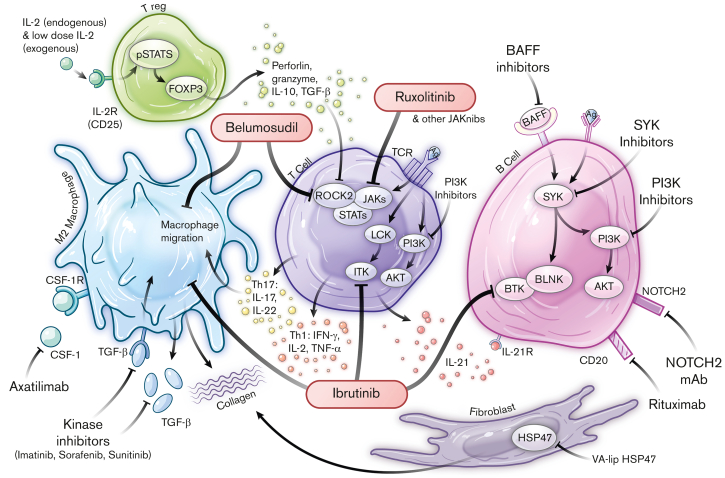
cGvHD can affect many organs and systems, typically involving barrier sites that are entry points for pathogens and home to cellular populations within the adaptive as well as innate immune systems.4,11,12 Human and animal studies have implicated inflammatory mediators, cytokines, danger-associated molecular patterns, and metabolites as contributors to cGvHD pathogenesis.4,13, 14, 15, 16, 17 The immune system dysregulation that leads to cGvHD can be mediated by T cells, B cells, natural killer (NK) cells, NKT cells, monocytes, and macrophages, and can be ameliorated by regulatory populations of T cells, B cells, myeloid cells (monocytes, macrophages, myeloid derived suppressor cells) and NK cells4,11,12 (Figure 1). Whether the affected organ systems share pathogenic mechanisms that initiate and sustain cGvHD is not yet fully elucidated, albeit certain immune populations have been shown in animal models to mediate cGvHD in multiple target organs.4,18,19 Whether clinical symptoms in patients represent protean manifestations of a limited set of pathophysiological processes or diverse mechanisms that invoke specific cGvHD manifestations is unclear. Clinically, variability in organ involvement is compounded by a spectrum of clinical subtypes and variable posttransplant timing, which adds to the complexity of discerning underlying mechanisms and devising strategies to overcome cGvHD. Taken together, these studies support the conclusion that the biology of cGvHD is complex and likely to be heterogenous. New treatment approaches for cGvHD focused around the concept of personalized therapy are greatly needed.
Figure 1.
Pathophysiological networks and targeted approaches for prevention and treatment of cGvHD. FDA-approved drugs are highlighted within red bubbles. Ag, antigen; AKT, Ak strain transforming; BAFF, B-cell activating factor; BAFF R, BAFF receptor; BCR, B-cell receptor; BLNK, B-cell linker; BTK, Bruton’s Tyrosine Kinase; BTK/ITK, Bruton’s Tyrosine Kinase /IL-2 Inducible T-cell Kinase; CD, cluster of differentiation; FOXP3, forkhead box P3; HSP47, heat shock protein 47; INF-γ, interferon gamma; ITK, IL-2-inducible T-cell kinase; Jakinibs, Janus kinase inhibitors; JAKs, Janus kinases; LCK, lymphocyte-specific protein tyrosine kinase; NOTCH2, Neurogenic locus notch homolog protein 2; NOTCH2 mAb, neurogenic locus notch homolog protein 2 mAb; PI3K, phosphoinositide 3-kinase; pSTAT5, phosphorylated signal transducer and activator of transcription 5; ROCK2, Rho associated coiled-coil containing protein kinase 2; STATs, signal transducers and activators of transcription; SYK, spleen associated tyrosine kinase; TCR, T-cell receptor; TGF-β, transforming growth factor beta; Th, T helper; TNF-α, tumor necrosis factor alpha; Treg, T regulatory cell; VA-lip HSP47, vitamin A coupled liposomal containing small interfering RNA (siRNA) against heat shock protein 47.
FDA-approved approaches targeting pathophysiologic mechanisms in cGvHD
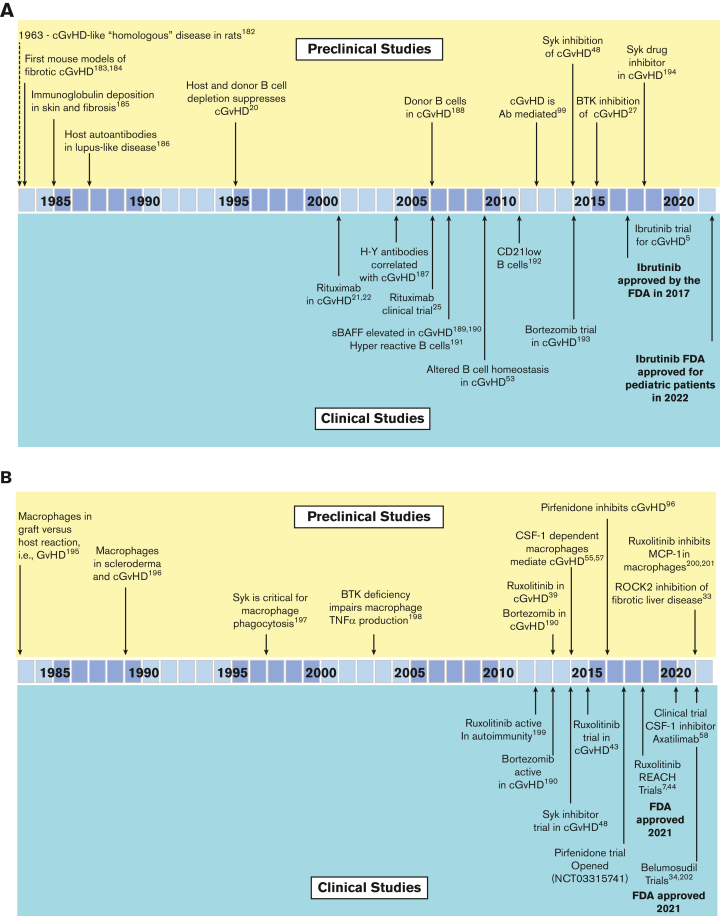
The development of the first FDA-approved therapeutic agent for cGvHD, ibrutinib, illustrates the iterative process that can exist between both preclinical models and correlative human biology studies (Figure 2A). From the first preclinical murine cGvHD studies, which established the role of B cells in cGvHD,20 the preclinical models and clinical human biomarker studies detailed the B-cell abnormalities associated with cGvHD development. This resulted in the testing of the anti-CD20 monoclonal antibody (mAb), rituximab, as a B-cell targeting strategy for cGvHD21, 22, 23, 24, 25, 26 that demonstrated clinical responses in steroid-refactory cGvHD. Preclinical cGvHD mouse studies focused on inhibiting Bruton tyrosine kinase/interleukin-2 (IL-2) inducible T-cell kinase, with amelioration of disease manifestations observed in several models.27 B and T cells from patients with active and persistent cGvHD showed signs of hyperactivity that were lowered by adding ibrutinib to cell culture. Based on these aggregate results and the high unmet medical need for agents to treat patients with steroid-refractory cGvHD, a single-arm open-label study ibrutinib gained FDA regulatory approval in 2017.5,28
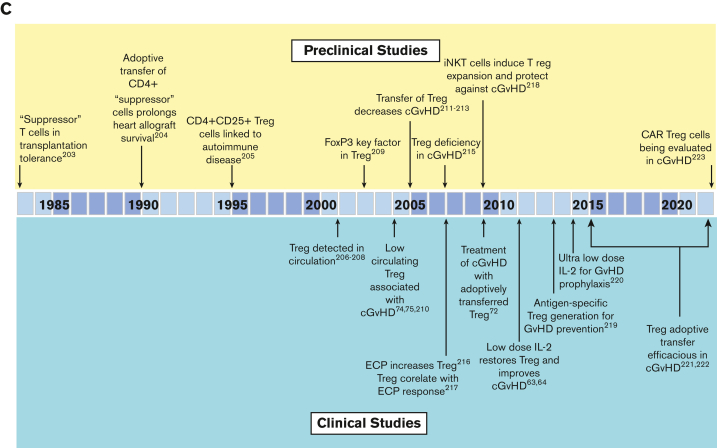
Figure 2.
Summary of the preclinical modeling and clinical studies that led to the development of FDA-approved agents for chronic GvHD. (A) The role of B cells and targeting of B cells in cGvHD. (B) The role of macrophages and targeting of macrophage function in cGvHD. (C) The role of Tregs, in suppressing cGvHD and the development of cGvHD therapies aimed at Treg expansion/improved function. Ab, antibody; BTK, Bruton’s Tyrosine Kinase; CAR Treg, chimeric antigen receptor T regulatory cell; ECP, extracorporeal photopheresis; FoxP3, forkhead box P3; H-Y Ab, antibodies specific for male (Y) antigens; MCP-1, monocyte chemoattractant protein-1; iNKT, invariant NK T cells; ROCK2, Rho associated coiled-coil containing protein kinase 2; sBAFF, soluble B-cell activating factor; SYK, spleen sssociated tyrosine kinase; TNF-α, tumor necrosis factor alpha. Reference citations used: 5,7,20, 21, 22,25,27,33,39,43,45,48,53,55,57,58,63,64,72,74,75,96,99,182, 183, 184, 185, 186, 187, 188, 189, 190, 191, 192, 193, 194, 195, 196, 197, 198, 199, 200, 201, 202, 203, 204, 205, 206, 207, 208, 209, 210, 211, 212, 213, 214, 215, 216, 217, 218, 219, 220, 221, 222, 223.
Two additional agents have garnered FDA approval in 2021 (Figure 2B-C) and both emanated from preclinical studies. Belumosudil, a Rho associated coiled-coil containing protein kinase 2 inhibitor, tipped the balance from phosphorylated signal transducer and activator of transcription 3 to phosphorylated signal transducer and activator of transcription 5, dampened IL-17 and IL-21 production that plays a role in fibrotic manifestations in animal cGvHD models,29, 30, 31, 32, 33, 34 and led to the initiation of a first-in-human and first-in-disease clinical trial culminating in FDA approval for the treatment of steroid-refractory cGvHD.6
Ruxolitinib, a janus kinase/signal transducers and activators of transcription inhibitor (Figure 1) that has known benefits in myelofibrosis35,36 and autoimmunity,37,38 was evaluated in acute GvHD animal models,39, 40, 41, 42, 43 followed by clinical trials, REACH-144 and REACH-2.7,45 Positive findings led to FDA approval for treatment of steroid-refractory acute GvHD. Subsequently, REACH-3, a prospective randomized phase 3 trial in steroid-refractory (or -dependent) cGvHD as compared to the best available therapy,7 led to the approval from FDA for this indication.46
Agents being evaluated for FDA approval in cGvHD treatment
Other cGvHD B-cell targeting strategies have been vetted in mouse cGvHD models (Figure 2A). Of note, increased B-cell receptor responsiveness was observed in B cells from patients with cGvHD.47 In vitro exposure of cGvHD B cells to a spleen associated tyrosine kinase inhibitor selectively induced B-cell apoptosis in cells derived from patients with cGvHD compared with those without cGvHD. In vivo testing in mouse cGvHD models resulted a consistent reduction in disease severity.48 Beyond targeting of spleen associated tyrosine kinase, positive preclinical data for inhibitors of phosphoinositide-3 kinase delta and B-cell activating factor delineated subsequent clinical investigations in patients with cGvHD5,34,49, 50, 51, 52, 53 with welcome promising results given modest postapproval clinical response rates, now reported with ibrutinib.54
In mice with cGvHD, tissue accumulation of monocytes and macrophages that depend upon colony stimulating factor-1 receptor (CSF-1R) signaling for generation and survival was observed55, 56, 57 (Figure 2B). Anti-CSF-1R mAb treatment was effective in multiple cGvHD models providing the impetus for initiating the ongoing clinical trial of a CSF-1R mAb, axatilimab, to treat steroid-refractory cGvHD.55 To date, axatilimab is demonstrating very promising activity58 and is now undergoing pivotal clinical trials.
Thymus injury that accompanies cGvHD, along with cell exhaustion within target organs, leads to a deficiency of regulatory T cells (Tregs). Adoptive transfer of ex vivo expanded Tregs or in vivo expansion via low-dose IL-2 administration has clear efficacy in cGvHD, as seen in animal and clinical studies59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76 (Figure 2C). It will soon be tested in a steroid-refractory cGvHD setting through the Children’s Oncology Group in a trial that combines low-dose IL-2 with ex vivo expanded Tregs.
To summarize, numerous bench-to-bedside studies have advanced the understanding of cGvHD pathogenesis, which has resulted in the development of new therapies. Furthermore, biological pathways implicated in autoimmune diseases have also yielded therapeutic targets proven efficacious in acute and cGvHD upon bench-to-bedside evaluations.
Other available treatment strategies
Currently, available therapies to treat steroid-refractory cGvHD have been previously extensively reviewed and include extracorporeal photopheresis, hydroxychloroquine, methotrexate, bortezomib, pentamidine, etanercept, calcineurin inhibitors, sirolimus, and others.49
Influence of graft and early post alloHSCT manipulations on cGvHD
A number of interventions at the time of alloHSCT have resulted in a decreased cGvHD incidence. This illustrates that early immune modulations can impact cGvHD onset that occurs many months later and can potentially affect long-term immune reconstitution and tolerance patterns. In vivo T-cell depletion, including peritransplant alemtuzumab and antithymocyte globulin hello, decrease cGvHD occurrence,77 presumably by reducing the number of alloreactive T cells that are able to orchestrate cGvHD, while allowing B and NK cell expansion, which may not be beneficial for reducing cGvHD. Another graft cell depletion approach includes ex vivo naïve T-cell depletion, which was associated with a diminution of cGvHD,78 and is supported by results of a recent clinical trial.79
When given as prophylaxis early after donor graft infusion, post-transplant cyclophosphamide (PTCy) significanctly suppressed rodent acute and cGvHD, which was initially thought to be mediated through the in vivo depletion of alloreactive T cells, with clinical efficacy confirmed in human trials.80 With low cost, favorable tolerability, and efficacy in preventing cGvHD, PTCy is now a widely used cGvHD prophylaxis approach.81, 82, 83 Despite the clinical utility of PTCy, its exact mechanism of action in alloHSCT is not fully elucidated.84 As a result, further studies in alloHSCT animal models85,86 and clinical samples87,88 are ongoing in order to refine and optimize PTCy for alloHSCT. To date, murine models have identified several potential mechanisms of action, including reduction of alloreactive CD4+ effector T cells, impairment of function in surviving alloreactive CD4+ and CD8+ effector T cells, and early expansion of Treg cells.84
It has been found that the graft stem cell source significantly impacts later cGvHD development, with a higher cGvHD incidence after donor G-CSF mobilized peripheral blood stem cells (G-PBSC) than bone marrow (BM). One study found that low CD56bright NK cell frequency in recipients of G-PBSC is associated with higher cGvHD rates than G-BM,89 but this has not been directly compared to unstimulated BM grafts. Others observed the association between faster reconstitution of naïve and memory T-cell recovery in G-PBSC and increased cGvHD, albeit with better survival.90 In the same study, higher classical dendritic cell number in circulation of G-BM recipients was associated with higher cGvHD incidence, but again with better survival. Plerixafor mobilization has been used in place of G-CSF91 and such grafts may phenotypically resemble BM-like grafts that would be expected to lead to lower GvHD rates.92,93 However, this too has yet to be confirmed clinically by direct comparison to G-PB or unstimulated BM and murine data suggest that plerixafor may be associated with more severe sclerotic GvHD than G-PBSC.94
The use of umbilical cord blood grafts is associated with lower rates of cGvHD90; yet, there is also evidence that poor immune reconstitution after umbilical cord blood can be associated with lower circulating total Th cells, slower naïve Th cells reconstitution and increased cGvHD development.95 Whereas, in another study, circulating Tfh cells were found to be lower in frequency but more highly activated in patients with cGvHD.29 Further work is needed to delineate how impaired immune reconstitution impacts on immune tolerance and cGvHD.
Ongoing and future preclinical and clinical studies to identify targets for treatment and prevention of cGvHD
Preclinical models
Fibrotic cGvHD manifestations have long been recognized clinically and explored at the bench.55, 56, 57,96, 97, 98, 99 Several pathways involving macrophage reprogramming are implicated in cGvHD, including CSF-1R55, 56, 57 as well as fibroblast differentiation with aberrant collagen production and uncontrolled fibrosis in mouse models,97,98 findings that are also seen in cGvHD clinical specimens.100 A topical collagen inhibitor has shown promising preclinical efficacy as prophylaxis and treatment for ocular98 and cutaneous cGvHD.97 The antifibrotic agent, pirfenidone, dampens inflammatory mediators and SMAD2/3 signaling, decreases fibroblast proliferation, and TGFβ-induced procollagen production with encouraging results in mouse models of lung and sclerotic skin cGvHD96 and efficacy in a clinical phase 1 study for bronchiolitis obliterans.101
Preclinical testing in rodent,102 canine,103 and nonhuman primate104, 105, 106 studies indicated that the inhibition of CD28/B7 costimulation suppressed GvHD. Positive results of a clinical trial of abatacept, CTLA4-Ig that blocks CD28/B7, combined with a calcineurin inhibitor and methotrexate, led to FDA approval for acute GvHD prevention in patients receiving HLA-matched or 1 allele mismatched donor grafts.107 Testing for steroid-refractory cGvHD is ongoing (NCT01954979).108
Bedside approaches undergoing bench interrogation include microbiota classification and modulation designed to preempt and ameliorate gut acute GvHD that often precedes cGvHD in patients.109, 110, 111, 112, 113, 114, 115, 116, 117 Despite differences in microbiome composition, diet, and environment between rodents and humans, overall patterns can yield generalizable principles, easing extrapolation between species. Clinical data from geographically diverse study centers pointed to distinct microbiota data sets that inform pertinent microbiome components117 and potential interventions.118 Microbiota driven systemic metabolic changes have been elucidated in clinical studies and modeled in animals, including in cGvHD.117 In a primary case-control cohort and 1 of 2 cross-sectional cohorts, lower day 100 plasma levels of microbial derived short chain fatty acids, proprionate and butyrate, were associated with cGVHD.117 An active cGvHD research area is cellular immune metabolism. Emerging laboratory-based15,119, 120, 121 and early clinical biospecimen analyses of cellular and plasma metabolites16,122 suggest that the metabolic reprogramming of immune cells represents a potential therapeutic and diagnostic target for acute and cGvHD.13,14,17,123,124
Other targets recently implicated in mouse125,126 and canine127 cGvHD models are the inducible costimulatory (ICOS) and Notch pathways. ICOS signaling blockade with anti-ICOS mAb in preclinical studies provides evidence for this treatment strategy.127,128 The Notch pathway has been identified as a driving force in cGvHD pathogenesis in murine129 and clinical49 cGvHD, with numerous inhibitors currently undergoing clinical testing in oncology, but not yet in GvHD.
Clinical annotation of cGvHD
Chronic GvHD represents 3 intertwined pathophysiologic processes involving inflammation, immune dysregulation, and fibrotic manifestations that contribute to the development of the disease.3,130 Although the inflammatory and fibrotic phases are often identifiable on physical exam and clinical evaluation, especially cutaneous and oral erythema (inflammatory) or dermal sclerosis (fibrotic), they may occur concurrently. Thus, a constellation of clinical findings may not fit neatly into a single category or continuum of cGvHD progression. Recently, machine learning and computational analyses that take into account clinically relevant patterns and organ involvement have expanded risk strata for cGvHD survival for application to decisions to test the validity and exportability of choosing and initiating the most appropriate therapies.131 To enable personalized cGvHD treatment, additional diagnostic tools, objective clinical features, imaging, and laboratory parameters are needed. Although laboratory, imaging, cellular, molecular, and metabolic data are being gathered, clinical annotation and scoring will be essential to categorize and diagnose GvHD not simply by severity, but by biological subtypes. With such data, rational therapy selection can yield the highest chance of efficacy for the individual patient.132
Biomarkers
Disease predictive biomarker panels are being tested for validation and adaptation in prospective studies of acute133, 134, 135, 136 and chronic137, 138, 139 GvHD. The biomarkers, in addition to being clinically useful, may identify potential mechanisms and biologic targets for therapeutic interventions. Identified biomarkers can then be used to probe hypotheses for the pathophysiological basis of identified targets in animal modeling. As a general rule, biomarkers probably represent underlying biology, but may only be a surrogate with no direct association with cGvHD, primarily serving as a reproducible means to guide and optimize therapy, Table 1.
Table 1.
Application of BEST (Biomarkers EndpointS & other Tools) biomarker definitions in cGvHD∗
| Type of marker | Definition | Application in alloHSCT |
|---|---|---|
| Diagnostic | A biomarker used to detect or confirm presence of disease or condition of interest or to identify individuals with a subtype of the disease. | At the onset of cGvHD or late aGvHD compared with time-matched control |
| Response | A biomarker used to show that a biological response has occurred in an individual who has been exposed to a medical product or an environmental agent. | Measured 4-8 wk after treatment initiation for cGvHD |
| Predictive | A biomarker used to identify individuals who are more likely than similar individuals without the biomarker to experience a favorable or unfavorable effect from exposure to a medical product or an environmental agent. | Measured at the onset of treatment of cGvHD |
| Prognostic | A biomarker used to identify likelihood of a clinical event, disease recurrence or progression in patients who have the disease or medical condition of interest. | Measured at the onset of treatment of cGvHD |
| Risk | A biomarker that indicates the potential for developing a disease or medical condition who does not currently have clinically apparent disease or the medical condition. | Measured before cGvHD has developed, eg, at engraftment |
Definitions are based on the FDA-NIH Biomarker Working Group Resource224.
Diagnostic biomarkers may assist the clinician in early detection of insidious cGvHD, allowing for early intitiation of therapy or more accurate criteria for enrollment onto clinical trials. Predictive and prognostic biomarkers, usually measured at therapy intiation, may allow for biologic classification of cGvHD and aid in treatment selection most likely to engender a response to cGvHD therapy or a specific therapeutic intervention.
Risk assignment biomarkers may allow determination of whether the patient is at a high, moderate, or low risk of subsequently developing cGvHD and used in the design of preventive or preemptive trials or treatment strategies. With risk algorithms, patients may receive either a preemptive increase or decrease in therapy to avert onset of cGvHD or to decrease therapy to minimize the toxicity of immunosuppressive prophylaxis, respectively. Biomarkers not only of cGvHD, but also of operational immune tolerance, may potentially identify the safest time for a patient to stop immune suppression or predict which patient is likely not to respond to the recommended therapy.
Reports from the 2020 NIH Consensus Development Project on Criteria for Clinical Trials in cGvHD offer a vision for personalized preemptive interventions for cGvHD based on clinical risk factors and biomarkers measured before symptom onset.140,141 As summarized in the report from the Etiology and Prevention Working Group of the 2020 NIH Consensus Development Project,142 the field has long recognized pretransplant clinical risk factors associated with cGvHD, though no risk assessment prognostic systems exist at this time. Progress has been made in identifying candidate biomarkers or biomarker signatures measured at specific time points after transplantation that could identify patients who have a high risk of developing cGvHD. At 3 months after alloHSCT, pediatric and adolescent patients who subsequently developed cGvHD had decreased numbers of CD21low B cells and CD56bright regulatory NK cells in the blood, increased naïve T helper cells and PD1+ naïve T cytotoxic cells, and increased plasma ST2 (IL-33 receptor) and soluble CD13 concentrations.137 At 6 months after alloHSCT, adult patients with low numbers of circulating Tregs had an increased cGvHD risk.126 For such patients, low-dose IL-2 or IL-2 mutant proteins (muteins) with decreased CD122 (IL-2Rb) affinity will favor Treg cells over NK or CD8 T cells and may ameliorate active cGvHD by expanding Treg cells in vivo. Whether the 3-month biomarkers have a causal relationship with cGvHD incidence or severity is unknown but warrants testing. Because GvHD-causing Teffectors are glycolytic, metabolic imaging with nonradioactive glucose isotopes18,119 or radioactive tracers143, 144, 145, 146 may allow noninvasive cGvHD diagnosis, serve as an objective measurement of in situ therapeutic responses,147 and facilitate the selection of patients who are most likely to benefit from metabolic inhibitors. Multidirectional bedside-to-bench and bench-to-bedside approaches will continue to elucidate the biological understanding of cGvHD.
Clinical trial design optimization
To better understand the underlying pathophysiological cGvHD mechanisms, future trials will need to expand the scope of immunological analyses in sufficient subgroups of transplant types and cGvHD clinical presentations.148 As a field, we are receptive to new tools and sample bio-banking for incorporation into clinical studies. The careful, detailed annotation of clinical features at sample collection remains to be of critical importance. Such data should be paired with laboratory and imaging correlates and treatment responses initiated at the time of collection.149 One promising path forward is the continued accrual of prospectively collected clinical and biological data before the initiation of therapy with continued collections as interventions are implemented.150 This approach would allow determination of the clinical utility of the identified markers and guide preclinical evaluation of pathways that incorporate them. Adjusting for clinical factors is critical. As an example, recipient age, potentially associated with the onset of puberty, has a direct effect on immune biomarkers of cGvHD.151
To date, clinical trials have incorporated correlative studies based on either a hypothesized mechanism of the therapeutic intervention or broadly based assays, while omitting evaluation of known biological pathways associated with cGvHD. For blood sampling, the complexity and heterogeneity of cGvHD immunologic mechanisms and clinical factors, confounded by how samples are collected, processed, and analyzed, can explain some of the conflicting findings between clinical research groups. Logistical factors that may have a meaningful impact on such analyses include timing of collection in relation to cGvHD onset, processing, transport and storage of samples, evaluations of whole blood vs Ficoll separated peripheral blood mononuclear cells, as well as the degradation of cytokines and metabolites in plasma before evaluation.152,153 Plasma or serum samples have usually been processed immediately and frozen at the participating center, or processed in a central laboratory after overnight shipping. However, such differences may introduce variability, potentially affecting the quality of the samples. Collection processes that partially fix cells for immune phenotyping or transcriptome evaluation are more expensive but may be necessary to ensure consistency of correlative biology assay results. Plasma may need to be separated and frozen shortly after collection to preserve sample quality, which will add to shipping and storage costs for multicenter studies that typically involve downstream centralized laboratory analyses. Of note, dried blood spot, which is an inexpensive collection option, may be both low-cost and high-yield for certain analyses,154,155 for example, metabolomics. To move this field forward, it is critical that detailed descriptions of sample procurement and processing procedures are reported in publications methods sections.
Collection of samples obtained early in the course of cGvHD before the escalation of therapy138 or before first-line therapy initiation, as proposed by the recent NIH cGvHD Consensus Working Group III report,150 will further advance risk stratification at disease onset unencumbered by therapies, eventually leading to precision therapy. Few prospective cGvHD biology studies have been performedand few studies have included evaluations or sampling of tissue/target organ involvement. One attempt at addressing these concerns was the first137 of the ABLE studies performed by the Pediatric Transplant and Cellular Therapy Consortium, which enrolled patients prospectively from over 25 centers and included adjudication of clinical disease classification.156 Several open consortia studies are collecting samples and clinical data. These include Close Assessment and Testing for cGvHD, CATCH Study (NCT04188912), which collects serial samples of blood, skin and oral biopsies, tears, saliva, and fecal microbiome, starting before HSCT and every 2 months for the first year after alloHSCT. In addition, Predicting the Quality of Response to Specific Treatments in Patients with cGvHD, PQRST Study (#NCT04431479) calls for the collection of blood samples and clinical data before starting treatment for cGvHD after 1 month of therapy along with clinical data collected at 3 and 6 months after alloHSCT, if treatment has changed. Tissue immunohistopathology data emerging from trials which inlcuded pre- and posttargeted intervention organ biopsies should be of great interest (#NCT03640481). Correlative studies recommendations for future clinical trials, include standardized collection times, sample collection methodology, and suggested assays.157 Blood is likely to remain the main material that can be collected serially on trials, although lymphoid and affected organ tissue analyses would likely yield superior interrogation of upfront disease biology and changes as a result of therapies. Thus, animal models, in which target, lymphoid, and blood can be sampled and evaluated serially will continue to be used for elucidating biological responses to therapeutic interventions.
Emerging technologies for in-depth cGvHD biology interrogations in clinical and bench studies
New technologies have emerged that will allow greater insight into underlying biological processes gleaned from preclinical and clinical samples. These include new omics tools, that is, metabolomics directly measured122 or computed by in silico single cell RNAseq data,158 lipidomics, high-parameter (30-50) proteomic analyses by mass cytometry in situ or traditional flow cytometry, combinatorial proteomics (>150 parameter), discovery transcriptomics, such as cellular indexing of transcriptomes and epitopes by sequencing/RNAseq that couples DNA bar-coded antibodies directed against surface proteins with RNAseq), and epigenetic assays, such as assay for transposase-accessible chromatin using sequencing to gauge open chromatin patterns. These approaches may be applied to cell suspensions or whole tissue. For the latter, high-parameter multispectral platforms, such as mass spectrometry, Vectra, and CO-Detection by inDEXing based imaging are now feasible. As proteomics and spatial transcriptomics platforms rapidly evolve to true subcellular definition with transcriptomics, the interrogation of immune networks in tissue should be readily attainable. Single cell T-cell receptor and B-cell receptor sequencing can assess clonotypic donor-, host- and tumor-specific immune responses. Such OMICS technologies can be applied to large animal models, as recently reported for single cell RNAseq of gut-infiltrating donor T cells,159 and as a technique for in vivo T-cell clonal tracking in nonhuman primates to characterize alloreactive T-cell clones identified via mixed lymphocyte reaction in GvHD target organs after alloHSCT.160 Other advances include multiple cell labeling in situ with techniques like multiplexed ion beam imaging by time of flight of metal-tagged antibodies,161 which will be highly informative in preclinical models and in patients. When combined with single cell transcriptomics, this approach could become an especially powerful tool for studying the pathologic activation networks in human T cells.132 Logistics, such as how these data will be acquired and analyzed and financial constraints they will impose, deserve consideration. Nonetheless, as cumulative data sets expand and as understanding of how to best deploy these new technologies grows, there is an opportunity to turn empiricisms into personalized precision medicine.
Preclinical modeling gaps and suggestions for early development of the next generation cGvHD therapies
Although preclinical models with reproducible and highly penetrant multiorgan involvement have yielded insights into cGvHD biological underpinnings,162 the simulation of clinical disease is complicated by numerous variables that can impact the underlying alloimmune processes in patients. These variables include age,151,163, 164, 165, 166 sex,4,165,167,168 obesity,169 metabolism,170 microbiome,116 preceding therapy/conditioning,4,171 primary disease,4,165 antecedent and ongoing infections,165,172, 173, 174 and thymic function,73,175, 176, 177, 178, 179, 180 among others. Although few preclinical studies have been designed to incorporate these key disease initiators and modifiers, adjustments in preclinical mouse modeling can be undertaken before translation or after therapeutic agent/s have been tested, the latter through bedside-to-bench approaches. Moreover, biological assessments of pathway targeting in multiple anatomical sites over time, that is, gastrointestinal, hepatic, and pulmonary chronic GvHD162 should be undertaken in preclinical models.127,162,181 Whether a mechanism is initially identified through clinical studies or generated in preclinical GvHD models, it is best to use preclinical tools to further refine and dissect pertinent biology for successful translation into clinical trials.
Conclusion
New, effective, and well-tolerated targeted therapies for cGvHD have been developed and FDA-approved, but they continue to be used empirically and deployed once the lack of response to systemic corticosteroids and/or calcineurin inhibitors is established. Furthermore, rate of complete and or durable responses are unsatisfactory and choice of therapy for refractory cases remains largerly empiric. There is a gap between clinical manifestations of cGvHD and understanding of biological and molecular features of disease. Closing this gap would allow biological stratification of disease, precise assessment of treatment responses, and will ultimately lead to the development of personalized therapies guided by the detection of the active pathways in cGvHD initiation, maintenance, and progression. Powerful analytical tools and technologies are becoming increasingly available and should be used in cGvHD to decipher in greater depth its biological puzzles. Evaluation of responses by objective laboratory or imaging criteria, and selection of subsequent therapies based on reassessment of disease may be realized. To achieve these goals, cross talk between preclinical and clinical investigators is essential, including the current NIH consensus and other groups that include patient advocates and industry stakeholders. New hybrid collaborative networks may need to be formed for faster and more effective means of propelling novel agents through clinical trials. This effort seeks to maximize an exchange of ideas, opinions, and expertise to continue coordinating clinical development of the next generation of personalized therapies for patients with cGvHD.
Conflict-of-interest disclosure: G.S. receives renumeration for serving on the advisory board of Equillium Incyte, Novartis, and PharmaCyclic. G.R.H. has consulted for Generon Corporation, NapaJen Pharma, iTeos Therapeutics, and Neoleukin Therapeutics, and has received research funding from Compass Therapeutics, Syndax Pharmaceuticals, Applied Molecular Transport, Serplus Technology, Heat Biologics, Laevoroc Oncology, and iTeos Therapeutics. S.J.L. has consulted for Mallinckrodt, Equillium, and Kadmon; has received research funding from Amgen, AstraZeneca, Incyte, Kadmon, Novartis, Pfizer, Syndax, and Takeda; serves on the steering committee for Incyte; and has received drug supply from Janssen. J.R. receives research funding from Amgen, Equillium, Kite/Gilead and Novartis; serves on Data Safety Monitoring Committees for AvroBio and scientific advisory boards for Akron Biotech, Clade Therapeutics, Garuda Therapeutics, LifeVault Bio, Novartis, Rheos Medicines, Talaris Therapeutics, and TScan Therapeutics. S.P. holds a patent on “Biomarkers and assays to detect chronic graft-versus-host disease” (US Patent # 10571478 B2). L.L. holds a patent with WindMiL therapeutics; receives grant/research/clinical trial support from Genentech; and is a consultant/advisory board member for Gilead Sciences, Rubius Therapeutics, Precision Biosciences, and Talaris Therapeutics. P.J.M. receives research funding from AltruBio; renumeration as an adviser to Mallinckrodt, Mesoblast, Rigel, Talaris; renumeration as a member of the Data and Safety Monitoring Board for Pfizer, Pediatric Transplantation and Cellular Therapy Consortium; and has received honoraria from Janssen, Mount Sinai School of Medicine, Therakos, Florida Department of Health, and Deutsche Knochenmarkspenderdatei. S.Z.P. receives research support from the Center for Cancer Research at the National Cancer Institute through the National Institutes of Health Intramural Research Program, including Clinical Research Development Agreements with Celgene, Actelion, Eli Lilly, Pharmacyclics and Kadmon. B.R.B. receives renumeration as an adviser to Magenta Therapeutics, BlueRock Therapeutics, Childrens’ Cancer Research Fund, and KidsFirst Fund, and is a cofounder of Tmunity Therapeutics.
Acknowledgments
Supported in part by National Institutes of Health (NIH) grants P01 HL158505, P01 AI056299, R37 AI34495, R01 HL155114, and R01 HL11879, a CIHR Team grant, a CIHR Foundation grant, a CIHR operating grant, and also by the Center for Cancer Research, National Cancer Institute, NIH.
Dedicated to the memory of John A. Hansen.
Authorship
Contribution: All authors contributed to the writing of this review after B.R.B. received the invitation to submit.
Footnotes
∗S.Z.P., K.R.S., and B.R.B. contributed equally to this study.
References
- 1.Wingard JR, Majhail NS, Brazauskas R, et al. Long-term survival and late deaths after allogeneic hematopoietic cell transplantation. J Clin Oncol. 2011;29(16):2230–2239. doi: 10.1200/JCO.2010.33.7212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bachier CR, Aggarwal SK, Hennegan K, et al. Epidemiology and treatment of chronic graft-versus-host disease post-allogeneic hematopoietic cell transplantation: a US claims analysis. Transplant Cell Ther. 2021;27(6):504.e1–504.e6. doi: 10.1016/j.jtct.2020.12.027. [DOI] [PubMed] [Google Scholar]
- 3.Hill GR, Betts BC, Tkachev V, Kean LS, Blazar BR. Current concepts and advances in graft-versus-host disease immunology. Annu Rev Immunol. 2021;39:19–49. doi: 10.1146/annurev-immunol-102119-073227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeiser R, Blazar BR. Pathophysiology of chronic graft-versus-host disease and therapeutic targets. N Engl J Med. 2017;377(26):2565–2579. doi: 10.1056/NEJMra1703472. [DOI] [PubMed] [Google Scholar]
- 5.Miklos D, Cutler CS, Arora M, et al. Ibrutinib for chronic graft-versus-host disease after failure of prior therapy. Blood. 2017;130(21):2243–2250. doi: 10.1182/blood-2017-07-793786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cutler CS, Lee SJ, Arai S, et al. Belumosudil for chronic graft-versus-host disease after 2 or more prior lines of therapy: the ROCKstar study. Blood. 2021;138(22):2278–2289. doi: 10.1182/blood.2021012021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zeiser R, Polverelli N, Ram R, et al. Ruxolitinib for glucocorticoid-refractory chronic graft-versus-host disease. N Engl J Med. 2021;385(3):228–238. doi: 10.1056/NEJMoa2033122. [DOI] [PubMed] [Google Scholar]
- 8.Jagasia MH, Greinix HT, Arora M, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2014 Diagnosis and Staging Working Group report. Biol Blood Marrow Transplant. 2015;21(3):389–401.e1. doi: 10.1016/j.bbmt.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee SJ, Wolff D, Kitko C, et al. Measuring therapeutic response in chronic graft-versus-host disease. National Institutes of Health consensus development project on criteria for clinical trials in chronic graft-versus-host disease: IV. The 2014 Response Criteria Working Group report. Biol Blood Marrow Transplant. 2015;21(6):984–999. doi: 10.1016/j.bbmt.2015.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pavletic SZ, Martin PJ, Schultz KR, Lee SJ. The future of chronic graft-versus-host disease: introduction to the 2020 National Institutes of Health Consensus Development Project reports. Transplant Cell Ther. 2021;27(6):448–451. doi: 10.1016/j.jtct.2021.02.034. [DOI] [PubMed] [Google Scholar]
- 11.Simonetta F, Alvarez M, Negrin RS. Natural killer cells in graft-versus-host-disease after allogeneic hematopoietic cell transplantation. Front Immunol. 2017;8:465. doi: 10.3389/fimmu.2017.00465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perkey E, Maillard I. New insights into graft-versus-host disease and graft rejection. Annu Rev Pathol. 2018;13:219–245. doi: 10.1146/annurev-pathol-020117-043720. [DOI] [PubMed] [Google Scholar]
- 13.Mohamed FA, Thangavelu G, Rhee SY, et al. Recent metabolic advances for preventing and treating acute and chronic graft versus host disease. Front Immunol. 2021;12:757836. doi: 10.3389/fimmu.2021.757836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mhandire K, Saggu K, Buxbaum NP. Immunometabolic therapeutic targets of graft-versus-host disease (GvHD) Metabolites. 2021;11(11) doi: 10.3390/metabo11110736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Byersdorfer CA, Tkachev V, Opipari AW, et al. Effector T cells require fatty acid metabolism during murine graft-versus-host disease. Blood. 2013;122(18):3230–3237. doi: 10.1182/blood-2013-04-495515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Subburaj D, Ng B, Kariminia A, et al. Metabolomic identification of alpha-ketoglutaric acid elevation in pediatric chronic graft-versus-host disease. Blood. 2022;139(2):287–299. doi: 10.1182/blood.2021013244. [DOI] [PubMed] [Google Scholar]
- 17.Kumari R, Palaniyandi S, Hildebrandt GC. Metabolic reprogramming-a new era how to prevent and treat graft versus host disease after allogeneic hematopoietic stem cell transplantation has begun. Front Pharmacol. 2020;11:588449. doi: 10.3389/fphar.2020.588449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buxbaum NP, Farthing DE, Maglakelidze N, et al. In vivo kinetics and nonradioactive imaging of rapidly proliferating cells in graft-versus-host disease. JCI Insight. 2017;2(12) doi: 10.1172/jci.insight.92851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Beilhack A, Schulz S, Baker J, et al. Alloreactive T-cell trafficking after hematopoietic stem cell transplantation. J Stem Cells Regen Med. 2007;2(1):107. [PubMed] [Google Scholar]
- 20.Schultz KR, Paquet J, Bader S, HayGlass KT. Requirement for B cells in T cell priming to minor histocompatibility antigens and development of graft-versus-host disease. Bone Marrow Transplant. 1995;16(2):289–295. [PubMed] [Google Scholar]
- 21.Ratanatharathorn V, Carson E, Reynolds C, et al. Anti-CD20 chimeric monoclonal antibody treatment of refractory immune-mediated thrombocytopenia in a patient with chronic graft-versus-host disease. Ann Intern Med. 2000;133(4):275–279. doi: 10.7326/0003-4819-133-4-200008150-00011. [DOI] [PubMed] [Google Scholar]
- 22.Ratanatharathorn V, Ayash L, Reynolds C, et al. Treatment of chronic graft-versus-host disease with anti-CD20 chimeric monoclonal antibody. Biol Blood Marrow Transplant. 2003;9(8):505–511. doi: 10.1016/s1083-8791(03)00216-7. [DOI] [PubMed] [Google Scholar]
- 23.Canninga-van Dijk MR, van der Straaten HM, Fijnheer R, Sanders CJ, van den Tweel JG, Verdonck LF. Anti-CD20 monoclonal antibody treatment in 6 patients with therapy-refractory chronic graft-versus-host disease. Blood. 2004;104(8):2603–2606. doi: 10.1182/blood-2004-05-1855. [DOI] [PubMed] [Google Scholar]
- 24.Okamoto M, Okano A, Akamatsu S, et al. Rituximab is effective for steroid-refractory sclerodermatous chronic graft-versus-host disease. Leukemia. 2006;20(1):172–173. doi: 10.1038/sj.leu.2403996. [DOI] [PubMed] [Google Scholar]
- 25.Cutler C, Miklos D, Kim HT, et al. Rituximab for steroid-refractory chronic graft-versus-host disease. Blood. 2006;108(2):756–762. doi: 10.1182/blood-2006-01-0233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Teshima T, Nagafuji K, Henzan H, et al. Rituximab for the treatment of corticosteroid-refractory chronic graft-versus-host disease. Int J Hematol. 2009;90(2):253–260. doi: 10.1007/s12185-009-0370-x. [DOI] [PubMed] [Google Scholar]
- 27.Dubovsky JA, Flynn R, Du J, et al. Ibrutinib treatment ameliorates murine chronic graft-versus-host disease. J Clin Invest. 2014;124(11):4867–4876. doi: 10.1172/JCI75328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jaglowski SM, Blazar BR. How ibrutinib, a B-cell malignancy drug, became an FDA-approved second-line therapy for steroid-resistant chronic GVHD. Blood Adv. 2018;2(15):2012–2019. doi: 10.1182/bloodadvances.2018013060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Forcade E, Paz K, Flynn R, et al. An activated Th17-prone T cell subset involved in chronic graft-versus-host disease sensitive to pharmacological inhibition. JCI Insight. 2017;2(12) doi: 10.1172/jci.insight.92111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gartlan KH, Bommiasamy H, Paz K, et al. A critical role for donor-derived IL-22 in cutaneous chronic GVHD. Am J Transplant. 2018;18(4):810–820. doi: 10.1111/ajt.14513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hill GR, Olver SD, Kuns RD, et al. Stem cell mobilization with G-CSF induces type 17 differentiation and promotes scleroderma. Blood. 2010;116(5):819–828. doi: 10.1182/blood-2009-11-256495. [DOI] [PubMed] [Google Scholar]
- 32.Zanin-Zhorov A, Blazar BR. ROCK2, a critical regulator of immune modulation and fibrosis has emerged as a therapeutic target in chronic graft-versus-host disease. Clin Immunol. 2021;230:108823. doi: 10.1016/j.clim.2021.108823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Nalkurthi C, Schroder WA, Melino M, et al. ROCK2 inhibition attenuates profibrogenic immune cell function to reverse thioacetamide-induced liver fibrosis. JHEP Rep. 2022;4(1):100386. doi: 10.1016/j.jhepr.2021.100386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Flynn R, Paz K, Du J, et al. Targeted Rho-associated kinase 2 inhibition suppresses murine and human chronic GVHD through a Stat3-dependent mechanism. Blood. 2016;127(17):2144–2154. doi: 10.1182/blood-2015-10-678706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Verstovsek S, Kantarjian H, Mesa RA, et al. Safety and efficacy of INCB018424, a JAK1 and JAK2 inhibitor, in myelofibrosis. N Engl J Med. 2010;363(12):1117–1127. doi: 10.1056/NEJMoa1002028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Harrison C, Kiladjian JJ, Al-Ali HK, et al. JAK inhibition with ruxolitinib versus best available therapy for myelofibrosis. N Engl J Med. 2012;366(9):787–798. doi: 10.1056/NEJMoa1110556. [DOI] [PubMed] [Google Scholar]
- 37.Genovese MC, Kremer J, Zamani O, et al. Baricitinib in patients with refractory rheumatoid arthritis. N Engl J Med. 2016;374(13):1243–1252. doi: 10.1056/NEJMoa1507247. [DOI] [PubMed] [Google Scholar]
- 38.Schwartz DM, Kanno Y, Villarino A, Ward M, Gadina M, O'Shea JJ. JAK inhibition as a therapeutic strategy for immune and inflammatory diseases. Nat Rev Drug Discov. 2017;17(1):78. doi: 10.1038/nrd.2017.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spoerl S, Mathew NR, Bscheider M, et al. Activity of therapeutic JAK 1/2 blockade in graft-versus-host disease. Blood. 2014;123(24):3832–3842. doi: 10.1182/blood-2013-12-543736. [DOI] [PubMed] [Google Scholar]
- 40.Carniti C, Gimondi S, Vendramin A, et al. Pharmacologic inhibition of JAK1/JAK2 signaling reduces experimental murine acute GVHD while preserving GVT effects. Clin Cancer Res. 2015;21(16):3740–3749. doi: 10.1158/1078-0432.CCR-14-2758. [DOI] [PubMed] [Google Scholar]
- 41.Choi J, Ziga ED, Ritchey J, et al. IFNgammaR signaling mediates alloreactive T-cell trafficking and GVHD. Blood. 2012;120(19):4093–4103. doi: 10.1182/blood-2012-01-403196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Choi J, Cooper ML, Alahmari B, et al. Pharmacologic blockade of JAK1/JAK2 reduces GvHD and preserves the graft-versus-leukemia effect. PLoS One. 2014;9(10):e109799. doi: 10.1371/journal.pone.0109799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zeiser R, Burchert A, Lengerke C, et al. Ruxolitinib in corticosteroid-refractory graft-versus-host disease after allogeneic stem cell transplantation: a multicenter survey. Leukemia. 2015;29(10):2062–2068. doi: 10.1038/leu.2015.212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jagasia M, Perales MA, Schroeder MA, et al. Ruxolitinib for the treatment of steroid-refractory acute GVHD (REACH1): a multicenter, open-label phase 2 trial. Blood. 2020;135(20):1739–1749. doi: 10.1182/blood.2020004823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jagasia M, Zeiser R, Arbushites M, Delaite P, Gadbaw B, Bubnoff NV. Ruxolitinib for the treatment of patients with steroid-refractory GVHD: an introduction to the REACH trials. Immunotherapy. 2018;10(5):391–402. doi: 10.2217/imt-2017-0156. [DOI] [PubMed] [Google Scholar]
- 46.Zeiser R, Lee SJ. Three US Food and Drug Administration-approved therapies for chronic GVHD. Blood. 2022;139(11):1642–1645. doi: 10.1182/blood.2021014448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Allen JL, Tata PV, Fore MS, et al. Increased BCR responsiveness in B cells from patients with chronic GVHD. Blood. 2014;123(13):2108–2115. doi: 10.1182/blood-2013-10-533562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Flynn R, Allen JL, Luznik L, et al. Targeting Syk-activated B cells in murine and human chronic graft-versus-host disease. Blood. 2015;125(26):4085–4094. doi: 10.1182/blood-2014-08-595470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Saidu NEB, Bonini C, Dickinson A, et al. New approaches for the treatment of chronic graft-versus-host disease: current status and future directions. Front Immunol. 2020;11:578314. doi: 10.3389/fimmu.2020.578314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Poe JC, Jia W, Su H, et al. An aberrant NOTCH2-BCR signaling axis in B cells from patients with chronic GVHD. Blood. 2017;130(19):2131–2145. doi: 10.1182/blood-2017-05-782466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zeiser R, Sarantopoulos S, Blazar BR. B-cell targeting in chronic graft-versus-host disease. Blood. 2018;131(13):1399–1405. doi: 10.1182/blood-2017-11-784017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sarantopoulos S, Ritz J. Aberrant B-cell homeostasis in chronic GVHD. Blood. 2015;125(11):1703–1707. doi: 10.1182/blood-2014-12-567834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sarantopoulos S, Stevenson KE, Kim HT, et al. Altered B-cell homeostasis and excess BAFF in human chronic graft-versus-host disease. Blood. 2009;113(16):3865–3874. doi: 10.1182/blood-2008-09-177840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chin KK, Kim HT, Inyang EA, et al. Ibrutinib in steroid-refractory chronic graft-versus-host disease, a single-center experience. Transplant Cell Ther. 2021;27(12):990.e1–990.e7. doi: 10.1016/j.jtct.2021.08.017. [DOI] [PubMed] [Google Scholar]
- 55.Alexander KA, Flynn R, Lineburg KE, et al. CSF-1-dependant donor-derived macrophages mediate chronic graft-versus-host disease. J Clin Invest. 2014;124(10):4266–4280. doi: 10.1172/JCI75935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hume DA, MacDonald KP. Therapeutic applications of macrophage colony-stimulating factor-1 (CSF-1) and antagonists of CSF-1 receptor (CSF-1R) signaling. Blood. 2012;119(8):1810–1820. doi: 10.1182/blood-2011-09-379214. [DOI] [PubMed] [Google Scholar]
- 57.MacDonald KP, Palmer JS, Cronau S, et al. An antibody against the colony-stimulating factor 1 receptor depletes the resident subset of monocytes and tissue- and tumor-associated macrophages but does not inhibit inflammation. Blood. 2010;116(19):3955–3963. doi: 10.1182/blood-2010-02-266296. [DOI] [PubMed] [Google Scholar]
- 58.Lee SJ, Arora M, Defilipp Z, et al. Safety, tolerability, and efficacy of axatilimab, a CSF-1R humanized antibody, for chronic graft-versus-host disease after 2 or more lines of systemic treatment. Blood. 2021;138(Supplement 1):263. [Google Scholar]
- 59.Jones SC, Murphy GF, Korngold R. Post-hematopoietic cell transplantation control of graft-versus-host disease by donor CD425 T cells to allow an effective graft-versus-leukemia response. Biol Blood Marrow Transplant. 2003;9(4):243–256. doi: 10.1053/bbmt.2003.50027. [DOI] [PubMed] [Google Scholar]
- 60.Edinger M, Hoffmann P, Ermann J, et al. CD4+CD25+ regulatory T cells preserve graft-versus-tumor activity while inhibiting graft-versus-host disease after bone marrow transplantation. Nat Med. 2003;9(9):1144–1150. doi: 10.1038/nm915. [DOI] [PubMed] [Google Scholar]
- 61.Di Ianni M, Falzetti F, Carotti A, et al. Tregs prevent GVHD and promote immune reconstitution in HLA-haploidentical transplantation. Blood. 2011;117(14):3921–3928. doi: 10.1182/blood-2010-10-311894. [DOI] [PubMed] [Google Scholar]
- 62.Beres AJ, Drobyski WR. The role of regulatory T cells in the biology of graft versus host disease. Front Immunol. 2013;4:163. doi: 10.3389/fimmu.2013.00163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Koreth J, Matsuoka K, Kim HT, et al. Interleukin-2 and regulatory T cells in graft-versus-host disease. N Engl J Med. 2011;365(22):2055–2066. doi: 10.1056/NEJMoa1108188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Matsuoka K, Koreth J, Kim HT, et al. Low-dose interleukin-2 therapy restores regulatory T cell homeostasis in patients with chronic graft-versus-host disease. Sci Transl Med. 2013;5(179) doi: 10.1126/scitranslmed.3005265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Whangbo JS, Kim HT, Mirkovic N, et al. Dose-escalated interleukin-2 therapy for refractory chronic graft-versus-host disease in adults and children. Blood Adv. 2019;3(17):2550–2561. doi: 10.1182/bloodadvances.2019000631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Blazar BR, MacDonald KPA, Hill GR. Immune regulatory cell infusion for graft-versus-host disease prevention and therapy. Blood. 2018;131(24):2651–2660. doi: 10.1182/blood-2017-11-785865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hirai T, Ramos TL, Lin PY, et al. Selective expansion of regulatory T cells using an orthogonal IL-2/IL-2 receptor system facilitates transplantation tolerance. J Clin Invest. 2021;131(8) doi: 10.1172/JCI139991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Riley JL, June CH, Blazar BR. Human T regulatory cell therapy: take a billion or so and call me in the morning. Immunity. 2009;30(5):656–665. doi: 10.1016/j.immuni.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hoffmann P, Ermann J, Edinger M, Fathman CG, Strober S. Donor-type CD4(+)CD25(+) regulatory T cells suppress lethal acute graft-versus-host disease after allogeneic bone marrow transplantation. J Exp Med. 2002;196(3):389–399. doi: 10.1084/jem.20020399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Taylor PA, Lees CJ, Blazar BR. The infusion of ex vivo activated and expanded CD4(+)CD25(+) immune regulatory cells inhibits graft-versus-host disease lethality. Blood. 2002;99(10):3493–3499. doi: 10.1182/blood.v99.10.3493. [DOI] [PubMed] [Google Scholar]
- 71.Young KJ, Yang L, Phillips MJ, Zhang L. Donor-lymphocyte infusion induces transplantation tolerance by activating systemic and graft-infiltrating double-negative regulatory T cells. Blood. 2002;100(9):3408–3414. doi: 10.1182/blood-2002-01-0235. [DOI] [PubMed] [Google Scholar]
- 72.Trzonkowski P, Bieniaszewska M, Juscinska J, et al. First-in-man clinical results of the treatment of patients with graft versus host disease with human ex vivo expanded CD4+CD25+CD127- T regulatory cells. Clin Immunol. 2009;133(1):22–26. doi: 10.1016/j.clim.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 73.Wu T, Young JS, Johnston H, et al. Thymic damage, impaired negative selection, and development of chronic graft-versus-host disease caused by donor CD4+ and CD8+ T cells. J Immunol. 2013;191(1):488–499. doi: 10.4049/jimmunol.1300657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Miura Y, Thoburn CJ, Bright EC, et al. Association of Foxp3 regulatory gene expression with graft-versus-host disease. Blood. 2004;104(7):2187–2193. doi: 10.1182/blood-2004-03-1040. [DOI] [PubMed] [Google Scholar]
- 75.Zorn E, Kim HT, Lee SJ, et al. Reduced frequency of FOXP3+ CD4+CD25+ regulatory T cells in patients with chronic graft-versus-host disease. Blood. 2005;106(8):2903–2911. doi: 10.1182/blood-2005-03-1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McDonald-Hyman C, Flynn R, Panoskaltsis-Mortari A, et al. Therapeutic regulatory T-cell adoptive transfer ameliorates established murine chronic GVHD in a CXCR5-dependent manner. Blood. 2016;128(7):1013–1017. doi: 10.1182/blood-2016-05-715896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Samarasinghe S, Clesham K, Iacobelli S, et al. Impact of T-cell depletion strategies on outcomes following hematopoietic stem cell transplantation for idiopathic aplastic anemia: a study on behalf of the European blood and marrow transplant severe aplastic anemia working party. Am J Hematol. 2019;94(1):80–86. doi: 10.1002/ajh.25314. [DOI] [PubMed] [Google Scholar]
- 78.Naeije L, Kariminia A, Abdossamadi S, et al. Anti-thymocyte globulin prophylaxis induces a decrease in naive Th cells to inhibit the onset of chronic graft-versus-host disease: results from the Canadian Bone Marrow Transplant Group (CBMTG) 0801 study. Biol Blood Marrow Transplant. 2020;26(3):438–444. doi: 10.1016/j.bbmt.2019.11.015. [DOI] [PubMed] [Google Scholar]
- 79.Bleakley M, Sehgal A, Seropian S, et al. Naive T-cell depletion to prevent chronic graft-versus-host disease. J Clin Oncol. 2022;40(11):1174–1185. doi: 10.1200/JCO.21.01755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Luznik L, O'Donnell PV, Symons HJ, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transplant. 2008;14(6):641–650. doi: 10.1016/j.bbmt.2008.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kanakry CG, Tsai HL, Bolanos-Meade J, et al. Single-agent GVHD prophylaxis with posttransplantation cyclophosphamide after myeloablative, HLA-matched BMT for AML, ALL, and MDS. Blood. 2014;124(25):3817–3827. doi: 10.1182/blood-2014-07-587477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kanakry CG, O'Donnell PV, Furlong T, et al. Multi-institutional study of post-transplantation cyclophosphamide as single-agent graft-versus-host disease prophylaxis after allogeneic bone marrow transplantation using myeloablative busulfan and fludarabine conditioning. J Clin Oncol. 2014;32(31):3497–3505. doi: 10.1200/JCO.2013.54.0625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Luznik L, Bolanos-Meade J, Zahurak M, et al. High-dose cyclophosphamide as single-agent, short-course prophylaxis of graft-versus-host disease. Blood. 2010;115(16):3224–3230. doi: 10.1182/blood-2009-11-251595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Nunes NS, Kanakry CG. Mechanisms of graft-versus-host disease prevention by post-transplantation cyclophosphamide: an evolving understanding. Front Immunol. 2019;10:2668. doi: 10.3389/fimmu.2019.02668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Wachsmuth LP, Patterson MT, Eckhaus MA, Venzon DJ, Gress RE, Kanakry CG. Post-transplantation cyclophosphamide prevents graft-versus-host disease by inducing alloreactive T cell dysfunction and suppression. J Clin Invest. 2019;129(6):2357–2373. doi: 10.1172/JCI124218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ikegawa S, Meguri Y, Kondo T, et al. PTCy ameliorates GVHD by restoring regulatory and effector T-cell homeostasis in recipients with PD-1 blockade. Blood Adv. 2019;3(23):4081–4094. doi: 10.1182/bloodadvances.2019000134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kanakry CG, Ganguly S, Zahurak M, et al. Aldehyde dehydrogenase expression drives human regulatory T cell resistance to posttransplantation cyclophosphamide. Sci Transl Med. 2013;5(211):211ra157. doi: 10.1126/scitranslmed.3006960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.McCurdy SR, Radojcic V, Tsai HL, et al. Signatures of GVHD and relapse after posttransplant cyclophosphamide revealed by immune profiling and machine learning. Blood. 2022;139(4):608–623. doi: 10.1182/blood.2021013054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Kariminia A, Ivison S, Ng B, et al. CD56(bright) natural killer regulatory cells in filgrastim primed donor blood or marrow products regulate chronic graft-versus-host disease: the Canadian Blood and Marrow Transplant Group randomized 0601 study results. Haematologica. 2017;102(11):1936–1946. doi: 10.3324/haematol.2017.170928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Waller EK, Logan BR, Fei M, et al. Kinetics of immune cell reconstitution predict survival in allogeneic bone marrow and G-CSF-mobilized stem cell transplantation. Blood Adv. 2019;3(15):2250–2263. doi: 10.1182/bloodadvances.2018029892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Chen YB, Le-Rademacher J, Brazauskas R, et al. Plerixafor alone for the mobilization and transplantation of HLA-matched sibling donor hematopoietic stem cells. Blood Adv. 2019;3(6):875–883. doi: 10.1182/bloodadvances.2018027599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wong PPC, Kariminia A, Jones D, et al. Plerixafor effectively mobilizes CD56(bright) NK cells in blood, providing an allograft predicted to protect against GVHD. Blood. 2018;131(25):2863–2866. doi: 10.1182/blood-2018-03-836700. [DOI] [PubMed] [Google Scholar]
- 93.Schroeder MA, Rettig MP, Lopez S, et al. Mobilization of allogeneic peripheral blood stem cell donors with intravenous plerixafor mobilizes a unique graft. Blood. 2017;129(19):2680–2692. doi: 10.1182/blood-2016-09-739722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Lundqvist A, Smith AL, Takahashi Y, et al. Differences in the phenotype, cytokine gene expression profiles, and in vivo alloreactivity of T cells mobilized with plerixafor compared with G-CSF. J Immunol. 2013;191(12):6241–6249. doi: 10.4049/jimmunol.1301148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bejanyan N, Brunstein CG, Cao Q, et al. Delayed immune reconstitution after allogeneic transplantation increases the risks of mortality and chronic GVHD. Blood Adv. 2018;2(8):909–922. doi: 10.1182/bloodadvances.2017014464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Du J, Paz K, Flynn R, et al. Pirfenidone ameliorates murine chronic GVHD through inhibition of macrophage infiltration and TGF-beta production. Blood. 2017;129(18):2570–2580. doi: 10.1182/blood-2017-01-758854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Yamakawa T, Ohigashi H, Hashimoto D, et al. Vitamin A-coupled liposomes containing siRNA against HSP47 ameliorate skin fibrosis in chronic graft-versus-host disease. Blood. 2018;131(13):1476–1485. doi: 10.1182/blood-2017-04-779934. [DOI] [PubMed] [Google Scholar]
- 98.Ohigashi H, Hashimoto D, Hayase E, et al. Ocular instillation of vitamin A-coupled liposomes containing HSP47 siRNA ameliorates dry eye syndrome in chronic GVHD. Blood Adv. 2019;3(7):1003–1010. doi: 10.1182/bloodadvances.2018028431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Srinivasan M, Flynn R, Price A, et al. Donor B-cell alloantibody deposition and germinal center formation are required for the development of murine chronic GVHD and bronchiolitis obliterans. Blood. 2012;119(6):1570–1580. doi: 10.1182/blood-2011-07-364414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Ogawa Y, Razzaque MS, Kameyama K, et al. Role of heat shock protein 47, a collagen-binding chaperone, in lacrimal gland pathology in patients with cGVHD. Invest Ophthalmol Vis Sci. 2007;48(3):1079–1086. doi: 10.1167/iovs.06-0601. [DOI] [PubMed] [Google Scholar]
- 101.Matthaiou EI, Sharifi H, O'Donnell C, et al. The safety and tolerability of pirfenidone for bronchiolitis obliterans syndrome after hematopoietic cell transplant (STOP-BOS) trial. Bone Marrow Transplant. 2022;57(8):1319–1326. doi: 10.1038/s41409-022-01716-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Blazar BR, Taylor PA, Linsley PS, Vallera DA. In vivo blockade of CD28/CTLA4: B7/BB1 interaction with CTLA4-Ig reduces lethal murine graft-versus-host disease across the major histocompatibility complex barrier in mice. Blood. 1994;83(12):3815–3825. [PubMed] [Google Scholar]
- 103.Yu C, Linsley P, Seidel K, et al. Cytotoxic T lymphocyte antigen 4-immunoglobulin fusion protein combined with methotrexate/cyclosporine as graft-versus-host disease prevention in a canine dog leukocyte antigen-nonidentical marrow transplant model. Transplantation. 2000;69(3):450–454. doi: 10.1097/00007890-200002150-00027. [DOI] [PubMed] [Google Scholar]
- 104.Miller WP, Srinivasan S, Panoskaltsis-Mortari A, et al. GVHD after haploidentical transplantation: a novel, MHC-defined rhesus macaque model identifies CD28- CD8+ T cells as a reservoir of breakthrough T-cell proliferation during costimulation blockade and sirolimus-based immunosuppression. Blood. 2010;116(24):5403–5418. doi: 10.1182/blood-2010-06-289272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Tkachev V, Furlan SN, Watkins B, et al. Combined OX40L and mTOR blockade controls effector T cell activation while preserving Treg reconstitution after transplant. Sci Transl Med. 2017;9(408) doi: 10.1126/scitranslmed.aan3085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Watkins BK, Tkachev V, Furlan SN, et al. CD28 blockade controls T cell activation to prevent graft-versus-host disease in primates. J Clin Invest. 2018;128(9):3991–4007. doi: 10.1172/JCI98793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Watkins B, Qayed M, McCracken C, et al. Phase II trial of costimulation blockade with abatacept for prevention of acute GVHD. J Clin Oncol. 2021;39(17):1865–1877. doi: 10.1200/JCO.20.01086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Nahas MR, Soiffer RJ, Kim HT, et al. Phase 1 clinical trial evaluating abatacept in patients with steroid-refractory chronic graft-versus-host disease. Blood. 2018;131(25):2836–2845. doi: 10.1182/blood-2017-05-780239. [DOI] [PubMed] [Google Scholar]
- 109.Socie G, Kean LS, Zeiser R, Blazar BR. Insights from integrating clinical and preclinical studies advance understanding of graft-versus-host disease. J Clin Invest. 2021;131(12) doi: 10.1172/JCI149296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Rafei H, Jenq RR. Microbiome-intestine cross talk during acute graft-versus-host disease. Blood. 2020;136(4):401–409. doi: 10.1182/blood.2019000950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mathewson ND, Jenq R, Mathew AV, et al. Gut microbiome-derived metabolites modulate intestinal epithelial cell damage and mitigate graft-versus-host disease. Nat Immunol. 2016;17(5):505–513. doi: 10.1038/ni.3400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jenq RR, Ubeda C, Taur Y, et al. Regulation of intestinal inflammation by microbiota following allogeneic bone marrow transplantation. J Exp Med. 2012;209(5):903–911. doi: 10.1084/jem.20112408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Jenq RR, Taur Y, Devlin SM, et al. Intestinal blautia is associated with reduced death from graft-versus-host disease. Biol Blood Marrow Transplant. 2015;21(8):1373–1383. doi: 10.1016/j.bbmt.2015.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Taur Y, Jenq RR, Perales MA, et al. The effects of intestinal tract bacterial diversity on mortality following allogeneic hematopoietic stem cell transplantation. Blood. 2014;124(7):1174–1182. doi: 10.1182/blood-2014-02-554725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Stein-Thoeringer CK, Nichols KB, Lazrak A, et al. Lactose drives Enterococcus expansion to promote graft-versus-host disease. Science. 2019;366(6469):1143–1149. doi: 10.1126/science.aax3760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Shono Y, Docampo MD, Peled JU, et al. Increased GVHD-related mortality with broad-spectrum antibiotic use after allogeneic hematopoietic stem cell transplantation in human patients and mice. Sci Transl Med. 2016;8(339) doi: 10.1126/scitranslmed.aaf2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Markey KA, Schluter J, Gomes ALC, et al. The microbe-derived short-chain fatty acids butyrate and propionate are associated with protection from chronic GVHD. Blood. 2020;136(1):130–136. doi: 10.1182/blood.2019003369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Andermann TM, Rezvani A, Bhatt AS. Microbiota manipulation with prebiotics and probiotics in patients undergoing stem cell transplantation. Curr Hematol Malig Rep. 2016;11(1):19–28. doi: 10.1007/s11899-016-0302-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Assmann JC, Farthing DE, Saito K, et al. Glycolytic metabolism of pathogenic T cells enables early detection of GVHD by 13C-MRI. Blood. 2021;137(1):126–137. doi: 10.1182/blood.2020005770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Brown RA, Byersdorfer CA. Metabolic pathways in alloreactive T cells. Front Immunol. 2020;11:1517. doi: 10.3389/fimmu.2020.01517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Nguyen HD, Chatterjee S, Haarberg KM, et al. Metabolic reprogramming of alloantigen-activated T cells after hematopoietic cell transplantation. J Clin Invest. 2016;126(4):1337–1352. doi: 10.1172/JCI82587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Michonneau D, Latis E, Curis E, et al. Metabolomics analysis of human acute graft-versus-host disease reveals changes in host and microbiota-derived metabolites. Nat Commun. 2019;10(1):5695. doi: 10.1038/s41467-019-13498-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Tijaro-Ovalle NM, Karantanos T, Wang HT, Boussiotis VA. Metabolic targets for improvement of allogeneic hematopoietic stem cell transplantation and graft-vs.-host disease. Front Immunol. 2019;10:295. doi: 10.3389/fimmu.2019.00295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Nguyen HD, Kuril S, Bastian D, Yu XZ. T-cell metabolism in hematopoietic cell transplantation. Front Immunol. 2018;9:176. doi: 10.3389/fimmu.2018.00176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Watanabe S, Ogawa S, Hara Y, Tanabe K, Toma H, Abe R. Expression level of costimulatory receptor ICOS is critical for determining the polarization of helper T cell function. Transpl Immunol. 2006;15(4):255–263. doi: 10.1016/j.trim.2006.01.002. [DOI] [PubMed] [Google Scholar]
- 126.Zhang M, Wu Y, Bastian D, et al. Inducible T-cell co-stimulator impacts chronic graft-versus-host disease by regulating both pathogenic and regulatory T cells. Front Immunol. 2018;9:1461. doi: 10.3389/fimmu.2018.01461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Graves SS, Parker MH, Stone D, et al. Anti-inducible costimulator monoclonal antibody treatment of canine chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2018;24(1):50–54. doi: 10.1016/j.bbmt.2017.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Flynn R, Du J, Veenstra RG, et al. Increased T follicular helper cells and germinal center B cells are required for cGVHD and bronchiolitis obliterans. Blood. 2014;123(25):3988–3998. doi: 10.1182/blood-2014-03-562231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Radojcic V, Paz K, Chung J, et al. Notch signaling mediated by Delta-like ligands 1 and 4 controls the pathogenesis of chronic GVHD in mice. Blood. 2018;132(20):2188–2200. doi: 10.1182/blood-2018-03-841155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Cooke KR, Luznik L, Sarantopoulos S, et al. The biology of chronic graft-versus-host disease: a task force report from the National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2017;23(2):211–234. doi: 10.1016/j.bbmt.2016.09.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Gandelman JS, Byrne MT, Mistry AM, et al. Machine learning reveals chronic graft-versus-host disease phenotypes and stratifies survival after stem cell transplant for hematologic malignancies. Haematologica. 2019;104(1):189–196. doi: 10.3324/haematol.2018.193441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Dubouchet L, Todorov H, Seurinck R, et al. Operational tolerance after hematopoietic stem cell transplantation is characterized by distinct transcriptional, phenotypic, and metabolic signatures. Sci Transl Med. 2022;14(633) doi: 10.1126/scitranslmed.abg3083. [DOI] [PubMed] [Google Scholar]
- 133.Paczesny S, Krijanovski OI, Braun TM, et al. A biomarker panel for acute graft-versus-host disease. Blood. 2009;113(2):273–278. doi: 10.1182/blood-2008-07-167098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Srinagesh HK, Ozbek U, Kapoor U, et al. The MAGIC algorithm probability is a validated response biomarker of treatment of acute graft-versus-host disease. Blood Adv. 2019;3(23):4034–4042. doi: 10.1182/bloodadvances.2019000791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Major-Monfried H, Renteria AS, Pawarode A, et al. MAGIC biomarkers predict long-term outcomes for steroid-resistant acute GVHD. Blood. 2018;131(25):2846–2855. doi: 10.1182/blood-2018-01-822957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Hartwell MJ, Ozbek U, Holler E, et al. An early-biomarker algorithm predicts lethal graft-versus-host disease and survival. JCI Insight. 2017;2(3) doi: 10.1172/jci.insight.89798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Schultz KR, Kariminia A, Ng B, et al. Immune profile differences between chronic GVHD and late acute GVHD: results of the ABLE/PBMTC 1202 studies. Blood. 2020;135(15):1287–1298. doi: 10.1182/blood.2019003186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Giesen N, Schwarzbich MA, Dischinger K, et al. CXCL9 predicts severity at the onset of chronic graft-versus-host disease. Transplantation. 2020;104(11):2354–2359. doi: 10.1097/TP.0000000000003108. [DOI] [PubMed] [Google Scholar]
- 139.Yu J, Storer BE, Kushekhar K, et al. Biomarker panel for chronic graft-versus-host disease. J Clin Oncol. 2016;34(22):2583–2590. doi: 10.1200/JCO.2015.65.9615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Kitko CL, Pidala J, Schoemans HM, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: IIa. The 2020 Clinical Implementation and Early Diagnosis Working Group Report. Transplant Cell Ther. 2021;27(7):545–557. doi: 10.1016/j.jtct.2021.03.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Pidala J, Kitko C, Lee SJ, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: IIb. The 2020 Preemptive Therapy Working Group Report. Transplant Cell Ther. 2021;27(8):632–641. doi: 10.1016/j.jtct.2021.03.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Williams KM, Inamoto Y, Im A, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: I. The 2020 Etiology and Prevention Working Group Report. Transplant Cell Ther. 2021;27(6):452–466. doi: 10.1016/j.jtct.2021.02.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Bodet-Milin C, Lacombe M, Malard F, et al. 18F-FDG PET/CT for the assessment of gastrointestinal GVHD: results of a pilot study. Bone Marrow Transplant. 2014;49(1):131–137. doi: 10.1038/bmt.2013.144. [DOI] [PubMed] [Google Scholar]
- 144.Dejanovic D, Amtoft A, Loft A. 18 F-FDG PET/CT in extensive graft-versus-host disease of the gastrointestinal tract following autologous stem cell transplantation. Diagnostics. 2018;8(4) doi: 10.3390/diagnostics8040072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Roll W, Schindler P, Masthoff M, et al. 18F-FDG-PET-MRI for the assessment of acute intestinal graft-versus-host-disease (GvHD) BMC Cancer. 2021;21(1):1015. doi: 10.1186/s12885-021-08748-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Stelljes M, Hermann S, Albring J, et al. Clinical molecular imaging in intestinal graft-versus-host disease: mapping of disease activity, prediction, and monitoring of treatment efficiency by positron emission tomography. Blood. 2008;111(5):2909–2918. doi: 10.1182/blood-2007-10-119164. [DOI] [PubMed] [Google Scholar]
- 147.Woitek R, Gallagher FA. The use of hyperpolarised 13C-MRI in clinical body imaging to probe cancer metabolism. Br J Cancer. 2021;124(7):1187–1198. doi: 10.1038/s41416-020-01224-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zouali H, Lemasson J, Calugareanu A, et al. RNA sequencing of chronic GVHD skin lesions defines shared and unique inflammatory pathways characterizing lichen planus and morphea. Blood Adv. 2022;6(9):2805–2811. doi: 10.1182/bloodadvances.2021004707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Wolff D, Greinix H, Lee SJ, et al. Biomarkers in chronic graft-versus-host disease: quo vadis? Bone Marrow Transplant. 2018;53(7):832–837. doi: 10.1038/s41409-018-0092-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.DeFilipp Z, Couriel DR, Lazaryan A, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: III. The 2020 Treatment of Chronic GVHD Report. Transplant Cell Ther. 2021;27(9):729–737. doi: 10.1016/j.jtct.2021.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Cuvelier GDE, Li A, Drissler S, et al. Age related differences in the biology of chronic graft-versus-host disease after hematopoietic stem cell transplantation. Front Immunol. 2020;11:571884. doi: 10.3389/fimmu.2020.571884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Cruickshank-Quinn C, Zheng LK, Quinn K, Bowler R, Reisdorph R, Reisdorph N. Impact of blood collection tubes and sample handling time on serum and plasma metabolome and lipidome. Metabolites. 2018;8(4):88. doi: 10.3390/metabo8040088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Gonzalez-Dominguez R, Gonzalez-Dominguez A, Sayago A, Fernandez-Recamales A. Recommendations and best practices for standardizing the pre-analytical processing of blood and urine samples in metabolomics. Metabolites. 2020;10(6):229. doi: 10.3390/metabo10060229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Li K, Naviaux JC, Monk JM, Wang L, Naviaux RK. Improved dried blood spot-based metabolomics: a targeted, broad-spectrum, single-injection method. Metabolites. 2020;10(3):82. doi: 10.3390/metabo10030082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Tobin NH, Murphy A, Li F, et al. Comparison of dried blood spot and plasma sampling for untargeted metabolomics. Metabolomics. 2021;17(7):62. doi: 10.1007/s11306-021-01813-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Cuvelier GDE, Nemecek ER, Wahlstrom JT, et al. Benefits and challenges with diagnosing chronic and late acute GVHD in children using the NIH consensus criteria. Blood. 2019;134(3):304–316. doi: 10.1182/blood.2019000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Paczesny S, Hakim FT, Pidala J, et al. National Institutes of Health Consensus Development Project on criteria for clinical trials in chronic graft-versus-host disease: III. The 2014 Biomarker Working Group Report. Biol Blood Marrow Transplant. 2015;21(5):780–792. doi: 10.1016/j.bbmt.2015.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Zhang H, Madi A, Yosef N, et al. An IL-27-driven transcriptional network identifies regulators of IL-10 expression across T helper cell subsets. Cell Rep. 2020;33(8):108433. doi: 10.1016/j.celrep.2020.108433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Tkachev V, Kaminski J, Potter EL, et al. Spatiotemporal single-cell profiling reveals that invasive and tissue-resident memory donor CD8+ T cells drive gastrointestinal acute graft-versus-host disease. Sci Transl Med. 2021;13(576):eabc0227. doi: 10.1126/scitranslmed.abc0227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Gerdemann U, Fleming RA, Kaminski J, et al. Identification and tracking of alloreactive T cell clones in Rhesus Macaques through the RM-scTCR-seq platform. Front Immunol. 2021;12:804932. doi: 10.3389/fimmu.2021.804932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Keren L, Bosse M, Thompson S, et al. MIBI-TOF: a multiplexed imaging platform relates cellular phenotypes and tissue structure. Sci Adv. 2019;5(10) doi: 10.1126/sciadv.aax5851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Zeiser R, Blazar BR. Preclinical models of acute and chronic graft-versus-host disease: how predictive are they for a successful clinical translation? Blood. 2016;127(25):3117–3126. doi: 10.1182/blood-2016-02-699082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Baird K, Cooke K, Schultz KR. Chronic graft-versus-host disease (GVHD) in children. Pediatr Clin North Am. 2010;57(1):297–322. doi: 10.1016/j.pcl.2009.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Qayed M, Wang T, Hemmer MT, et al. Influence of age on acute and chronic GVHD in children undergoing HLA-identical sibling bone marrow transplantation for acute leukemia: implications for prophylaxis. Biol Blood Marrow Transplant. 2018;24(3):521–528. doi: 10.1016/j.bbmt.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Flowers ME, Inamoto Y, Carpenter PA, et al. Comparative analysis of risk factors for acute graft-versus-host disease and for chronic graft-versus-host disease according to National Institutes of Health consensus criteria. Blood. 2011;117(11):3214–3219. doi: 10.1182/blood-2010-08-302109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Friedrich P, Guerra-Garcia P, Stetson A, Duncan C, Lehmann L. Young female donors do not increase the risk of graft-versus-host disease or impact overall outcomes in pediatric HLA-matched sibling hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2018;24(1):96–102. doi: 10.1016/j.bbmt.2017.09.014. [DOI] [PubMed] [Google Scholar]
- 167.Nannya Y, Kataoka K, Hangaishi A, Imai Y, Takahashi T, Kurokawa M. The negative impact of female donor/male recipient combination in allogeneic hematopoietic stem cell transplantation depends on disease risk. Transpl Int. 2011;24(5):469–476. doi: 10.1111/j.1432-2277.2011.01229.x. [DOI] [PubMed] [Google Scholar]
- 168.Nakasone H, Remberger M, Tian L, et al. Risks and benefits of sex-mismatched hematopoietic cell transplantation differ according to conditioning strategy. Haematologica. 2015;100(11):1477–1485. doi: 10.3324/haematol.2015.125294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Khuat LT, Le CT, Pai CS, et al. Obesity induces gut microbiota alterations and augments acute graft-versus-host disease after allogeneic stem cell transplantation. Sci Transl Med. 2020;12(571):eaay7713. doi: 10.1126/scitranslmed.aay7713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Gebremedhin E, Behrendt CE, Nakamura R, Parker P, Salehian B. Severe hyperglycemia immediately after allogeneic hematopoietic stem-cell transplantation is predictive of acute graft-versus-host disease. Inflammation. 2013;36(1):177–185. doi: 10.1007/s10753-012-9533-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Afram G, Simon JAP, Remberger M, et al. Reduced intensity conditioning increases risk of severe cGVHD: identification of risk factors for cGVHD in a multicenter setting. Med Oncol. 2018;35(6):79. doi: 10.1007/s12032-018-1127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Hahn T, McCarthy PL, Jr., Zhang MJ, et al. Risk factors for acute graft-versus-host disease after human leukocyte antigen-identical sibling transplants for adults with leukemia. J Clin Oncol. 2008;26(35):5728–5734. doi: 10.1200/JCO.2008.17.6545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Jacobsen N, Badsberg JH, Lonnqvist B, et al. Graft-versus-leukaemia activity associated with CMV-seropositive donor, post-transplant CMV infection, young donor age and chronic graft-versus-host disease in bone marrow allograft recipients. The Nordic Bone Marrow Transplantation Group. Bone Marrow Transplant. 1990;5(6):413–418. [PubMed] [Google Scholar]
- 174.Styczynski J, Tridello G, Gil L, et al. Impact of donor Epstein-Barr virus serostatus on the incidence of graft-versus-host disease in patients with acute leukemia after hematopoietic stem-cell transplantation: a study from the Acute Leukemia and Infectious Diseases Working Parties of the European Society for Blood and Marrow Transplantation. J Clin Oncol. 2016;34(19):2212–2220. doi: 10.1200/JCO.2015.64.2405. [DOI] [PubMed] [Google Scholar]
- 175.Krenger W, Hollander GA. The thymus in GVHD pathophysiology. Best Pract Res Clin Haematol. 2008;21(2):119–128. doi: 10.1016/j.beha.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 176.Alawam AS, Cosway EJ, James KD, et al. Failures in thymus medulla regeneration during immune recovery cause tolerance loss and prime recipients for auto-GVHD. J Exp Med. 2022;219(2) doi: 10.1084/jem.20211239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Sakoda Y, Hashimoto D, Asakura S, et al. Donor-derived thymic-dependent T cells cause chronic graft-versus-host disease. Blood. 2007;109(4):1756–1764. doi: 10.1182/blood-2006-08-042853. [DOI] [PubMed] [Google Scholar]
- 178.Moutuou MM, Page G, Zaid I, Lesage S, Guimond M. Restoring T cell homeostasis after allogeneic stem cell transplantation; principal limitations and future challenges. Front Immunol. 2018;9:1237. doi: 10.3389/fimmu.2018.01237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Williams KM, Gress RE. Immune reconstitution and implications for immunotherapy following haematopoietic stem cell transplantation. Best Pract Res Clin Haematol. 2008;21(3):579–596. doi: 10.1016/j.beha.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.van den Brink MR, Moore E, Ferrara JL, Burakoff SJ. Graft-versus-host-disease-associated thymic damage results in the appearance of T cell clones with anti-host reactivity. Transplantation. 2000;69(3):446–449. doi: 10.1097/00007890-200002150-00026. [DOI] [PubMed] [Google Scholar]
- 181.Graves SS, Parker MH, Storb R. Animal models for preclinical development of allogeneic hematopoietic cell transplantation. ILAR J. 2018;59(3):263–275. doi: 10.1093/ilar/ily006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Stastny P, Stembridge VA, Ziff M. Homologous Disease in the Adult Rat, a Model for Autoimmune Disease. I. General Features adn Cutaneous Lesions. J Exp Med. 1963;118(4):635–648. doi: 10.1084/jem.118.4.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Hamilton BL, Parkman R. Acute and chronic graft-versus-host disease induced by minor histocompatibility antigens in mice. Transplantation. 1983;36(2):150–155. doi: 10.1097/00007890-198308000-00008. [DOI] [PubMed] [Google Scholar]
- 184.Claman HN, Jaffee BD. Minor antigen graft-versus-host reactions revealed in irradiated spleen and popliteal lymph node assays. Transplantation. 1984;38(4):392–395. doi: 10.1097/00007890-198410000-00015. [DOI] [PubMed] [Google Scholar]
- 185.Claman HN, Jaffee BD, Huff JC, Clark RA. Chronic graft-versus-host disease as a model for scleroderma. II. Mast cell depletion with deposition of immunoglobulins in the skin and fibrosis. Cell Immunol. 1985;94(1):73–84. doi: 10.1016/0008-8749(85)90086-3. [DOI] [PubMed] [Google Scholar]
- 186.Via CS, Sharrow SO, Shearer GM. Role of cytotoxic T lymphocytes in the prevention of lupus-like disease occurring in a murine model of graft-vs-host disease. J Immunol. 1987;139(6):1840–1849. [PubMed] [Google Scholar]
- 187.Miklos DB, Kim HT, Miller KH, et al. Antibody responses to H-Y minor histocompatibility antigens correlate with chronic graft-versus-host disease and disease remission. Blood. 2005;105(7):2973–2978. doi: 10.1182/blood-2004-09-3660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Zhang C, Todorov I, Zhang Z, et al. Donor CD4+ T and B cells in transplants induce chronic graft-versus-host disease with autoimmune manifestations. Blood. 2006;107(7):2993–3001. doi: 10.1182/blood-2005-09-3623. [DOI] [PubMed] [Google Scholar]
- 189.Sarantopoulos S, Stevenson KE, Kim HT, et al. High levels of B-cell activating factor in patients with active chronic graft-versus-host disease. Clin Cancer Res. 2007;13(20):6107–6114. doi: 10.1158/1078-0432.CCR-07-1290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Fujii H, Cuvelier G, She K, et al. Biomarkers in newly diagnosed pediatric-extensive chronic graft-versus-host disease: a report from the Children's Oncology Group. Blood. 2008;111(6):3276–3285. doi: 10.1182/blood-2007-08-106286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.She K, Gilman AL, Aslanian S, et al. Altered Toll-like receptor 9 responses in circulating B cells at the onset of extensive chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2007;13(4):386–397. doi: 10.1016/j.bbmt.2006.12.441. [DOI] [PubMed] [Google Scholar]
- 192.Kuzmina Z, Greinix HT, Weigl R, et al. Significant differences in B-cell subpopulations characterize patients with chronic graft-versus-host disease-associated dysgammaglobulinemia. Blood. 2011;117(7):2265–2274. doi: 10.1182/blood-2010-07-295766. [DOI] [PubMed] [Google Scholar]
- 193.Herrera AF, Kim HT, Bindra B, et al. A phase II study of bortezomib plus prednisone for initial therapy of chronic graft-versus-host disease. Biol Blood Marrow Transplant. 2014;20(11):1737–1743. doi: 10.1016/j.bbmt.2014.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Poe JC, Jia W, Di Paolo JA, et al. SYK inhibitor entospletinib prevents ocular and skin GVHD in mice. JCI Insight. 2018;3(19) doi: 10.1172/jci.insight.122430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Rappaport H, Khalil A, Halle-Pannenko O, Pritchard L, Dantchev D, Mathe G. Histopathologic sequence of events in adult mice undergoing lethal graft-versus-host reaction developed across H-2 and/or non-H-2 histocompatibility barriers. Am J Pathol. 1979;96(1):121–142. [PMC free article] [PubMed] [Google Scholar]
- 196.Claman HN. On scleroderma. Mast cells, endothelial cells, and fibroblasts. JAMA. 1989;262(9):1206–1209. doi: 10.1001/jama.262.9.1206. [DOI] [PubMed] [Google Scholar]
- 197.Crowley MT, Costello PS, Fitzer-Attas CJ, et al. A critical role for Syk in signal transduction and phagocytosis mediated by Fcgamma receptors on macrophages. J Exp Med. 1997;186(7):1027–1039. doi: 10.1084/jem.186.7.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Horwood NJ, Mahon T, McDaid JP, et al. Bruton's tyrosine kinase is required for lipopolysaccharide-induced tumor necrosis factor alpha production. J Exp Med. 2003;197(12):1603–1611. doi: 10.1084/jem.20021845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Yarilina A, Xu K, Chan C, Ivashkiv LB. Regulation of inflammatory responses in tumor necrosis factor-activated and rheumatoid arthritis synovial macrophages by JAK inhibitors. Arthritis Rheum. 2012;64(12):3856–3866. doi: 10.1002/art.37691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Ryu DB, Lim JY, Kim TW, et al. Preclinical evaluation of JAK1/2 inhibition by ruxolitinib in a murine model of chronic graft-versus-host disease. Exp Hematol. 2021;98:36–46.e2. doi: 10.1016/j.exphem.2021.03.004. [DOI] [PubMed] [Google Scholar]
- 201.Huarte E, Peel M, Juvekar A, et al. Ruxolitinib, a JAK1/JAK2 selective inhibitor, ameliorates acute and chronic steroid-refractory GvHD mouse models. Immunotherapy. 2021;13(12):977–987. doi: 10.2217/imt-2021-0013. [DOI] [PubMed] [Google Scholar]
- 202.Jagasia M, Lazaryan A, Bachier CR, et al. ROCK2 inhibition with belumosudil (KD025) for the treatment of chronic graft-versus-host disease. J Clin Oncol. 2021;39(17):1888–1898. doi: 10.1200/JCO.20.02754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Hilgert I. The involvement of activated specific suppressor T cells in maintenance of transplantation tolerance. Immunol Rev. 1979;46:27–53. doi: 10.1111/j.1600-065x.1979.tb00283.x. [DOI] [PubMed] [Google Scholar]
- 204.Hall BM, Pearce NW, Gurley KE, Dorsch SE. Specific unresponsiveness in rats with prolonged cardiac allograft survival after treatment with cyclosporine. III. Further characterization of the CD4+ suppressor cell and its mechanisms of action. J Exp Med. 1990;171(1):141–157. doi: 10.1084/jem.171.1.141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Sakaguchi S, Sakaguchi N, Asano M, Itoh M, Toda M. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases. J Immunol. 1995;155(3):1151–1164. [PubMed] [Google Scholar]
- 206.Jonuleit H, Schmitt E, Stassen M, Tuettenberg A, Knop J, Enk AH. Identification and functional characterization of human CD4(+)CD25(+) T cells with regulatory properties isolated from peripheral blood. J Exp Med. 2001;193(11):1285–1294. doi: 10.1084/jem.193.11.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Baecher-Allan C, Brown JA, Freeman GJ, Hafler DA. CD4+CD25high regulatory cells in human peripheral blood. J Immunol. 2001;167(3):1245–1253. doi: 10.4049/jimmunol.167.3.1245. [DOI] [PubMed] [Google Scholar]
- 208.Dieckmann D, Plottner H, Berchtold S, Berger T, Schuler G. Ex vivo isolation and characterization of CD4(+)CD25(+) T cells with regulatory properties from human blood. J Exp Med. 2001;193(11):1303–1310. doi: 10.1084/jem.193.11.1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol. 2003;4(4):330–336. doi: 10.1038/ni904. [DOI] [PubMed] [Google Scholar]
- 210.Rieger K, Loddenkemper C, Maul J, et al. Mucosal FOXP3+ regulatory T cells are numerically deficient in acute and chronic GvHD. Blood. 2006;107(4):1717–1723. doi: 10.1182/blood-2005-06-2529. [DOI] [PubMed] [Google Scholar]
- 211.Albert MH, Liu Y, Anasetti C, Yu XZ. Antigen-dependent suppression of alloresponses by Foxp3-induced regulatory T cells in transplantation. Eur J Immunol. 2005;35(9):2598–2607. doi: 10.1002/eji.200526077. [DOI] [PubMed] [Google Scholar]
- 212.Giorgini A, Noble A. Blockade of chronic graft-versus-host disease by alloantigen-induced CD4+CD25+Foxp3+ regulatory T cells in nonlymphopenic hosts. J Leukoc Biol. 2007;82(5):1053–1061. doi: 10.1189/jlb.0407227. [DOI] [PubMed] [Google Scholar]
- 213.Zhao D, Zhang C, Yi T, et al. In vivo-activated CD103+CD4+ regulatory T cells ameliorate ongoing chronic graft-versus-host disease. Blood. 2008;112(5):2129–2138. doi: 10.1182/blood-2008-02-140277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Zorn E, Nelson EA, Mohseni M, et al. IL-2 regulates FOXP3 expression in human CD4+CD25+ regulatory T cells through a STAT-dependent mechanism and induces the expansion of these cells in vivo. Blood. 2006;108(5):1571–1579. doi: 10.1182/blood-2006-02-004747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Chen X, Vodanovic-Jankovic S, Johnson B, Keller M, Komorowski R, Drobyski WR. Absence of regulatory T-cell control of TH1 and TH17 cells is responsible for the autoimmune-mediated pathology in chronic graft-versus-host disease. Blood. 2007;110(10):3804–3813. doi: 10.1182/blood-2007-05-091074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Biagi E, Di Biaso I, Leoni V, et al. Extracorporeal photochemotherapy is accompanied by increasing levels of circulating CD4+CD25+GITR+Foxp3+CD62L+ functional regulatory T-cells in patients with graft-versus-host disease. Transplantation. 2007;84(1):31–39. doi: 10.1097/01.tp.0000267785.52567.9c. [DOI] [PubMed] [Google Scholar]
- 217.Di Biaso I, Di Maio L, Bugarin C, et al. Regulatory T cells and extracorporeal photochemotherapy: correlation with clinical response and decreased frequency of proinflammatory T cells. Transplantation. 2009;87(9):1422–1425. doi: 10.1097/TP.0b013e3181a27a5d. [DOI] [PubMed] [Google Scholar]
- 218.Pillai AB, George TI, Dutt S, Strober S. Host natural killer T cells induce an interleukin-4-dependent expansion of donor CD4+CD25+Foxp3+ T regulatory cells that protects against graft-versus-host disease. Blood. 2009;113(18):4458–4467. doi: 10.1182/blood-2008-06-165506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Veerapathran A, Pidala J, Beato F, et al. Human regulatory T cells against minor histocompatibility antigens: ex vivo expansion for prevention of graft-versus-host disease. Blood. 2013;122(13):2251–2261. doi: 10.1182/blood-2013-03-492397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Kennedy-Nasser AA, Ku S, Castillo-Caro P, et al. Ultra low-dose IL-2 for GVHD prophylaxis after allogeneic hematopoietic stem cell transplantation mediates expansion of regulatory T cells without diminishing antiviral and antileukemic activity. Clin Cancer Res. 2014;20(8):2215–2225. doi: 10.1158/1078-0432.CCR-13-3205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Theil A, Tuve S, Oelschlagel U, et al. Adoptive transfer of allogeneic regulatory T cells into patients with chronic graft-versus-host disease. Cytotherapy. 2015;17(4):473–486. doi: 10.1016/j.jcyt.2014.11.005. [DOI] [PubMed] [Google Scholar]
- 222.Landwehr-Kenzel S, Muller-Jensen L, Kuehl JS, et al. Adoptive transfer of ex vivo expanded regulatory T cells improves immune cell engraftment and therapy-refractory chronic GvHD. Mol Ther. 2022;30(6):2298–2314. doi: 10.1016/j.ymthe.2022.02.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Bolivar-Wagers S, Loschi ML, Jin S, et al. Murine CAR19 Tregs suppress acute graft-versus-host disease and maintain graft-versus-tumor responses. JCI Insight. 2022;7(17):e160674. doi: 10.1172/jci.insight.160674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Califf RM. Biomarker definitions and their applications. Exp Biol Med (Maywood) 2018;243(3):213–221. doi: 10.1177/1535370217750088. [DOI] [PMC free article] [PubMed] [Google Scholar]